GUIDED TISSUE REGENERATION AND GROWTH FACTORS Specific Learning
























- Slides: 59
GUIDED TISSUE REGENERATION AND GROWTH FACTORS
Specific Learning Objectives The student should be able to understand answer • What is GTR and growth factor • The rationale and biologic concept for GTR • Indications and contraindications of GTR • The types, advantages, and disadvantages of GTR • Techniques of using guided tissue regeneration.
Introduction • Periodontal Regeneration is defined as a reproduction or reconstruction of a lost or injured part in such a way that the architecture and function of a lost or injured tissue is completely restored (Glossary of periodontal terminologies 1992)
What is GTR (Guided Tissue Regeneration)? • IN 1996, World Workshop in Periodontics defined GTR as ‘procedures attempting to regenerate lost periodontal tissues through differential tissue responses’. • AAP has defined GTR as ’the procedure by which a barrier is utilized to exclude epithelium from the root surfaces’.
History • 1976 - Melcher described the basic concept of cell population in periodontal regeneration which led to development of GTR. • 1982 - Nyman et al first described the clinical procedure of GTR using non absorbable barrier membrane made of cellulose acetate laboratory filter(millipore filter).
• 1982 – WL Gore et al investigated materials which would limit epithelial migration around tooth and implants. • Classic studies of Nyman(1982), Lindhe(1984), Karring(1986) and Gottlow(1986) have assumed that only periodontal ligament cells have regenerative potential.
Biologic concept of GTR • Excluding the epithelium and gingival connective tissue from the root surface during post surgical healing phase (cell exclusion) 1. Prevents epithelial migration into the wound 2. Favours repopulation of the area from the periodontal ligament cells and bone cells.


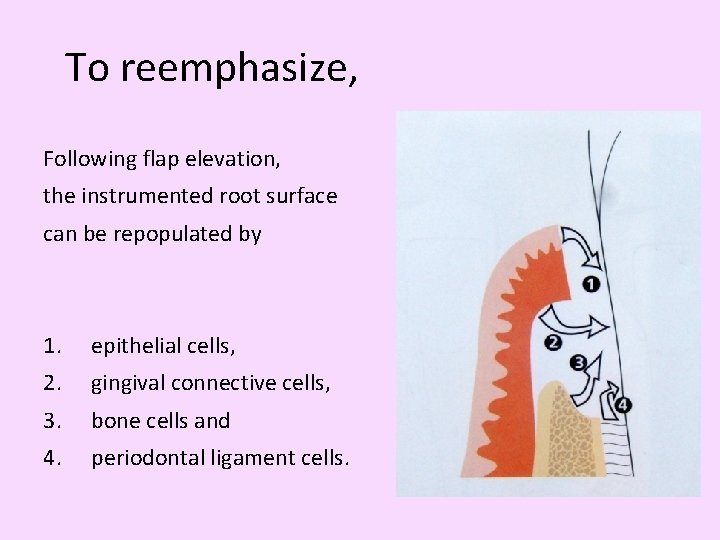
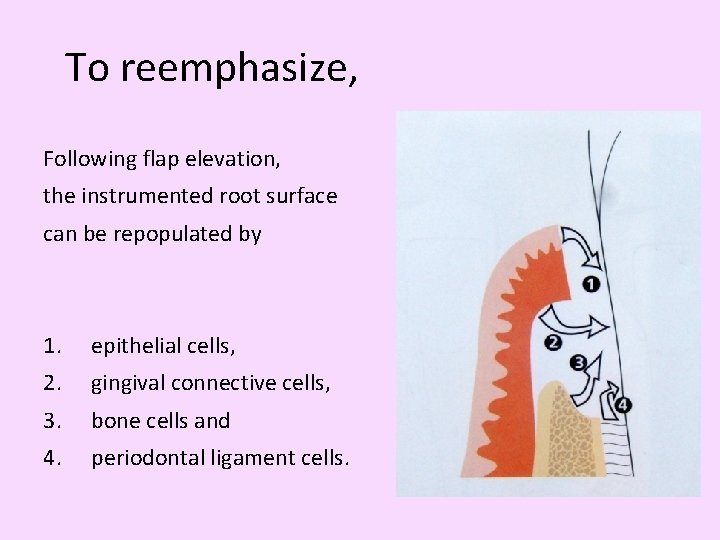
To reemphasize, Following flap elevation, the instrumented root surface can be repopulated by 1. epithelial cells, 2. gingival connective cells, 3. bone cells and 4. periodontal ligament cells.
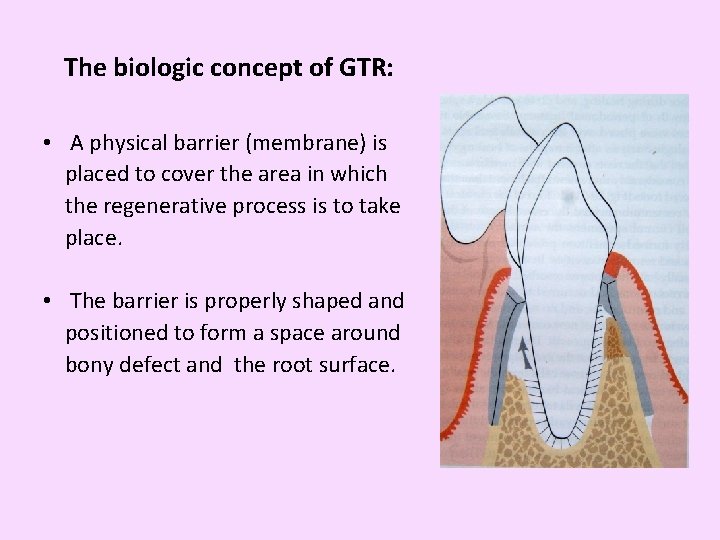
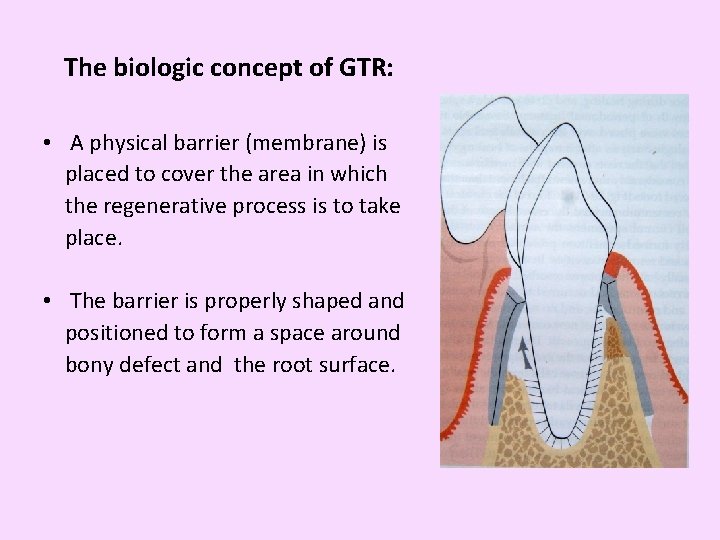
The biologic concept of GTR: • A physical barrier (membrane) is placed to cover the area in which the regenerative process is to take place. • The barrier is properly shaped and positioned to form a space around bony defect and the root surface.

