RENAL FAILURE Main Menu Classifications Acute versus chronic


- Slides: 91
RENAL FAILURE Main Menu
Classifications Ø Acute versus chronic Ø Pre-renal, post-renal Ø Anuric, oliguric, polyuric Main Menu
Renal Physiology Review a. b. c. d. e. f. The Kidneys: Control the fluid/electrolyte balance for the body Remove metabolic wastes from the blood & excrete them to the outside Regulate red-blood cell production Regulate blood-pressure Important in calcium ion absorption Control volume, composition and p. H of the blood Main Menu
Renal Hormone Regulation Synthesis and activation of hormones by the kidney include: • Active form of Vitamin D • Erythropoietin Renal blood flow regulated by: Renin-angiotensin aldosterone system (RAAS) Main Menu
Fluid and Electrolyte Control Mechanisms Ø RAAS – Renin-Angiotensin Aldosterone System Ø Aldosterone Ø ADH – Anti-Diuretic Hormone Main Menu
Aldosterone Ø Increases rate of sodium ion absorption Ø Chloride moves along with sodium because of + charge of sodium Ø Increases rate of potassium & hydrogen ion secretion Result: Fluid and sodium retention increases bloodpressure Main Menu
ACUTE RENAL FAILURE Main Menu
Acute Renal Failure Ø Definition l l The loss of renal function (measured as GFR) over hours to days Expressed clinically as the retention of nitrogenous waste products in the blood Main Menu
Acute Renal Failure Ø Definitions l l Azotemia - the accumulation of nitrogenous wastes Uremia - symptomatic renal failure Oliguria - urine output < 400 -500 m. L/24 hours Anuria - urine output < 100 m. L/24 hours Main Menu
Ø Pre-renal = l l Ø vomiting, diarrhea, poor fluid intake, fever, use of diuretics, and heart failure cardiac failure, liver dysfunction, or septic shock Intrinsic l Ø Causes of ARF Interstitial nephritis, acute glomerulonephritis, tubular necrosis, ischemia, toxins Post-renal = l l l prostatic hypertrophy, cancer of the prostate or cervix, or retroperitoneal disorders neurogenic bladder bilateral renal calculi, papillary necrosis, coagulated blood, bladder carcinoma, and fungus Main Menu
Symptoms of ARF Decrease urine output (70%) Ø Edema, esp. lower extremity Ø Mental changes Ø Heart failure Ø Nausea, vomiting Ø Pruritus Ø Anemia Ø Tachypenic Ø Cool, pale, moist skin Ø Main Menu
Hyperkalemia Symptoms Weakness Ø Lethargy Ø Muscle cramps Ø Paresthesias Ø Dysrhythmias Ø Main Menu
Hyperkalemia Treatment Ø Calcium gluconate (carbonate) Ø Sodium Bicarbonate Ø Insulin/glucose Ø Diuretics (Furosemid) Ø Albuterol Ø Hemodialysis Main Menu
Prerenal Acute Renal Failure Volume Depletion Ø Decreased effective blood volume Ø l l Ø congestive heart failure cirrhosis nephrotic syndrome sepsis Renal vasoconstriction l l l hepatorenal syndrome hypercalcemia nonsteroidal anti-inflammatory drugs Main Menu
Prerenal Acute Renal Failure: Clinical Presentation Ø History l l l l volume loss (e. g. , diarrhea, acute blood loss) heart disease liver disease evidence of infection diuretic use thirst orthostatic symptoms Main Menu
Prerenal Acute Renal Failure: Clinical Presentation Ø Physical Examination l l l l Blood pressure and pulse Orthostatic changes in blood pressure Skin turgor Dryness of mucous membranes and axillae Neck veins Cardiopulmonary exam Peripheral edema Main Menu
