The Spinal Cord and Spinal Nerves Dr Michael

- Slides: 81
The Spinal Cord and Spinal Nerves Dr. Michael P. Gillespie
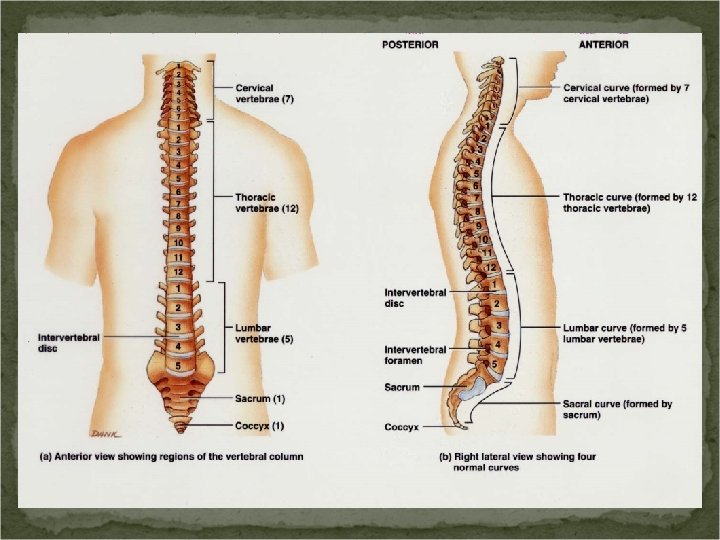
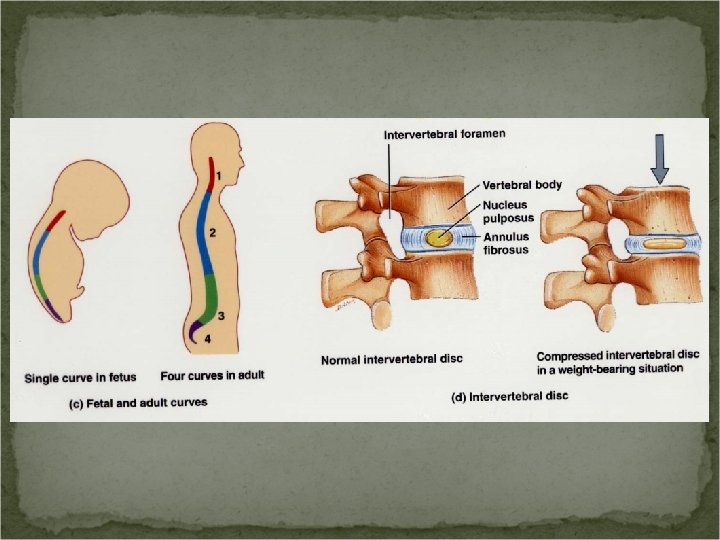
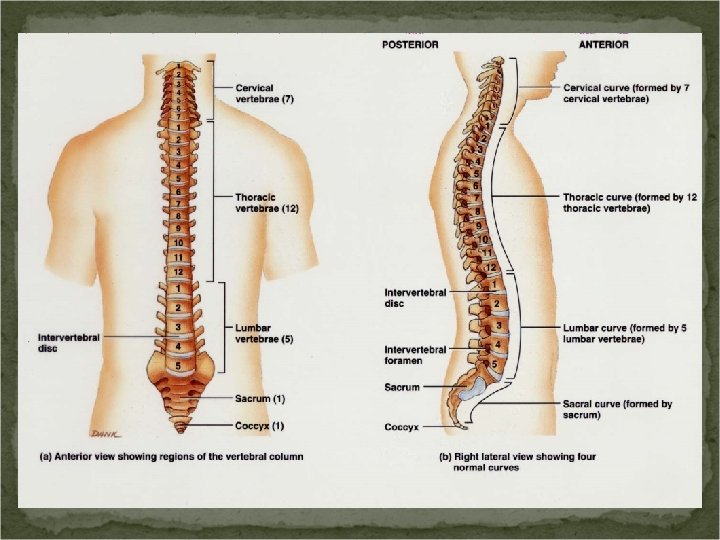
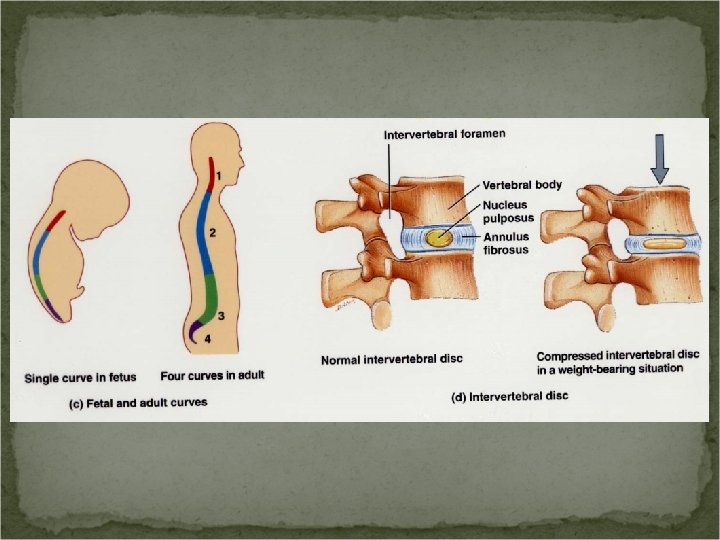
Medical Terminology Kyphosis – exaggeration of the thoracic curve Lordosis – an exaggeration of the lumbar curve or cervical curve Lumbar spine stenosis – narrowing of the spinal canal Scoliosis – lateral bending of the vertebral column
Protective Structures Bony vertebrae Meninges Cerebrospinal fluid (produced in the brain)
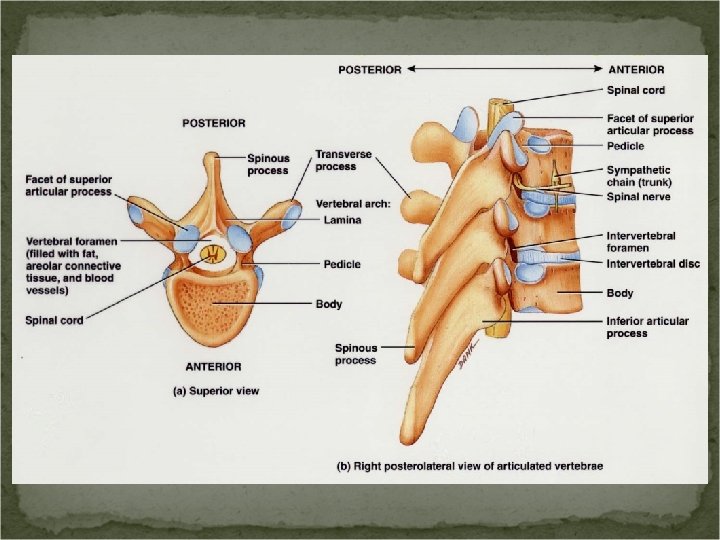
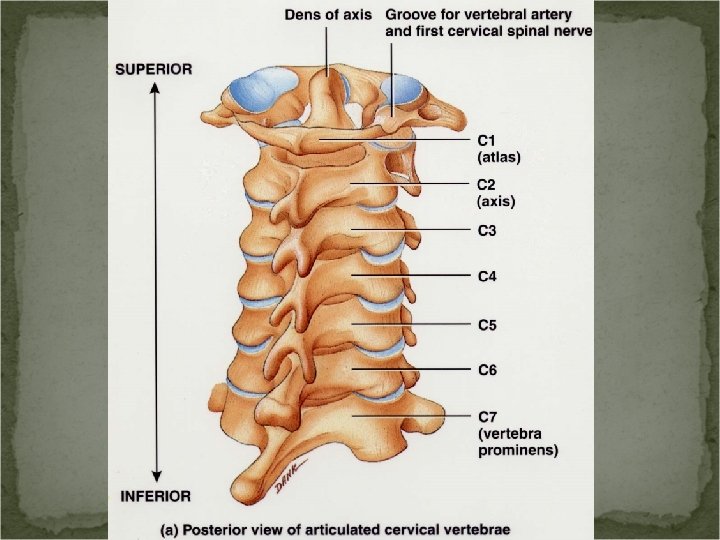
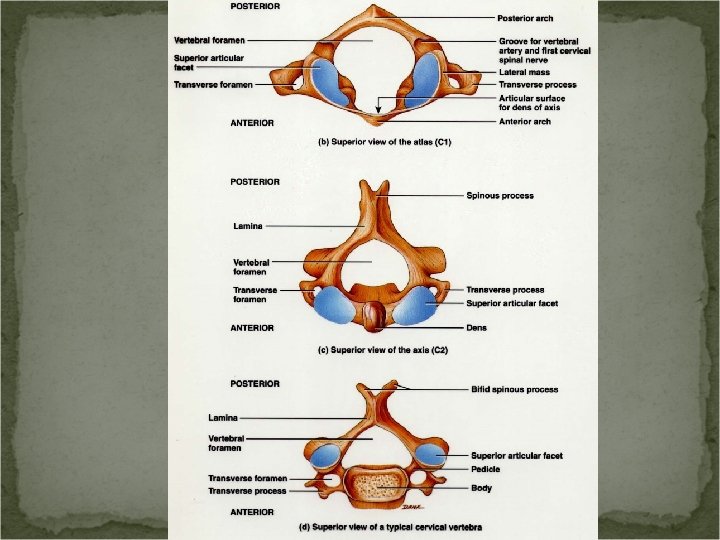
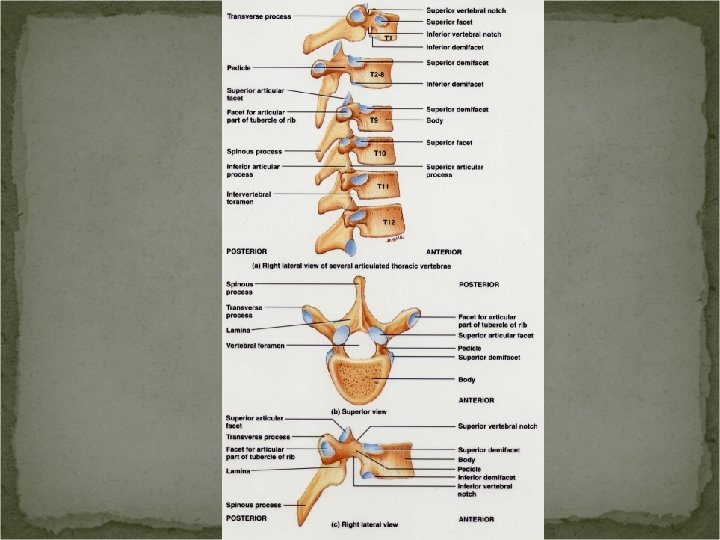
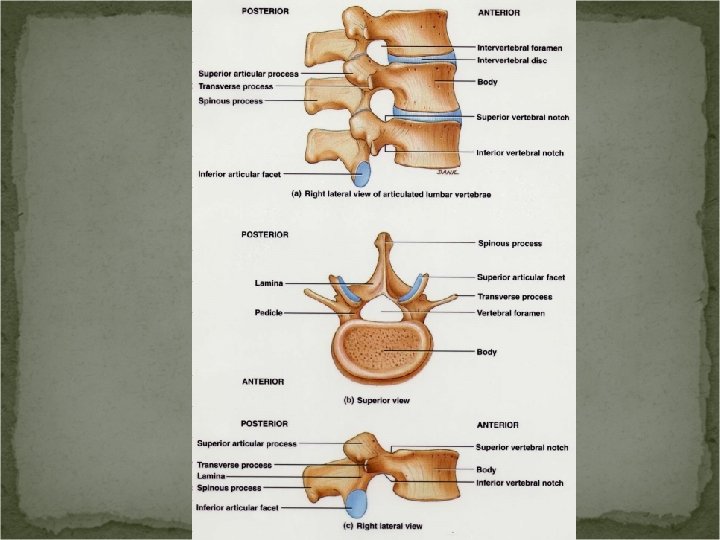
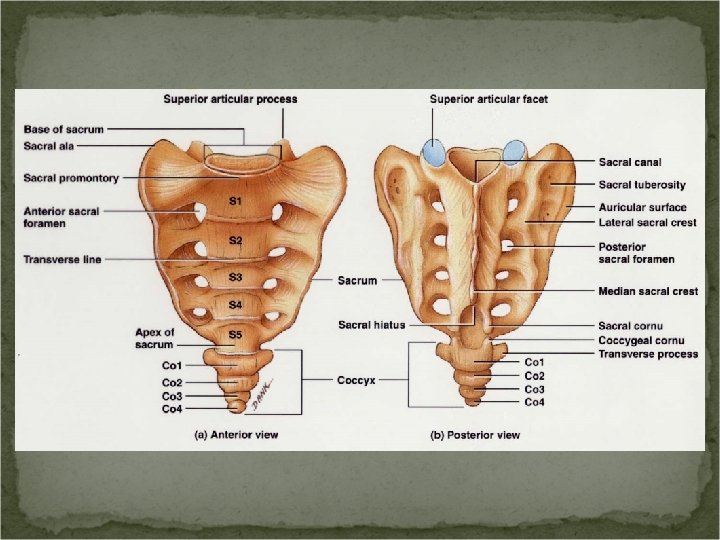
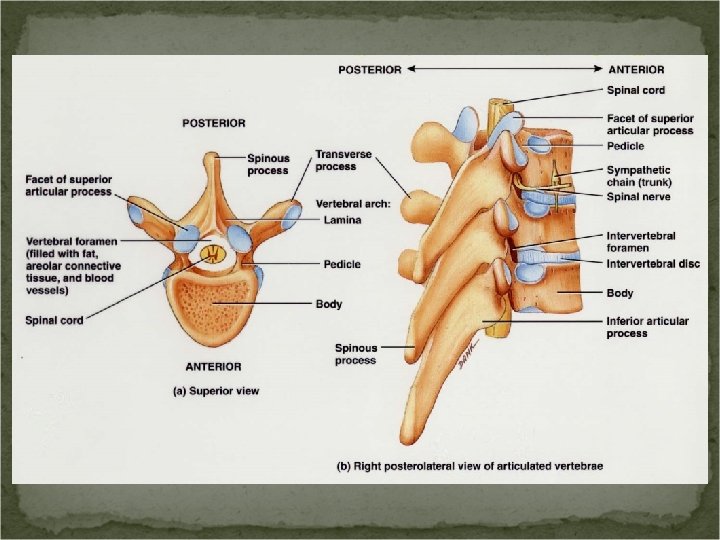
