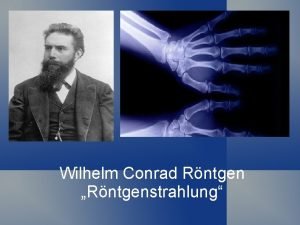
RADIOGRAPHIC INTERPRETATION IN PERIODONTAL DIAGNOSIS yyy Wilhelm Conrad



- Slides: 77
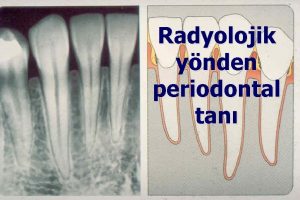
RADIOGRAPHIC INTERPRETATION IN PERIODONTAL DIAGNOSIS
yyy Wilhelm Conrad Roentgen (March 27, 1845 – February 10, 1923) Discovered X rays on Nov 8, 1895.
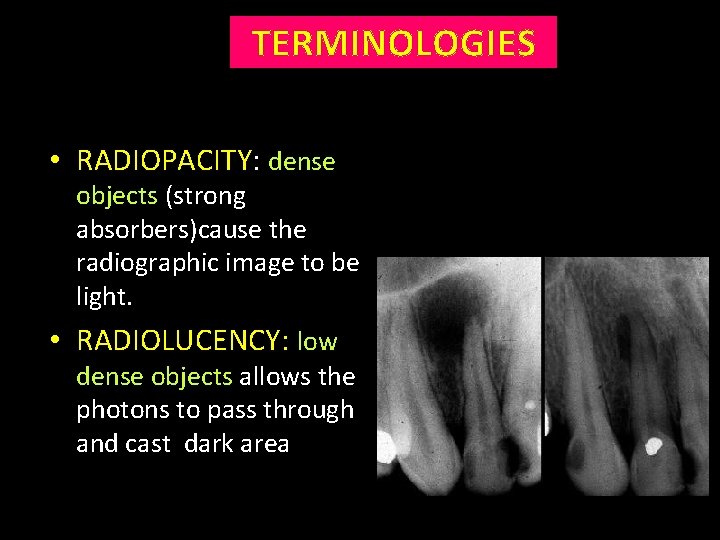
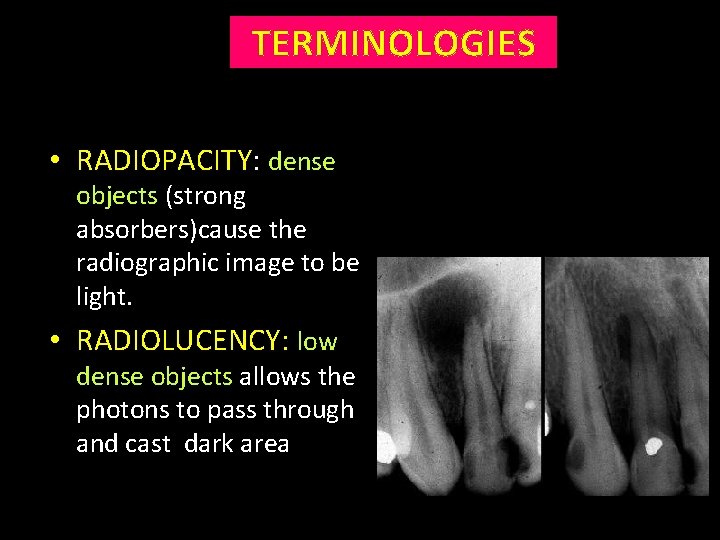
TERMINOLOGIES • RADIOPACITY: dense objects (strong absorbers)cause the radiographic image to be light. • RADIOLUCENCY: low dense objects allows the photons to pass through and cast dark area
POINTS TO PONDER…. . • Radiograph an adjunct to clinical examination and not a substitute. • Shows the post cellular effect on bone & not the current cellular activity.
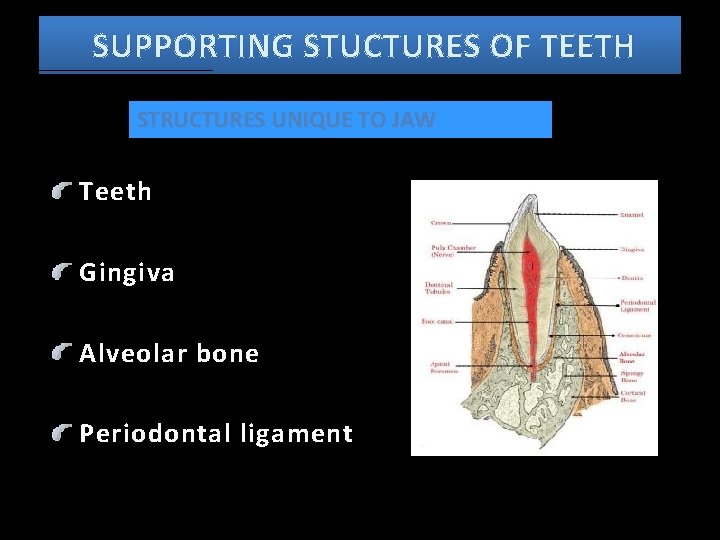
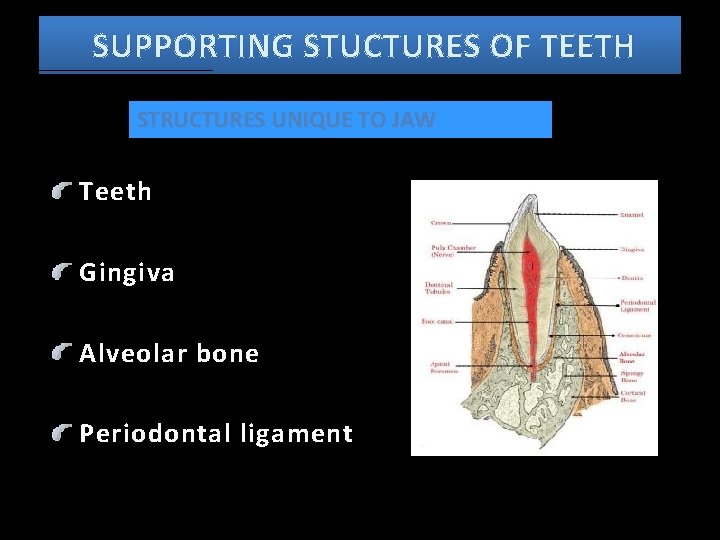
SUPPORTING STUCTURES OF TEETH STRUCTURES UNIQUE TO JAW Teeth Gingiva Alveolar bone Periodontal ligament
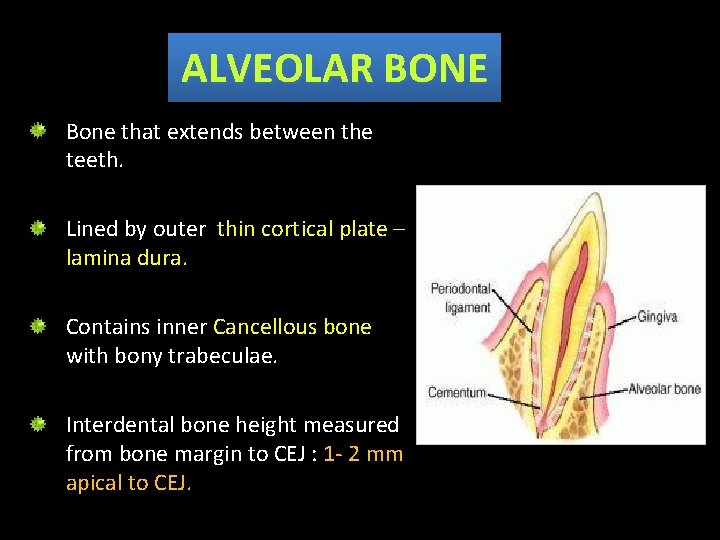
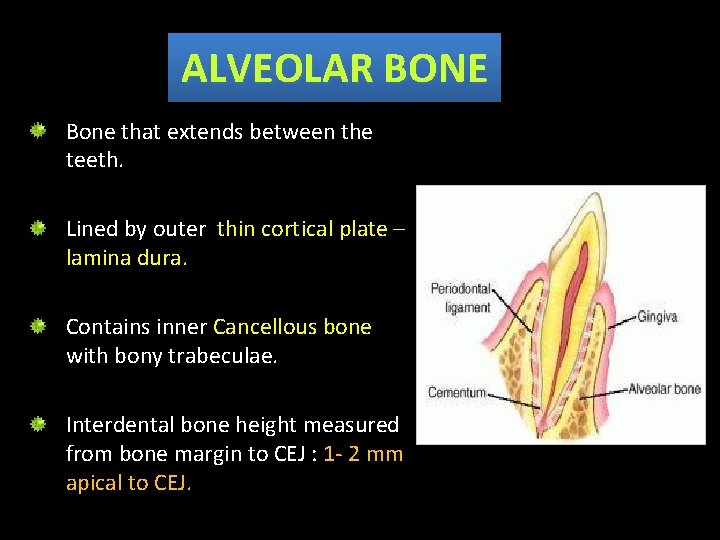
ALVEOLAR BONE Bone that extends between the teeth. Lined by outer thin cortical plate – lamina dura. Contains inner Cancellous bone with bony trabeculae. Interdental bone height measured from bone margin to CEJ : 1 - 2 mm apical to CEJ.
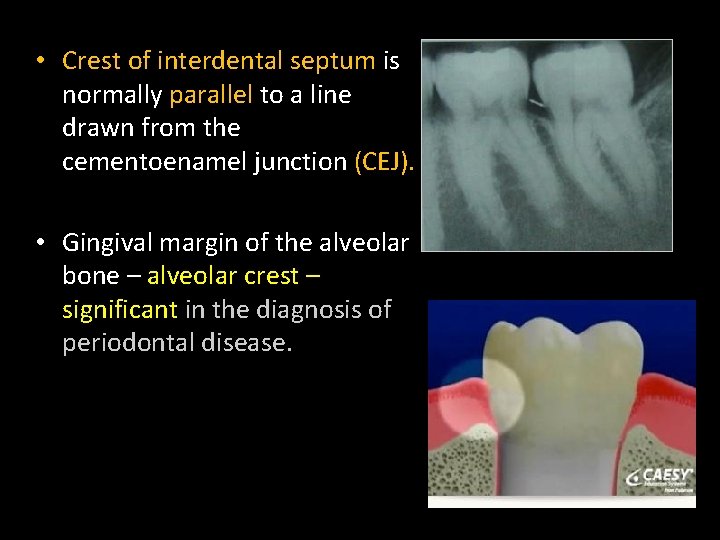
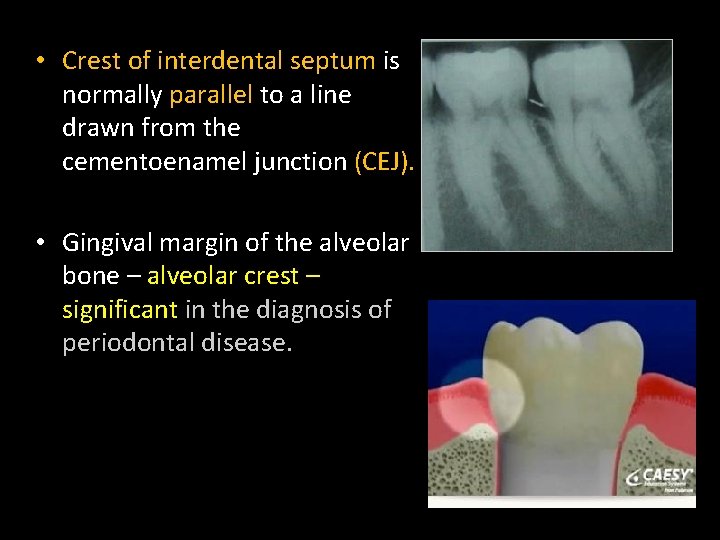
• Crest of interdental septum is normally parallel to a line drawn from the cementoenamel junction (CEJ). • Gingival margin of the alveolar bone – alveolar crest – significant in the diagnosis of periodontal disease.
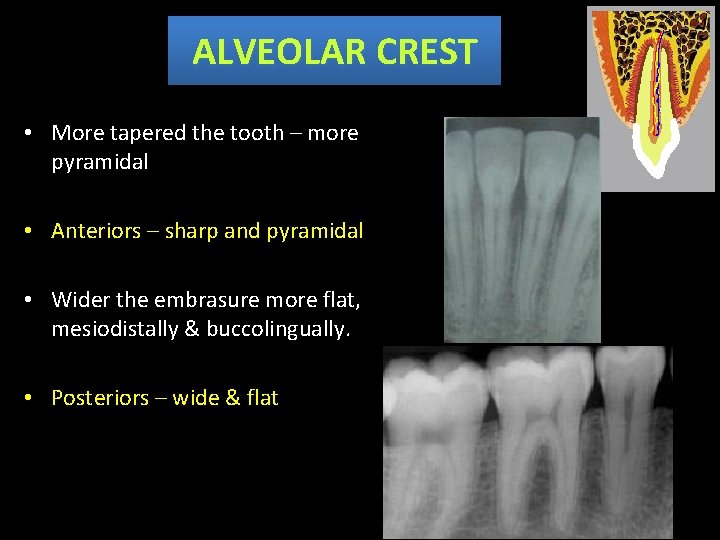
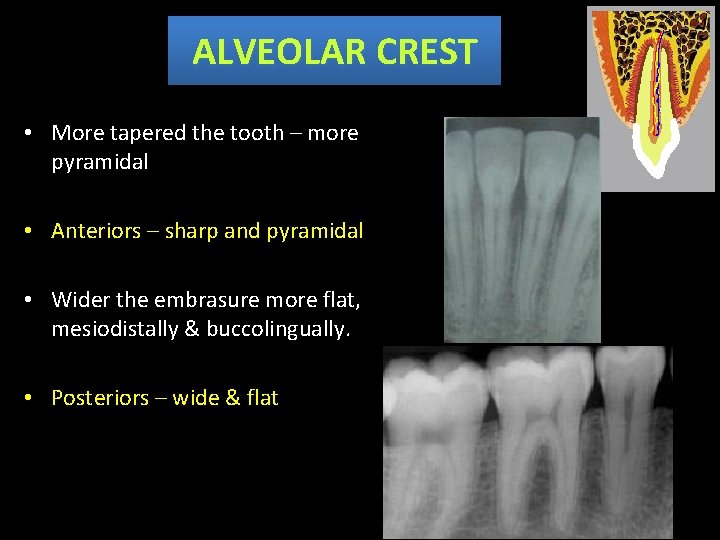
ALVEOLAR CREST • More tapered the tooth – more pyramidal • Anteriors – sharp and pyramidal • Wider the embrasure more flat, mesiodistally & buccolingually. • Posteriors – wide & flat
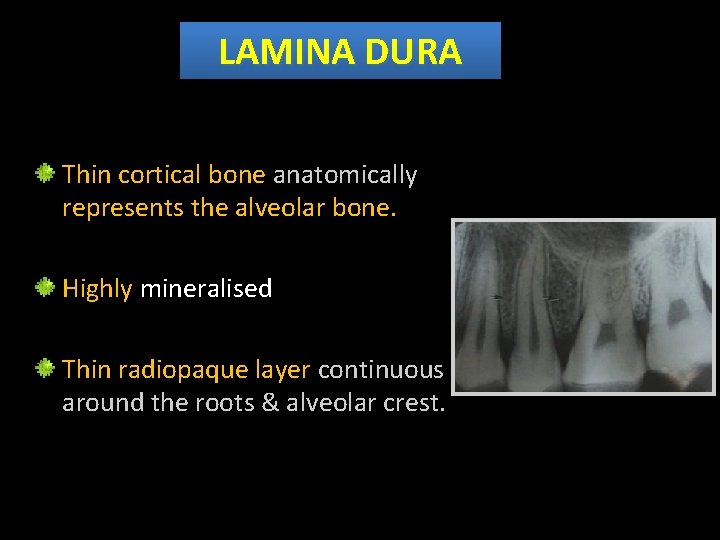
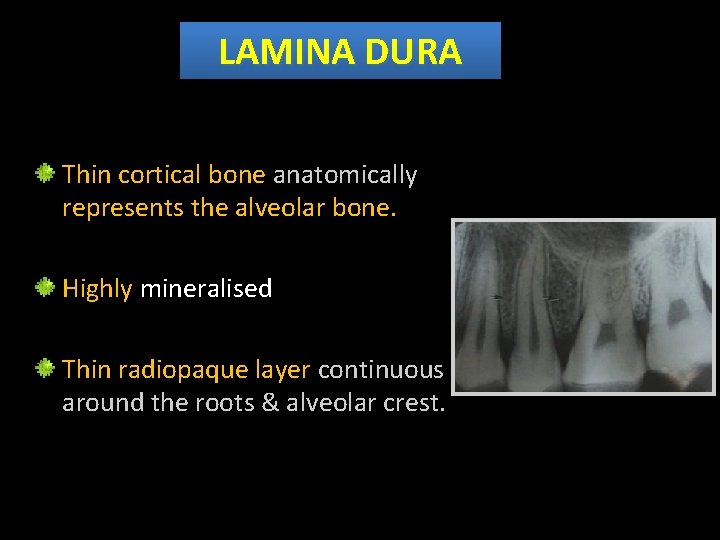
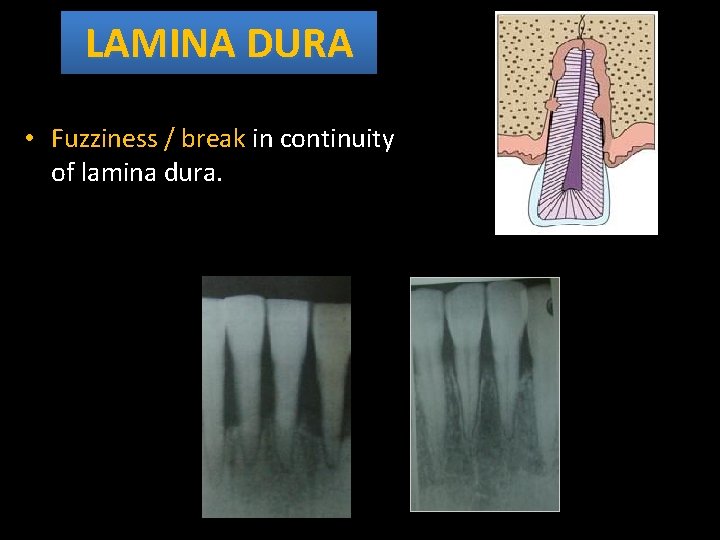
LAMINA DURA Thin cortical bone anatomically represents the alveolar bone. Highly mineralised Thin radiopaque layer continuous around the roots & alveolar crest.
