G I T II Prof Mandira Sharma The















- Slides: 125
G I T - II Prof Mandira Sharma
The Stomach Gastritis and Ca stomach
STOMACH NORMAL STRUCTURE The stomach is ‘gland with cavity’, extending from its junction with lower end of the oesophagus (cardia) to its junction with the duodenum (pylorus). The lesser curvature is inner concavity on the right, while the greater curvature is the outer convexity on the left side of the stomach.
The stomach has 5 anatomical regions 1. Cardia is the oesophago gastric junction and lacks the sphincter. 2. Fundus is the portion above the horizontal line drawn across the esophagastric junction. 3. Body is the middle portion of the stomach between the fundus and the pyloric antrum. 4. Pyloric antrum is the distal third of the stomach. 5. Pylorus is the junction of distal end of the stomach with the duodenum. It has powerful sphincter muscle.

The mucosal folds in the region of the body and the fundus are loose (rugae), while the antral mucosa is somewhat flattened. Gastric canal is the relatively fixed portion of the pyloric antrum and the adjoining lesser curvature; it is the site for numerous pathological changes such as gastritis, peptic ulcer and gastric carcinoma.
The stomach receives its blood supply from the left gastric artery and the branches of the hepatic and splenic arteries Numerous gastric lymphatics which communicate freely with each other are also present. The innervations of the stomach is by the vagus and branches of the sympathetic nerve which are connected with ganglia in the muscular and submucous layers.
Histologically, the wall of the stomach consists of 4 layers— Serosa, muscularis, Submucosa and mucosa. 1. Serosa is derived from the peritoneum which is deficient in the region of lesser and greater curvatures. 2. Muscularis consists of 3 layers of smooth muscle fibres—the outer longitudinal, the middle circular and the inner oblique. Nerve plexuses and ganglion cells are present between the longitudinal and circular layers of muscle. The pyloric sphincter is the thickened circular muscle layer at the gastro-duodenal junction.
3. Submucosa is a layer of loose fibro connective tissue binding the mucosa to the muscularis loosely and contains branches of blood vessels, lymphatics and nerve plexuses and ganglion cells. 4. Mucosa consists of 2 layers—superficial and deep. Between the two layers is the lamina propria composed of network of fibro collagen with a few lymphocytes, plasma cells, macrophages and eosinophils. The mucosa is externally bounded by muscularis mucosae
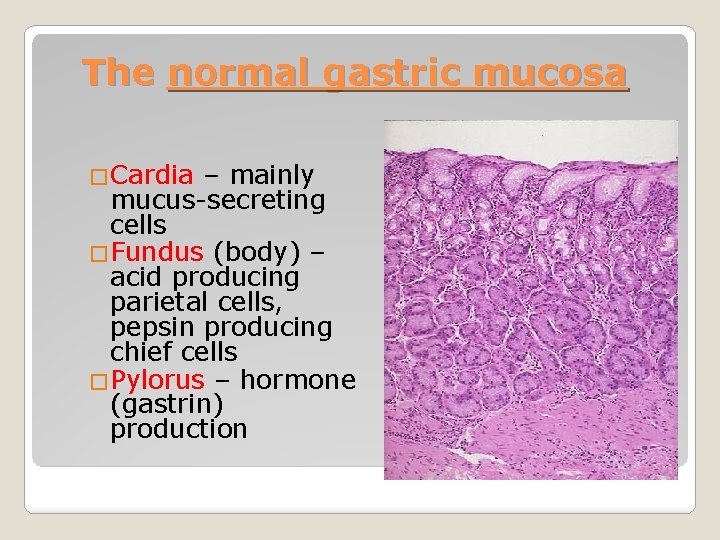
i) Superficial layer. It consists of a single layer of surface epithelium composed of regular, mucin-secreting, tall columnar cells with basal nuclei. There is a very rapid turnover of these cells. These dip down at places to form crypts (or pits or foveolae). Cardiac mucosa is the transition zone between the oesophageal squamous mucosa and the oxyntic mucosa of the fundus and body with which it gradually merges. Oxyntic mucosa lines both gastric fundus and body. Antral mucosa lines the pyloric antrum.
ii) Deep layer: It consists of glands that open into the bottom of the crypts. Depending upon the structure, these glands are of 3 types: a) Glands of the cardia are simple tubular or compound tubulo-racemose, lined by mucin secreting cells. A few endocrine cells and occasional parietal and chief cells are also present. • b) Glands of the body-fundus are long, tubular and tightly packed which may be coiled or dilated. c) Glands of the pylorus are much longer than the body-fundic glands. These are simple tubular glands which are often coiled

There are 4 types of cells present in the glands of bodyfundus mucosa: Parietal (Oxyntic) cells—are the most numerous and line the superficial (upper) part of the glands. Parietal cells are triangular in shape, have dark-staining nuclei and eosinophilic cytoplasm. These cells are responsible for production of hydrochloric acid of the gastric juice and the blood group substances. Endocrine (Kulchitsky or Enterochromaffin) cells—are widely distributed in the mucosa of all parts of the alimentary tract.
Chief (Peptic) cells—are the dominant cells in the deeper (lower) parts of the glands. Their basal nuclei are large with prominent nucleoli and the cytoplasm is coarsely granular and basophilic. These cells secrete pepsin of the gastric juice. Mucin-secreting neck cells—are small and fewer. These cells are present in the region of the narrow neck of the gastric glands i. e. at the junction of the glands with the pits.
Glands of the pylorus are much longer than the bodyfundic glands. These are simple tubular glands which are often coiled. They are lined mainly by small, granular, mucin secreting cells resembling neck cells and occasional parietal cells but no chief cells. Gastrin-producing G-cells are present predominantly in the region of antropyloric mucosa, The secretory products of the gastric mucosa are the gastric juice and the intrinsic factor, required for absorption of vitamin B 12
The control of gastric secretions chiefly occurs in one of the following 3 ways: 1. Cephalic phase—is stimulated by the sight, smell, taste or even thought of food. A neural reflex is initiated via branches of the vagus nerve that promotes the release of hydrochloric acid, pepsinogen and mucus.
2. Gastric phase—is triggered by the mechanical and chemical stimuli. i) Mechanical stimulation comes from stretching of the wall of the stomach and conveying neural messages to the medulla for gastric secretion. ii) Chemical stimulation is by digested proteins, amino acids, bile salts and alcohol which act on gastrin-producing G cells. Gastrin then passes into the blood stream and on return to the stomach promotes the release of gastric juice. 3. Intestinal phase—is triggered by the entry of protein rich food in the small intestine. An intestinal hormone capable of stimulating gastric secretion is probably released into blood stream
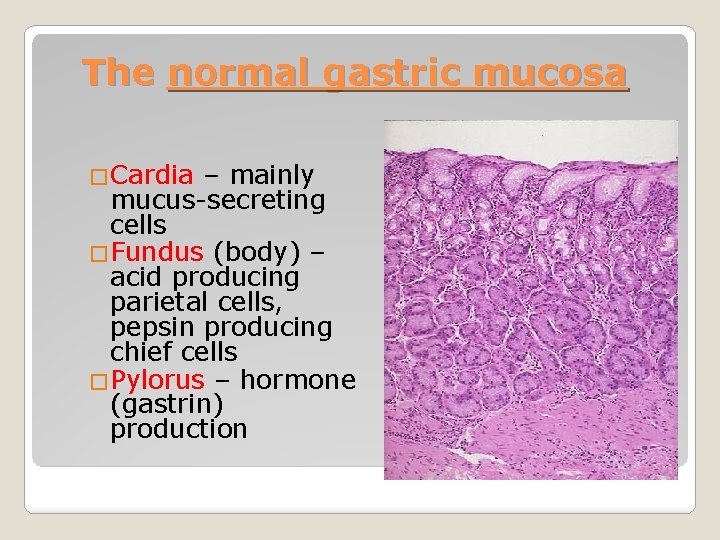
The normal gastric mucosa �Cardia – mainly mucus-secreting cells �Fundus (body) – acid producing parietal cells, pepsin producing chief cells �Pylorus – hormone (gastrin) production
Functions: 1. Digestion of food, reduce the size of food 2. Acts as reservoir 3. Absorption of Vit. 12, iron and calcium Stimulant of Gastric secretion: 1. Gastrin -----> (+) parietal cell 2. Acetylcholine (vagus) ---> (+) gastric cells 3. Histamine (mast cells) ---> parietal & chief cells PHYSIOLOGY
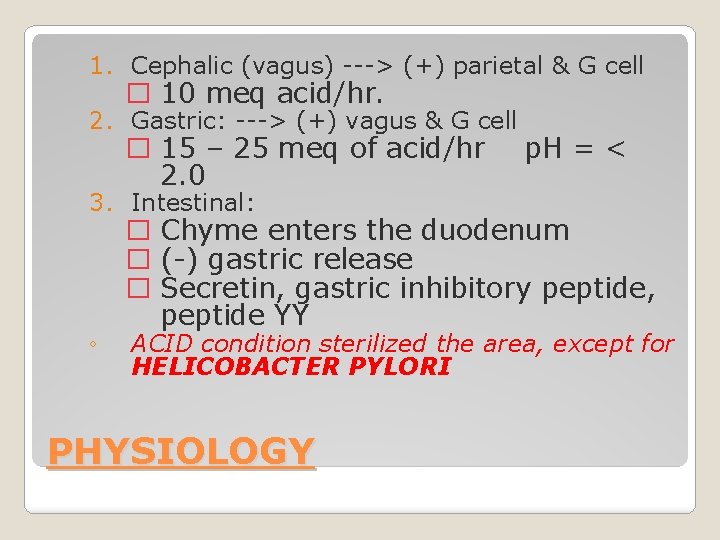
1. Cephalic (vagus) ---> (+) parietal & G cell � 10 meq acid/hr. 2. Gastric: ---> (+) vagus & G cell � 15 – 25 meq of acid/hr 2. 0 p. H = < 3. Intestinal: ◦ � Chyme enters the duodenum � (-) gastric release � Secretin, gastric inhibitory peptide, peptide YY ACID condition sterilized the area, except for HELICOBACTER PYLORI PHYSIOLOGY
�Hiatus hernia �Diaphragmatic hernia (through a nonphysiological defect) �Congenital pyloric stenosis- Male infants with hypertrophy of pyloric smooth muscle leading to projectile vomiting Congenital disorders
�Acid peptic Disease �Neoplasm GASTRIC DISEASES:
�Acute gastritis often due to chemical injury (alcohol, drugs) �Chronic gastritis: ◦ Helicobacter pylori infection ◦ Chemical damage (bile reflux, drugs) ◦ Autoimmune (associated with vitamin B 12 malabsorption (pernicious anaemia) Gastritis

Acute Gastritis Acute gastritis is a transient acute inflammatory involvement of the stomach, mainly mucosa. ETIOPATHOGENESIS. A variety of etiologic agents have been implicated in the causation of acute gastritis. These are as follows: 1. Diet and personal habits: 2. Infections: Bacterial infections e. g. Helicobacter pylori, diphtheria, salmonellosis, pneumonia, staphylococcal food poisoning. Viral infections e. g. viral hepatitis, influenza, infectious mononucleosis.
ETIOPATHOGENESIS. 3. Drugs: Intake of drugs like non-steroidal anti-inflammatory, drugs (NSAIDs), aspirin, cortisone, 4. Chemical and physical agents: Intake of corrosive chemicals such as caustic soda, phenol, lysol , Gastric irradiation 5. Severe stress: Emotional factors like shock, anger, resentment etc. Extensive burns , Trauma , Surgery.