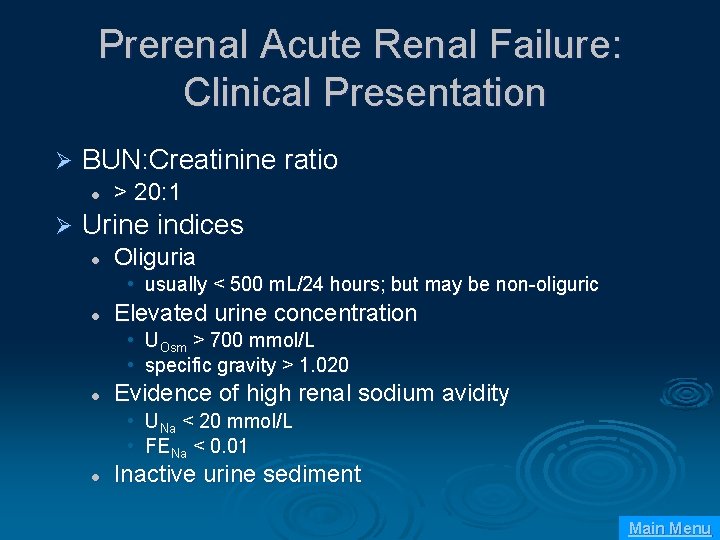
Prerenal Acute Renal Failure: Clinical Presentation Ø BUN: Creatinine ratio l Ø > 20: 1 Urine indices l Oliguria • usually < 500 m. L/24 hours; but may be non-oliguric l Elevated urine concentration • UOsm > 700 mmol/L • specific gravity > 1. 020 l Evidence of high renal sodium avidity • UNa < 20 mmol/L • FENa < 0. 01 l Inactive urine sediment Main Menu
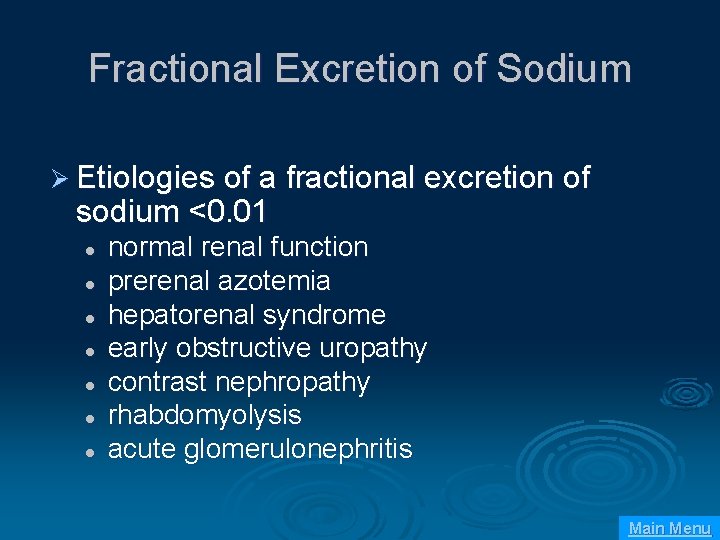
Fractional Excretion of Sodium Ø Etiologies of a fractional excretion of sodium <0. 01 l l l l normal renal function prerenal azotemia hepatorenal syndrome early obstructive uropathy contrast nephropathy rhabdomyolysis acute glomerulonephritis Main Menu
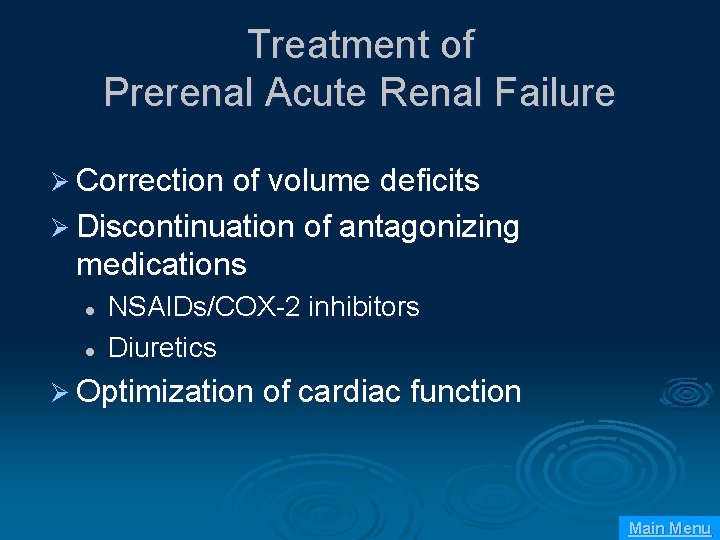
Treatment of Prerenal Acute Renal Failure Ø Correction of volume deficits Ø Discontinuation of antagonizing medications l l NSAIDs/COX-2 inhibitors Diuretics Ø Optimization of cardiac function Main Menu
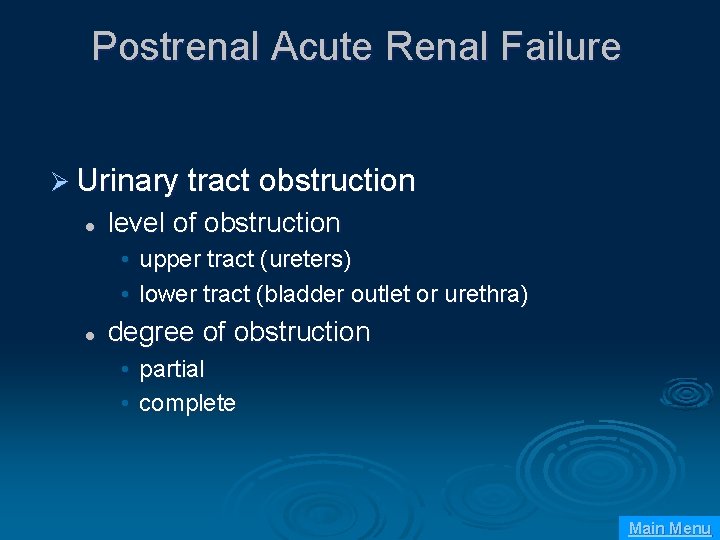
Postrenal Acute Renal Failure Ø Urinary tract obstruction l level of obstruction • upper tract (ureters) • lower tract (bladder outlet or urethra) l degree of obstruction • partial • complete Main Menu
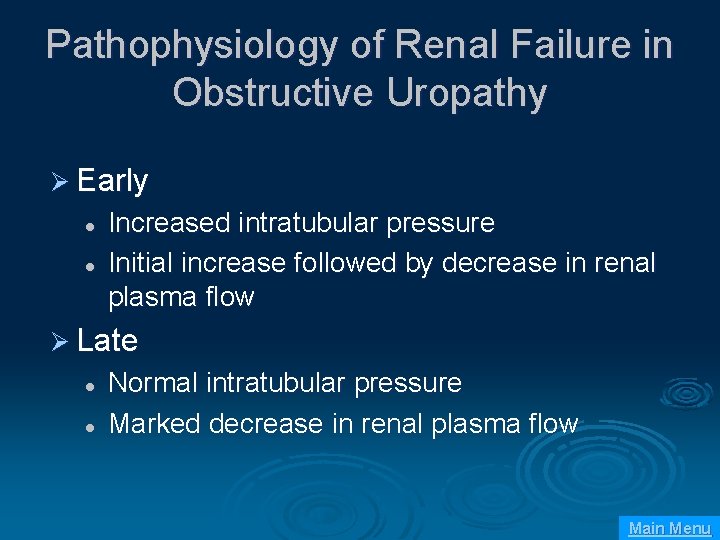
Pathophysiology of Renal Failure in Obstructive Uropathy Ø Early l l Increased intratubular pressure Initial increase followed by decrease in renal plasma flow Ø Late l l Normal intratubular pressure Marked decrease in renal plasma flow Main Menu
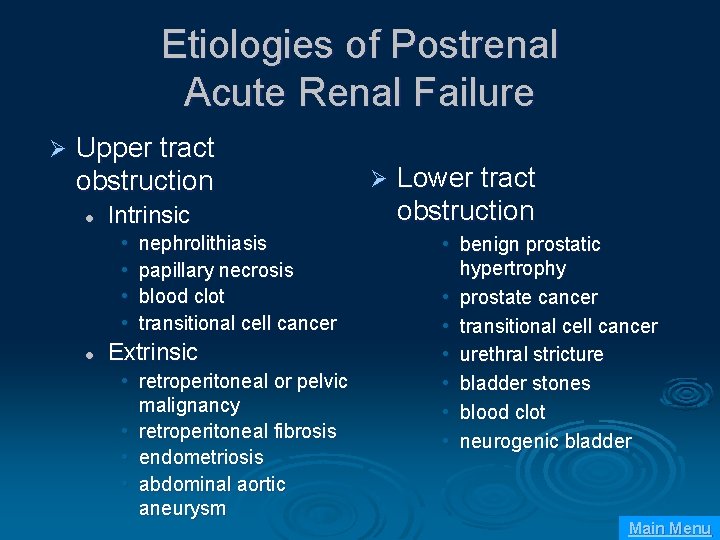
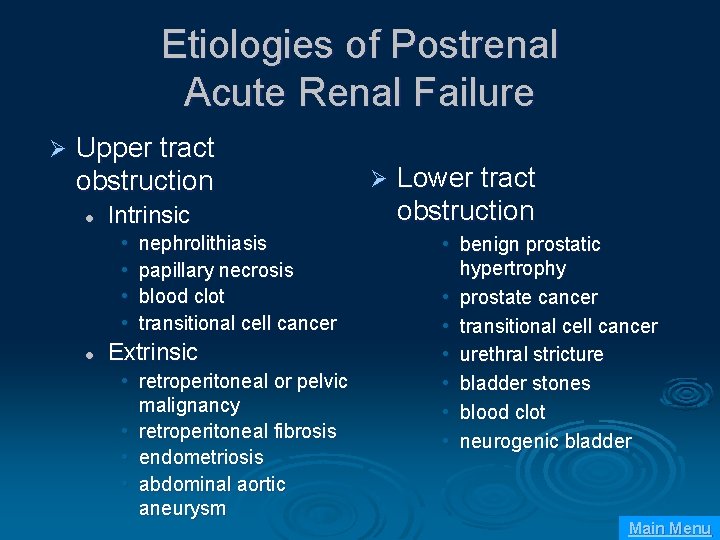
Etiologies of Postrenal Acute Renal Failure Ø Upper tract obstruction l Intrinsic • • l nephrolithiasis papillary necrosis blood clot transitional cell cancer Extrinsic • retroperitoneal or pelvic malignancy • retroperitoneal fibrosis • endometriosis • abdominal aortic aneurysm Ø Lower tract obstruction • benign prostatic hypertrophy • prostate cancer • transitional cell cancer • urethral stricture • bladder stones • blood clot • neurogenic bladder Main Menu
Postrenal Acute Renal Failure: Clinical Presentation Ø History l Symptoms of bladder outlet obstruction • • • urinary frequency urgency intermittency hesitancy nocturia incomplete voiding Main Menu
Postrenal Acute Renal Failure: Clinical Presentation Ø History l Changes in urine volume • • • l l l anuria polyuria fluctuating urine volume Flank pain Hematuria History of pelvic malignancy Main Menu
Postrenal Acute Renal Failure: Clinical Presentation Ø Physical Examination l l Suprapubic mass Prostatic enlargement Pelvic masses Adenopathy Main Menu
Postrenal Acute Renal Failure: Clinical Evaluation Ø Diagnostic studies l l l BUN: Creatinine ratio > 20: 1 Unremarkable urine sediment Variable urine chemistries Main Menu
Postrenal Acute Renal Failure: Clinical Evaluation Ø Diagnostic studies l Post-void residual bladder volume • > 100 m. L consistent with voiding dysfunction l Radiologic studies • • • Ultrasound CT scan Nuclear medicine Retrograde pyelography Antegrade nephrostograms Main Menu
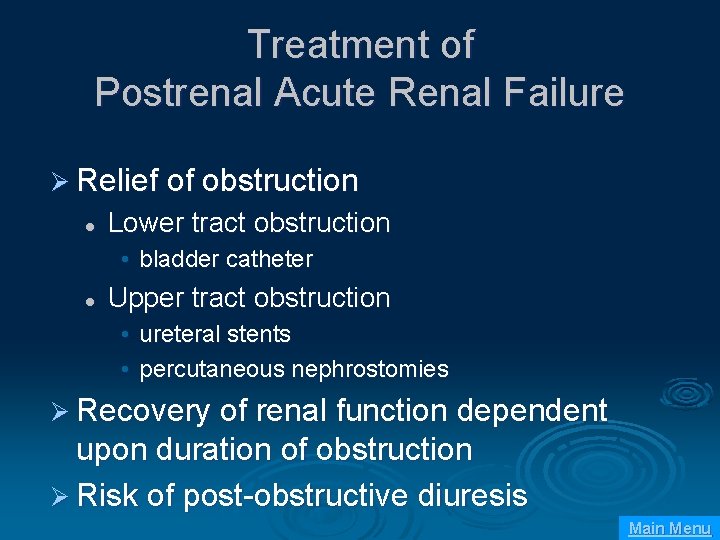
