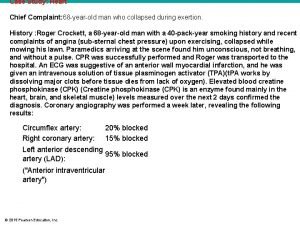
Cardiac Diagnostic Testing Victor Politi M D FACP





- Slides: 112
Cardiac Diagnostic Testing Victor Politi, M. D, FACP Medical Director, SVCMC, School of Allied Health Professions, Physician Assistant Program
Electrocardiographic Tests • Electrocardiographic tests are noninvasives tests which uses the electrocardiogram to evaluate the electrical activity generated by the heart at rest and with activity
Electrocardiographic Tests • • • Ambulatory Monitors EKG/ECG Exercise Stress Test Head Upright Tilt Test Metabolic Exercise Stress Test
Ambulatory Monitors • Ambulatory monitors are small, portable electrocardiograph machines that are able to record the heart’s rhythm. Each type of monitor has unique features related to length of recording time and ability to send the recordings over the phone
Ambulatory Monitors • assess heart rhythm over time • correlate symptoms with heart rhythm • diagnose abnormal heart rhythms: – what kind they are, how long they last, and what may cause them guide treatment for abnormal heart rhythms
Types of Ambulatory Monitors • Holter • Loop Recorder • Cardio. Net (mobile cardiac outpatient telemetry) • Transtelephonic transmitter
Holter Monitor (also called Ambulatory ECG) • A Holter monitor is a portable ECG recorder that is worn during normal daily activities, including sleeping. It can be worn up to 24 hours.
Holter Monitor • Electrodes are placed on the skin of the chest. Wires are attached from the electrodes to a box about the size of a portable tape player and worn on a belt or shoulder strap. The electrical impulses are continuously recorded and stored in the Holter Monitor
Holter Monitor • The patient is asked to keep a diary of activities and symptoms, such as fluttering feelings in the chest (palpitations), rapid heartbeats, and any episodes of dizziness or faintness.
Loop Recorder (also called an Event Recorder) • This device, similar to a Holter monitor, is worn during normal daily activities including sleeping; however, it is worn for a longer period of time. It can be removed during showers and baths. It is used for arrhythmias that occur less frequently.
Loop Recorder • When the patient feels symptoms, they depress a button and the recorder is activated. The monitor records the event for the 60 seconds prior to pushing the button and up to 40 seconds after the arrhythmia is over. The loop recorder can store up to three events.
Loop Recorder • The rhythm can be sent immediately or saved and transmitted later, over the phone line. The technician will give the recordings to the doctor for review. If the reading indicates an emergency, the technician will instruct the patient to go to the emergency room
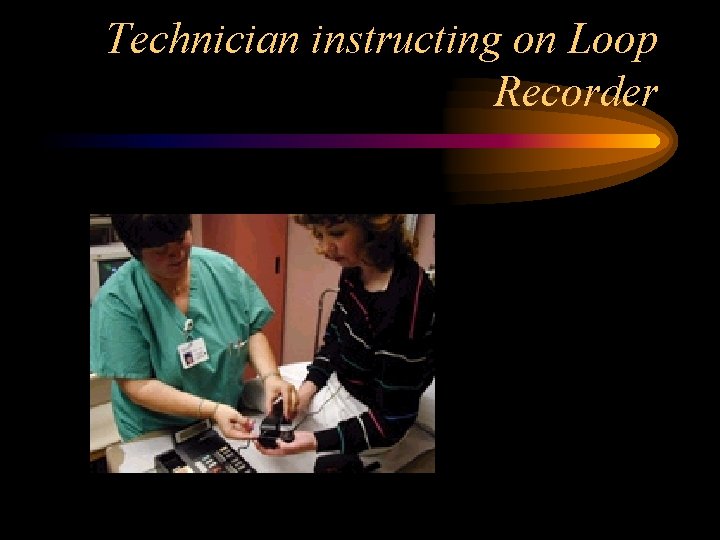
Technician instructing on Loop Recorder
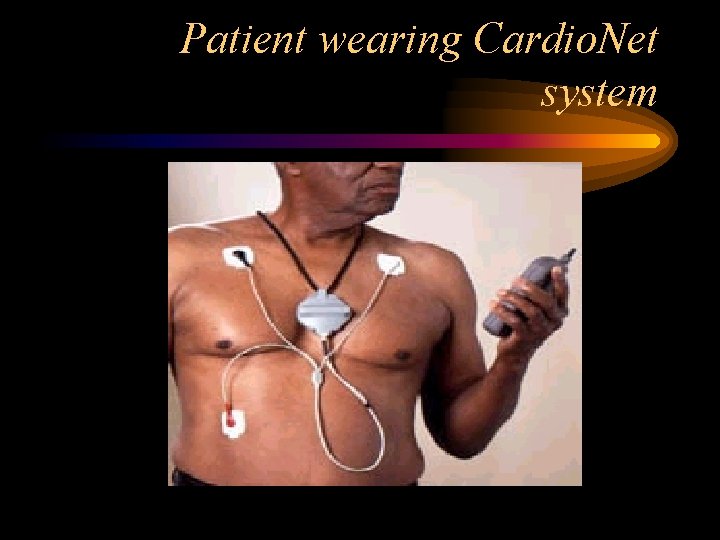
Cardio. Net (Mobile Cardiac Outpatient Telemetry) • Cardio. Net mobile telemetry allows continuous heartbeat monitoring as the patient goes about daily activities. Most people are on the Cardio. Net service from 7 to 14 days.
