DEGENERATIVE SPINE DISEASE Merve Grkk Spinal cord The



- Slides: 57
DEGENERATIVE SPINE DISEASE Merve Gürkök
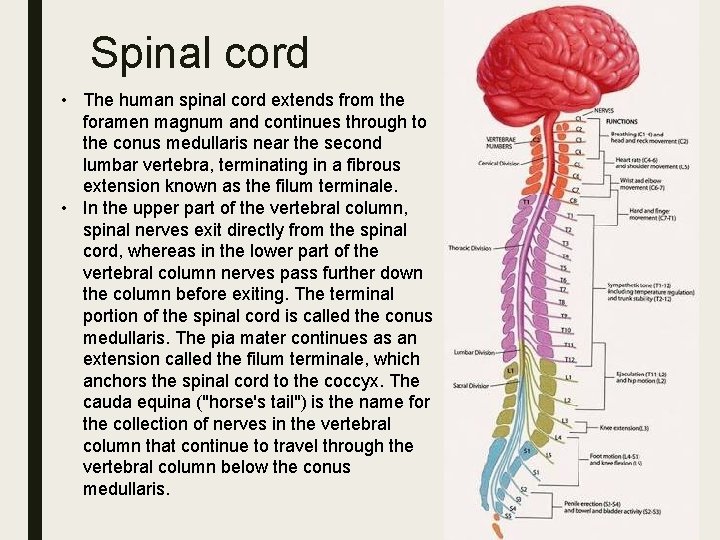
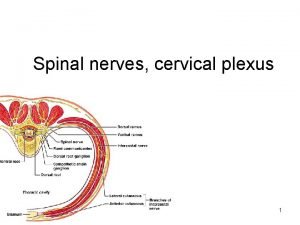
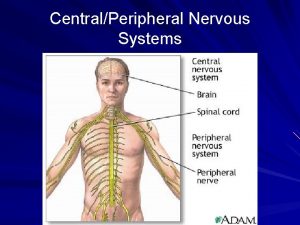
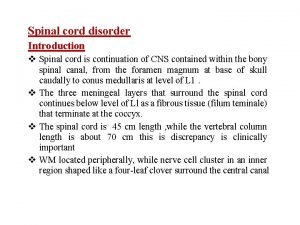
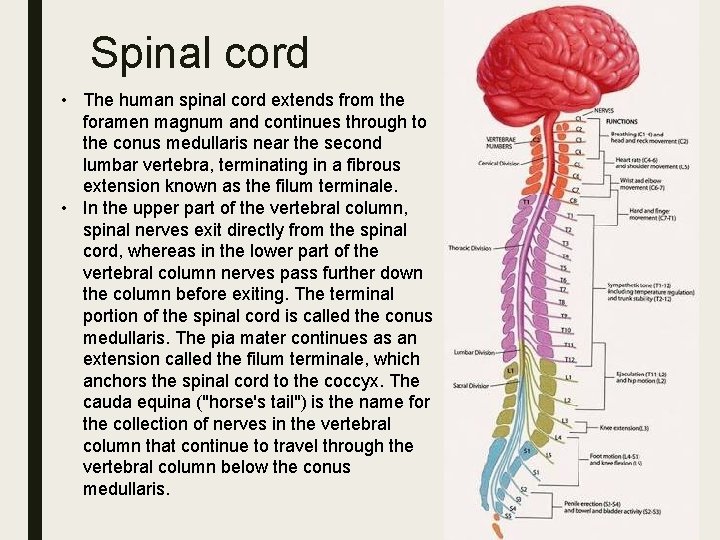
Spinal cord • The human spinal cord extends from the foramen magnum and continues through to the conus medullaris near the second lumbar vertebra, terminating in a fibrous extension known as the filum terminale. • In the upper part of the vertebral column, spinal nerves exit directly from the spinal cord, whereas in the lower part of the vertebral column nerves pass further down the column before exiting. The terminal portion of the spinal cord is called the conus medullaris. The pia mater continues as an extension called the filum terminale, which anchors the spinal cord to the coccyx. The cauda equina ("horse's tail") is the name for the collection of nerves in the vertebral column that continue to travel through the vertebral column below the conus medullaris.
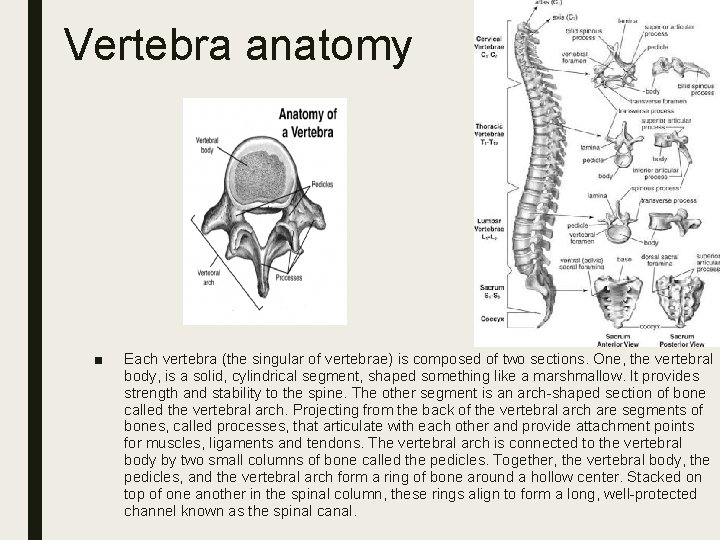
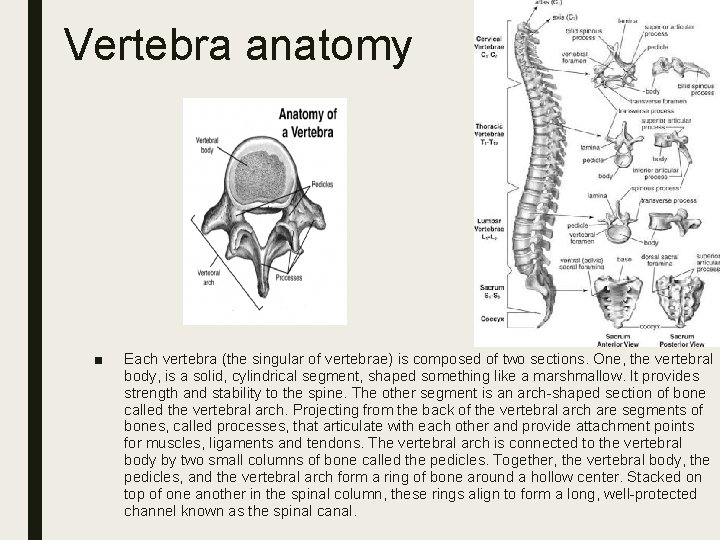
Vertebra anatomy ■ Each vertebra (the singular of vertebrae) is composed of two sections. One, the vertebral body, is a solid, cylindrical segment, shaped something like a marshmallow. It provides strength and stability to the spine. The other segment is an arch-shaped section of bone called the vertebral arch. Projecting from the back of the vertebral arch are segments of bones, called processes, that articulate with each other and provide attachment points for muscles, ligaments and tendons. The vertebral arch is connected to the vertebral body by two small columns of bone called the pedicles. Together, the vertebral body, the pedicles, and the vertebral arch form a ring of bone around a hollow center. Stacked on top of one another in the spinal column, these rings align to form a long, well-protected channel known as the spinal canal.
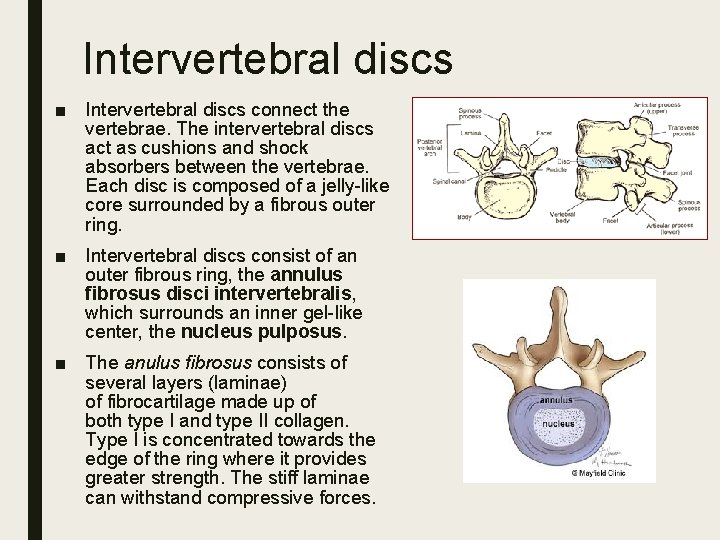
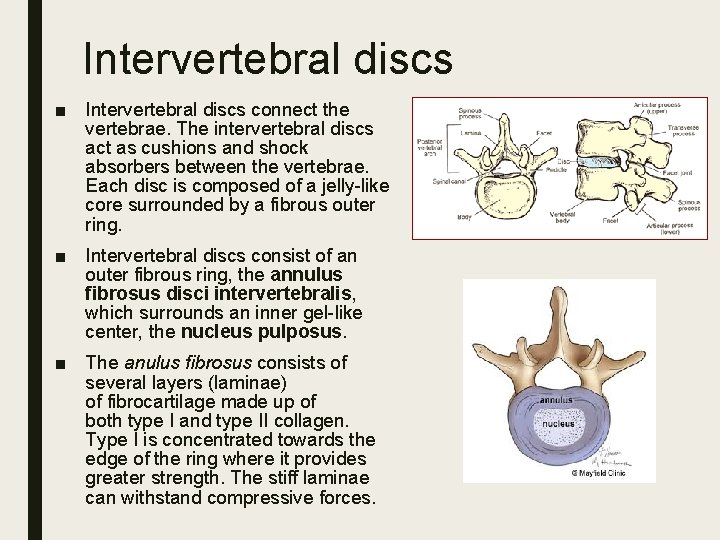
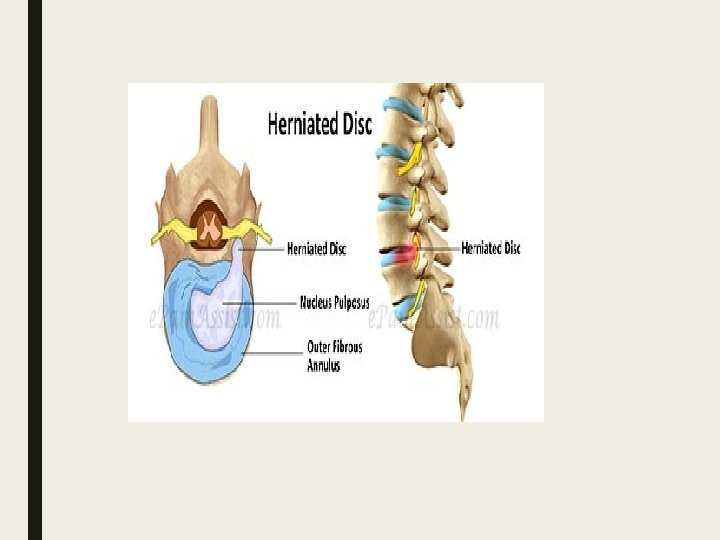
Intervertebral discs ■ Intervertebral discs connect the vertebrae. The intervertebral discs act as cushions and shock absorbers between the vertebrae. Each disc is composed of a jelly-like core surrounded by a fibrous outer ring. ■ Intervertebral discs consist of an outer fibrous ring, the annulus fibrosus disci intervertebralis, which surrounds an inner gel-like center, the nucleus pulposus. ■ The anulus fibrosus consists of several layers (laminae) of fibrocartilage made up of both type I and type II collagen. Type I is concentrated towards the edge of the ring where it provides greater strength. The stiff laminae can withstand compressive forces.
