HISTOLOGY OF URINARY SYSTEM Dr Haydar AlTukmagi AlMustaffa
- Slides: 26
HISTOLOGY OF URINARY SYSTEM Dr. Haydar Al-Tukmagi Al-Mustaffa University College
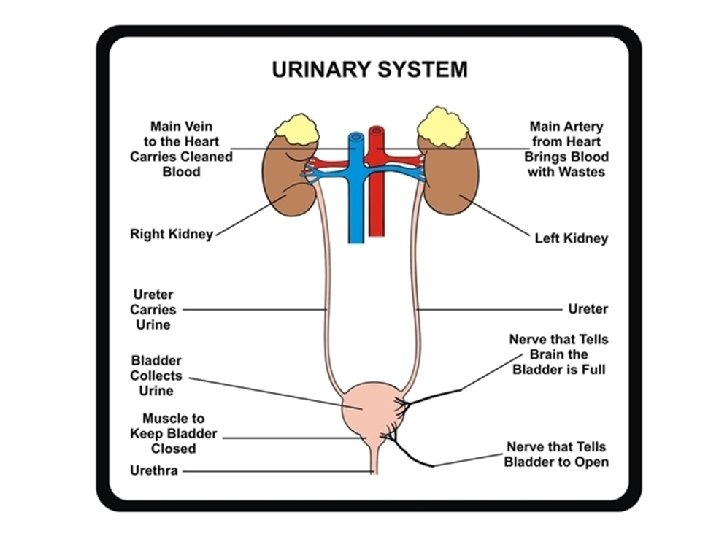
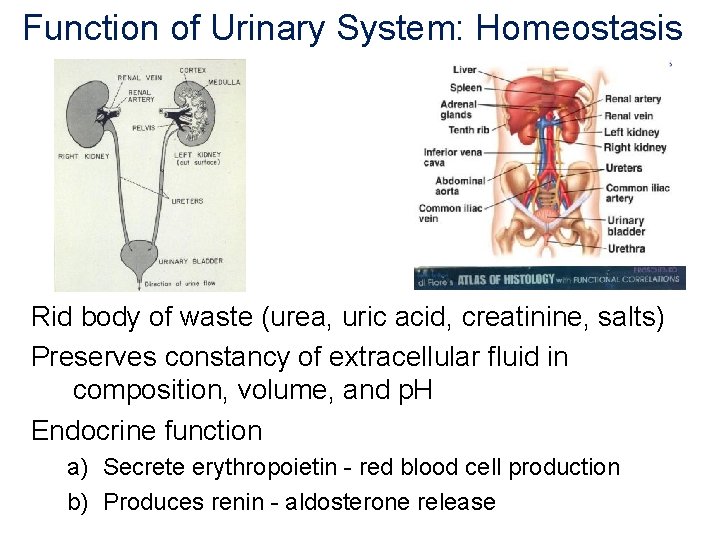
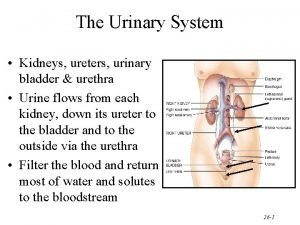
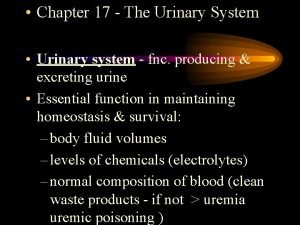
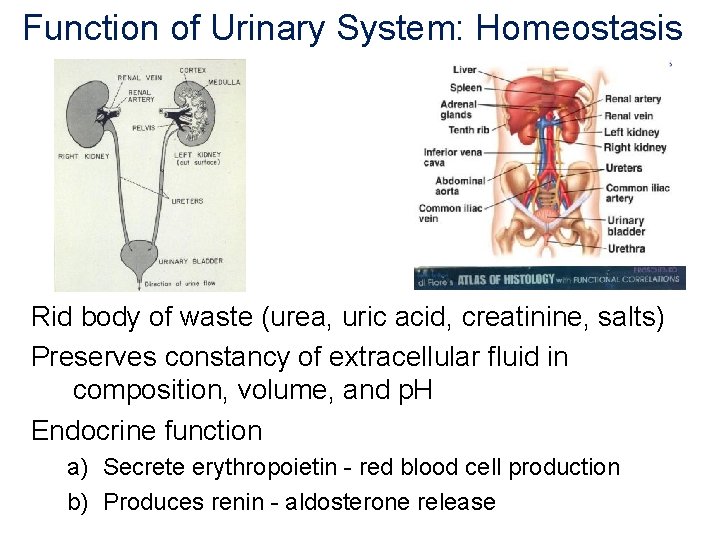
Function of Urinary System: Homeostasis Rid body of waste (urea, uric acid, creatinine, salts) Preserves constancy of extracellular fluid in composition, volume, and p. H Endocrine function a) Secrete erythropoietin - red blood cell production b) Produces renin - aldosterone release
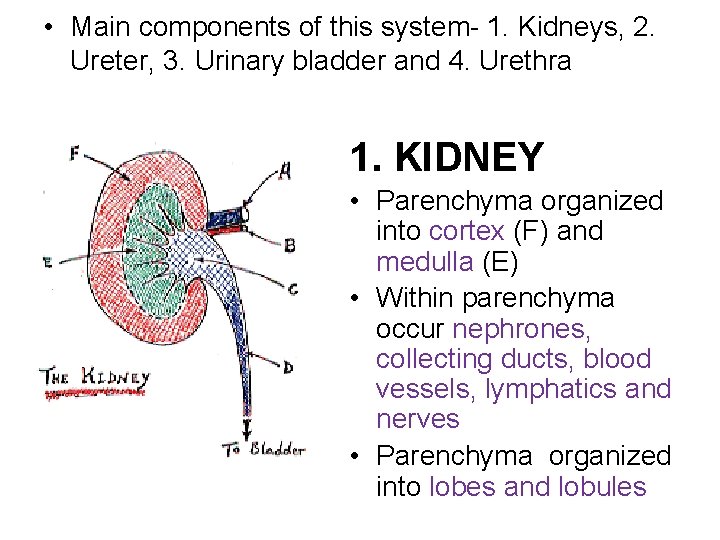
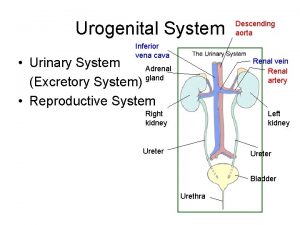
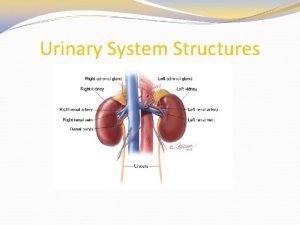
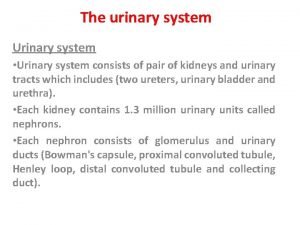
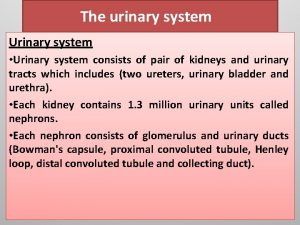
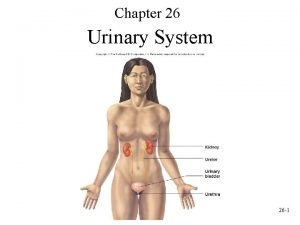
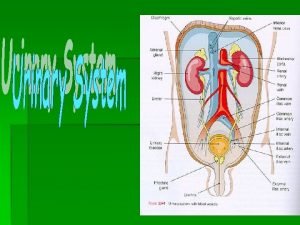
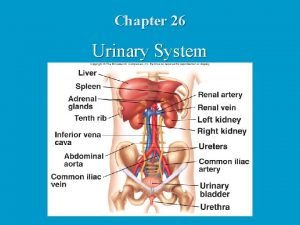
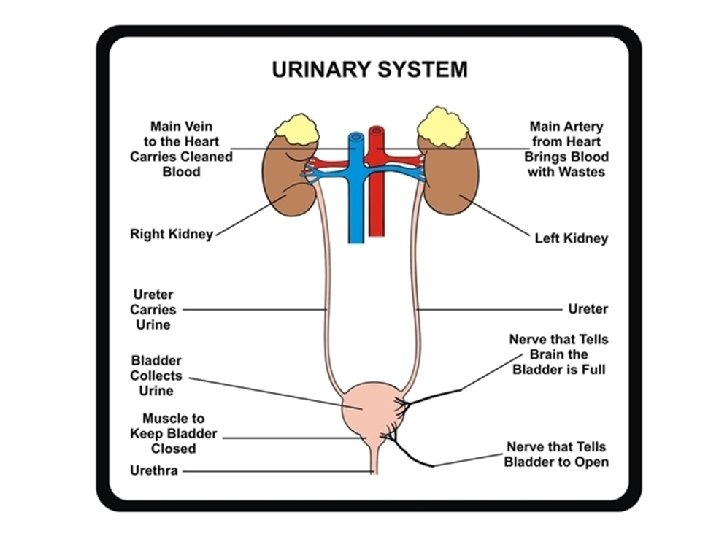
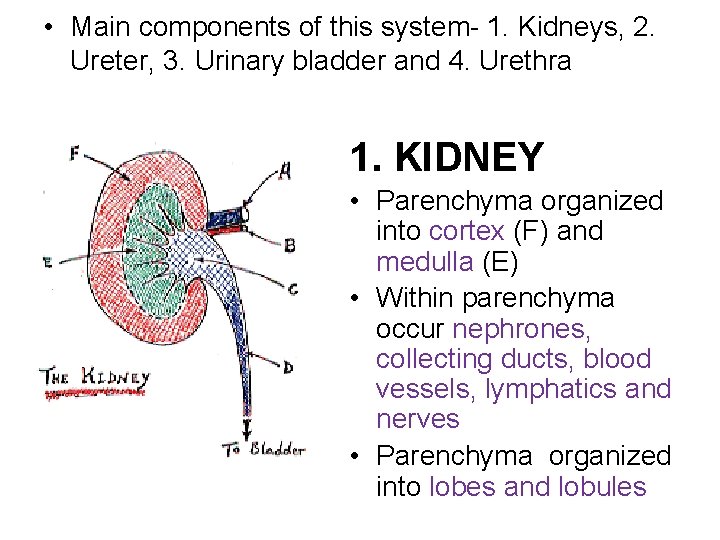
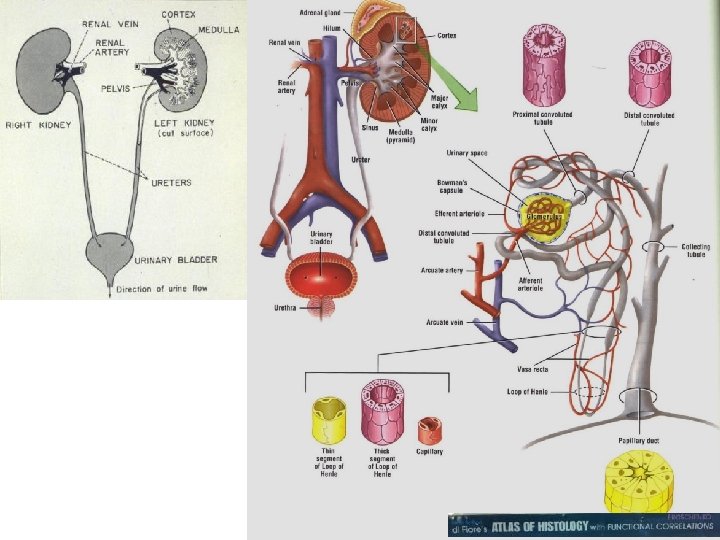
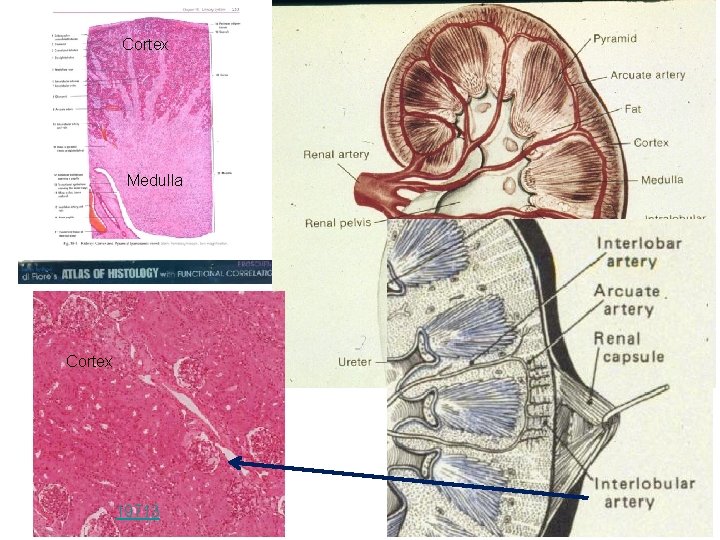
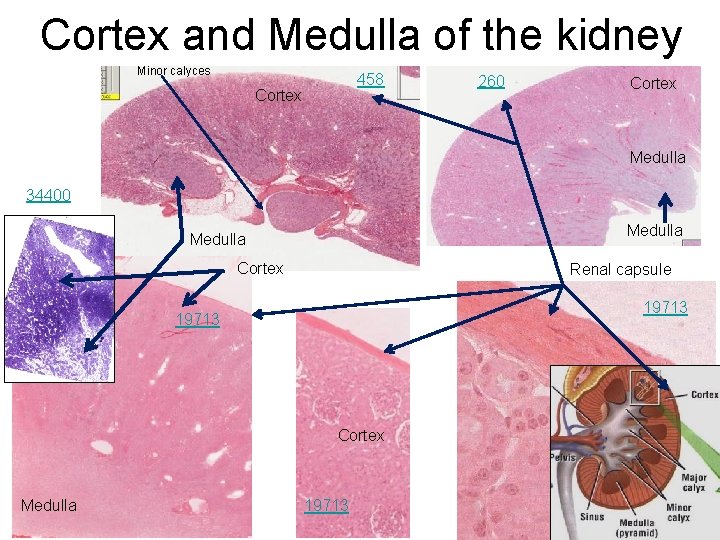
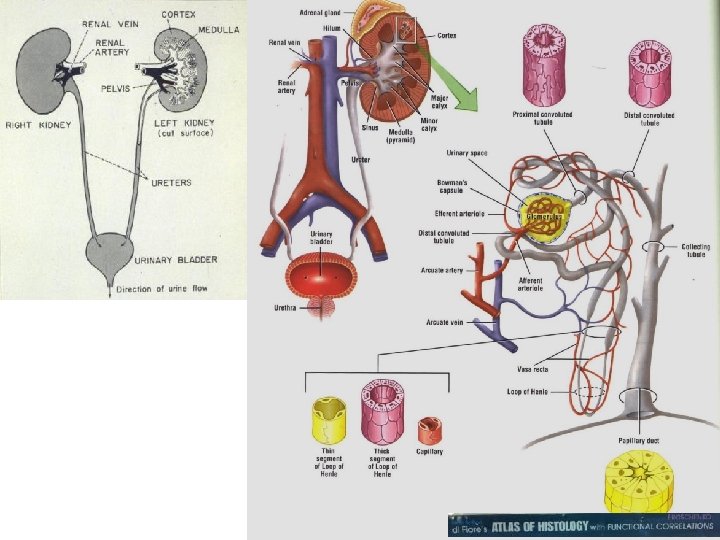
• Main components of this system- 1. Kidneys, 2. Ureter, 3. Urinary bladder and 4. Urethra 1. KIDNEY • Parenchyma organized into cortex (F) and medulla (E) • Within parenchyma occur nephrones, collecting ducts, blood vessels, lymphatics and nerves • Parenchyma organized into lobes and lobules
