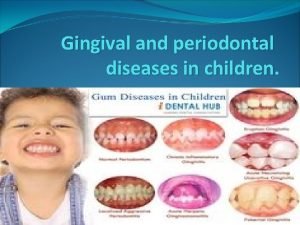
GINGIVAL AND PERIODONTAL DISEASES AND CONDITIONS OF CHILDHOOD
- Slides: 35
GINGIVAL AND PERIODONTAL DISEASES AND CONDITIONS OF CHILDHOOD AND ADOLESCENCE
INTRODUCTION n It is postulated that periodontal disease in adults is, at least in part, precipitated by Gingival inflammation in the formative years of childhood and early adolescence.
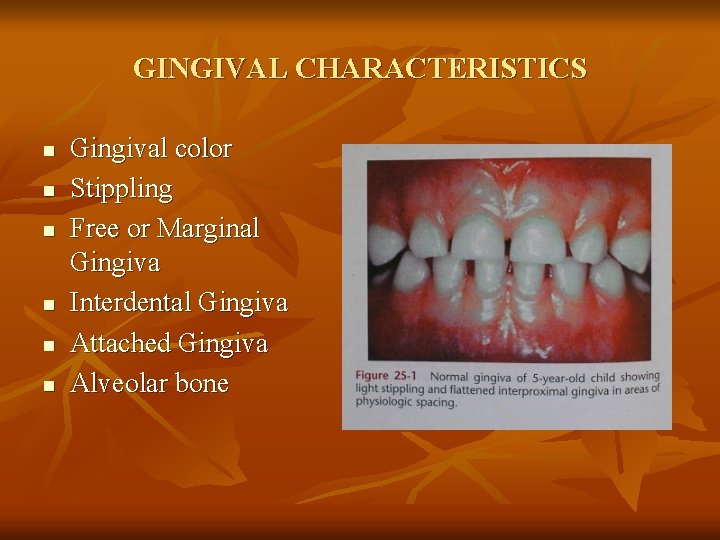
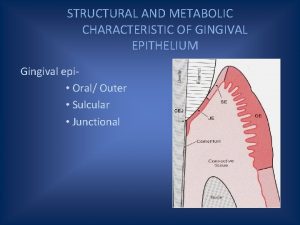
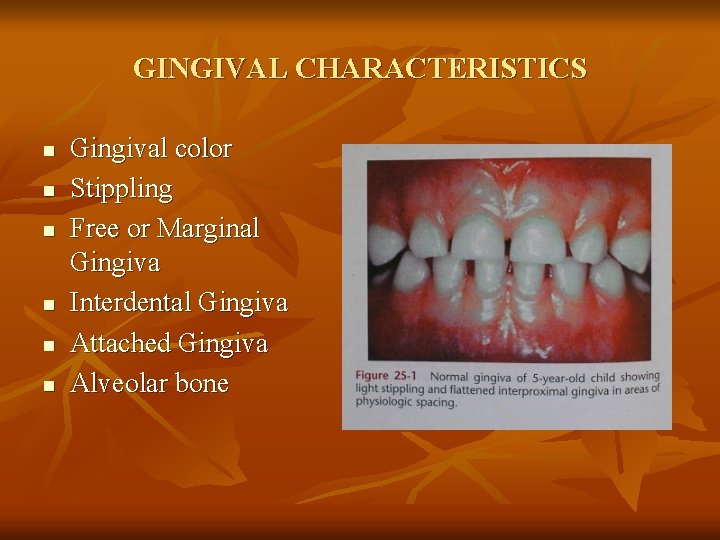
GINGIVAL CHARACTERISTICS n n n Gingival color Stippling Free or Marginal Gingiva Interdental Gingiva Attached Gingiva Alveolar bone
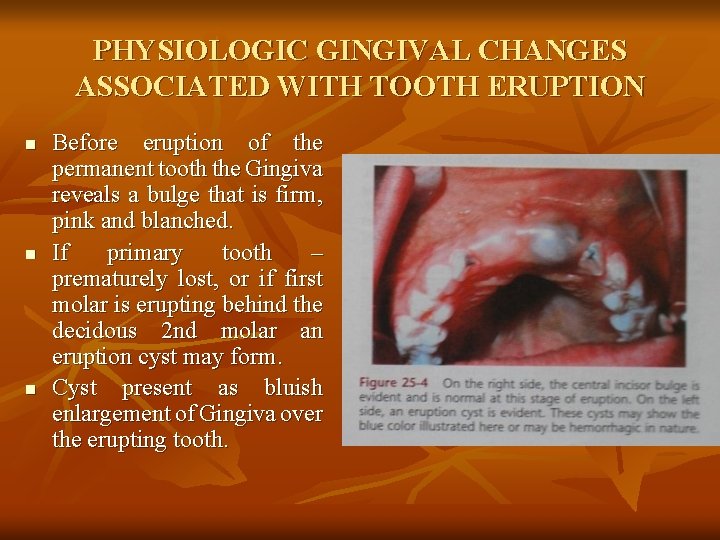
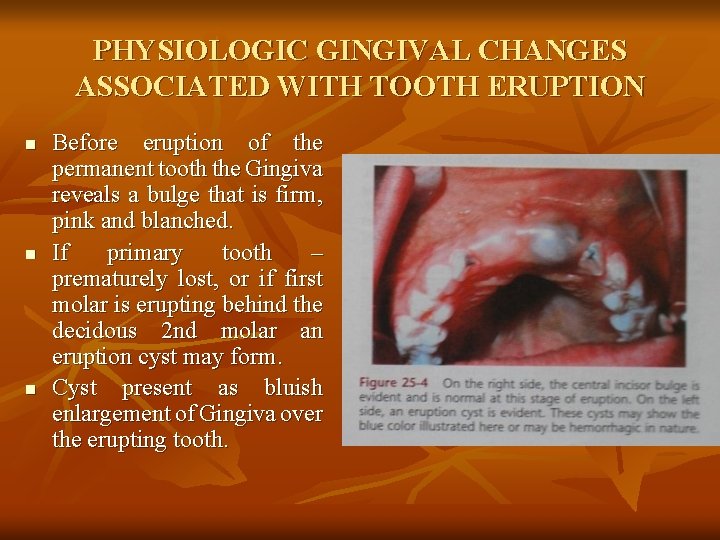
PHYSIOLOGIC GINGIVAL CHANGES ASSOCIATED WITH TOOTH ERUPTION n n n Before eruption of the permanent tooth the Gingiva reveals a bulge that is firm, pink and blanched. If primary tooth – prematurely lost, or if first molar is erupting behind the decidous 2 nd molar an eruption cyst may form. Cyst present as bluish enlargement of Gingiva over the erupting tooth.
Sites: n Permanent mandibular incisors and first molars. Treatment: n many resolve with out treatment. n If painful – marsupialized
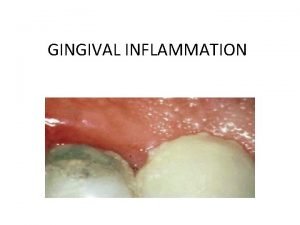
GINGIVAL DISEASE 1. Plaque induced gingivitis: It is an inflammation of the Gingiva resulting from bacterial plaque located at the Gingival margin.
