PERIODONTAL LIGAMENT CONTENTS INTRODUCTION PERIODONTAL LIGAMENT definition synonyms


- Slides: 39
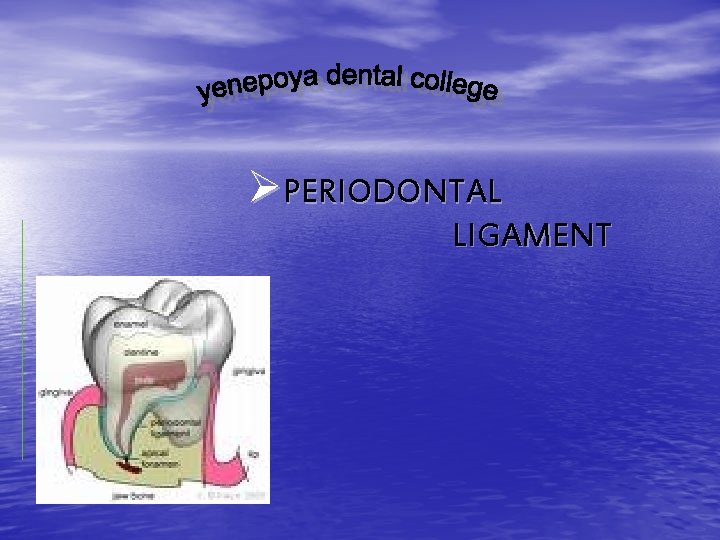
ØPERIODONTAL LIGAMENT
ØCONTENTS • INTRODUCTION • PERIODONTAL LIGAMENT • • • -definition -synonyms -development of periodontal ligament -structure -cells -principal fibers -blood supply -lymphatics -nerve supply -cementicles -functions of periodontal ligament CLINICAL CONSIDERATION CONCLUSION BIBILOGRAPHY
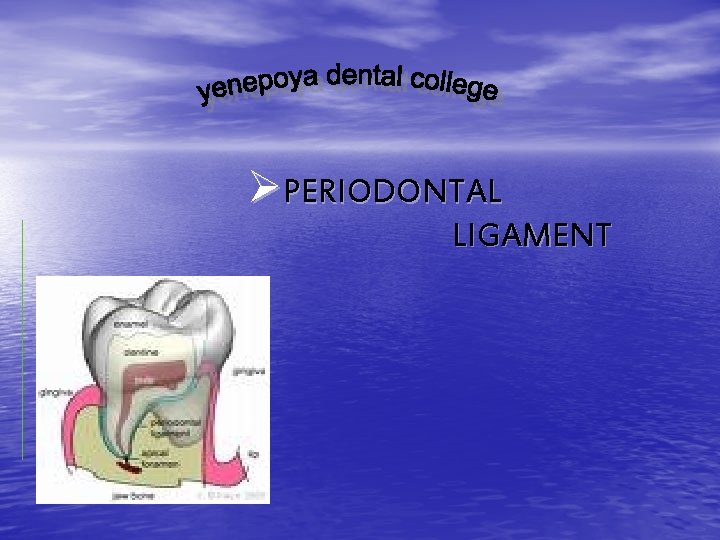
ØPERIODONTIUM • The tissues which invest and support the tooth are • • • collectively called as “PERIDONTIUM”. Periodontium is the functional unit of tissues supporting the tooth including gingiva, periodontal ligament, the cementum and the alveolar process. The tooth and periodontium together called as dento periodontal unit. The main support of the tooth is provided by periodontal ligament, which connects the cementum of the roots to the alveolar bone or tooth socket in to which root fits.
ØCOMPONENTS • MINERALISED TISSUES › Cementum › Alveolar bone • FIBROUS CONNECTIVE TISSUE › Periodontal ligament › Lamina propria
ØPERIODONTAL LIGAMENT The attachment apparatus of the tooth includes periodontal ligament, cementum and alveolar bone. v DEFINATIONPeriodontal ligament is an connective tissue organ covered by epithelium that attaches teeth to the bones of the jaws and provide continuous attachment and support to the teeth during function. it is continuous with the connective tissue of the gingiva that is lamina propria and communicates with the marrow spaces of the alveolar bone through volkmans’s canal.