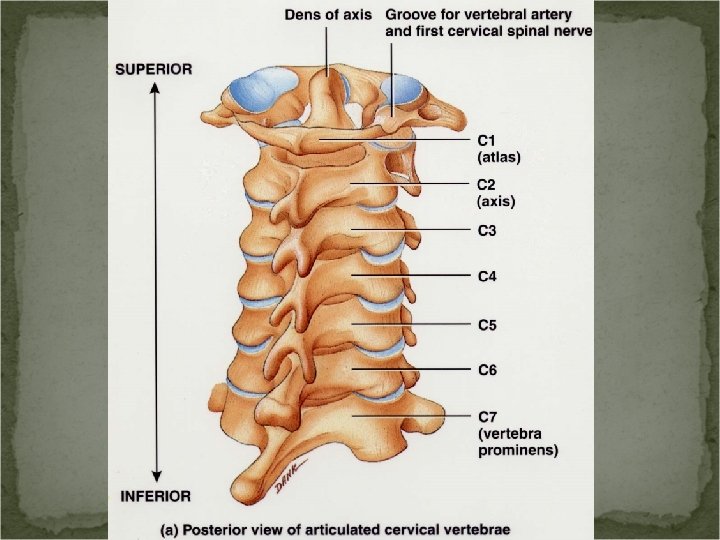
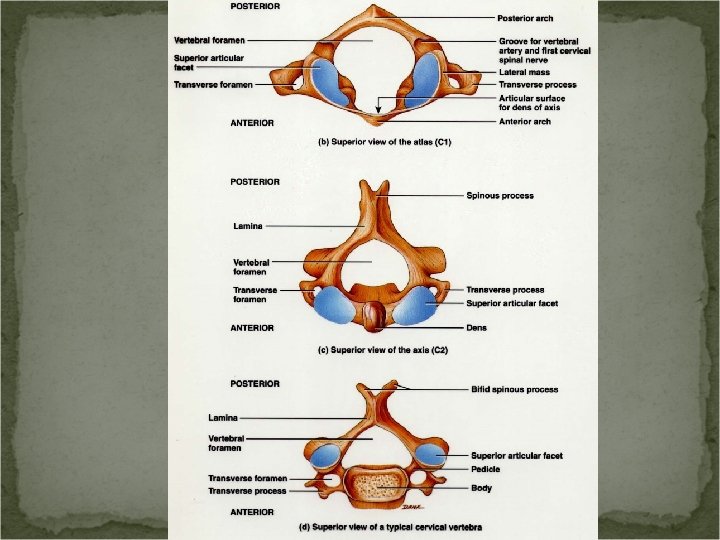
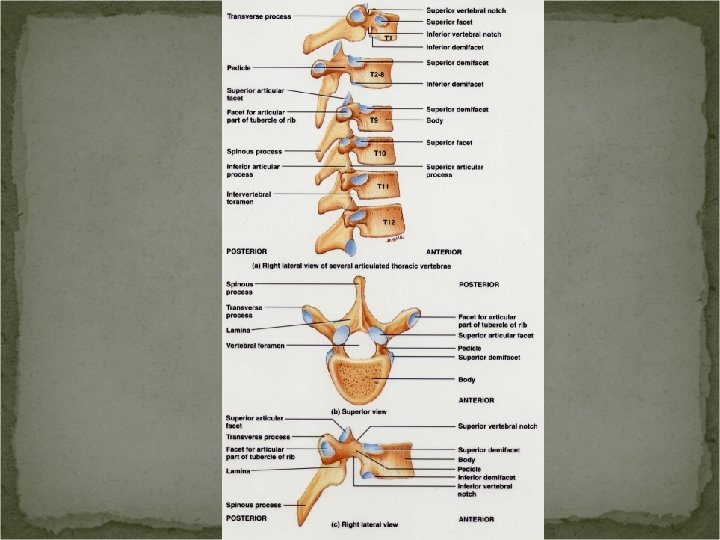
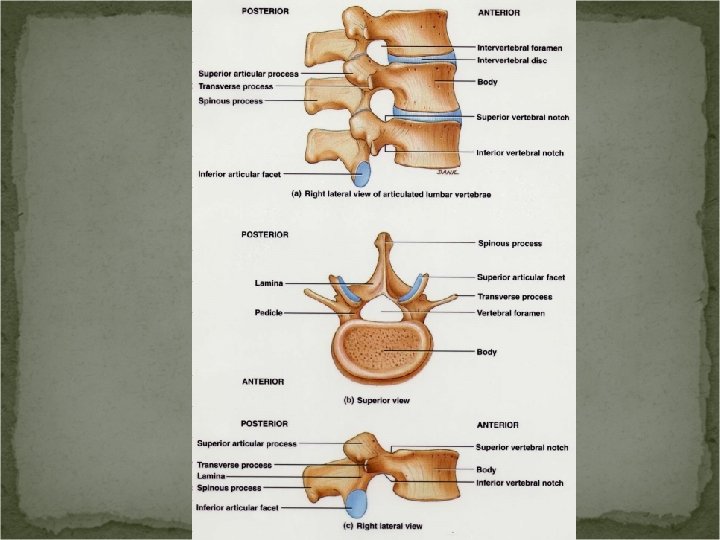
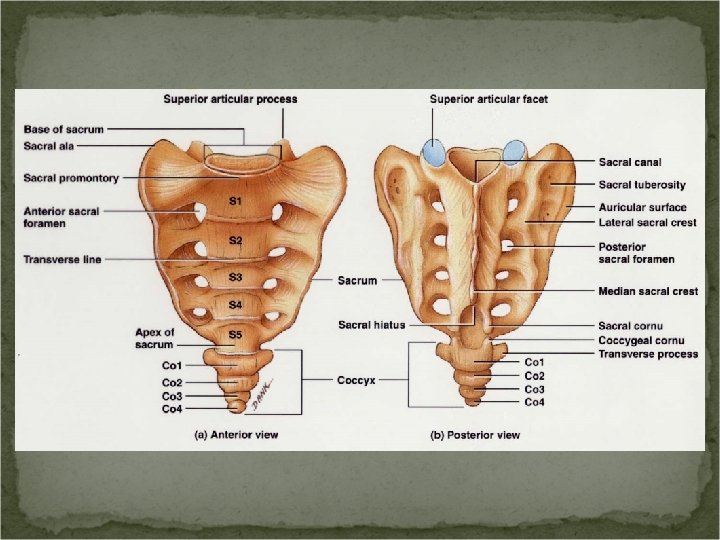
Vertebral Column The spinal cord is located within the vertebral canal of the vertebral column. The vertebral foramina form the canal. The vertebrae form a shelter for the cord. The vertebral ligaments, meninges and CSF also provide protection.
Functions of the Spinal Cord and Spinal Nerves White matter – contains the sensory and motor tracts (“highways”). Gray matter – site for integration (summing) of action potentials. Spinal nerves – connect the CNS to sensory receptors, muscles, and glands.
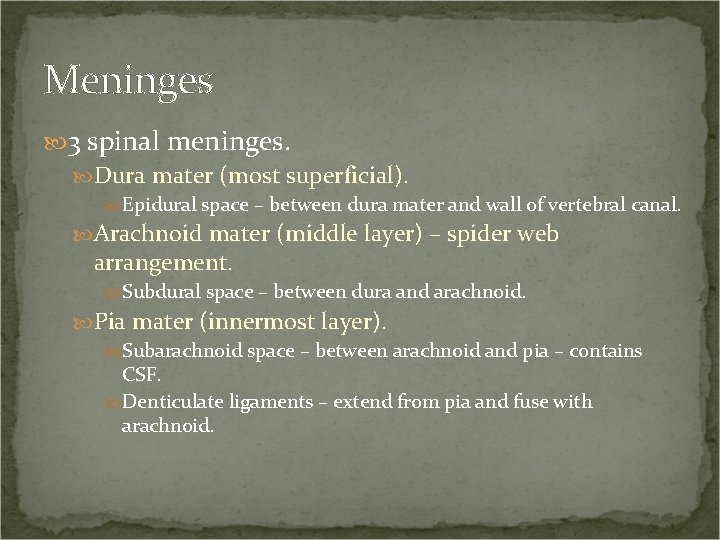
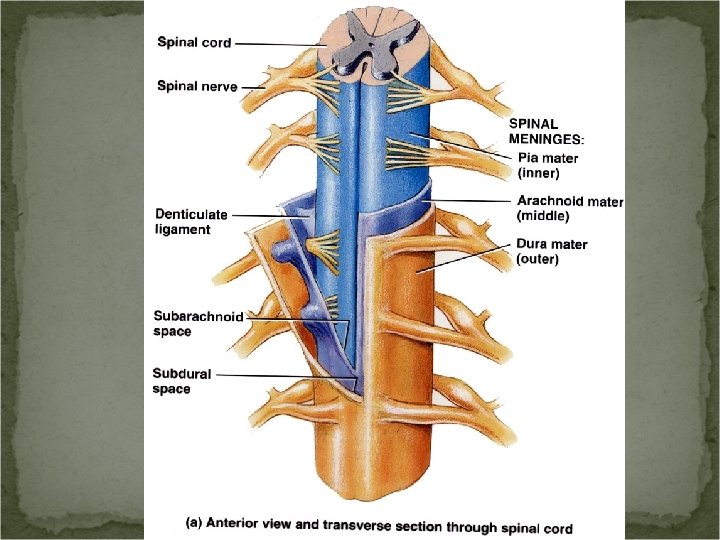
Meninges Connective tissue coverings that encircle the spinal cord and brain. Spinal meninges. Cranial meninges.