Treatment of Postrenal Acute Renal Failure Ø Relief of obstruction l Lower tract obstruction • bladder catheter l Upper tract obstruction • ureteral stents • percutaneous nephrostomies Ø Recovery of renal function dependent upon duration of obstruction Ø Risk of post-obstructive diuresis Main Menu
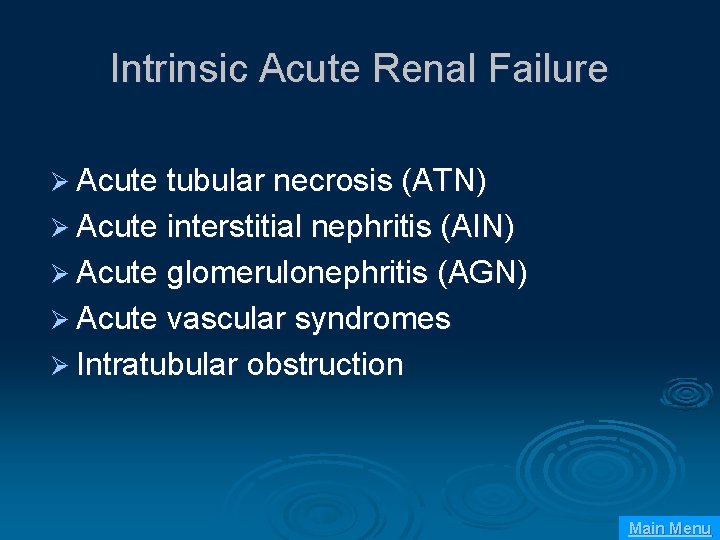
Intrinsic Acute Renal Failure Ø Acute tubular necrosis (ATN) Ø Acute interstitial nephritis (AIN) Ø Acute glomerulonephritis (AGN) Ø Acute vascular syndromes Ø Intratubular obstruction Main Menu
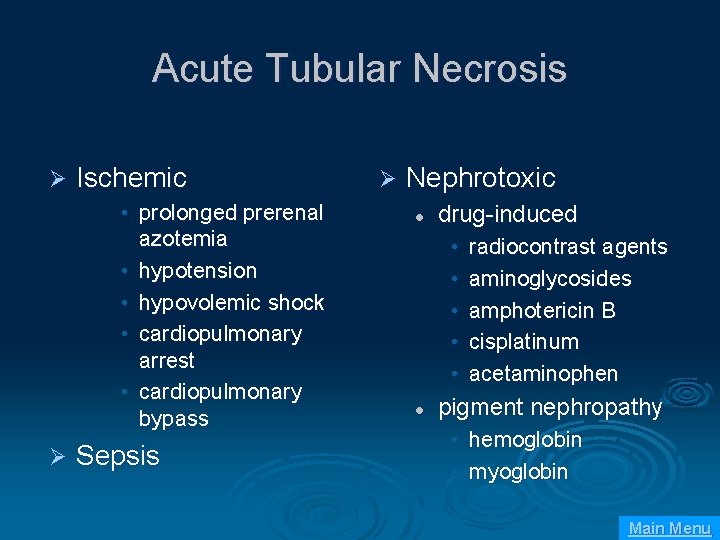
Acute Tubular Necrosis Ø Ischemic • prolonged prerenal azotemia • hypotension • hypovolemic shock • cardiopulmonary arrest • cardiopulmonary bypass Ø Sepsis Ø Nephrotoxic l drug-induced • • • l radiocontrast agents aminoglycosides amphotericin B cisplatinum acetaminophen pigment nephropathy • hemoglobin • myoglobin Main Menu
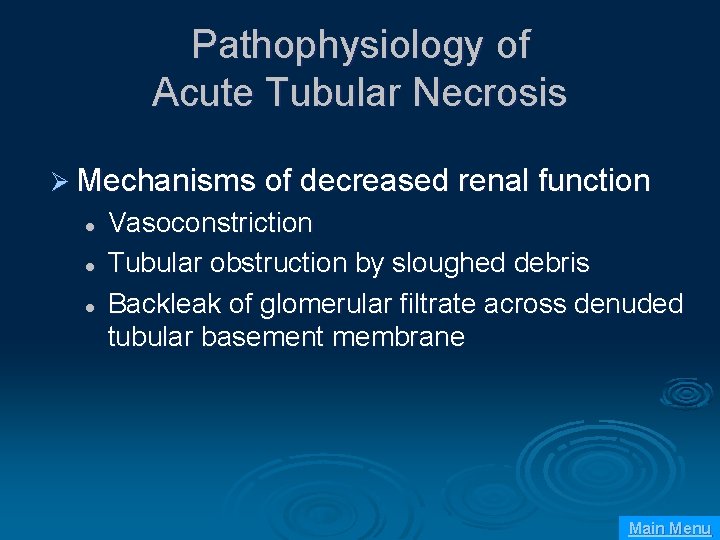
Pathophysiology of Acute Tubular Necrosis Ø Mechanisms of decreased renal function l l l Vasoconstriction Tubular obstruction by sloughed debris Backleak of glomerular filtrate across denuded tubular basement membrane Main Menu
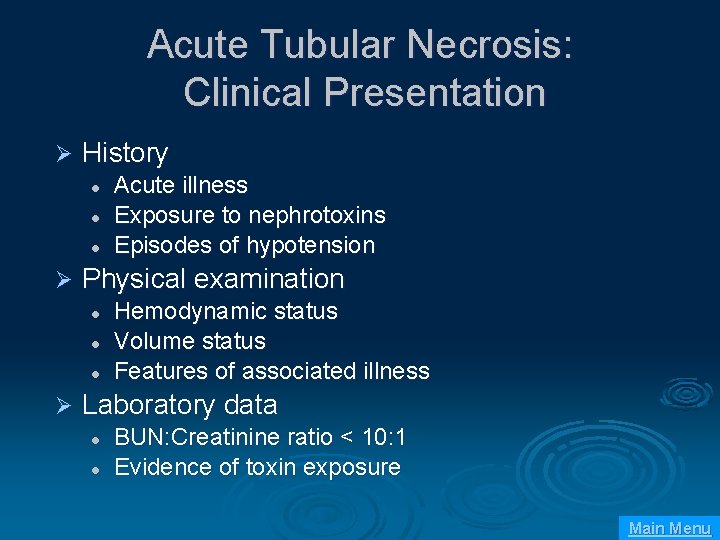
Acute Tubular Necrosis: Clinical Presentation Ø History l l l Ø Physical examination l l l Ø Acute illness Exposure to nephrotoxins Episodes of hypotension Hemodynamic status Volume status Features of associated illness Laboratory data l l BUN: Creatinine ratio < 10: 1 Evidence of toxin exposure Main Menu
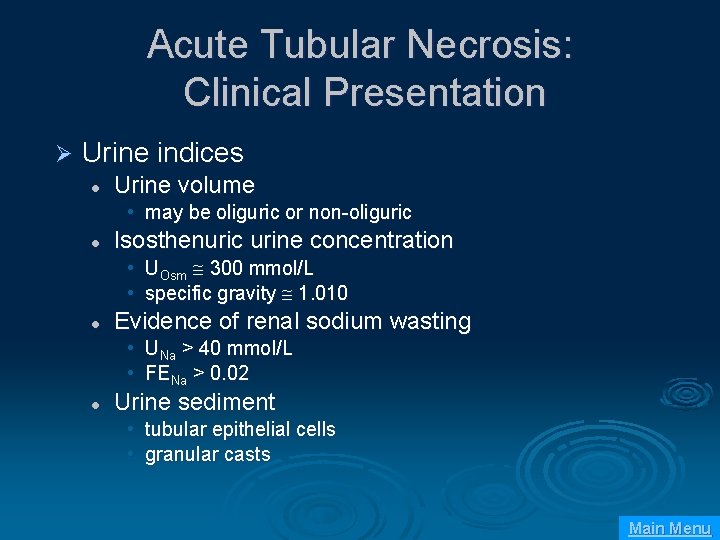
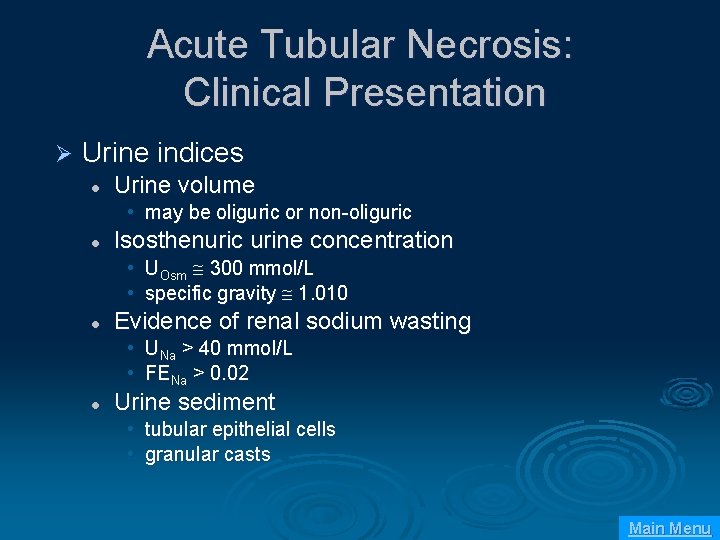
Acute Tubular Necrosis: Clinical Presentation Ø Urine indices l Urine volume • may be oliguric or non-oliguric l Isosthenuric urine concentration • UOsm 300 mmol/L • specific gravity 1. 010 l Evidence of renal sodium wasting • UNa > 40 mmol/L • FENa > 0. 02 l Urine sediment • tubular epithelial cells • granular casts Main Menu
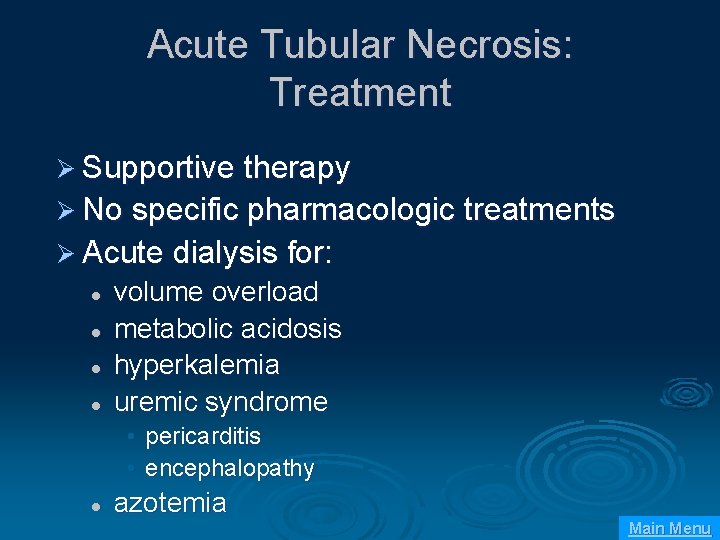
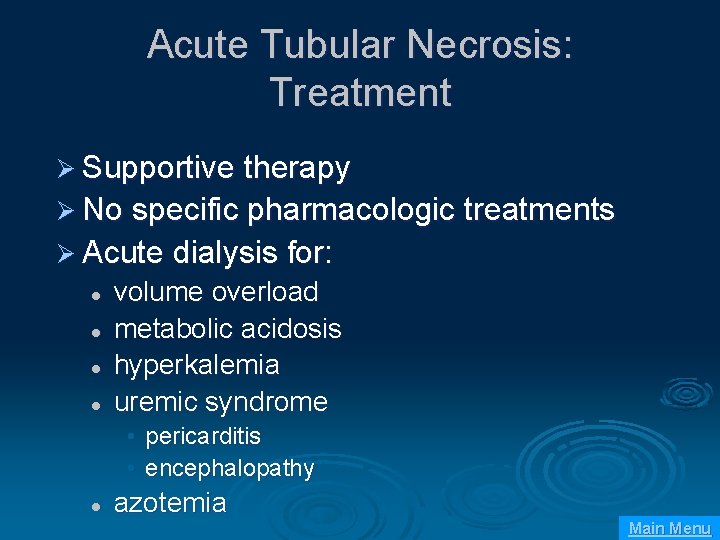
Acute Tubular Necrosis: Treatment Ø Supportive therapy Ø No specific pharmacologic treatments Ø Acute dialysis for: l l volume overload metabolic acidosis hyperkalemia uremic syndrome • pericarditis • encephalopathy l azotemia Main Menu
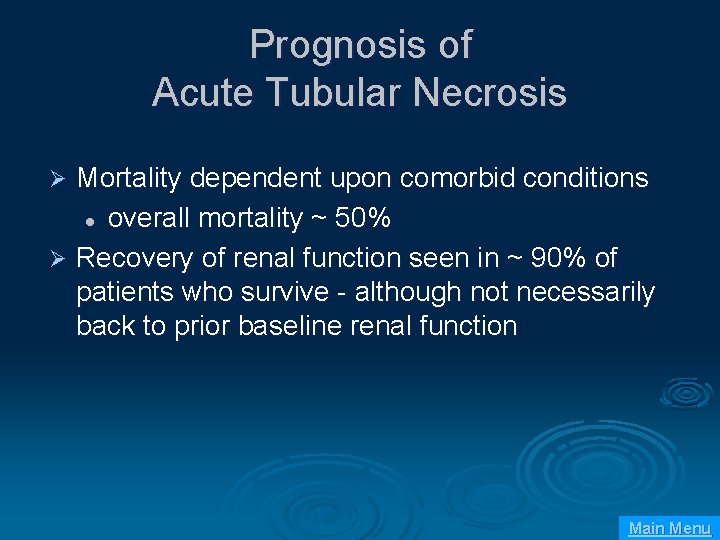
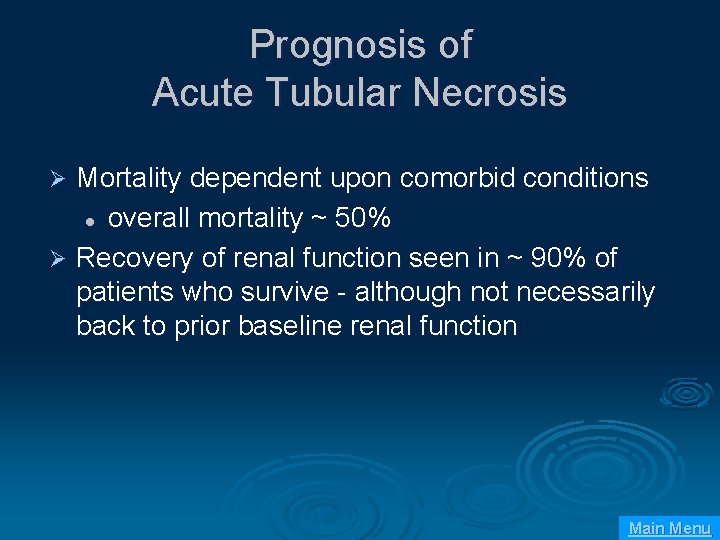
Prognosis of Acute Tubular Necrosis Mortality dependent upon comorbid conditions l overall mortality ~ 50% Ø Recovery of renal function seen in ~ 90% of patients who survive - although not necessarily back to prior baseline renal function Ø Main Menu
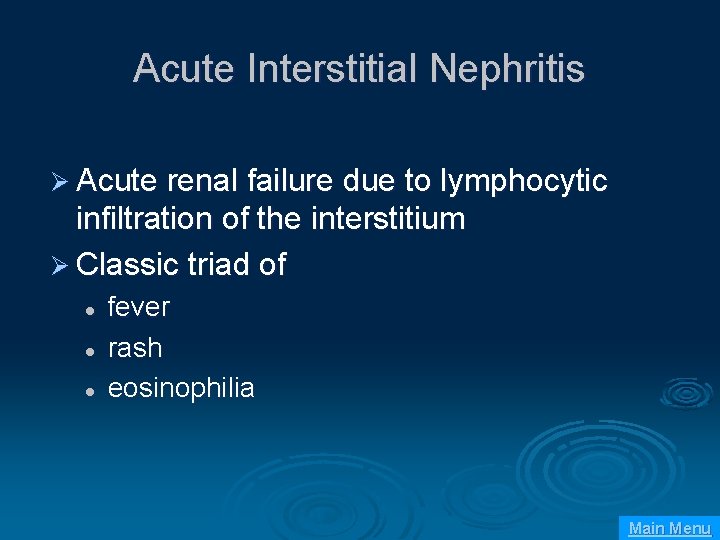
Acute Interstitial Nephritis Ø Acute renal failure due to lymphocytic infiltration of the interstitium Ø Classic triad of l l l fever rash eosinophilia Main Menu
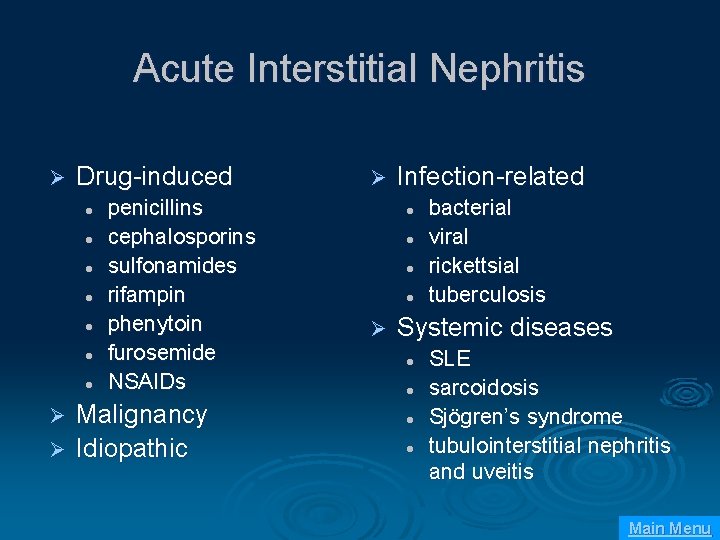
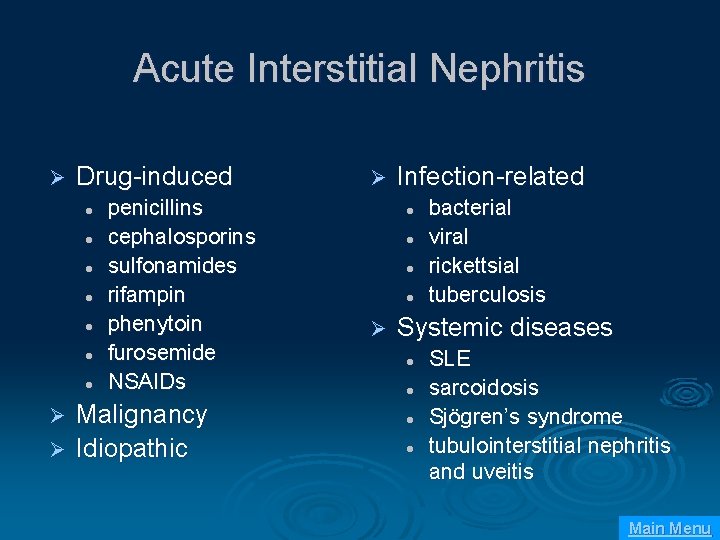
Acute Interstitial Nephritis Ø Drug-induced l l l l penicillins cephalosporins sulfonamides rifampin phenytoin furosemide NSAIDs Malignancy Ø Idiopathic Ø Ø Infection-related l l Ø bacterial viral rickettsial tuberculosis Systemic diseases l l SLE sarcoidosis Sjögren’s syndrome tubulointerstitial nephritis and uveitis Main Menu
