Diverticulosis Diverticulitis Victor Politi M D FACP Medical




- Slides: 63
Diverticulosis & Diverticulitis Victor Politi, M. D. , FACP Medical Director, SVCMC School of Allied Health Physician Assistant Program
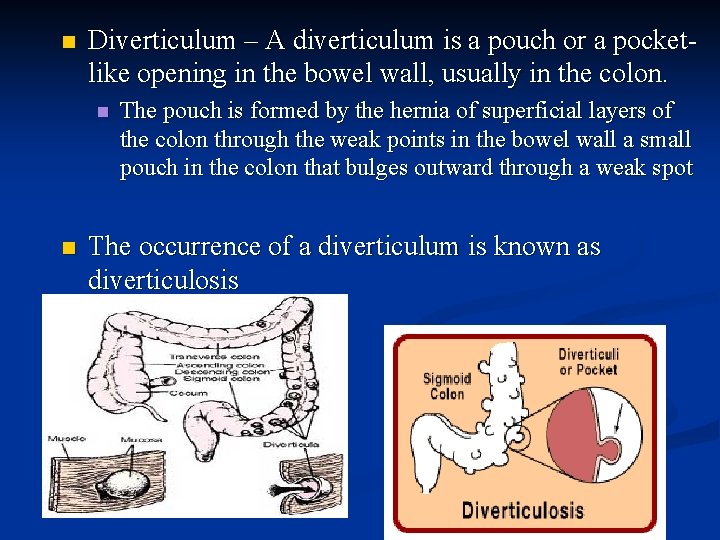
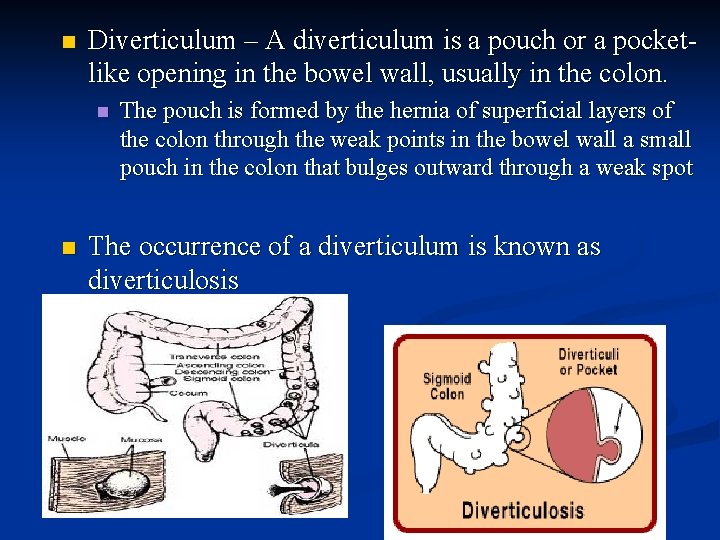
n Diverticulum – A diverticulum is a pouch or a pocketlike opening in the bowel wall, usually in the colon. n n The pouch is formed by the hernia of superficial layers of the colon through the weak points in the bowel wall a small pouch in the colon that bulges outward through a weak spot The occurrence of a diverticulum is known as diverticulosis
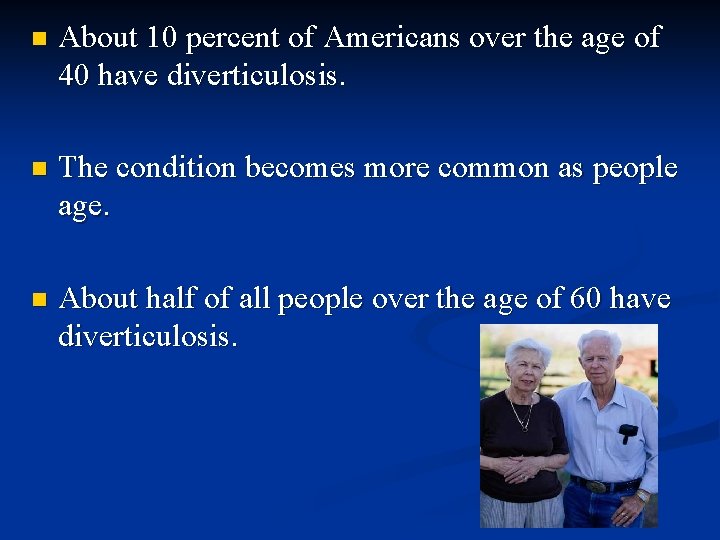
n About 10 percent of Americans over the age of 40 have diverticulosis. n The condition becomes more common as people age. n About half of all people over the age of 60 have diverticulosis.
