GINGIVA THE MIRROR OF PERIODONTAL HEALTH CONTENTS q




- Slides: 171
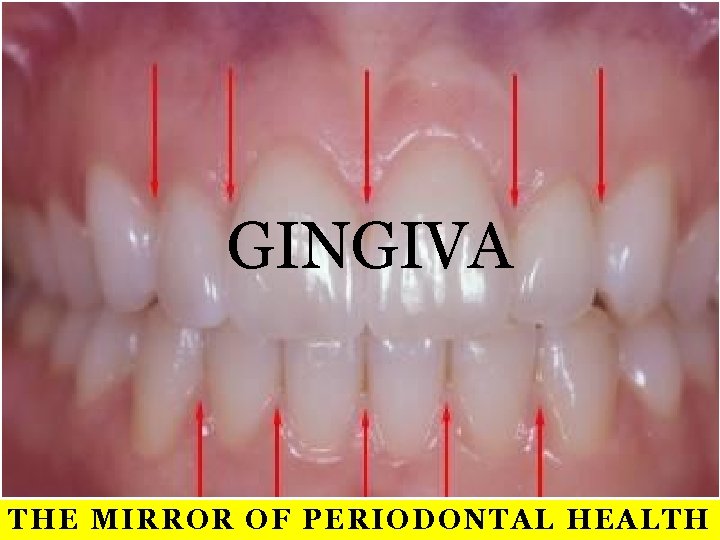
GINGIVA THE MIRROR OF PERIODONTAL HEALTH
CONTENTS q Introduction q Macroscopic features q Microscopic features q q q q Gingival epithelium Oral epithelium Sulcular epithelium Junctional epithelium Renewal of gingival epithelium Cuticular structures Gingival crevicular fluid Gingival connective tissue Gingival fibres Blood supply, nerve supply and lymphatics Correlation of clinical & microscopic features Age changes
INTRODUCTION ORAL MUCOSA
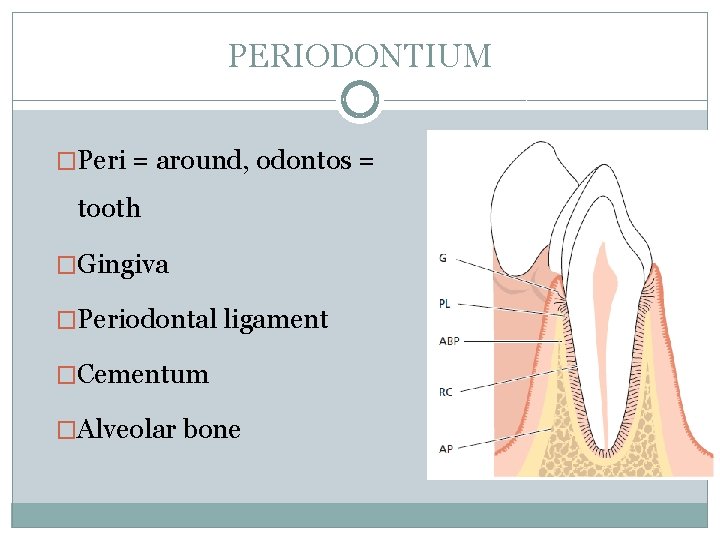
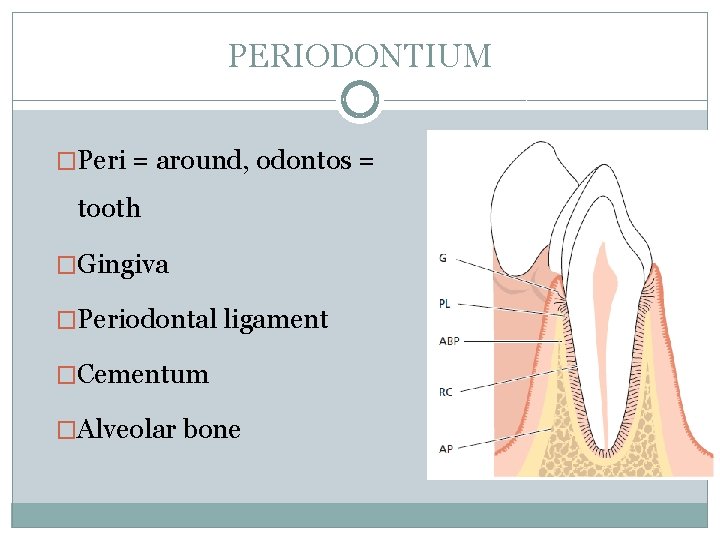
PERIODONTIUM �Peri = around, odontos = tooth �Gingiva �Periodontal ligament �Cementum �Alveolar bone
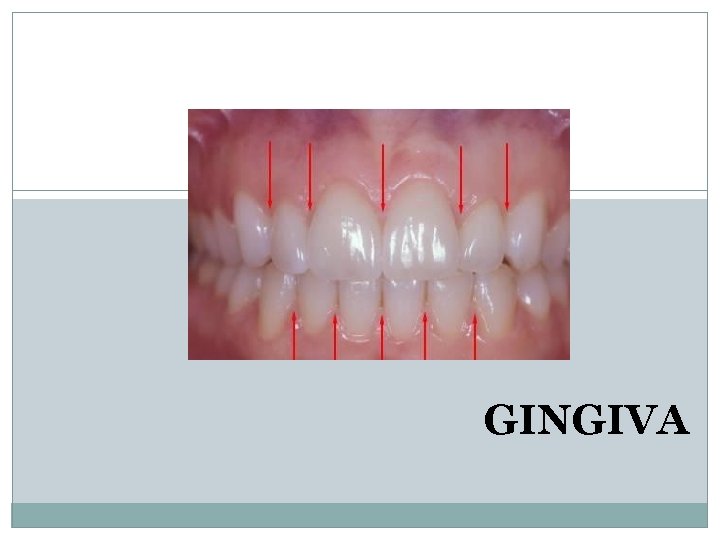
GINGIVA Gingiva is the part of the oral mucosa that covers the alveolar processes of the jaws & surrounds the necks of the teeth Carranza
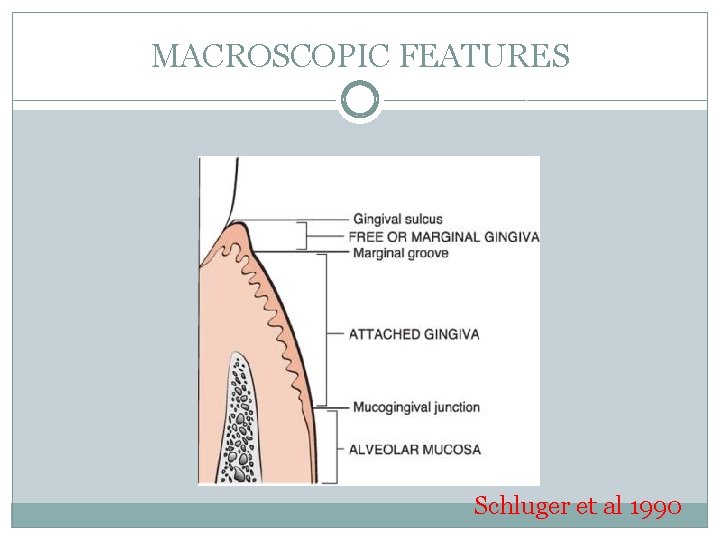
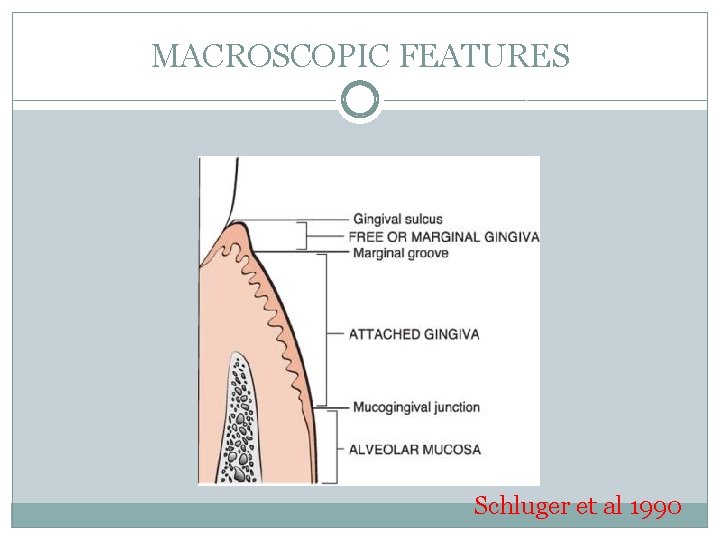
MACROSCOPIC FEATURES Schluger et al 1990
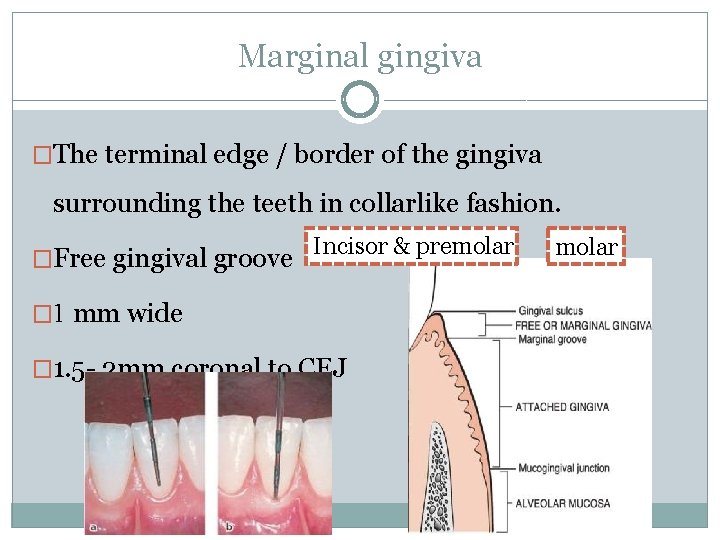
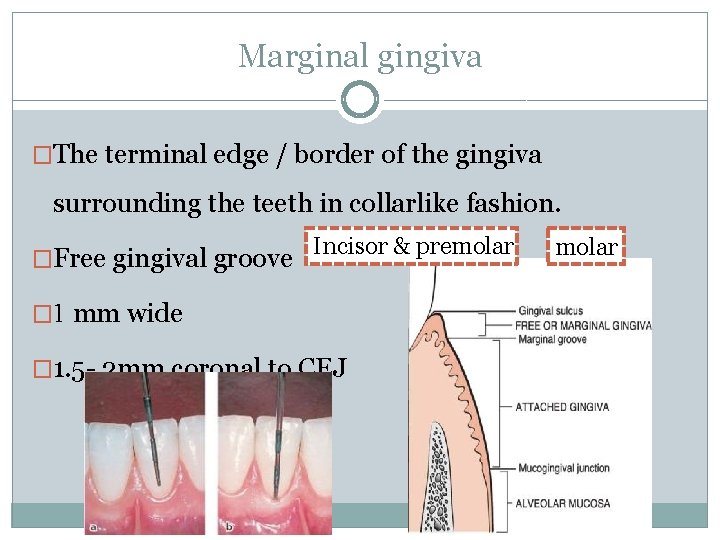
Marginal gingiva �The terminal edge / border of the gingiva surrounding the teeth in collarlike fashion. �Free gingival groove Incisor & premolar � 1 mm wide � 1. 5 - 2 mm coronal to CEJ molar
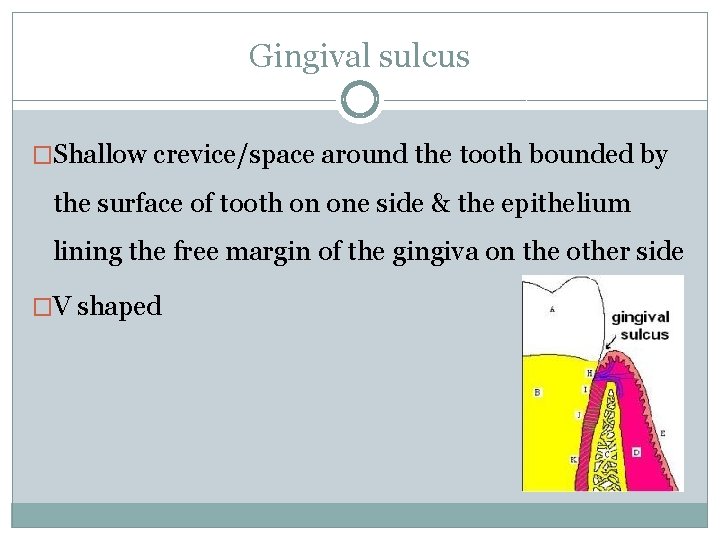
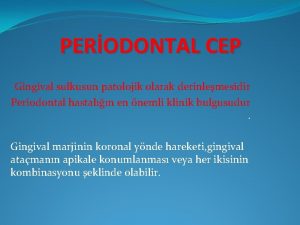
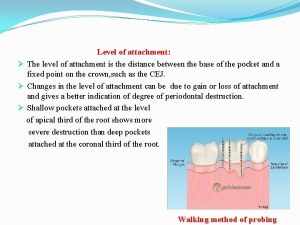
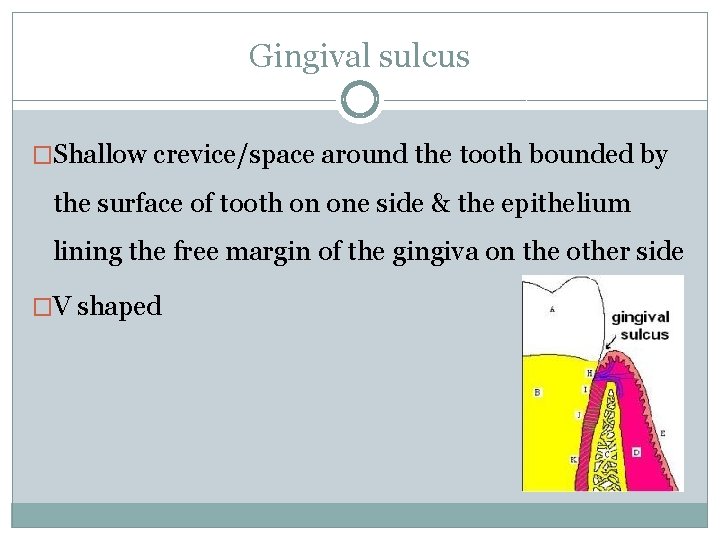
Gingival sulcus �Shallow crevice/space around the tooth bounded by the surface of tooth on one side & the epithelium lining the free margin of the gingiva on the other side �V shaped
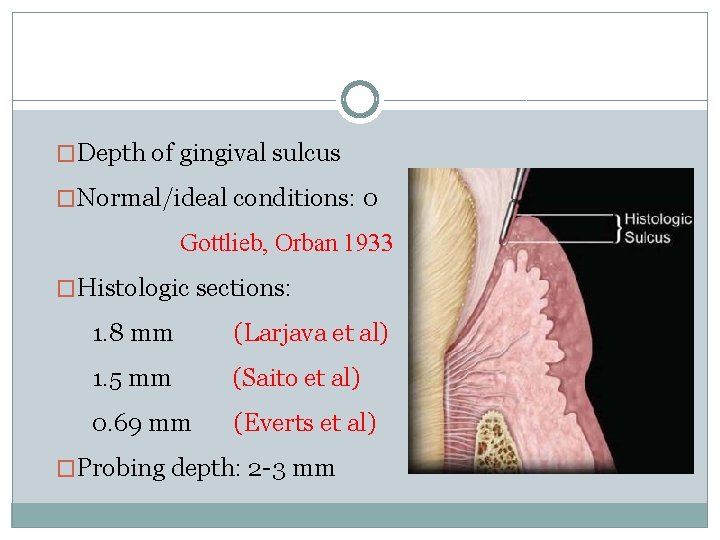
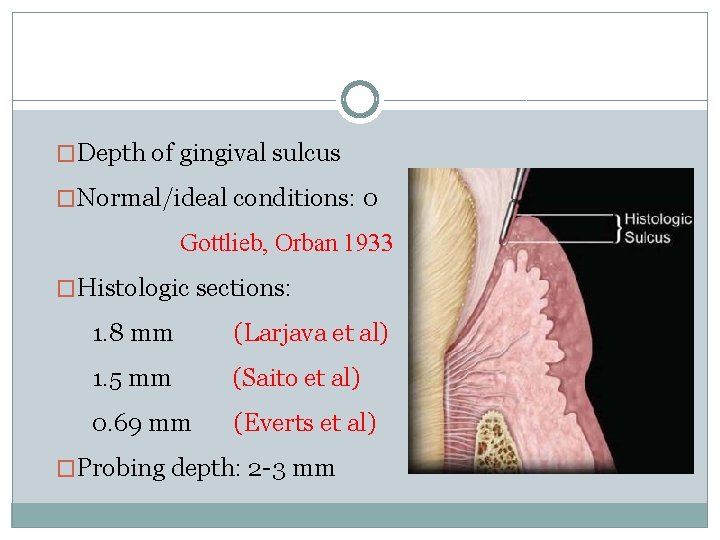
�Depth of gingival sulcus �Normal/ideal conditions: 0 Gottlieb, Orban 1933 �Histologic sections: 1. 8 mm (Larjava et al) 1. 5 mm (Saito et al) 0. 69 mm (Everts et al) �Probing depth: 2 -3 mm
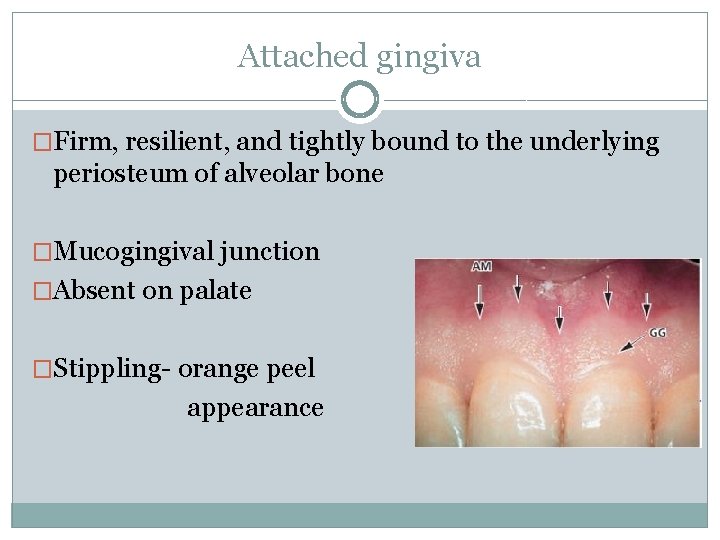
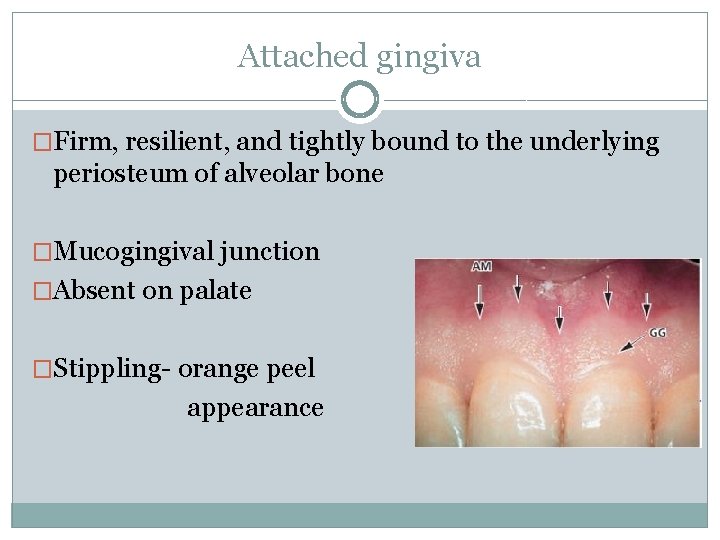
Attached gingiva �Firm, resilient, and tightly bound to the underlying periosteum of alveolar bone �Mucogingival junction �Absent on palate �Stippling- orange peel appearance
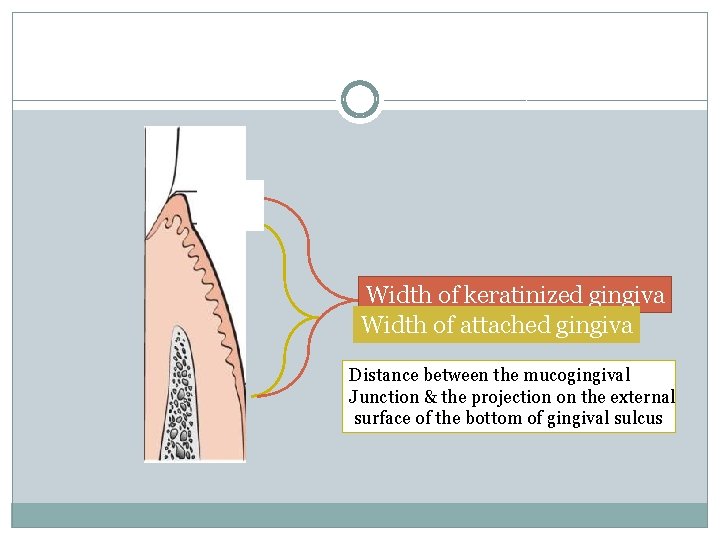
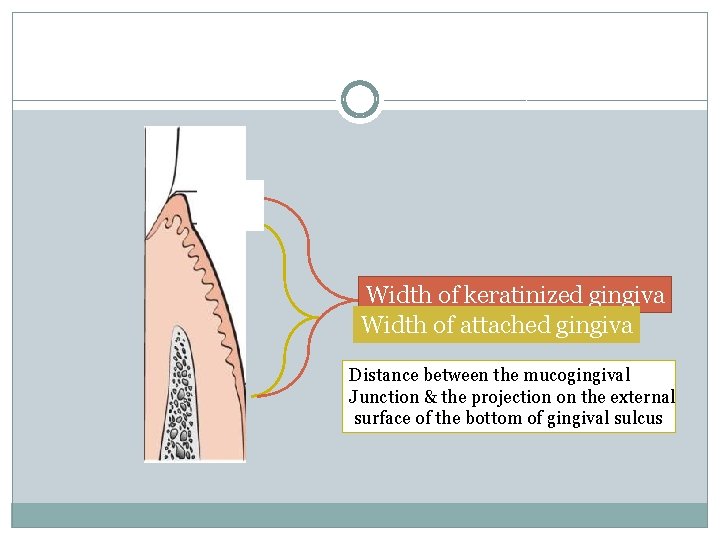
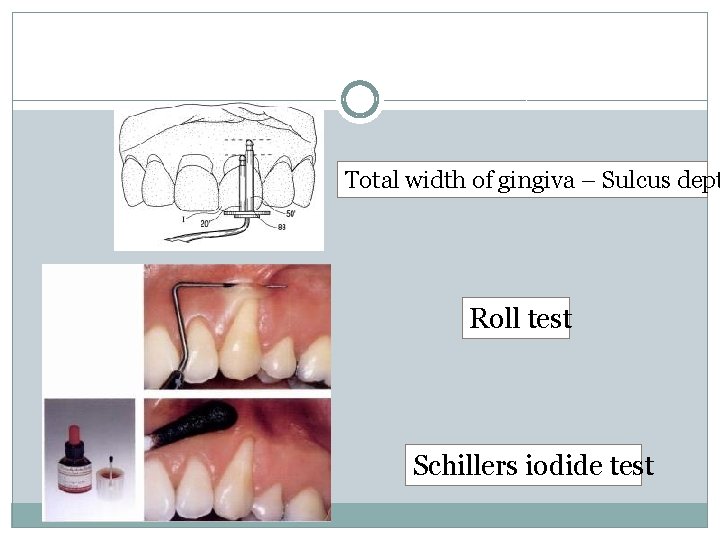
Width of keratinized gingiva Width of attached gingiva Distance between the mucogingival Junction & the projection on the external surface of the bottom of gingival sulcus
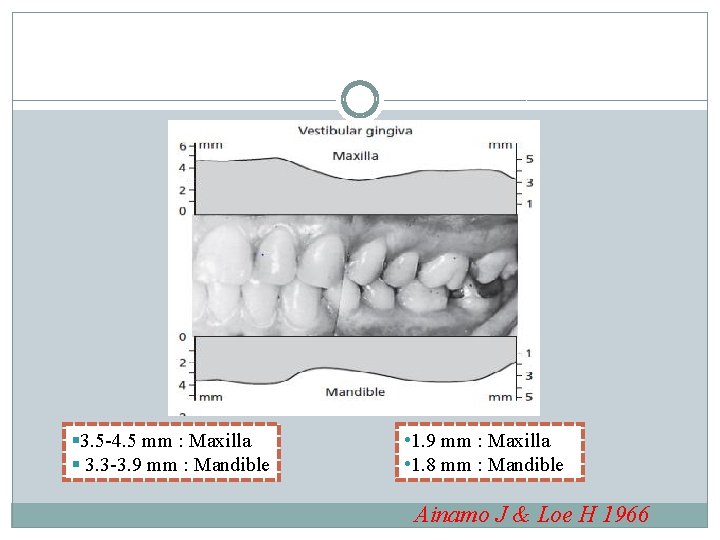
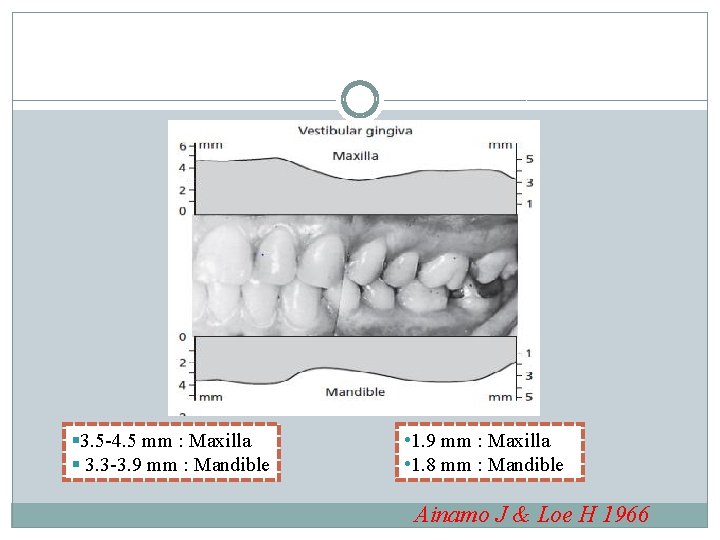
§ 3. 5 -4. 5 mm : Maxilla § 3. 3 -3. 9 mm : Mandible • 1. 9 mm : Maxilla • 1. 8 mm : Mandible Ainamo J & Loe H 1966
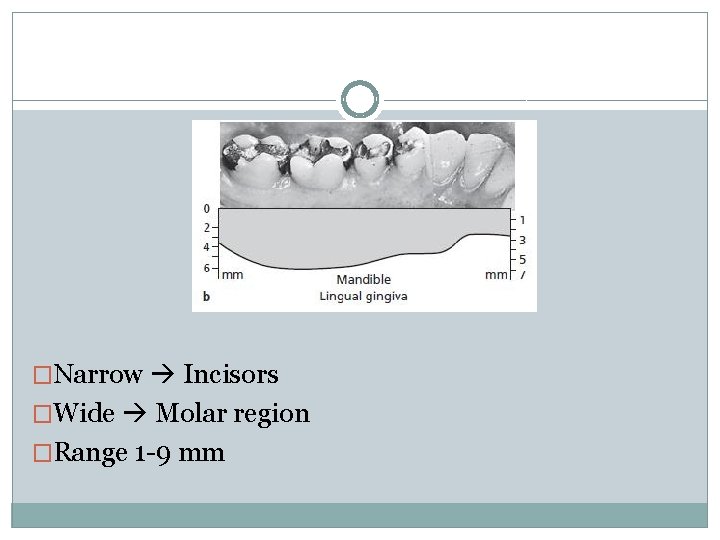
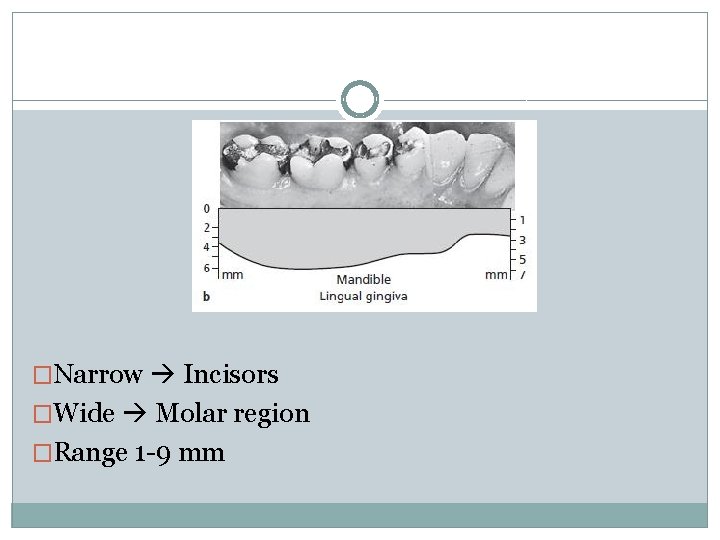
�Narrow Incisors �Wide Molar region �Range 1 -9 mm
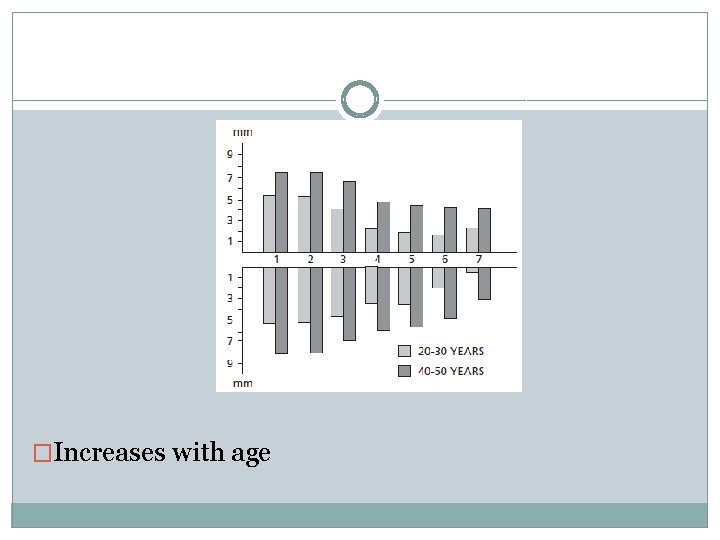
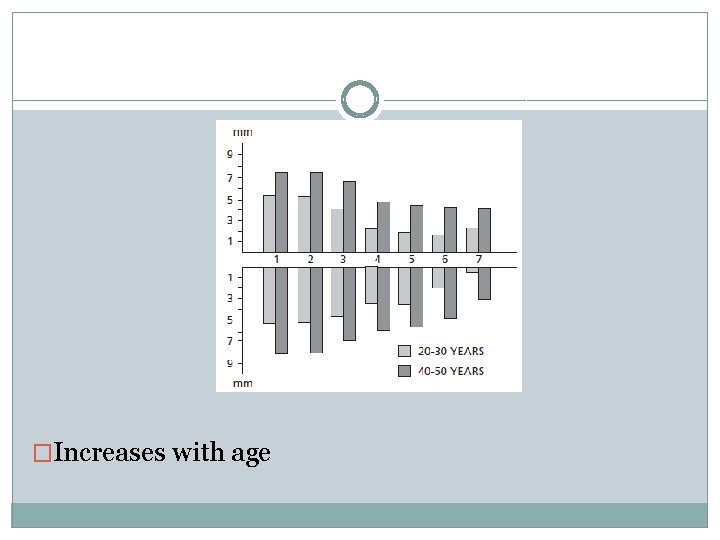
�Increases with age
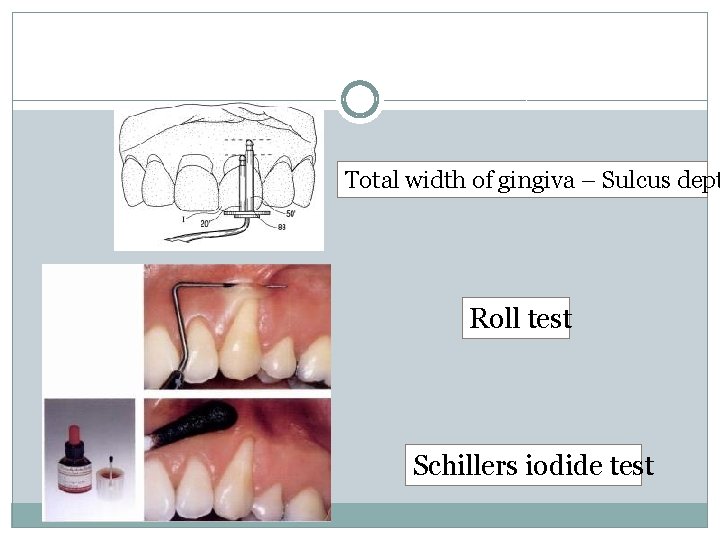
Total width of gingiva – Sulcus dept Roll test Schillers iodide test
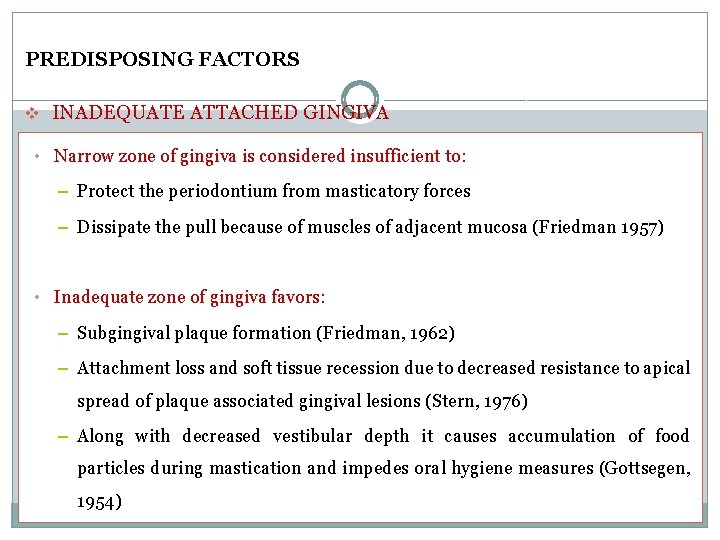
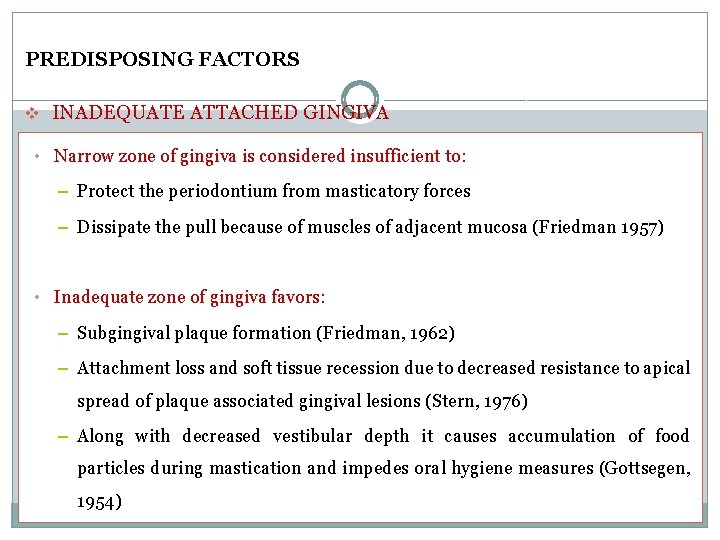
PREDISPOSING FACTORS v INADEQUATE ATTACHED GINGIVA • Narrow zone of gingiva is considered insufficient to: – Protect the periodontium from masticatory forces – Dissipate the pull because of muscles of adjacent mucosa (Friedman 1957) • Inadequate zone of gingiva favors: – Subgingival plaque formation (Friedman, 1962) – Attachment loss and soft tissue recession due to decreased resistance to apical spread of plaque associated gingival lesions (Stern, 1976) – Along with decreased vestibular depth it causes accumulation of food particles during mastication and impedes oral hygiene measures (Gottsegen, 1954)
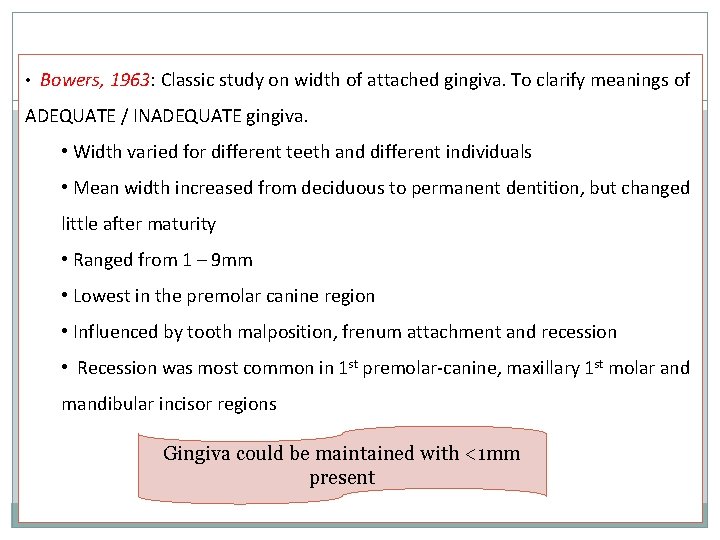
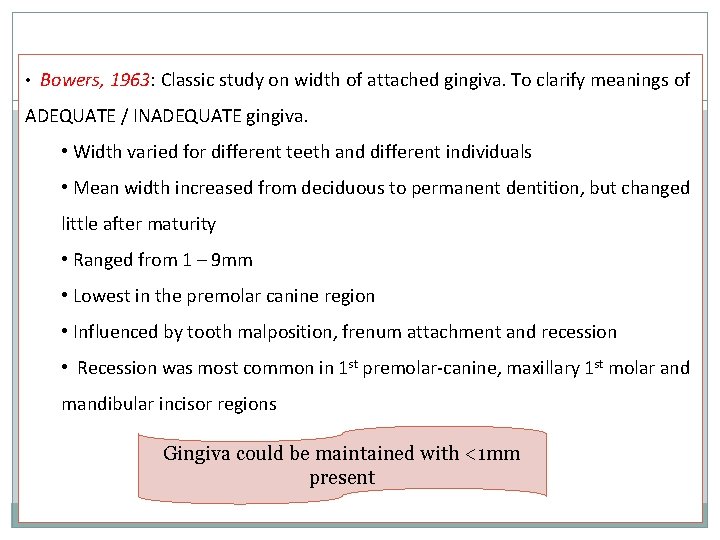
• Bowers, 1963: Classic study on width of attached gingiva. To clarify meanings of ADEQUATE / INADEQUATE gingiva. • Width varied for different teeth and different individuals • Mean width increased from deciduous to permanent dentition, but changed little after maturity • Ranged from 1 – 9 mm • Lowest in the premolar canine region • Influenced by tooth malposition, frenum attachment and recession • Recession was most common in 1 st premolar-canine, maxillary 1 st molar and mandibular incisor regions Gingiva could be maintained with <1 mm present
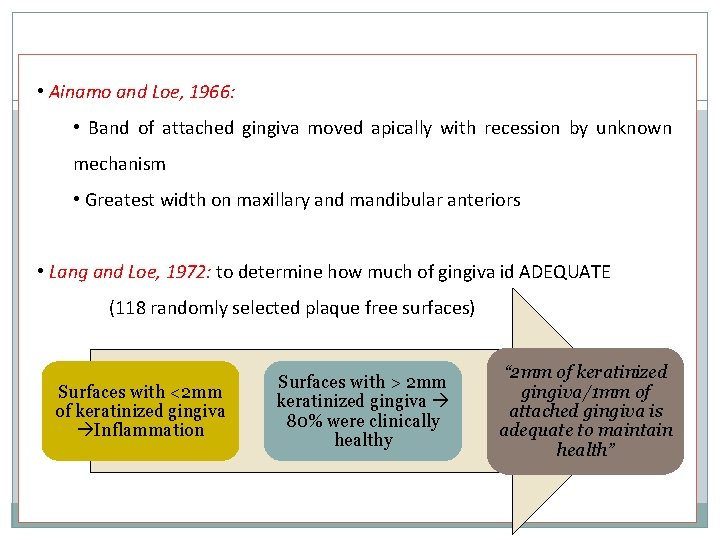
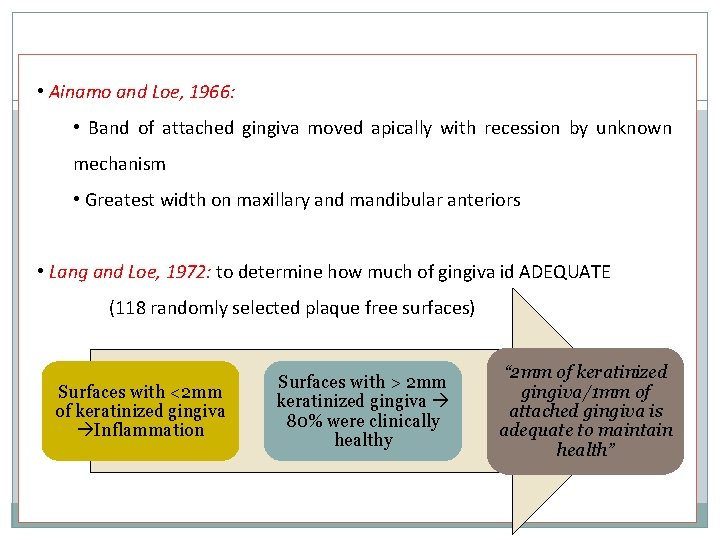
• Ainamo and Loe, 1966: • Band of attached gingiva moved apically with recession by unknown mechanism • Greatest width on maxillary and mandibular anteriors • Lang and Loe, 1972: to determine how much of gingiva id ADEQUATE (118 randomly selected plaque free surfaces) Surfaces with <2 mm of keratinized gingiva Inflammation Surfaces with > 2 mm keratinized gingiva 80% were clinically healthy “ 2 mm of keratinized gingiva/1 mm of attached gingiva is adequate to maintain health”
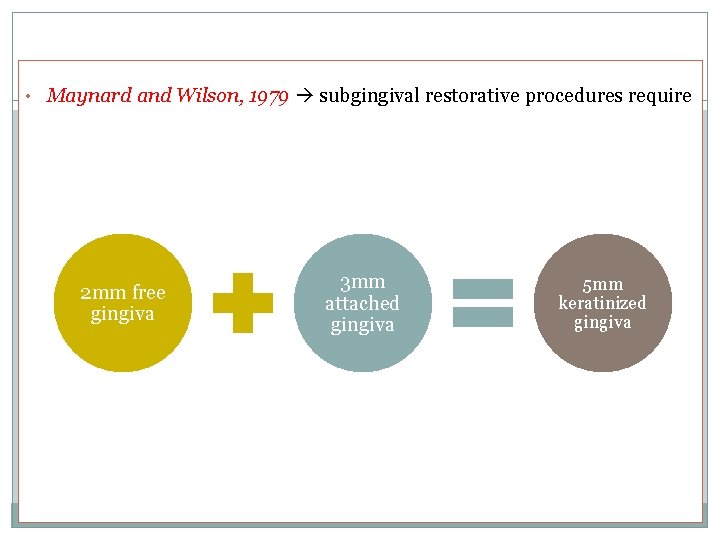
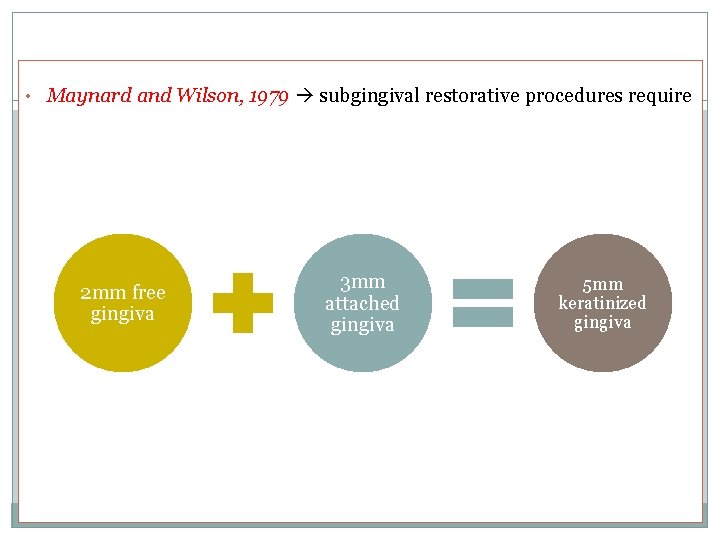
• Maynard and Wilson, 1979 subgingival restorative procedures require 2 mm free gingiva 3 mm attached gingiva 5 mm keratinized gingiva
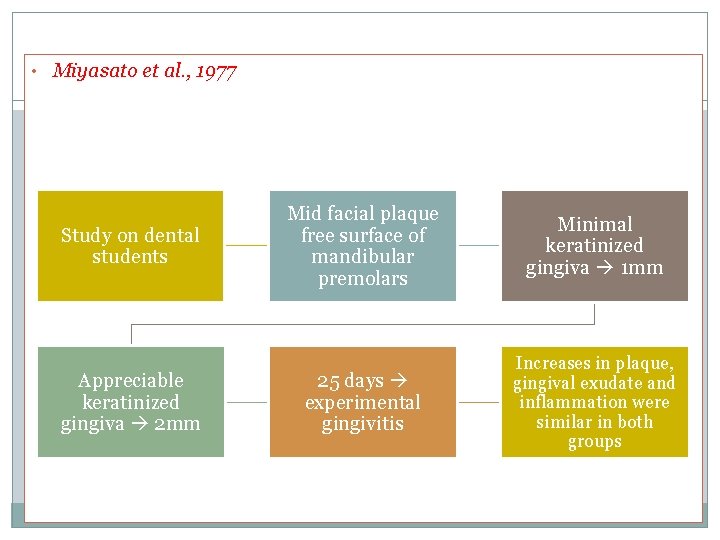
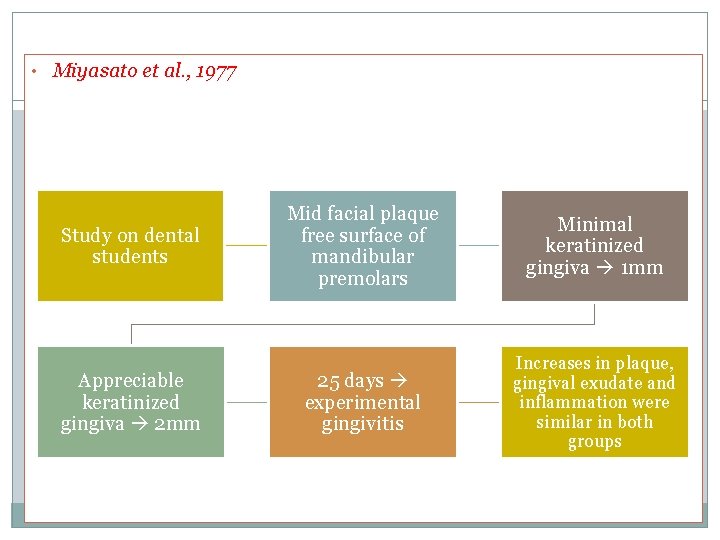
• Miyasato et al. , 1977 Study on dental students Appreciable keratinized gingiva 2 mm Mid facial plaque free surface of mandibular premolars Minimal keratinized gingiva 1 mm 25 days experimental gingivitis Increases in plaque, gingival exudate and inflammation were similar in both groups
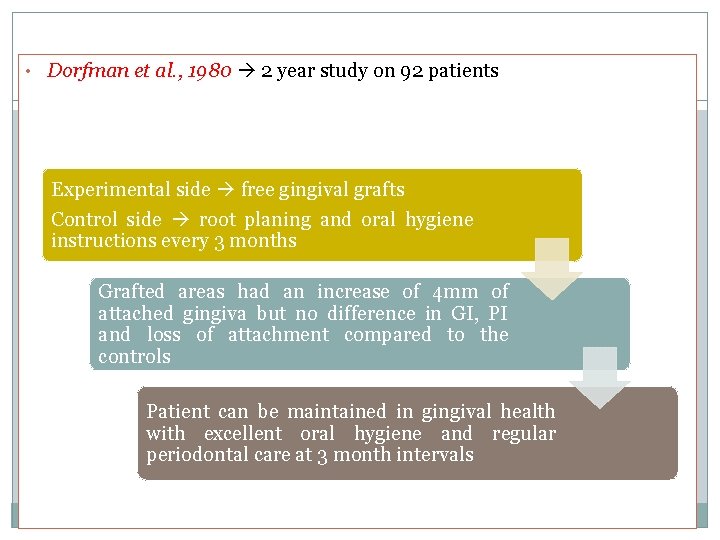