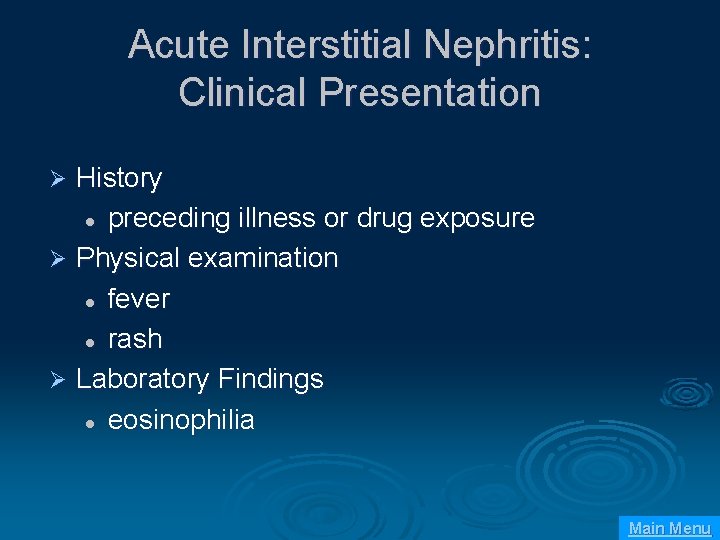
Acute Interstitial Nephritis: Clinical Presentation History l preceding illness or drug exposure Ø Physical examination l fever l rash Ø Laboratory Findings l eosinophilia Ø Main Menu

Acute Interstitial Nephritis: Clinical Presentation Ø Urine findings l non-nephrotic protinuria l hematuria l pyuria l WBC casts l eosinophiluria Main Menu
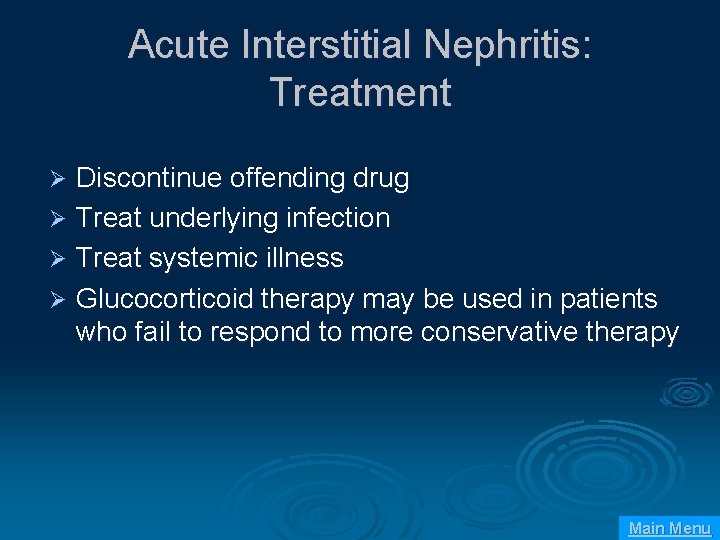
Acute Interstitial Nephritis: Treatment Discontinue offending drug Ø Treat underlying infection Ø Treat systemic illness Ø Glucocorticoid therapy may be used in patients who fail to respond to more conservative therapy Ø Main Menu
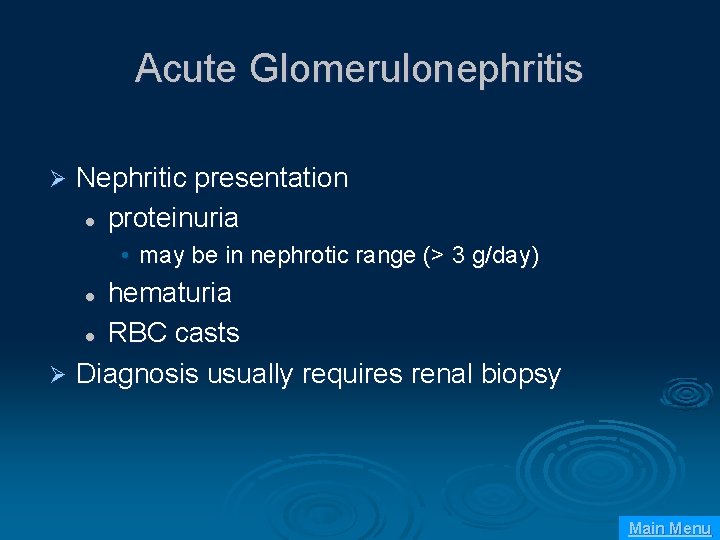
Acute Glomerulonephritis Ø Nephritic presentation l proteinuria • may be in nephrotic range (> 3 g/day) hematuria l RBC casts Ø Diagnosis usually requires renal biopsy l Main Menu
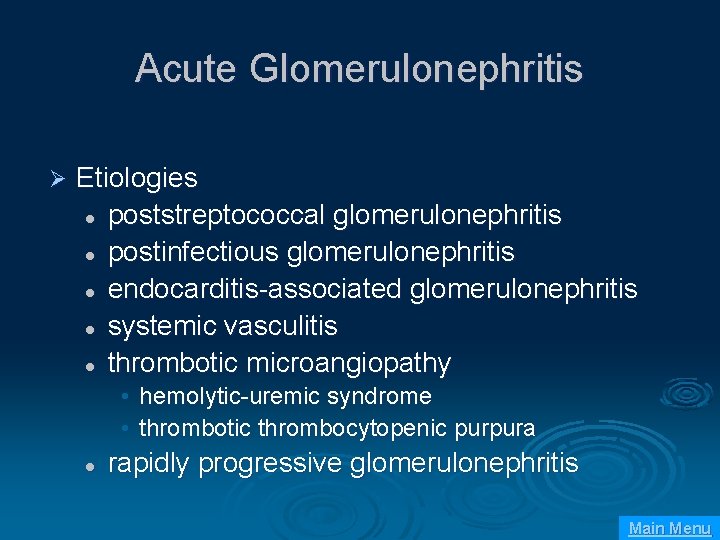
Acute Glomerulonephritis Ø Etiologies l poststreptococcal glomerulonephritis l postinfectious glomerulonephritis l endocarditis-associated glomerulonephritis l systemic vasculitis l thrombotic microangiopathy • hemolytic-uremic syndrome • thrombotic thrombocytopenic purpura l rapidly progressive glomerulonephritis Main Menu
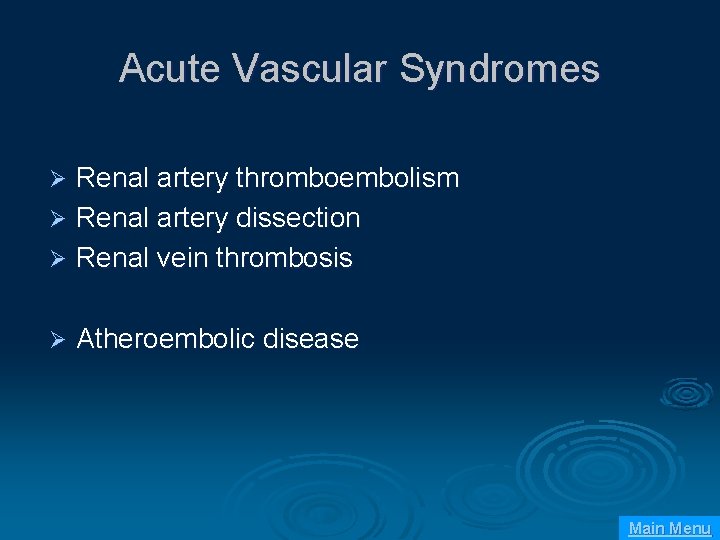
Acute Vascular Syndromes Renal artery thromboembolism Ø Renal artery dissection Ø Renal vein thrombosis Ø Ø Atheroembolic disease Main Menu

Intratubular Obstruction Ø Intratubular crystal deposition l tumor lysis syndrome • acute urate nephropathy l ethylene glycol toxicity • calcium oxylate deposition Ø Intratubular protein deposition l multiple myeloma • -Bence-Jones protein deposition Main Menu
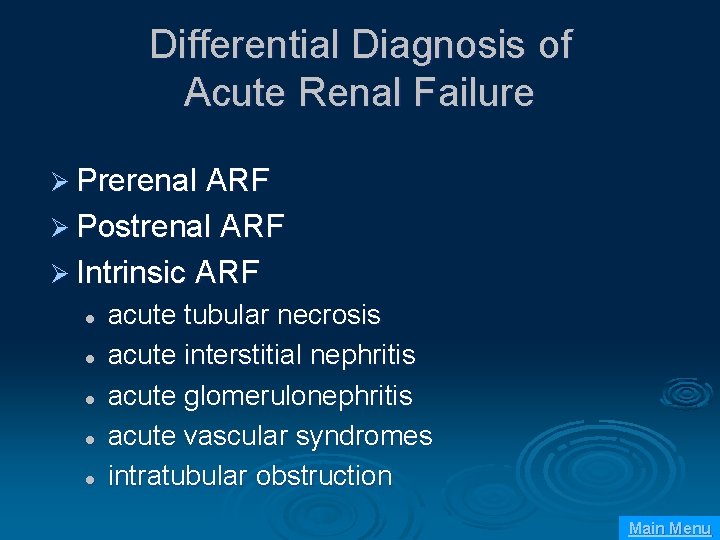
Differential Diagnosis of Acute Renal Failure Ø Prerenal ARF Ø Postrenal ARF Ø Intrinsic ARF l l l acute tubular necrosis acute interstitial nephritis acute glomerulonephritis acute vascular syndromes intratubular obstruction Main Menu
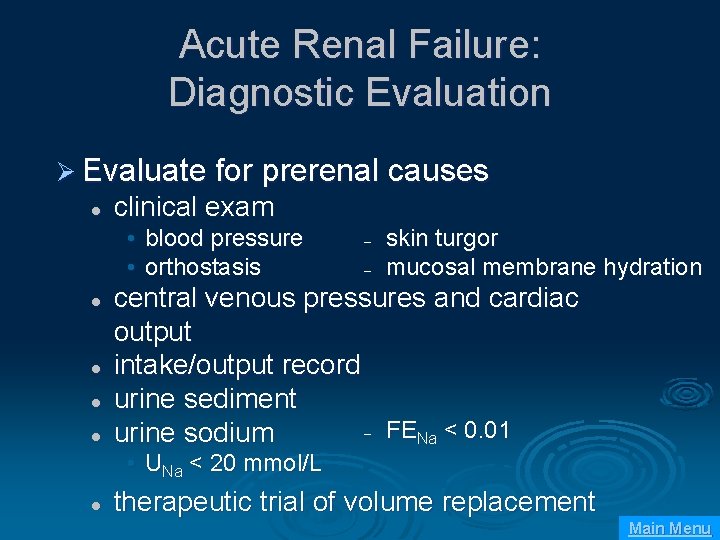
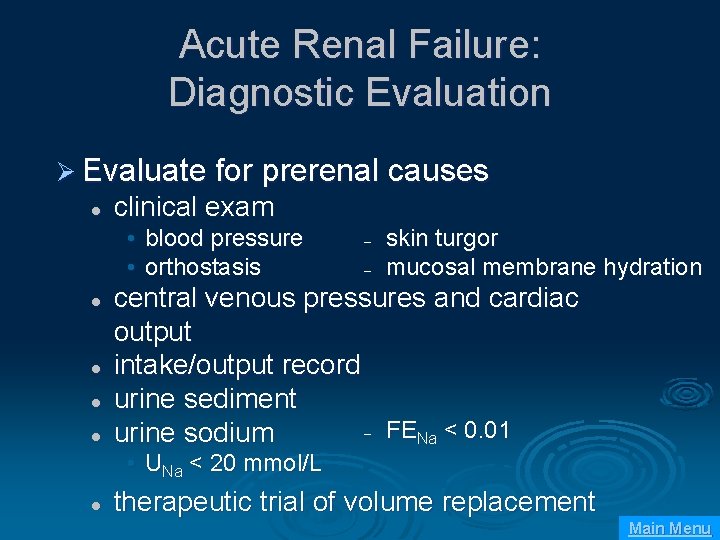
Acute Renal Failure: Diagnostic Evaluation Ø Evaluate for prerenal causes l clinical exam • blood pressure • orthostasis l l – – skin turgor mucosal membrane hydration central venous pressures and cardiac output intake/output record urine sediment – FENa < 0. 01 urine sodium • UNa < 20 mmol/L l therapeutic trial of volume replacement Main Menu
Acute Renal Failure: Diagnostic Evaluation Ø Evaluate for postrenal causes l l bladder catheterization renal ultrasound Main Menu
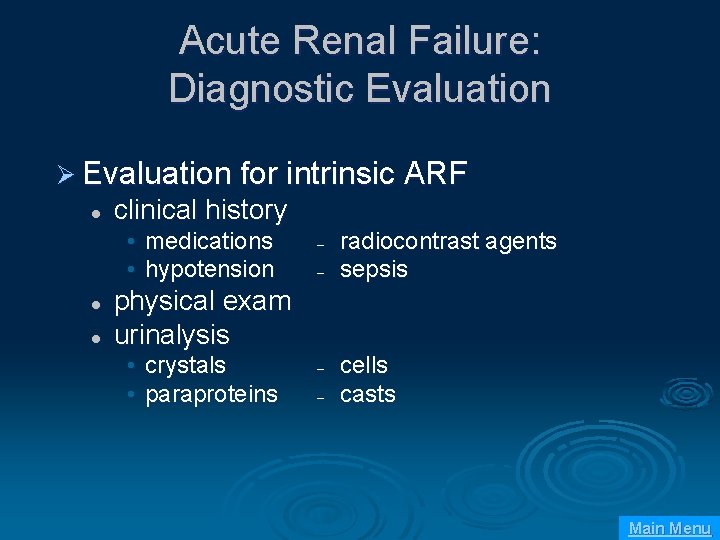
Acute Renal Failure: Diagnostic Evaluation Ø Evaluation for intrinsic ARF l clinical history • medications • hypotension l l – – radiocontrast agents sepsis physical exam urinalysis • crystals • paraproteins – – cells casts Main Menu
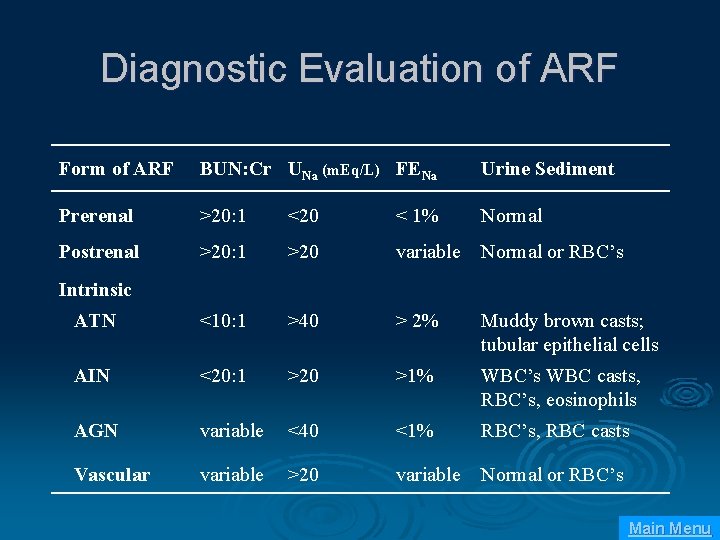
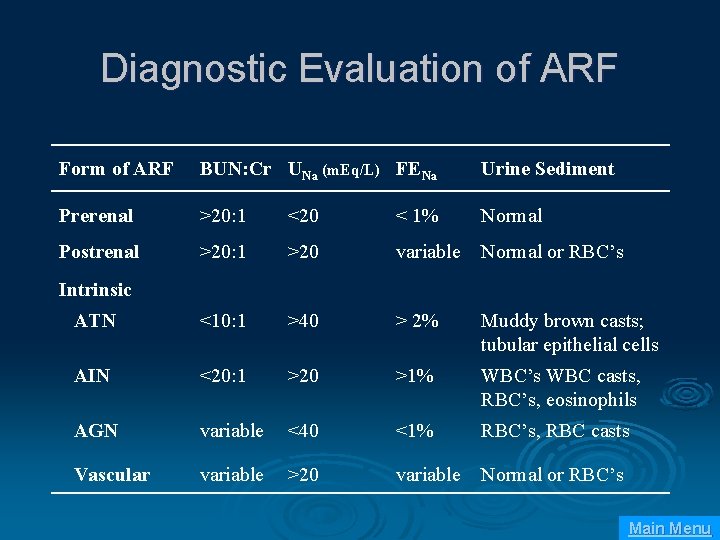
Diagnostic Evaluation of ARF Form of ARF BUN: Cr UNa (m. Eq/L) FENa Urine Sediment Prerenal >20: 1 <20 < 1% Normal Postrenal >20: 1 >20 variable Normal or RBC’s ATN <10: 1 >40 > 2% Muddy brown casts; tubular epithelial cells AIN <20: 1 >20 >1% WBC’s WBC casts, RBC’s, eosinophils AGN variable <40 <1% RBC’s, RBC casts Vascular variable >20 variable Normal or RBC’s Intrinsic Main Menu
