Sepsis Severe Sepsis and Septic Shock Anna Piekarska
![Special procedures Anticoagulants n a. PC (drotrecogin alfa [Xigris]) Indication: severe sepsis with DIC Special procedures Anticoagulants n a. PC (drotrecogin alfa [Xigris]) Indication: severe sepsis with DIC](https://slidetodoc.com/presentation_image/77e2e1a16a7fd2a66800cdc07b2b6ced/image-41.jpg)
- Slides: 43
Sepsis, Severe Sepsis, and Septic Shock Anna Piekarska MD, Ph. D
Epidemiology n severe sepsis, defined as documented infection and acute organ dysfunction, occurred in 300 cases per 100, 000 population n Incidence was higher in men than in women and in nonwhite persons than in white persons.
Epidemiology n median age for patients with a sepsisrelated hospital discharge diagnosis is approximately 60 years n low-birth-weight newborns - 500 cases/100, 000 population per year
Epidemiology n 80% of the cases of severe sepsis in adults occurred in individuals who were already hospitalized for another reason n In 30% to 50% of the cases, a definite microbial etiology was not found
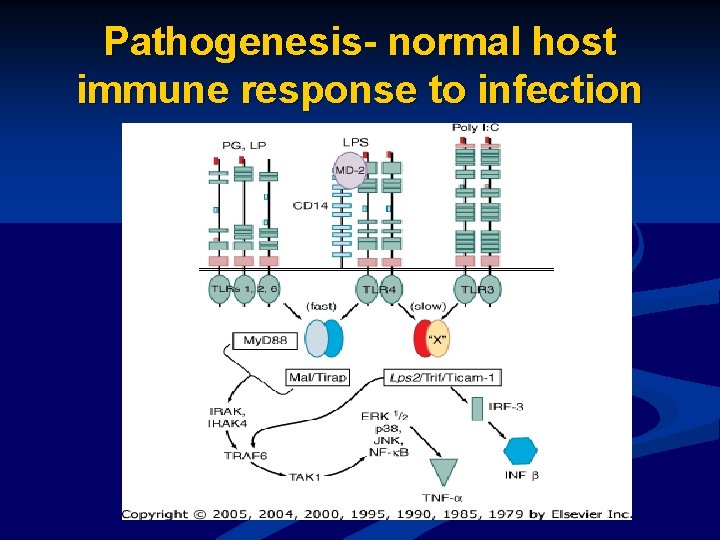
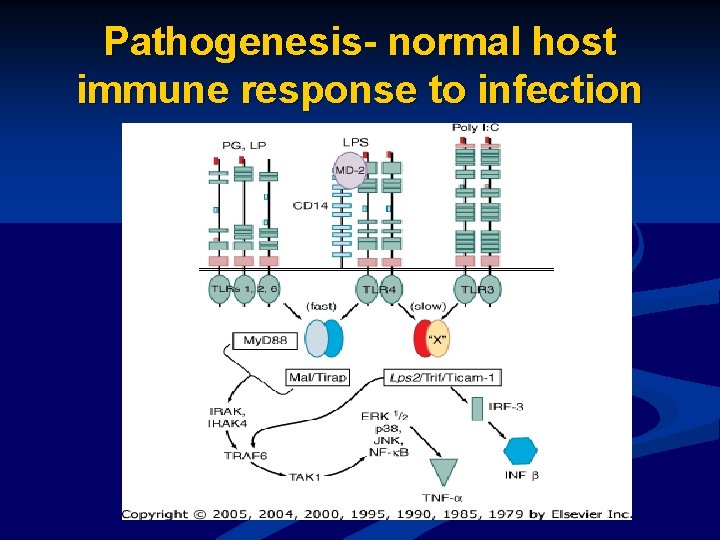
Pathogenesis- normal host immune response to infection
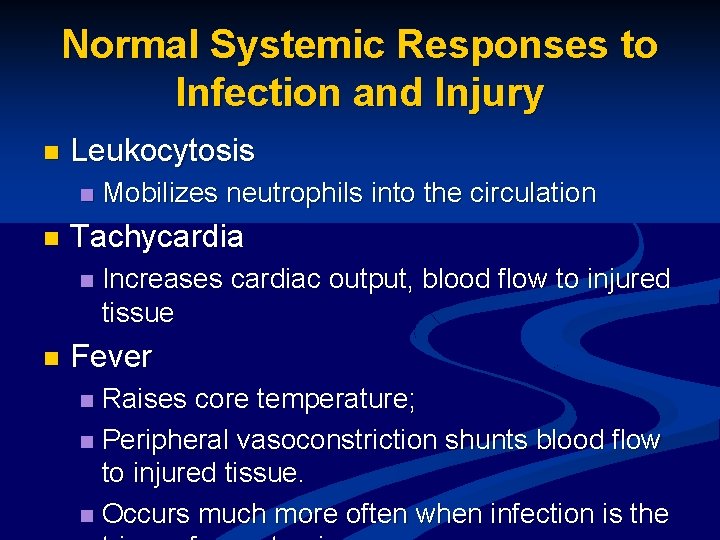
Normal Systemic Responses to Infection and Injury n Leukocytosis n n Tachycardia n n Mobilizes neutrophils into the circulation Increases cardiac output, blood flow to injured tissue Fever Raises core temperature; n Peripheral vasoconstriction shunts blood flow to injured tissue. n Occurs much more often when infection is the n
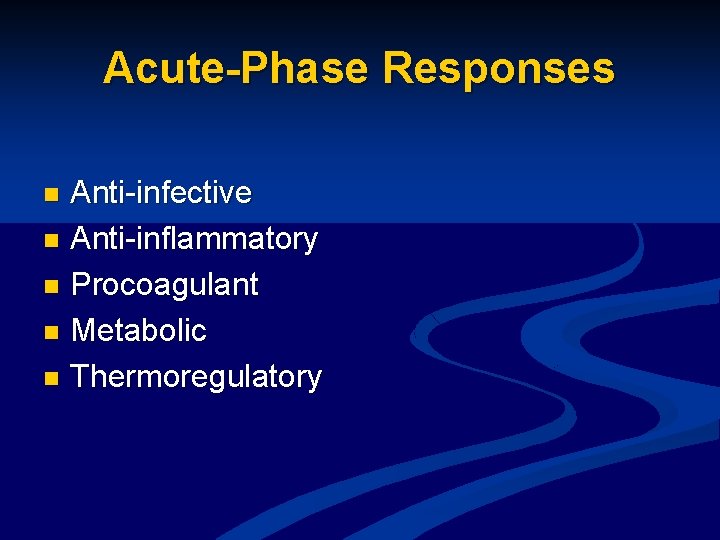
Acute-Phase Responses Anti-infective n Anti-inflammatory n Procoagulant n Metabolic n Thermoregulatory n
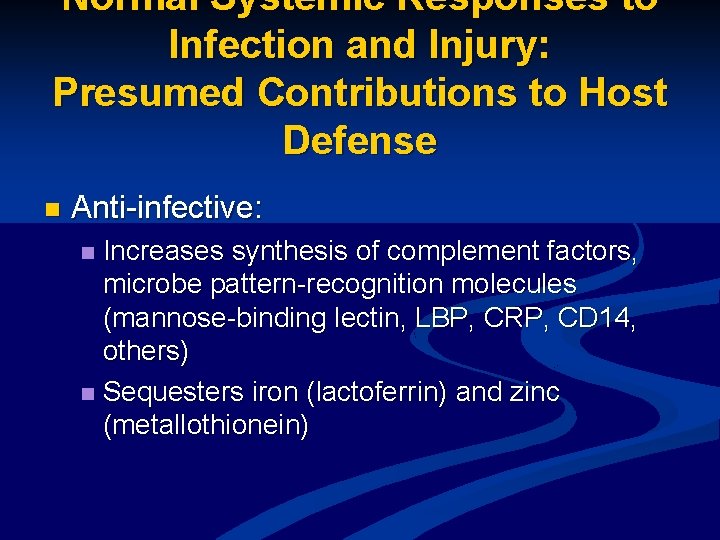
