Radiographic Diagnosis Of Periodontal Disease l Why Imaging















- Slides: 65
Radiographic Diagnosis Of Periodontal Disease
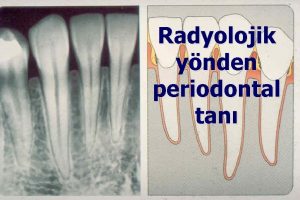
l Why Imaging? It is widely accepted that the management of a patient with destructive periodontal diseases necessitates a thorough clinical and radiographic examination to assess fully the presenting condition and to plan and execute appropriate treatment. l Much of the information required to make a diagnosis and generate a treatment plan will already be available to the clinician by the end of the clinical examination. l Some features relevant to the periodontal diseases may be detectable both by clinical and radiographic means.
l Bone levels can be assessed by radiographs, by sounding under local analgesia or by direct visualisation during surgery. l Periapical pathology, including combined lesions of both endodontic and periodontal origin, may be suspected clinically but can only be visualised radiographically on appropriate radiographs. l Needless to say, the most commonly employed method of bone level assessment that cannot be gained through routine clinical examination in use is the conventional radiograph, which requires the least intervention.
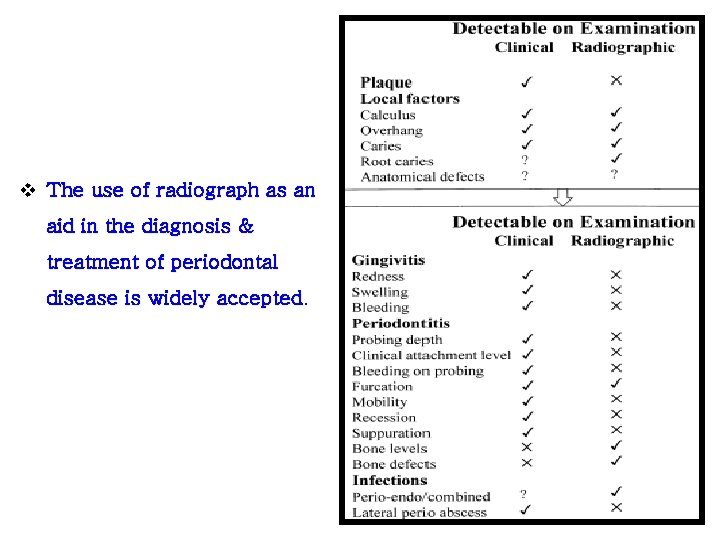
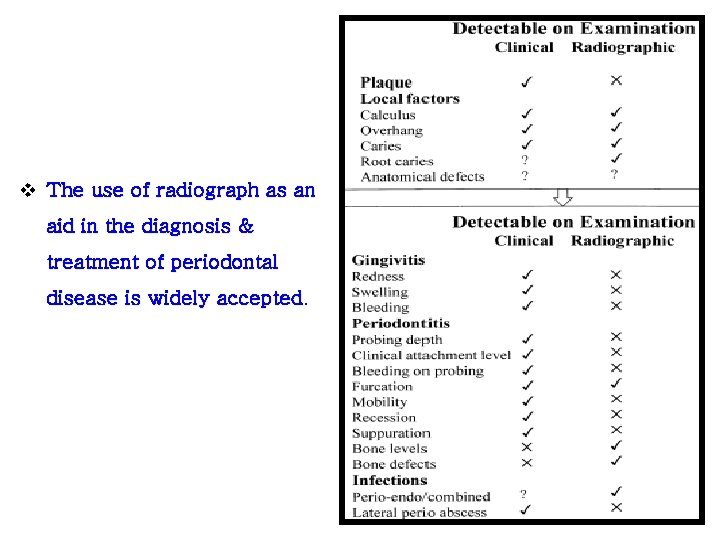
v The use of radiograph as an aid in the diagnosis & treatment of periodontal disease is widely accepted.
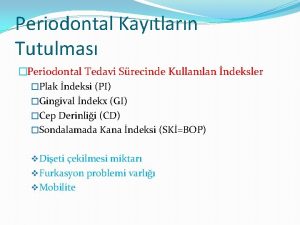
v Both Clinical and Radiographic examinations when combined are complementary. v Radiographs aid in the § diagnosis of periodontal disease, § determination of the prognosis, and § evaluation of the outcome of treatment.
What type of Imaging? l Intra Oral & Extra oral Imaging methods are available. l Commonly used methods include Ø Bite wing Ø Peri-apical & Ø Panoramic radiography
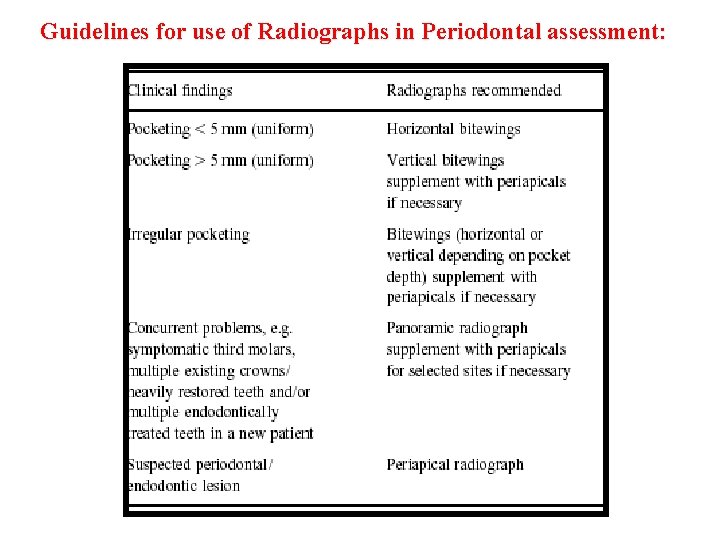
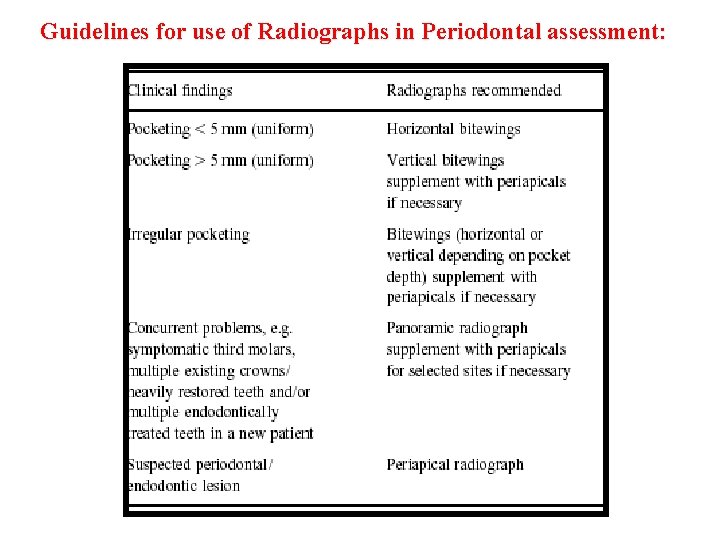
Guidelines for use of Radiographs in Periodontal assessment:
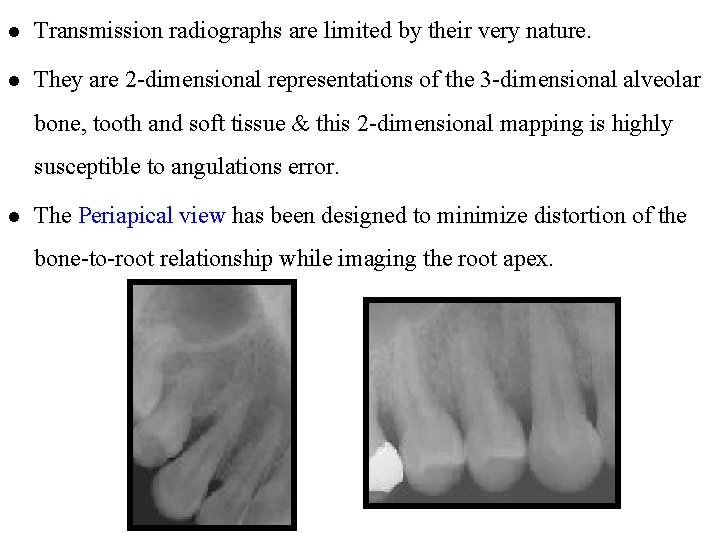
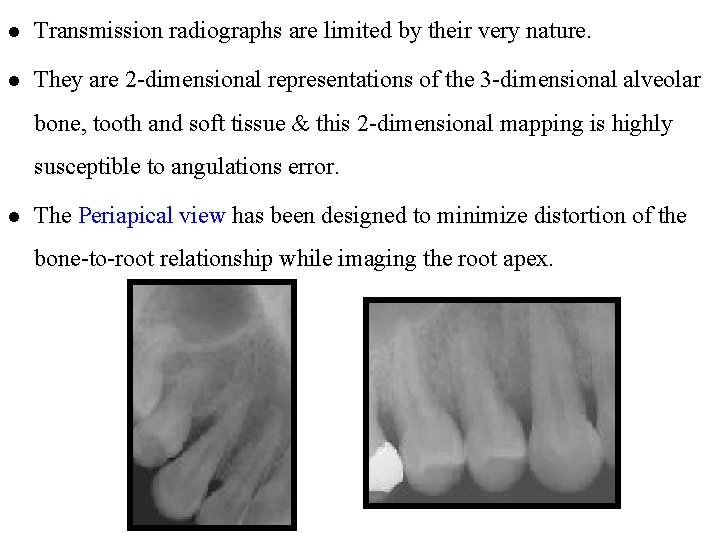
l Transmission radiographs are limited by their very nature. l They are 2 -dimensional representations of the 3 -dimensional alveolar bone, tooth and soft tissue & this 2 -dimensional mapping is highly susceptible to angulations error. l The Periapical view has been designed to minimize distortion of the bone-to-root relationship while imaging the root apex.
l The bitewing is often the forgotten radiograph in periodontal diagnosis. l A disadvantage of the conventional bitewing film is that a limited view of the osseous crest is available, so even moderate bone loss due to periodontitis may preclude its usefulness as a diagnostic image. l Vertical bitewing films can be used to assess bone height in patients with moderate to severe bone loss.

