Rationale for Periodontal Treatment The effectiveness of periodontal


- Slides: 23
Rationale for Periodontal Treatment
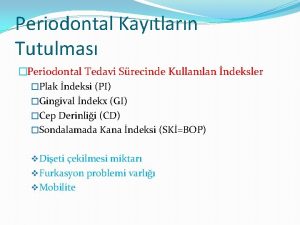
• The effectiveness of periodontal therapy is made possible by the remarkable healing capacity of the periodontal tissues. Periodontal therapy can restore chronically inflamed gingiva so that from a clinical and structural point of view it is almost Identical with gingiva that has never been exposed to excessive plaque accumulation.

Proper Periodontal treatment accomplishs the following: -eliminate pain, gingival inflammation and gingival bleeding, -reduce periodontal pockets and eliminate infection, stop pus formation, arrest the destruction of soft tissue and bone, reduce abnormal tooth mobility, establish optimal occlusal function, - restore tissue destroyed by disease in some instances, reestablish the physiologic gingival contour necessary for the preservation of periodontal health, prevent the recurrence of disease, and reduce tooth loss.

• Local Therapy • The accumulation of plaque • can be favored by a variety of local factors, such as calculus, overhanging margins of restorations, and food impaction. • The removal of plaque and of all the factors that favor its accumulation is therefore the primary consideration in local therapy.
• Abnormal forces on the tooth increase tooth mobility. The thorough elimination of plaque and the prevention of its new formation, by themselves, maintain periodontal health, even if traumatic forces are allowed to persist. However, the elimination of trauma may increase the chances of bone regeneration and gain of attachment. "
Systemic Therapy • Systemic therapy may be employed as an adjunct to local measures and for specific purposes, control of systemic complications 1. acute infections, 2. chemotherapy to prevent harmful effects of post treatment bacteremia, 3. supportive nutritional therapy, 4. control of systemic diseases that aggravate the patient's periodontal Condition.
Systemic therapy for treatment of the periodontal condition and in conjunction with local therapy is indicated in localized and generalized aggressive periodontitis.
• FACTORS THAT AFFECT HEALINg In the periodontium, as elsewhere in the body, healing is affected by local and systemic factors. Systemic conditions that impair healing may reduce the effectiveness of local periodontal treatment and should be corrected before, or along with, local procedures. Local Factors; Healing is also delayed by excessive tissue manipulation during treatment, trauma to the tissues, the presence of foreign bodies, and repetitive treatment procedures
• An adequate blood supply is needed for the increased cellular activity during healing; if this is impaired or insufficient, areas of necrosis will develop and delay the healing process. Healing is improved by debridement (the removal of degenerated and necrotic tissue), immobilization of the healing area, and pressure on the wound. The cellular activity in healing entails an increase in oxygen consumption, but healing of the gingiva is not accelerated by artificially increasing the oxygen supply beyond the normal requirements. '
• Systemic Factors Healing capacity diminishes with age, probably due to atherosclerotic vascular changes, which are common in aging, and result in reduction in blood circulation. Healing is delayed in patients with generalized infections and in those with diabetes and other debilitating diseases. Healing is retarded by insufficient food intake; bodily conditions that interfere with the use of nutrients; and deficiencies in vitamin , proteins, and other nutrients. However, the nutrient requirements of the healing
• Healing is also affected by hormones. Systemically administered glucocorticoids e. g. cortisone hinder repair by depressing the inflammatory reaction or by inhibiting the growth of fibroblasts, the production of collagen, and the formation of endothelial cells.