Acute Renal Failure: Management Ø Prerenal ARF l l l volume repletion inotropic support discontinue diuretics Ø Postrenal ARF l l l bladder catheterization percutaneous nephrostomy or ureteral stents fluid management during post-obstructive diuresis Main Menu
Acute Renal Failure: Management Ø Intrinsic ARF l General supportive care • • fluid management diuretics bicarbonate supplementation potassium phosphate drug dosing nutrition Main Menu
Acute Renal Failure: Management Ø Indications for dialysis l l volume overload metabolic acidosis hyperkalemia uremic syndrome • pericarditis • encephalopathy l azotemia Main Menu
Dialysis Indications Ø Refractory hyperkalemia Ø Metabolic acidosis Ø Volume overload Ø Mental status changes Main Menu
CHRONIC RENAL FAILURE Main Menu
Pathophysiology of CRF What is Chronic Renal Failure? It is progressive tissue destruction with permanent loss of nephrons and renal function. Main Menu
Risk Factors Age > 60 years Race or ethnic background African-American Hispanic American Indian Asian Ø History of exposure to chemicals/toxins Cigarette smoke Heavy metals Ø Family history of chronic kidney disease Ø Ø Main Menu
Chronic vs. Acute Renal Failure Ø a. b. Acute Renal Failure (ARF): Abrupt onset Potentially reversible Chronic Renal Failure (CRF): Progresses over at least 3 months Permanent- non-reversible damage to nephrons Main Menu
Pathophysiology of CRF Progressive destruction of nephrons leads to: a. Decreased glomerular filtration, tubular reabsorption & renal hormone regulation b. Remaining functional nephrons compensate c. Functional and structural changes occur d. Inflammatory response triggered e. Healthy glomeruli so overburdened they become stiff, sclerotic and necrotic Lippincott Williams & Wilkins (2005). Pathophysiology A 2 -1 reference for nurses (1 st ed. ) Ambler, Pa. : Lippincott Williams & Wilkins Main Menu
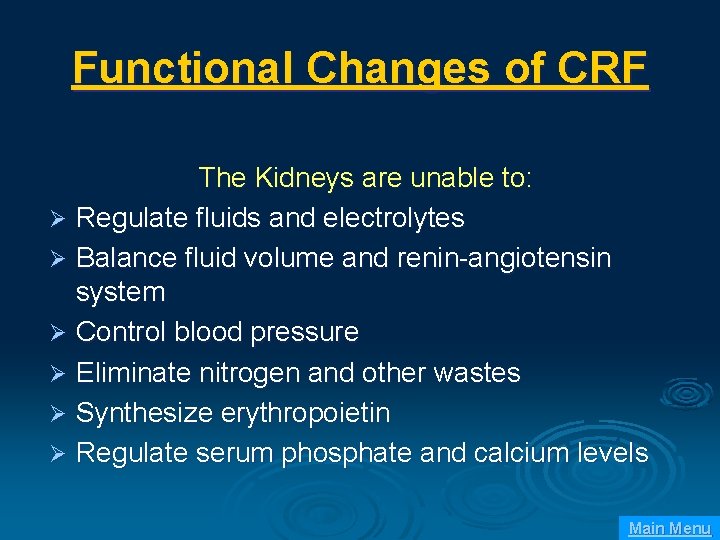
Functional Changes of CRF The Kidneys are unable to: Ø Regulate fluids and electrolytes Ø Balance fluid volume and renin-angiotensin system Ø Control blood pressure Ø Eliminate nitrogen and other wastes Ø Synthesize erythropoietin Ø Regulate serum phosphate and calcium levels Main Menu
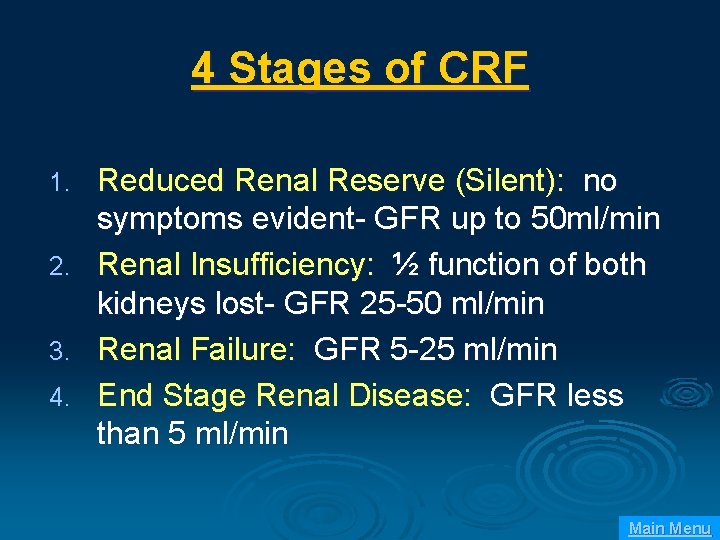
4 Stages of CRF 1. 2. 3. 4. Reduced Renal Reserve (Silent): no symptoms evident- GFR up to 50 ml/min Renal Insufficiency: ½ function of both kidneys lost- GFR 25 -50 ml/min Renal Failure: GFR 5 -25 ml/min End Stage Renal Disease: GFR less than 5 ml/min Main Menu
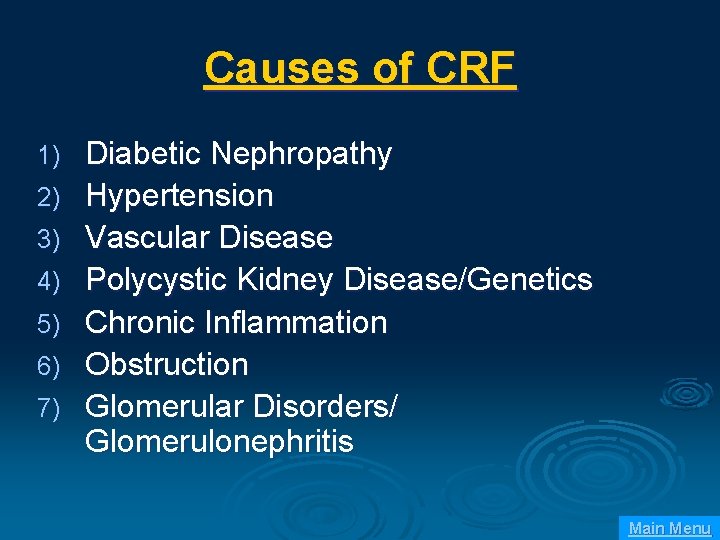
Causes of CRF 1) 2) 3) 4) 5) 6) 7) Diabetic Nephropathy Hypertension Vascular Disease Polycystic Kidney Disease/Genetics Chronic Inflammation Obstruction Glomerular Disorders/ Glomerulonephritis Main Menu
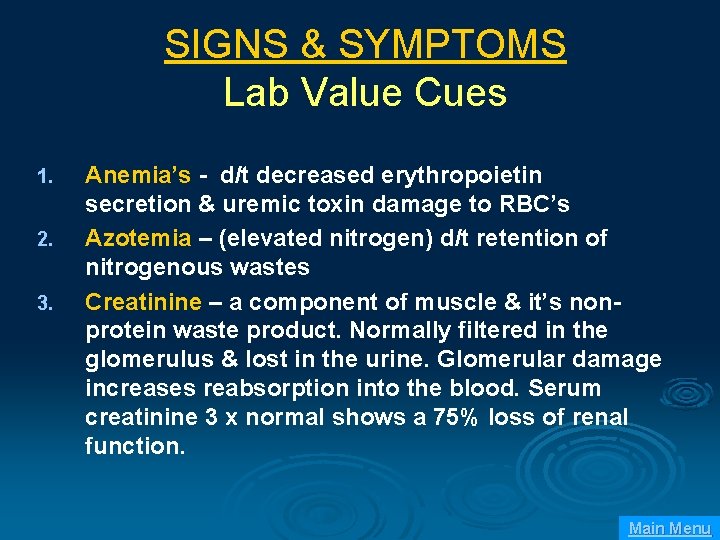
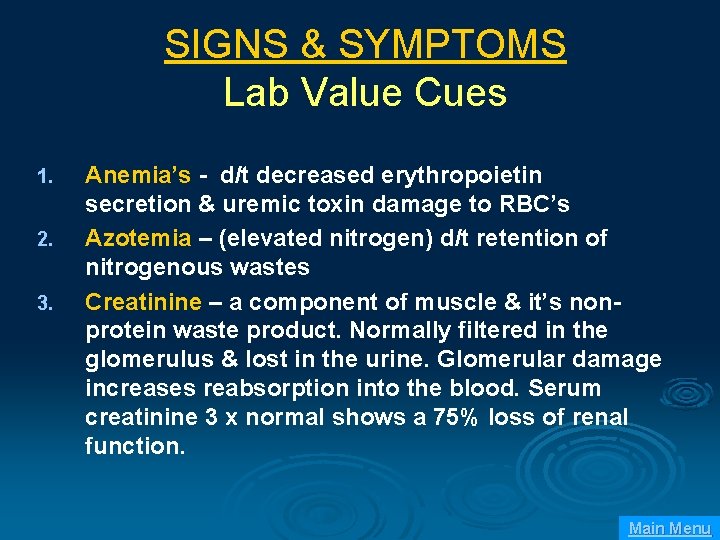
SIGNS & SYMPTOMS Lab Value Cues 1. 2. 3. Anemia’s - d/t decreased erythropoietin secretion & uremic toxin damage to RBC’s Azotemia – (elevated nitrogen) d/t retention of nitrogenous wastes Creatinine – a component of muscle & it’s nonprotein waste product. Normally filtered in the glomerulus & lost in the urine. Glomerular damage increases reabsorption into the blood. Serum creatinine 3 x normal shows a 75% loss of renal function. Main Menu
