Renal Disease Victor Politi M D FACP Medical




- Slides: 151
Renal Disease Victor Politi, M. D. , FACP Medical Director, SVCMC School of Allied Health Professions, Physician Assistant Program
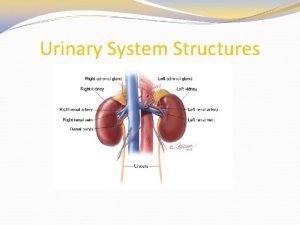
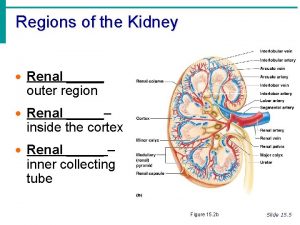
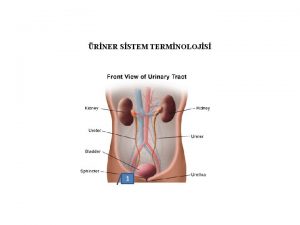
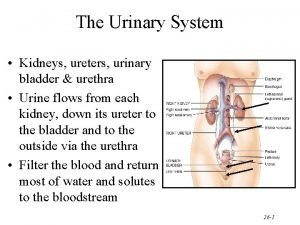
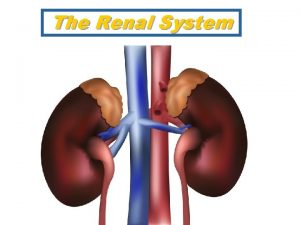
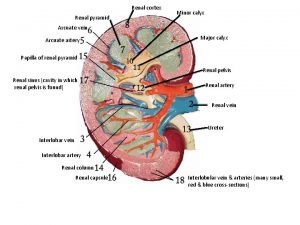
Kidney Function • The kidneys are bean-shaped organs, each about the size of a fist. • They are located near the middle of the back, just below the rib cage. • Every day, the kidneys process about 200 quarts of blood to sift out about 2 quarts of waste products and extra water. • The waste and extra water become urine, which flows to the bladder through tubes called ureters.
Kidney Function • Blood enters the kidneys through arteries that branch inside the kidneys into tiny clusters of looping blood vessels. – Each cluster is called a glomerulus, which comes from the Greek word meaning filter. – The plural form of the word is glomeruli. – There approximately 1 million glomeruli, or filters, in each kidney.
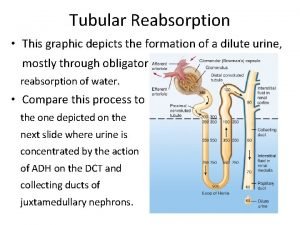
Kidney Function • The glomerulus is attached to the opening of a small fluid-collecting tube called a tubule. • Blood is filtered in the glomerulus, and extra water and wastes pass into the tubule and become urine. • Eventually, the urine drains from the kidneys into the bladder through larger tubes called ureters
Kidney Function • Each glomerulus-and-tubule unit is called a nephron. • Each kidney is composed of about 1 million nephrons. • In healthy nephrons, the glomerular membrane that separates the blood vessel from the tubule allows waste products and extra water to pass into the tubule while keeping blood cells and protein in the bloodstream.

The Kidneys • In addition to removing wastes, the kidneys release three important hormones: – erythropoietin or EPO, which stimulates the bone marrow to make red blood cells – renin, which regulates blood pressure – the active form of vitamin D, which helps maintain calcium for bones and for normal chemical balance in the body
Kidney Disease • Most kidney diseases attack the nephrons, causing them to lose their filtering capacity. • Damage to the nephrons may happen quickly, often as the result of injury or poisoning. But most kidney diseases destroy the nephrons slowly and silently. • Only after years or even decades will the damage become apparent. • Most kidney diseases attack both kidneys simultaneously.
Common Causes of Kidney Disease • Each year in the United States, nearly 100, 000 people are diagnosed with kidney failure – Diabetes is the most common cause of kidney failure, accounting for more than 40 percent of new cases. – Even when drugs and diet are able to control diabetes, the disease can lead to nephropathy and kidney failure.

Common Causes of Kidney Disease • The two most common causes of kidney disease are – diabetes – high blood pressure. • Hereditary also plays a role
Diabetic Nephropathy • Damage to the nephrons from unused glucose in the blood is called diabetic nephropathy. • Keeping blood glucose levels down can delay or prevent diabetic nephropathy • Overall, kidney damage rarely occurs in the first 10 years of diabetes, and usually 15 to 25 years will pass before kidney failure occurs. • For people who live with diabetes for more than 25 years without any signs of kidney failure, the risk of ever developing it decreases.
High Blood Pressure • High blood pressure (hypertension) is a major factor in the development of kidney problems in people with diabetes. • Both a family history of hypertension and the presence of hypertension appear to increase chances of developing kidney disease. • Hypertension also accelerates the progress of kidney disease where it already exists.
High Blood Pressure • High blood pressure can damage the small blood vessels in the kidneys. • Blood pressure medicines called angiotensin -converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) have been found to protect the kidneys even more than other medicines that lower blood pressure to similar levels.
High Blood Pressure • The National Heart, Lung, and Blood Institute (NHLBI), one of the National Institutes of Health, recommends that people with diabetes or reduced kidney function should keep their blood pressure below 130/80 mm Hg.
