The Thigh and Knee 1 Compartments Anterior Medial
- Slides: 56
The Thigh and Knee 1. Compartments Anterior Medial Posterior 2. Knee 3. Biomechanics
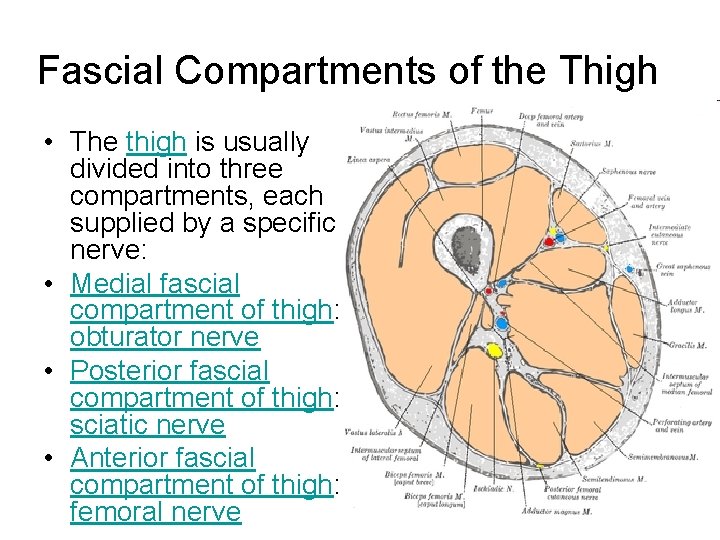
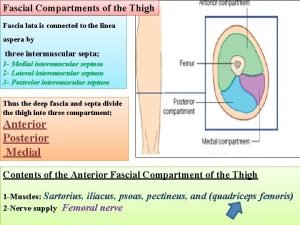
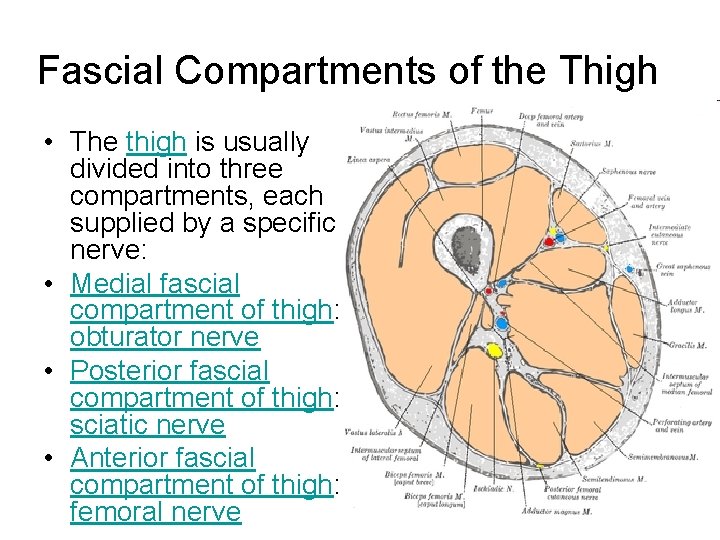
Fascial Compartments of the Thigh • The thigh is usually divided into three compartments, each supplied by a specific nerve: • Medial fascial compartment of thigh: obturator nerve • Posterior fascial compartment of thigh: sciatic nerve • Anterior fascial compartment of thigh: femoral nerve
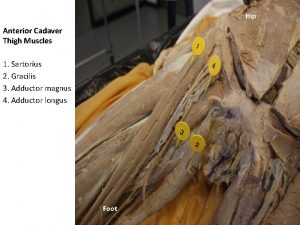
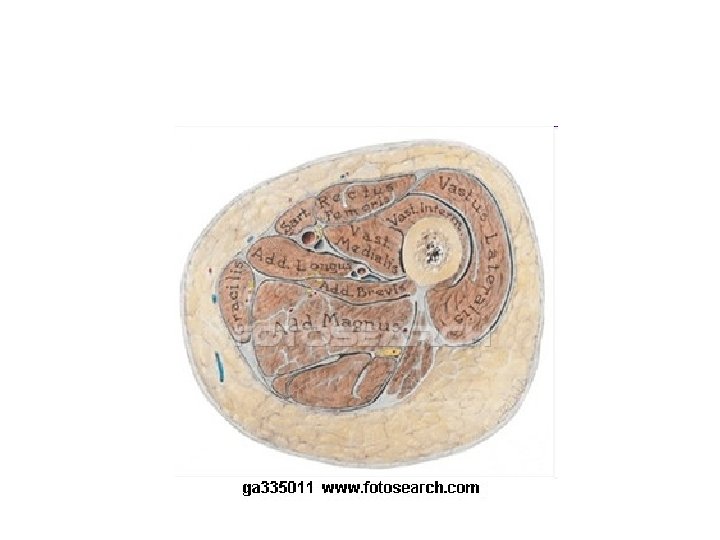
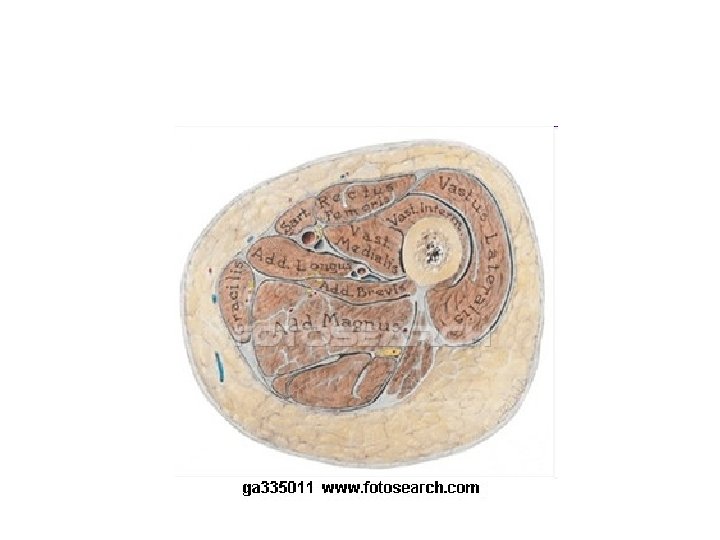
Compartments of the Thigh: Muscles and other contents • Anterior : sartorius · quadriceps (rectus femoris, vastus lateralis, vastus intermedius, vastus medialis) · articularis genu • Posterior/hamstring: biceps femoris · semitendinosus · semimembranosus • Medial: pectineus · obturator externus · gracilis · adductor (longus, brevis, magnus, minimus) • Fascia Femoral sheath (Femoral canal) · Femoral ring Adductor canal · Adductor hiatus • fascia lata (Iliotibial tract, Lateral intermuscular septum of thigh, Medial intermuscular septum of thigh, Fascia cribrosa/Saphenous opening) · Muscular lacuna
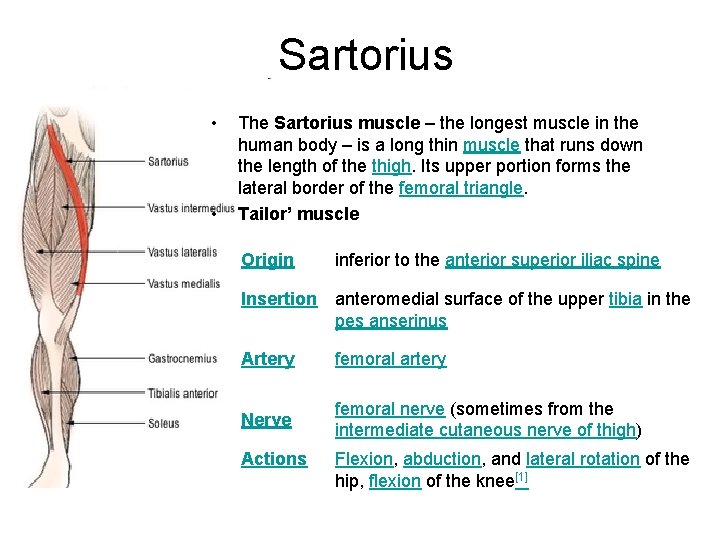
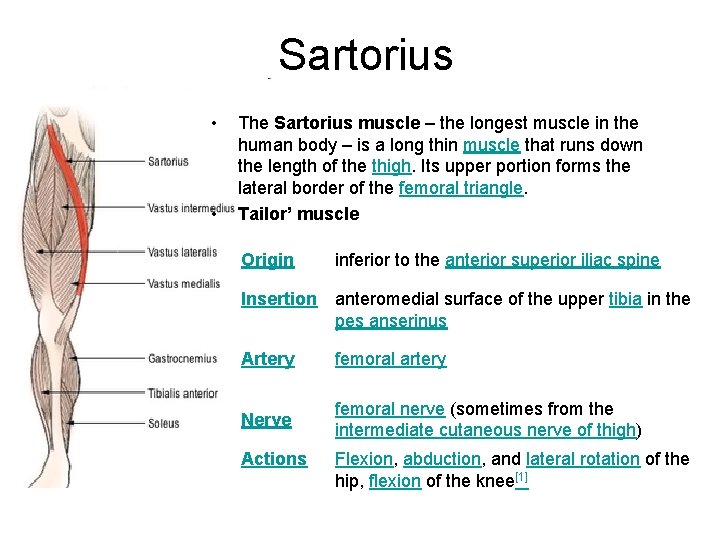
Sartorius • • The Sartorius muscle – the longest muscle in the human body – is a long thin muscle that runs down the length of the thigh. Its upper portion forms the lateral border of the femoral triangle. Tailor’ muscle Origin inferior to the anterior superior iliac spine Insertion anteromedial surface of the upper tibia in the pes anserinus Artery femoral artery Nerve femoral nerve (sometimes from the intermediate cutaneous nerve of thigh) Actions Flexion, abduction, and lateral rotation of the hip, flexion of the knee[1]
Pathology One of the many conditions that can disrupt the use of the sartorius is pes anserine bursitis. Pes anserine bursitis is an inflammatory condition of the medial portion of the knee. This condition usually occurs in athletes from overuse and is characterized by pain, swelling and tenderness. The Pes anserine is made up from the tendons of the gracilis, semitendinosus, and Sartorius muscles; these tendons attach on to the anteromedial proximal tibia. When inflammation of the bursa underlying the tendons occurs they separate from the tibia.
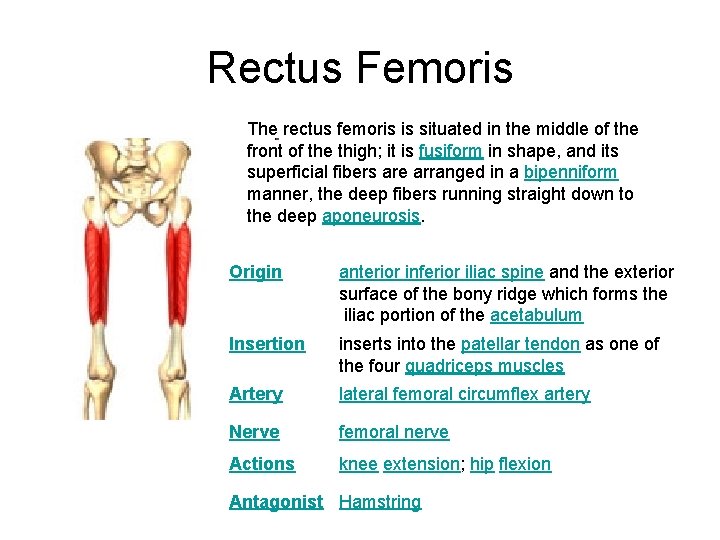
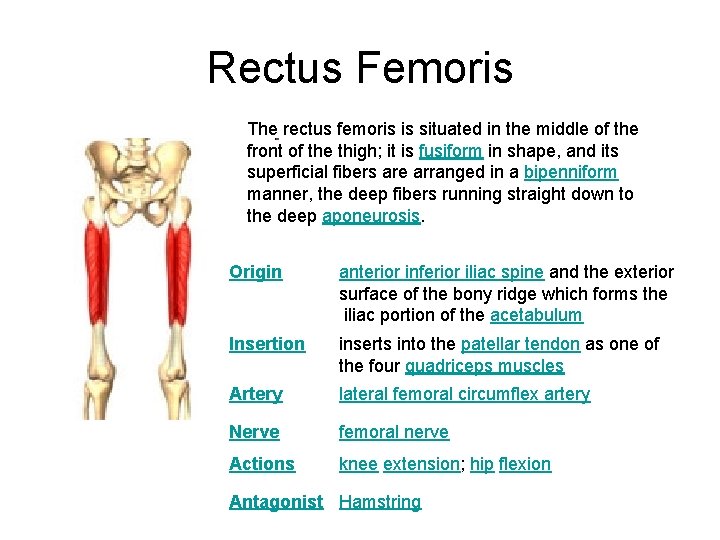
Rectus Femoris The rectus femoris is situated in the middle of the front of the thigh; it is fusiform in shape, and its superficial fibers are arranged in a bipenniform manner, the deep fibers running straight down to the deep aponeurosis. Origin anterior inferior iliac spine and the exterior surface of the bony ridge which forms the iliac portion of the acetabulum Insertion inserts into the patellar tendon as one of the four quadriceps muscles Artery lateral femoral circumflex artery Nerve femoral nerve Actions knee extension; hip flexion Antagonist Hamstring
Function of rectus femoris The rectus femoris and sartorius are the only muscles in the quadriceps group that are involved in flexion of the hip, since they are the only ones that originate in the pelvis and not the femur. By crossing the pelvic femoral joint they can act as a lever to flex the leg at the hip. The rectus femoris is a weaker hip flexor when the knee is extended because it is already shortened and thus suffers from active insufficiency. In essence: the action of raising a straightened leg will recruit more iliacus, psoas major, tensor fasciae latae, and the remaining hip flexors than it will the rectus femoris. Similarly, the rectus femoris is not dominant in knee extension when the hip is flexed since it is already shortened and thus suffers from active insufficiency. In essence: the action of extending a leg from a seated position is primarily driven by the vastus lateralis, vastus medialis, and vastus intermedius, and less by the rectus femoris. The rectus femoris is considered a direct antagonist to the hamstrings. The hamstrings oppose the rectus femoris at the hip joint through extension and at the knee joint through flexion. The rectus femoris can be torn which can be very painful.
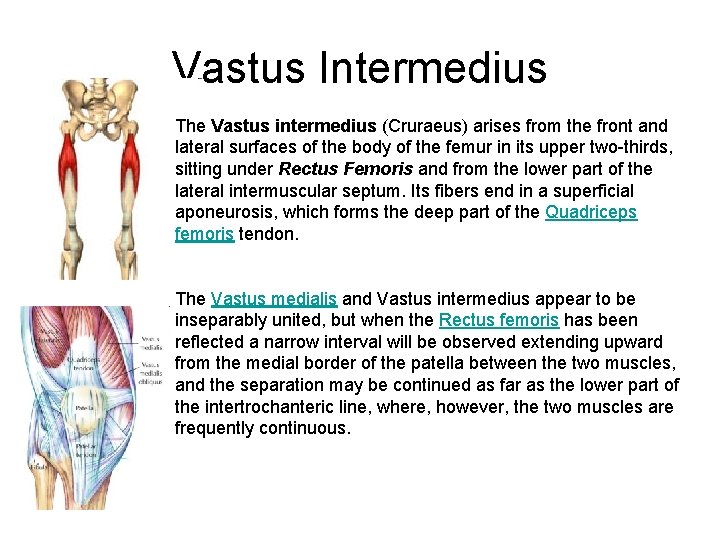
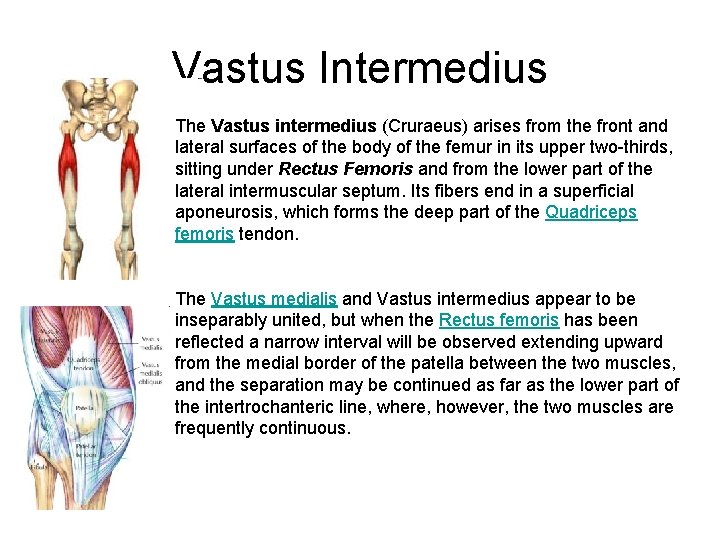
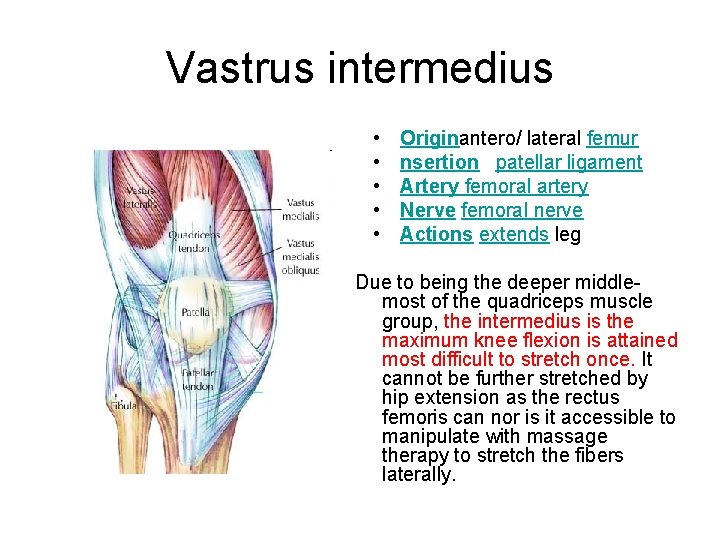
Vastus Intermedius The Vastus intermedius (Cruraeus) arises from the front and lateral surfaces of the body of the femur in its upper two-thirds, sitting under Rectus Femoris and from the lower part of the lateral intermuscular septum. Its fibers end in a superficial aponeurosis, which forms the deep part of the Quadriceps femoris tendon. The Vastus medialis and Vastus intermedius appear to be inseparably united, but when the Rectus femoris has been reflected a narrow interval will be observed extending upward from the medial border of the patella between the two muscles, and the separation may be continued as far as the lower part of the intertrochanteric line, where, however, the two muscles are frequently continuous.