• Thickness & density varies with occlusal stress. Wider & more dense – tooth in heavy occlusion. Thinner & less dense – impacted & tooth not in occlusion
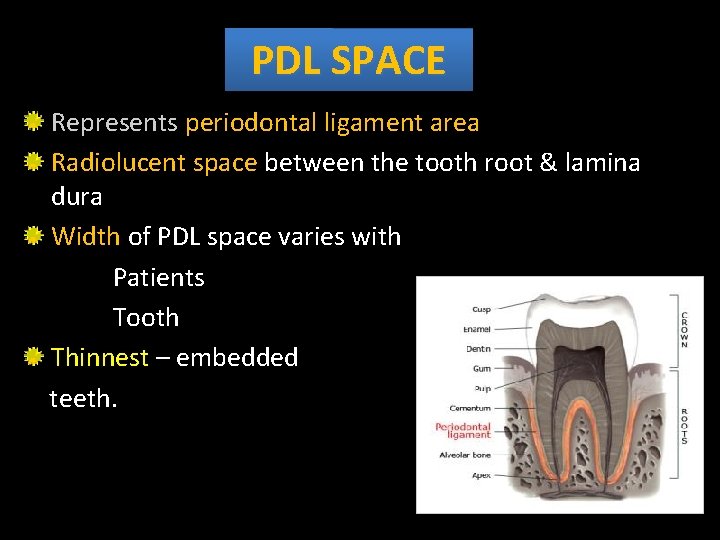
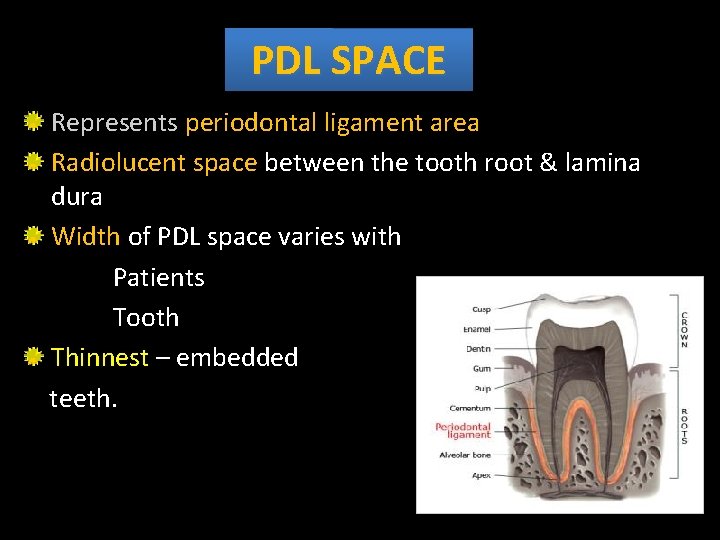
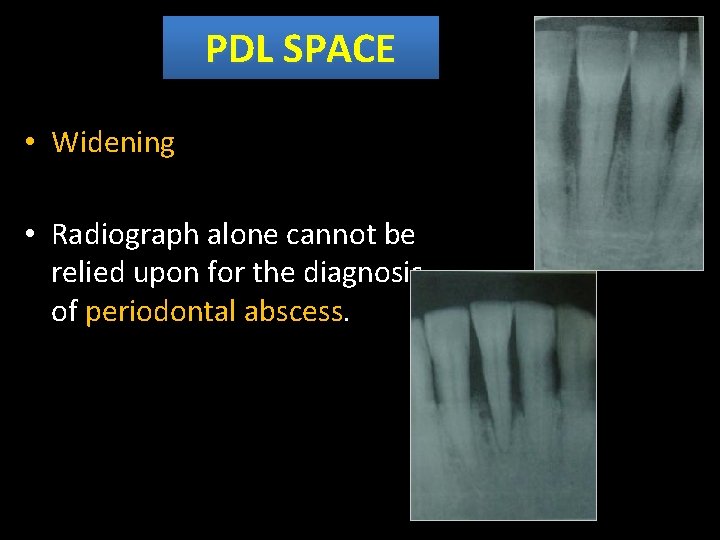
PDL SPACE Represents periodontal ligament area Radiolucent space between the tooth root & lamina dura Width of PDL space varies with Patients Tooth Thinnest – embedded teeth.
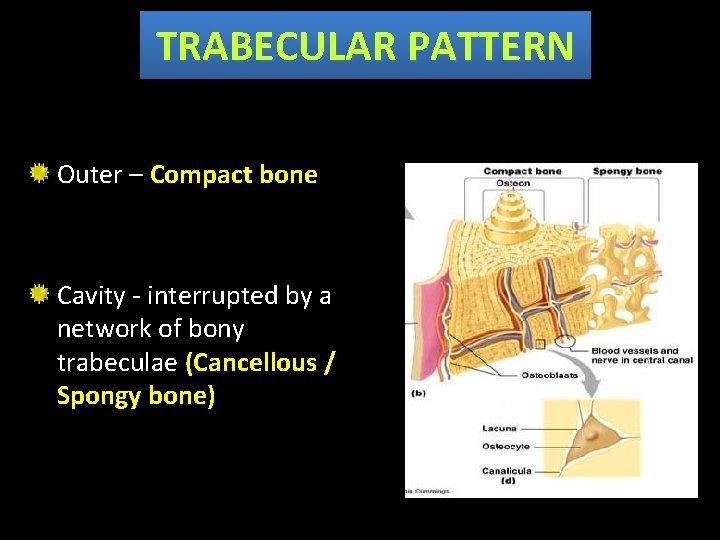
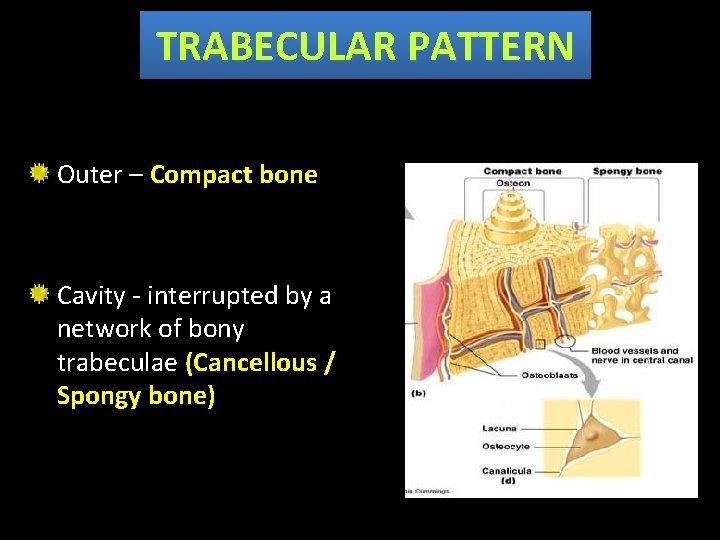
TRABECULAR PATTERN Outer – Compact bone Cavity - interrupted by a network of bony trabeculae (Cancellous / Spongy bone)
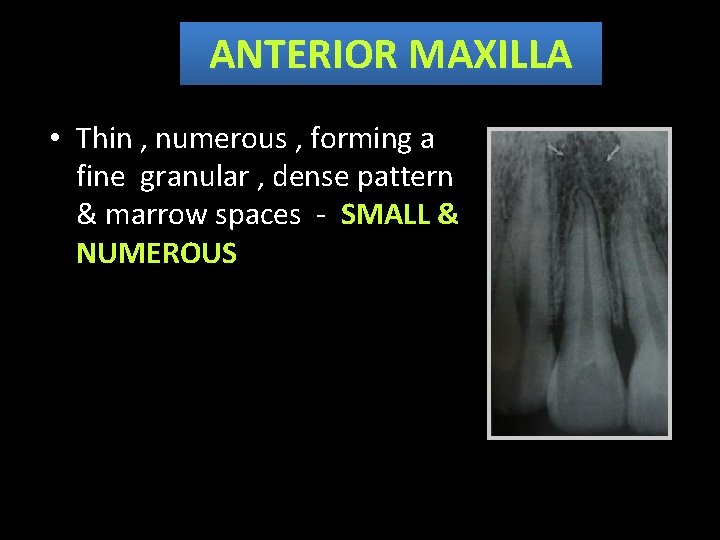
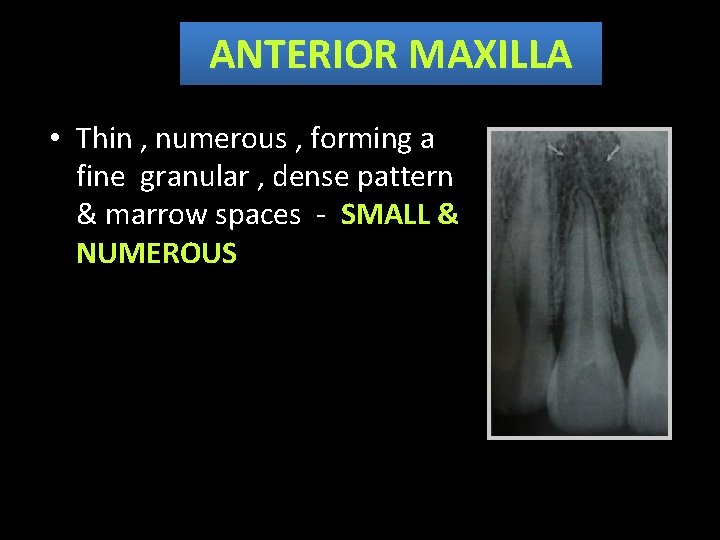
ANTERIOR MAXILLA • Thin , numerous , forming a fine granular , dense pattern & marrow spaces - SMALL & NUMEROUS
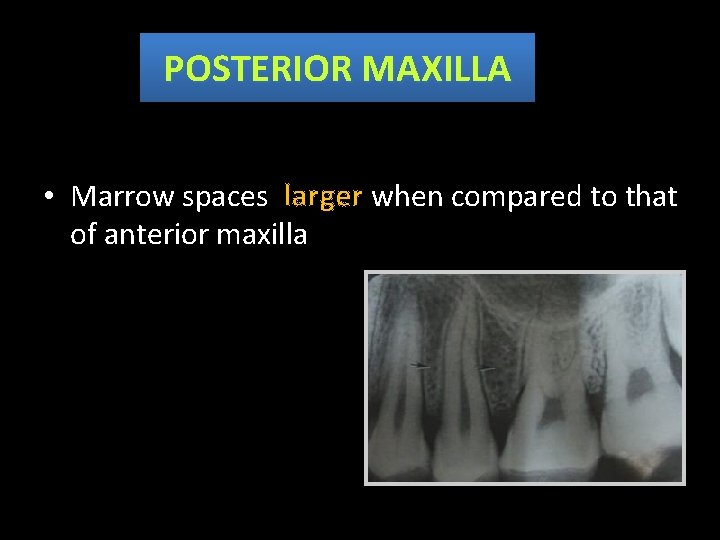
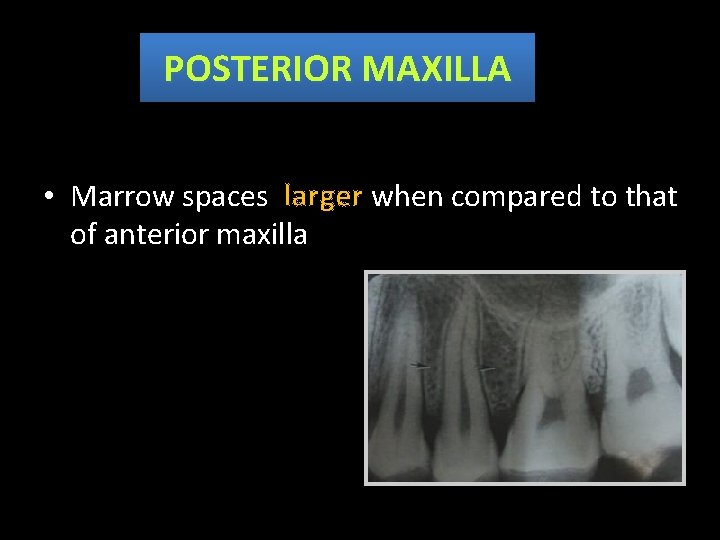
POSTERIOR MAXILLA • Marrow spaces larger when compared to that of anterior maxilla
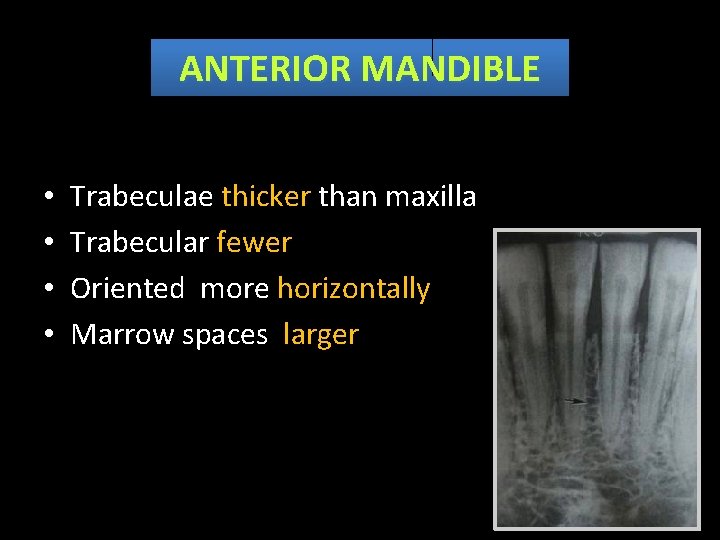
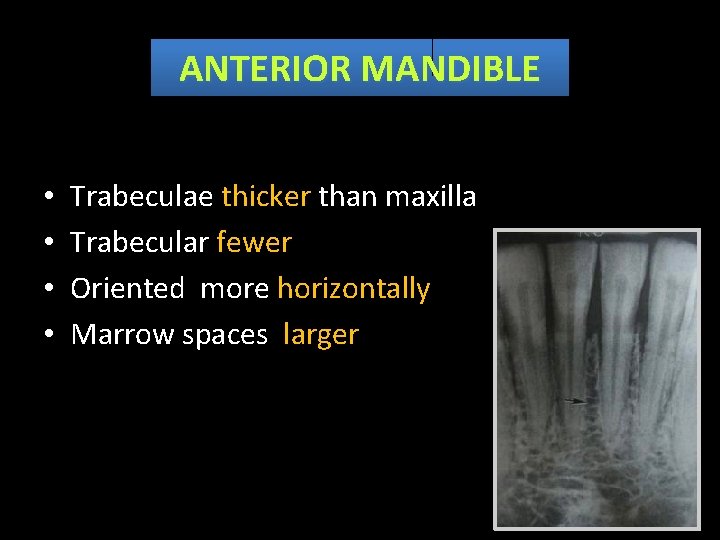
ANTERIOR MANDIBLE • • Trabeculae thicker than maxilla Trabecular fewer Oriented more horizontally Marrow spaces larger
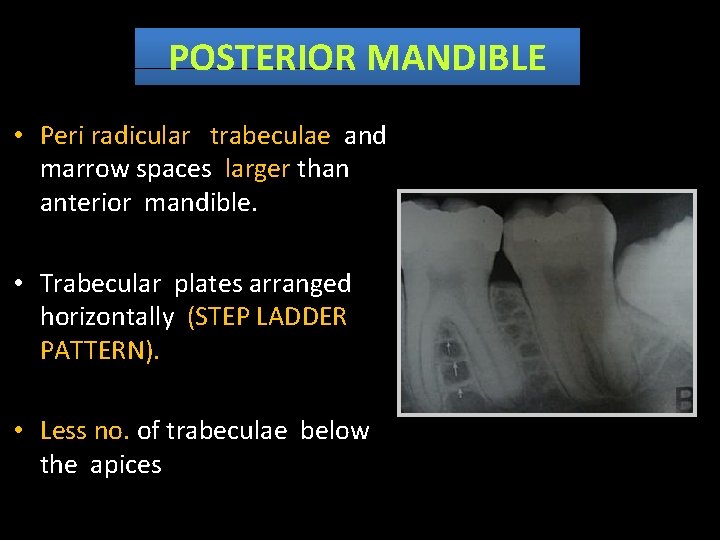
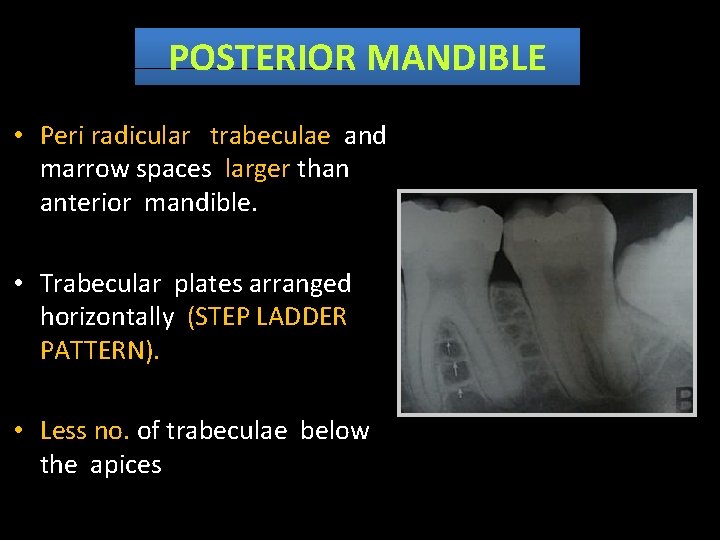
POSTERIOR MANDIBLE • Peri radicular trabeculae and marrow spaces larger than anterior mandible. • Trabecular plates arranged horizontally (STEP LADDER PATTERN). • Less no. of trabeculae below the apices