Cardio. Net (Mobile Cardiac Outpatient Telemetry) • This device consists of a small sensor attached to three electrode pads, worn on a belt clip. The sensor sends each heartbeat to a handheld monitor that can be tucked into a pocket or purse.
Cardio. Net (Mobile Cardiac Outpatient Telemetry) • When the monitor detects a heart rhythm problem — whether the patient feels it or not — it automatically transmits your ECG to the Cardio. Net monitoring center. A cardiac technician analyzes each transmission, responds appropriately to each event and transmit diagnostic reports to the doctor.
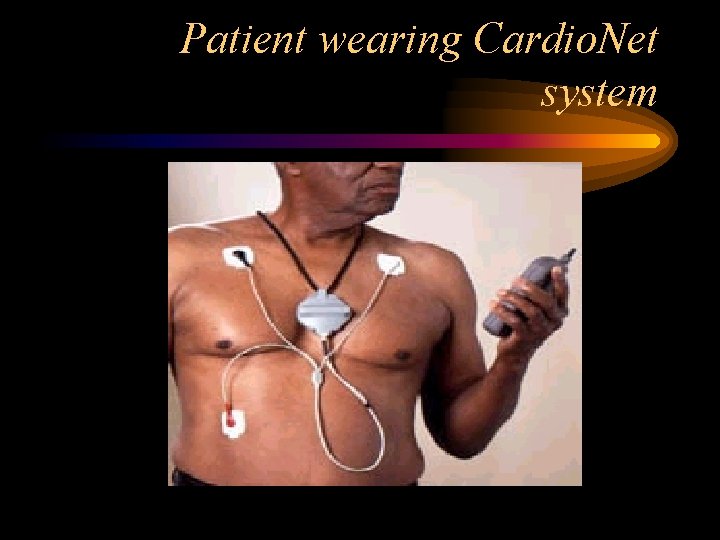
Patient wearing Cardio. Net system
Transtelephonic Transmitter • Transtelephonic transmitters are not worn continuously. • They are used only during the phonemonitoring period. In the past, this type of transmitter was used for monitoring pacemaker function. • However, now it is used for patients with arrhythmias to monitor certain events indicated by their doctor.
Transtelephonic Transmitter • The electrode may be a finger electrode, wrist bracelet or chest plate. The patient dials the center and places the telephone into a transmitter. After the transmission is completed, the nurse or technician will ask questions about the patient’s symptoms and current medications.

Patient testing transtelephonic transmitter
Electrocardiogram (ECG or EKG) • The ECG is a device used to record on graph paper the electrical activity of the heart. The picture is drawn by a computer from information supplied by the electrodes
Electrocardiogram (ECG or EKG) • assess your heart rhythm • diagnose poor blood flow to the heart muscle (ischemia) • diagnose a heart attack diagnose abnormalities of your heart, such as: heart chamber enlargement abnormal electrical conduction
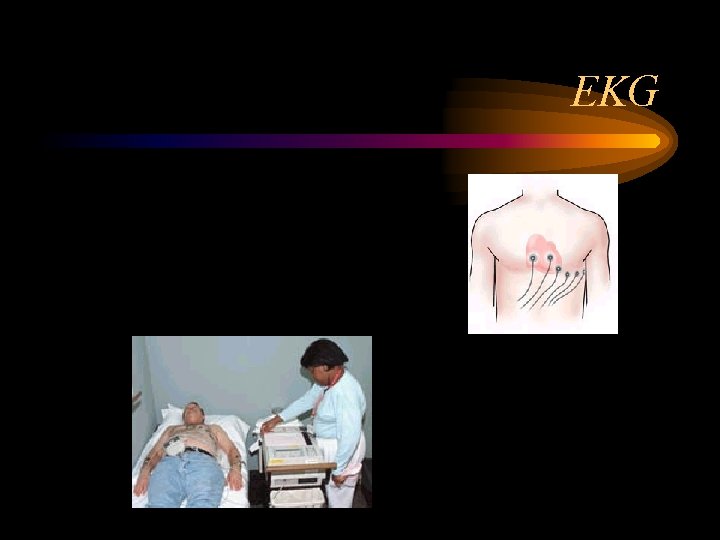
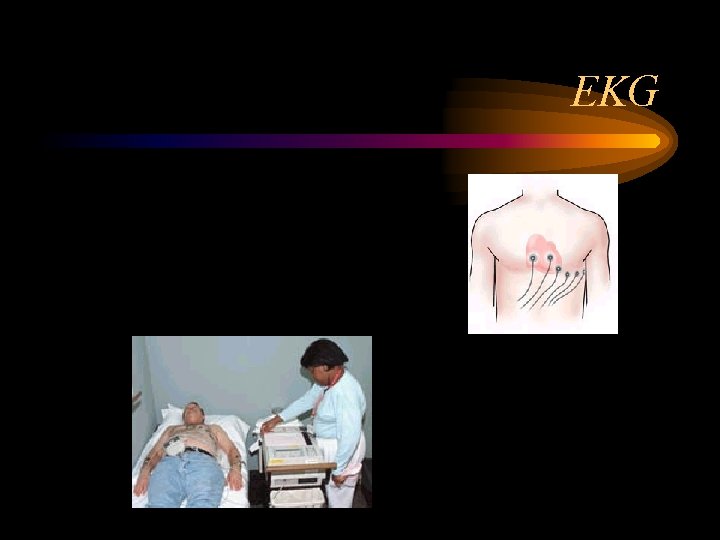
EKG
Ex ercise Stress Test (stress test, exercise electrocardiogram, treadmill test, graded exercise test, stress ECG) • A test used to provide information about how the heart responds to stress. • It usually involves walking on a treadmill or pedaling a stationary bike at increasing levels of difficulty, while the electrocardiogram, heart rate and blood pressure are monitored.