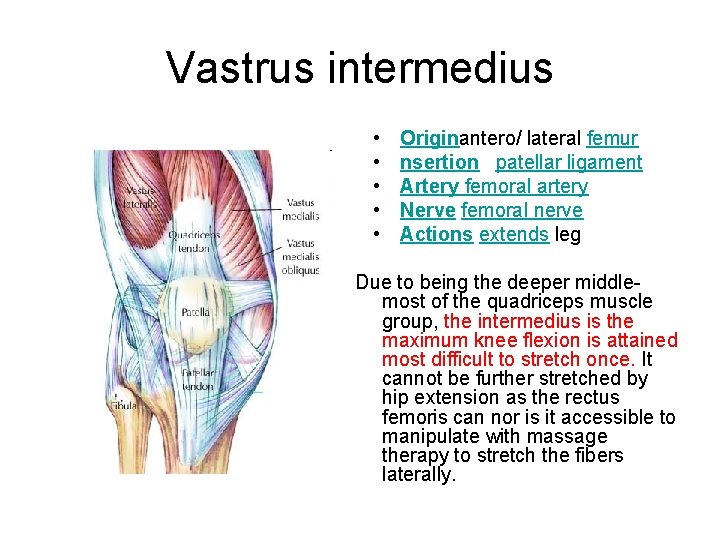
Vastrus intermedius • • • Originantero/ lateral femur nsertion patellar ligament Artery femoral artery Nerve femoral nerve Actions extends leg Due to being the deeper middlemost of the quadriceps muscle group, the intermedius is the maximum knee flexion is attained most difficult to stretch once. It cannot be further stretched by hip extension as the rectus femoris can nor is it accessible to manipulate with massage therapy to stretch the fibers laterally.
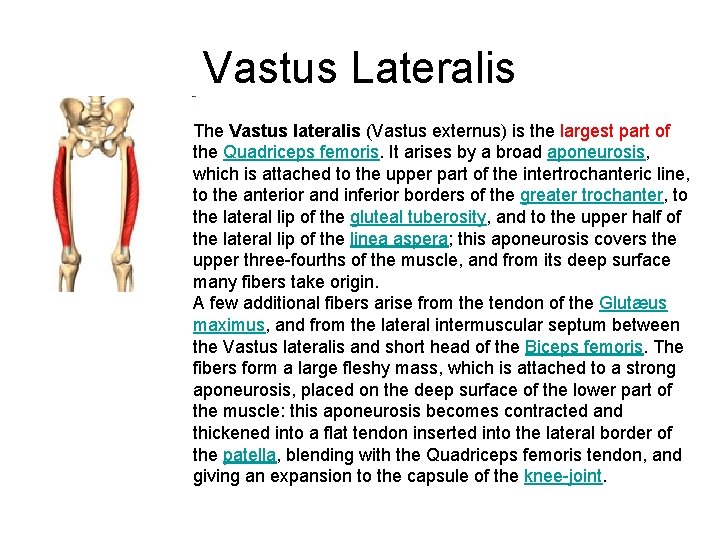
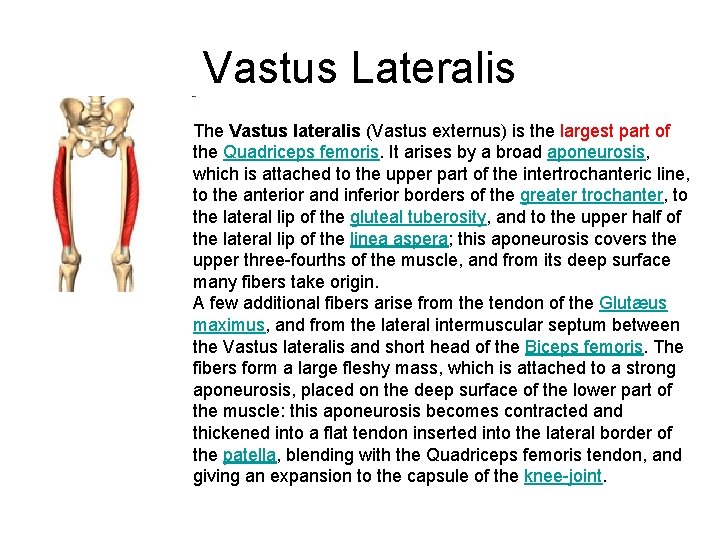
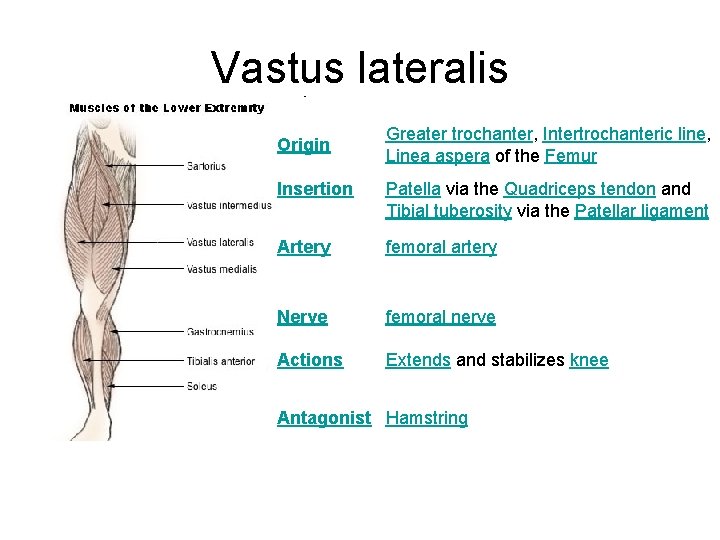
Vastus Lateralis The Vastus lateralis (Vastus externus) is the largest part of the Quadriceps femoris. It arises by a broad aponeurosis, which is attached to the upper part of the intertrochanteric line, to the anterior and inferior borders of the greater trochanter, to the lateral lip of the gluteal tuberosity, and to the upper half of the lateral lip of the linea aspera; this aponeurosis covers the upper three-fourths of the muscle, and from its deep surface many fibers take origin. A few additional fibers arise from the tendon of the Glutæus maximus, and from the lateral intermuscular septum between the Vastus lateralis and short head of the Biceps femoris. The fibers form a large fleshy mass, which is attached to a strong aponeurosis, placed on the deep surface of the lower part of the muscle: this aponeurosis becomes contracted and thickened into a flat tendon inserted into the lateral border of the patella, blending with the Quadriceps femoris tendon, and giving an expansion to the capsule of the knee-joint.
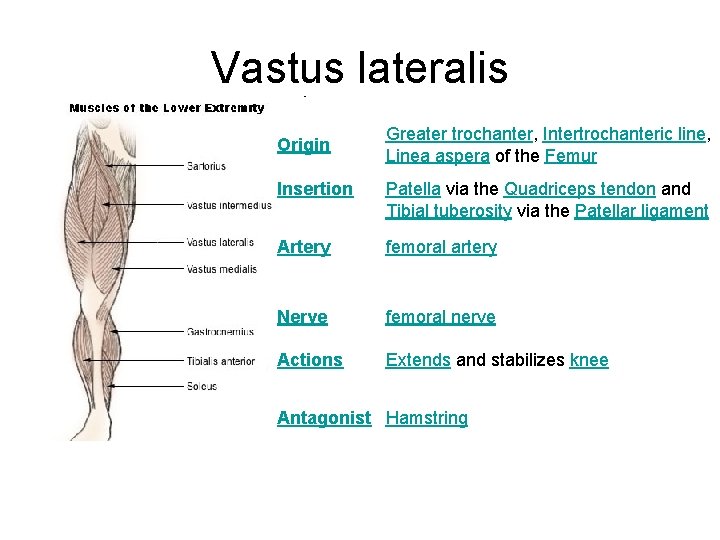
Vastus lateralis Origin Greater trochanter, Intertrochanteric line, Linea aspera of the Femur Insertion Patella via the Quadriceps tendon and Tibial tuberosity via the Patellar ligament Artery femoral artery Nerve femoral nerve Actions Extends and stabilizes knee Antagonist Hamstring
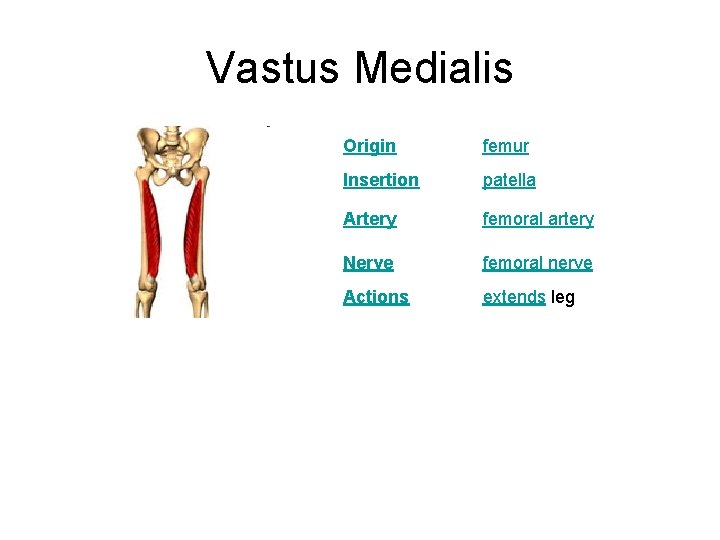
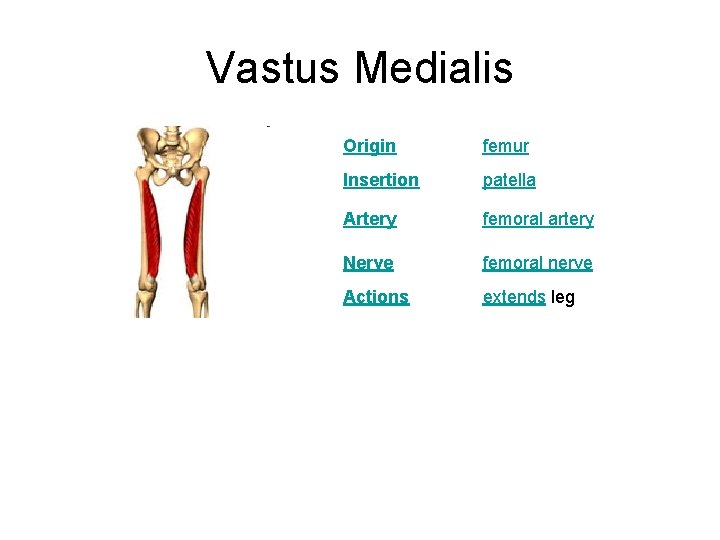
Vastus Medialis Origin femur Insertion patella Artery femoral artery Nerve femoral nerve Actions extends leg
Vastus medialis obliquus The vastus medialis, often called the 'teardrop' muscle, is a medially located muscle of the quadriceps. The vasti appear to act largely in a co-ordinated manner throughout the control of knee extension. Much has been made of the ability of the Vastus Medialis to translate the patella medially, however since approximately 70% of the contractile fibres attach directly to the common extensor tendon (which then inserts centrally to the superior patella) the functional ability to achieve this goal may be overstated, and is likely dwarfed by the bony congruence of the patella in the trochlea notch. However, this does not apply to persons with trochlear aplasia or hypoplasia, which refer to an absence or extreme shallowness of the trochlear groove. Some authorities maintain there is a separate aspect to the Vastus Medialis muscle - the "Vastus Medialis Obliquus" or more commonly the "VMO" which is reported to have a more oblique or horizontal orientation to the bulk of the remainder of the muscle thereby disposing it to be better able to 'pull' the patella medially. Unfortunately careful inspection of many cadavers reveals that the fibres of the Vastus Medialis are largely parallel and there is no significant separate aspect of the contractile fibres fitting this description which would suggest it is time to lay this clinical myth to rest.
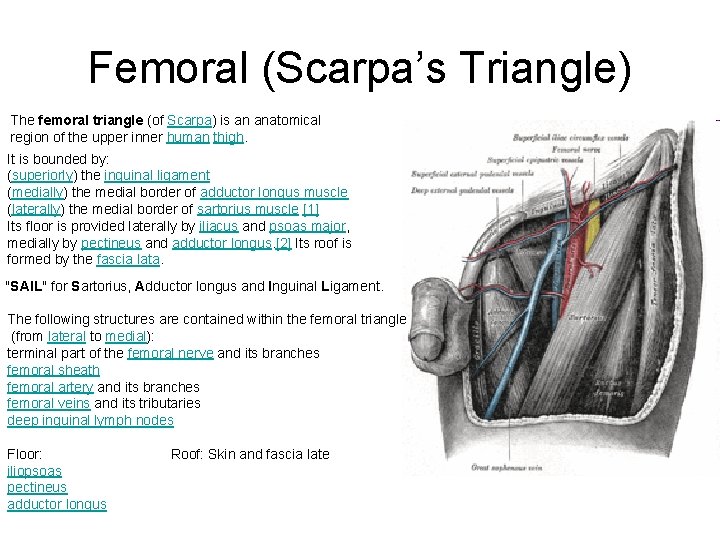
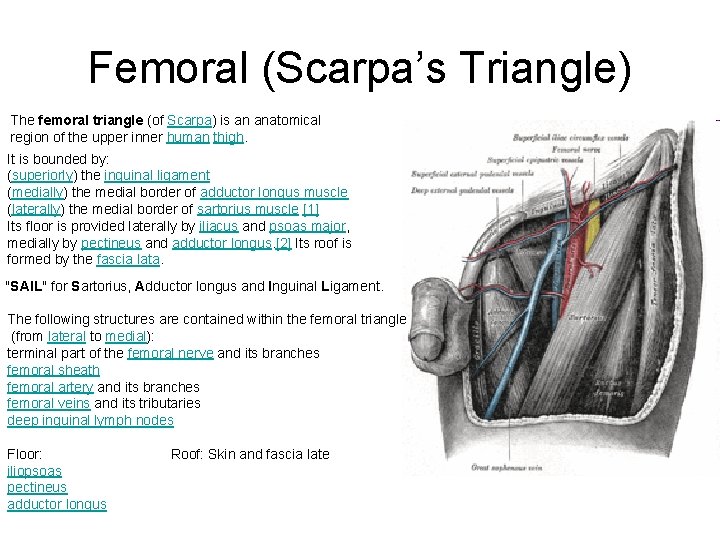
Femoral (Scarpa’s Triangle) The femoral triangle (of Scarpa) is an anatomical region of the upper inner human thigh. It is bounded by: (superiorly) the inguinal ligament (medially) the medial border of adductor longus muscle (laterally) the medial border of sartorius muscle [1] Its floor is provided laterally by iliacus and psoas major, medially by pectineus and adductor longus. [2] Its roof is formed by the fascia lata. "SAIL" for Sartorius, Adductor longus and Inguinal Ligament. The following structures are contained within the femoral triangle (from lateral to medial): terminal part of the femoral nerve and its branches femoral sheath femoral artery and its branches femoral veins and its tributaries deep inguinal lymph nodes Floor: Roof: Skin and fascia late iliopsoas pectineus adductor longus
Clinical significance Since the femoral triangle provides easy access to a major artery, coronary angioplasty and peripheral angioplasties. often performed by entering the femoral artery at the femoral triangle. Heavy bleeding in the leg can be stopped by applying pressure to points in the femoral triangle. Another clinical significance of the femoral triangle is that the femoral artery is positioned at the midinguinal point (midpoint between the pubic symphysis and the anterior superior iliac spine); medial to it lies the femoral vein. Thus the femoral vein, once located, allows for femoral venopuncture. Femoral venopuncture is useful when there are no superficial veins that can be aspirated in a patient, in the case of collapse. The positive pulsation of the femoral artery signifies that the heart is beating and also blood is flowing to the lower extremity. It is also necessary to appreciate clinically that this is a case where the nerve is more lateral than the vein. In most other cases the a nerve (relative to its associated artery and vein)would be the deepest or more medial followed by the artery and then the vein. But in this case it is the opposite. This must be remembered when venous or arterial samples are required from the femoral vessels. The order of this neurovascular bundle can be remembered using the mnemonic, "NAVY" for Nerve, Artery, Vein, Y -fronts (the British term of a style of men's underwear with a "Y" shaped front that acts as a fly). The "Y" is midline (corresponding with the penis) and the mnemonic always reads from the outside - in, so that the Femoral Nerve is always lateral. An alternate to this mnemonic is "NAVa. L" for Nerve, Artery, Vein, and Lymph, to include the deep inguinal lymph nodes located medial to the Femoral vein.