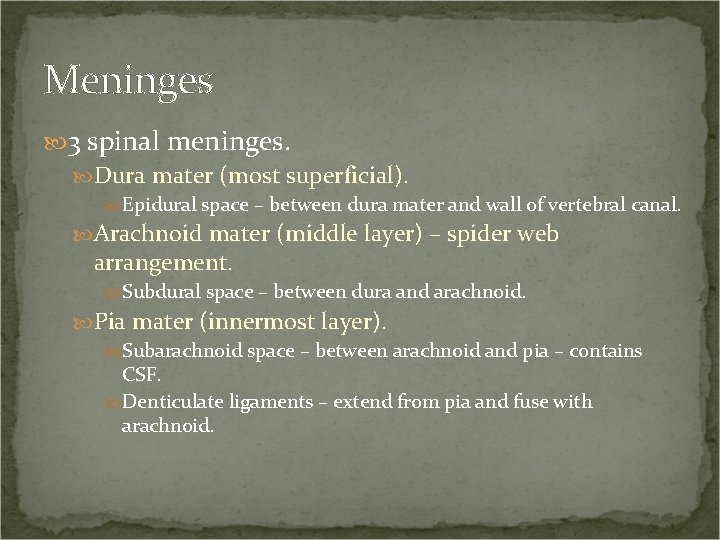
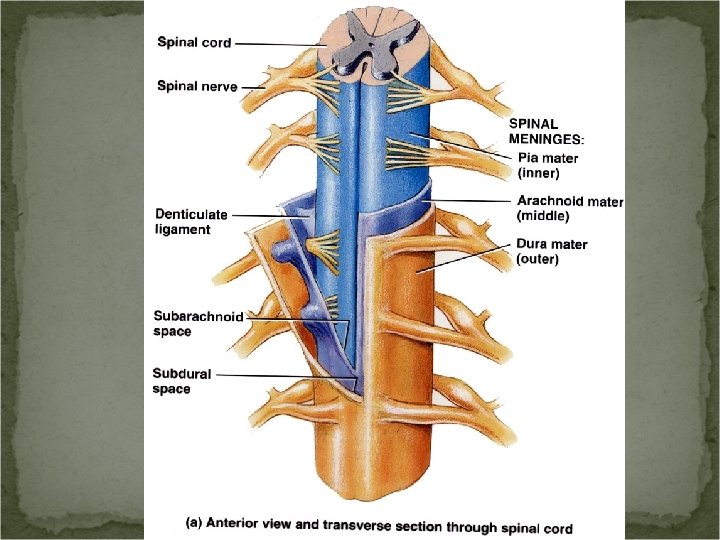
Meninges 3 spinal meninges. Dura mater (most superficial). Epidural space – between dura mater and wall of vertebral canal. Arachnoid mater (middle layer) – spider web arrangement. Subdural space – between dura and arachnoid. Pia mater (innermost layer). Subarachnoid space – between arachnoid and pia – contains CSF. Denticulate ligaments – extend from pia and fuse with arachnoid.
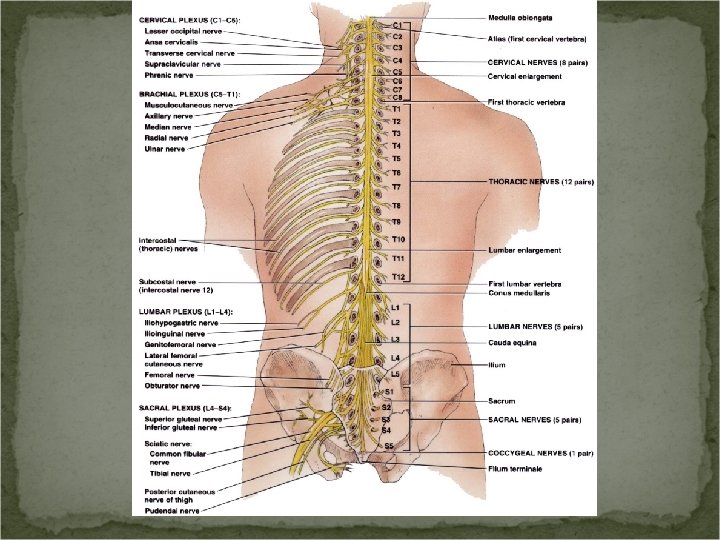
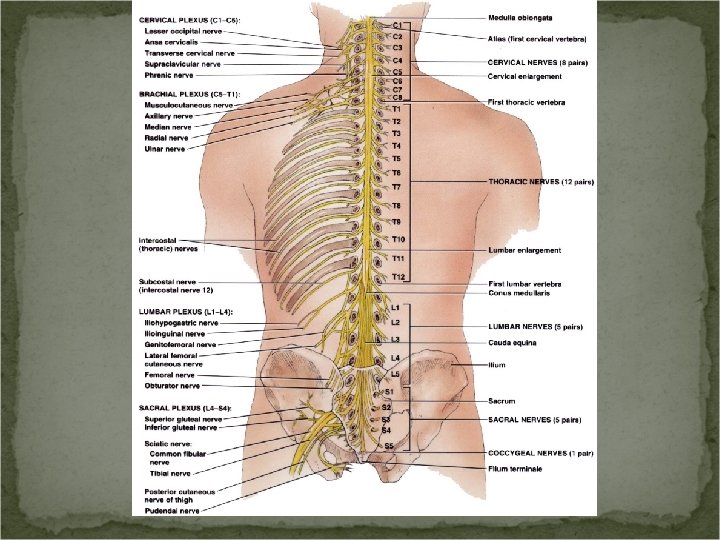
External Anatomy of the Spinal Cord Cervical enlargement – nerves to and from the upper limbs Lumbar enlargement – nerves to and from the lower limbs
External Anatomy of the Spinal Cord Conus medullaris – the spinal cord tapers to a conical portion Filum terminale – an extension of the pia mater that anchors the spinal cord to the coccyx
External Anatomy of the Spinal Cord Cauda equina “horse’s tail” Spinal nerves – paths of communication between the cord and the nerves innervating specific regions of the body Posterior (dorsal) root Sensory nerve axons Posterior (dorsal) root ganglion – swelling – cell bodies Anterior (ventral) root Motor nerve axons
Spinal Tap Spinal tap (lumbar puncture). Local anesthetic is given and a long needle is inserted into the subarachnoid space. Uses. Withdraw CSF for diagnosis. Introduce antiobiotics, contrast media, anesthetics. Introduce chemotherapy. Measure CSF pressure.
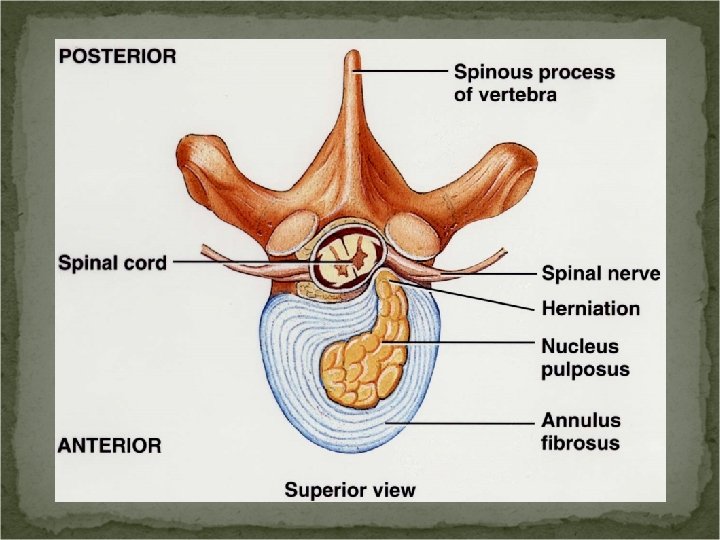
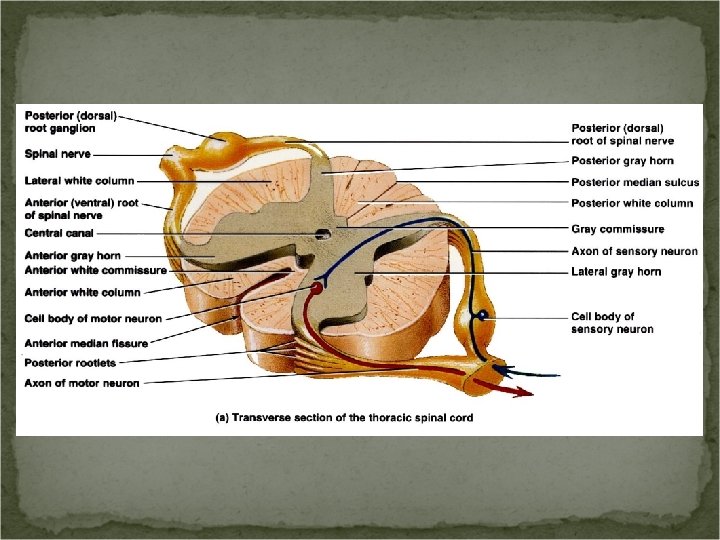
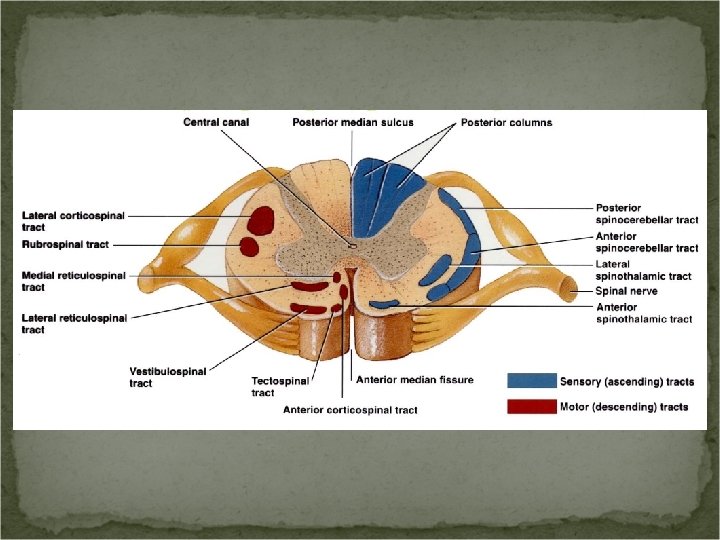
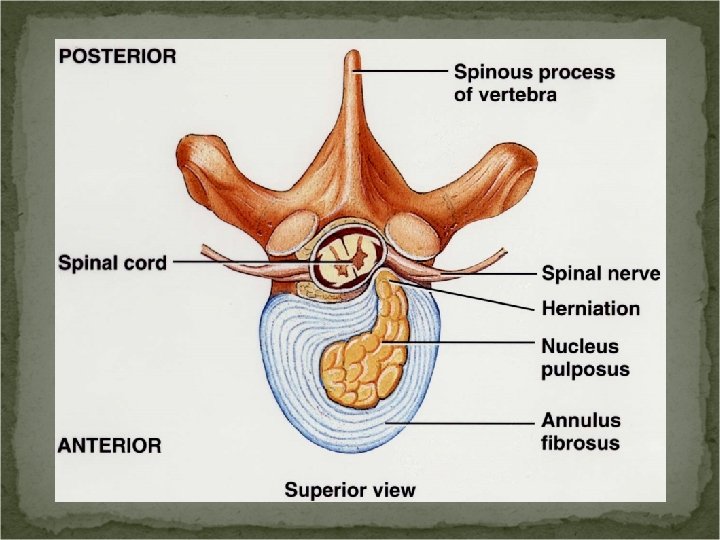
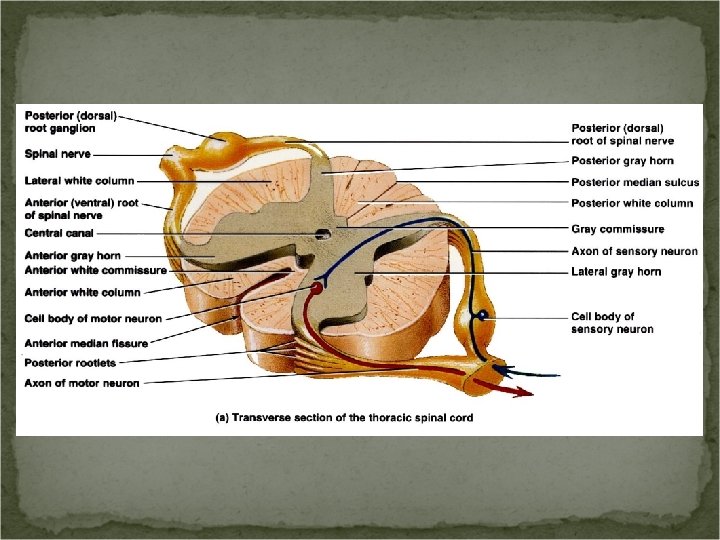
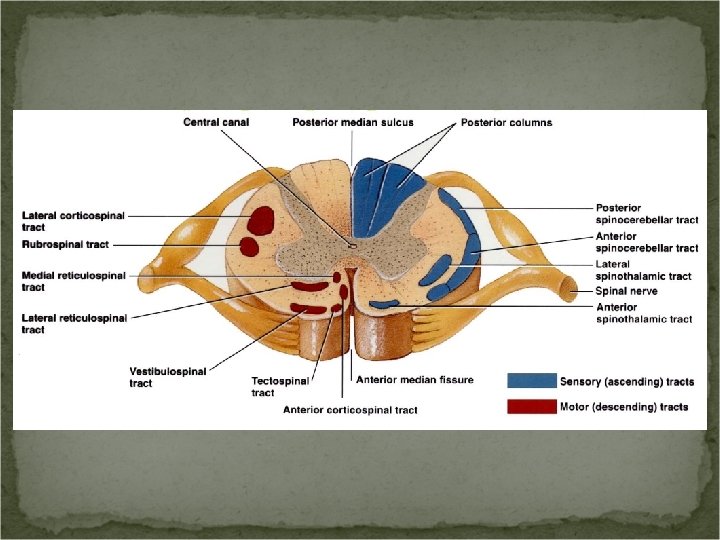
Internal Anatomy of the Spinal Cord Anterior median fissure. Posterior median sulcus.
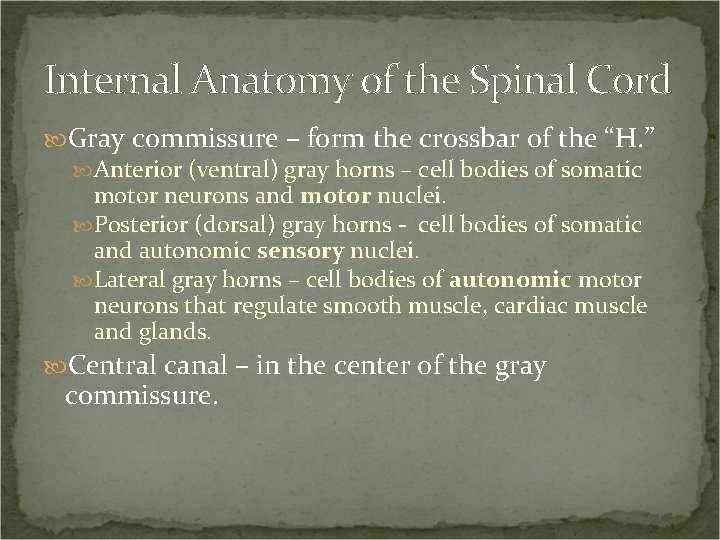
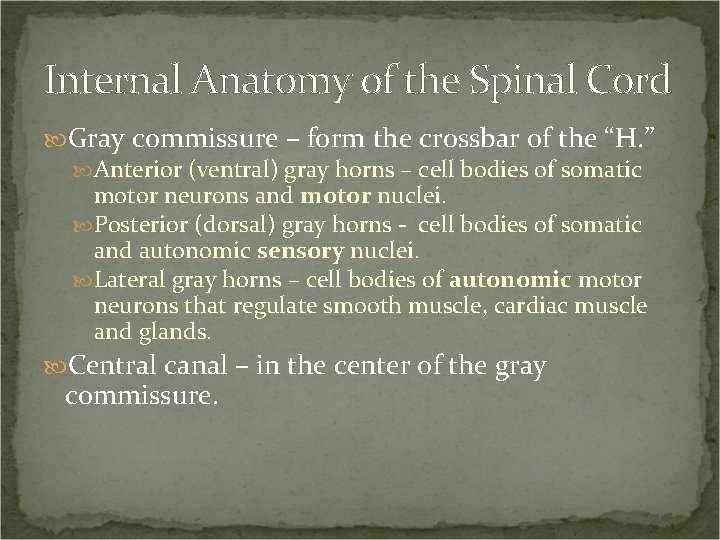
Internal Anatomy of the Spinal Cord Gray commissure – form the crossbar of the “H. ” Anterior (ventral) gray horns – cell bodies of somatic motor neurons and motor nuclei. Posterior (dorsal) gray horns - cell bodies of somatic and autonomic sensory nuclei. Lateral gray horns – cell bodies of autonomic motor neurons that regulate smooth muscle, cardiac muscle and glands. Central canal – in the center of the gray commissure.
Internal Anatomy of the Spinal Cord White columns. Sensory (ascending) tracts. Motor (descending) tracts.
Spinal Cord Physiology 2 principle functions. Nerve impulse propagation – white matter tracts. Sensory impulses flow toward the brain. Motor impulses flow from the brain. Information integration – gray matter.