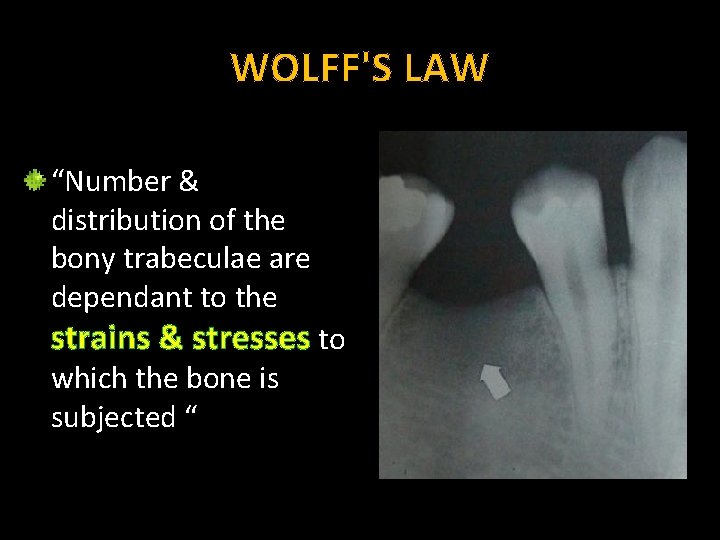
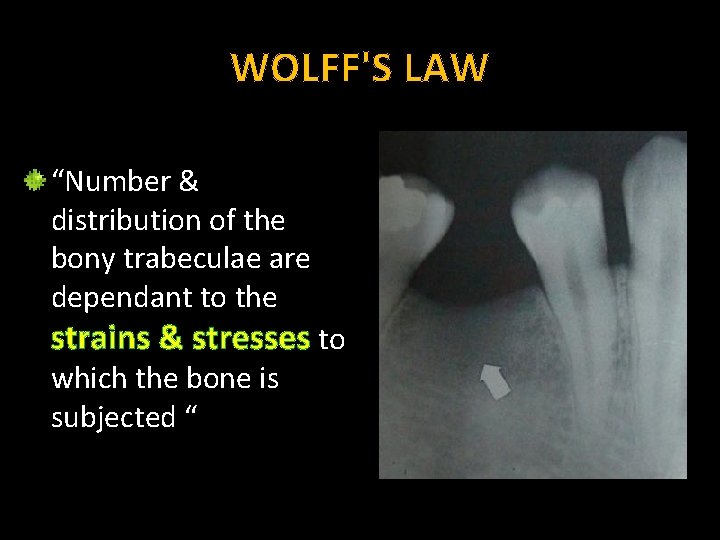
WOLFF'S LAW “Number & distribution of the bony trabeculae are dependant to the strains & stresses to which the bone is subjected “
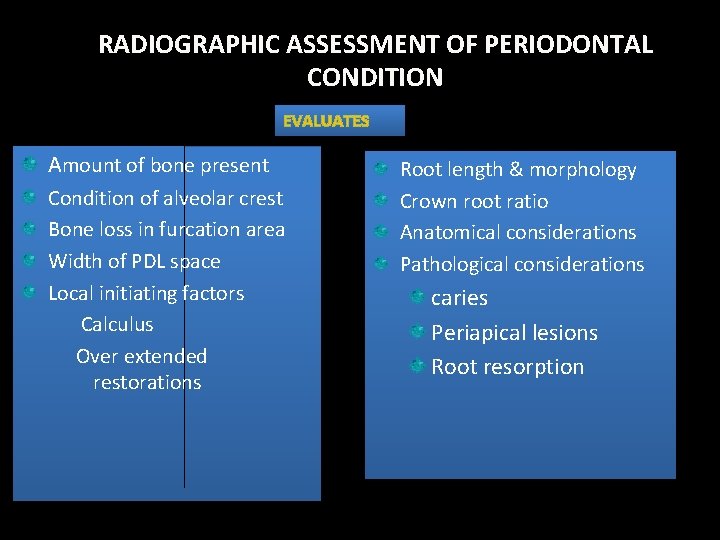
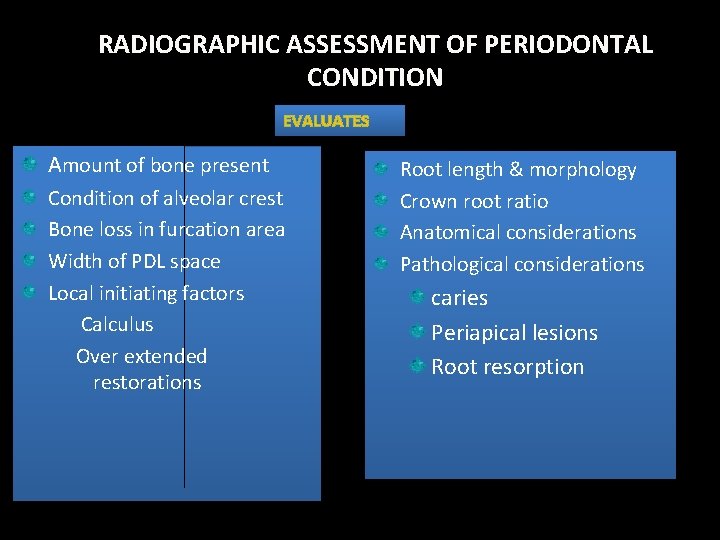
RADIOGRAPHIC ASSESSMENT OF PERIODONTAL CONDITION EVALUATES Amount of bone present Condition of alveolar crest Bone loss in furcation area Width of PDL space Local initiating factors Calculus Over extended restorations Root length & morphology Crown root ratio Anatomical considerations Pathological considerations caries Periapical lesions Root resorption
RADIOLOGICAL CHANGES OF THE SUPPORTING STRUCTURES
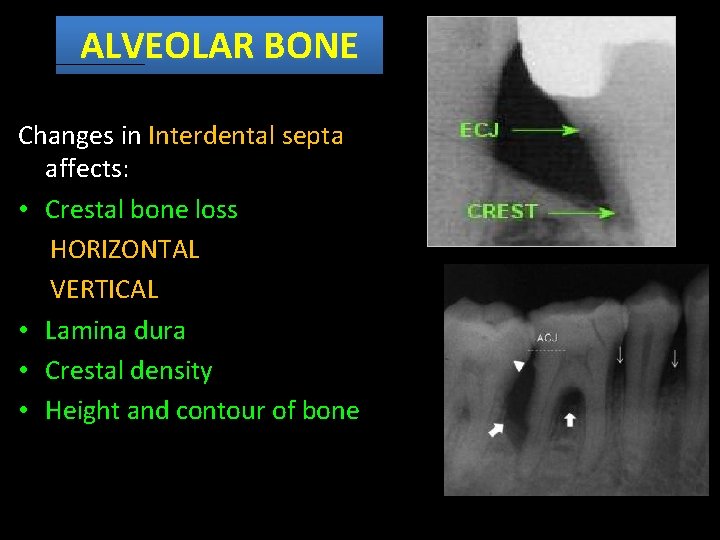
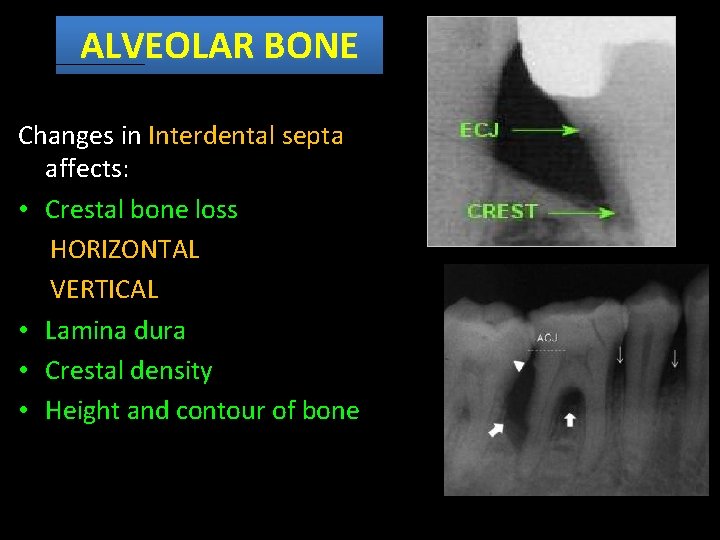
ALVEOLAR BONE Changes in Interdental septa affects: • Crestal bone loss HORIZONTAL VERTICAL • Lamina dura • Crestal density • Height and contour of bone
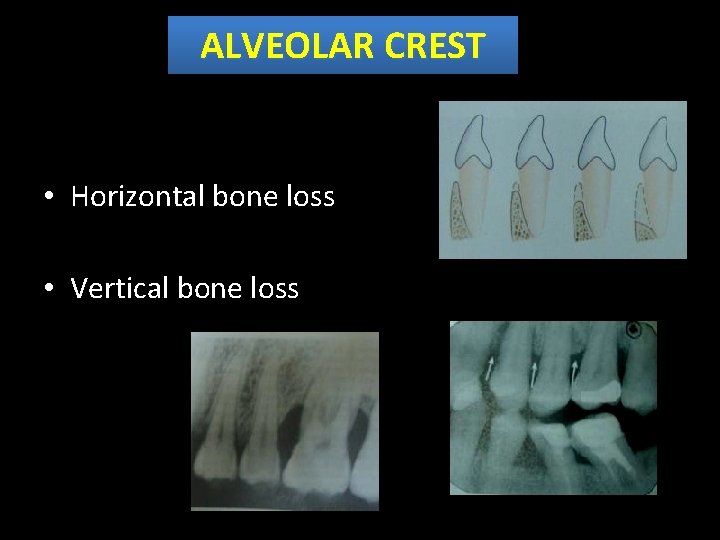
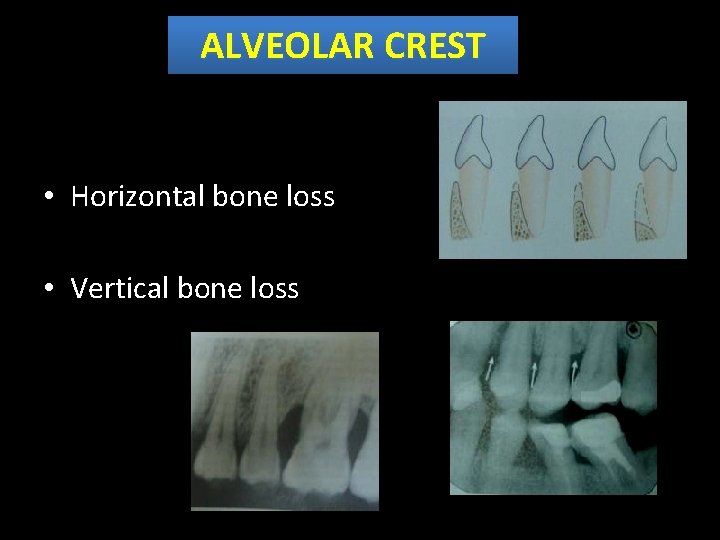
ALVEOLAR CREST • Horizontal bone loss • Vertical bone loss
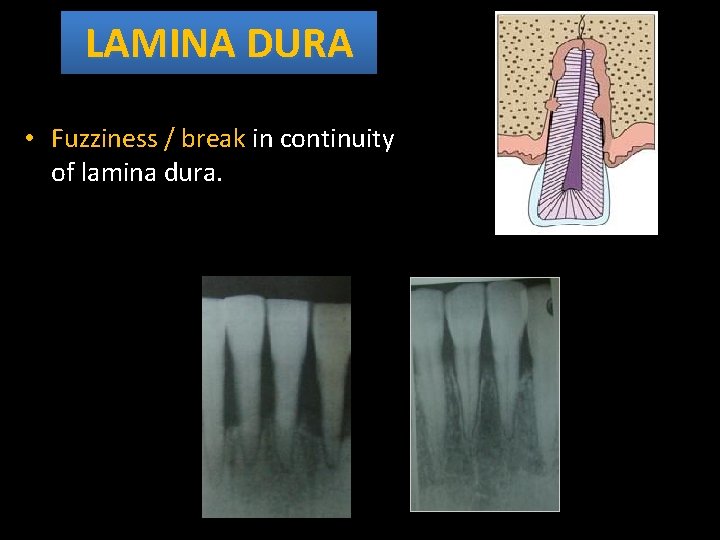
LAMINA DURA • Fuzziness / break in continuity of lamina dura.
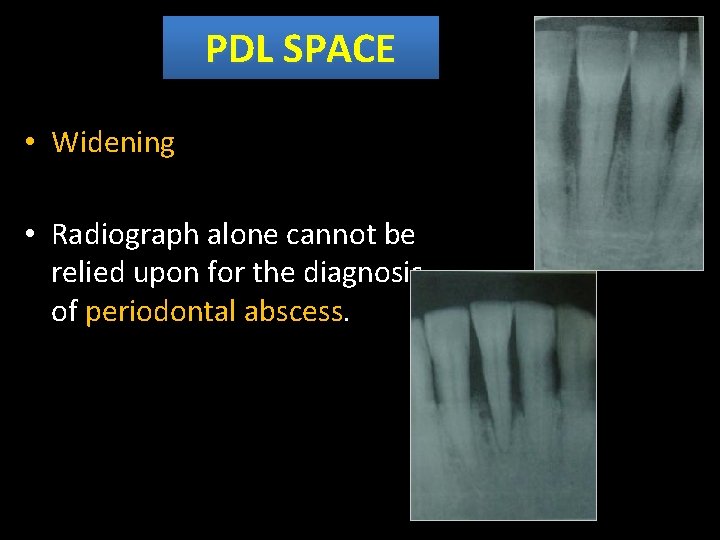
PDL SPACE • Widening • Radiograph alone cannot be relied upon for the diagnosis of periodontal abscess.