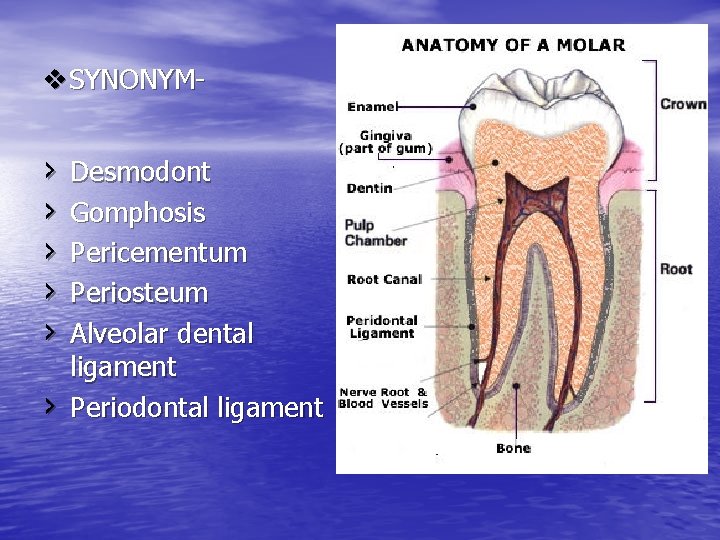
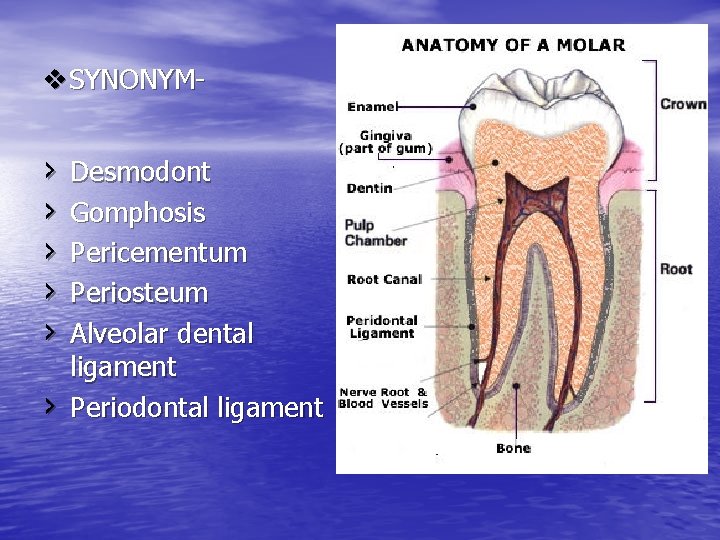
v. SYNONYM- › › › Desmodont Gomphosis Pericementum Periosteum Alveolar dental ligament Periodontal ligament
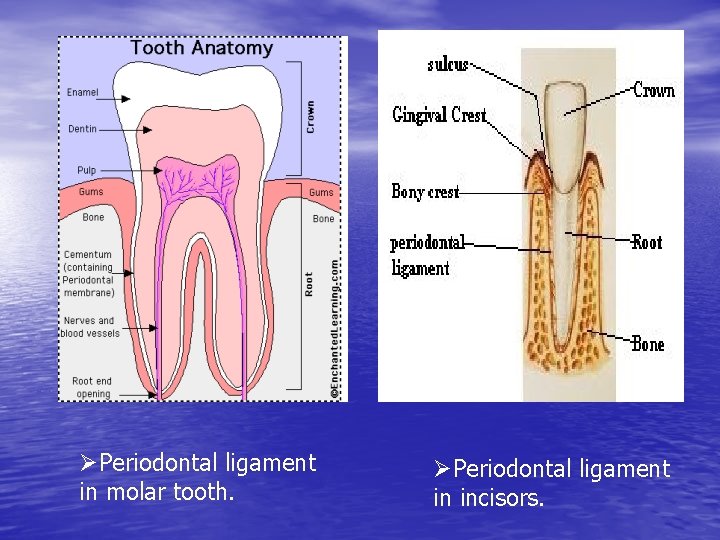
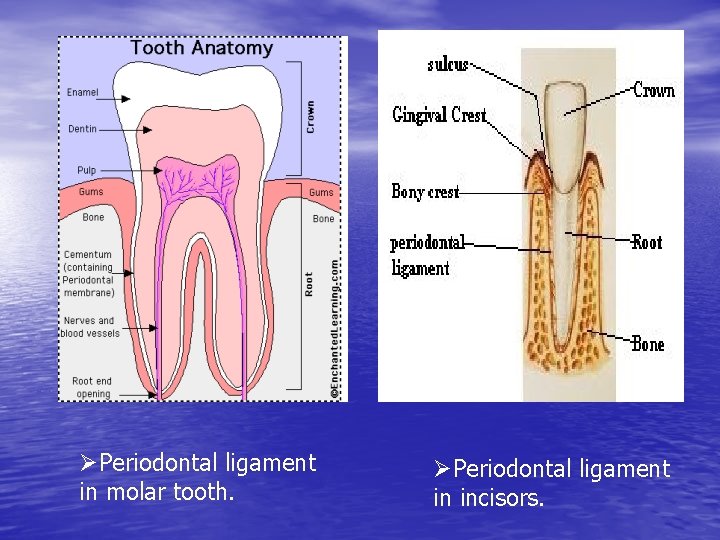
ØPeriodontal ligament in molar tooth. ØPeriodontal ligament in incisors.
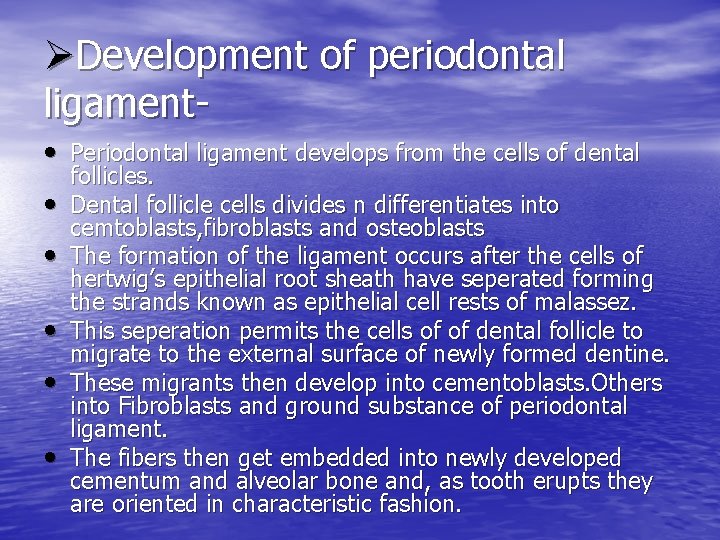
ØDevelopment of periodontal ligament • Periodontal ligament develops from the cells of dental • • • follicles. Dental follicle cells divides n differentiates into cemtoblasts, fibroblasts and osteoblasts The formation of the ligament occurs after the cells of hertwig’s epithelial root sheath have seperated forming the strands known as epithelial cell rests of malassez. This seperation permits the cells of of dental follicle to migrate to the external surface of newly formed dentine. These migrants then develop into cementoblasts. Others into Fibroblasts and ground substance of periodontal ligament. The fibers then get embedded into newly developed cementum and alveolar bone and, as tooth erupts they are oriented in characteristic fashion.