Exercis e Stress Test (stress test, exercise electrocardiogram, treadmill test, graded exercise test, stress ECG) • Used to determine if there is adequate blood flow to your heart during increasing levels of activity • evaluate the effectiveness of cardiac treatment plan • determine the likelihood of having coronary artery disease and the need for future testing
EST • an electrocardiograph (ECG) monitor that charts the heart’s electrical activity during the test. • Blood pressure and ECG recording will be taken before, during and after exercise.

EST • The patient begins to exercise by walking on a treadmill or pedaling a stationary cycle. The degree of difficulty is gradually increased.
EST • It is normal for the heart rate, blood pressure, breathing rate and perspiration to increase during the test. • The lab personnel will watch for any symptoms or changes on the ECG monitor that suggest the test should be stopped.
EST • the appointment lasts about 60 minutes, the actual exercise time is usually between 7 and 12 minutes.
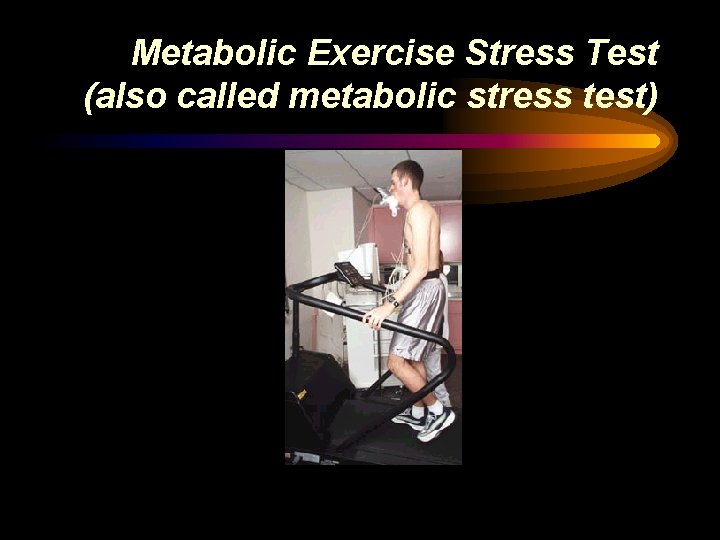
Metabolic Exercise Stress Test (also called metabolic stress test) • A test used to measure the performance of the heart and lungs while they are under physical stress. The test involves walking on a treadmill or pedaling a stationary bike at increasing levels of difficulty, while being closely monitored.
Metabolic Exercise Stress Test (also called metabolic stress test) 1. determine how fit the heart and lungs are 2. determine if symptoms of shortness of breath or chronic fatigue are due to a medical problem (such as heart or lung disease) or due to poor fitness 3. measure the heart’s ability to do work (functional capacity) 4. determine if certain surgical treatments are appropriate 5. evaluate the effectiveness the cardiac treatment plan 6. help develop a safe and effective exercise program
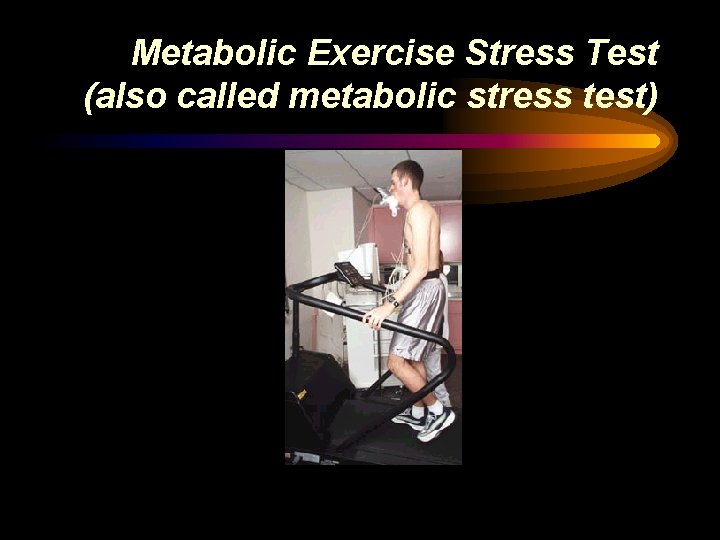
Metabolic Exercise Stress Test (also called metabolic stress test)
Laboratory testing • Laboratory tests include a number of blood tests used to diagnose and monitor treatment for heart disease.