Indications for GTR • • 2 or 3 walled intrabony defects Grade II furcation defects Circumferential osseous defects Recession defects Alveolar ridge augmentation Repair of apicoectomy defects. Osseous fill around immediate implants and repair around failing implants.
Contra Indications for GTR • • Infection at the site of defect. Medically compromised, unfit for surgery. Poor oral hygiene, smokers. Reduced attached gingiva width and thickness Advanced lesions with reduced bone support Tooth mobility Multiple defects Furcation defect with short root trunks
Objectives of an ideal GTR membrane It should be • Biocompatible; allow tissue integration • Chemically inert • Non antigenic • Non toxic and non carcinogenic • Easily retrievable in case of complications • Easily adaptable to defects and be available in different designs
Objectives……continued • Easily sterilizable • Easy to handle during surgeries • Sufficiently rigid to allow space between root and membrane • Easily storable with long shelf life • Not too expensive • Not resorb too early before its stipulated time

Classification of GTR • Gottlow 1993 First generation membranes: Non resorbable membranes 1. Millipore filters 2. Expanded poly tetra fluoroethylene membrane( e. PTFE) Gore tex 3. Nucleopore membrane 4. Rubber dam 5. Ethyl cellulose 6. Semi permeable silicon barrier
• Second generation Membranes: Resorbable membrane 1. Collagen- Biomend, Perioguide, Biostite 2. Polylactic acid membrane- Guidor, Atrisorb, Resolut, 3. Vicryl mesh 4. Cargile membrane 5. Oxidized cellulose membrane