• Dorfman et al. , 1980 2 year study on 92 patients Experimental side free gingival grafts Control side root planing and oral hygiene instructions every 3 months Grafted areas had an increase of 4 mm of attached gingiva but no difference in GI, PI and loss of attachment compared to the controls Patient can be maintained in gingival health with excellent oral hygiene and regular periodontal care at 3 month intervals
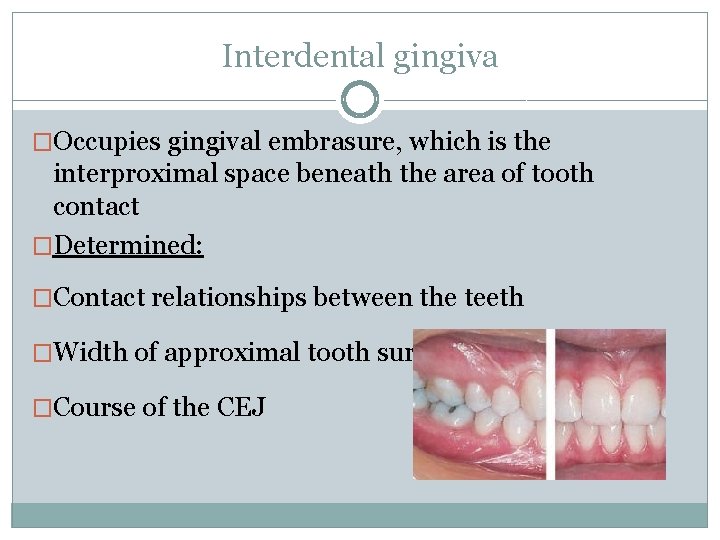
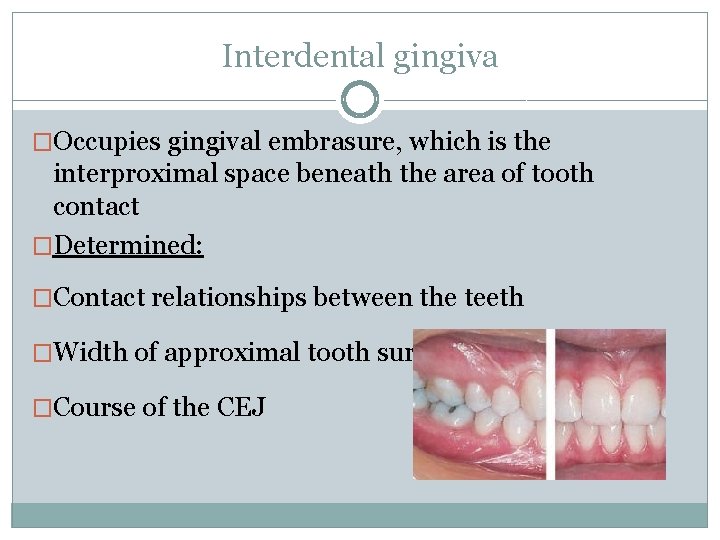
Interdental gingiva �Occupies gingival embrasure, which is the interproximal space beneath the area of tooth contact �Determined: �Contact relationships between the teeth �Width of approximal tooth surfaces �Course of the CEJ
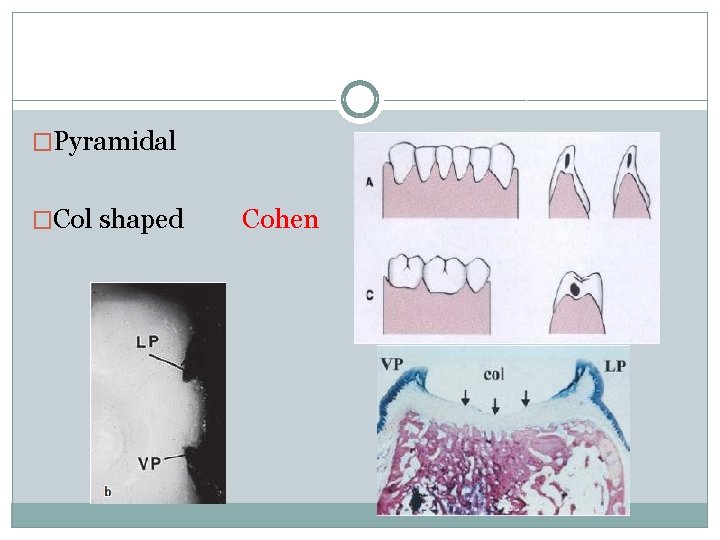
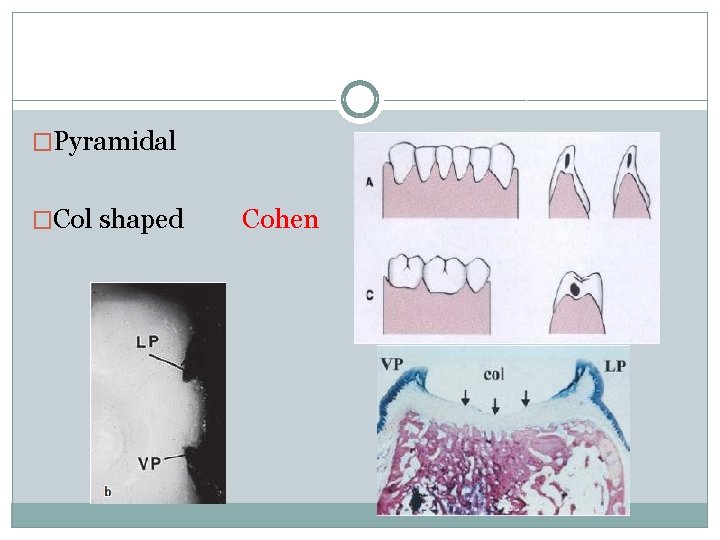
�Pyramidal �Col shaped Cohen
MICROSCOPIC FEATURES �Stratified squamous epithelium �Central core of connective tissue
GINGIVAL EPITHELIUM General aspects of gingival epithelium biology �Function: �Protects deep structures �Mechanical, chemical, water, microbial barrier �Signalling function
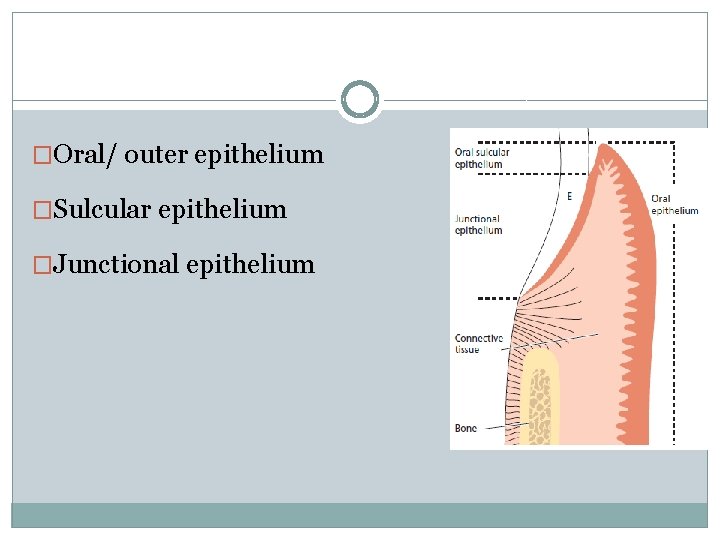
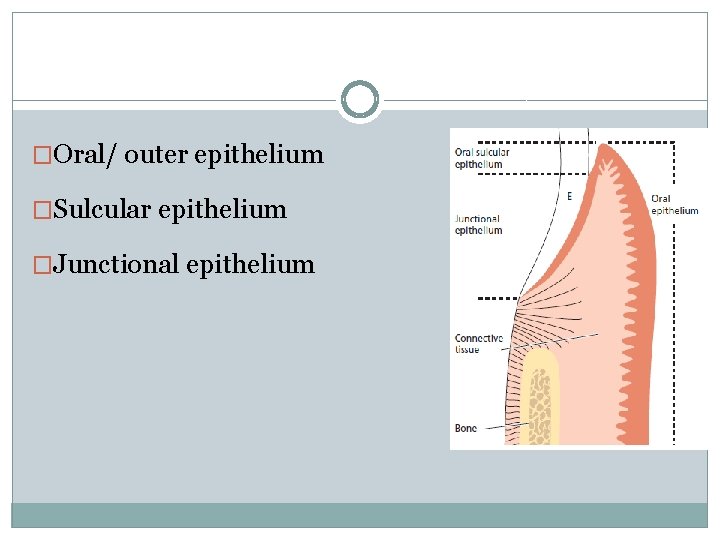
�Oral/ outer epithelium �Sulcular epithelium �Junctional epithelium
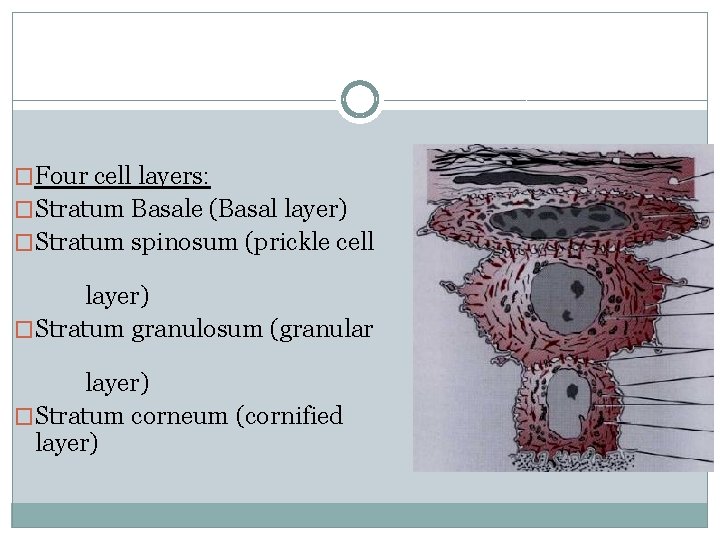
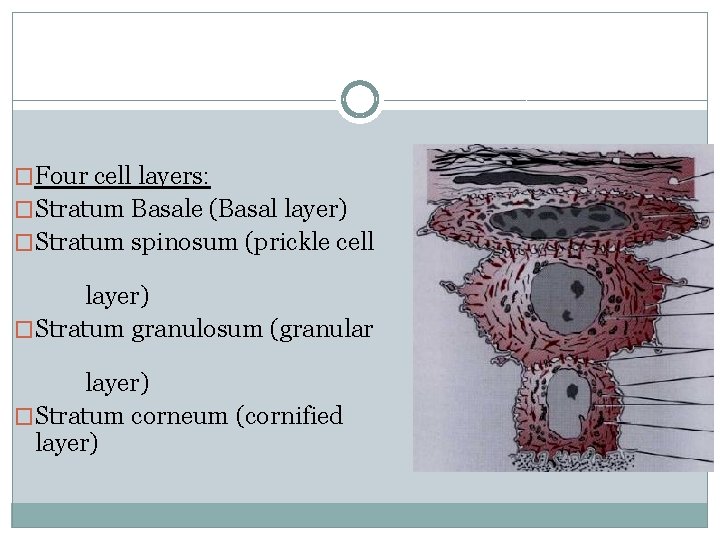
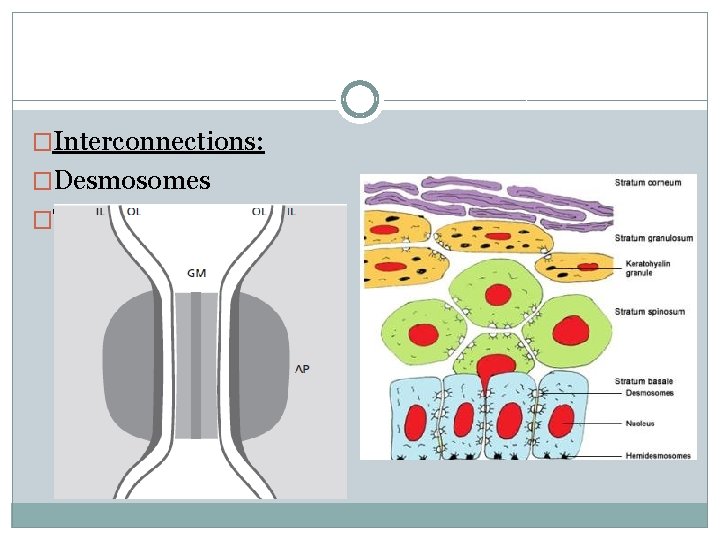
�Four cell layers: �Stratum Basale (Basal layer) �Stratum spinosum (prickle cell layer) �Stratum granulosum (granular layer) �Stratum corneum (cornified layer)
�Principal cell: keratinocytes �Clear cells / Nonkeratinocytes: Langerhans cells Merkels cells Melanocytes Inflammatory cells
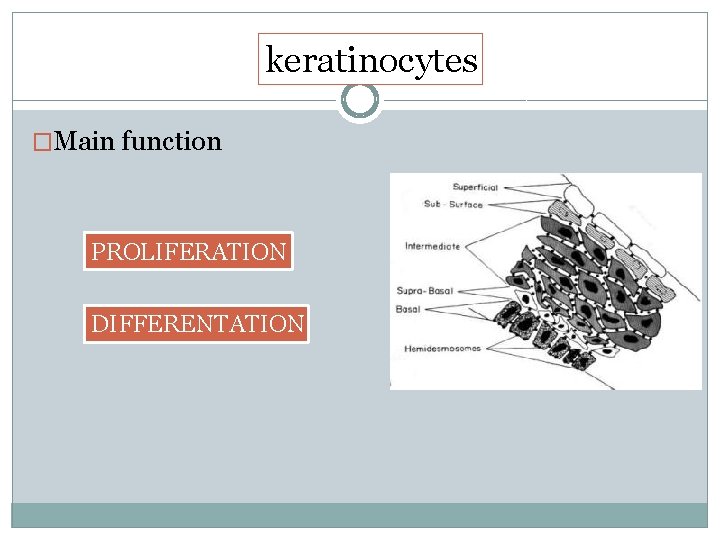
keratinocytes �Main function PROLIFERATION DIFFERENTATION
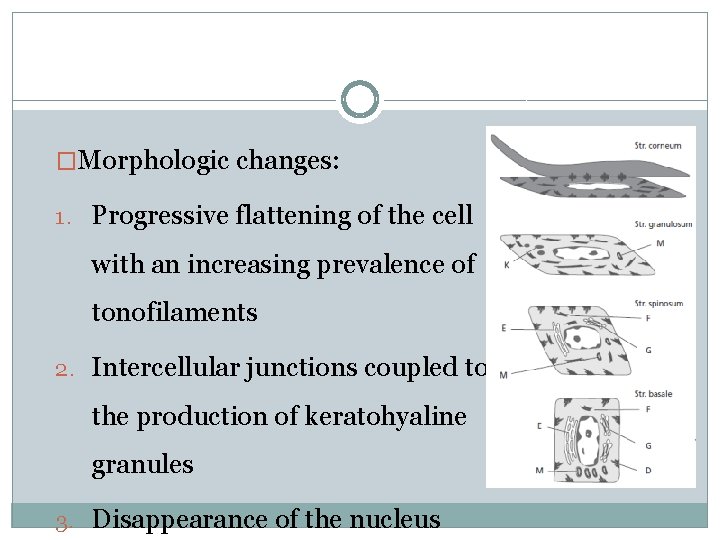
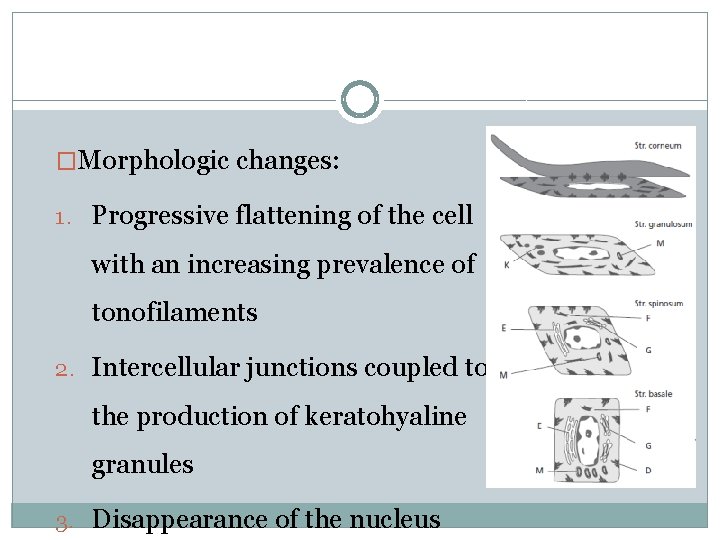
�Morphologic changes: 1. Progressive flattening of the cell with an increasing prevalence of tonofilaments 2. Intercellular junctions coupled to the production of keratohyaline granules 3. Disappearance of the nucleus
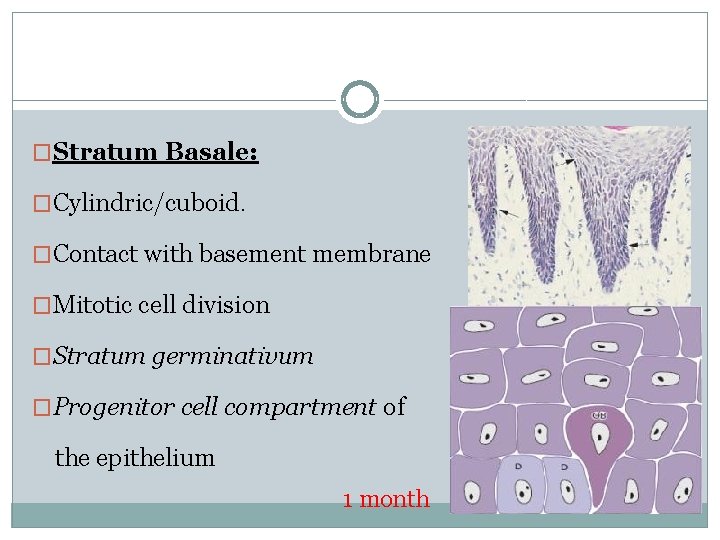
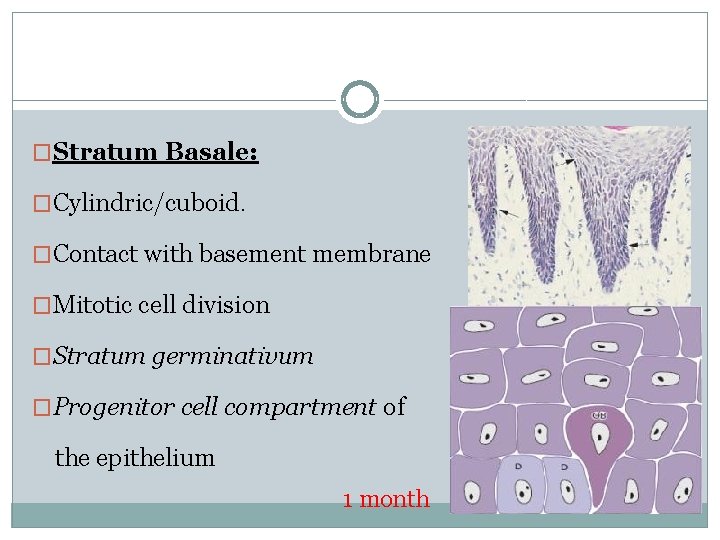
�Stratum Basale: �Cylindric/cuboid. �Contact with basement membrane �Mitotic cell division �Stratum germinativum �Progenitor cell compartment of the epithelium 1 month
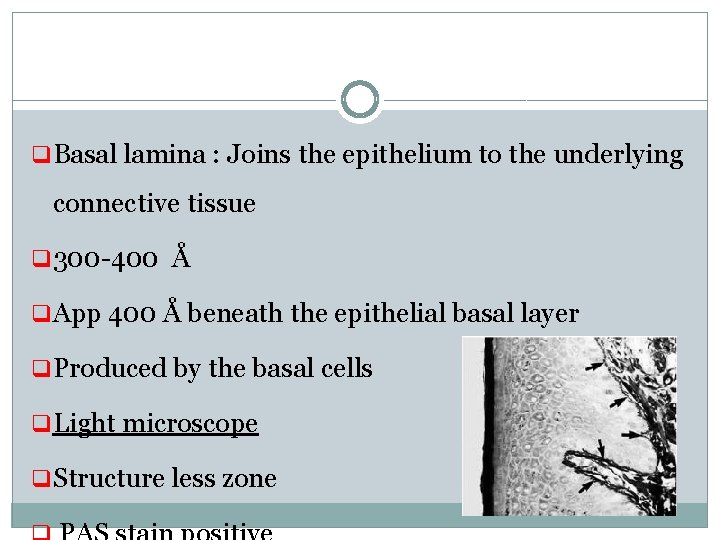
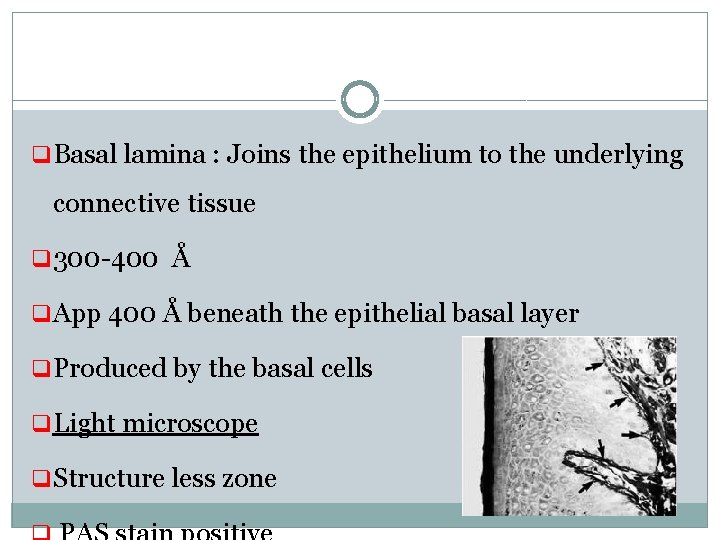
q Basal lamina : Joins the epithelium to the underlying connective tissue q 300 -400 Å q App 400 Å beneath the epithelial basal layer q Produced by the basal cells q Light microscope q Structure less zone
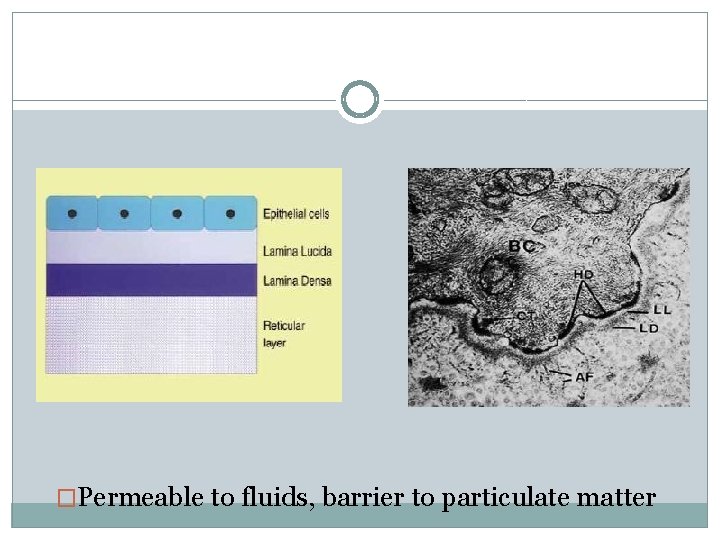
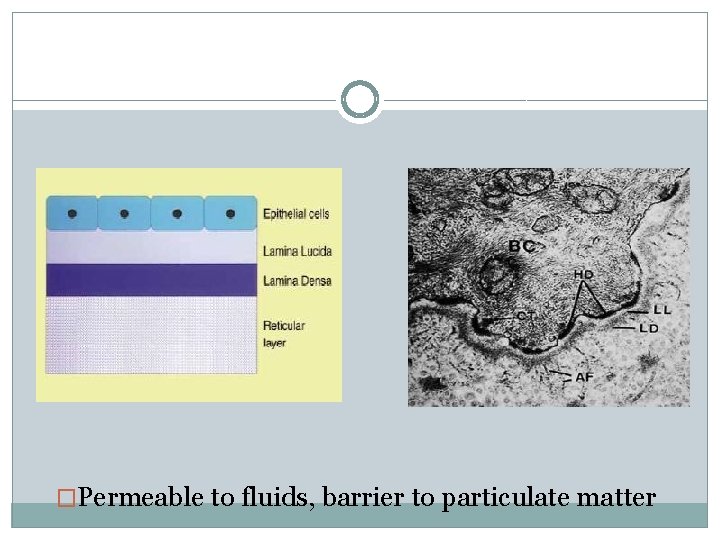
�Permeable to fluids, barrier to particulate matter
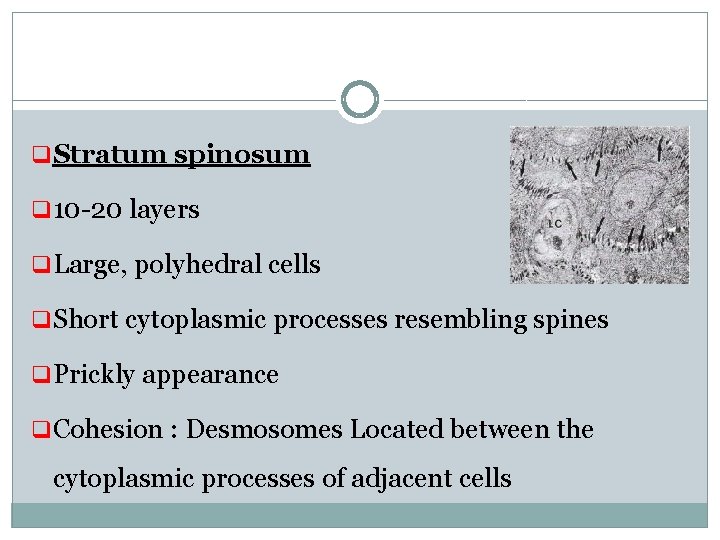
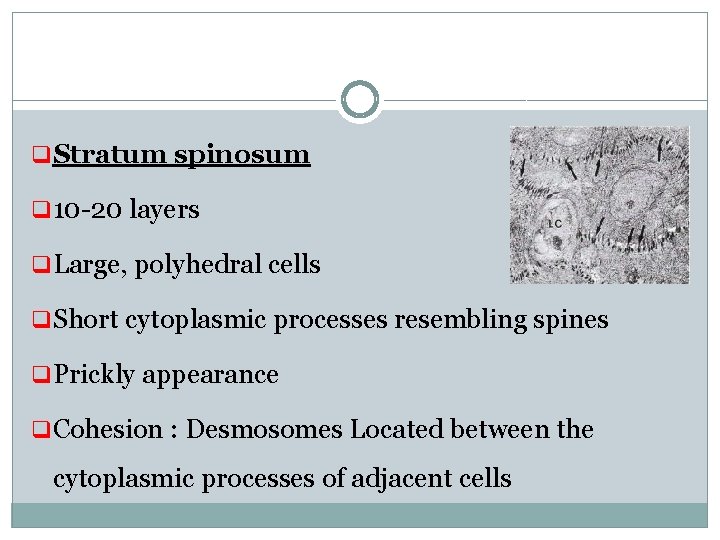
q Stratum spinosum q 10 -20 layers q Large, polyhedral cells q Short cytoplasmic processes resembling spines q Prickly appearance q Cohesion : Desmosomes Located between the cytoplasmic processes of adjacent cells
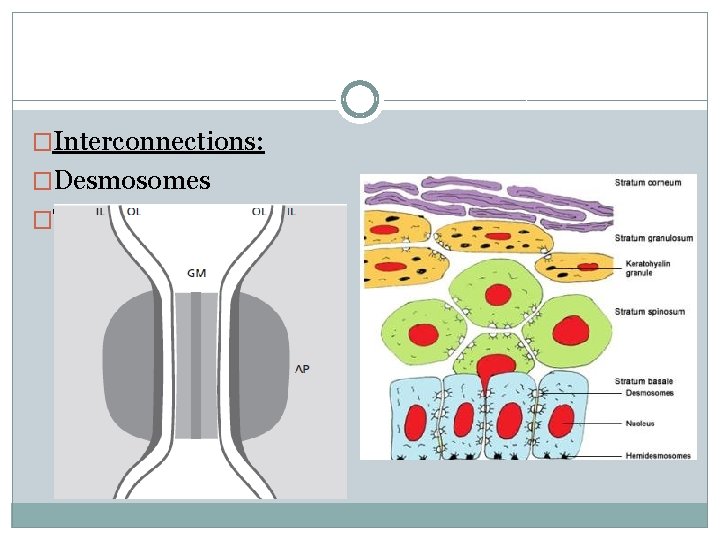
�Interconnections: �Desmosomes �Tight junctions (Zonae occludens)
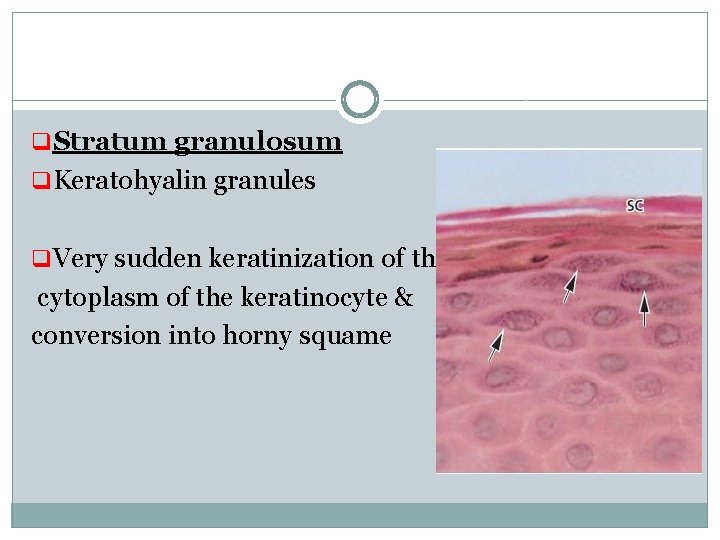
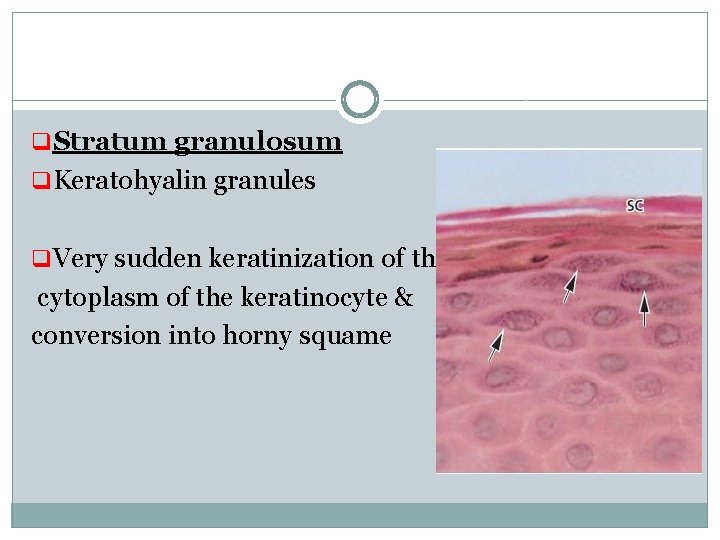
q Stratum granulosum q Keratohyalin granules q Very sudden keratinization of the cytoplasm of the keratinocyte & conversion into horny squame
q Stratum corneum q Filled with keratin q Apparatus for protein synthesis & energy production lost q Complete keratinization q Parakeratinized epithelium q Nonkeratinized epithelium Orthokeratinized
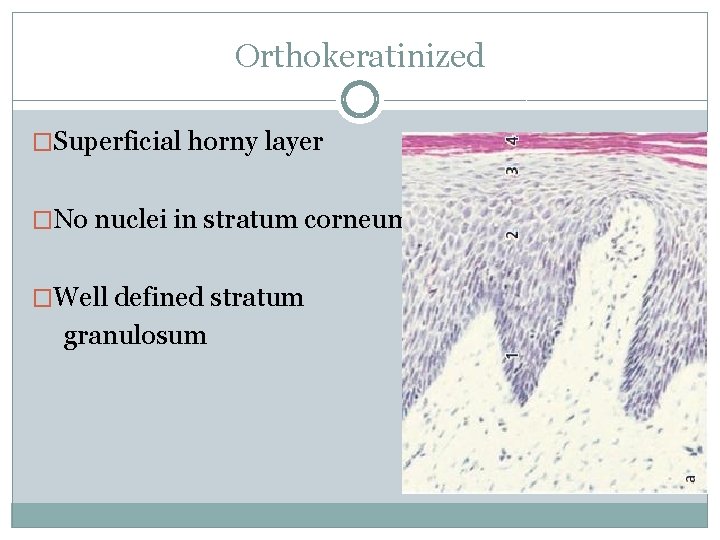
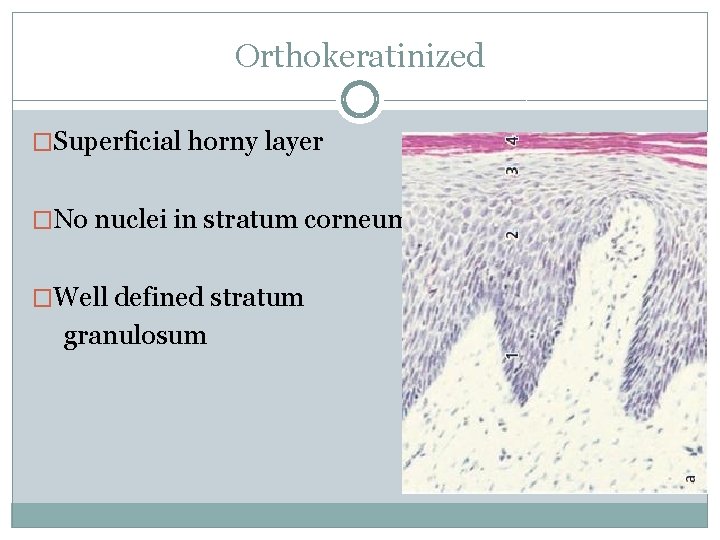
Orthokeratinized �Superficial horny layer �No nuclei in stratum corneum �Well defined stratum granulosum
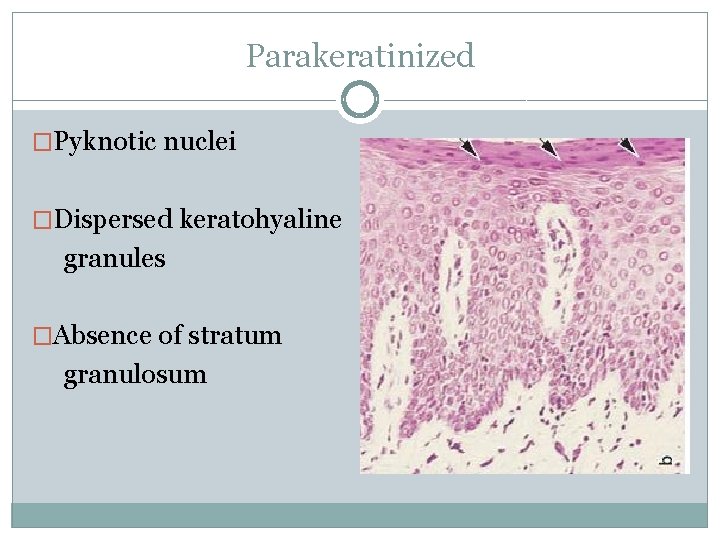
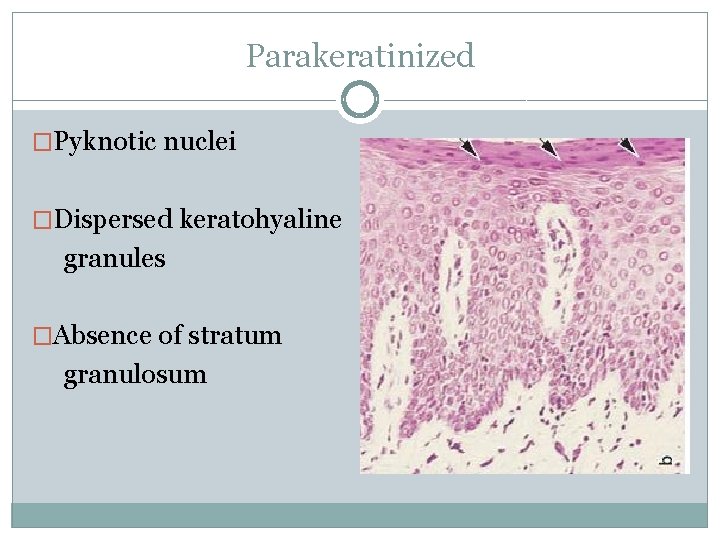
Parakeratinized �Pyknotic nuclei �Dispersed keratohyaline granules �Absence of stratum granulosum

Nonkeratinized �Viable nuclei �Absence of stratum granulosum & corneum
keratinization �Immunohistochemistry, Gel electrophoresis, Immunoblot technique �Keratin proteins different polypeptide subunits �Basal cells: K 19 (40 KD) �Stratum corneum: K 1 (68 KD)
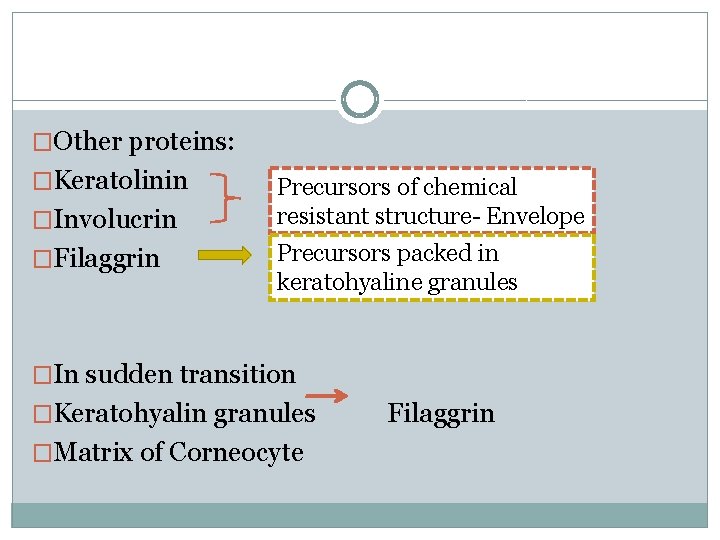
�Other proteins: �Keratolinin �Involucrin �Filaggrin Precursors of chemical resistant structure- Envelope Precursors packed in keratohyaline granules �In sudden transition �Keratohyalin granules �Matrix of Corneocyte Filaggrin
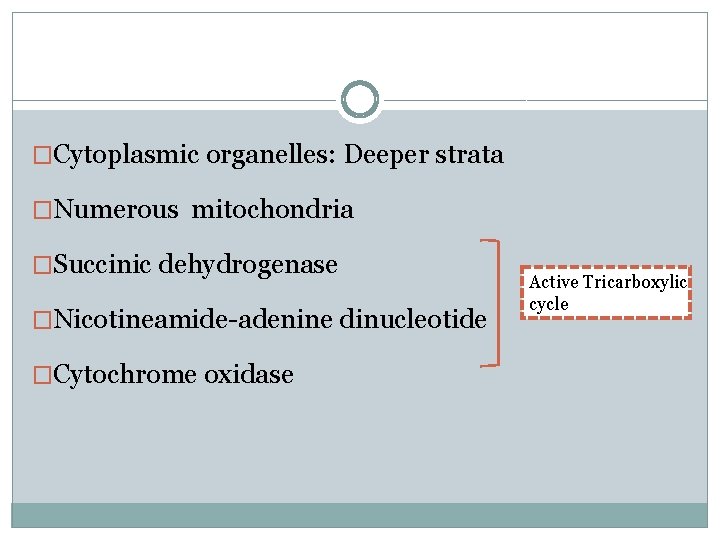
�Cytoplasmic organelles: Deeper strata �Numerous mitochondria �Succinic dehydrogenase �Nicotineamide-adenine dinucleotide �Cytochrome oxidase Active Tricarboxylic cycle
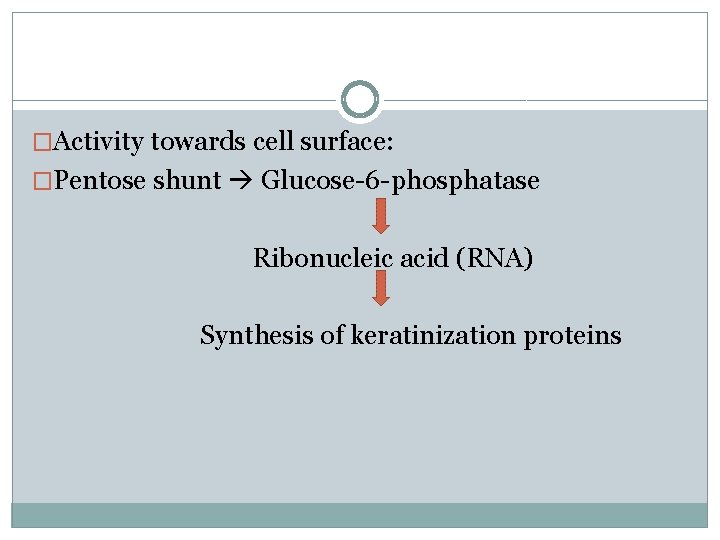
�Activity towards cell surface: �Pentose shunt Glucose-6 -phosphatase Ribonucleic acid (RNA) Synthesis of keratinization proteins
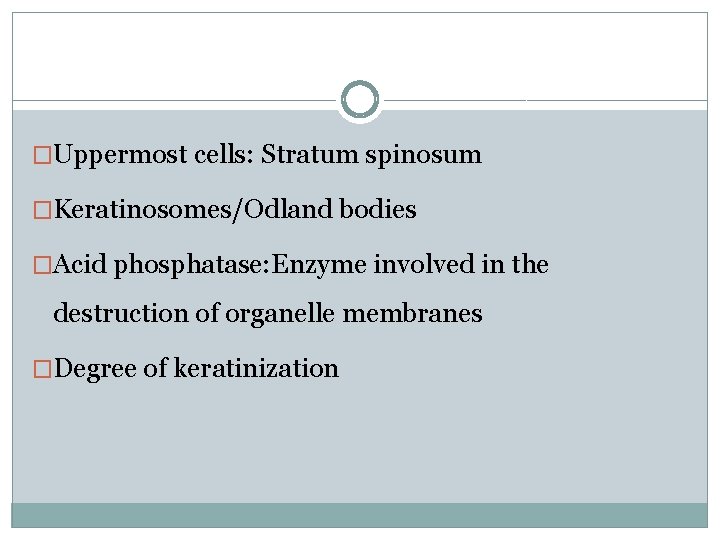
�Uppermost cells: Stratum spinosum �Keratinosomes/Odland bodies �Acid phosphatase: Enzyme involved in the destruction of organelle membranes �Degree of keratinization
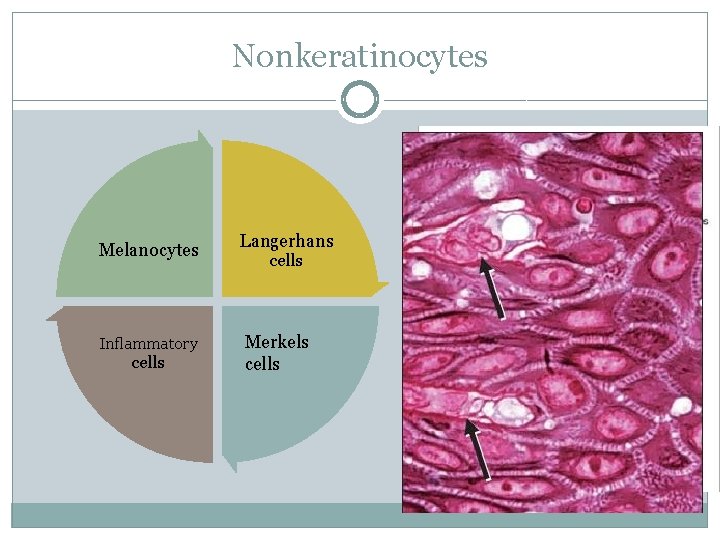
Nonkeratinocytes Melanocytes Inflammatory cells Langerhans cells Merkels cells
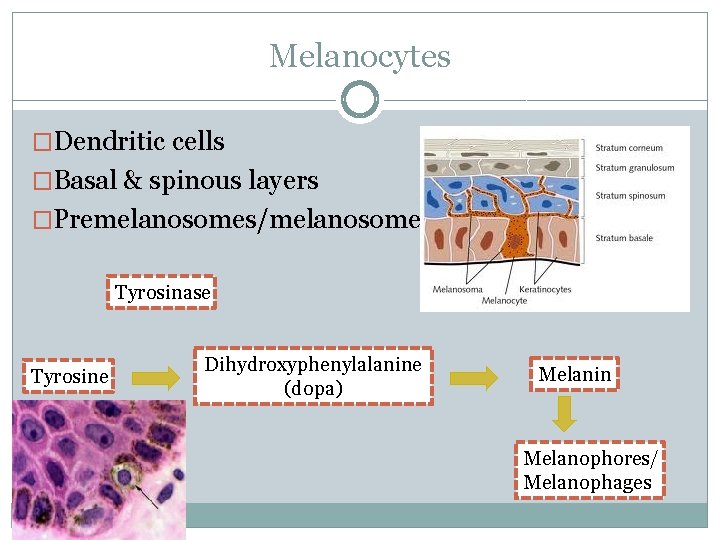
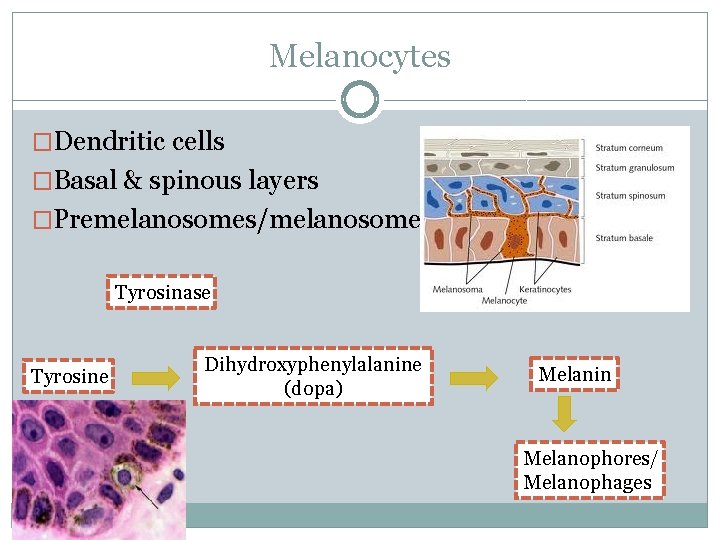
Melanocytes �Dendritic cells �Basal & spinous layers �Premelanosomes/melanosomes Tyrosinase Tyrosine Dihydroxyphenylalanine (dopa) Melanin Melanophores/ Melanophages
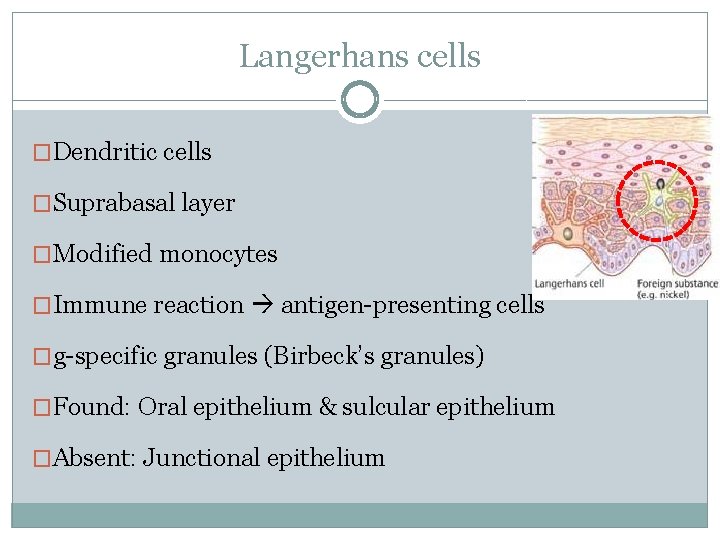
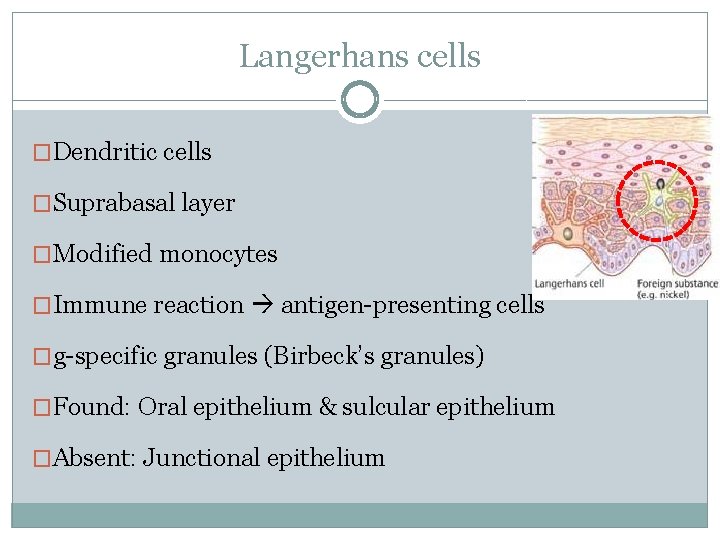
Langerhans cells �Dendritic cells �Suprabasal layer �Modified monocytes �Immune reaction antigen-presenting cells �g-specific granules (Birbeck’s granules) �Found: Oral epithelium & sulcular epithelium �Absent: Junctional epithelium
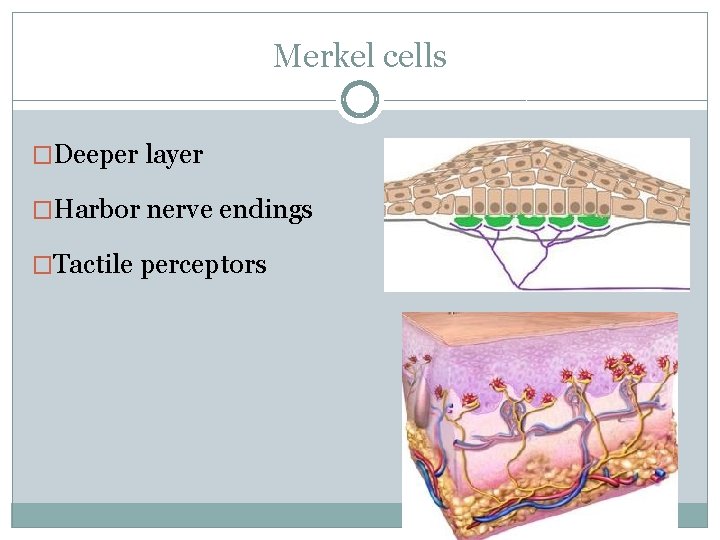
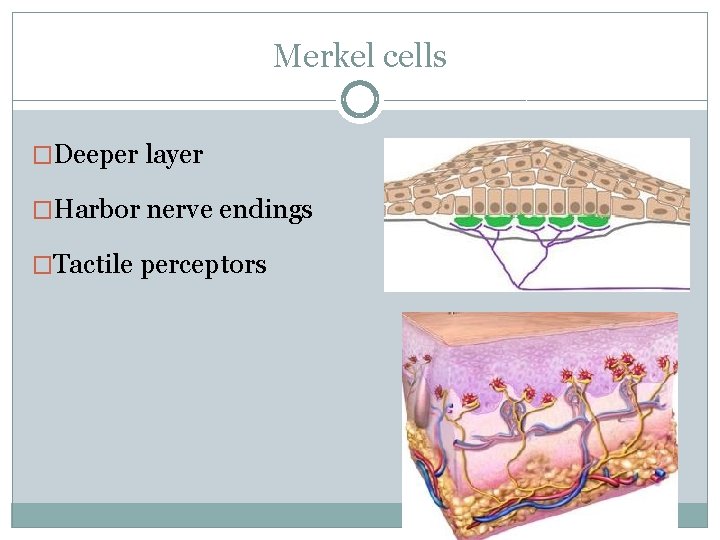
Merkel cells �Deeper layer �Harbor nerve endings �Tactile perceptors