Laboratory Testing • • • CBC Lipids electrolytes BNP (B-type Natriuretic peptide) Enzymes and Proteins
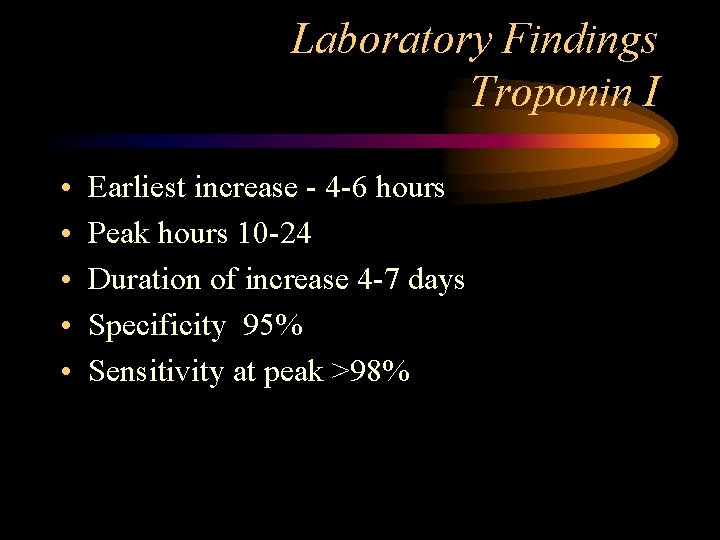
Laboratory Findings Troponin I • • • Earliest increase - 4 -6 hours Peak hours 10 -24 Duration of increase 4 -7 days Specificity 95% Sensitivity at peak >98%
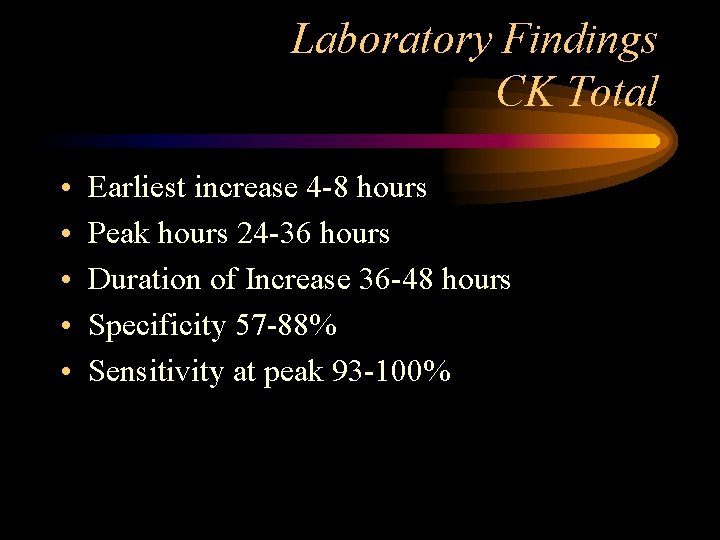
Laboratory Findings CK Total • • • Earliest increase 4 -8 hours Peak hours 24 -36 hours Duration of Increase 36 -48 hours Specificity 57 -88% Sensitivity at peak 93 -100%
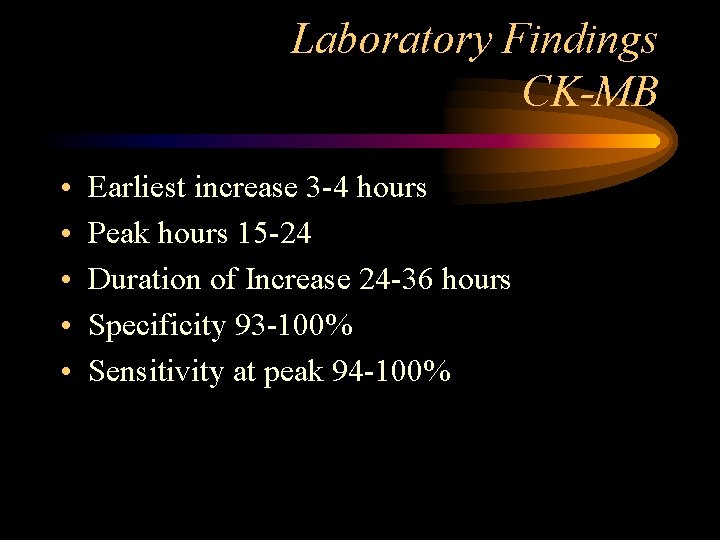
Laboratory Findings CK-MB • • • Earliest increase 3 -4 hours Peak hours 15 -24 Duration of Increase 24 -36 hours Specificity 93 -100% Sensitivity at peak 94 -100%

Nuclear Imaging • Nuclear imaging is a method of producing images by detecting radiation from different parts of the body after the administration of a radioactive tracer material.
Nuclear Imaging • Radioactive tracers are not dyes. They have no side effects. • The amount of radiation a patient receives in a typical nuclear imaging scan is very low, similar to the exposure received in a routine chest x-ray. • In most cases the tracers are injected into a vein. In some cases they may be given by mouth.
Nuclear Imaging • • Multigated Acquisition Scan (MUGA) Positron Emission Tomography (PET) Sestamibi Exercise Stress Test Thallium Exercise Stress Test
Multigated Acquisition Scan (MUGA scan, nuclear ventriculogram, radionuclide scan) • A nuclear scan that evaluates the pumping function of the ventricles. • An ECG, IV started. • A resting ECG & blood pressure recorded.
Multigated Acquisition Scan (MUGA scan, nuclear ventriculogram, radionuclide scan) • A small amount of blood is withdrawn and mixed with a radioactive tracer. • The radioactive tracer binds to the red blood cells, the mixture is re-injected into the IV. • The tracer stays in the bloodstream for several hours and does not enter tissue cells.
Multigated Acquisition Scan (MUGA scan, nuclear ventriculogram, radionuclide scan) 1. A MUGA scan analyzes the amount of radiolabeled red blood cells pumped out of the heart with each heartbeat. 2. This test calculates the amount of blood pumped out of the heart with each heartbeat, called the ejection fraction. 3. The MUGA scan takes about one to two hours to perform.
Positron Emission Tomography (PET or cardiac viability study) • An imaging procedure that uses radioactive tracers to create threedimensional pictures of the tissues inside of the body and that can monitor metabolic processes.
PET · PET is used to: · determine if there is adequate blood flow to the heart · assess the amount of damage to the heart after a heart attack · evaluate the effectiveness of your treatment plan • PET is used for patients who are unable to exercise on a treadmill or stationary cycle.
PET • An ECG and IV are started • A resting ECG, and BP reading recorded • A small amount of rubidium injected into the IV. Rubidium is a radioactive tracer that allows the physician to view the blood flow in the heart at rest. It is not a dye.