• During tooth eruption, the fibroblasts becomes active and start producing collagen fibrils. • The first collagen fibrils appear in the region immediately apical to gingivo dental fiber group. • The transseptal and alveolar crest fibers develop when the tooth merges in to oral cavity • Alveolar bone deposition occurs simultaneously with periodontal ligament organization.
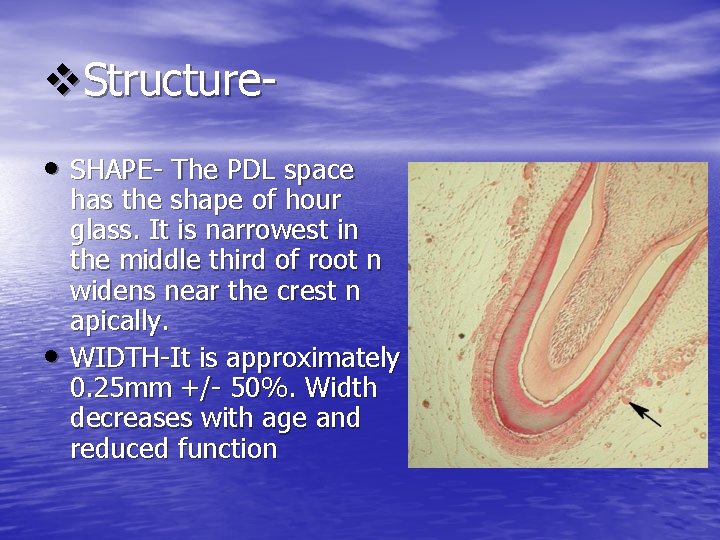
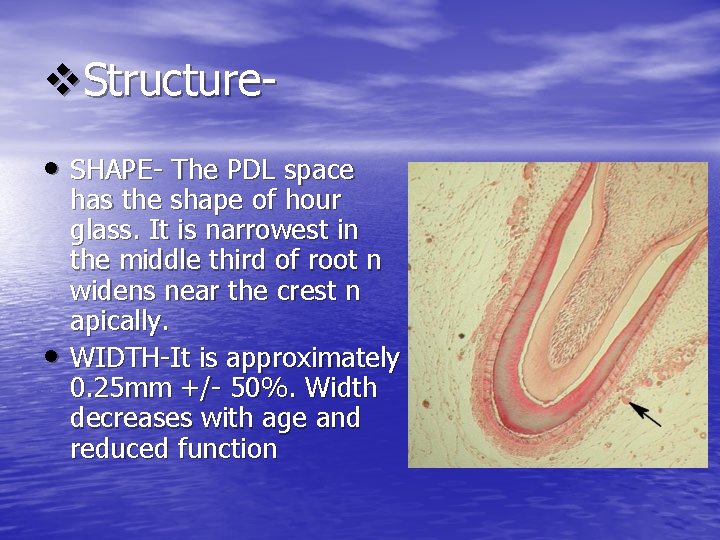
v. Structure • SHAPE- The PDL space • has the shape of hour glass. It is narrowest in the middle third of root n widens near the crest n apically. WIDTH-It is approximately 0. 25 mm +/- 50%. Width decreases with age and reduced function
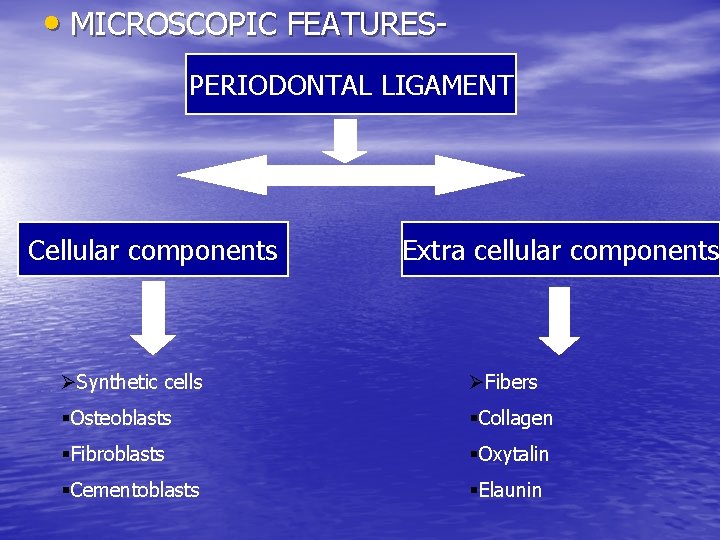
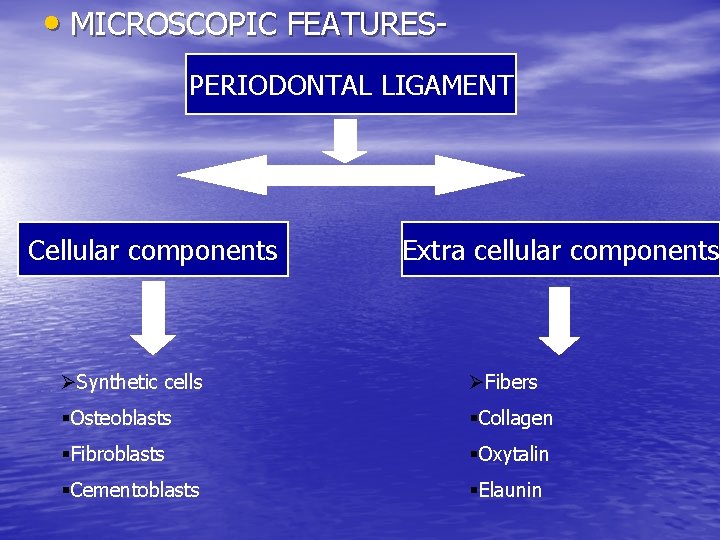
• MICROSCOPIC FEATURESPERIODONTAL LIGAMENT Cellular components Extra cellular components ØSynthetic cells ØFibers §Osteoblasts §Collagen §Fibroblasts §Oxytalin §Cementoblasts §Elaunin
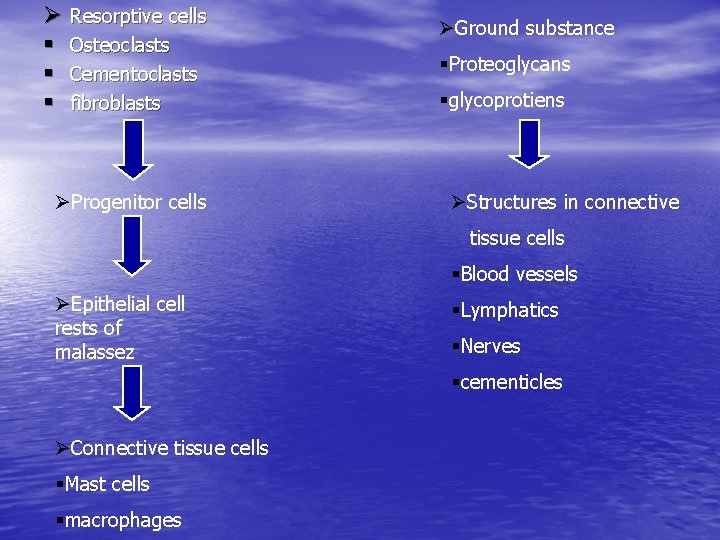
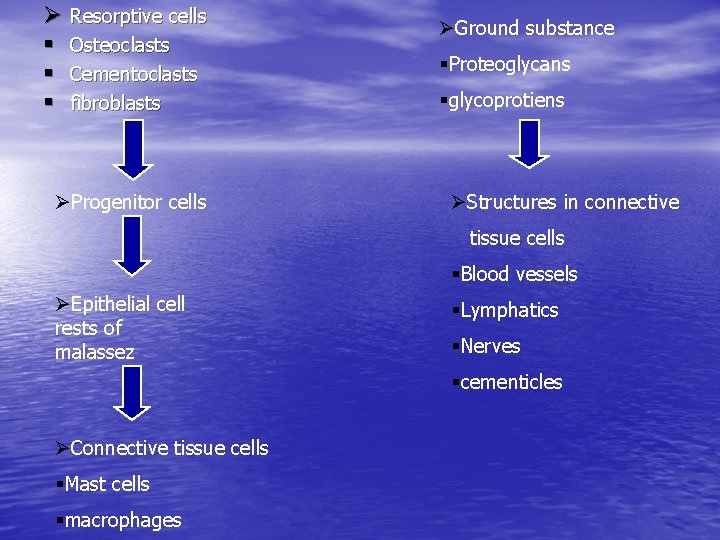
Ø Resorptive cells § Osteoclasts § Cementoclasts § fibroblasts ØProgenitor cells ØGround substance §Proteoglycans §glycoprotiens ØStructures in connective tissue cells §Blood vessels ØEpithelial cell rests of malassez §Lymphatics §Nerves §cementicles ØConnective tissue cells §Mast cells §macrophages
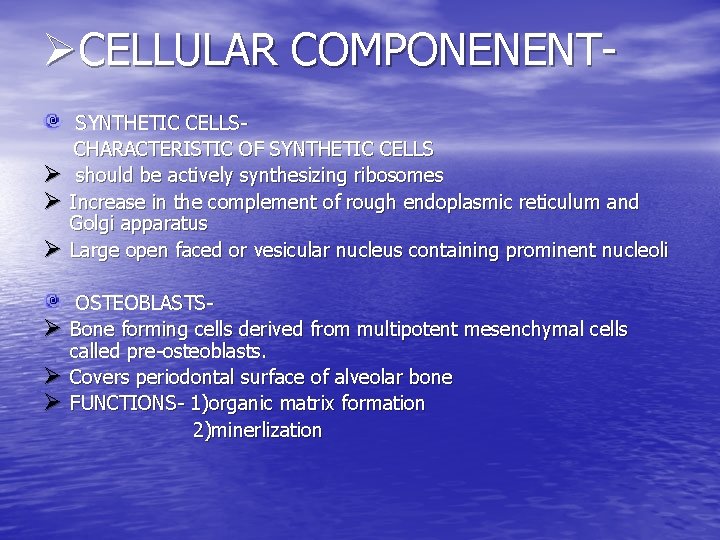