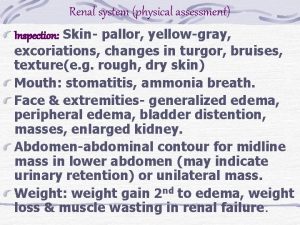
Approach to Kidney Disease • Often discovered incidentally during routine exam • Or patient presents with symptoms of renal dysfunction: – HTN – Edema – nausea – hematuria
Approach to Kidney Disease • Evaluation of patient includes: – time estimate of disease duration – urinalysis – GFR glomerular filtration rate assessment
Approach to Kidney Disease • Diagnostic Categories – Prerenal disease – Postrenal disease – Intrinsic renal disease • • Glomerular Tubular Interstitial Vascular
Urinalysis • • “Poor man’s renal biopsy” midstream sample or by bladder cath urine should be examined within one hour dipstick eval - if positive findings follow by microscopic assessment
Urinalysis • Dipstick measures – urinary specific gravity – p. H – protein – hemoglobin – glucose – ketones – bilirubin – nitrites
Urinalysis • Microscopy searches for – all formed elements • • crystals cells casts infecting organisms • Wright’s stain can detect eosinophiluria
Urinalysis • Bland urinary sediment common especially in – CRD – prerenal disorders – postrenal disorders • hematuria with dysmorphic red blood cells, red blood cell casts, and mild proteinuria is indicative of glomerulonephritis
Urinalysis • Red blood cells are misshapen during passage from the capillary through the glomerular basement membrane into the urinary space of Bowman’s capsule
Urinalysis • Casts are composed of Tamm-Horsfall urinary mucoprotein in the shape of the nephron segment where they were formed • Heavy proteinuria and lipiduria are consistent with the nephrotic syndrome • pigmented granular casts and renal tubular epithelial cells alone or in casts suggest acute tubular necrosis
Microalbuminuria and Proteinuria • small amounts of albumin, microalbuminuria, is a sign of deteriorating kidney function • As kidney function worsens, the amount of albumin and other proteins in the urine increases, and the condition is called proteinuria (generally >150 -160 mg/24 h in adults • Usually glomerular in origin when >1 g/d
Primary reasons for development of Proteinuria • Functional proteinuria - benign process from stressors (acute illness) • Orthostatic proteinuria – generally in people < age 30 – diagnosed by 8 -hour overnight supine urinary protein excretion - should be < 50 mg
Primary reasons for development of Proteinuria • Overload Proteinuria – Bence Jones proteins (multiple myeloma) – myoglobinuria in rhabdomyolysis – lysozymuria in some leukemias
Proteinuria • The most reliable way to quantify proteinuria is a 24 hour urine collection – a finding of >150 mg/24 h is abnormal and >3. 5 g/24 hr is consistent with nephrotic range proteinuria
Proteinuria • ACE inhibitors are effective by lowering efferent arteriolar resistance out of proportion to afferent arteriolar resistance reducing glomerular capillary pressure and lowering urinary protein excretion • hyperkalemia does not occur and serum creatinine rises less than 30%
Hematuria • Hematuria is significant if there are more than 3 to 5 red cells per high power field • positive dipstick tests can be caused by vitamin C, beets, and rhubarb, bacteria, and myoglobin
Glomerular Filtration Rate (GFR) Based on Creatinine Measurement • Creatinine is a waste product in the blood created by the normal breakdown of muscle cells during activity. • Healthy kidneys take creatinine out of the blood and put it into the urine to leave the body. • When kidneys are not working well, creatinine builds up in the blood.
Glomerular Filtration Rate (GFR) Based on Creatinine Measurement • GFR is a calculation of how efficiently the kidneys are filtering wastes from the blood. • A traditional GFR calculation requires an injection into the bloodstream of a substance that is later measured in a 24 -hour urine collection. – Recently, scientists found they could calculate GFR without an injection or urine collection. – The new calculation requires only a measurement of the creatinine in a blood sample.
Glomerular Filtration Rate (GFR) Based on Creatinine Measurement • blood will be tested to see how many milligrams of creatinine are in one deciliter of blood (mg/d. L). • Creatinine levels in the blood can vary, and each laboratory has its own normal range, usually 0. 6 to 1. 2 mg/d. L.
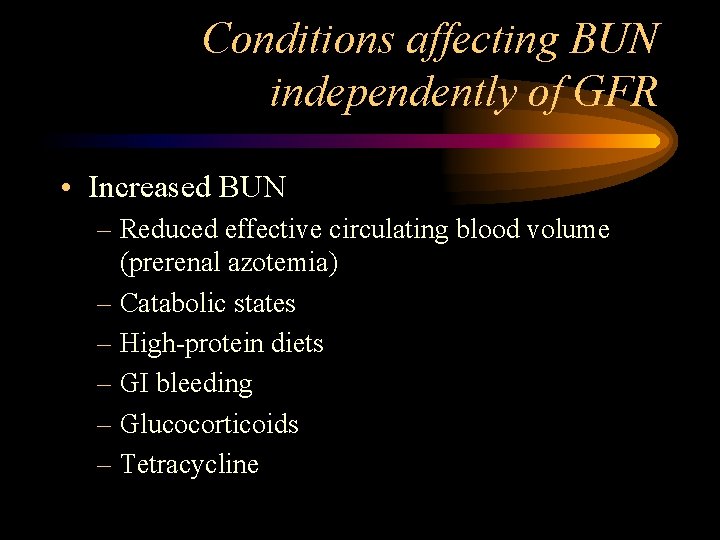
Conditions affecting BUN independently of GFR • Increased BUN – Reduced effective circulating blood volume (prerenal azotemia) – Catabolic states – High-protein diets – GI bleeding – Glucocorticoids – Tetracycline
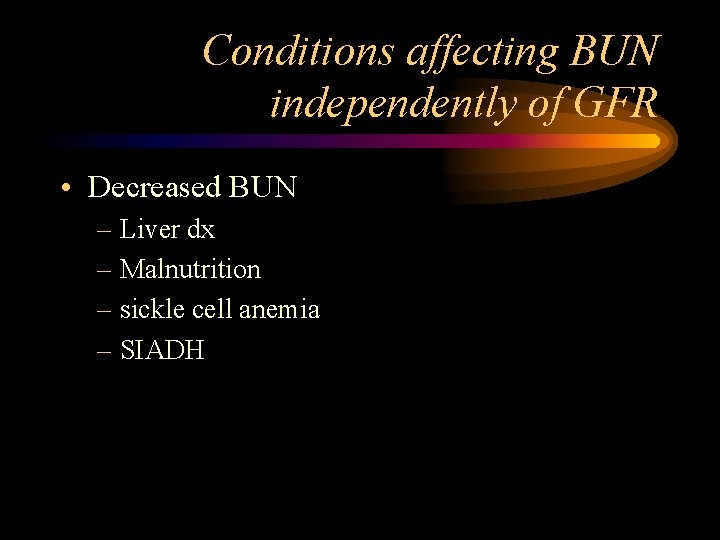
Conditions affecting BUN independently of GFR • Decreased BUN – Liver dx – Malnutrition – sickle cell anemia – SIADH
Blood Urea Nitrogen (BUN) • A deciliter of normal blood contains 7 to 20 milligrams of urea. • If the BUN is more than 20 mg/d. L, the kidneys may not be working at full strength. • Other possible causes of an elevated BUN include dehydration and heart failure.