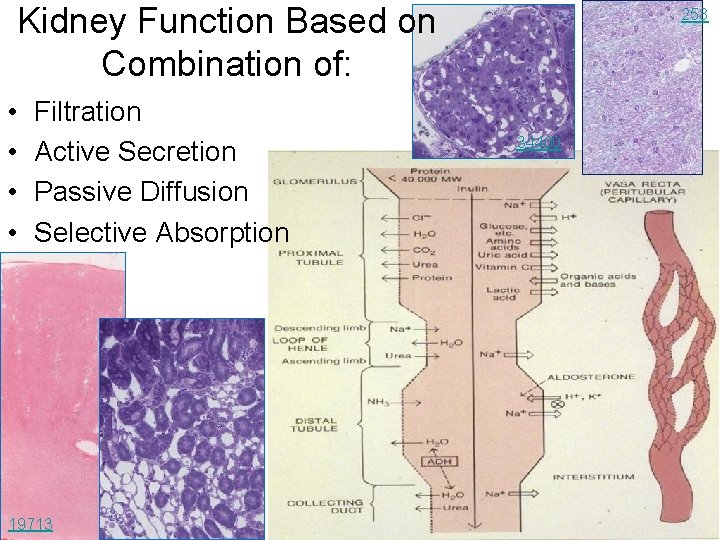
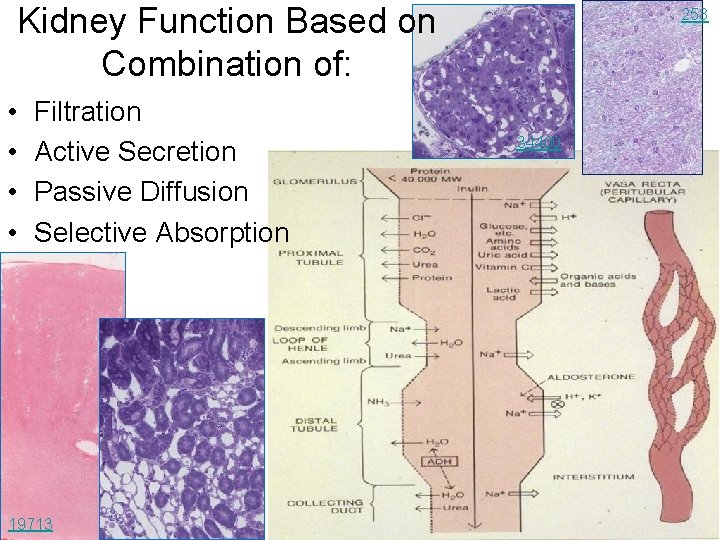
Kidney Function Based on Combination of: • • Filtration Active Secretion Passive Diffusion Selective Absorption 19713 258 34400
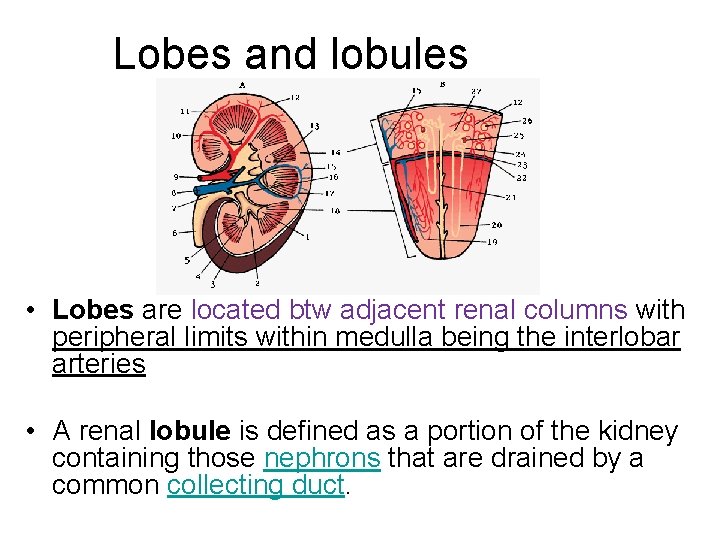
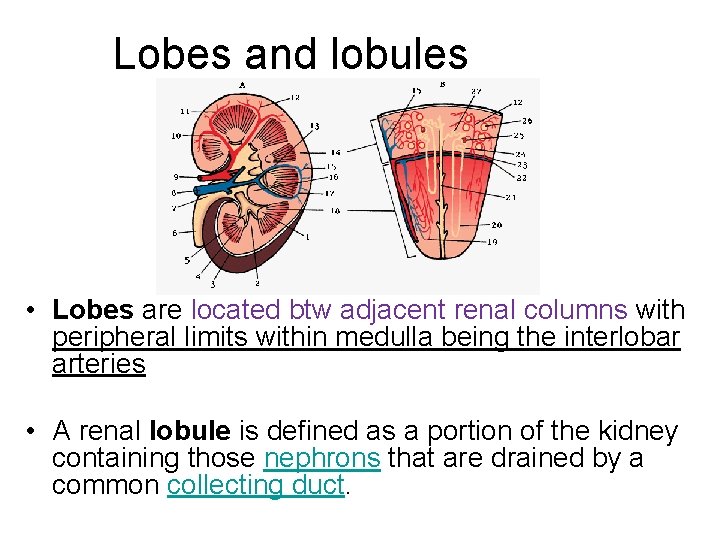
Lobes and lobules • Lobes are located btw adjacent renal columns with peripheral limits within medulla being the interlobar arteries • A renal lobule is defined as a portion of the kidney containing those nephrons that are drained by a common collecting duct.
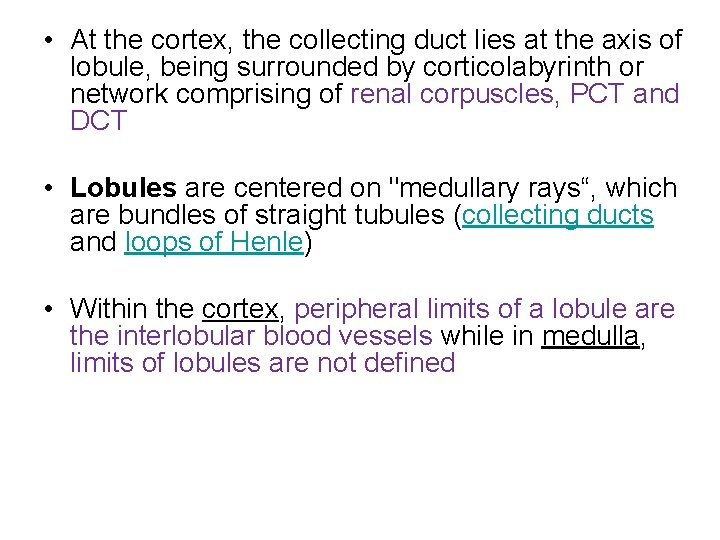
• At the cortex, the collecting duct lies at the axis of lobule, being surrounded by corticolabyrinth or network comprising of renal corpuscles, PCT and DCT • Lobules are centered on "medullary rays“, which are bundles of straight tubules (collecting ducts and loops of Henle) • Within the cortex, peripheral limits of a lobule are the interlobular blood vessels while in medulla, limits of lobules are not defined
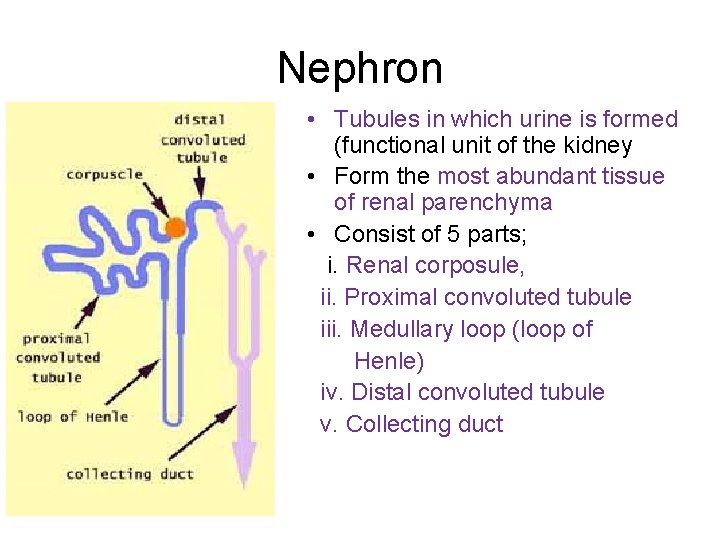
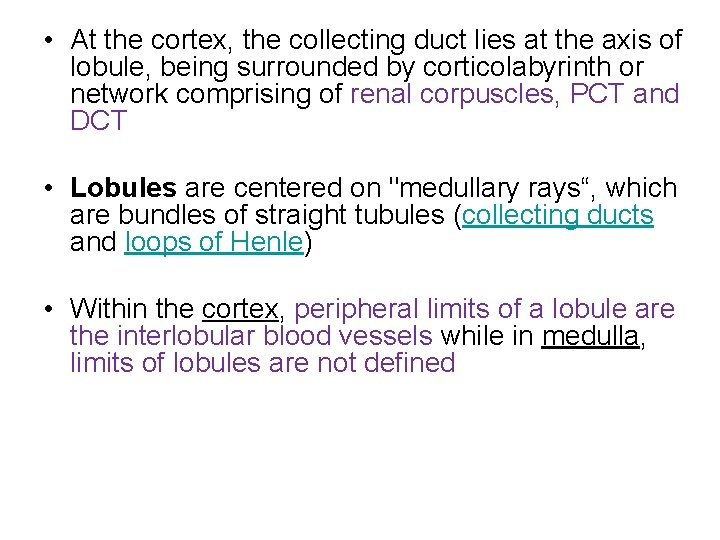
Nephron • Tubules in which urine is formed (functional unit of the kidney • Form the most abundant tissue of renal parenchyma • Consist of 5 parts; i. Renal corposule, ii. Proximal convoluted tubule iii. Medullary loop (loop of Henle) iv. Distal convoluted tubule v. Collecting duct