Site: n Begins at the gingival margin and can spread through out the remaining Gingival unit. Prevalence: n Increases with age until it reaches puberty. Clinical Signs: n Inflammation – changes to Gingival contour, colour, consistency. n Stable periodontium with no loss of periodontal attachment or alveolar bone. n In children, Gingvitis is not as intense as that found in young adults. COMMON CLINICAL FINDINGS: n Erythema, Edema, bleeding, sensitivity, tenderness and enlargement.
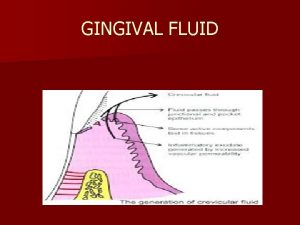
Development and severity of Gingivitis is associated with n quantity or quality of dental plaque. n Response of immune system. n Morphological differences in the periodontium between children and adults. Dental plaque of children contains: n lower concentrations of putative periodontal pathogens. n Few B lymphocytes and plasma cells. n Presence of thicker junctional Epithelium and increased vascularity in Gingival connective tissues and developing immune system.
2. n n Gingival diseases associated with Endogenous sex steroid hormones: Steroid hormones – affect the host by influencing cellular function immune function together with hormone – selected bacterial populations occupying the Gingival sulcus.
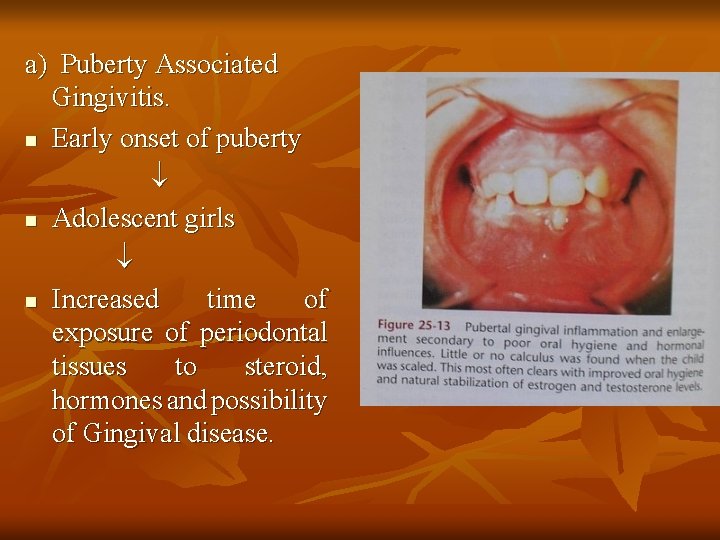
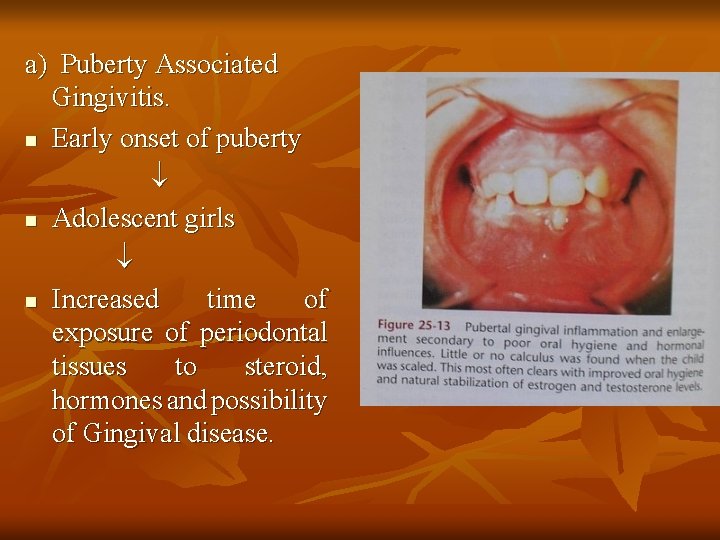
a) Puberty Associated Gingivitis. n Early onset of puberty n Adolescent girls n Increased time of exposure of periodontal tissues to steroid, hormones and possibility of Gingival disease.