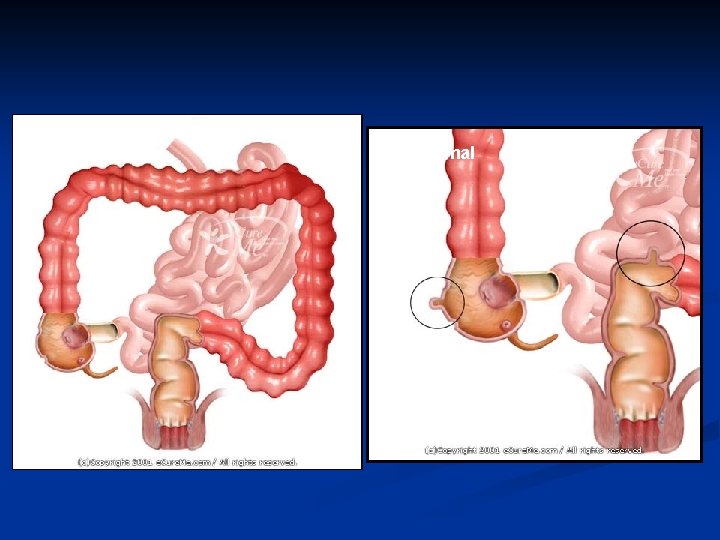
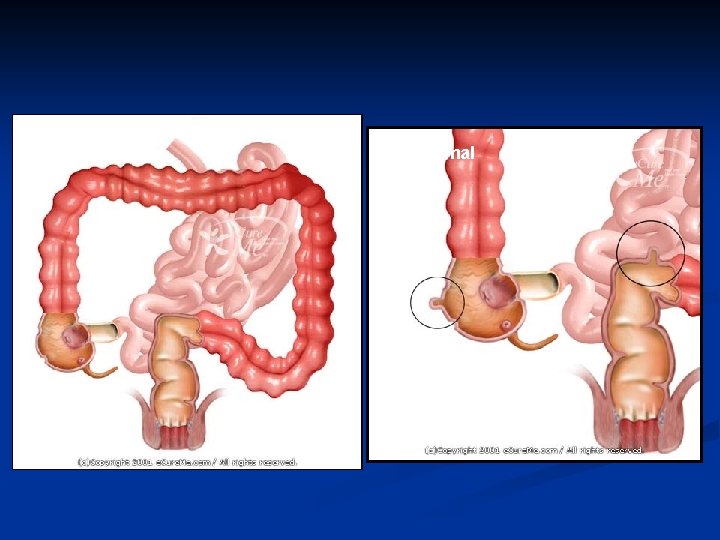
Normal Abnormal
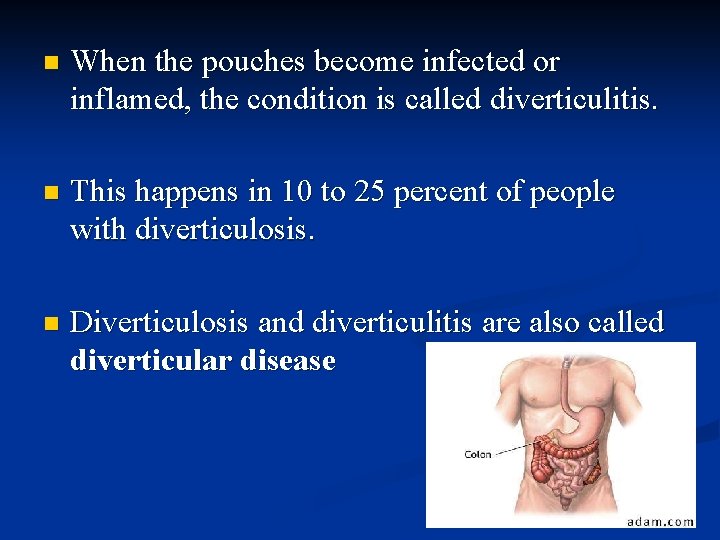
n When the pouches become infected or inflamed, the condition is called diverticulitis. n This happens in 10 to 25 percent of people with diverticulosis. n Diverticulosis and diverticulitis are also called diverticular disease
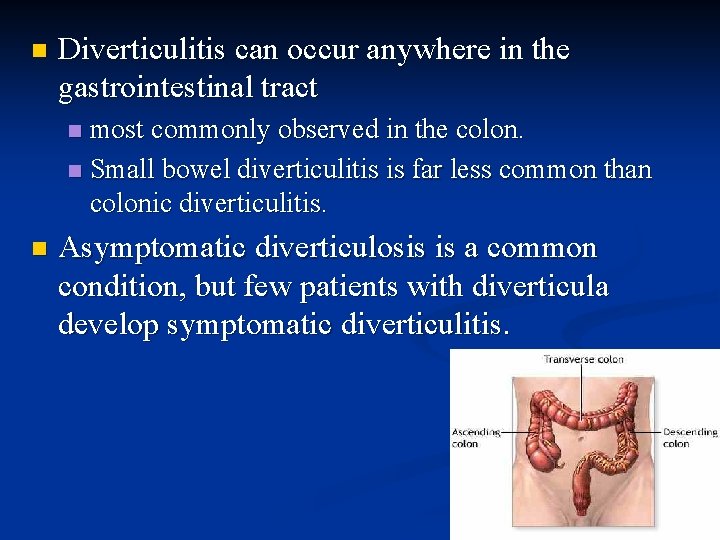
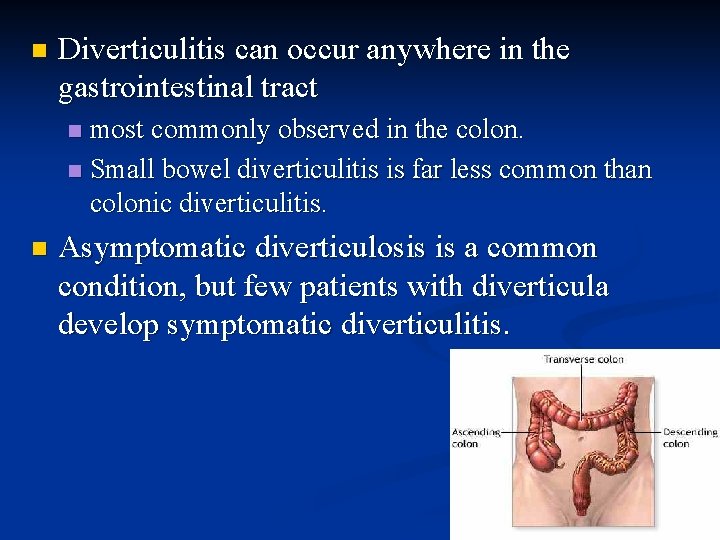
n Diverticulitis can occur anywhere in the gastrointestinal tract most commonly observed in the colon. n Small bowel diverticulitis is far less common than colonic diverticulitis. n n Asymptomatic diverticulosis is a common condition, but few patients with diverticula develop symptomatic diverticulitis.