ØCELLULAR COMPONENENTØ Ø Ø SYNTHETIC CELLSCHARACTERISTIC OF SYNTHETIC CELLS should be actively synthesizing ribosomes Increase in the complement of rough endoplasmic reticulum and Golgi apparatus Large open faced or vesicular nucleus containing prominent nucleoli OSTEOBLASTSBone forming cells derived from multipotent mesenchymal cells called pre-osteoblasts. Covers periodontal surface of alveolar bone FUNCTIONS- 1)organic matrix formation 2)minerlization
Ø Ø Ø Ø FIBROBLASTSIt is the most prominent connective tissue cell. (65%). They are spindle shaped or ovoid cells with extensive cytoplasm containing abundant cellular organelles. They are oriented parallel to principal fibers. They consist of subtypes with distinct phenotypes and found to synthesize higher quantities of chondroitin sulfate and lesser quantities of heparin sulfate. These cells produce collagen fibers, reticulin fibers, oxytalin fibers and elastin fibers. FUNCTIONS-1)synthesis and degradation of collagen. CEMENTOBLASTSThey are cementum forming cells derived from undifferentiated ectomesenchymal cells of dental follicle and they resemble osteoblast. and distributed along cemental surface of PDL. FUNCTION-1) formation of cementoid
Ø Ø Ø Ø Ø RESORPTIVE CELLSOSTEOCLASTSThese are cells that resorbs bone. They are large and multinucleated. Approx 20 -100 micron in diameter. They have brush or ruffled border and found in Howship’s lacunae. FUNCTION-1)resorption of bone. CEMENTOCLASTSThey resemble osteoclasts. In this cementum is not remodeled in the fashion of alveolar bone and periodontal ligament, but that it undergoes continual deposition during life. Resorption of cementum occurs in certain circumstances and in this circumstances cementoclasts are located in Howship’s lacunae. FUNCTION-1)Resorption of cementum.