PET • dipyridamole is injected into the IV for about four minutes. The medication causes the heart to react as if the patient were exercising
PET • After all the medication has entered the bloodstream, a small amount of rubidium will again be injected into the IV. • The rubidium allows the physician to view the blood flow to the heart muscle while it is in stress
PET • The PET takes about three to four hours. The first part of the test will take about one hour. The second part will take about two hours, although the usual exercise time is between 7 and 12 minutes.
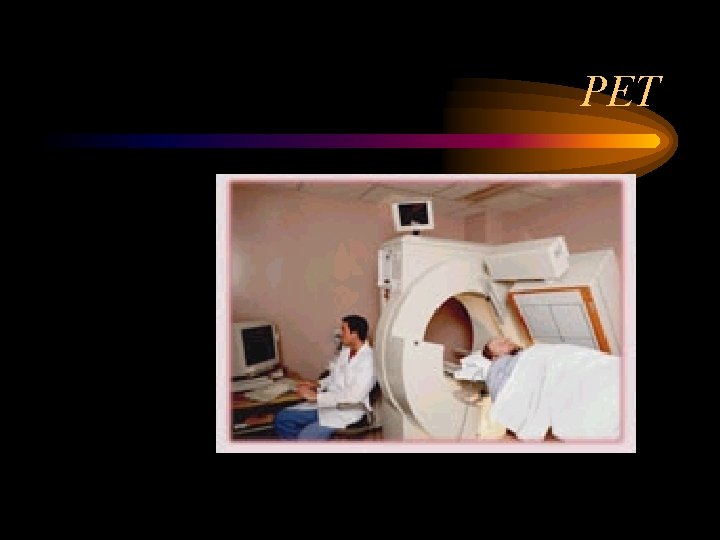
PET
Sestamibi Exercise Stress Test (sestamibi stress test, stress perfusion scan, stress sestamibi) • A diagnostic study, that uses a small amount of radioactive tracer, injected into the body, and a special camera, that detects the radiation released by the substance to produce a computer image of the heart. • Combined with exercise, the study can help determine if there is adequate blood flow to the heart at rest, as compared with activity.
Sestamibi Exercise Stress Test (sestamibi stress test, stress perfusion scan, stress sestamibi) · Used to: · determine if there is adequate blood flow to your heart during increasing levels of activity · evaluate the effectiveness of your cardiac treatment plan · determine the likelihood of having coronary artery disease and the need for future testing
Sestamibi Exercise Stress Test (sestamibi stress test, stress perfusion scan, stress sestamibi) • a small amount of thallium is injected into a vein. • Thallium is a radioactive tracer that allows the physician to assess heart function. Thallium is not a dye. • The patient lies under a camera with their arms over their head for about 15 to 20 minutes. • The camera records images that show the blood flow to each area of the heart muscle at rest.
Sestamibi Exercise Stress Test (sestamibi stress test, stress perfusion scan, stress sestamibi) • Next the patient goes to the Stress Lab. A resting ECG, and BP rate recorded. An IV will be started. • The patient will begin to exercise by walking on a treadmill or pedaling a stationary cycle. The degree of difficulty will gradually increase.
Sestamibi Exercise Stress Test (sestamibi stress test, stress perfusion scan, stress sestamibi) • One minute before stopping exercise, a small amount of sestamibi (a different type of radioactive tracer) will be injected in the IV. Once the sestamibi is administered, the IV will be removed. The patient may be asked to drink milk, which enhances the quality of the images.
Sestamibi Exercise Stress Test (sestamibi stress test, stress perfusion scan, stress sestamibi) • About 30 minutes after exercise is complete, the patient returns to nuclear medicine images are again taken (for about 20 minutes). The camera will now record images that show well blood flows through the coronary arteries to each area of the heart muscle during exercise
Sestamibi Exercise Stress Test (sestamibi stress test, stress perfusion scan, stress sestamibi) • The appointment lasts about three to four hours, the actual exercise time is usually between 7 and 12 minutes.
Thallium Exercise Stress Test (stress thallium test, perfusion scan) • A type of nuclear scanning technique that uses the radioactive substance thallium. • A thallium stress test combines nuclear scanning with exercise on a treadmill or stationary bicycle to assess heart function and determine if there is adequate blood flow to the myocardium.
Thallium Exercise Stress Test (stress thallium test, perfusion scan) • A thallium stress test is used to– determine if there is adequate blood flow to the heart during increasing levels of activity – evaluate the effectiveness of a cardiac treatment plan – determine the likelihood of having coronary artery disease and the need for future testing
Thallium Exercise Stress Test (stress thallium test, perfusion scan) • BP and ECG recording will be taken before, during and after exercise. • The patient will begin to exercise by walking on a treadmill or pedaling a stationary cycle. • The degree of difficulty will gradually increase.
Thallium Exercise Stress Test (stress thallium test, perfusion scan) • At the maximum level of exercise, a small amount of thallium is injected into a vein. • The thallium travels through the bloodstream, reaching the coronary arteries and then the cells of the heart muscle. • A camera detects the distribution of thallium in the myocardium.
Thallium Exercise Stress Test (stress thallium test, perfusion scan) • Because thallium works as a tracer to indicate the areas of the myocardium that blood is reaching, regions that show less thallium have a loss of perfusion, or blood flow • the appointment lasts about 60 minutes, the actual exercise time is usually between 7 and 12 minutes.
Ultrasound • Ultrasound tests are noninvasive tests which use ultrasound, or high frequency sound wave, to create graphic images of the heart's structures, pumping action, and direction of blood flow.
Ultrasound Studies • • Echocardiogram Dobutamine Stress Echo Transesophageal Echocardiogram (TEE) Exercise Stress Echo
Echocardiogram • An echocardiogram (often called "echo") is a graphic outline of the heart's movement.