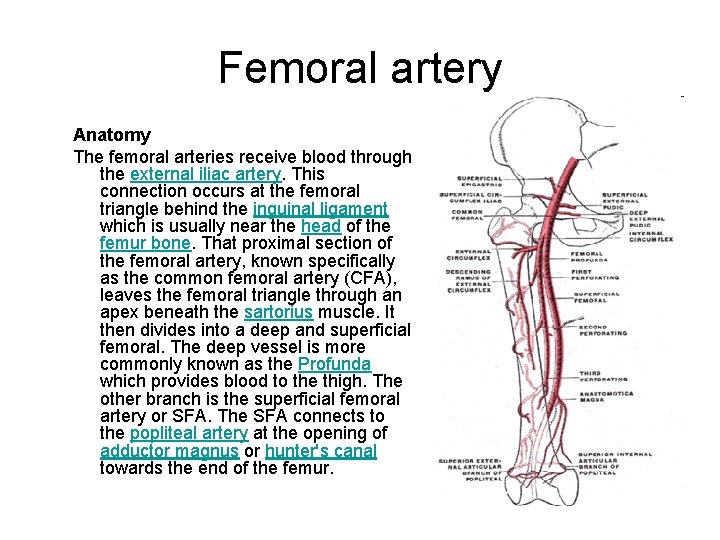
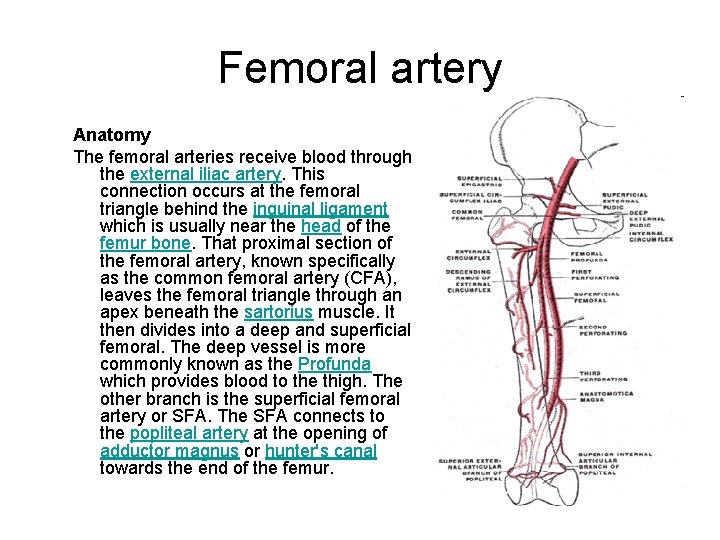
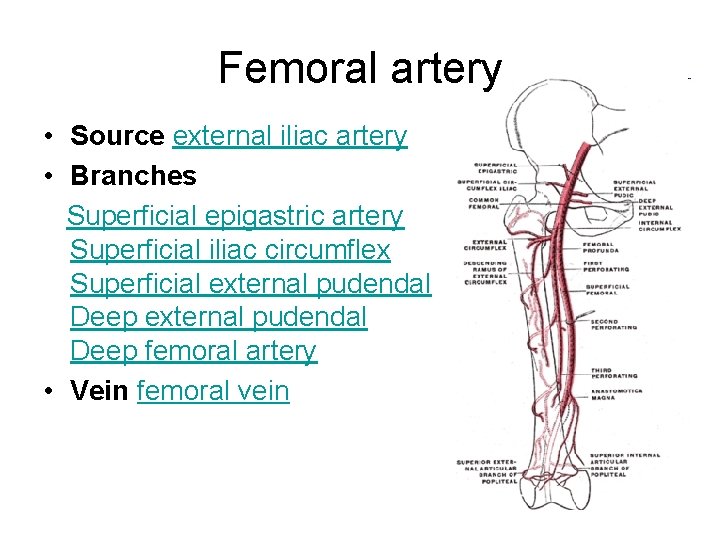
Femoral artery Anatomy The femoral arteries receive blood through the external iliac artery. This connection occurs at the femoral triangle behind the inguinal ligament which is usually near the head of the femur bone. That proximal section of the femoral artery, known specifically as the common femoral artery (CFA), leaves the femoral triangle through an apex beneath the sartorius muscle. It then divides into a deep and superficial femoral. The deep vessel is more commonly known as the Profunda which provides blood to the thigh. The other branch is the superficial femoral artery or SFA. The SFA connects to the popliteal artery at the opening of adductor magnus or hunter's canal towards the end of the femur.
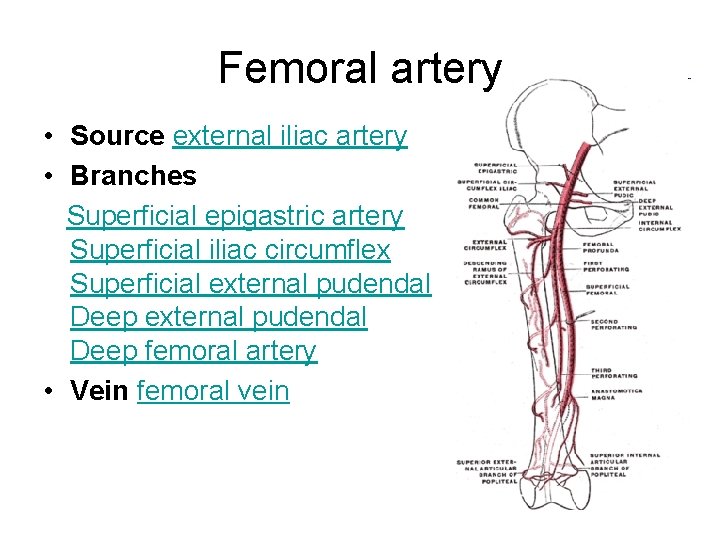
Femoral artery • Source external iliac artery • Branches Superficial epigastric artery Superficial iliac circumflex Superficial external pudendal Deep femoral artery • Vein femoral vein
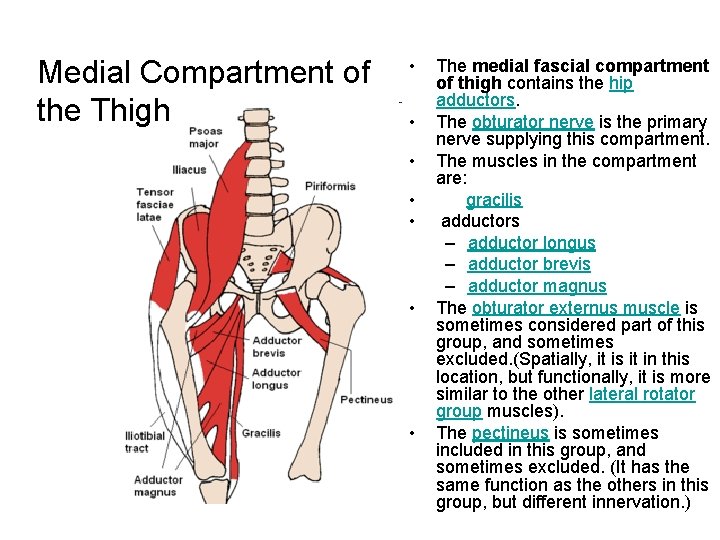
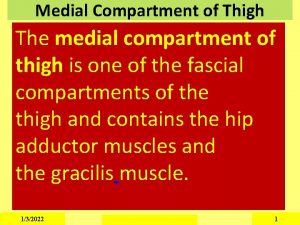
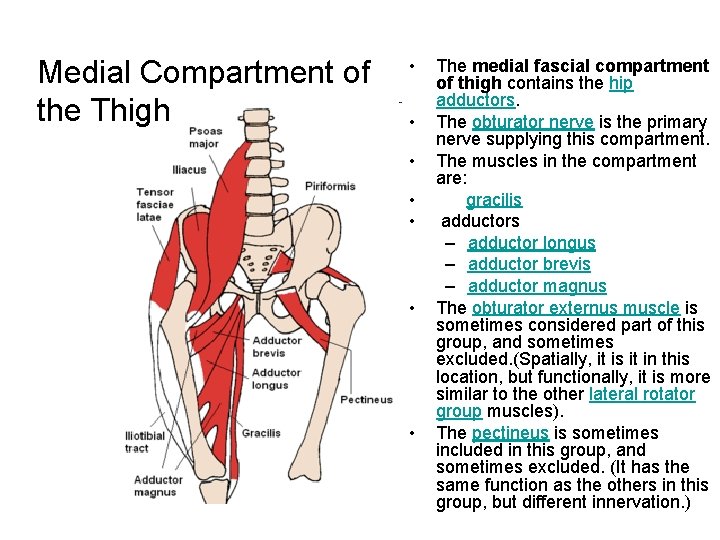
Medial Compartment of the Thigh • • The medial fascial compartment of thigh contains the hip adductors. The obturator nerve is the primary nerve supplying this compartment. The muscles in the compartment are: gracilis adductors – adductor longus – adductor brevis – adductor magnus The obturator externus muscle is sometimes considered part of this group, and sometimes excluded. (Spatially, it is it in this location, but functionally, it is more similar to the other lateral rotator group muscles). The pectineus is sometimes included in this group, and sometimes excluded. (It has the same function as the others in this group, but different innervation. )
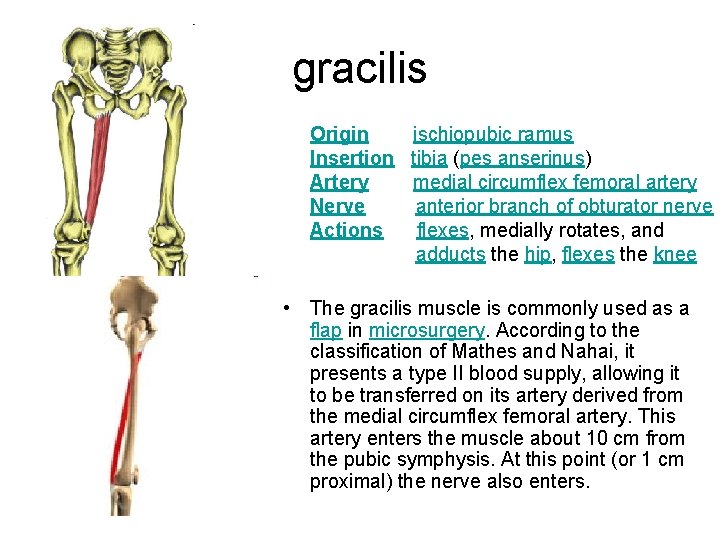
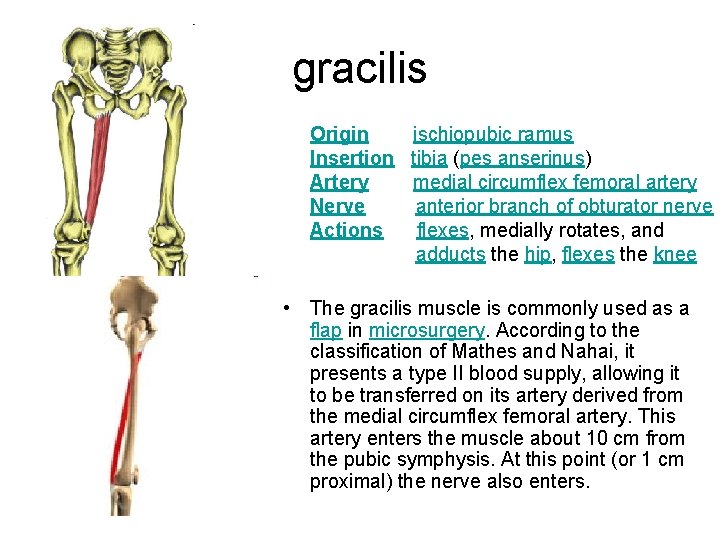
gracilis Origin ischiopubic ramus Insertion tibia (pes anserinus) Artery medial circumflex femoral artery Nerve anterior branch of obturator nerve Actions flexes, medially rotates, and adducts the hip, flexes the knee • The gracilis muscle is commonly used as a flap in microsurgery. According to the classification of Mathes and Nahai, it presents a type II blood supply, allowing it to be transferred on its artery derived from the medial circumflex femoral artery. This artery enters the muscle about 10 cm from the pubic symphysis. At this point (or 1 cm proximal) the nerve also enters.