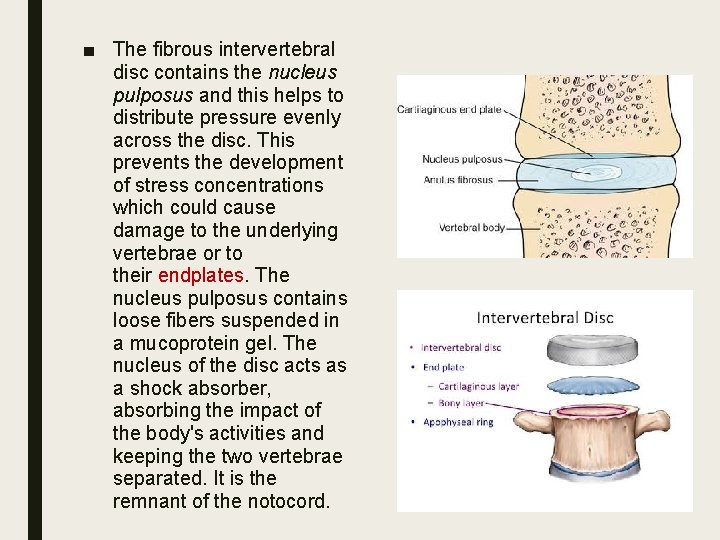
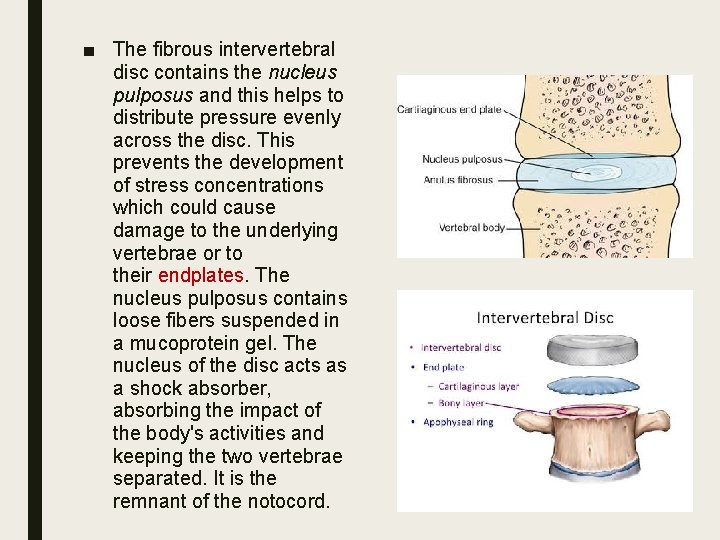
■ The fibrous intervertebral disc contains the nucleus pulposus and this helps to distribute pressure evenly across the disc. This prevents the development of stress concentrations which could cause damage to the underlying vertebrae or to their endplates. The nucleus pulposus contains loose fibers suspended in a mucoprotein gel. The nucleus of the disc acts as a shock absorber, absorbing the impact of the body's activities and keeping the two vertebrae separated. It is the remnant of the notocord.
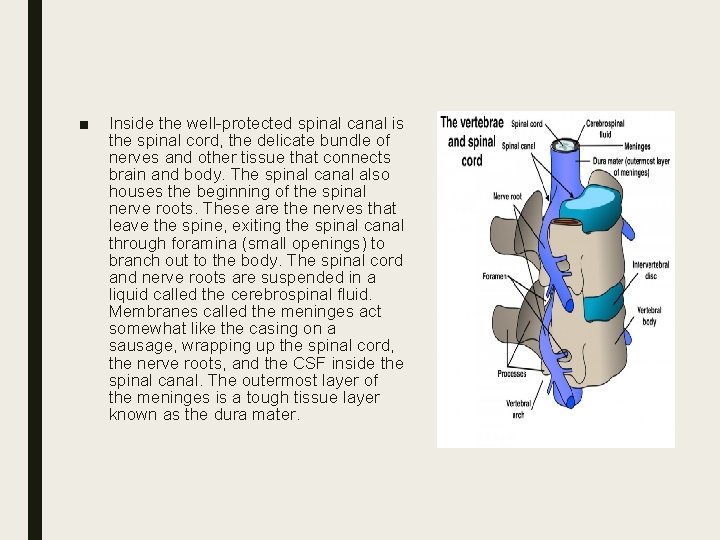
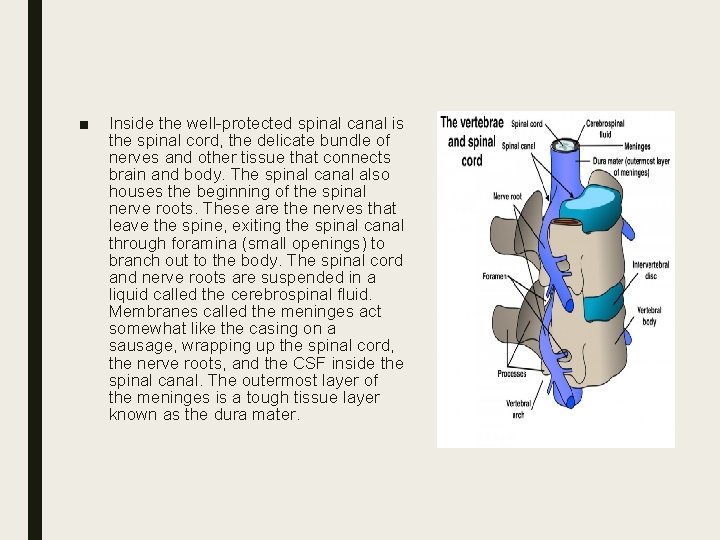
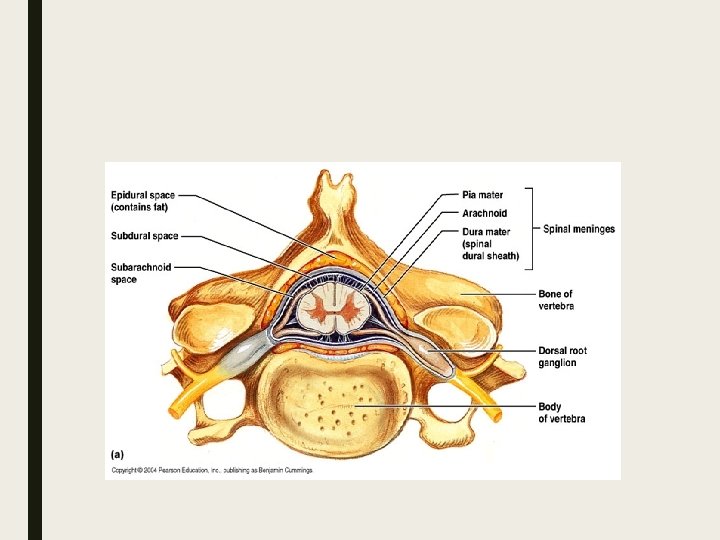
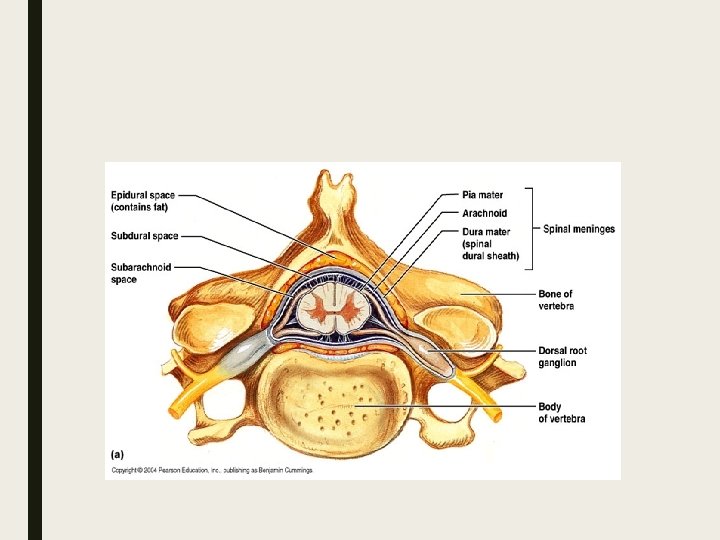
■ Inside the well-protected spinal canal is the spinal cord, the delicate bundle of nerves and other tissue that connects brain and body. The spinal canal also houses the beginning of the spinal nerve roots. These are the nerves that leave the spine, exiting the spinal canal through foramina (small openings) to branch out to the body. The spinal cord and nerve roots are suspended in a liquid called the cerebrospinal fluid. Membranes called the meninges act somewhat like the casing on a sausage, wrapping up the spinal cord, the nerve roots, and the CSF inside the spinal canal. The outermost layer of the meninges is a tough tissue layer known as the dura mater.
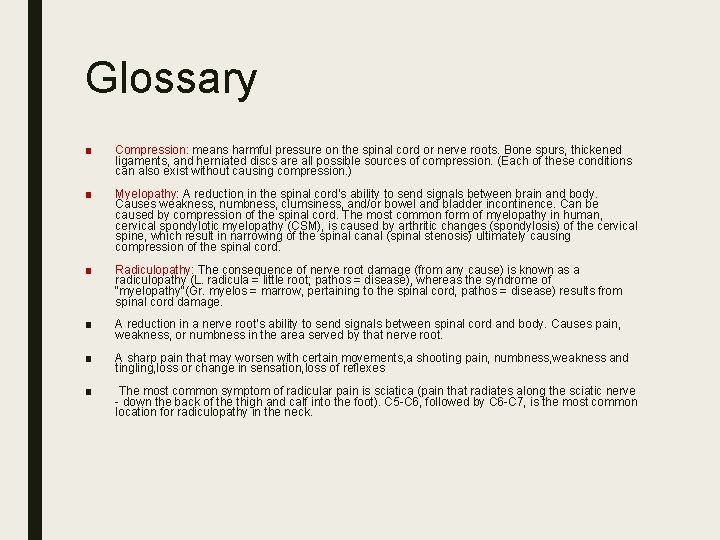
Glossary ■ Compression: means harmful pressure on the spinal cord or nerve roots. Bone spurs, thickened ligaments, and herniated discs are all possible sources of compression. (Each of these conditions can also exist without causing compression. ) ■ Myelopathy: A reduction in the spinal cord’s ability to send signals between brain and body. Causes weakness, numbness, clumsiness, and/or bowel and bladder incontinence. Can be caused by compression of the spinal cord. The most common form of myelopathy in human, cervical spondylotic myelopathy (CSM), is caused by arthritic changes (spondylosis) of the cervical spine, which result in narrowing of the spinal canal (spinal stenosis) ultimately causing compression of the spinal cord. ■ Radiculopathy: The consequence of nerve root damage (from any cause) is known as a radiculopathy (L. radicula = little root; pathos = disease), whereas the syndrome of "myelopathy"(Gr. myelos = marrow, pertaining to the spinal cord, pathos = disease) results from spinal cord damage. ■ A reduction in a nerve root’s ability to send signals between spinal cord and body. Causes pain, weakness, or numbness in the area served by that nerve root. ■ A sharp pain that may worsen with certain movements, a shooting pain, numbness, weakness and tingling, loss or change in sensation, loss of reflexes ■ The most common symptom of radicular pain is sciatica (pain that radiates along the sciatic nerve - down the back of the thigh and calf into the foot). C 5 -C 6, followed by C 6 -C 7, is the most common location for radiculopathy in the neck.
■ Stenosis: a narrowing of the spinal canal. Stenosis can compress the spinal cord or nerve roots and may lead to myelopathy or neurogenic claudication. ■ Arthritis: joint inflammation that causes pain and stiffness. The most common type is osteoarthritis, which occurs when cartilage in the joints wears down. ■ Bone spurs: extra bone that may grow on joints affected by osteoarthritis. Bone spurs may compress the spinal cord or nerve roots.
Symptoms ■ Degenerative spine conditions vary widely in their presentation. Some cause no symptoms at all. When symptoms do occur, they often include back pain or neck pain. Other symptoms depend on the location and type of problem.