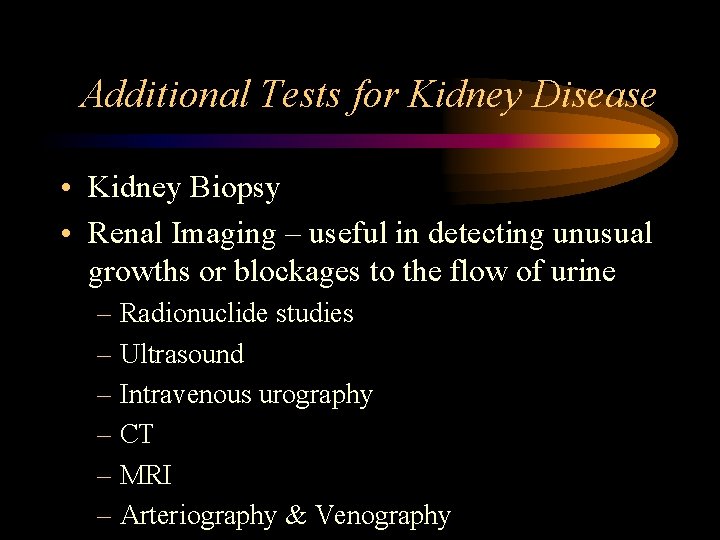
Additional Tests for Kidney Disease • Kidney Biopsy • Renal Imaging – useful in detecting unusual growths or blockages to the flow of urine – Radionuclide studies – Ultrasound – Intravenous urography – CT – MRI – Arteriography & Venography
Prerenal Azotemia • Most common cause of acute renal failure • due to renal hypoperfusion • can be immediately reversed – with restoration of renal blood flow, renal parenchymal damage does not occur
Prerenal Azotemia • Decreased renal perfusion can occur in one of three ways – decrease in intravascular volume – change in vascular resistance – low cardiac output
Postrenal Azotemia • Least common cause of acute renal failure (5% of cases) • occurs when urinary flow to both kidneys obstructed – each nephron has an elevated intraluminal pressure causing a decrease in GFR
Postrenal Azotemia • Causes include: – bladder dysfunction – bladder obstruction – obstruction of both ureters or renal pelvises – Men - benign prostatic hyperplasia most common cause – anticholinergic drugs - at risk – less common causes - ureteral or urethral stones/strictures, bilateral papillary necrosis
Intrinsic Renal Failure • Intrinsic renal disorders account for 50% of cases of acute renal failure • Intrinsic or parenchymal dysfunction is considered after prerenal and postrenal causes have been excluded
Intrinsic Renal Failure • Sites of injury – tubules – interstitium – vasculature – glomeruli
Acute Tubular Necrosis • ARF due to tubular damage - acute tubular necrosis • 85% of intrinsic acute renal failure • Two major causes: – ischemia - often preceded by prerenal azotemia – toxin exposure
Acute Tubular Necrosis • Exogenous nephrotoxins – Up to 25% of hospitalized patients receiving therapeutic levels of aminoglycosides sustain some degree of acute tubular necrosis – Nonoliguric renal failure typically occurs 5 -10 days after exposure – Aminoglycosides can remain in renal tissues for up to one month
Acute Tubular Necrosis • Exogenous nephrotoxins – Gentamicin is the most toxic – tobramycin the least – Amphotericin B is typically nephrotoxic after a dose of 2 -3 g – Vancomycin, acyclovir and several cephalosporins have been known to cause acute tubular necrosis
Acute Tubular Necrosis • Exogenous nephrotoxins – Radiographic contrast media • Contrast media is the 3 rd leading cause of new acute renal failure in hospitalized patients
Acute Tubular Necrosis • Endogenous Nephrotoxins – heme-containing products, uric acid, and paraproteins – Myoglobinuria as a consequence of rhabdomyolysis leads to acute tubular necrosis – Necrotic muscle releases large amounts of myoglobin which is freely filtered across the glomerulus
Acute Tubular Necrosis • Endogenous Nephrotoxins – The myoglobin is reabsorbed by the renal tubules, and direct damage can occur – Rhabdomyolysis of clinical importance commonly occurs with a serum creatine kinase > 20, 000 -50, 000 IU/L
Acute Tubular Necrosis • Endogenous Nephrotoxins – The globin moiety of myoglobin will cause the urine dipstick to read falsely positive for hemoglobin; the urine appears dark brown, but no red cells are present – With lysis of muscle cells, patients also become hyperkalemic, hyperphosphatemic and hyperuricemic
Acute Tubular Necrosis – Endogenous Nephrotoxins • Mainstay of treatment - hydration and diuresis as well as alkalinization of the urine • Massive intravascular hemolysis is seen in transfusion reactions an in certain hemolytic anemias • Hyperuricemia can occur in the setting of rapid cell turnover and lysis – chemotherapy for germ cell neoplasms and leukemias and lymphomas are the primary causes
Acute Tubular Necrosis • Endogenous Nephrotoxins – Bence Jones protein seen in conjunction with multiple myeloma can cause direct tubular toxicity and tubular obstruction
Interstitial Nephritis • Accounts of 10 -15% of cases of intrinsic renal failure • An interstitial inflammatory response with edema and possible tubular cell damage is the typical pathological finding • T lymphocytes can cause direct cytotoxicity or release lymphokines that recruit monocytes and inflammatory cells
Interstitial Nephritis • Drugs account for over 70% of cases • Also occurs in infectious diseases or immunologic disorders or idiopathic • Most common drugs - penicillins and cephalosporins, sulfonamides, and sulfonamide containing diuretics, NSAIDs, rifampin, phenytoin, allopurinol
Interstitial Nephritis • Infectious causes - streptococcal infections, leptospirosis, CMV, histoplasmosis, Rocky mountain spotted fever
Glomerular Diseases • Many diseases affect kidney function by attacking the glomeruli, the tiny units within the kidney where blood is cleaned. • Glomerular diseases include many conditions with a variety of genetic and environmental causes, but they fall into two major categories: – Glomerulonephritis – Glomerulosclerosis
symptoms of glomerular disease • • • proteinuria hematuria reduced glomerular filtration rate hypoproteinemia edema
Diagnosis • • Urinalysis Blood tests Ultrasound Kidney biopsy
Glomerulonephritis • describes the inflammation of the membrane tissue in the kidney that serves as a filter, separating wastes and extra fluid from the blood.
Glomerulosclerosis • describes the scarring or hardening of the tiny blood vessels within the kidney.
Glomerular disease • Glomerular diseases damage the glomeruli, letting protein and sometimes red blood cells leak into the urine. • Sometimes a glomerular disease also interferes with the clearance of waste products by the kidney, so they begin to build up in the blood. • Furthermore, loss of blood proteins like albumin in the urine can result in a fall in their level in the bloodstream.
Causes • A number of different diseases can result in glomerular disease. – direct result of infection or drug toxic to the kidneys – may result from a disease that affects the entire body, like diabetes or lupus. • Many different kinds of diseases can cause swelling or scarring of the nephron or glomerulus. • Sometimes glomerular disease is idiopathic.
Glomerular disease • In normal blood, albumin acts like a sponge, drawing extra fluid from the body into the bloodstream, where it remains until the kidneys remove it. • But when albumin leaks into the urine, the blood loses its capacity to absorb extra fluid from the body. – Fluid can accumulate outside the circulatory system in the face, hands, feet, or ankles and cause swelling.