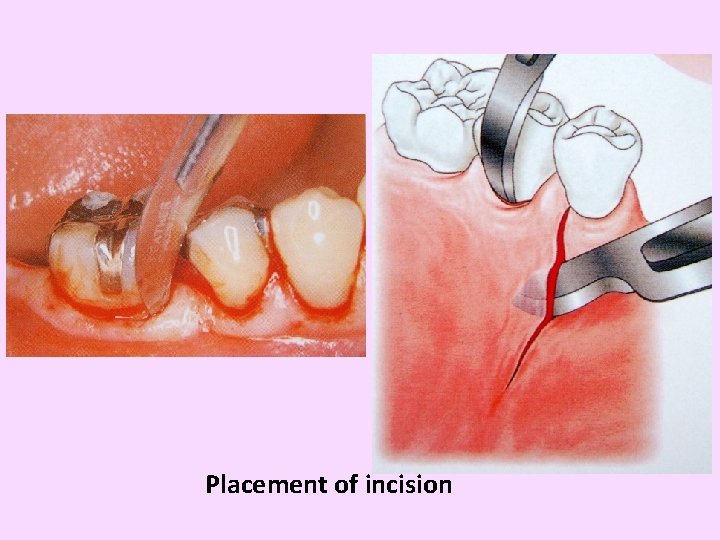
Procedural guidelines
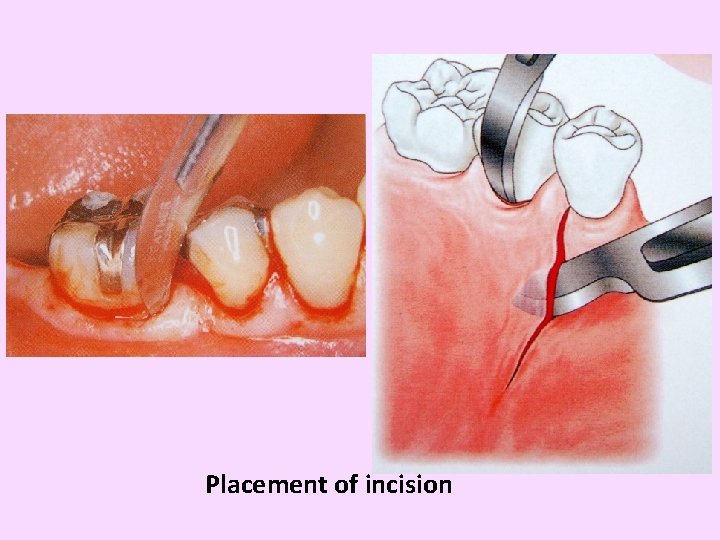
Placement of incision

Flap reflection
Debridement of the defect area
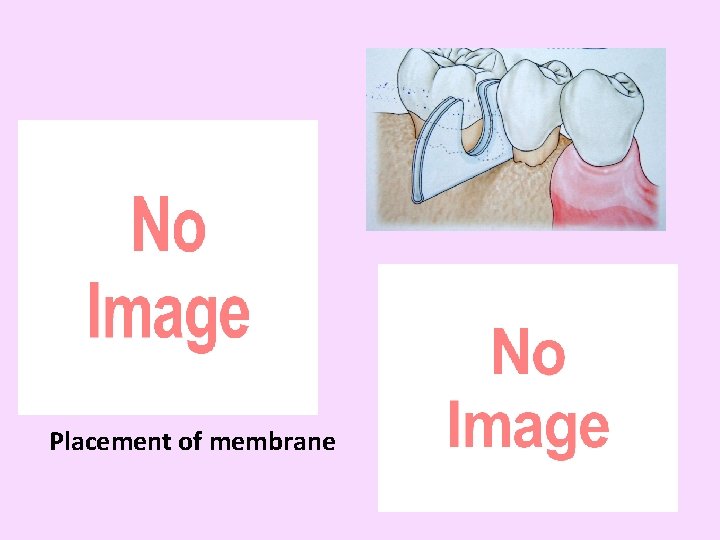
Placement of membrane

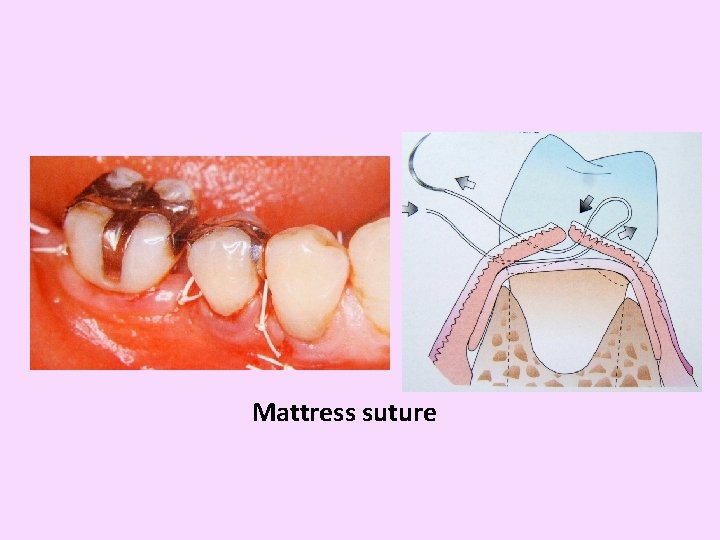
Sutures in place
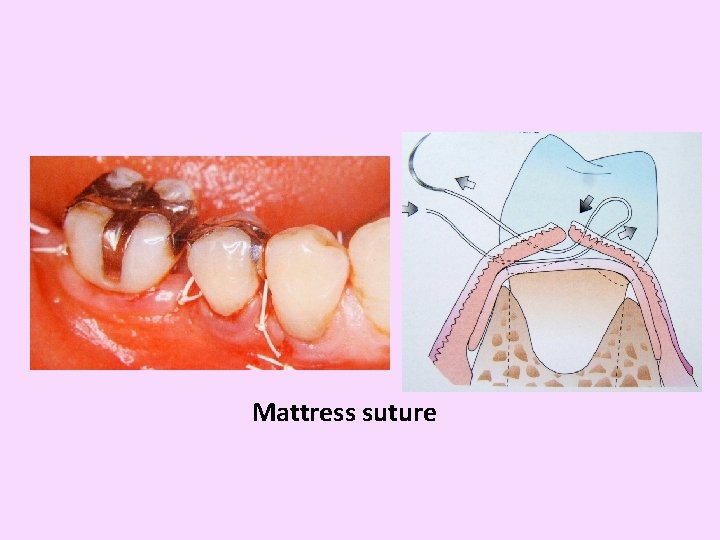
Mattress suture