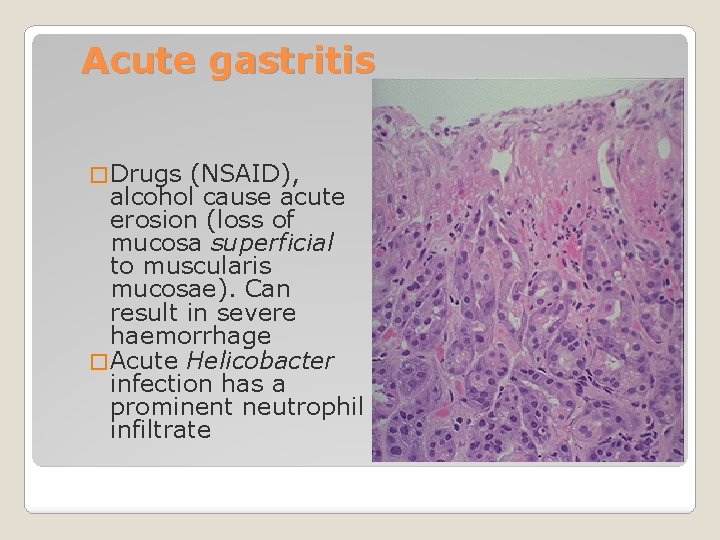
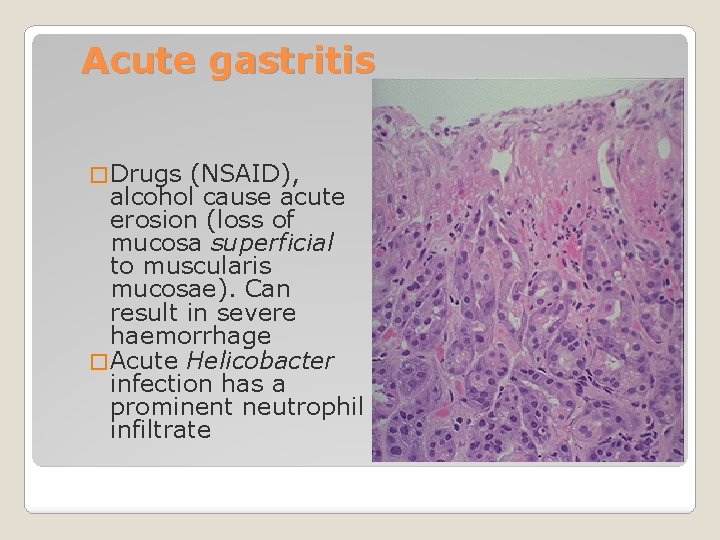
Acute gastritis � Drugs (NSAID), alcohol cause acute erosion (loss of mucosa superficial to muscularis mucosae). Can result in severe haemorrhage � Acute Helicobacter infection has a prominent neutrophil infiltrate
-Severe illness, trauma, burns (Cushing ulcer) or sepsis -CNS trauma: ◦ Increase gastrin ---> elevated acid secretion ◦ Curling ulcer Acute gastritis
The mucosal injury and subsequent acute inflammation in acute gastritis occurs by one of the following mechanisms: 1. Reduced blood flow, resulting in mucosal hypoperfusion due to ischaemia. 2. Increased acid secretion and its accumulation due to H. pylori infection resulting in damage to epithelial barrier. 3. Decreased production of bicarbonate buffer.
MORPHOLOGIC FEATURES. Grossly, the gastric mucosa is oedematous with abundant mucus and haemorrhagic spots. Microscopically, depending upon the stage, there is variable amount of oedema and infiltration by neutrophils in the lamina propria. In acute haemorrhagic and erosive gastritis, the mucosa is sloughed off and there are haemorrhages on the surface. MORPHOLOGIC FEATURES
Chronic Gastritis Chronic gastritis is the commonest histological change observed in biopsies from the stomach. The microscopic change is usually poorly correlated to the symptomatology, as the change is observed in about 35% of endoscopically normal mucosal biopsies. The condition occurs more frequently with advancing age; average for symptomatic chronic gastritis being 45 years which corresponds well with the age incidence of gastric ulcer.
ETIOPATHOGENESIS. In the absence of clear etiology of chronic gastritis, a number of etiologic factors have been implicated. Recurrent attacks of acute gastritis may result in chronic gastritis. 1. Reflux of duodenal contents into the stomach, especially in cases which have undergone surgical intervention in the region of pylorus. 2. Infection with H. pylori is strongly implicated 3. Associated disease of the stomach and duodenum, such as gastric or duodenal ulcer, gastric carcinoma. 4. Chronic hypochromic anaemia, especially associated with atrophic gastritis. 5. Immunological factors such as autoantibodies to gastric parietal cells in atrophic gastritis and autoantibodies against intrinsic factor.
The mechanism of chronic gastric injury by any of the etiologic agents is by - Cytotoxic effect of the injurious agent on the gastric mucosal epithelium, thus breaking the barrier and then inciting the inflammatory response. Etiology of chronic gastritis and is more common
CLASSIFICATION. Based on the type of mucosa affected 1. Type A gastritis (Autoimmune gastritis). Type A gastritis involves mainly the body-fundic mucosa. 2. Type B gastritis (H. pylori-related). Type B gastritis mainly involves the region of antral mucosa and is more common, commonly due to infection with H. Pylori. 3. Type AB gastritis affects the mucosal region of A as well as B types (body-fundic and antral mucosa). This is the most common type of gastritis in all age groups. pseudopyloric type.
�A – autoimmune �B – bacterial (helicobacter) �C - chemical Chronic gastritis ABC
�Autoantibodies to gastric parietal cells �Hypochlorhydria/achlorhydria �Loss of gastric intrinsic factor leads to malabsorption of vitamin B 12 with macrocytic, megaloblastic anaemia Autoimmune chronic gastritis
B – bacterial (helicobacter) Helicobacter pylori gastritis is usually a chronic inflammatory disease of the antrum and body of the stomach. Incidence – H. Pylori has been found in over 90% of the biopsies showing chronic. Recurrent attacks of acute gastritis may result in chronic gastritis. Some additional causes are as under: Sites of H. Pylori – Between the apical surface epithelium and the covering mucous gel. In the region of the tight junctions between adjacent mucosal epithelial cells. H. Pylori do not invade the gastric mucosa
Characteristics of H. Pylori – -these are spiral shaped gram negative bacilli. - It has urea splitting property and produces ammonia from urea , thus neutralizing the gastric acid to survive. - It has cytotoxin – associated gene A which is associated with duodenal ulcer and gastric cancer. -It also has a Vac A gene, which also causes duodenal ulcer.
Pathogenesis – The virulence factors cag A and Vac A protein along with the bacterial toxins liberated by H. Pylori cause mucosal damage and inflammation. Epithelial damage is also produce by ammonia released during splitting of urea by the bacteria. The inflammation persists causing chronic mucosal injury.
Morphology– • Lamina propria is infiltrated with neutrophils mixed plasma cells and lymphocytes. • lymphoid hyperplasia with germinal centre formation may be seen. • Frequently causes gastric atrophy • Intestinal metaplasia is quite frequent. • In long standing gastritis the epithelium may show dysplastic change leading to gastric carcinoma.