Factors influencing: n plaque levels n Dental caries n Mouth breathing n Crowding of teeth n Tooth eruption Clinical features: n signs of Gingival inflammation in the presence of relatively small amounts of local irritants.
b) Menstrual cycle – associated gingivitis: - minor signs of gingival inflammation during ovulation. n - Gingival exudate increases. n
c) Pregnancy – associated Gingivitis: - Increase in prevalence and severity – 2 nd and 3 rd trimesters. - Pregnancy associated pyogenic Granuloma. (pregnancy tumor) - Exaggerated inflammatory response during pregnancy. Clinical features: Painless, protuberant, mushroom like exophytic mass – sessile or pedunculated base. Site: n Gingival margin, interproximal papilla.
3. Gingival Diseases associated with medication. n Drug induced Gingival enlargement. a) Anti convulsants. n Eg. Phenytoin sodium: Etiology n Growth of genetically distinct populations of Gingival fibroblasts. n Accumulation of connective tissues because of reduced catabolism of collagen molecule.
b) Calcium channel blockers: Eg. Nifedipine, verapamil, diltiazem. n Directly influence Gingival connective tissues. n Stimulating an increase of Gingival fibroblasts and increase in production of connective tissue matrix. c) Immuno suppressants: Eg. Cyclosporine n more vascularized than phenytoin enlargement.
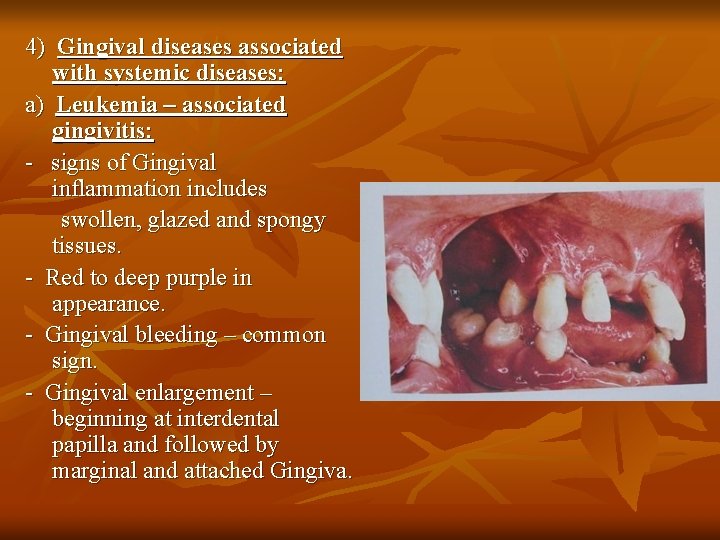
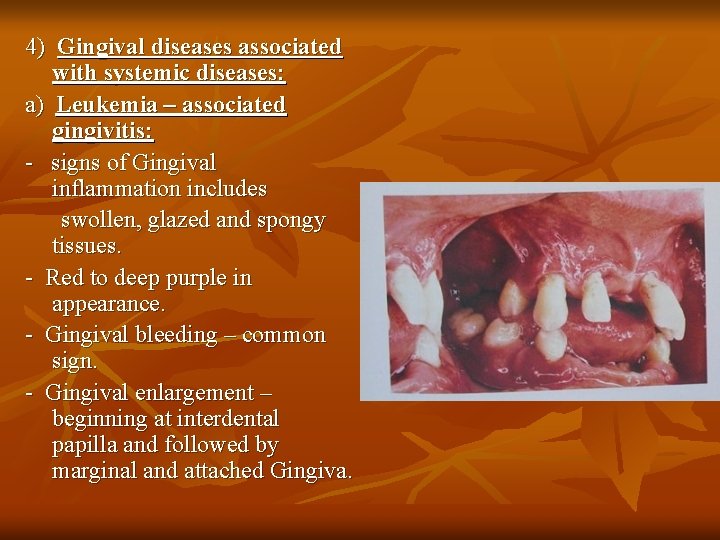
4) Gingival diseases associated with systemic diseases: a) Leukemia – associated gingivitis: - signs of Gingival inflammation includes swollen, glazed and spongy tissues. - Red to deep purple in appearance. - Gingival bleeding – common sign. - Gingival enlargement – beginning at interdental papilla and followed by marginal and attached Gingiva.
