PERIODONTAL LIGAMENT INTRODUCTION A ligament is defined as


- Slides: 65

PERIODONTAL LIGAMENT
INTRODUCTION Ø A ligament is defined as a band of fibrous tissue binding together skeletal elements. Ø The root of the tooth is connected to its socket in alveolar bone by a dense fibrous connective tissue, which can be regarded as a ligament. Ø PDL is unique among the various ligaments in the body that it is the only ligament to span to distict hard tissues – namely tooth cementum and bone.
Ø Maintenance and remodeling of the PDL collagen fibrous and embedding and calcification of their extremities to form sharpeys fibers, requires the concerted action of numerous cell types. Ø Central to these integrated activities is the PDL fibroblast. Ø The rapid growth of interest in endosseous implants as surrogates for natural teeth could indicate that the demise of the PDL is imminent. Implants do not employ a gomphosis to provide support and attachment to the jaw bone as does the PDL, but still it serves as a replacement for natural teeth.
DEFINITION Ø Is the connective tissue that surrounds the root and connects it to the bone. Ø It is continue with the connective tissue of the gingiva and communicate with narrow space through vascular channels in the bone.
SHAPE OF THE PDL Hour glass appearance Narrowest at the mid root level. Width of PDL 0. 25 mm. Range 0. 2 – 0. 4 mm.
OTHER NAMES Ø Desmodent Ø Gomphosis Ø Pericementum Ø Dental periosteum Ø Alveolo dental ligament Ø Periodontal membrane.
PERIODONTAL LIGAMENT DEVELOPMENT Ø The PDL is derived from the cells of the dental follicle. Ø As the crown approaches the oral mucosa during tooth eruption, these fibroblasts become active and start producing collagen fibrils.
Ø That the term “Dental follicle” be reserved for this layer of cells and the term “ Peri follicular mesenchyme” for the cells that surround the dental follicle. Ø The formation of the PDL occurs after the cells of hertwigs epithelial root sheath have forming the strands knows as epithelial rests of malassez. Ø These migrant follicle cells then differentiates into cementoblasts and deposit cementum on the surface dentin other cells of the dental follicle differentiate into fibroblasts, which synthesize the fibers and ground substance of PDL. Ø The fibers of the PDL become embedded in newly developed cementum and alveolar bone and the tooth erupts are oriented in characteristic fashion.
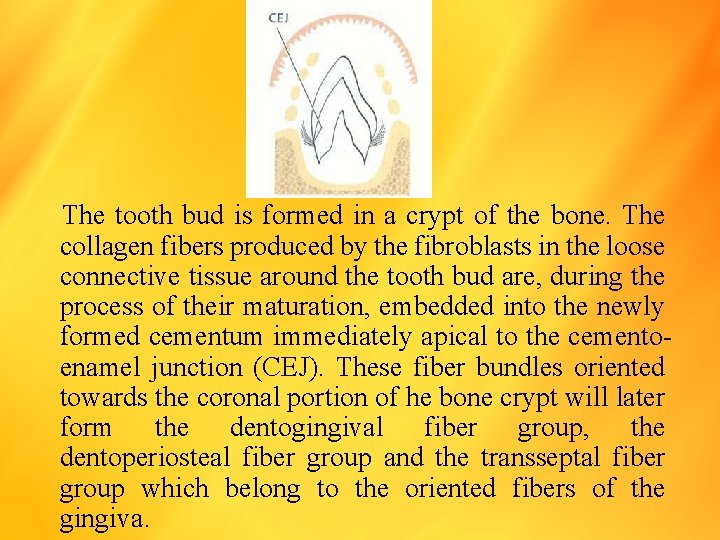
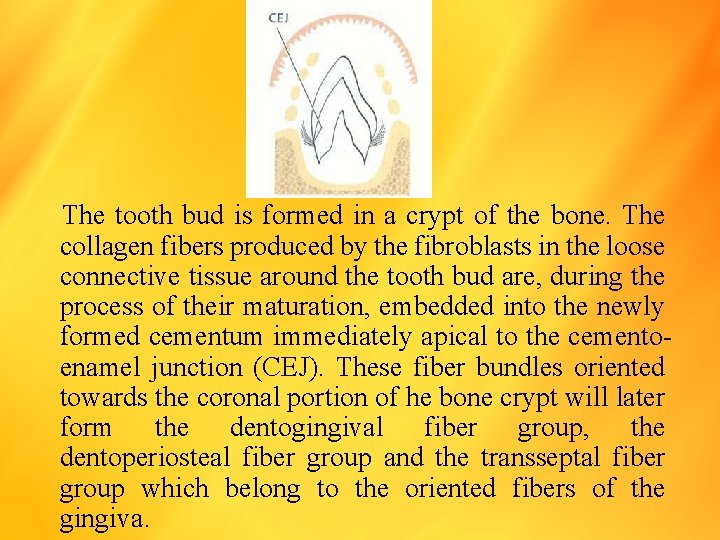
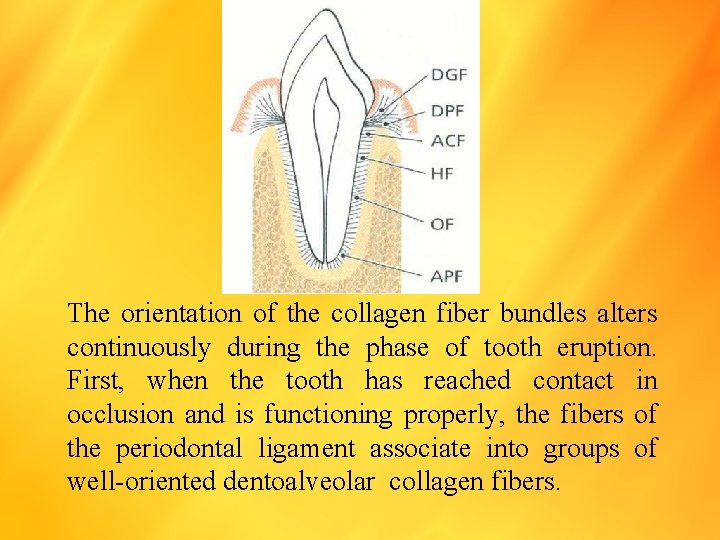
The tooth bud is formed in a crypt of the bone. The collagen fibers produced by the fibroblasts in the loose connective tissue around the tooth bud are, during the process of their maturation, embedded into the newly formed cementum immediately apical to the cementoenamel junction (CEJ). These fiber bundles oriented towards the coronal portion of he bone crypt will later form the dentogingival fiber group, the dentoperiosteal fiber group and the transseptal fiber group which belong to the oriented fibers of the gingiva.
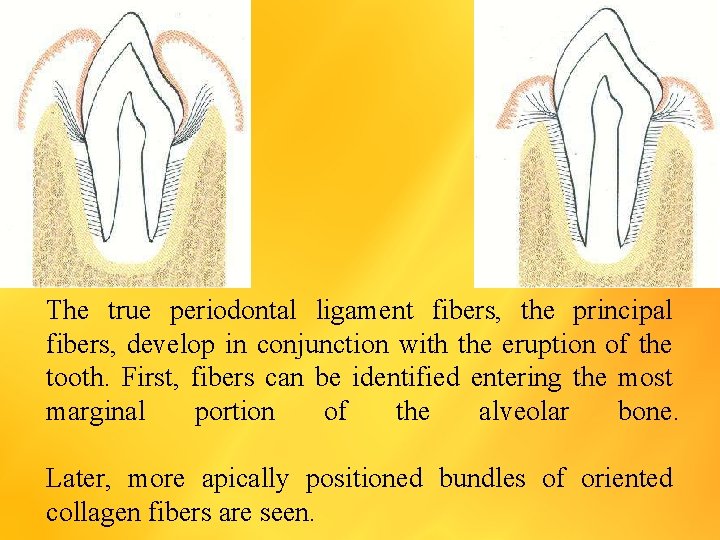
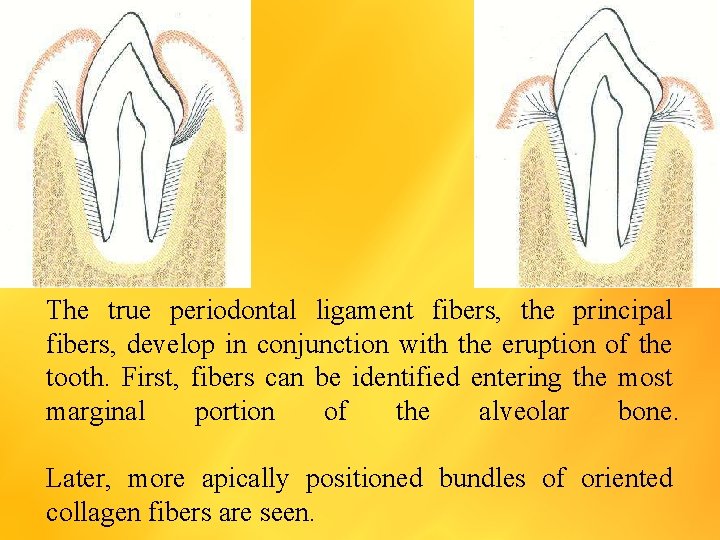
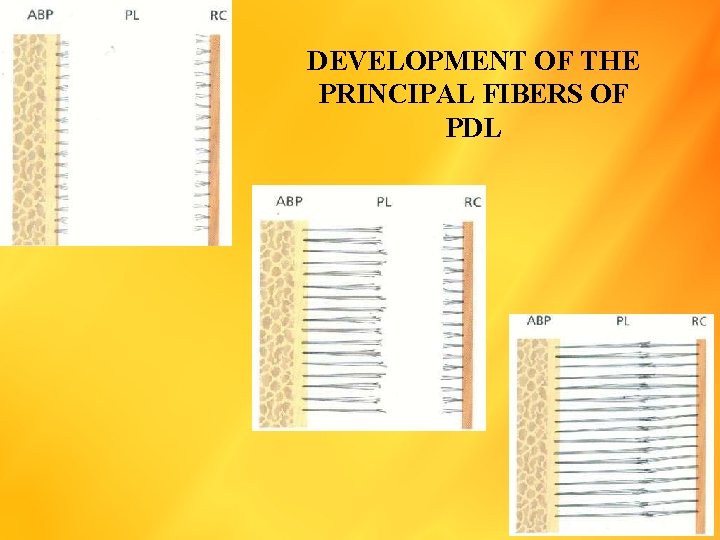
The true periodontal ligament fibers, the principal fibers, develop in conjunction with the eruption of the tooth. First, fibers can be identified entering the most marginal portion of the alveolar bone. Later, more apically positioned bundles of oriented collagen fibers are seen.
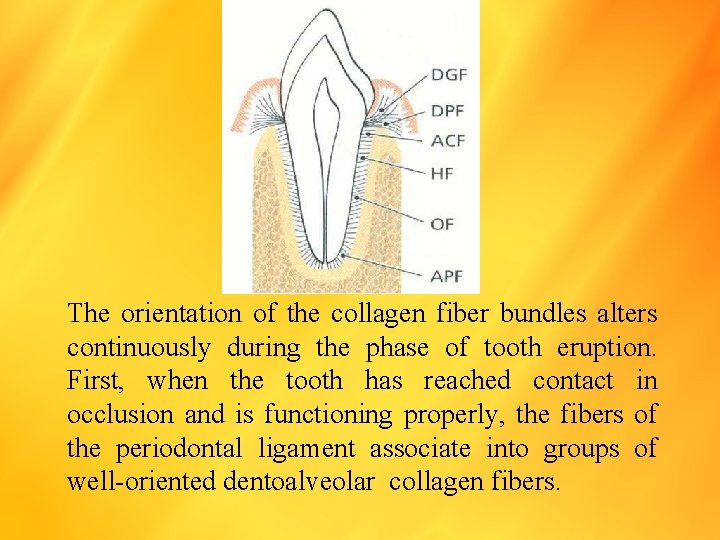
The orientation of the collagen fiber bundles alters continuously during the phase of tooth eruption. First, when the tooth has reached contact in occlusion and is functioning properly, the fibers of the periodontal ligament associate into groups of well-oriented dentoalveolar collagen fibers.