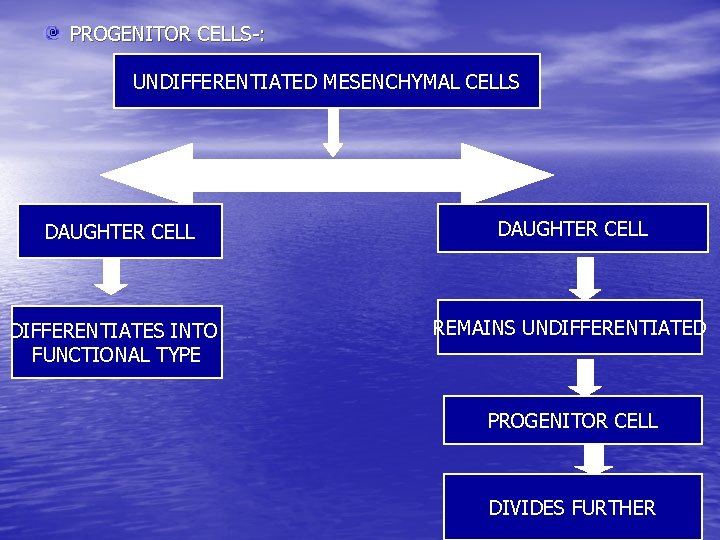
Ø Ø Ø FIBROBLASTSThe fibroblasts responsible for resorption contains fragments of collagen that appear to be undergoing digestion. The presence of these cells indicates resorption of fibers occurring during either disease or physiological turn over or remodeling of periodontal ligament. PROGENITOR CELLSAll connective tissue cells including periodontal ligament contain progenitor cells. The undifferentiated mesenchymal cells have the capability to undergo mitotic division. Progenitor cells have a small close faced nucleus and very little cytoplasm These are found in highest concentration close to the blood vessels
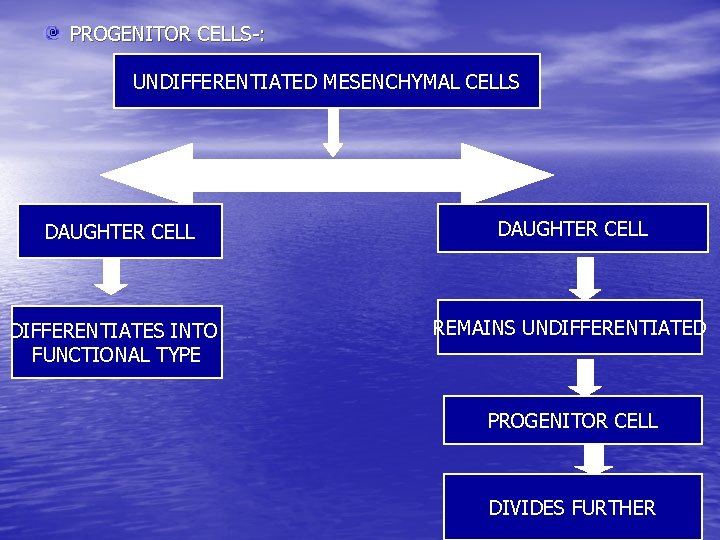
PROGENITOR CELLS-: UNDIFFERENTIATED MESENCHYMAL CELLS DAUGHTER CELL DIFFERENTIATES INTO FUNCTIONAL TYPE DAUGHTER CELL REMAINS UNDIFFERENTIATED PROGENITOR CELL DIVIDES FURTHER
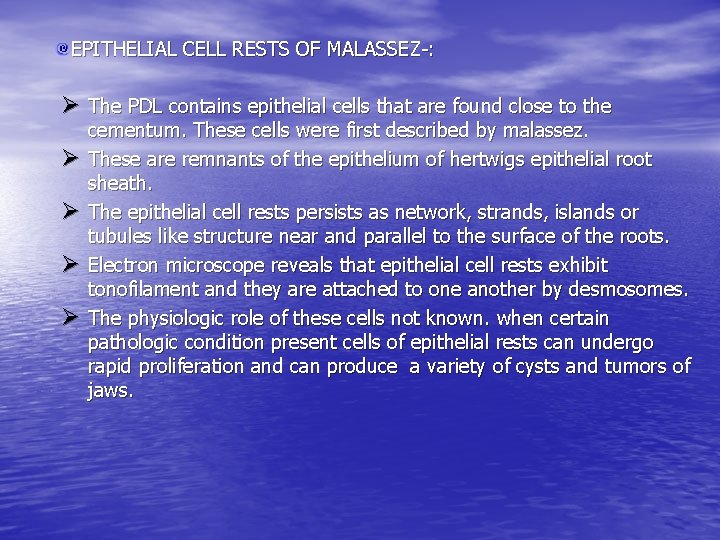
EPITHELIAL CELL RESTS OF MALASSEZ-: Ø The PDL contains epithelial cells that are found close to the Ø Ø cementum. These cells were first described by malassez. These are remnants of the epithelium of hertwigs epithelial root sheath. The epithelial cell rests persists as network, strands, islands or tubules like structure near and parallel to the surface of the roots. Electron microscope reveals that epithelial cell rests exhibit tonofilament and they are attached to one another by desmosomes. The physiologic role of these cells not known. when certain pathologic condition present cells of epithelial rests can undergo rapid proliferation and can produce a variety of cysts and tumors of jaws.
