Superior mesenteric artery syndrome SMA syndrome Joint hospital
- Slides: 44
Superior mesenteric artery syndrome (SMA syndrome) Joint hospital surgical grandround 19/7/2014 Cheung Hing Fong
1. 2. 3. 4. 5. 6. 7. 8. Case presentation Pathophysiology Predisposing conditions Presentation Epidemiology Diagnosis and imaging finding Treatment Summary
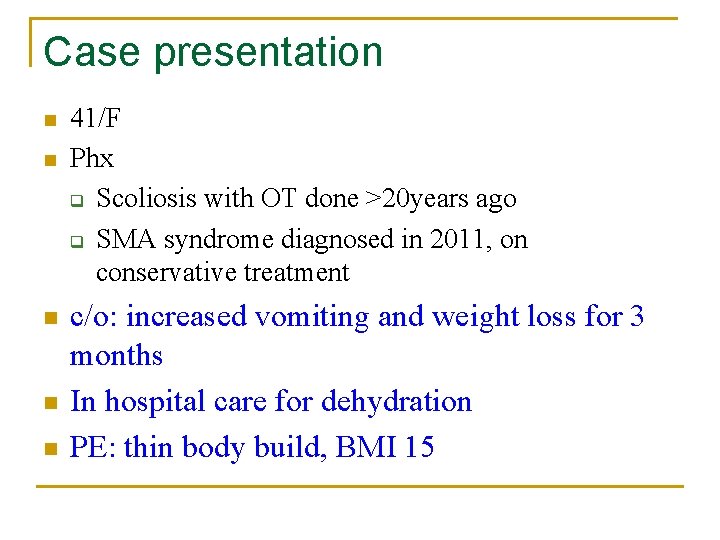
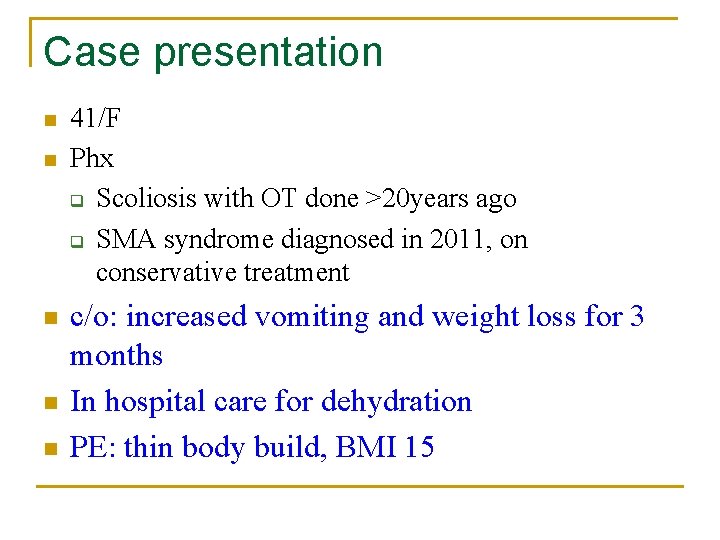
Case presentation n n 41/F Phx q Scoliosis with OT done >20 years ago q SMA syndrome diagnosed in 2011, on conservative treatment c/o: increased vomiting and weight loss for 3 months In hospital care for dehydration PE: thin body build, BMI 15
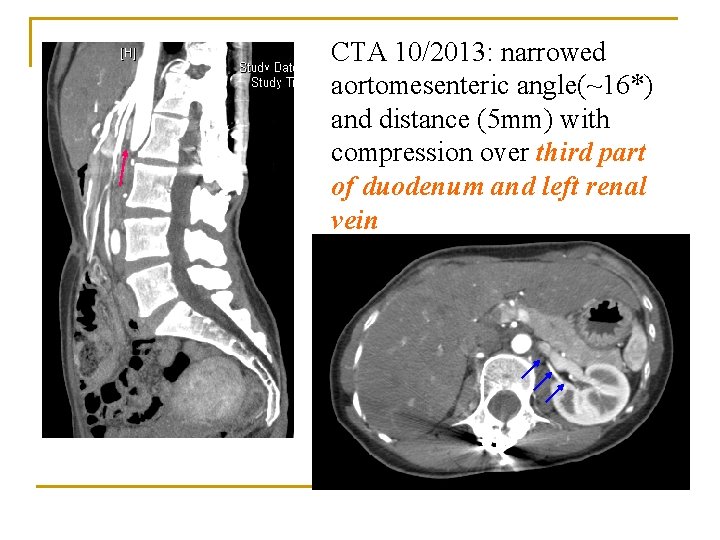
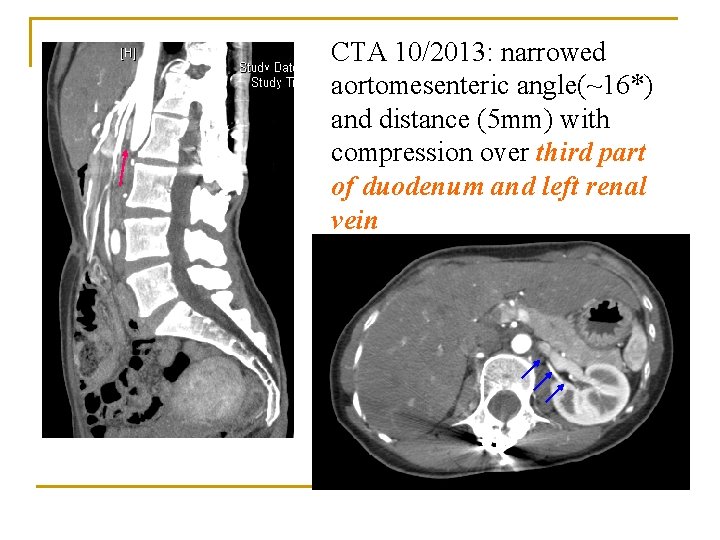
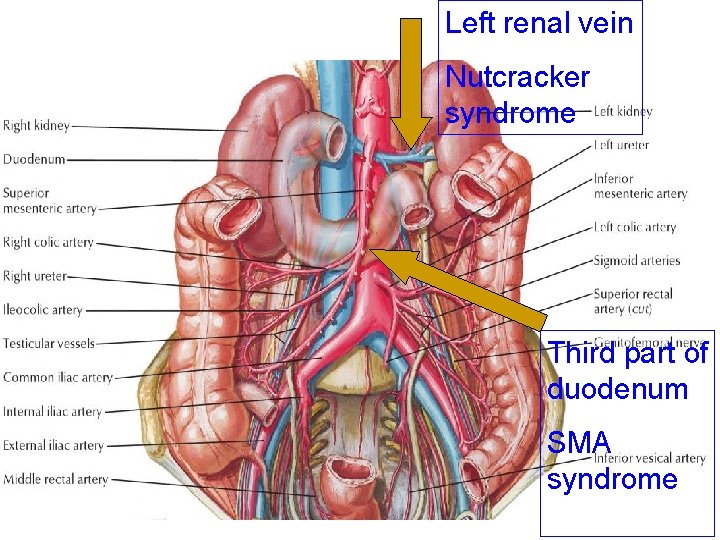
CTA 10/2013: narrowed aortomesenteric angle(~16*) and distance (5 mm) with compression over third part of duodenum and left renal vein
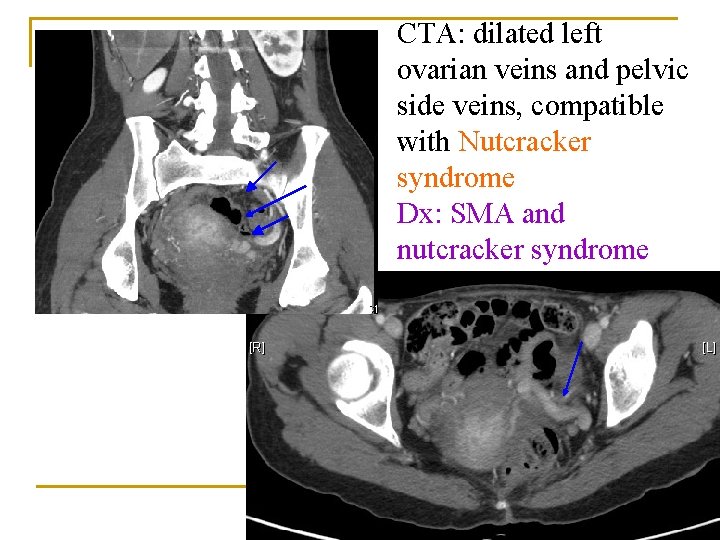
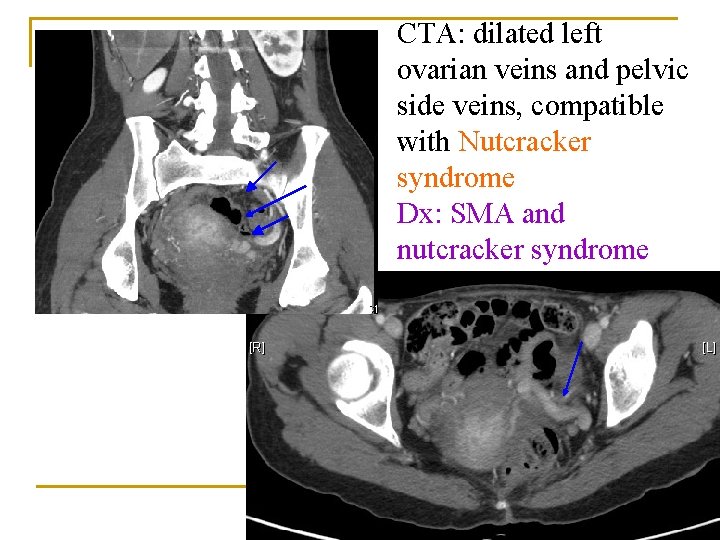
CTA: dilated left ovarian veins and pelvic side veins, compatible with Nutcracker syndrome Dx: SMA and nutcracker syndrome
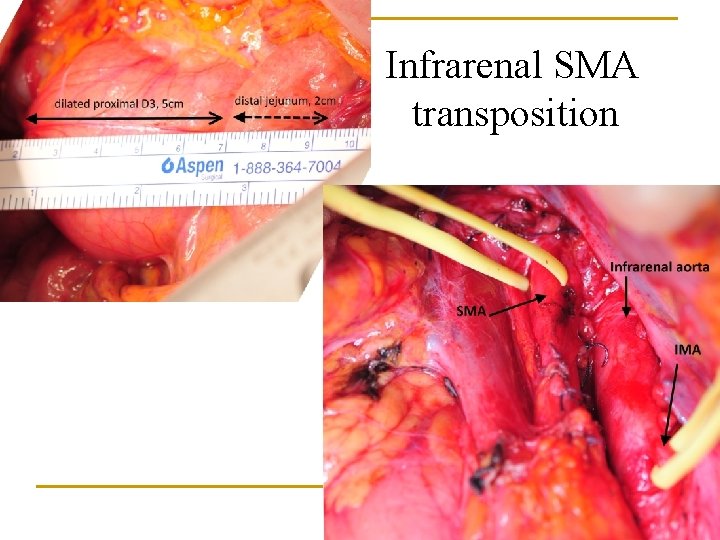
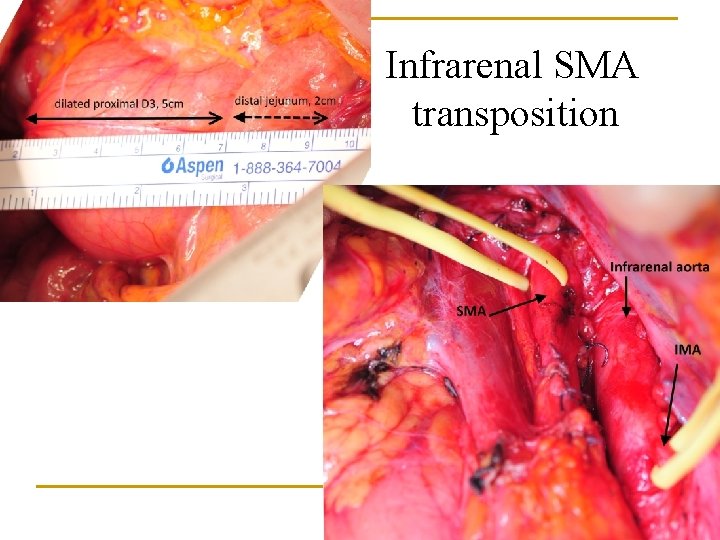
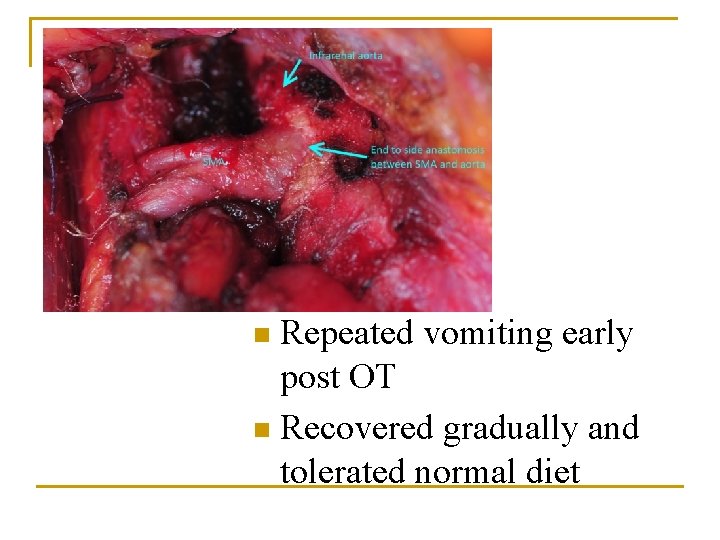
Infrarenal SMA transposition
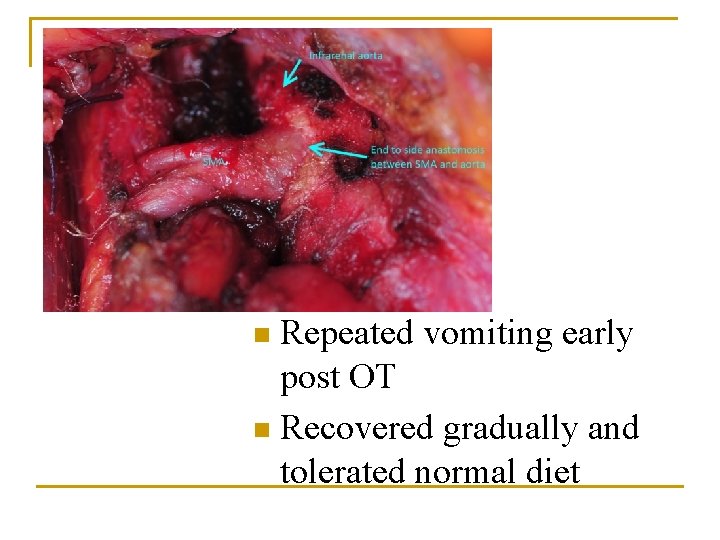
Repeated vomiting early post OT n Recovered gradually and tolerated normal diet n
1. 2. 3. 4. 5. 6. 7. 8. Case presentation Pathophysiology Predisposing conditions Presentation Epidemiology Diagnosis and imaging finding Treatment Summary