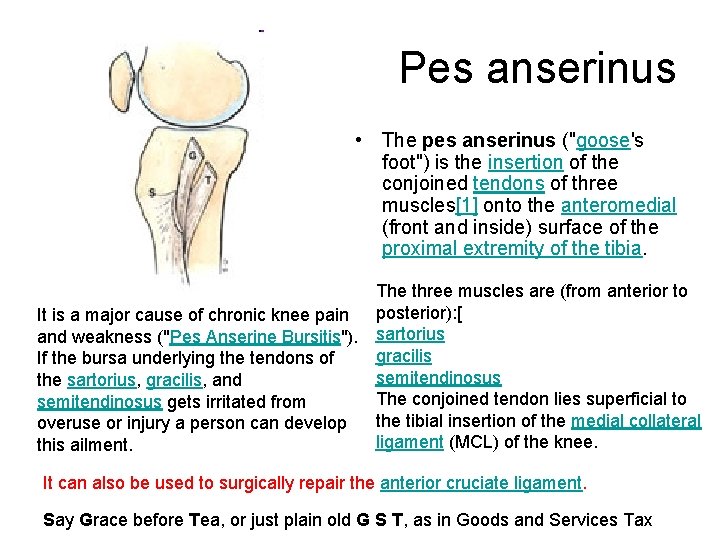
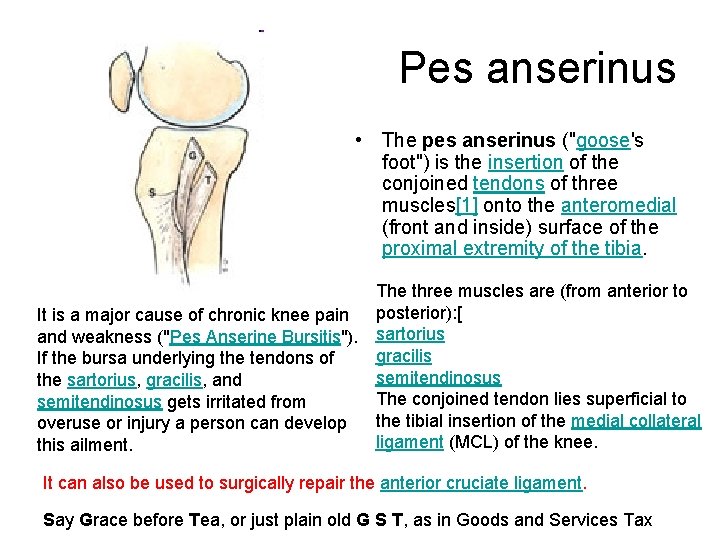
Pes anserinus • The pes anserinus ("goose's foot") is the insertion of the conjoined tendons of three muscles[1] onto the anteromedial (front and inside) surface of the proximal extremity of the tibia. The three muscles are (from anterior to It is a major cause of chronic knee pain posterior): [ and weakness ("Pes Anserine Bursitis"). sartorius gracilis If the bursa underlying the tendons of semitendinosus the sartorius, gracilis, and The conjoined tendon lies superficial to semitendinosus gets irritated from overuse or injury a person can develop the tibial insertion of the medial collateral ligament (MCL) of the knee. this ailment. It can also be used to surgically repair the anterior cruciate ligament. Say Grace before Tea, or just plain old G S T, as in Goods and Services Tax
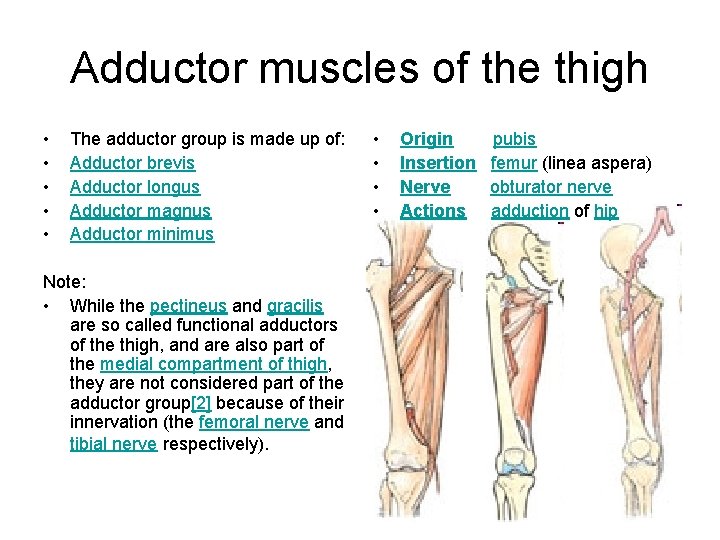
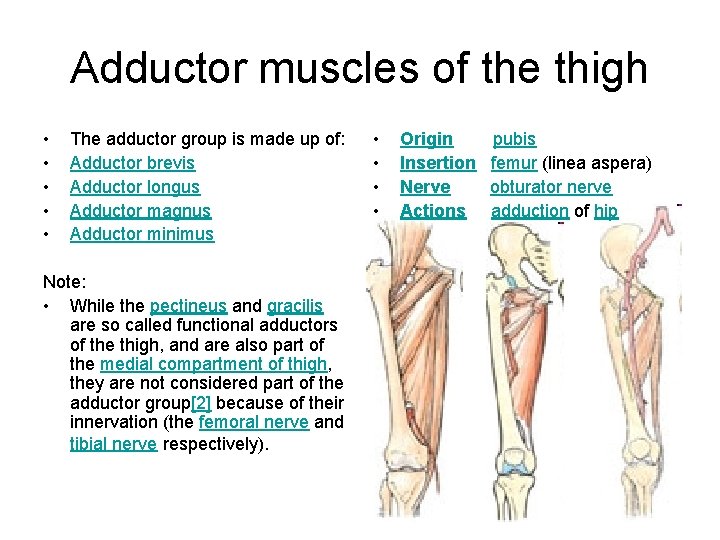
Adductor muscles of the thigh • • • The adductor group is made up of: Adductor brevis Adductor longus Adductor magnus Adductor minimus Note: • While the pectineus and gracilis are so called functional adductors of the thigh, and are also part of the medial compartment of thigh, they are not considered part of the adductor group[2] because of their innervation (the femoral nerve and tibial nerve respectively). • • Origin pubis Insertion femur (linea aspera) Nerve obturator nerve Actions adduction of hip
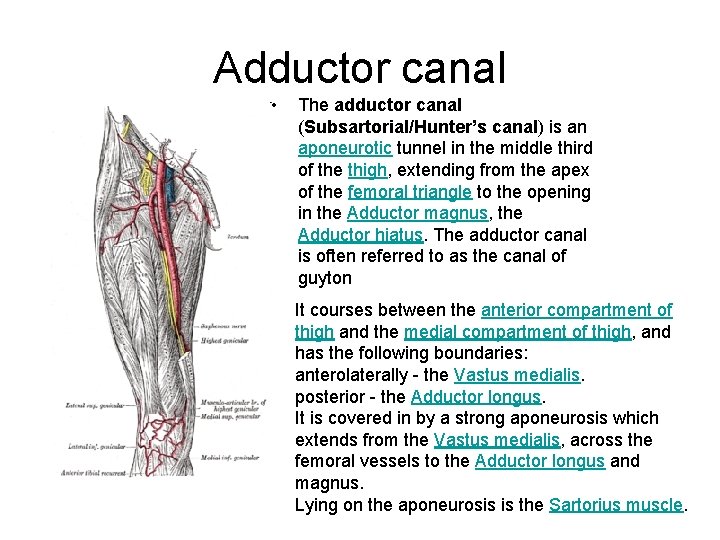
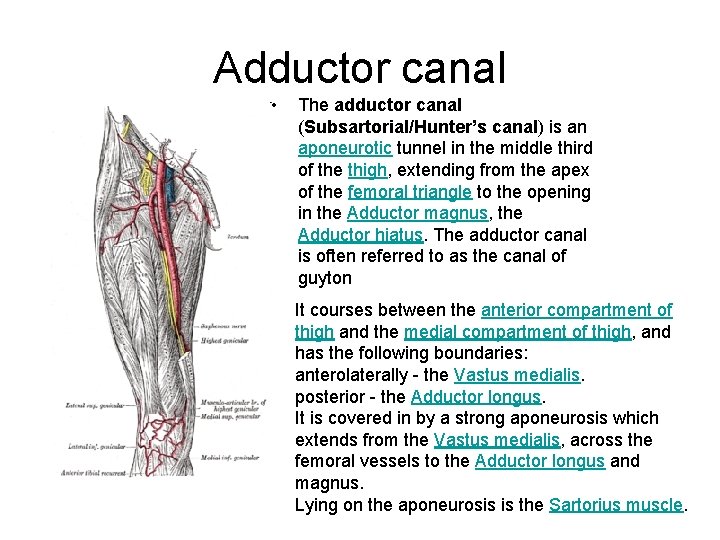
Adductor canal • The adductor canal (Subsartorial/Hunter’s canal) is an aponeurotic tunnel in the middle third of the thigh, extending from the apex of the femoral triangle to the opening in the Adductor magnus, the Adductor hiatus. The adductor canal is often referred to as the canal of guyton It courses between the anterior compartment of thigh and the medial compartment of thigh, and has the following boundaries: anterolaterally - the Vastus medialis. posterior - the Adductor longus. It is covered in by a strong aponeurosis which extends from the Vastus medialis, across the femoral vessels to the Adductor longus and magnus. Lying on the aponeurosis is the Sartorius muscle.
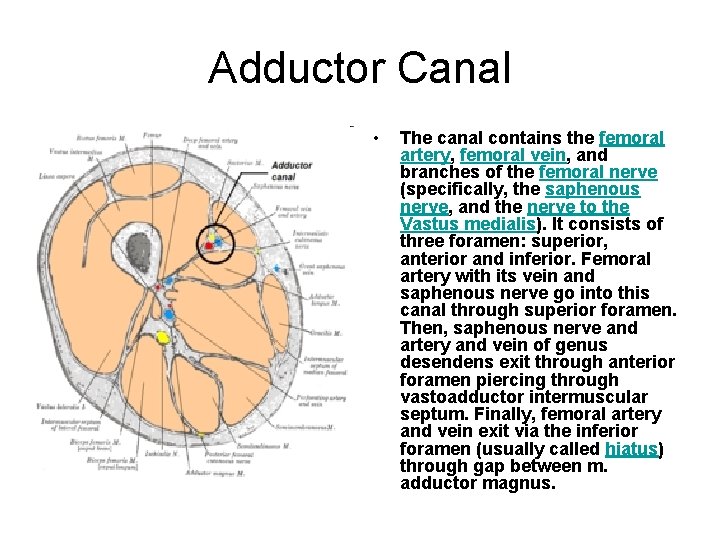
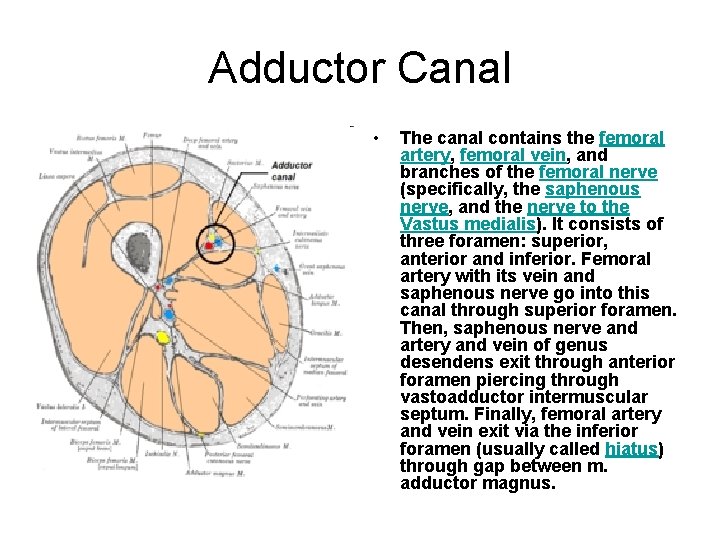
Adductor Canal • The canal contains the femoral artery, femoral vein, and branches of the femoral nerve (specifically, the saphenous nerve, and the nerve to the Vastus medialis). It consists of three foramen: superior, anterior and inferior. Femoral artery with its vein and saphenous nerve go into this canal through superior foramen. Then, saphenous nerve and artery and vein of genus desendens exit through anterior foramen piercing through vastoadductor intermuscular septum. Finally, femoral artery and vein exit via the inferior foramen (usually called hiatus) through gap between m. adductor magnus.
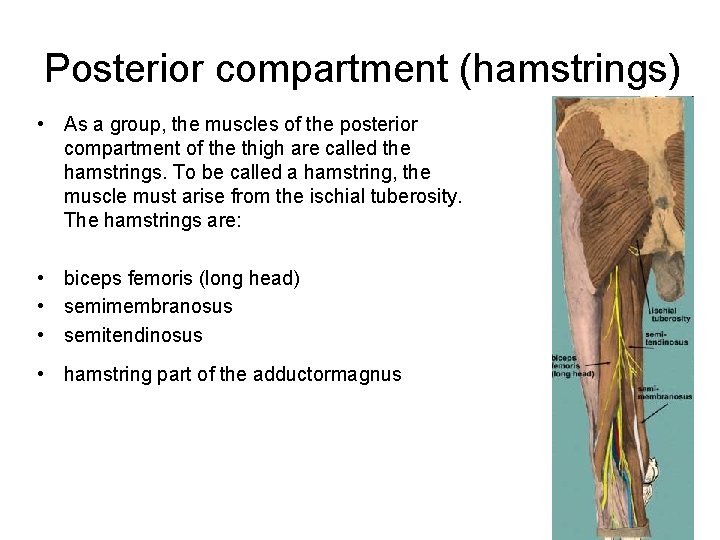
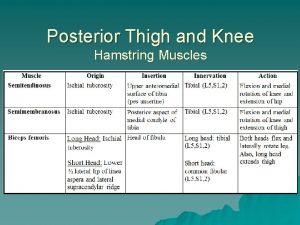
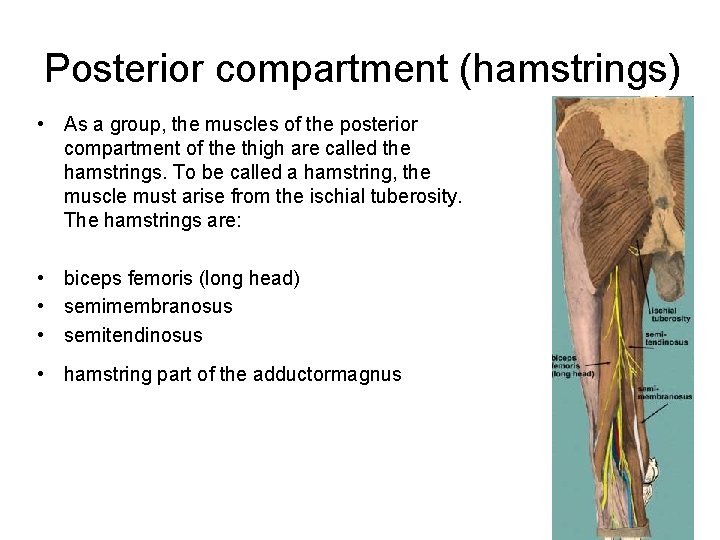
Posterior compartment (hamstrings) • As a group, the muscles of the posterior compartment of the thigh are called the hamstrings. To be called a hamstring, the muscle must arise from the ischial tuberosity. The hamstrings are: • biceps femoris (long head) • semimembranosus • semitendinosus • hamstring part of the adductormagnus
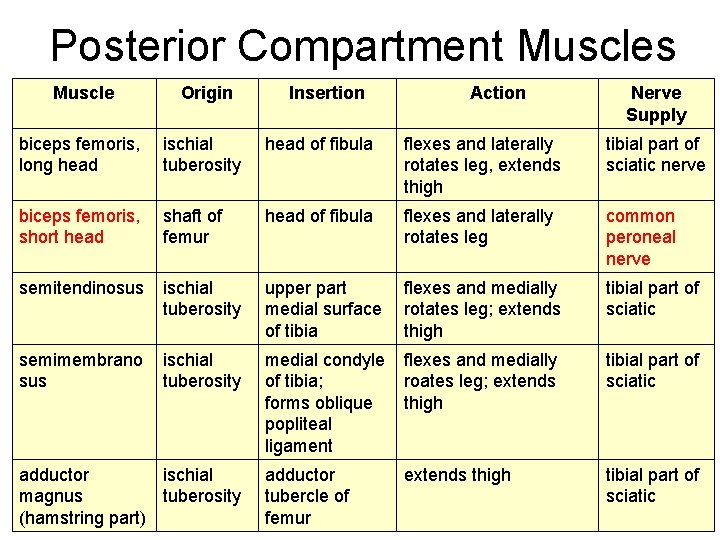
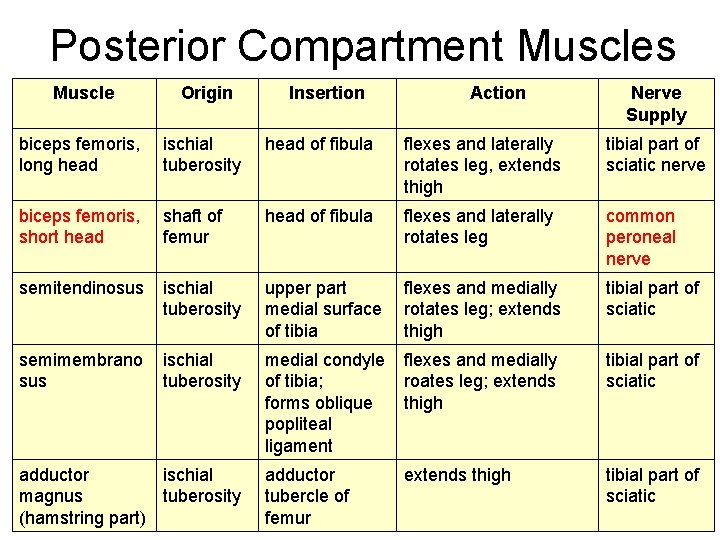
Posterior Compartment Muscles Muscle Origin biceps femoris, long head ischial tuberosity head of fibula flexes and laterally rotates leg, extends thigh tibial part of sciatic nerve biceps femoris, short head shaft of femur head of fibula flexes and laterally rotates leg common peroneal nerve semitendinosus ischial tuberosity upper part flexes and medially medial surface rotates leg; extends of tibia thigh tibial part of sciatic semimembrano sus ischial tuberosity medial condyle flexes and medially of tibia; roates leg; extends forms oblique thigh popliteal ligament tibial part of sciatic adductor tubercle of femur tibial part of sciatic adductor ischial magnus tuberosity (hamstring part) Insertion Action extends thigh Nerve Supply