Glomerulonephritis Causes: Autoimmune Diseases • When the body's immune system functions properly, it creates protein-like substances called antibodies and immunoglobulins to protect the body against invading organisms. • In an autoimmune disease, the immune system creates autoantibodies, which are antibodies or immunoglobulins that attack the body itself. • Autoimmune diseases may be systemic and affect many parts of the body, or they may affect only specific organs or regions.
Glomerulonephritis Causes: Autoimmune Diseases • Systemic lupus erythematosus (SLE) – affects many parts of the body: primarily the skin and joints, but also the kidneys. – women are more likely to develop SLE than men Lupus nephritis is the name given to the kidney disease caused by SLE, and it occurs when autoantibodies form or are deposited in the glomeruli, causing inflammation.
Glomerulonephritis Causes: Autoimmune Diseases • Goodpasture's syndrome – involves an autoantibody that specifically targets the kidneys and the lungs – Often, the first indication that patients have the autoantibody is when they cough up blood – Lung damage in Goodpasture's syndrome is usually superficial compared with progressive and permanent damage to the kidneys
Glomerulonephritis Causes: Autoimmune Diseases • Goodpasture’s Syndrome – rare condition that affects mostly young men but also occurs in women, children, and older adults – Treatments include immunosuppressive drugs and plasmapheresis to remove autoantibodies
Glomerulonephritis Causes: Autoimmune Diseases • Ig. A nephropathy – form of glomerular disease that results when immunoglobulin A (Ig. A) forms deposits in the glomeruli, where it creates inflammation.
Glomerulonephritis Causes: Autoimmune Diseases • Ig. A nephropathy – was not recognized as a cause of glomerular disease until the late 1960 s, when sophisticated biopsy techniques were developed that could identify Ig. A deposits in kidney tissue.
Glomerulonephritis Causes: Autoimmune Diseases • Ig. A nephropathy – most common symptom hematuria – but often a silent disease that may go undetected for many years – the most common cause of primary glomerulonephritis- not caused by systemic disease
Glomerulonephritis Causes: Autoimmune Diseases • Ig. A nephropathy • affects men more than women • found in all age groups – young people rarely display signs of kidney failure because it takes several years for disease to progress to stage where it causes detectable complications
Glomerulonephritis Causes: Autoimmune Diseases • Ig. A nephropathy – Researchers funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) are trying to discover why these deposits in the glomeruli are formed and whether dietary supplements of fish oil can inhibit Ig. A-induced inflammation and scarring in the kidney.
Glomerulonephritis Causes: Autoimmune Diseases • Hereditary Nephritis--Alport Syndrome – primary indicator of Alport syndrome is a family history of chronic glomerular disease, although it may also involve hearing or vision impairment. – Affects both men and women, but men are more likely to experience chronic renal failure and sensory loss
Glomerulonephritis Causes: Autoimmune Diseases • Hereditary Nephritis--Alport Syndrome – Men with Alport syndrome usually first show evidence of renal insufficiency while in their twenties and reach ESRD by age 40. – Women rarely have significant renal impairment, and hearing loss may be so slight that it can be detected only through testing. – Usually men can pass the disease only to their daughters. – Women can transmit the disease to either their sons or their daughters.
Glomerulonephritis Causes: Autoimmune Diseases • Infection-related Glomerular Disease • Glomerular disease sometimes develops rapidly after an infection in other parts of the body.
Glomerulonephritis Causes: Autoimmune Diseases • Acute post-streptococcal glomerulonephritis (PSGN) – can occur after an episode of strep throat or, in rare cases, impetigo. – The Streptococcus bacteria do not attack the kidney directly, but an infection may stimulate the immune system to overproduce antibodies, which are circulated in the blood and finally deposited in the glomeruli, causing damage.
Glomerulonephritis Causes: Autoimmune Diseases • Acute post-streptococcal glomerulonephritis (PSGN) – sudden symptoms of edema, oliguria, and hematuria – Tests will show large amounts of proteinuria and elevated levels of creatinine and urea nitrogen in the blood, thus indicating reduced kidney function. – High blood pressure frequently accompanies reduced kidney function in this disease.
Glomerulonephritis Causes: Autoimmune Diseases • Acute post-streptococcal glomerulonephritis (PSGN) – most common in children between the ages of 3 and 7, although it can strike at any age – most often affects boys – lasts only a brief time and usually allows the kidneys to recover – Rarely - kidney damage may be permanent, requiring dialysis or transplantation to replace renal function
Glomerulonephritis Causes: Autoimmune Diseases • Bacterial endocarditis – infection of the tissues inside the heart, is also associated with subsequent glomerular disease. – Researchers are not sure whether the renal lesions that form after a heart infection are caused entirely by the immune response or whether some other disease mechanism contributes to kidney damage.
Glomerulonephritis Causes: Autoimmune Diseases • Bacterial endocarditis – Treating the heart infection is the most effective way of minimizing kidney damage. Chronic renal failure can result from endocarditis, but is not inevitable.
Glomerulonephritis Causes: Autoimmune Diseases • HIV – can also cause glomerular disease. – Between 5 and 10% of people with HIV experience kidney failure, even before developing full-blown AIDS.
Glomerulonephritis Causes: Autoimmune Diseases • HIV-associated nephropathy usually begins with heavy proteinuria and progresses rapidly (within a year of detection) to ESRD.

Sclerotic Diseases
Sclerotic Diseases • Glomerulosclerosis is scarring (sclerosis) of the glomeruli. • In several sclerotic conditions, a systemic disease like lupus or diabetes is responsible. • Glomerulosclerosis is caused by the activation of glomerular cells to produce scar material.
Focal segmental glomerulosclerosis (FSGS) • Focal segmental glomerulosclerosis (FSGS) describes scarring in scattered regions of the kidney, typically limited to one part of the glomerulus and to a minority of glomeruli in the affected region.
Focal segmental glomerulosclerosis (FSGS) • FSGS may result from a systemic disorder or it may be idiopathic • Proteinuria is the most common symptom of FSGS • (proteinuria is associated with several other kidney conditions so a diagnosis of FSGS cannot be made on the basis of proteinuria alone)
Focal segmental glomerulosclerosis (FSGS) • Biopsy may confirm the presence of glomerular scarring if the tissue is taken from the affected section of the kidney. • But finding the affected section is a matter of chance, especially early in the disease process, when lesions may be scattered.
Focal segmental glomerulosclerosis (FSGS) • Confirming a diagnosis of FSGS may require repeat kidney biopsies. • Arriving at a diagnosis of idiopathic FSGS requires the identification of focal scarring and the elimination of possible systemic causes such as diabetes or an immune response to infection.
Focal segmental glomerulosclerosis (FSGS) • Since idiopathic FSGS is, by definition, of unknown cause, it is difficult to treat. • No universal remedy has been found, and most patients with FSGS progress to ESRD over 5 to 20 years. • Some patients with an aggressive form of FSGS reach ESRD in 2 to 3 years.
Focal segmental glomerulosclerosis (FSGS) • Treatments involving steroids or other immunosuppressive drugs appear to help some patients by decreasing proteinuria and improving kidney function. – But these treatments are beneficial to only a minority of those in whom they are tried, and some patients experience even poorer kidney function as a result.
Focal segmental glomerulosclerosis (FSGS) • ACE inhibitors and ARBs may also be used in FSGS to decrease proteinuria. • Treatment should focus on controlling blood pressure and blood cholesterol levels, factors that may contribute to kidney scarring.
Nephrotic Syndrome • Nephrotic syndrome is a condition marked by proteinuria; low levels of protein in the blood; swelling, especially around the eyes, feet, and hands; and high cholesterol. • Nephrotic syndrome results from damage to the kidneys' glomeruli
Nephrotic Syndrome • Nephrotic syndrome can occur with many diseases, including the kidney diseases caused by diabetes mellitus, but some causes are unknown. • Prevention of nephrotic syndrome relies on controlling these diseases.
Nephrotic Syndrome • Treatment of nephrotic syndrome focuses on identifying the underlying cause if possible and reducing high cholesterol, blood pressure, and protein in urine through diet, medications, or both. • ACE inhibitors also protect the kidneys by reducing proteinuria.
Nephrotic Syndrome • Nephrotic syndrome may go away once the underlying cause, if known, has been treated. • In children, 80% of cases of nephrotic syndrome are caused by minimal change disease, which can be successfully treated with prednisone.
Nephrotic Syndrome • In adults, most of the time the underlying cause is a kidney disease such as membranous nephropathy or focal segmental glomerulonephritis, and these diseases often persist even with treatment
Diabetic nephropathy • Diabetic nephropathy is the leading cause of glomerular disease and of ESRD in the United States. • Kidney disease is one of several problems caused by elevated levels of blood glucose, the central feature of diabetes. • In addition to scarring the kidney, elevated glucose levels appear to increase the speed of blood flow into the kidney, putting a strain on the filtering glomeruli and raising blood pressure.
Diabetic nephropathy • Diabetic nephropathy usually takes many years to develop. • People with diabetes can slow down damage to their kidneys by controlling their blood glucose through healthy eating with moderate protein intake, physical activity, and medications.
Diabetic nephropathy • blood pressure control- at a level below 130/85 mm Hg • Blood pressure medications – angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) -particularly effective at minimizing kidney damage – frequently prescribed to control blood pressure in patients with diabetes and in patients with many forms of kidney disease
Membranous nephropathy • also called membranous glomerulopathy • the second most common cause of the nephrotic syndrome (proteinuria, edema, high cholesterol) in U. S. adults after diabetic nephropathy
Membranous nephropathy • Diagnosis of membranous nephropathy requires a kidney biopsy, which reveals unusual deposits of immunoglobulin G and complement C 3, substances created by the body's immune system
Membranous nephropathy • 75% of cases are idiopathic • 25% of cases are the result of other diseases like systemic lupus erythematosus, hepatitis B or C infection, or some forms of cancer
Membranous nephropathy • Drug therapies involving penicillamine, gold, or captopril have also been associated with membranous nephropathy • About 20 to 40 % of patients with membranous nephropathy progress, usually over decades, to ESRD, but most patients experience either complete remission or continued symptoms without progressive kidney failure
Membranous nephropathy • ACE inhibitors and ARBs are generally used to reduce proteinuria. • Additional medication to control high blood pressure and edema is frequently required. • Some patients benefit from steroids, but this treatment does not work for everyone. • Additional immunosuppressive medications are helpful for some patients with progressive disease.
Minimal change disease (MCD) • Diagnosis given when a patient has the nephrotic syndrome and the kidney biopsy reveals little or no change to the structure of glomeruli or surrounding tissues when examined by a light microscope. • Tiny drops of a fatty substance called a lipid may be present, but no scarring has taken place within the kidney.
Minimal change disease (MCD) • MCD may occur at any age, but it is most common in childhood. • A small percentage of patients with idiopathic nephrotic syndrome do not respond to steroid therapy.
Minimal change disease (MCD) • Treatment – – low-sodium diet diuretic to control edema steroids to reduce proteinuria ACE inhibitors and ARBs have also been used to reduce proteinuria in patients with steroid-resistant MCD. – These patients may respond to larger doses of steroids, more prolonged use of steroids, or steroids in combination with immunosuppressant drugs, such as chlorambucil, cyclophosphamide, or cyclosporine
RTA • Renal tubular acidosis (RTA) is a disease that occurs when the kidneys fail to excrete acids into the urine, which causes a person's blood to remain too acidic. • Without proper treatment, chronic acidity of the blood leads to growth retardation, kidney stones, bone disease, and progressive renal failure.
Types of RTA • • Type III Type IV
RTA – Type I • Type 1 is also called classic distal RTA. "Distal, " which means distant, refers to the point in the urine-forming tube where the defect occurs. • It is relatively distant from the point where fluid from the blood enters the tiny tube (or tubule) that collects fluid and wastes to form urine.
RTA-Type I • This disorder may be inherited as a primary disorder or may be one symptom of a disease that affects many parts of the body. • Classic distal RTA is a complication of diseases that affect many organ systems (systemic diseases), like the autoimmune disorders Sjögren's syndrome and lupus.
RTA-Type I • Other diseases and conditions associated with distal RTA include: – hyperparathyroidism, a hereditary form of deafness, analgesic nephropathy, rejection of a transplanted kidney, renal medullary cystic disease, obstructive uropathy, and chronic urinary tract infections.
RTA-Type I • A major consequence of classic distal RTA is low blood-potassium. • The level drops if the kidneys excrete potassium into urine instead of returning it to the blood supply. • Since potassium helps regulate nerve and muscle health and heart rate, low levels can cause extreme weakness, cardiac arrhythmias, paralysis, and even death.
RTA-Type I • Untreated distal RTA causes growth retardation in children and progressive renal and bone disease in adults. • Restoring normal growth and preventing kidney stones, another common problem in this disorder, are the major goals of therapy.
RTA-Type I • If acidosis is corrected with sodium bicarbonate or sodium citrate, then low blood-potassium, salt depletion, and calcium leakage into urine will be corrected. • Alkali therapy also helps decrease the development of kidney stones. • Potassium supplements are rarely needed except in infants, since alkali therapy prevents the kidney from excreting potassium into the urine.
• Type 2 is called proximal RTA. The word "proximal, " which means near, indicates that the defect is closer to the point where fluid and wastes from the blood enter the tubule.
RTA- Type II • This form of RTA occurs most frequently in children as part of a disorder called Fanconi's syndrome. • The symptoms of Fanconi's syndrome include high levels of glucose, amino acids, citrate, and phosphate in the urine, as well as vitamin D deficiency and low bloodpotassium.
RTA- Type II • Proximal RTA can also result from inherited disorders that disrupt the body's normal breakdown and use of nutrients. – Examples include the rare disease cystinosis (in which cystine crystals are deposited in bones and other tissues), hereditary fructose intolerance, and Wilson's disease.
RTA- Type II • Proximal RTA also occurs in patients treated with ifosfamide, a drug used in chemotherapy. • A few older drugs--such as acetazolamide or outdated tetracycline--can also cause proximal RTA. • In adults, proximal RTA may complicate diseases like multiple myeloma, or it may occur in people who experience chronic rejection of a transplanted kidney.
RTA- Type II • When possible, identifying and correcting the underlying causes are important steps in treating the acquired forms of proximal RTA. • The diagnosis is based on the chemical analysis of blood and urine samples. • Children with this disorder would likely receive large doses of oral alkali, such as sodium bicarbonate or potassium citrate, to treat acidosis and prevent bone disorders, kidney stones, and growth failure.
RTA- Type II • Correcting acidosis and low potassium levels restores normal growth patterns, allowing bone to mature while preventing further renal disease. • Vitamin D supplements may also be needed to help prevent bone problems.
RTA- Type III • Type 3 is rarely used as a classification today because it is now thought to be a combination of type 1 and type 2.
RTA- Type IV • Type 4 RTA is caused by another defect in the distal tubule, but it is different from classic distal RTA and proximal RTA because it results in high levels of potassium in the blood instead of low levels. • Either low potassium (hypokalemia) or high potassium (hyperkalemia) can be a problem because potassium is important in regulating heart rate.
RTA- Type IV • It occurs when blood levels of the hormone aldosterone are low or when the kidneys do not respond to it. • Aldosterone directs the kidneys to regulate the levels of sodium, potassium, and chloride in the blood. • Type 4 RTA is distinguished by a high blood-potassium level.
RTA- Type IV • Hyperkalemic distal RTA may result from sickle cell disease, urinary tract obstruction, lupus, amyloidosis, or transplantation.
RTA- Type IV • Aldosterone's action may be impeded by drugs, including – diuretics such as spironolactone or eplerenone – ACE inhibitors and angiotensin receptor blockers (ARBs) – trimethoprim – heparin – pentamidine – NSAIDs – some immunosuppressive drugs
RTA- Type IV • To treat type 4 RTA successfully, patients may require alkaline agents to correct acidosis as well as medication to lower the potassium in their blood. • If treated early, most people with RTA will not develop permanent kidney failure. • Therefore, the goal is early recognition and adequate therapy, which will need to be maintained and monitored throughout the patient's lifetime.
Amyloidosis and Kidney Disease • In recent years, researchers have discovered that different kinds of proteins can form amyloid deposits and have identified several types of amyloidosis. • Two of these types are closely related to kidney disease. – primary amyloidosis, abnormal protein production occurs as a first step and can lead to kidney disease – Dialysis-related amyloidosis (DRA), on the other hand, is a result of kidney disease
Amyloidosis and Kidney Disease • One common sign of kidney amyloidosis is the presence of abnormally high levels of protein in the urine, a condition known as proteinuria.
Amyloidosis and Kidney Disease • No effective treatment has been found to reverse the effects of amyloidosis. • Combination drug therapy with melphalan (cancer drug) and prednisone may improve organ function and survival rates by interrupting the growth of the abnormal cells that produce amyloid protein.
Inherited and Congenital Kidney Diseases • Some kidney diseases result from hereditary factors. • Polycystic kidney disease (PKD), for example, is a genetic disorder in which many cysts grow in the kidneys. • PKD cysts can slowly replace much of the mass of the kidneys, reducing kidney function and leading to kidney failure.
Inherited and Congenital Kidney Diseases • Some kidney problems may show up when a child is still developing in the womb. – Examples include autosomal recessive PKD, a rare form of PKD, and other developmental problems that interfere with the normal formation of the nephrons. • The signs of kidney disease in children vary. A child may grow unusually slowly, may vomit often, or may have back or side pain. • Some kidney diseases may be "silent" for months or even years.
Inherited and Congenital Kidney Diseases • The first sign of a kidney problem may be high blood pressure, anemia, or blood or protein in the child's urine. • Further tests include additional blood/ urine tests, radiology studies or biopsy
Inherited and Congenital Kidney Diseases • Some hereditary kidney diseases may not be detected until adulthood. • The most common form of PKD was once called "adult PKD" because the symptoms of high blood pressure and renal failure usually do not occur until patients are in their twenties or thirties. • With advances in diagnostic imaging technology, cysts in children and adolescents are usually detected before any symptoms appear.
How do kidneys fail? • Many factors that influence the speed of kidney failure are not completely understood. • Researchers are still studying how protein in the diet and cholesterol levels in the blood affect kidney function.
Acute Renal Failure • Acute renal failure is worsening of renal failure over hours to days • Acute renal failure results in the retention of nitrogenous wastes (urea nitrogen) and creatinine in the blood - called azotemia
Acute Renal Failure • Some kidney problems happen quickly, like an accident that injures the kidneys. – Losing a lot of blood can cause sudden kidney failure. – Some drugs or poisons can make the kidneys stop working. • These sudden drops in kidney function are called acute renal failure (ARF). • ARF may lead to permanent loss of kidney function. But if the kidneys are not seriously damaged, acute renal failure may be reversed.
Chronic Renal Failure • Most kidney problems, however, happen slowly. “Silent" kidney disease may go on for years. • Gradual loss of kidney function (months to years) is called chronic kidney disease (CKD) or chronic renal insufficiency/failure (CRF).
Chronic Renal Failure • Some forms of CRF can be controlled or slowed down – For example, diabetic nephropathy can be delayed by tightly controlling blood glucose levels and using ACE inhibitors and ARBs to reduce proteinuria and control blood pressure.
Chronic Renal Failure • CRF cannot be cured. • Partial loss of renal function means that some portion of the patient's nephrons have been scarred, and scarred nephrons cannot be repaired. • In most cases, CRF leads to ESRD.
Chronic or Acute ? • Differentiating between the two types of renal disease (Acute or Chronic) is important for diagnosis, treatment and outcome.
Chronic or Acute ? • Oliguria is unusual in Chronic renal insufficiency • Anemia (from low renal erythropoietin production) is rare in the initial period of acute renal failure • Small kidneys are most consistent with chronic renal failure • Normal - Large kidneys are seen in both
ESRD • Complete and irreversible kidney failure is called end-stage renal disease, or ESRD. • If the kidneys stop working completely, the body fills with extra water and waste products. This condition is called uremia.
Uremia • Untreated uremia may lead to seizures or coma and will ultimately result in death. • If the kidneys stop working completely, dialysis or kidney transplant are the only options
Dialysis • There are two major forms of dialysis – Hemodialysis – Peritoneal dialysis
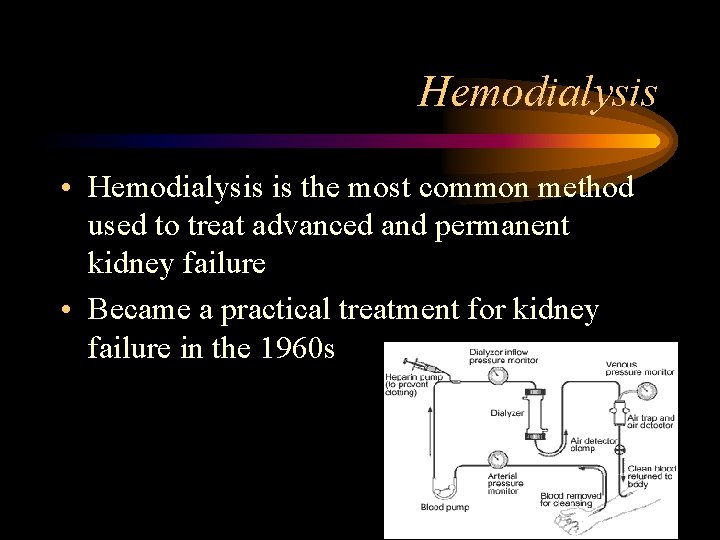
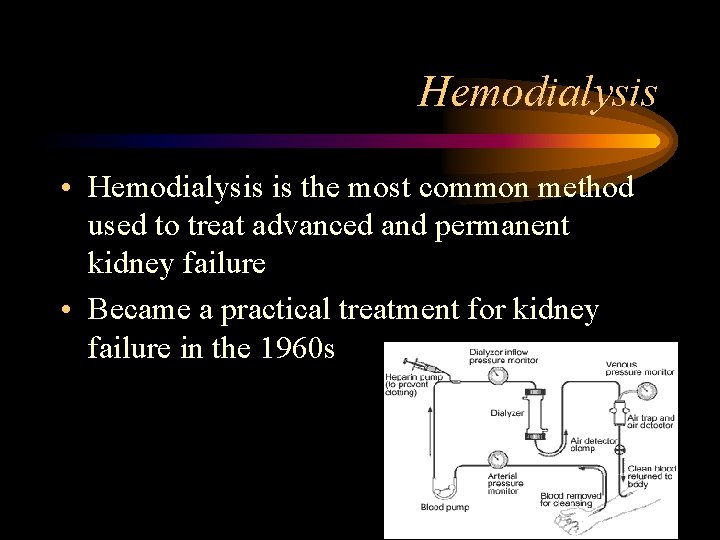
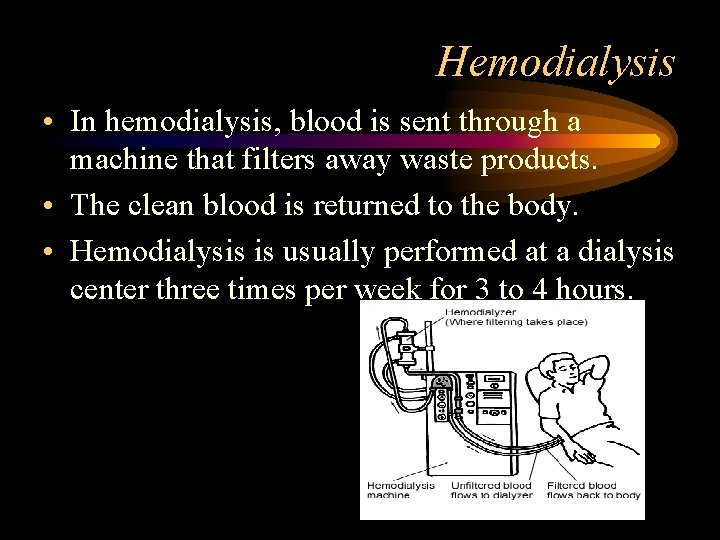
Hemodialysis • Hemodialysis is the most common method used to treat advanced and permanent kidney failure • Became a practical treatment for kidney failure in the 1960 s
Peritoneal Dialysis • In the 1980 s, PD first became a practical and widespread treatment for kidney failure • Types of PD – Continuous Ambulatory Peritoneal Dialysis (CAPD) – Continuous Cycler-Assisted Peritoneal Dialysis (CCPD) – Nocturnal Intermittent Peritoneal Dialysis (NIPD)
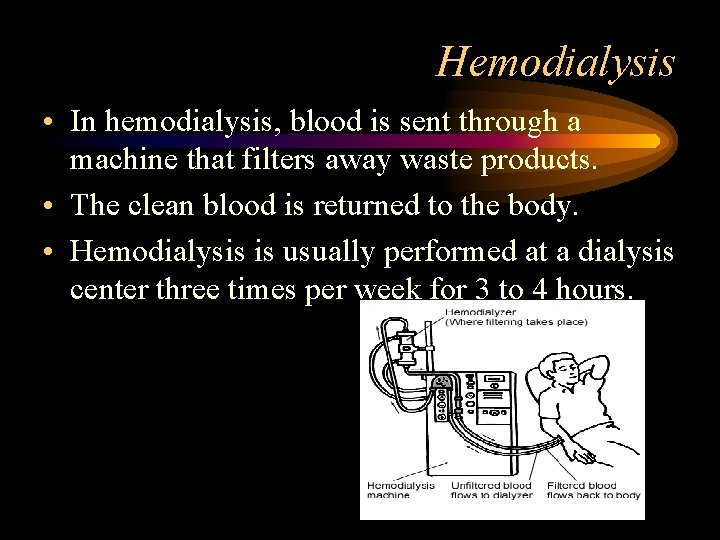
Hemodialysis • In hemodialysis, blood is sent through a machine that filters away waste products. • The clean blood is returned to the body. • Hemodialysis is usually performed at a dialysis center three times per week for 3 to 4 hours.
Peritoneal Dialysis • In peritoneal dialysis, fluid is put into the abdomen. This fluid, called dialysate, captures the waste products from the blood. • After a few hours, the dialysate containing the body's wastes is drained away. • Then, a fresh bag of dialysate is dripped into the abdomen. • Patients can perform peritoneal dialysis themselves. • Patients using continuous ambulatory peritoneal dialysis (CAPD), the most common form of peritoneal dialysis, change dialysate four times a day

Questions
 Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Victor politi
Victor politi Dr victor politi
Dr victor politi Victor politi
Victor politi Victor politi
Victor politi Renal corpuscle
Renal corpuscle Rachel politi
Rachel politi Loading dose formula
Loading dose formula Renal disease
Renal disease Communicable disease and non communicable disease
Communicable disease and non communicable disease Torrance memorial outpatient lab
Torrance memorial outpatient lab California medical license application
California medical license application Gbmc infoweb
Gbmc infoweb Difference between medical report and medical certificate
Difference between medical report and medical certificate Cartersville medical center medical records
Cartersville medical center medical records Function of basement membrane
Function of basement membrane Rifle akin
Rifle akin Capillary filtration coefficient
Capillary filtration coefficient Function of renal cortex
Function of renal cortex What is a renal lobule
What is a renal lobule Ifundibulo
Ifundibulo Clique nephretique
Clique nephretique Earthy look in chronic renal failure
Earthy look in chronic renal failure Bladder apex
Bladder apex Renal system
Renal system Renal vein
Renal vein Ajkd atlas of renal pathology
Ajkd atlas of renal pathology Macula densa
Macula densa Why does efferent arteriole constriction increased gfr
Why does efferent arteriole constriction increased gfr Barostim
Barostim Renal
Renal Renal cyst
Renal cyst Tubular secretion
Tubular secretion Renal dysplasia
Renal dysplasia Renal columns
Renal columns Tubular secretion in nephron
Tubular secretion in nephron Cva tenderness
Cva tenderness Ren nephros
Ren nephros Denervacion simpatica renal
Denervacion simpatica renal Renal cortex
Renal cortex Farmaco
Farmaco Urinalysis
Urinalysis Female reproductive system
Female reproductive system Site:slidetodoc.com
Site:slidetodoc.com Arteria renal
Arteria renal Renal failure
Renal failure Renal physiology
Renal physiology Renal pyramid
Renal pyramid Renal reabsorption
Renal reabsorption Nefrone iuxtamidollare
Nefrone iuxtamidollare Renal arter üfürümü nerden dinlenir
Renal arter üfürümü nerden dinlenir Renal travma sınıflaması
Renal travma sınıflaması Renal hücreli karsinom
Renal hücreli karsinom Vancomycin renal dose
Vancomycin renal dose Aorta zone
Aorta zone Juxtaglomerular apparatus
Juxtaglomerular apparatus Pelve renal
Pelve renal Renal angle
Renal angle Girft renal
Girft renal Prerenal renal ayrımı
Prerenal renal ayrımı Oncocitoma renal
Oncocitoma renal Renal angle
Renal angle Figure 15-4 is a diagram of a nephron
Figure 15-4 is a diagram of a nephron Arteria renal
Arteria renal Ceftriaxone in ckd
Ceftriaxone in ckd Renal papilla
Renal papilla Flujo plasmatico renal efectivo
Flujo plasmatico renal efectivo Percusion renal
Percusion renal Renal function test
Renal function test Trigone
Trigone Pah clearance
Pah clearance Renal tubule
Renal tubule Azotemia
Azotemia Cateterismo
Cateterismo Coarse granular cast in urine
Coarse granular cast in urine Renal dysplasia
Renal dysplasia Outer region of the kidney
Outer region of the kidney Renal
Renal Ira prerrenal
Ira prerrenal Osmoregulation
Osmoregulation Datos objetivos y subjetivos de enfermería
Datos objetivos y subjetivos de enfermería Vasos sanguineos
Vasos sanguineos Solvent drag definition
Solvent drag definition Renal ven trombozu triad
Renal ven trombozu triad Bowmans capsule
Bowmans capsule Insuficiencia renal aguda
Insuficiencia renal aguda Principais veias e artérias do abdome
Principais veias e artérias do abdome Carcinoma renal de células claras fuhrman
Carcinoma renal de células claras fuhrman Pleximetro y plexor
Pleximetro y plexor Aeiou rrt
Aeiou rrt Ectopic kidney
Ectopic kidney Lamivudine renal dose
Lamivudine renal dose Enfermedad renal cronica definicion
Enfermedad renal cronica definicion Bilan renal
Bilan renal Renal portal system
Renal portal system Inside a kidney the ureter expands as a renal pyramid
Inside a kidney the ureter expands as a renal pyramid Neuropatia periférica
Neuropatia periférica Anna neary
Anna neary Sistema renal
Sistema renal Pielonefrite
Pielonefrite Cytorrhaphy
Cytorrhaphy Wholey wire cardiac
Wholey wire cardiac Ureter diameter
Ureter diameter Punctele ureterale
Punctele ureterale Why does efferent arteriole constriction increased gfr
Why does efferent arteriole constriction increased gfr Ecuacion de henderson hasselbalch
Ecuacion de henderson hasselbalch Proximal convoluted tubule histology
Proximal convoluted tubule histology Difference between renal and cardiac edema
Difference between renal and cardiac edema Cortical nephron
Cortical nephron Renal pelvis
Renal pelvis Cociente albumina creatinina en orina valores normales
Cociente albumina creatinina en orina valores normales Nervos renais
Nervos renais Renal physiology
Renal physiology Dapar
Dapar Causes of secondary hyperparathyroidism
Causes of secondary hyperparathyroidism Epitelial
Epitelial Disequilibration syndrome
Disequilibration syndrome Renal corpuscle
Renal corpuscle Lung tissue
Lung tissue Signo de puño percusion renal
Signo de puño percusion renal Syndrome hepato renal
Syndrome hepato renal Lec renal
Lec renal Renal infarct
Renal infarct Renal medulla
Renal medulla Palidez terrosa renal
Palidez terrosa renal Apex of renal pyramid
Apex of renal pyramid Pearson education, inc
Pearson education, inc Two kidneys
Two kidneys Maniobra bimanual de guyon
Maniobra bimanual de guyon Renal papilla
Renal papilla Normal abg
Normal abg Insuficiencia renal aguda
Insuficiencia renal aguda Farmacocinetica
Farmacocinetica Akin clasificacion
Akin clasificacion Respiratory alkalosis renal compensation
Respiratory alkalosis renal compensation Renal portal system
Renal portal system Fasia renal
Fasia renal Vasa recta
Vasa recta Bladder infection
Bladder infection Structure of posterior pituitary gland
Structure of posterior pituitary gland Renal blood flow
Renal blood flow Ajkd atlas of renal pathology
Ajkd atlas of renal pathology Poliquistosis renal
Poliquistosis renal Pathophysiology of kidney stones
Pathophysiology of kidney stones Tipos de diabetes
Tipos de diabetes Renal vein thrombosis pathophysiology
Renal vein thrombosis pathophysiology Older adults
Older adults Renal halo sign
Renal halo sign Where are the kidneys located in the body
Where are the kidneys located in the body Renal
Renal Minor and major calyces
Minor and major calyces