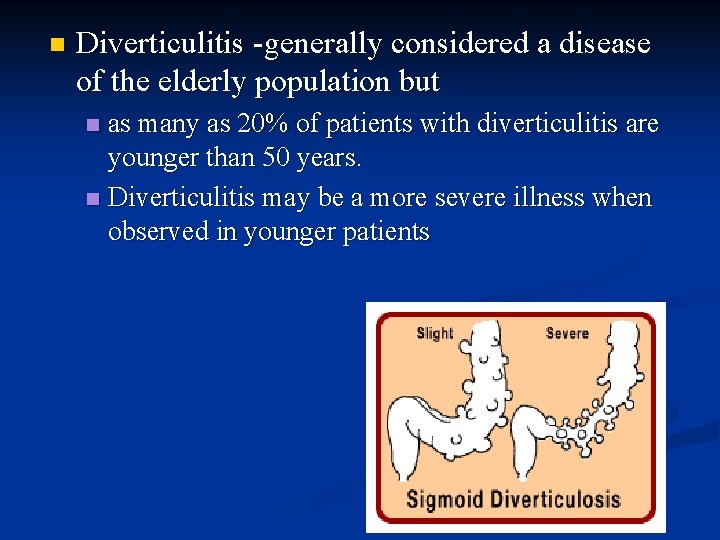
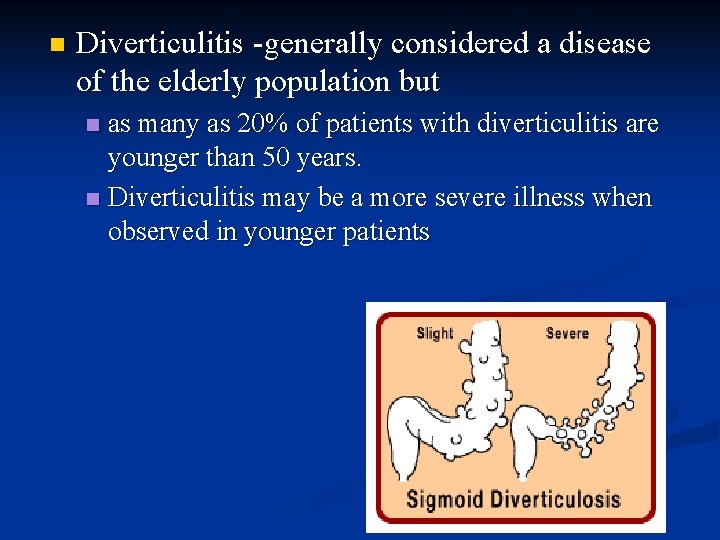
n Diverticulitis -generally considered a disease of the elderly population but as many as 20% of patients with diverticulitis are younger than 50 years. n Diverticulitis may be a more severe illness when observed in younger patients n
painful diverticular disease The diverticula are usually harmless and do not cause problems in 70 -80% of patients n Some persons may develop cramps, bloating, and irregular bowel movements without fever or other signs of infection. n These patients are believed to have "painful diverticular disease” n
painful diverticular disease n A cause-effect relationship between these symptoms and diverticulosis has not been established. n n patients usually treated with high fiber diet plus medications to relieve spasms Some of these patients may not respond to medical therapy. n Use of surgery in such patients in the absence of giant diverticula and or any of its complications is controversial
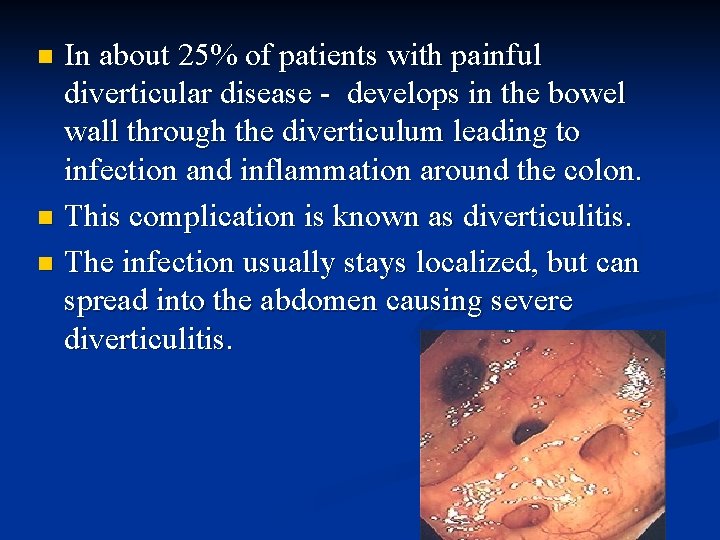
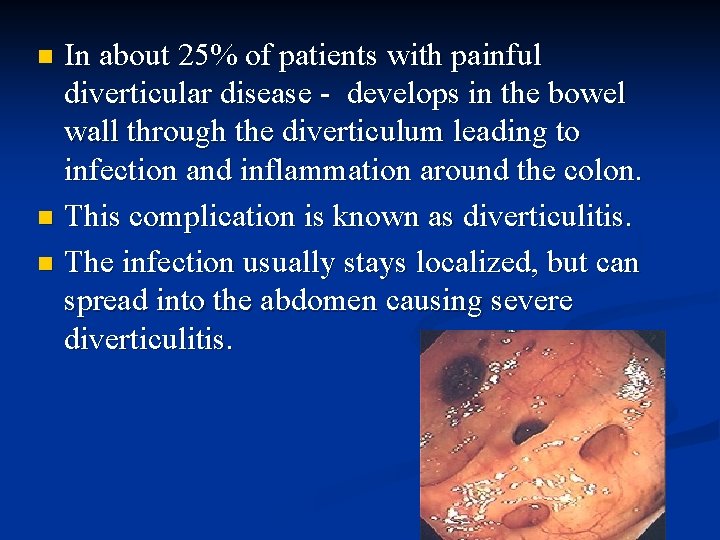
In about 25% of patients with painful diverticular disease - develops in the bowel wall through the diverticulum leading to infection and inflammation around the colon. n This complication is known as diverticulitis. n The infection usually stays localized, but can spread into the abdomen causing severe diverticulitis. n
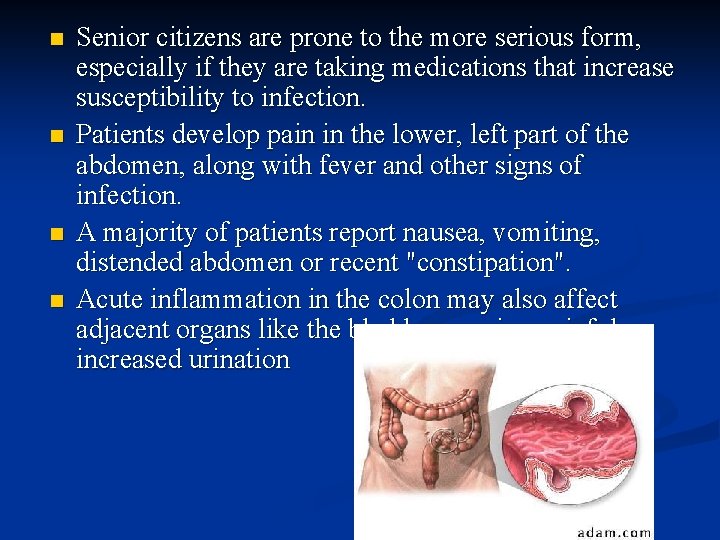
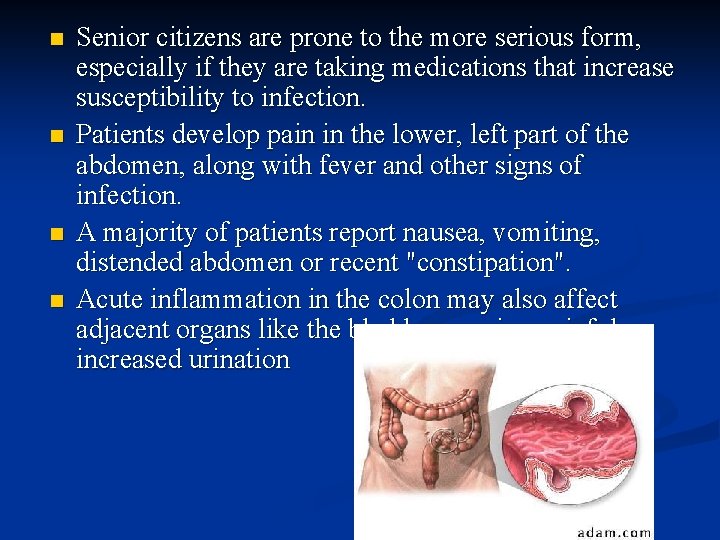
n n Senior citizens are prone to the more serious form, especially if they are taking medications that increase susceptibility to infection. Patients develop pain in the lower, left part of the abdomen, along with fever and other signs of infection. A majority of patients report nausea, vomiting, distended abdomen or recent "constipation". Acute inflammation in the colon may also affect adjacent organs like the bladder, causing painful or increased urination

What causes diverticular disease? Diverticulitis occurs when diverticula become infected or inflamed. n It is unclear as to what causes the infection. n n n It may begin when stool or bacteria are caught in the diverticula. An attack of diverticulitis can develop suddenly and without warning
What causes diverticular disease? n The etiology of diverticulitis remains unclear, n A low-fiber diet is considered a predisposing factor n Diverticular disease is common in developed or industrialized countries--particularly the United States, England, and Australia--where low-fiber diets are common. n The disease is rare in countries of Asia and Africa, where people eat high-fiber vegetable diets.
The low-fiber diet connection n Fiber is the part of fruits, vegetables, and grains that the body cannot digest. Some fiber dissolves easily in water (soluble fiber). It takes on a soft, jelly-like texture in the intestines. n Some fiber passes almost unchanged through the intestines (insoluble fiber). n