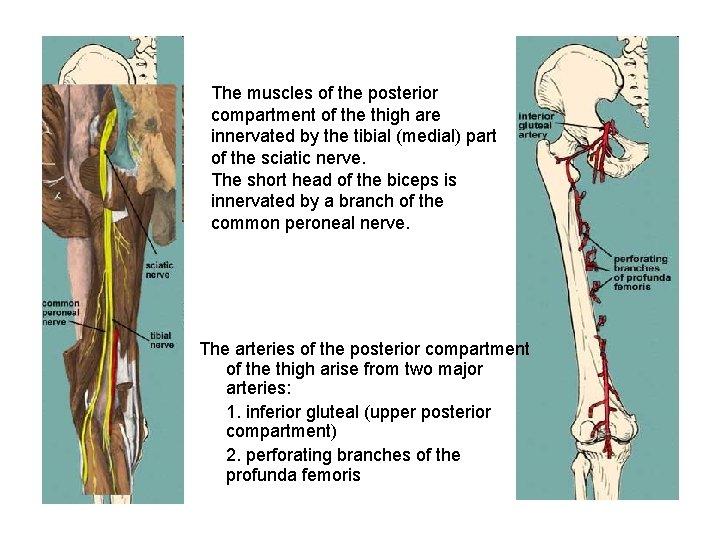
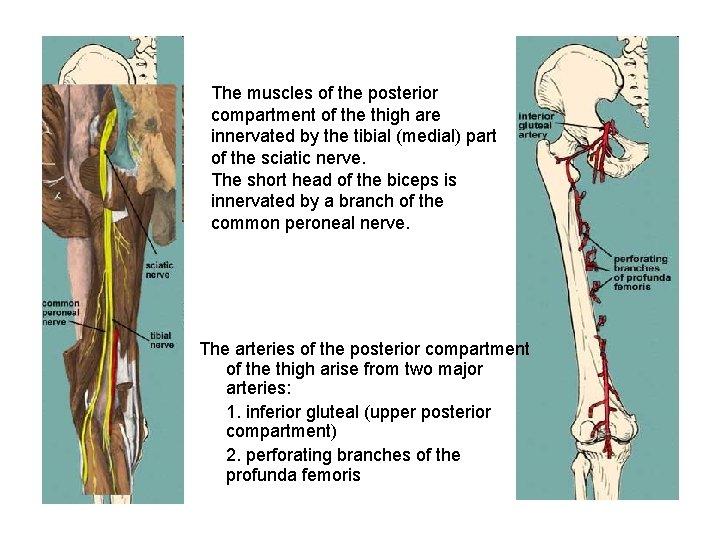
The muscles of the posterior compartment of the thigh are innervated by the tibial (medial) part of the sciatic nerve. The short head of the biceps is innervated by a branch of the common peroneal nerve. The arteries of the posterior compartment of the thigh arise from two major arteries: 1. inferior gluteal (upper posterior compartment) 2. perforating branches of the profunda femoris
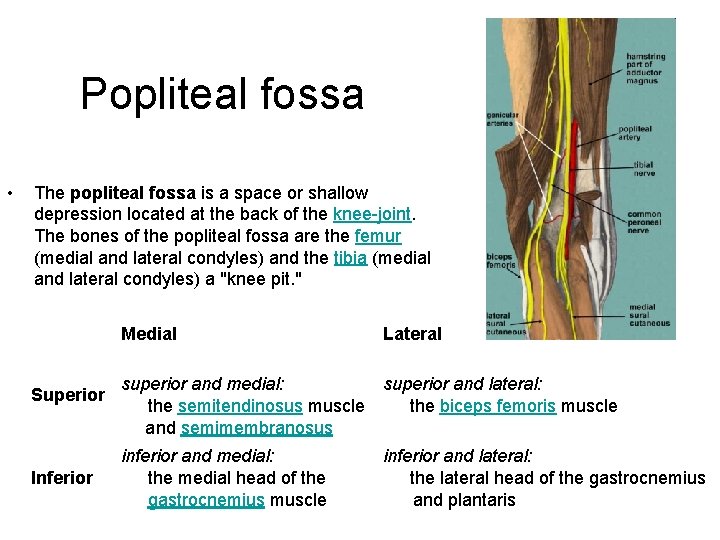
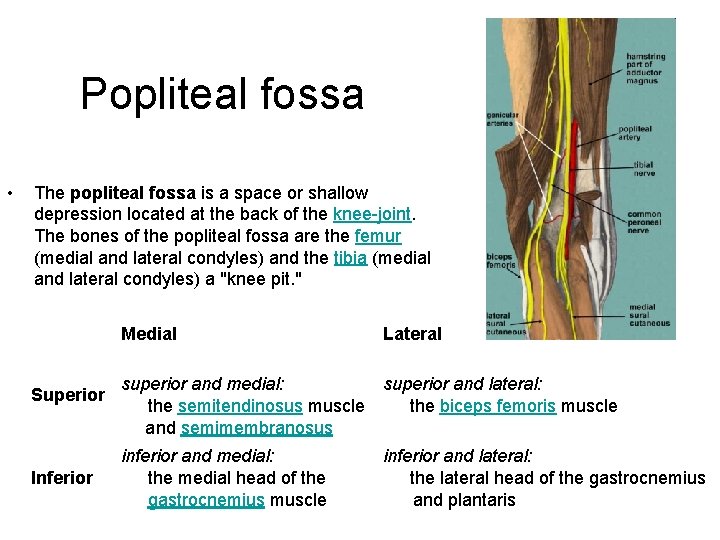
Popliteal fossa • The popliteal fossa is a space or shallow depression located at the back of the knee-joint. The bones of the popliteal fossa are the femur (medial and lateral condyles) and the tibia (medial and lateral condyles) a "knee pit. " Superior Inferior Medial Lateral superior and medial: superior and lateral: the semitendinosus muscle the biceps femoris muscle and semimembranosus inferior and medial: the medial head of the gastrocnemius muscle inferior and lateral: the lateral head of the gastrocnemius and plantaris
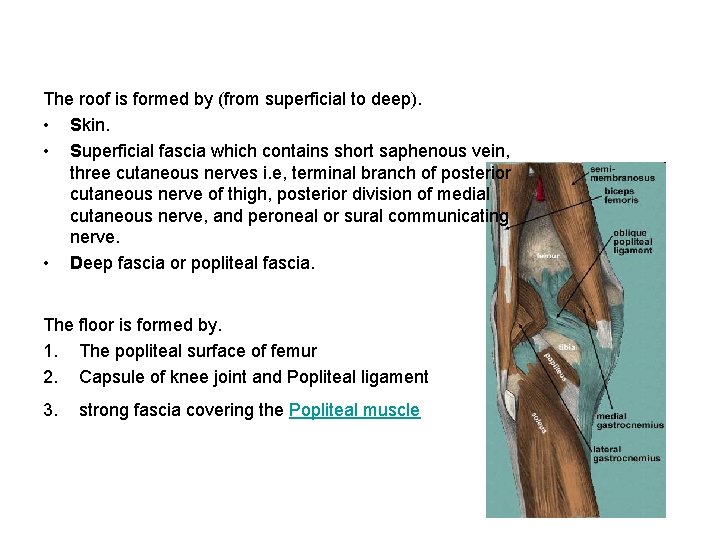
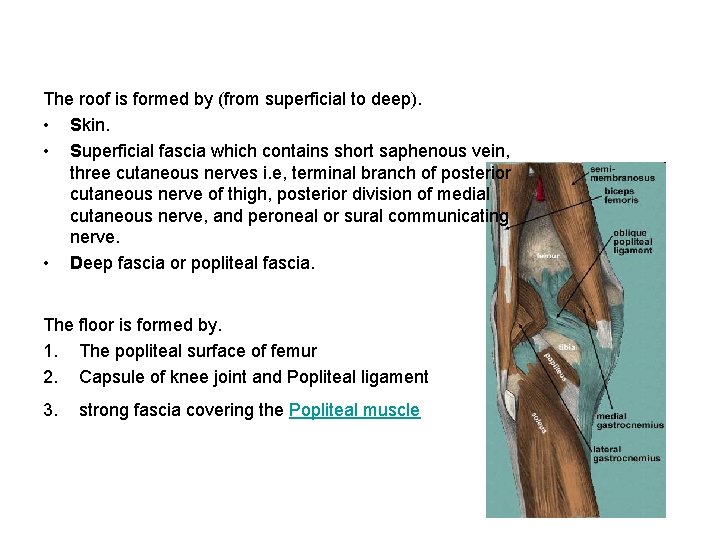
The roof is formed by (from superficial to deep). • Skin. • Superficial fascia which contains short saphenous vein, three cutaneous nerves i. e, terminal branch of posterior cutaneous nerve of thigh, posterior division of medial cutaneous nerve, and peroneal or sural communicating nerve. • Deep fascia or popliteal fascia. The floor is formed by. 1. The popliteal surface of femur 2. Capsule of knee joint and Popliteal ligament 3. strong fascia covering the Popliteal muscle
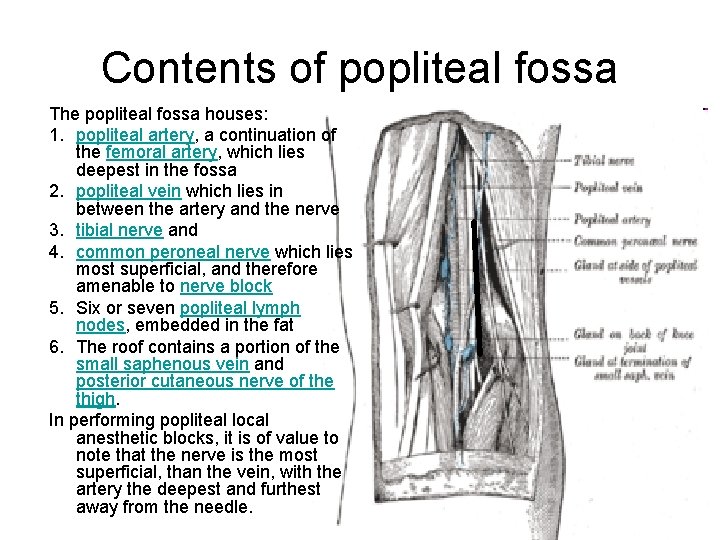
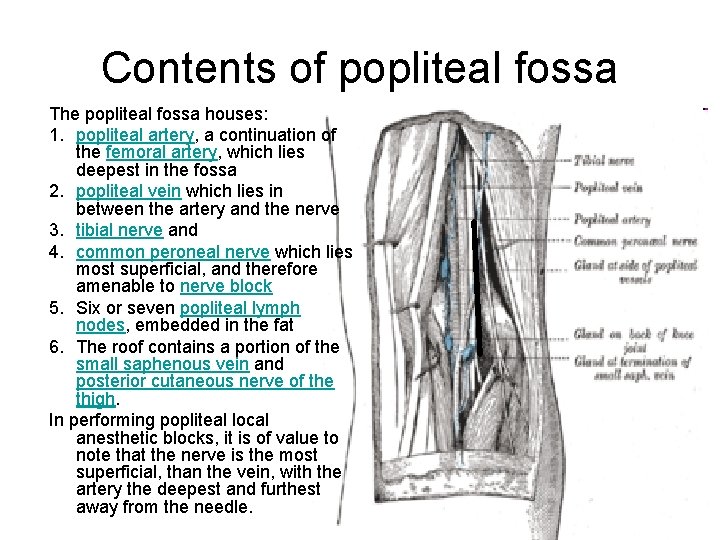
Contents of popliteal fossa The popliteal fossa houses: 1. popliteal artery, a continuation of the femoral artery, which lies deepest in the fossa 2. popliteal vein which lies in between the artery and the nerve 3. tibial nerve and 4. common peroneal nerve which lies most superficial, and therefore amenable to nerve block 5. Six or seven popliteal lymph nodes, embedded in the fat 6. The roof contains a portion of the small saphenous vein and posterior cutaneous nerve of the thigh. In performing popliteal local anesthetic blocks, it is of value to note that the nerve is the most superficial, than the vein, with the artery the deepest and furthest away from the needle.
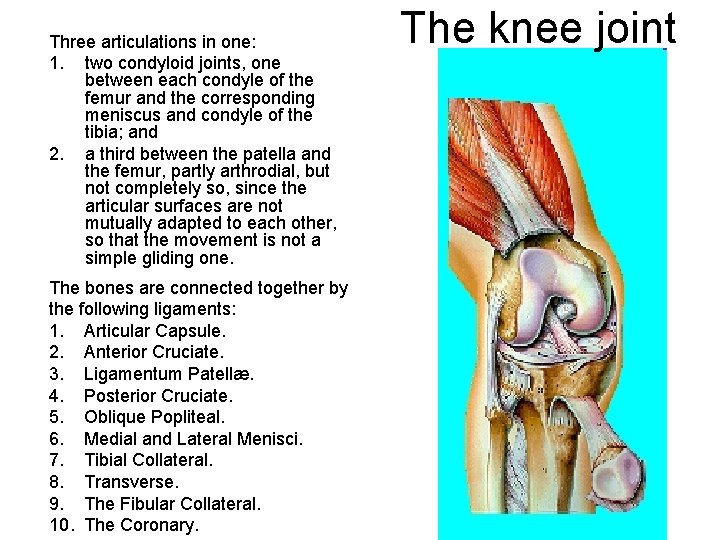
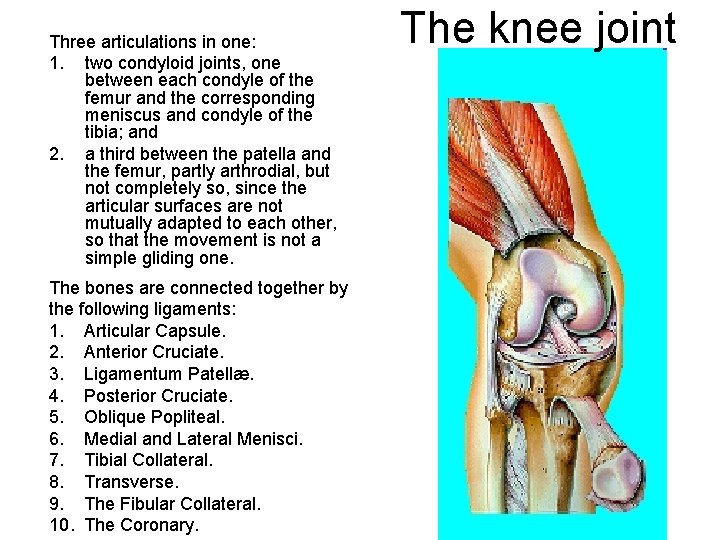
Three articulations in one: 1. two condyloid joints, one between each condyle of the femur and the corresponding meniscus and condyle of the tibia; and 2. a third between the patella and the femur, partly arthrodial, but not completely so, since the articular surfaces are not mutually adapted to each other, so that the movement is not a simple gliding one. The bones are connected together by the following ligaments: 1. Articular Capsule. 2. Anterior Cruciate. 3. Ligamentum Patellæ. 4. Posterior Cruciate. 5. Oblique Popliteal. 6. Medial and Lateral Menisci. 7. Tibial Collateral. 8. Transverse. 9. The Fibular Collateral. 10. The Coronary. The knee joint
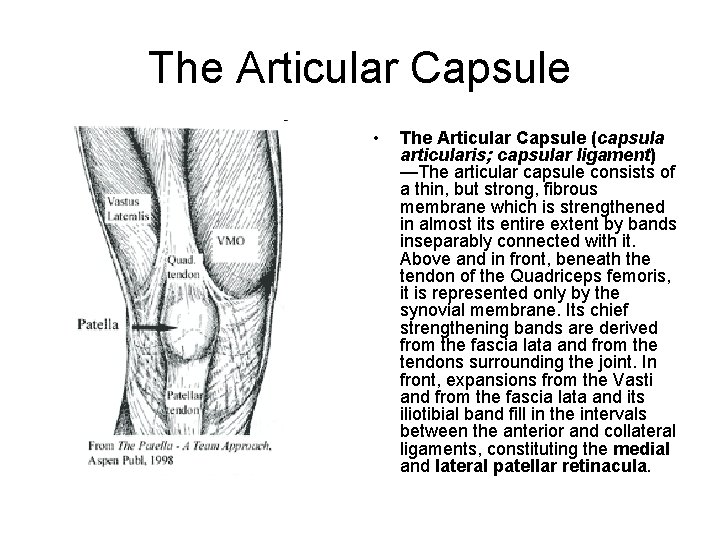
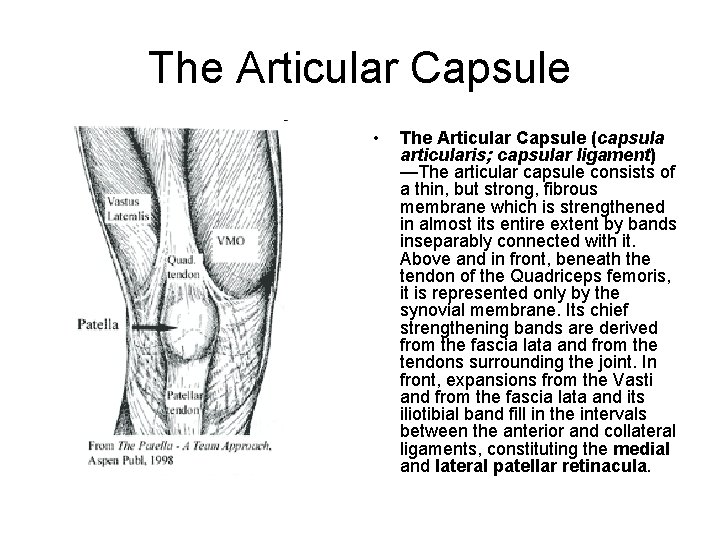
The Articular Capsule • The Articular Capsule (capsula articularis; capsular ligament) —The articular capsule consists of a thin, but strong, fibrous membrane which is strengthened in almost its entire extent by bands inseparably connected with it. Above and in front, beneath the tendon of the Quadriceps femoris, it is represented only by the synovial membrane. Its chief strengthening bands are derived from the fascia lata and from the tendons surrounding the joint. In front, expansions from the Vasti and from the fascia lata and its iliotibial band fill in the intervals between the anterior and collateral ligaments, constituting the medial and lateral patellar retinacula.