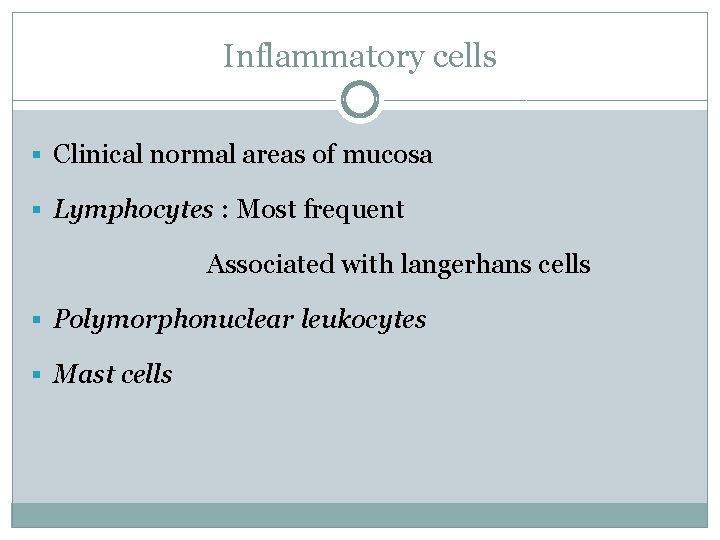
Inflammatory cells § Clinical normal areas of mucosa § Lymphocytes : Most frequent Associated with langerhans cells § Polymorphonuclear leukocytes § Mast cells
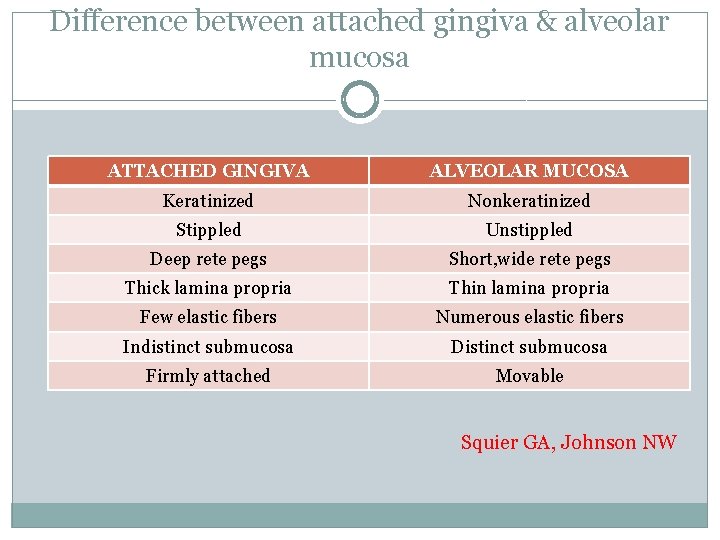
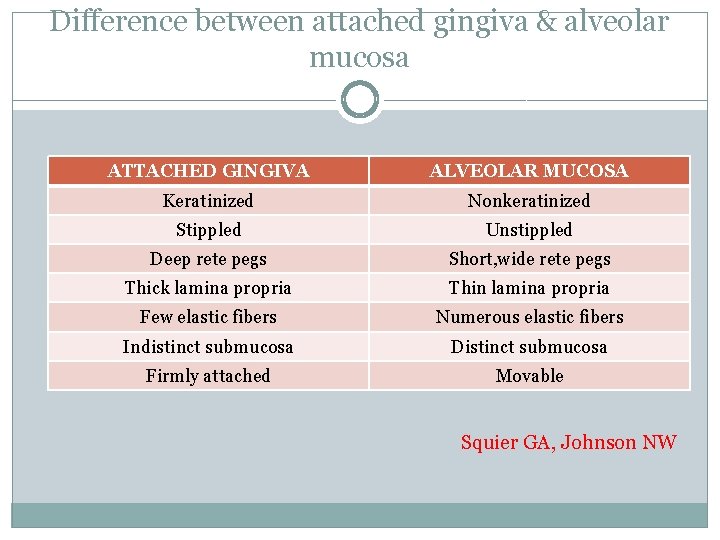
Difference between attached gingiva & alveolar mucosa ATTACHED GINGIVA ALVEOLAR MUCOSA Keratinized Nonkeratinized Stippled Unstippled Deep rete pegs Short, wide rete pegs Thick lamina propria Thin lamina propria Few elastic fibers Numerous elastic fibers Indistinct submucosa Distinct submucosa Firmly attached Movable Squier GA, Johnson NW
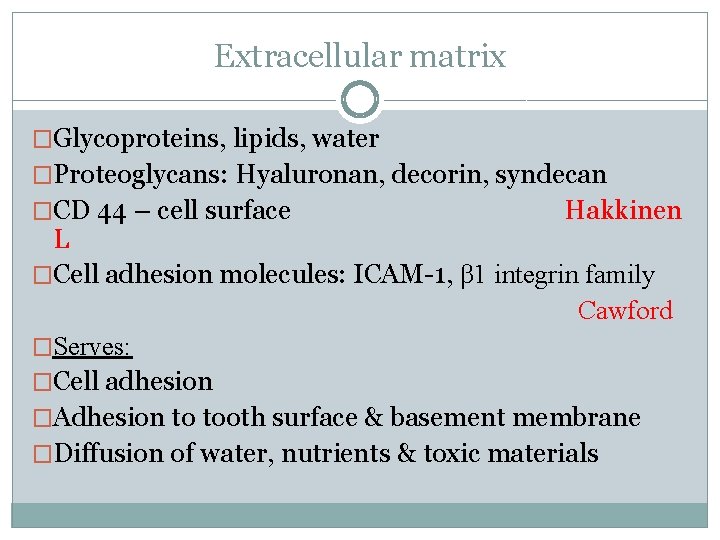
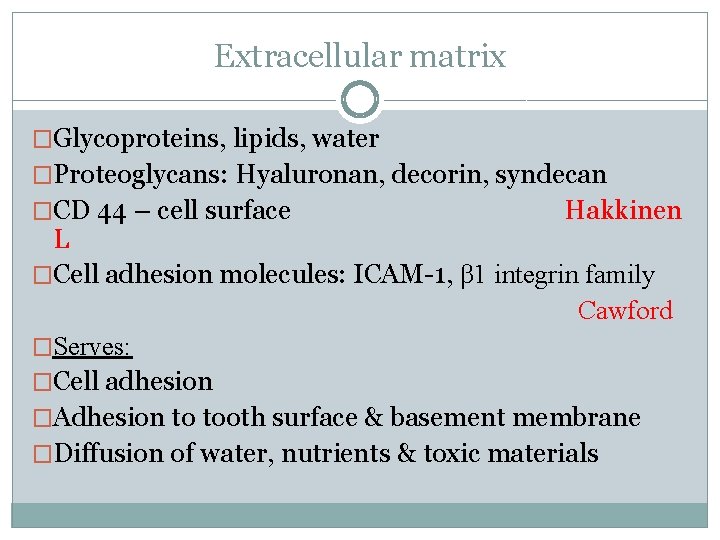
Extracellular matrix �Glycoproteins, lipids, water �Proteoglycans: Hyaluronan, decorin, syndecan �CD 44 – cell surface Hakkinen L �Cell adhesion molecules: ICAM-1, β 1 integrin family Cawford �Serves: �Cell adhesion �Adhesion to tooth surface & basement membrane �Diffusion of water, nutrients & toxic materials
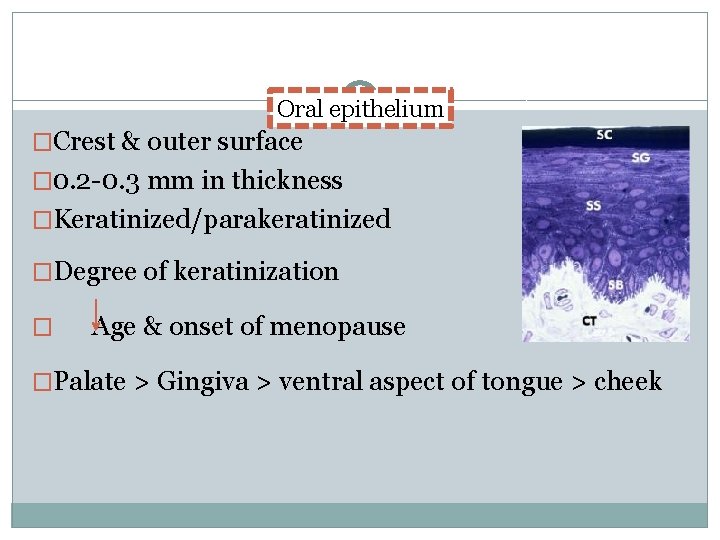
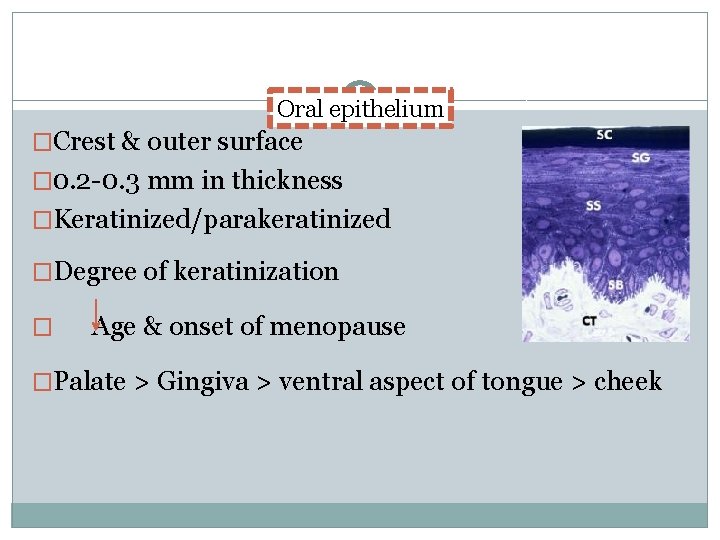
Oral epithelium �Crest & outer surface � 0. 2 -0. 3 mm in thickness �Keratinized/parakeratinized �Degree of keratinization � Age & onset of menopause �Palate > Gingiva > ventral aspect of tongue > cheek
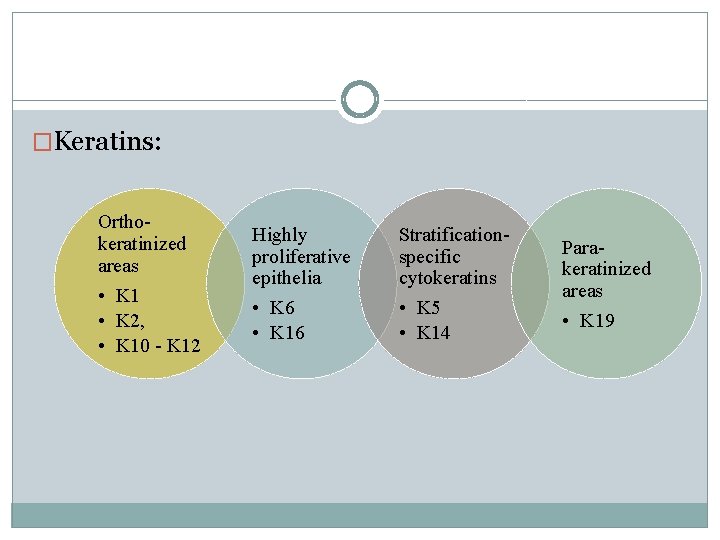
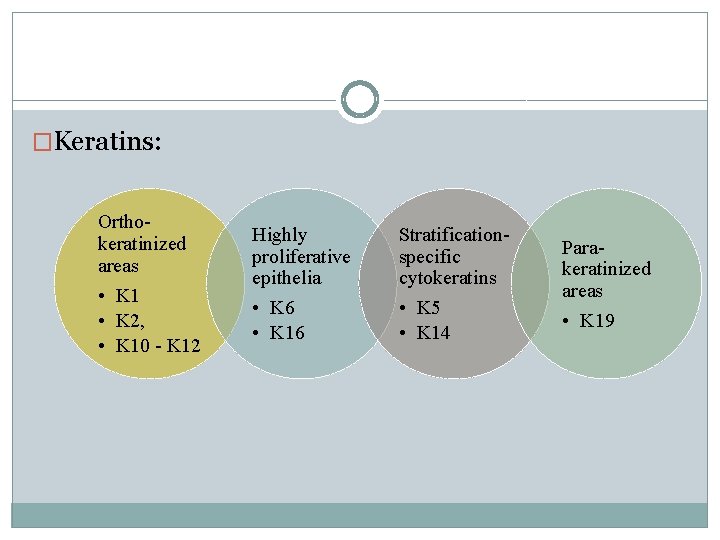
�Keratins: Orthokeratinized areas • K 1 • K 2, • K 10 - K 12 Highly proliferative epithelia • K 6 • K 16 Stratificationspecific cytokeratins • K 5 • K 14 Parakeratinized areas • K 19
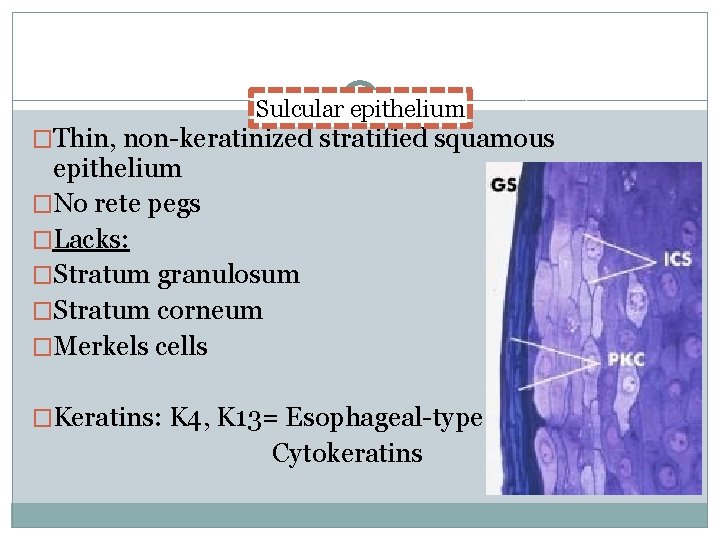
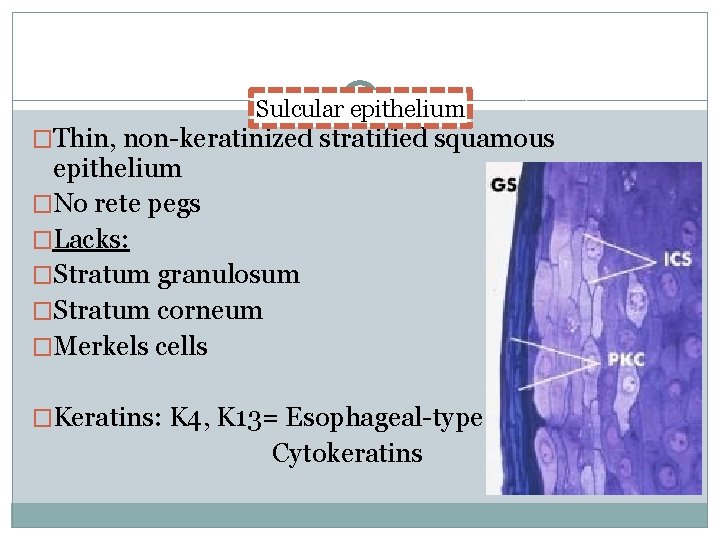
Sulcular epithelium �Thin, non-keratinized stratified squamous epithelium �No rete pegs �Lacks: �Stratum granulosum �Stratum corneum �Merkels cells �Keratins: K 4, K 13= Esophageal-type Cytokeratins
�Enzymes: low degree of activity �Acid phosphatase staining negative �Semipermeable membrane �Potential to keratinize: �It is reflected & exposed to oral cavity Caffesse �Absence of bacterial flora Bral & Caffesse
Junctional epithelium �The junctional epithelium is the epithelial component of the dentogingival unit that is in contact with the tooth surface. The innermost cells of the JE form & maintain a tight seal against the mineralized tooth surface, the so called epithelial attachment Schroeder & Listgarten, 1977 �Collar-like band of stratified squamous nonkeratinizing epithelium Glickman
Junctional epithelium Dentogingival unit Gingival fibers
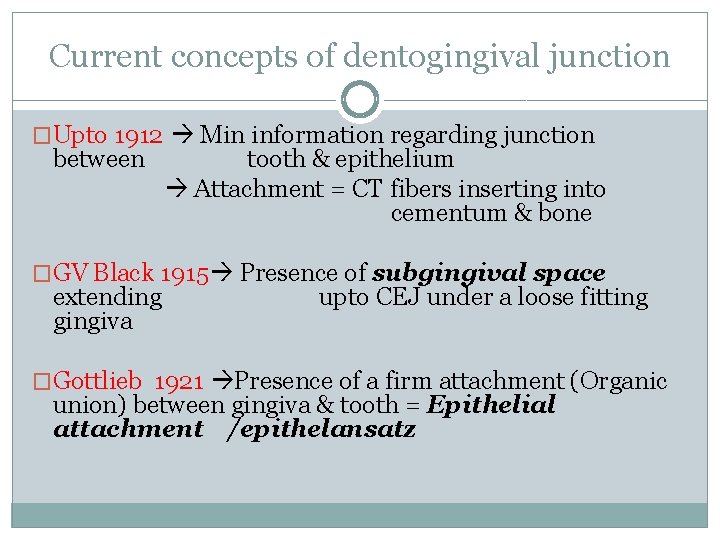
Current concepts of dentogingival junction �Upto 1912 Min information regarding junction between tooth & epithelium Attachment = CT fibers inserting into cementum & bone �GV Black 1915 Presence of subgingival space extending gingiva upto CEJ under a loose fitting �Gottlieb 1921 Presence of a firm attachment (Organic union) between gingiva & tooth = Epithelial attachment /epithelansatz
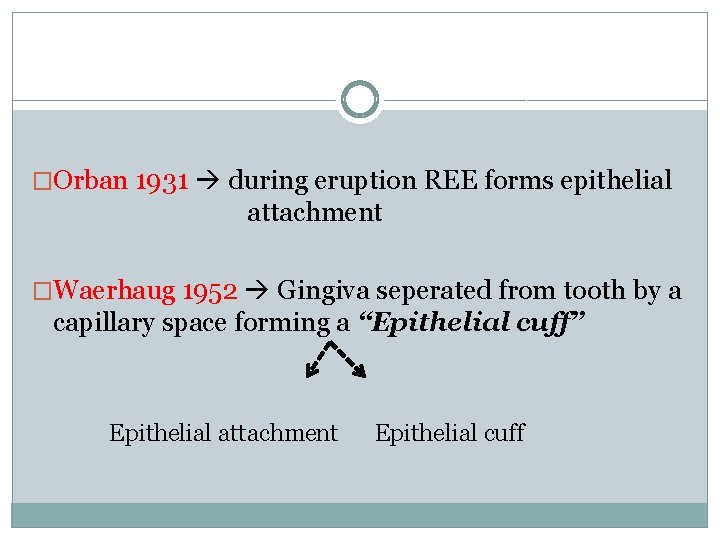
�Orban 1931 during eruption REE forms epithelial attachment �Waerhaug 1952 Gingiva seperated from tooth by a capillary space forming a “Epithelial cuff” Epithelial attachment Epithelial cuff
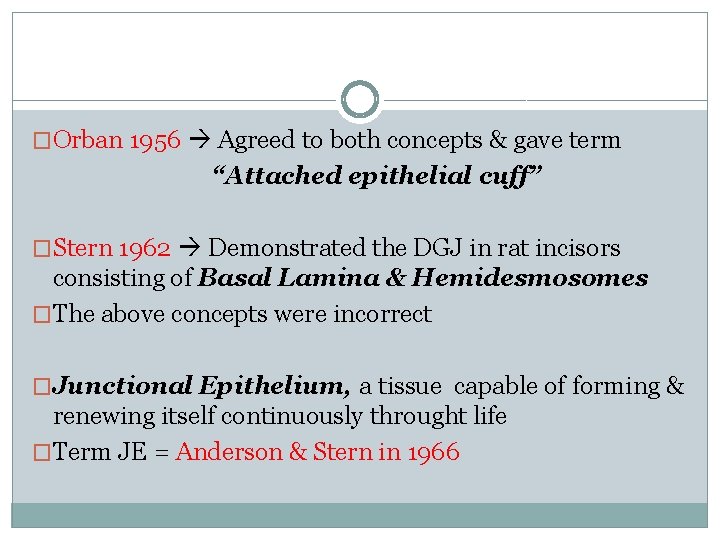
�Orban 1956 Agreed to both concepts & gave term “Attached epithelial cuff” �Stern 1962 Demonstrated the DGJ in rat incisors consisting of Basal Lamina & Hemidesmosomes �The above concepts were incorrect �Junctional Epithelium, a tissue capable of forming & renewing itself continuously throught life �Term JE = Anderson & Stern in 1966
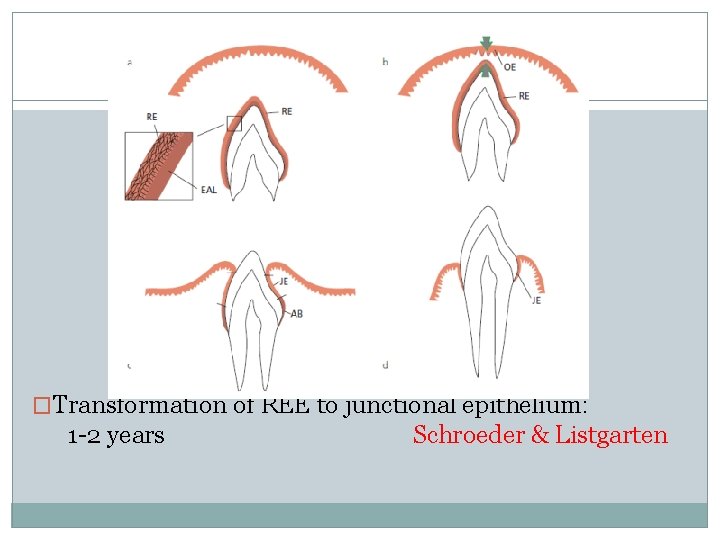
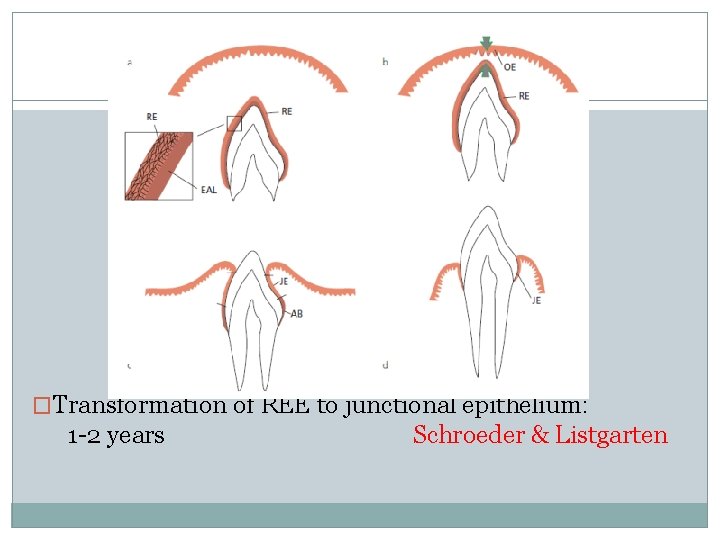
�Transformation of REE to junctional epithelium: 1 -2 years Schroeder & Listgarten
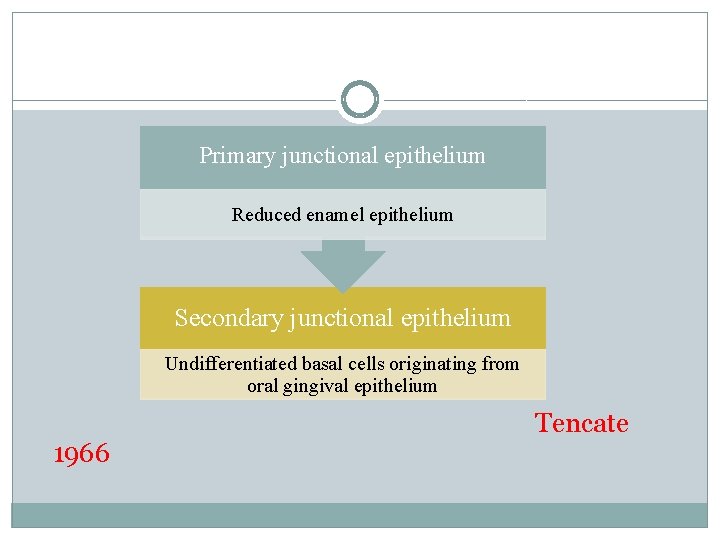
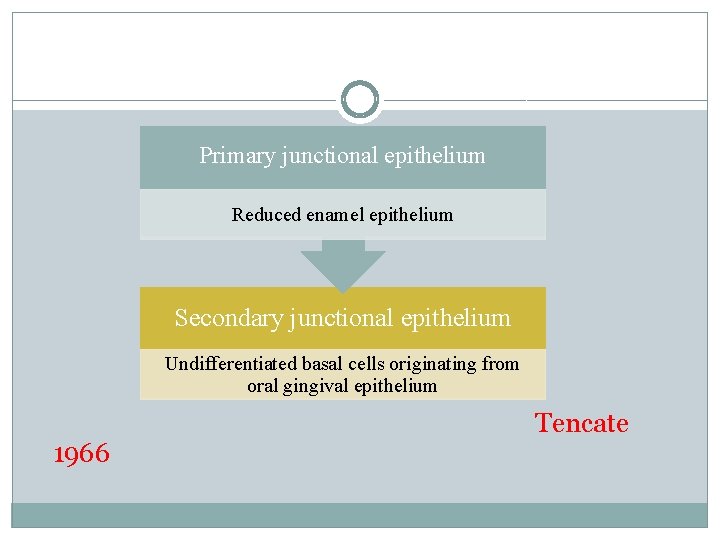
Primary junctional epithelium Reduced enamel epithelium Secondary junctional epithelium Undifferentiated basal cells originating from oral gingival epithelium 1966 Tencate
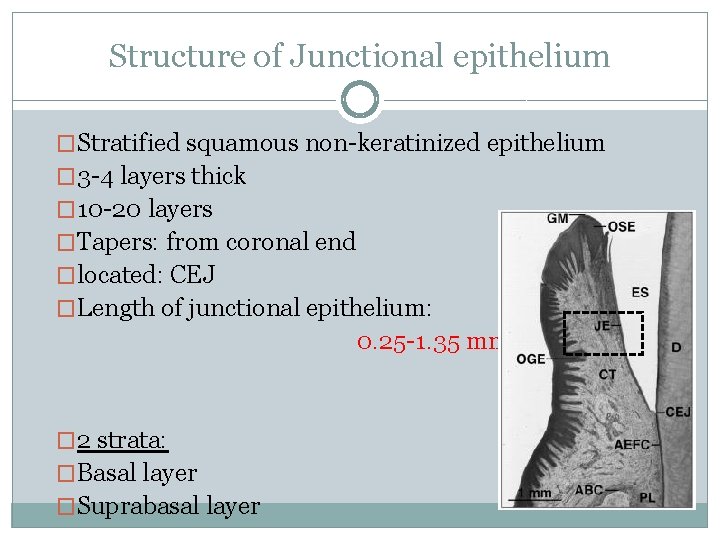
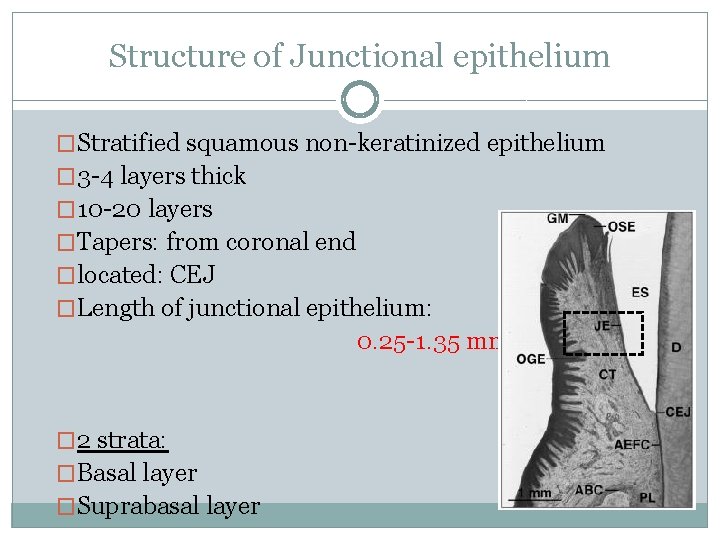
Structure of Junctional epithelium �Stratified squamous non-keratinized epithelium � 3 -4 layers thick � 10 -20 layers �Tapers: from coronal end �located: CEJ �Length of junctional epithelium: 0. 25 -1. 35 mm � 2 strata: �Basal layer �Suprabasal layer
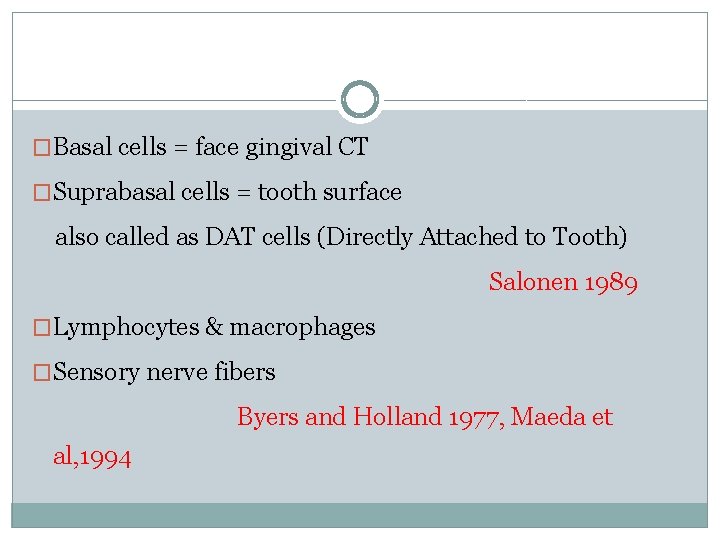
�Basal cells = face gingival CT �Suprabasal cells = tooth surface also called as DAT cells (Directly Attached to Tooth) Salonen 1989 �Lymphocytes & macrophages �Sensory nerve fibers Byers and Holland 1977, Maeda et al, 1994
� Keratins: K 19 � Stratification specific: K 5 & K 14 � Lack of expression: ü Morgan et al : Junctional area is the only stratified nonkeratinized epithelium in the oral cavity that does not synthesize K 4 or K 13 ü Lack of K 6 & K 16 : Though turnover of the cells is very high
§ Interconnections ü Few desmosomes only ü Occasional gap junctions Schroeder & Listgarten, 1977 Saito et al, 1981 Hashimoto et al, 1986 § Wide fluid-filled intercellular spaces Schroeder& Münzel-Pedrazzoli, 1970
� 3 Zones: �Apical zone germinative characteristics �Middle zone higher density of hemidesmosomes role in adhesion �Coronal zone numerous intercellular space increased permeability
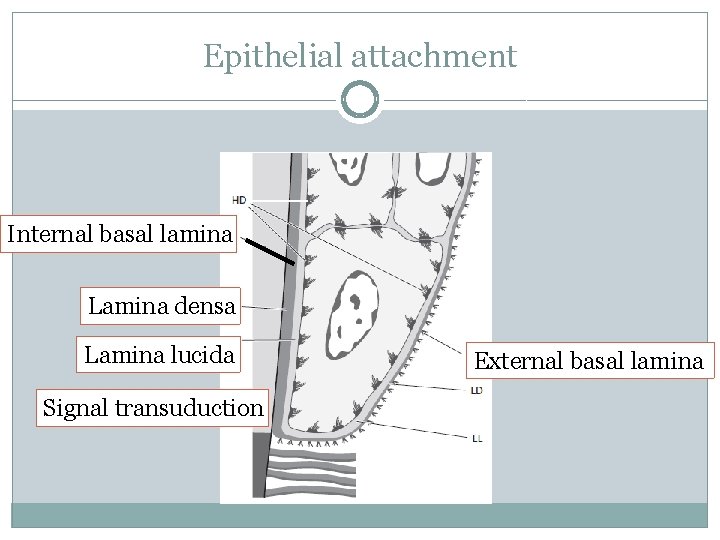
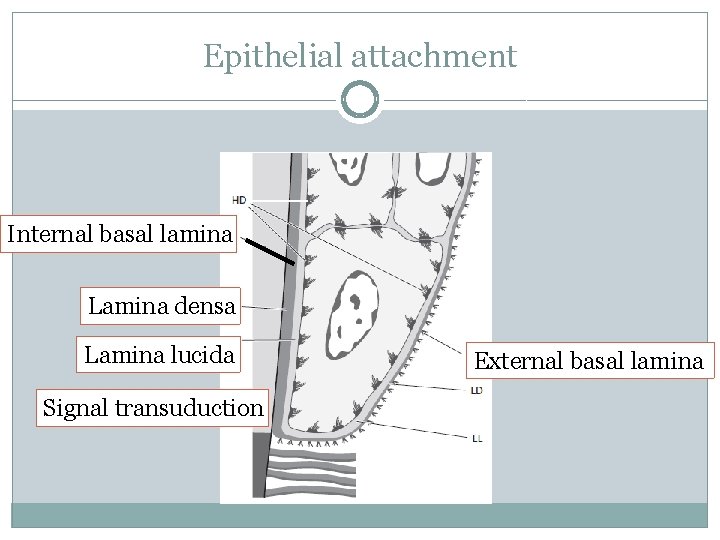
Epithelial attachment Internal basal lamina Lamina densa Lamina lucida Signal transuduction External basal lamina
�Histochemical evidence Neutral polysaccharide Thonard JC �Basal lamina: �Laminin: similar to endothelial & epithelial cells �Lack type IV & VII collagen, perlecan, lamina fibroreticularis. 1985 Salonen & Santti