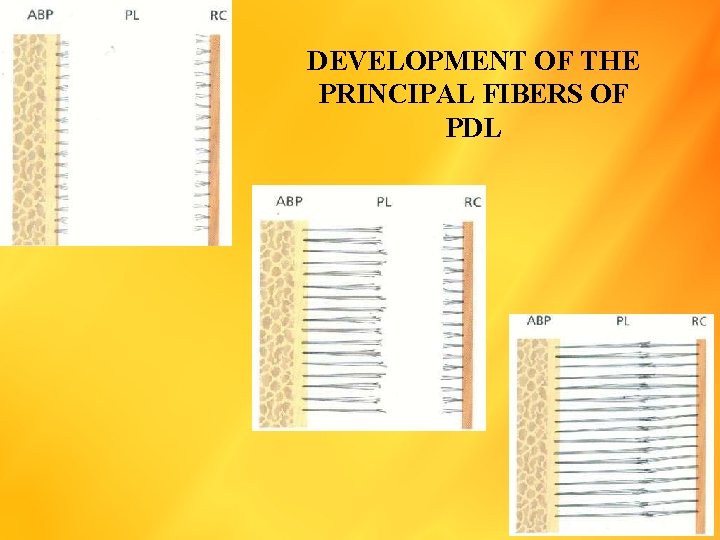
DEVELOPMENT OF THE PRINCIPAL FIBERS OF PDL
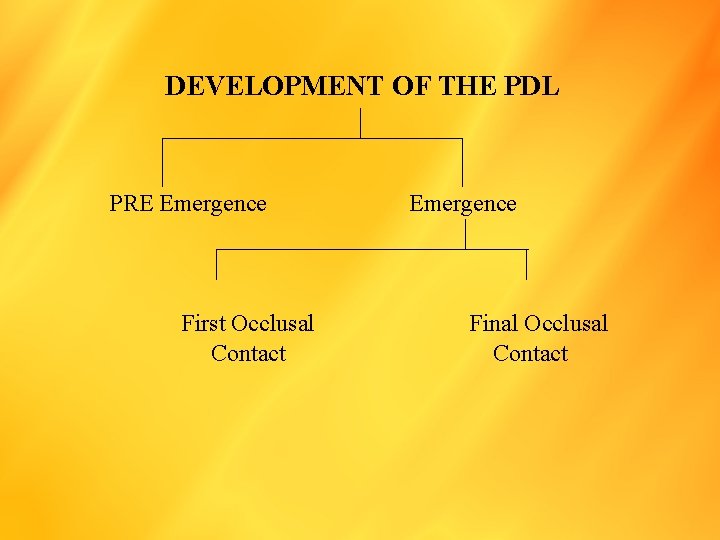
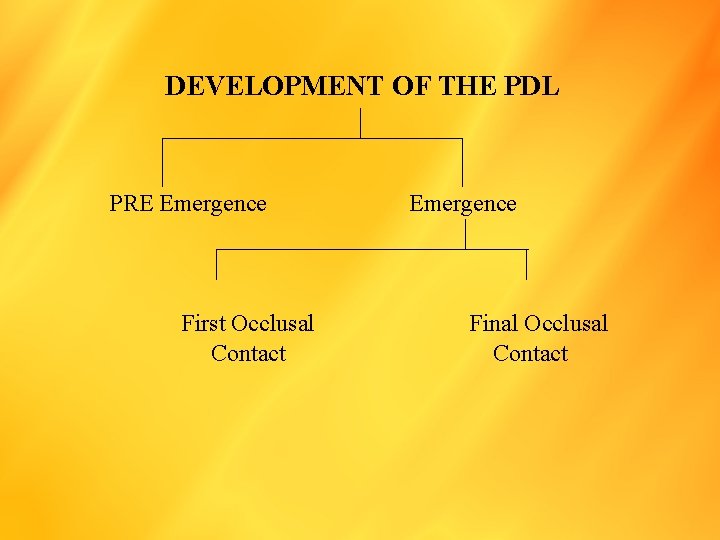
DEVELOPMENT OF THE PDL PRE Emergence First Occlusal Contact Emergence Final Occlusal Contact
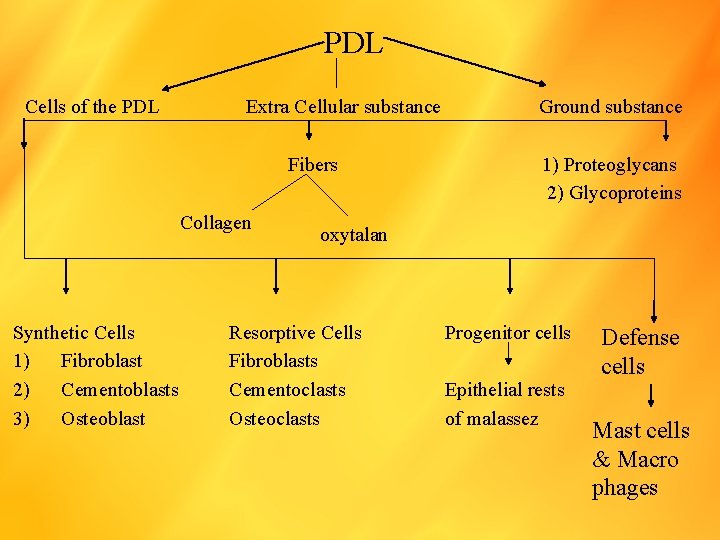
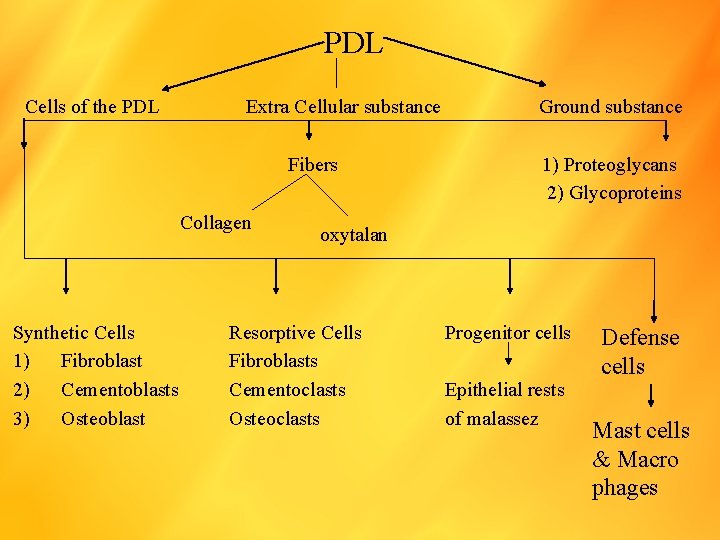
PDL Cells of the PDL Extra Cellular substance Fibers Collagen Synthetic Cells 1) Fibroblast 2) Cementoblasts 3) Osteoblast Ground substance 1) Proteoglycans 2) Glycoproteins oxytalan Resorptive Cells Fibroblasts Cementoclasts Osteoclasts Progenitor cells Epithelial rests of malassez Defense cells Mast cells & Macro phages
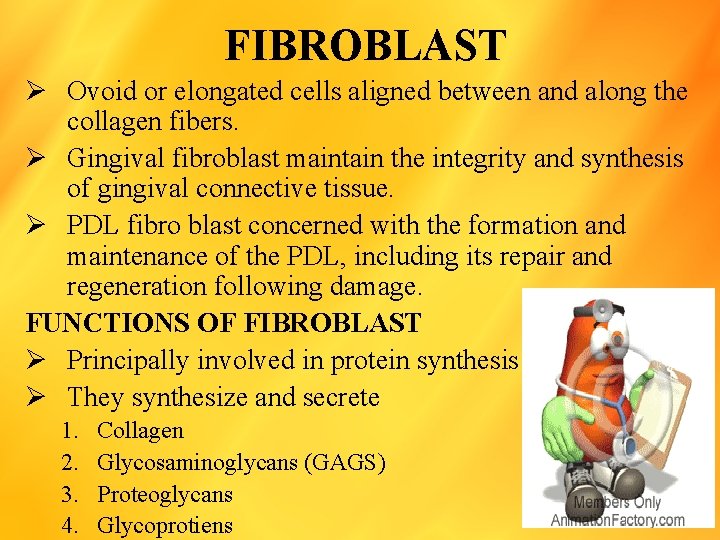
FIBROBLAST Ø Ovoid or elongated cells aligned between and along the collagen fibers. Ø Gingival fibroblast maintain the integrity and synthesis of gingival connective tissue. Ø PDL fibro blast concerned with the formation and maintenance of the PDL, including its repair and regeneration following damage. FUNCTIONS OF FIBROBLAST Ø Principally involved in protein synthesis Ø They synthesize and secrete 1. 2. 3. 4. Collagen Glycosaminoglycans (GAGS) Proteoglycans Glycoprotiens
Ø Fibroblast are also involved in collagen degradation with in the ligament Ø There are many reports showing that PDL fibroblast contain small fragments of collagen fibrils within membrane bound vesicles, and are termed “ Intracellular collagen profiles” Ø These are the evidence for intracellular process of degradation of collagen. Ø Fragment of collagens resulting phagosome lysosomes phagolysosome Ø Enzyme present in lysosme cysteine proteinases which degrade the fibril Ø Time taken for intracellular degradation of collagen is about 30 minutes.
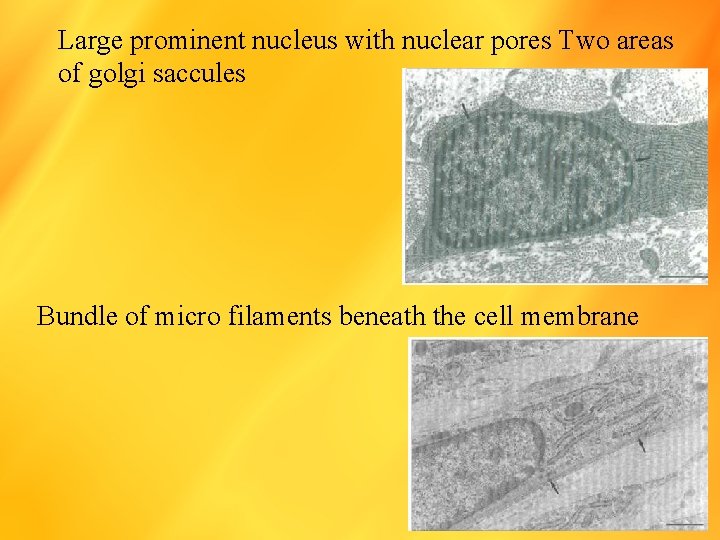
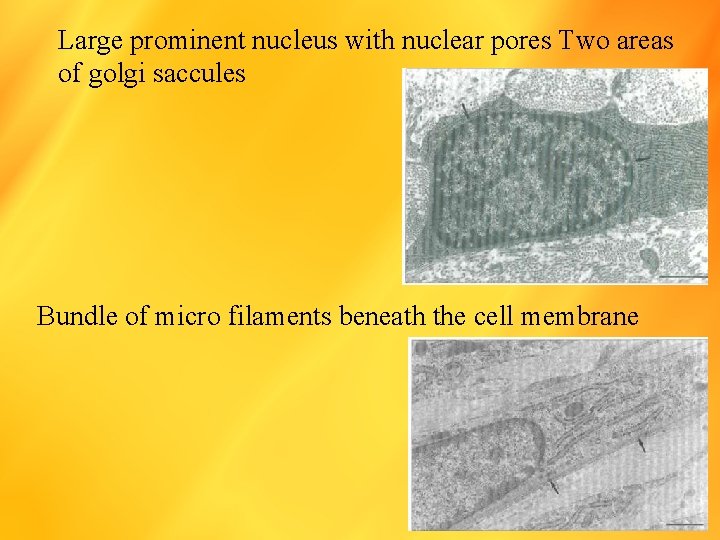
Large prominent nucleus with nuclear pores Two areas of golgi saccules Bundle of micro filaments beneath the cell membrane
REMODELING OF PDL Ø Resorption of old fibres and formation of new ones and fibroblast or involved in both processes Ø Cytokines such as FGF, PDGF, TGF- and stimulates synthesis of collagen. Ø Others cytokines such as IL-1 and IFN can stimulate collagenase secretion.