Complications – -Adenocarcinoma - Lymphoma Clinical Picture – H. Pylori causes ill- defined symptoms of : Abdominal discomfort Nausea Vomiting Staining : H. pylori can be stained - silver stain - Giemsa stain on the biopsy :
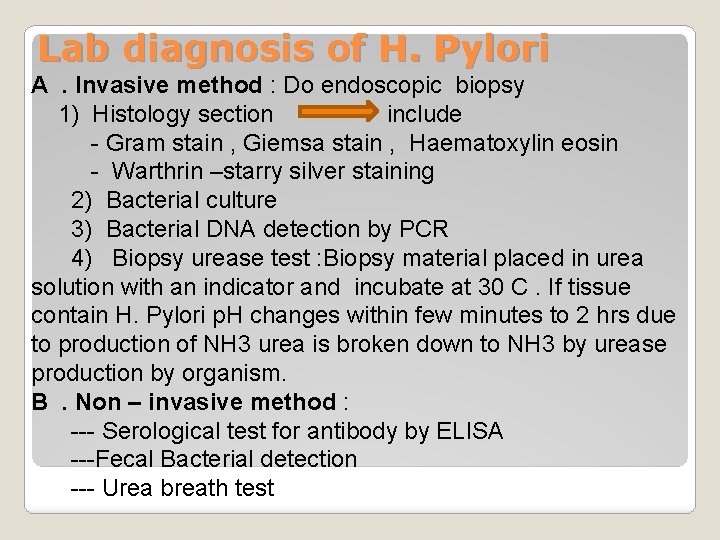
Lab diagnosis of H. Pylori A. Invasive method : Do endoscopic biopsy 1) Histology section include - Gram stain , Giemsa stain , Haematoxylin eosin - Warthrin –starry silver staining 2) Bacterial culture 3) Bacterial DNA detection by PCR 4) Biopsy urease test : Biopsy material placed in urea solution with an indicator and incubate at 30 C. If tissue contain H. Pylori p. H changes within few minutes to 2 hrs due to production of NH 3 urea is broken down to NH 3 by urease production by organism. B. Non – invasive method : --- Serological test for antibody by ELISA ---Fecal Bacterial detection --- Urea breath test
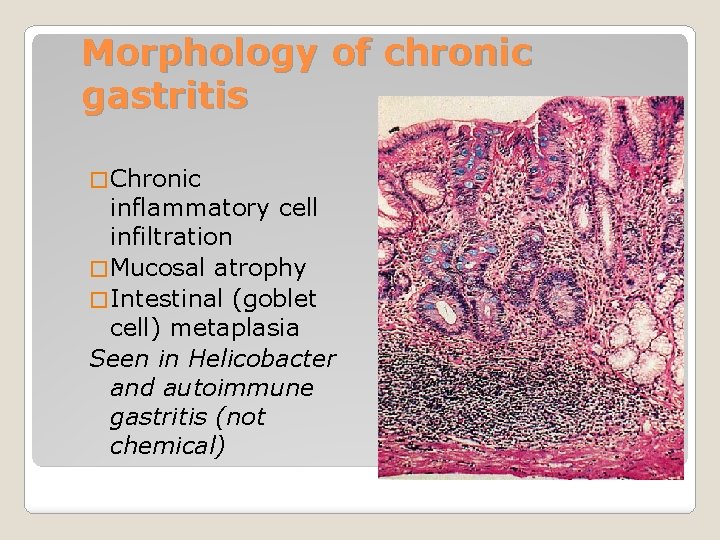
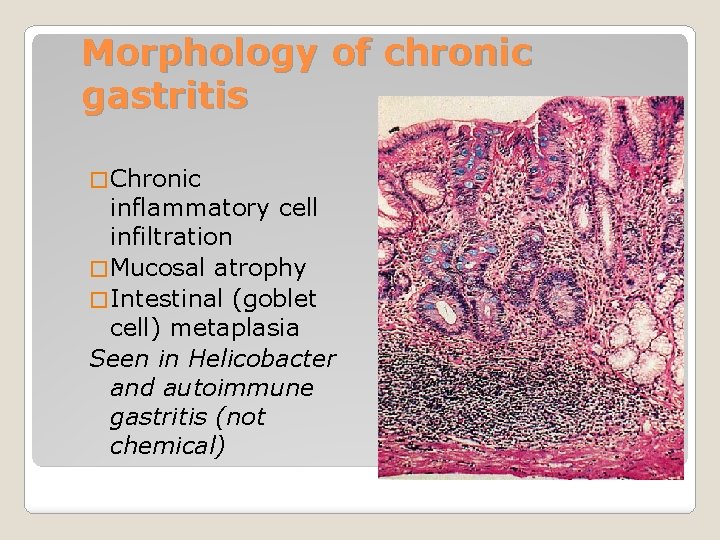
Morphology of chronic gastritis � Chronic inflammatory cell infiltration � Mucosal atrophy � Intestinal (goblet cell) metaplasia Seen in Helicobacter and autoimmune gastritis (not chemical)
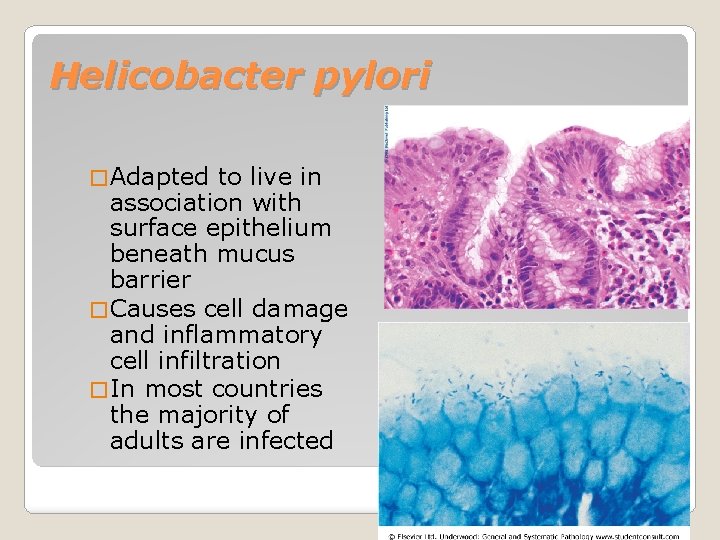
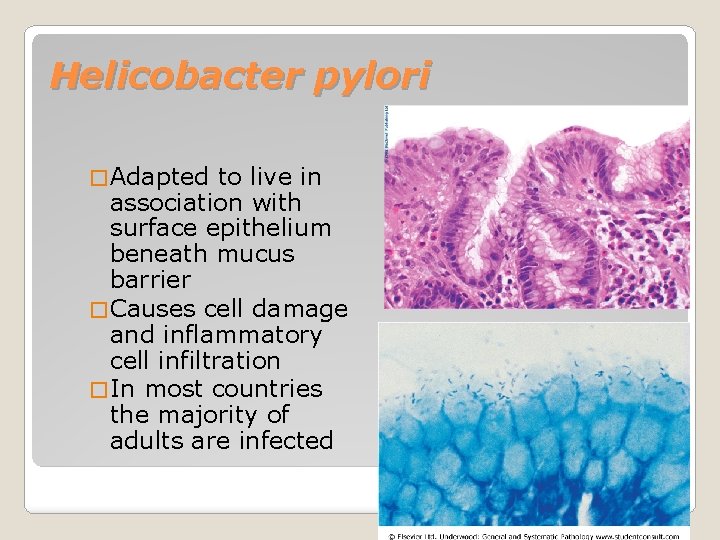
Helicobacter pylori � Adapted to live in association with surface epithelium beneath mucus barrier � Causes cell damage and inflammatory cell infiltration � In most countries the majority of adults are infected
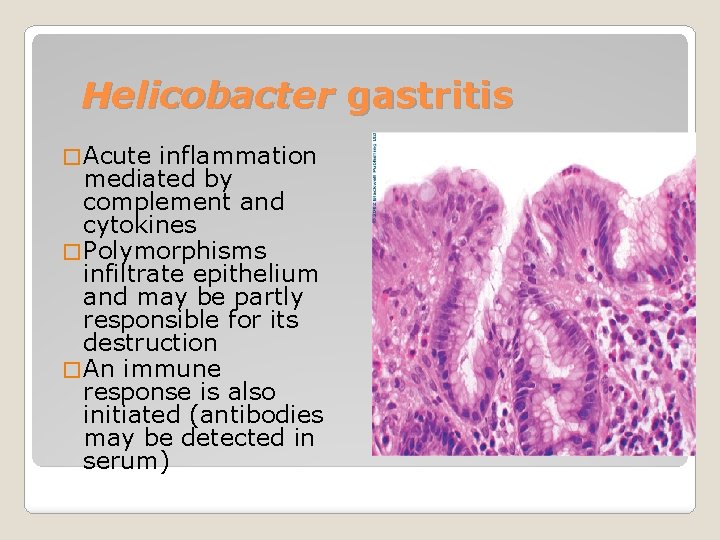
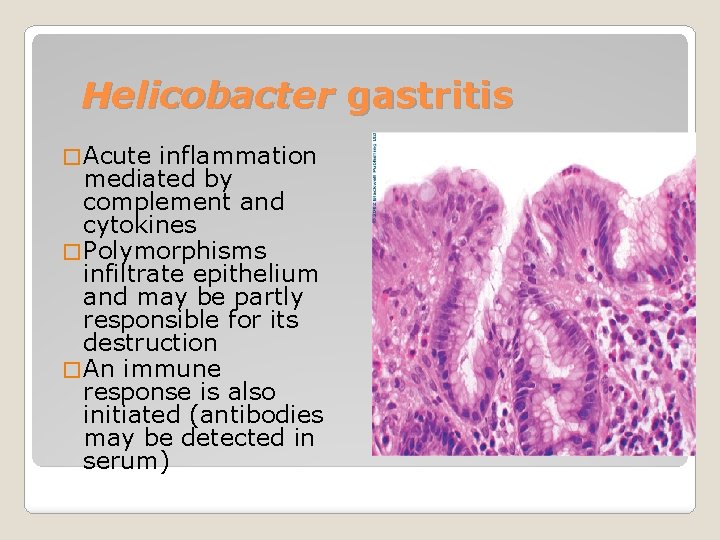
Helicobacter gastritis � Acute inflammation mediated by complement and cytokines � Polymorphisms infiltrate epithelium and may be partly responsible for its destruction � An immune response is also initiated (antibodies may be detected in serum)
� 2 patterns of infection ◦ Diffuse involvement of body and antrum (“pan gastritis” associated with diminishing acid output) ◦ Infection confined to antrum (antral gastritis, associate with increased acid output) Helicobacter gastritis

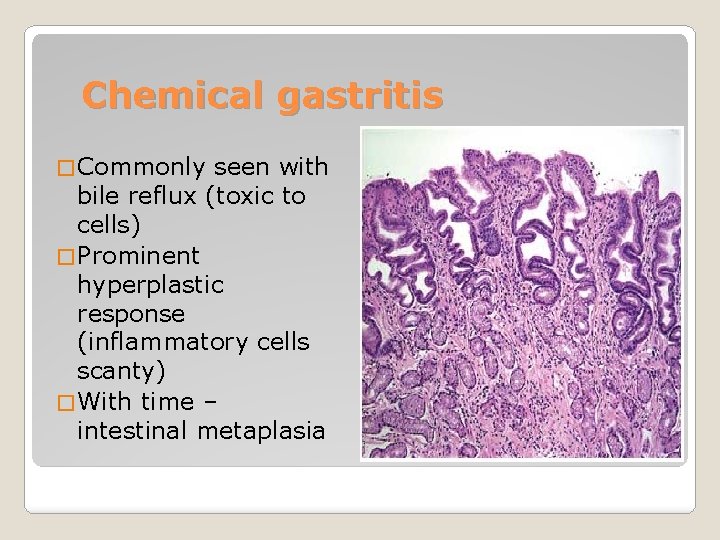
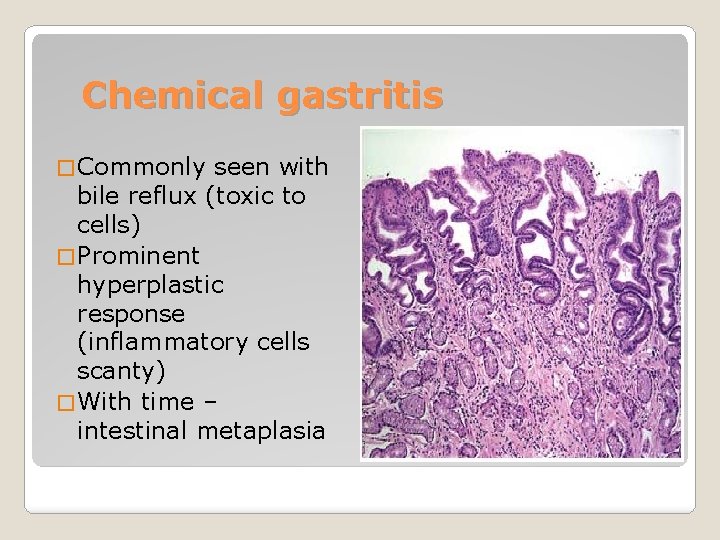
Chemical gastritis � Commonly seen with bile reflux (toxic to cells) � Prominent hyperplastic response (inflammatory cells scanty) � With time – intestinal metaplasia
�Peptic ulcer disease (Helicobacter) �Adenocarcinoma (all types) The “African enigma” – are complications of H. pylori infection less frequent in Africans? �Case not yet resolved Consequences of gastritis
Clinical manifestations: § Gastrointestinal bleeding § Abdominal pain Diagnosis: Endoscopy / radionuclide scanning / visceral angiography
Peptic ulcer disease
Peptic ulcer disease �Peptic ulcer disease is defined as ulceration of stomach , duodenum or small intestine associated with symptoms complex of burning epigastric pain increased by fasting and improved with food. �A surface breach of mucosal lining of GI tract occurring as a result of acid and pepsin attack �Sites: ◦ Duodenum (DU) ◦ Stomach (GU) ◦ Oesophagus ◦ Related to ectopic gastric mucosa (e. g. in Meckel’s diverticulum)
�Like acute erosion but breaching muscularis mucosae �Specific examples ◦ Curling’s ulcer (following severe burns) ◦ Cushing’s ulcer (following head injury) Acute peptic ulcer
�Complex epidemiology ◦ DU most common in Europe, GU in Japan ◦ Incidence of DU declining, GU stable Chronic peptic ulcer
ETIOLOGY. These ulcers occur following severe stress. The causes are as follows: i) Psychological stress ii) Physiological stress as in the following: Shock Severe trauma Septicaemia Extensive burns (Curling’s ulcers in the posterior aspect of the first part of the duodenum). Intracranial lesions (Cushing’s ulcers developing from hyperacidity following excessive vagus nerve stimulation). Drug intake (e. g. aspirin, steroids, butazolidine, indomethacin). Local irritants (e. g. alcohol, smoking, coffee etc).

PATHOGENESIS It is not clear how the mucosal erosions occur in stress ulcers In all other etiologic factors 1. Ischaemic hypoxic injury to the mucosal cells. 2. Depletion of the gastric mucus ‘barrier’ causing the mucosa susceptible to attack by acid-peptic secretions
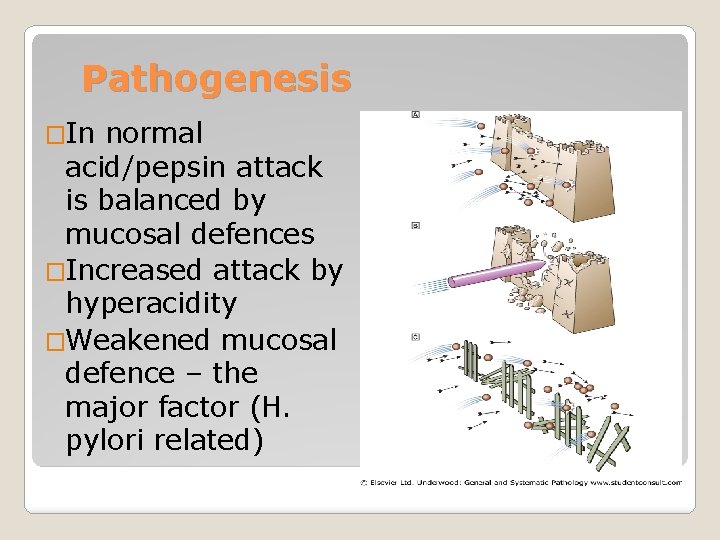
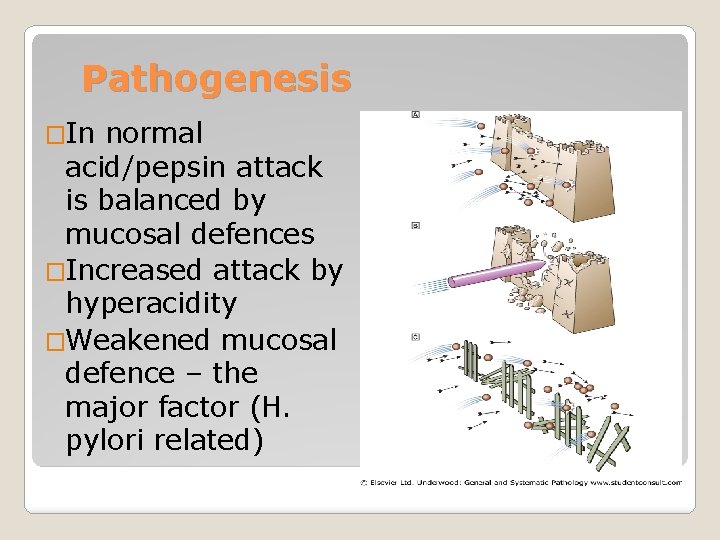
Pathogenesis �In normal acid/pepsin attack is balanced by mucosal defences �Increased attack by hyperacidity �Weakened mucosal defence – the major factor (H. pylori related)
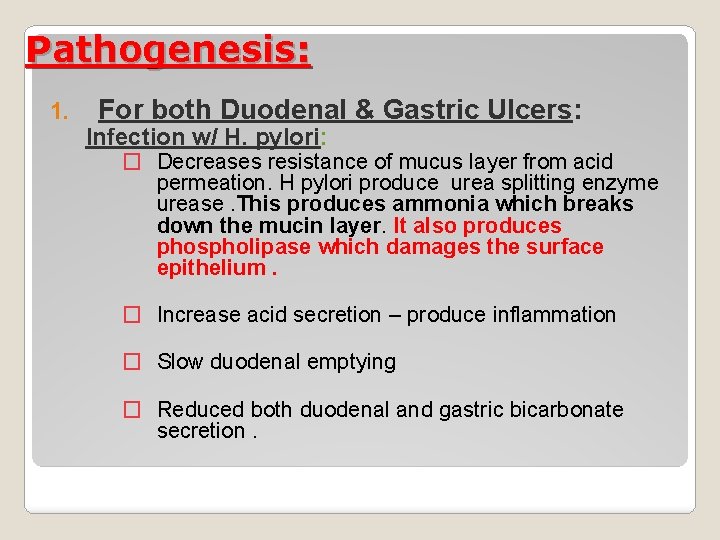
Pathogenesis: 1. For both Duodenal & Gastric Ulcers: Infection w/ H. pylori: � Decreases resistance of mucus layer from acid permeation. H pylori produce urea splitting enzyme urease. This produces ammonia which breaks down the mucin layer. It also produces phospholipase which damages the surface epithelium. � Increase acid secretion – produce inflammation � Slow duodenal emptying � Reduced both duodenal and gastric bicarbonate secretion.