LIMITATIONS OF RADIOGRAPHS : They have three broad limitations : 1. Radiographs provide a two-dimensional view of a three dimensional situation. l The radiographic image is a superimposition of the bone and tooth structures over each other because the image lacks the third dimension of depth. l Because of this, bony defects overlapped by higher bony walls may be hidden. l Also, because of overlapping, only the interproximal bone is seen clearly.
2. Radiographs typically show less severe bone destruction than is actually present. 3. Radiographs do not demonstrate the soft-tissue-to hard tissue relationships and thus provide no information about the depth of soft tissue pockets.
• Remember that radiographs are only two-dimensional and as a general rule, bone loss is always greater than it appears in the radiograph.
The following four criteria to determine adequate angulation of periapical radiographs were established by Prichard l The radiograph should show the tips of molar cusps with little or none of the occlusal surface showing. l Enamel caps and pulp chambers should be distinct. l Interproximal spaces should be open. l Proximal contacts should not overlap unless teeth are out of line anatomically.
Normal Anatomy : l A thin layer of opaque cortical bone often covers the alveolar crest and the height of the crest lies at a level approximately 1 to 1. 5 mm below the level of the cementoenamel junctions (CEJs) of adjacent teeth. l Between posterior teeth the alveolar crest also is parallel to a line connecting adjacent CEJs. l Between anterior teeth the alveolar crest usually is pointed and has a dense cortex.
• As between the posterior teeth, the alveolar crest between anterior teeth lies within 1 to 1. 5 mm of a line connecting the adjacent CEJs. • The alveolar crest is continuous with the lamina dura of adjacent teeth, this appears radiographically as a continuous white line. • Radiographic evaluation of bone changes in periodontal disease is based mainly on the appearance of the interdental septa, because the relatively dense root structure obscures the facial and lingual bony plates.

RADIOGRAPHIC ASSESSMENT OF PERIODONTAL CONDITIONS : Radiographs are especially helpful in the evaluation of : l Amount of bone present, l Condition of the alveolar crests, l Bone loss in the furcation areas, l Width of the periodontal ligament space, l Local initiating factors that cause or intensify periodontal disease l Calculus, l Poorly contoured or overextended restorations, l Root length and morphology and the crown-to-root ratio,
l Anatomic considerations l Position of the maxillary sinus in relation to a periodontal deformity, l Missing, supernumerary, or impacted teeth. l Pathologic considerations l l Caries l Peripheral lesions Root resorptions
Calculus : l Radiographs may be useful in detecting subgingival calculus. l The ability to detect calculus radiographically will depend on its degree of mineralization and on angulation factors of the Xray beam. l The radiograph shows heavy calculus deposits and calculus spurs or spicules interproximally and sometimes even on the facial and lingual Surfaces. l However, it cannot be relied on for the thorough detection of calculus.

Presence or Absence of Periodontal Pockets : l Because the periodontal pocket is a pathologically deepened gingival sulcus, the only reliable method of locating periodontal pockets and evaluating their extent is by careful probing of the gingival margin along each tooth surface. l The periodontal pocket is composed of soft tissue, so it will not show up on the radiograph. l However, if a radio opaque material such as gutta percha, rootcanal points or Hirschfeld calibrated points is inserted into the pocket, the base of the pocket can be recorded in most instances on the radiograph.

Radiographs and Clinical probing: l Regenerative and reparative flap designs and incisions require prior knowledge of the underlying osseous topography. l Careful probing of these pocket areas after scaling and root planing often require local anesthesia and definitive radiographic evaluation of the osseous lesions. l Radiographs taken with periodontal probes or other indicators places into the anaesthetized pocket show the true extent of the bone lesion. l The use of radiopaque indicators is an efficient diagnostic aid for the clinician to better visualize every aspect of the defect.