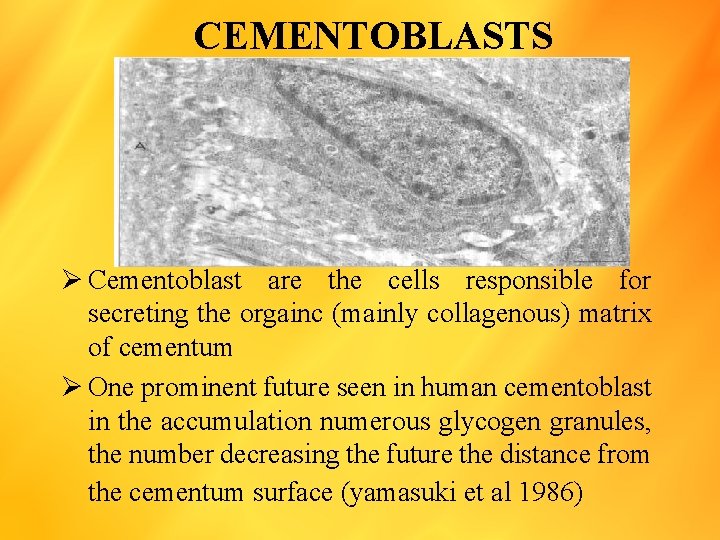
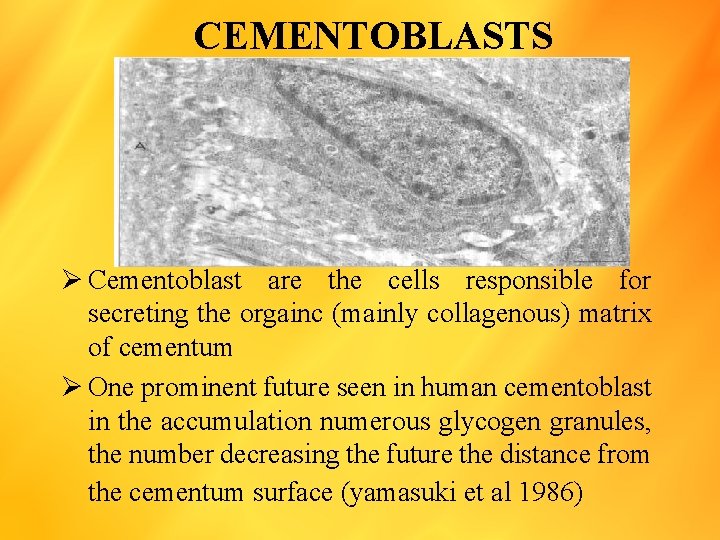
CEMENTOBLASTS Ø Cementoblast are the cells responsible for secreting the orgainc (mainly collagenous) matrix of cementum Ø One prominent future seen in human cementoblast in the accumulation numerous glycogen granules, the number decreasing the future the distance from the cementum surface (yamasuki et al 1986)
OSTEOBLASTS Ø Osteoblast within the PDL are found on the surface of the alveolar bone. Ø Then form a layer of cuboidal cells, which exhibit a strong basophilic cytoplasm. Ø A prominent nucleus lies towards the sacule and of the cell and a pale juxtanuclear area indicates the site of the golgi complex.
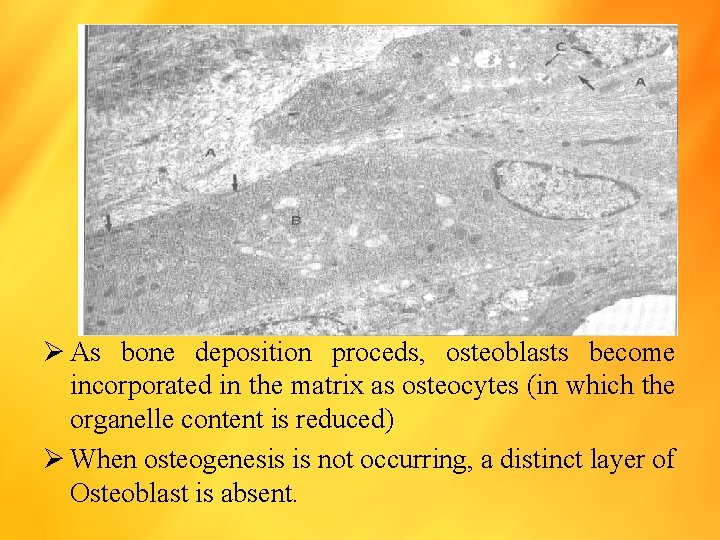
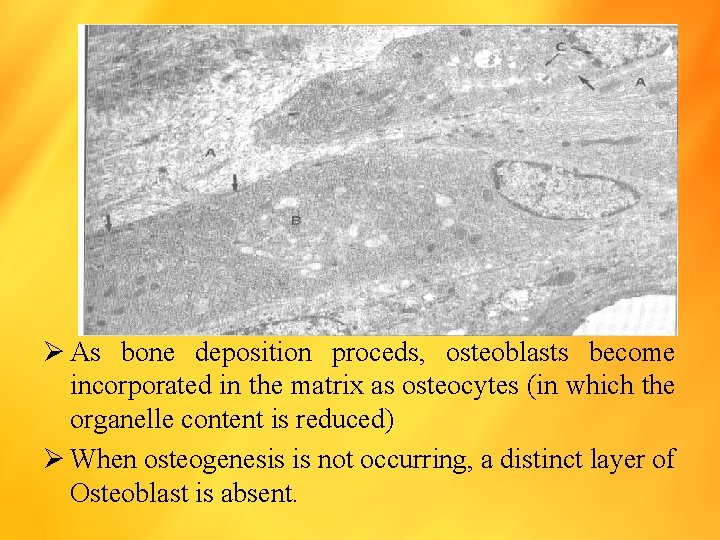
Ø As bone deposition proceds, osteoblasts become incorporated in the matrix as osteocytes (in which the organelle content is reduced) Ø When osteogenesis is not occurring, a distinct layer of Osteoblast is absent.
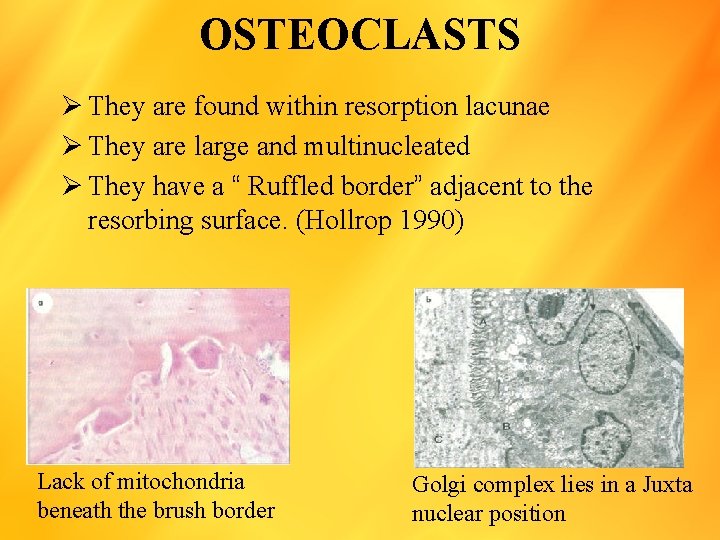
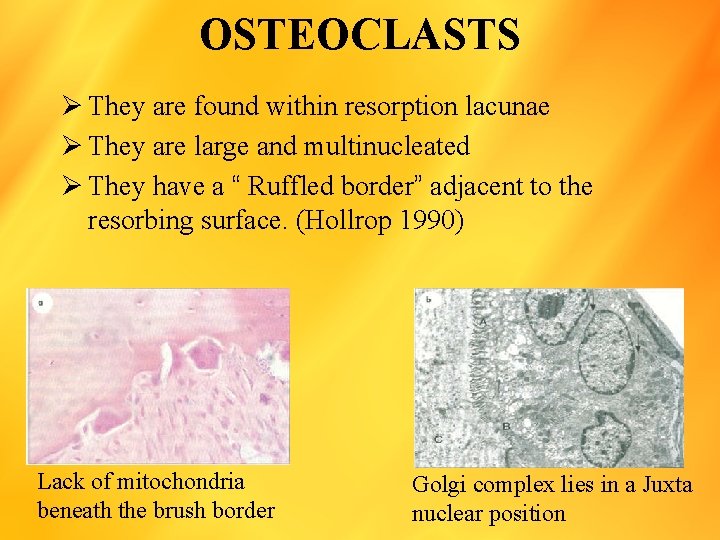
OSTEOCLASTS Ø They are found within resorption lacunae Ø They are large and multinucleated Ø They have a “ Ruffled border” adjacent to the resorbing surface. (Hollrop 1990) Lack of mitochondria beneath the brush border Golgi complex lies in a Juxta nuclear position
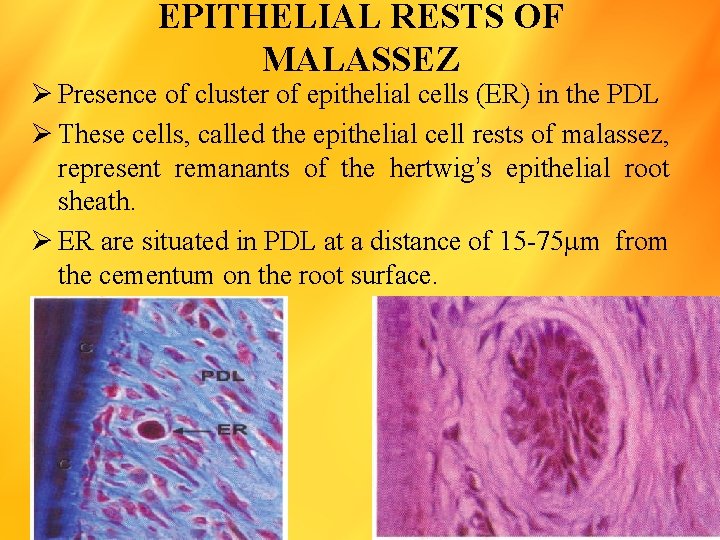
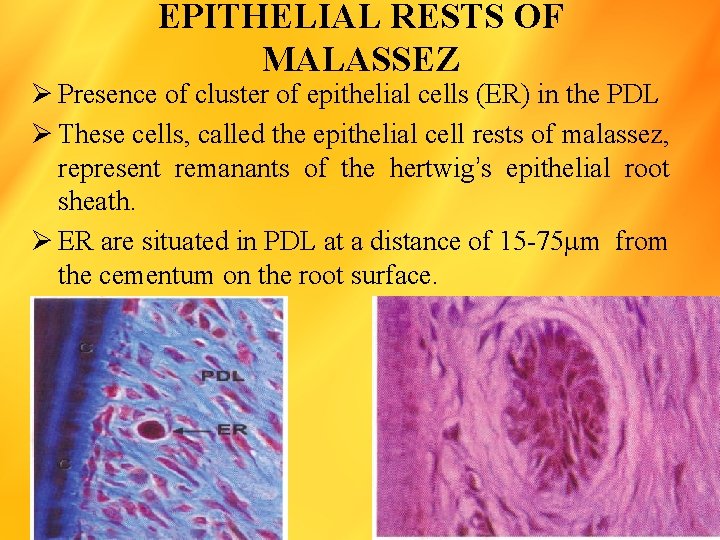
EPITHELIAL RESTS OF MALASSEZ Ø Presence of cluster of epithelial cells (ER) in the PDL Ø These cells, called the epithelial cell rests of malassez, represent remanants of the hertwig’s epithelial root sheath. Ø ER are situated in PDL at a distance of 15 -75 m from the cementum on the root surface.
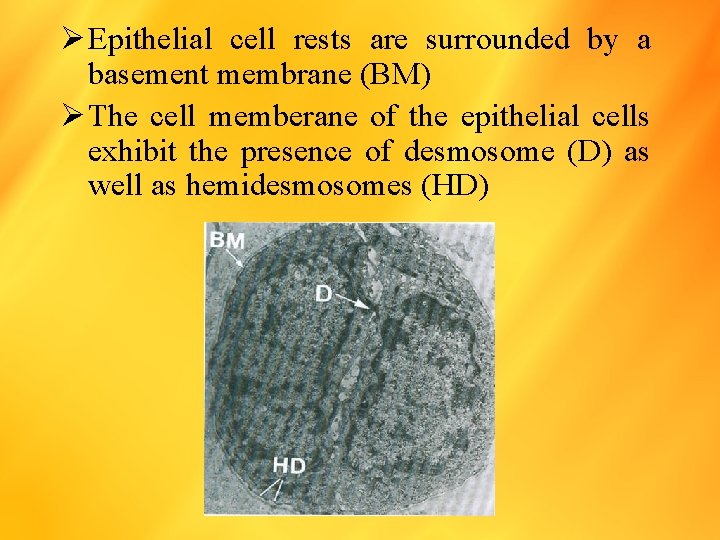
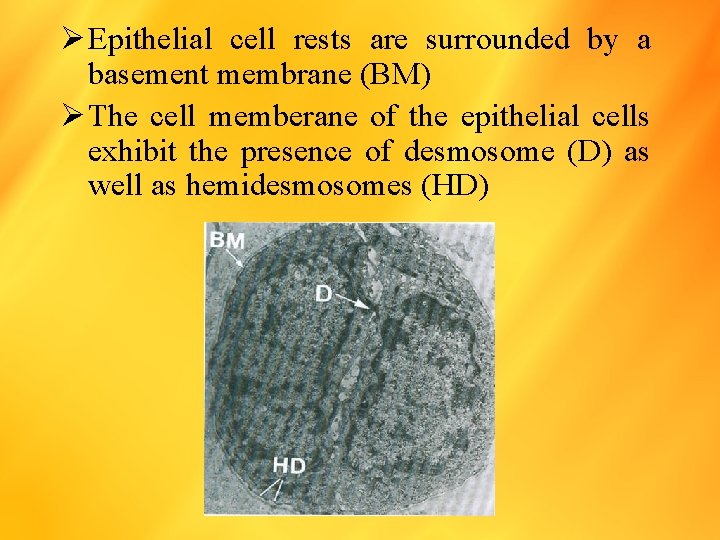
Ø Epithelial cell rests are surrounded by a basement membrane (BM) Ø The cell memberane of the epithelial cells exhibit the presence of desmosome (D) as well as hemidesmosomes (HD)

Ø PDL Removed from an extracted tooth Ø Epithelial cell rests of malassez appear as isolated groups of epithelial cells, in fact from a continuous network of epithelial cells surrounding the root.