Dynamics of junctional epithelium �Turnover is very high protective & regeneration �Earlier thought epithelial cells facing external basal lamina divide rapidly �Evidence DAT cells high mitotic activity �DAT cells Role in tissue dynamics & reparative capacity of JE
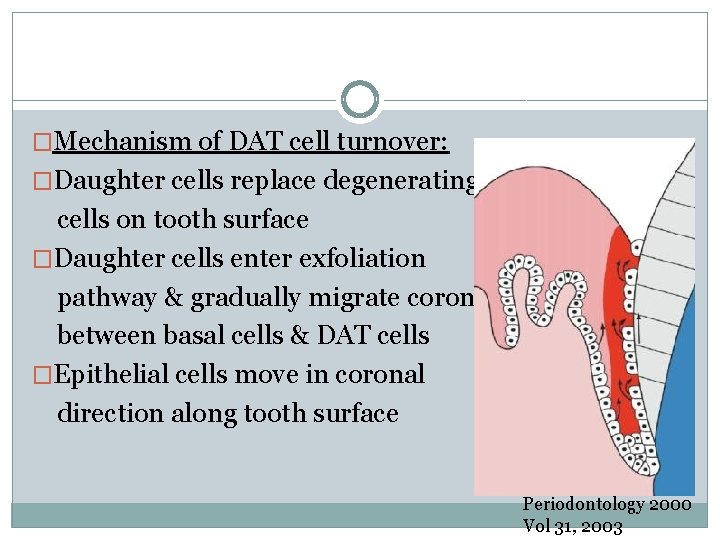
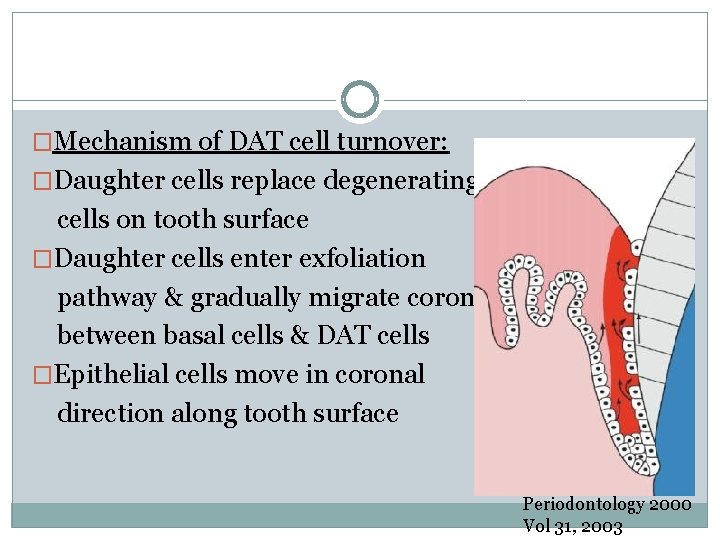
�Mechanism of DAT cell turnover: �Daughter cells replace degenerating cells on tooth surface �Daughter cells enter exfoliation pathway & gradually migrate coronally between basal cells & DAT cells �Epithelial cells move in coronal direction along tooth surface Periodontology 2000 Vol 31, 2003
�Structural & functional features: �Firm attachment: epithelial barrier �Immunologic host defense: Gingival fluid, inflammatory cells �Rapid cell turnover q Endocytic capacity equal to that of macrophages and neutrophils 0 Cho. Garant. 200
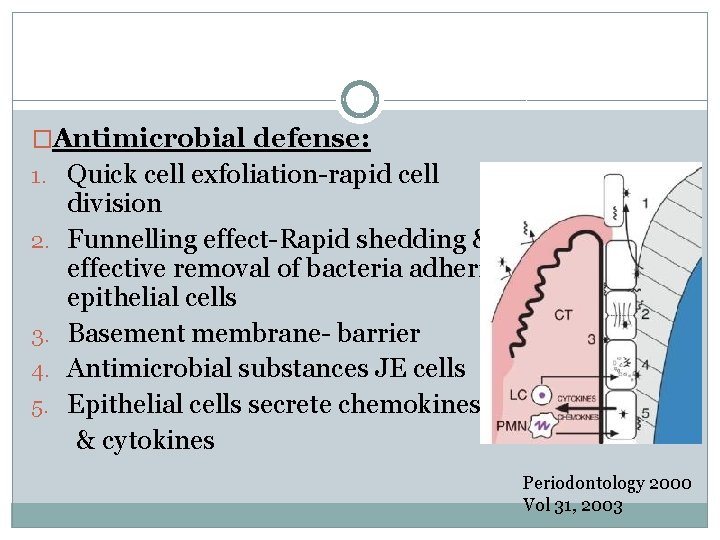
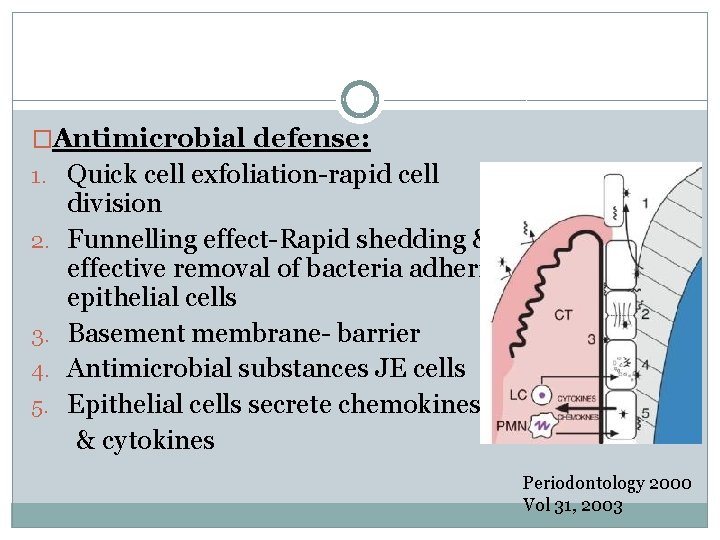
�Antimicrobial defense: 1. Quick cell exfoliation-rapid cell 2. 3. 4. 5. division Funnelling effect-Rapid shedding & effective removal of bacteria adhering epithelial cells Basement membrane- barrier Antimicrobial substances JE cells Epithelial cells secrete chemokines & cytokines to Periodontology 2000 Vol 31, 2003
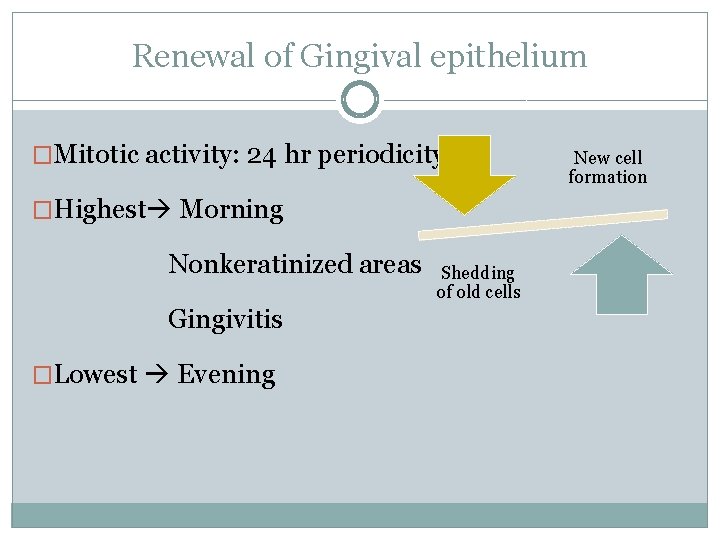
Renewal of Gingival epithelium �Mitotic activity: 24 hr periodicity �Highest Morning Nonkeratinized areas Gingivitis �Lowest Evening Shedding of old cells New cell formation
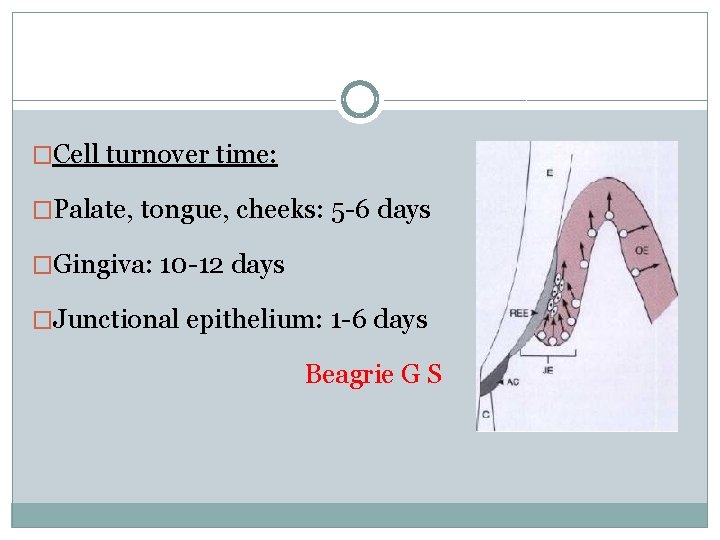
�Cell turnover time: �Palate, tongue, cheeks: 5 -6 days �Gingiva: 10 -12 days �Junctional epithelium: 1 -6 days Beagrie G S
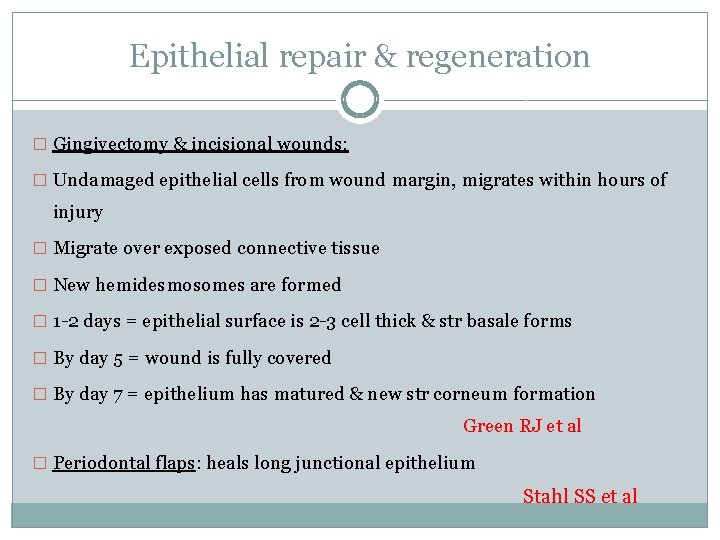
Epithelial repair & regeneration � Gingivectomy & incisional wounds: � Undamaged epithelial cells from wound margin, migrates within hours of injury � Migrate over exposed connective tissue � New hemidesmosomes are formed � 1 -2 days = epithelial surface is 2 -3 cell thick & str basale forms � By day 5 = wound is fully covered � By day 7 = epithelium has matured & new str corneum formation Green RJ et al � Periodontal flaps: heals long junctional epithelium Stahl SS et al
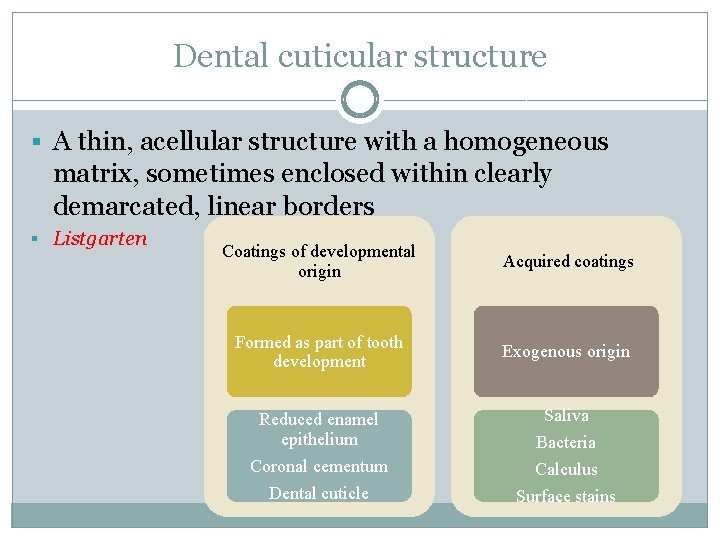
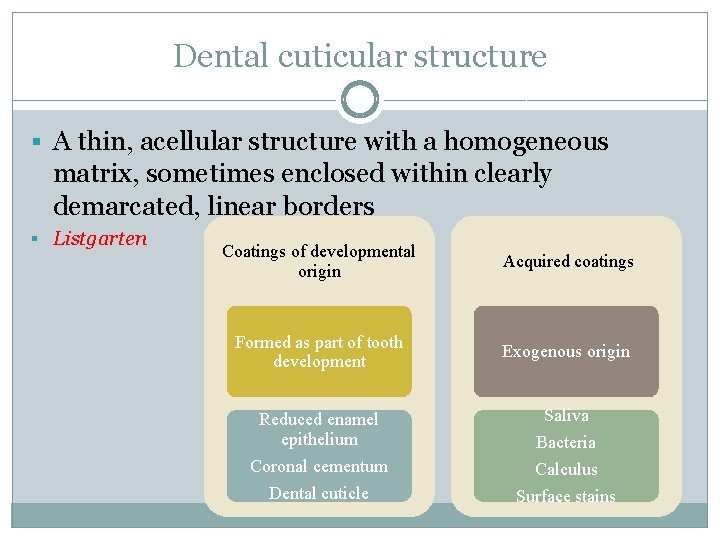
Dental cuticular structure § A thin, acellular structure with a homogeneous matrix, sometimes enclosed within clearly demarcated, linear borders § Listgarten Coatings of developmental origin Acquired coatings Formed as part of tooth development Exogenous origin Saliva Reduced enamel epithelium Coronal cementum Bacteria Calculus Dental cuticle Surface stains
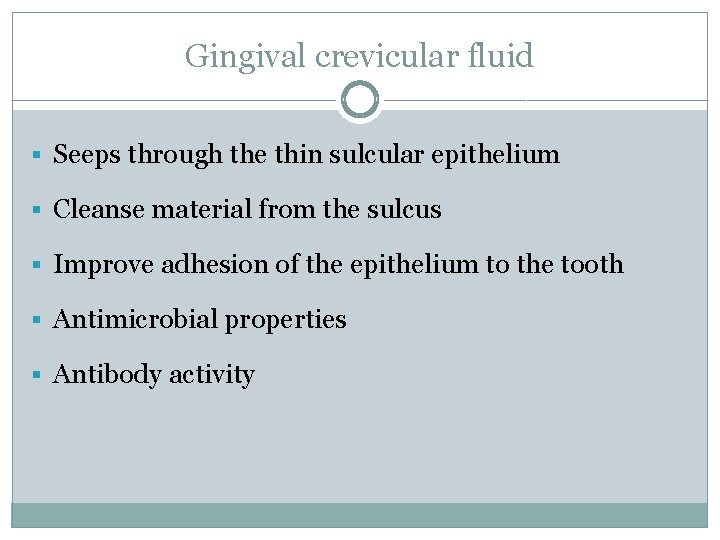
Gingival crevicular fluid § Seeps through the thin sulcular epithelium § Cleanse material from the sulcus § Improve adhesion of the epithelium to the tooth § Antimicrobial properties § Antibody activity

GINGIVA
CONTENTS q Introduction q Macroscopic features q Microscopic features q q q q Gingival epithelium Oral epithelium Sulcular epithelium Junctional epithelium Renewal of gingival epithelium Cuticular structures Gingival crevicular fluid Gingival connective tissue Gingival fibres Blood supply, nerve supply and lymphatics Correlation of clinical & microscopic features Age changes
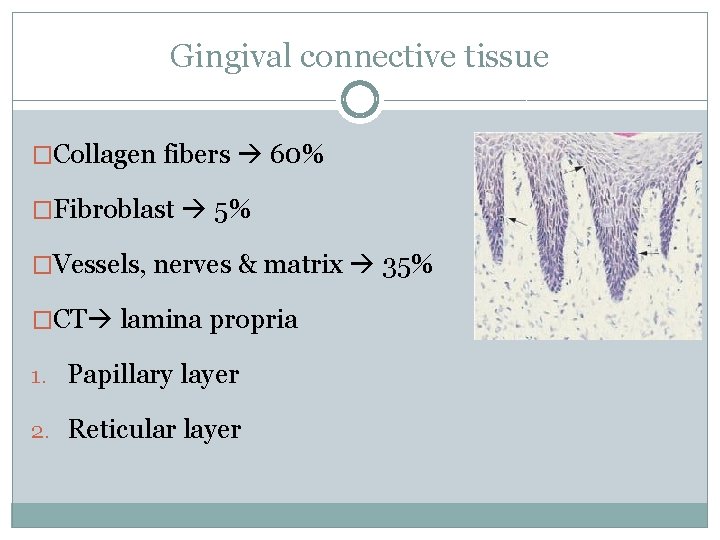
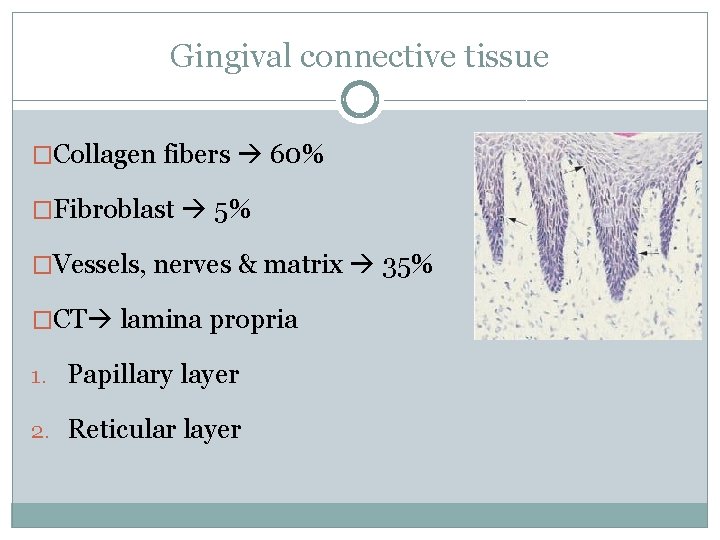
Gingival connective tissue �Collagen fibers 60% �Fibroblast 5% �Vessels, nerves & matrix 35% �CT lamina propria 1. Papillary layer 2. Reticular layer
Cellular Extracellular • Fibroblasts • Fibers • Mast cells • Ground substance • Macrophages • Inflammatory cells
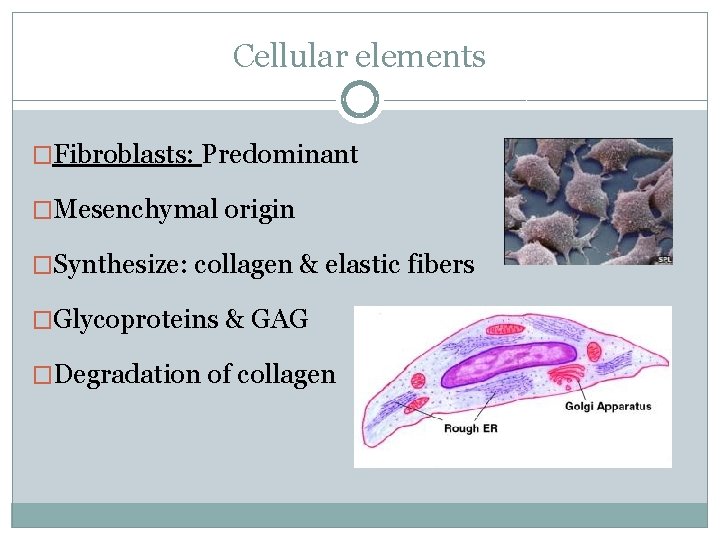
Cellular elements �Fibroblasts: Predominant �Mesenchymal origin �Synthesize: collagen & elastic fibers �Glycoproteins & GAG �Degradation of collagen
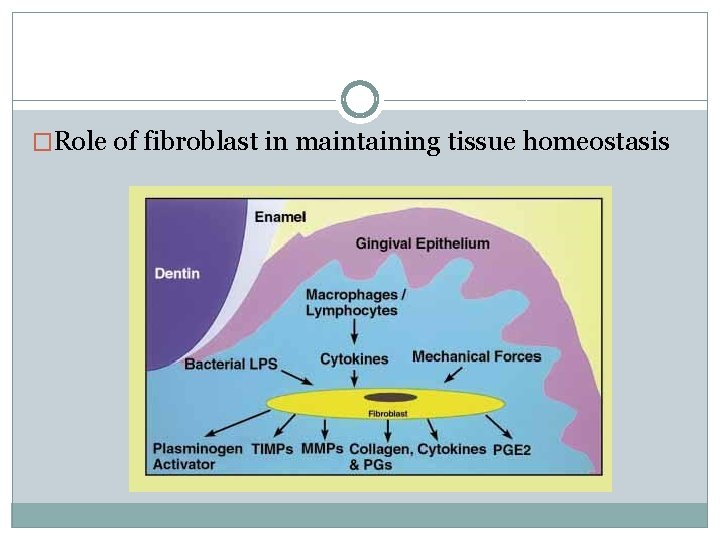
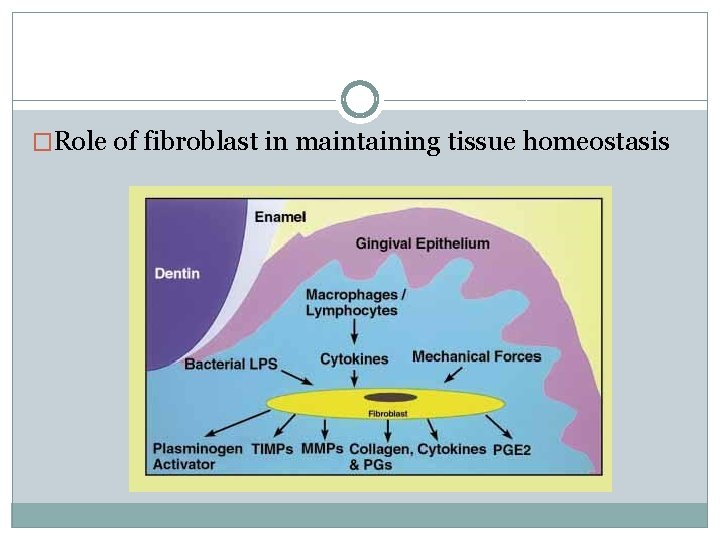
�Role of fibroblast in maintaining tissue homeostasis
�Mast cells: �Numerous, located perivascular region �Vasoactive substances: �Histamine �Heparin �Proteolytic enzymes
�Macrophages: �Phagocytic function �Numerous in inflammed tissue �Circulating blood monocytes
�Inflammatory cells: �Polymorphonuclear leukocytes �Lymphocytes �Plasma cells
§ Clinically normal gingiva : Small foci of plasma cell & lymphocytes : base of the sulcus § Neutrophils : High numbers in gingival connective tissue & sulcus § Recently erupted teeth in children : Area below the junctional epithelium of healthy gingiva : T-lymphocytes Early defense recognition system
§ As time elapses : B-lymphocytes & plasma cells ü Specific antibodies against already recognized antigens, always present in the sulcus of clinically normal gingiva
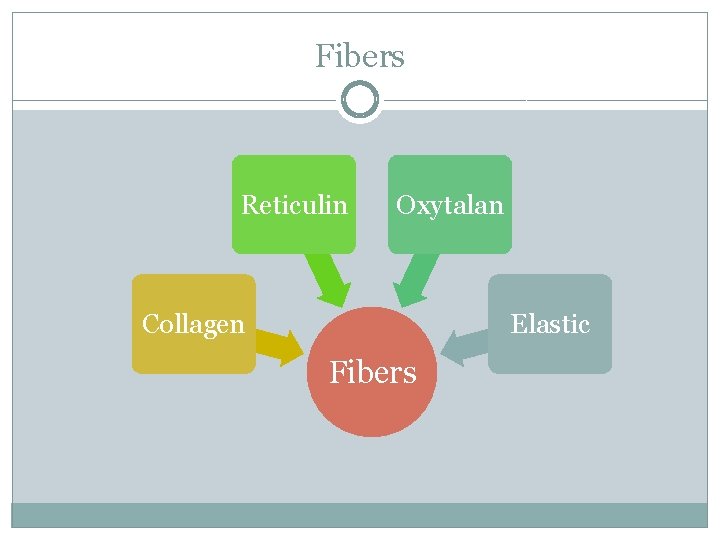
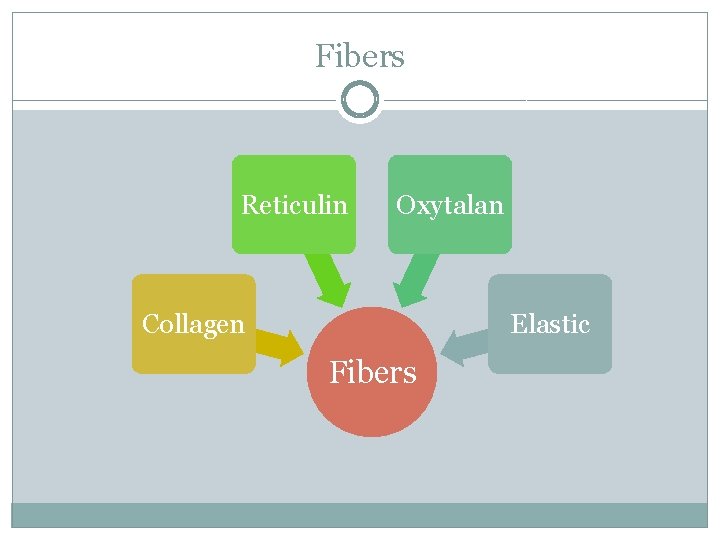
Fibers Reticulin Oxytalan Collagen Elastic Fibers
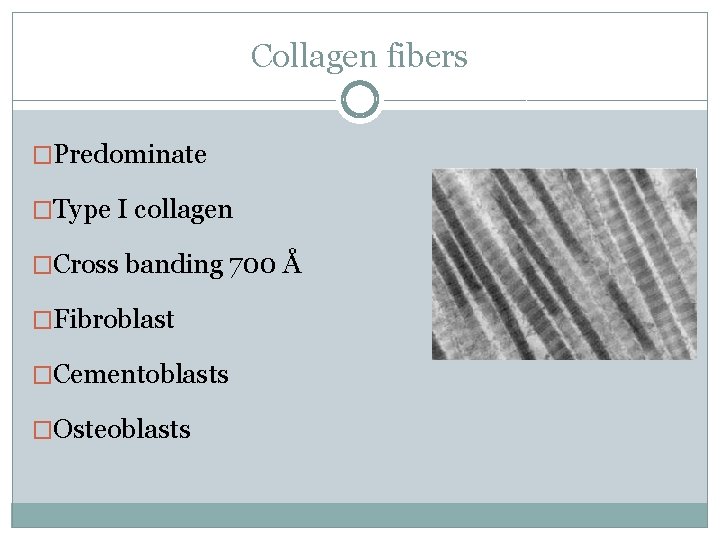
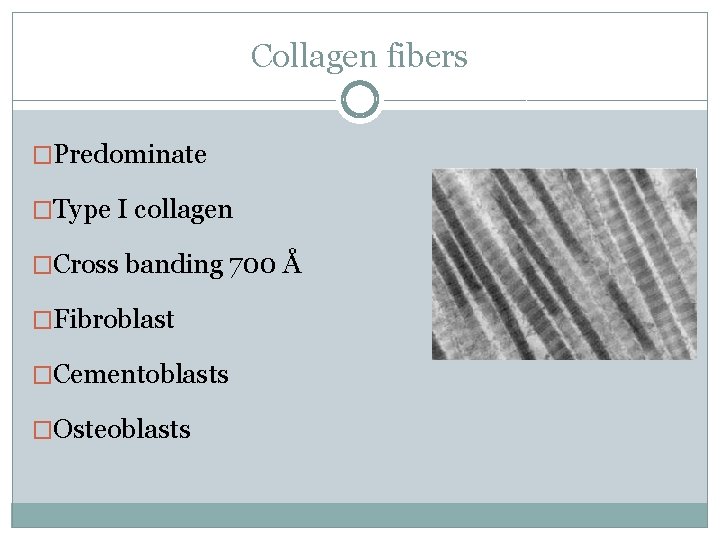
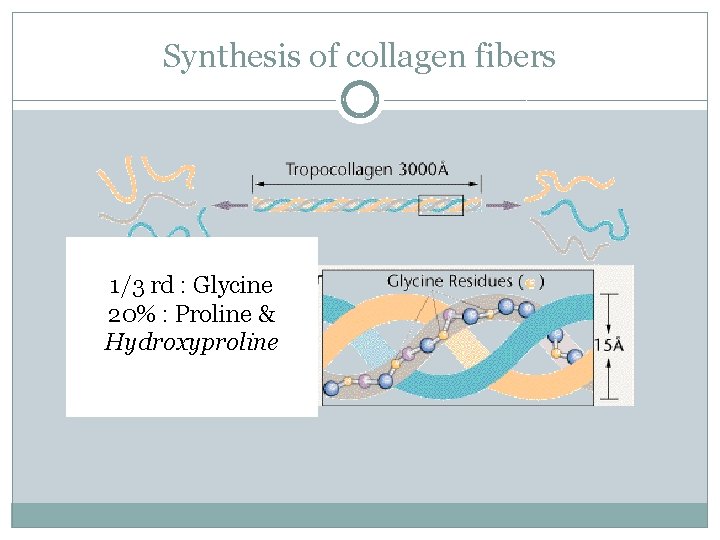
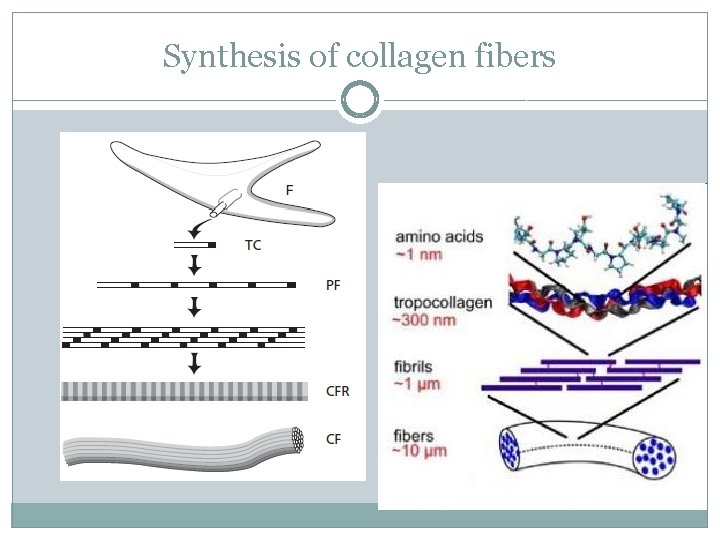
Collagen fibers �Predominate �Type I collagen �Cross banding 700 Å �Fibroblast �Cementoblasts �Osteoblasts
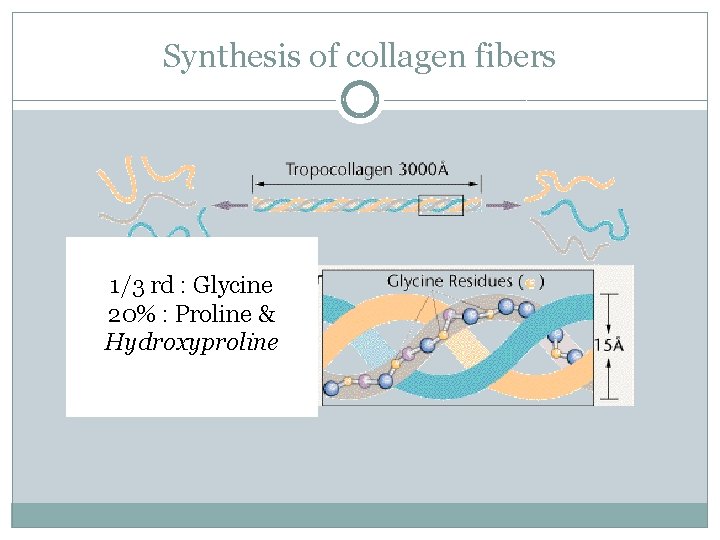
Synthesis of collagen fibers 1/3 rd : Glycine 20% : Proline & Hydroxyproline
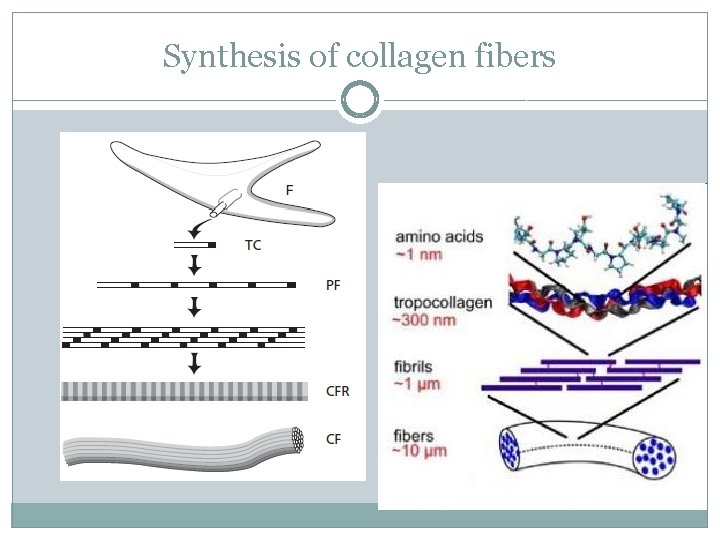
Synthesis of collagen fibers
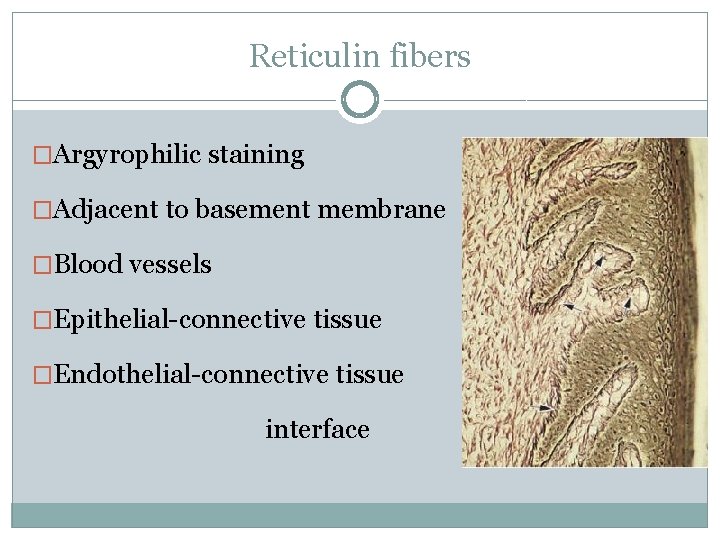
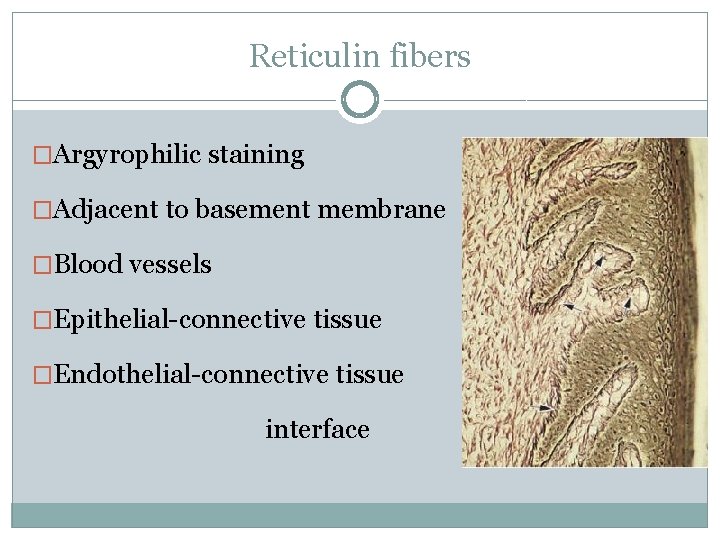
Reticulin fibers �Argyrophilic staining �Adjacent to basement membrane �Blood vessels �Epithelial-connective tissue �Endothelial-connective tissue interface
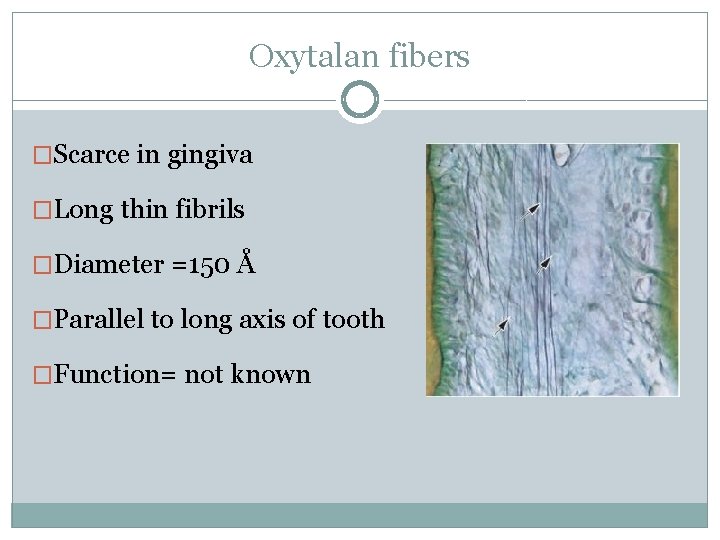
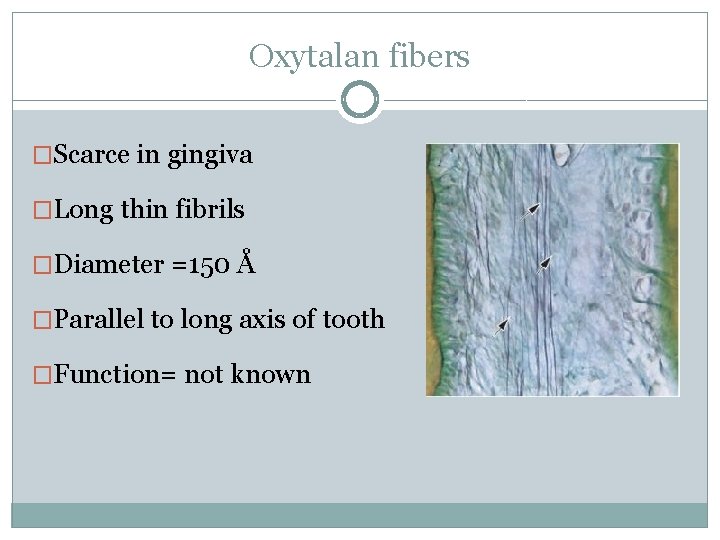
Oxytalan fibers �Scarce in gingiva �Long thin fibrils �Diameter =150 Å �Parallel to long axis of tooth �Function= not known
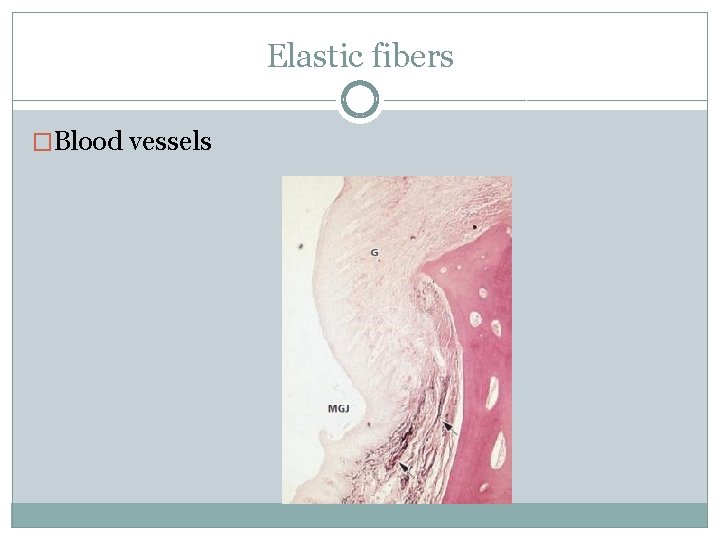