Membrane removal

Selection of the barrier membrane
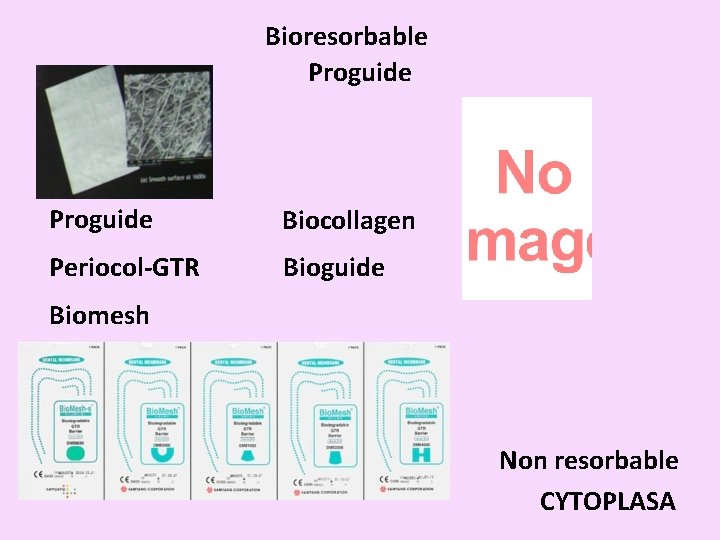
Bioresorbable Proguide Biocollagen Periocol-GTR Bioguide Biomesh Non resorbable CYTOPLASA
Clinical applications




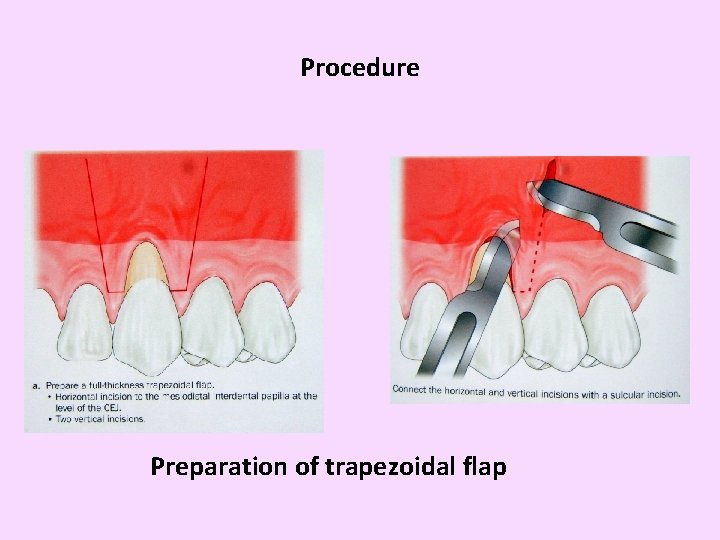
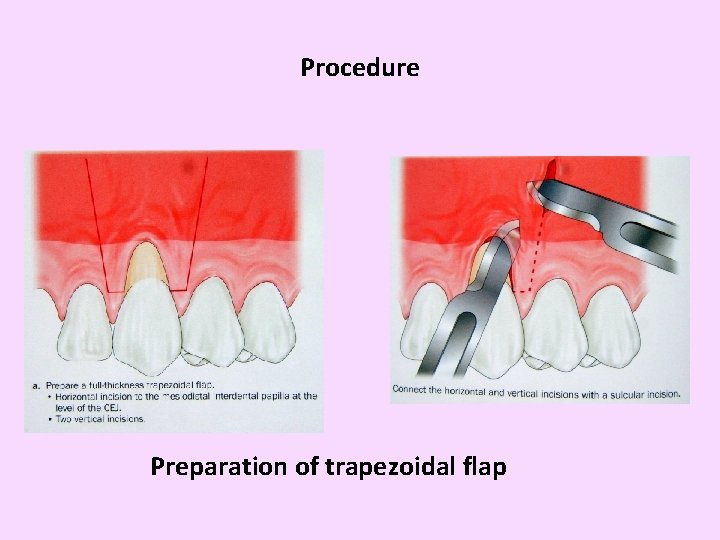
Procedure Preparation of trapezoidal flap