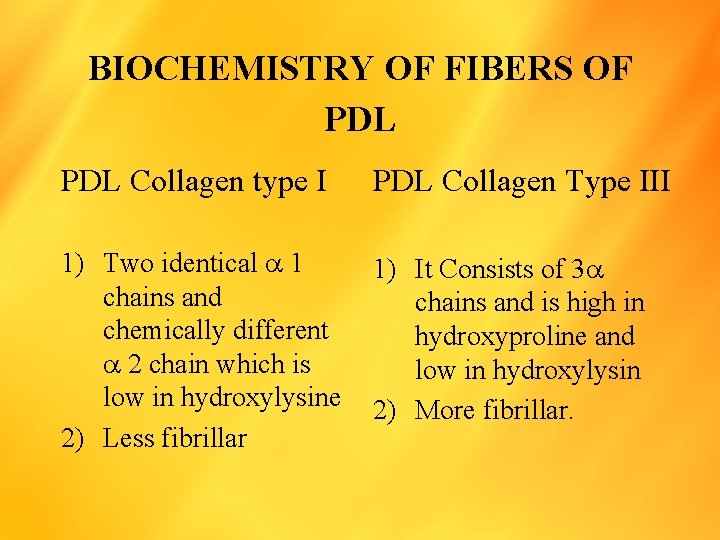
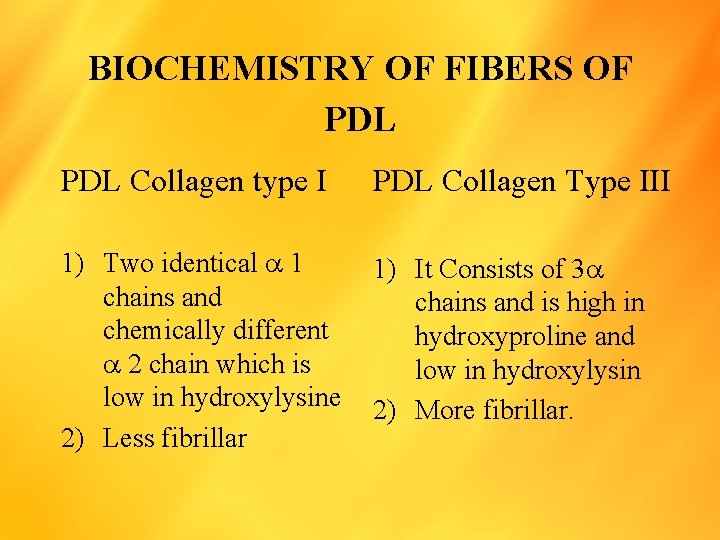
BIOCHEMISTRY OF FIBERS OF PDL Collagen type I PDL Collagen Type III 1) Two identical 1 chains and chemically different 2 chain which is low in hydroxylysine 2) Less fibrillar 1) It Consists of 3 chains and is high in hydroxyproline and low in hydroxylysin 2) More fibrillar.
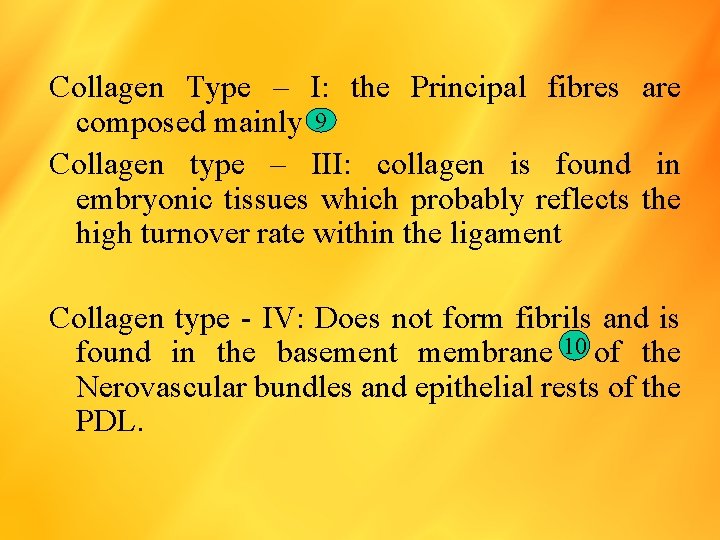
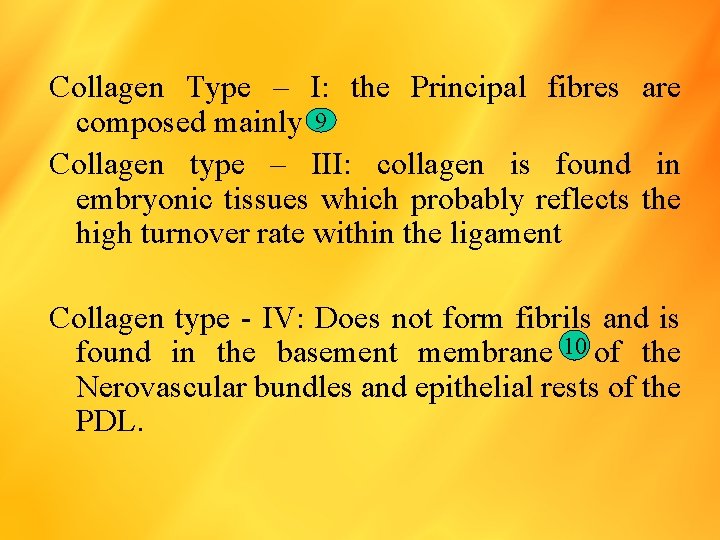
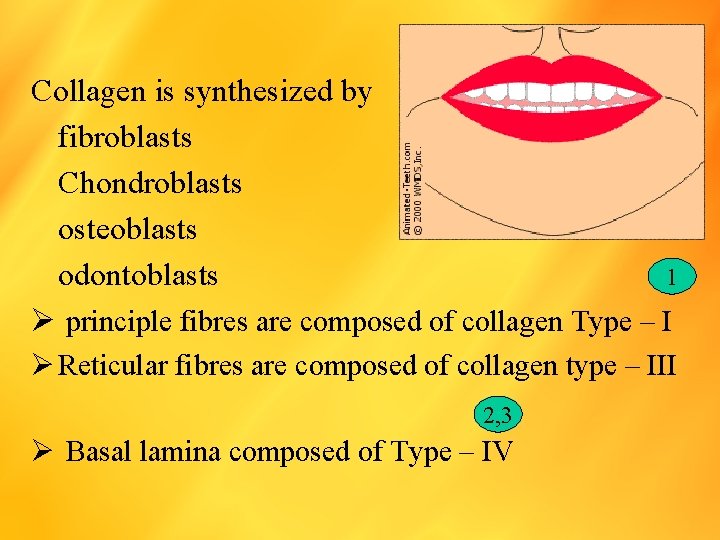
Collagen Type – I: the Principal fibres are composed mainly 9 Collagen type – III: collagen is found in embryonic tissues which probably reflects the high turnover rate within the ligament Collagen type - IV: Does not form fibrils and is found in the basement membrane 10 of the Nerovascular bundles and epithelial rests of the PDL.
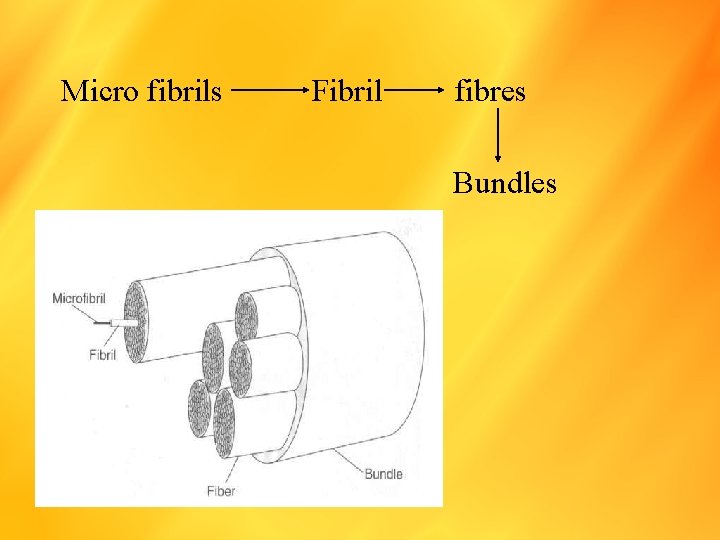
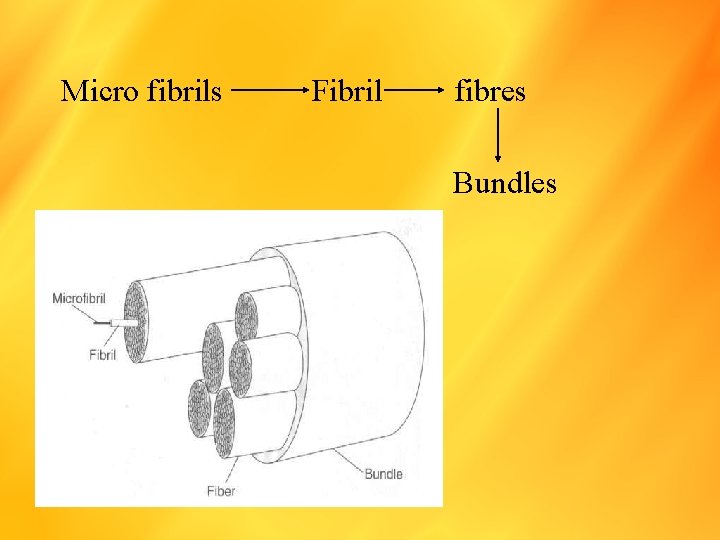
Micro fibrils Fibril fibres Bundles
Collagen is synthesized by fibroblasts Chondroblasts osteoblasts 1 odontoblasts Ø principle fibres are composed of collagen Type – I Ø Reticular fibres are composed of collagen type – III 2, 3 Ø Basal lamina composed of Type – IV
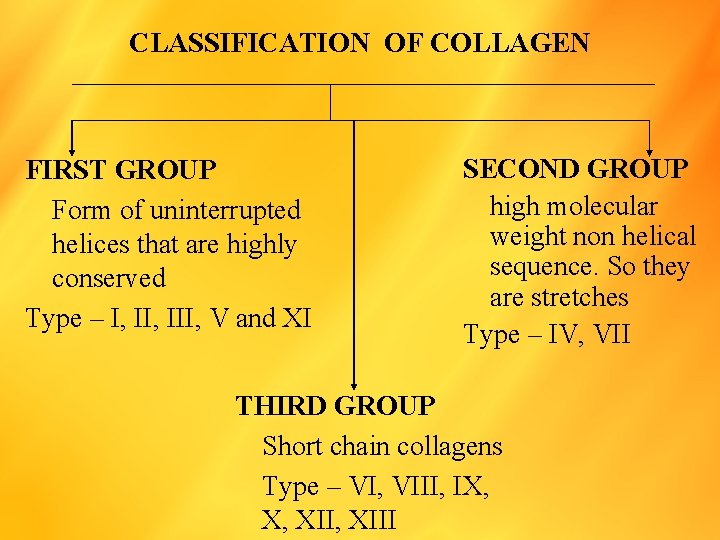
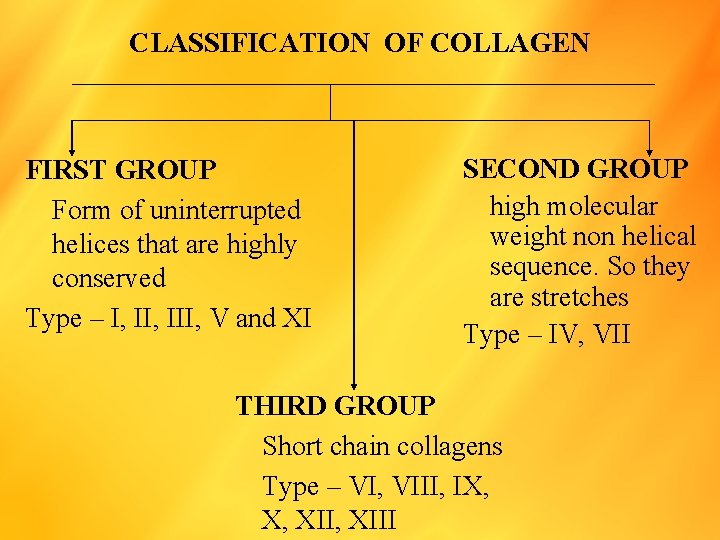
CLASSIFICATION OF COLLAGEN FIRST GROUP Form of uninterrupted helices that are highly conserved Type – I, III, V and XI SECOND GROUP high molecular weight non helical sequence. So they are stretches Type – IV, VII THIRD GROUP Short chain collagens Type – VI, VIII, IX, X, XIII
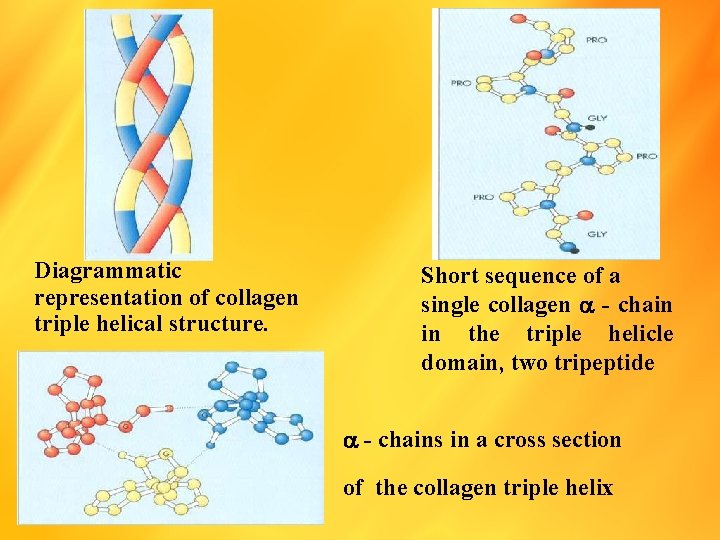
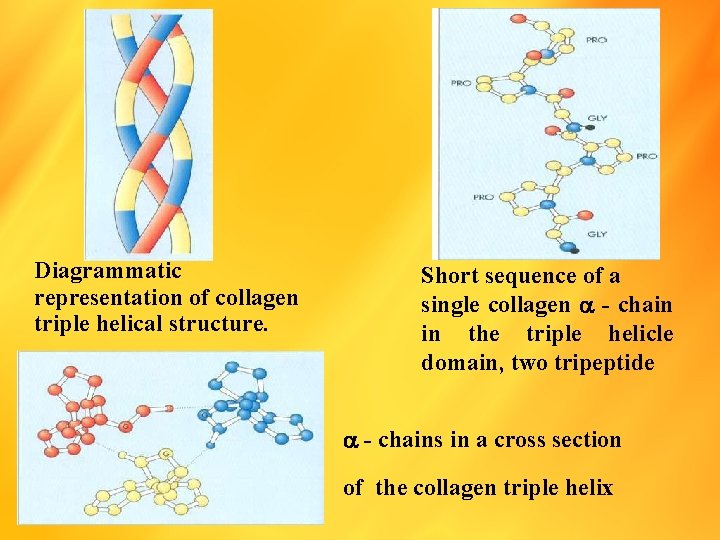
Diagrammatic representation of collagen triple helical structure. Short sequence of a single collagen - chain in the triple helicle domain, two tripeptide - chains in a cross section of the collagen triple helix
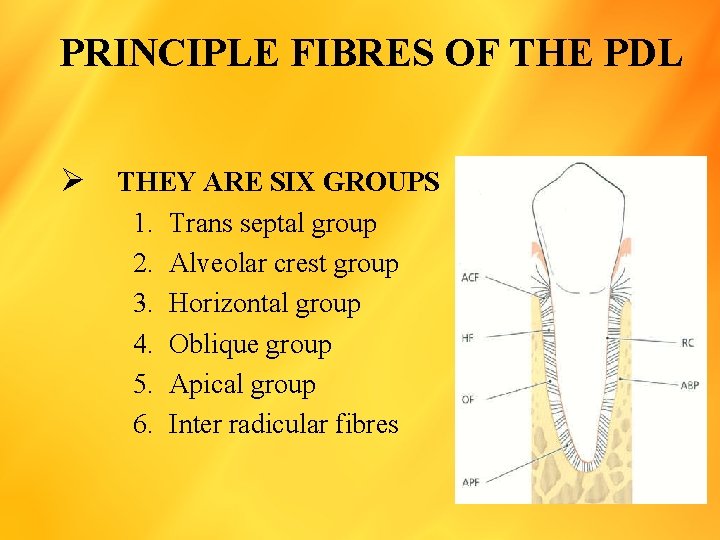
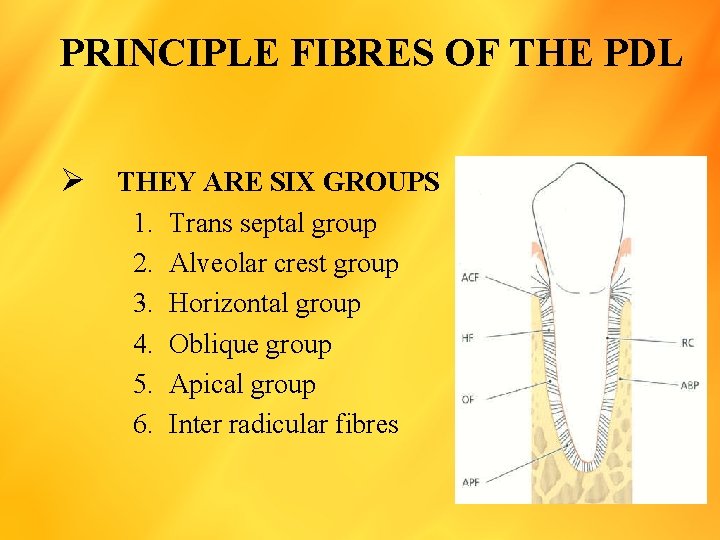
PRINCIPLE FIBRES OF THE PDL Ø THEY ARE SIX GROUPS 1. 2. 3. 4. 5. 6. Trans septal group Alveolar crest group Horizontal group Oblique group Apical group Inter radicular fibres