Elastic fibers �Blood vessels
Functions: �To brace marginal gingiva firmly against the tooth �To provide the rigidity necessary to withstand the forces of mastication without being deflected away from tooth surface �To unite the free marginal gingiva with the cementum of the root & the adjacent attached gingiva
�Principal groups Arnim S, Hargerman D. 1953 �Secondary groups Page R 1974
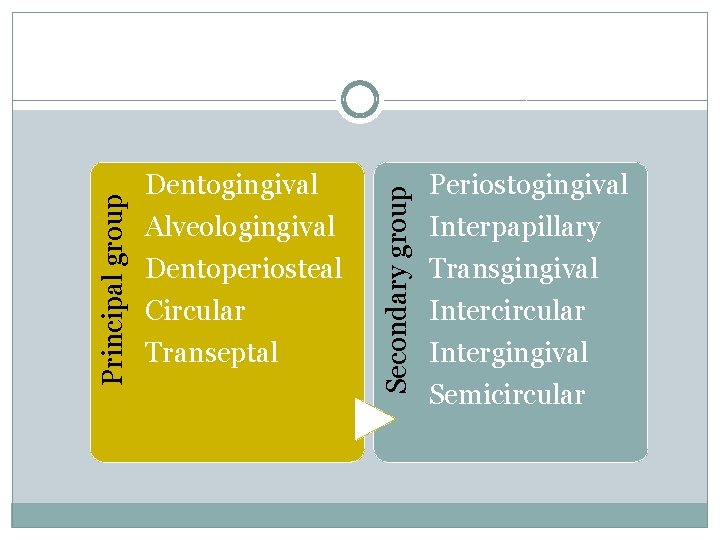
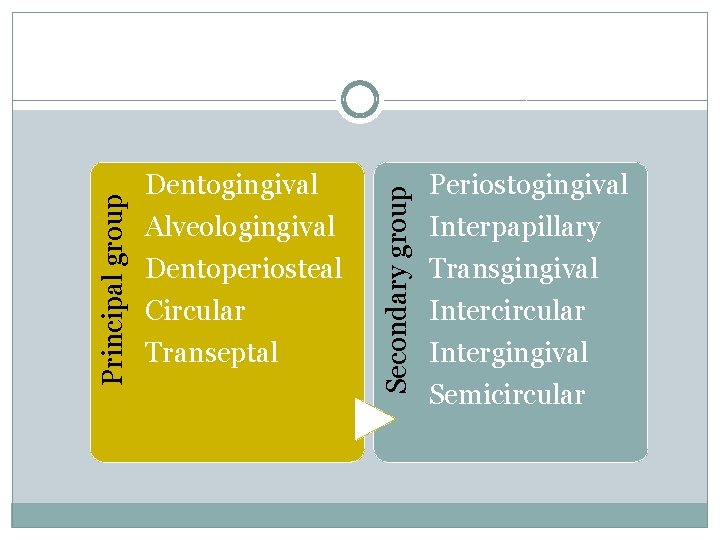
Alveologingival Dentoperiosteal Circular Transeptal Secondary group Principal group Dentogingival Periostogingival Interpapillary Transgingival Intercircular Intergingival Semicircular
Principal group
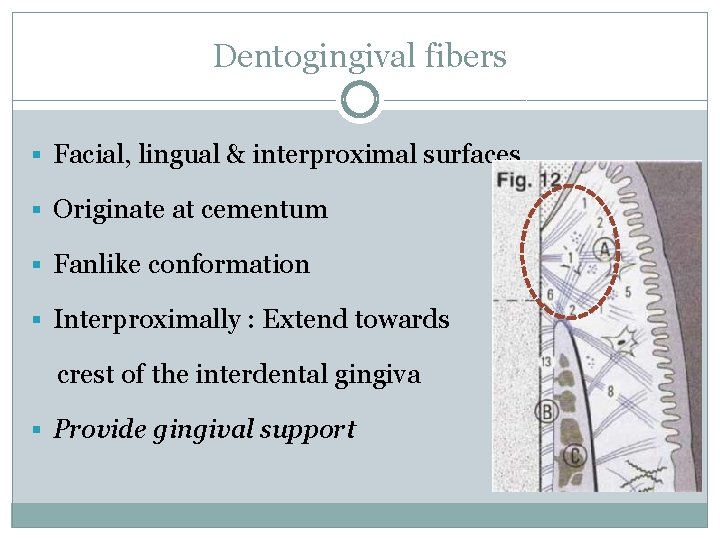
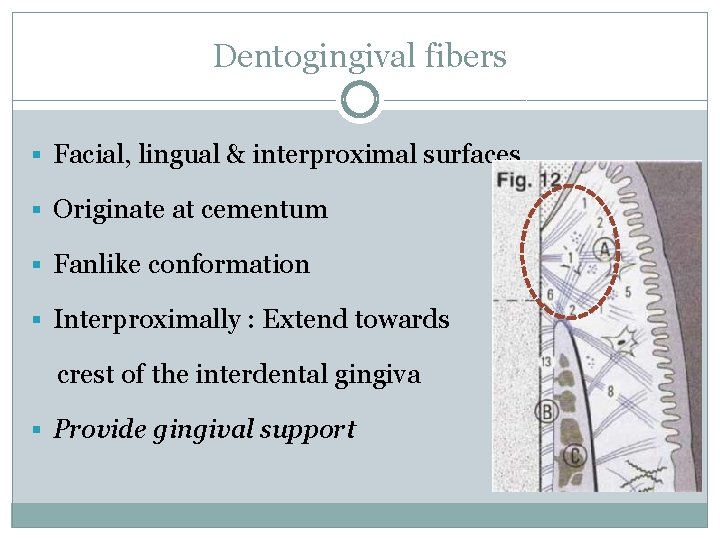
Dentogingival fibers § Facial, lingual & interproximal surfaces § Originate at cementum § Fanlike conformation § Interproximally : Extend towards crest of the interdental gingiva § Provide gingival support
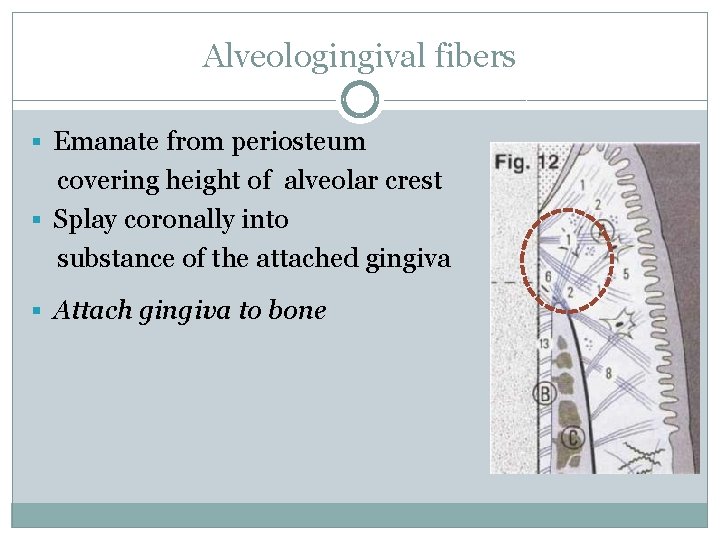
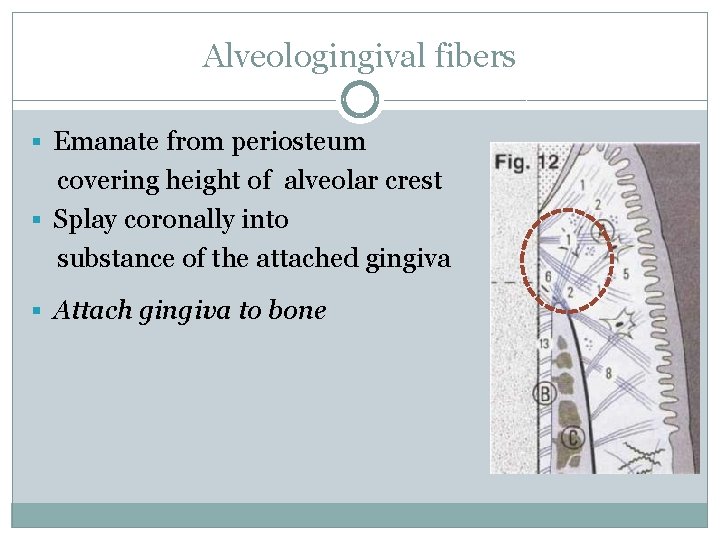
Alveologingival fibers § Emanate from periosteum covering height of alveolar crest § Splay coronally into substance of the attached gingiva § Attach gingiva to bone
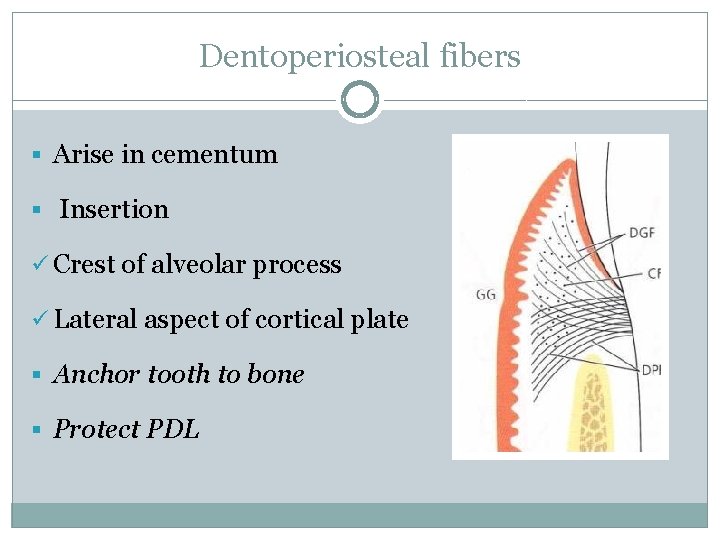
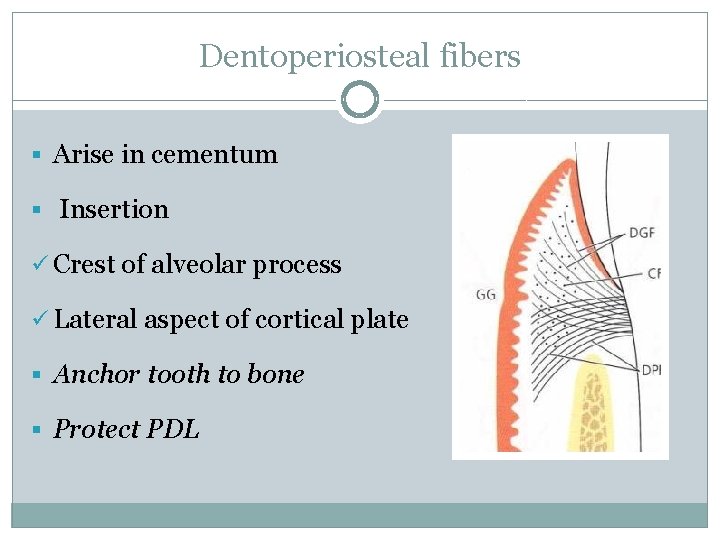
Dentoperiosteal fibers § Arise in cementum § Insertion ü Crest of alveolar process ü Lateral aspect of cortical plate § Anchor tooth to bone § Protect PDL
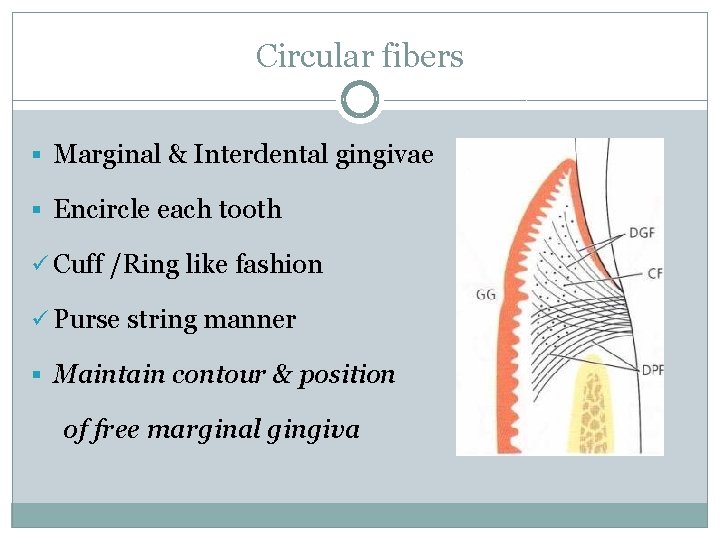
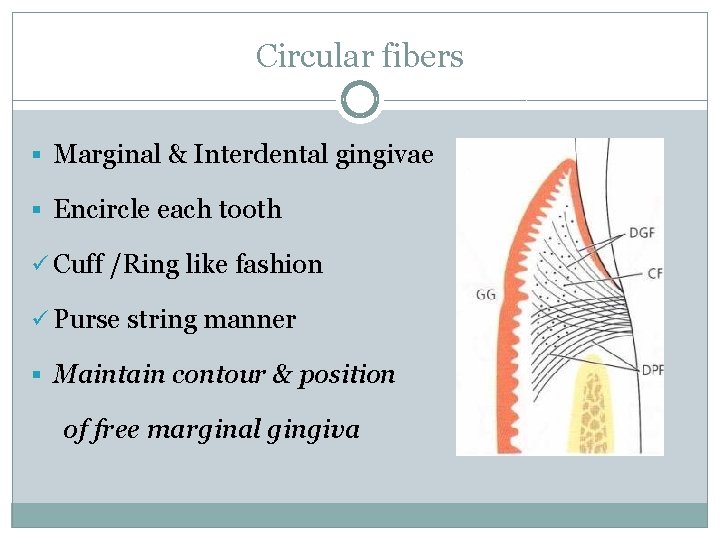
Circular fibers § Marginal & Interdental gingivae § Encircle each tooth ü Cuff /Ring like fashion ü Purse string manner § Maintain contour & position of free marginal gingiva
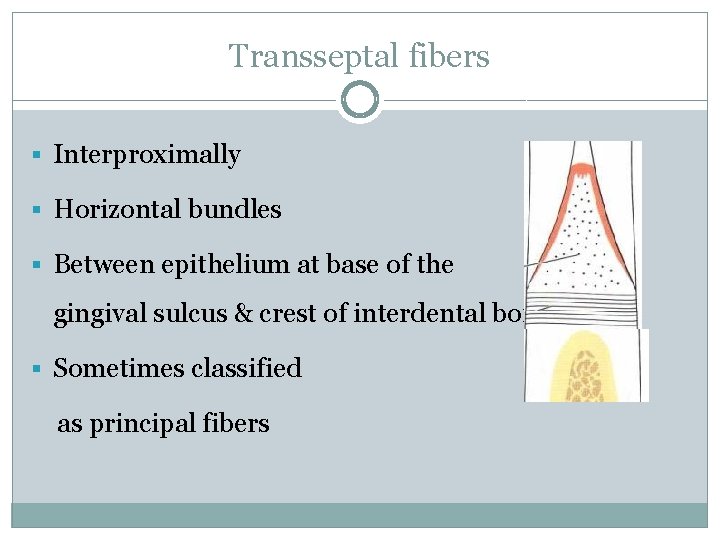
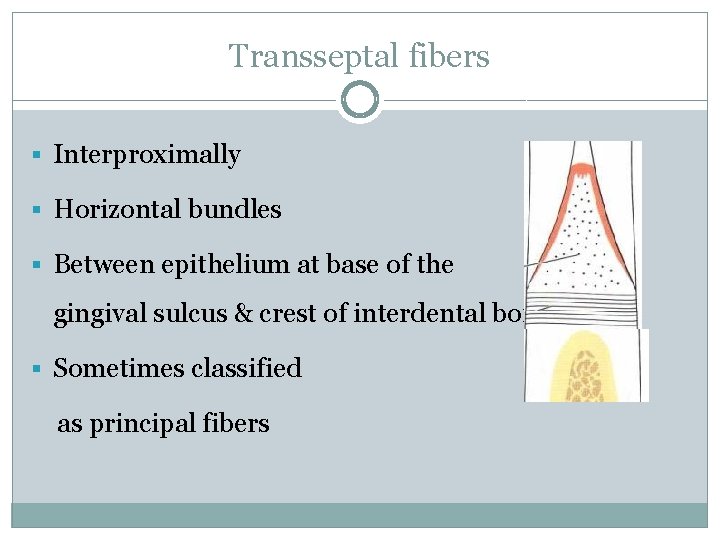
Transseptal fibers § Interproximally § Horizontal bundles § Between epithelium at base of the gingival sulcus & crest of interdental bone § Sometimes classified as principal fibers
§ Support for interdental gingiva § Secure positions of adjacent teeth § Protect interproximal bone § Maintain integrity of dentition within dental arch
Secondary group
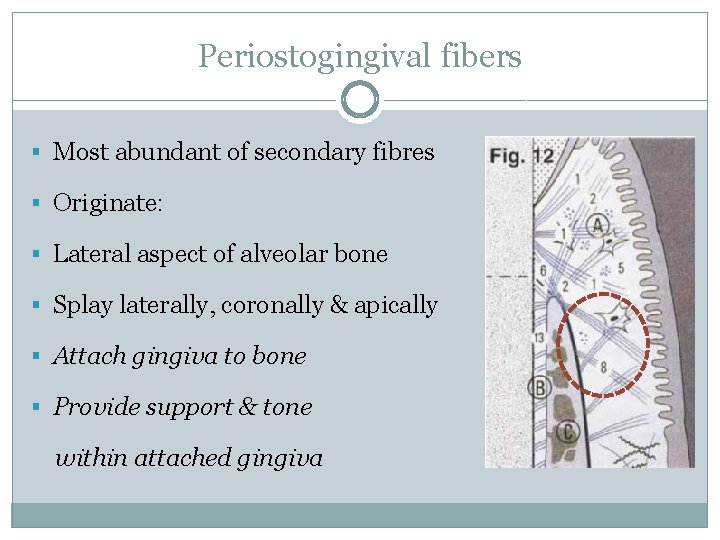
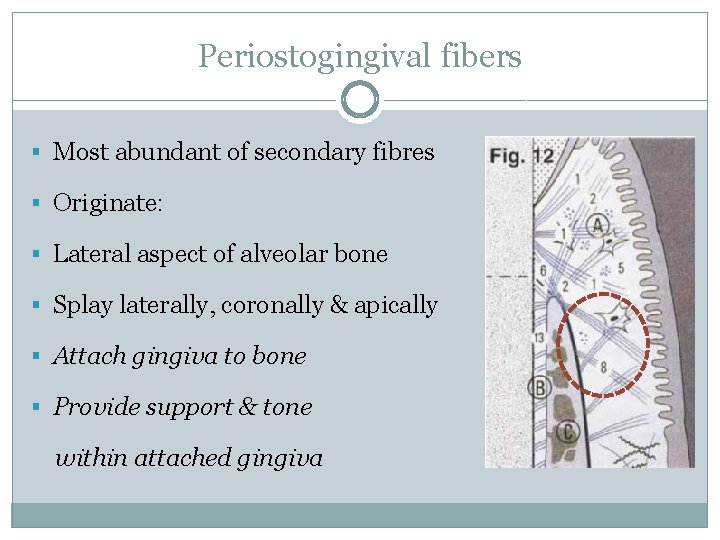
Periostogingival fibers § Most abundant of secondary fibres § Originate: § Lateral aspect of alveolar bone § Splay laterally, coronally & apically § Attach gingiva to bone § Provide support & tone within attached gingiva
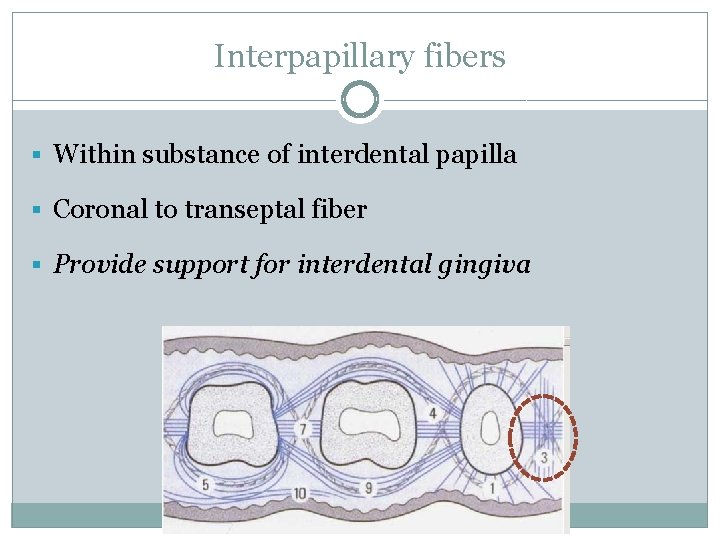
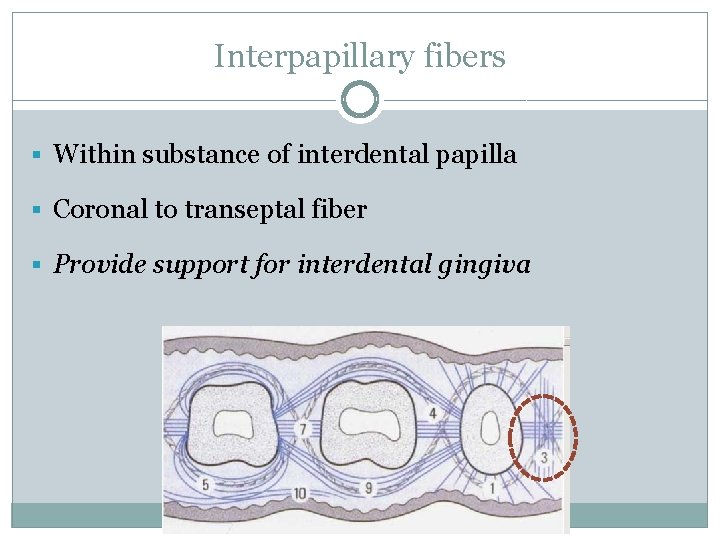
Interpapillary fibers § Within substance of interdental papilla § Coronal to transeptal fiber § Provide support for interdental gingiva
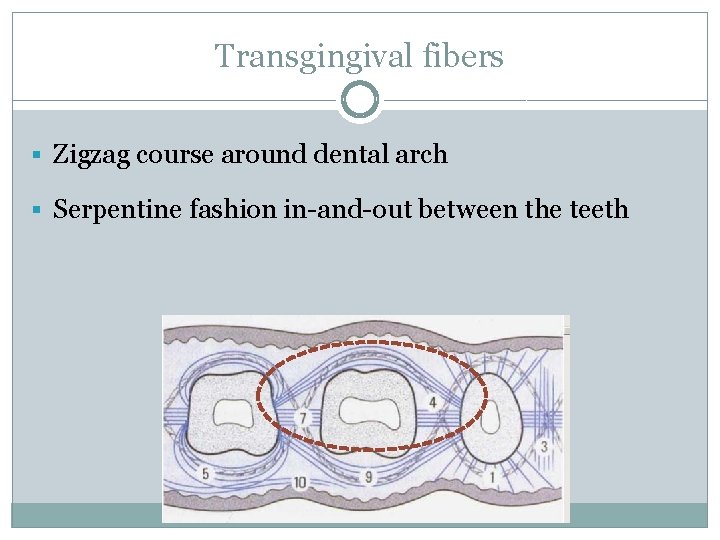
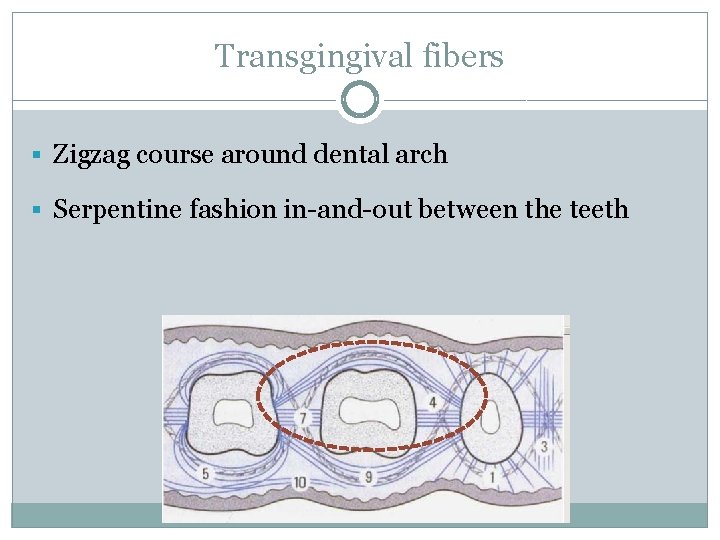
Transgingival fibers § Zigzag course around dental arch § Serpentine fashion in-and-out between the teeth
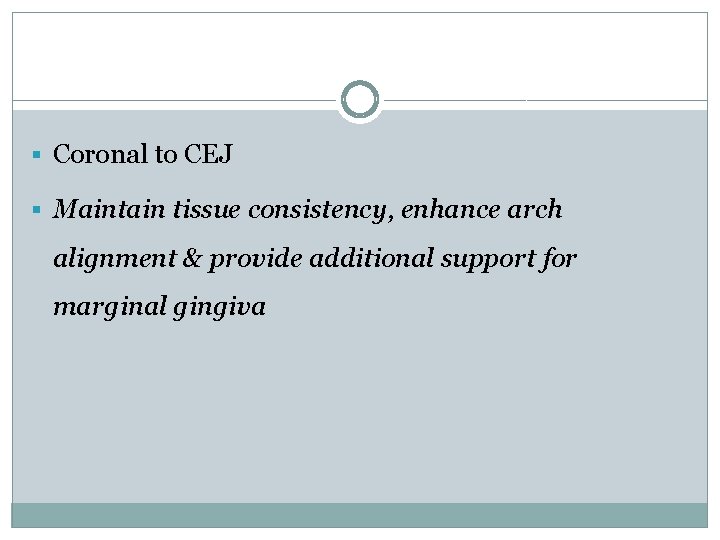
§ Coronal to CEJ § Maintain tissue consistency, enhance arch alignment & provide additional support for marginal gingiva
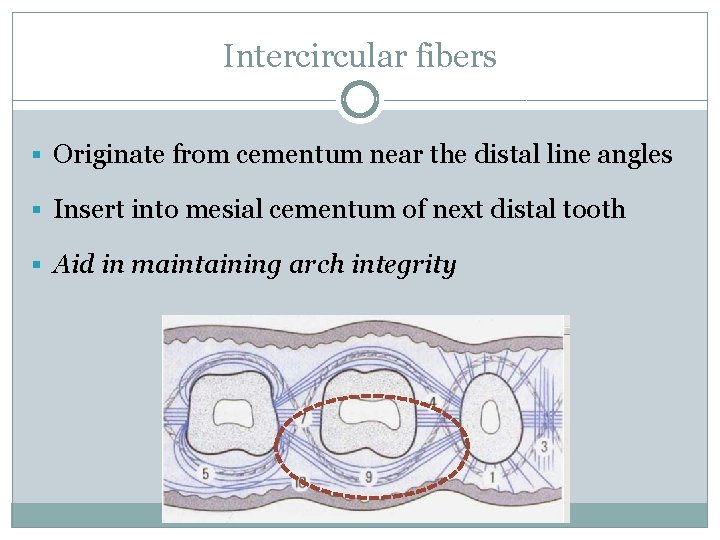
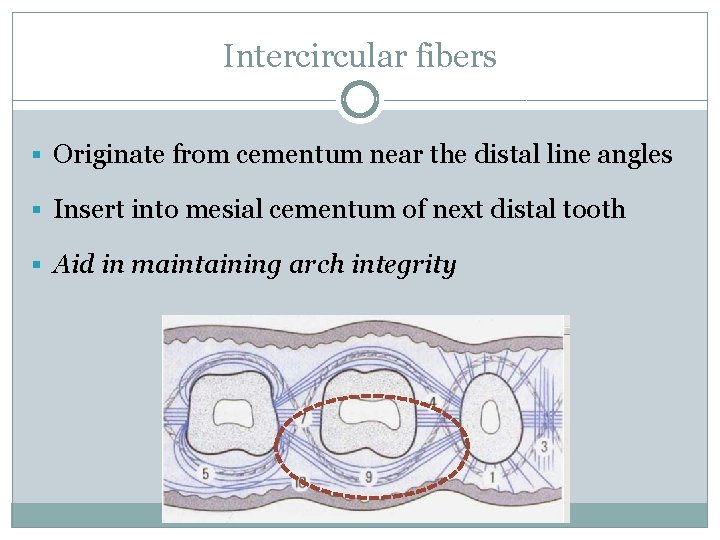
Intercircular fibers § Originate from cementum near the distal line angles § Insert into mesial cementum of next distal tooth § Aid in maintaining arch integrity
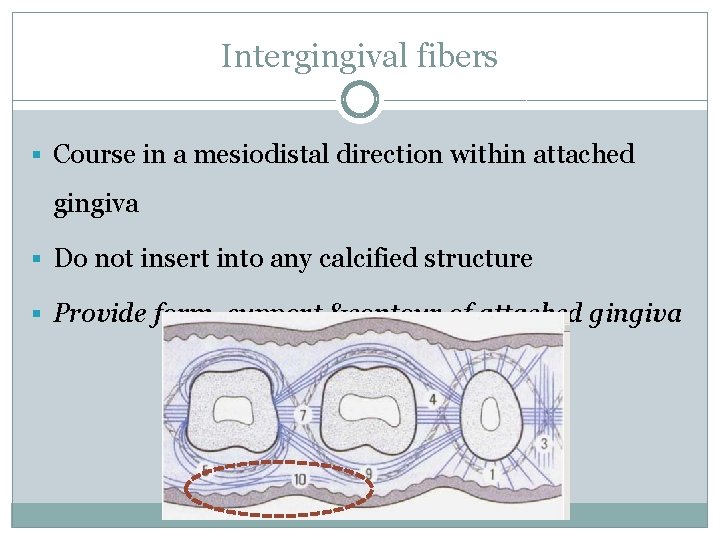
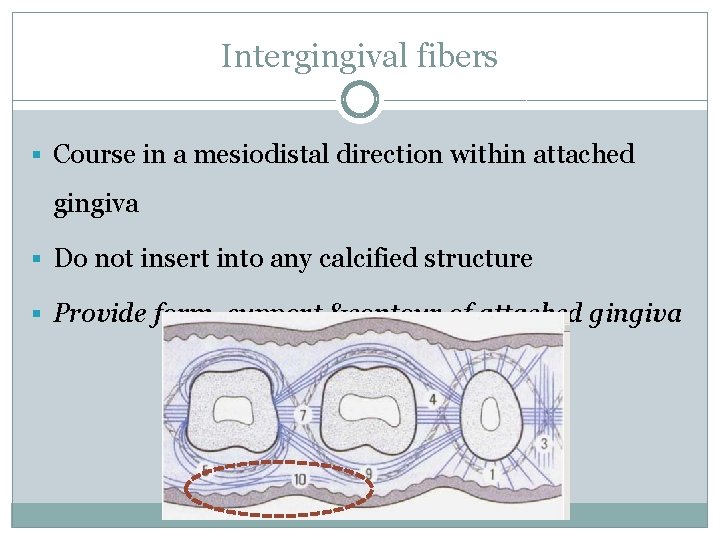
Intergingival fibers § Course in a mesiodistal direction within attached gingiva § Do not insert into any calcified structure § Provide form, support &contour of attached gingiva
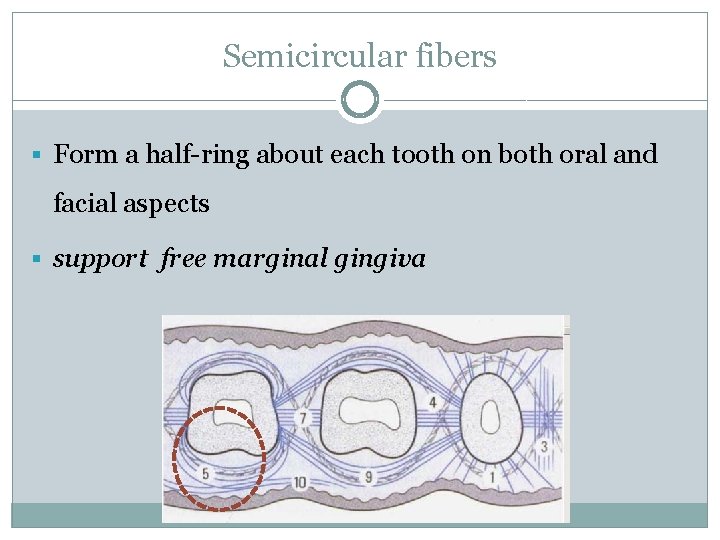
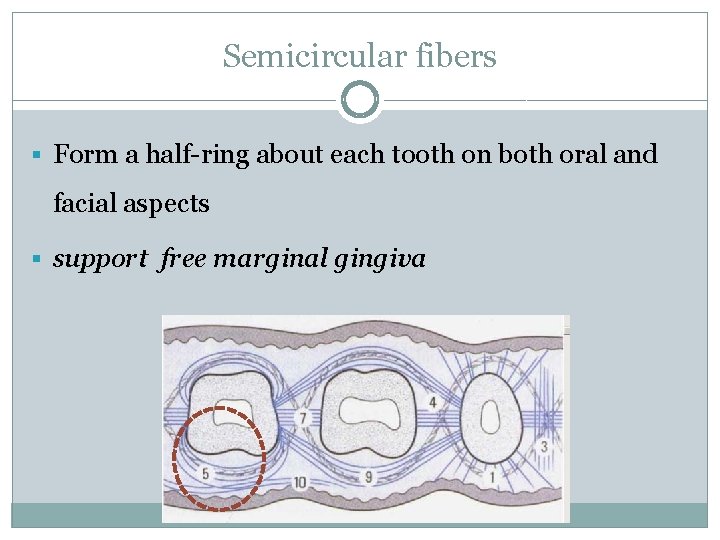
Semicircular fibers § Form a half-ring about each tooth on both oral and facial aspects § support free marginal gingiva
Ground substance § Fills the space between fibers & cells § Amorphous § Water § Proteoglycan § Glycoprotein
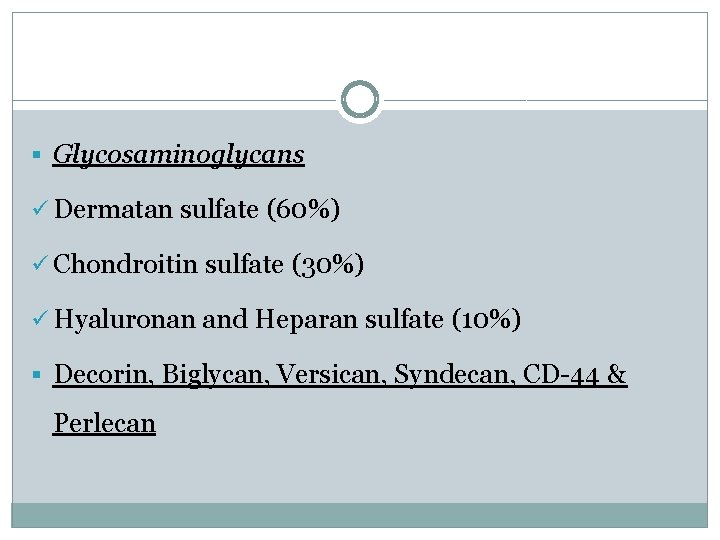
§ Glycosaminoglycans ü Dermatan sulfate (60%) ü Chondroitin sulfate (30%) ü Hyaluronan and Heparan sulfate (10%) § Decorin, Biglycan, Versican, Syndecan, CD-44 & Perlecan
§ Glycoprotein ü Fibronectin � Distributed throughout gingival connective tissues � Localized over collagen fibers � Binds fibroblasts to fibers � Mediate cell adhesion & migration
ü Osteonectin, Vitronectin, Elastin & Tenascin �Present diffusely �Near the subepithelial basement membrane in the upper connective tissue & capillary blood vessels ü Laminin �Basal laminae �Attach it to epithelial cells
Repair of gingival connective tissue § High turnover rate § Remarkably good healing and regenerative capacity § Generally shows little evidence of scarring after surgical procedures § Rapid reconstruction of the fibrous architecture of tissues Melcher 1976
§ Within hours ü Wound site stabilized by fibrin clot formation ü Heavy infiltrate of neutrophils § Within 3 days ü Granulation tissue evident ü Heavily infiltrate of inflammatory cells ü Fibrin clot is slowly degraded
§ Day 7 ü Rich in newly formed granulation tissue ü Collagen fibers align parallel along root surface § Day 14 ü Collagen fibers show signs of attachment to root surface § 3 weeks
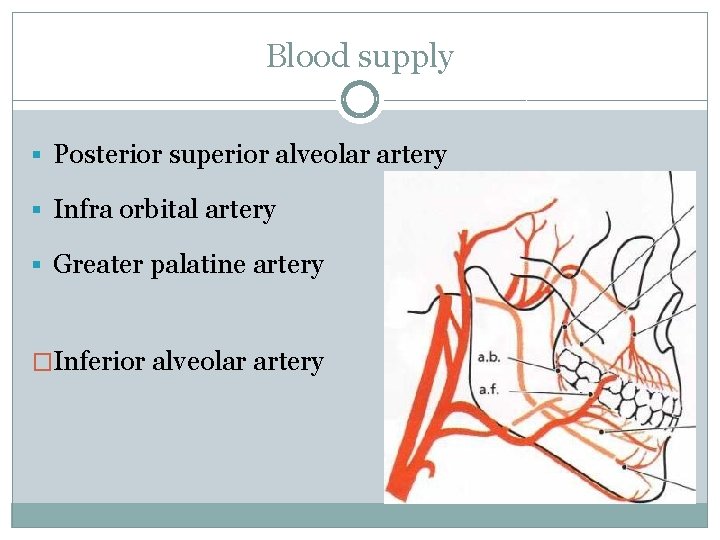
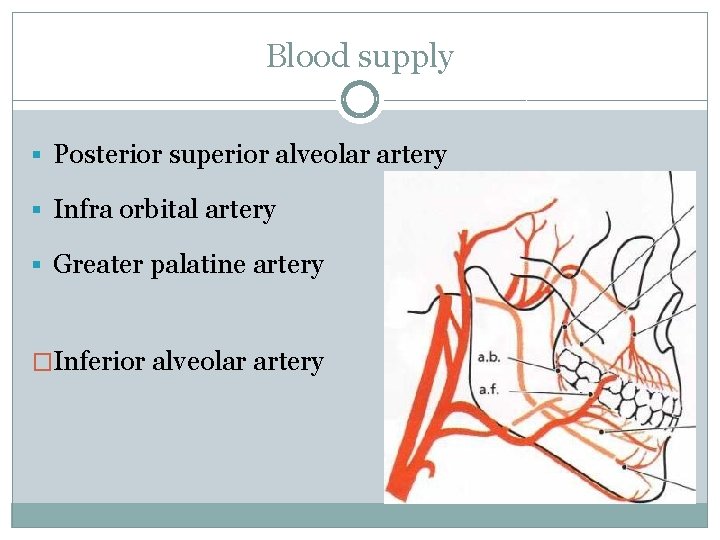
Blood supply § Posterior superior alveolar artery § Infra orbital artery § Greater palatine artery �Inferior alveolar artery
�Supraperiosteal arterioles �Arterioles from crest of interdental septa �Vessels of PDL
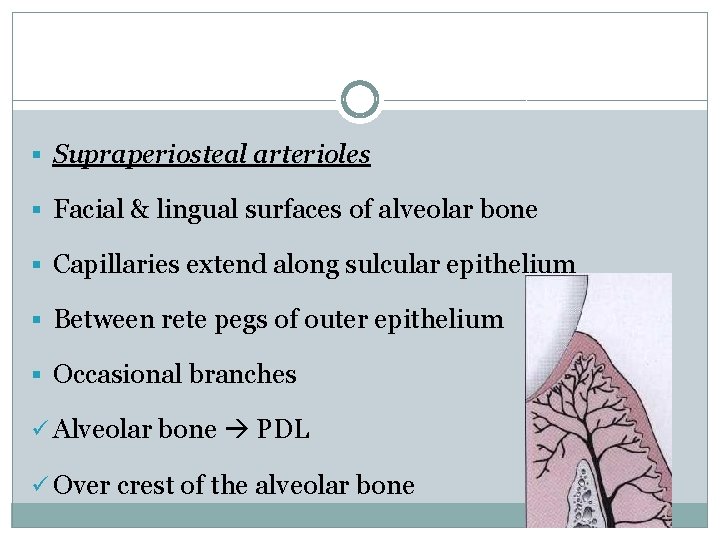
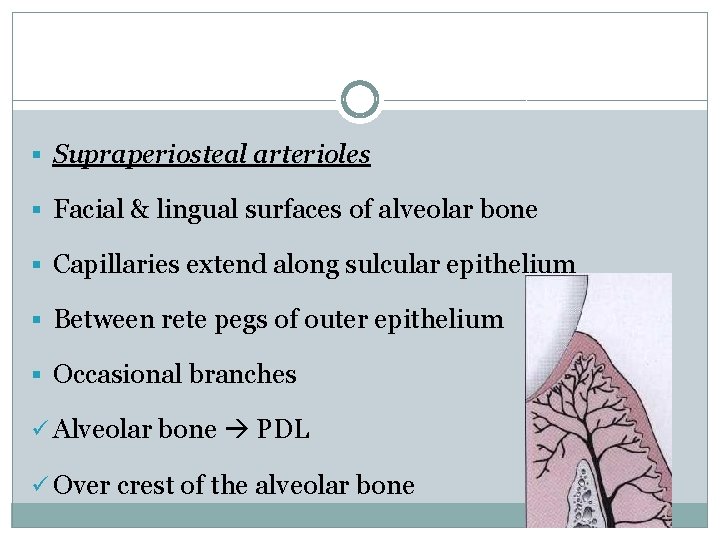
§ Supraperiosteal arterioles § Facial & lingual surfaces of alveolar bone § Capillaries extend along sulcular epithelium § Between rete pegs of outer epithelium § Occasional branches ü Alveolar bone PDL ü Over crest of the alveolar bone