b) Linear Gingival Erythema - Associated with HIV infection. - 2 – 3 mm marginal band of intense Erythema in the free gingiva, extend into attached Gingiva. - may be focal or diffuse Erythema and / or extend beyond mucogingival line into alveolar mucosa. - Localized to one or two teeth. - more commonly generalized Gingival condition. - increased number of Ig. G, plasma cells and PMNL.
5) Gingival diseases associated with mal nutrition. Eg. Vitamin C deficiency or scurvy. - scorbutic Gingivitis appears similar to plaque – induced Gingivitis. 6) Gingival diseases associated with heredity: - Benign, non-inflammatory fibrotic enlargement of maxillary and or mandibular Gingiva – familial aggregation.
n Slowly progressive Gingival enlargement which develops upon eruption of permanent dentition. Site: n Disease – localised or generalised and ultimately cover occlusal surfaces of teeth. Appearance: n Enlarged gingiva – non-hemorrhagic and firm, and Gingival inflammation is present.
GINGIVAL DISEASES ASSOCIATED WITH ULCERATIVE LESIONS. a) Acute Necrotising ulcerative gingivitis. Synonyms: n Trench mouth n Vincent’s infection
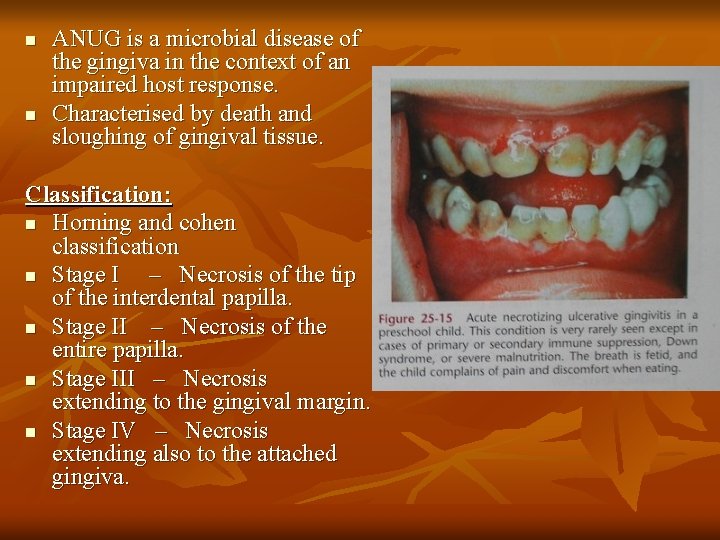
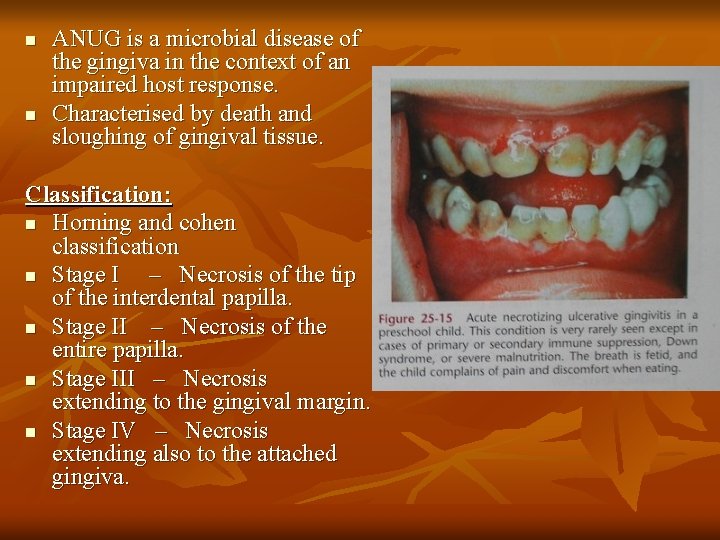
n n ANUG is a microbial disease of the gingiva in the context of an impaired host response. Characterised by death and sloughing of gingival tissue. Classification: n Horning and cohen classification n Stage I – Necrosis of the tip of the interdental papilla. n Stage II – Necrosis of the entire papilla. n Stage III – Necrosis extending to the gingival margin. n Stage IV – Necrosis extending also to the attached gingiva.
n n n Stage V – mucosa. Stage VI – Stage VII – Necrosis extending in to buccal or labial Necrosis exposing alveolar bone. Necrosis perforating skin of cheek. Etiology: n Fuso spirochaetal infection. Clinical Features: n punched out crater like depressions at the crest of the interdental papilla. n Gingival craters covered by gray, pseudomembranous slough. n Pronounced linear erythema. n Spontaneous gingival hemorrhage.