Trans septal group Ø These are extended interproximally over the alveolar bone crest and are embedded in the cementum of adjacent teeth. Ø these fibres may be considered as belonging to the gingiva because they do not have osseous attachment. Alveolar crest group Ø These are extended obliquely from the cementam just beneath the juncational epithelium, to the alveolar crest. 4 Ø The alveolar crest fibres prevent the extrusion of the tooth. Ø And resist lateral tooth movements. 5 Ø Their incision does not significantly increase tooth mobility.
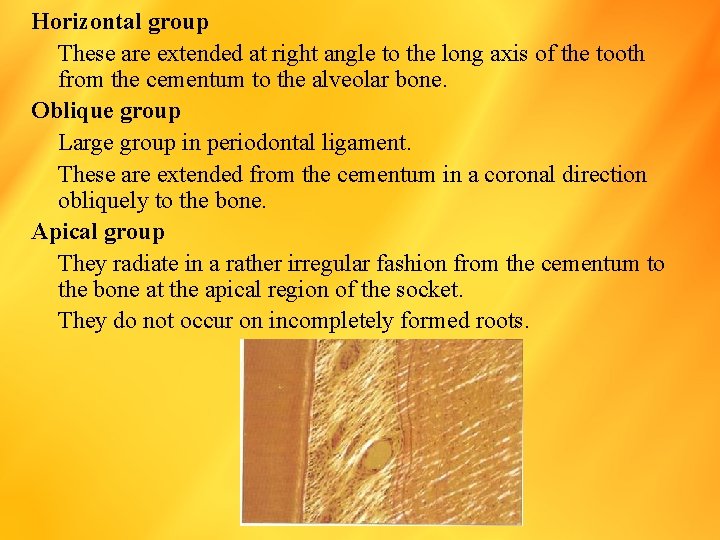
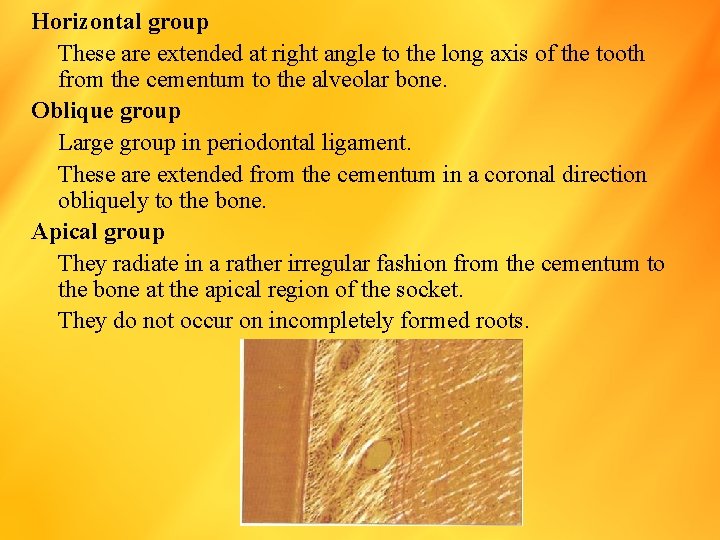
Horizontal group These are extended at right angle to the long axis of the tooth from the cementum to the alveolar bone. Oblique group Large group in periodontal ligament. These are extended from the cementum in a coronal direction obliquely to the bone. Apical group They radiate in a rather irregular fashion from the cementum to the bone at the apical region of the socket. They do not occur on incompletely formed roots.
Inter radicular fibres The inter radicular fibres fan out from the cementum to the tooth in the furcation areas of multirooted teeth oxytalan fibres they run parallel to the root surface in a vertical direction and bend to attach to cementum in the cervical third of the root. 6 7 they are thought to regulate vascular flow
GROUND SUBSTANCE OF THE PDL Ø The ligament ground substance is an amorphous matrix of glycosaminoglycans (GAGS), proteoglycans and glycoproteins. Ø It has high water content (70%) Ø This extra cellular matrix (ECM) place an important role in the absorption of functional stresses. Ø It is presumed that GAGS, proteoglycans and glycoproteins are secreted by fibroblast.
Ø Their water binding function are thought to produce a hydraulic cushion in the PDL, which resist the forces of mastication. Ø The cell surface proteoglycans mediate cell adhesion, migration, proliferation and differentiation.