Normal Systemic Responses to Infection and Injury: Presumed Contributions to Host Defense n Anti-infective: Increases synthesis of complement factors, microbe pattern-recognition molecules (mannose-binding lectin, LBP, CRP, CD 14, others) n Sequesters iron (lactoferrin) and zinc (metallothionein) n
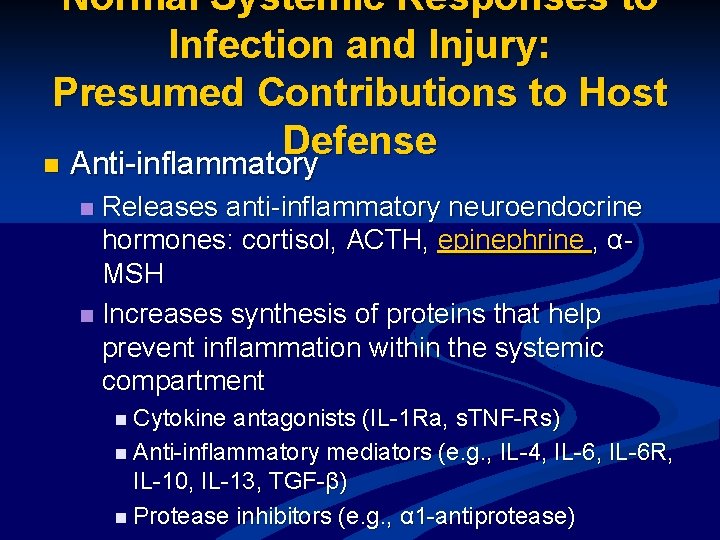
Normal Systemic Responses to Infection and Injury: Presumed Contributions to Host Defense n Anti-inflammatory Releases anti-inflammatory neuroendocrine hormones: cortisol, ACTH, epinephrine , αMSH n Increases synthesis of proteins that help prevent inflammation within the systemic compartment n n Cytokine antagonists (IL-1 Ra, s. TNF-Rs) n Anti-inflammatory mediators (e. g. , IL-4, IL-6 R, IL-10, IL-13, TGF-β) n Protease inhibitors (e. g. , α 1 -antiprotease)
Normal Systemic Responses to Infection and Injury: Presumed Contributions to Host Defense n Procoagulant: n Walls off infection, prevents systemic spread n Increases synthesis or release of fibrinogen, PAI-1, C 4 b n Decreases synthesis of protein C, anti -thrombin III
Normal Systemic Responses to Infection and Injury: Presumed Contributions to Host Defense n Metabolic: Preserves euglycemia, mobilizes fatty acids, amino acids n Epinephrine , cortisol, glucagon, cytokines n
Normal Systemic Responses to Infection and Injury: Presumed Contributions to Host Defense n Thermoregulatory; Inhibits microbial growth n Fever n
Pathologic Host Responses to Infection Sepsis n Severe Sepsis n Septic Shock n
Bacteremia n Cultivatable bacteria in the blood stream n May be transient and inconsequential; inconsistent correlation with severe sepsis
Sepsis n The systemic response to infection n If associated with proven or clinically suspected infection, SIRS is called "sepsis" in the American consensus scheme