Pathogenesis Effects of NSAIDs � Decreases Prostaglandin – increases acid secretion, decrease mucus and HCO 3 secretion and decrease epithelial cell proliferation. Thus depletion of prostaglandins causes impaired mucosal defence leading to ulceration
Zollinger-Ellison Syndrome (1%): � Massive secretion of HCL due to ectopic gastrin production from non-beta islet cell tumor (gastrinoma) � Associated w/ type I (MEN) PPP � 20% multiple, 2/3 malignant, w/ slow growing � Parietal cell mass is increased � > gastrin 3 -6 x the normal
3. Acid-pepsin secretions. There is conclusive evidence that some level of acid-pepsin secretion is essential for the development of duodenal as well as gastric ulcer. Peptic ulcers never occur in association with pernicious anaemia inwhich there are no acid and pepsin-secreting parietal and chief cells respectively. 4. Gastritis. Some degree of gastritis is always present in
5. Other local irritants. Pyloric antrum and lesser curvature of the stomach are the sites most exposed for longer periods to local irritants and thus are the common sites for occurrence of gastric ulcers. 6. Dietary factors. Nutritional deficiencies have beenregarded as etiologic factors in peptic ulcers e. g. gastric ulcer in poor socioeconomic strata,
7. Psychological factors. Psychological stress, anxiety, predispose to peptic ulcer disease. 8. Genetic factors. People with blood group O appear to be more prone to develop peptic ulcers than those with other blood groups. Genetic influences appear to have greater role in duodenal ulcers as evidenced by their occurrence in families, monozygotic twins and association with HLA -B 5 antigen.
9. Hormonal factors. Secretion of certain hormones by tumours is associated with peptic ulceration e. g. islet-cell tumour in Zollinger-Ellison syndrome, endocrine secretions in hyperplasia and adenomas ofparathyroid glands, adrenal cortex and anterior pituitary. 10. Miscellaneous. Duodenal ulcers have been observed to occur in association alcoholic cirrhosis, chronic renal failure, hyperparathyroidism, chronic obstructive pulmonary disease, and chronic pancreatitis.
Gastric ulcer The pathogenesis of gastric ulcer is mainly explained on the basis of impaired gastric mucosal defences against acid-pepsin secretions. 1. Hyperacidity may occur in gastric ulcer due to increased serum gastrin levels in response to ingested food in an atonic stomach. 2 However, many patients of gastric ulcer have low-to normal gastric acid levels. Ulcerogenesis in such patients is explained on the basis of damaging influence of other factors such as gastritis, bile reflux, cigarette smoke etc. 3. The normally protective gastric mucus ‘barrier’ against acid-pepsin is deranged in gastric ulcer.
Duodenal ulcer 1. There is generally hyper secretion of gastric acid into the fasting stomach at night which takes place under the influence of vagal stimulation. There is high basal as well as maximal acid output (BAO and MAO) in response to various stimuli. 2. Patients of duodenal ulcer have rapid emptying of the stomach so that the food which normally buffers and neutralises the gastric acid, passes down into the small intestine, leaving the duodenal mucosa exposed to the aggressive action of gastric acid. 3. Helicobacter gastritis caused by H. pylori is seen in 95100% cases of duodenal ulcers.
The underlying mechanisms of H pylori are as under: i) Gastric mucosal defence is broken by bacterial elaboration of urease, protease, catalase and phospholipase. ii) Host factors: H. pylori-infected mucosal epithelium releases pro inflammatory cytokines such as IL-1, IL-6, IL 8 and tumour necrosis factor-α, all of which cause intense inflammatory reaction. iii) Bacterial factors: Epithelial injury is also induced by cytotoxin-associated gene protein (Cag. A), while vacuolating cytotoxin (Vac. A) induces elaboration of cytokines.

MORPHOLOGIC FEATURES Gross and microscopic changes in gastric and duodenal ulcers are similar and quite characteristic. Gastric ulcers are found predominantly along the lesser curvature in the region of pyloric antrum, Most duodenal ulcers are found in the first part of the duodenum, usually immediate post-pyloric, more commonly on the anterior than the posterior wall. Uncommon locations include ulcer in the cardia, marginal ulcer and in the Meckel’s diverticulum.

Grossly, typical peptic ulcers are commonly solitary (80%), small (1 -2. 5 cm in diameter), round to oval and characteristically ‘punched out’. Benign ulcers usually have flat margins in level with the surrounding mucosa. The mucosal folds converge towards the ulcer. The ulcers may vary in depth from being superficial (confined to mucosa) to deep ulcers (penetrating into the muscular layer). In about 10 -20% of cases, gastric and duodenal ulcers are coexistent. Vast majority of the peptic ulcers are benign. Chronic duodenal ulcer never turns malignant, while chronic gastric ulcer may develop carcinoma in less than 1% of cases. Malignant gastric ulcers are larger, bowl-shaped with elevated and indurated mucosa at the margin.
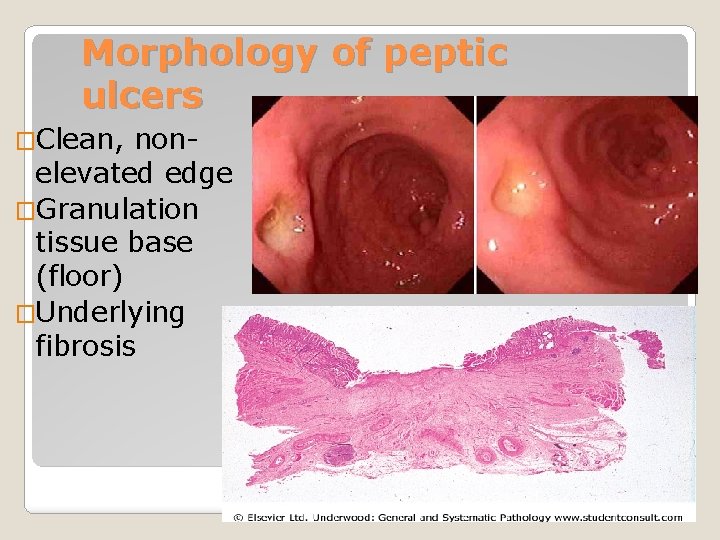
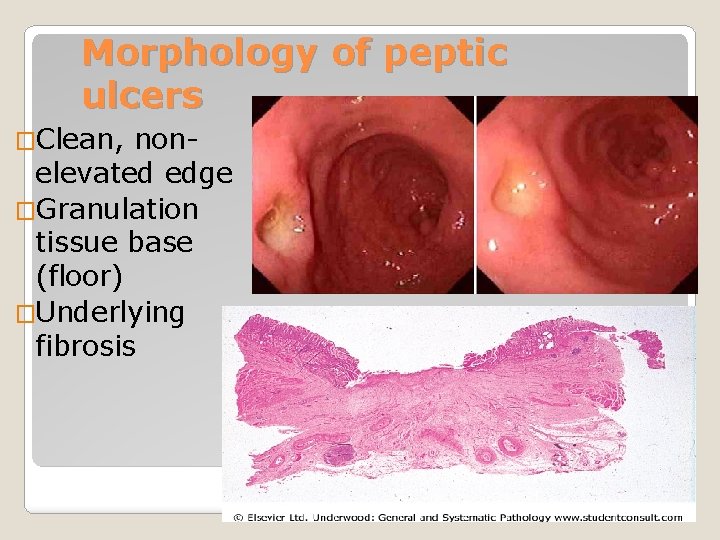
Morphology of peptic ulcers �Clean, nonelevated edge �Granulation tissue base (floor) �Underlying fibrosis
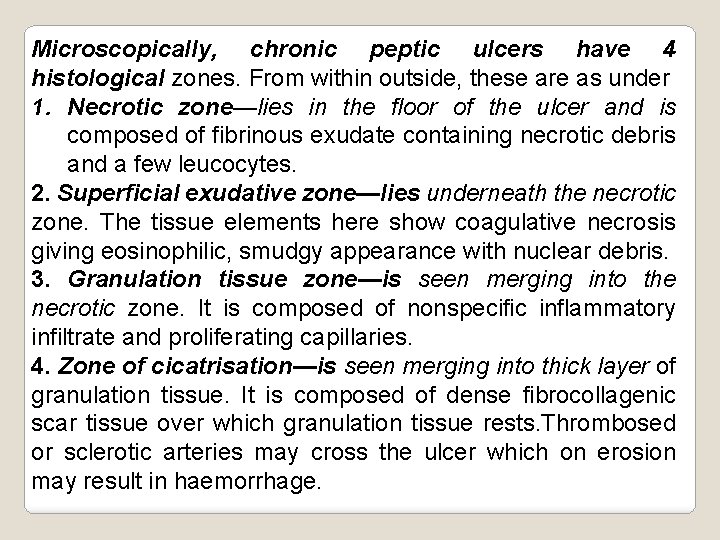
Microscopically, chronic peptic ulcers have 4 histological zones. From within outside, these are as under 1. Necrotic zone—lies in the floor of the ulcer and is composed of fibrinous exudate containing necrotic debris and a few leucocytes. 2. Superficial exudative zone—lies underneath the necrotic zone. The tissue elements here show coagulative necrosis giving eosinophilic, smudgy appearance with nuclear debris. 3. Granulation tissue zone—is seen merging into the necrotic zone. It is composed of nonspecific inflammatory infiltrate and proliferating capillaries. 4. Zone of cicatrisation—is seen merging into thick layer of granulation tissue. It is composed of dense fibrocollagenic scar tissue over which granulation tissue rests. Thrombosed or sclerotic arteries may cross the ulcer which on erosion may result in haemorrhage.