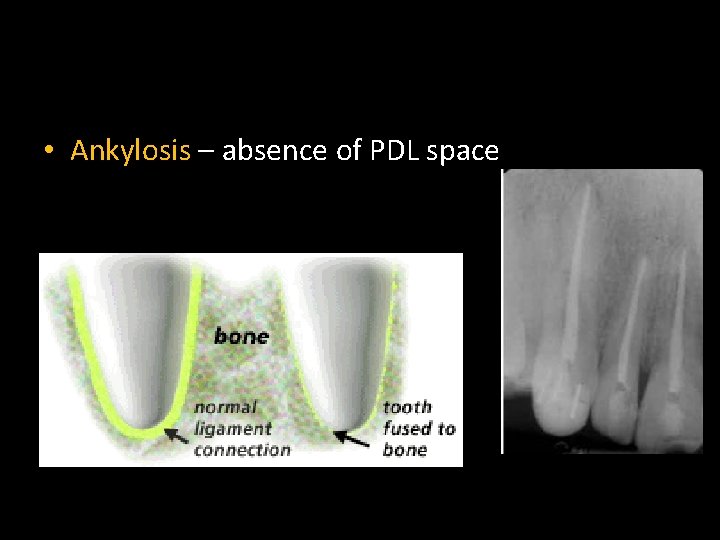
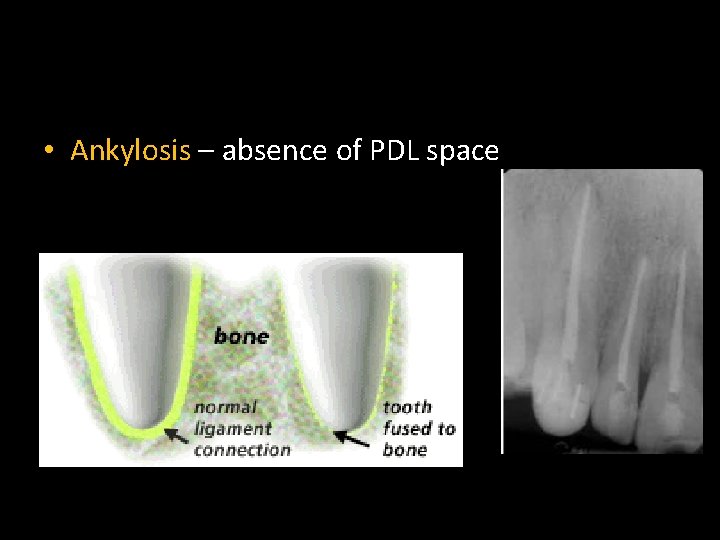
• Ankylosis – absence of PDL space
PERIODONTAL DISEASES

CHRONIC GINGIVITIS • No No bone loss
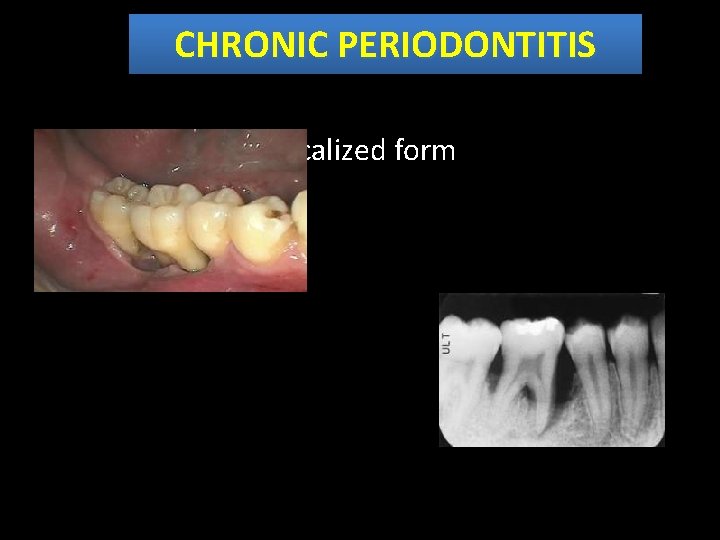
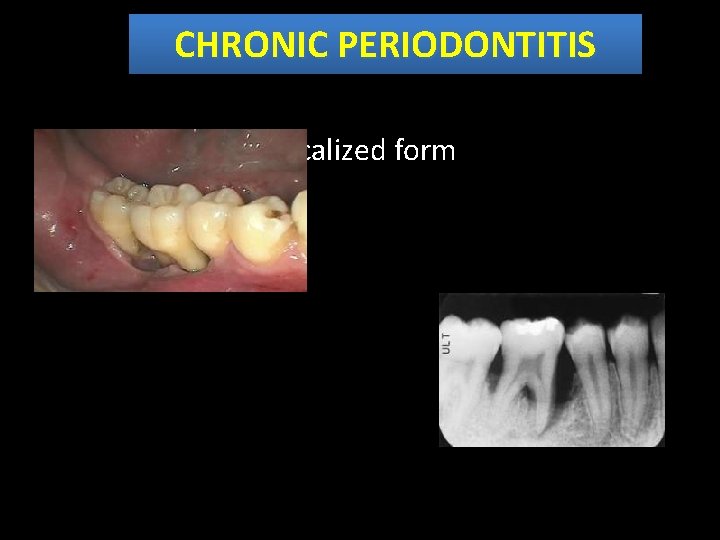
CHRONIC PERIODONTITIS Localized form
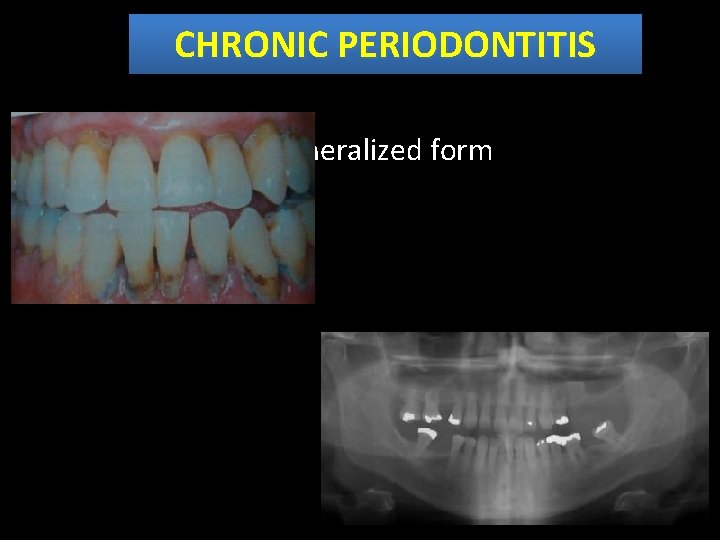
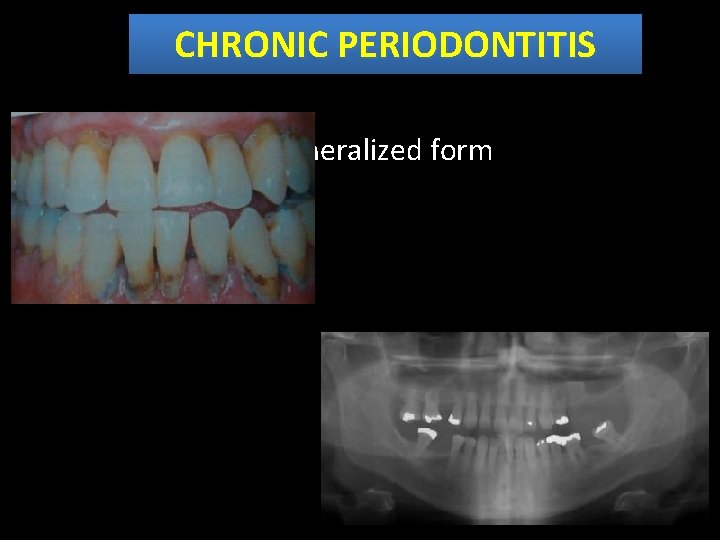
CHRONIC PERIODONTITIS Generalized form
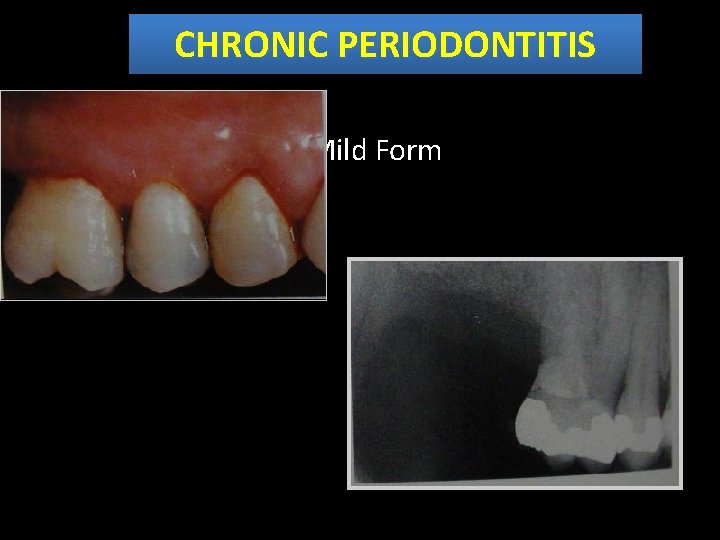
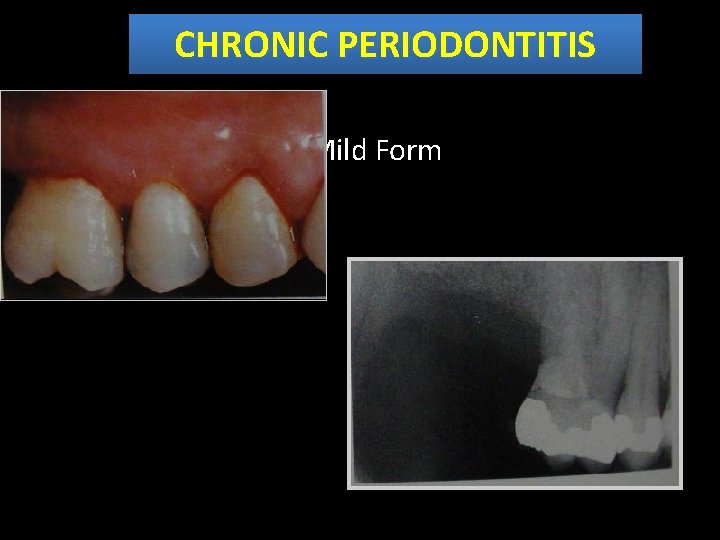
CHRONIC PERIODONTITIS • Mild Form
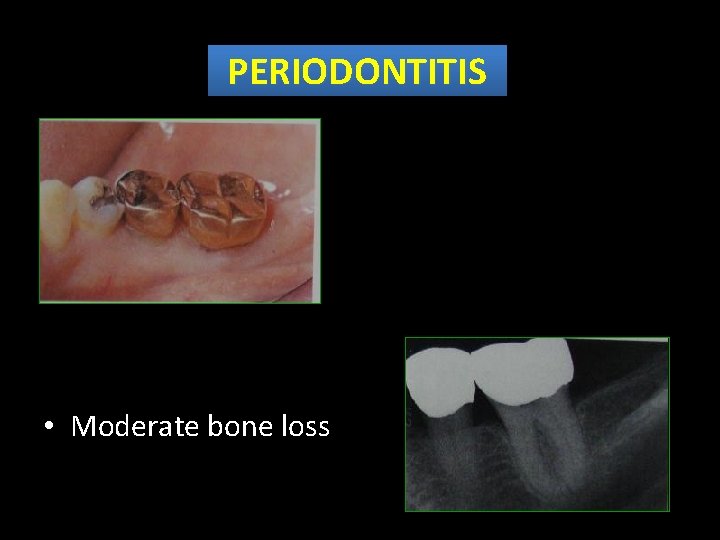
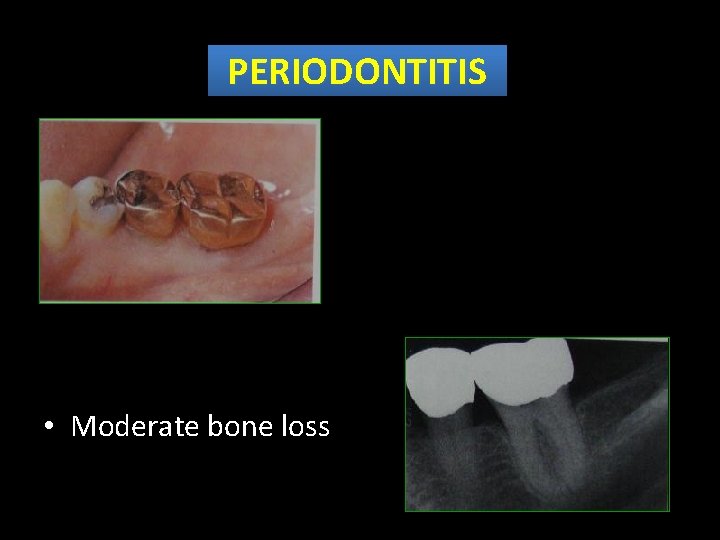
PERIODONTITIS • Moderate bone loss
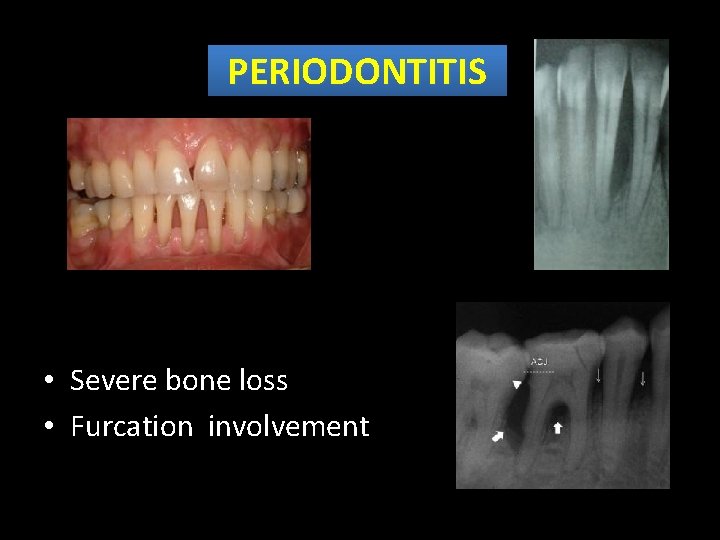
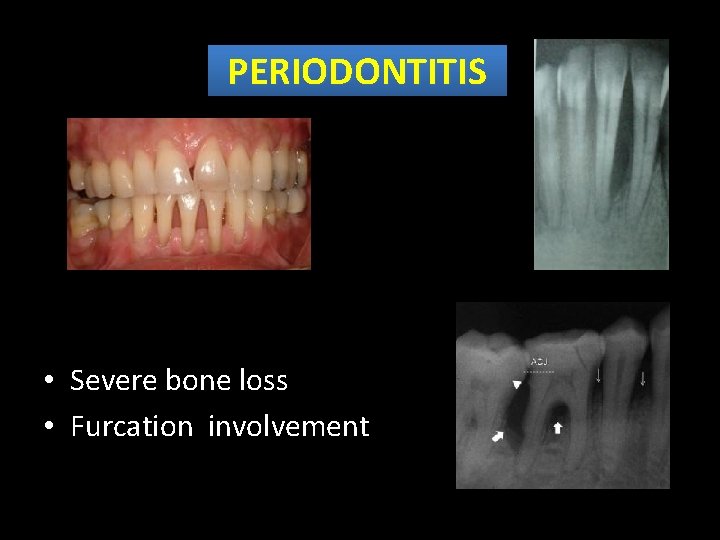
PERIODONTITIS • Severe bone loss • Furcation involvement
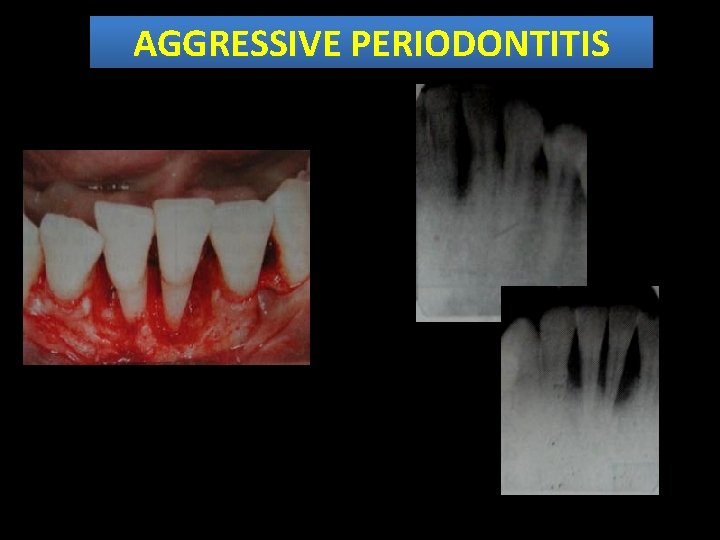
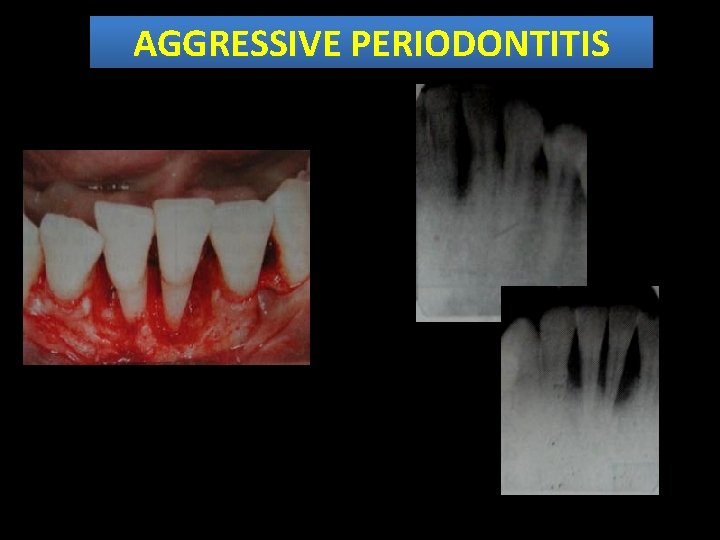
AGGRESSIVE PERIODONTITIS
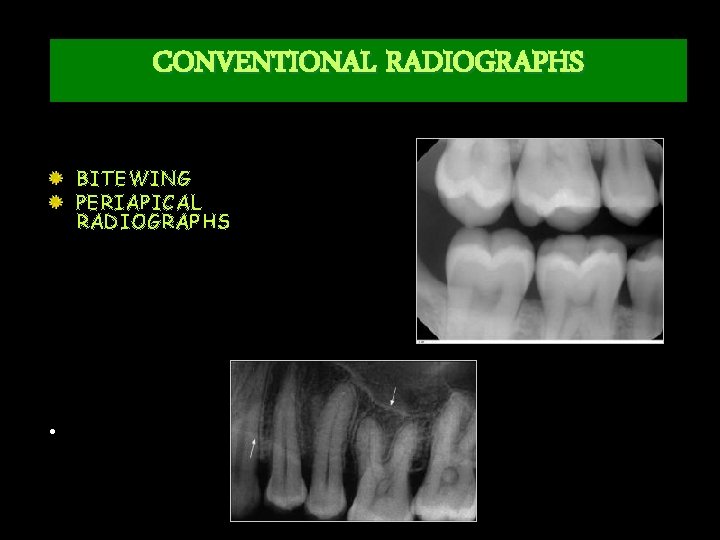
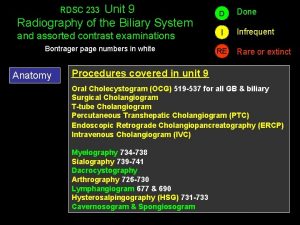
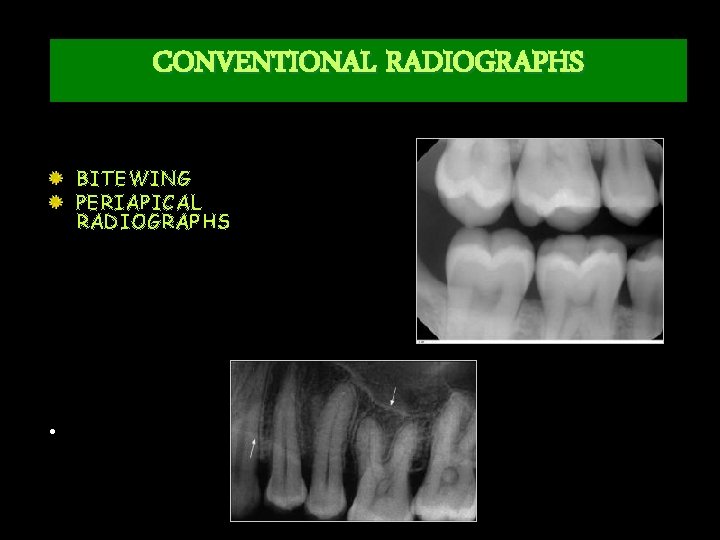
CONVENTIONAL RADIOGRAPHS BITEWING PERIAPICAL RADIOGRAPHS •
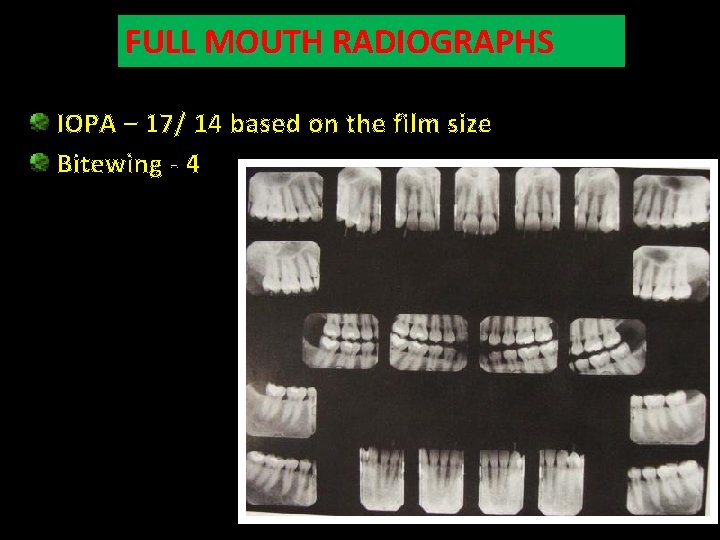
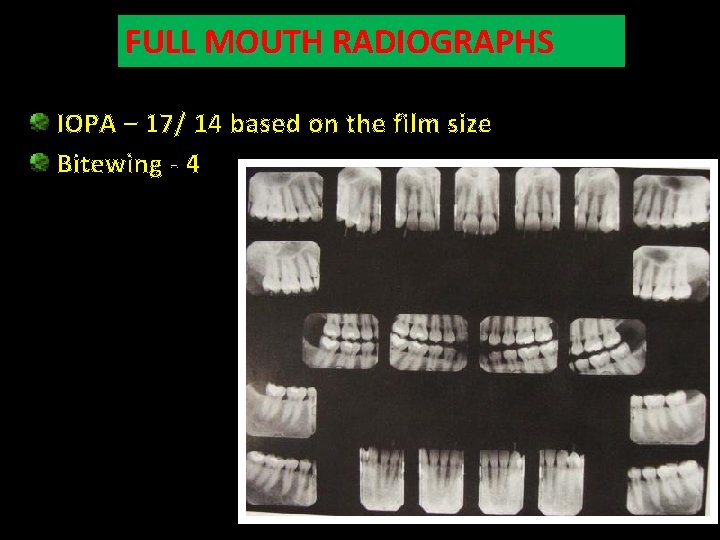
FULL MOUTH RADIOGRAPHS IOPA – 17/ 14 based on the film size Bitewing - 4
PERIAPICAL RADIOGRAPHS TECHNIQUES • BISECTING ANGLE • PARALLELING AXIS
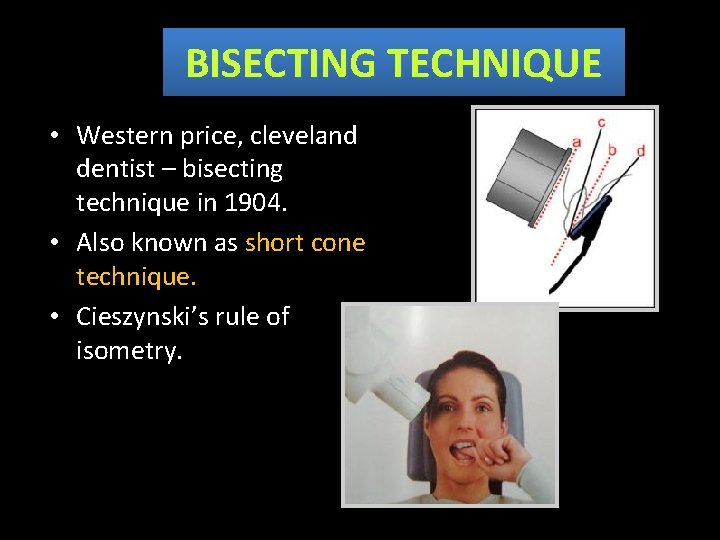
BISECTING TECHNIQUE • Western price, cleveland dentist – bisecting technique in 1904. • Also known as short cone technique. • Cieszynski’s rule of isometry.
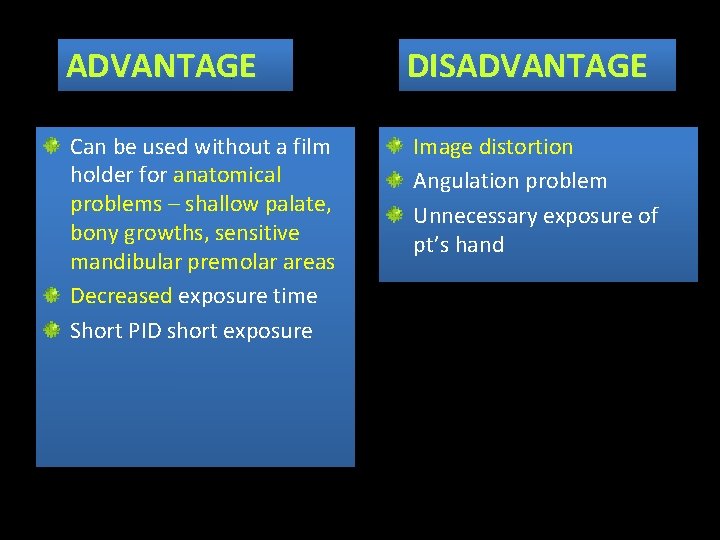
ADVANTAGE DISADVANTAGE Can be used without a film holder for anatomical problems – shallow palate, bony growths, sensitive mandibular premolar areas Decreased exposure time Short PID short exposure Image distortion Angulation problem Unnecessary exposure of pt’s hand
PARALLELING TECHNIQUE • 1 st developed by Mc Cormic in 1920. • Also known as Fitzgerald technique, long cone technique, extended cone technique.
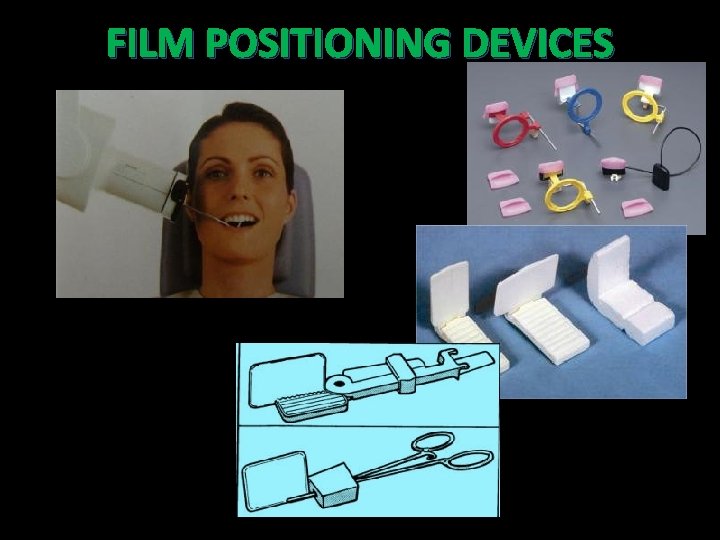
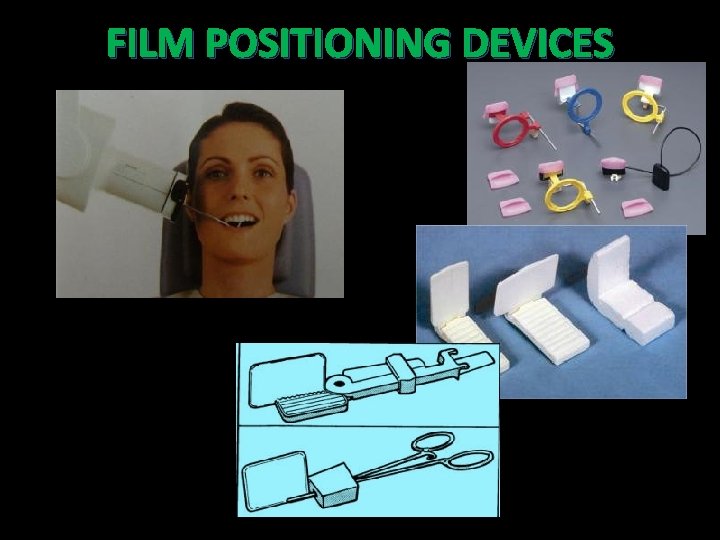
FILM POSITIONING DEVICES
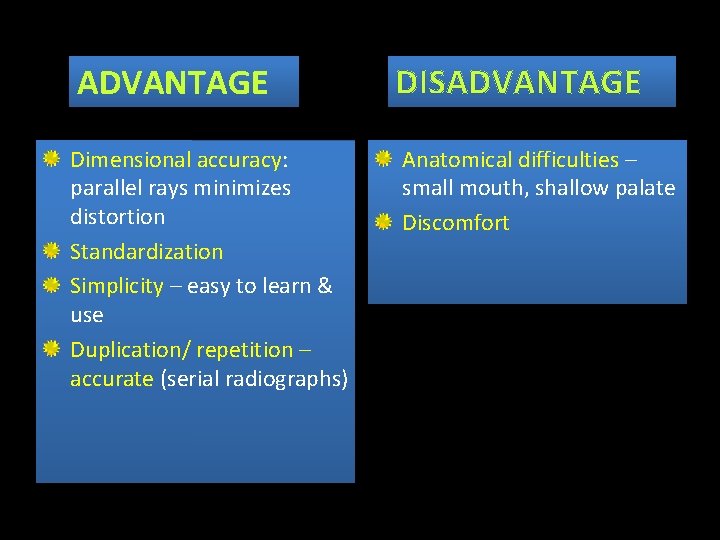
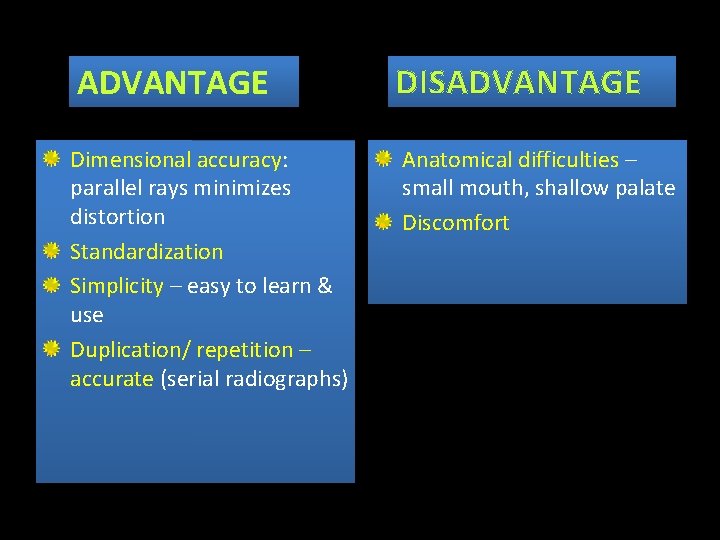