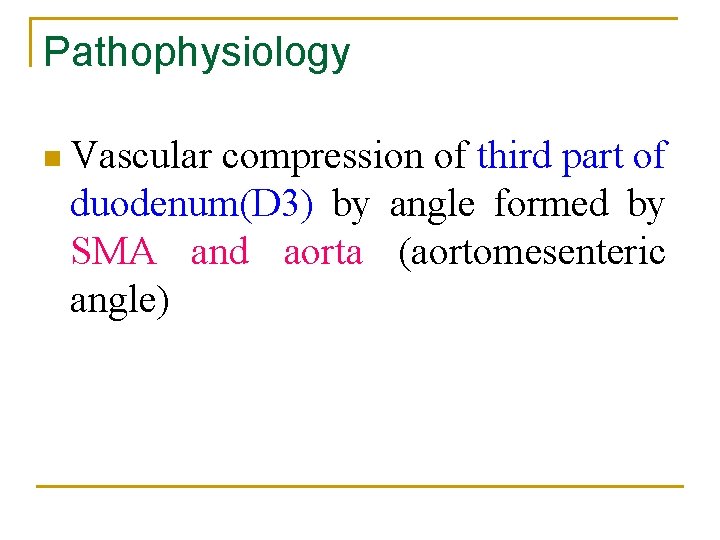
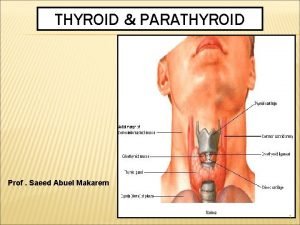
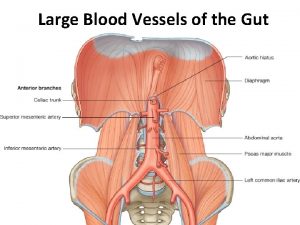
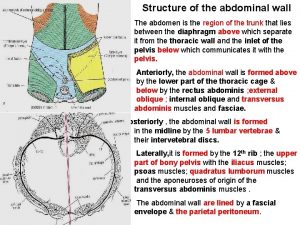
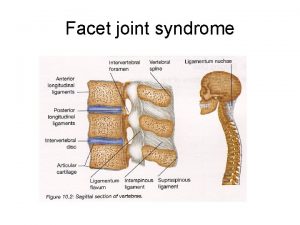
Pathophysiology n Vascular compression of third part of duodenum(D 3) by angle formed by SMA and aorta (aortomesenteric angle)
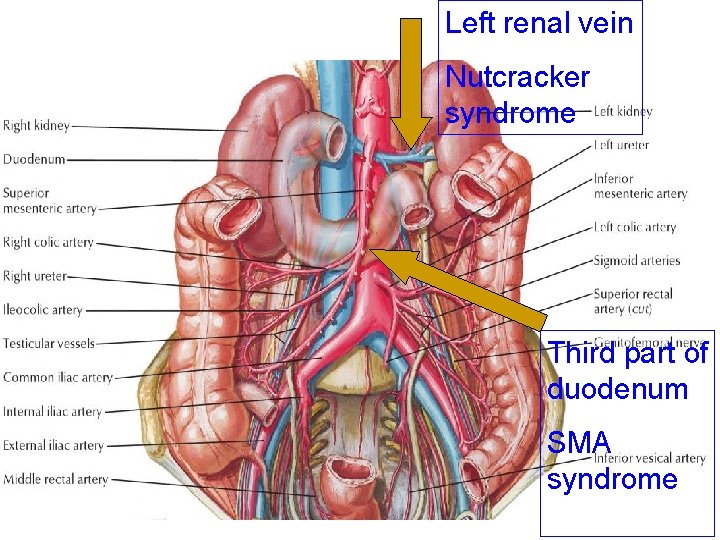
Left renal vein Nutcracker syndrome Third part of duodenum SMA syndrome
1. 2. 3. 4. 5. 6. 7. 8. Case presentation Pathophysiology Predisposing conditions Presentation Epidemiology Diagnosis and imaging finding Treatment Summary
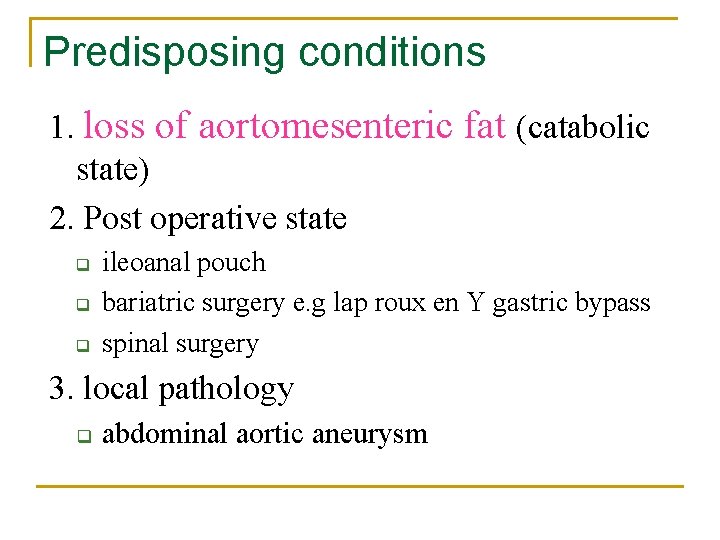
Predisposing conditions 1. loss of aortomesenteric fat (catabolic state) 2. Post operative state q q q ileoanal pouch bariatric surgery e. g lap roux en Y gastric bypass spinal surgery 3. local pathology q abdominal aortic aneurysm
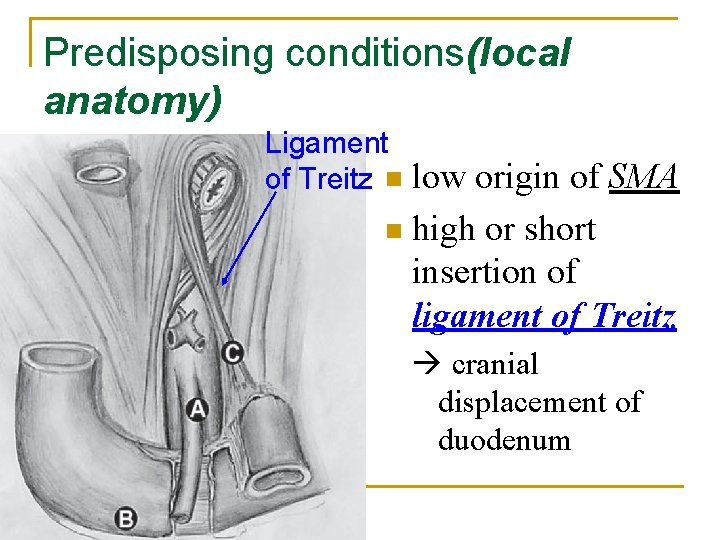
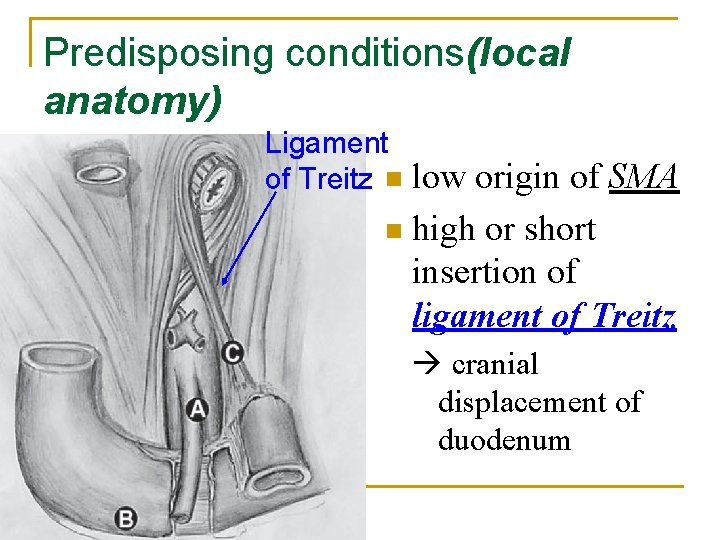
Predisposing conditions(local anatomy) Ligament of Treitz n low origin of SMA n high or short insertion of ligament of Treitz cranial displacement of duodenum
1. 2. 3. 4. 5. 6. 7. 8. Case presentation Pathophysiology Predisposing conditions Presentation Epidemiology Diagnosis and imaging finding Treatment Summary
Patient presentation Post-prandial epigastric pain then bilious vomiting n with prone/ knee chest/ left lateral position n n Food fear weight loss and anorexia
n Diagnosis is usually delayed Rare disease Diseases with similar presentation n n anorexia duodenal/ pancreatic tumour irritable bowel syndrome megaduodenum