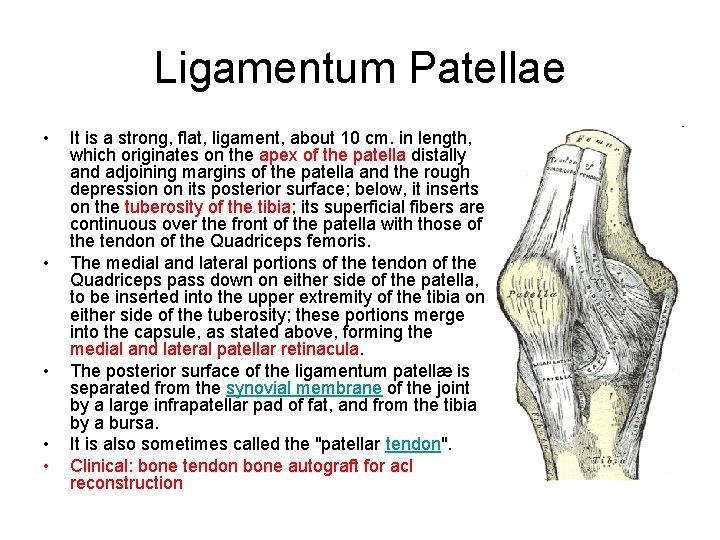
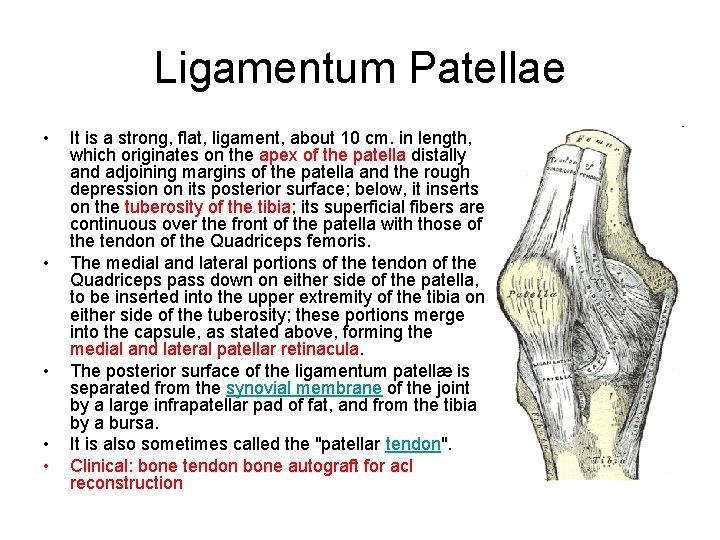
Ligamentum Patellae • • • It is a strong, flat, ligament, about 10 cm. in length, which originates on the apex of the patella distally and adjoining margins of the patella and the rough depression on its posterior surface; below, it inserts on the tuberosity of the tibia; its superficial fibers are continuous over the front of the patella with those of the tendon of the Quadriceps femoris. The medial and lateral portions of the tendon of the Quadriceps pass down on either side of the patella, to be inserted into the upper extremity of the tibia on either side of the tuberosity; these portions merge into the capsule, as stated above, forming the medial and lateral patellar retinacula. The posterior surface of the ligamentum patellæ is separated from the synovial membrane of the joint by a large infrapatellar pad of fat, and from the tibia by a bursa. It is also sometimes called the "patellar tendon". Clinical: bone tendon bone autograft for acl reconstruction
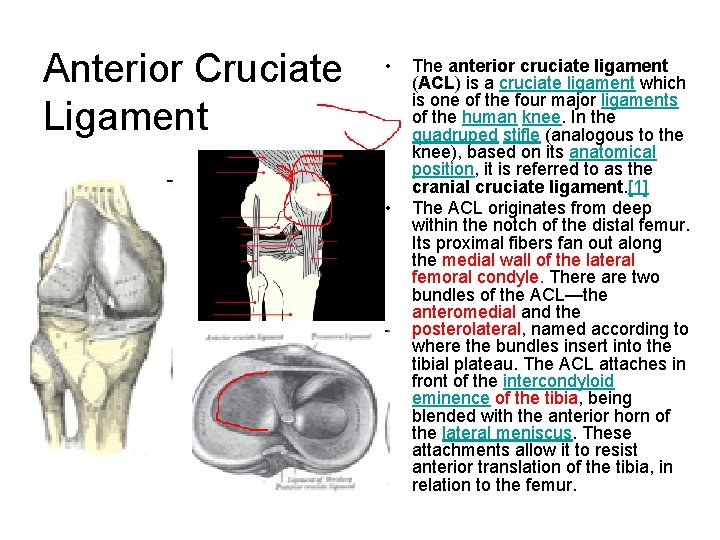
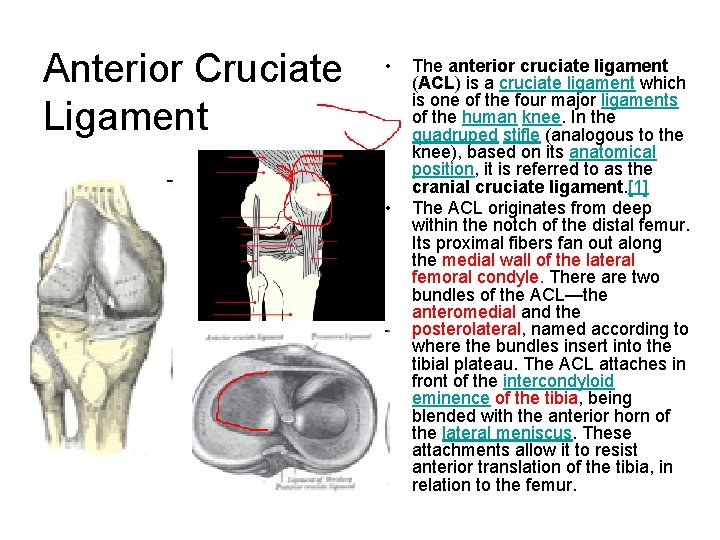
Anterior Cruciate Ligament • • The anterior cruciate ligament (ACL) is a cruciate ligament which is one of the four major ligaments of the human knee. In the quadruped stifle (analogous to the knee), based on its anatomical position, it is referred to as the cranial cruciate ligament. [1] The ACL originates from deep within the notch of the distal femur. Its proximal fibers fan out along the medial wall of the lateral femoral condyle. There are two bundles of the ACL—the anteromedial and the posterolateral, named according to where the bundles insert into the tibial plateau. The ACL attaches in front of the intercondyloid eminence of the tibia, being blended with the anterior horn of the lateral meniscus. These attachments allow it to resist anterior translation of the tibia, in relation to the femur.
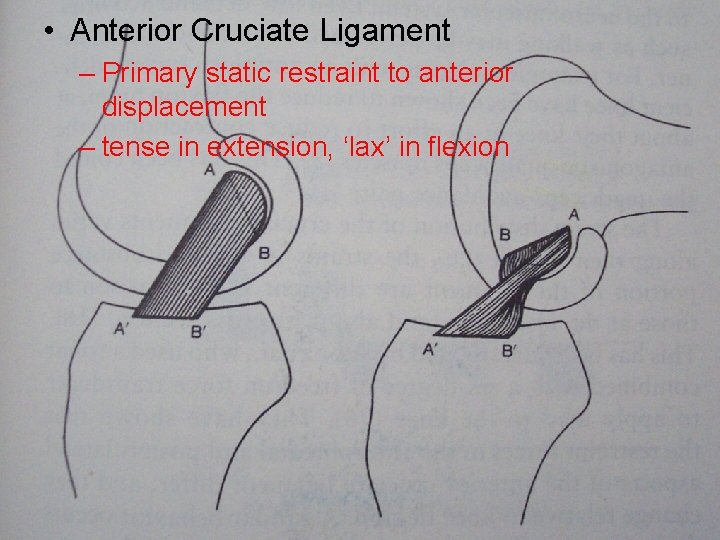
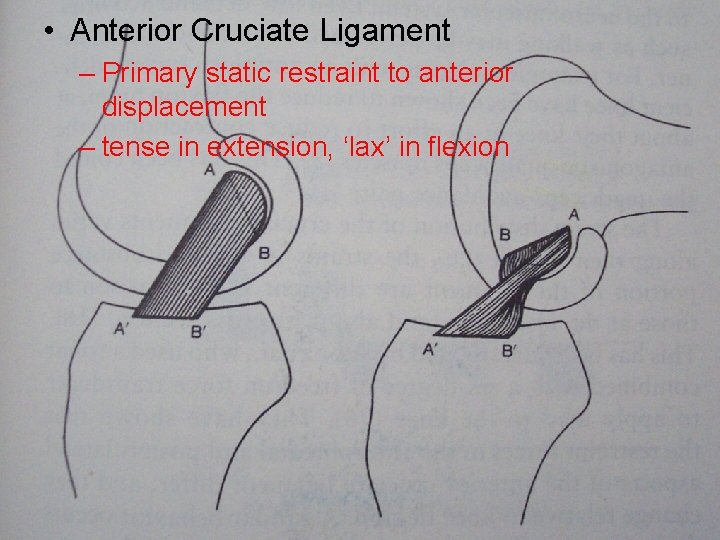
• Anterior Cruciate Ligament – Primary static restraint to anterior displacement – tense in extension, ‘lax’ in flexion
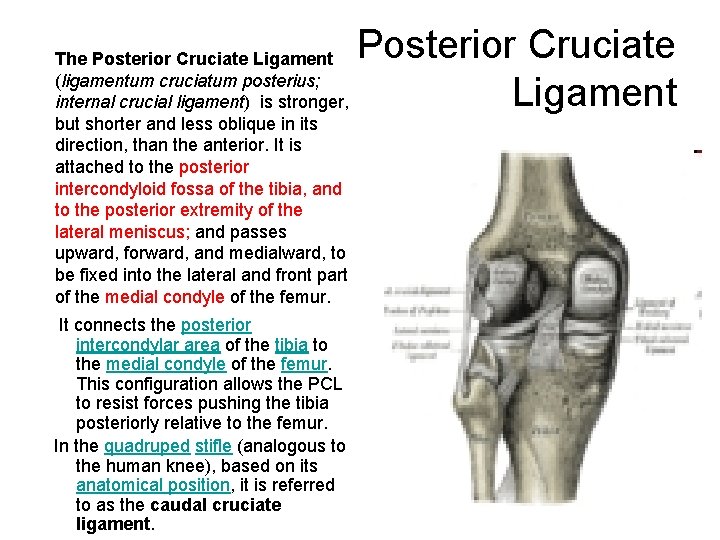
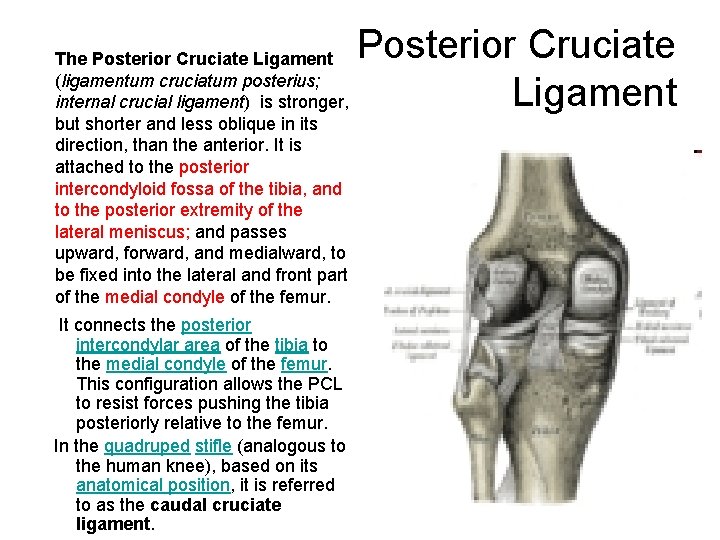
The Posterior Cruciate Ligament (ligamentum cruciatum posterius; internal crucial ligament) is stronger, but shorter and less oblique in its direction, than the anterior. It is attached to the posterior intercondyloid fossa of the tibia, and to the posterior extremity of the lateral meniscus; and passes upward, forward, and medialward, to be fixed into the lateral and front part of the medial condyle of the femur. It connects the posterior intercondylar area of the tibia to the medial condyle of the femur. This configuration allows the PCL to resist forces pushing the tibia posteriorly relative to the femur. In the quadruped stifle (analogous to the human knee), based on its anatomical position, it is referred to as the caudal cruciate ligament. Posterior Cruciate Ligament
Posterior Cruciate Ligament • PCL – Primary restraint to post. Displacement - 90% – relaxed in extension, tense in flexion – reinforced by Humphreys or Wrisberg – restraint to varus/valgus force – resists rotation, esp. int rot of tibia on femur
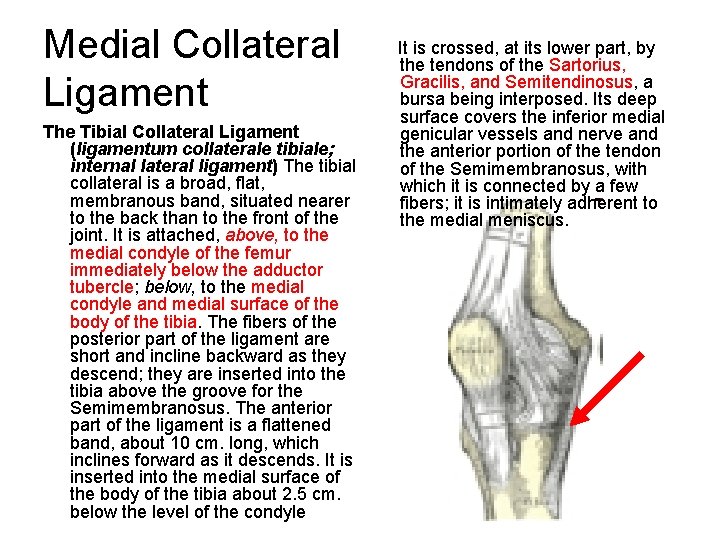
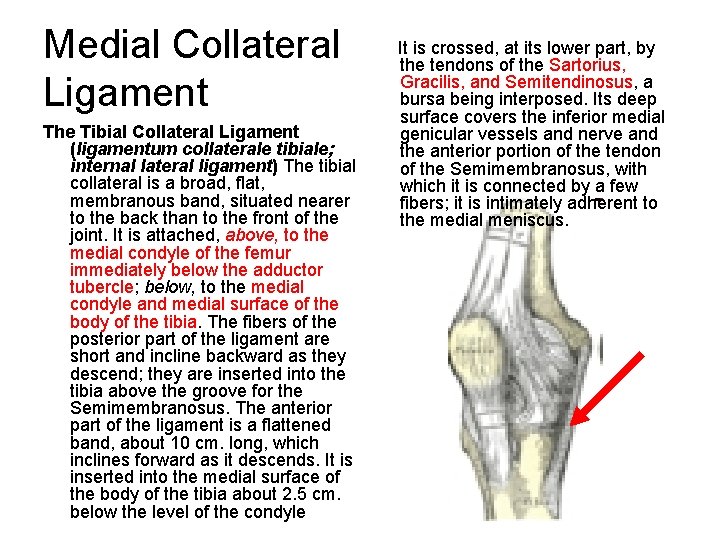
Medial Collateral Ligament It is crossed, at its lower part, by the tendons of the Sartorius, Gracilis, and Semitendinosus, a bursa being interposed. Its deep surface covers the inferior medial The Tibial Collateral Ligament genicular vessels and nerve and (ligamentum collaterale tibiale; the anterior portion of the tendon internal lateral ligament) The tibial of the Semimembranosus, with collateral is a broad, flat, which it is connected by a few membranous band, situated nearer fibers; it is intimately adherent to to the back than to the front of the medial meniscus. joint. It is attached, above, to the medial condyle of the femur immediately below the adductor tubercle; below, to the medial condyle and medial surface of the body of the tibia. The fibers of the posterior part of the ligament are short and incline backward as they descend; they are inserted into the tibia above the groove for the Semimembranosus. The anterior part of the ligament is a flattened band, about 10 cm. long, which inclines forward as it descends. It is inserted into the medial surface of the body of the tibia about 2. 5 cm. below the level of the condyle
Medial side • Superficial MCL – Primary valgus restraint -57 -78% restraining moment of knee – femoral attachment fans out around axis of rot. – Lax in flexion • Semimembranosus (expansion) – internally rot’s tibia on femur – tenses post/med capsular structures that are lax in knee flexion – acts with ACL
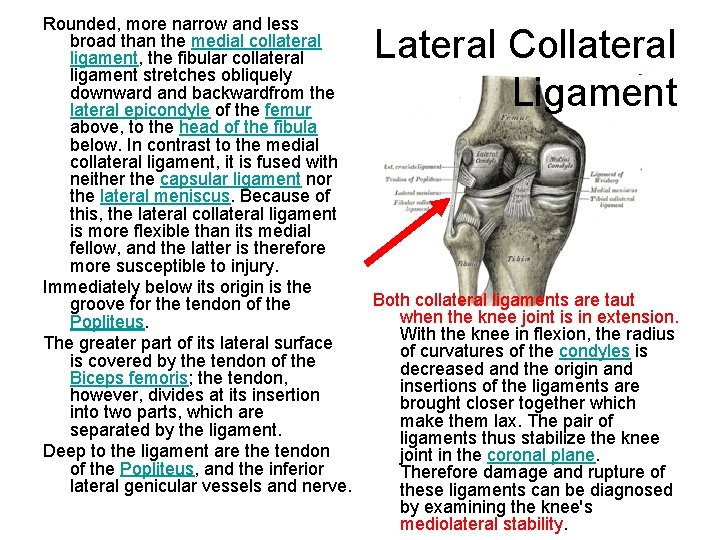
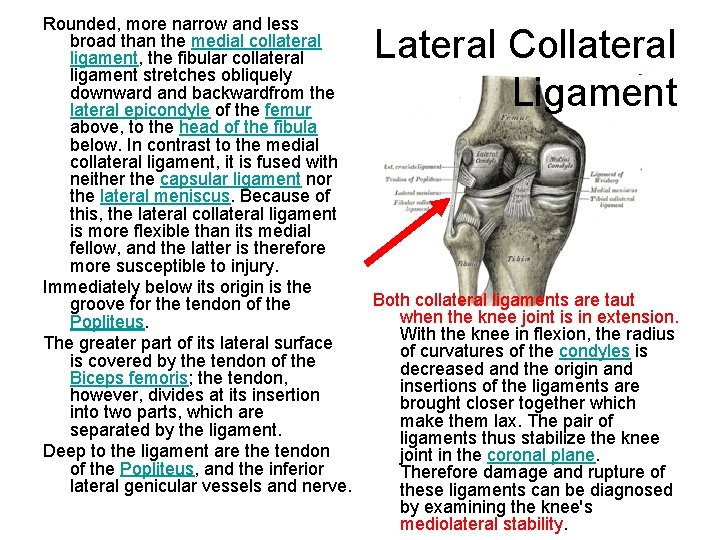
Rounded, more narrow and less broad than the medial collateral ligament, the fibular collateral ligament stretches obliquely downward and backwardfrom the lateral epicondyle of the femur above, to the head of the fibula below. In contrast to the medial collateral ligament, it is fused with neither the capsular ligament nor the lateral meniscus. Because of this, the lateral collateral ligament is more flexible than its medial fellow, and the latter is therefore more susceptible to injury. Immediately below its origin is the groove for the tendon of the Popliteus. The greater part of its lateral surface is covered by the tendon of the Biceps femoris; the tendon, however, divides at its insertion into two parts, which are separated by the ligament. Deep to the ligament are the tendon of the Popliteus, and the inferior lateral genicular vessels and nerve. Lateral Collateral Ligament Both collateral ligaments are taut when the knee joint is in extension. With the knee in flexion, the radius of curvatures of the condyles is decreased and the origin and insertions of the ligaments are brought closer together which make them lax. The pair of ligaments thus stabilize the knee joint in the coronal plane. Therefore damage and rupture of these ligaments can be diagnosed by examining the knee's mediolateral stability.