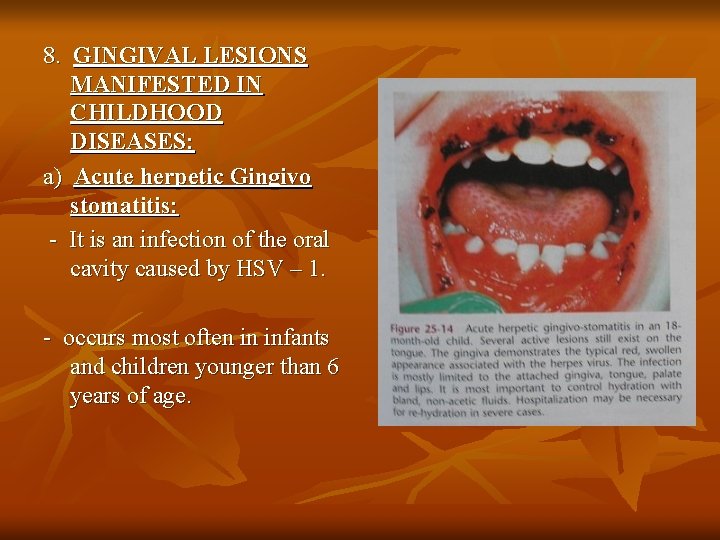
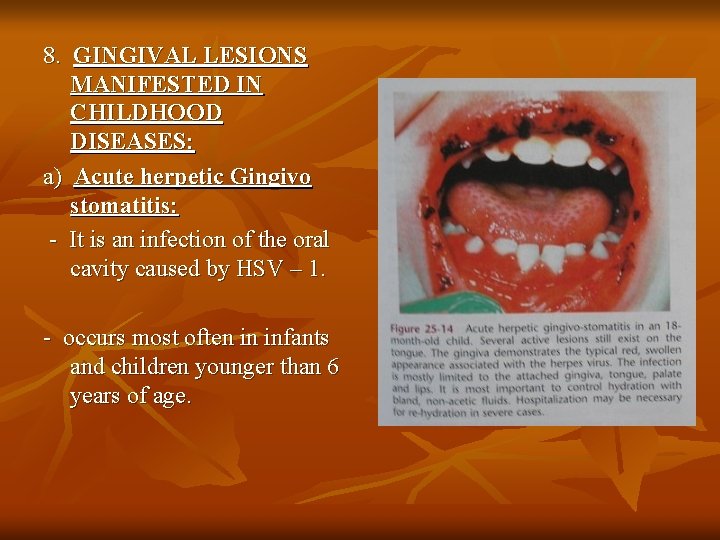
8. GINGIVAL LESIONS MANIFESTED IN CHILDHOOD DISEASES: a) Acute herpetic Gingivo stomatitis: - It is an infection of the oral cavity caused by HSV – 1. - occurs most often in infants and children younger than 6 years of age.
Clinical features: n appears as a diffuse, erythematous, shiny involvement of the gingiva and adjacent oral mucosa. n Characterized by presence of discrete, spherical gray vesicles. n After 24 hours, vesicles rupture n Painful small ulcers b) Gingival lesions associated with varicella zoster infection - affects individuals under the age of 15 years. - produces skin lesions characterized by pustules that break and crust over. - ulcers – palate, Gingiva, buccal mucosa and are not painful.
c) Gingival lesions associated with infectious mononucleosis. - Etiology: n Epstein – barr virus. n Gingival bleeding, petechiae of the soft palate, ulceration of gingiva and buccal mucosa, pericoronitis d) Soft tissue lesions associated with herpangina Etiology: Coxsackie Group A virus. Clinical presentation: n numerous small vesicles which proceed to small ulcers contained on a gray base and inflamed at the periphery.
n n Ulcers – anterior facial pillars, hard or soft plate, posterior pharyngeal wall, buccal mucosa or tongue. Ulcers are not painful and heals within a few days to a week. e) Soft tissue lesions associated with Hand foot and mouth disease. n - occur in children between 6 months and 5 years of age. Etiology: n coxsackie Group A virus. Presentation: n ulcerative lesions on hard palate, tongue and buccal mucosa. n Disease is generally self limiting and will regress in 1 – 2 weeks.
9. ACUTE INFLAMMATORY GINGIVAL ENLARGEMENT. - Acute painful, rapidly expanding lesion localized to the Gingiva. Site: n marginal gingiva or Interdental papilla. Presentation: n Bright red Gingival swelling n Pointed and fluctuant mass from which purulent exudates may be expressed. n Lesion is self limiting, ultimately, rupturing if permitted to progress.