Preparation of trapezoidal flap
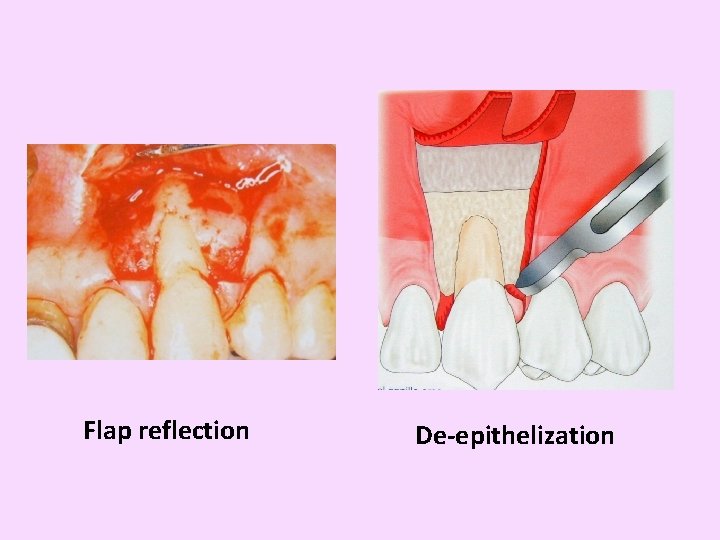
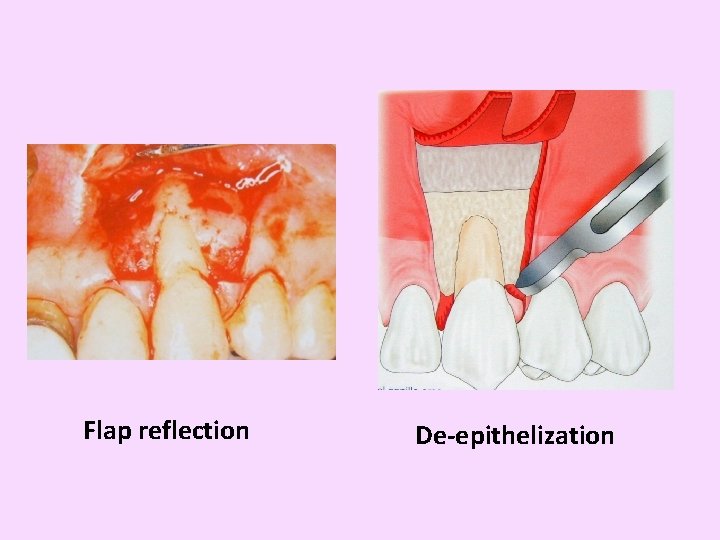
Flap reflection De-epithelization
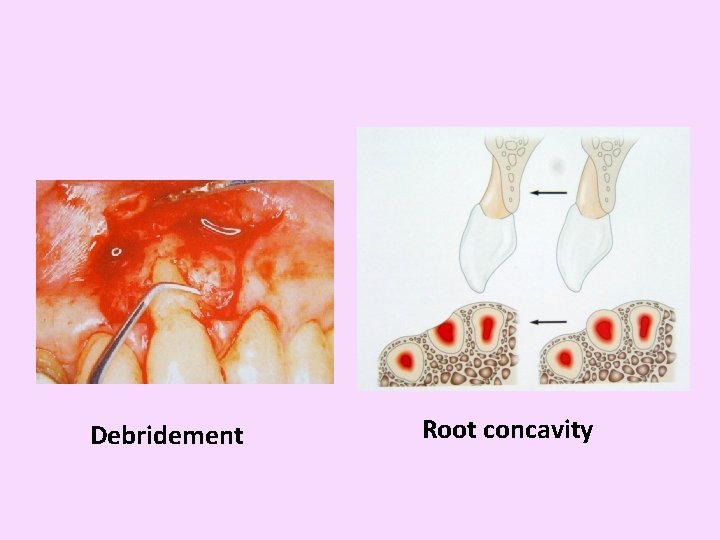
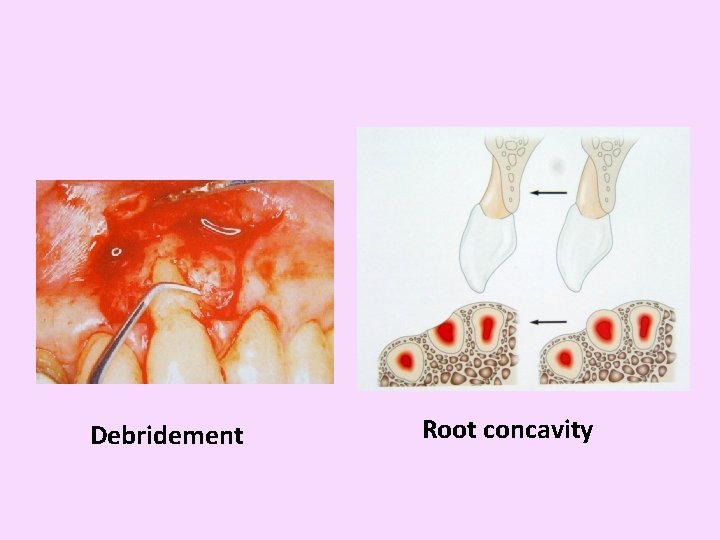
Debridement Root concavity