Lateral Collateral Ligament • Primary varus restraint • lax in flexion • Biceps passes it and blends with insertion • maintains tension?
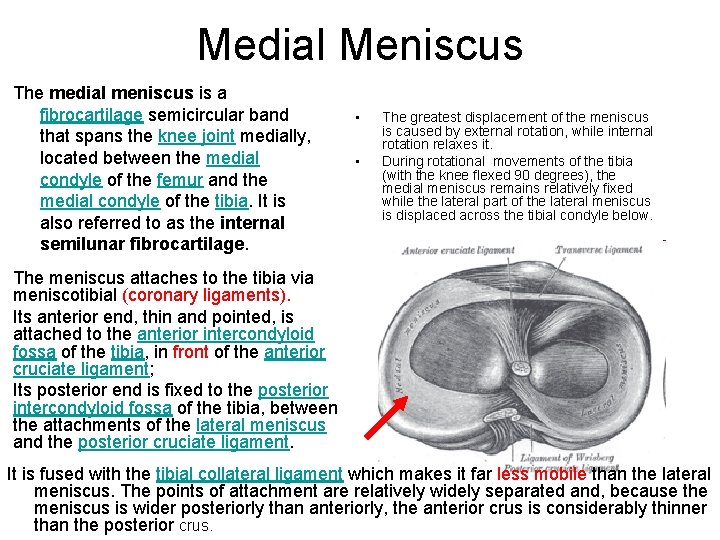
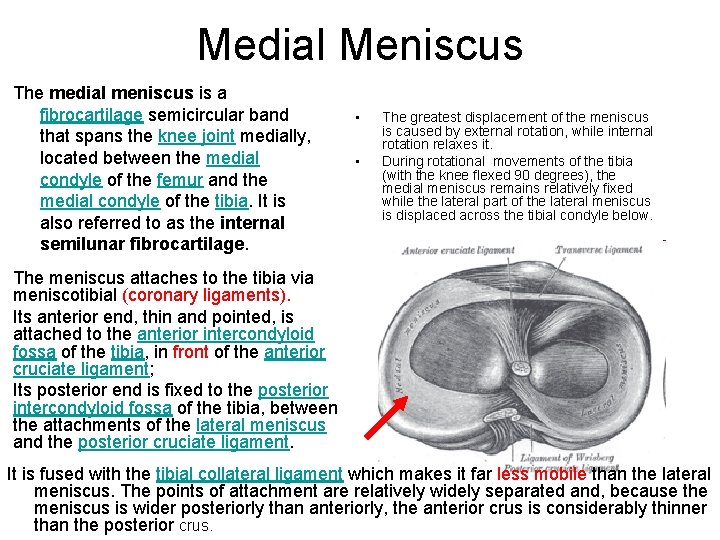
Medial Meniscus The medial meniscus is a fibrocartilage semicircular band that spans the knee joint medially, located between the medial condyle of the femur and the medial condyle of the tibia. It is also referred to as the internal semilunar fibrocartilage. • • The greatest displacement of the meniscus is caused by external rotation, while internal rotation relaxes it. During rotational movements of the tibia (with the knee flexed 90 degrees), the medial meniscus remains relatively fixed while the lateral part of the lateral meniscus is displaced across the tibial condyle below. The meniscus attaches to the tibia via meniscotibial (coronary ligaments). Its anterior end, thin and pointed, is attached to the anterior intercondyloid fossa of the tibia, in front of the anterior cruciate ligament; Its posterior end is fixed to the posterior intercondyloid fossa of the tibia, between the attachments of the lateral meniscus and the posterior cruciate ligament. It is fused with the tibial collateral ligament which makes it far less mobile than the lateral meniscus. The points of attachment are relatively widely separated and, because the meniscus is wider posteriorly than anteriorly, the anterior crus is considerably thinner than the posterior crus.
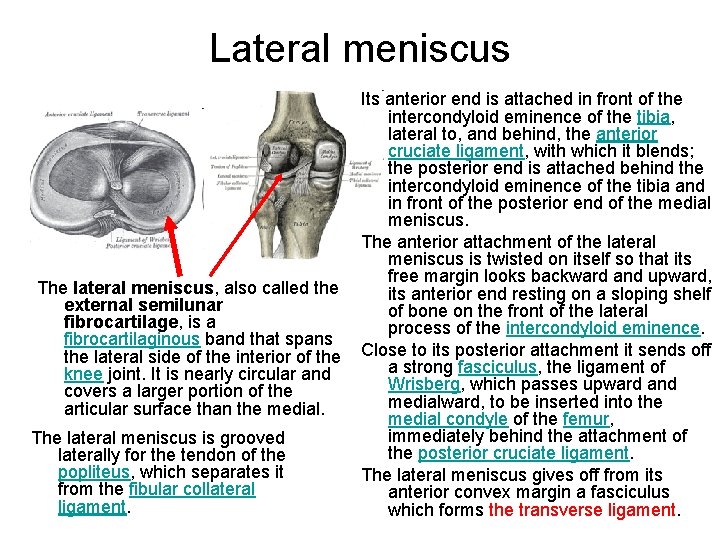
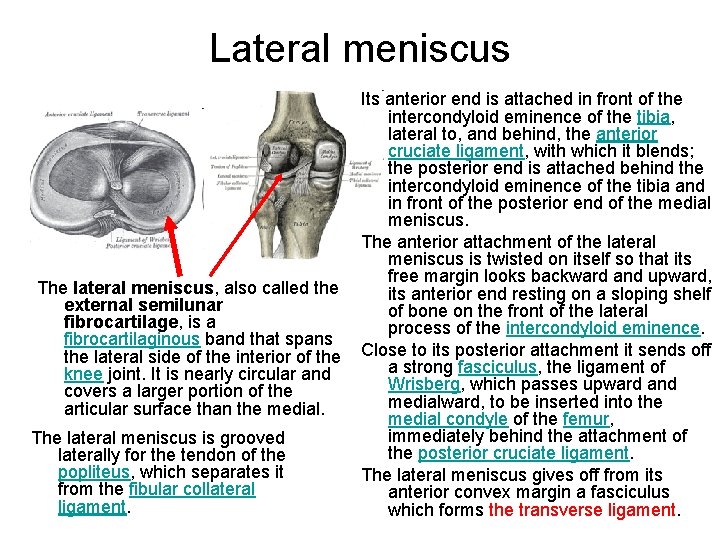
Lateral meniscus Its anterior end is attached in front of the intercondyloid eminence of the tibia, lateral to, and behind, the anterior cruciate ligament, with which it blends; the posterior end is attached behind the intercondyloid eminence of the tibia and in front of the posterior end of the medial meniscus. The anterior attachment of the lateral meniscus is twisted on itself so that its free margin looks backward and upward, The lateral meniscus, also called the its anterior end resting on a sloping shelf external semilunar of bone on the front of the lateral fibrocartilage, is a process of the intercondyloid eminence. fibrocartilaginous band that spans the lateral side of the interior of the Close to its posterior attachment it sends off a strong fasciculus, the ligament of knee joint. It is nearly circular and Wrisberg, which passes upward and covers a larger portion of the medialward, to be inserted into the articular surface than the medial condyle of the femur, immediately behind the attachment of The lateral meniscus is grooved the posterior cruciate ligament. laterally for the tendon of the popliteus, which separates it The lateral meniscus gives off from its from the fibular collateral anterior convex margin a fasciculus ligament. which forms the transverse ligament.
2 functions • load bearing • stability also, joint lubrication prevent capsule, synovial impingement shock absorbers Knee joint stability mainly rotational miniscectomy +/- ACL and translation why differences in lat vs med ? Structure attachments
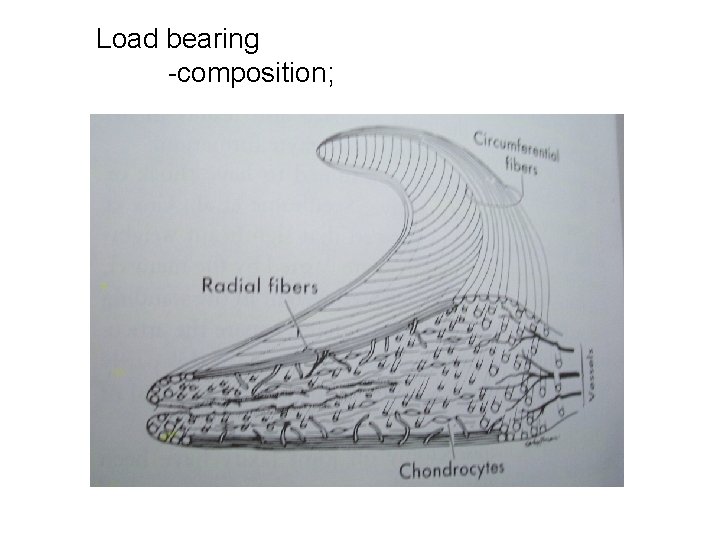
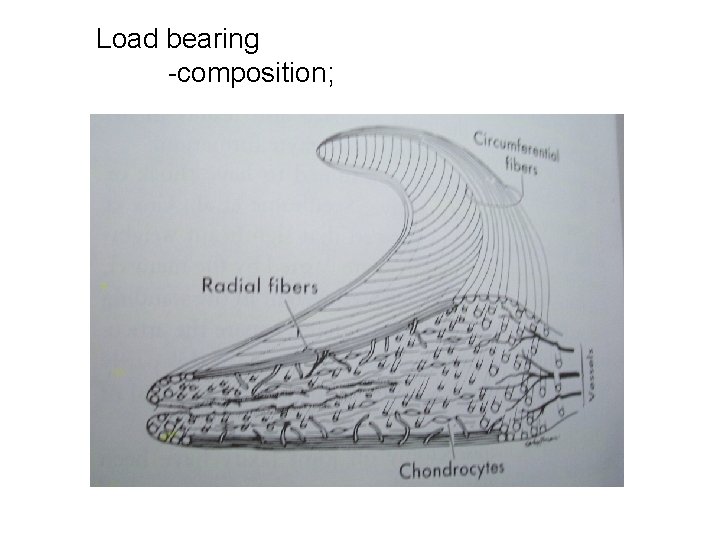
Load bearing -composition;
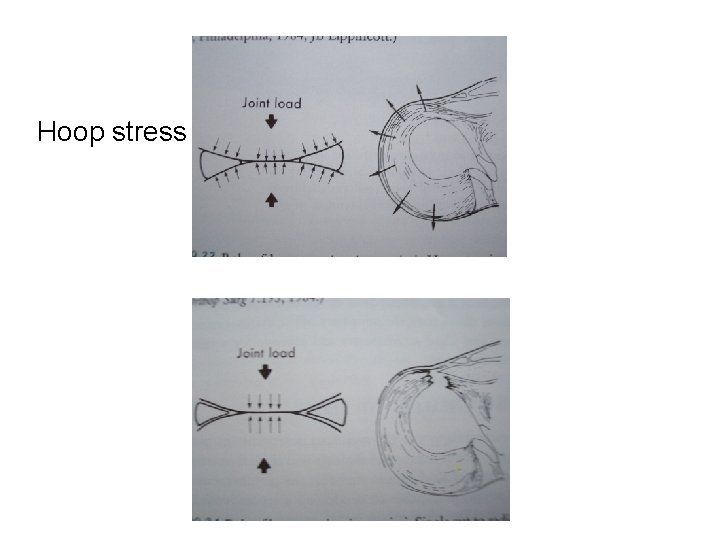
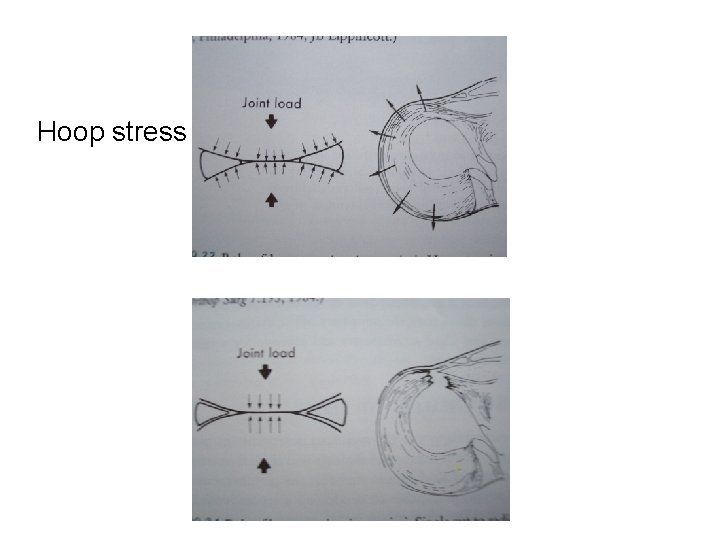
Hoop stress
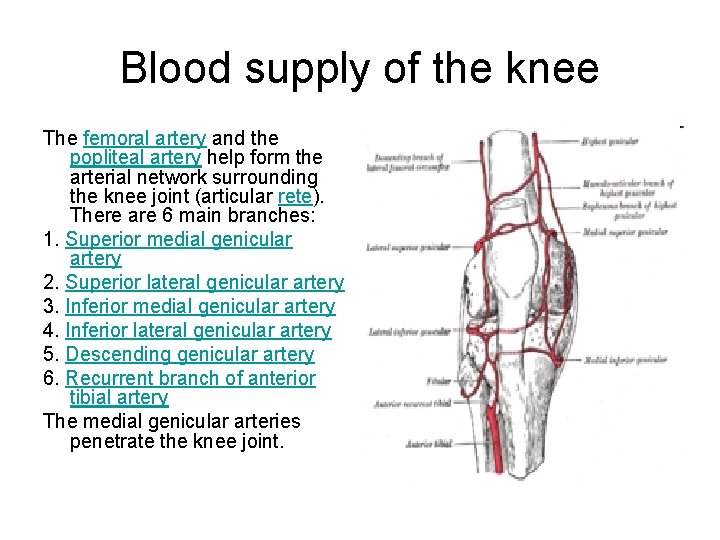
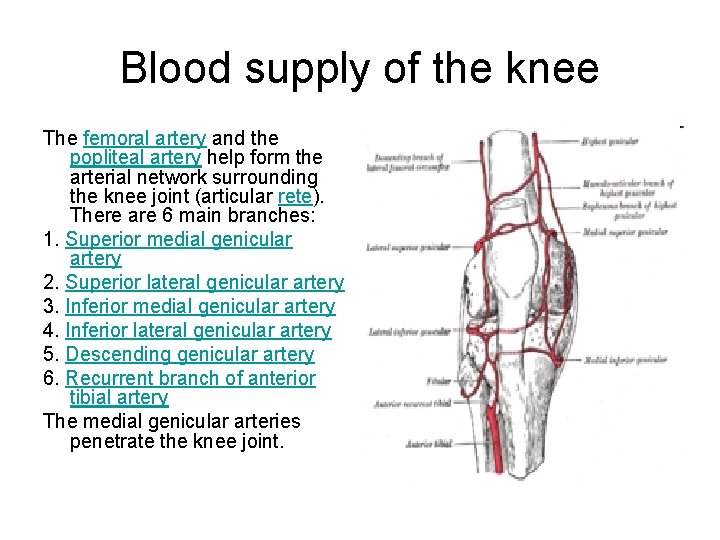
Blood supply of the knee The femoral artery and the popliteal artery help form the arterial network surrounding the knee joint (articular rete). There are 6 main branches: 1. Superior medial genicular artery 2. Superior lateral genicular artery 3. Inferior medial genicular artery 4. Inferior lateral genicular artery 5. Descending genicular artery 6. Recurrent branch of anterior tibial artery The medial genicular arteries penetrate the knee joint.