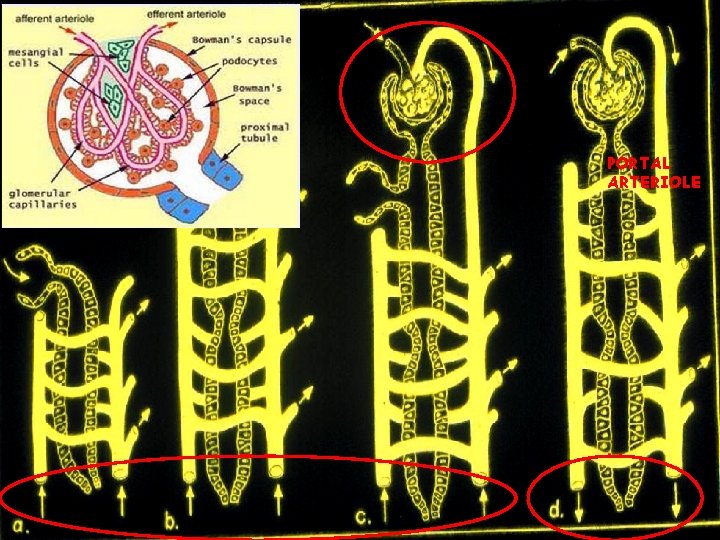
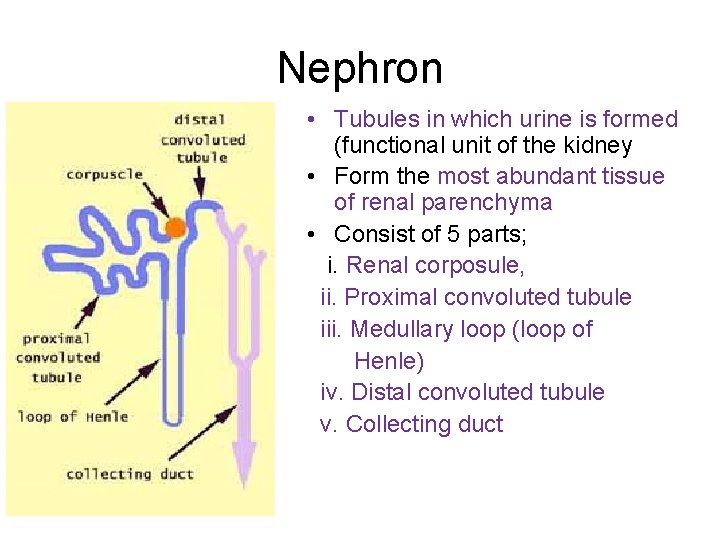
PORTAL ARTERIOLE
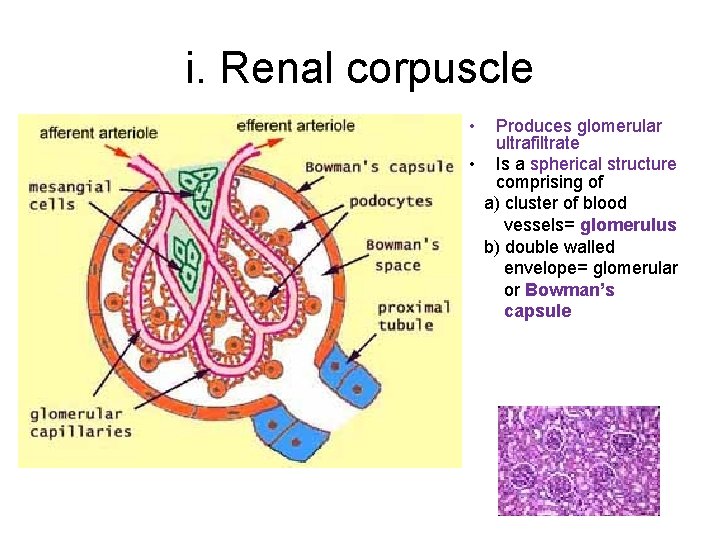
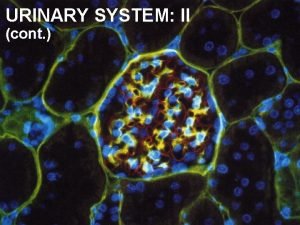
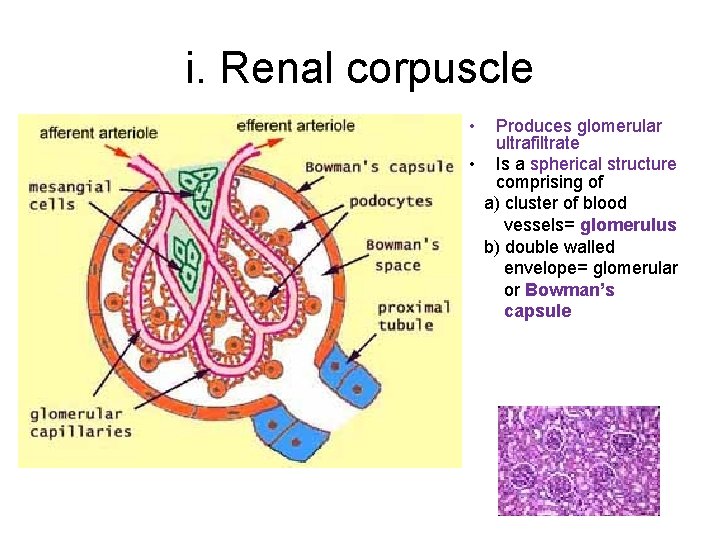
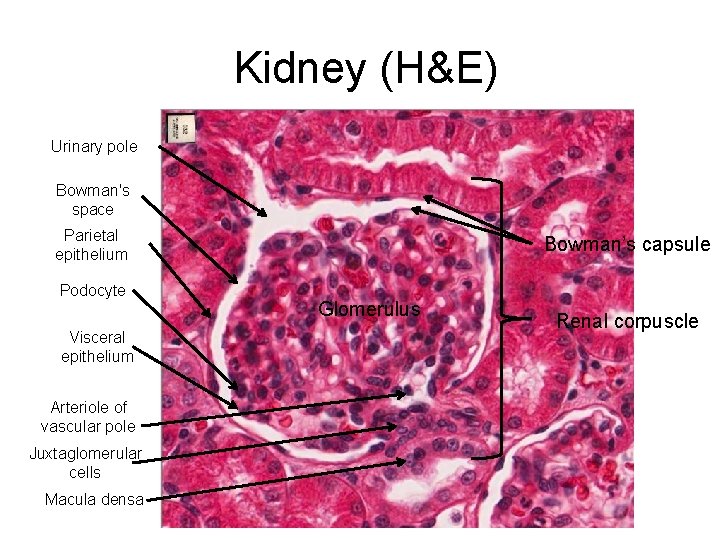
i. Renal corpuscle • Produces glomerular ultrafiltrate • Is a spherical structure comprising of a) cluster of blood vessels= glomerulus b) double walled envelope= glomerular or Bowman’s capsule
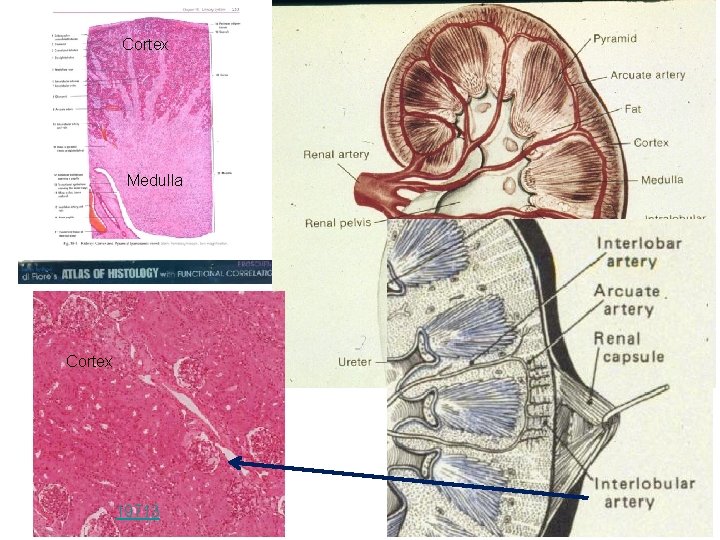
Cortex Medulla Cortex 19713
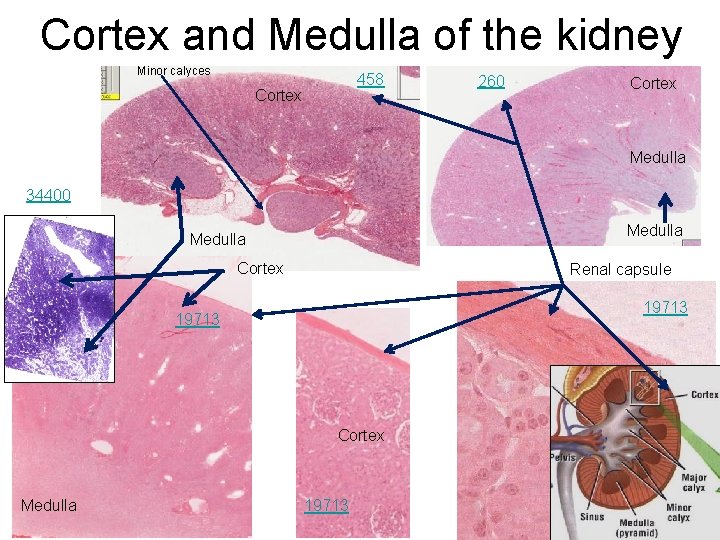
Cortex and Medulla of the kidney Minor calyces 458 Cortex 260 Cortex Medulla 34400 Medulla Cortex Renal capsule 19713 Cortex Medulla 19713
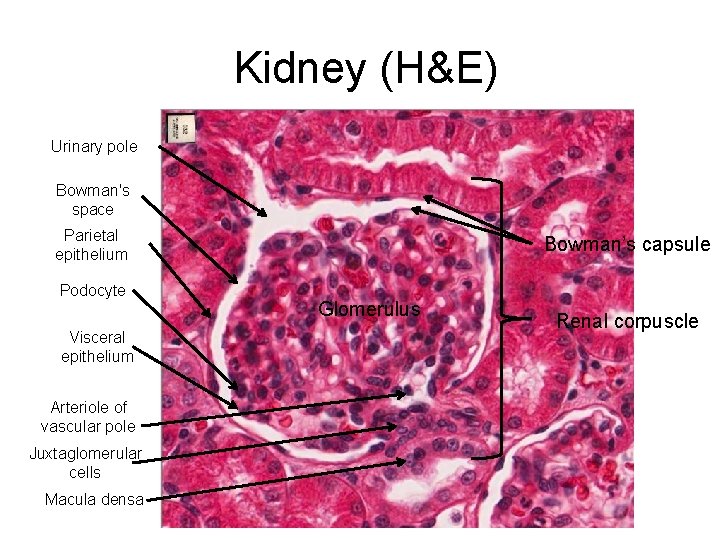
Kidney (H&E) Urinary pole Bowman's space Parietal epithelium Podocyte Visceral epithelium Arteriole of vascular pole Juxtaglomerular cells Macula densa Bowman’s capsule Glomerulus Renal corpuscle
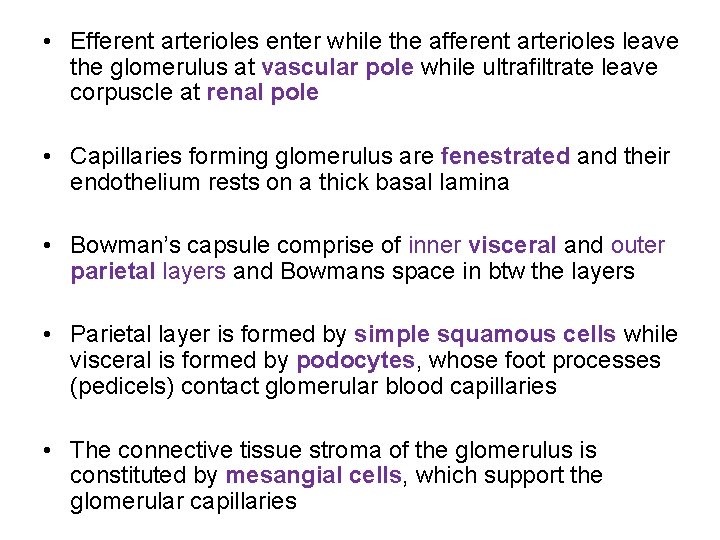
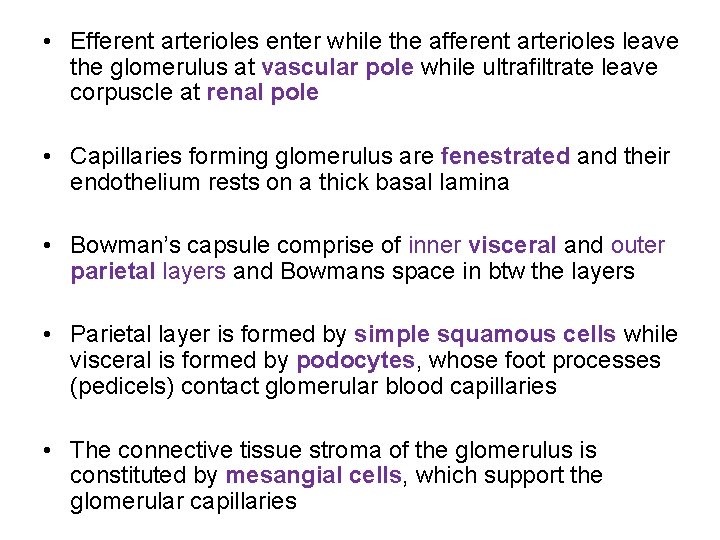
• Efferent arterioles enter while the afferent arterioles leave the glomerulus at vascular pole while ultrafiltrate leave corpuscle at renal pole • Capillaries forming glomerulus are fenestrated and their endothelium rests on a thick basal lamina • Bowman’s capsule comprise of inner visceral and outer parietal layers and Bowmans space