The low-fiber diet connection n Both kinds of fiber help make stools soft and easy to pass. Fiber also prevents constipation n Constipation makes the muscles strain to move stool that is too hard. It is the main cause of increased pressure in the colon. n This excess pressure might cause the weak spots in the colon to bulge out and become diverticula n
Other Possible Predisposing Factors n Aging n causes changes in collagen structure- may lead to weakening of the colonic wall. Colonic motility disorders n Long term Corticosteroid or NSAID use n Genetics n n believed to play a role, Asian people tend to have a predominance of right-sided diverticula, while Western people tend to have left-sided disease
Diverticulosis Symptoms Most people with diverticulosis do not have any discomfort or symptoms. n However, symptoms may include mild cramps, bloating, and constipation. n n Other diseases such as irritable bowel syndrome (IBS) and stomach ulcers cause similar problems, so these symptoms do not always mean a person has diverticulosis.
Diverticulitis Symptoms n n Most common symptom -abdominal pain Most common sign- tenderness around the left side of the lower abdomen n If infection is the cause, fever, nausea, vomiting, chills, cramping, and constipation may occur as well. n The severity of symptoms depends on the extent of the infection and complications
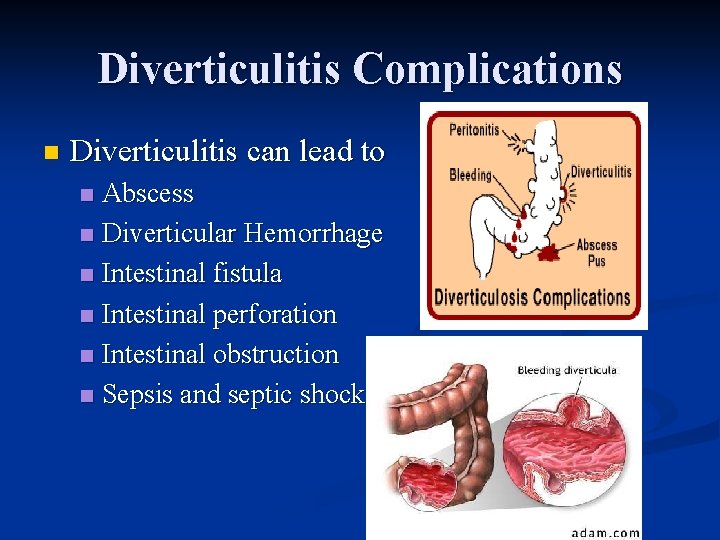
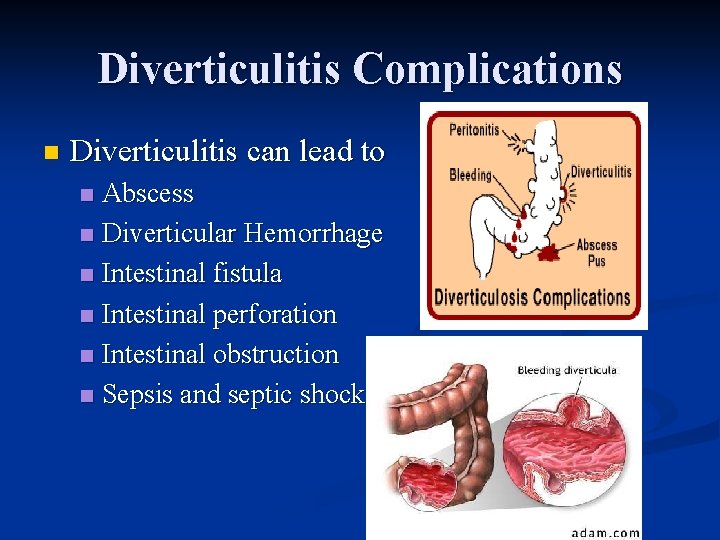
Diverticulitis Complications n Diverticulitis can lead to Abscess n Diverticular Hemorrhage n Intestinal fistula n Intestinal perforation n Intestinal obstruction n Sepsis and septic shock n
Diverticulitis Complications n Diverticular Hemorrhage rare complication 5% of cases n sudden in onset, painless and substantial -the result of a weakened blood vessel in a diverticulum bursting n Bleeding is usually not seen during an acute episode of acute diverticulitis - Diverticula bleed when they are otherwise healthy n bleeding stops spontaneously in most patients. n
Diverticulitis Complications n Diverticular Hemorrhage In some cases, the bleeding may continue intermittently for a few hours to a few days before resolving n Chronic intermittent bleeding due to diverticulosis is unusual n As many as 80% patients do not have any recurrence of bleeding. n Surgery may be needed in 50% of cases of massive diverticular bleeding. n

Diverticulitis Complications n Infection Treated with antibiotics n usually clears up after a few days of treatment n Rest the Gut n n Abscess n An abscess is an infected area with pus that may cause swelling and destroy tissue
Diverticulitis Complications n Perforationn n n Sometimes the infected diverticula may develop small holes (perforations) The perforations allow pus to leak out of the colon into the abdominal area If the abscess is small and remains in the colon, it may clear up after treatment with antibiotics. If the abscess does not clear up with antibiotics, it may require drainage (percutaneous catheter drainage) Sometimes surgery is needed to clean the abscess and, if necessary, remove part of the colon