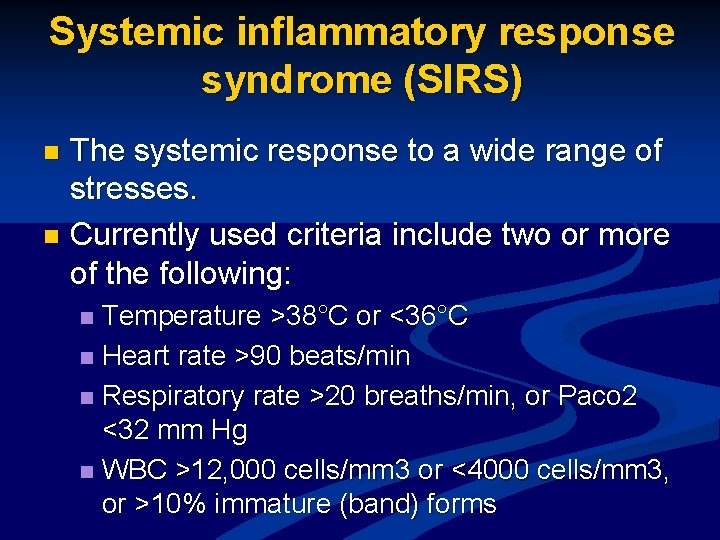
Systemic inflammatory response syndrome (SIRS) The systemic response to a wide range of stresses. n Currently used criteria include two or more of the following: n Temperature >38°C or <36°C n Heart rate >90 beats/min n Respiratory rate >20 breaths/min, or Paco 2 <32 mm Hg n WBC >12, 000 cells/mm 3 or <4000 cells/mm 3, or >10% immature (band) forms n
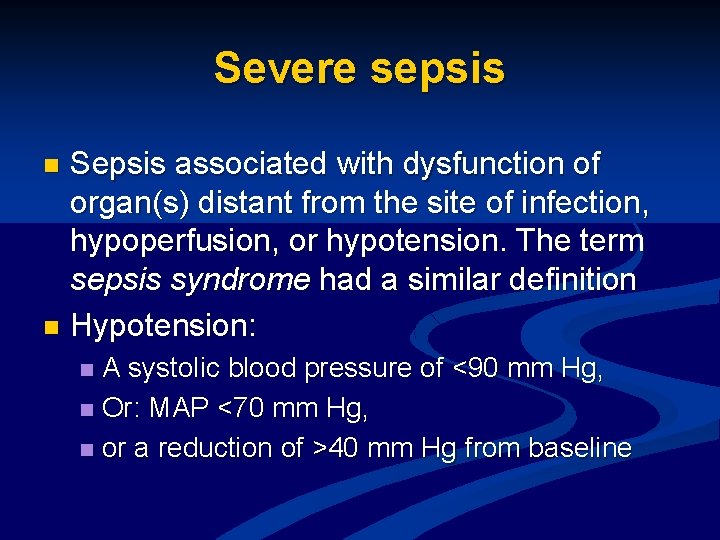
Severe sepsis Sepsis associated with dysfunction of organ(s) distant from the site of infection, hypoperfusion, or hypotension. The term sepsis syndrome had a similar definition n Hypotension: n A systolic blood pressure of <90 mm Hg, n Or: MAP <70 mm Hg, n or a reduction of >40 mm Hg from baseline n
Pathogenesis of Severe Sepsis Microcirculatory Dysfunction. n Activation or Injury of the Vascular Endothelium. n Cytokines and Other Mediators. n Complement Activation. n Coagulopathy. n Immunosuppression. n
Sepsis – what’s the point? 1. Patologic activation of immunology system 2. Immunosupression and anergy
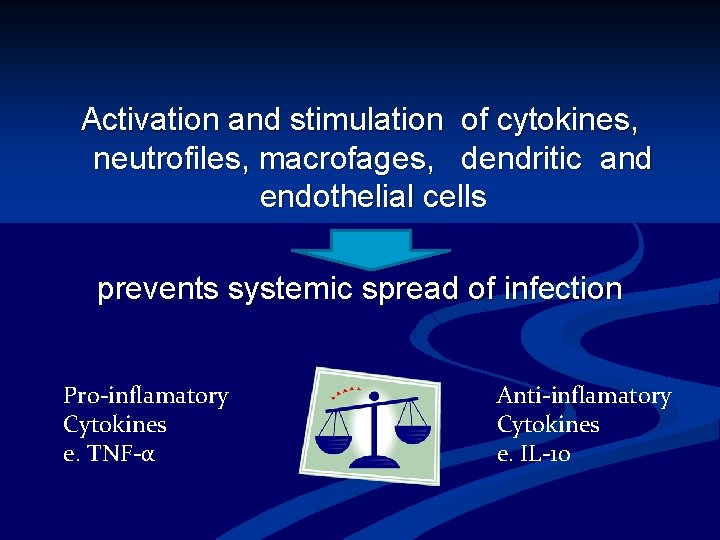
Activation and stimulation of cytokines, neutrofiles, macrofages, dendritic and endothelial cells prevents systemic spread of infection Pro-inflamatory Cytokines e. TNF-α Anti-inflamatory Cytokines e. IL-10
Severe sepsis Brain blood flow decreasing n Oliguria or anuria n ARDS- lung injury n Cardiovascular injury n Liver injury n DIC n
Septic shock Sepsis with hypotension that, despite adequate fluid resuscitation, requires pressor therapy. n In addition, there are perfusion abnormalities that may include: n lactic acidosis, n oliguria, n altered mental status, n and acute lung injury n