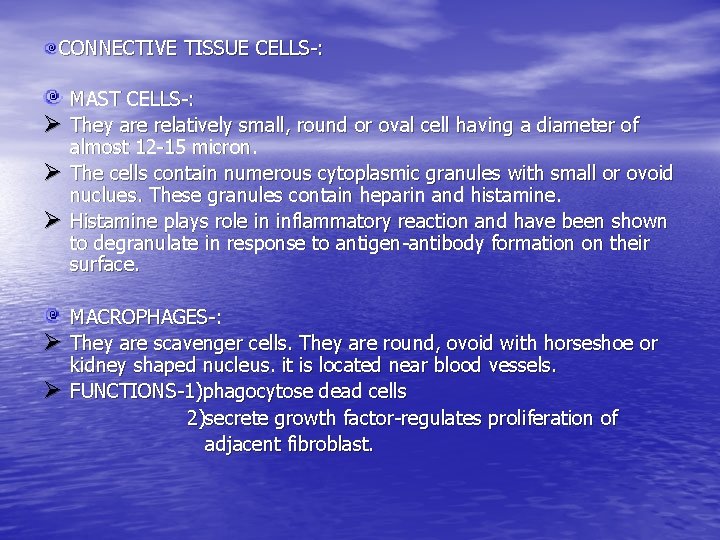
CONNECTIVE TISSUE CELLS-: Ø Ø Ø MAST CELLS-: They are relatively small, round or oval cell having a diameter of almost 12 -15 micron. The cells contain numerous cytoplasmic granules with small or ovoid nuclues. These granules contain heparin and histamine. Histamine plays role in inflammatory reaction and have been shown to degranulate in response to antigen-antibody formation on their surface. MACROPHAGES-: They are scavenger cells. They are round, ovoid with horseshoe or kidney shaped nucleus. it is located near blood vessels. FUNCTIONS-1)phagocytose dead cells 2)secrete growth factor-regulates proliferation of adjacent fibroblast.
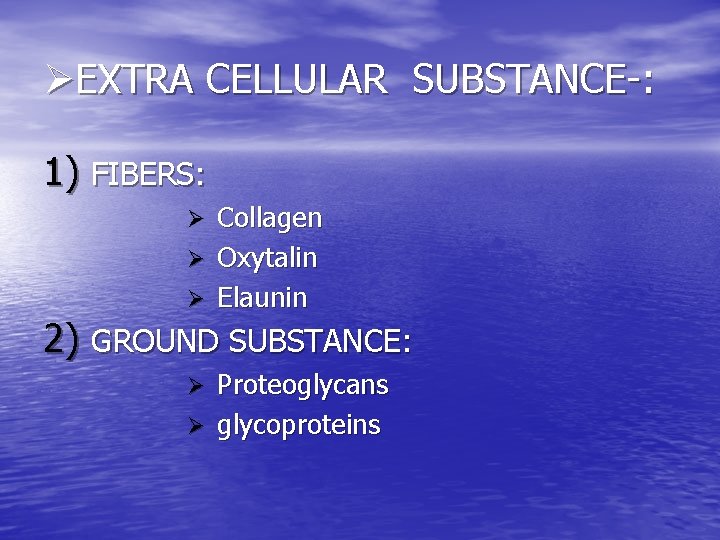
ØEXTRA CELLULAR SUBSTANCE-: 1) FIBERS: Collagen Ø Oxytalin Ø Elaunin Ø 2) GROUND SUBSTANCE: Proteoglycans Ø glycoproteins Ø

ØPERIODONTAL FIBERS-: • The most important elements of periodontal ligament are the principal fibers. PRINCIPAL FIBERS-: • Collagen fibers are gathered to be in bundles and organized into • • functional groups having clear orientation relative to periodontal space. These are termed as principal fibers. They run wavy course from cementum to bone and straighten out under load. The terminal portion of these fibers that insert into cementum and bone are termed as Sharpey’s fibers They are composed of type 1 collagen, where as reticular fibers are made up of type 3 and type 4 collagen as seen in basal lamina.
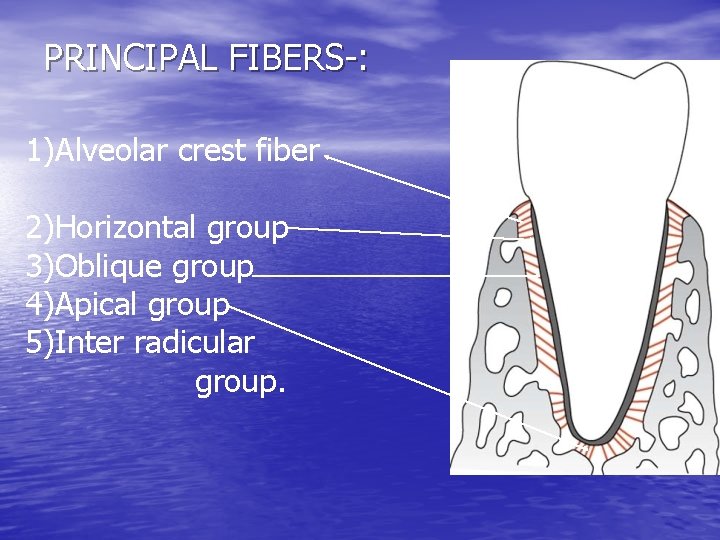
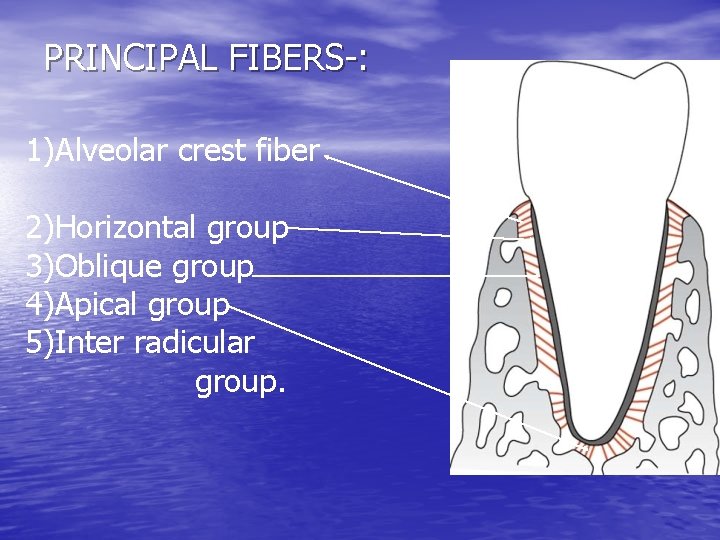
PRINCIPAL FIBERS-: 1)Alveolar crest fiber 2)Horizontal group 3)Oblique group 4)Apical group 5)Inter radicular group.