Red Flags ■ Back pain accompanied by bowel or bladder incontinence and/or numbness in the areas that would sit on a saddle (so-called saddle anesthesia)—may indicate cauda equina syndrome, a rare neurological condition that should be treated promptly ■ Neck or back pain that includes weakness, numbness, or pins-and-needles in the arms or legs–may indicate myelopathy ■ Neck or back pain that radiates (spreads) into the shoulder, arm, hand, leg, or foot–may indicate radiculopathy ■ Neck or back pain accompanied by fever ■ Neck or back pain that gets worse during the night ■ Neck or back pain accompanied by unexplained weight loss ■ Neck or back pain that continues for several weeks or months ■ Neck pain accompanied by difficulty breathing or swallowing ■ Neck or back pain following a fall, injury or other trauma
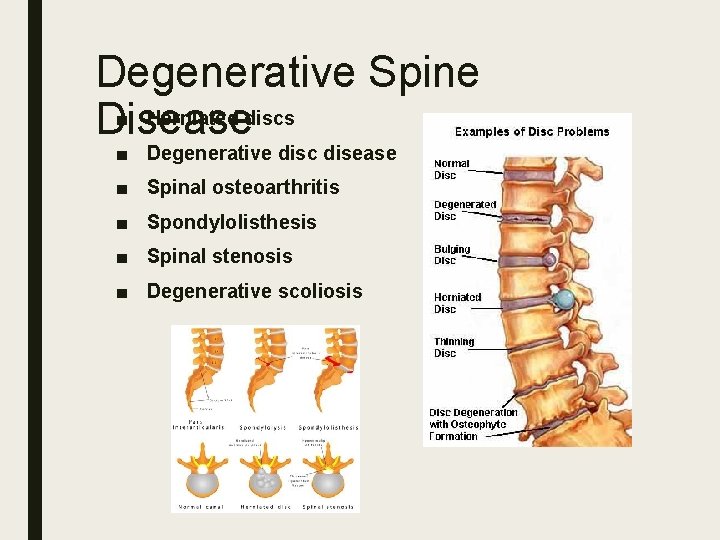
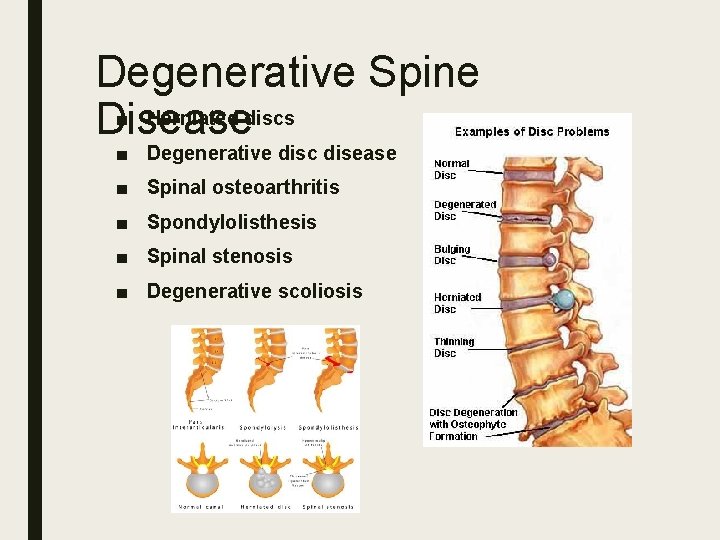
Degenerative Spine ■ Herniated discs Disease ■ Degenerative disc disease ■ Spinal osteoarthritis ■ Spondylolisthesis ■ Spinal stenosis ■ Degenerative scoliosis
Risk factors ■ Aging ■ Genetic predisposition ■ Smoking, diet, weight ■ Occupational (heavy lifting) ■ Sedentary lifestyle
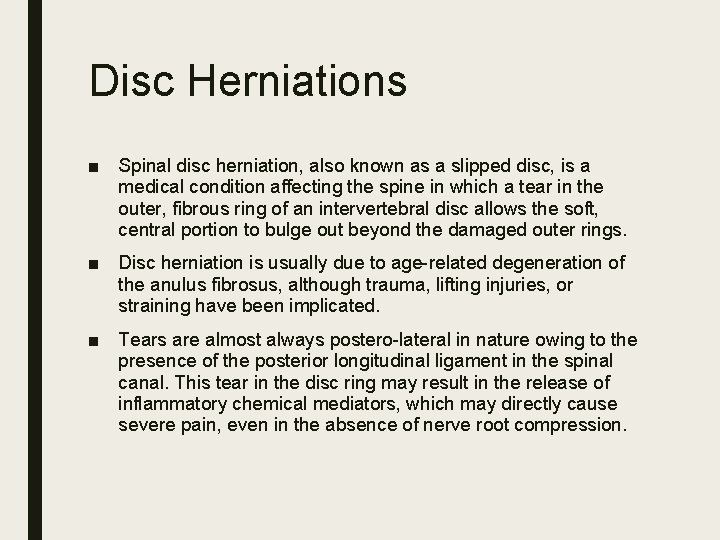
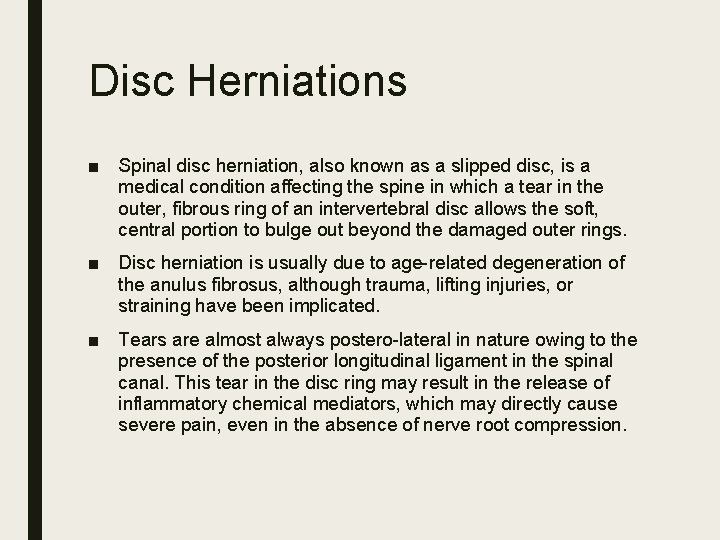
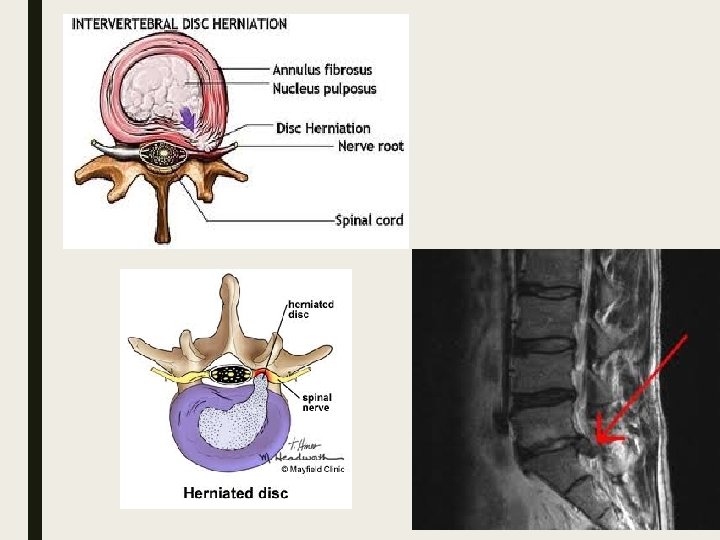
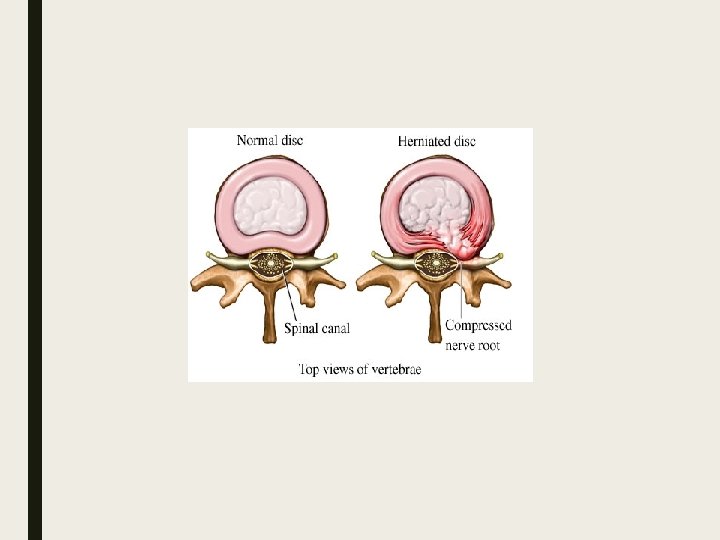
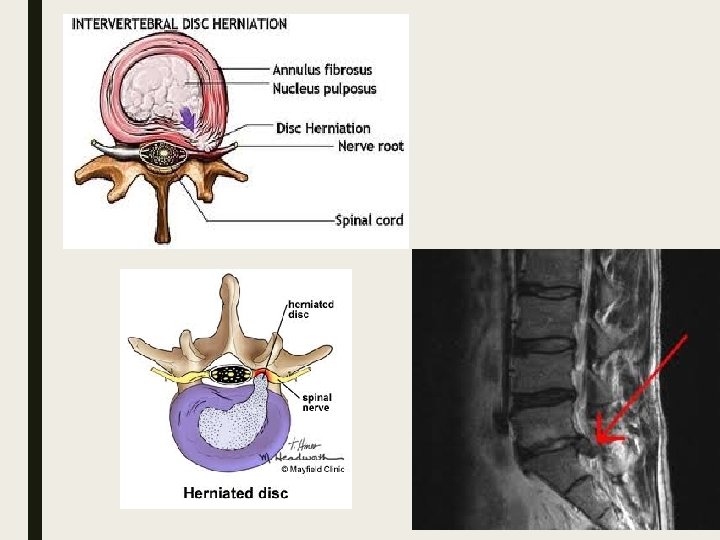
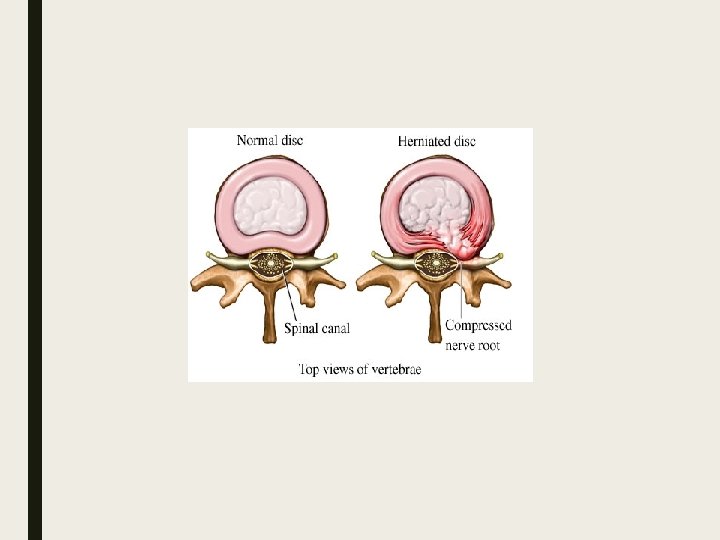
Disc Herniations ■ Spinal disc herniation, also known as a slipped disc, is a medical condition affecting the spine in which a tear in the outer, fibrous ring of an intervertebral disc allows the soft, central portion to bulge out beyond the damaged outer rings. ■ Disc herniation is usually due to age-related degeneration of the anulus fibrosus, although trauma, lifting injuries, or straining have been implicated. ■ Tears are almost always postero-lateral in nature owing to the presence of the posterior longitudinal ligament in the spinal canal. This tear in the disc ring may result in the release of inflammatory chemical mediators, which may directly cause severe pain, even in the absence of nerve root compression.