Pathogenesis of Septic Shock n n n n Tachyphylaxis to catecholamines, which diminishes the sensitivity of vascular smooth muscle to catecholamines as pressors The underproduction or ineffectiveness of glucocorticoids, which upregulate adrenergic receptors The production of adrenomedullin, which has vasodilatory actions, increases renal blood flow, and inhibits aldosterone secretion The release of nitric oxide from sites of inflammation and/or distant vascular endothelium The absence of the normal baroreflex response that increases circulating vasopressin levels (and depletion of neurohypophyseal vasopressin stores) The release of PAF The activation of KATP channels in arteriolar smooth muscle cells by hypoxia and lactate The generation of bradykinin, a vasodilator that also increases capillary permeability
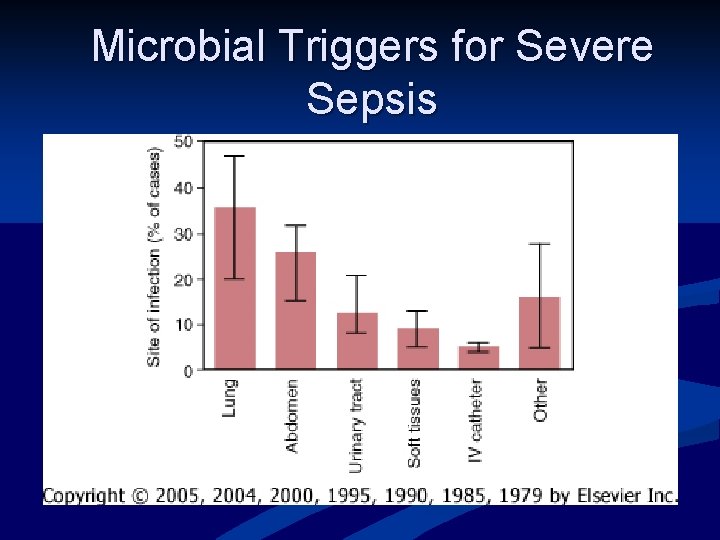
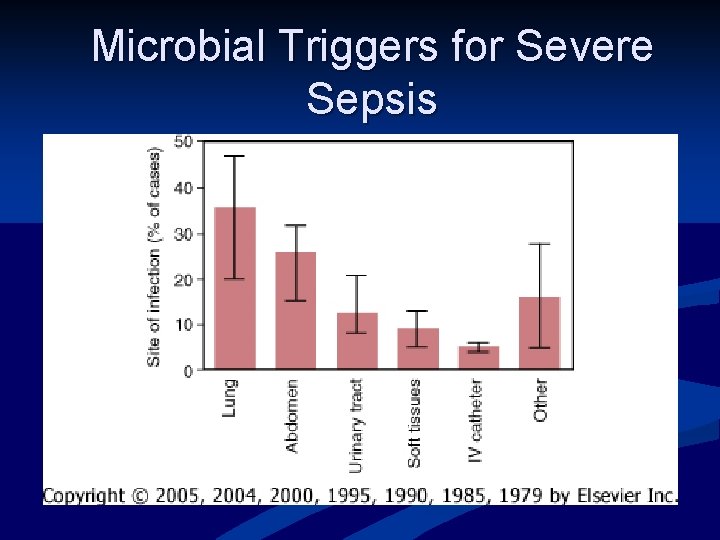
Microbial Triggers for Severe Sepsis
Diagnosis No bedside or laboratory test provides a definitive diagnosis. n SIRS (tachycardia, tachypnea, leukocytosis or leukopenia, and fever or hypothermia, n altered mental status, unexplained hyperbilirubinemia, metabolic acidosis, thrombocytopenia The appearance of new lesions on the skin or
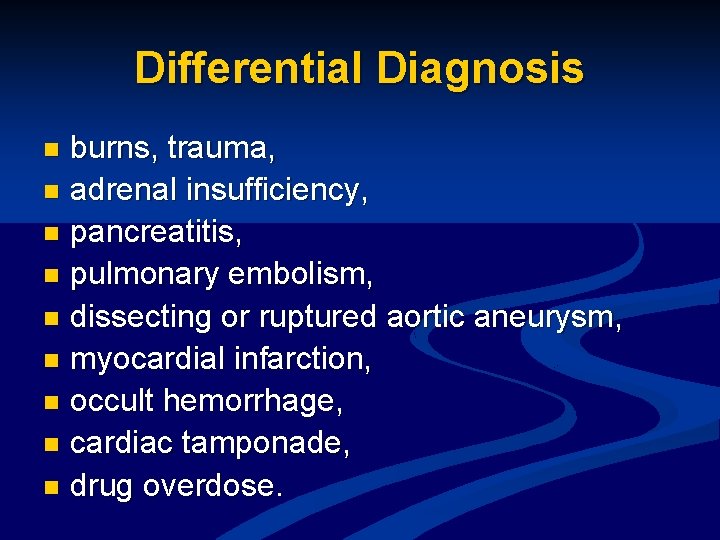
Differential Diagnosis burns, trauma, n adrenal insufficiency, n pancreatitis, n pulmonary embolism, n dissecting or ruptured aortic aneurysm, n myocardial infarction, n occult hemorrhage, n cardiac tamponade, n drug overdose. n
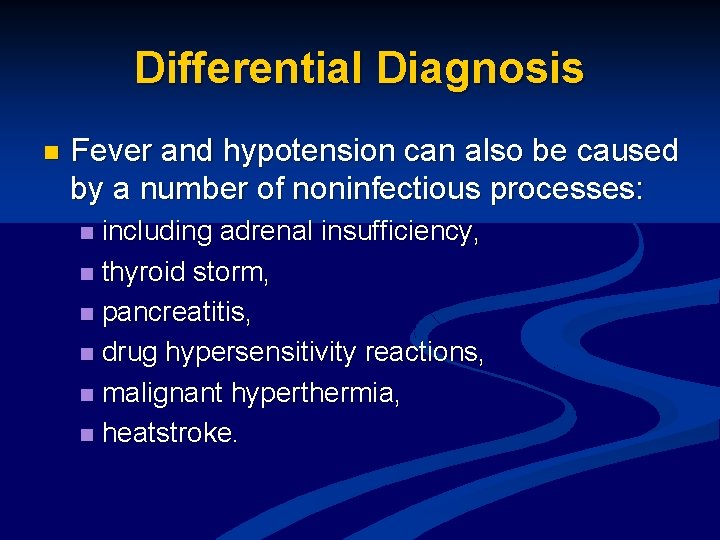
Differential Diagnosis n Fever and hypotension can also be caused by a number of noninfectious processes: including adrenal insufficiency, n thyroid storm, n pancreatitis, n drug hypersensitivity reactions, n malignant hyperthermia, n heatstroke. n