Ø ALVEOLAR CREST GROUP-: • They extend obliquely from cementum just beneath junctional • epithelium to alveolar crest. FUNCTION-: 1)prevents extrusion of teeth 2)resists lateral tooth movement. Ø HORIZONTAL GROUP-: • These fibers extend from cementum to alveolar crest at right angles • to long axis of the tooth. FUNCTION-: 1)Resists the tooth displacement against lateral pressure. Ø OBLIQUE GROUP-: • They are most numerous in PDL. • It extends coronally in oblique direction from cementum to the bone. • FUNCTIONS-: 1)Suspends tooth in socket 2)bear vertical occlusal forces 3)transform masticatory forces on alveolar bone.
Ø APICAL GROUP -: • These fibers radiate in irregular fashion from one cementum to the • • bone at the apical region of the socket. They do not occur on incompletely formed roots. FUNCTIONS-1)Prevents oral tipping of tooth 2)resists luxation 3)protects blood vessels, lymph and nerve supply to the tooth. Ø INTER RADICULAR GROUP-: • These fibers fan out from the cementum to the tooth in the • furcation area of the multirooted tooth. FUNCTIONS-1)It resists luxation, tipping and torquing.
ØDevelopment of principal fibers of periodontal ligament-: • • The principal fibers develop in conjunction with the eruption of the tooth. the fibroblasts surrounding the developing root produces collagen fibers these fibers are seen in periodontal space without any orientation. as and when tooth erupts the orientation of fibers alters. First small, fine brush like fibrils are seen arising from root cementum and projecting into periodontal ligament space. Similar fibers seen on surface of bone. Later number and thickness of fibers originating from the bone increases and elongates. they radiate towards connective tissue in mid portion of PDL space. Fibers originating from cementum also increase in length and thickness and fuse with fibers originating from bone.
• They mature progressively towards root apex as the eruption progresses. when tooth reaches occlusion and starts to function , these fibers become organized in to bundles and run continuously from bone to cementum. Ø SECONDARY FIBERS OF PERIODONTAL LIGAMENT-: • OXYTALIN AND ELUANIN-: • Ø Well formed fiber bundles that interdigitate at right angles around and in between the regular fiber bundles. these fibers are immature elastic fibers. they run in axial direction, one end embedded in the cementum or bone, and the other in wall of blood vessels. FUNCTION-: 1)Supports the blood vessel of PDL. GROUND SUBSTANCE-: The space between cells, fibers, blood vessels and nerves in PDL space is occupied by ground substance. it is made up of glycosaminoglycans(hyaluronic acid and proteoglycans), glycoproteins (fibronectin and laminin). it also has high water content(70%).
ØACCESORRY FIBERS-: Ø TRANS SEPTAL FIBRES-: These fibers extend interproximally over the alveolar bone crest and are embedded into cementum of adjacent teeth. these fibers are considered to belong to gingiva because they do not have osseous attachment. Ø INTERMEDIATE PLEXUS-: • • Light microscopic examination of longitudinal section of PDL gives an appearance , as though fibers arising from bone n cementum are joined in mid-region of periodontal space giving rise to a zone of distinct appearance. this is “INTERMEDIATE PLEXUS” This provides a site where rapid remodeling of fibers occur allowing adjustment in PDL to accommodate small tooth movement. It is just an artifact arising out of plane of sectioning.
ØSTRUCTURES PRESENT IN CONNECTIVE TISSUE-: 1) BLOOD VESSELS-: • Periodontal ligament is supplied by branches derived from three sources-dental, interradicular and interdental arteries. DENTAL ARTERY- before it enters apical foramen it gives of branches to the periodontal ligament which also supplies pulp. • INTERDENTAL ARTERY-emerges from crest of alveolar bone n supplies coronal part of PDL. • INTERRADICULAR ARTERY –It gives off branches in the alveolar process that supplies the coronal part of PDL.
2) 3) LYMPHATICS-: A network of lymphatic vessels following path of blood vessels provide the lymph drainage of the PDL. the flow is from ligament towards and into the adjacent alveolar bone. NERVE SUPPLY-: Long diameter fibers Myelinated fibers nerve fibers Myelinated fibers Small diameter fibers unmyelinated fibers periodontal ligament mainly supplied by dental branches of alveolar nerve through apical perforation of tooth socket. Ø • NERVE ENDINGS-: FREE ENDINGS-: ramify in tree like fashion originates mainly from unmyelinated fibers located at regular intervals along length of root.
• RUFFNI ENDINGS-: It appears dendritic. simple and compound found around root • • apex. COILED ENDINGS-: Found in mid region of periodontal ligament. SPINDLE SHAPED ENDINGS-: found at root apex Ø CEMENTICLES-: • • • These are small foci of calcified tissue which is free in the PDL. they represent areas of dystrophic calcification, commonly seen in older individuals. SIZE: 0. 2 -0. 3 mm in diameter. TYPES: 1) free 2) attached 3)embedded ORIGIN: 1)Calcification of degenerated epithelial cells 2)calcification of Sharpey’s fibers 3)calcification of thrombosed blood vessels 4)cemental tears.