Bone destruction in periodontal disease: l Early and associates (1979) estimated that, for interpretation of radiographs, a 30 -50% change in bone mineral is needed before the dentist is reasonably certain that bone loss has occurred. § The radiographic image tends to show less severe bone loss than that actually present. § The difference between the alveolar crest height and the radiographic appearance ranges from 0 to 1. 6 mm, mostly accounted for by x-ray angulation.
Early bone loss in periodontal disease : • In a study by Pauls and Trott (1966), interseptal bony defects smaller than 3 mm could not be seen on radiographs. • The sensitivity of radiographs in measuring early bone destruction in periodontal disease is only fair. • In their studies, Ramadan and Mitchell (1962) reported that when periodontal bone destruction first is seen on the radiograph, it usually has progressed beyond its earliest stage.
• Therefore, the very earliest signs of periodontal disease must be detected clinically. • Also, the status of bone on facial and lingual aspects of the teeth is difficult to evaluate because the dense tooth structures are superimposed over the bone. Early Furcation involvement : • Furcation involvement is detected by clinical examination, which includes careful probing with specialized probes. • Radiographs are helpful, but they usually show less bone loss than actually present.
Pattern of bone destruction : • In periodontal disease, the interdental septa undergo changes that affect the lamina dura, crestal radiodensity, size and shape of the medullary spaces, and height and contour of the bone. • The interdental septa may be reduced in height, with the crest horizontal and perpendicular to the long axis of the adjacent teeth or they may have angular or arcuate defects.
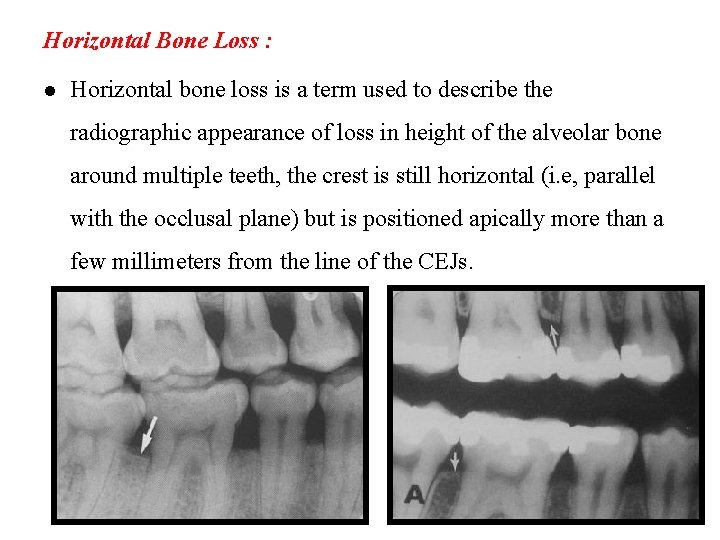
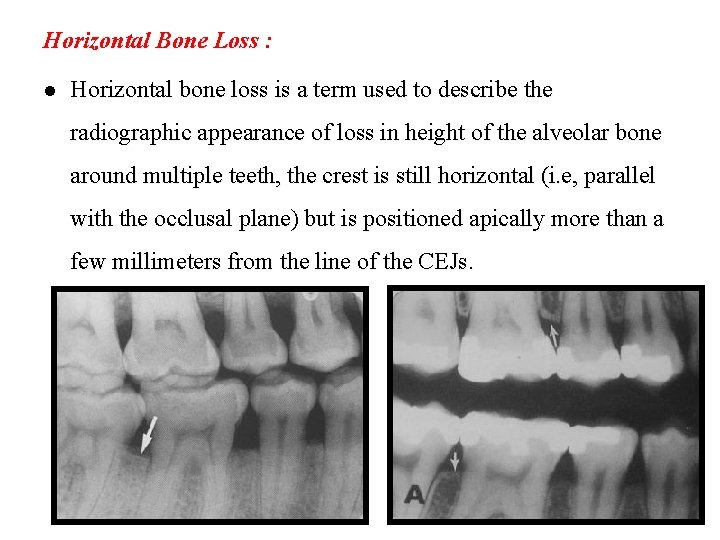
Horizontal Bone Loss : l Horizontal bone loss is a term used to describe the radiographic appearance of loss in height of the alveolar bone around multiple teeth, the crest is still horizontal (i. e, parallel with the occlusal plane) but is positioned apically more than a few millimeters from the line of the CEJs.

Vertical Osseous Defects : • In these defects the occlusal border of the remaining alveolar bone typically displays an oblique angulation to the line of the CEJs in the area of involved teeth. • Often infrabony defects are difficult to recognize on a radiograph because one or both of the cortical bony plates remain superimposed with the defect. • Clinical and surgical inspections are the best means of determining the number of remaining bony walls. • Visualization of the depth of pockets may be aided by inserting a gutta-percha point.