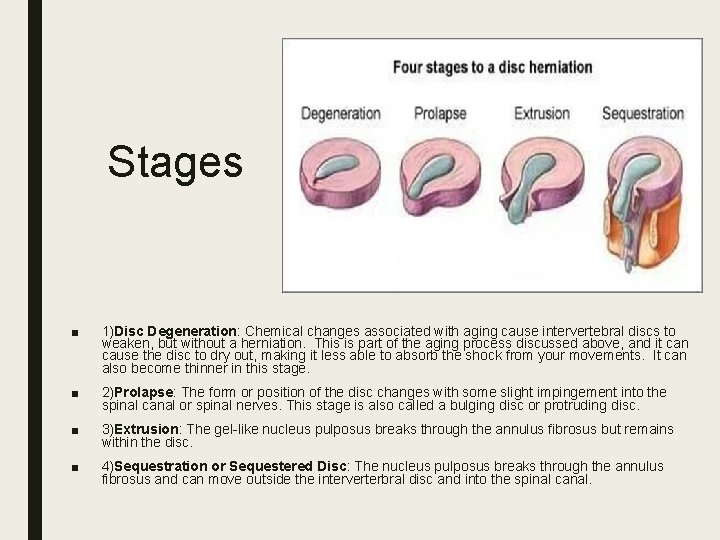
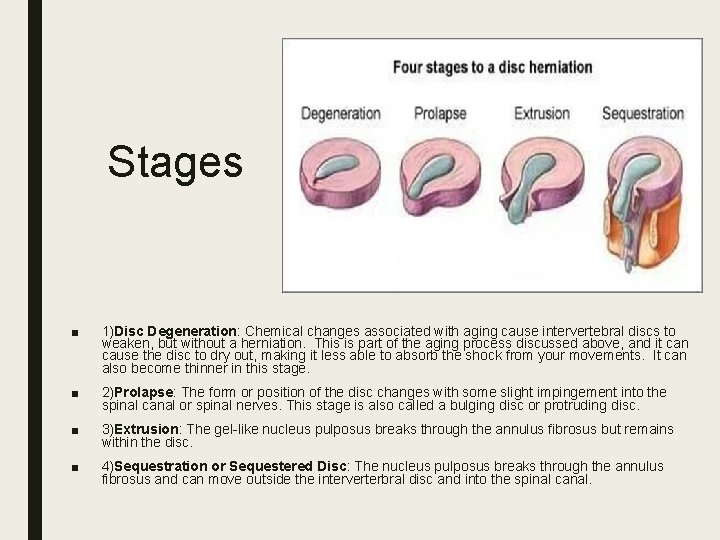
Stages ■ 1)Disc Degeneration: Chemical changes associated with aging cause intervertebral discs to weaken, but without a herniation. This is part of the aging process discussed above, and it can cause the disc to dry out, making it less able to absorb the shock from your movements. It can also become thinner in this stage. ■ 2)Prolapse: The form or position of the disc changes with some slight impingement into the spinal canal or spinal nerves. This stage is also called a bulging disc or protruding disc. ■ 3)Extrusion: The gel-like nucleus pulposus breaks through the annulus fibrosus but remains within the disc. ■ 4)Sequestration or Sequestered Disc: The nucleus pulposus breaks through the annulus fibrosus and can move outside the interverterbral disc and into the spinal canal.
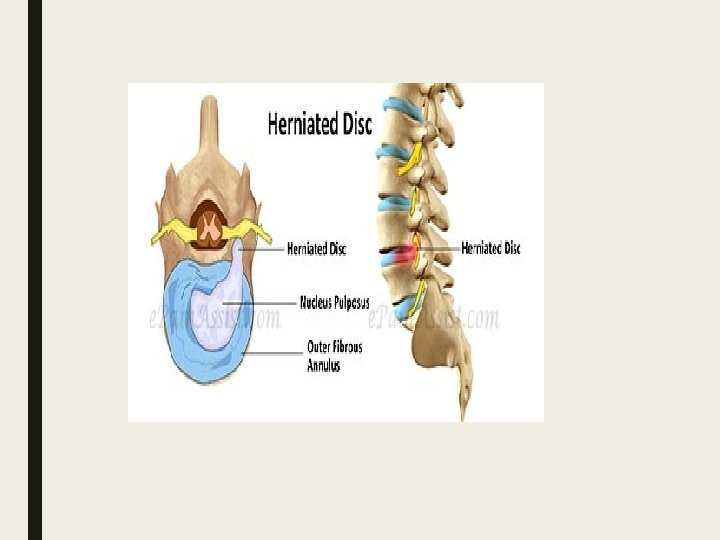
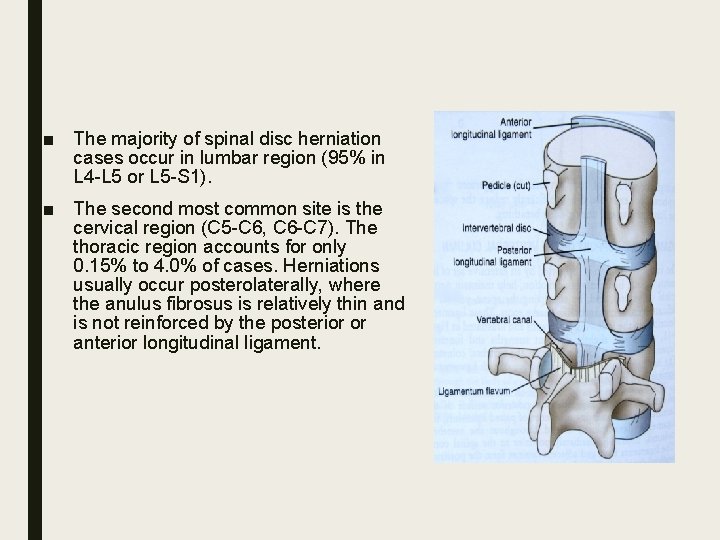
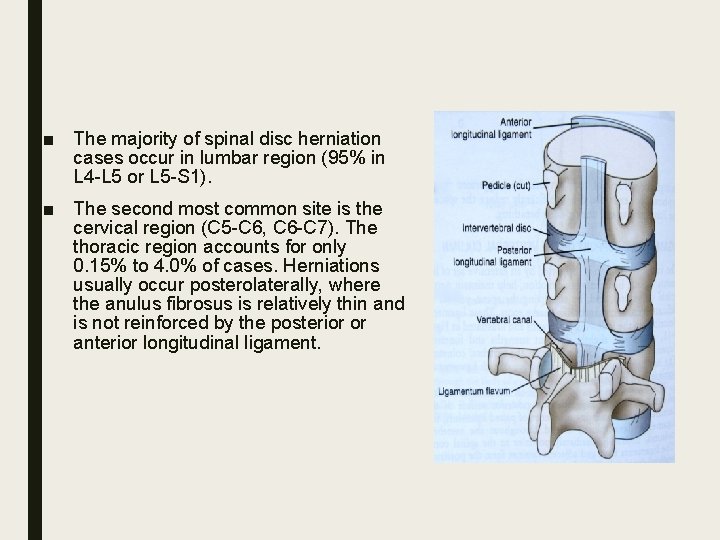
■ The majority of spinal disc herniation cases occur in lumbar region (95% in L 4 -L 5 or L 5 -S 1). ■ The second most common site is the cervical region (C 5 -C 6, C 6 -C 7). The thoracic region accounts for only 0. 15% to 4. 0% of cases. Herniations usually occur posterolaterally, where the anulus fibrosus is relatively thin and is not reinforced by the posterior or anterior longitudinal ligament.
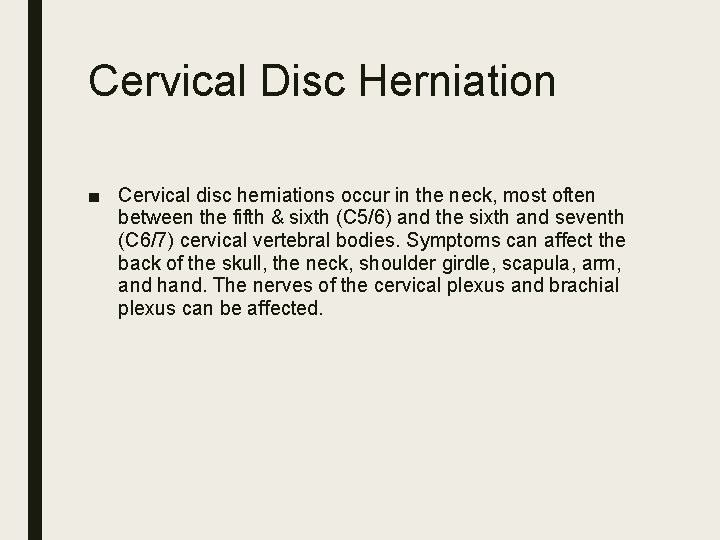
Cervical Disc Herniation ■ Cervical disc herniations occur in the neck, most often between the fifth & sixth (C 5/6) and the sixth and seventh (C 6/7) cervical vertebral bodies. Symptoms can affect the back of the skull, the neck, shoulder girdle, scapula, arm, and hand. The nerves of the cervical plexus and brachial plexus can be affected.
Symptoms ■ Pain(neck, shoulder, arm, hand) ■ Radiculopathy ■ Numbness ■ Muscle weakness ■ Paresthesia ■ Severe cases, a herniated disk can compress nerves that control the bowel and bladder, causing urinary incontinence and loss of bowel control
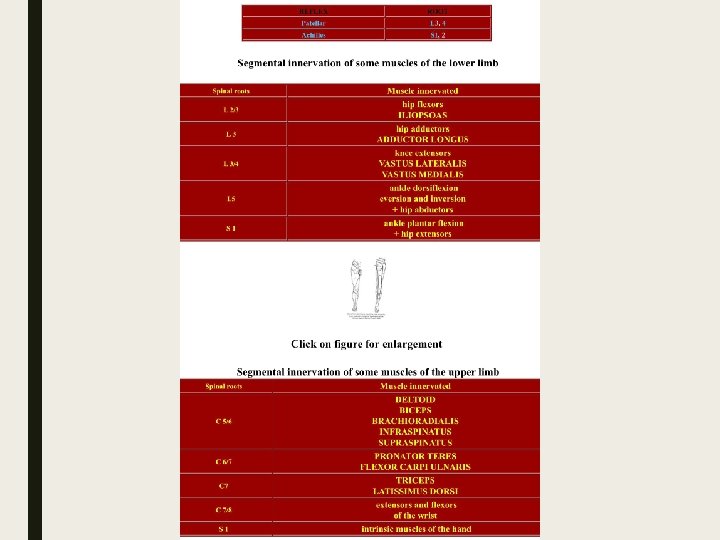
■ C 4 -C 5 (C 5 nerve root): A herniation at this level can cause shoulder pain and weakness in the deltoid muscle at the top of the upper arm, and does not usually cause numbness or tingling. ■ C 5 -C 6 (C 6 nerve root): A C 5 -C 6 disc herniation cause weakness in the biceps (muscles in the front of the upper arms) and wrist extensor muscles. Numbness and tingling along with pain can radiate to the thumb side of the hand. This is one of the most common levels for a cervical disc herniation to occur.
■ C 6 -C 7 (C 7 nerve root): A herniated disc in this area can cause weakness in the triceps (muscles in the back of the upper arm and extending to the forearm) and the finger extensor muscles. Numbness and tingling along with pain can radiate down the triceps and into the middle finger. This level is also one of the most common areas for a cervical disc herniation. ■ C 7 -T 1 (C 8 nerve root): This level is located at the very bottom of the neck, where the cervical spine meets the thoracic, or upper, back. A herniation here can cause weakness with handgrip, along with numbness and tingling and pain that radiates down the arm to the little finger side of hand.