Membrane stabilization

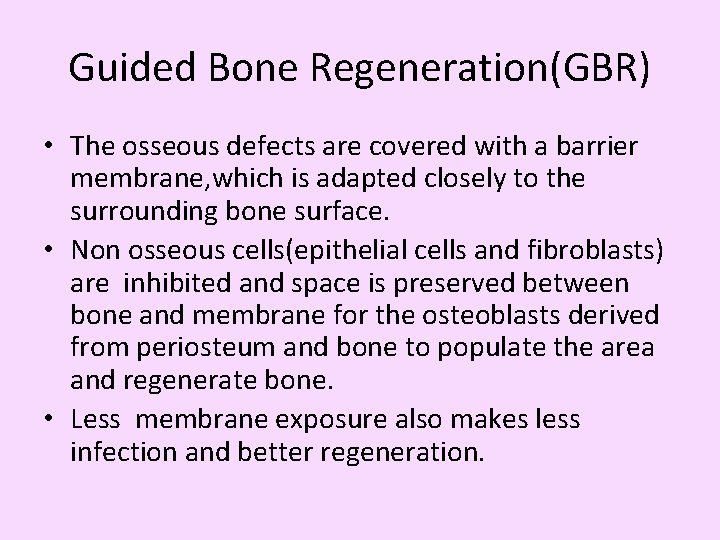
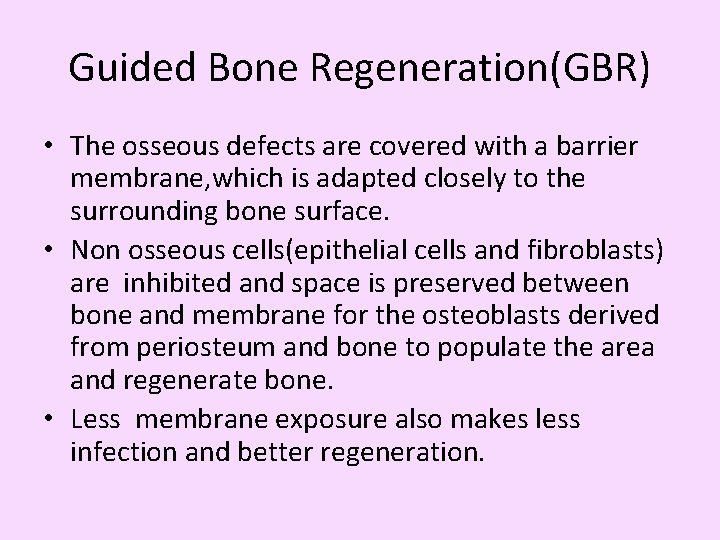
Guided Bone Regeneration(GBR) • The osseous defects are covered with a barrier membrane, which is adapted closely to the surrounding bone surface. • Non osseous cells(epithelial cells and fibroblasts) are inhibited and space is preserved between bone and membrane for the osteoblasts derived from periosteum and bone to populate the area and regenerate bone. • Less membrane exposure also makes less infection and better regeneration.