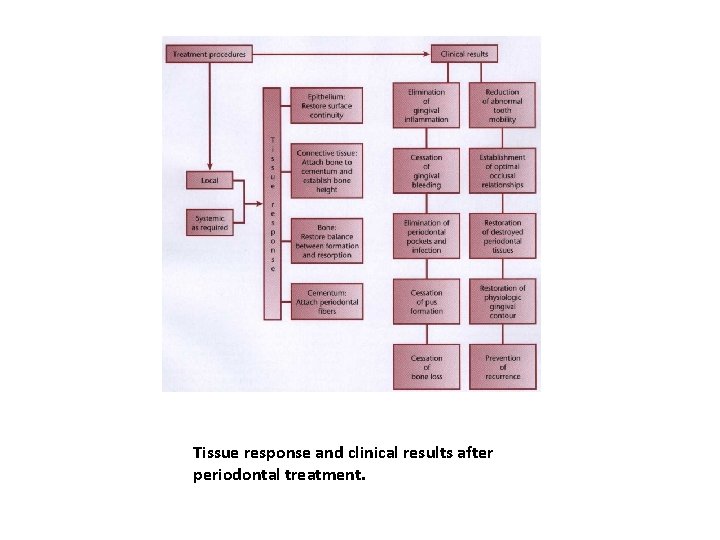
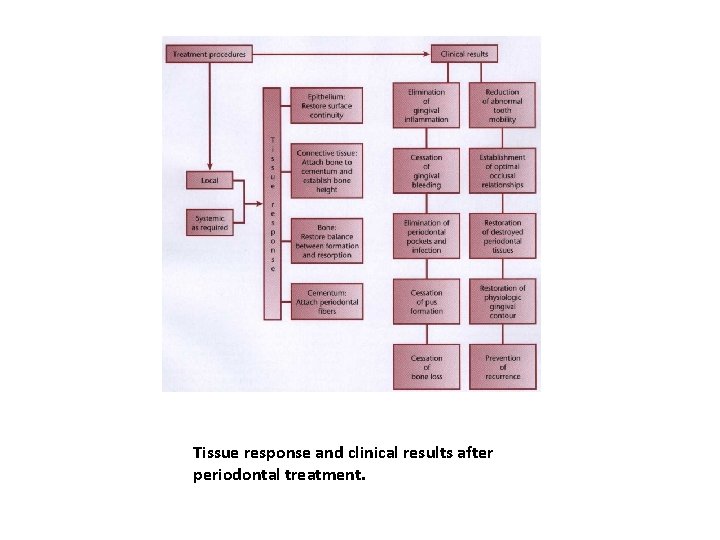
Tissue response and clinical results after periodontal treatment.
• HEALING AFTER PERIODONTAL THERAPY The basic healing processes are the same following all forms of periodontal therapy. They consist of the removal of degenerated tissue debris and the replacement of tissues destroyed by disease. Regeneration, repair, and new attachment are aspects of periodontal healing that have a special bearing on the results obtainable by treatment.
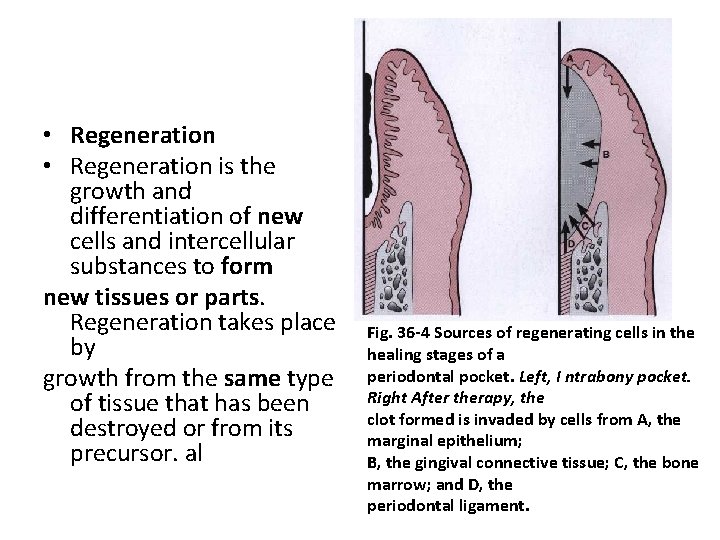
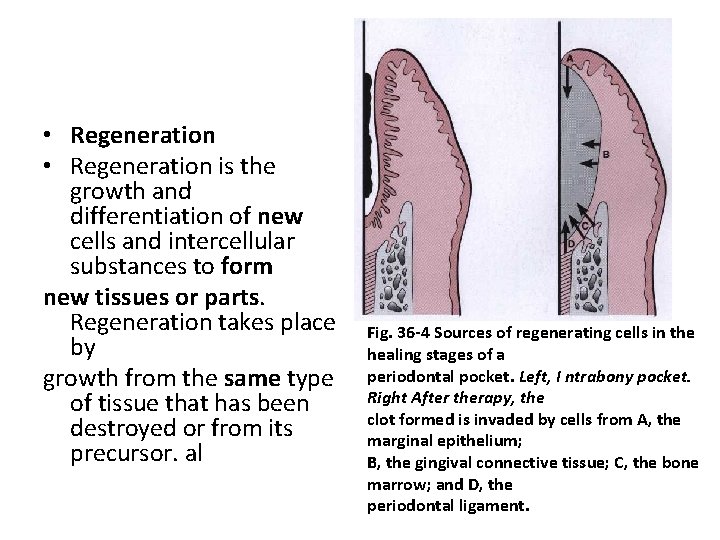
• Regeneration is the growth and. differentiation of new cells and intercellular substances to form new tissues or parts. Regeneration takes place by growth from the same type of tissue that has been destroyed or from its precursor. al Fig. 36 -4 Sources of regenerating cells in the healing stages of a periodontal pocket. Left, I ntrabony pocket. Right After therapy, the clot formed is invaded by cells from A, the marginal epithelium; B, the gingival connective tissue; C, the bone marrow; and D, the periodontal ligament.