Diagnosis ■ Physical examination ■ MRI(The single best to diagnose a herniated disc is an MRI scan. An MRI scan image any nerve root pinching caused by a herniated cervical disc. ) ■ CT with myelogram (it is more sensitive and can diagnose even subtle cases of nerve root pinching) ■ X-ray ■ EMG
Threatment ■ Medications(NSAID) ■ Physical therapy and exercise ■ Steroid injection ■ Surgery
Surgery ■ Anterior cervical discectomy and spine fusion (ACDF) (This is the most common method among spine surgeons for most cervical herniated discs. ) ■ Posterior cervical discectomy ■ Cervical artificial disc replacement
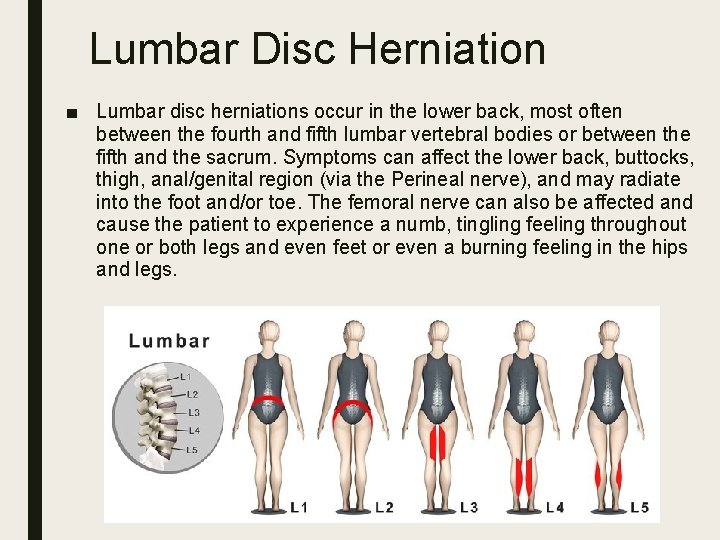
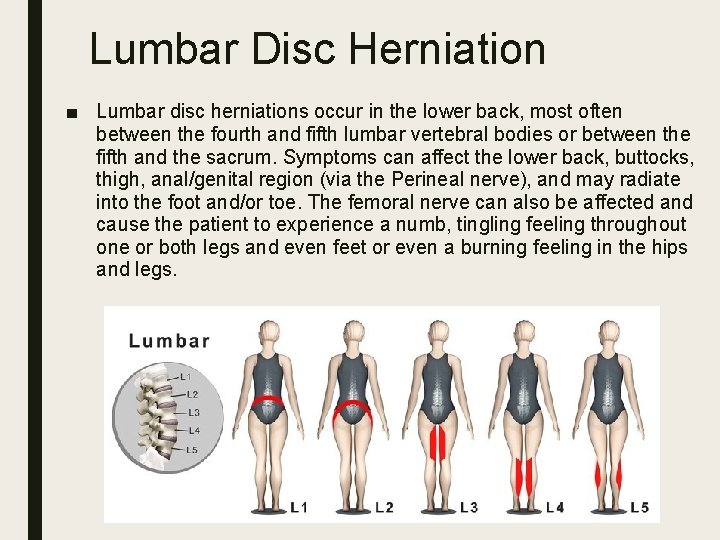
Lumbar Disc Herniation ■ Lumbar disc herniations occur in the lower back, most often between the fourth and fifth lumbar vertebral bodies or between the fifth and the sacrum. Symptoms can affect the lower back, buttocks, thigh, anal/genital region (via the Perineal nerve), and may radiate into the foot and/or toe. The femoral nerve can also be affected and cause the patient to experience a numb, tingling feeling throughout one or both legs and even feet or even a burning feeling in the hips and legs.
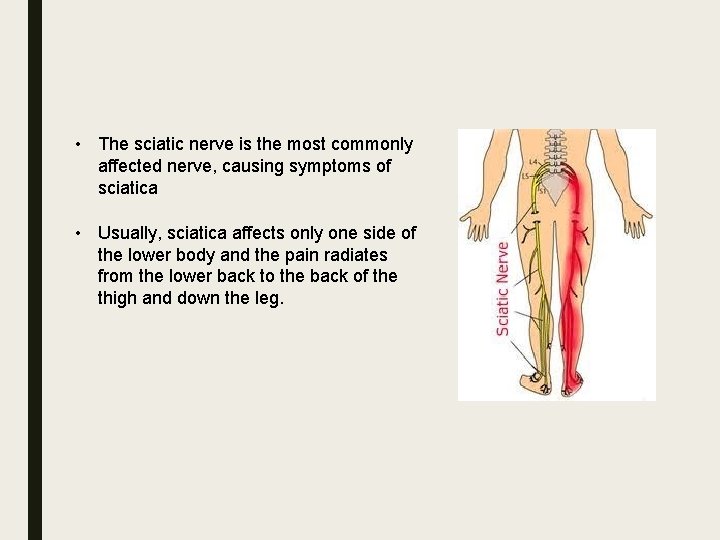
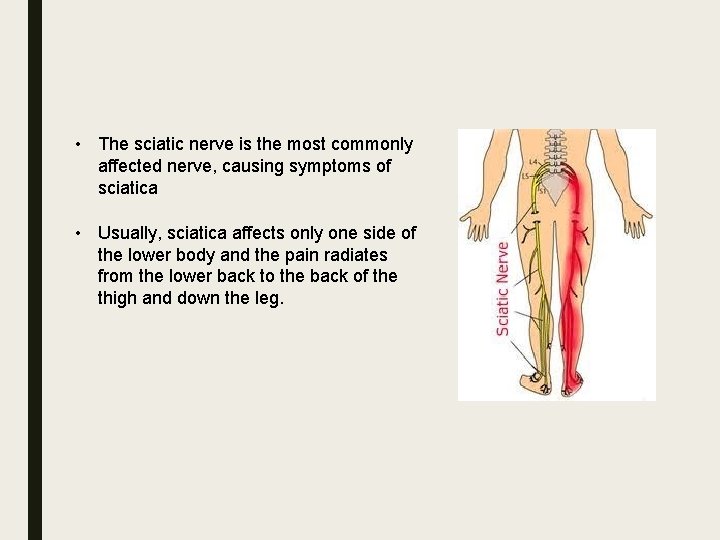
• The sciatic nerve is the most commonly affected nerve, causing symptoms of sciatica • Usually, sciatica affects only one side of the lower body and the pain radiates from the lower back to the back of the thigh and down the leg.
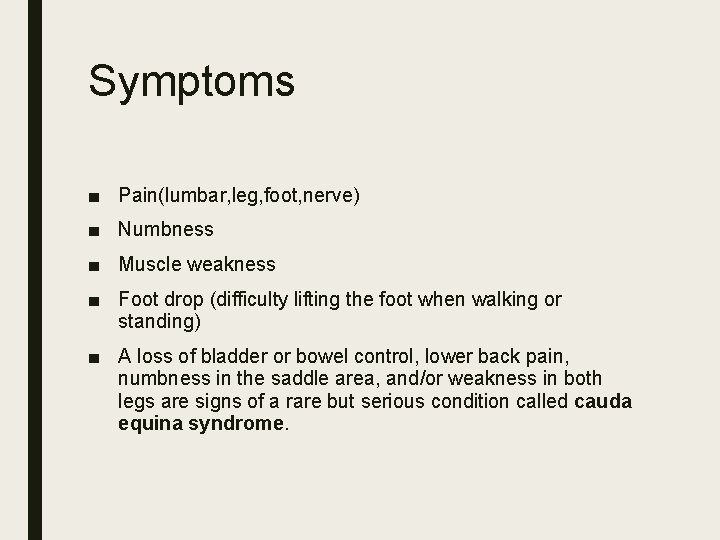
Symptoms ■ Pain(lumbar, leg, foot, nerve) ■ Numbness ■ Muscle weakness ■ Foot drop (difficulty lifting the foot when walking or standing) ■ A loss of bladder or bowel control, lower back pain, numbness in the saddle area, and/or weakness in both legs are signs of a rare but serious condition called cauda equina syndrome.
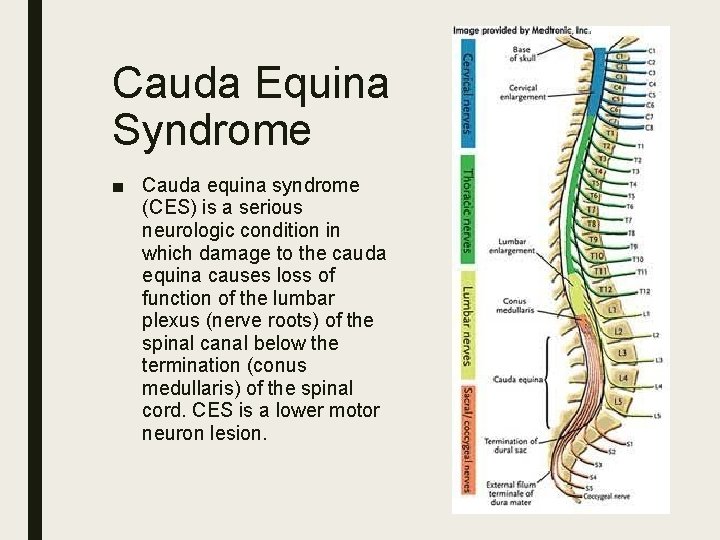
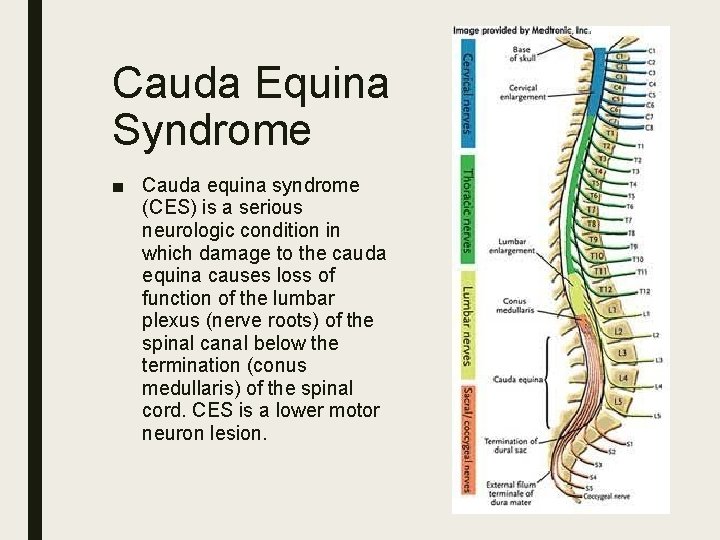
Cauda Equina Syndrome ■ Cauda equina syndrome (CES) is a serious neurologic condition in which damage to the cauda equina causes loss of function of the lumbar plexus (nerve roots) of the spinal canal below the termination (conus medullaris) of the spinal cord. CES is a lower motor neuron lesion.
Symptoms ■ Severe back pain ■ Saddle anesthesia ■ Sciatica-type pain on one side or both sides ■ Bladder and bowel dysfunction ■ Gait disturbance ■ Anal and Achilles reflex absent ■ Sexual dysfunction
Diagnosis ■ Pyhsical examination (Leg raise test) ■ MRI (usually provides the most accurate assessment of the lumbar spine area) ■ CT ■ X-ray ■ EMG
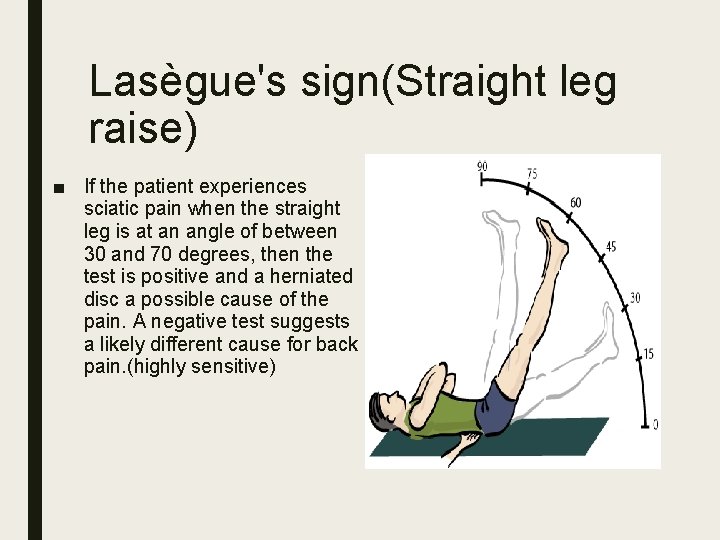
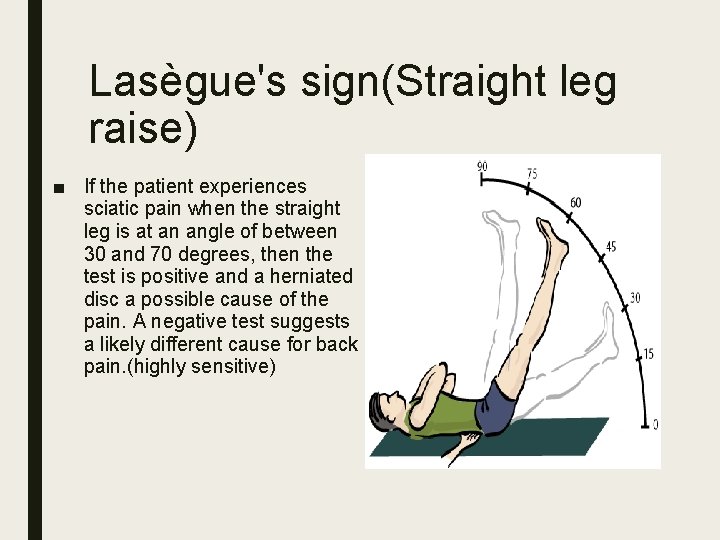
Lasègue's sign(Straight leg raise) ■ If the patient experiences sciatic pain when the straight leg is at an angle of between 30 and 70 degrees, then the test is positive and a herniated disc a possible cause of the pain. A negative test suggests a likely different cause for back pain. (highly sensitive)

Threatment ■ Pain medications ■ Ice application ■ Muscle relaxants ■ Heat therapy ■ Heat and ice ■ Physical therapy ■ Acupuncture ■ Epidural injections ■ Surgery
Surgery may be recommended if: ■ There is severe pain and the person is having difficulty maintaining a reasonable level of daily functions, such as standing or walking. ■ The person is experiencing progressive neurological symptoms, such as worsening leg weakness. and/or numbness ■ There is a loss of bowel and bladder functions. ■ Medication, physical therapy, and/or other nonsurgical treatments have not significantly eased symptoms.