PERIODONTAL DISEASES n It includes: i) periodontal abscess ii) Aggressive periodontitis - localized - generalized iii) Periodontitis associated with systemic disease and genetic abnormalities.
a) Systemic diseases and conditions that enhance susceptibility for periodontitis. - Diabetes mellitus AIDS Stress Leukemias Neutropenia and agranulocytosis. Genetic abnormalities. Eg. Papillon lefevre syndrome. b) Periodontitis that enhance the risk for certain systemic diseases and conditions. v) Necrotising ulcerative periodontitis (NUP)
PERIODONTAL ABSCESS: n It is an acute suppurative inflammation of the deeper periodontal tissues caused by an infection of pyogenic bacteria. Mechanism of abscess formation. n Extension of pocket in to the supporting periodontal tissues along the lateral aspect of the tooth root. n Lateral extension of the inner pocket surface into the connective tissue of the pocket wall. n Incomplete removal of calculus results in tissue shrinkage with subsequent occlusion of the pocket opening. n Following traumatic injury of a tooth or a perforation of the lateral wall of the root during endodontic treatment.
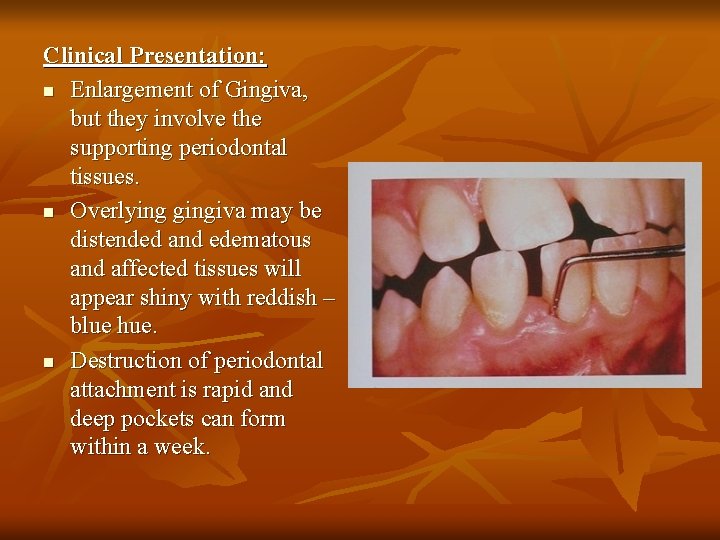
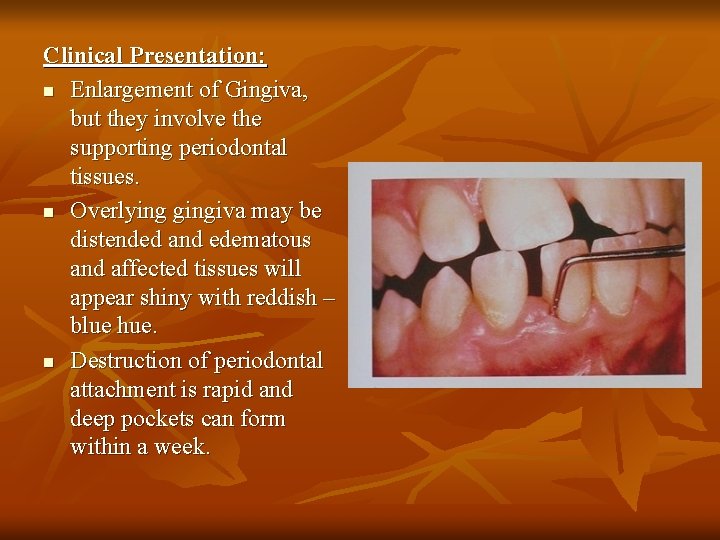
Clinical Presentation: n Enlargement of Gingiva, but they involve the supporting periodontal tissues. n Overlying gingiva may be distended and edematous and affected tissues will appear shiny with reddish – blue hue. n Destruction of periodontal attachment is rapid and deep pockets can form within a week.