Diverticulitis Complications n Peritonitis- (an infection of the abdominal cavity) A large abscess can become a serious problem if the infection leaks out and contaminates areas outside the colon. n Infection that spreads into the abdominal cavity is called peritonitis. n Peritonitis requires immediate surgery to clean the abdominal cavity and remove the damaged part of the colon. n Without surgery, peritonitis can be fatal. n
Diverticulitis Complications n Fistulan n n Abnormal connection of tissue between two organs or between an organ and the skin When damaged tissues come into contact with each other during infection, they sometimes stick together. If they heal that way, a fistula forms When diverticulitis-related infection spreads outside the colon, the colon's tissue may stick to nearby tissues. n The organs usually involved are the bladder, small intestine, and skin.
Diverticulitis Complications n Fistula n The most common type of fistula occurs between the bladder and the colon. Colovesicular fistula (colon to urinary bladder). n n n This is observed almost exclusively in men Also seen in women following hysterectomy This type of fistula can result in a severe, long-lasting infection of the urinary tract. Can be corrected with surgery to remove the fistula and the affected part of the colon Colovaginal and colocutaneous fistulae are much less common
Diverticulitis Complications n Intestinal Obstruction The scarring caused by infection may cause partial or total blockage of the large intestine. n When this happens, the colon is unable to move bowel contents normally. n If the obstruction totally blocks the intestine, emergency surgery is necessary n
n The diagnosis of acute diverticulitis is often made on the basis of history and physical examination, followed by confirmatory laboratory and radiologic tests
diagnosing diverticular disease n medical history n n physical exam n n digital rectal exam, occult blood, bloodwork, diagnostic tests n n bowel habits, symptoms, pain, diet, medications Imaging studies, endoscopy Most people do not have symptoms so diverticulosis is often found through tests ordered for another ailment
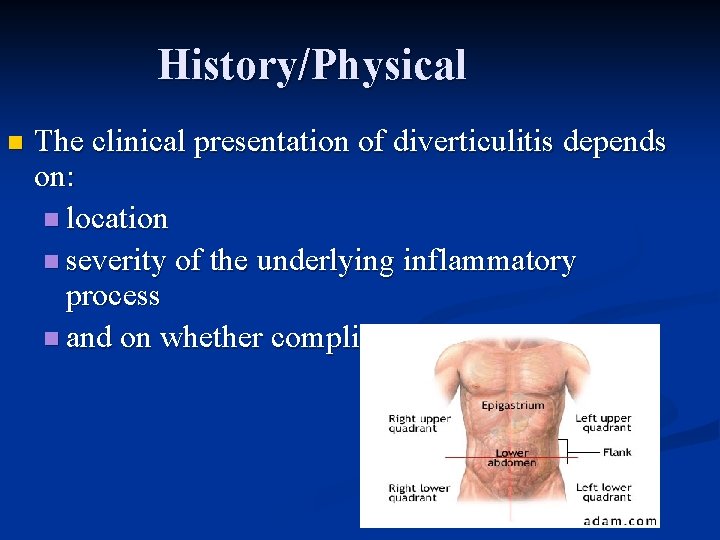
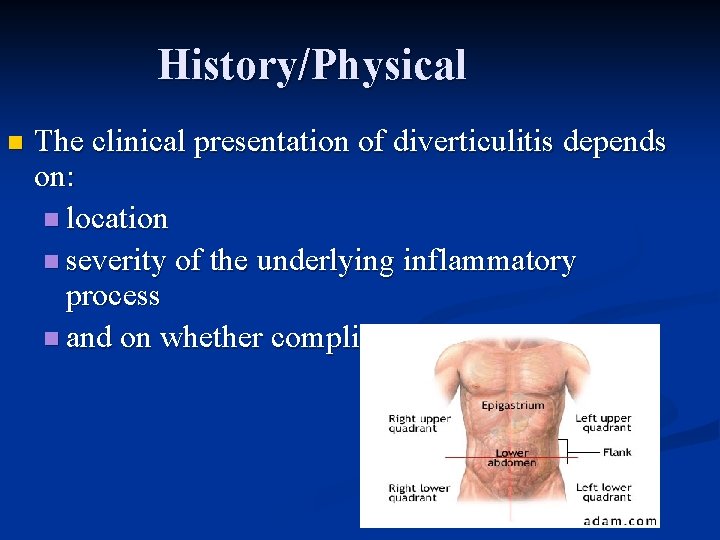
History/Physical n The clinical presentation of diverticulitis depends on: n location n severity of the underlying inflammatory process n and on whether complications are present
History/Physical n Frequent Symptoms of acute diverticulitis abdominal pain and fever n n n Usually, pain is severe, abrupt in onset, localized to the left lower abdominal quadrant, and worsens steadily over time. Sometimes referred to as left-sided appendicitis, diverticulitis is often accompanied by anorexia, nausea, and vomiting. Altered bowel habit, especially constipation, is common
History/Physical n Because diverticula and diverticulitis can develop anywhere in the gastrointestinal tract, symptoms may mimic multiple conditions.