in btw the layers • Parietal layer is formed by simple squamous cells while visceral is formed by podocytes, whose foot processes (pedicels) contact glomerular blood capillaries • The connective tissue stroma of the glomerulus is constituted by mesangial cells, which support the glomerular capillaries
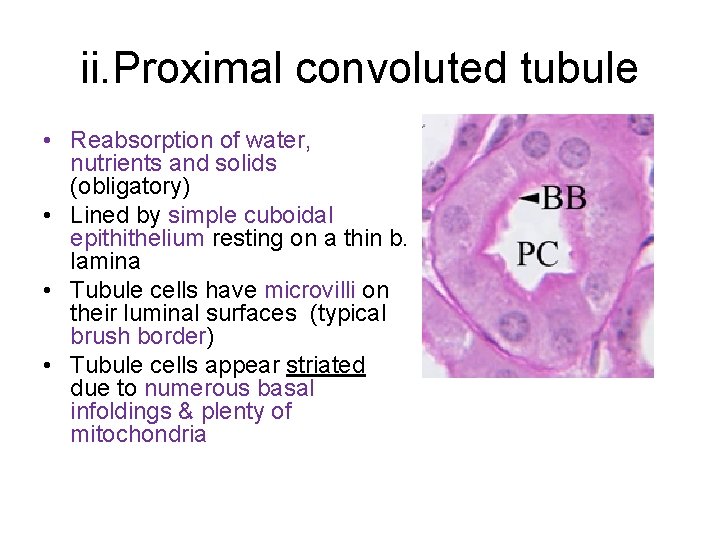
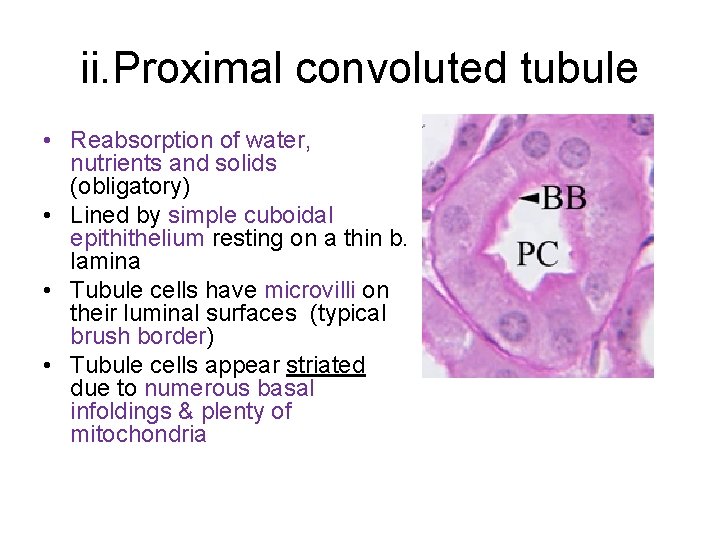
ii. Proximal convoluted tubule • Reabsorption of water, nutrients and solids (obligatory) • Lined by simple cuboidal epithithelium resting on a thin b. lamina • Tubule cells have microvilli on their luminal surfaces (typical brush border) • Tubule cells appear striated due to numerous basal infoldings & plenty of mitochondria
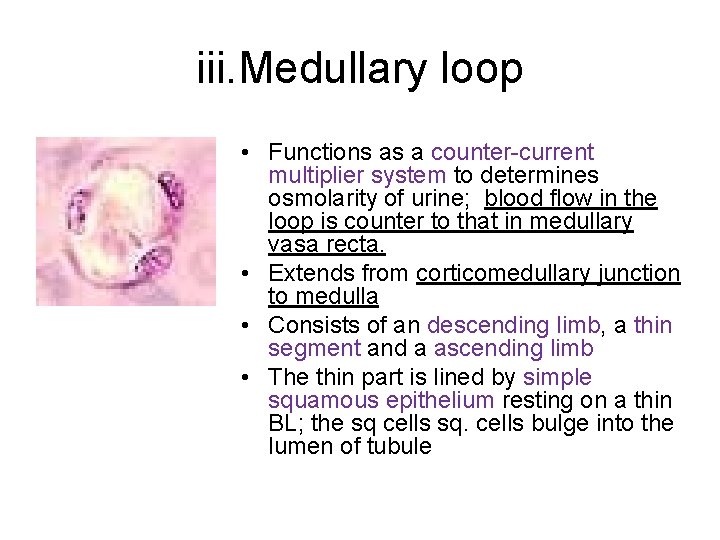
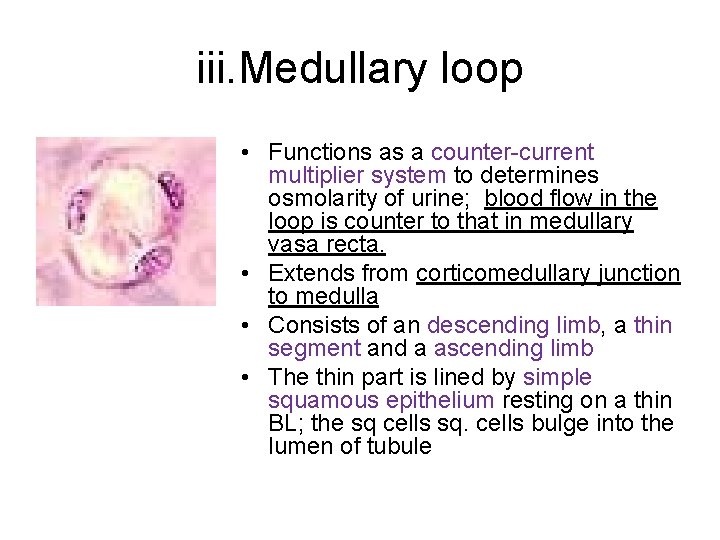
iii. Medullary loop • Functions as a counter-current multiplier system to determines osmolarity of urine; blood flow in the loop is counter to that in medullary vasa recta. • Extends from corticomedullary junction to medulla • Consists of an descending limb, a thin segment and a ascending limb • The thin part is lined by simple squamous epithelium resting on a thin BL; the sq cells sq. cells bulge into the lumen of tubule
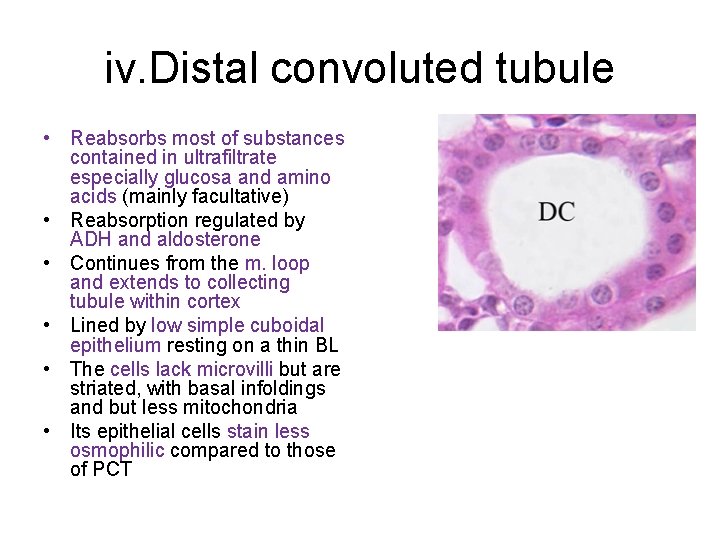
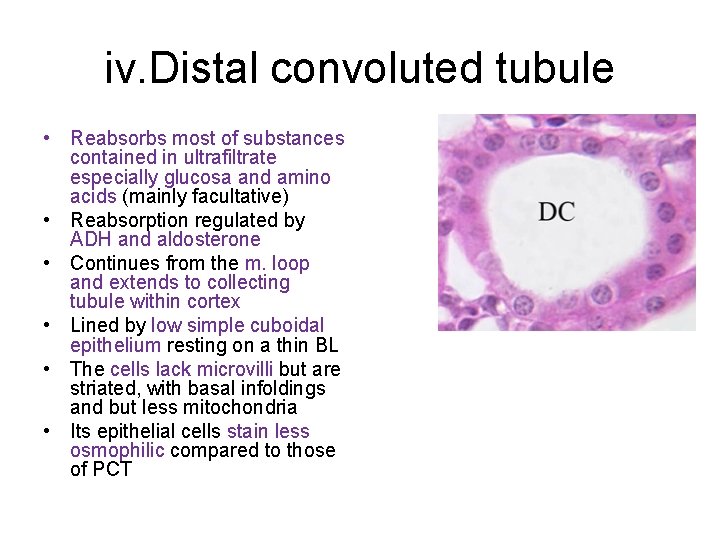