1. 2. 3. 4. 5. 6. 7. 8. Case presentation Pathophysiology Predisposing conditions Presentation Epidemiology Diagnosis and imaging finding Management Summary
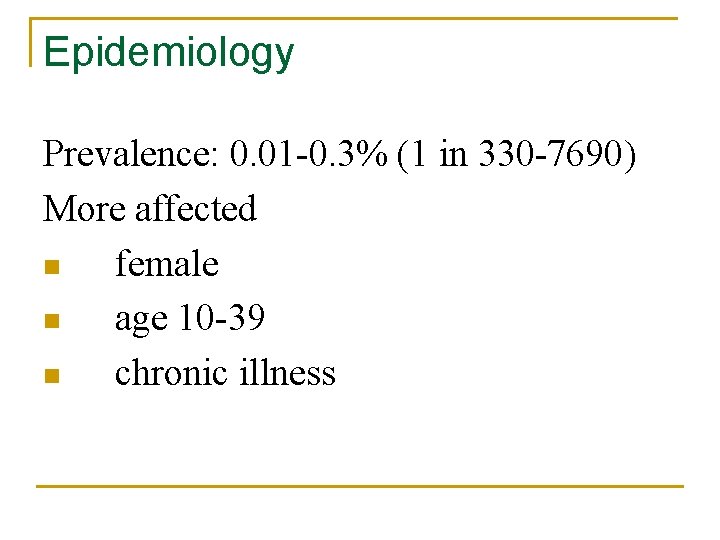
Epidemiology Prevalence: 0. 01 -0. 3% (1 in 330 -7690) More affected n female n age 10 -39 n chronic illness
1. 2. 3. 4. 5. 6. 7. 8. Case presentation Pathophysiology Predisposing conditions Presentation Epidemiology Diagnosis and imaging finding Treatment Summary
Investigations n Barium study n CT angiogram (abdomen) n Upper endoscopy+/- EUS
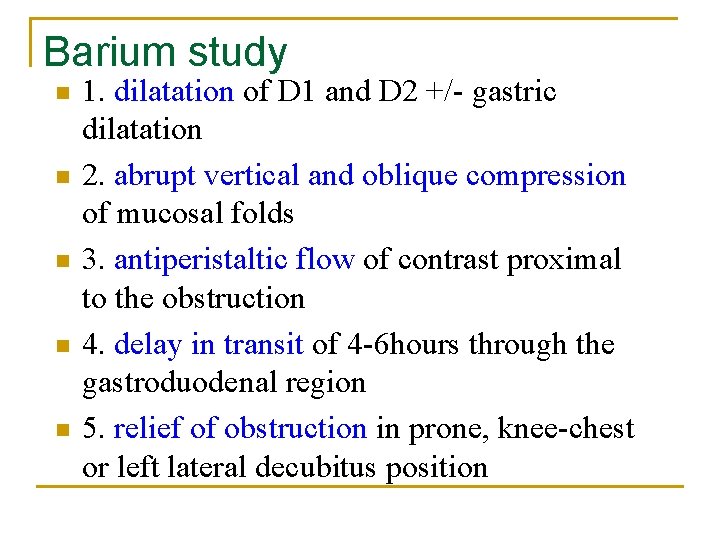
Barium study n n n 1. dilatation of D 1 and D 2 +/- gastric dilatation 2. abrupt vertical and oblique compression of mucosal folds 3. antiperistaltic flow of contrast proximal to the obstruction 4. delay in transit of 4 -6 hours through the gastroduodenal region 5. relief of obstruction in prone, knee-chest or left lateral decubitus position
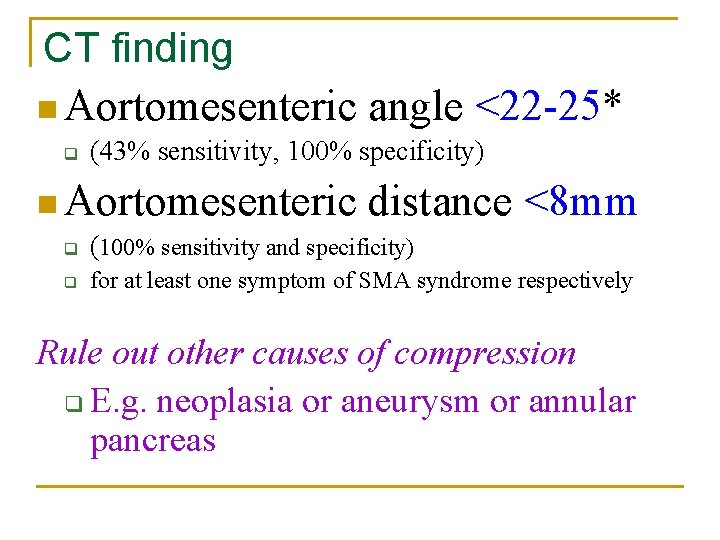
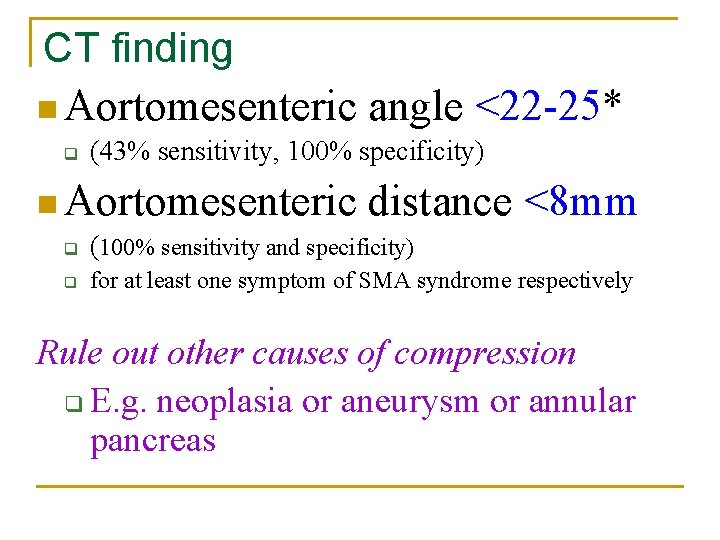
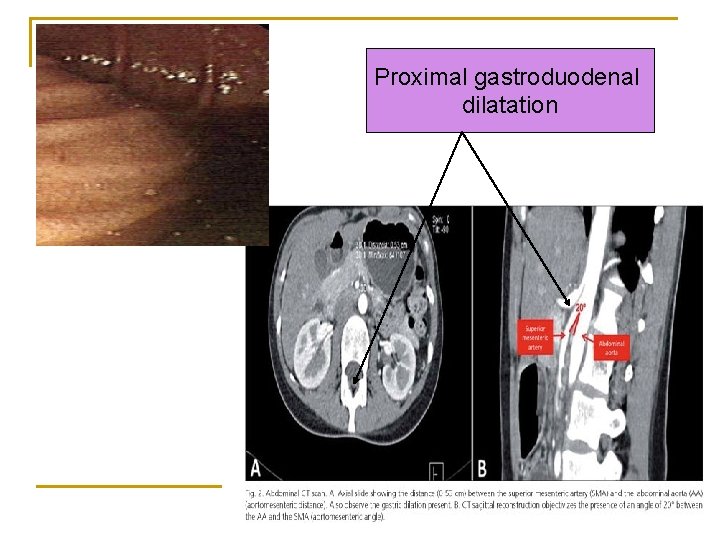
CT finding n Aortomesenteric angle <22 -25* q (43% sensitivity, 100% specificity) n Aortomesenteric distance q (100% sensitivity and specificity) q <8 mm for at least one symptom of SMA syndrome respectively Rule out other causes of compression q E. g. neoplasia or aneurysm or annular pancreas
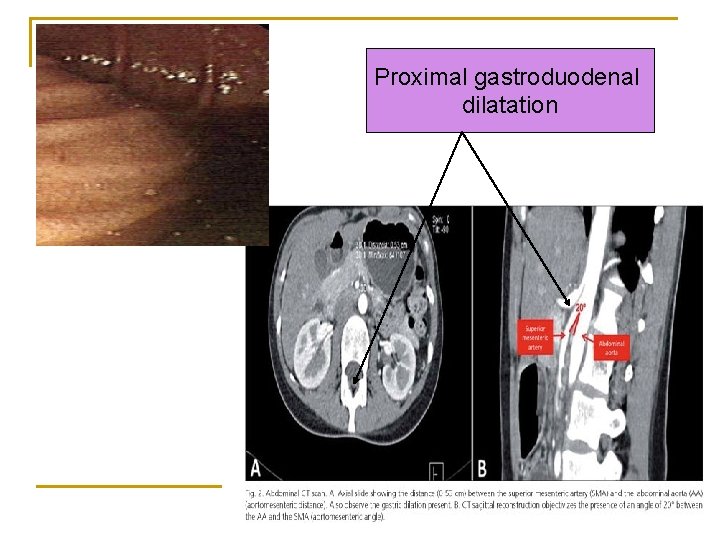
Proximal gastroduodenal dilatation
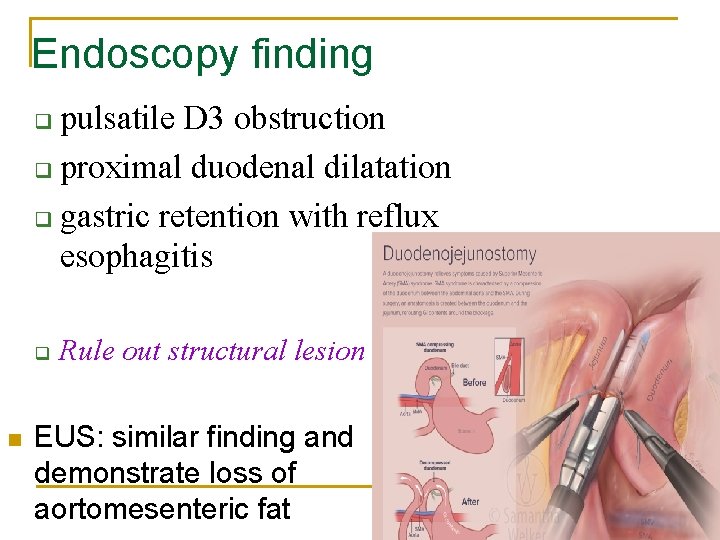