Echocardiogram • During an echocardiogram test, ultrasound ( high-frequency sound waves) that come from a hand-held wand placed on the chest, is used to provide pictures of the heart's valves and chambers and help the sonographer evaluate the pumping action of the heart.
Echocardiogram • Echo is often combined with Doppler ultrasound and color Doppler to evaluate blood flow across the heart’s valves.
Dobutamine Stress Echocardiogram (dobutamine echo, pharmacological echocardiogram) • An echocardiogram is used to – assess the heart’s function – determine the presence of disease of the heart muscle, valves and pericardium, heart tumors, and congenital heart disease – evaluate the effectiveness of medical or surgical treatments – follow the progress of valve disease
Dobutamine Stress Echocardiogram (dobutamine echo, pharmacological echocardiogram) • The dobutamine stress echo test involves infusing a medication through an intravenous (IV) line, called dobutamine. • The dobutamine stimulates the heart and makes it "think" it is exercising. • The test is used to evaluate the heart and valve function when the patient is unable to exercise on a treadmill or stationary cycle
Dobutamine Stress Echocardiogram (dobutamine echo, pharmacological echocardiogram) 1. A dobutamine stress echo is used to: 2. Determine how well the heart tolerates stress or exertion 3. Evaluate the function of your heart and valves 4. Evaluate the effectiveness of your cardiac treatment plan 5. Determine the likelihood of having coronary artery disease and the need for further testing
Dobutamine Stress Echocardiogram (dobutamine echo, pharmacological echocardiogram) • A resting ECG and BP are recorded • A resting sonogram is done • The dobutamine is administered via IV as the sonogram continues • The dobutamine causes the heart to react as it would under exercise • The dobutamine stress echo takes about 60 minutes. The actual infusion time is usually 15 minutes.
TEE- Transesophageal echocardiogram • During the transesophageal echocardiogram (TEE) test, an ultrasound transducer (which produces high frequency sound waves) provides pictures of the heart's valves and chambers and helps evaluate the pumping action of the heart.
TEE- Transesophageal echocardiogram • The ultrasound transducer is positioned on an endoscope. The endoscope is placed into the mouth and passed into the esophagus to provide a close look at the heart's valves and chambers without interference from the ribs or lungs.
TEE- Transesophageal echocardiogram • TEE is often combined with Doppler ultrasound and color Doppler to evaluate blood flow across the heart’s valves. TEE is often used when the results from standard echo studies were not sufficient
TEE- Transesophageal echocardiogram • TEE is used to: – Assess the overall function of the heart's chambers and valves – Determine the presence of many types of heart disease (I. e. valvular/myocardial heart disease, pericardial disease, cardiac masses and congenital heart disease) – Evaluate the effectiveness of medical or surgical treatments Evaluate abnormalities of the left atrium

Exercise Stress Echo • The exercise stress echo test involves exercising on a treadmill or stationary cycle. • The test is used to evaluate heart and valve function at rest and with exertion
Exercise Stress Echo • An exercise stress echo is used to · Determine how well the heart tolerates activity · Evaluate the function of the heart and valves · Determine the likelihood of coronary artery disease · Evaluate the effectiveness of a cardiac treatment plan
Exercise Stress Echo • A resting ECG, resting heart rate and BP will be recorded before exercise • A resting echo will also be performed. • The patient will exercise either on a treadmill or stationary bicycle - gradually increasing the rate of exercise
Exercise Stress Echo • if the patient was exercising on a bike, the echo test may be performed while the patient is still pedaling. Another echocardiogram after exercising may also be performed • If exercise was on a treadmill, the patient will return to the table to lie down for another echo.
Exercise Stress Echo • The appointment takes about 60 minutes. The actual exercise time is usually between 7 and 12 minutes.
Radiographic Tests • Radiographic tests are noninvasive tests which use x-ray machines or specialized equipment with computer technology to create pictures of the internal structures of the chest
Radiographic Studies • • Calcium-Score Screening Cardiac CT Chest x-ray MRI
Radiographic Test- Calcium Score Screening Heart Scan • A test used to detect calcium deposits found in atherosclerotic plaque in the coronary arteries. • CT methods, such as this one, are the most sensitive approaches to detecting coronary calcification from atherosclerosis, before symptoms develop.
Radiographic Test- Calcium Score Screening Heart Scan • More coronary calcium means more coronary atherosclerosis, suggesting a greater likelihood of significant narrowing somewhere in the coronary system and a higher risk of future cardiovascular events
Radiographic Test- Calcium Score Screening Heart Scan • Those at increased risk include individuals with the following traits: · family or personal history of coronary artery disease · male over 45 years of age, female over 55 years of age · past or present smoker · history of high cholesterol, diabetes or high blood pressure · overweight · inactive lifestyle
Radiographic Test- Calcium Score Screening Heart Scan • there are certain forms of coronary disease - such as "soft plaque" atherosclerosis – that escape detection during this CT scan, it is important to remember that this test is not absolute in predicting risk for a lifethreatening event, such as a heart attack.
Radiographic Test- Calcium Score Screening Heart Scan • CT scan captures multiple images, synchronized with the heartbeat. A computer program, guided by the cardiovascular radiologist, then analyzes the images for presence of calcification within the coronary arteries
Radiographic Test- Calcium Score Screening Heart Scan · Absence of calcium is considered a "negative" exam. It does not exclude the presence of "soft" noncalcified plaque. · If calcium is present, the computer will create a calcium score that estimates the extent of coronary artery disease.