Radiographic changes in periodontitis : • Although the radiograph is not sensitive enough to detect the earliest signs of periodontal disease, it is still an essential part of the clinical examination. • Glickman (1972) listed the following sequence of early radiographic changes that occur in periodontitis. • Crestal irregularities. • Triangulation. • Interdental septal bone changes.
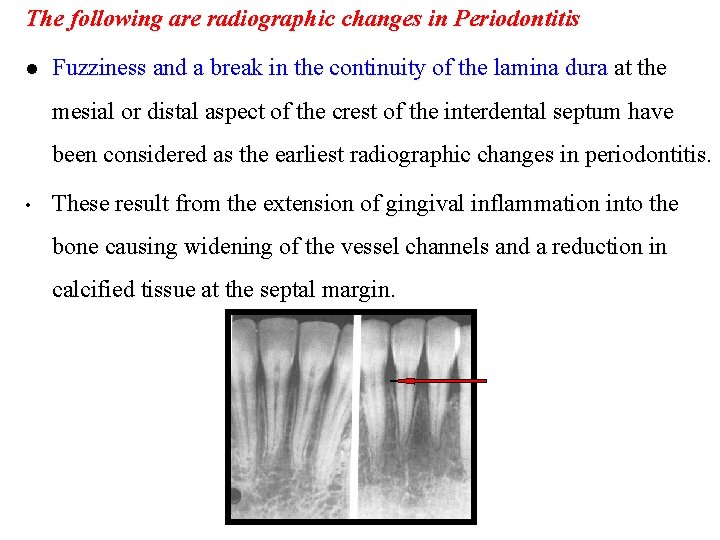
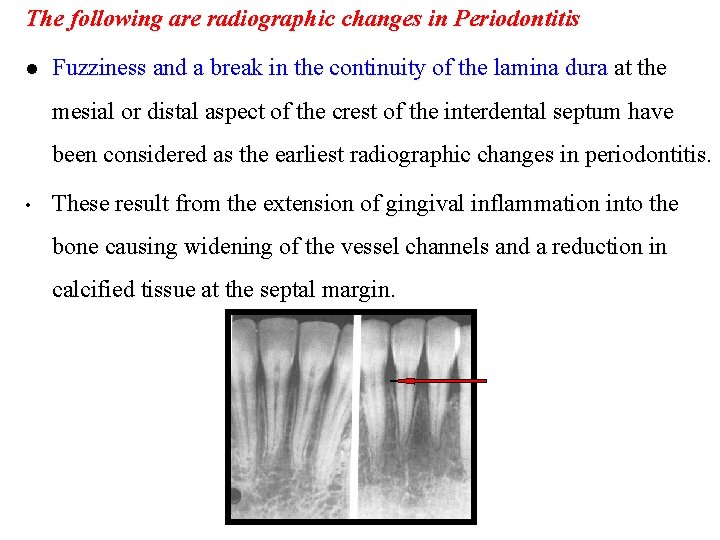
The following are radiographic changes in Periodontitis l Fuzziness and a break in the continuity of the lamina dura at the mesial or distal aspect of the crest of the interdental septum have been considered as the earliest radiographic changes in periodontitis. • These result from the extension of gingival inflammation into the bone causing widening of the vessel channels and a reduction in calcified tissue at the septal margin.
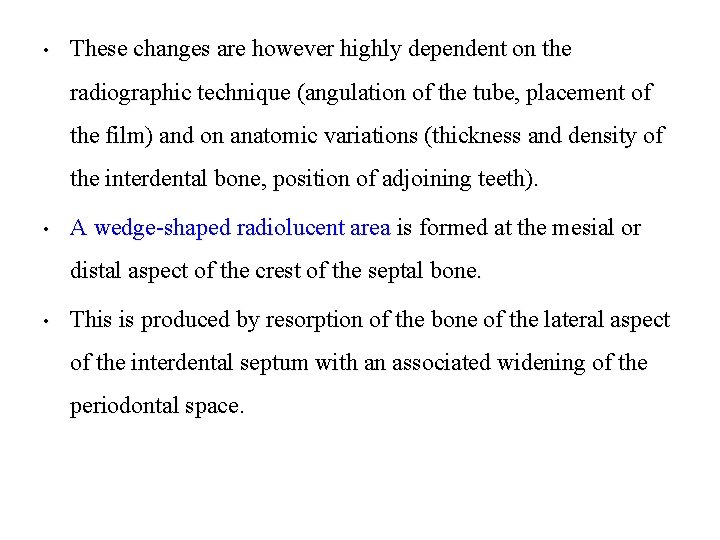
• These changes are however highly dependent on the radiographic technique (angulation of the tube, placement of the film) and on anatomic variations (thickness and density of the interdental bone, position of adjoining teeth). • A wedge-shaped radiolucent area is formed at the mesial or distal aspect of the crest of the septal bone. • This is produced by resorption of the bone of the lateral aspect of the interdental septum with an associated widening of the periodontal space.
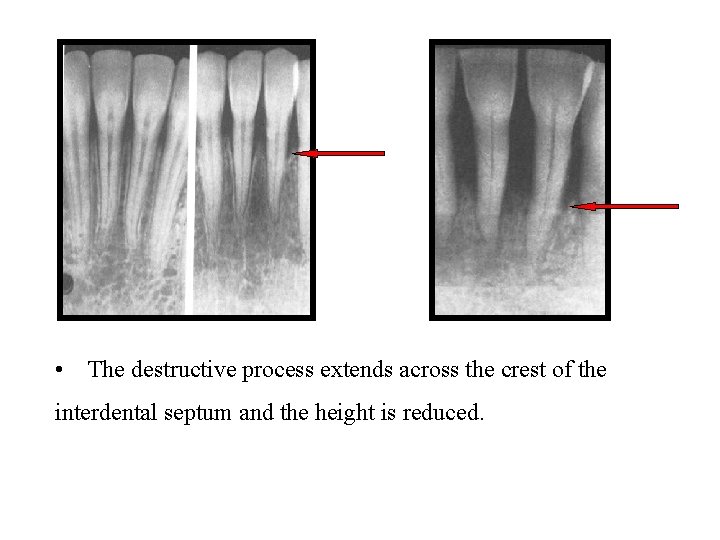
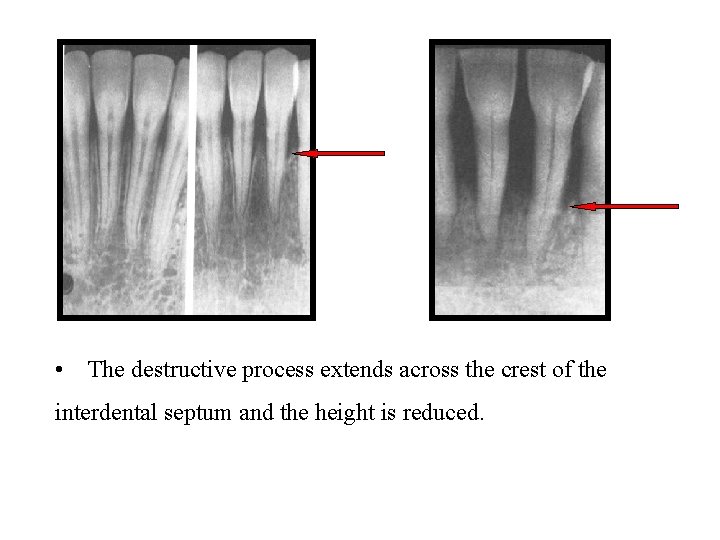
• The destructive process extends across the crest of the interdental septum and the height is reduced.
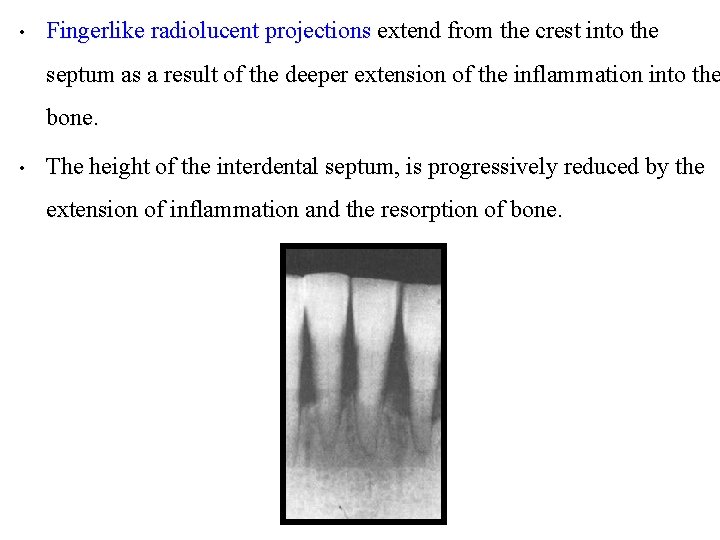
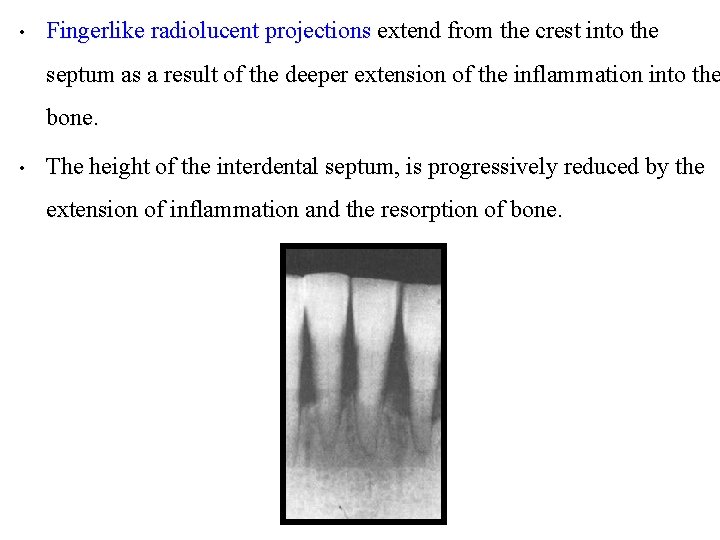
• Fingerlike radiolucent projections extend from the crest into the septum as a result of the deeper extension of the inflammation into the bone. • The height of the interdental septum, is progressively reduced by the extension of inflammation and the resorption of bone.
Radiographic appearance of furcation involvements : • Definitive diagnosis of furcation involvement is made by clinical examination, which includes careful probing with specially designed probe (Nabers probe). • Radiographs are helpful but show artifacts that make it possible for furcation involvement to be present. • A tooth may present marked bifurcation involvement in one film but appear to be uninvolved in another. • Radiographs should be taken at different angles to reduce the risk of missing furcation involvement.
The following diagnostic criteria are suggested: • The slightest radiographic change in the furcation area should be investigated clinically, especially if there is bone loss on adjacent roots. • Diminished radiodensity in the furcation area in which outlines of bony trabeculae are visible suggests furcation involvement. • Whenever there is marked bone loss in relation to a single molar root, it may be assumed that the furcation is also involved.