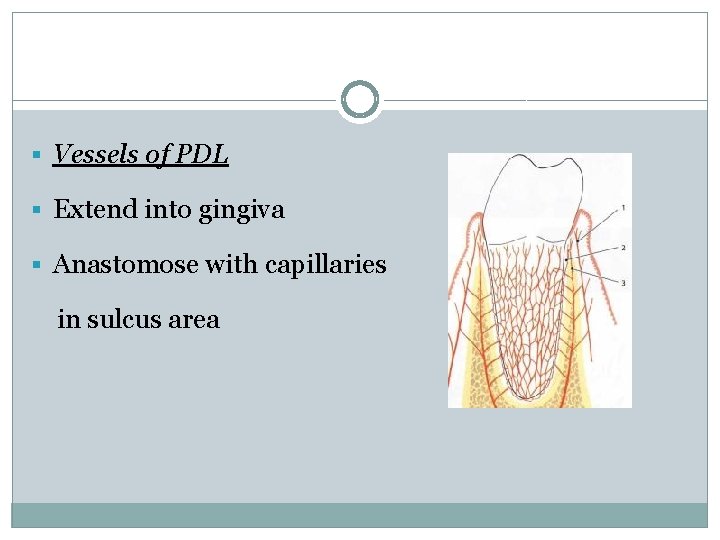
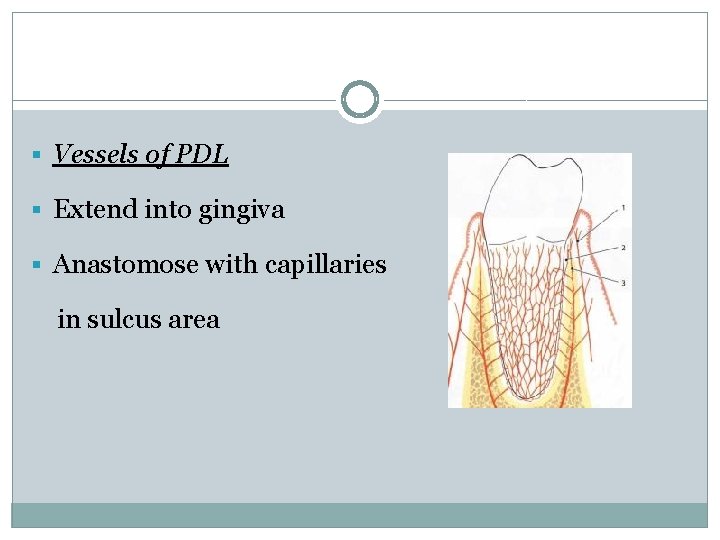
§ Vessels of PDL § Extend into gingiva § Anastomose with capillaries in sulcus area
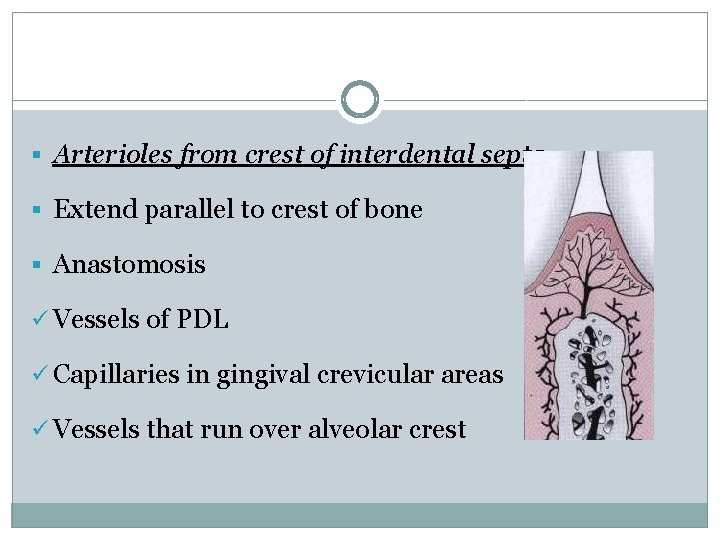
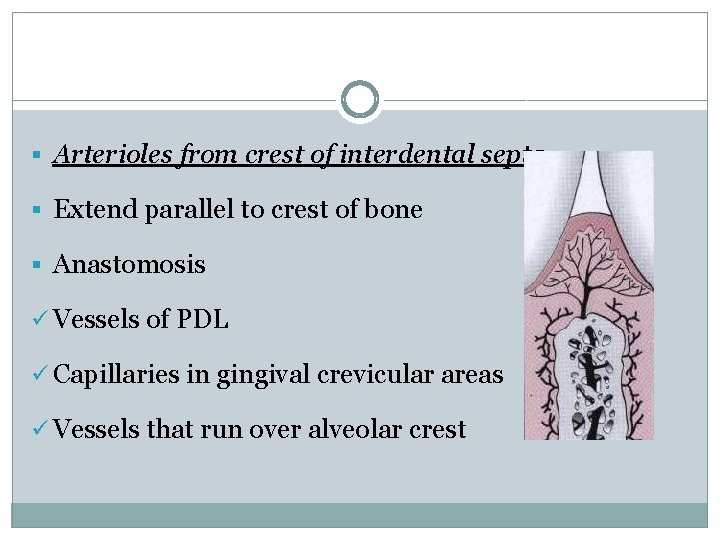
§ Arterioles from crest of interdental septa § Extend parallel to crest of bone § Anastomosis ü Vessels of PDL ü Capillaries in gingival crevicular areas ü Vessels that run over alveolar crest
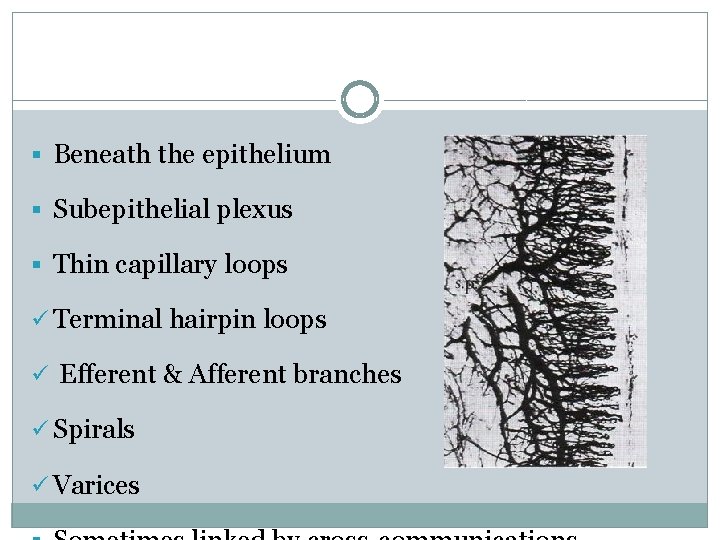
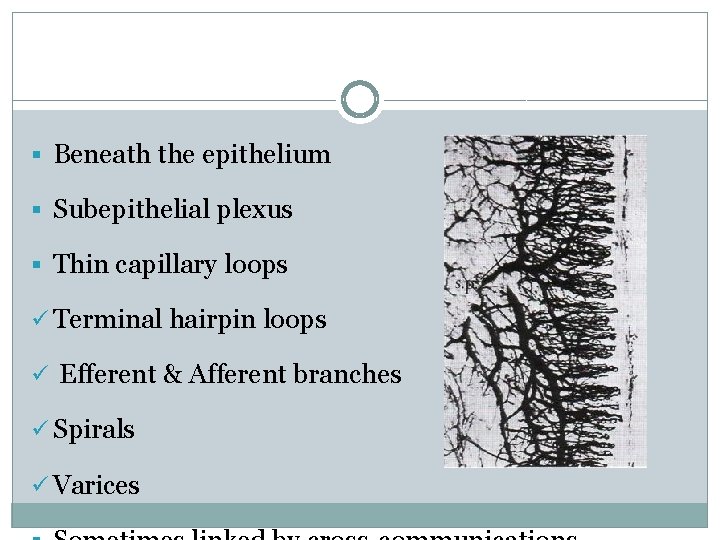
§ Beneath the epithelium § Subepithelial plexus § Thin capillary loops ü Terminal hairpin loops ü Efferent & Afferent branches ü Spirals ü Varices
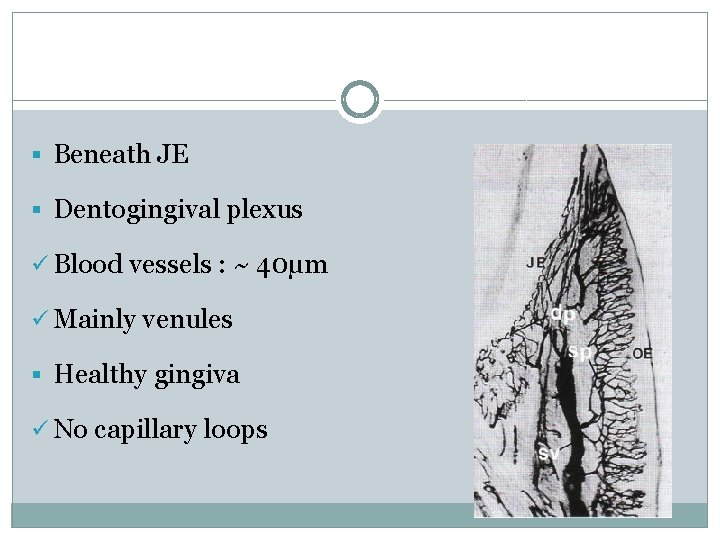
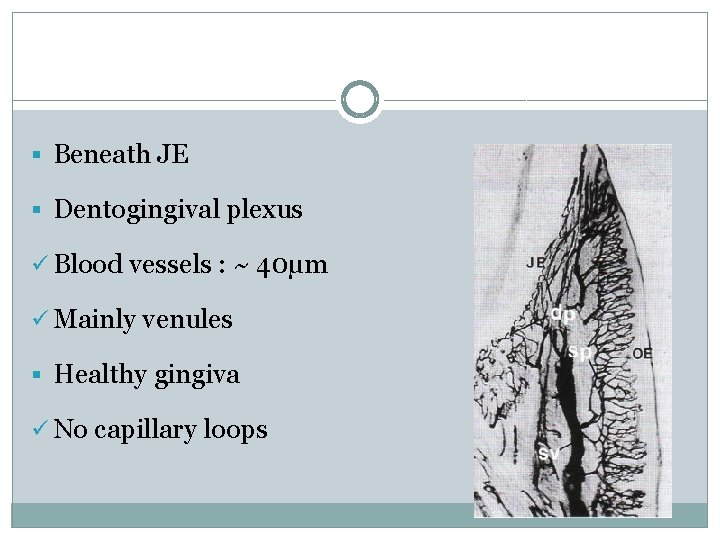
§ Beneath JE § Dentogingival plexus ü Blood vessels : ~ 40µm ü Mainly venules § Healthy gingiva ü No capillary loops

§ Sulcular epithelium : Flat anastomosing plexus § Col area : Mixed pattern of anastomosing capillaries & loops § Absence of inflammation ü Regular, repetitive & layered pattern § Inflamed gingival vasculature ü Irregular vascular plexus pattern
Lymphatics § Remove excess fluids, cellular and protein debris, microorganisms & other elements § Control diffusion § Resolution of inflammatory processes
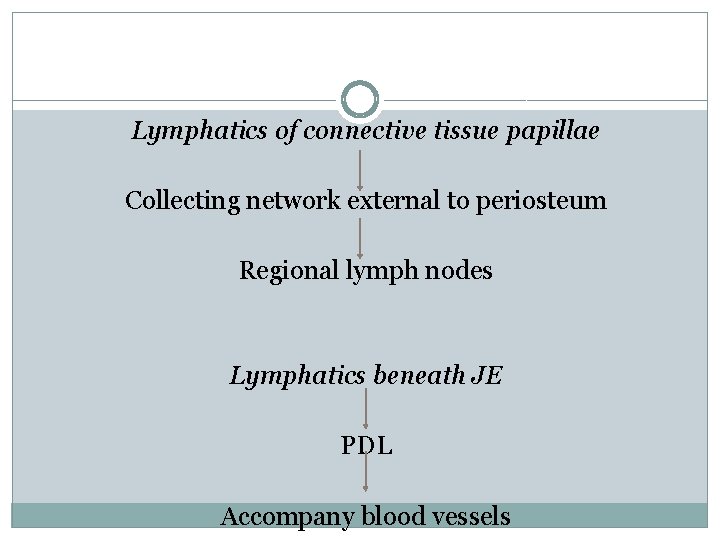
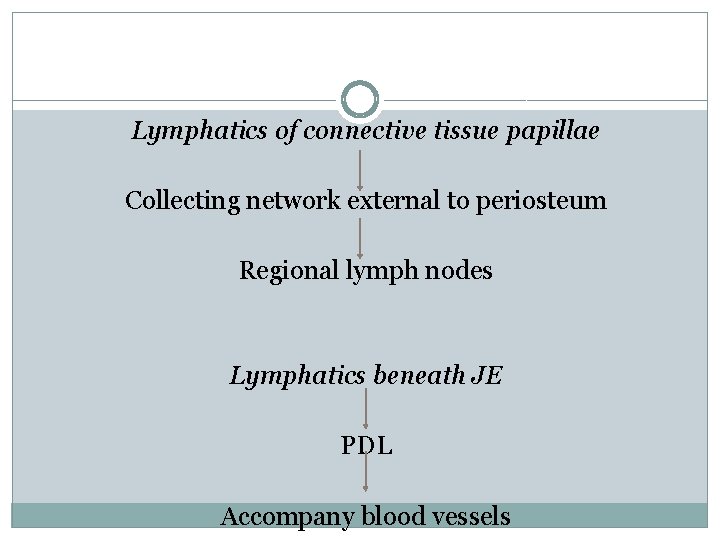
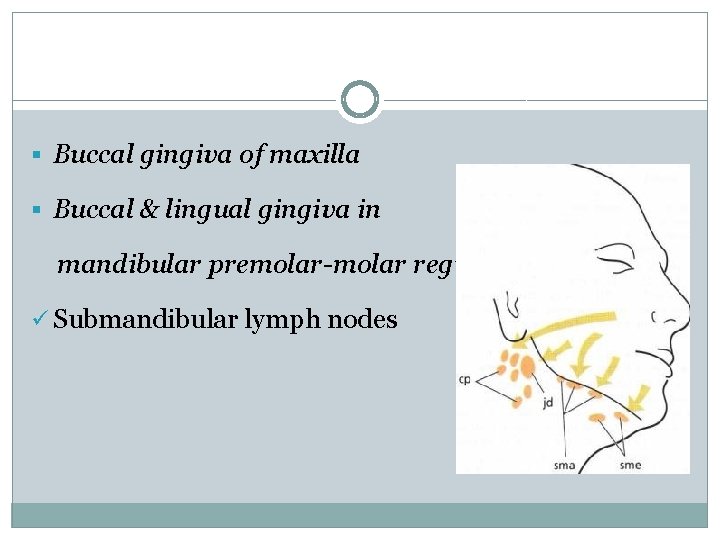
Lymphatics of connective tissue papillae Collecting network external to periosteum Regional lymph nodes Lymphatics beneath JE PDL Accompany blood vessels
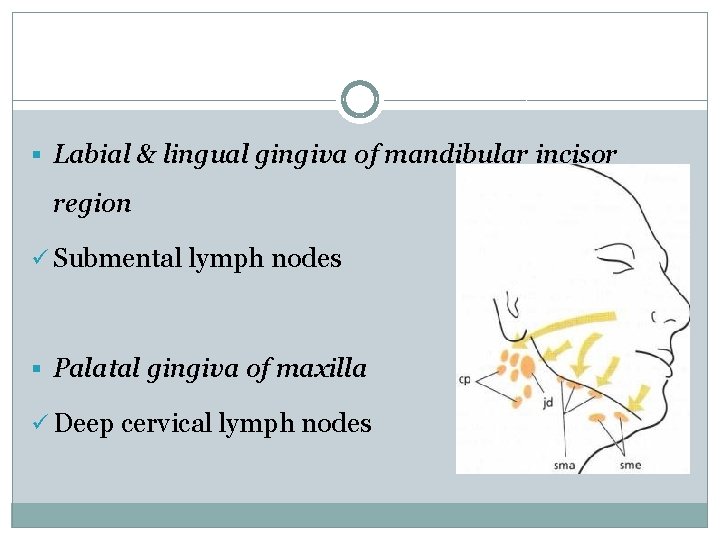
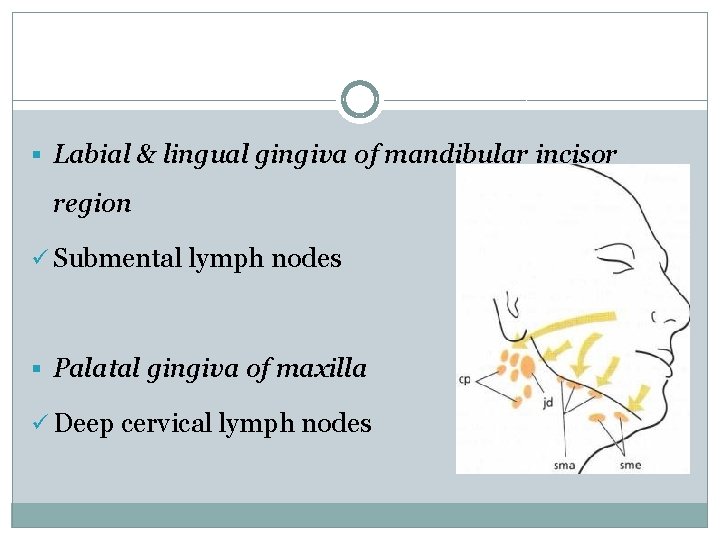
§ Labial & lingual gingiva of mandibular incisor region ü Submental lymph nodes § Palatal gingiva of maxilla ü Deep cervical lymph nodes
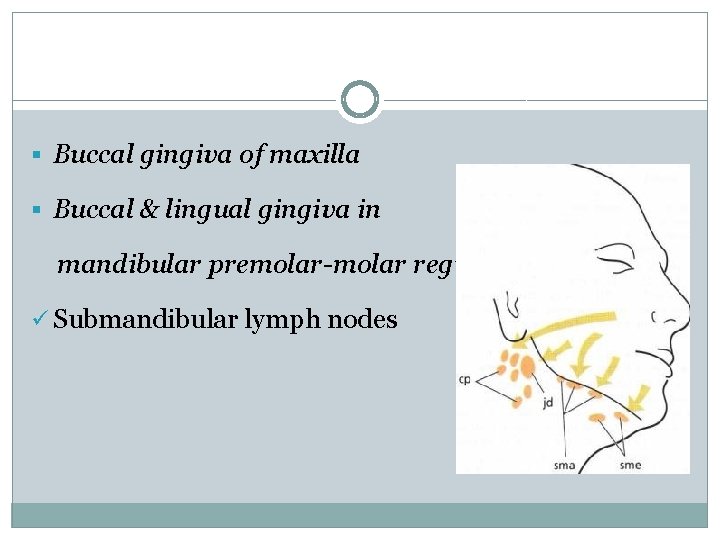
§ Buccal gingiva of maxilla § Buccal & lingual gingiva in mandibular premolar-molar region ü Submandibular lymph nodes
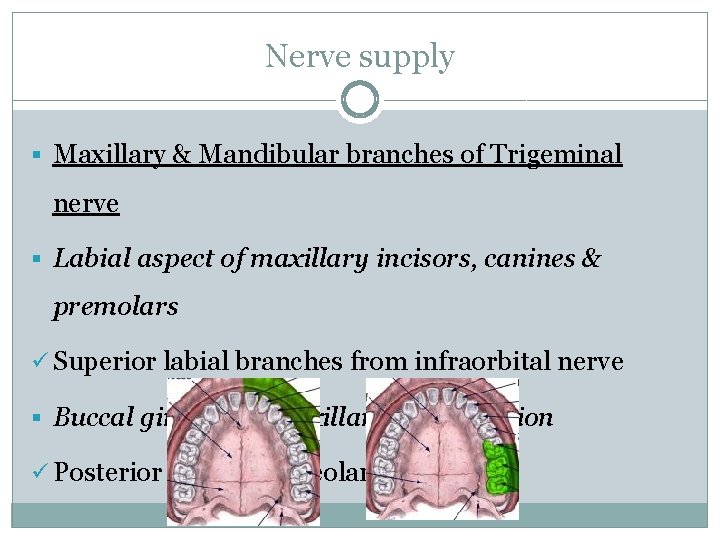
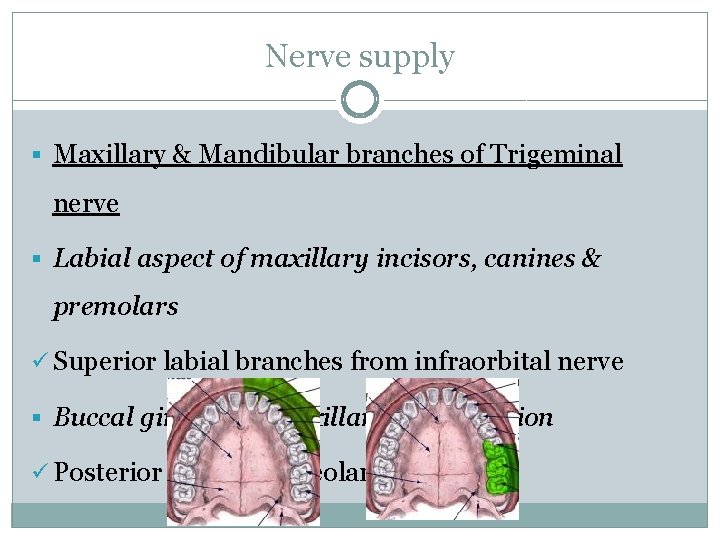
Nerve supply § Maxillary & Mandibular branches of Trigeminal nerve § Labial aspect of maxillary incisors, canines & premolars ü Superior labial branches from infraorbital nerve § Buccal gingiva in maxillary molar region ü Posterior superior alveolar nerve
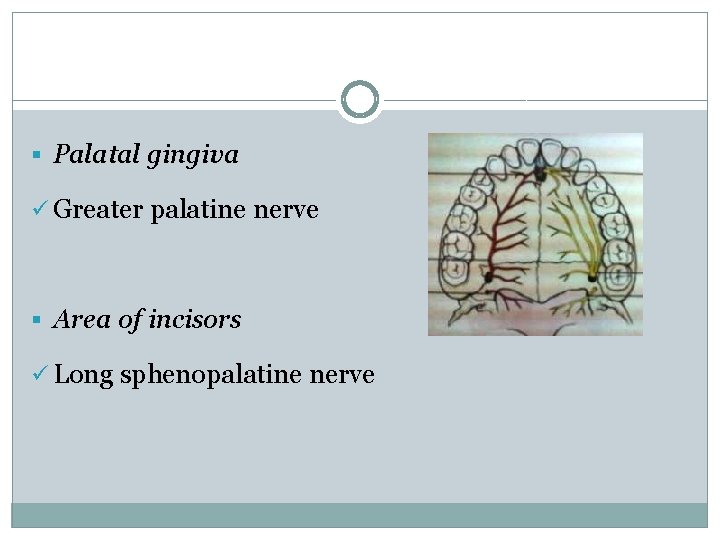
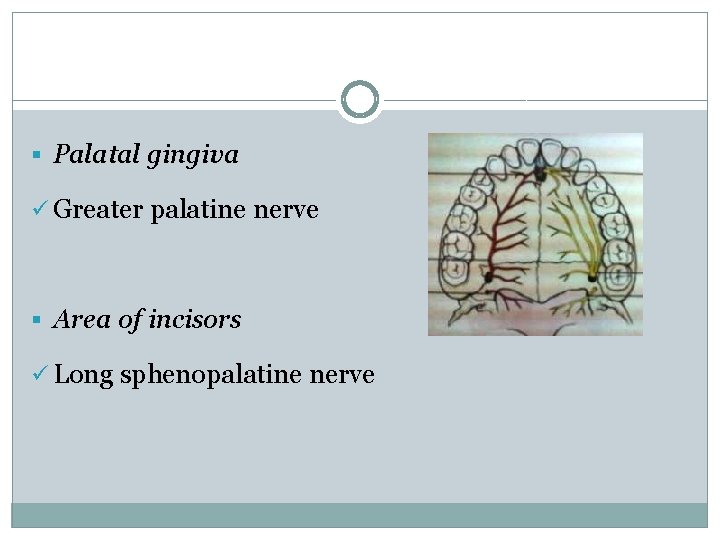
§ Palatal gingiva ü Greater palatine nerve § Area of incisors ü Long sphenopalatine nerve
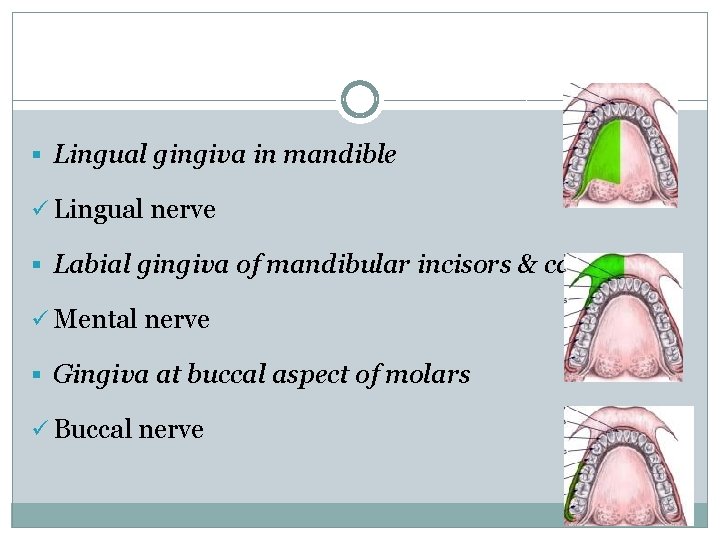
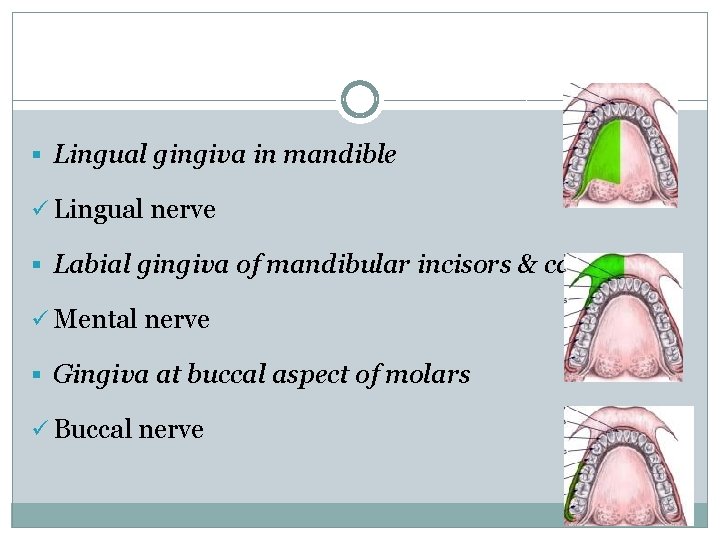
§ Lingual gingiva in mandible ü Lingual nerve § Labial gingiva of mandibular incisors & canines ü Mental nerve § Gingiva at buccal aspect of molars ü Buccal nerve
§ Gingival connective tissues § Most nerve fibres : Myelinated § Blood vessels § Gingival innervation : Derived from fibers arising from nerves in the PDL & from the labial, buccal, and palatal nerves
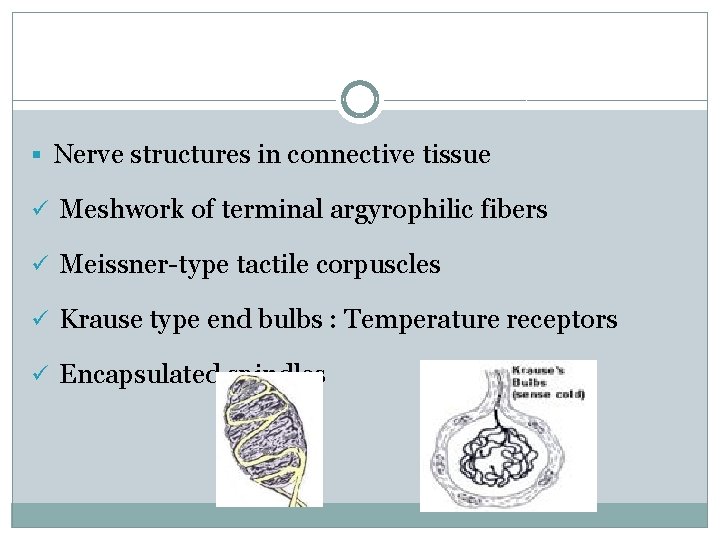
§ Nerve structures in connective tissue ü Meshwork of terminal argyrophilic fibers ü Meissner-type tactile corpuscles ü Krause type end bulbs : Temperature receptors ü Encapsulated spindles
Correlation of clinical & microscopic features § Color § Size § Contour § Shape § Consistency § Surface texture § Position
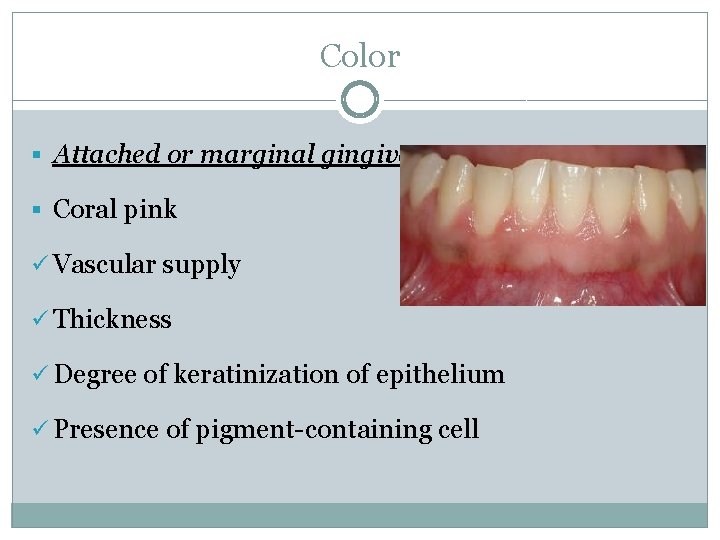
Color § Attached or marginal gingiva § Coral pink ü Vascular supply ü Thickness ü Degree of keratinization of epithelium ü Presence of pigment-containing cell
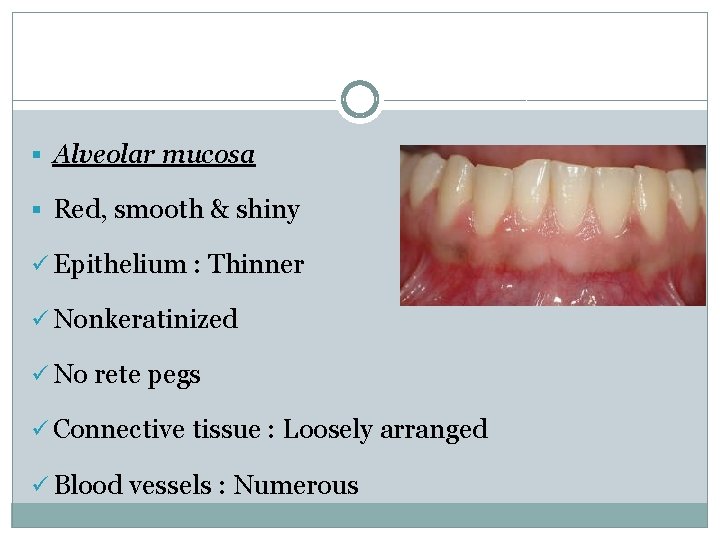
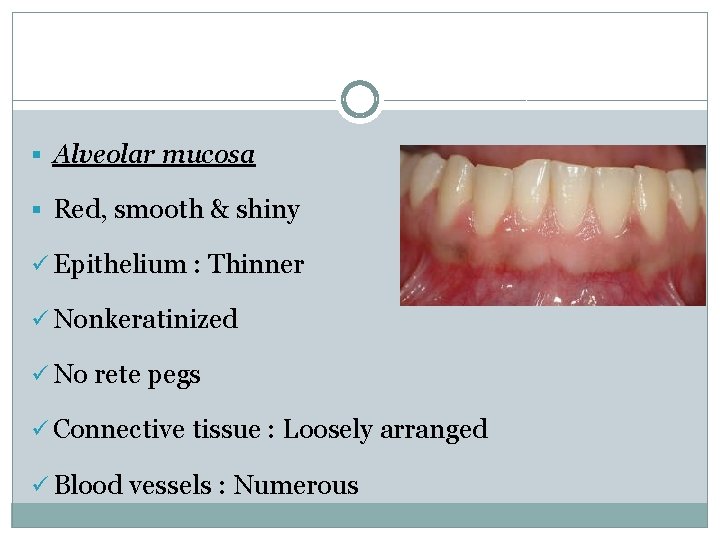
§ Alveolar mucosa § Red, smooth & shiny ü Epithelium : Thinner ü Nonkeratinized ü No rete pegs ü Connective tissue : Loosely arranged ü Blood vessels : Numerous
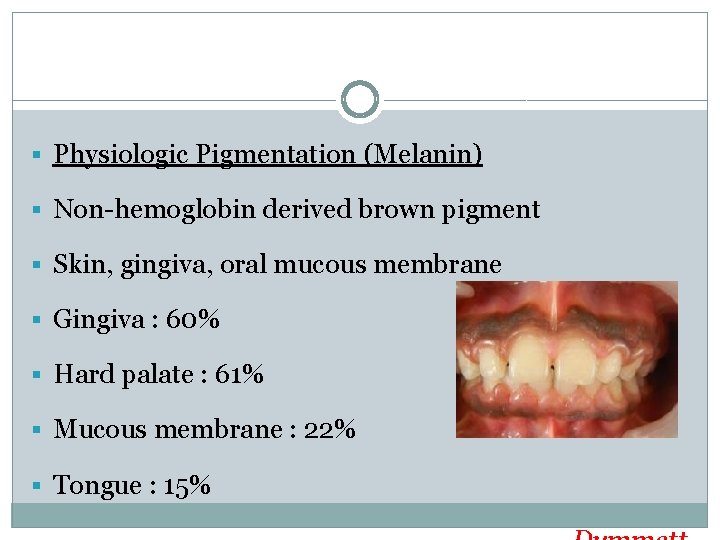
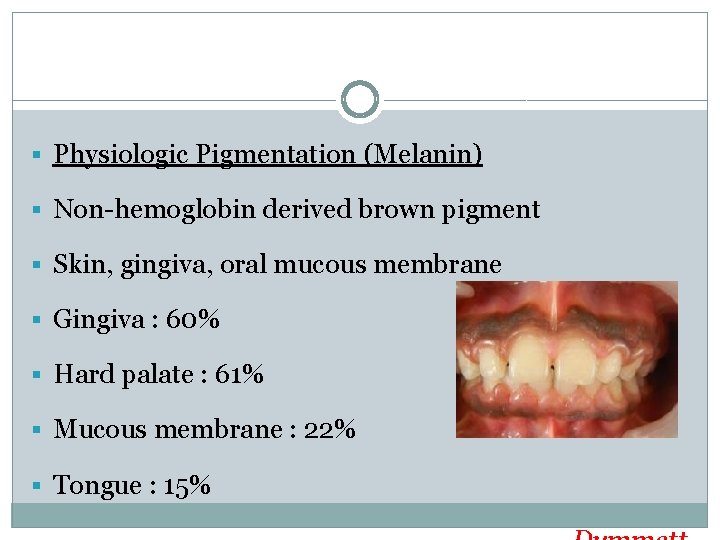
§ Physiologic Pigmentation (Melanin) § Non-hemoglobin derived brown pigment § Skin, gingiva, oral mucous membrane § Gingiva : 60% § Hard palate : 61% § Mucous membrane : 22% § Tongue : 15%
§ Diffuse, deep-purplish discoloration § Irregularly shaped brown & light brown patches § As early as 3 hours after birth

Size Cellular & Intercellular elements Vascular supply size
Contour § Shape of the teeth § Alignment in the arch § Location & Size of proximal contact § Facial & lingual gingival embrasures § Marginal gingiva : Scalloped outline § Flat surfaces : Straight line
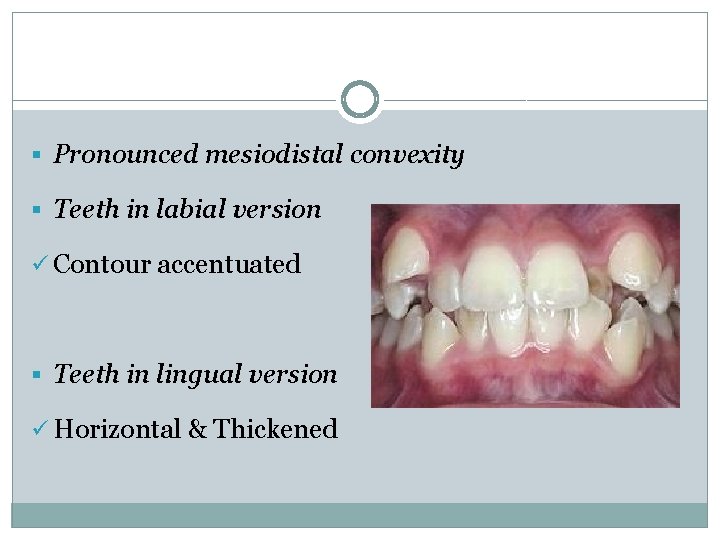
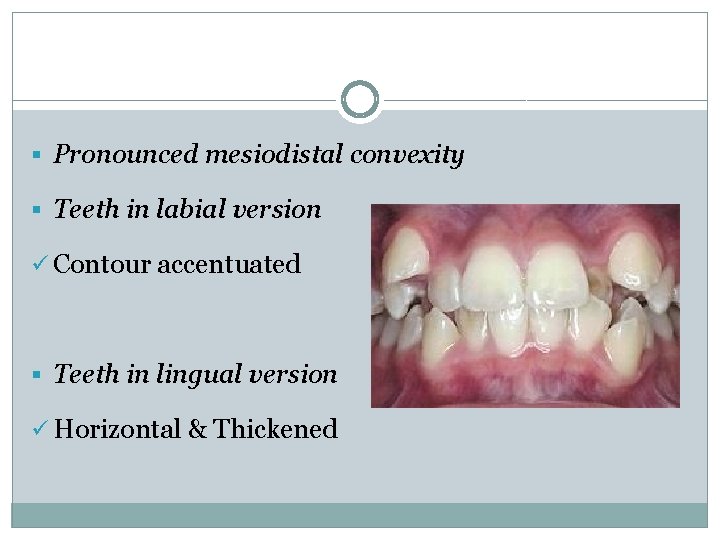
§ Pronounced mesiodistal convexity § Teeth in labial version ü Contour accentuated § Teeth in lingual version ü Horizontal & Thickened
Shape § Interdental gingiva ü Contour of proximal tooth surfaces ü Location & shape of gingival embrasures
Proximal surfaces relatively flat faciolingually Roots are close together Interdental bone thin mesiodistally Gingival embrasures & interdental gingiva are narrow mesiodistally
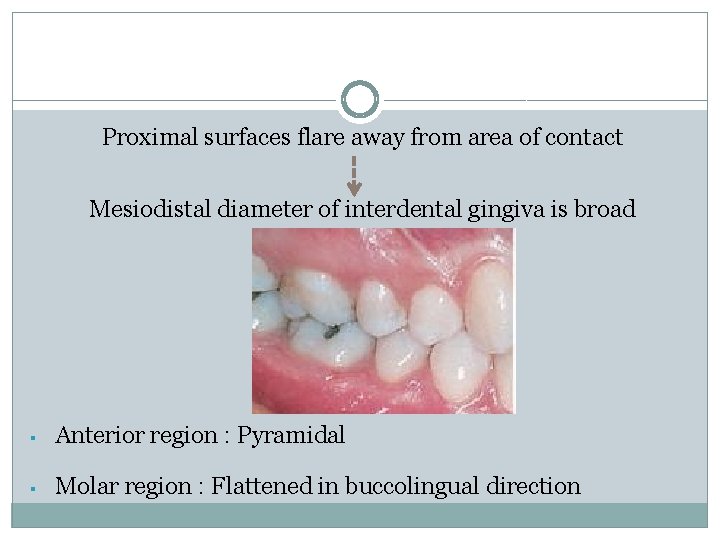
Proximal surfaces flare away from area of contact Mesiodistal diameter of interdental gingiva is broad § Anterior region : Pyramidal § Molar region : Flattened in buccolingual direction
Consistency § Firm & Resilient § Tightly bound to underlying bone § Exception : Movable free margin § Collagenous lamina propria § Contiguity with mucoperiosteum § Gingival fibers
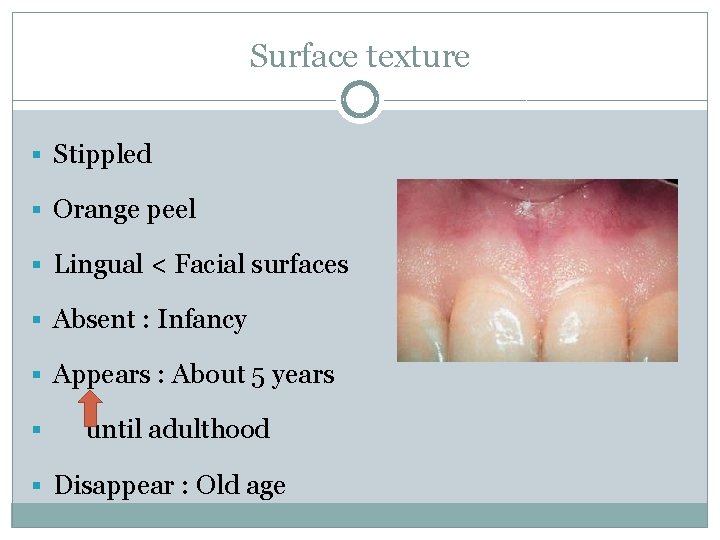
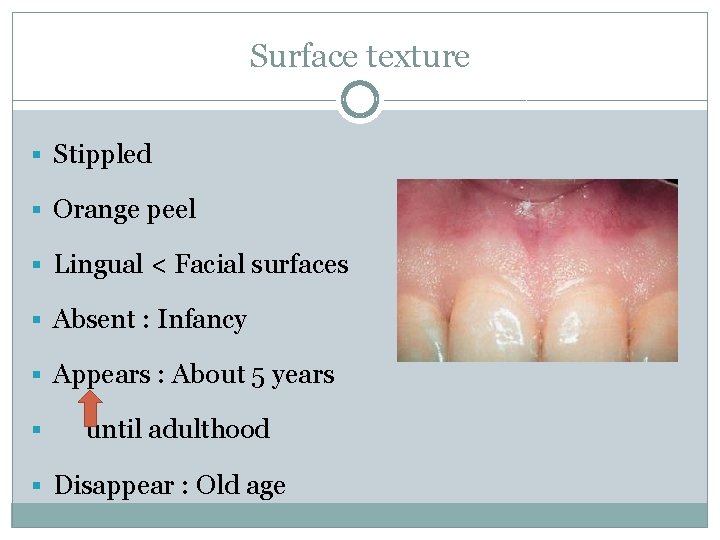
Surface texture § Stippled § Orange peel § Lingual < Facial surfaces § Absent : Infancy § Appears : About 5 years § until adulthood § Disappear : Old age
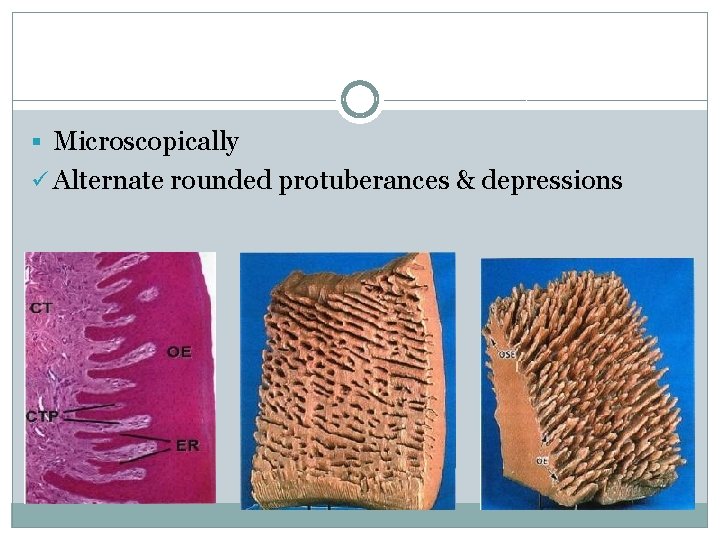
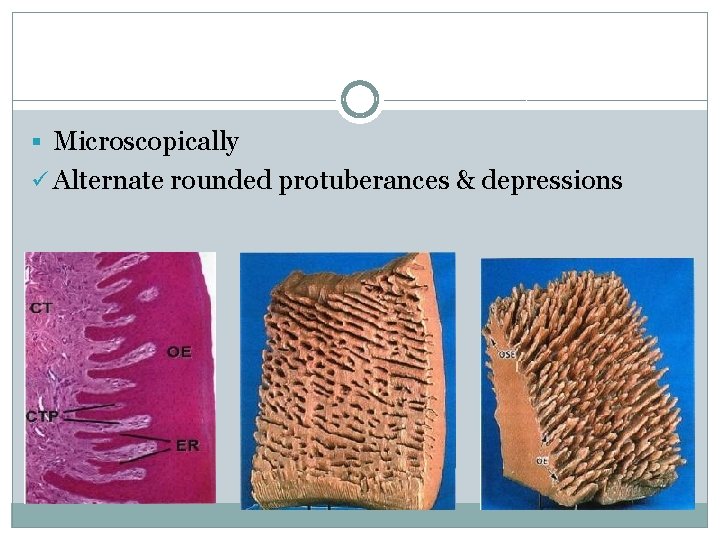
§ Microscopically ü Alternate rounded protuberances & depressions
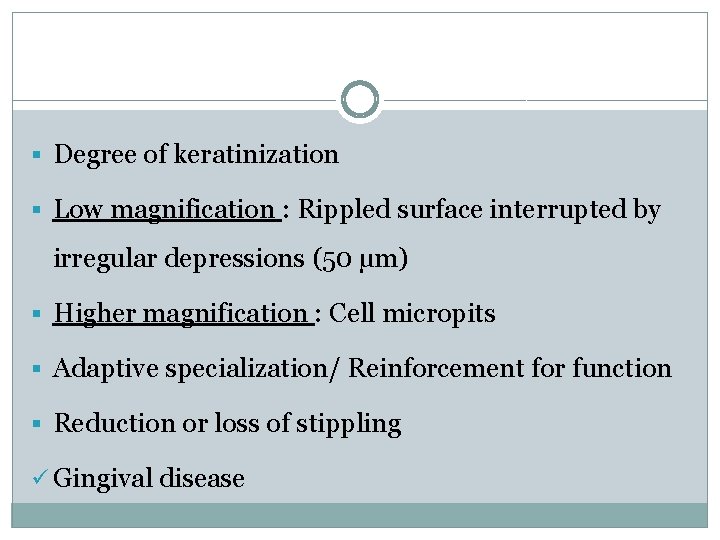