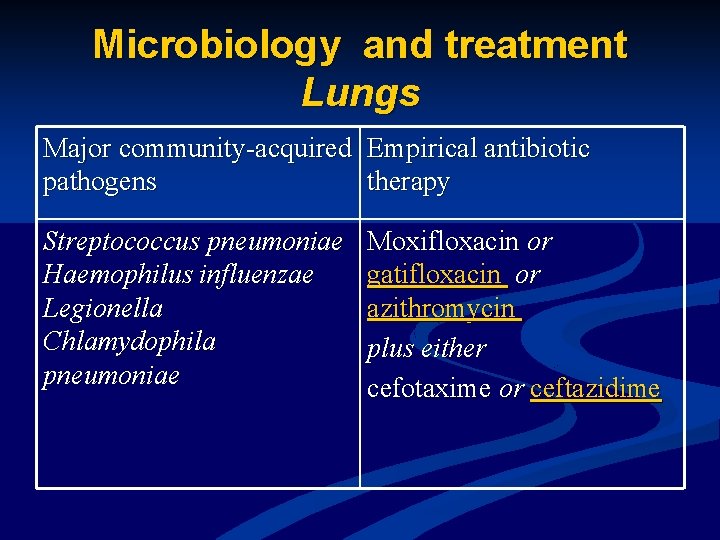
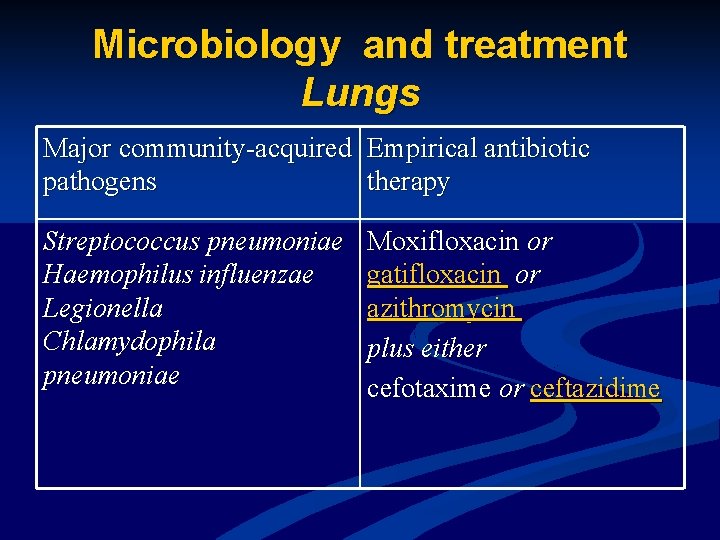
Microbiology and treatment Lungs Major community-acquired Empirical antibiotic pathogens therapy Streptococcus pneumoniae Haemophilus influenzae Legionella Chlamydophila pneumoniae Moxifloxacin or gatifloxacin or azithromycin plus either cefotaxime or ceftazidime
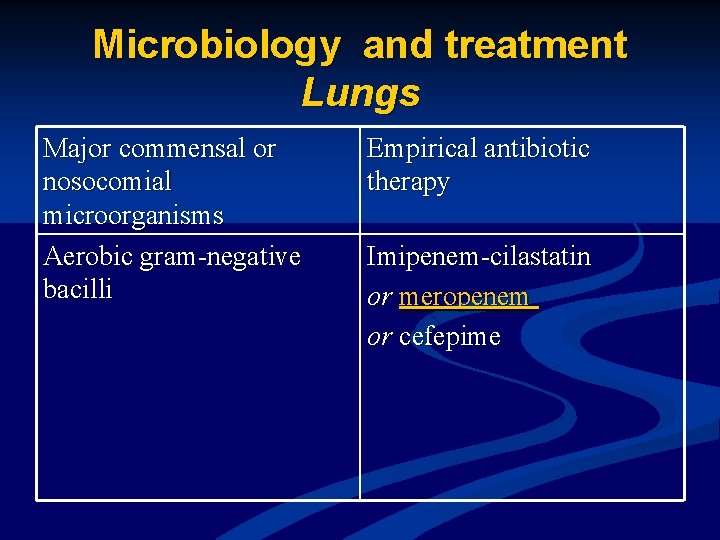
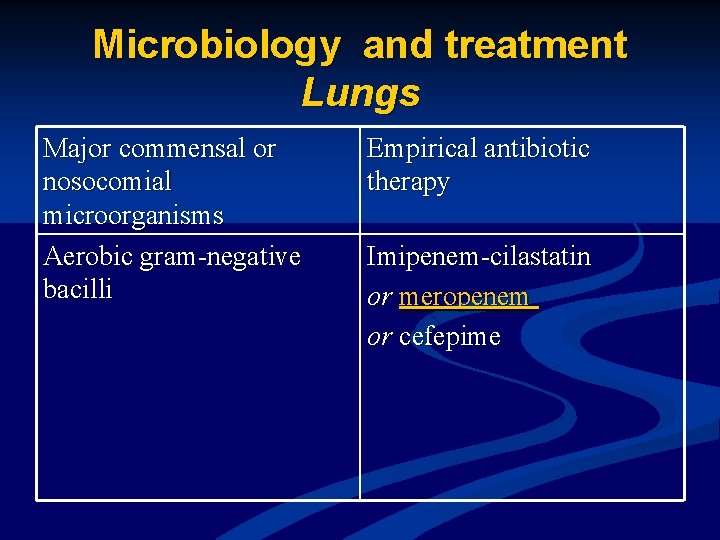
Microbiology and treatment Lungs Major commensal or nosocomial microorganisms Aerobic gram-negative bacilli Empirical antibiotic therapy Imipenem-cilastatin or meropenem or cefepime
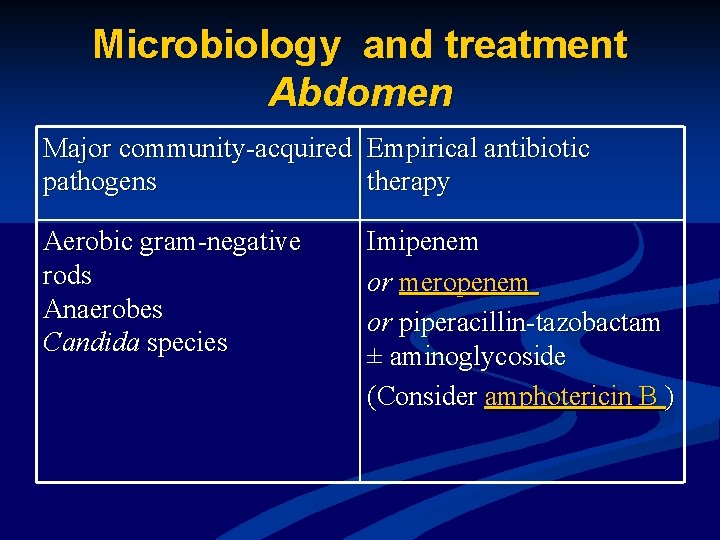
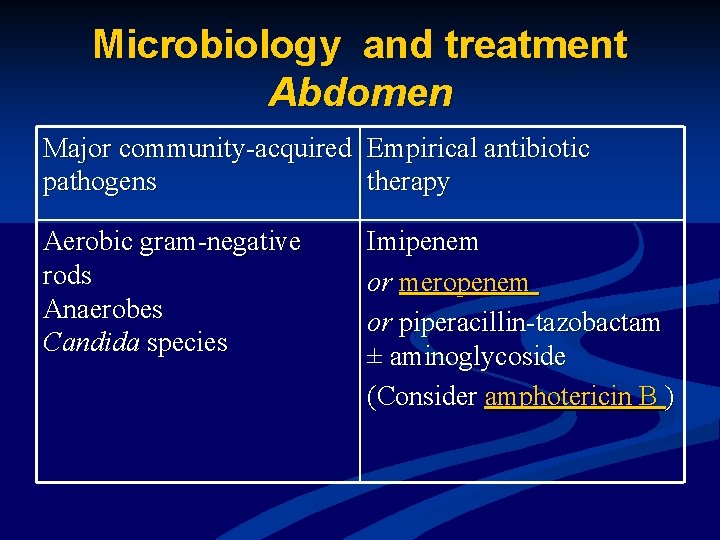
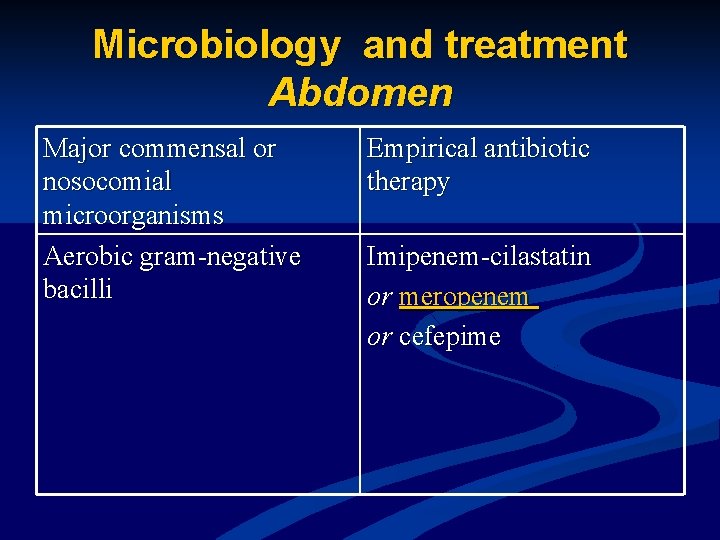
Microbiology and treatment Abdomen Major community-acquired Empirical antibiotic pathogens therapy Aerobic gram-negative rods Anaerobes Candida species Imipenem or meropenem or piperacillin-tazobactam ± aminoglycoside (Consider amphotericin B )
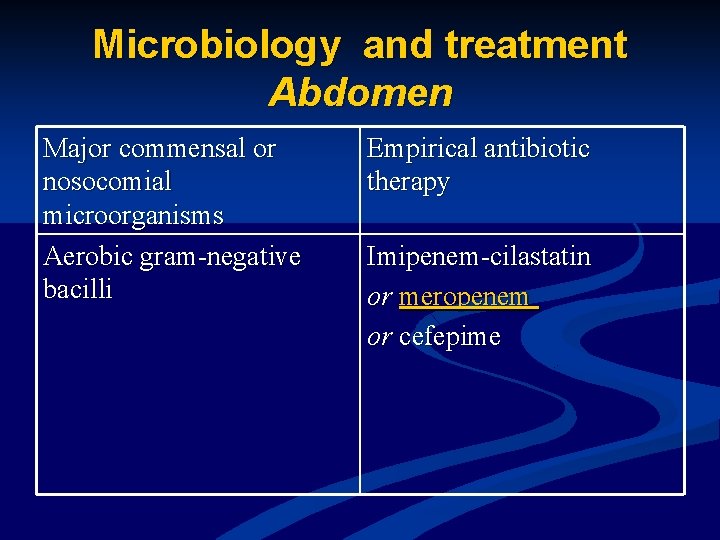
Microbiology and treatment Abdomen Major commensal or nosocomial microorganisms Aerobic gram-negative bacilli Empirical antibiotic therapy Imipenem-cilastatin or meropenem or cefepime
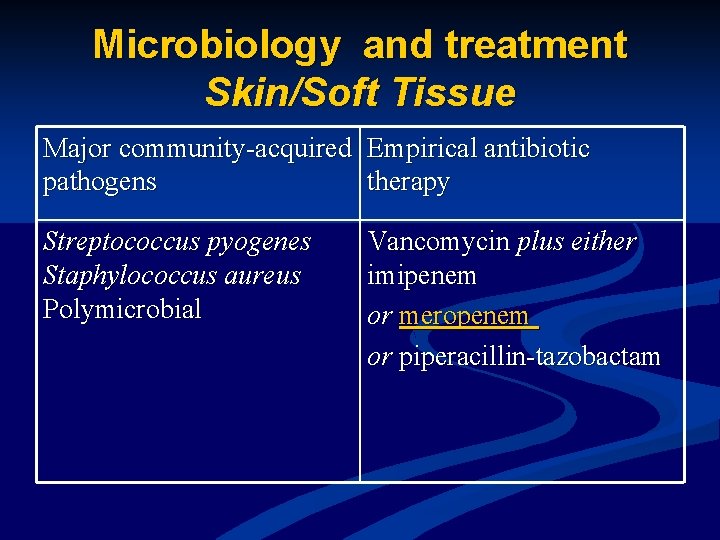
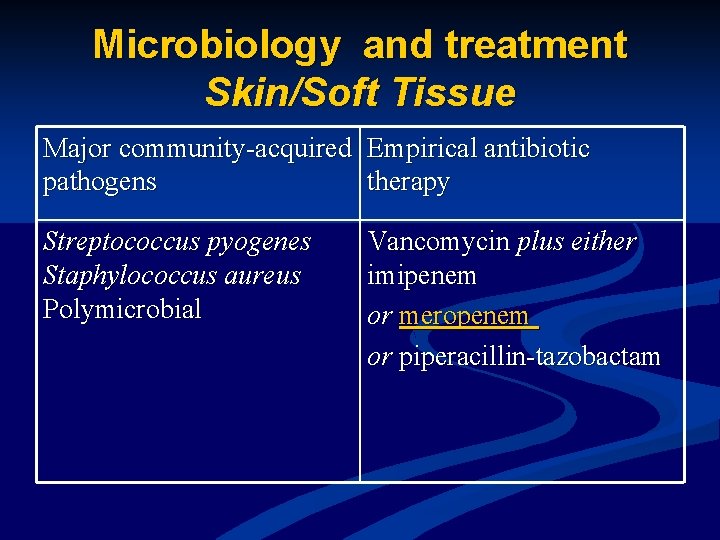
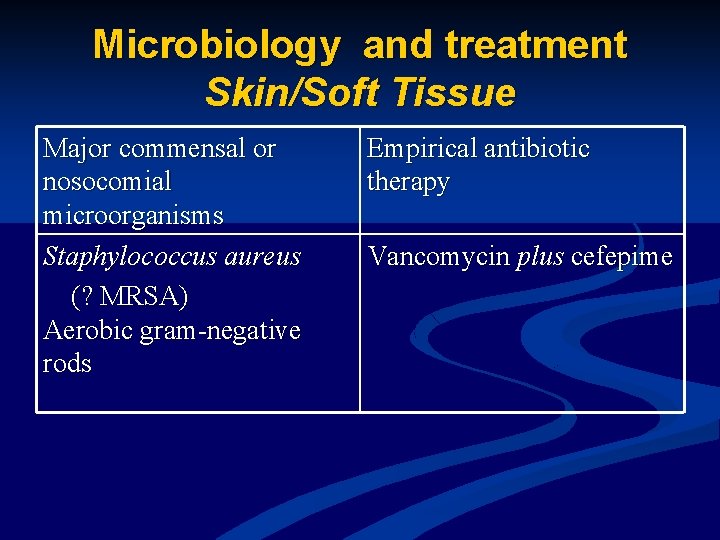
Microbiology and treatment Skin/Soft Tissue Major community-acquired Empirical antibiotic pathogens therapy Streptococcus pyogenes Staphylococcus aureus Polymicrobial Vancomycin plus either imipenem or meropenem or piperacillin-tazobactam
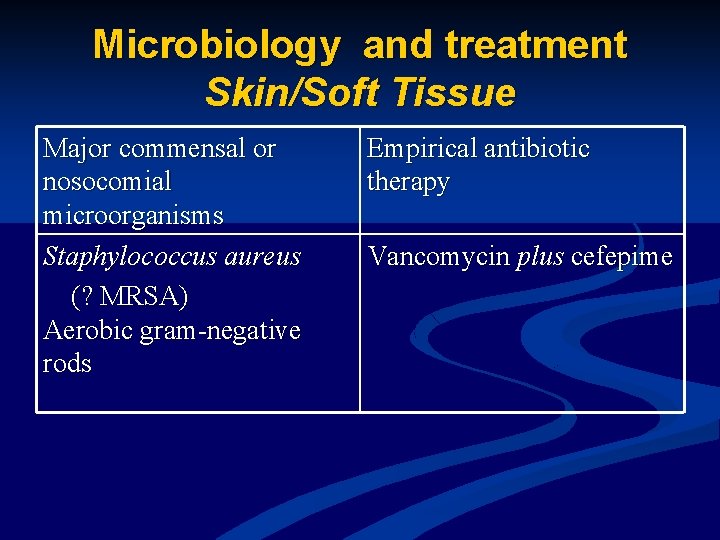
Microbiology and treatment Skin/Soft Tissue Major commensal or nosocomial microorganisms Staphylococcus aureus (? MRSA) Aerobic gram-negative rods Empirical antibiotic therapy Vancomycin plus cefepime