History/Physical Diverticulitis in the transverse colon may mimic peptic ulcer disease, pancreatitis, or cholecystitis. n Diverticulitis in the right colon may be confused with acute appendicitis. n With disease progression, localized abscess and phlegmonous formation may occur. n Systemic signs of infection, such as fever and leukocytosis, become more pronounced. n
History/Physical n n n Localized peritonitis may lead to direct and rebound tenderness over the involved area. On physical examination, rebound tenderness is generally most pronounced in the left lower abdominal quadrant. The abdomen may become distended and tympanic to percussion. Bowel sounds may become diminished or absent. Sometimes, a mass may be felt at the site of the inflammation. n This may be apparent not only on abdominal palpation but also on pelvic or rectal examination
History/Physical n Elderly patients and those taking corticosteroids may have unremarkable findings on physical examination, even in the presence of severe diverticulitis. n Such patients must be approached with a high index of suspicion, in order to avoid a significant delay in arriving at the correct diagnosis.
History/Physical n Hematochezia, or bright red blood per rectum, is not a symptom of diverticulitis, although occult blood in the stool is present in approximately 25% of patients with diverticulitis. n When hematochezia is noted, other causes (eg, hemorrhoids, neoplastic disease, colitis, vascular ectasias, arterial bleeding from diverticulosis) should be considered
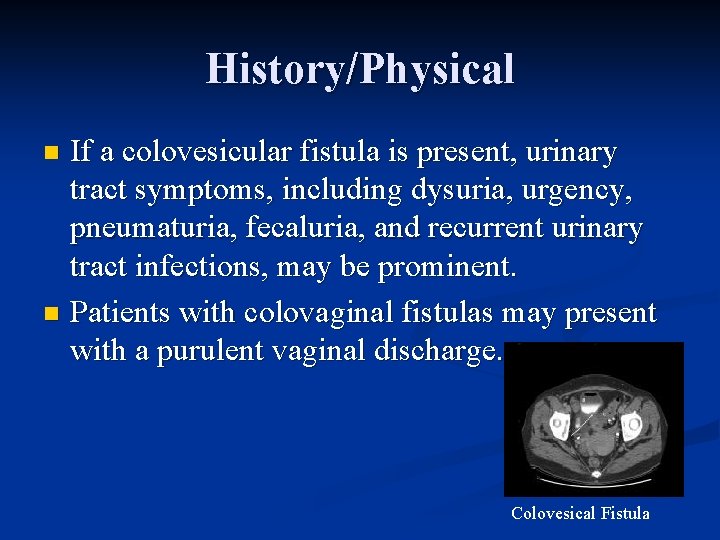
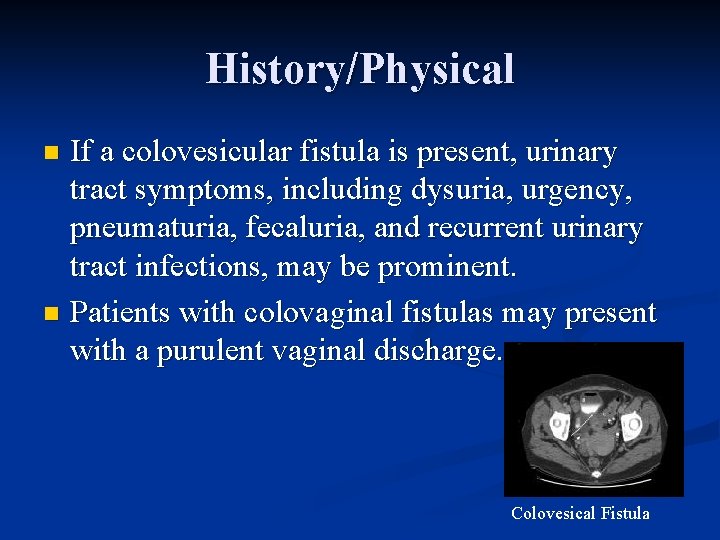
History/Physical If a colovesicular fistula is present, urinary tract symptoms, including dysuria, urgency, pneumaturia, fecaluria, and recurrent urinary tract infections, may be prominent. n Patients with colovaginal fistulas may present with a purulent vaginal discharge. n Colovesical Fistula
History/Physical n Leg pain, possibly associated with thigh abscess, and leg emphysema secondary to retroperitoneal perforation from diverticulitis have been reported.

Lab Studies n Routine laboratory data are important to confirm the presence of infection and to exclude other possible etiologies of abdominal pain.