Sensory & Motor Tracts The name of the tract often indicates its position in the white matter and where it begins and ends.
Sensory Tracts Lateral and anterior spinothalamic tracts. Convey impulses for pain, warmth, tickling, itching, deep pressure, and a crude sense of touch (poorly localized). Posterior columns. Convey impulses for proprioception, discriminative touch, 2 point discrimination, light pressure sensations, and vibrations.
Motor Tracts Direct pathways – convey precise voluntary movements. Lateral corticospinal. Anterior corticospinal. Corticobulbar.
Motor Tracts Indirect pathways – govern automatic movements (I. E. Reflexes). Rubrospinal. Tectospinal. Vestibulospinal.
Reflexes and Reflex Arcs Reflex – a fast, unplanned sequence of actions that occurs in response to a particular stimulus. Location of integration. Spinal reflex. Cranial reflex – integration in brain stem. Types of reflexes. Somatic reflexes – contraction of skeletal muscles. Autonomic (visceral) reflexes – responses of smooth muscle, cardiac muscle, and glands.
Reflex Arc Reflex arc (reflex circuit) - the pathway followed by nerve impulses.
Five Functional Components of a Reflex Arc Sensory receptor. Distal end of a sensory neuron. Responds to a stimulus. Sensory neuron. Nerves terminate in the brain stem or spinal cord.
Five Functional Components of a Reflex Arc Integrating center. Monosynaptic reflex arc - A synapse between a sensory neuron and a motor neuron. Polysynaptic reflex arc – one or more interneurons and a motor neuron.
Five Functional Components of a Reflex Arc Motor neuron. Effector. The part of the body that responds to the motor nerve impulse. Somatic reflex – the effector is a skeletal muscle. Autonomic reflex – the effector is smooth muscle, cardiac muscle or a gland.

Reflexes are normally predictable. They can provide information about the health of the nervous system.
Reflexes Damage or disease anywhere along the reflex arc can cause the reflex to be absent or abnormal. Somatic reflexes can be tested by tapping or stroking the body surface. Autonomic reflexes cannot be tested easily because the visceral receptors are deep inside the body.
Four Important Somatic Spinal Reflexes Stretch reflex Tendon reflex Flexor (withdrawal) reflex Crossed (extensor) reflex
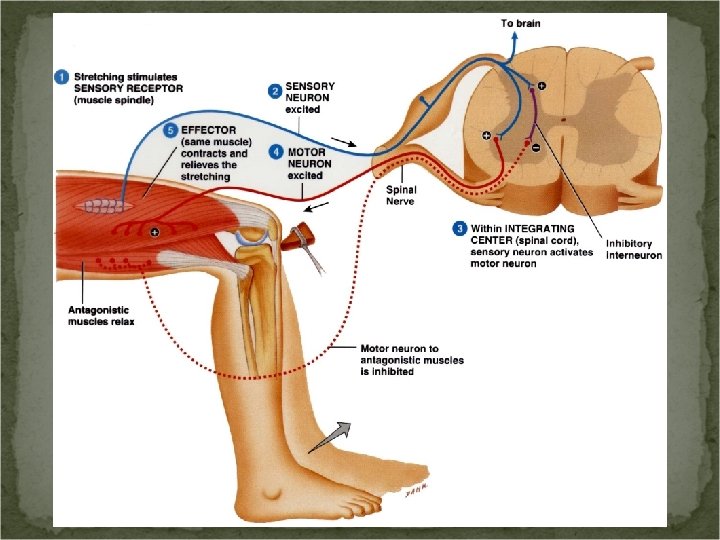
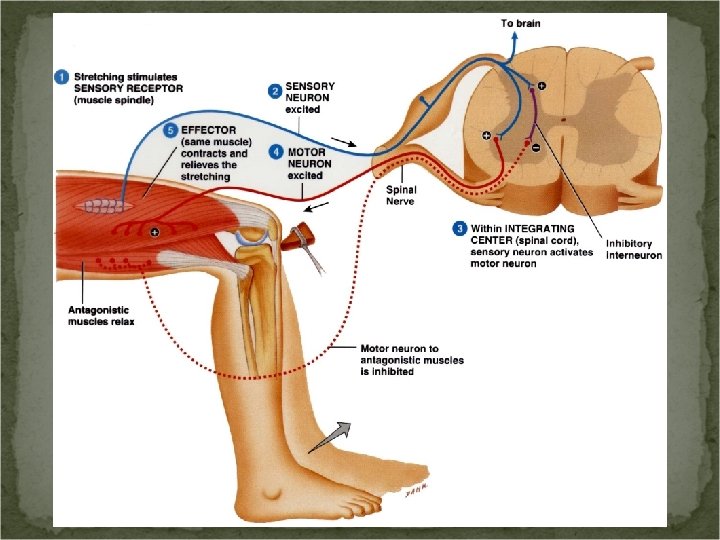
Stretch Reflex A stretch reflex causes contraction of a skeletal muscle in response to stretching of the muscle. Monosynaptic reflex arc. Ipsilateral reflex. This reflex helps avert injury by preventing overstretching of a muscle. Reciprocal inhibition – when the stretched muscle contracts, the antagonistic muscle(s) relax.