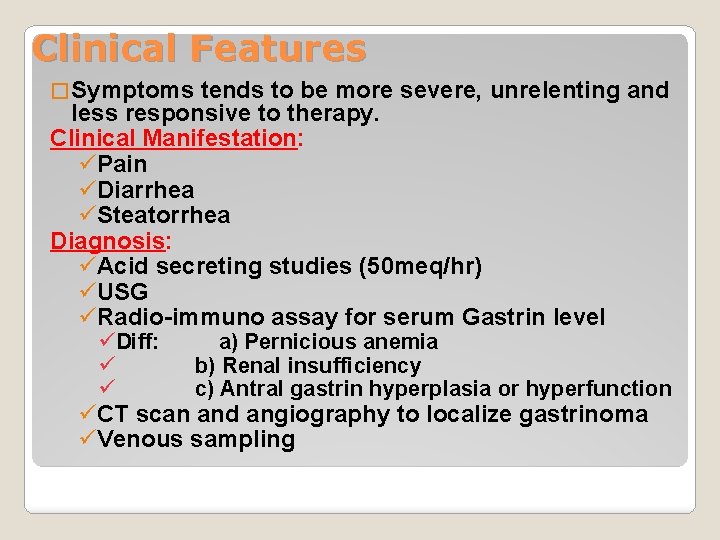
Clinical Features � Symptoms tends to be more severe, unrelenting and less responsive to therapy. Clinical Manifestation: üPain üDiarrhea üSteatorrhea Diagnosis: üAcid secreting studies (50 meq/hr) üUSG üRadio-immuno assay for serum Gastrin level üDiff: ü ü a) Pernicious anemia b) Renal insufficiency c) Antral gastrin hyperplasia or hyperfunction üCT scan and angiography to localize gastrinoma üVenous sampling
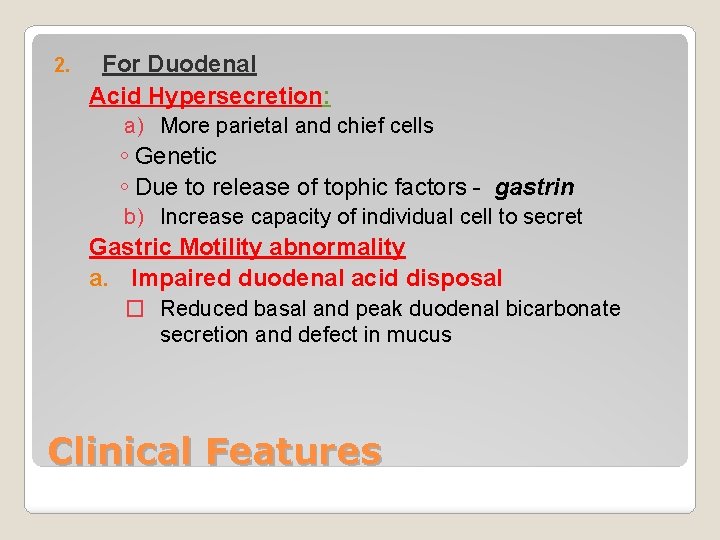
2. For Duodenal Acid Hypersecretion: a) More parietal and chief cells ◦ Genetic ◦ Due to release of tophic factors - gastrin b) Increase capacity of individual cell to secret Gastric Motility abnormality a. Impaired duodenal acid disposal � Reduced basal and peak duodenal bicarbonate secretion and defect in mucus Clinical Features
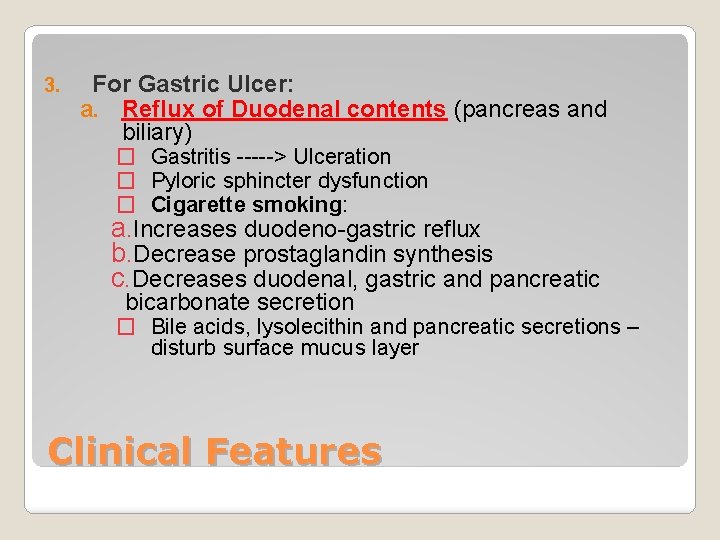
3. For Gastric Ulcer: a. Reflux of Duodenal contents (pancreas and biliary) � Gastritis -----> Ulceration � Pyloric sphincter dysfunction � Cigarette smoking: a. Increases duodeno-gastric reflux b. Decrease prostaglandin synthesis c. Decreases duodenal, gastric and pancreatic bicarbonate secretion � Bile acids, lysolecithin and pancreatic secretions – disturb surface mucus layer Clinical Features
�Tends to be high in DU patients. Antral gastritis causes increased gastrin production and acid secretion �Acid stimulates development of gastric metaplasia in the duodenum �Helicobacter organisms colonise the metaplastic epithelium and cause inflammatory damage leading to ulceration Acid production
�Pan gastritis diminishes acid secretion �Ongoing gastritis and epithelial damage is the main causal factor for ulceration Acid in GU
�Some strains are more pathogenic than others. The Cag A (cytotoxic) antigen is one important virulence factor �Human variability also plays a part (e. g. individuals who produce high levels of IL 1 b in inflammation get pan gastritis and GU, lower levels associated with antral gastritis and DU) Helicobacter factors in pathogenesis
A. B. Duodenal Ulcer Gastric Ulcer Duodenal ulcer > gastric ulcer Female > Male Duodenal ulcer is younger by 10 yrs Location: 1. Duodenal: ◦ duodenal bulb ◦ Hyper-secretion of acid Peptic ulcer
2. Gastric Type I - proximal antrum and body (disturbance in mucosal defense) Type II - arises secondary to duodenal ulcer w/ pyloric stenosis Type III - Pre pyloric and pyloric channel - (hyper-secretion of acid) Location:
1. ◦ Abdominal pain: Due to irritation of afferent nerves w/in the ulcer by the acid or due to peristaltic waves passing through the ulcer � Duodenal: colicky or burning pain relieved w/ food intake � Gastric: gnawing or burning usually during or after eating. 2. 3. 4. Anorexia Weight loss Epigastric tenderness Clinical Manifestation
�Perforation leading to peritonitis �Haemorrhage by erosion of vessel in base �Penetration of surrounding organ (liver/pancreas) �Obstruction (by scarring) – pyloric stenosis �(Cancer – rare event in true peptic ulcer) Complications of peptic ulcer
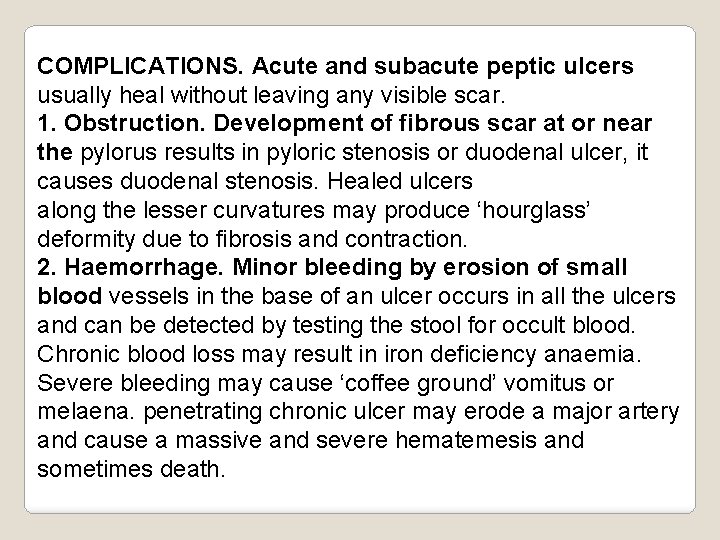
COMPLICATIONS. Acute and subacute peptic ulcers usually heal without leaving any visible scar. 1. Obstruction. Development of fibrous scar at or near the pylorus results in pyloric stenosis or duodenal ulcer, it causes duodenal stenosis. Healed ulcers along the lesser curvatures may produce ‘hourglass’ deformity due to fibrosis and contraction. 2. Haemorrhage. Minor bleeding by erosion of small blood vessels in the base of an ulcer occurs in all the ulcers and can be detected by testing the stool for occult blood. Chronic blood loss may result in iron deficiency anaemia. Severe bleeding may cause ‘coffee ground’ vomitus or melaena. penetrating chronic ulcer may erode a major artery and cause a massive and severe hematemesis and sometimes death.
3. Perforation. A perforated peptic ulcer is an acute abdominal emergency. Perforation occurs more commonly in chronic duodenal ulcers than chronic gastric ulcers. i) causing acute peritonitis. ii) Air escapes from the stomach and lies between the liver and the diaphragm giving the characteristic radiological appearance of air under the diaphragm. iii) Subphrenic abscess between the liver and the diaphragm may develop due to infection. iv) Perforation may extend to involve the adjacent organs e. g. the liver and pancreas. 4. Malignant transformation. but ulcers rarely cancerate’ holds true for most peptic ulcers. A chronic duodenal ulcer never turns malignant, while less than 1% of chronic gastric ulcers may transform into Ca