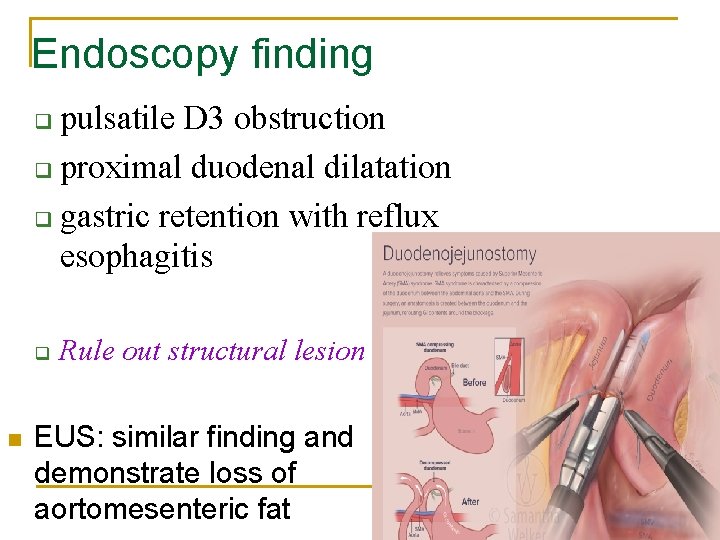
Endoscopy finding pulsatile D 3 obstruction q proximal duodenal dilatation q gastric retention with reflux esophagitis q q n Rule out structural lesion EUS: similar finding and demonstrate loss of aortomesenteric fat
1. 2. 3. 4. 5. 6. 7. 8. Case presentation Pathophysiology Predisposing conditions Presentation Epidemiology Diagnosis and imaging finding Treatment Summary
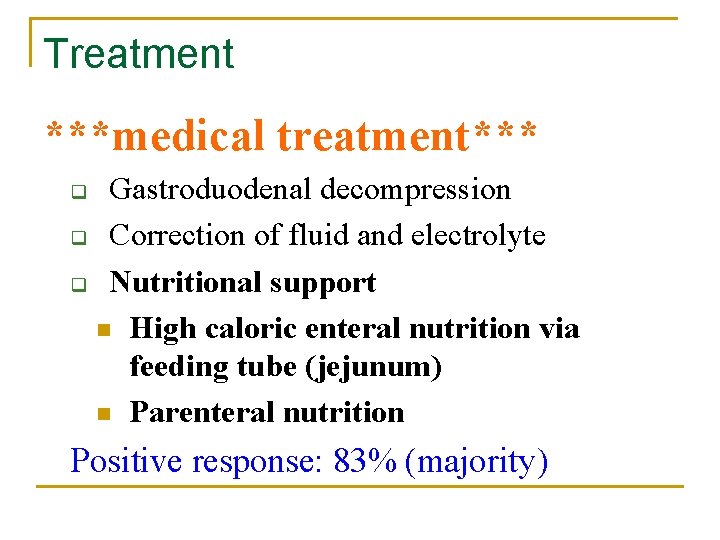
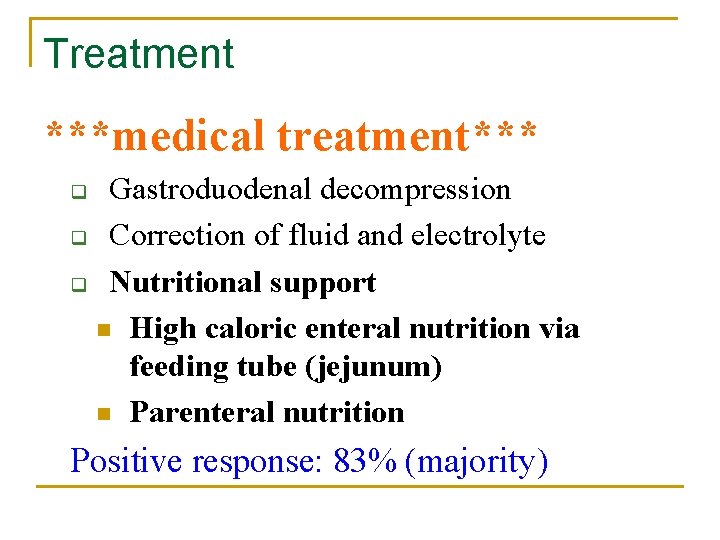
Treatment ***medical treatment*** Gastroduodenal decompression q Correction of fluid and electrolyte q Nutritional support n High caloric enteral nutrition via feeding tube (jejunum) n Parenteral nutrition q Positive response: 83% (majority)
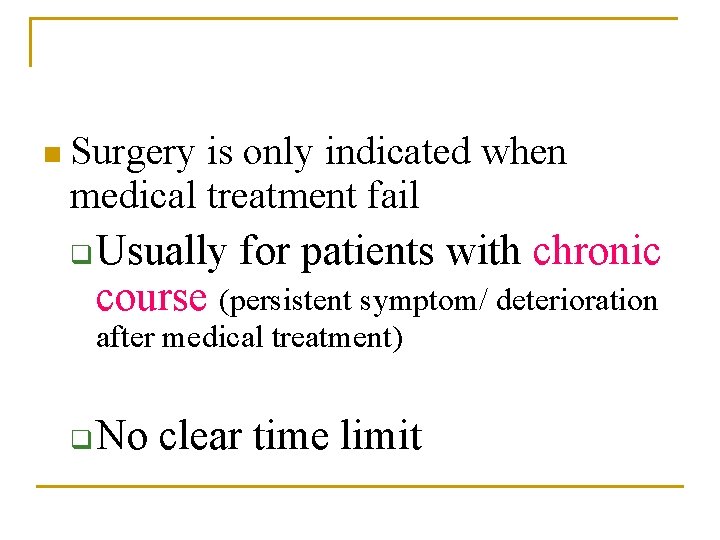
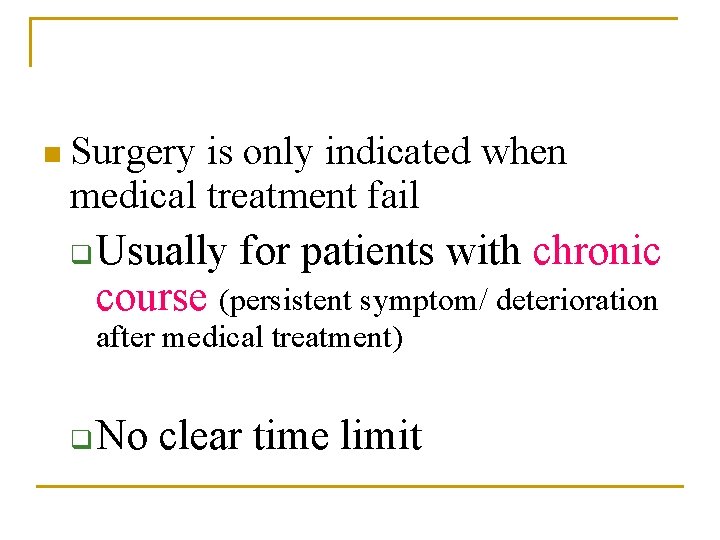
n Surgery is only indicated when medical treatment fail q Usually for patients with chronic course (persistent symptom/ deterioration after medical treatment) q No clear time limit
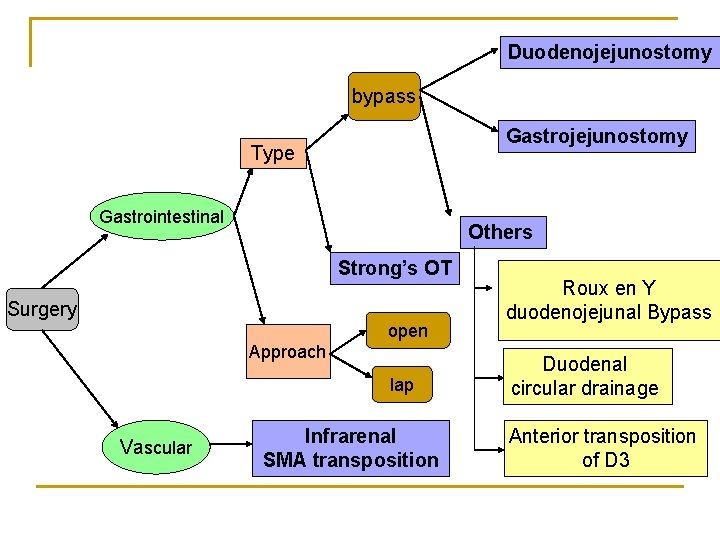
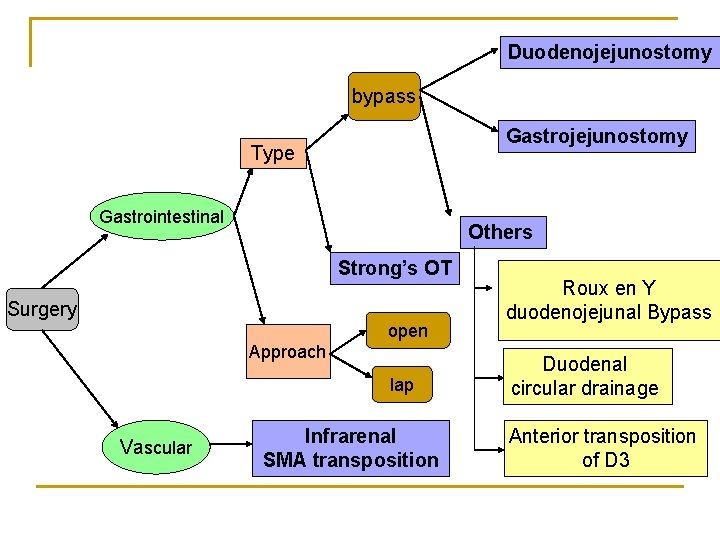
Duodenojejunostomy bypass Gastrojejunostomy Type Gastrointestinal Others Strong’s OT Surgery open Approach lap Vascular Infrarenal SMA transposition Roux en Y duodenojejunal Bypass Duodenal circular drainage Anterior transposition of D 3
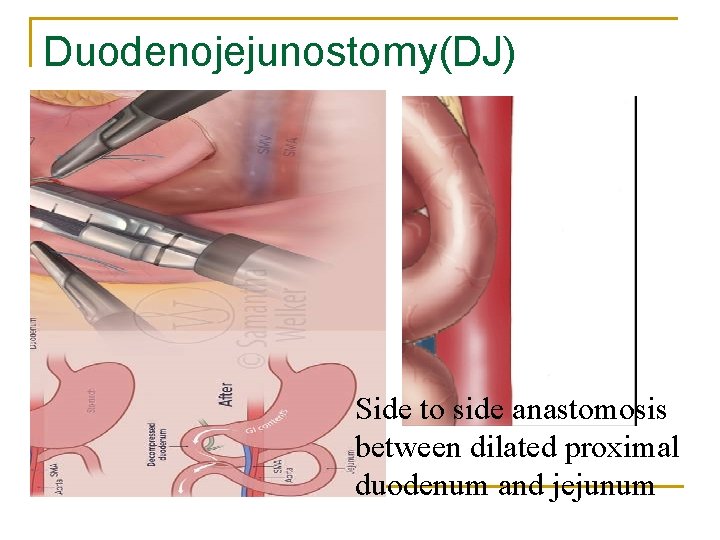
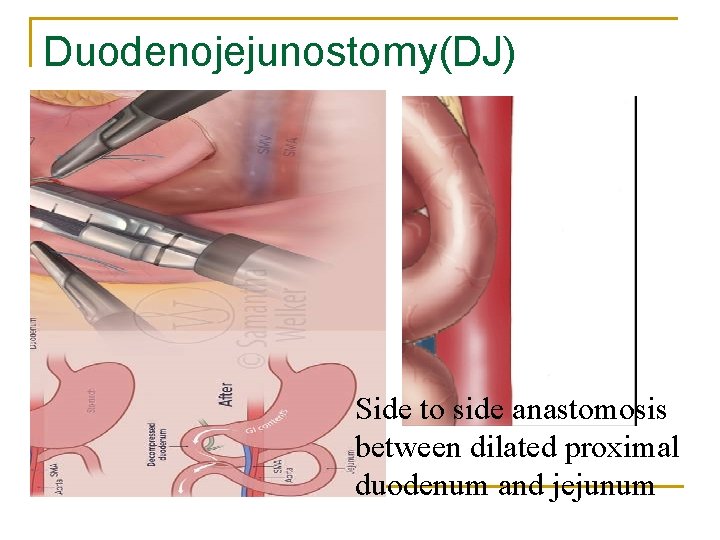
Duodenojejunostomy(DJ) Side to side anastomosis between dilated proximal duodenum and jejunum
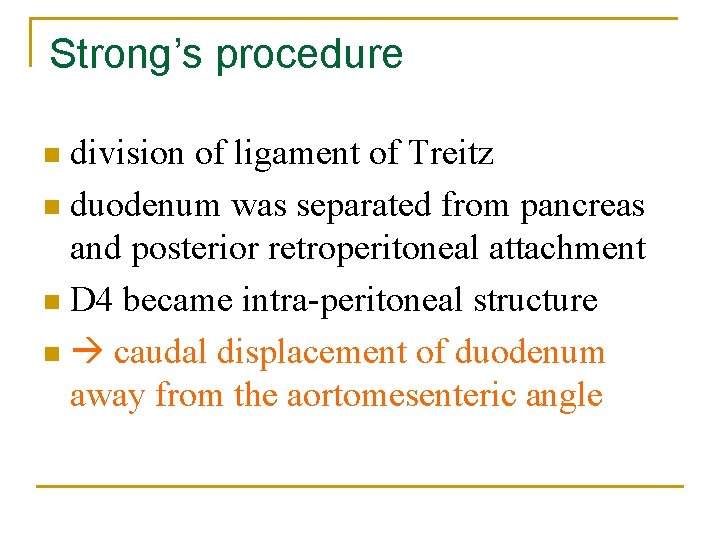