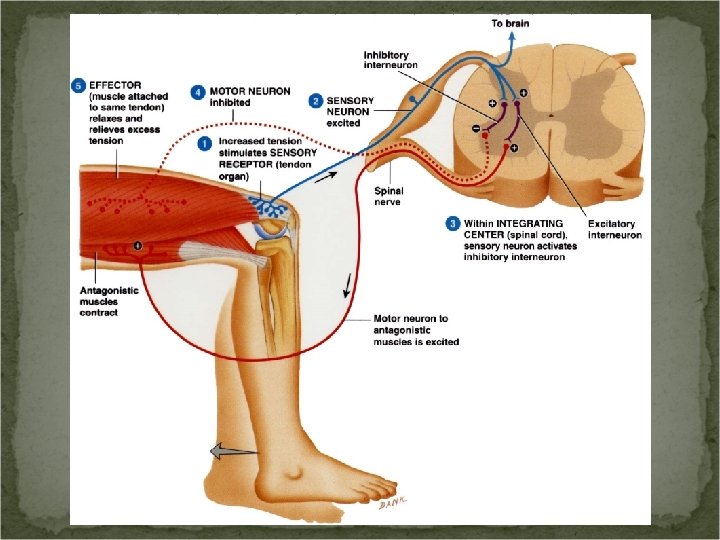
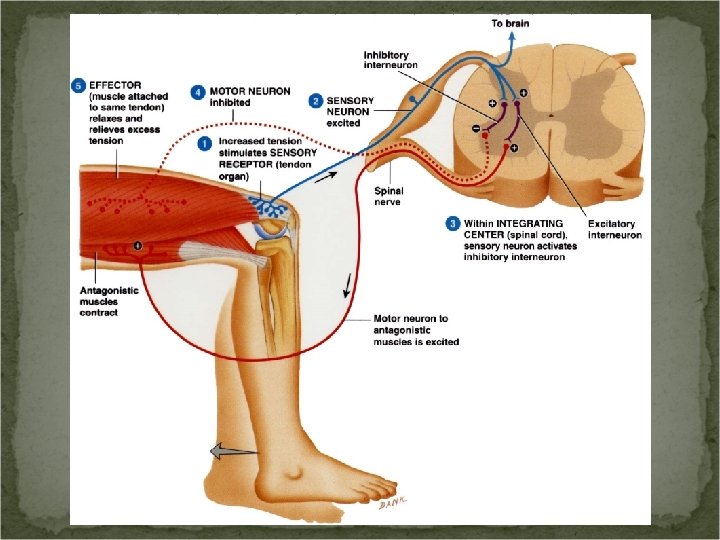
Tendon Reflex The tendon reflex controls muscle tension by causing muscle relaxation before muscle forces become so great they tear tendons. Ipsilateral reflex. Sensory receptors – tendon (Golgi tendon) organs.
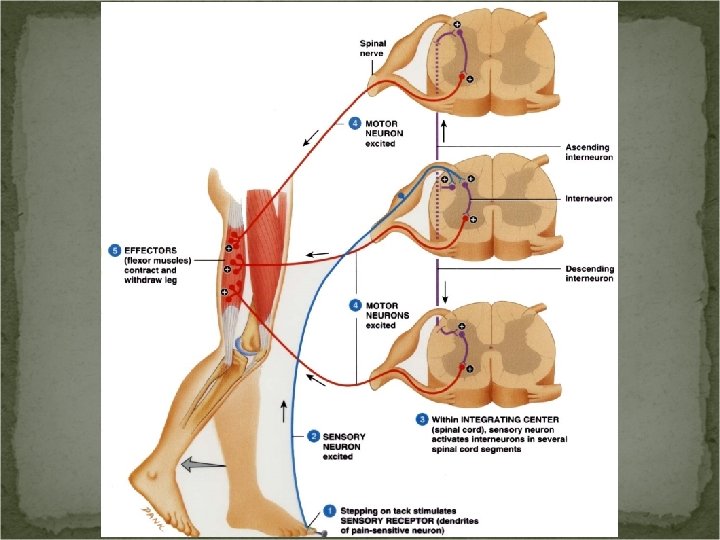
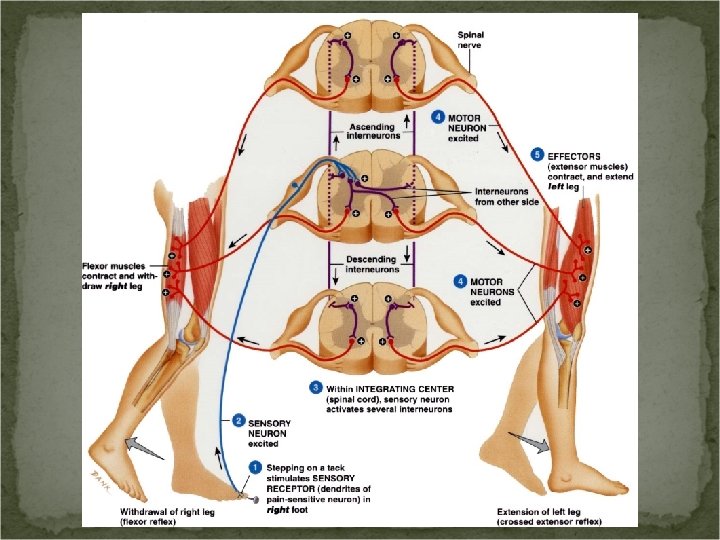
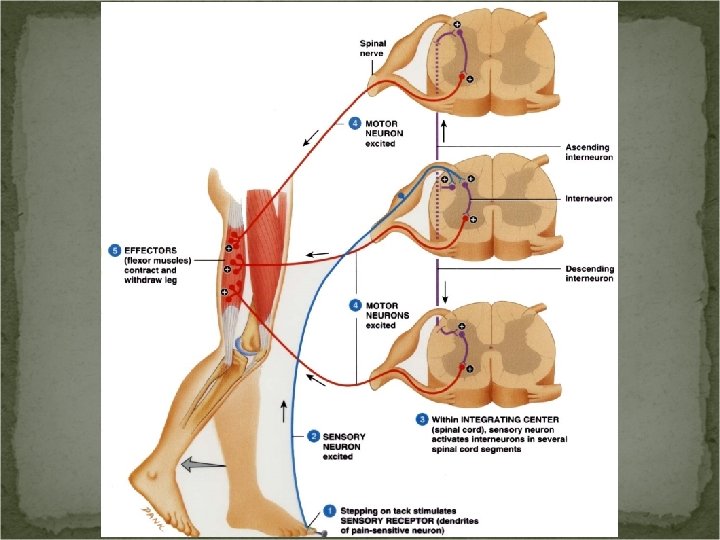
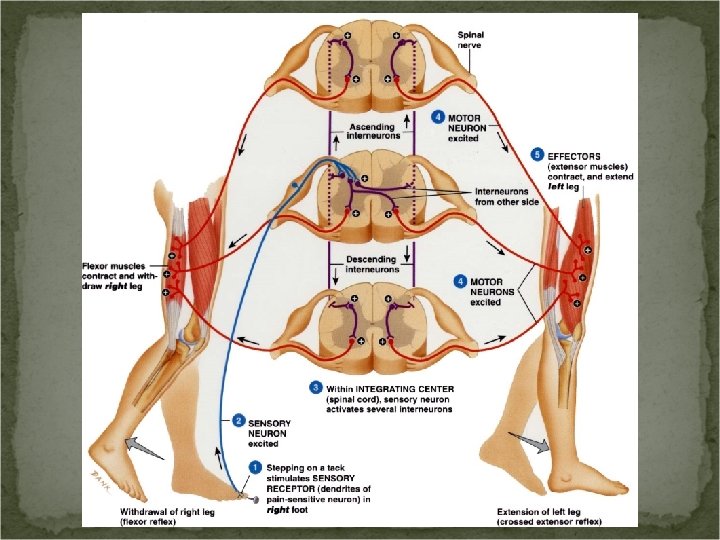
Flexor (Withdrawal Reflex) Causes withdrawal from a painful stimulus. This reflex causes contraction of the flexor muscles with causes withdrawal from a painful stimulus. Ipsilateral reflex. Several motor units at different levels of the spinal cord are recruited – intersegmental reflex arc. Reciprocal innervation occurs.
Crossed Extensor Reflex Helps you maintain balance. Contralateral reflex arc. Reciprocal innervation occurs.
Plantar Flexion Reflex The plantar flexion reflex is elicited by stroking the lateral outer margin of the sole. The normal response is curling under of the toes. Babinski sign – the great toe extends – this indicates damage to the descending motor pathways. The babinski sign is normal in children under 18 months due to incomplete myelination of the axons.
Spinal Nerves The spinal nerve has two connections to the cord: a posterior root and an anterior root. The posterior and anterior roots unite to form a spinal nerve at the intervertebral foramen. The posterior root contains sensory axons and the anterior root contains motor axons; Therefore, the spinal nerve is a mixed nerve.
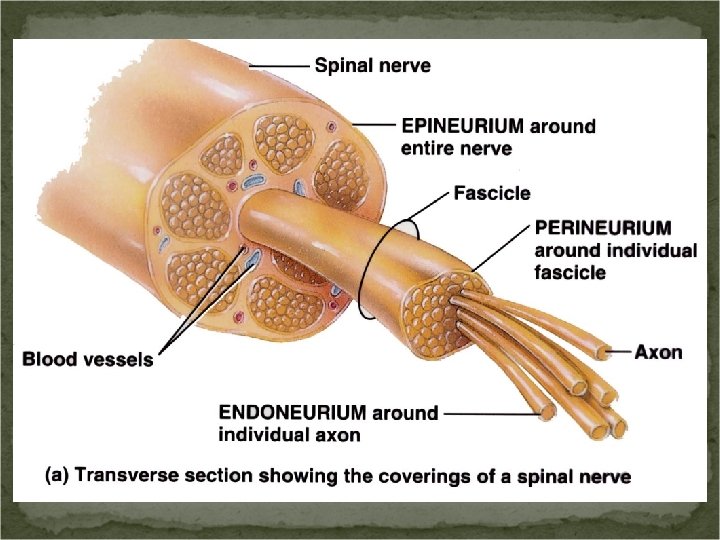
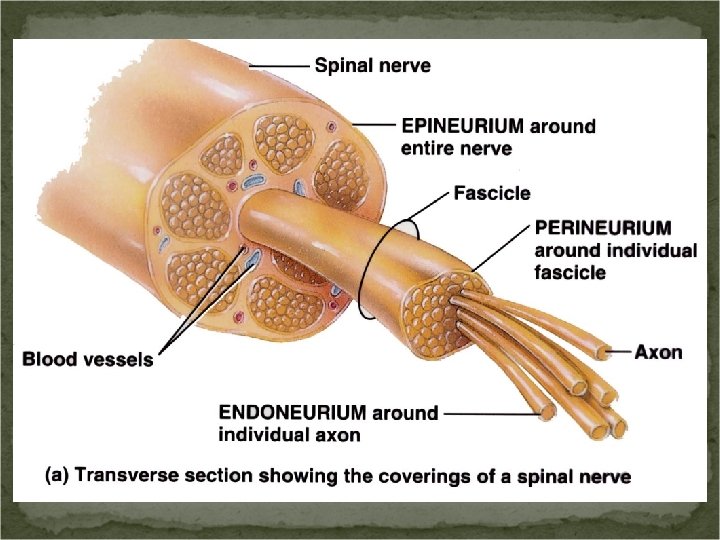
Connective Tissue Coverings of Spinal Nerves Endoneurium – surrounds individual axons. Perineurium - surrounds bundles of axons called fascicles. Epineurium – surrounds the entire nerve.