§ Degree of keratinization § Low magnification : Rippled surface interrupted by irregular depressions (50 µm) § Higher magnification : Cell micropits § Adaptive specialization/ Reinforcement for function § Reduction or loss of stippling ü Gingival disease
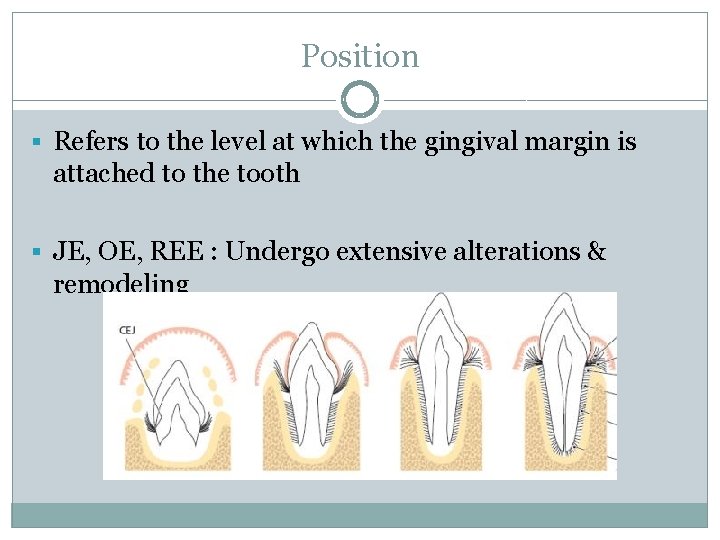
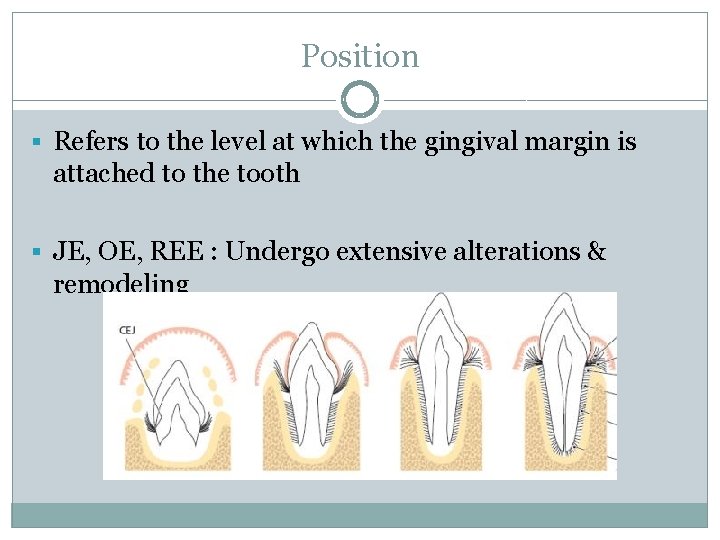
Position § Refers to the level at which the gingival margin is attached to the tooth § JE, OE, REE : Undergo extensive alterations & remodeling
§ Continuous Tooth Eruption Gottlieb & Orban, 1933 § Active eruption : Movement of the teeth in the direction of the occlusal plane § Passive eruption : Exposure of the teeth by apical migration of the gingiva
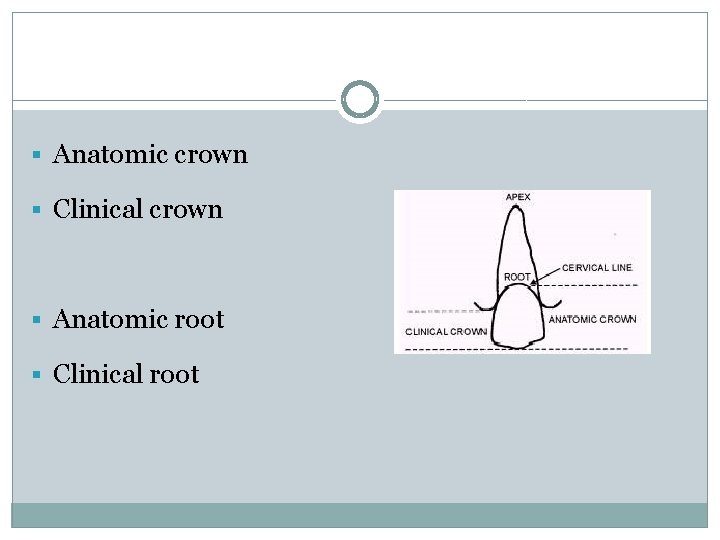
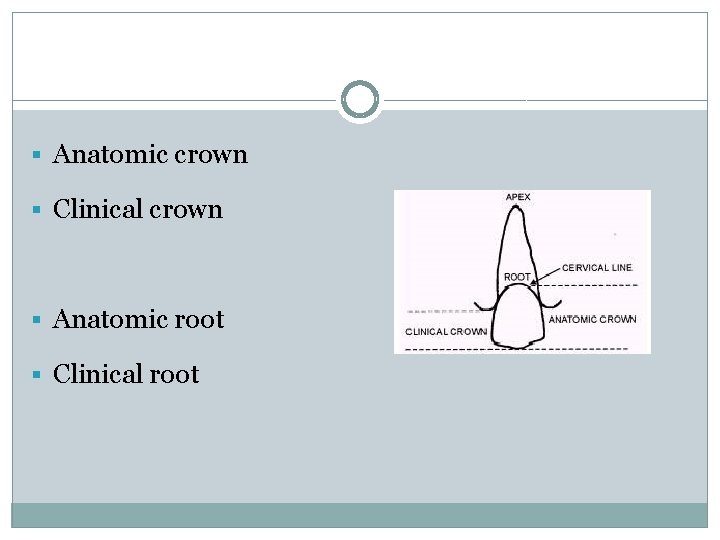
§ Anatomic crown § Clinical crown § Anatomic root § Clinical root
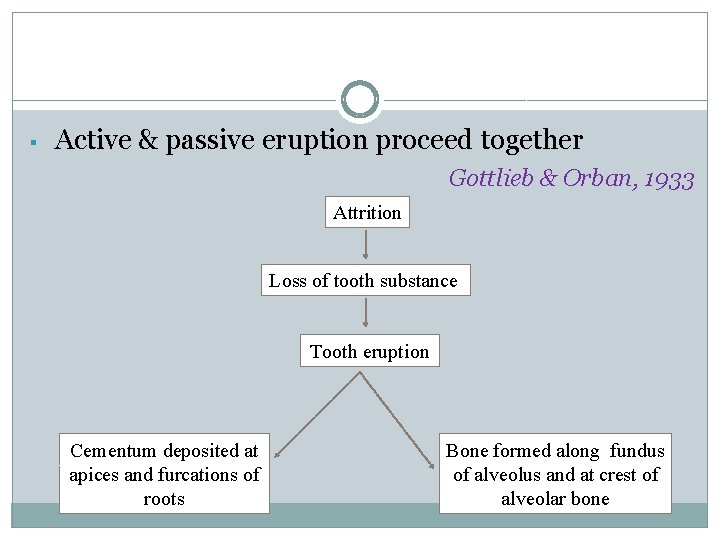
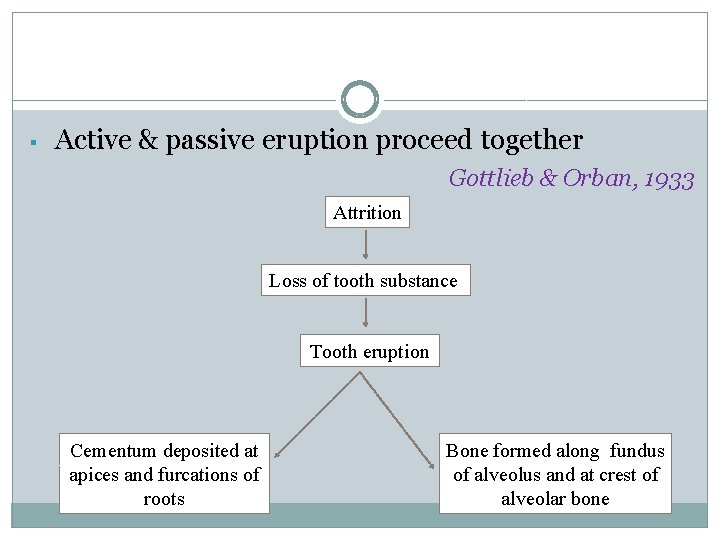
§ Active & passive eruption proceed together Gottlieb & Orban, 1933 Attrition Loss of tooth substance Tooth eruption Cementum deposited at apices and furcations of roots Bone formed along fundus of alveolus and at crest of alveolar bone
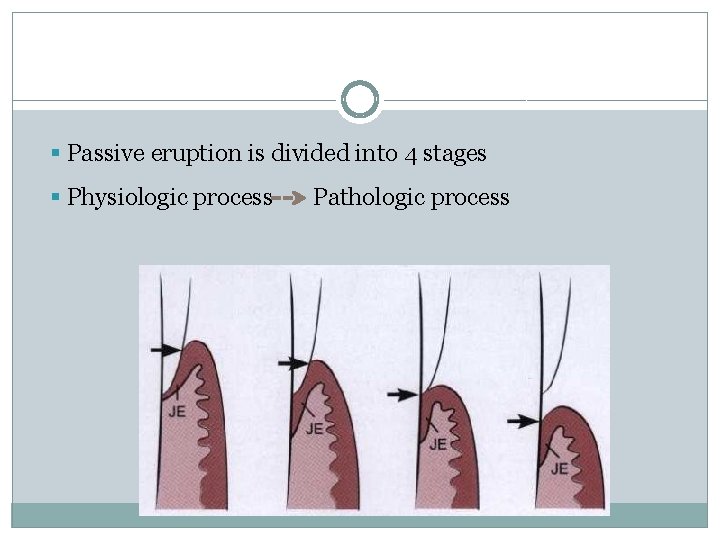
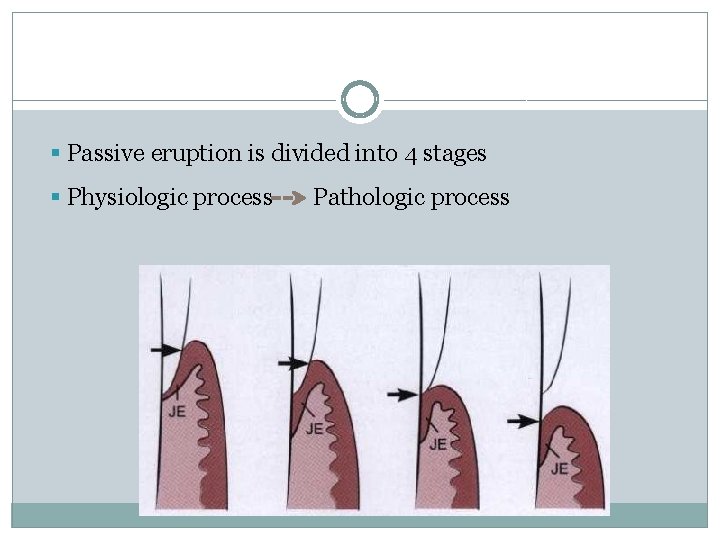
§ Passive eruption is divided into 4 stages § Physiologic process Pathologic process
Age changes § Gingival Epithelium § Thinning of epithelium Shklar 1966 § Decreased keratinization Glickman 1950
§ Shape of the Rete pegs (Conflicting results) ü Flattening of rete pegs Shklar 1966 ü Height of epithelial ridges increased Wentz 1952 ü Formation of epithelial cross ridges Loe & Karring 1972
§ ↑ cell density Meyer 1956, Ryan 1974 § Morphology : Do not change Wentz 1952 § Regeneration time (Conflicting results) ü Mitotic activity ↑ Meyer 1956, Gargiulo 1961 ü Constant Ryan 1974 ü Mitotic activity↓ Karring and Loe 1973
§ Location of JE § Health: Apical termination of JE located at CEJ § Dental plaque : Etiological factor in development of gingivitis Suami, 1971
§ Absence of plaque : Periodontal breakdown does not occur : periodontal pocket will not occur Lindhe & Nyman 1975; Axellsson & Lindhe 1978 § Continuous presence of plaque & its quantity : Development & course of periodontal disease
Contradicting studies § Apical migration of JE can occur in absence of plaque & inflammatory cells Skilleni 1930, Rushton 1951, Beersten et al 1982 § Continuous passive eruption theory Gottlieb and Orban 1933 ü Age : Gradual physiological recession of gingiva concomitantly with apical migration of epithelium
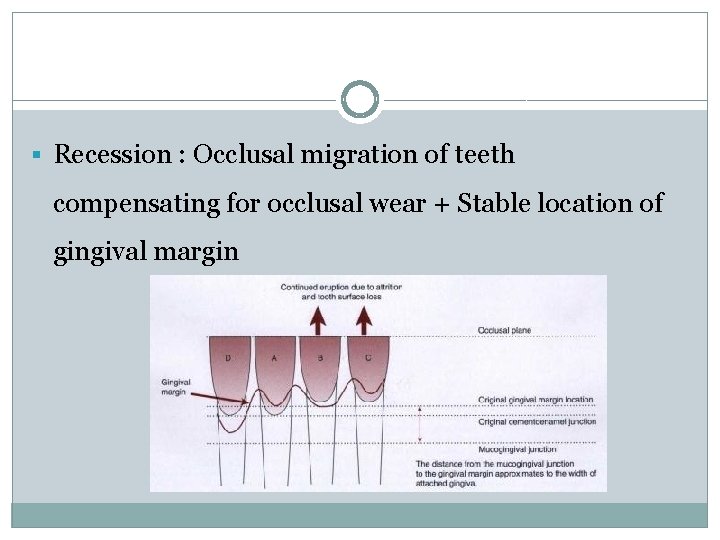
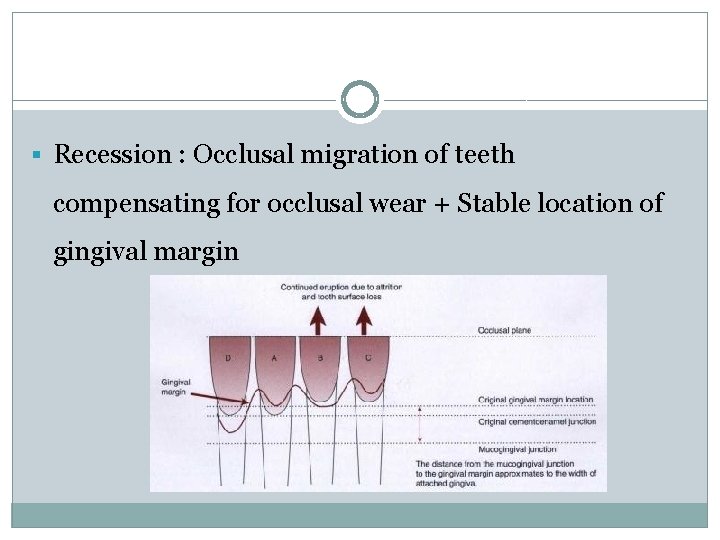
§ Recession : Occlusal migration of teeth compensating for occlusal wear + Stable location of gingival margin
§ In contrast § Recession ü Mechanical trauma e. g. tooth brushing Loe et al 1978 ü Extrusion of teeth Batenhorst et al 1974 § Occlusal movement of teeth does not imply apical migration of JE Manson 1963, Anneroth & Ericsson 1967, Loe 1967
Gingival Connective Tissue § Coarser & dense § Rate of maturation changes § Cellular elements § Rate of collagen synthesis § Soluble - Insoluble collagen § Mechanical strength § Denaturing temperature § Collagen stabilization
Conclusion § knowledge of architecture of the gingiva, how the tissue structure develops & how it relates to function is fundamental importance for understanding the disease process, and for devising effective therapeutic strategies
References § Newman MG, Takei HH, Klokevold PR, Carranza FA. Carranza’s Clinical § § § § Periodontology. Saunders Elsevier; 10 th Edition. Lindhe, Karring, Lang: Clinical Periodontology & Implant Dentistry. Blackwell Munksgaard; 5 th Edititon. P. Mark Bartold, Laurence J. Walsh & A. Sampath Narayanan. Molecular and cell biology of the gingiva. Periodontology 2000, Vol. 24, 2000, 28– 55. D. D. Bosshardt and N. P. Lang. The Junctional Epithelium: from Health to Disease. J Dent Res 2005; 84(1); 9 -20. Thomas M. Hassell. Tissues and cells of the periodontium. Periodontology 2000, Vol. 3, 1993, 9 -38. Van Der Velden. Effect of age on the periodontium. Journal of Clinical Periodontology 1984: 11; 281 -294. Marja T. Pollanen, Jukka I. Salonen & Veli-Jukka Uitto. Structure and function of the tooth–epithelial interface in health and disease. Periodontology 2000, Vol. 31, 2003, 12– 31 Stern IB. Current concepts of the dentogingival junction: The epithelial and connective tissue attachments to the tooth. J Periodontol 1981; 52: 465 -476.
 A mirror with a flat surface
A mirror with a flat surface Convex mirror is a diverging mirror
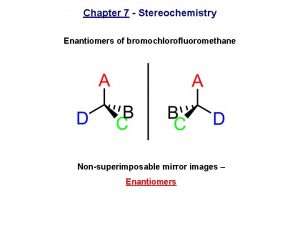
Convex mirror is a diverging mirror Nonsuperposable
Nonsuperposable Mirror mirror commonwealth fund
Mirror mirror commonwealth fund The rearview mirror should be checked
The rearview mirror should be checked Define health education?
Define health education? Actual and apparent position of gingiva
Actual and apparent position of gingiva кератолинин
кератолинин Scorbutic gingivitis ppt
Scorbutic gingivitis ppt Macro anatomy of gingiva
Macro anatomy of gingiva Gingiva
Gingiva Dental alveolus
Dental alveolus Birleşim epiteli
Birleşim epiteli Gingival attachment
Gingival attachment Mc call festoons
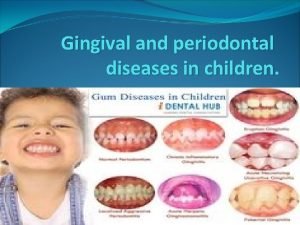
Mc call festoons Gingival diseases
Gingival diseases Contour of gingiva in gingivitis
Contour of gingiva in gingivitis Gingiva
Gingiva Defense mechanism of gingiva
Defense mechanism of gingiva Biological width dental
Biological width dental Gingival curettage indications
Gingival curettage indications Pristine gingiva
Pristine gingiva Periodontal instruments classification
Periodontal instruments classification Perimylolysis
Perimylolysis Politür patı
Politür patı Oxytalin
Oxytalin Periodontal case study