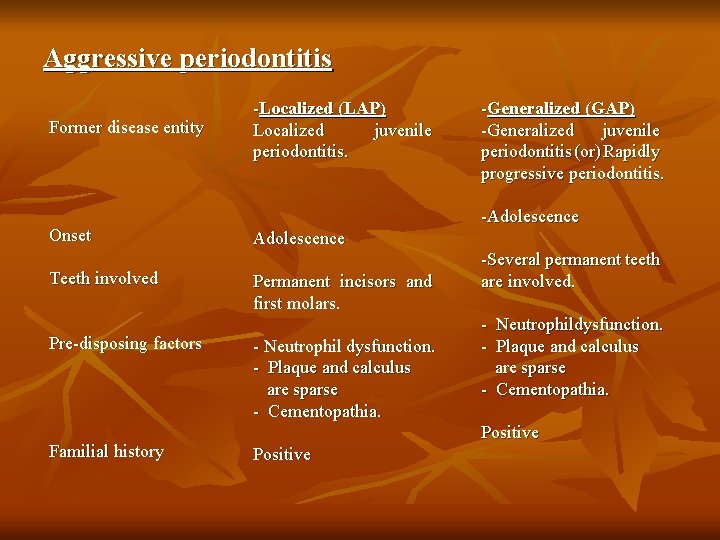
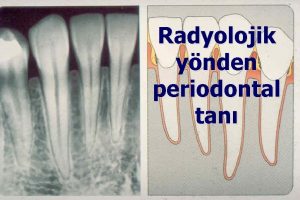
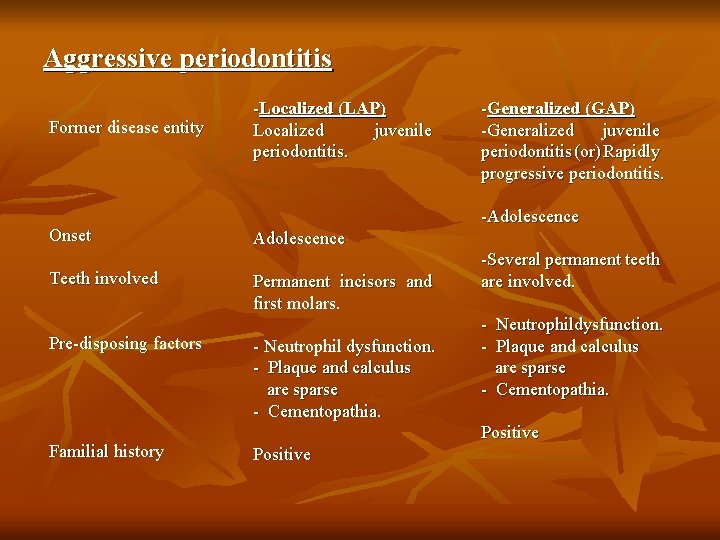
Aggressive periodontitis Former disease entity Onset Teeth involved Pre-disposing factors Familial history -Localized (LAP) Localized juvenile periodontitis. -Generalized (GAP) -Generalized juvenile periodontitis (or) Rapidly progressive periodontitis. -Adolescence Permanent incisors and first molars. - Neutrophil dysfunction. - Plaque and calculus are sparse - Cementopathia. -Several permanent teeth are involved. - Neutrophildysfunction. - Plaque and calculus are sparse - Cementopathia. Positive
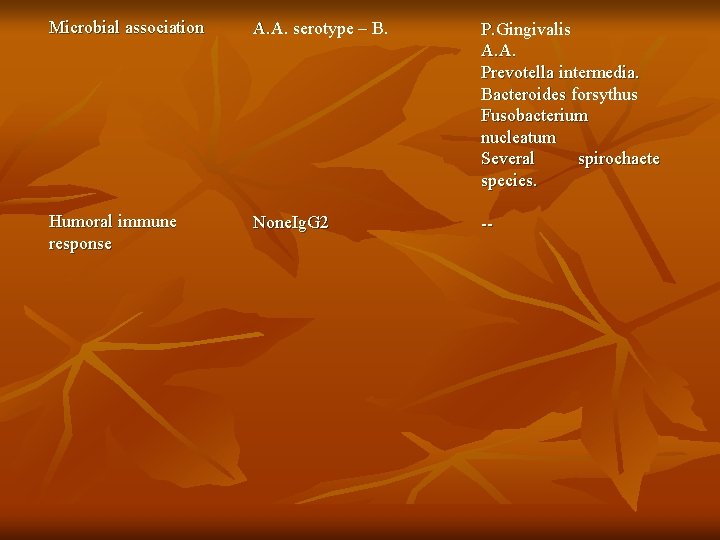
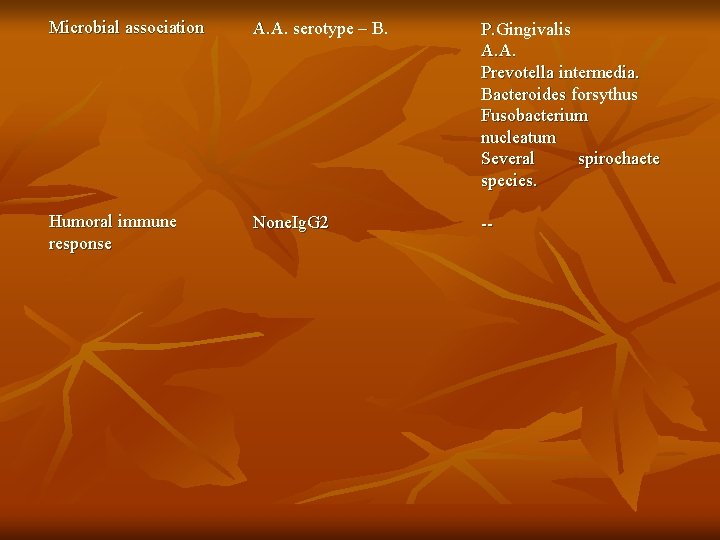
Microbial association A. A. serotype – B. P. Gingivalis A. A. Prevotella intermedia. Bacteroides forsythus Fusobacterium nucleatum Several spirochaete species. Humoral immune response None. Ig. G 2 --
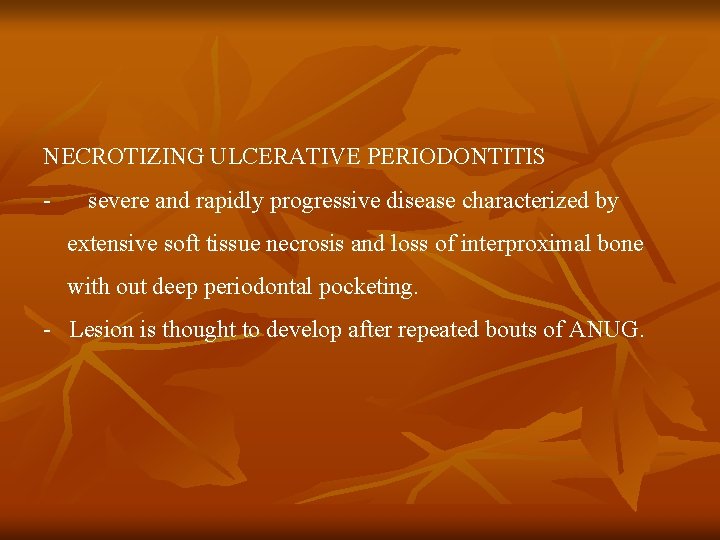
NECROTIZING ULCERATIVE PERIODONTITIS - severe and rapidly progressive disease characterized by extensive soft tissue necrosis and loss of interproximal bone with out deep periodontal pocketing. - Lesion is thought to develop after repeated bouts of ANUG.