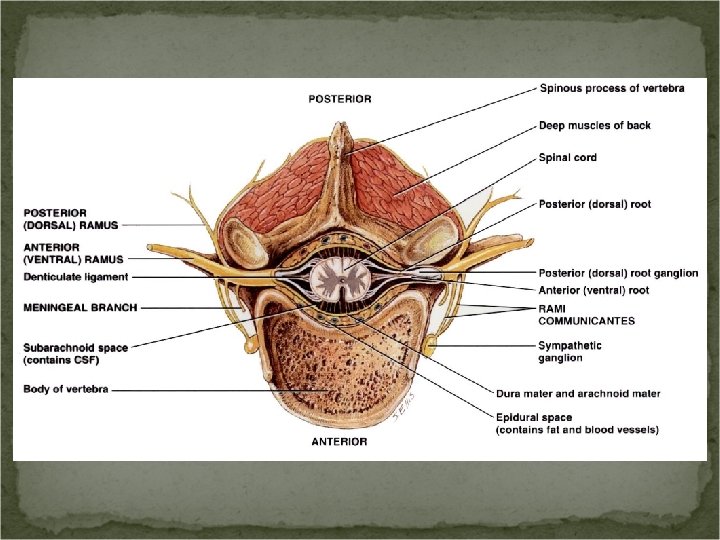
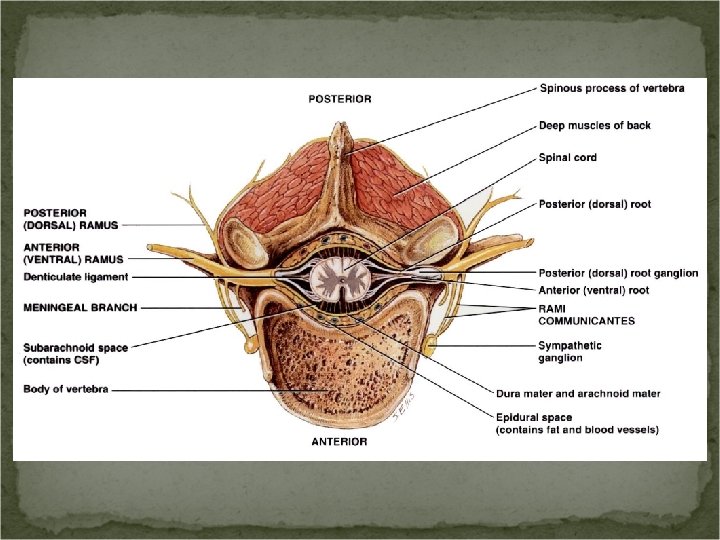
Branches After passing through the IVF, the spinal nerve forms rami (branches). Posterior (dorsal) ramus. Anterior (ventral) ramus. Meningeal branch. Rami communicantes – serves the autonomic nervous system.
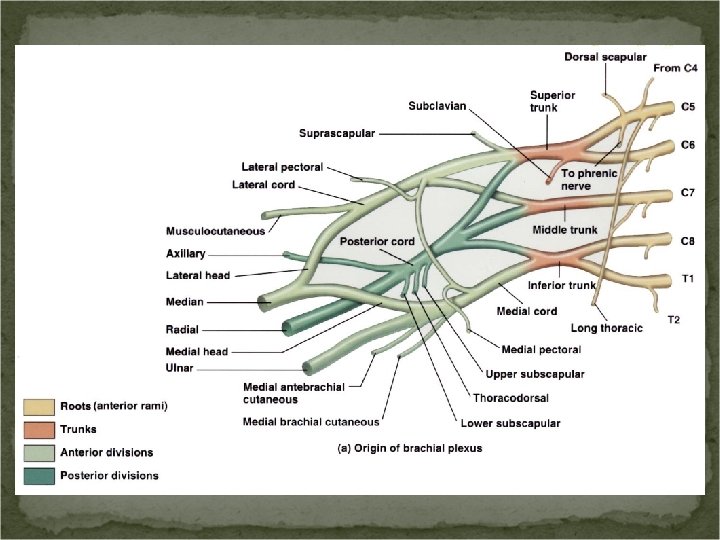
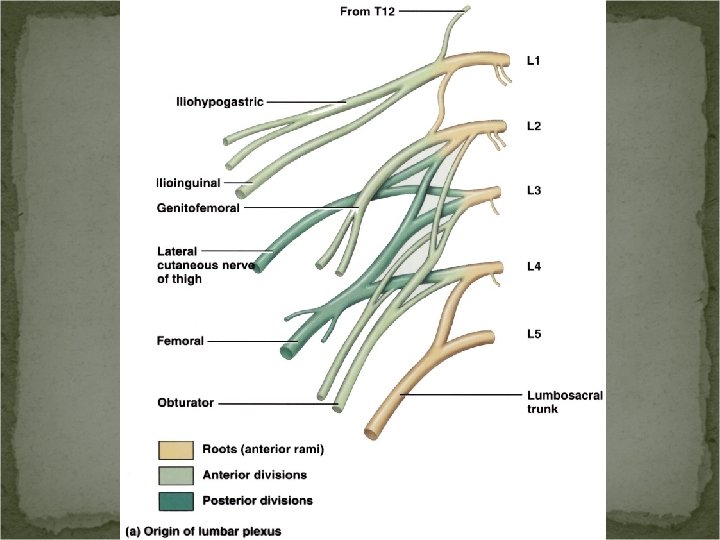
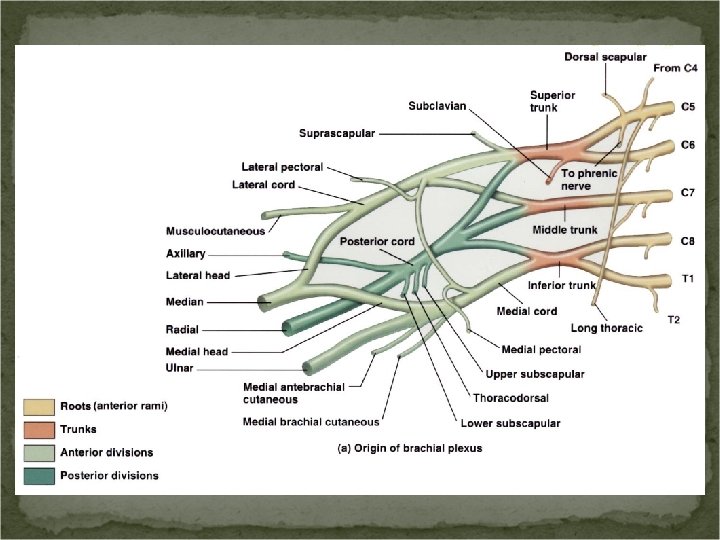
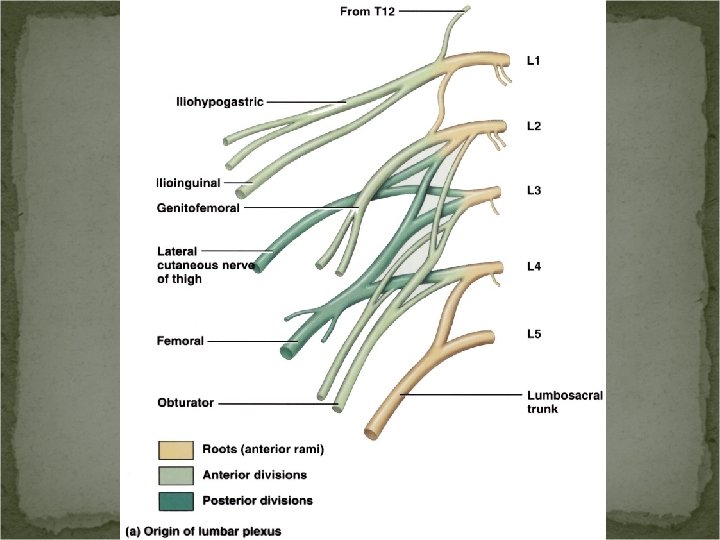
Plexuses A network of axons. Principle plexuses: Cervical plexus. Brachial plexus. Lumbar plexus. Sacral plexus. Coccygeal plexus. The nerves have branches named for the structures they innervate.
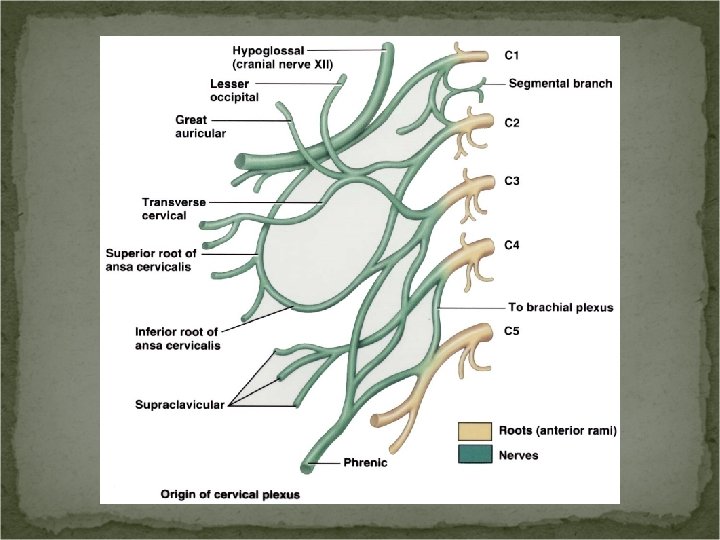
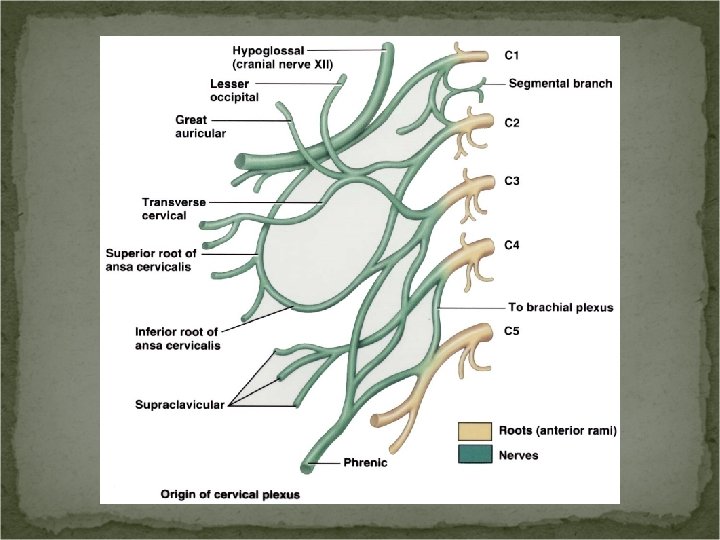
Cervical Plexus The cervical plexus supplies the skin and muscles of the head, neck, and superior part of the shoulders and chest. The phrenic nerves arise from the cervical plexus and innervates the diaphragm. “C 3, 4 & 5 keep the diaphragm alive. ”
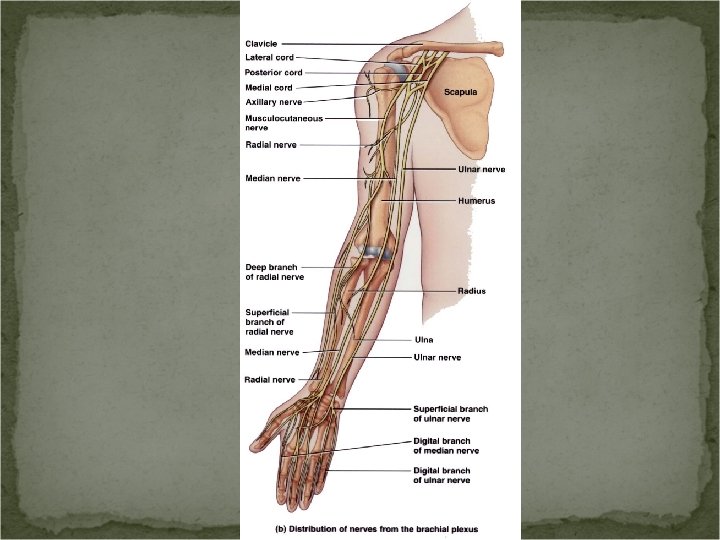
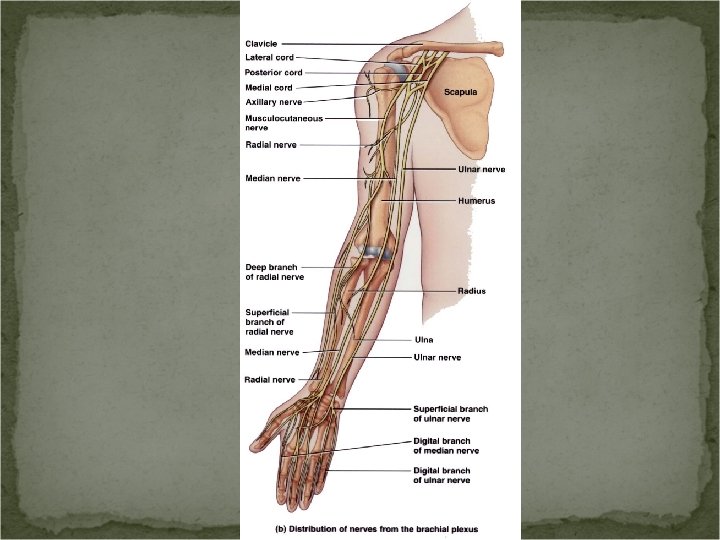
Brachial Plexus The brachial plexus provides the entire nerve supply of the shoulders and upper limbs.