ØFUNCTIONS-: 1) 2) 3) 4) 5) 6) Physical/ supportive function Formative and remodeling Nutritional and sensory function Co-ordinates chewing Prevents bacteria Protects nerves and blood vessels
1) PHYSICAL/SUPPORTIVE FUNCTION-: The physical functions area. Provides soft tissue casing to protect vessels n nerves from injury. b. Transmits occlusal forces to bone. c. Attaches teeth to the bone. d. Maintains gingival tissue in relationship to the teeth. e. Resistance to the impact of occlusal forces (shock absorption) Three theories explained for mechanism of tooth support are: a. Tensional theory b. Viscoelastic theory c. Thixotropic theory Ø TENSIONAL THEORY-: force Straightening of PDL fibers Forces passed to alveolar bone Elastic deformation Forces passed to basal bone
Ø VISCOELASTIC THEORY-: It considers the displacement of the tooth to be largely controlled by fluid movements, with fibers having only a secondary role. when forces are transmitted to the tooth, the extra cellular fluid is pushed from PDL into marrow spaces through cribriform plate. after the depletion of the fluids the bundle fibers absorb the shock and tighten. this leads to blood vessel stenosis arterial back pressure ballooning of vessels tissue replenishes with fluids. Ø THIXOTROPIC THEORY-: According to this theory periodontal ligament has a rheologic behaviour of a thixotropic gel
2) • • FORMATIVE AND REMODELLING FUNCTION-: Cells of PDL participate in the formation and resorption of cementum and bone , which occurs in physiologic tooth movement in the accommodation of the periodontium to occlusal forces, and in repair of injuries. The periodontal ligament is constantly undergoing remodeling, old cells and fibers are broken down and replaced by new ones. 3) NUTRITIONAL AND SENSORY FUNCTION-: • since PDL has rich vascular supply it provides nutrition to the • • cementum, bone and gingiva. PDL is supplied by nerve fibers that can transmit sensation of touch, pressure and pain to higher centers. The nerve bundles follows the course of blood vessels and enters PDL from periapical area through channels from alveolar bone.
ØCLINICAL CONSIDERATION-: • The primary role of PDL is to support the tooth in the bony socket. • Its thickness varies in individuals and in different teeth in same • • • person. PDL is hour glass shape with narrowest in the middle region of the root and thus seems to be the fulcrum of physiological movement. The thickness of the PDL seems to be maintained by functional movements of tooth. It is thin in functionless and embedded teeth and wide in teeth that are under excessive occlusal stress.
Ø RESTORATIVE DENTISTRY AND PROSTHETIC DENTISTRY-: For practice of restorative dentistry the importance of changes in the PDL is obvious. The supporting tissues of the tooth long out of function are poorly adapted to carry load suddenly placed on the tooth by a restoration. this applies to teeth opposing bridges or dentures and teeth used as anchorage for removable bridges. This accounts for inability of patient to use restoration immediately after placement. Ø ORTHODONTIC TOOTH MOVEMENT-: Depends on formation and resorption of bone and PDL. if movement of tooth is within physiologic limits, the compression of PDL on pressure side results in bone resorption, where as tension side bone deposition. large force application results in necrosis of PDL.
Ø PERIAPICAL INFLAMMATION-: The PDL in the periapical region is the most common site of a pathological lesion. inflammatory diseases of pulp progresses to the apical periodontal ligament and replaces its fiber bundles with granulation tissue. this lesion is called as “dental granuloma”. it may further lead to cyst. Ø GINGIVAL INFLAMMATION-: In periodontitis if gingivitis is not treated it will extend to PDL and bone and produces the destruction of the same. once they are destroyed it is difficult to regenerate and therefore disease of PDL is Irreversible.
ØCONCLUSION • • • Safe gaurding the integrity of the periodontal ligament is one of the most important challenges for the clinician. gingivitis or inflammation of gingiva, is the most common dental disease of human if not controlled or treated, periodontitis may develop and destruction may extend into periodontal ligament and bone. once destroyed by periodontitis, the periodontal ligament and alveolar bone is very difficult to regenerate.

Thank you
 Periodontal space
Periodontal space Transseptal fiber
Transseptal fiber Periodontal ligament injection definition
Periodontal ligament injection definition Periodontal ligament lifleri
Periodontal ligament lifleri Aa palatinae minores
Aa palatinae minores Notching of the crestal lamina dura
Notching of the crestal lamina dura Contents introduction
Contents introduction Corrective phase
Corrective phase Classification of periodontal instruments
Classification of periodontal instruments Perimylolysis
Perimylolysis Modifiye stillman
Modifiye stillman Periodontal case study
Periodontal case study Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Plaque index scoring criteria
Plaque index scoring criteria Fases de la enfermedad periodontal
Fases de la enfermedad periodontal Indikasi gingivektomi
Indikasi gingivektomi Rationale of periodontal therapy
Rationale of periodontal therapy Deskuame
Deskuame Periodonto de insercion
Periodonto de insercion Glickman's concept
Glickman's concept Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Anug tedavisi
Anug tedavisi Lima apical maestra
Lima apical maestra Prevalencia
Prevalencia Diagnosis of periodontal disease
Diagnosis of periodontal disease Lateral periodontal cyst
Lateral periodontal cyst Periapical cemento-osseous dysplasia
Periapical cemento-osseous dysplasia Periodontal abscess
Periodontal abscess Periodontal disease
Periodontal disease Kista ort
Kista ort Periodontal charting symbols
Periodontal charting symbols Gtr indications
Gtr indications Principles of periodontal surgery
Principles of periodontal surgery Como se divide el periodonto
Como se divide el periodonto Undisplaced flap
Undisplaced flap Seccin 7
Seccin 7 Periodontal radyoloji
Periodontal radyoloji Murat alikan
Murat alikan Periodontal case study
Periodontal case study Sahithya reddy periodontics
Sahithya reddy periodontics