Periodontal case study Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Plaque index scoring criteria
Plaque index scoring criteria Fases del tratamiento periodontal
Fases del tratamiento periodontal Corrective phase
Corrective phase Indikasi enap
Indikasi enap Rationale for periodontal treatment
Rationale for periodontal treatment Ligamento periodontal
Ligamento periodontal Glickman's concept
Glickman's concept Cva
Cva Streptokokal gingivitis
Streptokokal gingivitis Necropulpectomía y biopulpectomía
Necropulpectomía y biopulpectomía Margen gingival
Margen gingival Desmodent
Desmodent Sharpey lifleri
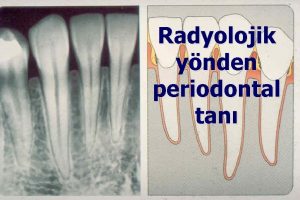
Sharpey lifleri Diagnosis of periodontal disease
Diagnosis of periodontal disease Non corticated
Non corticated Conventional ameloblastoma
Conventional ameloblastoma Periodontal abscess
Periodontal abscess Periodontal ligament injection definition
Periodontal ligament injection definition Periodontal disease
Periodontal disease Lamina dura radiografi
Lamina dura radiografi Periodontal charting symbols
Periodontal charting symbols Periodontal healing
Periodontal healing Principles of periodontal surgery
Principles of periodontal surgery Caruncula sublingualis
Caruncula sublingualis Como se divide el periodonto
Como se divide el periodonto Widman flap
Widman flap Ligamento periodontal
Ligamento periodontal Who sondu nedir
Who sondu nedir Interdental septum
Interdental septum Deskuamatif gingivitis
Deskuamatif gingivitis Periodontal case study
Periodontal case study Do93
Do93 Periodontal tendonitis
Periodontal tendonitis Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Glasgow thang điểm
Glasgow thang điểm Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 101012 bằng
101012 bằng Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thứ tự các dấu thăng giáng ở hóa biểu
Thứ tự các dấu thăng giáng ở hóa biểu Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Career portfolio definition
Career portfolio definition Deep perineal pouch contents
Deep perineal pouch contents Febrile non hemolytic transfusion reaction
Febrile non hemolytic transfusion reaction Ffp clotting factors
Ffp clotting factors Mediastinum
Mediastinum Popliteal fossa structures
Popliteal fossa structures Identify
Identify The immortal life of henrietta lacks table of contents
The immortal life of henrietta lacks table of contents Contents of internal capsule
Contents of internal capsule Subscapularis insertion and origin
Subscapularis insertion and origin Ark of the covenant lampstand
Ark of the covenant lampstand Comic book table of contents
Comic book table of contents Suspensory ligament of treitz
Suspensory ligament of treitz Mla table of contents
Mla table of contents Contents of stylistic lexis
Contents of stylistic lexis Content page magazine
Content page magazine Continuous variable example
Continuous variable example Example of appendix in report
Example of appendix in report Platelets transfusion indication
Platelets transfusion indication Occupied
Occupied Pericardial sinuses
Pericardial sinuses Contents of an abstract
Contents of an abstract Persepolis table of contents
Persepolis table of contents Persepolis table of contents
Persepolis table of contents Interactive notebook table of contents
Interactive notebook table of contents Fresh frozen plasma contents
Fresh frozen plasma contents Funiculus separans
Funiculus separans Vaginal hydrocele
Vaginal hydrocele Greater sciatic foramen
Greater sciatic foramen Swot analysis of event venue
Swot analysis of event venue Anterior mediastinum contents
Anterior mediastinum contents Definition of mediastinum
Definition of mediastinum Contents of carotid sheath
Contents of carotid sheath Triangular space contents
Triangular space contents Contents of curriculum vitae
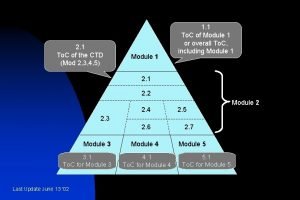
Contents of curriculum vitae Ctd module 5 table of contents
Ctd module 5 table of contents Cost audit report contains
Cost audit report contains Civics interactive notebook
Civics interactive notebook City of ember poppy
City of ember poppy Fresh frozen plasma transfusion time
Fresh frozen plasma transfusion time Contents of air pollution
Contents of air pollution Magazine contents page analysis
Magazine contents page analysis Biceps brachii
Biceps brachii Cubital fossa boundaries
Cubital fossa boundaries External carotid artery terminal branches
External carotid artery terminal branches Femoral triangle contents
Femoral triangle contents Cubital fossa contents
Cubital fossa contents Content of femoral triangle
Content of femoral triangle Rotator cuff interval
Rotator cuff interval Historical background of hamlet
Historical background of hamlet Mnemonic operation code
Mnemonic operation code Ctd module 5 table of contents
Ctd module 5 table of contents Contents of urogenital triangle
Contents of urogenital triangle Importance of entrepreneurship development programme
Importance of entrepreneurship development programme Scrapbook table of contents
Scrapbook table of contents Scalene muscle
Scalene muscle Table of contents science
Table of contents science Styloid apparatus
Styloid apparatus How to write a logbook for a science project
How to write a logbook for a science project Plasmatic
Plasmatic Bovie pad
Bovie pad Transverse perineal muscle
Transverse perineal muscle High palate
High palate Trial master file contents
Trial master file contents Module 3 ctd table contents
Module 3 ctd table contents Acknowledgement for chemistry project
Acknowledgement for chemistry project Cruropopliteal canal contents
Cruropopliteal canal contents Contents of the dead man's pocket plot diagram
Contents of the dead man's pocket plot diagram