ADVANTAGE DISADVANTAGE Dimensional accuracy: parallel rays minimizes distortion Standardization Simplicity – easy to learn & use Duplication/ repetition – accurate (serial radiographs) Anatomical difficulties – small mouth, shallow palate Discomfort
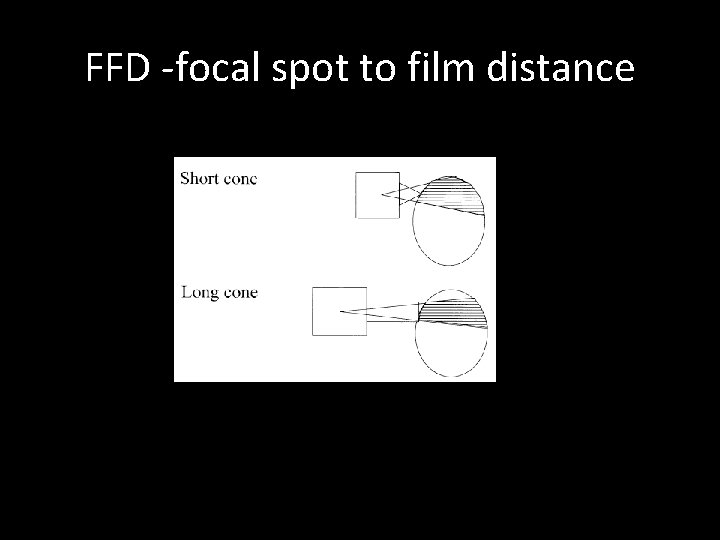
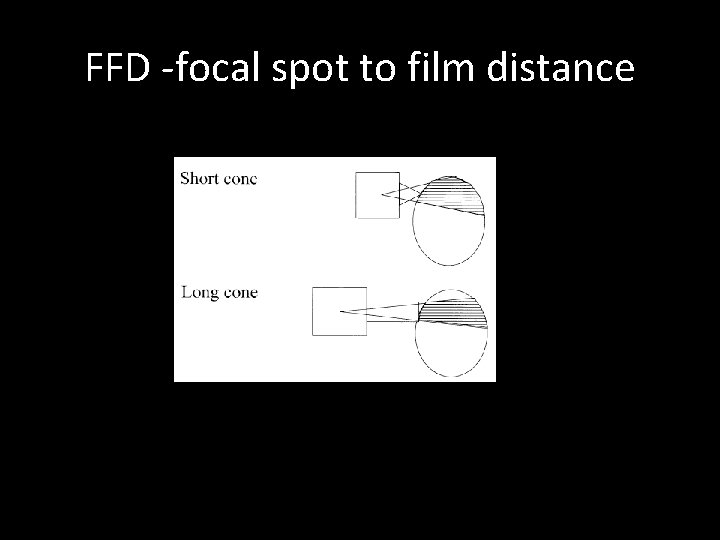
FFD -focal spot to film distance
BISECTING VS PARALLELING TECH PREFERRED TECHNIQUE LONG CONE TECHNIQUE: More accurate Less distortion of images
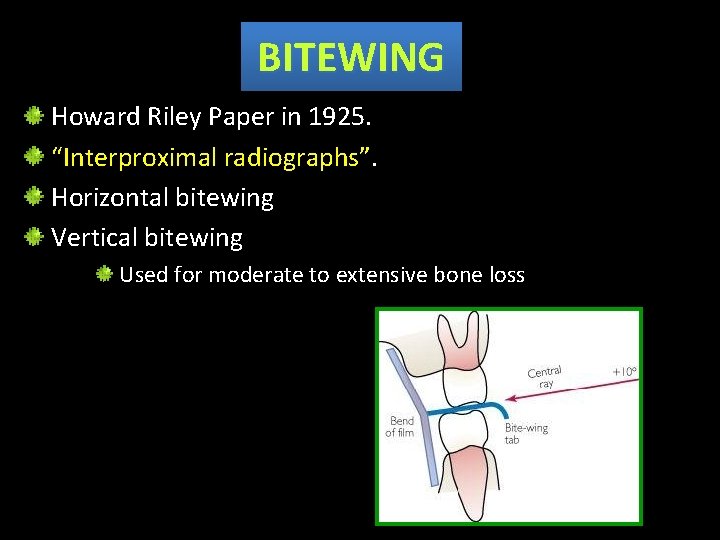
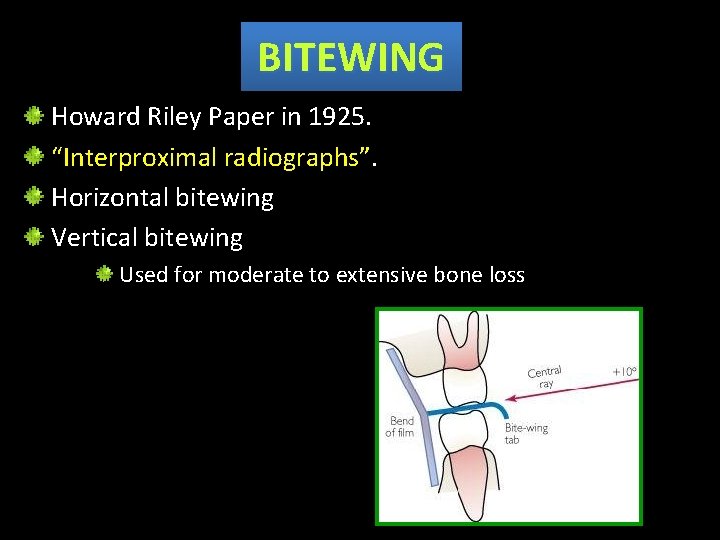
BITEWING Howard Riley Paper in 1925. “Interproximal radiographs”. Horizontal bitewing Vertical bitewing Used for moderate to extensive bone loss
USES Crestal bone level Calculus deposits in interproximal areas Interproximal caries Secondary caries
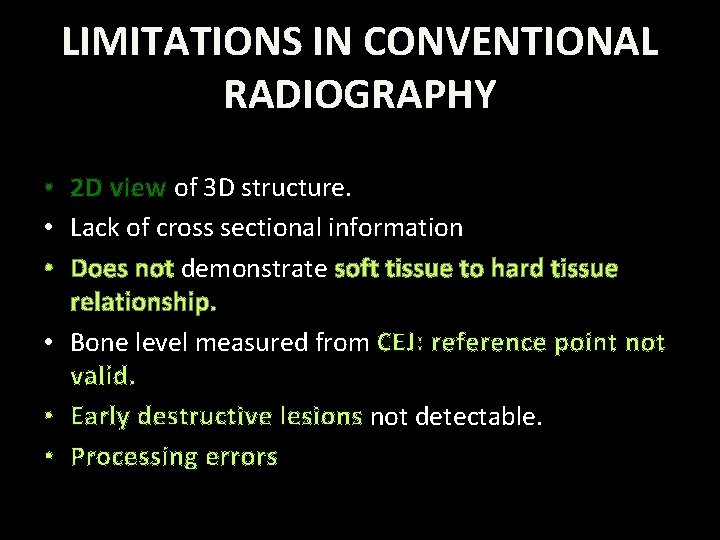
LIMITATIONS IN CONVENTIONAL RADIOGRAPHY • 2 D view of 3 D structure. • Lack of cross sectional information • Does not demonstrate soft tissue to hard tissue relationship. • Bone level measured from CEJ: reference point not valid. • Early destructive lesions not detectable. • Processing errors
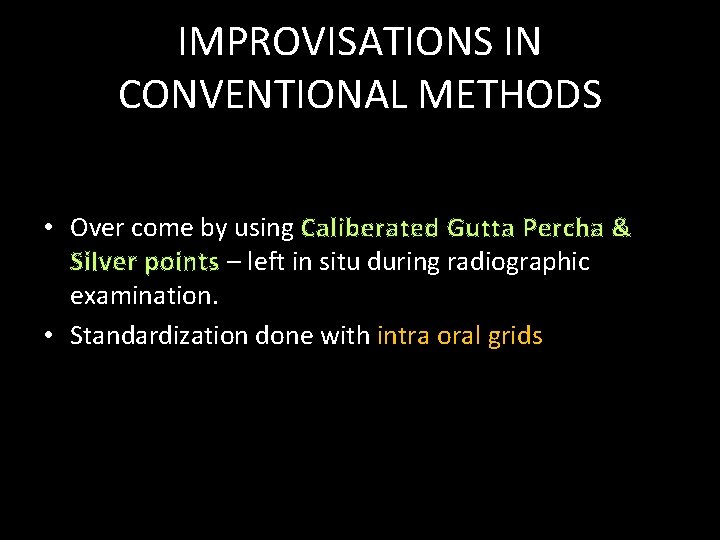
IMPROVISATIONS IN CONVENTIONAL METHODS • Over come by using Caliberated Gutta Percha & Silver points – left in situ during radiographic examination. • Standardization done with intra oral grids
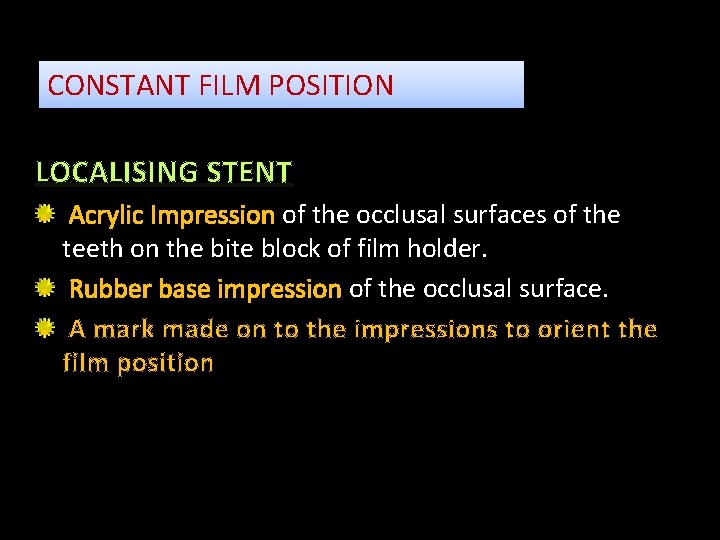
CONSTANT FILM POSITION LOCALISING STENT Acrylic Impression of the occlusal surfaces of the teeth on the bite block of film holder. Rubber base impression of the occlusal surface. A mark made on to the impressions to orient the film position
CONSTANT TUBE GEOMETRY • Relating the tube to positioning devices attached to film holder (Rinn system)
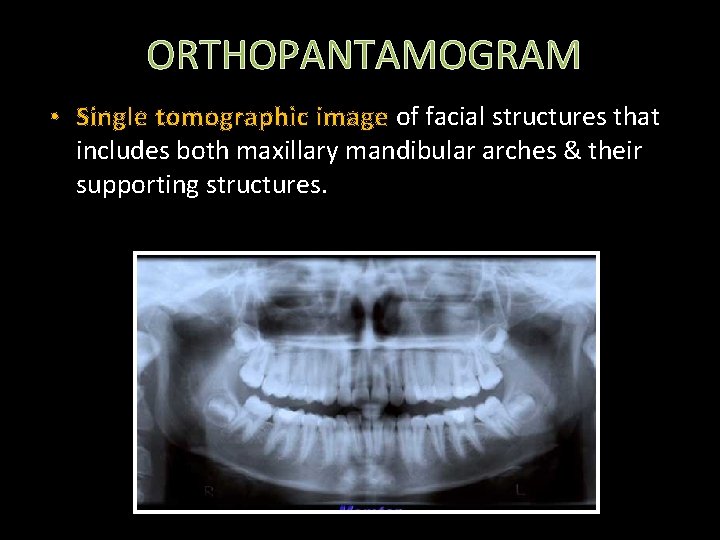
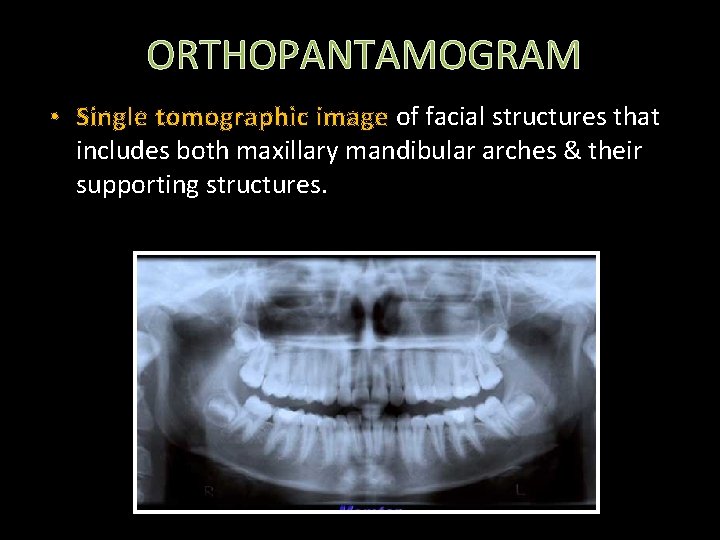
ORTHOPANTAMOGRAM • Single tomographic image of facial structures that includes both maxillary mandibular arches & their supporting structures.
• Curvilinear variant of conventional tomography. • Reciprocal movement of an X ray source and image receptor around a central point or plane – “image layer”
ADAVANTAGES Broad coverage Evaluation of trauma Location of third molars Extensive disease Large lesions Tooth development Retained teeth Development anomalies Low pt radiation dose Convenience of examination of the pt Used in pts unable to open their mouth Short time required Visual Aid in pt education
LIMITATIONS • Lacks fine anatomic details: fine structures of marginal periodontium, small carious lesion. • Overlapping structures & ghost images. • Lack of clarity of midline structures • Unequal magnification & distortion of images. • Clinically important structure – outside image layer - distorted • Resolution – poor
DIGITAL RADIOGRAPHS RADIOVISIOGRAPHY Sensor CCD, CMOS, BCMD, PSP (CCD charged couple device, CMOS Complementory metal oxide semiconductor, PSP photostimulable phosphor plates) BCMD Bulk charged modulated device Processing unit Image display and analysis

Length measurement Magnification Angle measurement IMAGE PROCESSING -ve image Density measurement Histogram Curvature measurement
ADVANTAGES Speed of image capture & display Low X – ray exposure Manipulation of image Use of digital tools Density measurements Improved patient education Ease of storage, transfer& copying
LIMITATIONS • • Smaller detection area in the sensor Patient discomfort Hard to position Subject to operator error.
DIGITAL SUBTRACTION RADIOGRAPHY • Digital subtraction radiography (DSR) was developed in the 1980. PURPOSE: • To subtract all unchanged structures from a pair of serial films & display only the areas of change. • For periodontal films - subtraction of the teeth , cortical bone and trabecular pattern leaving only bone loss or bone gain standing out against a neutral grey back ground.
• This process does not increase the information on the radiograph. • Aids in detection of changes in bone level not visible to the unaided eye in the original radiograph.
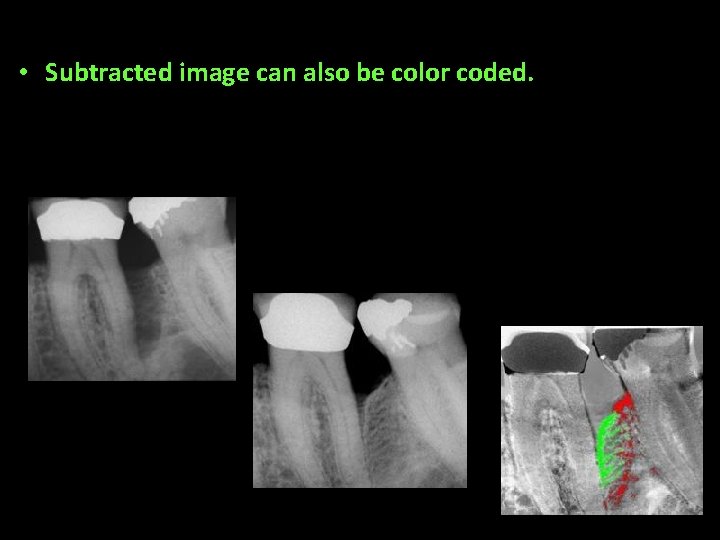
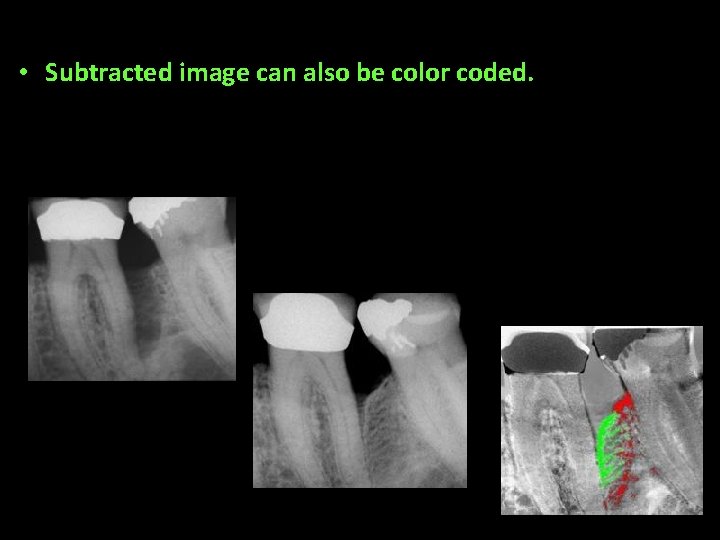
• Subtracted image can also be color coded.
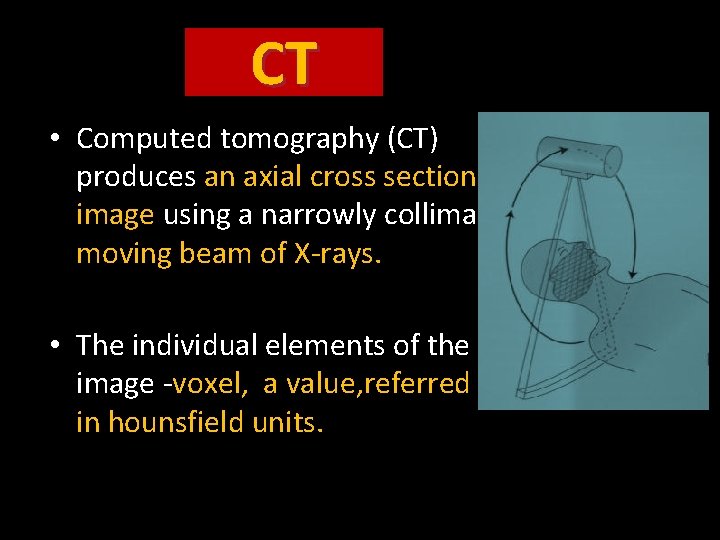
CT • Computed tomography (CT) produces an axial cross sectional image using a narrowly collimated moving beam of X-rays. • The individual elements of the CT image -voxel, a value, referred to in hounsfield units.
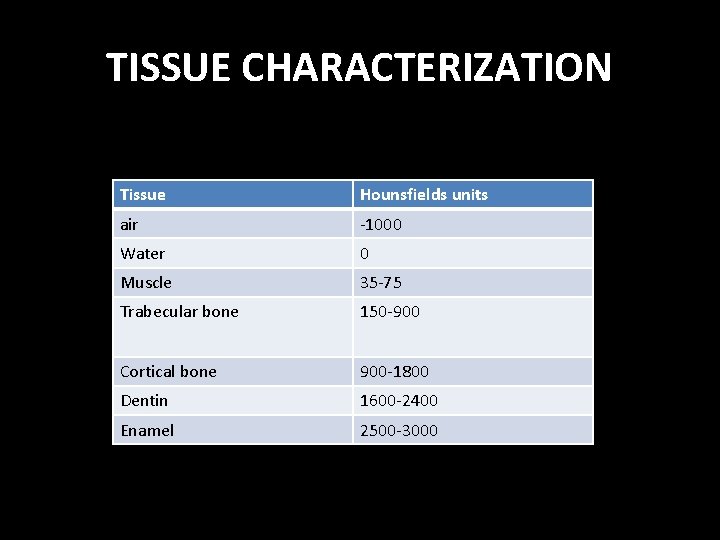
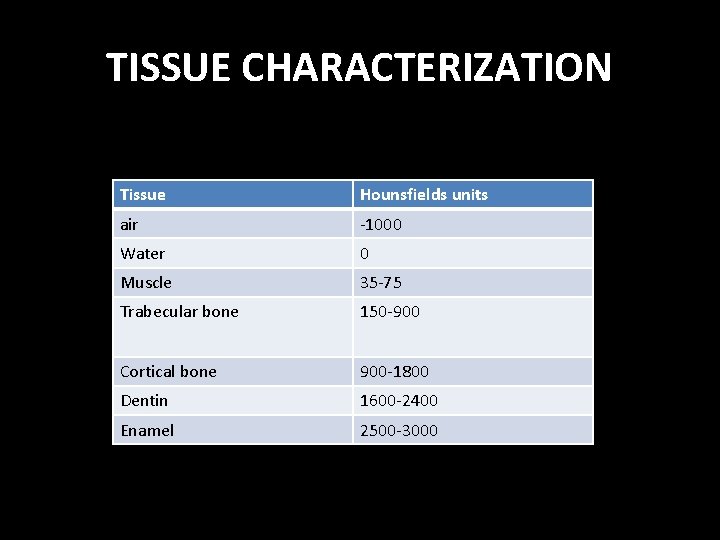
TISSUE CHARACTERIZATION Tissue Hounsfields units air -1000 Water 0 Muscle 35 -75 Trabecular bone 150 -900 Cortical bone 900 -1800 Dentin 1600 -2400 Enamel 2500 -3000
Advantages of CT: • High contrast resolution • It provides sagittal, coronal, axial view of the tissue – multiplanar reformatted imaging • Completely eliminates superimposition of images. • Tissues that differ in physical density by 1% can be distinguished. • It allows reconstruction of cross sectional images of the entire maxilla or mandible or both from a single imaging procedure. • Treatment planning for implants
DISADVANTAGE • Expensive • Technique sensitive • Very high density material like dental restoration produce severe artifact on CT, which makes the interpretation difficult. • Very thin contiguous or overlapping slices may result in a high dose of radiation.
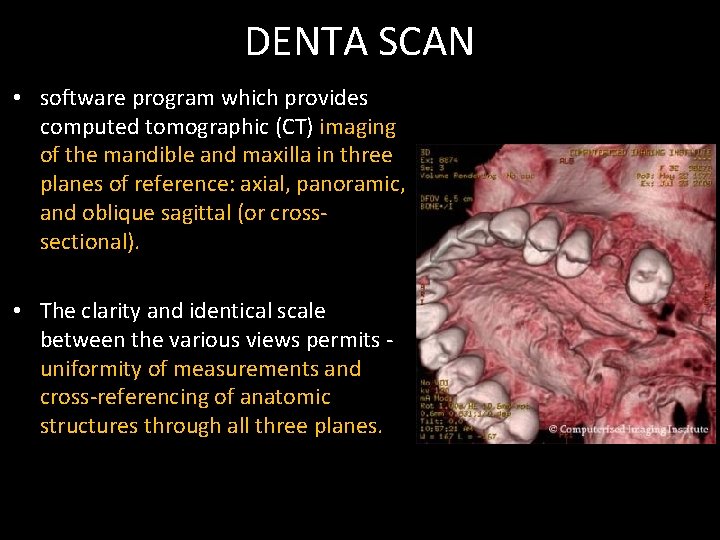
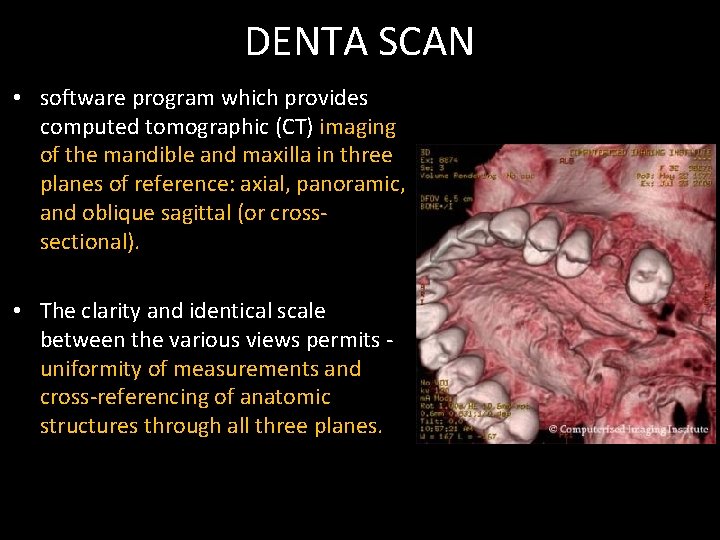
DENTA SCAN • software program which provides computed tomographic (CT) imaging of the mandible and maxilla in three planes of reference: axial, panoramic, and oblique sagittal (or crosssectional). • The clarity and identical scale between the various views permits uniformity of measurements and cross-referencing of anatomic structures through all three planes.
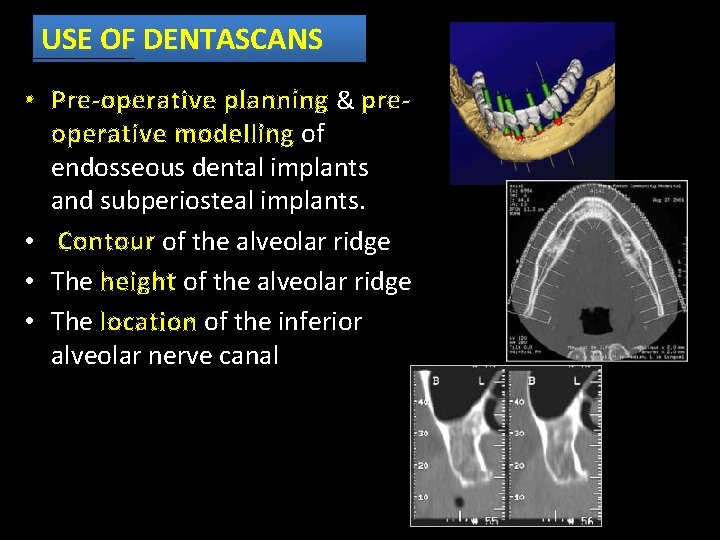
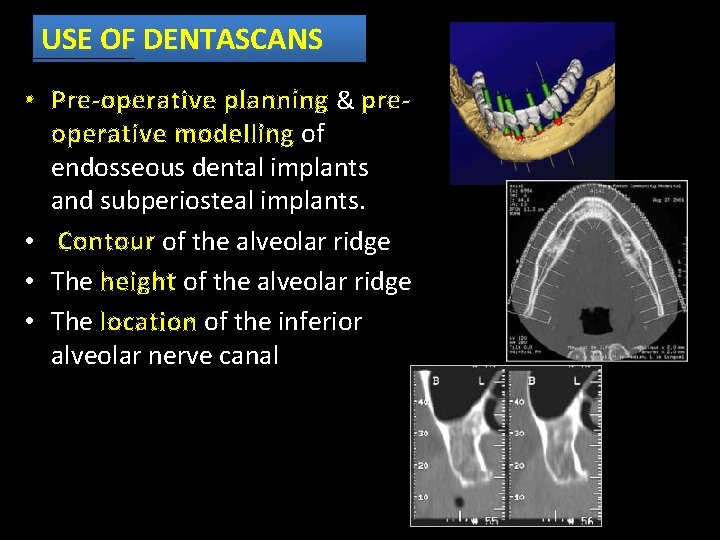
USE OF DENTASCANS • Pre-operative planning & preoperative modelling of endosseous dental implants and subperiosteal implants. • Contour of the alveolar ridge • The height of the alveolar ridge • The location of the inferior alveolar nerve canal
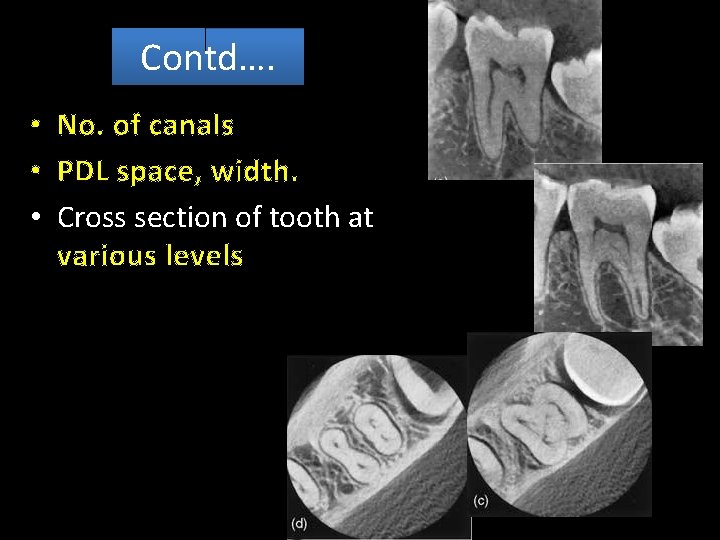
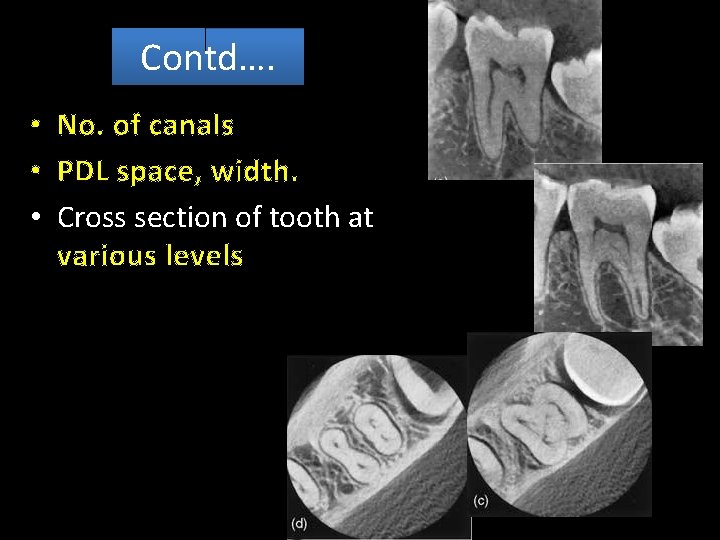
Contd…. • No. of canals • PDL space, width. • Cross section of tooth at various levels
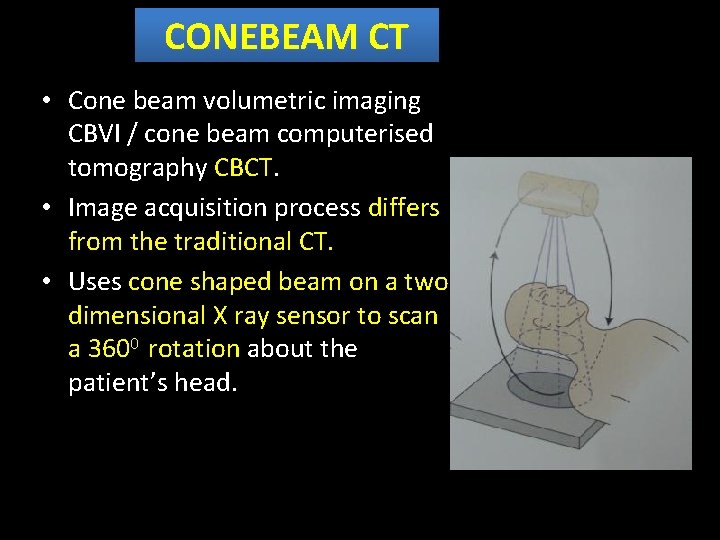
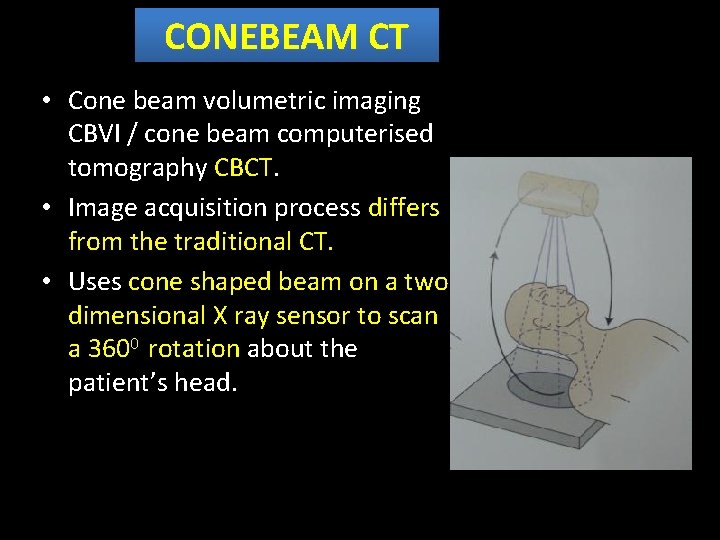
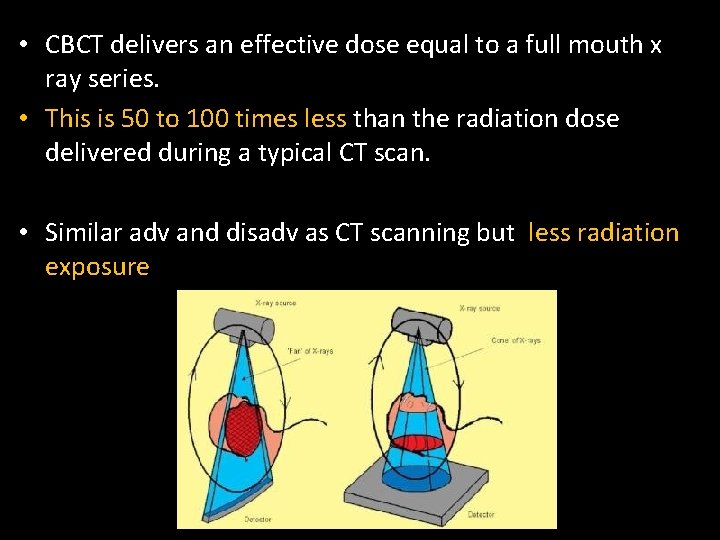
CONEBEAM CT • Cone beam volumetric imaging CBVI / cone beam computerised tomography CBCT. • Image acquisition process differs from the traditional CT. • Uses cone shaped beam on a two dimensional X ray sensor to scan a 3600 rotation about the patient’s head.