Cardiac Computed Tomography (CT, cardiac CT or cardiac CAT scan) • A traditional CT scan is an x-ray procedure that combines many x-ray images with the aid of a computer to generate cross-sectional views of the body. • Cardiac CT uses the advanced CT technology with intravenous (IV) contrast (dye) to visualize your cardiac anatomy, coronary circulation and great vessels.
Cardiac Computed Tomography (CT, cardiac CT or cardiac CAT scan) • the cardiac CT is used to evaluate: · the heart muscle · the coronary arteries · the pulmonary veins · the thoracic aorta · the sac around the heart (pericardium)
Chest X-Ray (CXR, chest film) • an image of the structures of the chest (heart, lungs and bones) on film • used to: · look at the structures of the chest (bones, heart, lungs) · evaluate placement of devices (pacemakers, defibrillators) or tubes placed during hospitalization for treatment and monitoring (catheters, chest tubes) · diagnose lung and cardiac diseases
Magnetic Resonance Imaging (MRI) • A test that produces high-quality still and moving pictures of the heart and great vessels. • MRI uses large magnets and radiofrequency waves to produce pictures of the body’s internal structures; no x-ray exposure is involved.
MRI • MRI acquires information about the heart as it is beating; creating moving images of the heart throughout its pumping cycle.
MRI • MRI to evaluate: · The anatomy and function of the structures of the chest: heart, lungs, great vessels and pericardium · Presence of disease: ischemic heart disease, thoracic aortic disease, pericardial disease, right ventricular abnormalities, cardiac tumors, valve disease, heart muscle disease (cardiomyopathy), pulmonary artery disease and complex congenital heart disease
Invasive Tests • Invasive tests involve inserting catheters into the blood vessels of the heart in order to get a closer look at the coronary arteries or to stimulate and test the electrical system of the heart.
Invasive Tests • • • Carotid Angiography Cardiac Catheterization Electrophysiology Study Intravascular Ultrasound Myocardial Biopsy
Carotid Angiography • An invasive imaging procedure that involves inserting a catheter into a blood vessel in the arm or leg, and guiding it to the carotid arteries with the aid of a special xray machine. • Contrast dye is injected through the catheter so that x-ray movies of the carotid arteries are taken.

Carotid Angiography
Carotid angiography • carotid angiography is used to: · evaluate or confirm the presence of narrowing or blockage in carotid arteries · determine risk for future stroke · determine the need for further treatment (angioplasty or surgery)
Carotid angiography • A plastic introducer sheath (a short, hollow tube through which the catheter is placed) is inserted a blood vessel in the arm or groin. A catheter is inserted through the sheath and threaded to the arteries of the neck (right and left carotid artery). • When the catheter is in place, contrast material will be injected. The contrast material outlines the vessels.
Cardiac Catheterization • An invasive imaging procedure that involves inserting a catheter into a blood vessel in the arm or leg, and guiding it to the heart with the aid of a special xray machine. • Contrast dye is injected through the catheter so that the valves, coronary arteries and heart chambers are can be visualized.
Cardiac Catheterization • cardiac cath is used to: · evaluate or confirm the presence of heart disease (such as coronary artery disease, valve disease or disease of the aorta) · evaluate heart muscle function · determine the need for further treatment (angioplasty or bypass surgery)
Intravascular Ultrasound (IVUS) • An invasive procedure, performed along with cardiac catheterization; a miniature sound probe (transducer) on the tip of a coronary catheter is threaded through the coronary arteries and, using highfrequency sound waves, produces detailed images of the interior walls of the arteries.
Intravascular Ultrasound (IVUS) • IVUS is used to: · assess the inside of the vessel walls, making it possible to evaluate the size of fatty matter; how it is distributed, and in some cases, what it is made of · determine the need for further treatment (angioplasty or bypass surgery) · determine the need for aggressive management of risk factors prior to onset of symptoms and advanced disease · determine the predictors of transplant coronary artery disease
Intravascular Ultrasound (IVUS) • A plastic introducer sheath is inserted in the groin. A catheter will be inserted through the sheath and threaded to the arteries of the heart. Through the catheter, a wire with an ultrasound tip will be passed into the coronary arteries.
Intravascular Ultrasound (IVUS) • Once the catheter is within the coronary artery, a series of cross-sectional pictures of the artery are produced
Myocardial Biopsy • An invasive procedure that involves using a bioptome (a small catheter with a grasping device on the end) to obtain a small piece of heart muscle tissue that is sent to a laboratory for analysis.
Myocardial Biopsy • myocardial biopsy is used to: · evaluate or confirm the presence of rejection after heart transplant · diagnose myocarditis (inflammation of the heart muscle)
Electrophysiology Study (EP) • An EP Study is a recording of the electrical activity of the heart. This test is used to help determine the cause of rhythm disturbances and the best treatment. • During the test, arrhythmia can be reproduced and various medications given to see which one controls it best.
Electrophysiology Study (EP) • the EP study is used to: · determine the cause of an abnormal heart rhythm · locate the site of origin of an abnormal heart rhythm · decide the best treatment for an abnormal heart rhythm
Electrophysiology Study (EP) • Several catheters are inserted into the vein in the groin • Guided by the fluoroscopy machine, the catheters are threaded to the heart. • The catheters sense the electrical activity in the heart and are used to evaluate the heart’s conduction system. • A pacemaker is used to give the heart electrical impulses through one of the catheters to increase heart rate.
Questions ? ?