iv. Distal convoluted tubule • Reabsorbs most of substances contained in ultrafiltrate especially glucosa and amino acids (mainly facultative) • Reabsorption regulated by ADH and aldosterone • Continues from the m. loop and extends to collecting tubule within cortex • Lined by low simple cuboidal epithelium resting on a thin BL • The cells lack microvilli but are striated, with basal infoldings and but less mitochondria • Its epithelial cells stain less osmophilic compared to those of PCT
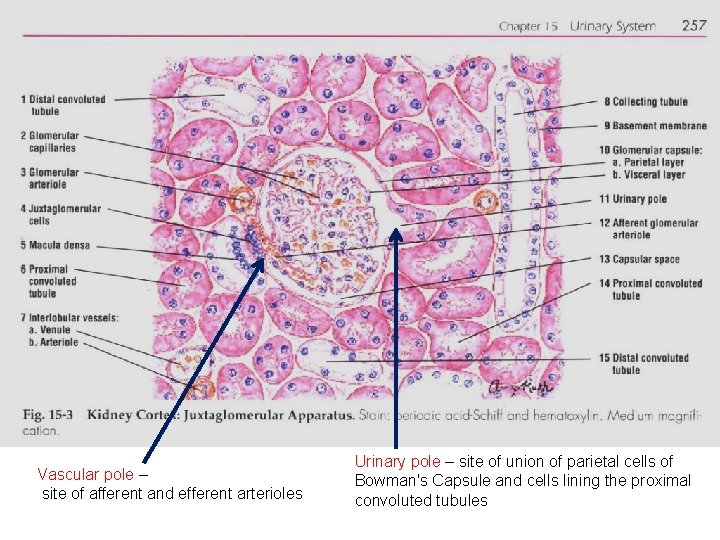
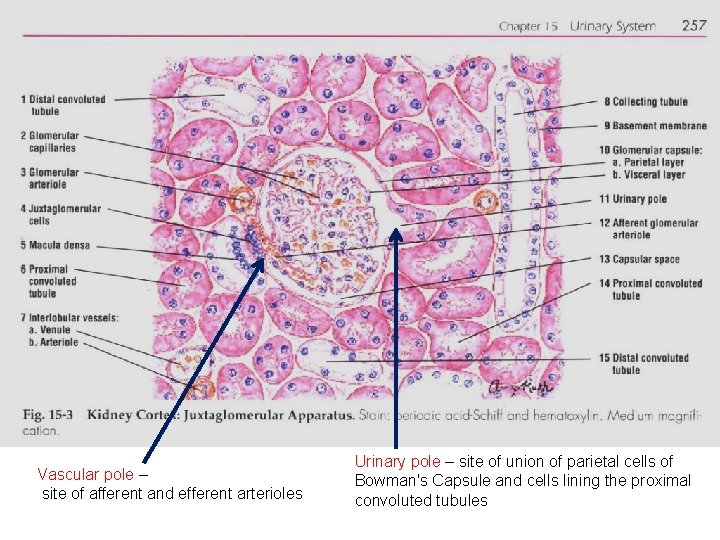
Vascular pole – site of afferent and efferent arterioles Urinary pole – site of union of parietal cells of Bowman's Capsule and cells lining the proximal convoluted tubules
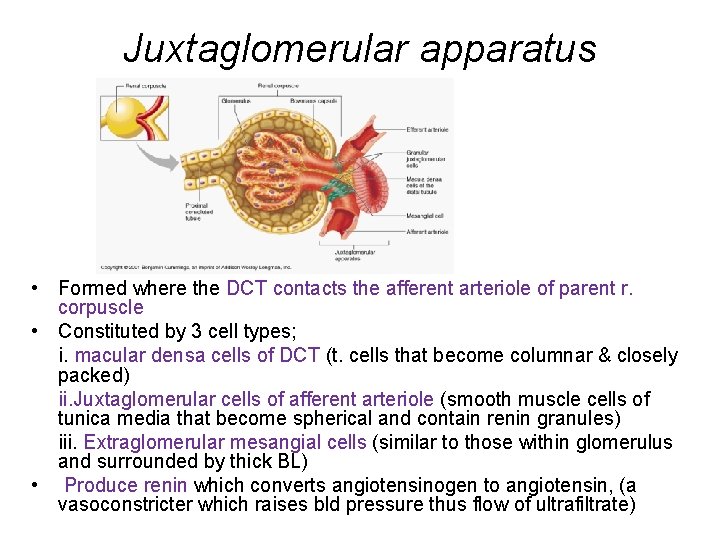
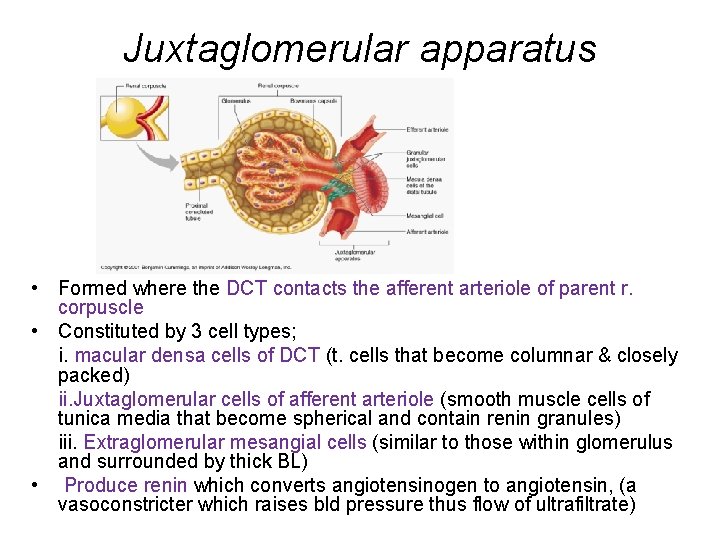
Juxtaglomerular apparatus • Formed where the DCT contacts the afferent arteriole of parent r. corpuscle • Constituted by 3 cell types; i. macular densa cells of DCT (t. cells that become columnar & closely packed) ii. Juxtaglomerular cells of afferent arteriole (smooth muscle cells of tunica media that become spherical and contain renin granules) iii. Extraglomerular mesangial cells (similar to those within glomerulus and surrounded by thick BL) • Produce renin which converts angiotensinogen to angiotensin, (a vasoconstricter which raises bld pressure thus flow of ultrafiltrate)