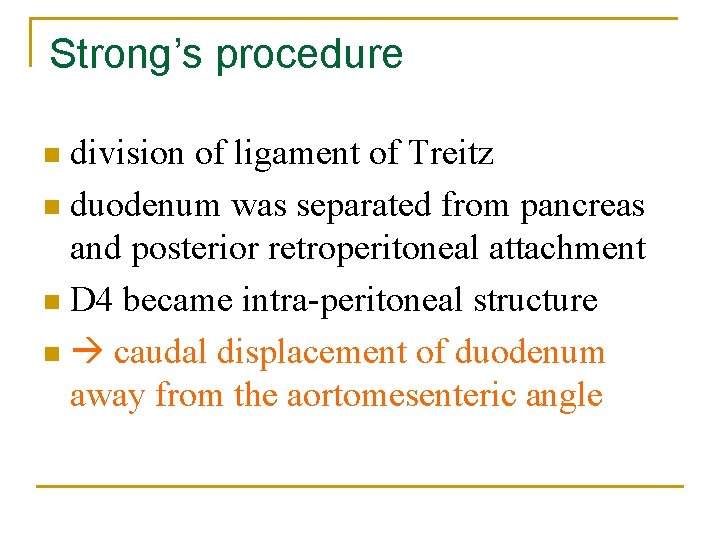
Strong’s procedure division of ligament of Treitz n duodenum was separated from pancreas and posterior retroperitoneal attachment n D 4 became intra-peritoneal structure n caudal displacement of duodenum away from the aortomesenteric angle n
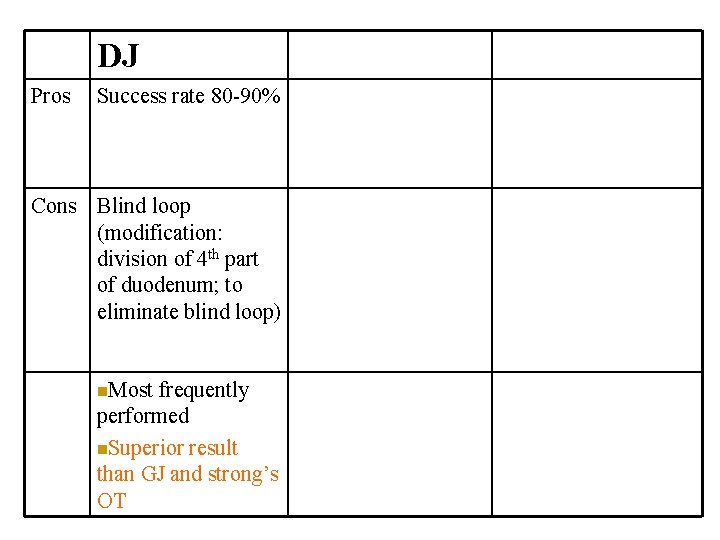
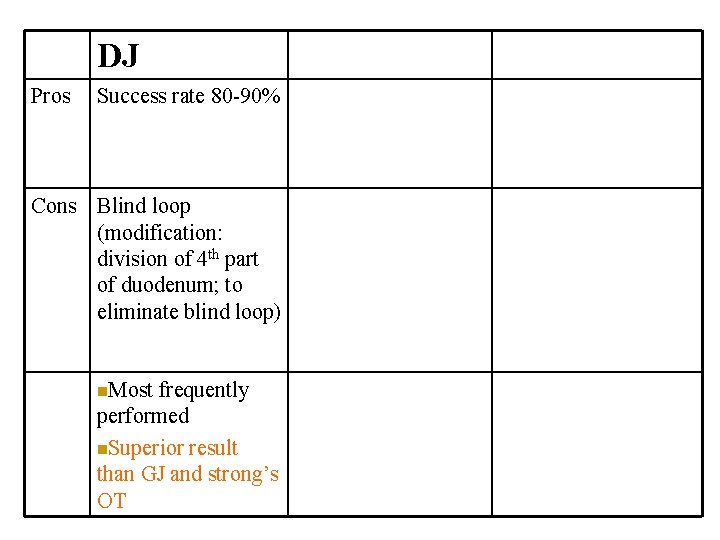
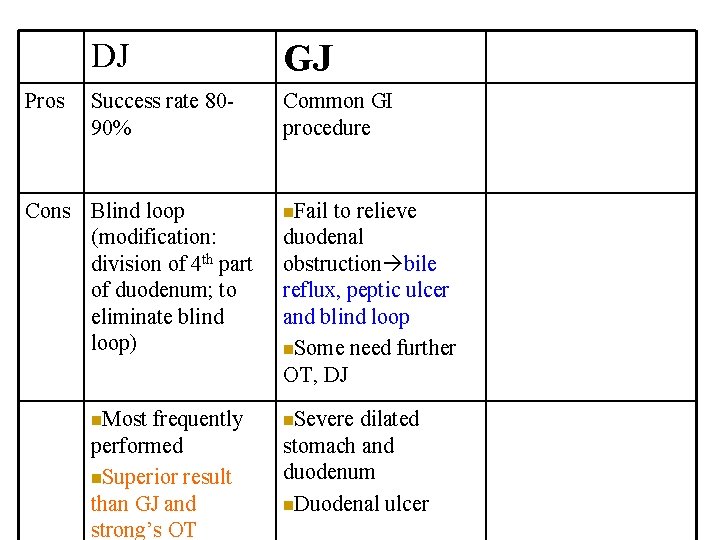
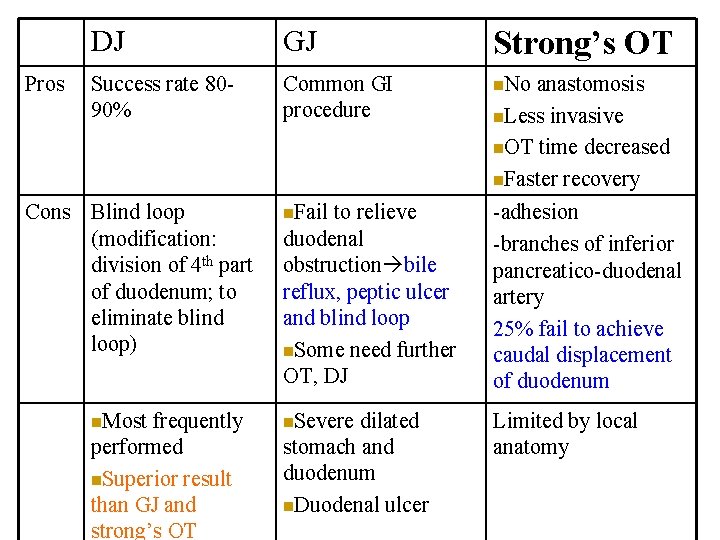
DJ Pros Success rate 80 -90% Cons Blind loop (modification: division of 4 th part of duodenum; to eliminate blind loop) n. Most frequently performed n. Superior result than GJ and strong’s OT
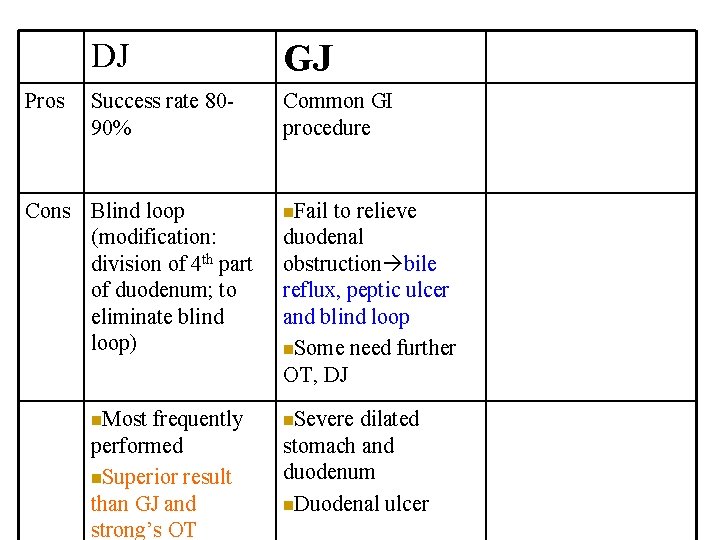
Pros DJ GJ Success rate 8090% Common GI procedure Cons Blind loop (modification: division of 4 th part of duodenum; to eliminate blind loop) n. Most frequently performed n. Superior result than GJ and strong’s OT n. Fail to relieve duodenal obstruction bile reflux, peptic ulcer and blind loop n. Some need further OT, DJ n. Severe dilated stomach and duodenum n. Duodenal ulcer
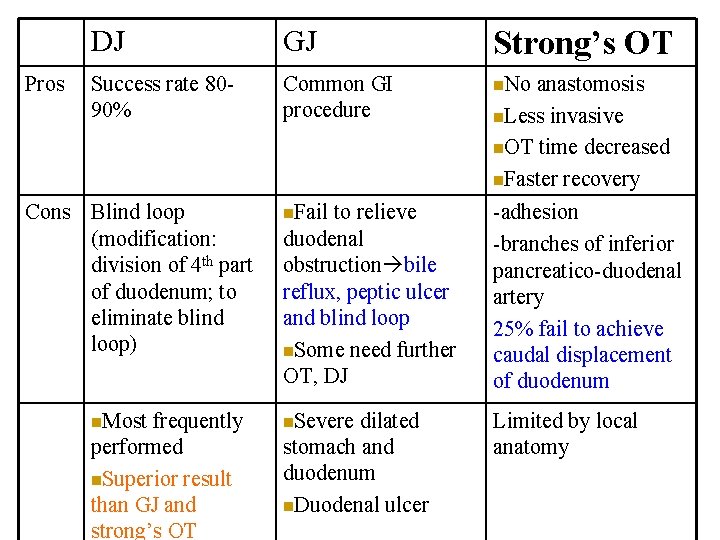
Pros DJ GJ Strong’s OT Success rate 8090% Common GI procedure n. No n. Fail to relieve duodenal obstruction bile reflux, peptic ulcer and blind loop n. Some need further OT, DJ -adhesion -branches of inferior pancreatico-duodenal artery 25% fail to achieve caudal displacement of duodenum n. Severe Limited by local anatomy Cons Blind loop (modification: division of 4 th part of duodenum; to eliminate blind loop) n. Most frequently performed n. Superior result than GJ and strong’s OT dilated stomach and duodenum n. Duodenal ulcer anastomosis n. Less invasive n. OT time decreased n. Faster recovery