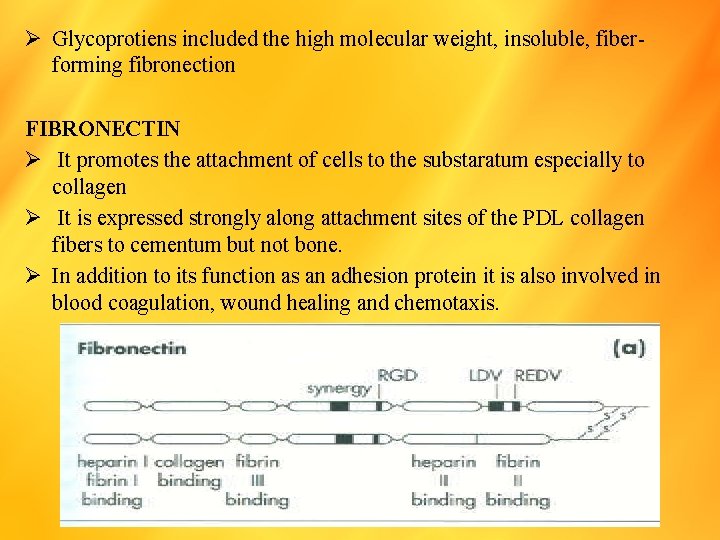
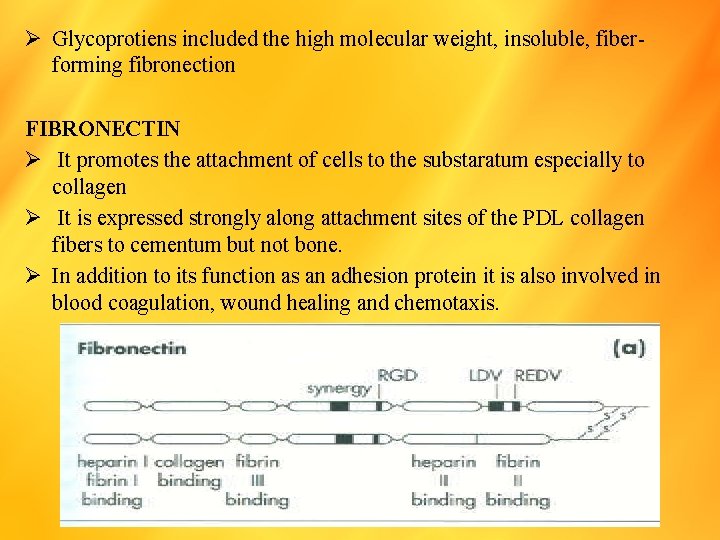
Ø Glycoprotiens included the high molecular weight, insoluble, fiberforming fibronection FIBRONECTIN Ø It promotes the attachment of cells to the substaratum especially to collagen Ø It is expressed strongly along attachment sites of the PDL collagen fibers to cementum but not bone. Ø In addition to its function as an adhesion protein it is also involved in blood coagulation, wound healing and chemotaxis.
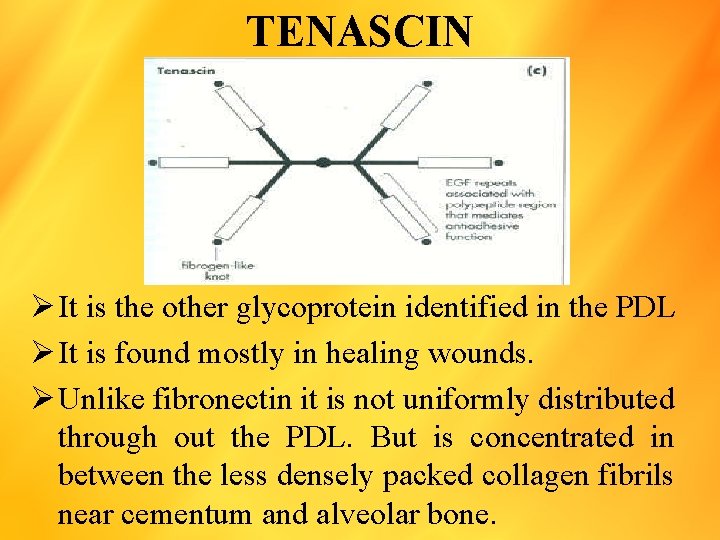
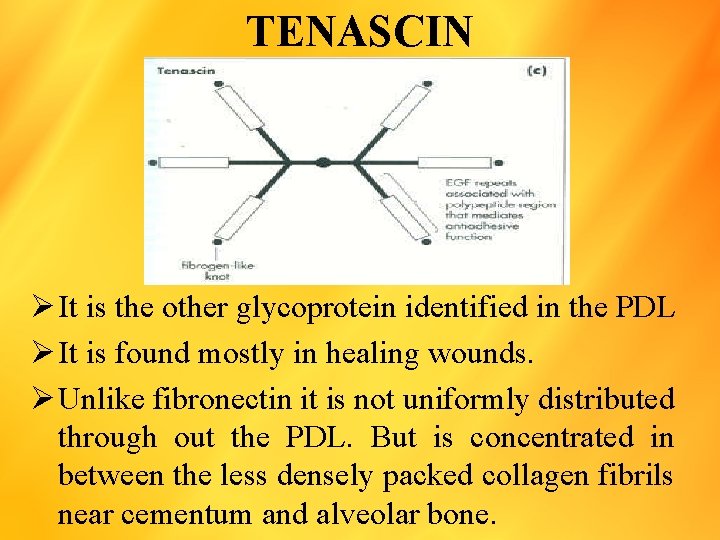
TENASCIN Ø It is the other glycoprotein identified in the PDL Ø It is found mostly in healing wounds. Ø Unlike fibronectin it is not uniformly distributed through out the PDL. But is concentrated in between the less densely packed collagen fibrils near cementum and alveolar bone.
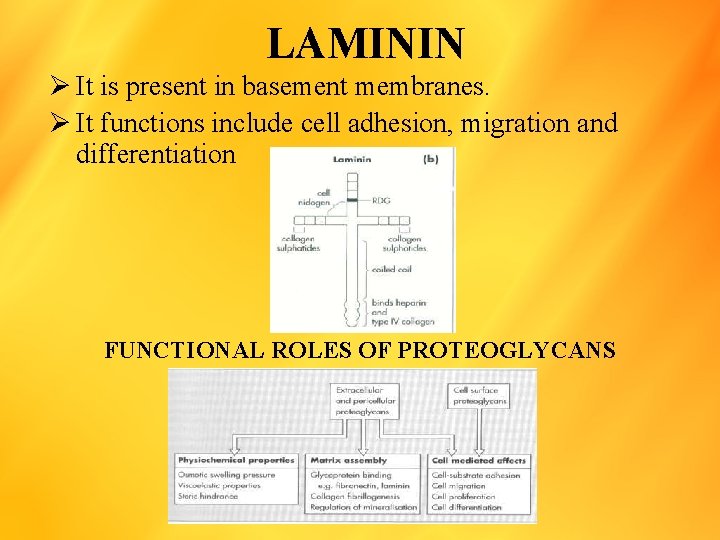
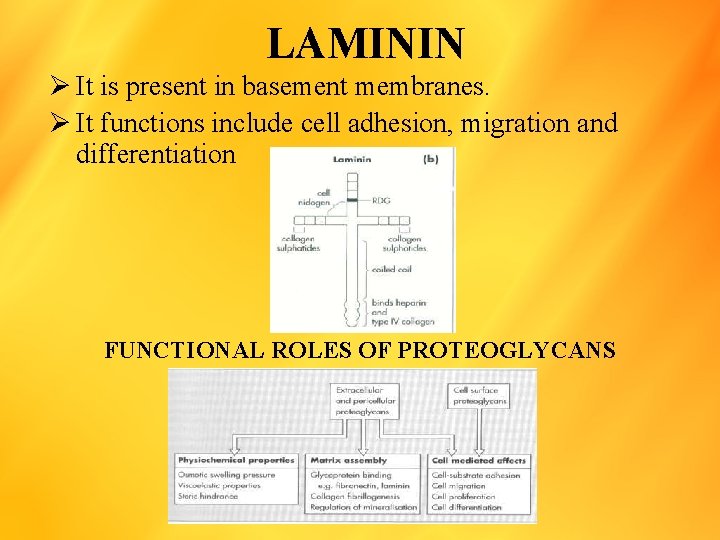
LAMININ Ø It is present in basement membranes. Ø It functions include cell adhesion, migration and differentiation FUNCTIONAL ROLES OF PROTEOGLYCANS
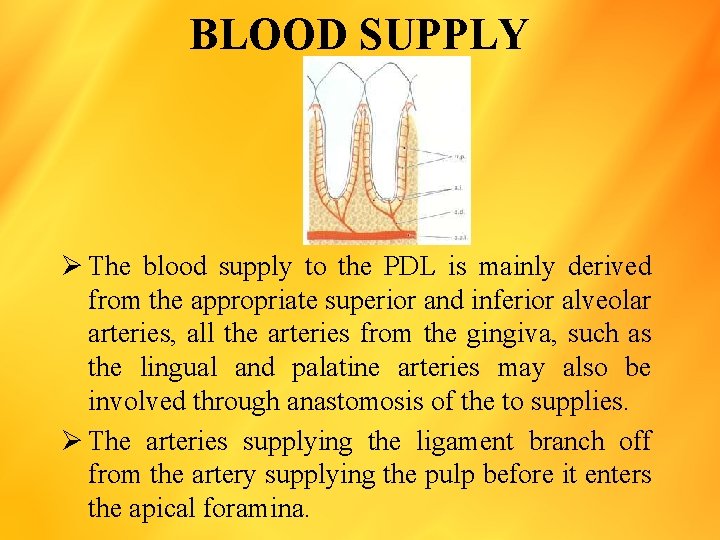
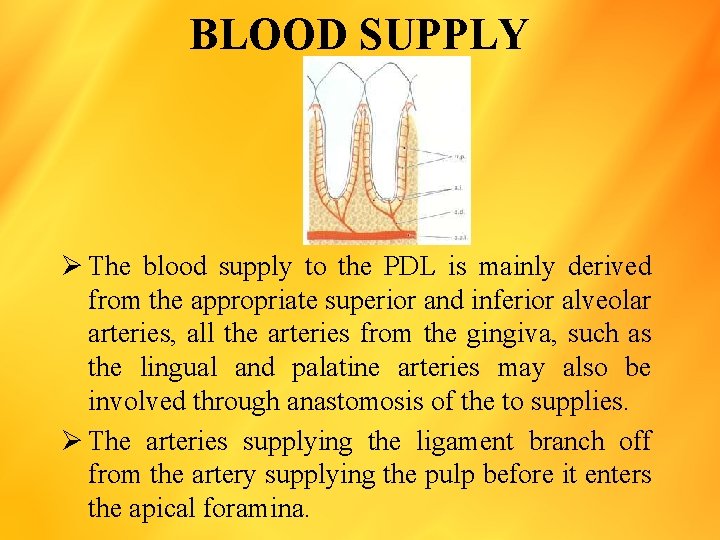
BLOOD SUPPLY Ø The blood supply to the PDL is mainly derived from the appropriate superior and inferior alveolar arteries, all the arteries from the gingiva, such as the lingual and palatine arteries may also be involved through anastomosis of the to supplies. Ø The arteries supplying the ligament branch off from the artery supplying the pulp before it enters the apical foramina.
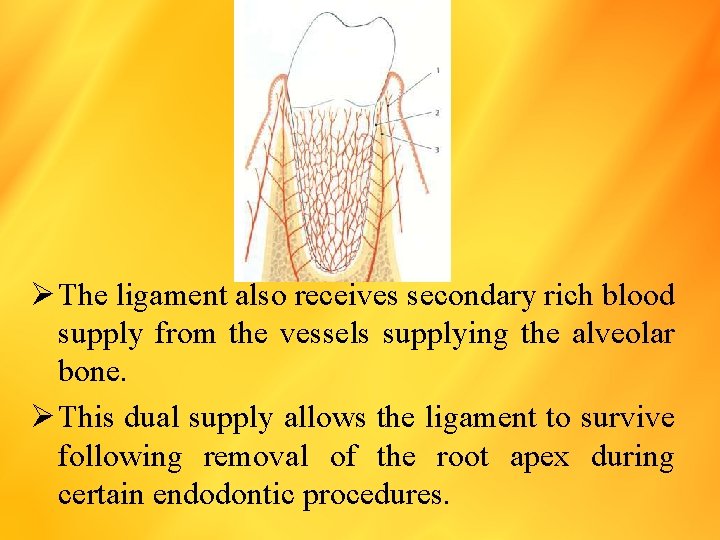
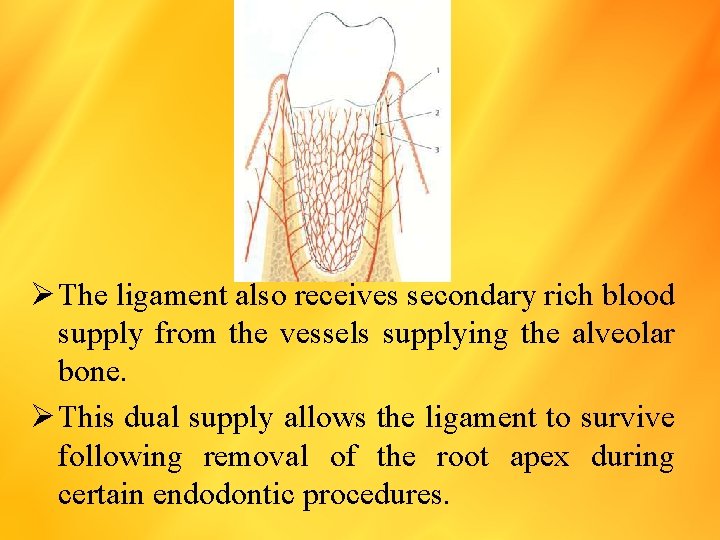
Ø The ligament also receives secondary rich blood supply from the vessels supplying the alveolar bone. Ø This dual supply allows the ligament to survive following removal of the root apex during certain endodontic procedures.