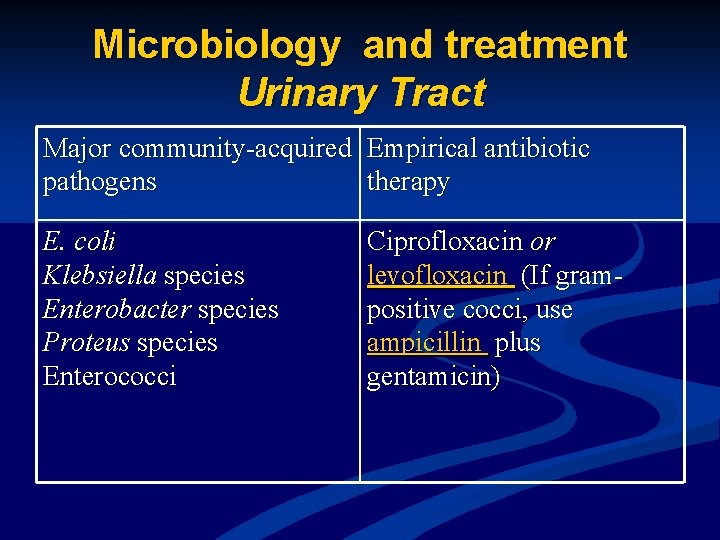
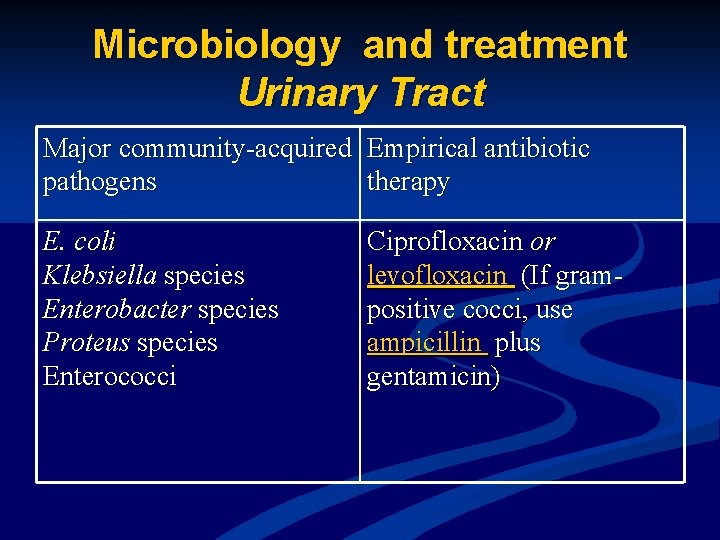
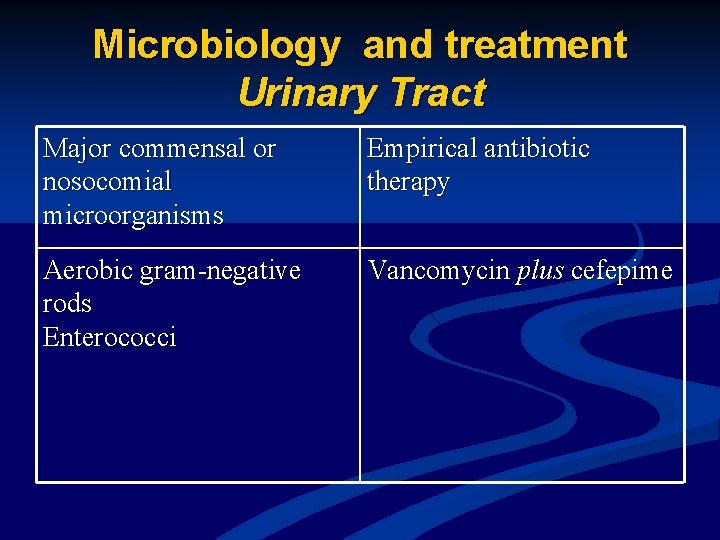
Microbiology and treatment Urinary Tract Major community-acquired Empirical antibiotic pathogens therapy E. coli Klebsiella species Enterobacter species Proteus species Enterococci Ciprofloxacin or levofloxacin (If grampositive cocci, use ampicillin plus gentamicin)
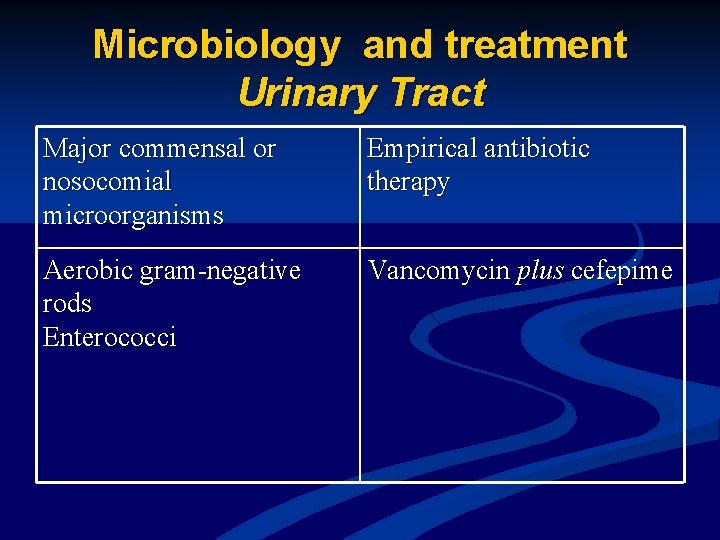
Microbiology and treatment Urinary Tract Major commensal or nosocomial microorganisms Empirical antibiotic therapy Aerobic gram-negative rods Enterococci Vancomycin plus cefepime
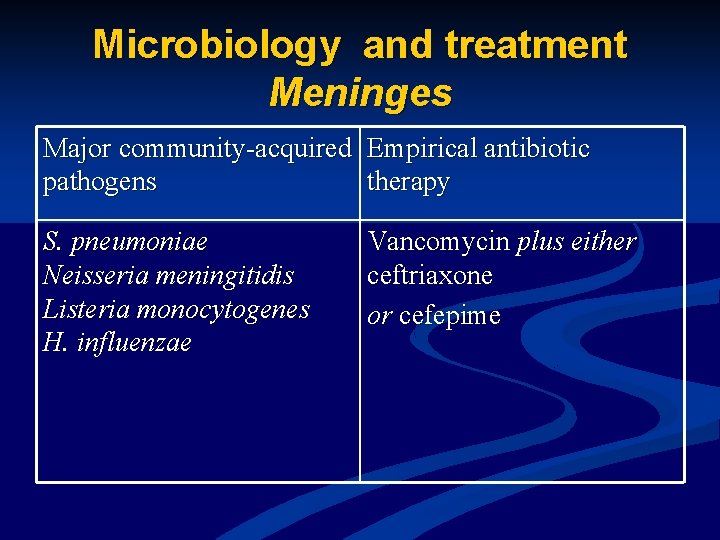
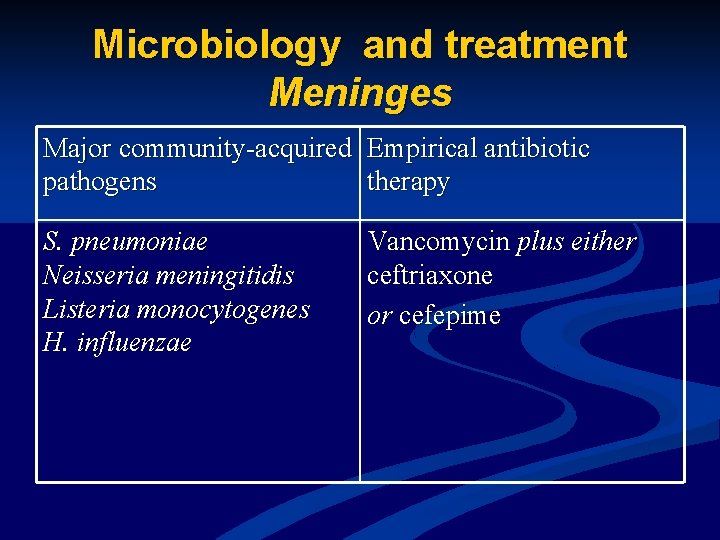
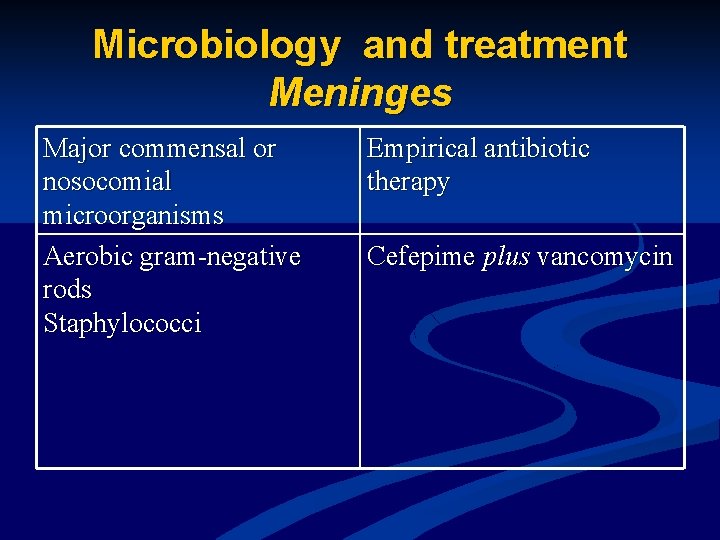
Microbiology and treatment Meninges Major community-acquired Empirical antibiotic pathogens therapy S. pneumoniae Neisseria meningitidis Listeria monocytogenes H. influenzae Vancomycin plus either ceftriaxone or cefepime
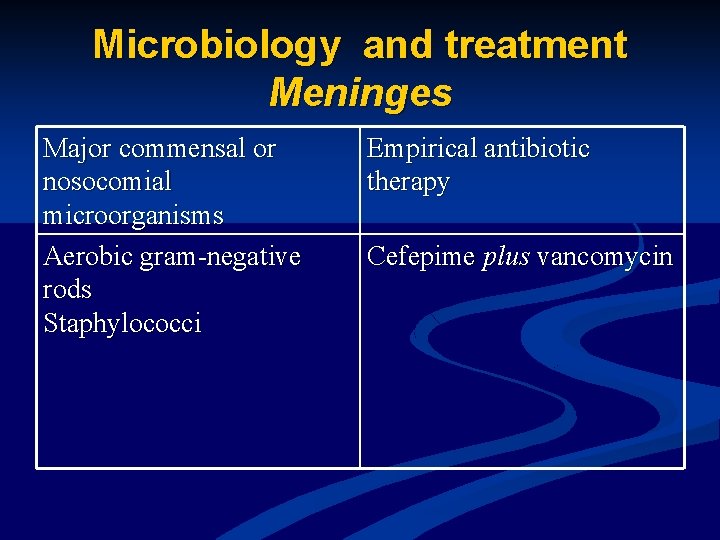
Microbiology and treatment Meninges Major commensal or nosocomial microorganisms Aerobic gram-negative rods Staphylococci Empirical antibiotic therapy Cefepime plus vancomycin
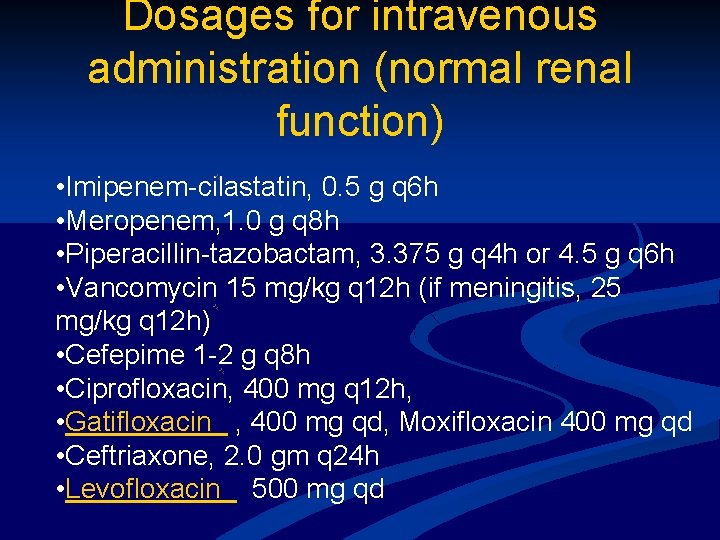
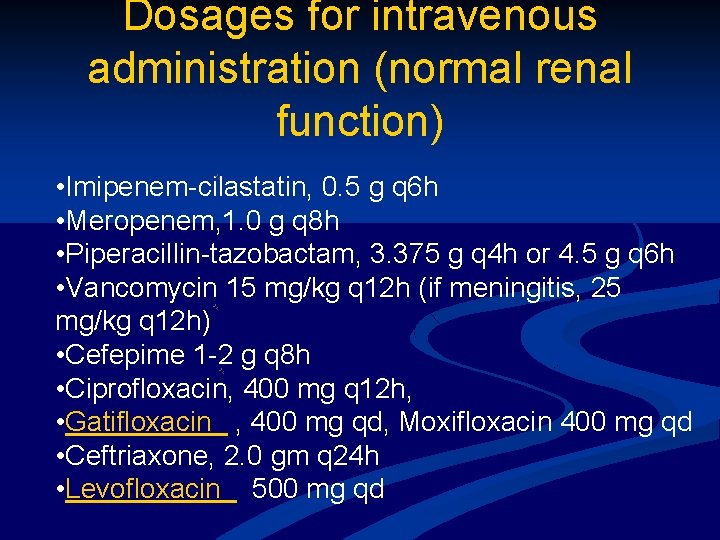
Dosages for intravenous administration (normal renal function) • Imipenem-cilastatin, 0. 5 g q 6 h • Meropenem, 1. 0 g q 8 h • Piperacillin-tazobactam, 3. 375 g q 4 h or 4. 5 g q 6 h • Vancomycin 15 mg/kg q 12 h (if meningitis, 25 mg/kg q 12 h) • Cefepime 1 -2 g q 8 h • Ciprofloxacin, 400 mg q 12 h, • Gatifloxacin , 400 mg qd, Moxifloxacin 400 mg qd • Ceftriaxone, 2. 0 gm q 24 h • Levofloxacin 500 mg qd
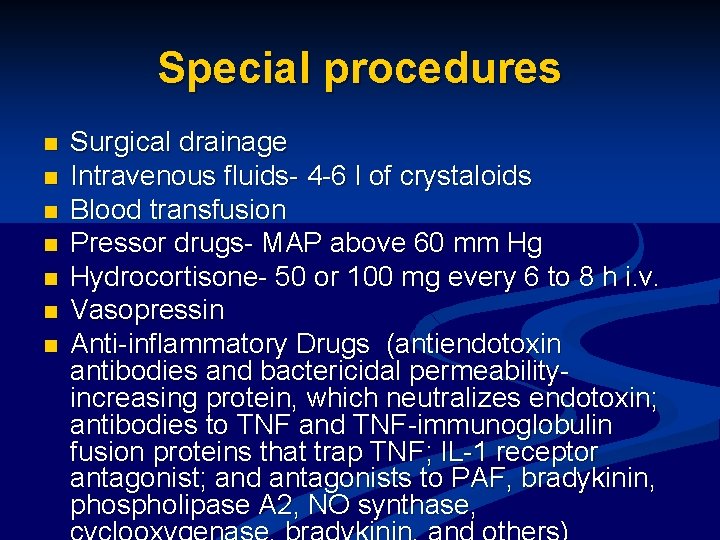
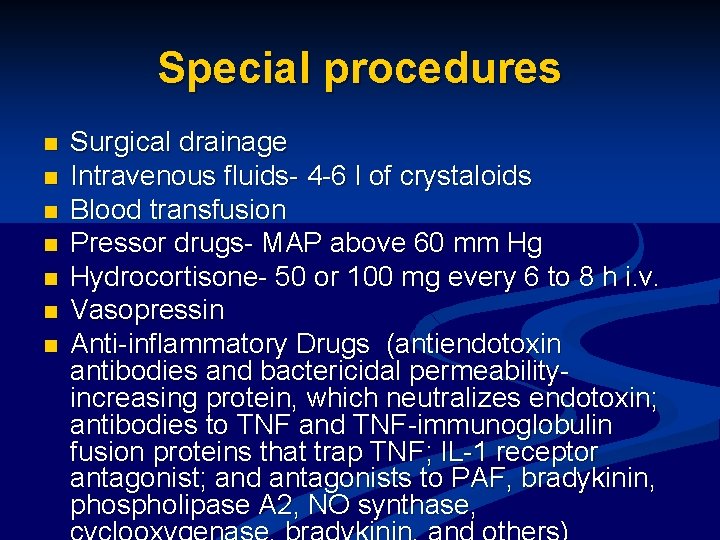