Dental conditions associated with periodontal diseases : l Various changes in the dentition and its supporting structures that frequently are associated with periodontal disease include l overhanging and faulty restorations, l occlusal trauma, l tooth mobility, l open contacts. l These conditions usually are apparent on radiographs.
Occlusal trauma : l Traumatic occlusion causes degenerative changes in response to occlusal pressures that are greater than the physiologic tolerances of the tooth’s supporting tissues. • Radiographic evidence may suggest increased tooth mobility, including widening of the periodontal ligament (PDL) space, thickening of the lamina dura, bone loss, and an increase in the number and size of trabeculae. • Other sequelae of traumatic occlusion include hypercementosis and root fractures. • However, traumatic occlusion can be diagnosed only by clinical evaluation.

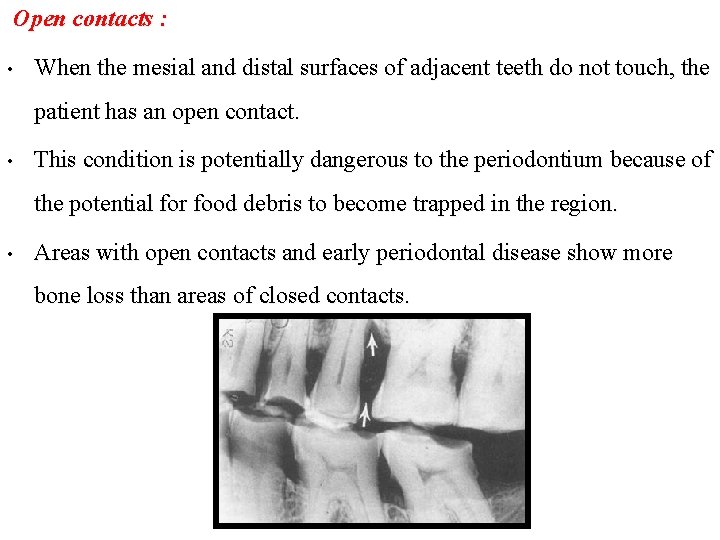
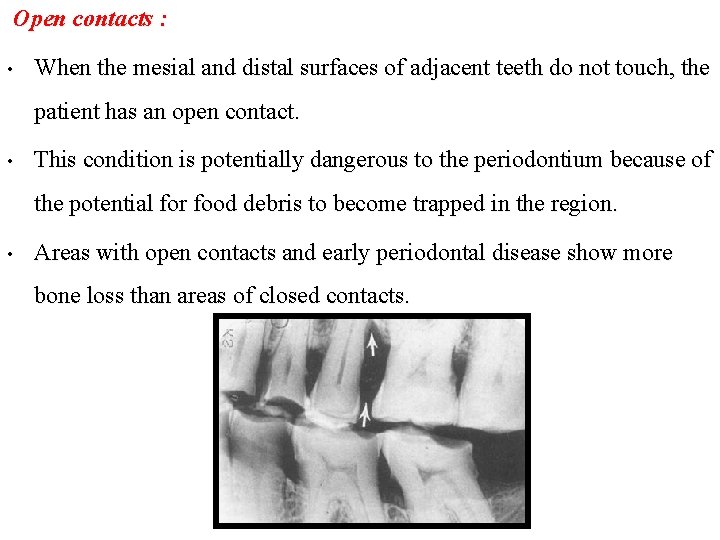
Open contacts : • When the mesial and distal surfaces of adjacent teeth do not touch, the patient has an open contact. • This condition is potentially dangerous to the periodontium because of the potential for food debris to become trapped in the region. • Areas with open contacts and early periodontal disease show more bone loss than areas of closed contacts.
Local irritating factors : • Local irritating factors may cause or aggravate periodontal defects. • Calculus deposits prevent effective cleansing of a sulcus and lead to the progression of periodontal disease. • Similarly, defective restorations with overhanging or poorly contoured margins can lead to the accumulation of bacterial deposits and periodontal disease.

Radiographic Appearance of the Periodontal Abscess: • The typical radiographic appearance of the periodontal abscess is that of a discrete area of radiolucency along the lateral aspect of the root because of many variables such as the following: The stage of the lesion: • In the early stages the acute periodontal abscess is extremely painful but presents no radiographic changes.
The Location of the abscess: • Lesions in the soft tissue wall of a periodontal pocket are less likely to produce radiographic changes than those deep in the supporting tissues. • Abscesses on the interproximal areas are more likely to be visualized radiographically. • Thus the radiograph alone cannot be relied on for the diagnosis of a periodontal abscess.

Radiographic Changes in Localized Aggressive Periodontitis: • Aggressive periodontitis is characterized by a combinations of the following radiographic features: • Bone loss may occur initially in the maxillary and mandible incisor and/or first molar areas, usually bilaterally, and results in vertical, arc like destructive patterns. • Loss of alveolar bone may become generalized as the disease progresses but remains less pronounced in the premolar areas.