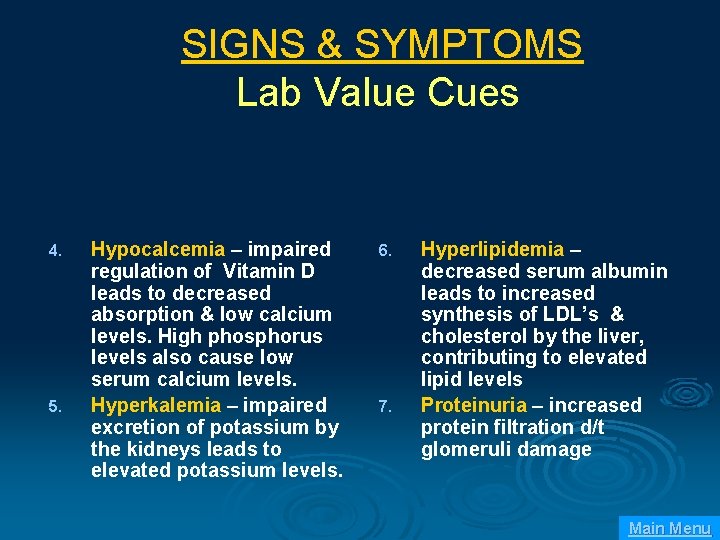
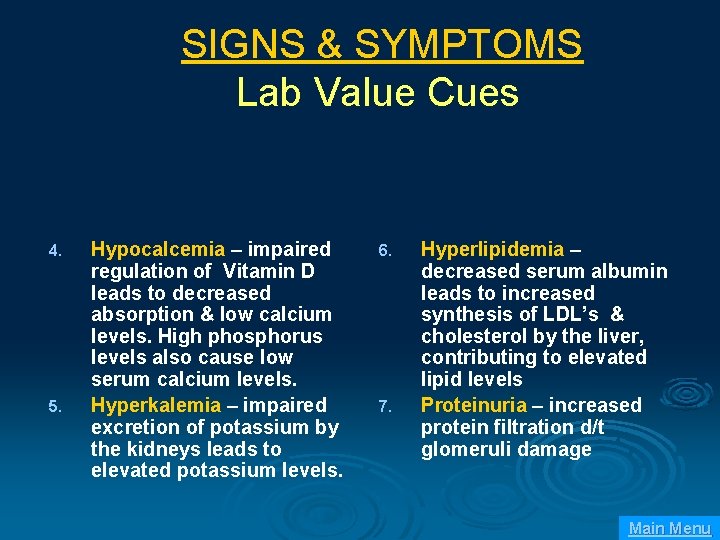
SIGNS & SYMPTOMS Lab Value Cues 4. 5. Hypocalcemia – impaired regulation of Vitamin D leads to decreased absorption & low calcium levels. High phosphorus levels also cause low serum calcium levels. Hyperkalemia – impaired excretion of potassium by the kidneys leads to elevated potassium levels. 6. 7. Hyperlipidemia – decreased serum albumin leads to increased synthesis of LDL’s & cholesterol by the liver, contributing to elevated lipid levels Proteinuria – increased protein filtration d/t glomeruli damage Main Menu
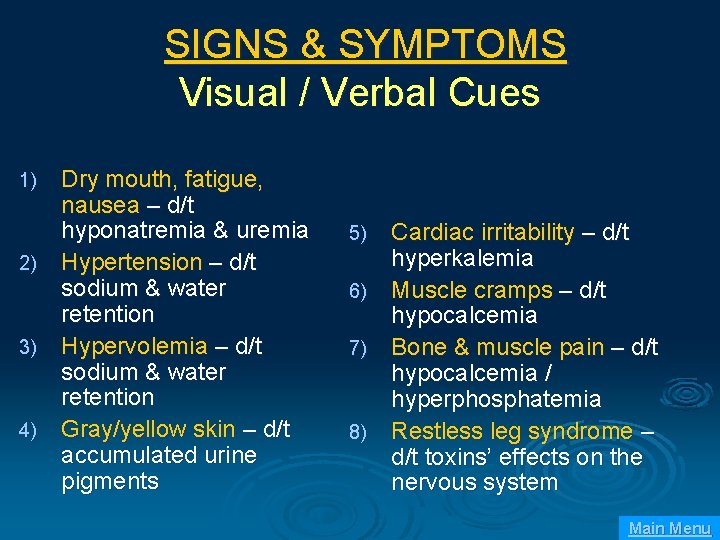
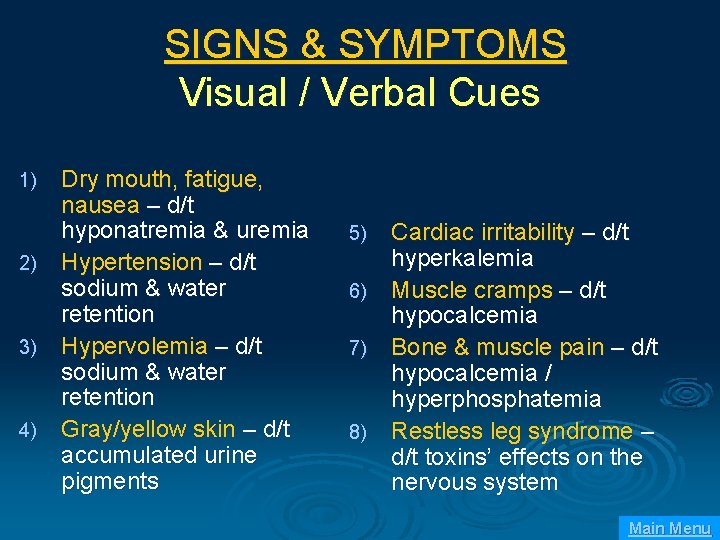
SIGNS & SYMPTOMS Visual / Verbal Cues Dry mouth, fatigue, nausea – d/t hyponatremia & uremia 2) Hypertension – d/t sodium & water retention 3) Hypervolemia – d/t sodium & water retention 4) Gray/yellow skin – d/t accumulated urine pigments 1) Cardiac irritability – d/t hyperkalemia 6) Muscle cramps – d/t hypocalcemia 7) Bone & muscle pain – d/t hypocalcemia / hyperphosphatemia 8) Restless leg syndrome – d/t toxins’ effects on the nervous system 5) Main Menu
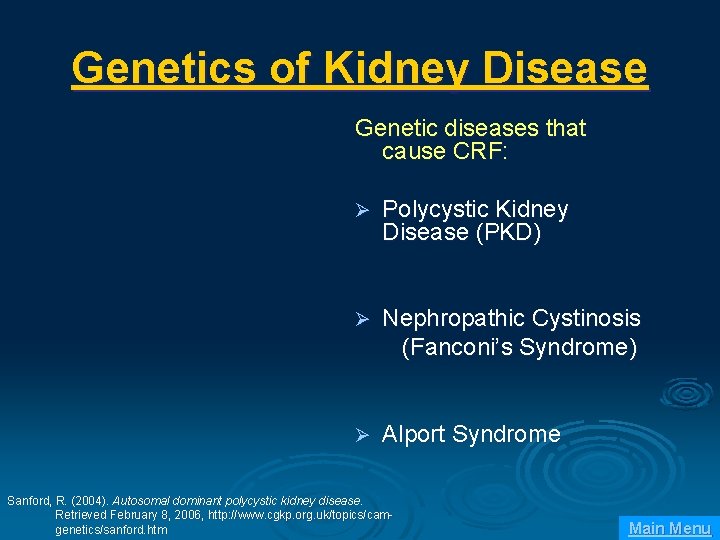
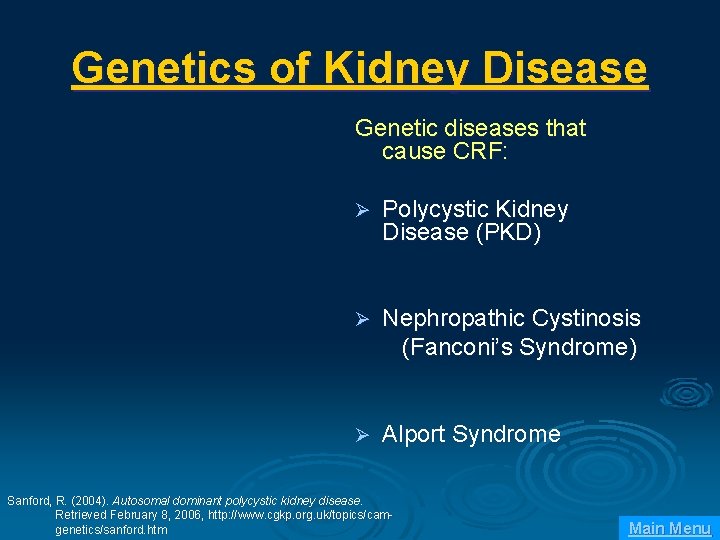
Genetics of Kidney Disease Genetic diseases that cause CRF: Ø Polycystic Kidney Disease (PKD) Ø Nephropathic Cystinosis (Fanconi’s Syndrome) Ø Alport Syndrome Sanford, R. (2004). Autosomal dominant polycystic kidney disease. Retrieved February 8, 2006, http: //www. cgkp. org. uk/topics/camgenetics/sanford. htm Main Menu
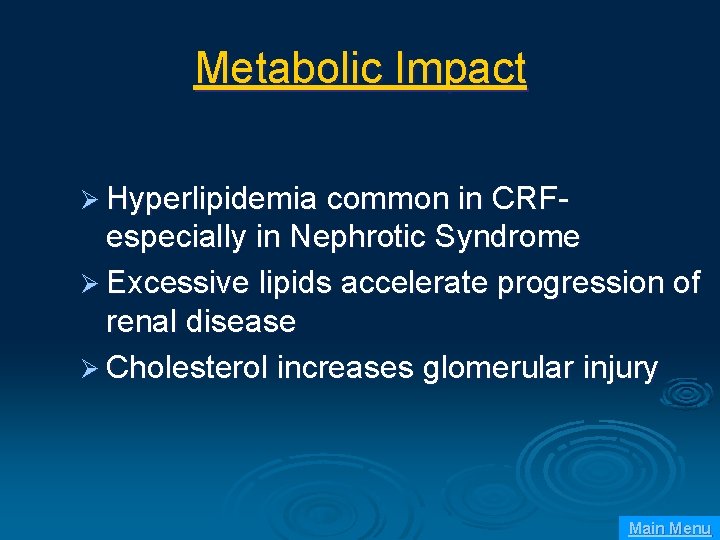
Metabolic Impact Ø Hyperlipidemia common in CRF- especially in Nephrotic Syndrome Ø Excessive lipids accelerate progression of renal disease Ø Cholesterol increases glomerular injury Main Menu
Contributing Mechanisms Two known paths of hyperlipidemia progression in CRF: Ø Hyperlipidemia activates LDL receptors in mesangial cells Ø Increased synthesis of lipoproteins in the liver related to increased albumin production Main Menu
Albumin Contribution Normal glomeruli structure limits proteins from filtering through the urine Ø Ø Ø Progression of glomeruli injury leads to increased capillary filtration of albumin The liver compensates and increases albumin production - to replace albumin lost in urine This leads to increased synthesis of lipoproteins by the liver secondary to the compensatory increase in albumin production. Results in increased LDL levels – predisposing to atherosclerosis Atherosclerosis further increases glomeruli injury Main Menu
Inflammation Ø Inflammatory response can be triggered by: tissue injury, infections, toxins, immune responses and/or Angiotensin II Ø Can be acute or chronic Ø Can affect the renal pelvis and interstitial tissue as in pyelonephritis Ø Can affect the glomeruli as in glomerulonephritis Main Menu
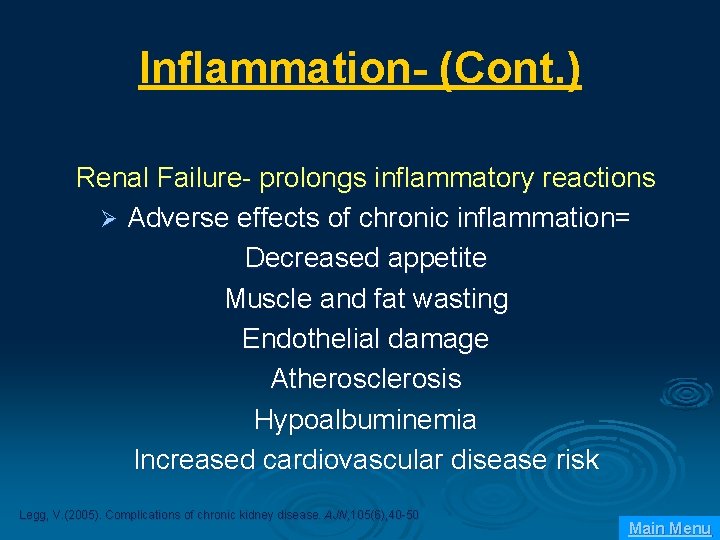