1. USG 2. Endoscopy Diagnosis:


Carcinoma of the stomach
�Polyps are common but usually not neoplastic (hyperplastic polyps. Hamartomas, ectopic pancreas) �Adenomas occur but are rare Gastric neoplasms
�The second most common fatal malignancy in the world �(after lung cancer) �Commonest in Far East (Japan) �Incidence declining �High mortality unless disease detected early Carcinoma of the stomach
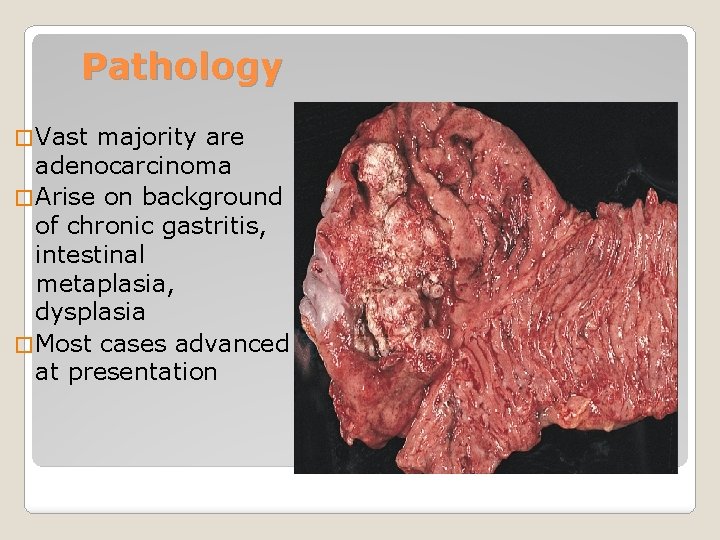
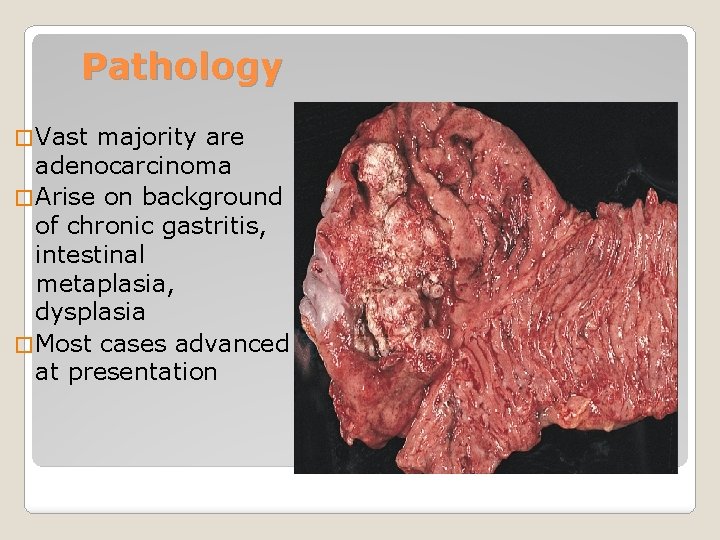
Pathology � Vast majority are adenocarcinoma � Arise on background of chronic gastritis, intestinal metaplasia, dysplasia � Most cases advanced at presentation
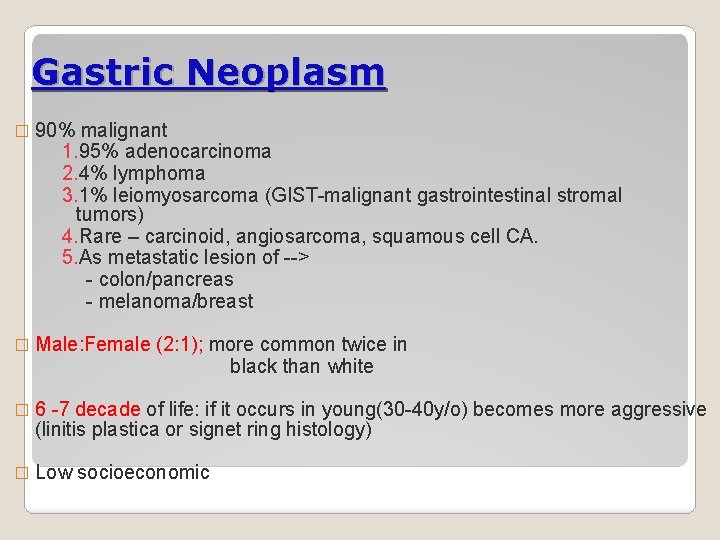
Gastric Neoplasm � 90% malignant 1. 95% adenocarcinoma 2. 4% lymphoma 3. 1% leiomyosarcoma (GIST-malignant gastrointestinal stromal tumors) 4. Rare – carcinoid, angiosarcoma, squamous cell CA. 5. As metastatic lesion of --> - colon/pancreas - melanoma/breast � Male: Female (2: 1); more common twice in black than white � 6 -7 decade of life: if it occurs in young(30 -40 y/o) becomes more aggressive (linitis plastica or signet ring histology) � Low socioeconomic

1. Diet - high in nitrates----->nitrites (bacteria & bile salts) - pickled, salted or smoked food - fresh fruit & vegetable and vit C & E ---> lowers 2. H. pylori infection � 3 fold increase risk 3. Ebstein Barr virus 4. Genetic factor: � Suppression of p 53 (tumor suppression gene); � over expression of COX-2 Etiology
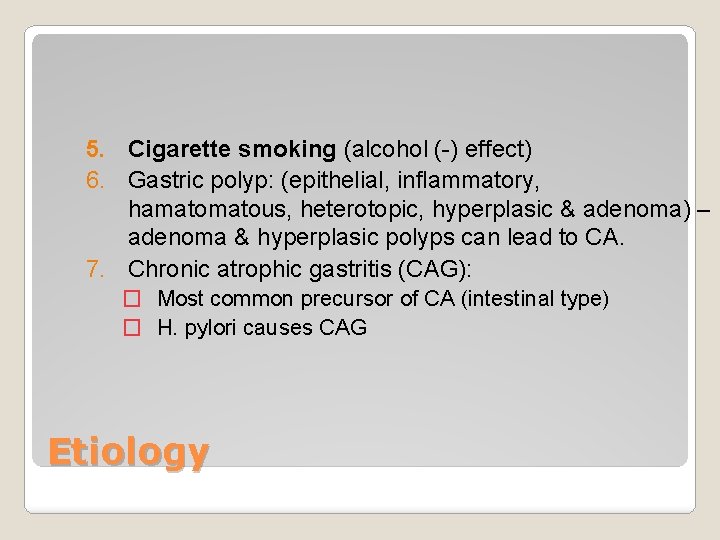
5. Cigarette smoking (alcohol (-) effect) 6. Gastric polyp: (epithelial, inflammatory, hamatous, heterotopic, hyperplasic & adenoma) – adenoma & hyperplasic polyps can lead to CA. 7. Chronic atrophic gastritis (CAG): � Most common precursor of CA (intestinal type) � H. pylori causes CAG Etiology
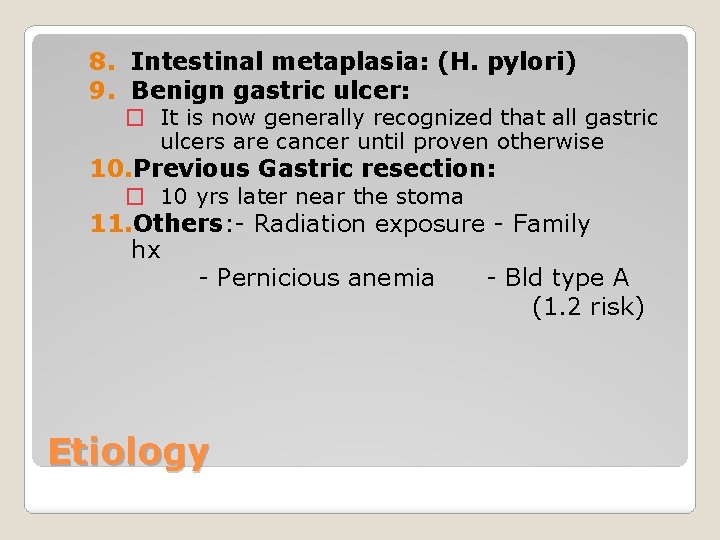
8. Intestinal metaplasia: (H. pylori) 9. Benign gastric ulcer: � It is now generally recognized that all gastric ulcers are cancer until proven otherwise 10. Previous Gastric resection: � 10 yrs later near the stoma 11. Others: - Radiation exposure - Family hx - Pernicious anemia - Bld type A (1. 2 risk) Etiology
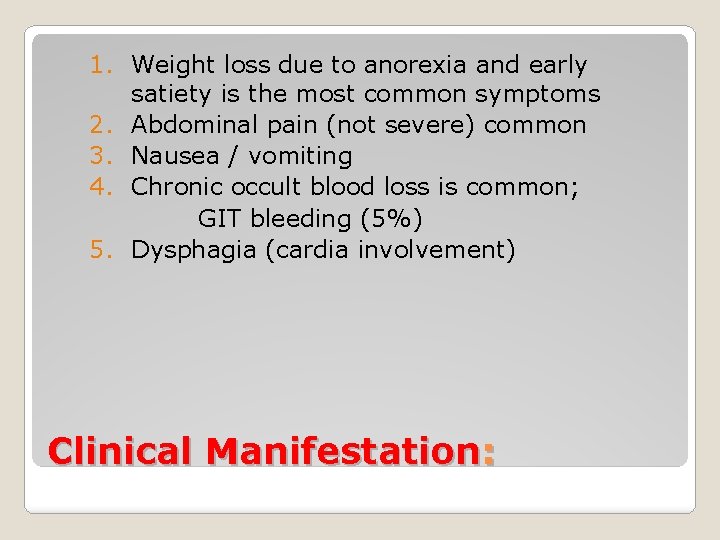
1. Weight loss due to anorexia and early satiety is the most common symptoms 2. Abdominal pain (not severe) common 3. Nausea / vomiting 4. Chronic occult blood loss is common; GIT bleeding (5%) 5. Dysphagia (cardia involvement) Clinical Manifestation:
6. Paraneoplastic syndromes ( Trousseau’s syndrome – thrombophlebitis; acanthosis nigricans – hyperpigmentation of axilla and groin; peripheral neuropathy) 7. Signs of distant metastasis: a. Hepatomegaly / ascites b. Krukenbergs tumor c. Blummers shelf (drop metastasis) d. Virchow’s node Clinical Manifestation
Gastric dysplasia ---> precursor of gastric CA Early gastric cancer: ◦ Limited to the mucosa and submucosa, regardless of LN status ◦ 70% are well differentiated ◦ Cure rate is 90% Pathology:

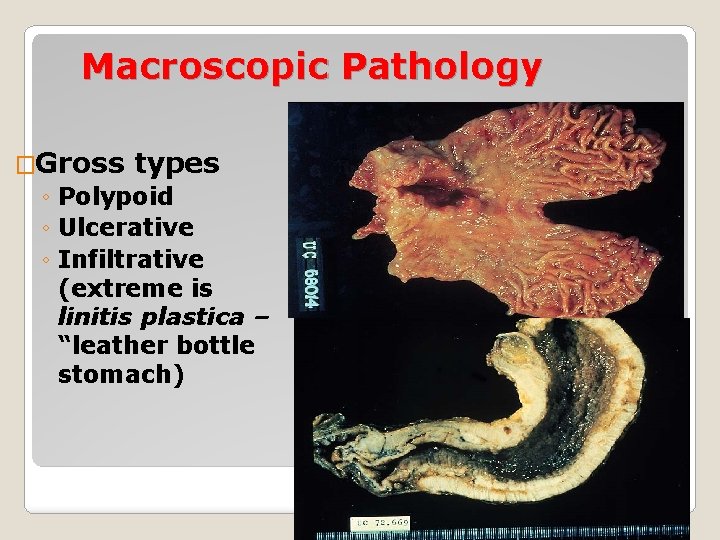
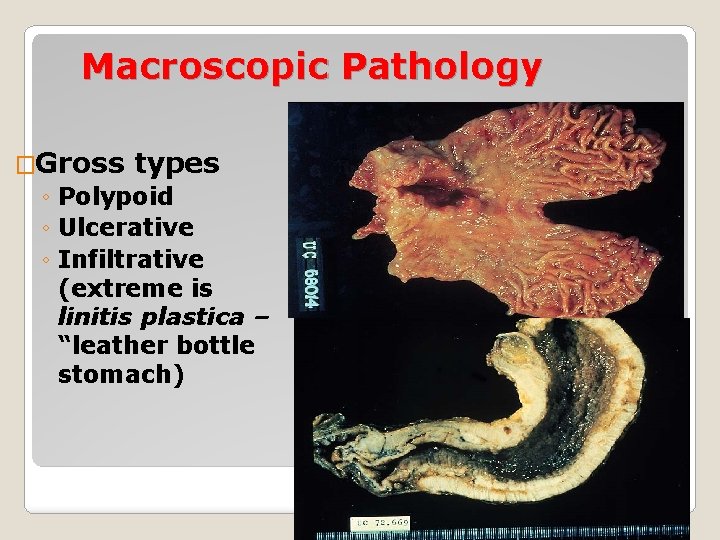
Macroscopic Pathology �Gross types ◦ Polypoid ◦ Ulcerative ◦ Infiltrative (extreme is linitis plastica – “leather bottle stomach)
Subtypes Macroscopic Subtypes: 1. 2. 3. 4. 5. Superficial spreading Polypoid (well differentiated) Fungating Ulceration Scirrhous (linitis plastica) : infiltrates the entire thickness of the wall � Leather bottle stomach � Poor prognosis � Usually undifferentiated Location of primary tumor: ◦ 40% distal / 30% middle / 30% distal
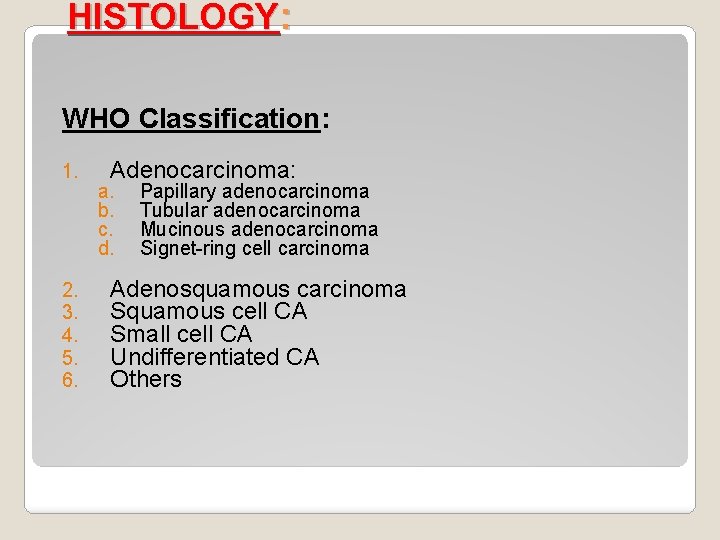
HISTOLOGY: WHO Classification: 1. 2. 3. 4. 5. 6. Adenocarcinoma: a. b. c. d. Papillary adenocarcinoma Tubular adenocarcinoma Mucinous adenocarcinoma Signet-ring cell carcinoma Adenosquamous carcinoma Squamous cell CA Small cell CA Undifferentiated CA Others
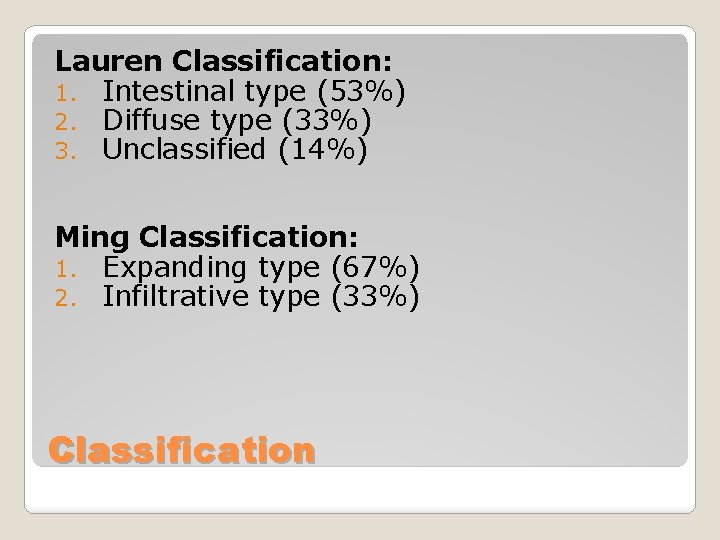
Lauren Classification: 1. Intestinal type (53%) 2. Diffuse type (33%) 3. Unclassified (14%) Ming Classification: 1. Expanding type (67%) 2. Infiltrative type (33%) Classification
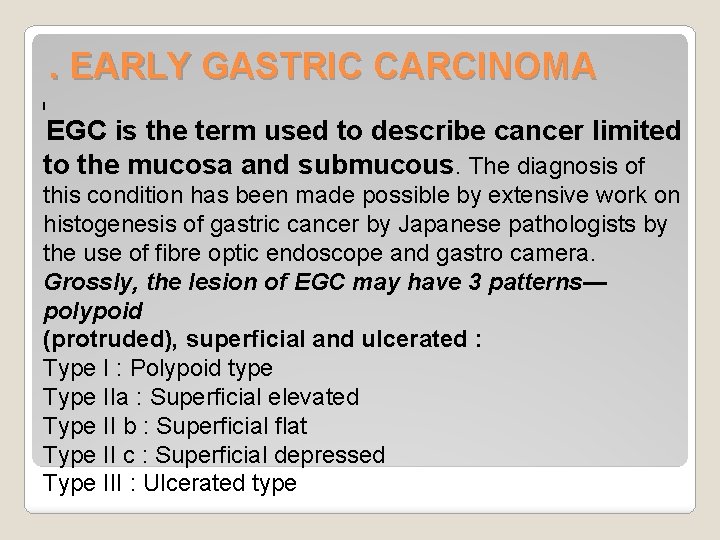
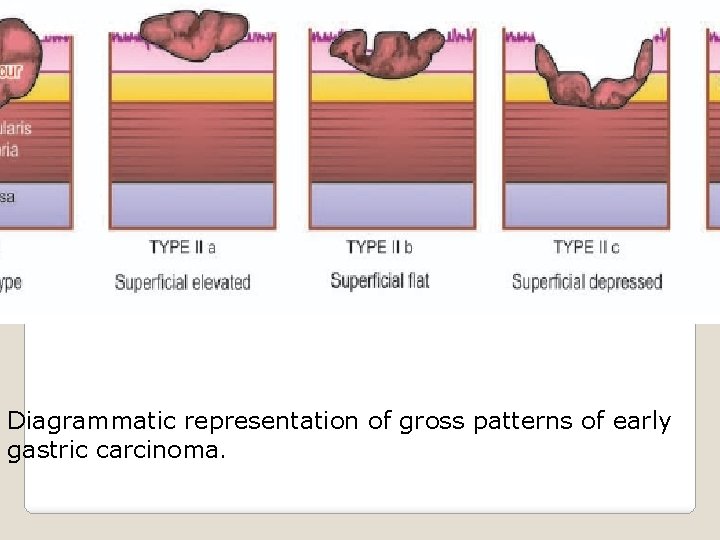
. EARLY GASTRIC CARCINOMA I EGC is the term used to describe cancer limited to the mucosa and submucous. The diagnosis of this condition has been made possible by extensive work on histogenesis of gastric cancer by Japanese pathologists by the use of fibre optic endoscope and gastro camera. Grossly, the lesion of EGC may have 3 patterns— polypoid (protruded), superficial and ulcerated : Type I : Polypoid type Type IIa : Superficial elevated Type II b : Superficial flat Type II c : Superficial depressed Type III : Ulcerated type