Brachial Plexus Major nerves: Axillary nerve – supplies deltoid and teres minor mm. Musculocutaneous nerve – supplies arm flexors. Radial nerve – supplies posterior arm and forearm mm. Median nerve – supplies anterior forearm mm and some hand mm. Ulnar nerve – supplies anteromedial mm of the forearm and most of the hand muscles.
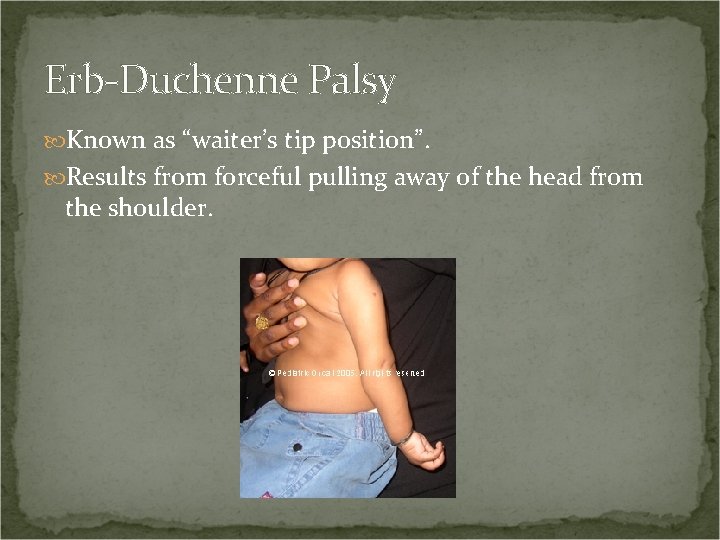
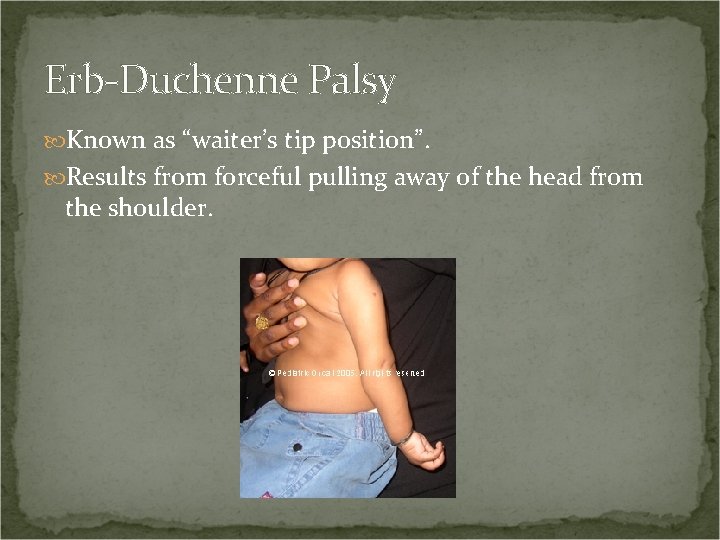
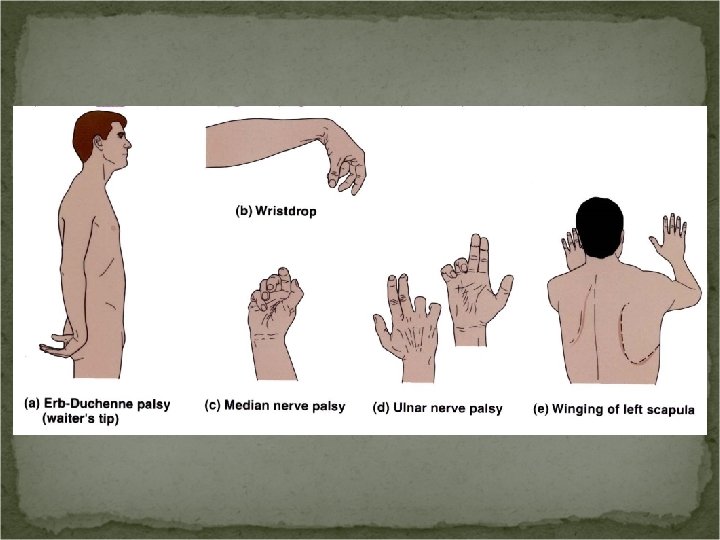
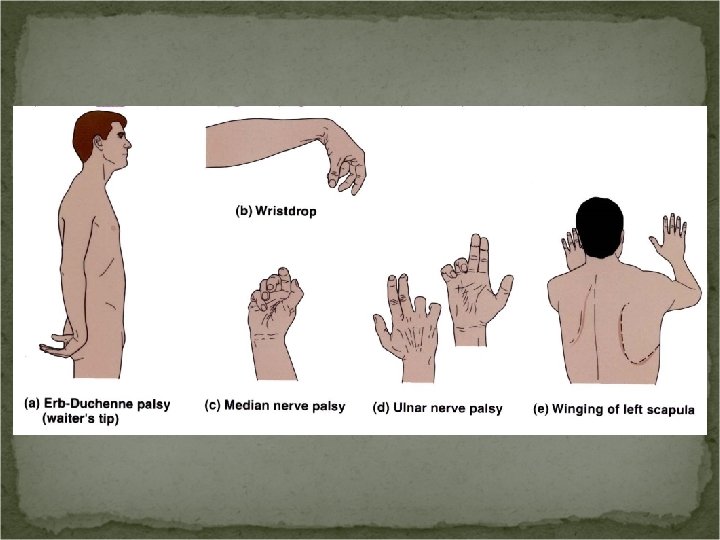
Erb-Duchenne Palsy Known as “waiter’s tip position”. Results from forceful pulling away of the head from the shoulder.
Radial Nerve Injury Caused by improper intramuscular injections into the deltoid or when the cast is applied too tightly around the mid-humerus. Indicated by wrist drop.
Median Nerve Injury Numbness, tingling, and pain in the palm and fingers. Inability to pronate the forearm. Weak wrist flexion.
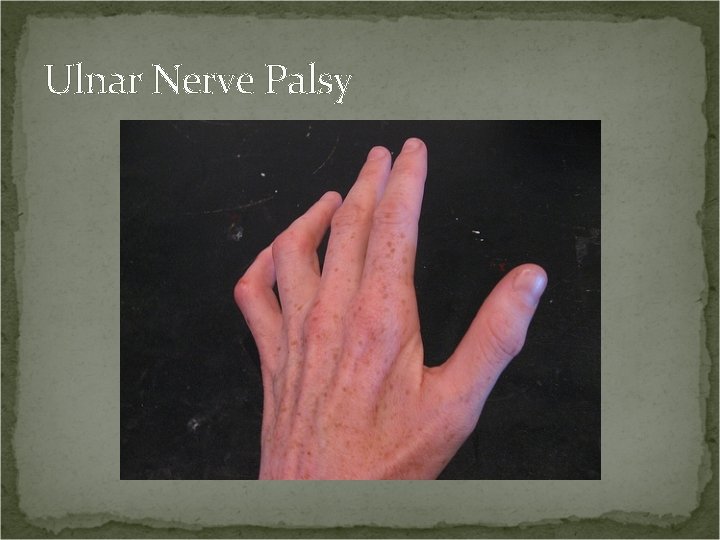
Ulnar Nerve Injury Inability to abduct or adduct the fingers. Atrophy of the interosseous mm of the hand. “Clawhand”. Loss of sensation over the little finger.
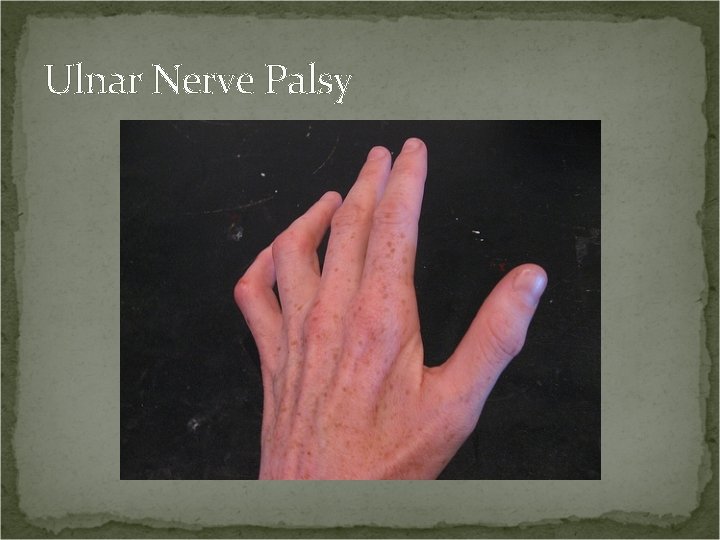
Ulnar Nerve Palsy
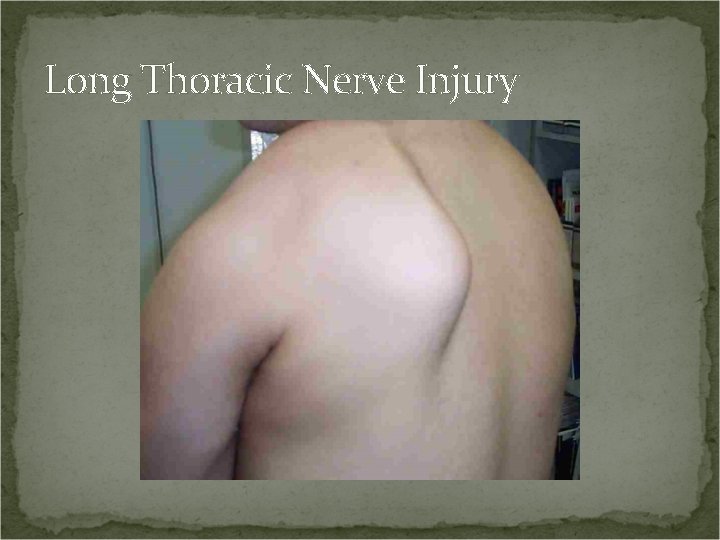
Long Thoracic Nerve Injury Paralysis of the serratus anterior mm. The scapula protrudes. “Winged scapula”.