Inflammation- (Cont. ) Renal Failure- prolongs inflammatory reactions Ø Adverse effects of chronic inflammation= Decreased appetite Muscle and fat wasting Endothelial damage Atherosclerosis Hypoalbuminemia Increased cardiovascular disease risk Legg, V. (2005). Complications of chronic kidney disease. AJN, 105(6), 40 -50 Main Menu
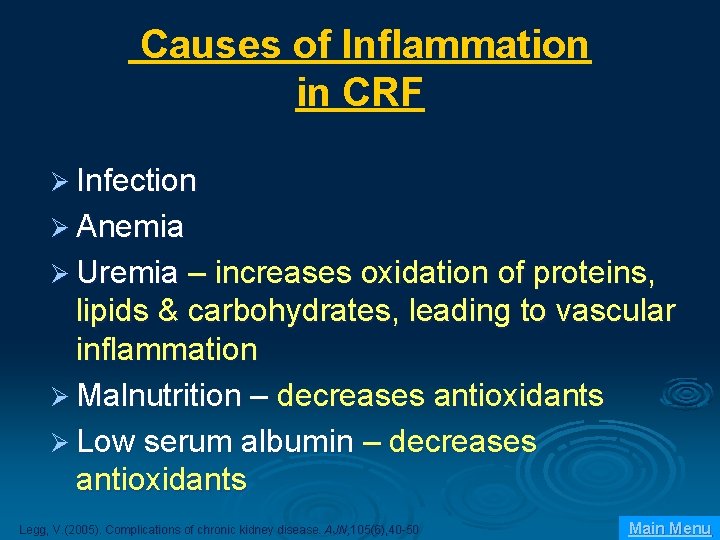
Causes of Inflammation in CRF Ø Infection Ø Anemia Ø Uremia – increases oxidation of proteins, lipids & carbohydrates, leading to vascular inflammation Ø Malnutrition – decreases antioxidants Ø Low serum albumin – decreases antioxidants Legg, V. (2005). Complications of chronic kidney disease. AJN, 105(6), 40 -50 Main Menu
Angiotensin II in the Inflammatory Process Inflammatory mediator causing: • • • Increased vascular permeability Increased leukocyte infiltration (monocytes, macrophages) Cell proliferation & hypertrophy Main Menu
Glomerular Inflammatory Disorders Reminder: The glomeruli filter blood & form urine filtrate. The selectively permeable, capillary membrane allows H 2 O and small particles (i. e. glucose) to leave the capillary membrane. Large particles (i. e. proteins & blood cells) stay in the blood. Main Menu
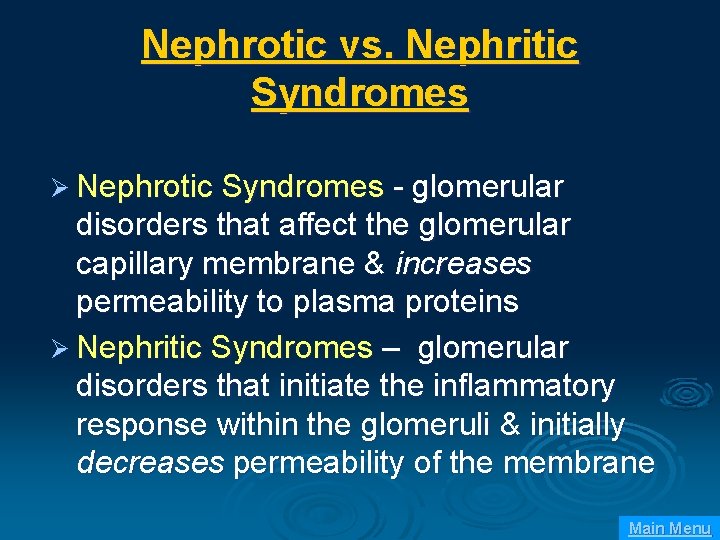
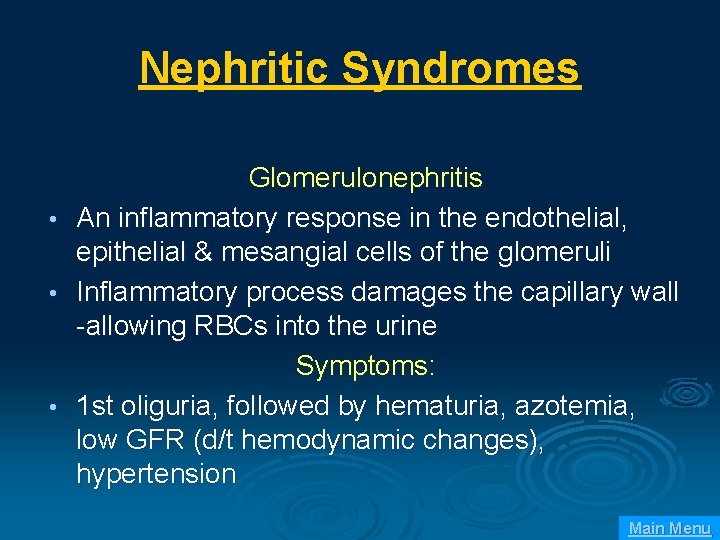
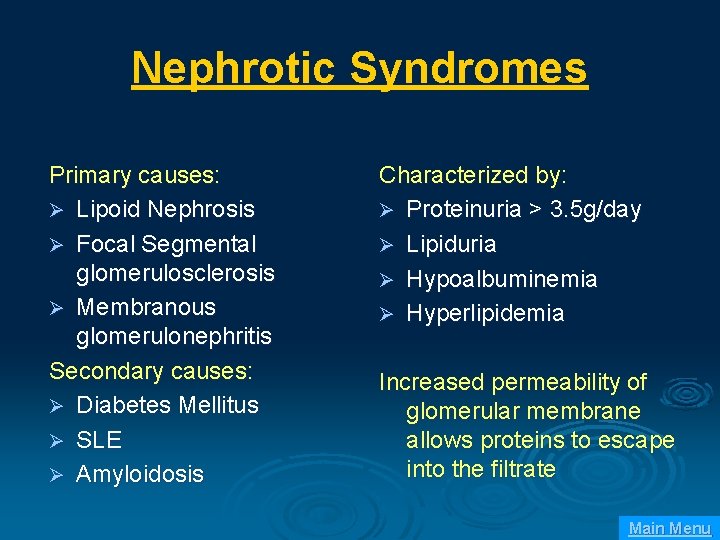
Nephrotic vs. Nephritic Syndromes Ø Nephrotic Syndromes - glomerular disorders that affect the glomerular capillary membrane & increases permeability to plasma proteins Ø Nephritic Syndromes – glomerular disorders that initiate the inflammatory response within the glomeruli & initially decreases permeability of the membrane Main Menu
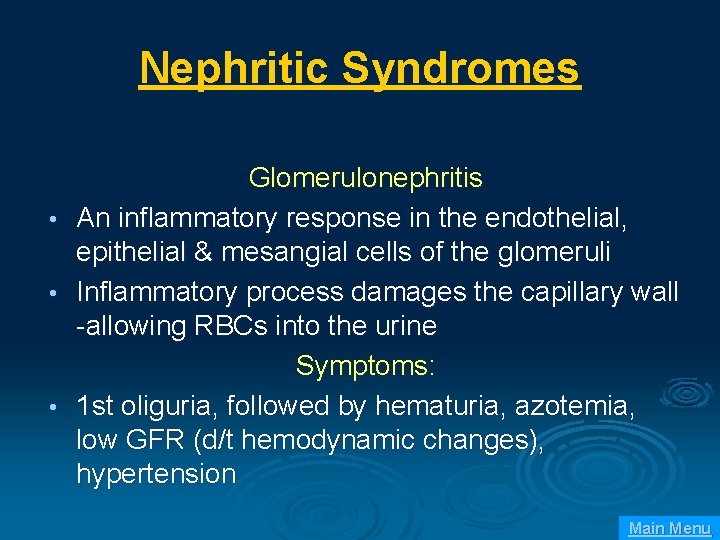
Nephritic Syndromes • • • Glomerulonephritis An inflammatory response in the endothelial, epithelial & mesangial cells of the glomeruli Inflammatory process damages the capillary wall -allowing RBCs into the urine Symptoms: 1 st oliguria, followed by hematuria, azotemia, low GFR (d/t hemodynamic changes), hypertension Main Menu
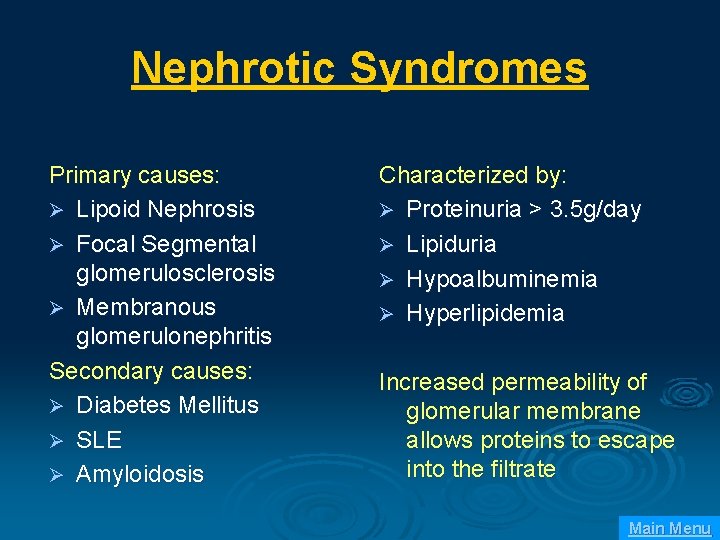
Nephrotic Syndromes Primary causes: Ø Lipoid Nephrosis Ø Focal Segmental glomerulosclerosis Ø Membranous glomerulonephritis Secondary causes: Ø Diabetes Mellitus Ø SLE Ø Amyloidosis Characterized by: Ø Proteinuria > 3. 5 g/day Ø Lipiduria Ø Hypoalbuminemia Ø Hyperlipidemia Increased permeability of glomerular membrane allows proteins to escape into the filtrate Main Menu
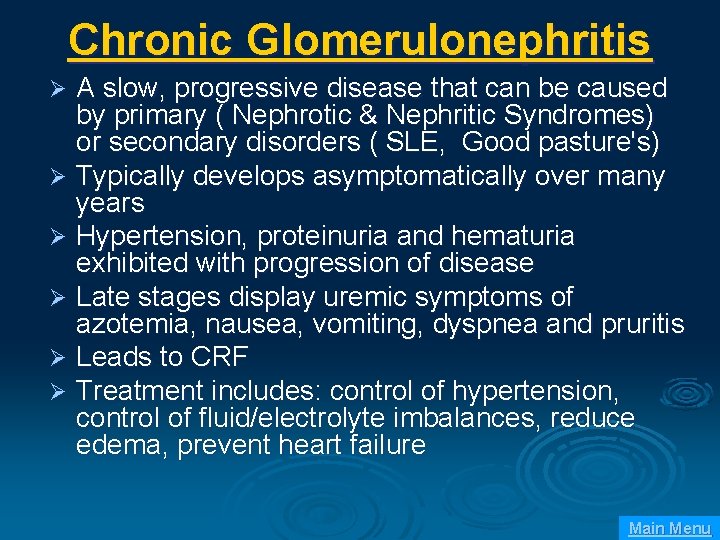
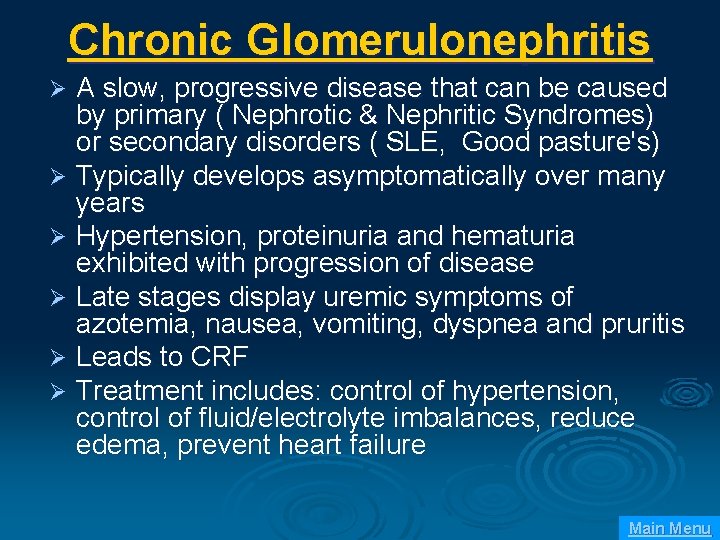
Chronic Glomerulonephritis A slow, progressive disease that can be caused by primary ( Nephrotic & Nephritic Syndromes) or secondary disorders ( SLE, Good pasture's) Ø Typically develops asymptomatically over many years Ø Hypertension, proteinuria and hematuria exhibited with progression of disease Ø Late stages display uremic symptoms of azotemia, nausea, vomiting, dyspnea and pruritis Ø Leads to CRF Ø Treatment includes: control of hypertension, control of fluid/electrolyte imbalances, reduce edema, prevent heart failure Ø Main Menu
Pharmacology in CRF Pharmacokinetics – drug absorption, distribution, metabolism & excretion Pharmacodynamics – A drug’s mechanism of action and effect at the target site Main Menu