v. Collecting tubule • Drain urine from nephron to renal pelvis • Lie on medullary ray within cortex • Progressively increase in diameter towards medullar • In inner medullar, CD from different renal lobes unite to form large papillary ducts, which open into renal pelvis
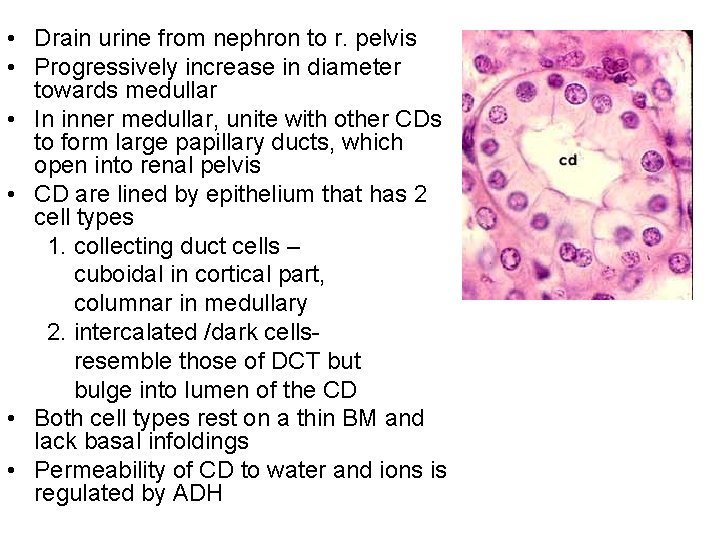
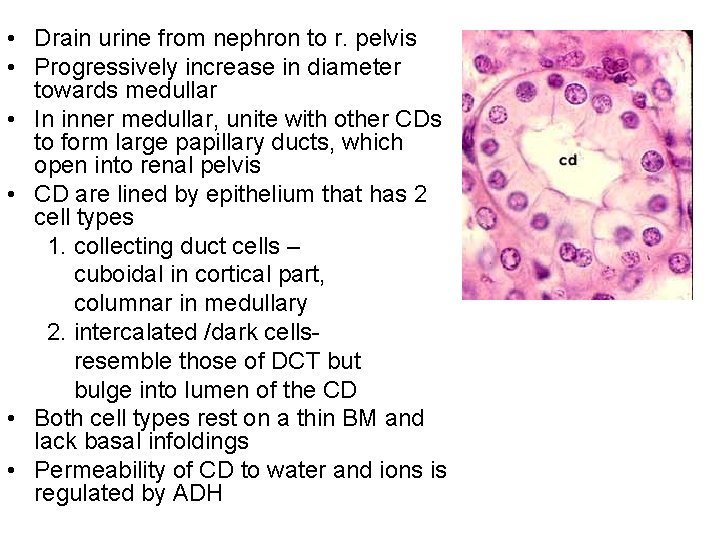
• Drain urine from nephron to r. pelvis • Progressively increase in diameter towards medullar • In inner medullar, unite with other CDs to form large papillary ducts, which open into renal pelvis • CD are lined by epithelium that has 2 cell types 1. collecting duct cells – cuboidal in cortical part, columnar in medullary 2. intercalated /dark cells- resemble those of DCT but bulge into lumen of the CD • Both cell types rest on a thin BM and lack basal infoldings • Permeability of CD to water and ions is regulated by ADH
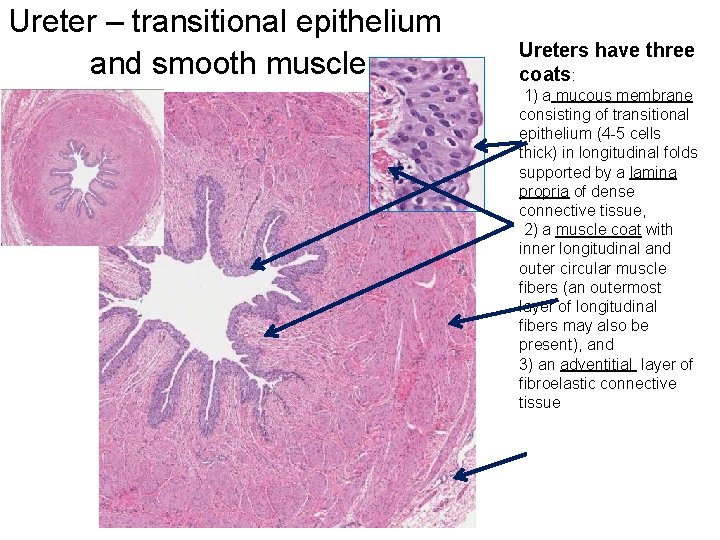
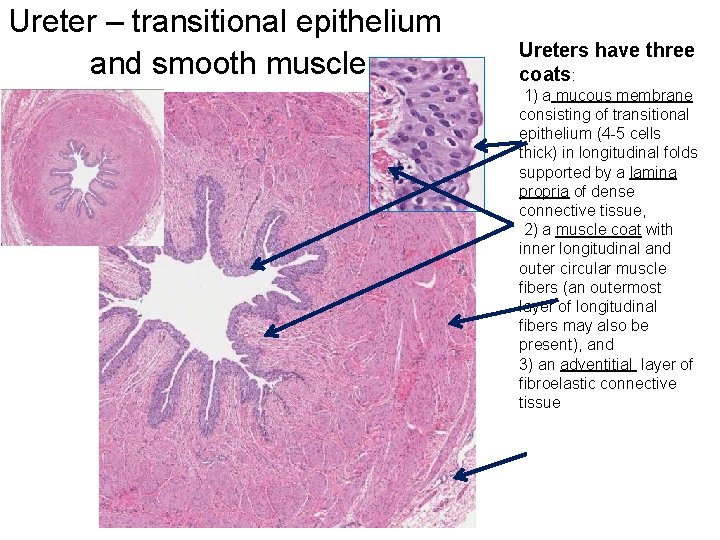
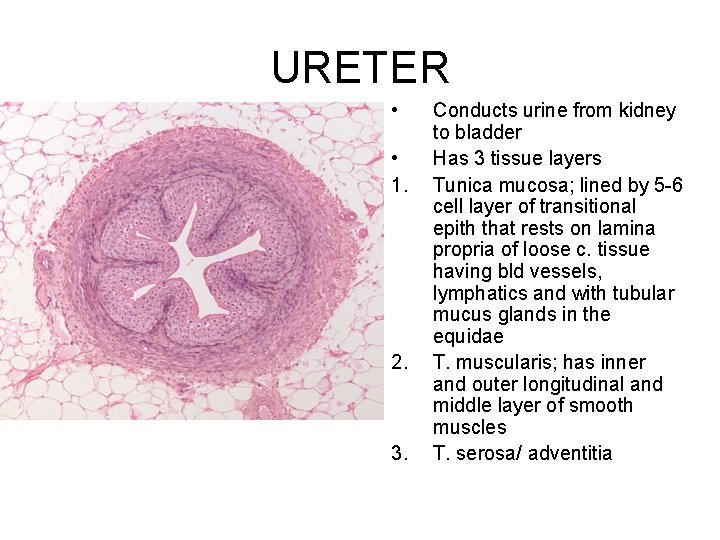
Ureter – transitional epithelium and smooth muscle Ureters have three coats: 1) a mucous membrane consisting of transitional epithelium (4 -5 cells thick) in longitudinal folds supported by a lamina propria of dense connective tissue, 2) a muscle coat with inner longitudinal and outer circular muscle fibers (an outermost layer of longitudinal fibers may also be present), and 3) an adventitial layer of fibroelastic connective tissue
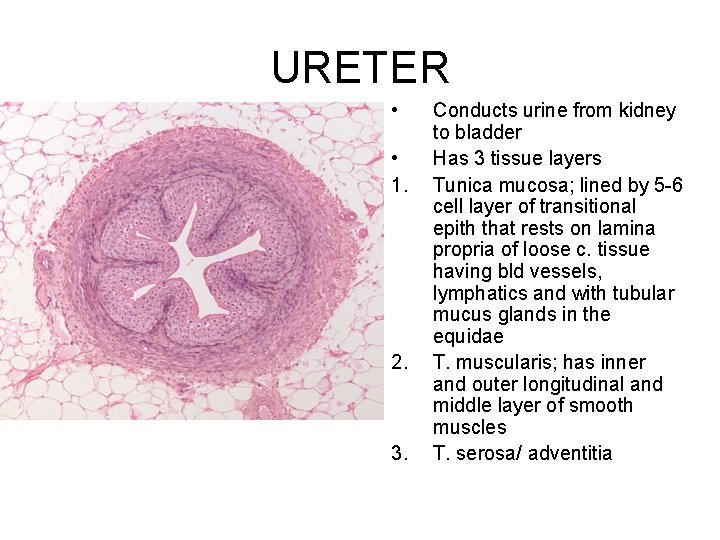