Lab Studies n CBC -identifies leukocytosis and/or a left shift. n n However, 20 -40% of patients may have a white blood cell count in the reference range, particularly patients who are immunocompromised and elderly. Chemistries Liver function tests and amylase/lipase may help exclude other causes of abdominal pain, especially in atypical presentations or generalized peritonitis. n Serum electrolyte findings can help detect important abnormalities in cases of sepsis or GI bleeding. n
Lab Studies Blood cultures should be obtained prior to administration of empiric antimicrobial therapy. n Urinalysis and urine cultures n to identify urinary tract infection n In the presence of a colovesicular fistulan n urinary cultures may reveal a polymicrobial infection
Imaging Studies X-rays to make sure the colon has not perforated n CT scan with contrast of the abdomen/pelvis if the diagnosis is unclear n Flexible Sigmoidoscopy and Barium enema only after symptoms are improved (if these tests are done too early, they can cause a colon perforation) n
Imaging Studies n On plain radiograph, an abdominal series with flat and upright abdominal films may show an obstruction, ileus, or free air, indicating visceral perforation. Radiopaque gallbladder or renal stones may also be observed
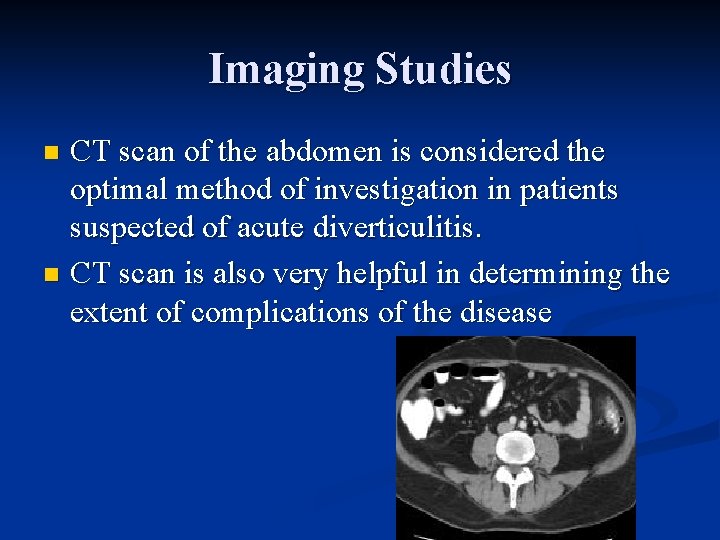
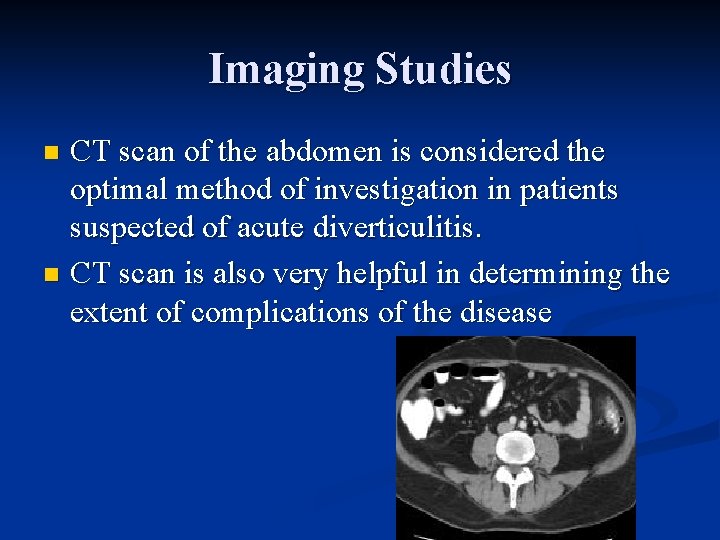
Imaging Studies CT scan of the abdomen is considered the optimal method of investigation in patients suspected of acute diverticulitis. n CT scan is also very helpful in determining the extent of complications of the disease n
Procedures n Endoscopy is not usually used in the evaluation of acute episodes of diverticulitis because of the possibility of perforation and subsequent development of peritonitis
Treatment of diverticulitis n Treatment for diverticulitis focuses on: clearing up the infection and inflammation n resting the colon (bed rest, liquid diet, pain meds as n needed) n preventing or minimizing complications n An attack of diverticulitis without complications may respond to antibiotics within a few days if treated early.
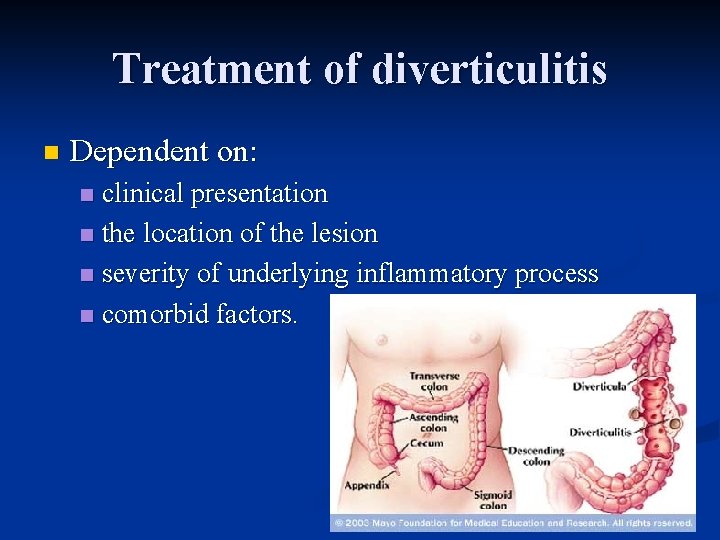
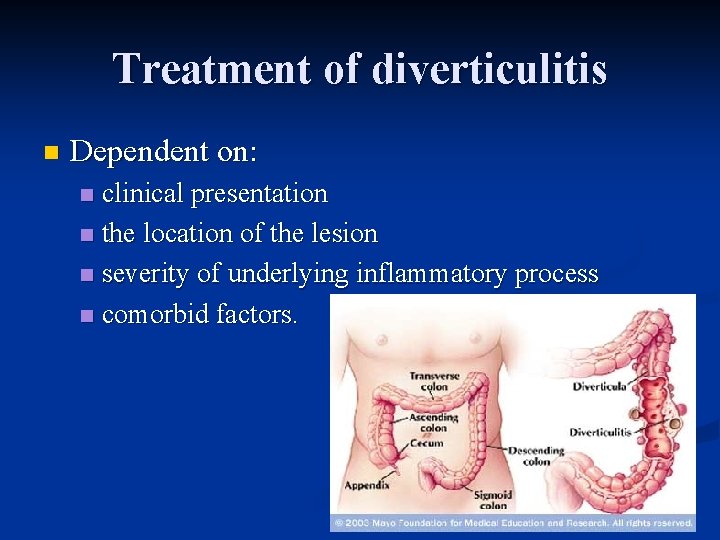
Treatment of diverticulitis n Dependent on: clinical presentation n the location of the lesion n severity of underlying inflammatory process n comorbid factors. n
Treatment of diverticulitis n In mild cases, the diagnosis of diverticulitis can be made with confidence on the basis of clinical examination findings. These patients are not very ill and are able to tolerate food and oral fluids. n Patients with mild diverticulitis can be started on an outpatient treatment regimen. n
Treatment of diverticulitis n Outpatient treatment consists of a liquid diet n 7 -10 days of oral broad-spectrum antimicrobial therapy n n n which covers anaerobic microorganisms such as Bacteroides fragilis and Peptostreptococcus and Clostridium organisms, as well as aerobic microorganisms such as Escherichia coli and Klebsiella, Proteus, Streptococcus, and Enterobacter organisms. One typical antibiotic regimen is a combination of ciprofloxacin and metronidazole
Treatment of diverticulitis n Hospitalization is required if: patients are unable to tolerate oral hydration n if outpatient therapy fails n if notable fever and/or peritoneal signs develop n if pain is severe enough to require narcotic analgesia n or if patients have a chronic underlying medical condition. n
Treatment of diverticulitis n These patients have moderate-to-severe diverticulitis; n n do not provide anything by mouth. Initiate intravenous fluid hydration and start broad-spectrum intravenous antibiotic coverage. n The typical standard triple antibiotic regimen in these situations is a combination of ampicillin, gentamicin, and metronidazole.