Surgery ■ Two minimally invasive procedures, microdiscectomy and endoscopic microdiscectomy, are most commonly recommended for lumbar herniated discs. These procedures take the pressure off the nerve root and provide a better healing environment for the disc.
Degenerative Disc Disease ■ Degeneration of one or more intervertebral disc(s) of the spine, often called "degenerative disc disease" (DDD) or "degenerative disc disorder, " is a pathologic process of certain pathology that may cause acute or chronic low back or neck pain. The typical radiographic findings in DDD are black discs, disc space narrowing, vacuum disc, end plate sclerosis, and osteophyte formation. DDD can greatly affect the sufferer's quality of life. Disc degeneration is a disease of micro/macro trauma and of aging, and though for most people is not a problem, in certain individuals a degenerated disc can cause severe chronic pain if left untreated.

The two findings most correlated with a pathological disc (a degenerating disc that is painful) are: ■ Cartilaginous end plate erosion ■ Disc space collapse
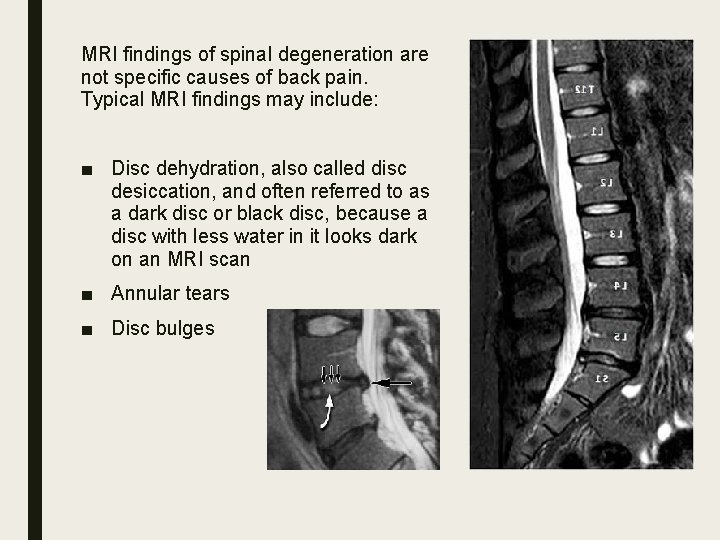
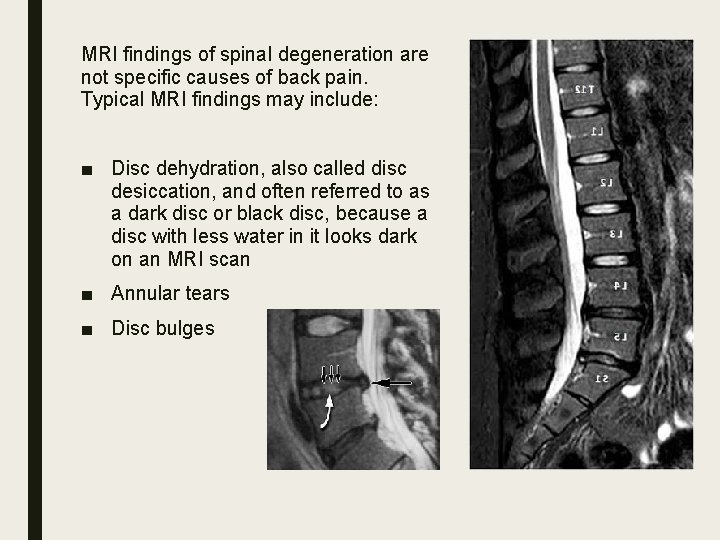
MRI findings of spinal degeneration are not specific causes of back pain. Typical MRI findings may include: ■ Disc dehydration, also called disc desiccation, and often referred to as a dark disc or black disc, because a disc with less water in it looks dark on an MRI scan ■ Annular tears ■ Disc bulges
Symptoms ■ With symptomatic degenerative disc disease, chronic low back pain sometimes radiates to the hips, or there is pain in the buttocks or thighs while walking; sporadic tingling or weakness through the knees, hands, and fingers may also be evident. Similar pain may be felt or may increase while sitting, bending, lifting, and twisting. Chronic neck pain can also come from the cervical spine, with pain radiating to the head, shoulders, arms and hands.
Threatment ■ Pain Control ■ Exercise and Rehabilitation ■ Lifestyle Modifications ■ Surgery
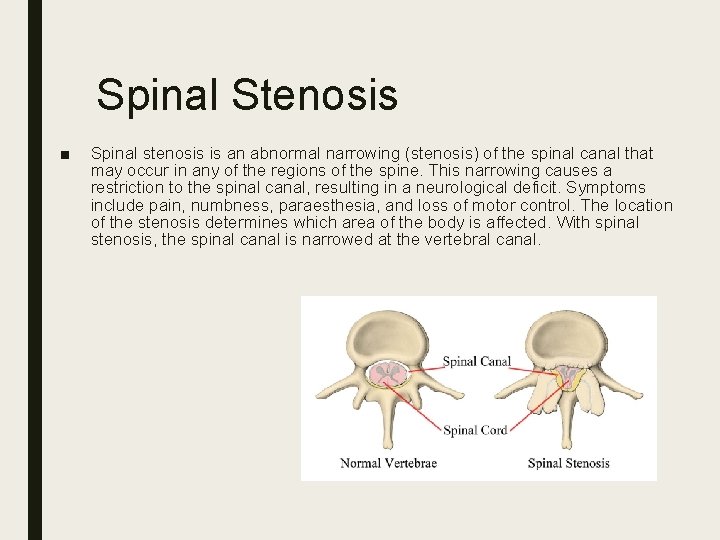
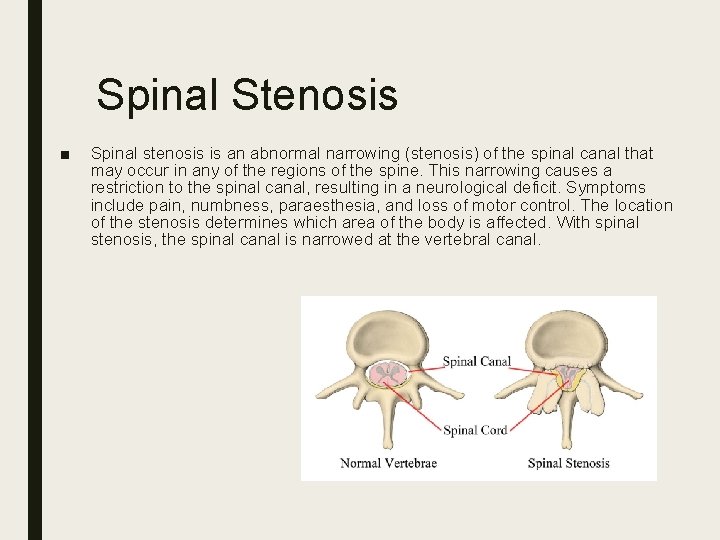
Spinal Stenosis ■ Spinal stenosis is an abnormal narrowing (stenosis) of the spinal canal that may occur in any of the regions of the spine. This narrowing causes a restriction to the spinal canal, resulting in a neurological deficit. Symptoms include pain, numbness, paraesthesia, and loss of motor control. The location of the stenosis determines which area of the body is affected. With spinal stenosis, the spinal canal is narrowed at the vertebral canal.
■ Some people are born with a congenital form, but most develop spinal stenosis as part of the degenerative cascade. A few do not feel any effects of the narrowing, but as part of the aging process, most people will eventually notice radiating pain, weakness, and/or numbness secondary to the compression of the nerves or spinal cord. ■ There are several types of spinal stenosis, with lumbar stenosis and cervical stenosis being the most frequent. While lumbar spinal stenosis is more common, cervical spinal stenosis is more dangerous because it involves compression of the spinal cord whereas the lumbar spinal stenosis involves compression of the cauda equina.
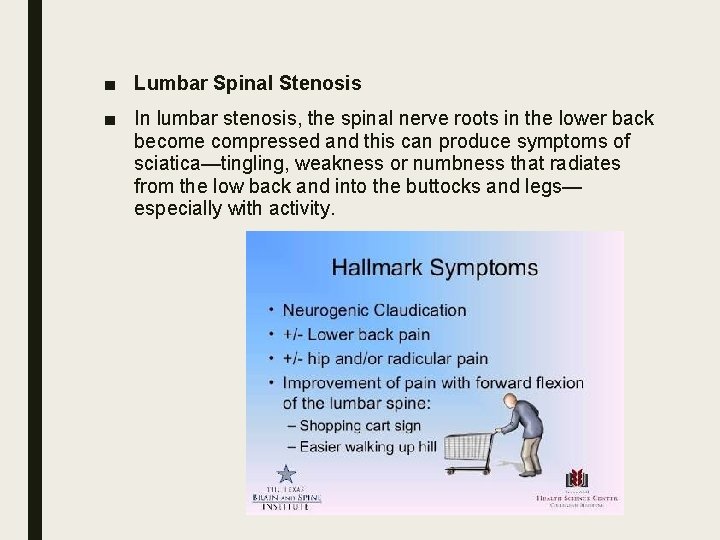
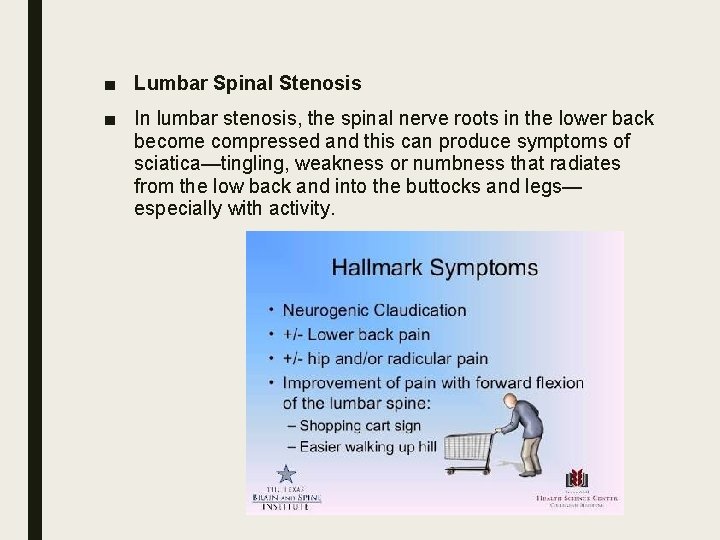
■ Lumbar Spinal Stenosis ■ In lumbar stenosis, the spinal nerve roots in the lower back become compressed and this can produce symptoms of sciatica—tingling, weakness or numbness that radiates from the low back and into the buttocks and legs— especially with activity.
Symptoms ■ Standing discomfort (94%) ■ Discomfort/pain, in shoulder, arm, hand (78%) ■ Bilateral symptoms (68%) ■ Numbness (63%) ■ Weakness (43%) ■ Buttock / Thigh only (8%) ■ Below the knee (3%) ■ Cervical (spondylotic) myelopathy ■ Numbness ■ Intermittent neurogenic claudication ■ Cauda Equina Syndrome
Threatment ■ Posterior laminectomy/laminoplasti ■ Anterior Cervical Discectomy and fusion
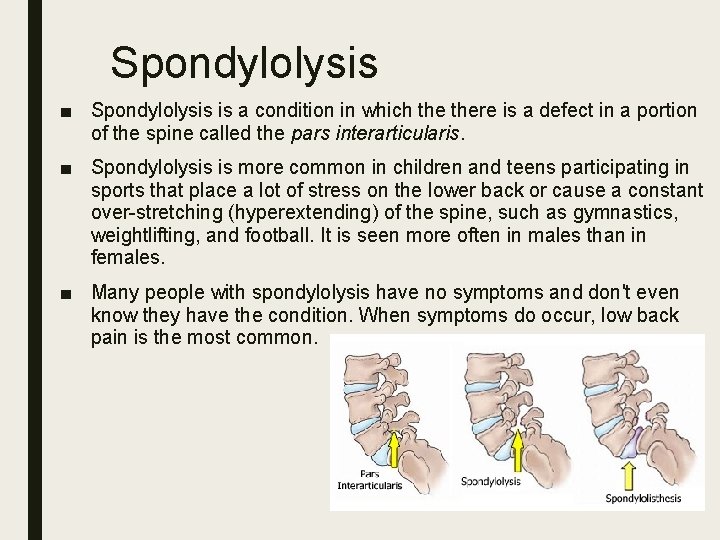
Spondylolysis ■ Spondylolysis is a condition in which there is a defect in a portion of the spine called the pars interarticularis. ■ Spondylolysis is more common in children and teens participating in sports that place a lot of stress on the lower back or cause a constant over-stretching (hyperextending) of the spine, such as gymnastics, weightlifting, and football. It is seen more often in males than in females. ■ Many people with spondylolysis have no symptoms and don't even know they have the condition. When symptoms do occur, low back pain is the most common.
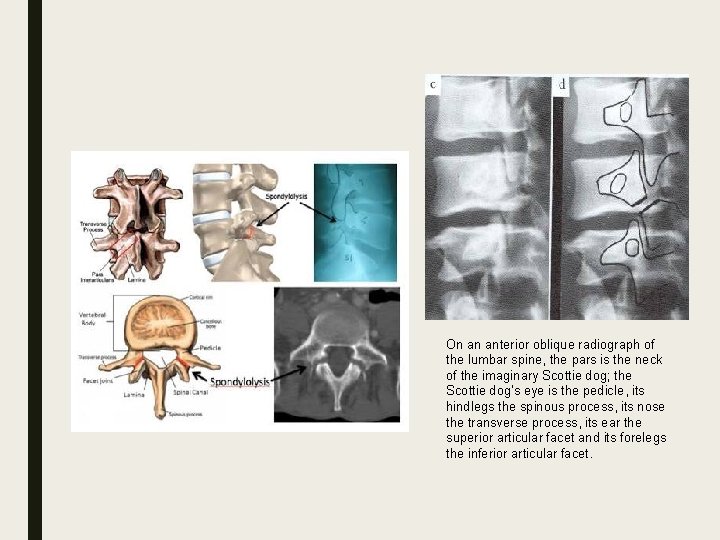
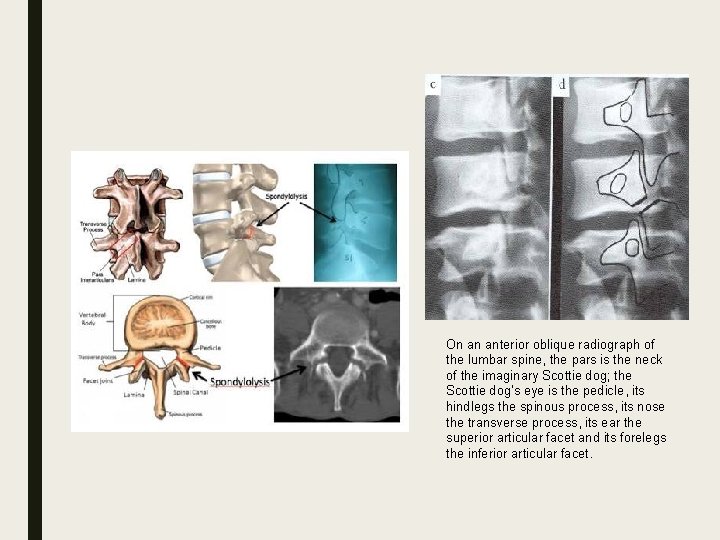
On an anterior oblique radiograph of the lumbar spine, the pars is the neck of the imaginary Scottie dog; the Scottie dog's eye is the pedicle, its hindlegs the spinous process, its nose the transverse process, its ear the superior articular facet and its forelegs the inferior articular facet.
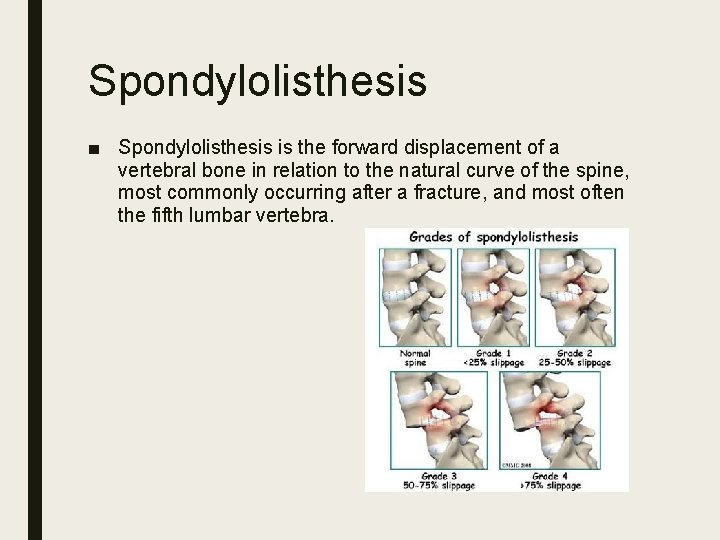
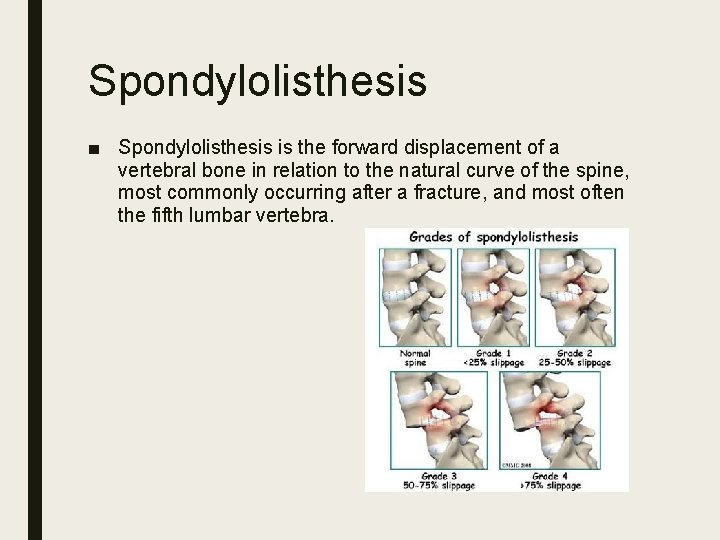
Spondylolisthesis ■ Spondylolisthesis is the forward displacement of a vertebral bone in relation to the natural curve of the spine, most commonly occurring after a fracture, and most often the fifth lumbar vertebra.
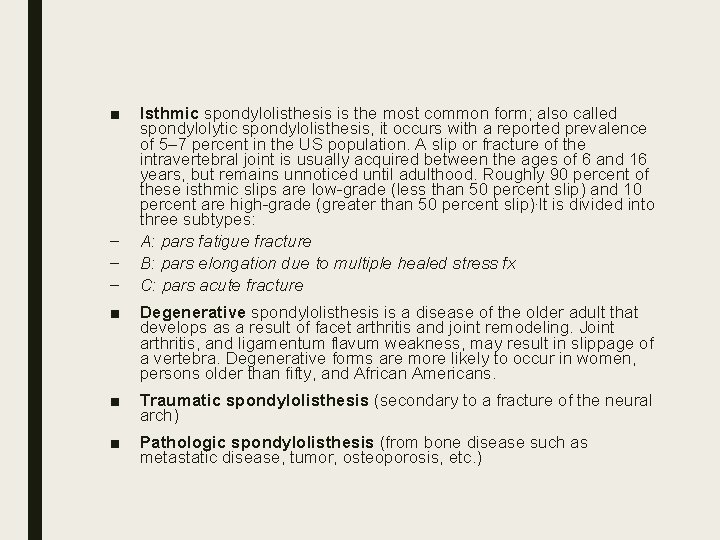
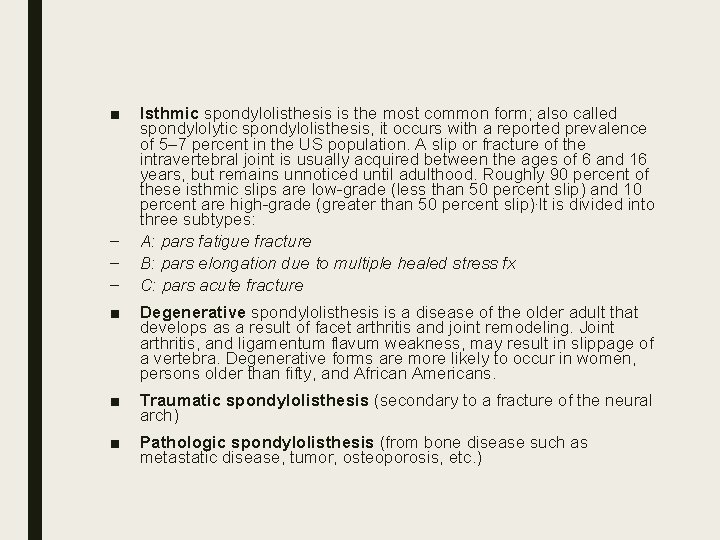
■ – – – Isthmic spondylolisthesis is the most common form; also called spondylolytic spondylolisthesis, it occurs with a reported prevalence of 5– 7 percent in the US population. A slip or fracture of the intravertebral joint is usually acquired between the ages of 6 and 16 years, but remains unnoticed until adulthood. Roughly 90 percent of these isthmic slips are low-grade (less than 50 percent slip) and 10 percent are high-grade (greater than 50 percent slip). It is divided into three subtypes: A: pars fatigue fracture B: pars elongation due to multiple healed stress fx C: pars acute fracture ■ Degenerative spondylolisthesis is a disease of the older adult that develops as a result of facet arthritis and joint remodeling. Joint arthritis, and ligamentum flavum weakness, may result in slippage of a vertebra. Degenerative forms are more likely to occur in women, persons older than fifty, and African Americans. ■ Traumatic spondylolisthesis (secondary to a fracture of the neural arch) ■ Pathologic spondylolisthesis (from bone disease such as metastatic disease, tumor, osteoporosis, etc. )
Symptoms ■ A general stiffening of the back and a tightening of the hamstrings, with a resulting change in both posture and gait. ■ A leaning-forward or semi-kyphotic posture may be seen, due to compensatory changes. ■ A "waddle" may be seen in more advanced causes, due to compensatory pelvic rotation due to decreased lumbar spine rotation. ■ A result of the change in gait is often a noticeable atrophy in the gluteal muscles due to lack of use. ■ Generalized lower-back pain may also be seen, with intermittent shooting pain from the buttocks to the posterior thigh, and/or lower leg via the sciatic nerve.
Threatment ■ NSAID ■ Pysical therapy ■ Surgical(laminectomy)
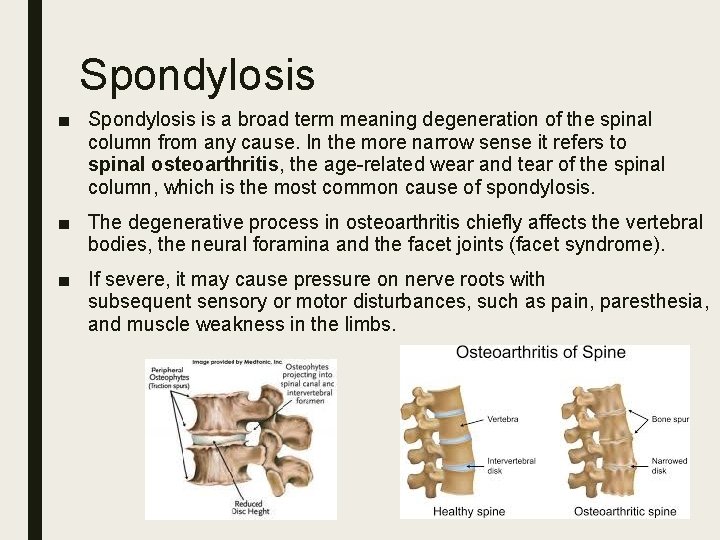
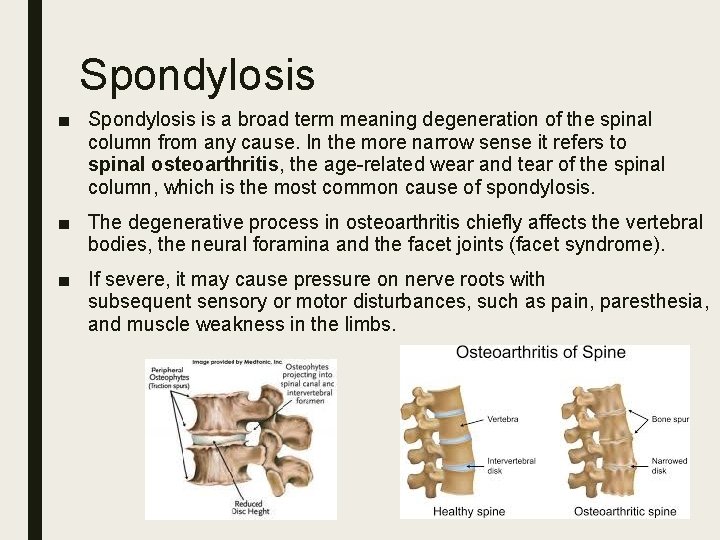
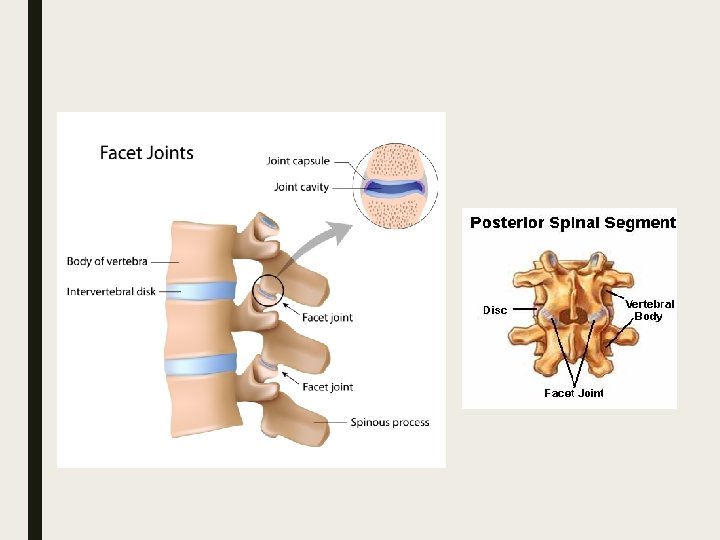
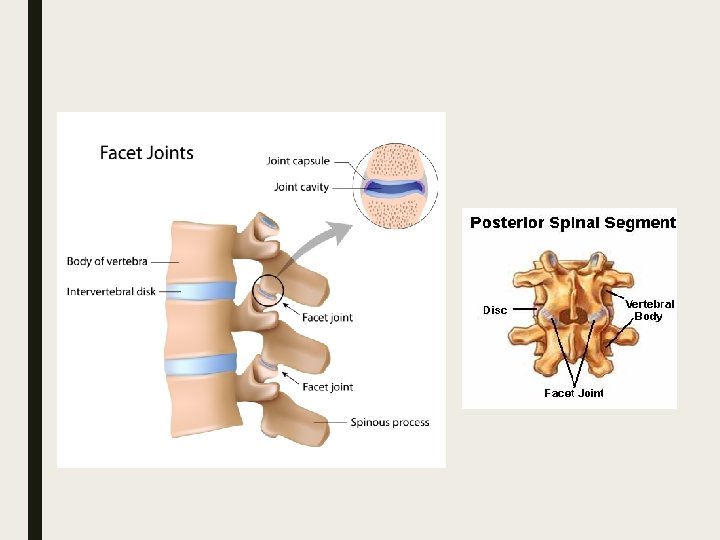
Spondylosis ■ Spondylosis is a broad term meaning degeneration of the spinal column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related wear and tear of the spinal column, which is the most common cause of spondylosis. ■ The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints (facet syndrome). ■ If severe, it may cause pressure on nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, and muscle weakness in the limbs.
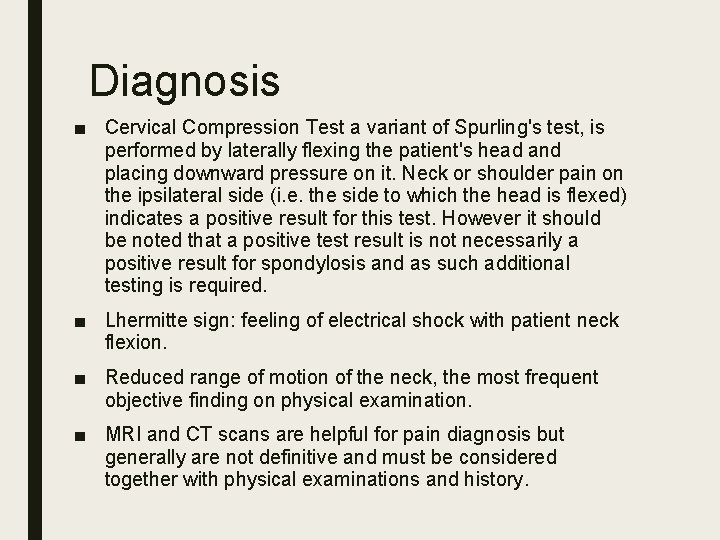
Diagnosis ■ Cervical Compression Test a variant of Spurling's test, is performed by laterally flexing the patient's head and placing downward pressure on it. Neck or shoulder pain on the ipsilateral side (i. e. the side to which the head is flexed) indicates a positive result for this test. However it should be noted that a positive test result is not necessarily a positive result for spondylosis and as such additional testing is required. ■ Lhermitte sign: feeling of electrical shock with patient neck flexion. ■ Reduced range of motion of the neck, the most frequent objective finding on physical examination. ■ MRI and CT scans are helpful for pain diagnosis but generally are not definitive and must be considered together with physical examinations and history.
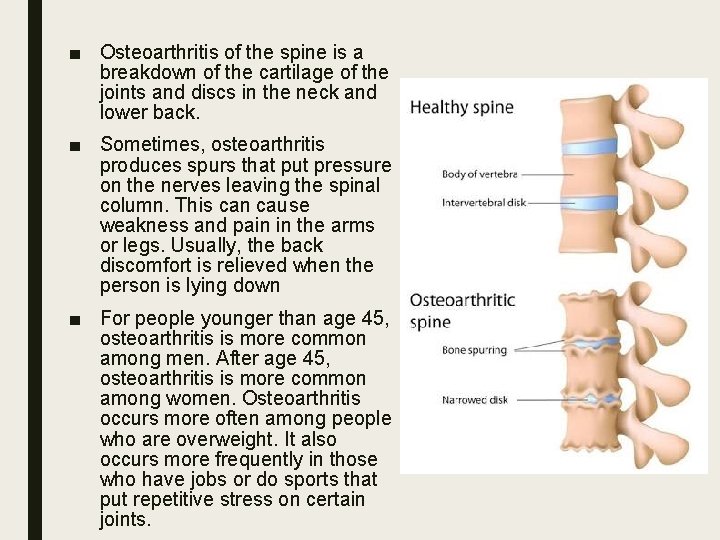
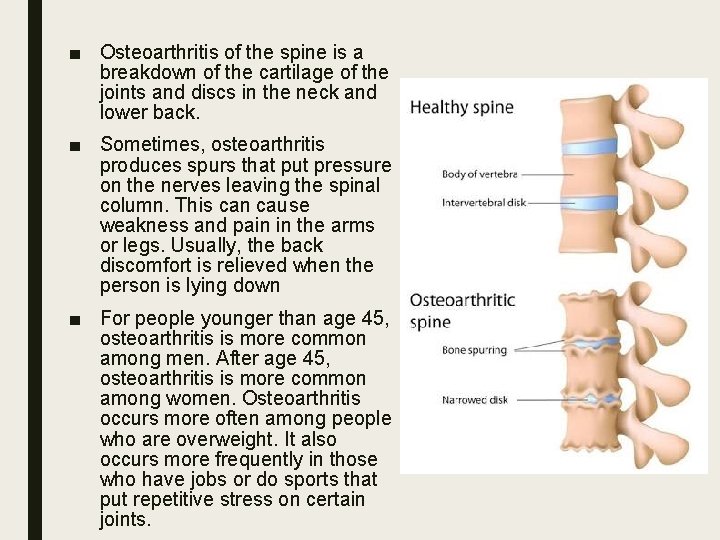
■ Osteoarthritis of the spine is a breakdown of the cartilage of the joints and discs in the neck and lower back. ■ Sometimes, osteoarthritis produces spurs that put pressure on the nerves leaving the spinal column. This can cause weakness and pain in the arms or legs. Usually, the back discomfort is relieved when the person is lying down ■ For people younger than age 45, osteoarthritis is more common among men. After age 45, osteoarthritis is more common among women. Osteoarthritis occurs more often among people who are overweight. It also occurs more frequently in those who have jobs or do sports that put repetitive stress on certain joints.
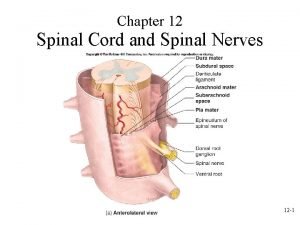
 The spinal nerves
The spinal nerves Exercise 15 spinal cord and spinal nerves
Exercise 15 spinal cord and spinal nerves Ligamentum denticulatum
Ligamentum denticulatum Spinal nerves labled
Spinal nerves labled Degenerative myelopathy wayne
Degenerative myelopathy wayne Degenerative disc
Degenerative disc Frogs kingdom meaning
Frogs kingdom meaning Central canal
Central canal Formation of csf
Formation of csf Spinal refleks
Spinal refleks Mezgovnice
Mezgovnice Components of reflex arc
Components of reflex arc Spinal cord injury rehabilitation st. louis
Spinal cord injury rehabilitation st. louis Spine meninges
Spine meninges Spinomedullary junction
Spinomedullary junction Renshaw cell inhibition
Renshaw cell inhibition Eat well live well
Eat well live well Causes of spinal cord compression
Causes of spinal cord compression Back hurts
Back hurts Nerves branching beyond the spinal cord into the body
Nerves branching beyond the spinal cord into the body Dura mater meaning
Dura mater meaning Spinal cord
Spinal cord Spinal shock symptoms
Spinal shock symptoms The spinal nerves
The spinal nerves Corticospinal tracts
Corticospinal tracts Spinal cord injury protocol
Spinal cord injury protocol Scottie dog lumbar spine
Scottie dog lumbar spine Nice spinal cord compression
Nice spinal cord compression Spinal cord
Spinal cord Vestibulospinal tract
Vestibulospinal tract Oligodendrocyte histology
Oligodendrocyte histology Anterior commissure of spinal cord
Anterior commissure of spinal cord Articularis cubiti muscle
Articularis cubiti muscle Spinebreal code
Spinebreal code Spinal cord
Spinal cord Spinal cord cross section
Spinal cord cross section Autonomic nervous system table
Autonomic nervous system table Spinal angiogram
Spinal angiogram Spinal cord muscles
Spinal cord muscles Spinal cord development
Spinal cord development Boston scientific spinal cord stimulator
Boston scientific spinal cord stimulator Spinal cord
Spinal cord Division of spinal cord
Division of spinal cord Christopher reeve spinal cord injury level
Christopher reeve spinal cord injury level Spinal cord diagram
Spinal cord diagram Spinal cord denticulate ligament
Spinal cord denticulate ligament Spinal cord parts
Spinal cord parts Tissue
Tissue Spinal cord
Spinal cord Neural circuits the organization of neuronal pools
Neural circuits the organization of neuronal pools Spinal cord diagram
Spinal cord diagram Dendirites
Dendirites Pain pathway spinal cord
Pain pathway spinal cord Extrapyramidal tract function
Extrapyramidal tract function Spinal cord and brain
Spinal cord and brain Somi brace
Somi brace Dermatome map
Dermatome map What covers spinal cord
What covers spinal cord