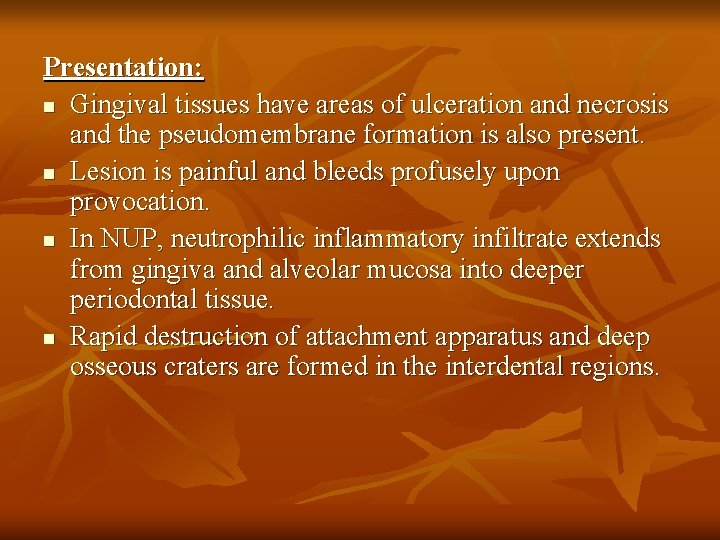
Presentation: n Gingival tissues have areas of ulceration and necrosis and the pseudomembrane formation is also present. n Lesion is painful and bleeds profusely upon provocation. n In NUP, neutrophilic inflammatory infiltrate extends from gingiva and alveolar mucosa into deeper periodontal tissue. n Rapid destruction of attachment apparatus and deep osseous craters are formed in the interdental regions.
 Retrocuspid papilla
Retrocuspid papilla Gingival diseases
Gingival diseases Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism Early childhood and middle childhood
Early childhood and middle childhood Malek periodontics
Malek periodontics Site:slidetodoc.com
Site:slidetodoc.com Gingival index
Gingival index Suprabony vs infrabony pocket
Suprabony vs infrabony pocket Principles of scaling and root planing
Principles of scaling and root planing Gingival duvar
Gingival duvar Periodontal therapy in female patients
Periodontal therapy in female patients Plak boyayıcı ajanlar
Plak boyayıcı ajanlar Oxytalin
Oxytalin Gingival description
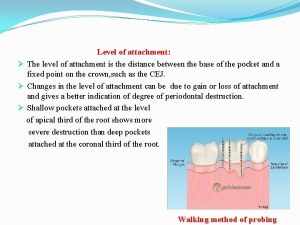
Gingival description Attachment level
Attachment level Bin angled chisel
Bin angled chisel Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Gingival anoxemia
Gingival anoxemia Russell periodontal index
Russell periodontal index Fases de la enfermedad periodontal
Fases de la enfermedad periodontal Twin flex clasp indication
Twin flex clasp indication Corrective phase
Corrective phase Enamel bevel for composite
Enamel bevel for composite Forward and backward caries
Forward and backward caries G j mount classification of caries
G j mount classification of caries Petele koplik
Petele koplik Indikasi gingivektomi
Indikasi gingivektomi Rationale of periodontal therapy
Rationale of periodontal therapy Osteocitos
Osteocitos Periodontal response to external forces
Periodontal response to external forces Non-infective
Non-infective Akut streptokokal gingivitis
Akut streptokokal gingivitis Tecnica step back modificada
Tecnica step back modificada Inlay definition dental
Inlay definition dental índice gingival de löe y silness
índice gingival de löe y silness Gingival index
Gingival index