 Victor politi
Victor politi Dr victor politi
Dr victor politi Victor politi
Victor politi Victor politi
Victor politi Rachel politi
Rachel politi Diagnostic testing in education
Diagnostic testing in education Chapter 24 diagnostic tests and specimen collection
Chapter 24 diagnostic tests and specimen collection Chapter 23 specimen collection and diagnostic testing
Chapter 23 specimen collection and diagnostic testing Cs 3250
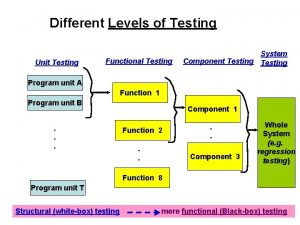
Cs 3250 Component testing is a black box testing
Component testing is a black box testing Decision table testing in software testing
Decision table testing in software testing Kv charts in software testing
Kv charts in software testing Decision table testing is white box
Decision table testing is white box Anuj magazine
Anuj magazine Software testing domains
Software testing domains Decision table based testing
Decision table based testing Data flow testing strategies in software testing
Data flow testing strategies in software testing Rigorous testing in software testing
Rigorous testing in software testing Decision table testing in software testing
Decision table testing in software testing Functional testing vs unit testing
Functional testing vs unit testing Pengertian black box
Pengertian black box Positive testing vs negative testing
Positive testing vs negative testing Testing blindness in software testing
Testing blindness in software testing Control structure testing in software engineering
Control structure testing in software engineering Domain test means
Domain test means Behavioral testing adalah
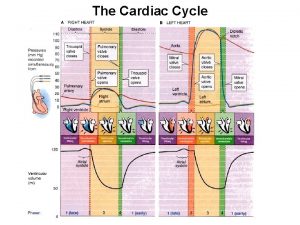
Behavioral testing adalah Cardiac cycle
Cardiac cycle Positions for patients in nursing
Positions for patients in nursing Anesthesia for cardiac tamponade
Anesthesia for cardiac tamponade Teixit muscular cardiac
Teixit muscular cardiac Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Cardiac index
Cardiac index Reason of cardiac arrest
Reason of cardiac arrest Stroke volume on ecg
Stroke volume on ecg Anterior vagal trunk
Anterior vagal trunk Tissue
Tissue Phase 2 cardiac rehab exercises
Phase 2 cardiac rehab exercises L
L Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Cardiac muscle striations
Cardiac muscle striations Muscle refractory period
Muscle refractory period Av
Av Moat house surgery
Moat house surgery Wandering atrial pacemaker
Wandering atrial pacemaker Cardiac glycoside
Cardiac glycoside Fick cardiac output
Fick cardiac output Good morning blood
Good morning blood Cardiac workload
Cardiac workload Esophageal junction histology
Esophageal junction histology Cardiac landmarks
Cardiac landmarks Torrance memorial lab manhattan beach
Torrance memorial lab manhattan beach Troponin meaning
Troponin meaning Lidocaine in cardiac arrest
Lidocaine in cardiac arrest Normal ci and co
Normal ci and co Cardiac index
Cardiac index Cardiac muscle
Cardiac muscle Pharynx
Pharynx Pearson education
Pearson education Spread of cardiac impulse
Spread of cardiac impulse Ertapenem
Ertapenem Jones and bartlett ekg strips
Jones and bartlett ekg strips Wiggers diagram
Wiggers diagram Cardio clearance meaning
Cardio clearance meaning Which muscle
Which muscle Cardiac cycle animation
Cardiac cycle animation Ejaculatory duct
Ejaculatory duct Cardiac muscle tissue
Cardiac muscle tissue Parts of the abdomen
Parts of the abdomen Cardiac excitation-contraction coupling
Cardiac excitation-contraction coupling Cardiac plexus
Cardiac plexus Negative chronotropic effect of digoxin
Negative chronotropic effect of digoxin Hemodynamic disorders
Hemodynamic disorders Co = hr x sv
Co = hr x sv Pleura
Pleura Revised cardiac risk index
Revised cardiac risk index Cardiac muscle histology labeled
Cardiac muscle histology labeled Mark wholey md
Mark wholey md The reflex protects the heart from overfilling.
The reflex protects the heart from overfilling. Cardiac poisons
Cardiac poisons What decreases stroke volume
What decreases stroke volume Sarcoplasm
Sarcoplasm Esophagus artery
Esophagus artery Massive hemothorax
Massive hemothorax Cardiac output trained vs untrained
Cardiac output trained vs untrained Cardiac muscle mitochondria
Cardiac muscle mitochondria Cardiac rehabilitation near south san francisco
Cardiac rehabilitation near south san francisco Cardiac edema
Cardiac edema Friction rub cardiac
Friction rub cardiac Cardiac distension
Cardiac distension Glycolysis in cardiac muscle
Glycolysis in cardiac muscle Torrance memorial cardiac rehab
Torrance memorial cardiac rehab Dullness to percussion
Dullness to percussion Cardiac sphincter
Cardiac sphincter Cardiac muscle cross section
Cardiac muscle cross section Svv cardiac
Svv cardiac All or none law
All or none law Cardiac cycle
Cardiac cycle Pathology of asthma
Pathology of asthma Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Pediatric pat
Pediatric pat Intrinsic conduction system of the heart
Intrinsic conduction system of the heart Properties of heart muscle
Properties of heart muscle Cardiac cycle
Cardiac cycle What is a tissue?
What is a tissue? Phase 2 cardiac rehab exercises
Phase 2 cardiac rehab exercises Cardiac output trained vs untrained
Cardiac output trained vs untrained Cardiac cycle
Cardiac cycle Heart wall
Heart wall Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Co= hr x sv
Co= hr x sv Tripod position breathing
Tripod position breathing Rugae
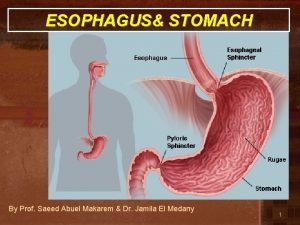
Rugae Cardiac orifice of stomach
Cardiac orifice of stomach