Growth factors Growth factor is a general term to denote a class of polypeptide hormones that stimulate a wide variety of cellular events such as proliferation, chemotaxis, differentiation and production of extracellular matrix proteins
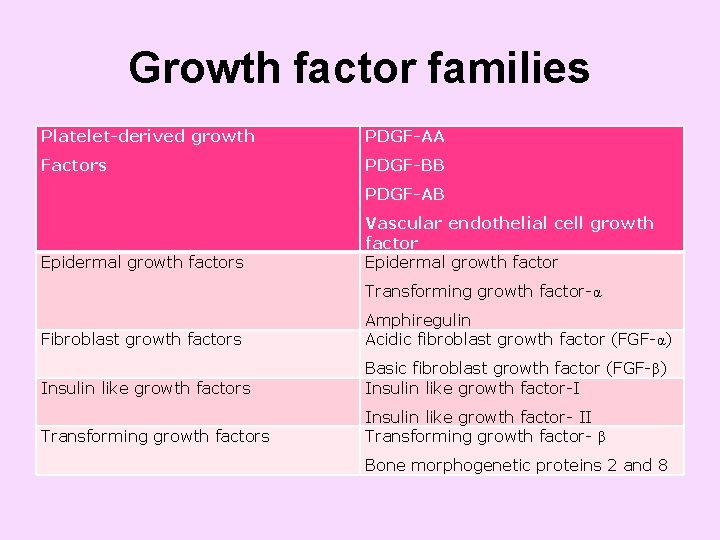
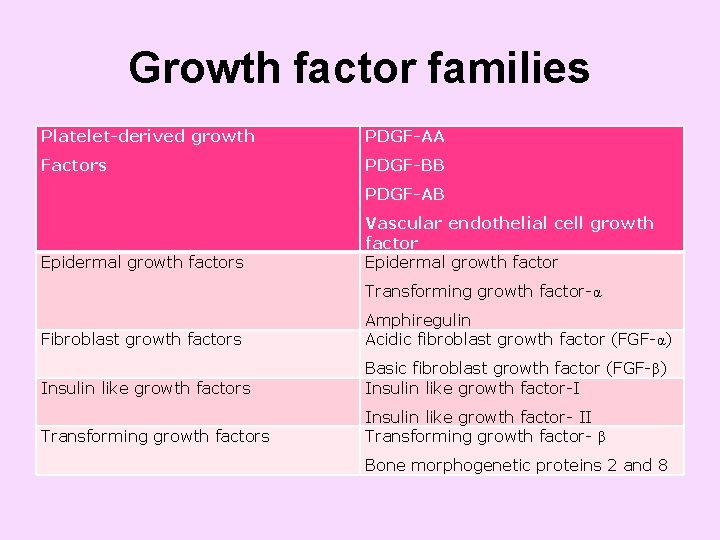
Growth factor families Platelet-derived growth PDGF-AA Factors PDGF-BB PDGF-AB Epidermal growth factors Vascular endothelial cell growth factor Epidermal growth factor Transforming growth factor-α Fibroblast growth factors Amphiregulin Acidic fibroblast growth factor (FGF-α) Insulin like growth factors Basic fibroblast growth factor (FGF-β) Insulin like growth factor-I Transforming growth factors Insulin like growth factor- II Transforming growth factor- β Bone morphogenetic proteins 2 and 8
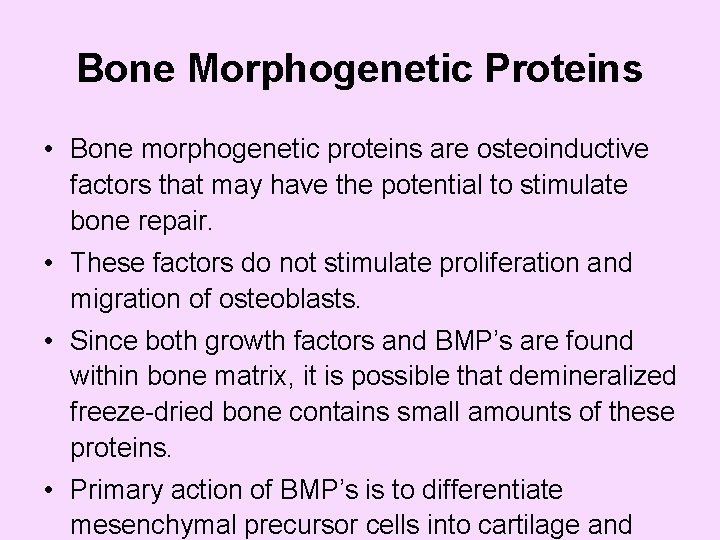
Bone Morphogenetic Proteins • Bone morphogenetic proteins are osteoinductive factors that may have the potential to stimulate bone repair. • These factors do not stimulate proliferation and migration of osteoblasts. • Since both growth factors and BMP’s are found within bone matrix, it is possible that demineralized freeze-dried bone contains small amounts of these proteins. • Primary action of BMP’s is to differentiate mesenchymal precursor cells into cartilage and
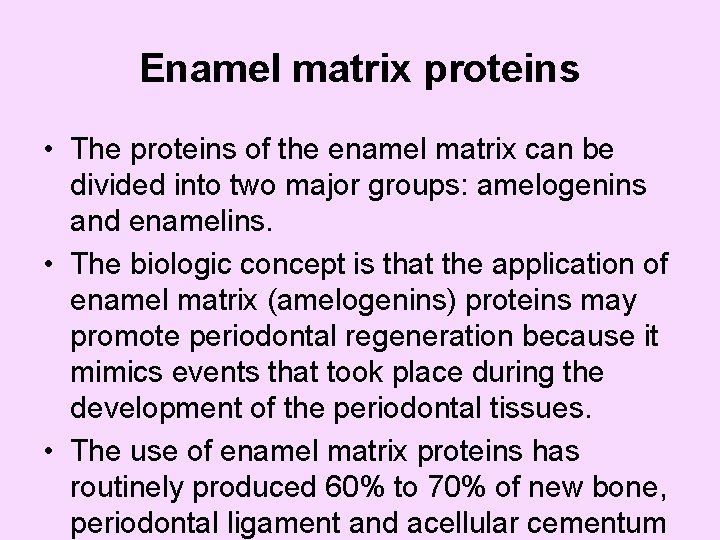