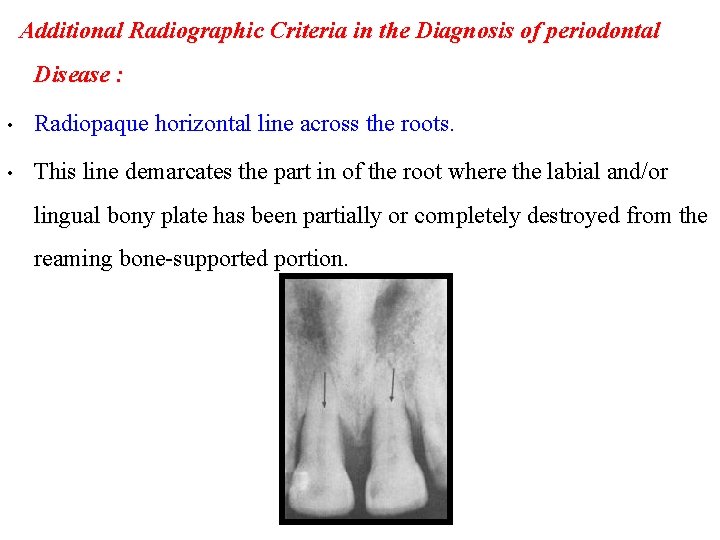
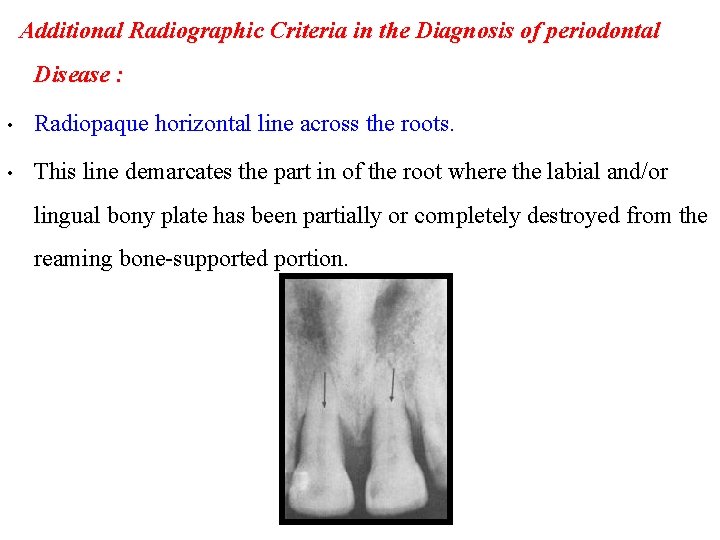
Additional Radiographic Criteria in the Diagnosis of periodontal Disease : • Radiopaque horizontal line across the roots. • This line demarcates the part in of the root where the labial and/or lingual bony plate has been partially or completely destroyed from the reaming bone-supported portion.
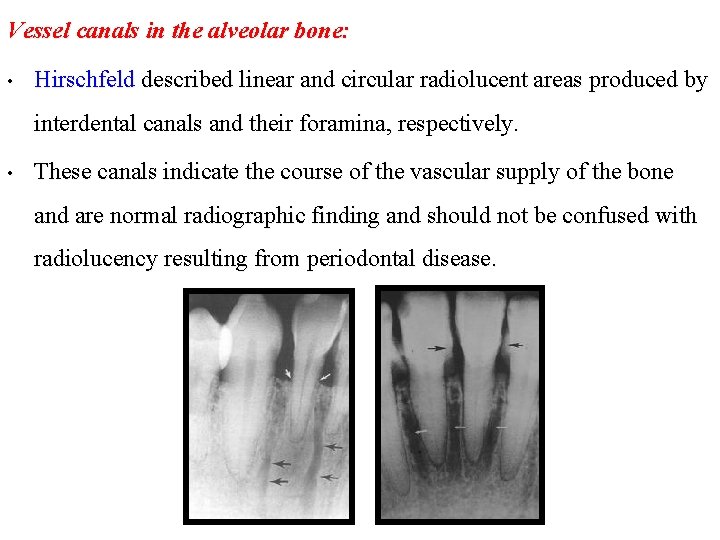
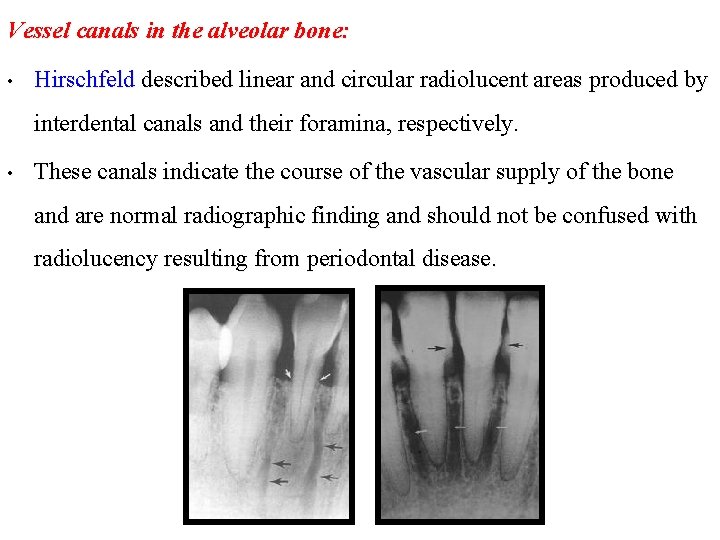
Vessel canals in the alveolar bone: • Hirschfeld described linear and circular radiolucent areas produced by interdental canals and their foramina, respectively. • These canals indicate the course of the vascular supply of the bone and are normal radiographic finding and should not be confused with radiolucency resulting from periodontal disease.
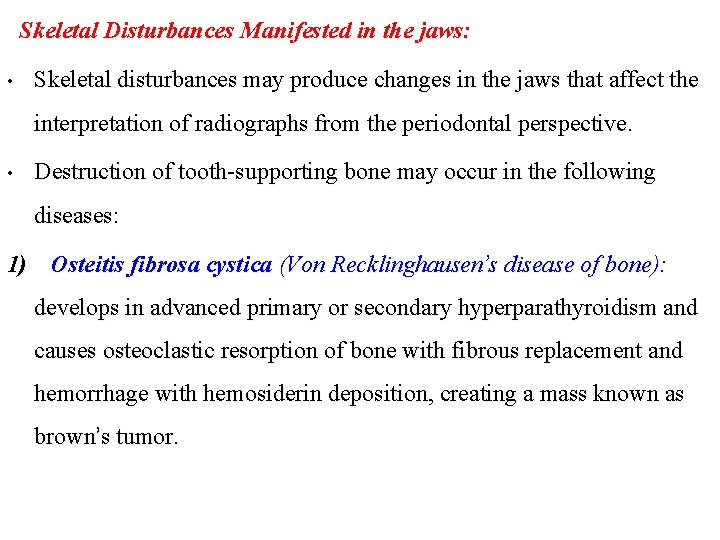
Skeletal Disturbances Manifested in the jaws: • Skeletal disturbances may produce changes in the jaws that affect the interpretation of radiographs from the periodontal perspective. • Destruction of tooth-supporting bone may occur in the following diseases: 1) Osteitis fibrosa cystica (Von Recklinghausen’s disease of bone): develops in advanced primary or secondary hyperparathyroidism and causes osteoclastic resorption of bone with fibrous replacement and hemorrhage with hemosiderin deposition, creating a mass known as brown’s tumor.
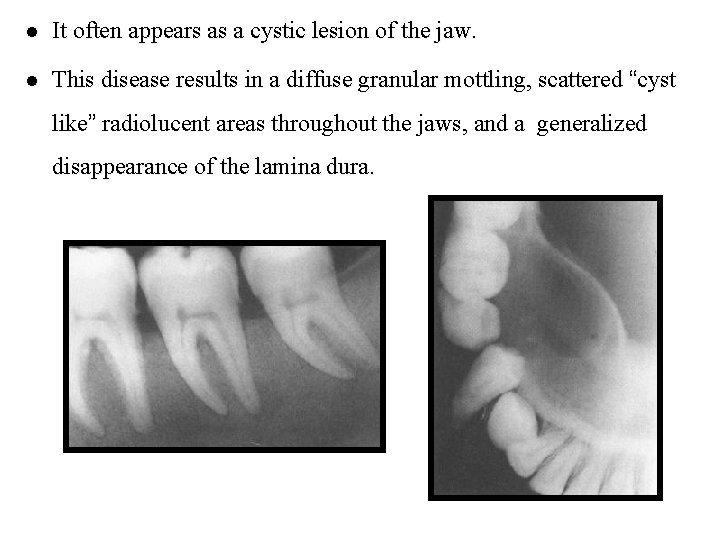
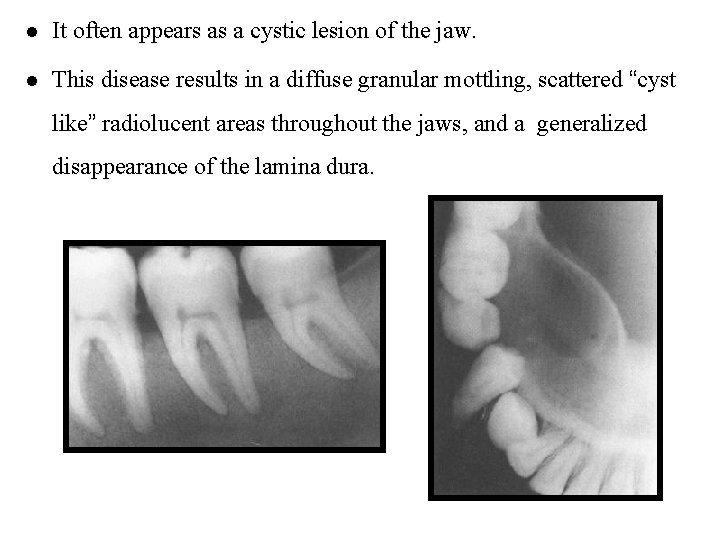
l It often appears as a cystic lesion of the jaw. l This disease results in a diffuse granular mottling, scattered “cyst like” radiolucent areas throughout the jaws, and a generalized disappearance of the lamina dura.
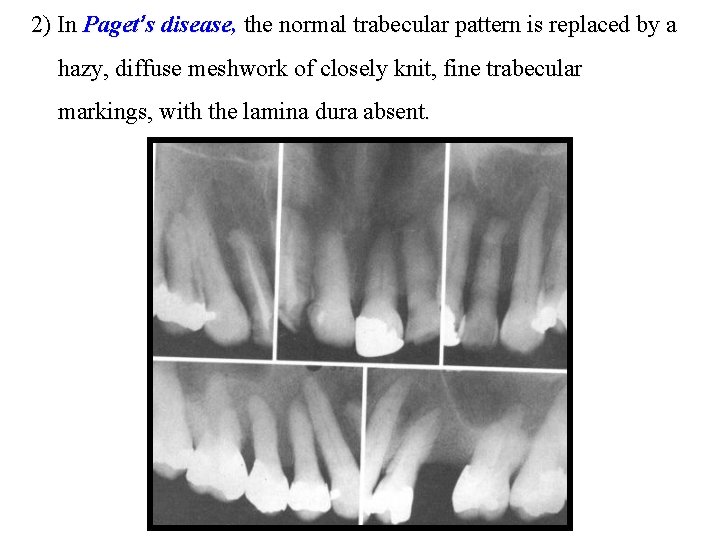
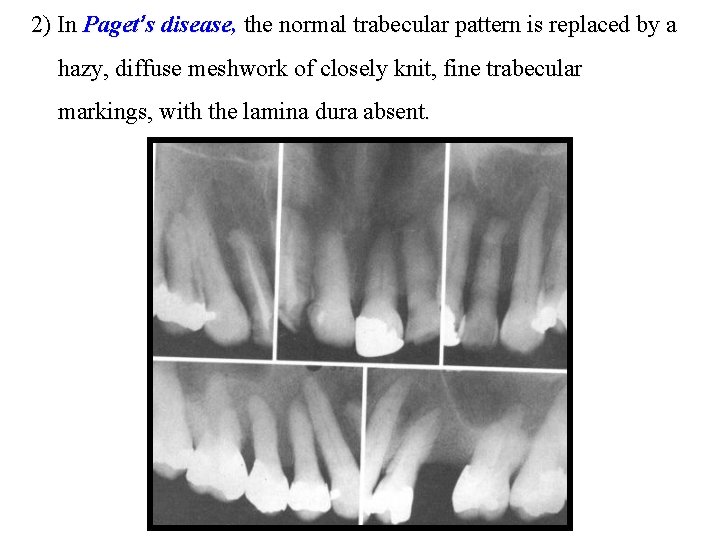
2) In Paget’s disease, the normal trabecular pattern is replaced by a hazy, diffuse meshwork of closely knit, fine trabecular markings, with the lamina dura absent.
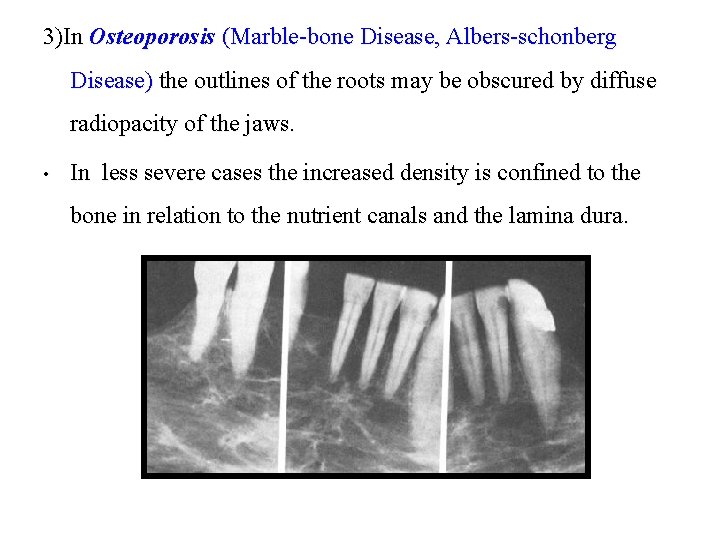
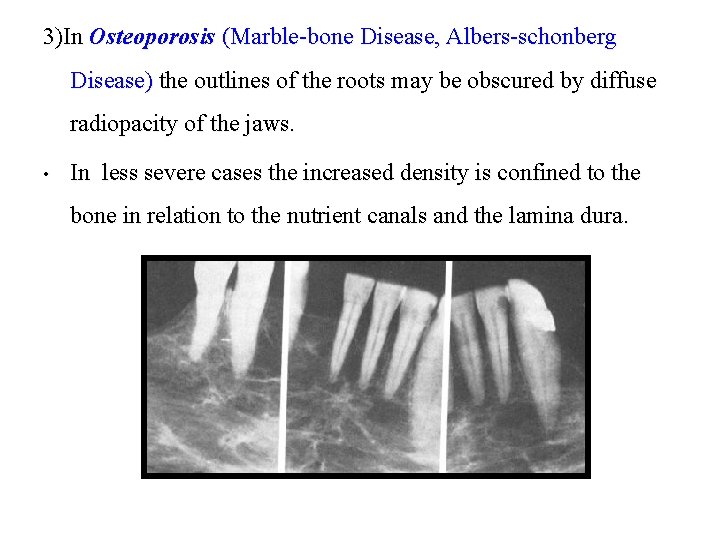
3)In Osteoporosis (Marble-bone Disease, Albers-schonberg Disease) the outlines of the roots may be obscured by diffuse radiopacity of the jaws. • In less severe cases the increased density is confined to the bone in relation to the nutrient canals and the lamina dura.