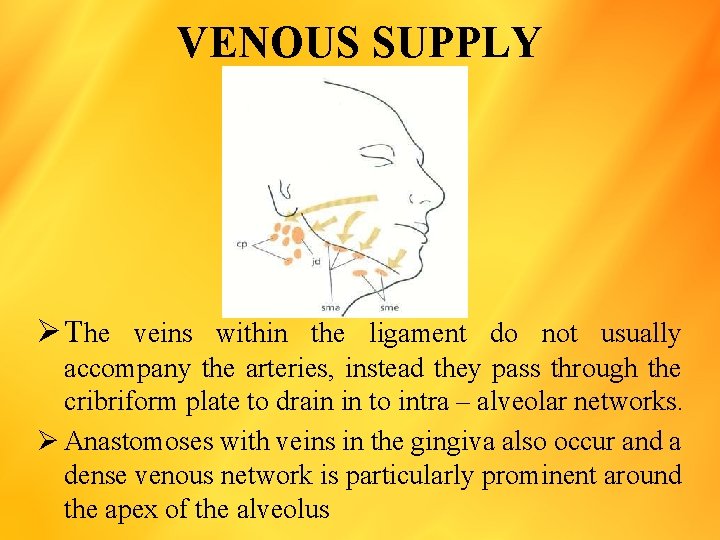
VENOUS SUPPLY Ø The veins within the ligament do not usually accompany the arteries, instead they pass through the cribriform plate to drain in to intra – alveolar networks. Ø Anastomoses with veins in the gingiva also occur and a dense venous network is particularly prominent around the apex of the alveolus
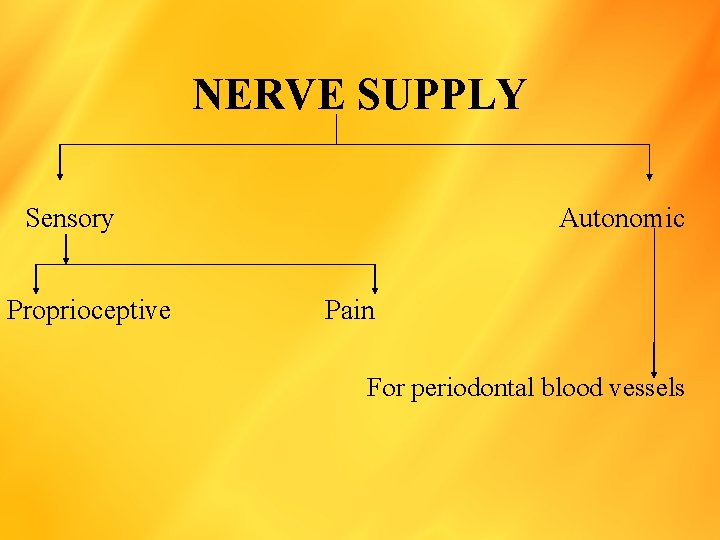
NERVE SUPPLY Sensory Proprioceptive Autonomic Pain For periodontal blood vessels
Ø Nerve bundles from the trigeminal nerve follow the blood vessels and are derived from two sources Ø Some nerve bundles branch off nerve supplying the pulp before it enters the apical foramen and supply the ligament directly. Ø Others enter the medial and cervical position of the ligament from the nerve supply to the alveolar bone, and enter the ligament as finer branches through the multiple foramina in the cribriform plate.
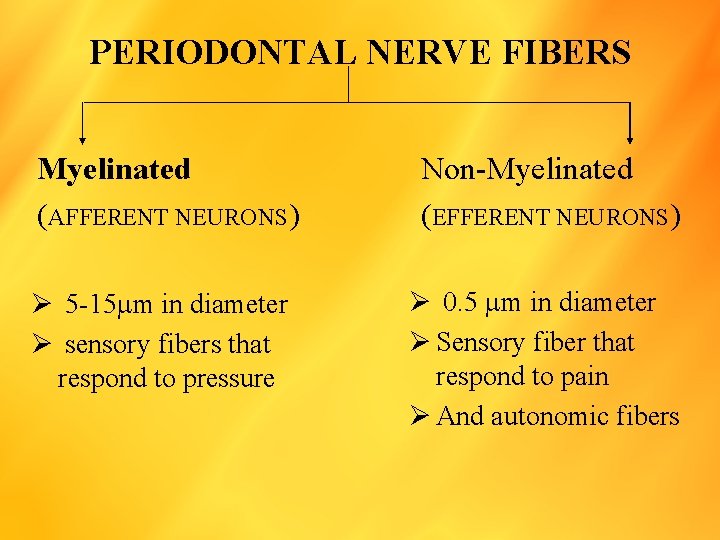
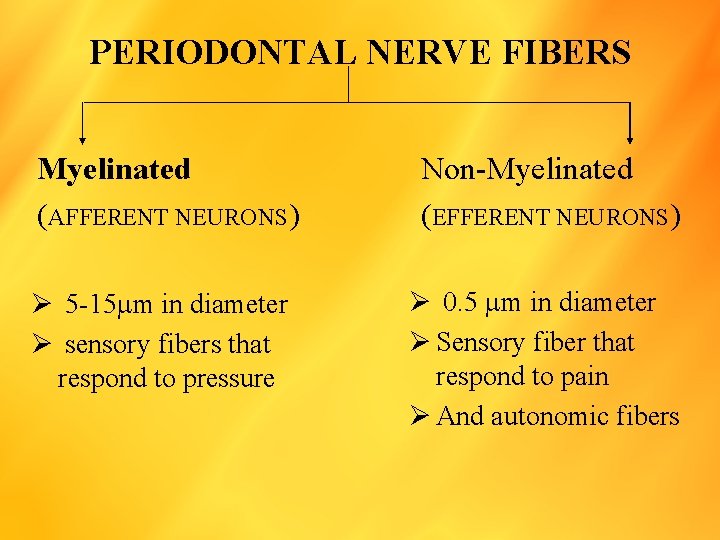
PERIODONTAL NERVE FIBERS Myelinated (AFFERENT NEURONS) Ø 5 -15 m in diameter Ø sensory fibers that respond to pressure Non-Myelinated (EFFERENT NEURONS) Ø 0. 5 m in diameter Ø Sensory fiber that respond to pain Ø And autonomic fibers
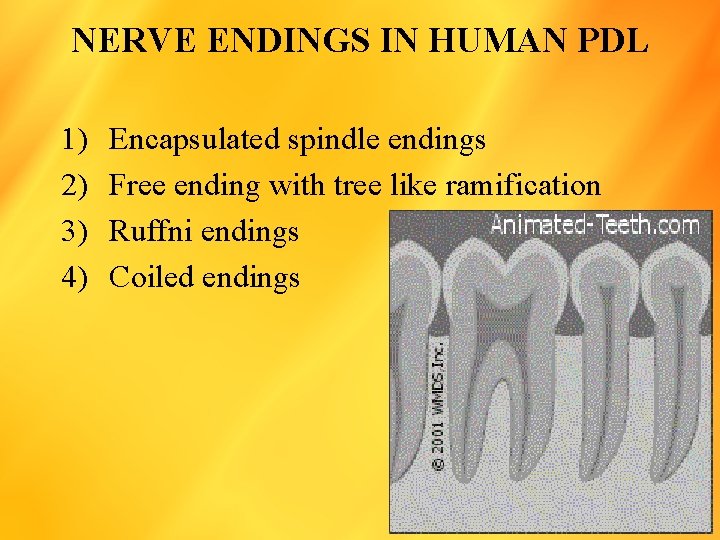
NERVE ENDINGS IN HUMAN PDL 1) 2) 3) 4) Encapsulated spindle endings Free ending with tree like ramification Ruffni endings Coiled endings
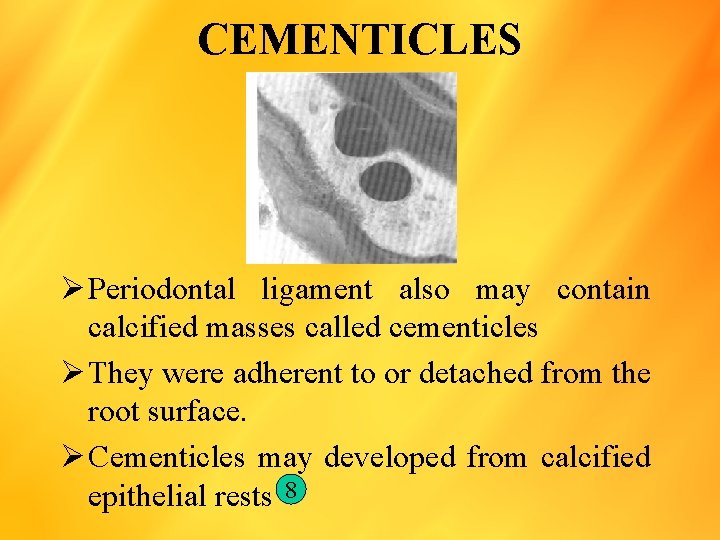
CEMENTICLES Ø Periodontal ligament also may contain calcified masses called cementicles Ø They were adherent to or detached from the root surface. Ø Cementicles may developed from calcified epithelial rests 8
AGE CHANGES IN PDL Ø With aging the changes that occur in the PDL include decreased numbers of fibroblasts, decreased organic matrix production and epithelial cell rests. Ø The structure of the PDL becomes more irregular. Ø There is an increased amount of elastic fiber AGE CHANGES IN FIBRES Ø With age there is an increased collagen fibrosis and the fiber bundles become thicker. Ø Areas of hyalinization and sporadic mineralization of fibers are also seen.
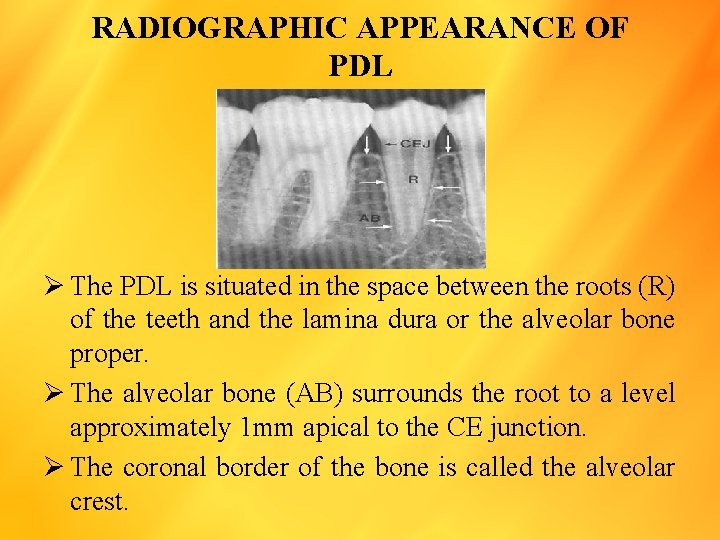
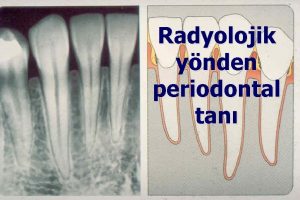
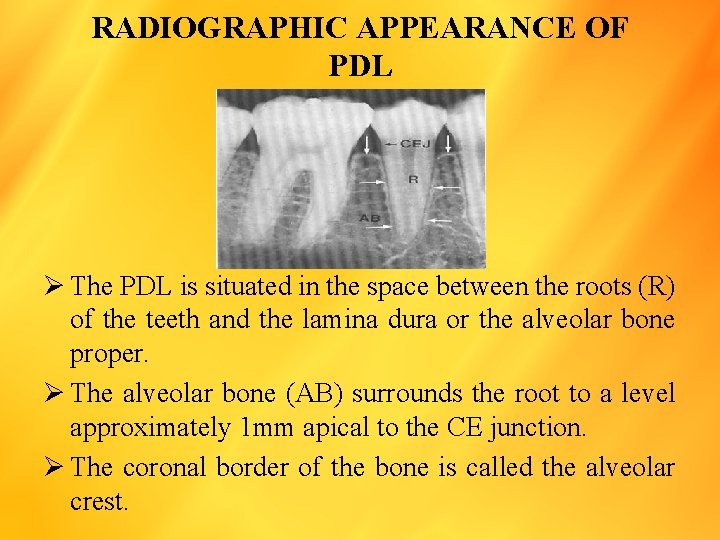
RADIOGRAPHIC APPEARANCE OF PDL Ø The PDL is situated in the space between the roots (R) of the teeth and the lamina dura or the alveolar bone proper. Ø The alveolar bone (AB) surrounds the root to a level approximately 1 mm apical to the CE junction. Ø The coronal border of the bone is called the alveolar crest.