Enamel matrix proteins • The proteins of the enamel matrix can be divided into two major groups: amelogenins and enamelins. • The biologic concept is that the application of enamel matrix (amelogenins) proteins may promote periodontal regeneration because it mimics events that took place during the development of the periodontal tissues. • The use of enamel matrix proteins has routinely produced 60% to 70% of new bone, periodontal ligament and acellular cementum
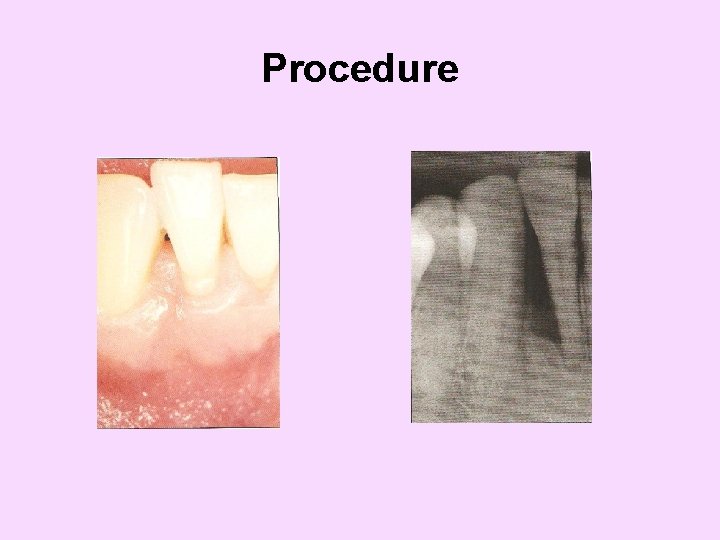
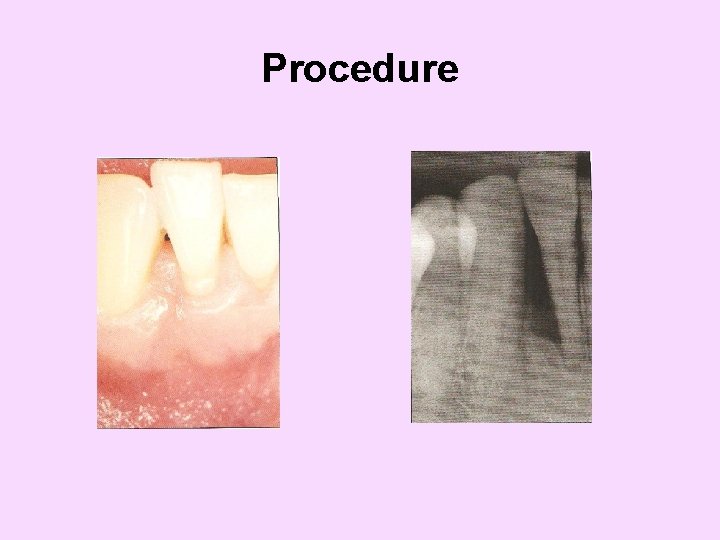
Procedure



Summary and conclusion • The principle of GTR lies in the establishment of cells of PDL, to selectively repopulate the root surface. • Clot establishment and stabilization, site selection, epithelial cell exclusion, space provision, neovascularisation and complete gingival coverage are favourable characteristics in GTR procedure.
……contd • The use of GTR membranes can significantly enhance the periodontal regeneration with cementum formation with inserting PDL fibres, the complete pd regeneration is still not reported. • In future, GTR can be combined with various biological growth factors that allowed for selectively controlling the type of cells proliferated from the fibroblast precursors.
References • Carranzas clinical Periodontology 10 thedition • Shalu bathla - 2 nd edition