URETER • • 1. 2. 3. Conducts urine from kidney to bladder Has 3 tissue layers Tunica mucosa; lined by 5 -6 cell layer of transitional epith that rests on lamina propria of loose c. tissue having bld vessels, lymphatics and with tubular mucus glands in the equidae T. muscularis; has inner and outer longitudinal and middle layer of smooth muscles T. serosa/ adventitia
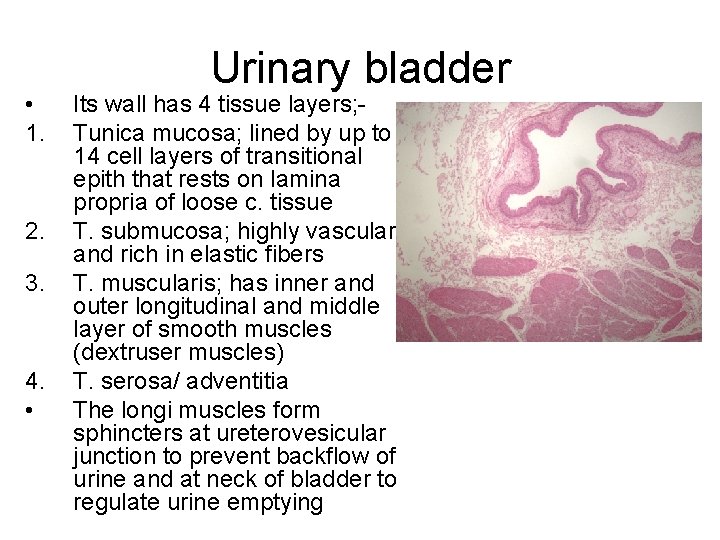
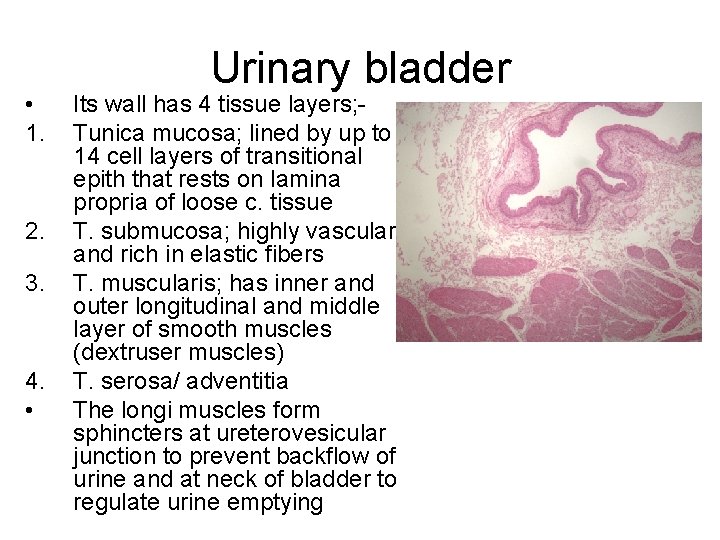
• 1. 2. 3. 4. • Urinary bladder Its wall has 4 tissue layers; Tunica mucosa; lined by up to 14 cell layers of transitional epith that rests on lamina propria of loose c. tissue T. submucosa; highly vascular and rich in elastic fibers T. muscularis; has inner and outer longitudinal and middle layer of smooth muscles (dextruser muscles) T. serosa/ adventitia The longi muscles form sphincters at ureterovesicular junction to prevent backflow of urine and at neck of bladder to regulate urine emptying
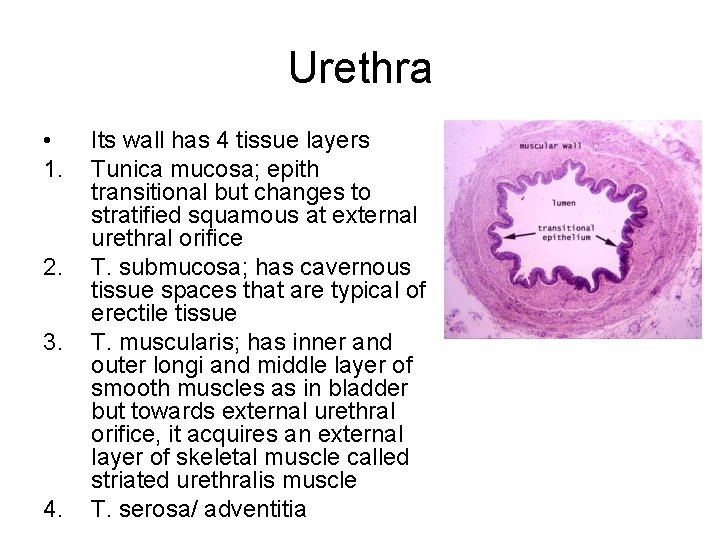
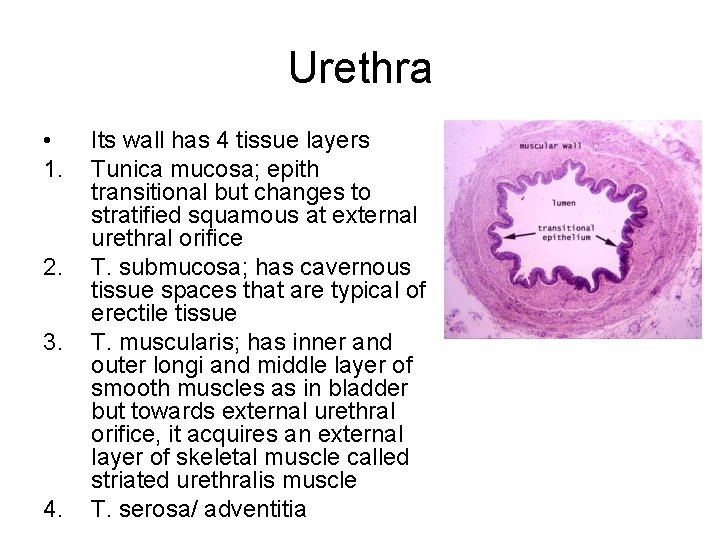
Urethra • 1. 2. 3. 4. Its wall has 4 tissue layers Tunica mucosa; epith transitional but changes to stratified squamous at external urethral orifice T. submucosa; has cavernous tissue spaces that are typical of erectile tissue T. muscularis; has inner and outer longi and middle layer of smooth muscles as in bladder but towards external urethral orifice, it acquires an external layer of skeletal muscle called striated urethralis muscle T. serosa/ adventitia