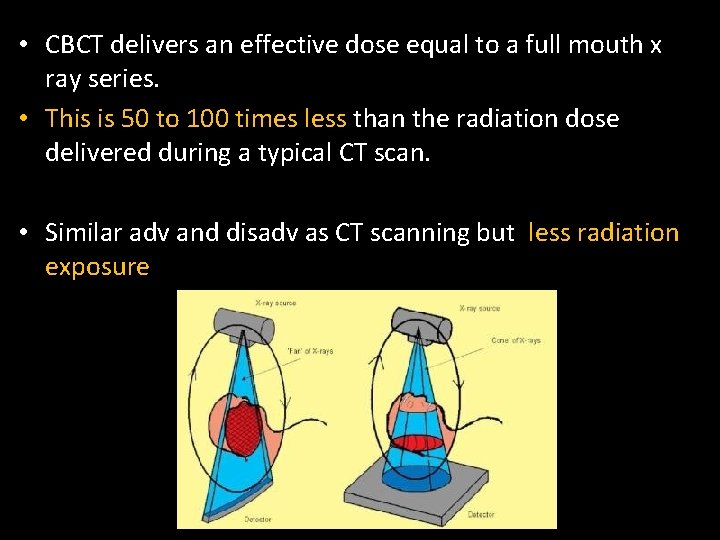
• CBCT delivers an effective dose equal to a full mouth x ray series. • This is 50 to 100 times less than the radiation dose delivered during a typical CT scan. • Similar adv and disadv as CT scanning but less radiation exposure
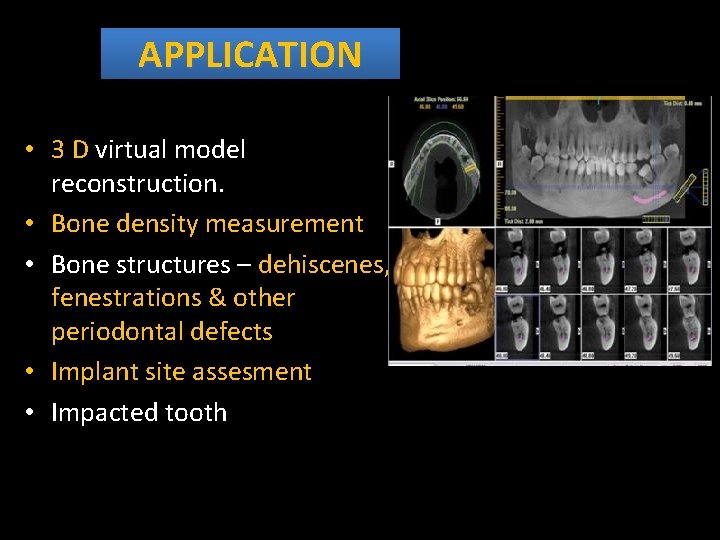
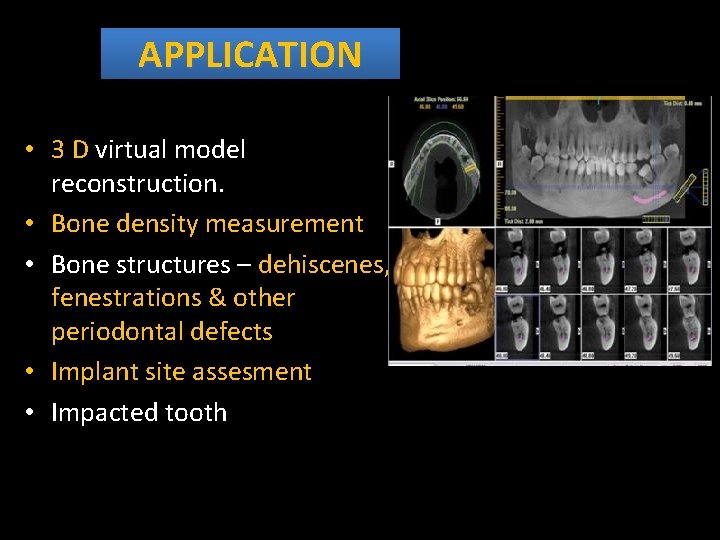
APPLICATION • 3 D virtual model reconstruction. • Bone density measurement • Bone structures – dehiscenes, fenestrations & other periodontal defects • Implant site assesment • Impacted tooth
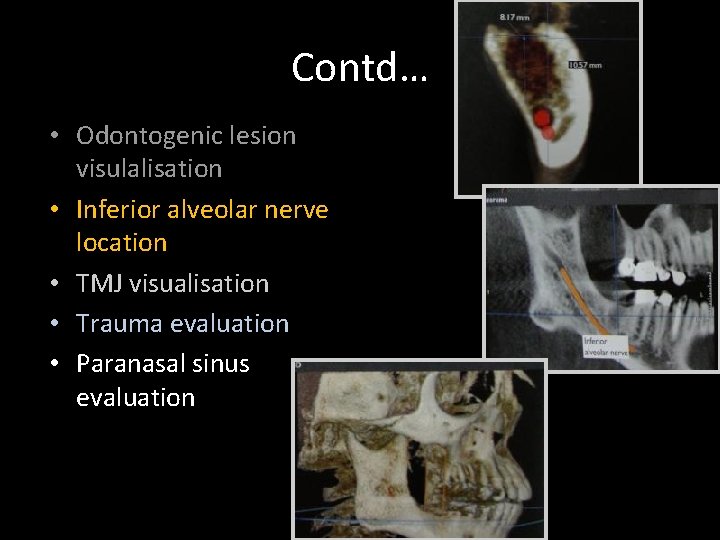
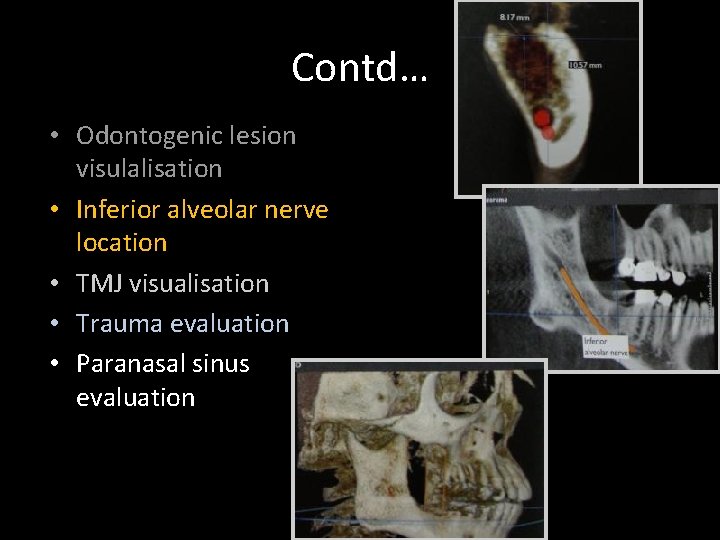
Contd… • Odontogenic lesion visulalisation • Inferior alveolar nerve location • TMJ visualisation • Trauma evaluation • Paranasal sinus evaluation
SCINTIGRAPHY & PDL DISEASES • Bone scintigraphy is a very sensitive method for the detection of osteoblast activity of the skeleton. • The technique consists of imaging the uptake of bone -seeking radiopharmaceuticals, particularly technetium-99 m labeled diphosphonates.
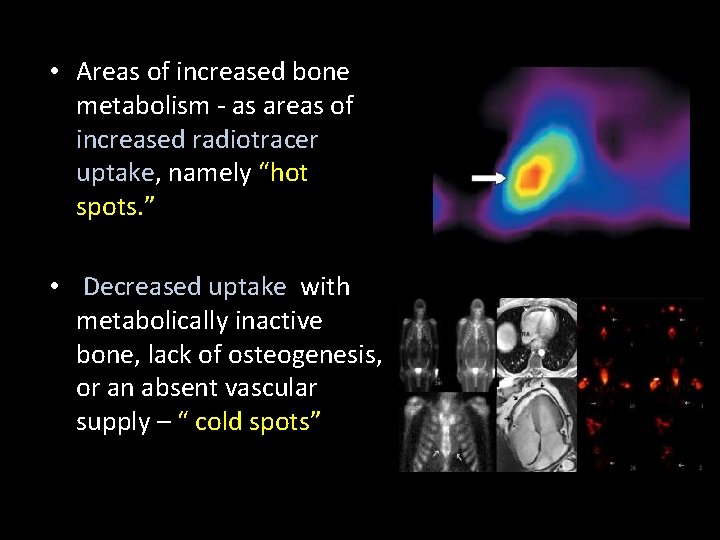
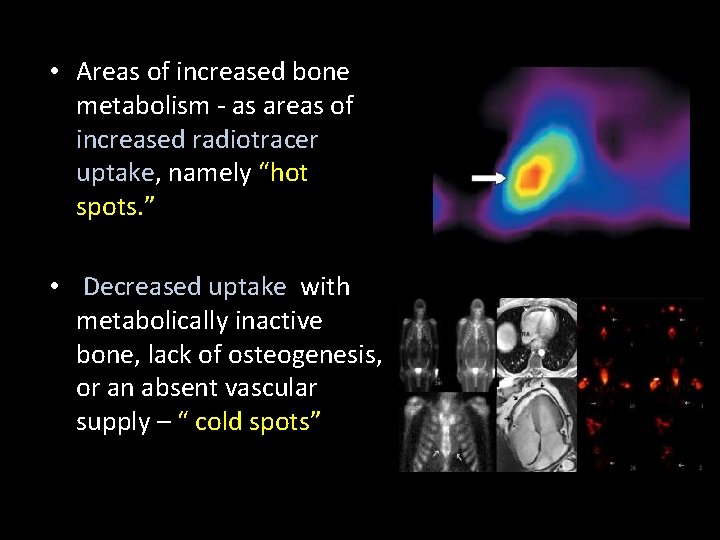
• Areas of increased bone metabolism - as areas of increased radiotracer uptake, namely “hot spots. ” • Decreased uptake with metabolically inactive bone, lack of osteogenesis, or an absent vascular supply – “ cold spots”
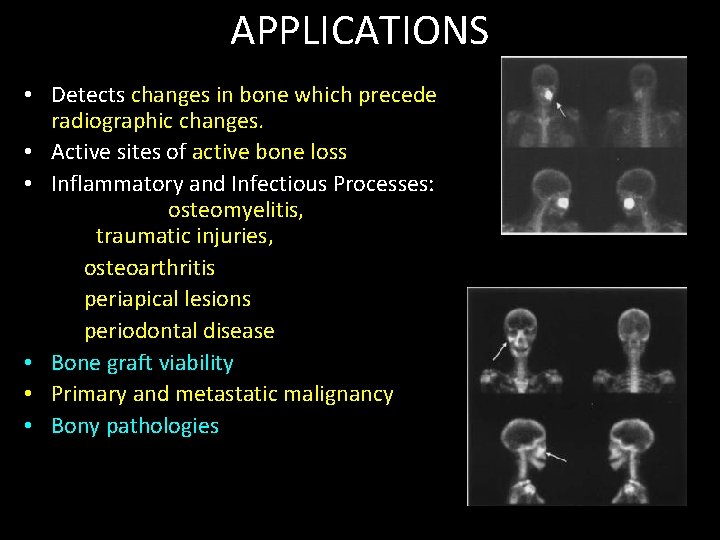
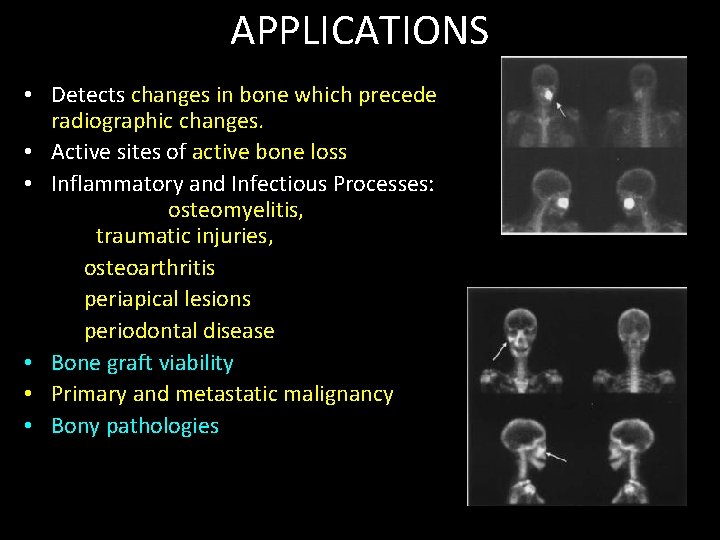
APPLICATIONS • Detects changes in bone which precede radiographic changes. • Active sites of active bone loss • Inflammatory and Infectious Processes: osteomyelitis, traumatic injuries, osteoarthritis periapical lesions periodontal disease • Bone graft viability • Primary and metastatic malignancy • Bony pathologies
LIMITATIONS Changes are not specific to a particular disease hence must be used in conjunction with clinical findings. Expensive
• Radiographs are adjunct to clinical evaluation. • Standardization of radiographic technique in pre & post operative treatment. • Use of accessory devices like film positioning devices, grids & GP points. • Newer imaging modalities to be used with caution
REFERENCES • Oral radiology-white & pharaoh 5 th ed • Diagnosis of dental caries, and periodontal diseases – Dental clinics of north America - 2008 • Carranza-clinical periodontology-10 th edition • Radiographic diagnosis in periodontal disease-journal of periodontology 2000. • Imaging methods in periodontology-perio 2004 • Implant dentistry by mish • British dental journal -1998.

Thank you
 Wilhelm conrad röntgen lebenslauf
Wilhelm conrad röntgen lebenslauf Dental radiographic interpretation ppt
Dental radiographic interpretation ppt Diagnosis of periodontal disease
Diagnosis of periodontal disease Der lindenbaum wilhelm müller analyse
Der lindenbaum wilhelm müller analyse Yyy
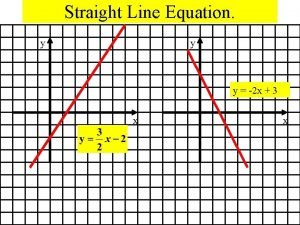
Yyy Gradient formula
Gradient formula ýyy
ýyy Yyy morningstar
Yyy morningstar Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Types of nursing diagnoses
Types of nursing diagnoses Independent nursing interventions
Independent nursing interventions Perbedaan diagnosis gizi dan diagnosis medis
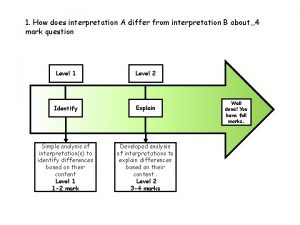
Perbedaan diagnosis gizi dan diagnosis medis How does interpretation b differ from interpretation a
How does interpretation b differ from interpretation a Radiographic film
Radiographic film Absorption unsharpness
Absorption unsharpness Radiographic base line
Radiographic base line Emulsion pickoff artifact
Emulsion pickoff artifact Hampton view positioning
Hampton view positioning Radiographic baseline skull
Radiographic baseline skull Dacrocystogram
Dacrocystogram Sid and oid
Sid and oid Reverse towne projection uses
Reverse towne projection uses Grid conversion formula
Grid conversion formula Horizontal
Horizontal Radiographic films
Radiographic films Loading bench in darkroom
Loading bench in darkroom Junctional epitel
Junctional epitel Periodontal case study
Periodontal case study Seccin 7
Seccin 7 Gingival description
Gingival description Periodontal therapy in female patients
Periodontal therapy in female patients Kista residual adalah
Kista residual adalah Principal fibres of pdl
Principal fibres of pdl Streptokokal gingivitis
Streptokokal gingivitis Aponeurosis palatina
Aponeurosis palatina Corrective phase periodontal therapy
Corrective phase periodontal therapy Periodontal abscess
Periodontal abscess Fibras oblicuas del ligamento periodontal
Fibras oblicuas del ligamento periodontal Do93
Do93 Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Politür lastiği
Politür lastiği Class v facial composite charting
Class v facial composite charting Sharpey fibrilleri
Sharpey fibrilleri Necropulpectomia 1 y 2
Necropulpectomia 1 y 2 Componentes del periodonto
Componentes del periodonto Indikasi enap
Indikasi enap Naber sondu
Naber sondu Periodontal ligament injection definition
Periodontal ligament injection definition Periodontal response to external forces
Periodontal response to external forces Stress strain curve physiotherapy
Stress strain curve physiotherapy Russell periodontal index
Russell periodontal index Periodontal healing
Periodontal healing Aot cyst
Aot cyst Heliprobe 2 positivo
Heliprobe 2 positivo Internal bevel incision
Internal bevel incision Rationale of periodontal treatment
Rationale of periodontal treatment Murat alikan
Murat alikan Classification of periodontal instruments
Classification of periodontal instruments Periodontal disease
Periodontal disease Alveolar crest
Alveolar crest Non-infective
Non-infective Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy Principles of periodontal surgery
Principles of periodontal surgery Fases del tratamiento periodontal
Fases del tratamiento periodontal Lateral periodontal cyst
Lateral periodontal cyst Lennart conrad
Lennart conrad Conrad chang
Conrad chang Conrad lutz
Conrad lutz Dr patrick conrad
Dr patrick conrad Cirrhosis pes statement
Cirrhosis pes statement Conrad mallett detroit
Conrad mallett detroit Inkarnationsvertrag
Inkarnationsvertrag Mevis fraunhofer
Mevis fraunhofer Dr samantha conrad
Dr samantha conrad Conrad bock
Conrad bock Joanna conrad
Joanna conrad Siegel actuarial
Siegel actuarial