• In the periodontium, gingival epithelium is replaced by epithelium, and the underlying connective tissue and periodontal ligament are derived from connective tissue. Bone and cementum are not replaced by existing bone or cementum but by connective tissue, which is the precursor of both. Undifferentiated connective tissue cells develop into osteoblasts and cementoblasts, which form bone and cementum. Regeneration of the periodontium is a continuous physiologic process.
• Regeneration is also going on during destructive periodontal disease. Most gingival and periodontal diseases are chronic inflammatory processes and, as such, are healing lesions. Regeneration is part of the healing. However, bacteria and bacterial products that perpetuate the disease process and the inflammatory exudate they elicit are injurious to the regenerating cells and tissues and prevent the healing from proceeding to completion.
• Repair simply restores the continuity of the diseased marginal gingiva and reestablishes a normal gingival sulcus at the same level on the root as the base of the preexistent periodontal pocket
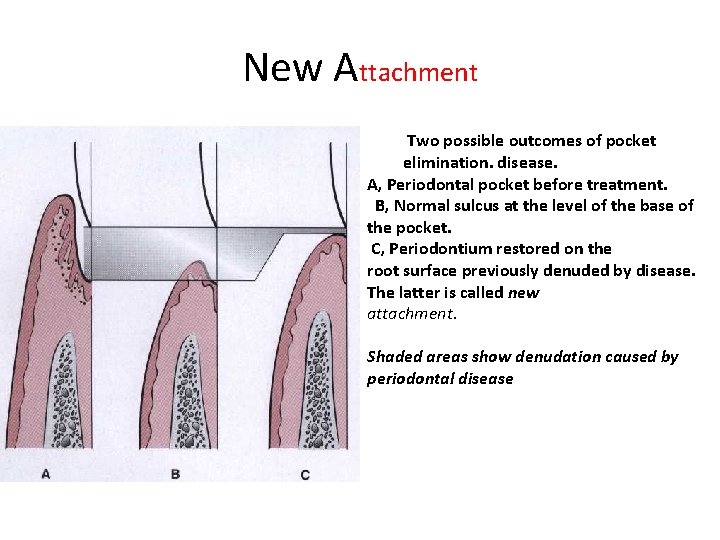
• New Attachment • New attachment is the embedding of new periodontal ligament fibers into new cementum and the attachment of the gingival epithelium to a tooth surface previously denuded by disease
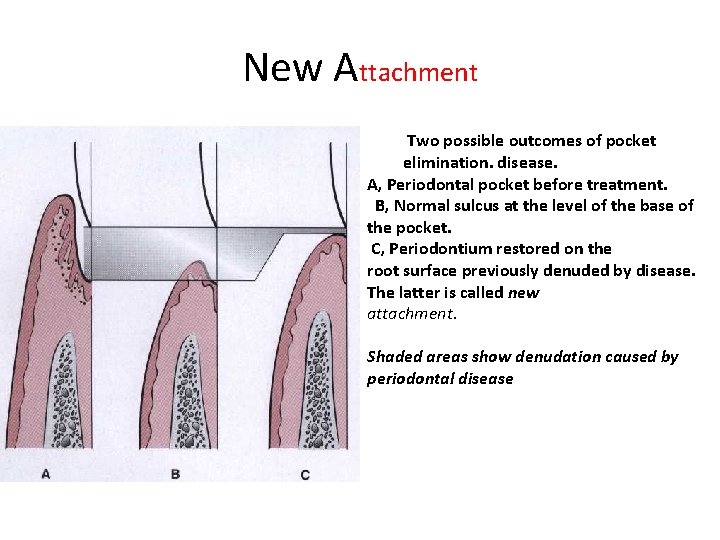
New Attachment Two possible outcomes of pocket elimination. disease. A, Periodontal pocket before treatment. B, Normal sulcus at the level of the base of the pocket. C, Periodontium restored on the root surface previously denuded by disease. The latter is called new attachment. Shaded areas show denudation caused by periodontal disease
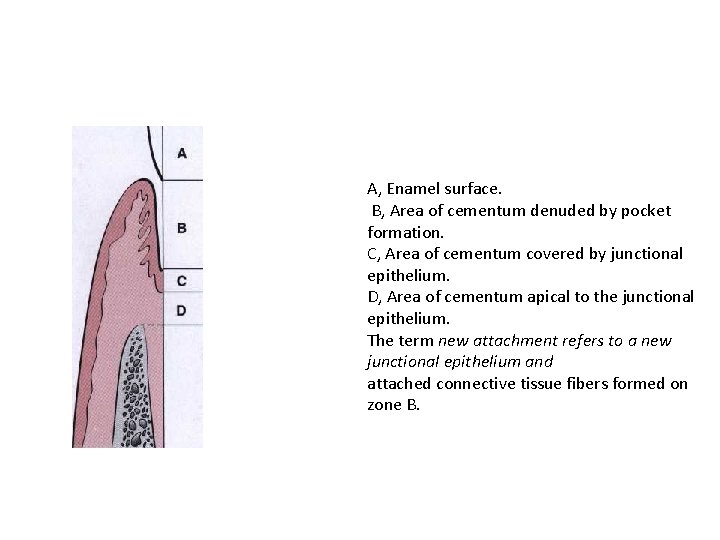
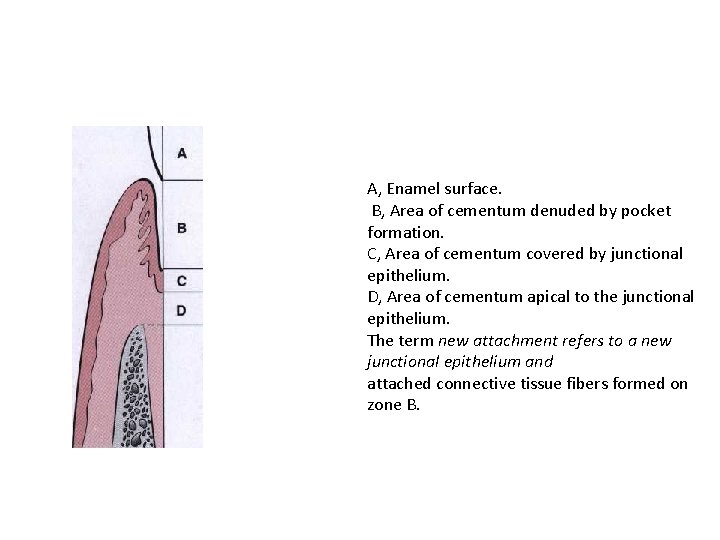
A, Enamel surface. B, Area of cementum denuded by pocket formation. C, Area of cementum covered by junctional epithelium. D, Area of cementum apical to the junctional epithelium. The term new attachment refers to a new junctional epithelium and attached connective tissue fibers formed on zone B.
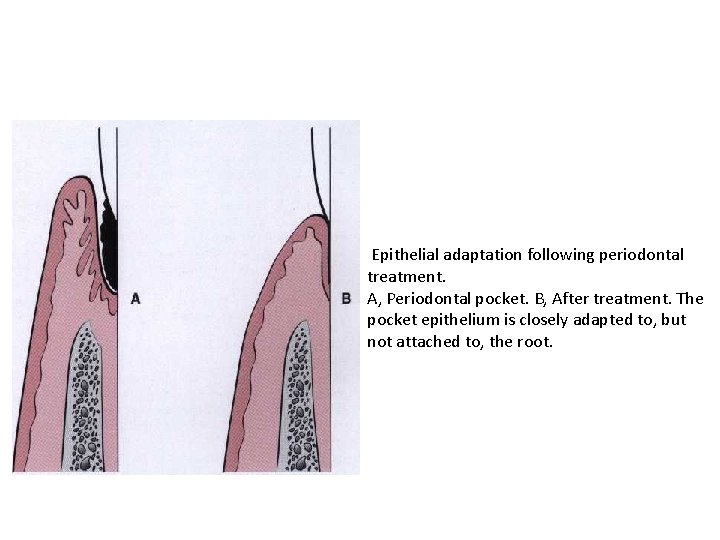
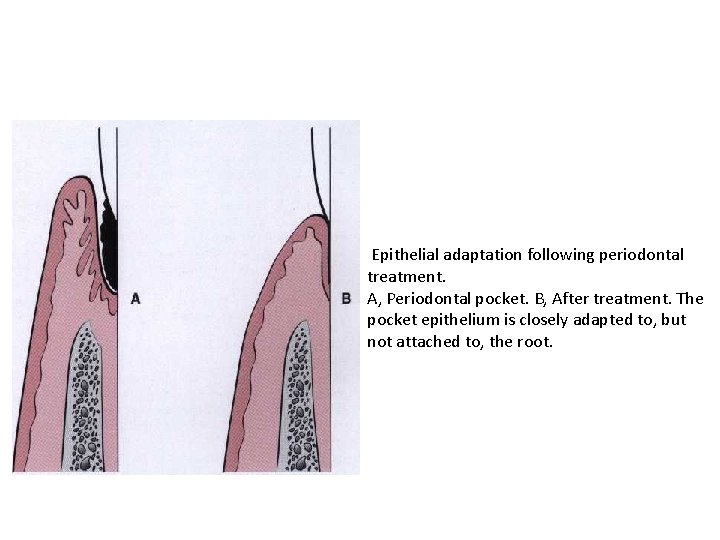
Epithelial adaptation following periodontal treatment. A, Periodontal pocket. B, After treatment. The pocket epithelium is closely adapted to, but not attached to, the root.
• The final outcome of periodontal pocket healing depends on the sequence of events during the healing stages. • If the epithelium proliferates along the tooth surface before the other tissues reach the area, the result will be a long junctional epithelium. If the cells from the gingival connective tissue are the first to populate the
• area, the result will be fibers parallel to the tooth surface and remodeling of the alveolar bone with no attachment to the cementum. If bone cells arrive first, root resorption and ankylosis may occur. Finally, only when cells from the periodontal ligament proliferate coronally there is formation of new cementum and periodontal ligament. • Several methods have been recommended to improve the likelihood of attaining new attachment.
 Rationale for periodontal treatment
Rationale for periodontal treatment Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden Tack för att ni har lyssnat
Tack för att ni har lyssnat Mjälthilus
Mjälthilus Lufttryck formel
Lufttryck formel Läkarutlåtande för livränta
Läkarutlåtande för livränta Tack för att ni lyssnade
Tack för att ni lyssnade Egg för emanuel
Egg för emanuel Bra mat för unga idrottare
Bra mat för unga idrottare A gastrica
A gastrica Tack för att ni har lyssnat
Tack för att ni har lyssnat Vad är vanlig celldelning
Vad är vanlig celldelning Jiddisch
Jiddisch Novell typiska drag
Novell typiska drag Rutin för avvikelsehantering
Rutin för avvikelsehantering Myndigheten för delaktighet
Myndigheten för delaktighet Delegerande ledarstil
Delegerande ledarstil Rbk fuktmätning
Rbk fuktmätning Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Debattinlägg mall
Debattinlägg mall Tack för att ni har lyssnat
Tack för att ni har lyssnat Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Bästa kameran för astrofoto
Bästa kameran för astrofoto