Alterations in Drug Responses in CRF Gastrointestinal impairments affect absorption of medications Ø Volume of distribution (Vd) – the availability of a drug distributed in body tissues is increased or decreased by alterations in body composition or protein binding Ø Metabolism of medications altered -the kidneys produce many enzymes involved in drug metabolism including cytochrome P-450 Ø Decreased glomerular filtration rate affects drug excretion Ø Campoy, S, Elwell, R. (2005). Pharmacology & CKD. AJN, 105(9), 60 -72. Main Menu
Medication Considerations in CRF Dilantin – increased Vd related to protein binding changes and low albumin, increasing risk of drug toxicity Ø Digoxin – increased Vd leading to toxicity due to decreased renal excretion Ø Insulin – metabolism of insulin decreases, requiring dose reduction Ø Tylenol and procainamide – liver metabolized drugs with metabolites that are excreted renally, can accumulate leading to drug toxicity Ø Campoy, S, Elwell, R. (2005). Pharmacology & CKD. AJN, 105(9), 60 -72. Main Menu
Medication Considerations (Cont. ) Impaired renal excretion leads to toxic drug accumulations with: Aminoglycoside antibiotics (tobramycin & gentamycin) Atenolol AIEC Lithium Vancomycin Metformin Main Menu
Over-the-Counter Medications and CRF NSAIDS – inhibit prostaglandins decreasing GFR and reduced sodium excretion Antacids and laxatives (containing magnesium & aluminum) – causes mineral accumulation and metabolic complications Campoy, S, Elwell, R. (2005). Pharmacology & CKD. AJN, 105(9), 60 -72. Main Menu
Acute Problems in CRF Ø Relating to underlying disease Ø Relating to ESRD Ø Dialysis related problems Main Menu
Problems Related to ESRD Ø Metabolic – K/Ca Ø Volume overload Ø Anemia, platelet disorder, GI bleed Ø HTN, pericarditis Ø Peripheral neuropathy, dialysis dementia Ø Abnormal immune function Main Menu
Dialysis Ø ½ of patients with CRF eventually require dialysis Ø Diffuse harmful waste out of body Ø Control BP Ø Keep safe level of chemicals in body Ø 2 types l l Hemodialysis Peritoneal dialysis Main Menu
Hemodialysis Ø 3 -4 times a week Ø Takes 2 -4 hours Ø Machine filters blood and returns it to body Main Menu
Types of Access Temporary site Ø AV fistula Ø l l Ø Surgeon constructs by combining an artery and a vein 3 to 6 months to mature AV graft l l Man-made tube inserted by a surgeon to connect artery and vein 2 to 6 weeks to mature Main Menu
What This Means Ø No BP on same arm as fistula Ø Protect arm from injury Ø Control obvious hemorrhage l l Bleeding will be arterial Maintain direct pressure Ø No IV on same arm as fistula Main Menu
Access Problems Ø AV graft thrombosis Ø AV fistula or graft bleeding Ø AV graft infection Ø Steal Phenomenon l l Early post-op Ischemic distally Main Menu
Peritoneal Dialysis Ø Abdominal lining filters blood Ø 3 types l l l Continuous ambulatory Continuous cyclical Intermittent Main Menu
Dialysis Related Problems Ø Lightheaded –give fluids Ø Hypotension Ø Dysrhythmias Ø Disequilibration Syndrome l l l At end of early sessions Confusion, tremor, Due to decrease concentration of blood versus brain leading to cerebral edema Main Menu