FUNCTIONS OF PDL 1) 2) 3) 4) 5) Physical Formative Remodeling Nutritional Sensory
PHYSICAL FUNCTION 1. Provision of a soft tissue “Casting” to protect the vessels and nerves from injury by mechanical forces 2. Transmission of occlusal forces to the bone 3. Attachment of the teeth to the bone 4. Maintenance of the gingival tissues in their proper relationship to the teeth. 5. Resistance to the impact of occlusal forces (shock absorption)
RESISTANCE TO THE IMPACT OF OCCLUSAL FORCES (Shock absorption) Theories 3 have been proposed to describe the mechanism of tooth support A. TENSIONAL THEORY The tensional theory of tooth support ascribes to the principal fibres of the periodontal ligament. The major responsibility in supporting the tooth and transmitting forces to the bone.
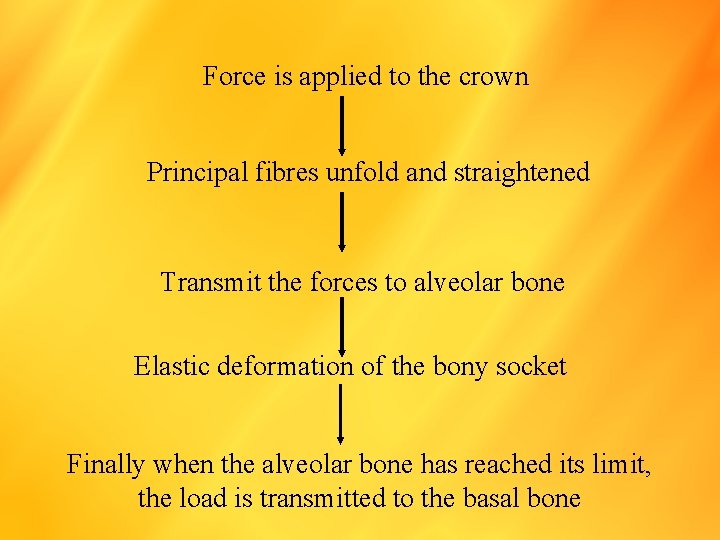
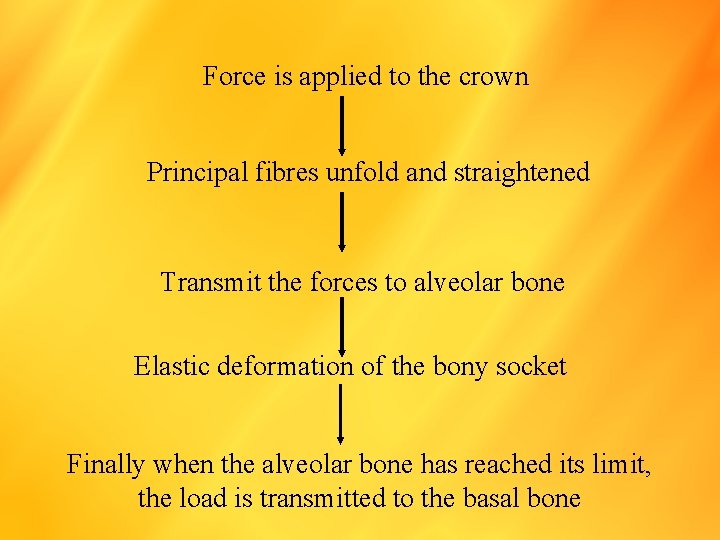
Force is applied to the crown Principal fibres unfold and straightened Transmit the forces to alveolar bone Elastic deformation of the bony socket Finally when the alveolar bone has reached its limit, the load is transmitted to the basal bone
B. VISCOELASTIC THEORY Ø It considers the displacement of the tooth to be largely controlled by fluid movements, with fibres having only a secondary role. Ø When forces are transmitted to the tooth, the extra cellular fluid passes from the periodontal ligament into the marrow spaces of bone through foramina in the cribriformplate Ø After depletion tissue fluids, the fiber bundles absorb the slack and tighten. Ø This leads to blood vessel stenosis Ø Arterial back pressure causes ballooning of the vessels, and passage of blood ultra filtrates into the tissues, there by replacing the tissue fluids. 10
C. THIXOTROPIC THEORY Ø Describes the PDL to behave like a thixotropic material is 1 which can undergo a gel/sol/gel transformation. Ø This theory considers the PDL to be a collagenous thixotropic gel and that fibres are only artifacts. Ø It is not been accepted
TRANSMISSION OF OCCLUSAL FORCES TO THE BONE Ø The arrangement of the principal fibres is similar to a suspension bridge or hammock. WHEN A HORIZONTAL OR TIPPLING FORCES IS APPLIED Ø Two phases of tooth movement occur 1 st with in the confines of the periodontal ligament 2 nd produces a displacement of facial and lingual bony plates 11 Ø In single rooted teeth the axis of rotation is located in the area between the apical third and the middle third of the root. Ø In multirooted teeth, the axis of rotation is located in the bone between the roots
FORMATIVE AND REMODELING FUNCTION Ø The PDL is constantly under going remodeling. Ø Old cells and fibers are broken down and replaced by new ones, and mitotic activity can be observed in the fibroblast and endothelial cells Ø Fibroblast form the collagen fibres, and the residual mesenchymal cells develop into osteoblasts and cementoblasts Ø Variation in cellular enzyme activate are corelated with a remodeling process 12 13
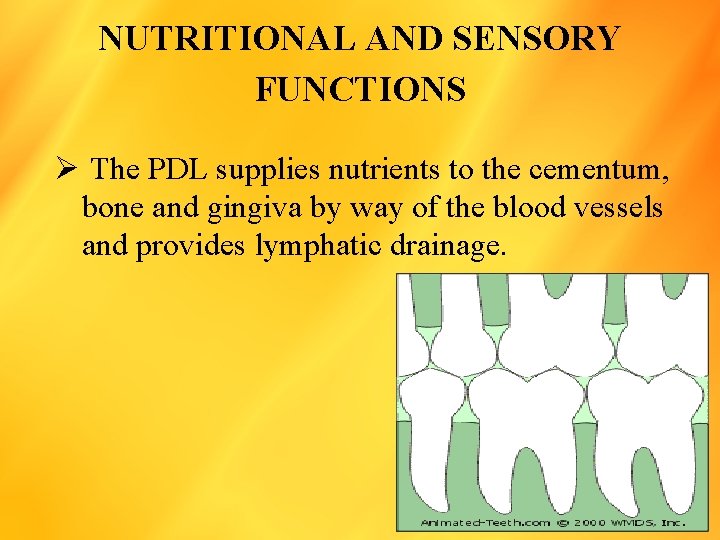
NUTRITIONAL AND SENSORY FUNCTIONS Ø The PDL supplies nutrients to the cementum, bone and gingiva by way of the blood vessels and provides lymphatic drainage.
CONCLUSION The PDL is a specialized and unique structure in the human body. The existence of the thixotropic theory by it self suggests that there is no consensus on the exact nature of the PDL. This provides room to conduct more research to understand is unique and dynamic tissue. The PDL as excellent regenerative potential and further research is required to completely understand regenerative procedures and apply it in a clinical setting.
BIBLIOGRAPHY 1. Romaniuk K: some observations of the fine structure of human cementum. J Dent Res 1967: 46: 152. 2. Romanos GE et al. Basis – element des parodonts: Immuno histo cemische, Parodontologie 1991: 1: 47. 3. Romanos GE et al. Immunehistochemical distribution of collagen types IV, V and VI and Glycoprotein lamin in the healthy rat and human gingiva. Matrix: 1991: 125 4. Carranza FA et al : a study of periodontal vascularization in different laboratory animals. J Periodont Res: 1966: 1: 120 5. Gilles pine B R et al. they relationship between the mobility of human teeth and there supra crestal fiber support. J Periodontal 1979: 50: 120. 6. Fullmer H M et al. oxytalan connective tissue fibres: a review: J Oral pathol 1974: 3: 291 7. Freeman E et al. the periodontium. In: Tencat R (ed) Oral histology, ed four st Louis, Mosloy 1994
8. Mikola O J et al: cementicals and fragments of cementum in the periodotnal membrane. Oral surg 1949: 2: 1063 9. Romaniuk K : some observations of the fine structure of human cementum. J Dent Res 1967: 46: 152 10. Bien SM et al: Hydrodynamic Danping of tooth movement. J dent Res 1966: 45: 907 11. Davies W I et al: dimensional changes in the periodontal membrane of monkey’s teeth with horizontal thrusts. J Dent Res 1967: 46: 114 12. Gibson W et al: histochemistry of the Periodotal ligament. Periodontics 1966: 4: 63 13. Gibson W et al: histochemistry of the Periodotal ligament. The Esterases, Periodontics 1968: 6: 71.
14. Clinical Periodontology by Carranza 9 th Edition 15. Clinical periodontology and implant Dentistry by Jan Lindhe 4 th Edition 16. Periodontal ligament health and diseases by Berkovitz 2 nd Edition 17. Oral histology by AR Tencate 4 th Edition
By SUJAI
 Periodontium definition
Periodontium definition Periodontium definition
Periodontium definition Dişin embriyolojik gelişim evreleri
Dişin embriyolojik gelişim evreleri Periodontal ligament injection definition
Periodontal ligament injection definition Periodontal ligament
Periodontal ligament Vertical
Vertical Well defined set example
Well defined set example Softrock ensemble ii rx
Softrock ensemble ii rx Classification of periodontal instruments
Classification of periodontal instruments Periodontal therapy in female patients
Periodontal therapy in female patients Politür patı
Politür patı Plaque index
Plaque index Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Russell periodontal index
Russell periodontal index Ligamento periodontal
Ligamento periodontal Modified widman flap
Modified widman flap Enap periodontal adalah
Enap periodontal adalah Rationale of periodontal treatment
Rationale of periodontal treatment Gingival lifler
Gingival lifler Espacio indiferenciado de black
Espacio indiferenciado de black Periodontal response to external forces
Periodontal response to external forces Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Nug tedavisi
Nug tedavisi Ligamento periodontal ensanchado
Ligamento periodontal ensanchado Heliprobe 2 positivo
Heliprobe 2 positivo Diagnosis of periodontal disease
Diagnosis of periodontal disease Aot cyst
Aot cyst Periapical granuloma vs abscess
Periapical granuloma vs abscess Periodontal abscess
Periodontal abscess Periodontal disease
Periodontal disease Kista primordial
Kista primordial Periodontal charting symbols
Periodontal charting symbols Gtr indications
Gtr indications General principles of periodontal surgery
General principles of periodontal surgery Grupos de fibras del ligamento periodontal
Grupos de fibras del ligamento periodontal Undisplaced flap procedure
Undisplaced flap procedure Ligamento periodontal
Ligamento periodontal Who sondu nedir
Who sondu nedir Periodontal cep
Periodontal cep Periodontal case study
Periodontal case study Microtopography of gingival wall
Microtopography of gingival wall Periodontal tendonitis
Periodontal tendonitis Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy Body paragraph
Body paragraph Culdocentesis
Culdocentesis Hip synovial joint
Hip synovial joint Spinal cord denticulate ligament
Spinal cord denticulate ligament Stomach ligaments
Stomach ligaments Ligament of treitz
Ligament of treitz Laryngeal surface of epiglottis
Laryngeal surface of epiglottis Branches of popliteal artery
Branches of popliteal artery Treitz ligament
Treitz ligament Ductus choleodochus
Ductus choleodochus Ascedens
Ascedens Duodenojejunostomy
Duodenojejunostomy Transverse metatarsal ligament
Transverse metatarsal ligament Articulating bones at shoulder joint
Articulating bones at shoulder joint Ligament fibulo poplité
Ligament fibulo poplité Transverse perineal muscle female
Transverse perineal muscle female Nerve supply of spleen
Nerve supply of spleen Porta hepatis
Porta hepatis Liver ligaments
Liver ligaments Sacrospinous ligament
Sacrospinous ligament Ligament de cooper coude
Ligament de cooper coude Transverse genicular ligament
Transverse genicular ligament Ligament falciforme du foie
Ligament falciforme du foie