Special procedures n n n n Surgical drainage Intravenous fluids- 4 -6 l of crystaloids Blood transfusion Pressor drugs- MAP above 60 mm Hg Hydrocortisone- 50 or 100 mg every 6 to 8 h i. v. Vasopressin Anti-inflammatory Drugs (antiendotoxin antibodies and bactericidal permeabilityincreasing protein, which neutralizes endotoxin; antibodies to TNF and TNF-immunoglobulin fusion proteins that trap TNF; IL-1 receptor antagonist; and antagonists to PAF, bradykinin, phospholipase A 2, NO synthase,
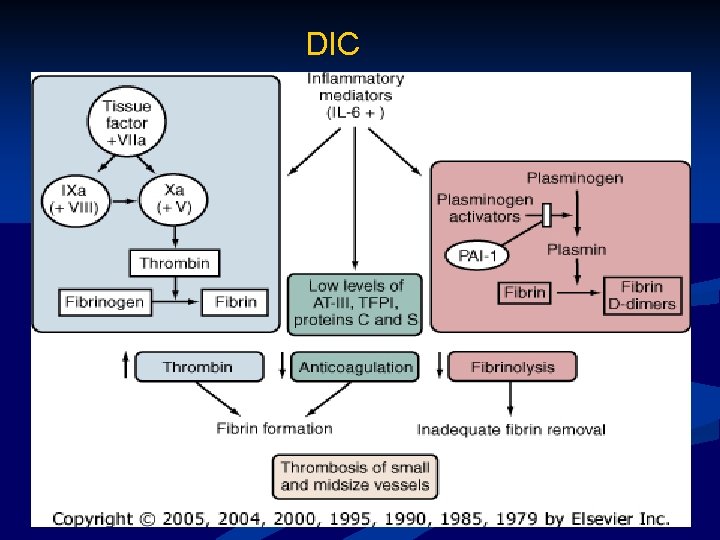
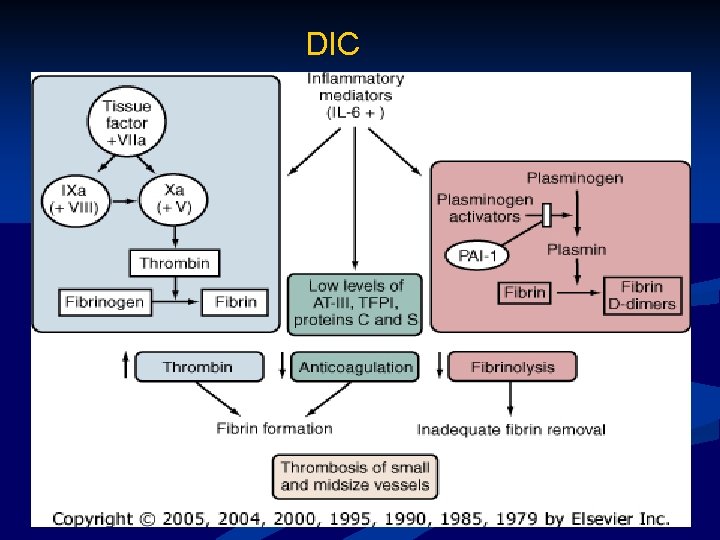
DIC
![Special procedures Anticoagulants n a PC drotrecogin alfa Xigris Indication severe sepsis with DIC Special procedures Anticoagulants n a. PC (drotrecogin alfa [Xigris]) Indication: severe sepsis with DIC](https://slidetodoc.com/presentation_image/77e2e1a16a7fd2a66800cdc07b2b6ced/image-41.jpg)
Special procedures Anticoagulants n a. PC (drotrecogin alfa [Xigris]) Indication: severe sepsis with DIC n Contrindications: n n severe liver disease, n a platelet count of less than 30, 000/mm 3, n prothrombin time- (INR) greater than 3. 0, n recent bleeding (including hemorrhagic stroke) n known bleeding diathesis, n recent surgery
Prevention n Prevention of hyperglycemia n n keep the blood glucose level between 100 and 140 mg/d. L Augmentation of host defenses
Prognosis n Mortality: 30% and 50%
 Prof. anna piekarska
Prof. anna piekarska Kryteria king's college
Kryteria king's college Prof anna piekarska
Prof anna piekarska Q sofa
Q sofa Cauda equina vs conus medullaris
Cauda equina vs conus medullaris Diferencia entre shock medular y shock neurogenico
Diferencia entre shock medular y shock neurogenico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock T10 spinal cord
T10 spinal cord Subacute combined degeneration
Subacute combined degeneration Jea septic tank phase out
Jea septic tank phase out Septic tank contamination groundwater
Septic tank contamination groundwater Septic arthritis gonorrhea
Septic arthritis gonorrhea Citizens energy group
Citizens energy group Ervin moore sign
Ervin moore sign Advantex ax20 price
Advantex ax20 price Barnstable septic loan
Barnstable septic loan Pickwickian syndrome in dogs
Pickwickian syndrome in dogs Septic arthritis complications
Septic arthritis complications Panhandle health septic
Panhandle health septic Septic arthritis antibiotics
Septic arthritis antibiotics Septic arthritis antibiotics
Septic arthritis antibiotics Bat septic
Bat septic Multi flo aerator replacement
Multi flo aerator replacement Puraflo peat
Puraflo peat Septic arthritis complications
Septic arthritis complications Doc's septic tank cleaning
Doc's septic tank cleaning Enthesitis
Enthesitis Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Haemophilus influenzae
Haemophilus influenzae Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Oxygen sag curve
Oxygen sag curve Septic spleen
Septic spleen Septic arthritis workup
Septic arthritis workup Septic
Septic Summit county septic permit
Summit county septic permit Rock solid precast
Rock solid precast Nitrex
Nitrex Jean luc meynard
Jean luc meynard Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Drag the example to connect with the description given
Drag the example to connect with the description given Magnesium sulfate toxicity level
Magnesium sulfate toxicity level Severe weather safety precautions worksheet
Severe weather safety precautions worksheet None mild moderate severe
None mild moderate severe