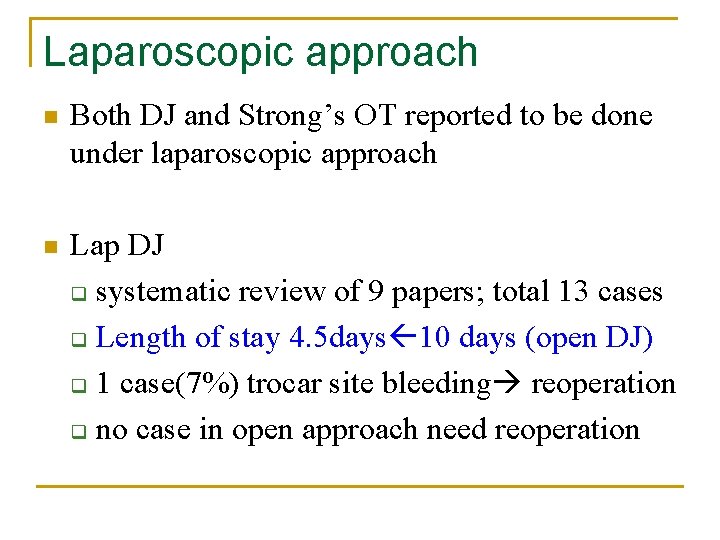
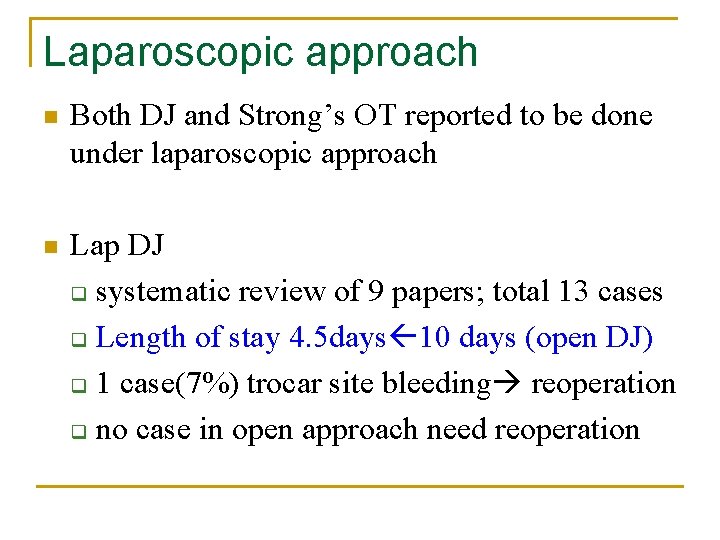
Laparoscopic approach n Both DJ and Strong’s OT reported to be done under laparoscopic approach n Lap DJ q systematic review of 9 papers; total 13 cases q Length of stay 4. 5 days 10 days (open DJ) q 1 case(7%) trocar site bleeding reoperation q no case in open approach need reoperation
Vascular surgery--Infrarenal SMA transposition n A therapeutic procedure for chronic mesenteric ischemia n Not a common surgery for SMA syndrome n caudal transposition of compressing SMA to infrarenal aorta compression over D 3
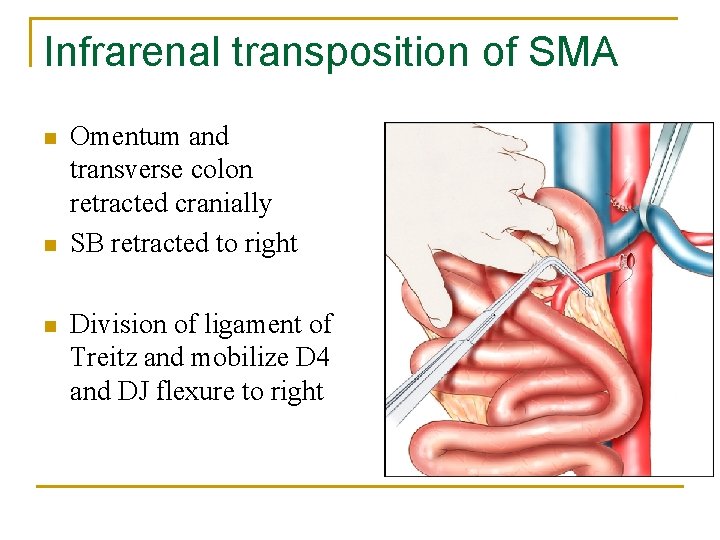
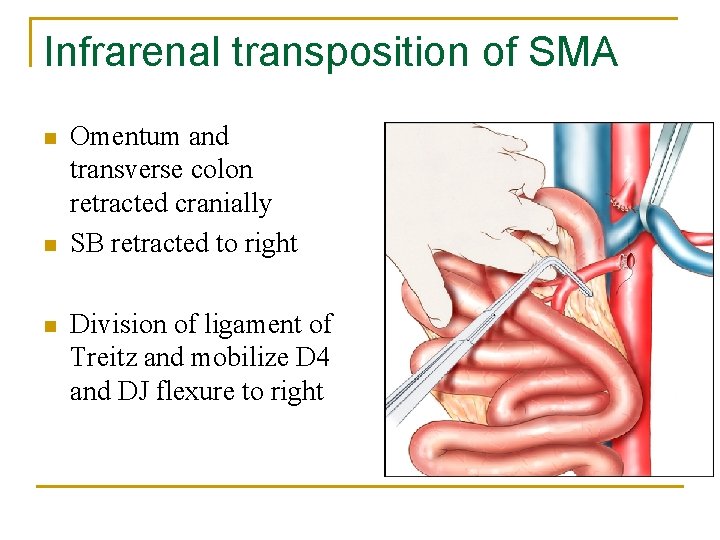
Infrarenal transposition of SMA n n n Omentum and transverse colon retracted cranially SB retracted to right Division of ligament of Treitz and mobilize D 4 and DJ flexure to right
Infrarenal transposition of SMA n n Infrarenal aorta cross clamp after iv heparin End to side anastomosis between SMA and infrarenal aorta with 5/0 prolene
Infrarenal transposition of SMA n Far less common than GI surgery n Only one case report (Germany) data regarding its outcome not available Merit q no bowel anastomosis q treat concomitant Nutcracker syndrome Higher risk compared with GI surgery n n q q q Anastomotic break down Bleeding Bowel ischemia Embolism