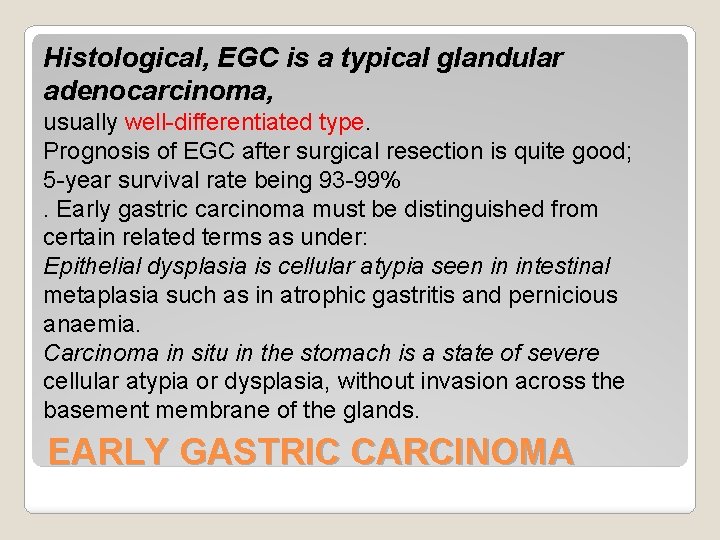
Histological, EGC is a typical glandular adenocarcinoma, usually well-differentiated type. Prognosis of EGC after surgical resection is quite good; 5 -year survival rate being 93 -99%. Early gastric carcinoma must be distinguished from certain related terms as under: Epithelial dysplasia is cellular atypia seen in intestinal metaplasia such as in atrophic gastritis and pernicious anaemia. Carcinoma in situ in the stomach is a state of severe cellular atypia or dysplasia, without invasion across the basement membrane of the glands. EARLY GASTRIC CARCINOMA
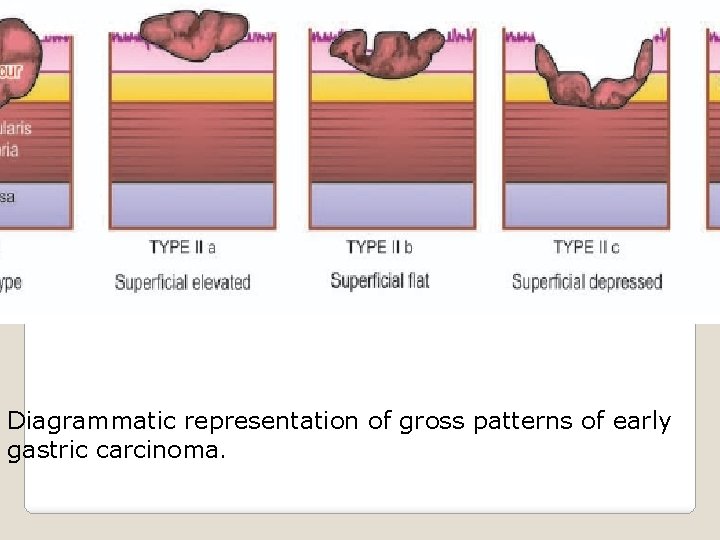
Diagrammatic representation of gross patterns of early gastric carcinoma.
ADVANCED GASTRIC CARCINOMA II. . When the carcinoma crosses the basement membrane into the muscularis propria or beyond, it is referred to as advanced gastric carcinoma. Advanced gastric carcinoma has following 5 patterns: i) Ulcerative carcinoma. This is the most common pattern. The tumour appears as a flat, infiltrating and ulcerative growth with irregular necrotic base and raised margin. Histologically, ulcerative carcinomas are poorly differentiated adenocarcinomas, which invade deeply into the stomach wall. Tubular and acinar patterns are seen more commonly seen. ADVANCED GASTRIC CARCINOMA
ii) Fungating (polypoid) carcinoma The second common pattern is a cauliflower growth projecting into the lumen, It is seen more often in the fundus. The tumour undergoes necrosis and infection commonly. Histological, fungating or polypoid carcinomas are well-differentiated adenocarcinoma, commonly papillary type. Fungating (polypoid) carcinoma
iii) Scirrhous carcinoma (Linitis plastica). stomach wall is thickened due to extensive desmoplasia giving the appearance as ‘leather bottle stomach’ or ‘linitis plastica’. The involvement may be localised to pyloric antrum, or diffuse affecting whole of the stomach from the cardia to pylorus. The lumen of the stomach is reduced. Histologically, it may be an adenocarcinoma or signet ring cell carcinoma, extensively infiltrating the stomach wall, but due to marked desmoplasia cancer cells may be difficult to find. Scirrhous carcinoma (Linitis plastica
Colloid (Mucoid) carcinoma iv) Colloid (Mucoid) carcinoma. This pattern is usually seen in the fundus. The tumour grows like masses having gelatinous appearance due to secretion of large quantities of mucus. Histologically, mucoid carcinoma contains abundant pools of mucin in which are seen a small number of tumour cells, sometimes having signet-ring appearance. v
) Ulcer-cancer. Development of cancer in chronic gastric ulcer is a rare occurrence. Majority of ulcer-cancers are malignant lesions from the beginning. For confirmation of cancer in a pre-existing gastric ulcer, the characteristic microscopic appearance of peptic ulcer should be demonstrable with one portion of the base or the margin of the ulcer showing carcinomatous changes. Histologically, ulcer-cancers are adenocarcinomas without any specific features.
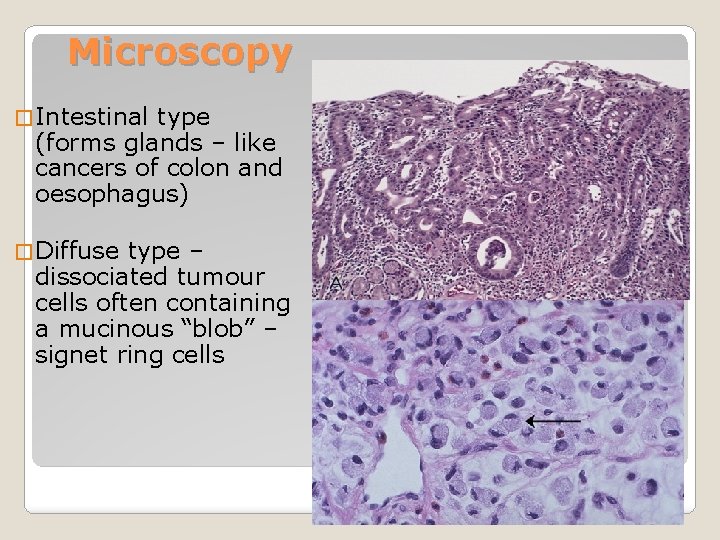
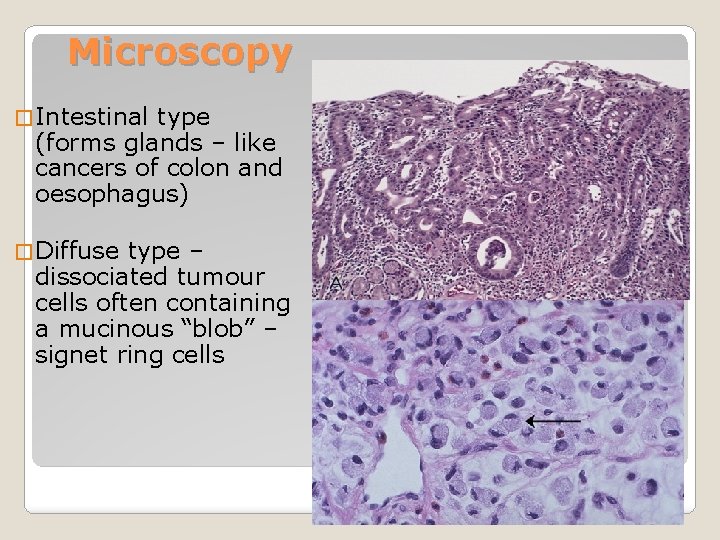
Microscopy � Intestinal type (forms glands – like cancers of colon and oesophagus) � Diffuse type – dissociated tumour cells often containing a mucinous “blob” – signet ring cells
�Local infiltration (through wall of stomach to peritoneum, pancreas etc) �Lymphatic – local and regional lymph nodes �Blood – liver, lungs �Trans coelomic (across peritoneal cavity). Often involves ovaries (esp. signet ring cancer) – Krukenberg tumour. Spread of gastric carcinoma
�Lymphoma �Gastrointestinal stromal tumour (GIST) �Neuroendocrine (carcinoid) tumours Less common gastric neoplasms
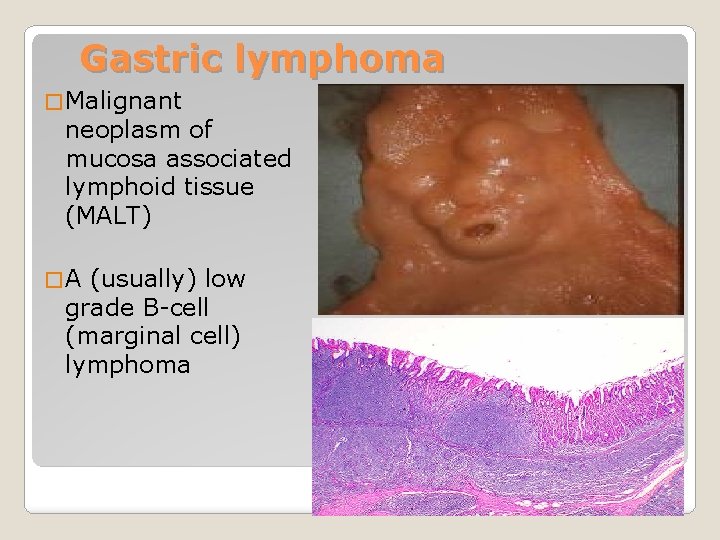
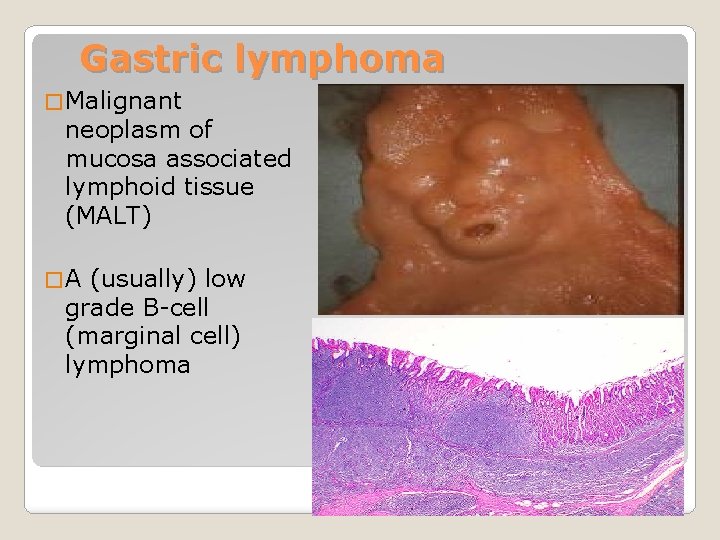
Gastric lymphoma � Malignant neoplasm of mucosa associated lymphoid tissue (MALT) �A (usually) low grade B-cell (marginal cell) lymphoma
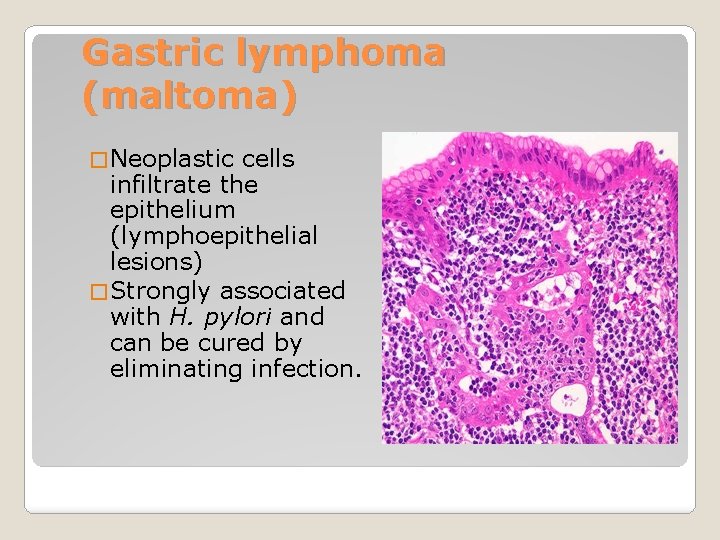
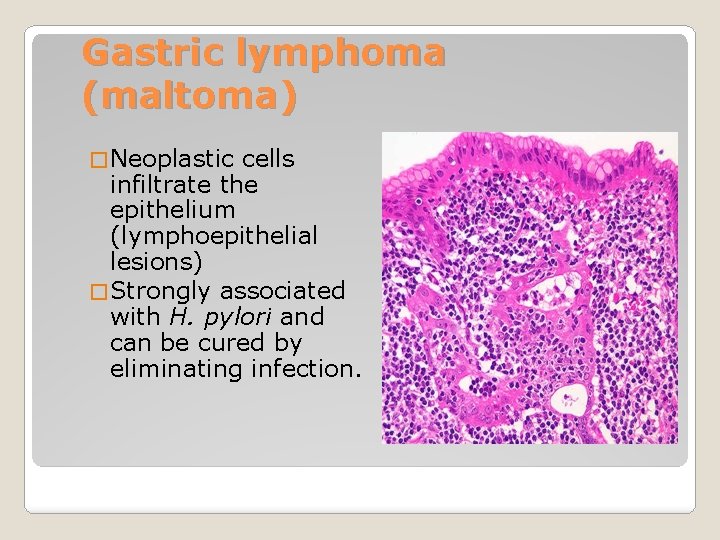
Gastric lymphoma (maltoma) � Neoplastic cells infiltrate the epithelium (lymphoepithelial lesions) � Strongly associated with H. pylori and can be cured by eliminating infection.
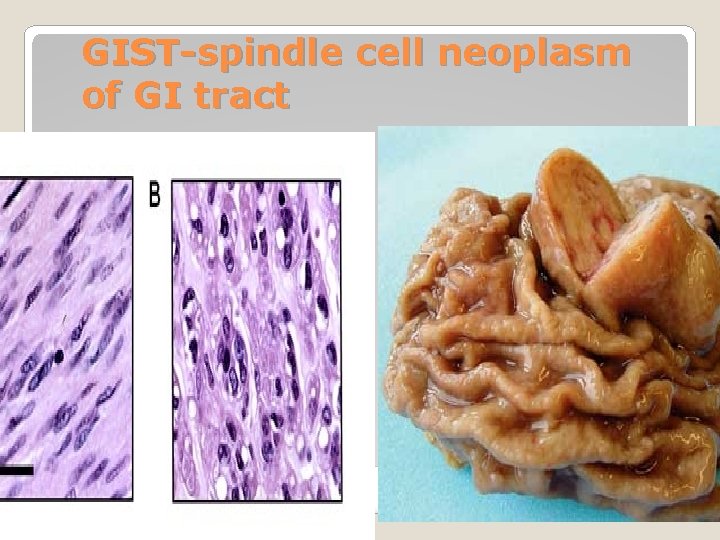
�Mesenchymal neoplasm's �Derived from interstitial cells of Cajal (pacemaker cells controlling peristalsis) �Overexpress c-kit oncogene ◦ Used as diagnostic aid on tissue ◦ A target for therapy with tyrosine kinase inhibitor imatinib (also used in CML) Gastrointestinal stromal tumours (GIST)