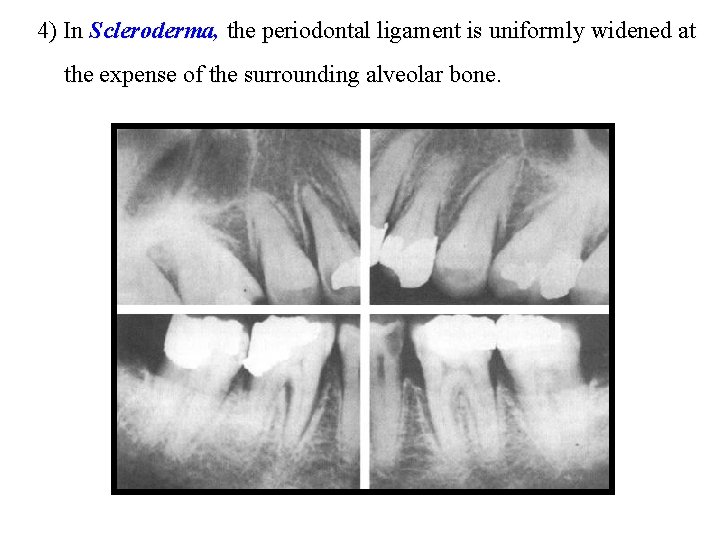
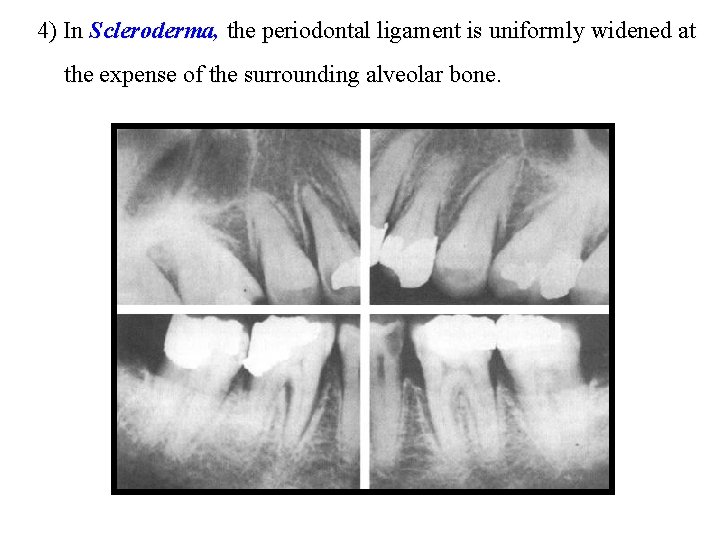
4) In Scleroderma, the periodontal ligament is uniformly widened at the expense of the surrounding alveolar bone.
Evaluation of periodontal therapy : • Radiographs may show signs of successful treatment of periodontal disease. • The relatively radiolucent margins of bone that were undergoing active resorption before treatment may become more sclerotic (radiopaque) after successful therapy. • The enlarged marrow spaces are reduced, and the bone becomes denser, creating the illusion of vertical bone growth (bone regeneration after therapy).
Conclusion l It is evident that despite some limitations, conventional radiographs provide information relevant to the diagnosis and management of the periodontal diseases. l It is widely held that the information generated by taking radiographs assists the overall management of patients and as such it is common practice to take radiographs for periodontal patients. l Less obvious is evidence of the extent to which the radiographs taken routinely, truly influence the treatment provided and its ultimate success.
l It may be that clinical assessments alone are appropriate for some groups of patients, with radiographs used as a second phase diagnostic test to be employed in specific situations or at specific sites rather than routinely and panorally. l It is now timely that clinicians critically appraise the traditional role of radiographs in the diagnosis and management of periodontal diseases to ensure that they do indeed provide a clearly defined benefit to patients.