In the case presented Before proceed to SMA transposition n Other alternatives: conservative, GI bypass and left renal vein stenting n She opted for SMA transposition q GI complications like bowel anastomotic leaks, blind loop syndrome q treat both SMA and Nutcracker syndrome by a single operation
Despite surgery Small number--developed persistent symptom after surgery Postulations duodenal atony after massive dilatation n strong reverse peristalsis after prolong obstruction n
1. 2. 3. 4. 5. 6. 7. 8. Case presentation Pathophysiology Predisposing conditions Presentation Epidemiology Diagnosis and imaging finding Treatment Summary
Points to note n Diagnosis not to miss q Vicious cycle starving n Different treatment options Depend on patients’ condition q Selection of optimal treatment q
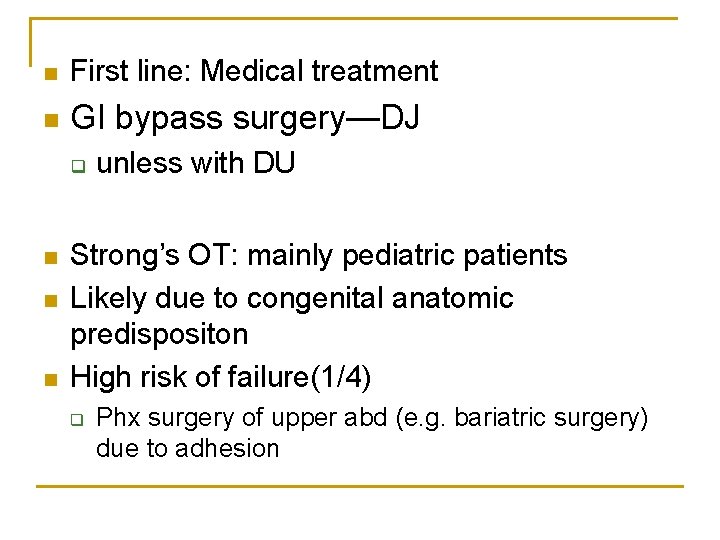
n First line: Medical treatment n GI bypass surgery—DJ q n n n unless with DU Strong’s OT: mainly pediatric patients Likely due to congenital anatomic predispositon High risk of failure(1/4) q Phx surgery of upper abd (e. g. bariatric surgery) due to adhesion
END
 Celiac artery and mesenteric artery
Celiac artery and mesenteric artery Blood vessel man model
Blood vessel man model Upper mesenteric artery
Upper mesenteric artery Pyramidal lobe
Pyramidal lobe Superior rectal artery is a branch of
Superior rectal artery is a branch of Deep artery of the arm
Deep artery of the arm Thin
Thin Thoracic inlet anatomy
Thoracic inlet anatomy Cruciate anastomosis
Cruciate anastomosis Olecranon bursitis
Olecranon bursitis Lesser peritoneal cavity