Treatment of diverticulitis n Pain management is also important. n n Meperidine is an appropriate choice if narcotics are required. Avoid morphine sulfate because it can cause colonic spasm. Once the acute episode has resolved, instruct the patient to maintain a high-fiber diet and to undergo elective colonoscopy
Treatment of diverticulitis n Surgical treatment is usually necessary in only 20 -30% of patients with acute diverticulitis
Treatment of diverticulitis n When is surgery necessary? If attacks are severe or frequent n complications of a fistula or intestinal obstruction n emergency surgery may be required for -a large abscess, perforation, peritonitis, or continued bleeding n
Treatment of diverticulitis n Emergency surgery usually involves two operations. n n n The first clears the infected abdominal cavity/removes part of the colon The second rejoins the ends of the colon Due to infection/obstruction, it is not safe to rejoin the colon during the first operation. n n Instead, a temporary hole, or stoma, in the abdomen is made The end of the colon is connected to the hole, a procedure called a colostomy, to allow normal eating and bowel movements.
Further Outpatient Management n n n In the elective setting, patient evaluation should be conducted after the resolution of an episode of acute diverticulitis. The colon requires full evaluation with colonoscopy or barium enema to establish the extent of disease and to rule out lesions such as polyps or carcinoma. Diverticulitis may lead to stricture formation that can have the appearance of carcinoma; a biopsy of such a lesion should be performed
Dietary Management Administer nothing by mouth in episodes of moderate-to-severe acute diverticulitis. n In mild episodes, a clear liquid diet is advised. n Long-term management includes a high-fiber, low-fat, and low-beef diet. n
Dietary Management n Increasing the amount of fiber in the diet may reduce symptoms of diverticulosis and prevent complications such as diverticulitis. Fiber keeps stool soft and lowers pressure inside the colon so that bowel contents can move through easily. n The American Dietetic Association recommends 20 to 35 grams of fiber each day. n
Dietary Management n Fiber product – n Citrucel or Metamucil once a day. These products are mixed with water and provide about 2 to 3. 5 grams of fiber per tablespoon, mixed with 8 ounces of water.
Diverticulosis is a very common, and usually a very benign condition n Complications occur only in a minority of patients, and most of them get well with medical treatment alone without any need for surgery n

 Victor politi
Victor politi Type i
Type i Victor politi
Victor politi Victor politi
Victor politi Mesenteric stranding
Mesenteric stranding Diverticulitis
Diverticulitis Rachel politi
Rachel politi Hinchey classification of diverticulitis
Hinchey classification of diverticulitis Diverticulitis
Diverticulitis Ertanecep
Ertanecep Esophageal diverticula
Esophageal diverticula Diverticulitis treatment diet
Diverticulitis treatment diet Diverticulitis treatment
Diverticulitis treatment Meckel's diverticulitis
Meckel's diverticulitis Dieta para diverticulitis fase aguda
Dieta para diverticulitis fase aguda Torrance memorial map
Torrance memorial map Ptal california medical board
Ptal california medical board Cartersville medical center medical records
Cartersville medical center medical records Gbmc medical records
Gbmc medical records Hepburn osteometric board
Hepburn osteometric board Jav
Jav Escuela secundaria 95 victor hugo
Escuela secundaria 95 victor hugo La vache victor hugo
La vache victor hugo La cocinelle victor hugo
La cocinelle victor hugo Victor piotrowski
Victor piotrowski Victor shoup
Victor shoup Dr victor tan
Dr victor tan University of medicine and pharmacy timisoara
University of medicine and pharmacy timisoara Gradient reversal layer
Gradient reversal layer Victor galarreta
Victor galarreta Victor papaneck
Victor papaneck The lonely shepherd histoire
The lonely shepherd histoire Victor e frankl
Victor e frankl Světový romantismus pracovní list
Světový romantismus pracovní list Victor frost ku
Victor frost ku Poema desejo victor hugo
Poema desejo victor hugo Frou frou
Frou frou Victor hugo te deseo
Victor hugo te deseo Víctor carvajal biografia
Víctor carvajal biografia Victor hurtig
Victor hurtig Escultor benjamin victor
Escultor benjamin victor How was jomon pottery made
How was jomon pottery made Victor adamchik
Victor adamchik Kaksiluonto-oppi
Kaksiluonto-oppi Vctor
Vctor Fluierul fermecat de victor eftimiu
Fluierul fermecat de victor eftimiu Sikke mange klokken slår
Sikke mange klokken slår Vector victor meaning
Vector victor meaning Dr victor matthews
Dr victor matthews Ift3355
Ift3355 Victor pestov
Victor pestov Analogue and digital images
Analogue and digital images Victor hugo desejo
Victor hugo desejo Victor molev
Victor molev Sds management delta
Sds management delta Spitalul victor babeş casa doru
Spitalul victor babeş casa doru Introduction de victor hugo
Introduction de victor hugo Introduction victor hugo
Introduction victor hugo Victor oder die kinder an der macht
Victor oder die kinder an der macht Victor vasarely
Victor vasarely Jeff wall manet
Jeff wall manet Victor hugo te deseo
Victor hugo te deseo Desejo primeiro que você ame victor hugo
Desejo primeiro que você ame victor hugo Caracterizarea unui personaj realist
Caracterizarea unui personaj realist