 Nephron urinary system
Nephron urinary system Urinary infection symptoms
Urinary infection symptoms Osman nuri bakırcı ortaokulu
Osman nuri bakırcı ortaokulu Dr haydar
Dr haydar Lymph tissue fluid
Lymph tissue fluid Physiology of urine formation
Physiology of urine formation The urinary system chapter 15
The urinary system chapter 15 Scanty urine medical term
Scanty urine medical term Interesting facts about the integumentary system
Interesting facts about the integumentary system Pig reproductive anatomy
Pig reproductive anatomy Chapter 30 the urinary system workbook answers
Chapter 30 the urinary system workbook answers Kidney pyramid labeled
Kidney pyramid labeled Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Urinary system model
Urinary system model Urinary system model
Urinary system model Placoid scales definition
Placoid scales definition Urinary system powerpoint
Urinary system powerpoint Parietal layer of bowman's capsule
Parietal layer of bowman's capsule Functions of adh
Functions of adh Abnormal constituents of urine
Abnormal constituents of urine Urinary system x ray labeled
Urinary system x ray labeled Defination of urine
Defination of urine Excretory system
Excretory system Diaphragm of rat
Diaphragm of rat Rat urinary system
Rat urinary system Urogenital system
Urogenital system Diagram of the renal system
Diagram of the renal system