Knee joint • Ginglymus (hinge) ? • Arthodial (gliding) ? • 6 degrees of freedom – 3 rotations – 3 translations
• Rotations – flex/ext - -15 to 140 deg – Varus/valgus - 6 -8 deg in extension – int/ext rotation - 25 - 30 deg in flexion • Translations AP 5 - 10 mm compression/distraction 2 - 5 mm medio-lateral 1 -2 mm
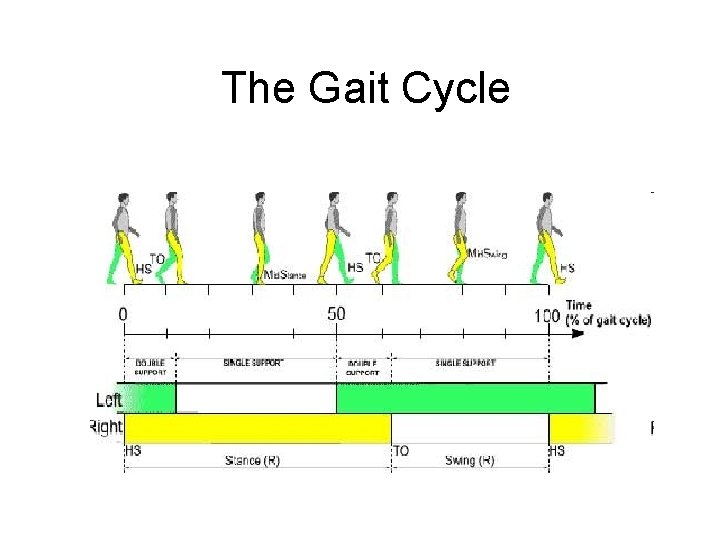
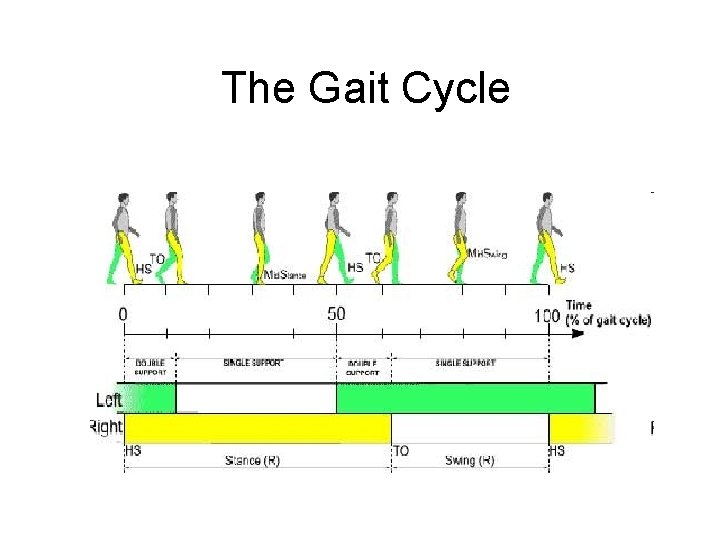
The Gait Cycle
Taking a step • Just prior to heel strike - max extension & max external rotation • heel strike - max valgus • flat foot - flexion & internal rotation progress • swing phase - internal rotation continues, max flexion, max anterior translation.
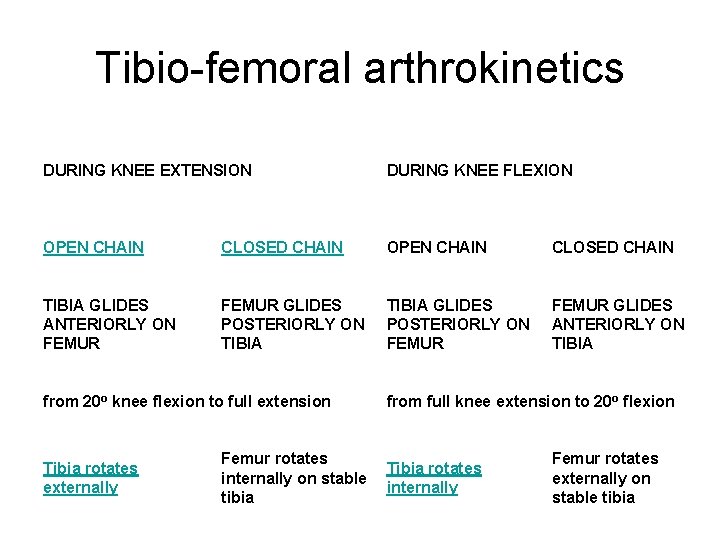
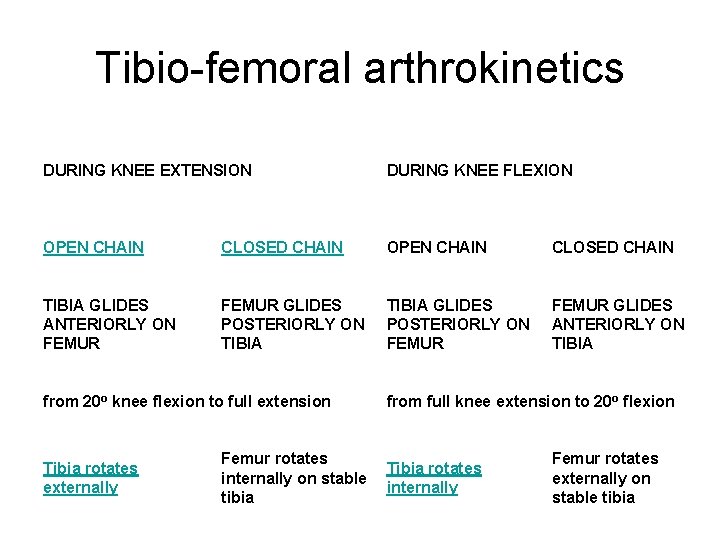
Tibio-femoral arthrokinetics DURING KNEE EXTENSION DURING KNEE FLEXION OPEN CHAIN CLOSED CHAIN TIBIA GLIDES ANTERIORLY ON FEMUR GLIDES POSTERIORLY ON TIBIA GLIDES POSTERIORLY ON FEMUR GLIDES ANTERIORLY ON TIBIA from 20 o knee flexion to full extension Tibia rotates externally from full knee extension to 20 o flexion Femur rotates Tibia rotates internally on stable internally tibia Femur rotates externally on stable tibia
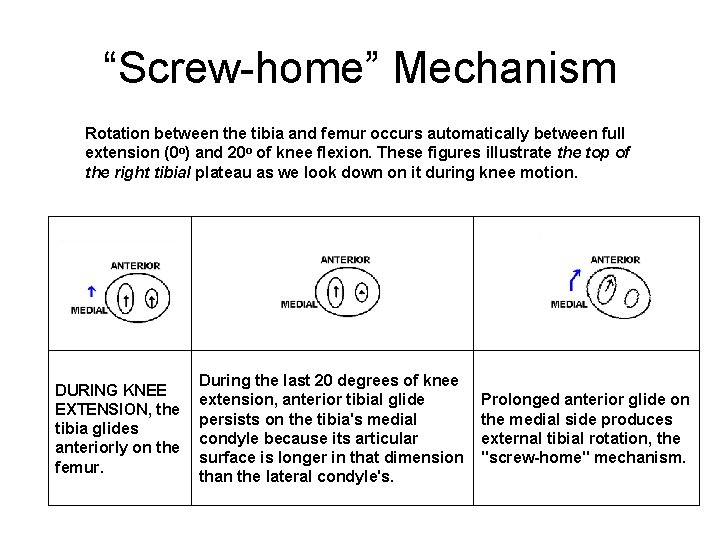
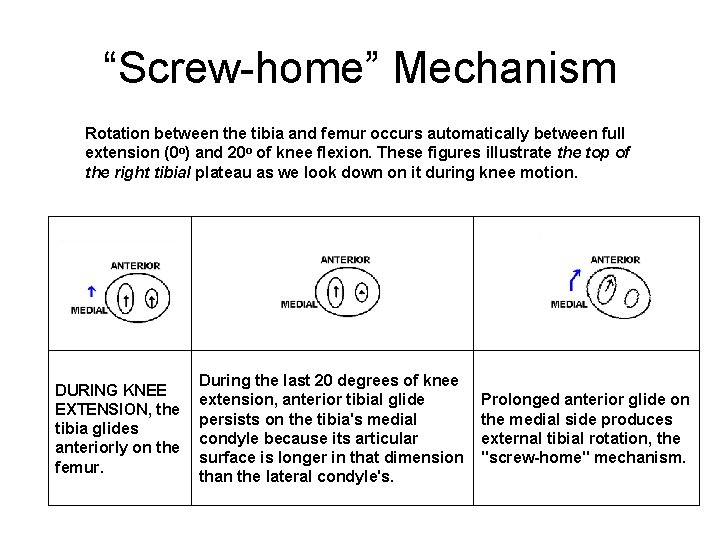
“Screw-home” Mechanism Rotation between the tibia and femur occurs automatically between full extension (0 o) and 20 o of knee flexion. These figures illustrate the top of the right tibial plateau as we look down on it during knee motion. DURING KNEE EXTENSION, the tibia glides anteriorly on the femur. During the last 20 degrees of knee extension, anterior tibial glide persists on the tibia's medial condyle because its articular surface is longer in that dimension than the lateral condyle's. Prolonged anterior glide on the medial side produces external tibial rotation, the "screw-home" mechanism.
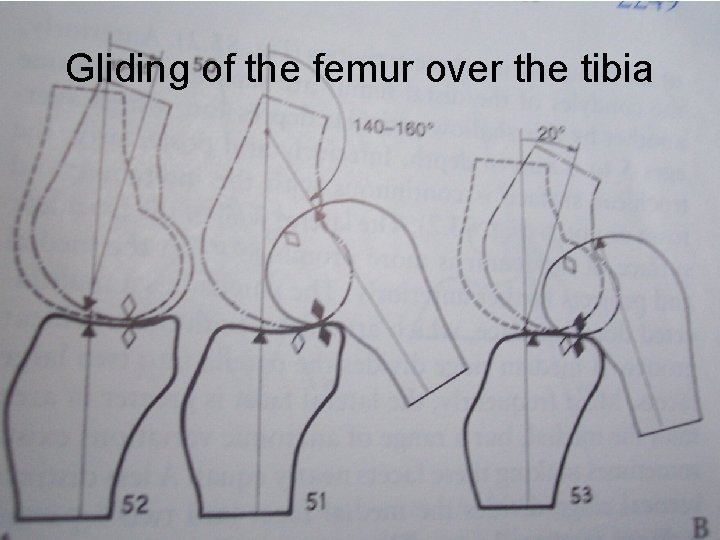
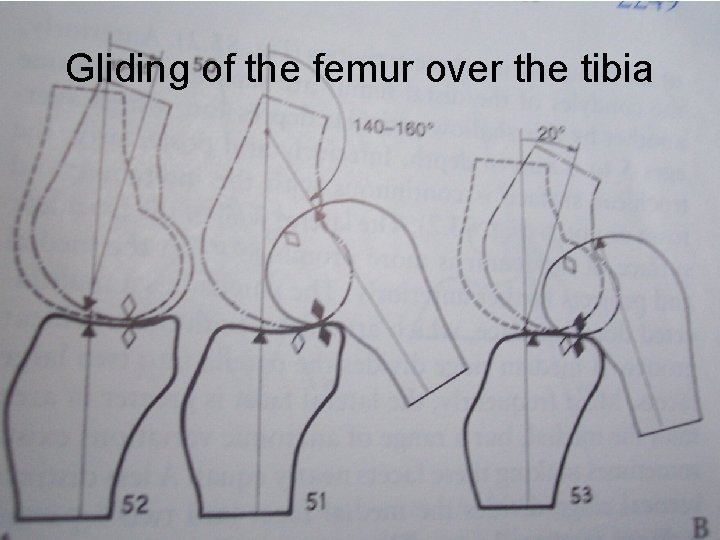
Gliding of the femur over the tibia
Bi-pedal ambulation
Thank you!
 Iliopsoas
Iliopsoas Extend thigh
Extend thigh Muscle compartment of thigh
Muscle compartment of thigh Thigh muscles medial
Thigh muscles medial Muscles innervated by obturator nerve
Muscles innervated by obturator nerve Gracilis cadaver
Gracilis cadaver Sacral plexus
Sacral plexus Unipennate
Unipennate Anterior knee pain ddx
Anterior knee pain ddx Envelope nuclear
Envelope nuclear Titanic watertight compartments diagram
Titanic watertight compartments diagram Comminuted fracture
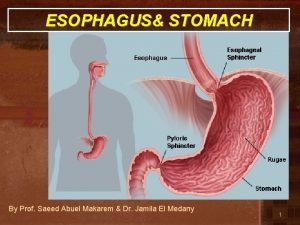
Comminuted fracture Cardiac orifice
Cardiac orifice Transcellular fluid
Transcellular fluid Extensor carpi ulnaris origin and insertion
Extensor carpi ulnaris origin and insertion Sci compartments si/tk/g/hcs
Sci compartments si/tk/g/hcs What is community bag
What is community bag Blood loss estimation gauze
Blood loss estimation gauze Estimated blood volume
Estimated blood volume Tonicity vs osmolarity
Tonicity vs osmolarity Gastroncnemius
Gastroncnemius Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Retroversion vs anteversion
Retroversion vs anteversion Ferratima
Ferratima Thigh foot angle
Thigh foot angle Fascia of thigh
Fascia of thigh Where is thigh located
Where is thigh located Medline
Medline Medial plantar nerve
Medial plantar nerve Thigh cross section
Thigh cross section Extend thigh
Extend thigh Lower extremity muscles
Lower extremity muscles Cribriform fascia
Cribriform fascia Greater sciatic foramen contents
Greater sciatic foramen contents Cross section thigh
Cross section thigh Slidetodoc.com
Slidetodoc.com Head body head body gif
Head body head body gif Lateral thigh injection site
Lateral thigh injection site Flexed thigh
Flexed thigh Thigh surface anatomy
Thigh surface anatomy Anterolateral thigh injection site
Anterolateral thigh injection site Sarcoma
Sarcoma Thigh lupa
Thigh lupa Superior gluteal artery
Superior gluteal artery Thigh sarcoma
Thigh sarcoma Mid inguinal point
Mid inguinal point What is hilton's law
What is hilton's law Anatomic adjective for thigh
Anatomic adjective for thigh Inner thigh caning
Inner thigh caning Hamstring short head
Hamstring short head Tuberoz meme
Tuberoz meme Intradermal injection
Intradermal injection Leg muscles
Leg muscles What is the name
What is the name Hip pointer moi
Hip pointer moi Orbicularis oculi origin and insertion
Orbicularis oculi origin and insertion