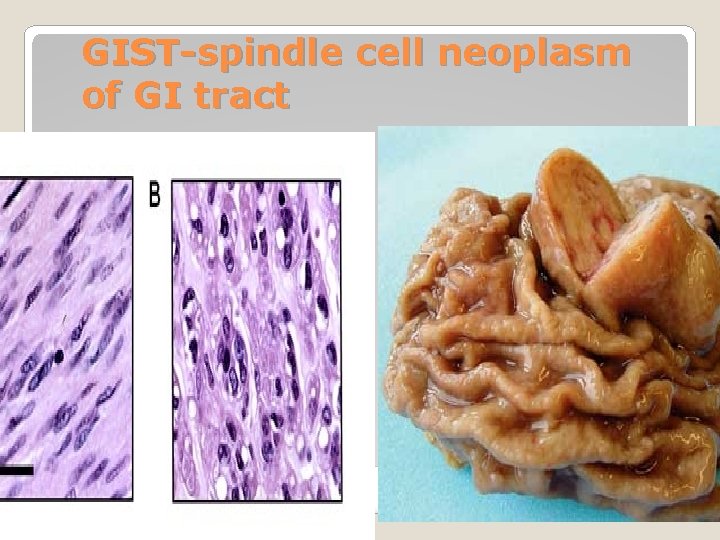
GIST-spindle cell neoplasm of GI tract
�Larger tumours with high mitotic rate tend to behave malignantly �Stomach is commonest site GIST
�Carcinoids are tumours of resident neuroendocrine cells in gastric glands �Usually seen in context of chronic atrophic gastritis (driven by gastrin) �Clinical behaviour variable Neuroendocrine tumours

THANKS… Thanks…
 Gaurav sharma cisco
Gaurav sharma cisco Ca umesh sharma
Ca umesh sharma Umesh sharma md
Umesh sharma md Pradeep sharma university of houston
Pradeep sharma university of houston First card repertory
First card repertory Keerti sharma md
Keerti sharma md Dr pushpa raj sharma
Dr pushpa raj sharma Sumit sharma teri
Sumit sharma teri Dr pushpa raj sharma contact number
Dr pushpa raj sharma contact number Pushpa raj sharma
Pushpa raj sharma Pushpa raj sharma
Pushpa raj sharma Hina sharma architect
Hina sharma architect Pawan sharma bits pilani
Pawan sharma bits pilani Gabriel sharma
Gabriel sharma Amrit sharma morgan stanley
Amrit sharma morgan stanley Dr pushpa raj sharma
Dr pushpa raj sharma Dr pushpa raj sharma contact number
Dr pushpa raj sharma contact number Rowena mittal
Rowena mittal Dr madhurima sharma
Dr madhurima sharma Dr rakesh sharma
Dr rakesh sharma Dr pushpa raj sharma
Dr pushpa raj sharma Define modern concept of child care
Define modern concept of child care Dr vivek sharma
Dr vivek sharma Ranipril
Ranipril Dr suman sharma
Dr suman sharma Articulato
Articulato Lasert tag
Lasert tag Dr pushpa raj sharma clinic
Dr pushpa raj sharma clinic Camcer
Camcer Dr pk sharma
Dr pk sharma Dr pushpa raj sharma pediatrician
Dr pushpa raj sharma pediatrician Cs deepak sharma
Cs deepak sharma Archana sharma psychologist
Archana sharma psychologist Gaurav sharma inside edge
Gaurav sharma inside edge Dr bikas sharma
Dr bikas sharma Jag sharma
Jag sharma Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết V cc cc
V cc cc Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Hát lên người ơi alleluia
Hát lên người ơi alleluia Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau 101012 bằng
101012 bằng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công của trọng lực
Công của trọng lực Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Phản ứng thế ankan
Phản ứng thế ankan Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Slidetodoc
Slidetodoc Thế nào là số nguyên tố
Thế nào là số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Tia chieu sa te
Tia chieu sa te Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Glasgow thang điểm
Glasgow thang điểm ưu thế lai là gì
ưu thế lai là gì Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết Chuvas convectivas
Chuvas convectivas Prof qomariyatus sholihah
Prof qomariyatus sholihah Yesari karter
Yesari karter Aya addema xxx
Aya addema xxx Sedat akdeniz
Sedat akdeniz Prof dr nafiye yılmaz
Prof dr nafiye yılmaz Prof.dr.murat akkaya
Prof.dr.murat akkaya Dr aris sudiyanto
Dr aris sudiyanto Prof jasper imungi
Prof jasper imungi Solubility examples
Solubility examples Prof paul browne
Prof paul browne Pressure prof
Pressure prof Edna st vincent millay sonnet 29
Edna st vincent millay sonnet 29 Prof soegeng soegijanto
Prof soegeng soegijanto Prof jamal wiwoho
Prof jamal wiwoho Prof. dr. kristan schneider
Prof. dr. kristan schneider Prof. onur mutlu
Prof. onur mutlu Murat vural itü
Murat vural itü Passenger transport safety
Passenger transport safety Prof anna piekarska
Prof anna piekarska Stephan anagnostaras
Stephan anagnostaras Posture assis
Posture assis Prof sandra lowe
Prof sandra lowe Xuhua xia
Xuhua xia Pletore yüz
Pletore yüz Prof ram meghe institute of technology and research
Prof ram meghe institute of technology and research Prof.sse
Prof.sse Rodzaj i gatunek syzyfowe prace
Rodzaj i gatunek syzyfowe prace Stammbaumanalyse und vererbungsmuster
Stammbaumanalyse und vererbungsmuster Fatih boyvat
Fatih boyvat Prof. norbert pohlmann
Prof. norbert pohlmann 740
740 Dr metin ingeç
Dr metin ingeç Dermatochalasis
Dermatochalasis Sbah definition
Sbah definition Agamenon roberto
Agamenon roberto Prof bart
Prof bart Prof dr svetlana stanisic
Prof dr svetlana stanisic Prof dr petek askar
Prof dr petek askar Prof dr esat arslan
Prof dr esat arslan Prof du jour questions
Prof du jour questions Tr prof software
Tr prof software Agamenon quimica
Agamenon quimica Prof. dr nenad glumbić
Prof. dr nenad glumbić Entrk
Entrk Prof dr solmaz akar
Prof dr solmaz akar Prof abdul bari azed
Prof abdul bari azed Prof samborski fibromialgia
Prof samborski fibromialgia