Lesser peritoneal cavity Mesenteric angiogram
Mesenteric angiogram Mesenteric arteriogram
Mesenteric arteriogram Cisterna chyli
Cisterna chyli Diverticulosis
Diverticulosis Aorta branches
Aorta branches Greater omentum
Greater omentum Mesenteric root
Mesenteric root Hopital avicenne
Hopital avicenne Knee joint superior view
Knee joint superior view Superior tibiofibular joint
Superior tibiofibular joint Hospital pharmacy organization
Hospital pharmacy organization Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Conclusion of oral medication
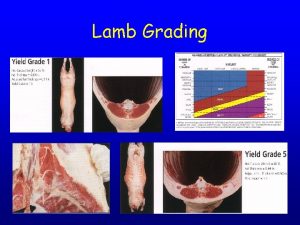
Conclusion of oral medication Lamb grading chart
Lamb grading chart Hyaline cartilage between vertebrae
Hyaline cartilage between vertebrae Define permanent joint
Define permanent joint Memorandum joint venture method
Memorandum joint venture method Lamb carcass grading
Lamb carcass grading Hinge joint
Hinge joint Causes of superior vena cava syndrome
Causes of superior vena cava syndrome Superior canal dehiscence syndrome symptoms
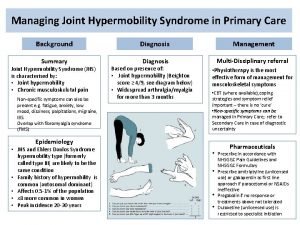
Superior canal dehiscence syndrome symptoms Joint hypermobility syndrome symptoms
Joint hypermobility syndrome symptoms Pasi hongisto
Pasi hongisto Contoh rancangan penelitian sejarah
Contoh rancangan penelitian sejarah Sma negeri 2 kuala kapuas
Sma negeri 2 kuala kapuas Spelling bee competition rules
Spelling bee competition rules Contoh pelajaran lintas minat
Contoh pelajaran lintas minat Blok dienes
Blok dienes Contoh soal teorema faktor kelas 11
Contoh soal teorema faktor kelas 11