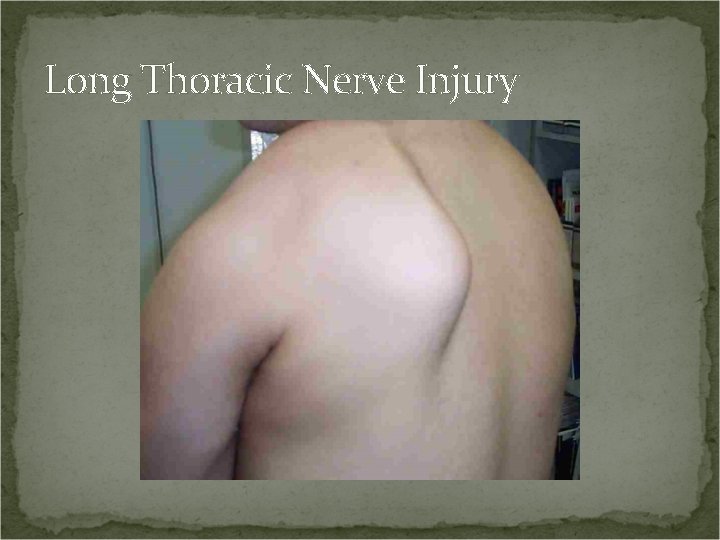
Long Thoracic Nerve Injury
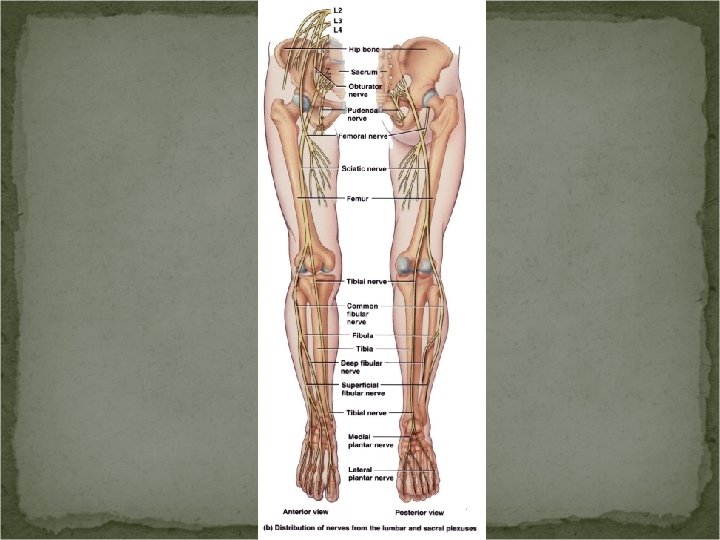
Lumbar Plexus The lumbar plexus supplies the anterolateral abdominal wall, external genitals, and part of the lower limbs.
Lumbar Plexus Injuries Femoral nerve injury. Can be caused by a stab or gunshot wounds. Inability to extend the leg and lost sensation. Obturator nerve injury. Complication of childbirth. Paralysis of the adductor muscles of the leg and loss of sensation.
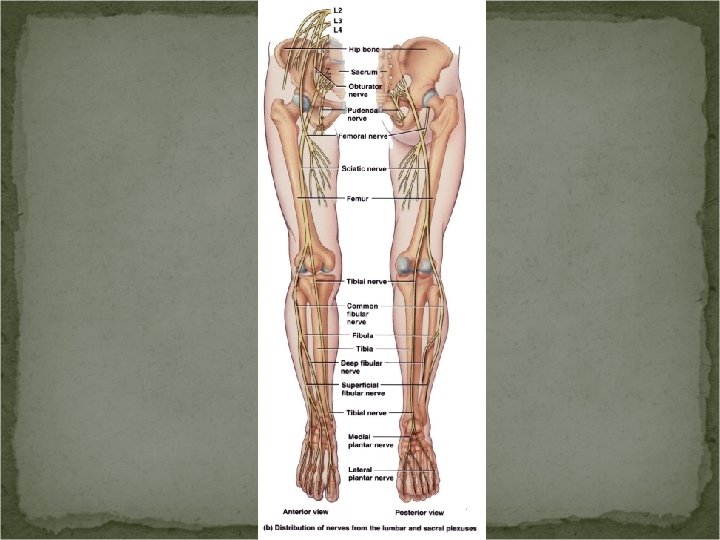
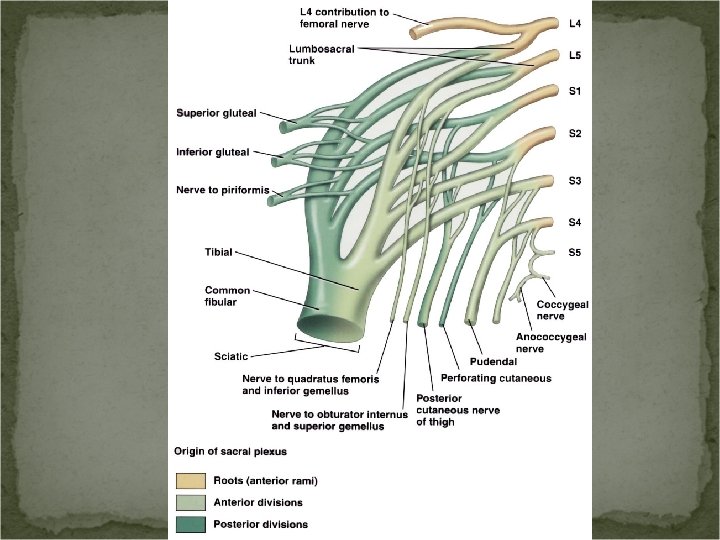
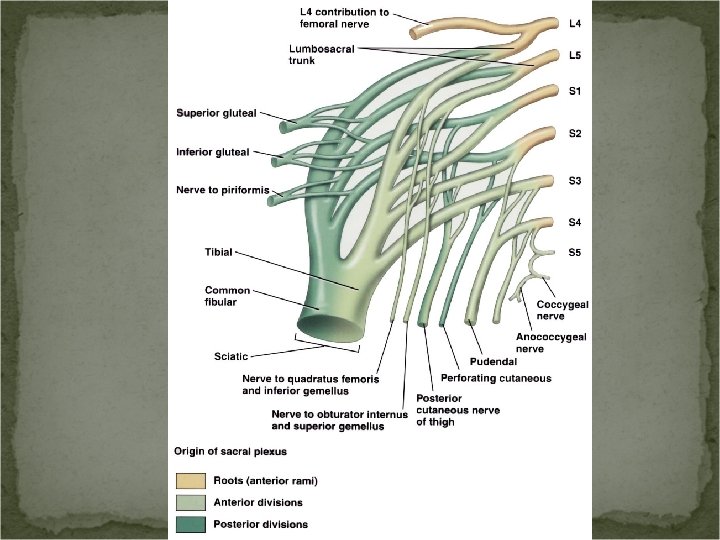
Sacral and Coccygeal Plexuses The sacral plexus supplies the buttocks, perineum and lower limbs. The sciatic nerve originates here. The coccygeal plexus supplies a small patch of skin in the coccygeal region.
Sciatic Nerve Injury to the sciatic nerve causes sciatica – pain the extends from the buttock, down the posterolateral aspect of the leg and to the foot. Damage to the fibular nerve can cause: Footdrop. Equinovarus – inverted foot. Calcaneovalgus – injury of the tibial portion of the sciatic nerve resulting in dorsiflexion.
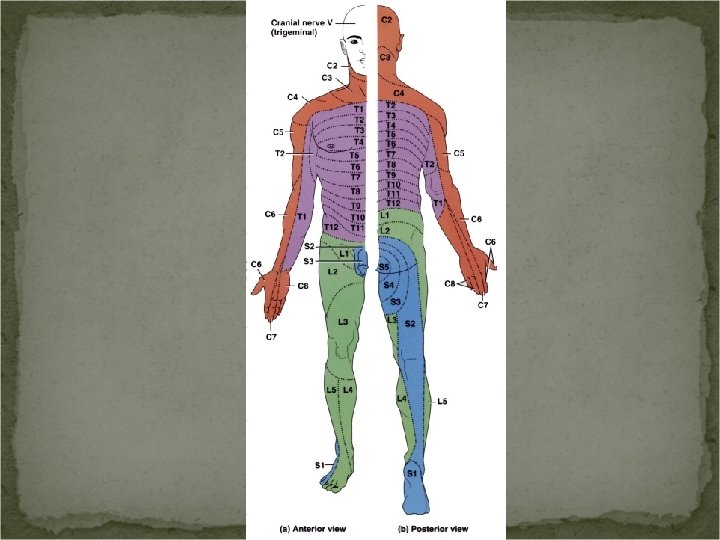
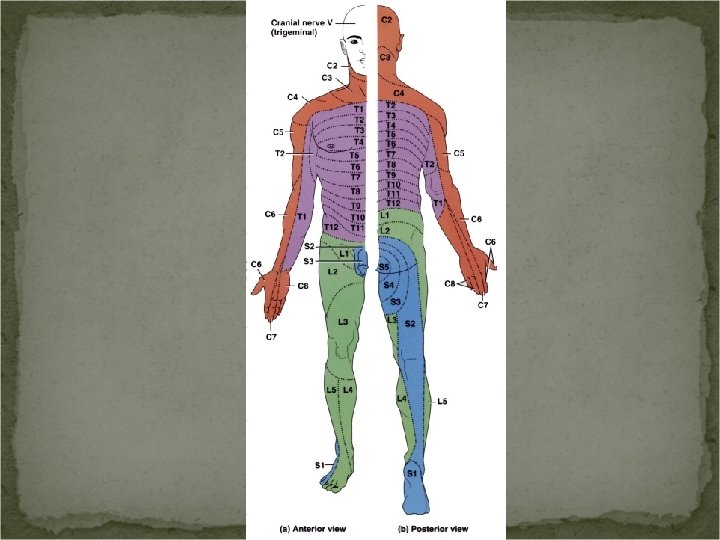
Dermatomes Specific segments of skin that are innervated by specific spinal segments or specific cranial nerves. The nerve supply in adjacent segments overlaps somewhat. Knowing which spinal segments supply each dermatome allows us to determine the location of nerve damage.
Terminolgy Meningitis – inflammation of the meninges. Nerve block – loss of sensation in a region due to injection of a local anesthetic. Neuralgia – pain along the course of a sensory nerve. Neuritis – inflammation of the nerves. Paresthesia – abnormal sensation.