Thank You
 Diagnosis of periodontal disease
Diagnosis of periodontal disease Frc control system
Frc control system Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Periodontal disease
Periodontal disease Why why why why
Why why why why Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Nursing process objectives
Nursing process objectives Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Anthropological baseline
Anthropological baseline Enema patient positioning
Enema patient positioning Grid conversion factors
Grid conversion factors Radiographic darkroom layout
Radiographic darkroom layout Dental radiography ppt
Dental radiography ppt Anthropological baseline
Anthropological baseline Oid radiography
Oid radiography Interdental septum
Interdental septum Radiographic film
Radiographic film Emulsion pickoff artifact
Emulsion pickoff artifact Reverse towne projection uses
Reverse towne projection uses Radiographic films
Radiographic films Geometric penumbra formula
Geometric penumbra formula Dacrocystogram
Dacrocystogram Nursing diagnosis for meniere's disease
Nursing diagnosis for meniere's disease Nursing diagnosis for meniere's disease
Nursing diagnosis for meniere's disease Behcet disease diagnosis
Behcet disease diagnosis Bharathi viswanathan
Bharathi viswanathan Don't ask why why why
Don't ask why why why Principles of scaling and root planing
Principles of scaling and root planing Perimylolysis
Perimylolysis Politür nedir
Politür nedir Periodontal space
Periodontal space Eoe ioe dental
Eoe ioe dental Plaque index scoring criteria
Plaque index scoring criteria Fases del tratamiento periodontal
Fases del tratamiento periodontal Corrective phase
Corrective phase Lanap perio
Lanap perio Rationale of periodontal therapy
Rationale of periodontal therapy Gingival lifler
Gingival lifler Periodonto de insercion
Periodonto de insercion Periodontal response to external forces
Periodontal response to external forces Non-infective
Non-infective Streptokokal gingivitis
Streptokokal gingivitis Step back tecnica
Step back tecnica Bolsa periodontal falsa y verdadera
Bolsa periodontal falsa y verdadera Thixotropic theory of pdl
Thixotropic theory of pdl Birleşim epiteli
Birleşim epiteli Non corticated
Non corticated Lateral periodontal cyst
Lateral periodontal cyst Periodontal abscess
Periodontal abscess Periodontal ligament injection definition
Periodontal ligament injection definition Kista residual adalah
Kista residual adalah Class v facial composite charting
Class v facial composite charting Periodontal healing
Periodontal healing Principles of periodontal surgery
Principles of periodontal surgery Oral git
Oral git Grupos de fibras del ligamento periodontal
Grupos de fibras del ligamento periodontal Undisplaced flap procedure
Undisplaced flap procedure Ligamento periodontal
Ligamento periodontal Who sondu nedir
Who sondu nedir Periodontal cep
Periodontal cep Periodontal case study
Periodontal case study Suprabony pocket
Suprabony pocket Stress strain curve physiotherapy
Stress strain curve physiotherapy Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy