Renal Physiology College of Dentistry 2017 2018 The
![• The kidneys have several functions including the following: • [1] Kidneys regulate • The kidneys have several functions including the following: • [1] Kidneys regulate](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-2.jpg)
![Anatomy and function of the kidney The kidney consists of: [A] Nephron. [B] Blood Anatomy and function of the kidney The kidney consists of: [A] Nephron. [B] Blood](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-11.jpg)
![• [3] Loops of Henle: The nephrons with their glomeruli located in the • [3] Loops of Henle: The nephrons with their glomeruli located in the](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-12.jpg)
![• [4] Distal convoluted tubule: They lie in the renal cortex. • [5] • [4] Distal convoluted tubule: They lie in the renal cortex. • [5]](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-15.jpg)
![• [C] Nerve supply: The kidney has a rich adrenergic sympathetic nerve supply • [C] Nerve supply: The kidney has a rich adrenergic sympathetic nerve supply](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-16.jpg)



- Slides: 34
Renal Physiology College of Dentistry 2017 -2018
![The kidneys have several functions including the following 1 Kidneys regulate • The kidneys have several functions including the following: • [1] Kidneys regulate](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-2.jpg)
• The kidneys have several functions including the following: • [1] Kidneys regulate water and electrolytes balance • [2] Kidneys responsible for excretion of metabolic waste products like urea • [3] Kidneys play essential role in regulation of arterial • [4] Kidneys contribute to acid-base regulation • [5] Kidneys responsible for regulation of erythrocyte production from the bone marrow • [6] Kidneys regulate 1, 25 - dihydroxy vit D 3 production which is essential in regulation of Ca and phosphate.
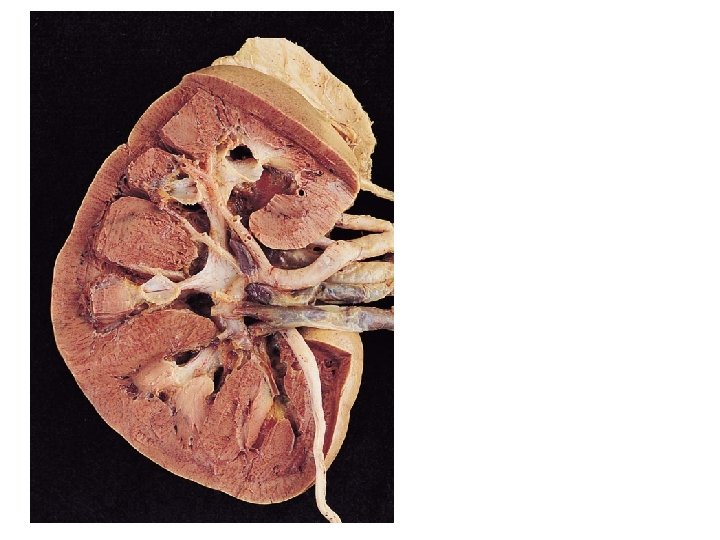
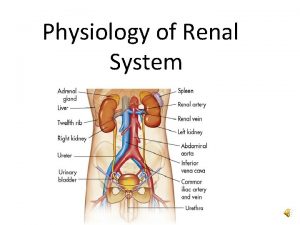
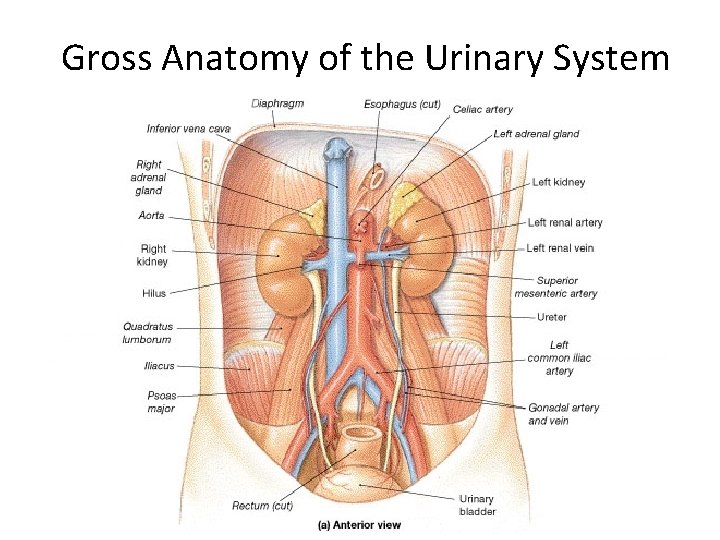
Urinary System
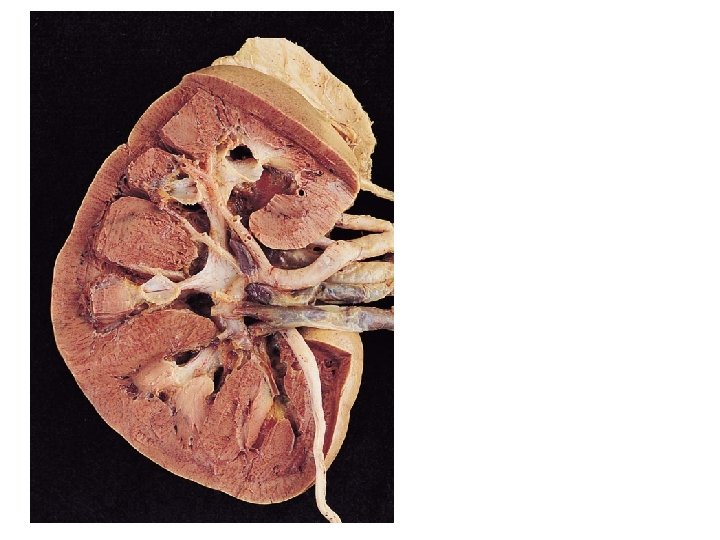
Gross Anatomy of the Urinary System
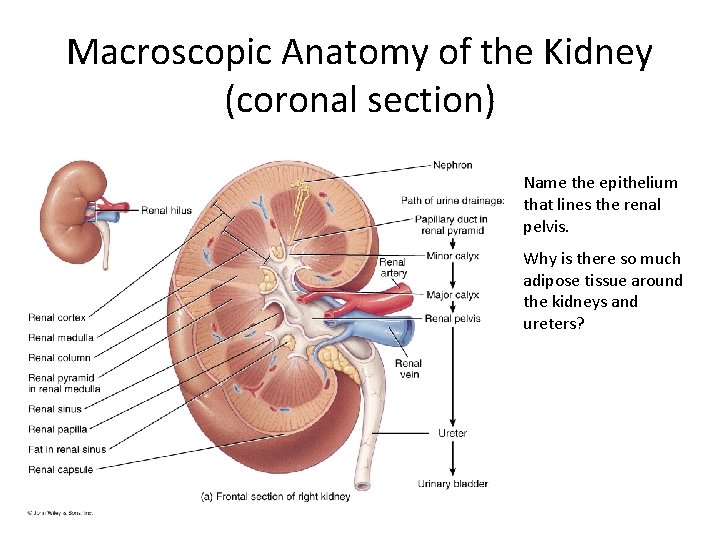
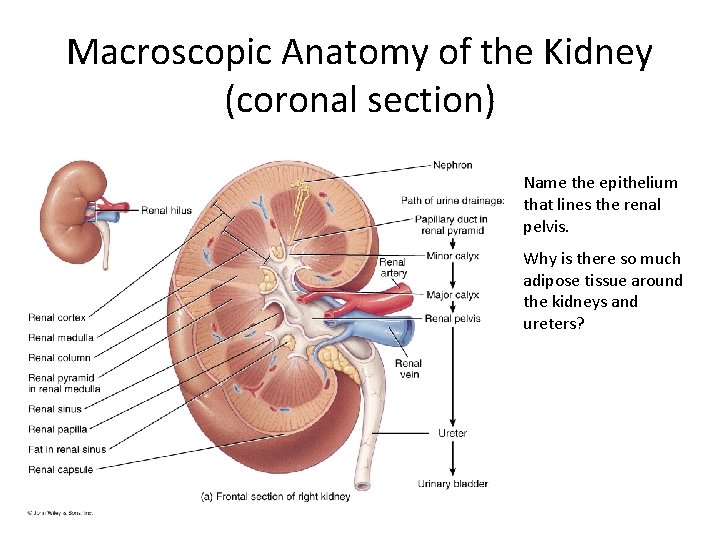
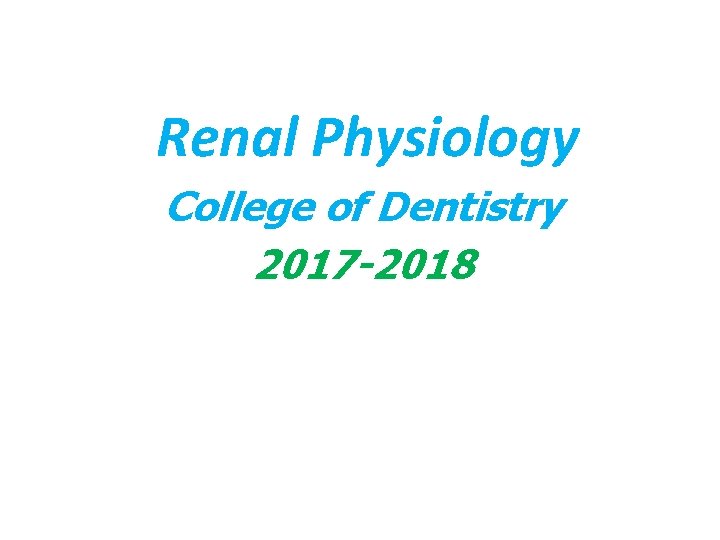
Macroscopic Anatomy of the Kidney (coronal section) Name the epithelium that lines the renal pelvis. Why is there so much adipose tissue around the kidneys and ureters?
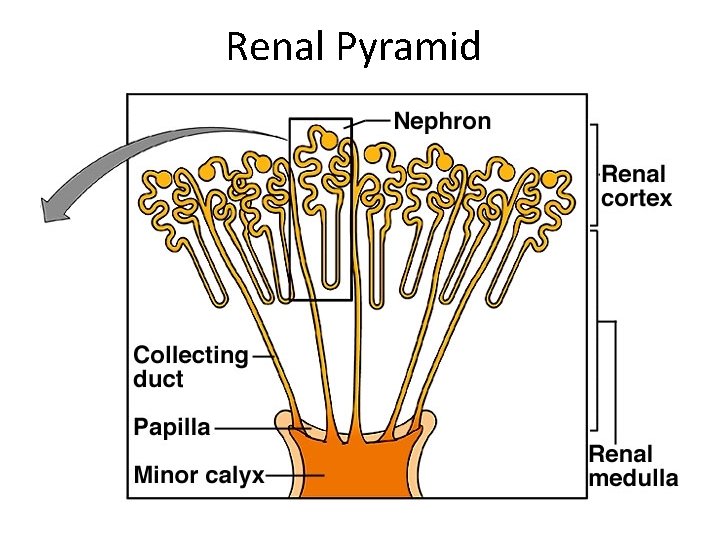
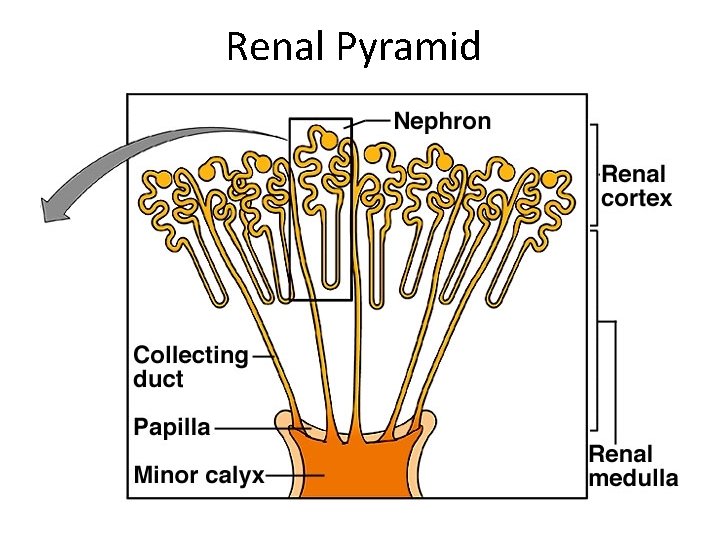
Renal Pyramid
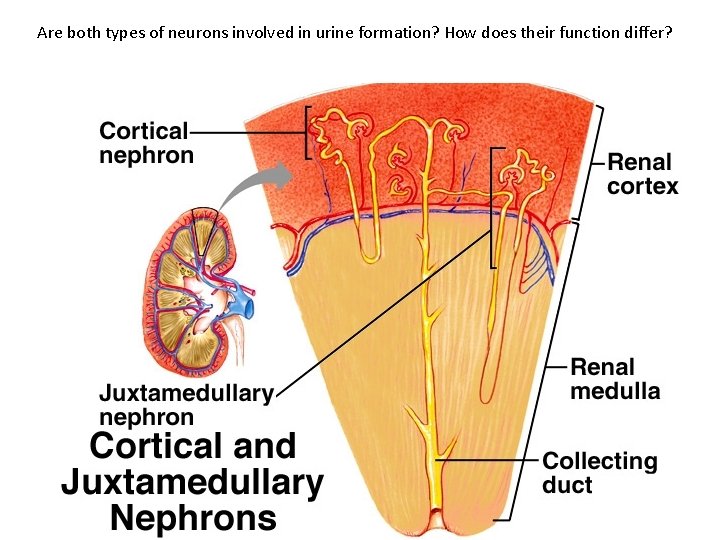
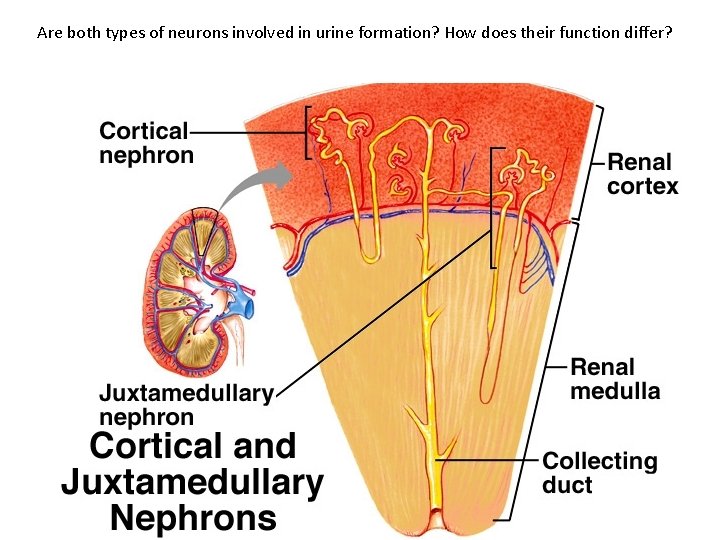
Are both types of neurons involved in urine formation? How does their function differ?
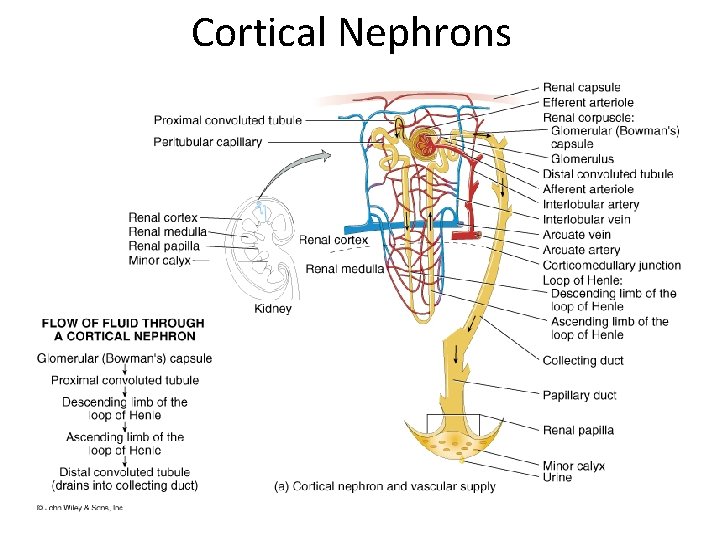
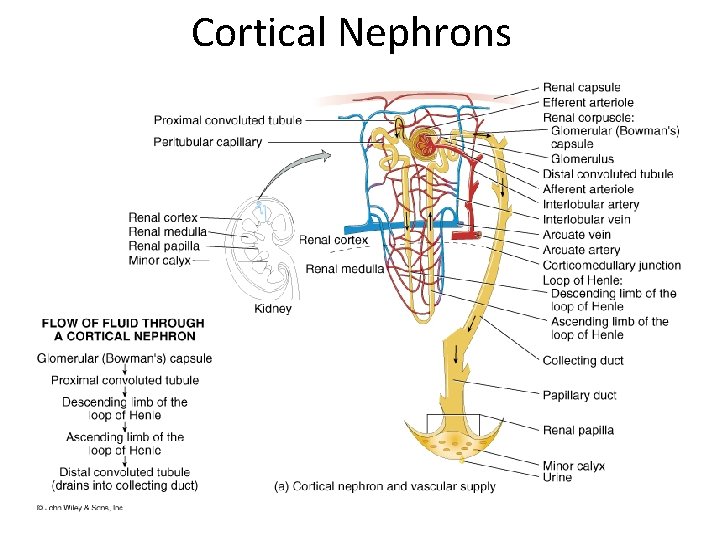
Cortical Nephrons
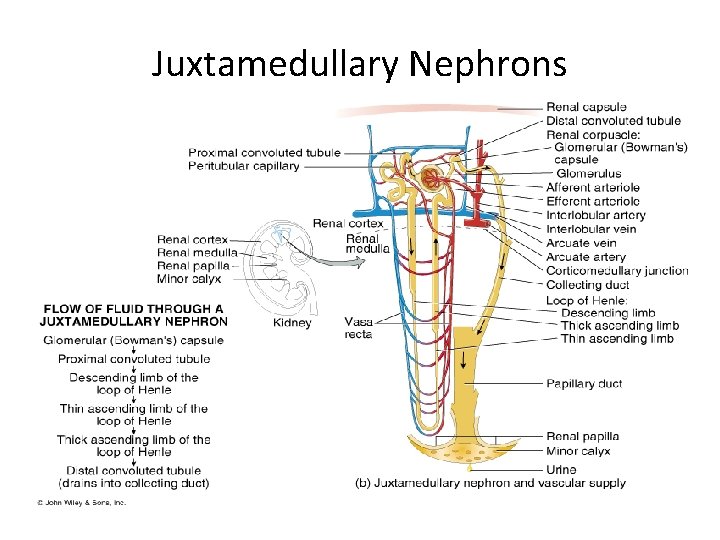
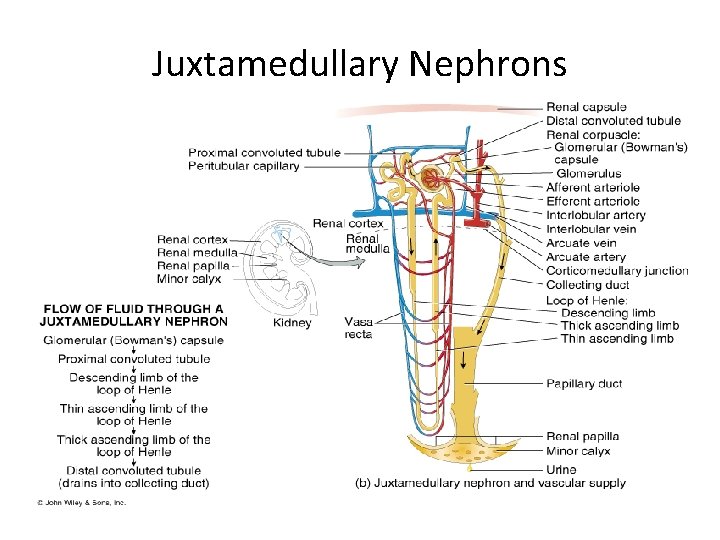
Juxtamedullary Nephrons
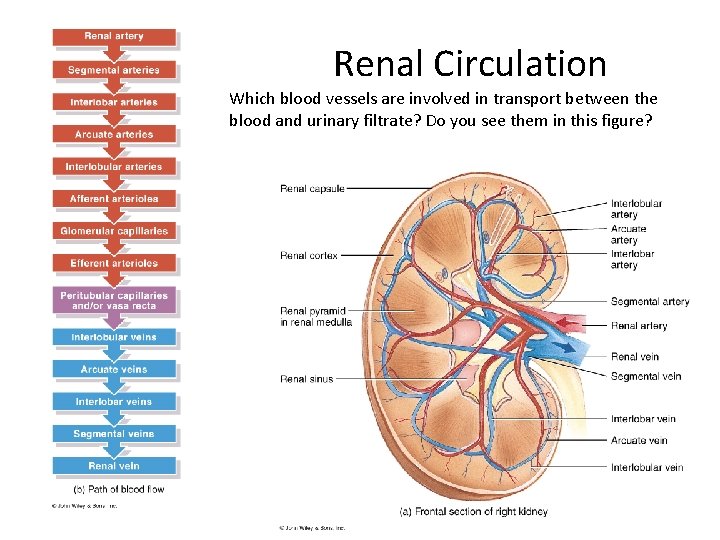
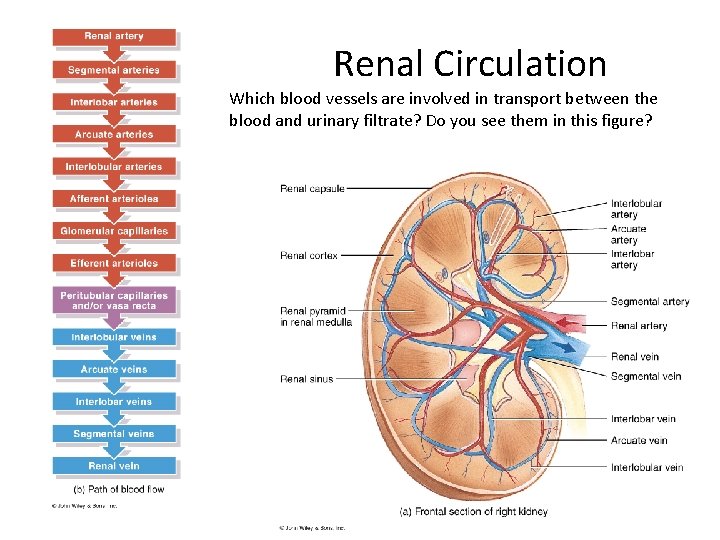
Renal Circulation Which blood vessels are involved in transport between the blood and urinary filtrate? Do you see them in this figure?
![Anatomy and function of the kidney The kidney consists of A Nephron B Blood Anatomy and function of the kidney The kidney consists of: [A] Nephron. [B] Blood](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-11.jpg)
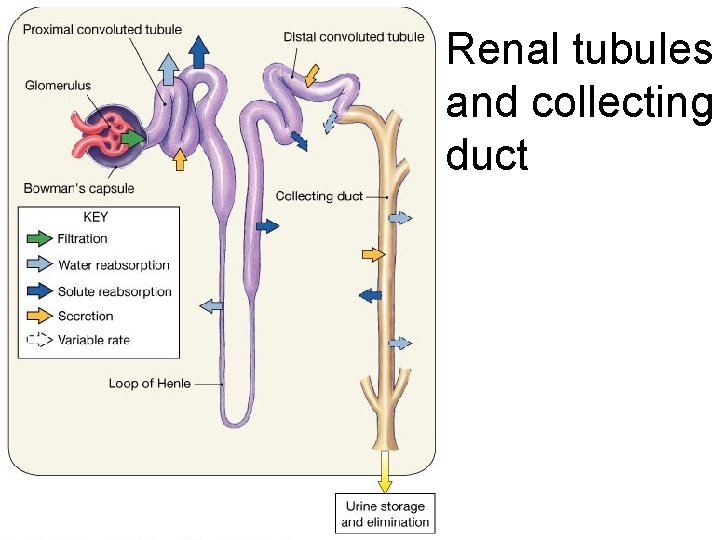
Anatomy and function of the kidney The kidney consists of: [A] Nephron. [B] Blood vessels. [C] Nerves (A) Nephron: It is the basic functional unit of the kidney and capable of forming urine by itself. There about 1 million nephrons in each kidney in human. [1] Bowman`s capsule: It is the invaginated blind end of the tubule that encased the glomerulus The membrane of the glomerular capillaries is called the glomerular membrane. [2] Proximal convoluted tubules: Reabsorption in the proximal tubule is of the filtered Na and water, almost all the filtered glucose, amino acids, organic acids, and small amount of protein which is present, as well as much of the K, Ca, phosphate and urea are reabsorbed in the proximal tubule.
![3 Loops of Henle The nephrons with their glomeruli located in the • [3] Loops of Henle: The nephrons with their glomeruli located in the](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-12.jpg)
• [3] Loops of Henle: The nephrons with their glomeruli located in the outer portion of the renal cortex have short loops of Henle (cortical nephrons, 70%), where as those with glomeruli in the juxtamedullary region of the cortex (juxtamedullary nephrons, 30%) have long loop extending down into medullary pyramids.
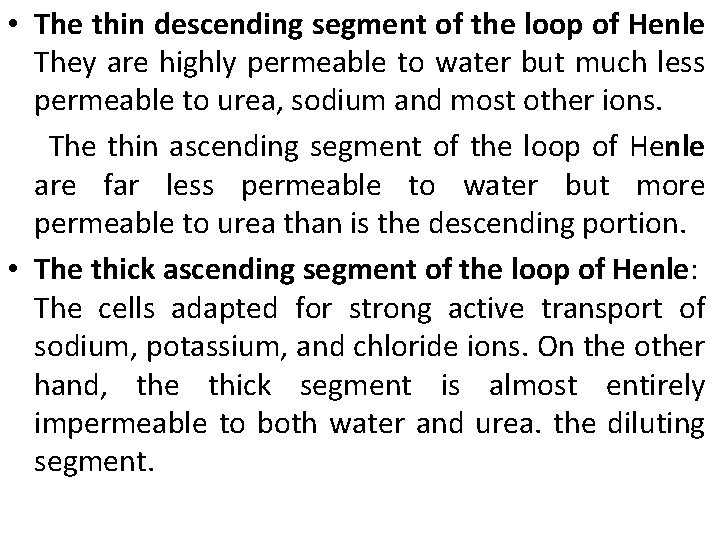
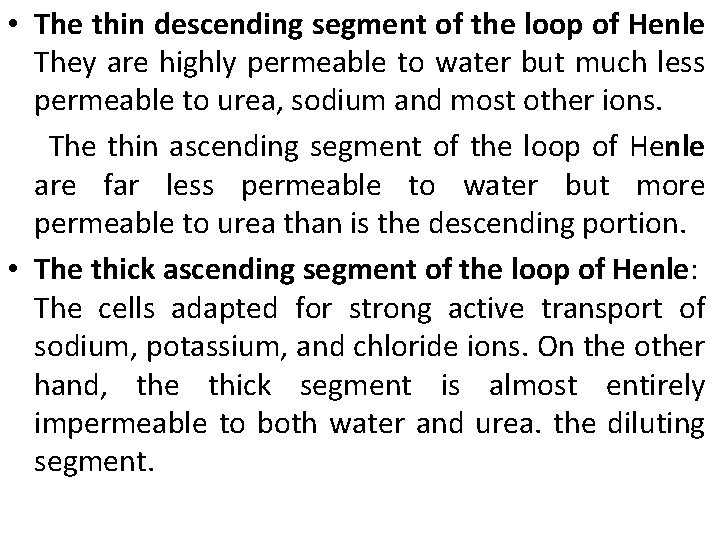
• The thin descending segment of the loop of Henle They are highly permeable to water but much less permeable to urea, sodium and most other ions. The thin ascending segment of the loop of Henle are far less permeable to water but more permeable to urea than is the descending portion. • The thick ascending segment of the loop of Henle: The cells adapted for strong active transport of sodium, potassium, and chloride ions. On the other hand, the thick segment is almost entirely impermeable to both water and urea. the diluting segment.
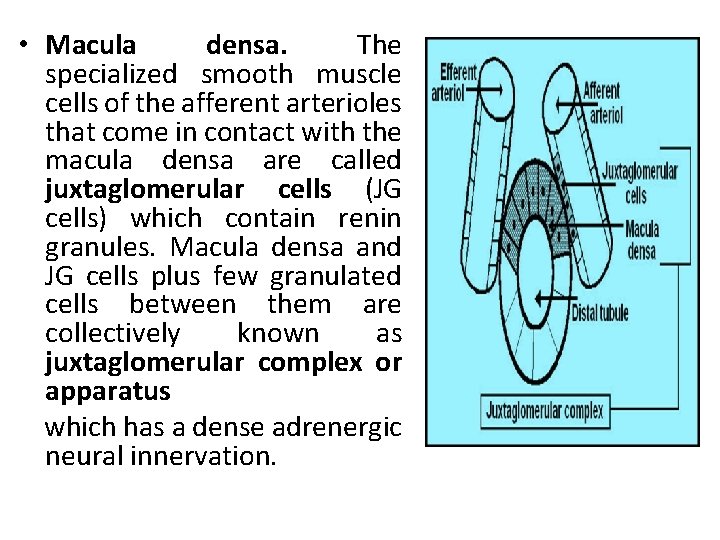
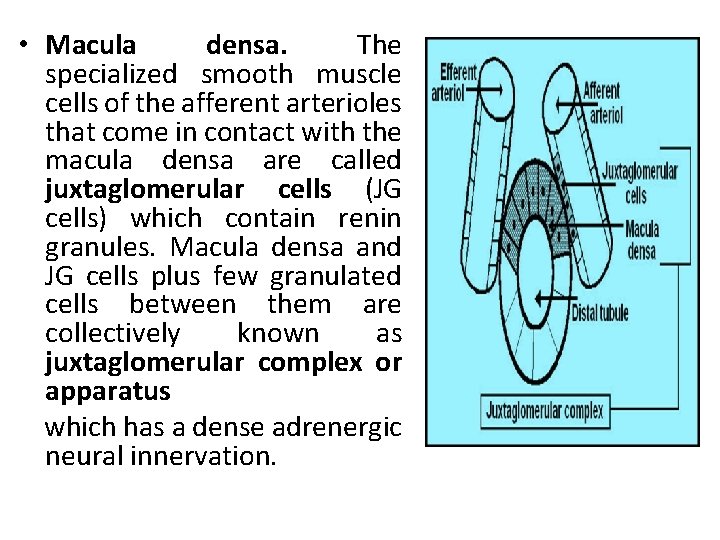
• Macula densa. The specialized smooth muscle cells of the afferent arterioles that come in contact with the macula densa are called juxtaglomerular cells (JG cells) which contain renin granules. Macula densa and JG cells plus few granulated cells between them are collectively known as juxtaglomerular complex or apparatus which has a dense adrenergic neural innervation.
![4 Distal convoluted tubule They lie in the renal cortex 5 • [4] Distal convoluted tubule: They lie in the renal cortex. • [5]](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-15.jpg)
• [4] Distal convoluted tubule: They lie in the renal cortex. • [5] Collecting tubules and ducts: • Its permeability to water is under the control of ADH similar to the cortical collecting duct. • It is permeable to urea (unlike the cortical collecting duct). • It is capable of secreting H ions against concentration gradient.
![C Nerve supply The kidney has a rich adrenergic sympathetic nerve supply • [C] Nerve supply: The kidney has a rich adrenergic sympathetic nerve supply](https://slidetodoc.com/presentation_image/77b5ddb84ea10bfae530a38cc27e2732/image-16.jpg)
• [C] Nerve supply: The kidney has a rich adrenergic sympathetic nerve supply distributed to the: • [A] Vascular smooth muscle to cause vasoconstriction. • [B] Juxtaglomerular cells to cause renin secretion. • [C] Tubular cells to stimulate Na and water reabsorption.
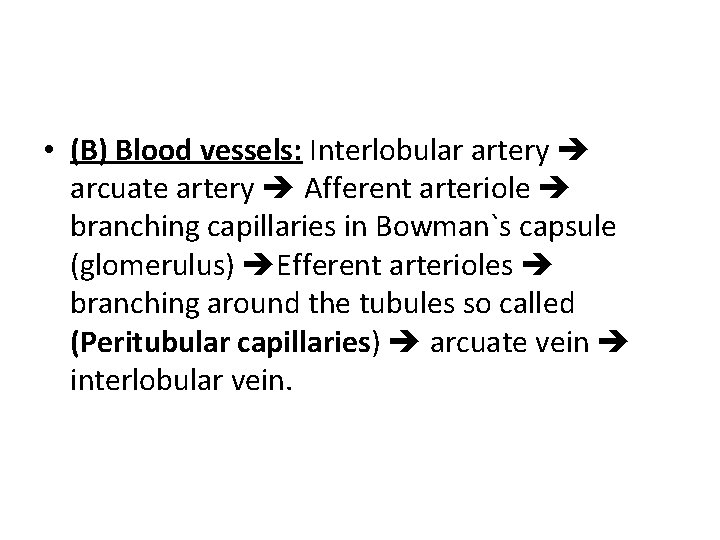
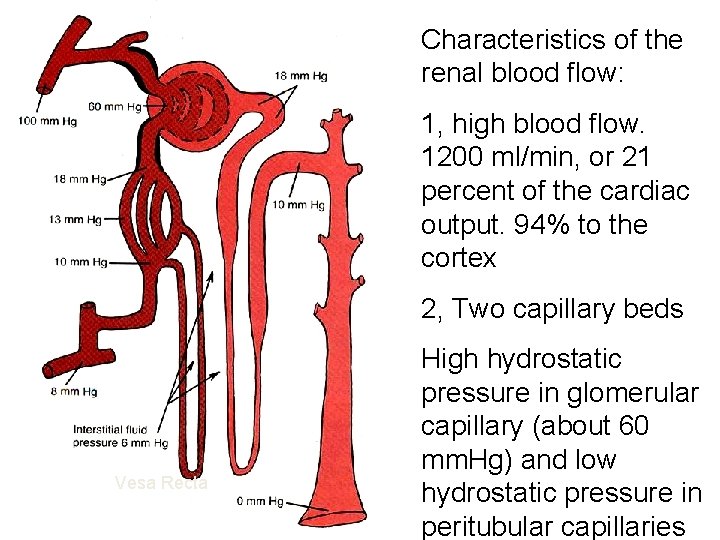
• (B) Blood vessels: Interlobular artery arcuate artery Afferent arteriole branching capillaries in Bowman`s capsule (glomerulus) Efferent arterioles branching around the tubules so called (Peritubular capillaries) arcuate vein interlobular vein.
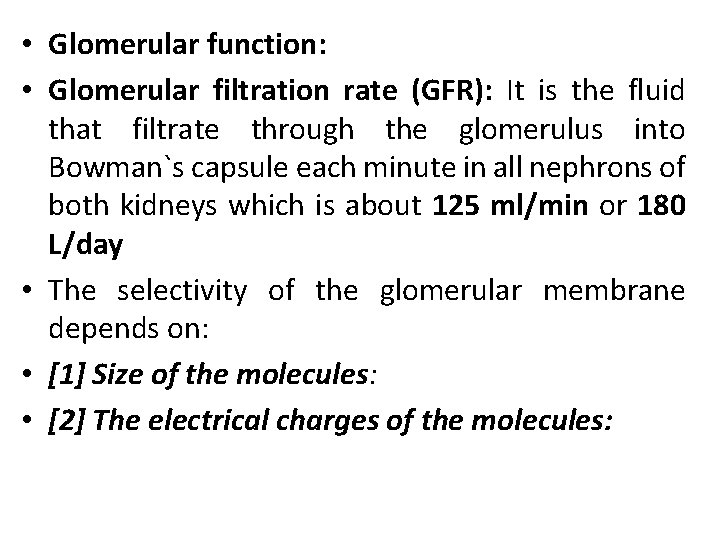
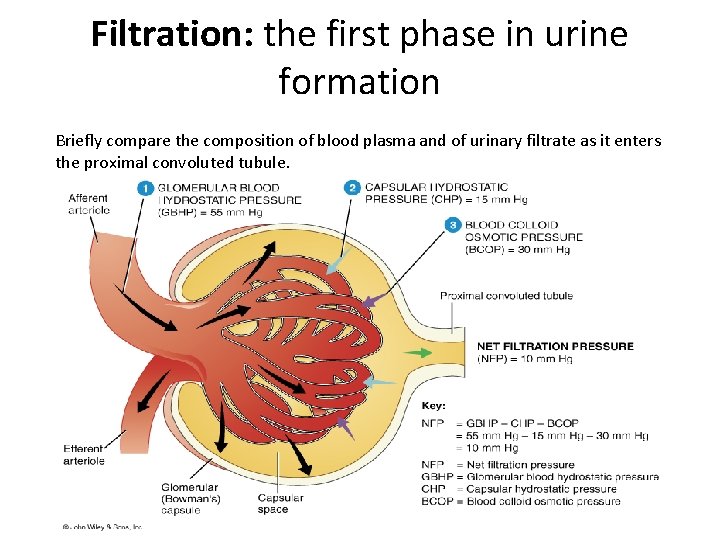
• Glomerular function: • Glomerular filtration rate (GFR): It is the fluid that filtrate through the glomerulus into Bowman`s capsule each minute in all nephrons of both kidneys which is about 125 ml/min or 180 L/day • The selectivity of the glomerular membrane depends on: • [1] Size of the molecules: • [2] The electrical charges of the molecules:
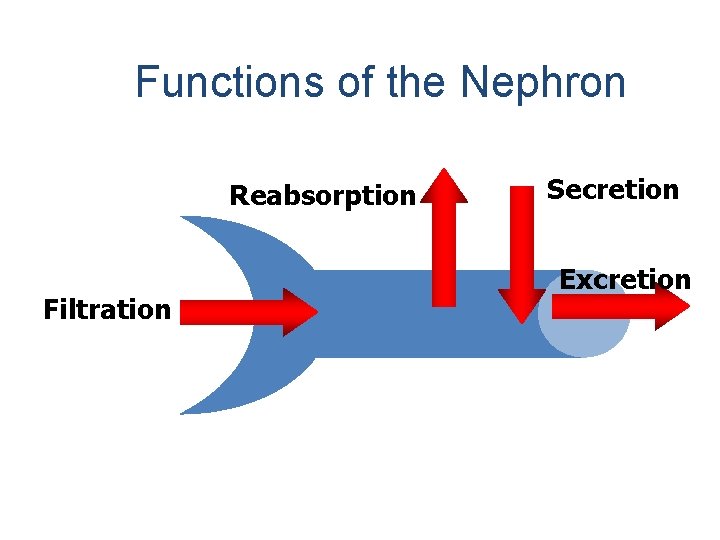
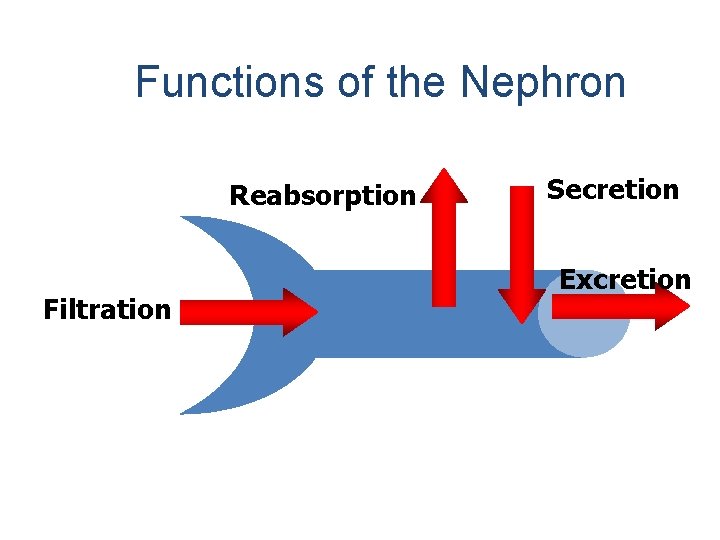
Functions of the Nephron Reabsorption Filtration Secretion Excretion
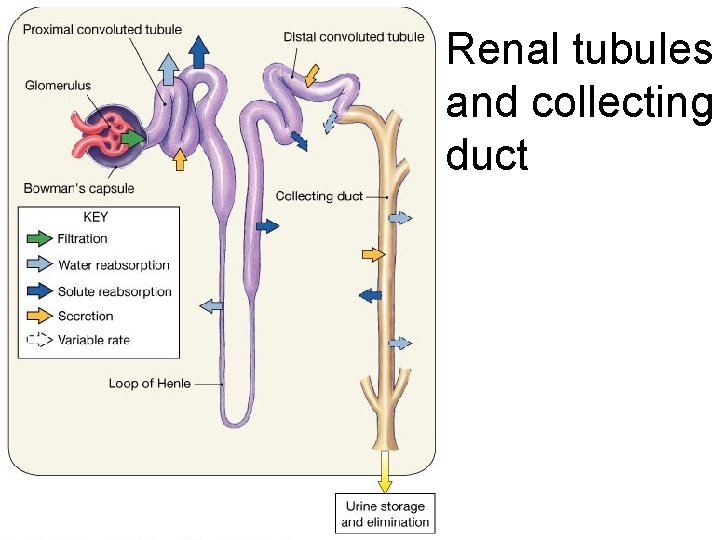
Renal tubules and collecting duct
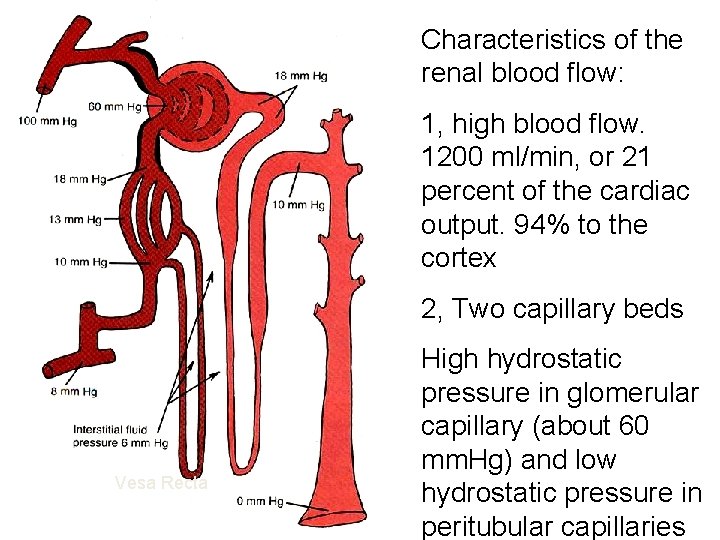
Characteristics of the renal blood flow: 1, high blood flow. 1200 ml/min, or 21 percent of the cardiac output. 94% to the cortex 2, Two capillary beds Vesa Recta High hydrostatic pressure in glomerular capillary (about 60 mm. Hg) and low hydrostatic pressure in peritubular capillaries
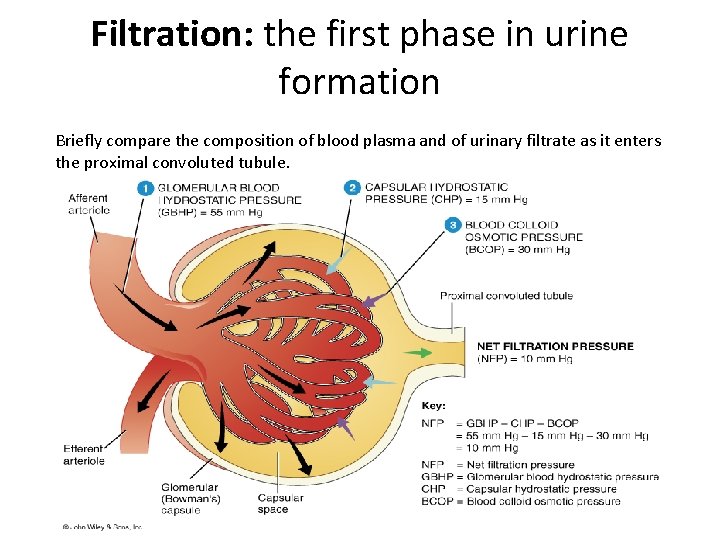
Filtration: the first phase in urine formation Briefly compare the composition of blood plasma and of urinary filtrate as it enters the proximal convoluted tubule.
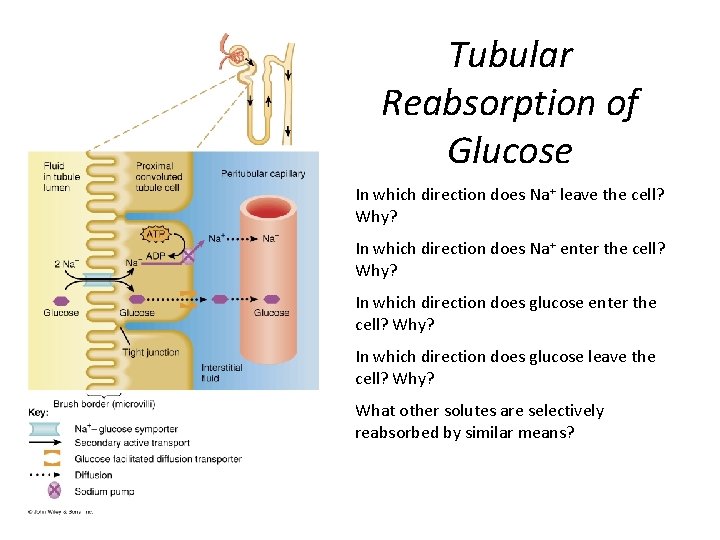
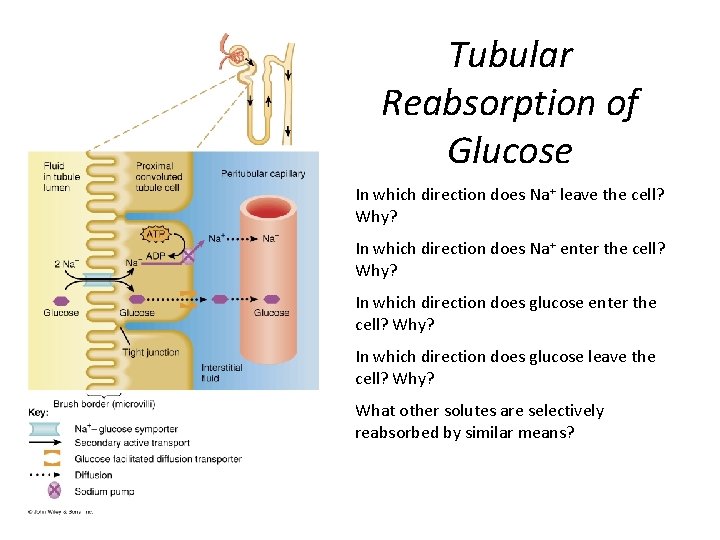
Tubular Reabsorption of Glucose In which direction does Na+ leave the cell? Why? In which direction does Na+ enter the cell? Why? In which direction does glucose enter the cell? Why? In which direction does glucose leave the cell? Why? What other solutes are selectively reabsorbed by similar means?
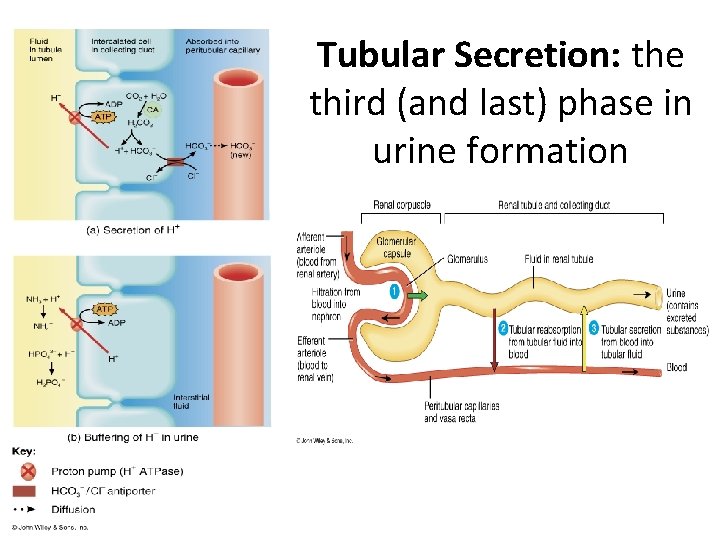
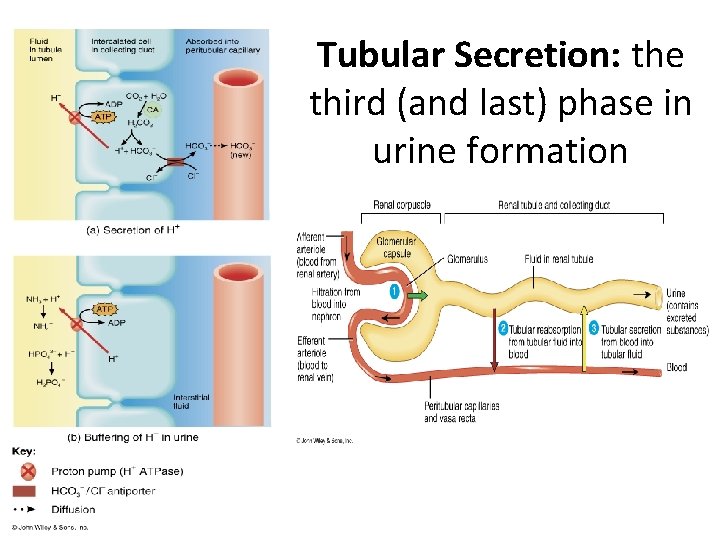
Tubular Secretion: the third (and last) phase in urine formation
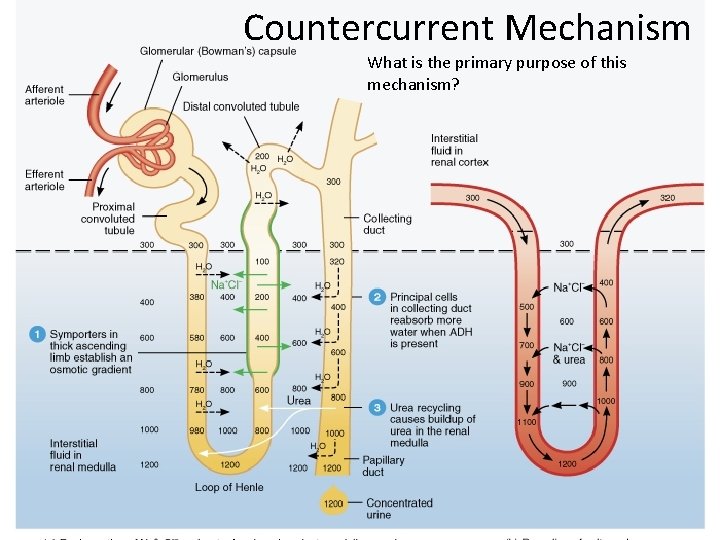
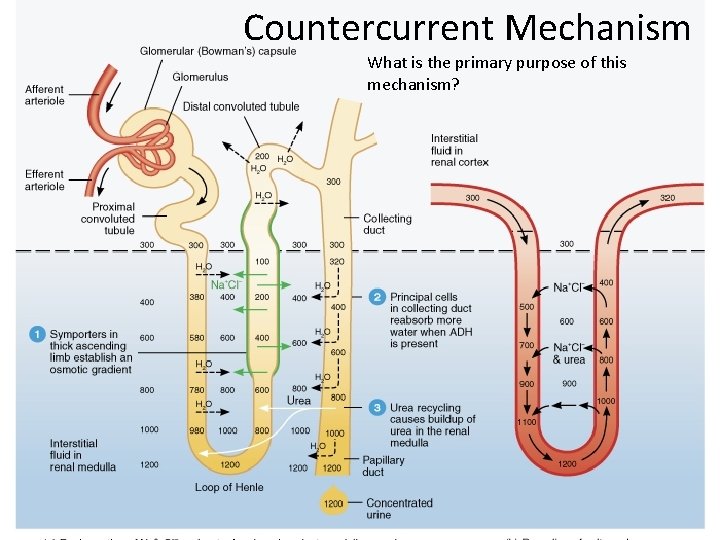
Countercurrent Mechanism What is the primary purpose of this mechanism?
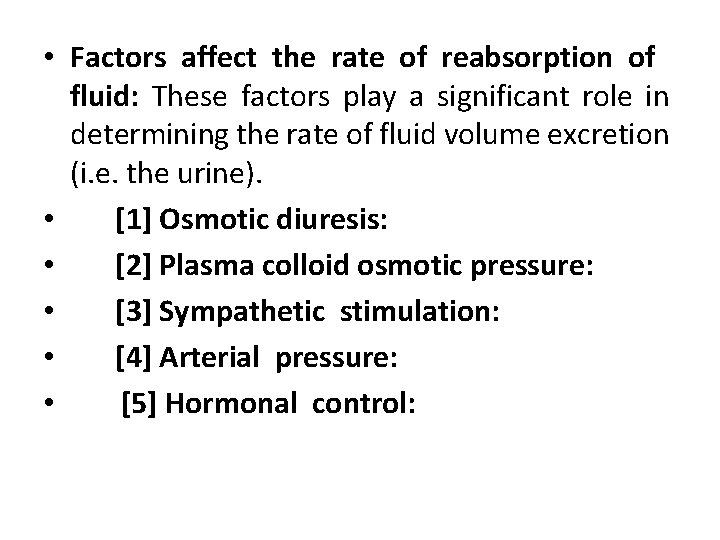
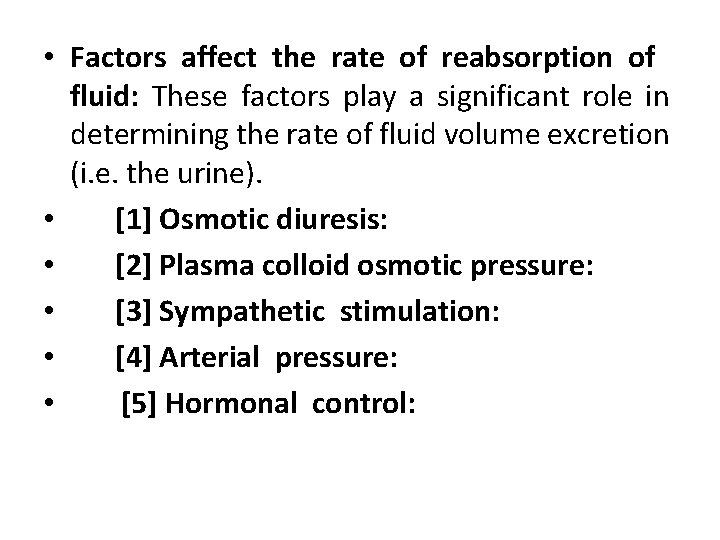
• Factors affect the rate of reabsorption of fluid: These factors play a significant role in determining the rate of fluid volume excretion (i. e. the urine). • [1] Osmotic diuresis: • [2] Plasma colloid osmotic pressure: • [3] Sympathetic stimulation: • [4] Arterial pressure: • [5] Hormonal control:
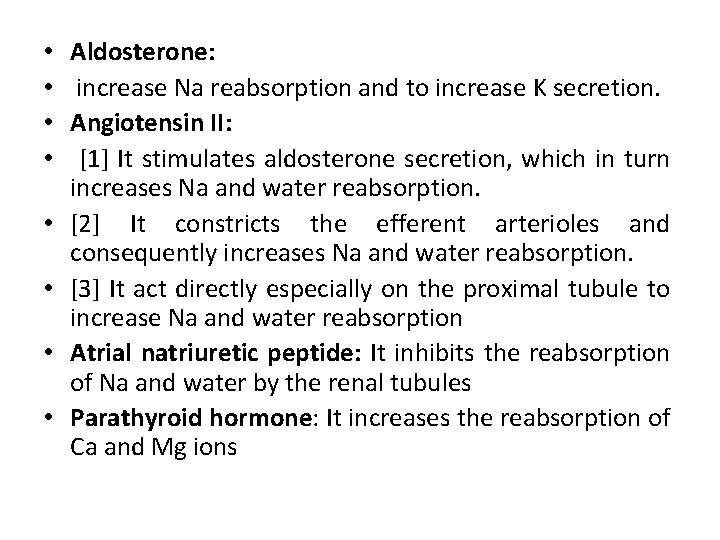
• • Aldosterone: increase Na reabsorption and to increase K secretion. Angiotensin II: [1] It stimulates aldosterone secretion, which in turn increases Na and water reabsorption. [2] It constricts the efferent arterioles and consequently increases Na and water reabsorption. [3] It act directly especially on the proximal tubule to increase Na and water reabsorption Atrial natriuretic peptide: It inhibits the reabsorption of Na and water by the renal tubules Parathyroid hormone: It increases the reabsorption of Ca and Mg ions
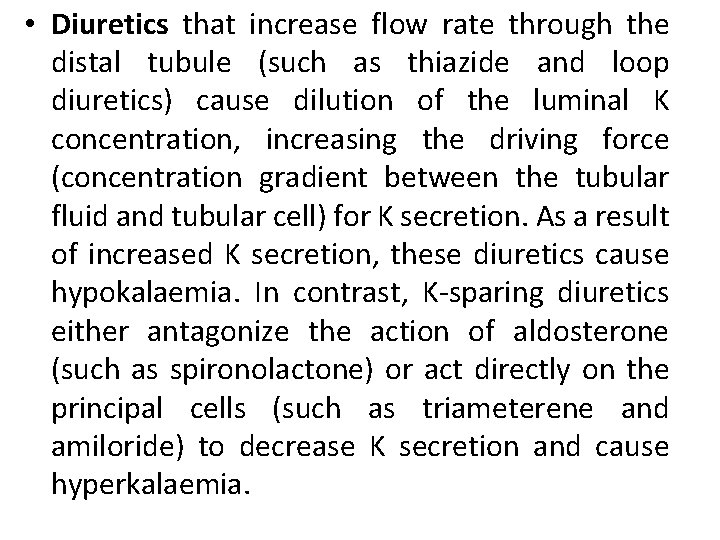
• Diuretics that increase flow rate through the distal tubule (such as thiazide and loop diuretics) cause dilution of the luminal K concentration, increasing the driving force (concentration gradient between the tubular fluid and tubular cell) for K secretion. As a result of increased K secretion, these diuretics cause hypokalaemia. In contrast, K-sparing diuretics either antagonize the action of aldosterone (such as spironolactone) or act directly on the principal cells (such as triameterene and amiloride) to decrease K secretion and cause hyperkalaemia.
• Micturition: • Is the process by which the urinay bladder empties when it becomes filled.
• The micturition reflex: As the bladder fills, it stretches the bladder wall, thus stimulating stretch receptors especially in the bladder neck. The first urge to void is felt at a bladder volume of about 150 ml, and a marked sense of fullness at about 300 -400 ml. Then, sensory signals are conducted to the sacral segments of the spinal cord through the pelvic nerves and then back again to the bladder through the parasympathetic fibers in these same nerves initiating micturition contraction of the detrusor muscles. Once a micturition reflex begins, it is self-regenerative and the high pressure inside the bladder forces the bladder neck to open against its tonic contraction.
• Stretching the bladder neck exacerbates the intensity of the micturition reflex and also activates another reflex. This reflex passes to the sacral portion of the spinal cord and then back through the pudendal nerve to the external sphincter to inhibit it. If this inhibition is more potent than the voluntary constrictor signals from the brain, then urination will occur. Then after a few seconds to more than a minute, the reflex begins to fatigue allowing rapid reduction in bladder contraction.



 Res extra commercium
Res extra commercium Diagnostico etiologico
Diagnostico etiologico Cortical and juxtamedullary nephrons difference
Cortical and juxtamedullary nephrons difference Renal physiology
Renal physiology Sodium reabsorption
Sodium reabsorption Georgia limniatis
Georgia limniatis Tsds peims 2017 2018
Tsds peims 2017 2018 Državna matura 2017
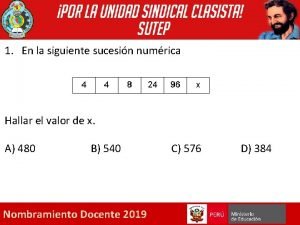
Državna matura 2017 Dada la siguiente secuencia rusia 2018 rusia 2018
Dada la siguiente secuencia rusia 2018 rusia 2018 University of iowa college of dentistry
University of iowa college of dentistry Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worms-breton
Tư thế worms-breton Chúa sống lại
Chúa sống lại Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc cc
V cc cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể