Investigation of the heart and great vessels Inspection
- Slides: 20
Investigation of the heart and great vessels. Inspection, palpation, and percussion of the heart. Apical impulse Dr. Szathmári Miklós Semmelweis University First Department of Medicine 17. Oct. 2011.
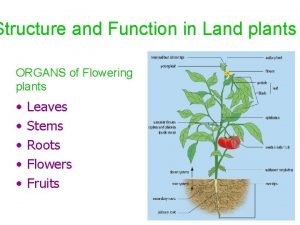
Surface projection of the heart and great vessels – Right ventricle occupies most of the anterior cardiac surface – The inferior border of the right ventricle lies below the junction of the sternum and the xiphoid process – The right ventricle narrows superiorly and meets the pulmonary artery at the level of the 3 rd left costal cartilage to the sternum : base of the heart. )
Surface projection of the heart and great vessels • The left ventricle forms the left lateral margin of the heart. Its tapered tip is termed the cardiac apex. It produces apical impulse (the point of maximal impulse). This impulse locates the left border of the heart and is usually found in the 5 th interspace 7 -9 cm lateral to the midsternal line. • The right heart border is formed by the right atrium behind the sternum. Normally the right heart border does not exceed the right border margin of the sternum.
Surface projection of the heart and great vessels • The pulmonary artery bifurcates quickly into its left and right branches. • The aorta curves upward from the left ventricle to the level of sternal angle, where it arches backward and then down • On the right, the superior and inferior vena cava empties in the right atrium.
Cardiac valves • Because of their positions, the tricuspid and mitral valves are often called atrioventricular valves. • The aortic and pulmonic valves are called semilunar valves because each of their leaflets is shaped like a half moon. • At the heart valves close, the heart sounds arise from vibrations emanating from the leaflets, the adjacent cardiac structures, and the flow of blood.
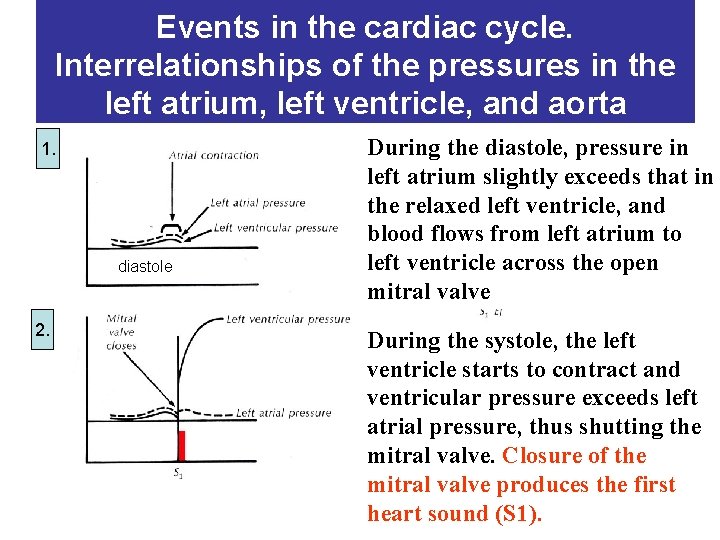
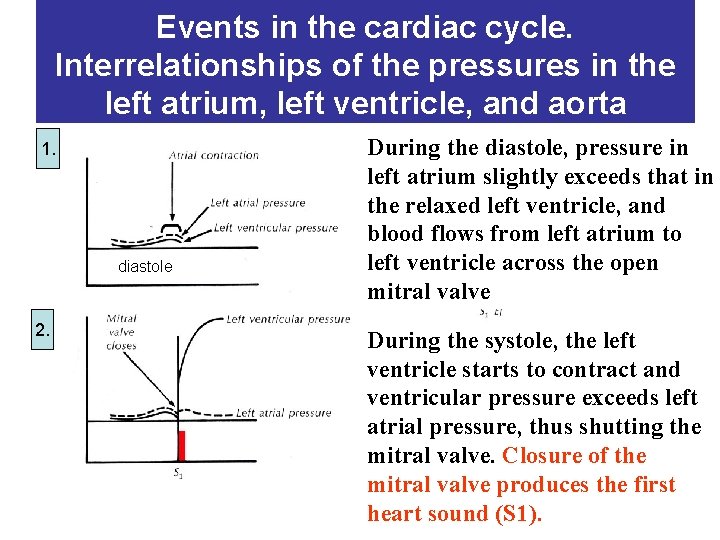
Events in the cardiac cycle. Interrelationships of the pressures in the left atrium, left ventricle, and aorta 1. diastole 2. During the diastole, pressure in left atrium slightly exceeds that in the relaxed left ventricle, and blood flows from left atrium to left ventricle across the open mitral valve During the systole, the left Az ejekció ventricle starts to contract and után csökken ventricular pressure exceeds left a bal kamrai nyomás, atrial pressure, thus shutting the becsapódig mitral valve. Closure of az the aorta S 2 mitral valve produces billentyű the first heart sound (S 1).
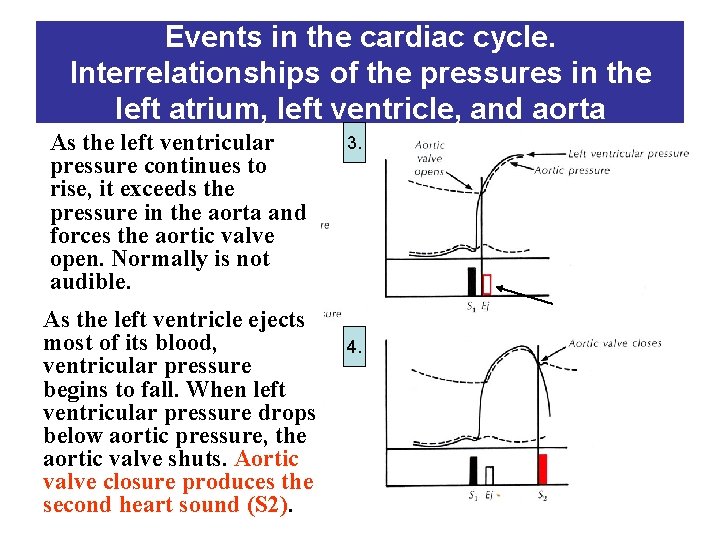
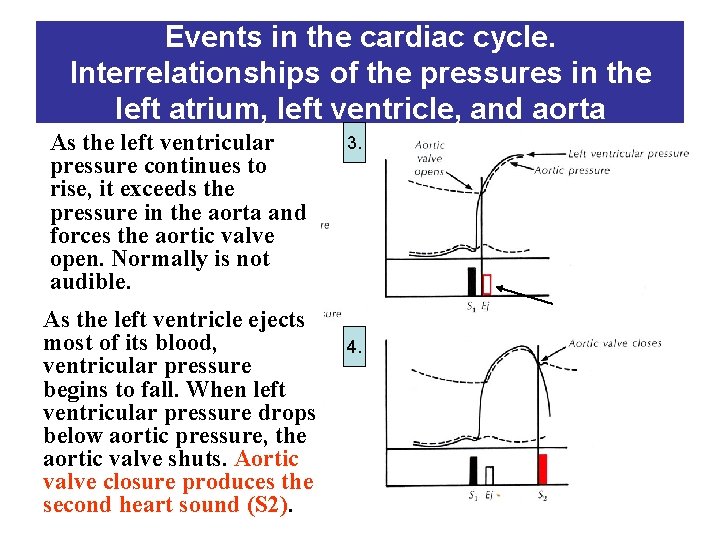
Events in the cardiac cycle. Interrelationships of the pressures in the left atrium, left ventricle, and aorta As the left ventricular pressure continues to rise, it exceeds the pressure in the aorta and forces the aortic valve open. Normally is not diasztolé audible. As the left ventricle ejects most of its blood, ventricular pressure begins to fall. When left ventricular pressure drops below aortic pressure, the aortic valve shuts. Aortic valve closure produces the second heart sound (S 2). 3. 4.
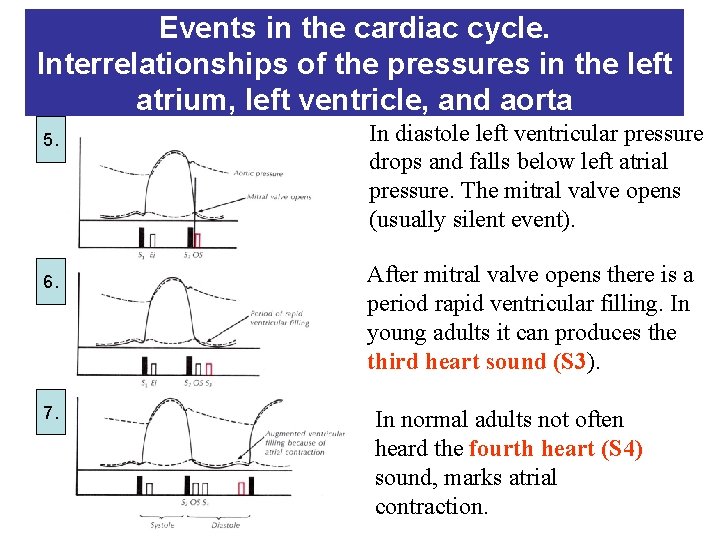
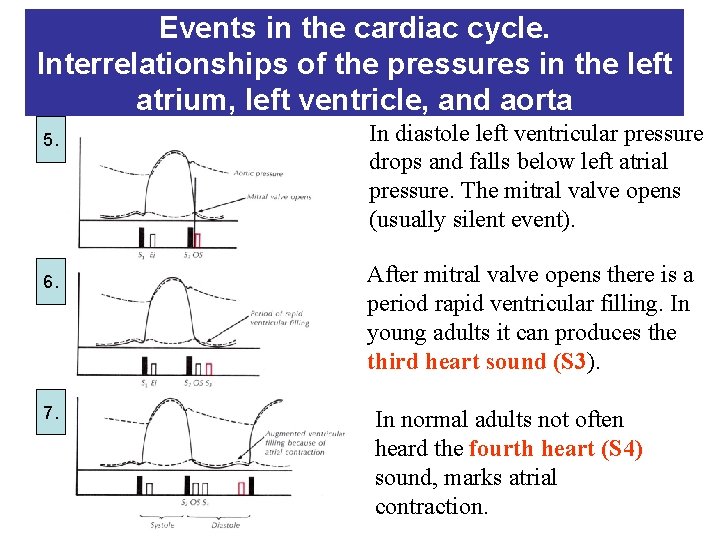
Events in the cardiac cycle. Interrelationships of the pressures in the left atrium, left ventricle, and aorta 5. 6. 7. In diastole left ventricular pressure drops and falls below left atrial pressure. The mitral valve opens (usually silent event). After mitral valve opens there is a period rapid ventricular filling. In young adults it can produces the third heart sound (S 3). In normal adults not often heard the fourth heart (S 4) sound, marks atrial contraction.
Inspection of cardiac area • Anteriorly displaced chest wall above the cardiac area indicates hereditary cardiac failure, because of the plasticity of the chest wall during the childhood. • Careful inspection of the anterior chest may reveal the location of the apical impulse (tangential light much improves your chances of seeing impulses. • Systolic retraction at the site of apical impulse indicates pericardial accretio (a form of adhesive pericarditis in which adhesions extend from the pericardium to the chest wall)
Inspection of cardiac area • Apical impulse. – The brief early systolic pulsation of the left ventricle – May not be visible in the supine position ask the patient to roll partly onto the left side • Right ventricular hypertrophy often results in a sustained systolic lift at the lower left parasternal area • Pulmonary artery pulsation is often visible (and palpable) in the left second interspace indicating pulmonary hypertension • Epigastrical pulsation: sign of the right ventricle hypertrophy (also in case of emphysema)
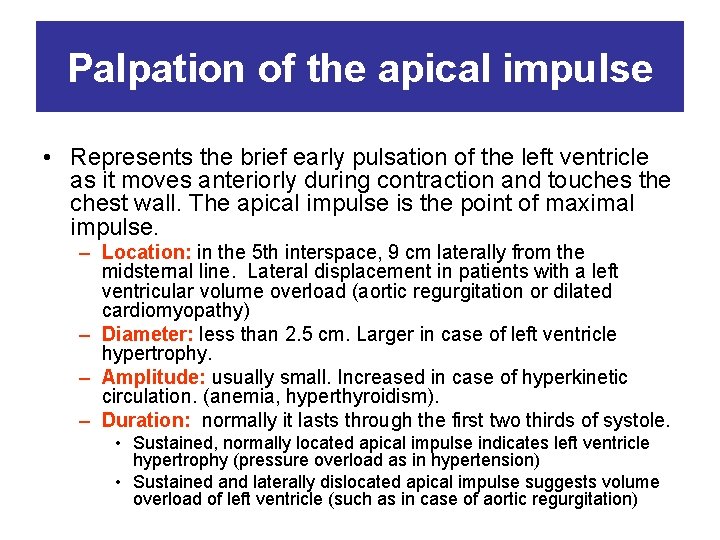
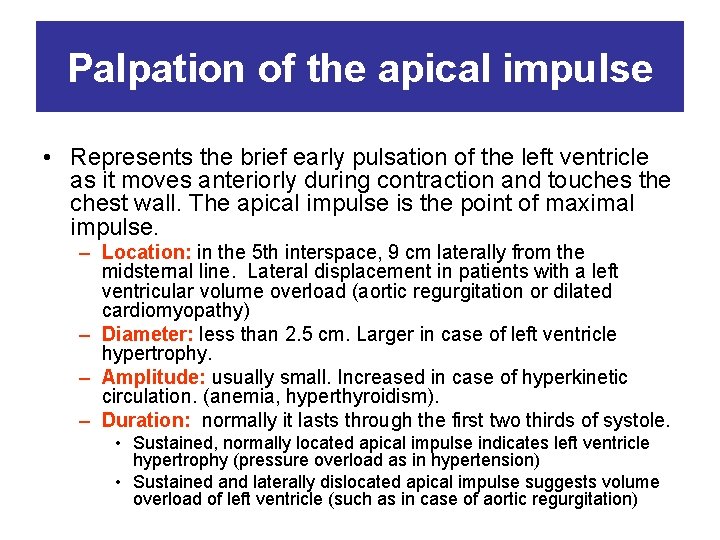
Palpation of the apical impulse • Represents the brief early pulsation of the left ventricle as it moves anteriorly during contraction and touches the chest wall. The apical impulse is the point of maximal impulse. – Location: in the 5 th interspace, 9 cm laterally from the midsternal line. Lateral displacement in patients with a left ventricular volume overload (aortic regurgitation or dilated cardiomyopathy) – Diameter: less than 2. 5 cm. Larger in case of left ventricle hypertrophy. – Amplitude: usually small. Increased in case of hyperkinetic circulation. (anemia, hyperthyroidism). – Duration: normally it lasts through the first two thirds of systole. • Sustained, normally located apical impulse indicates left ventricle hypertrophy (pressure overload as in hypertension) • Sustained and laterally dislocated apical impulse suggests volume overload of left ventricle (such as in case of aortic regurgitation)
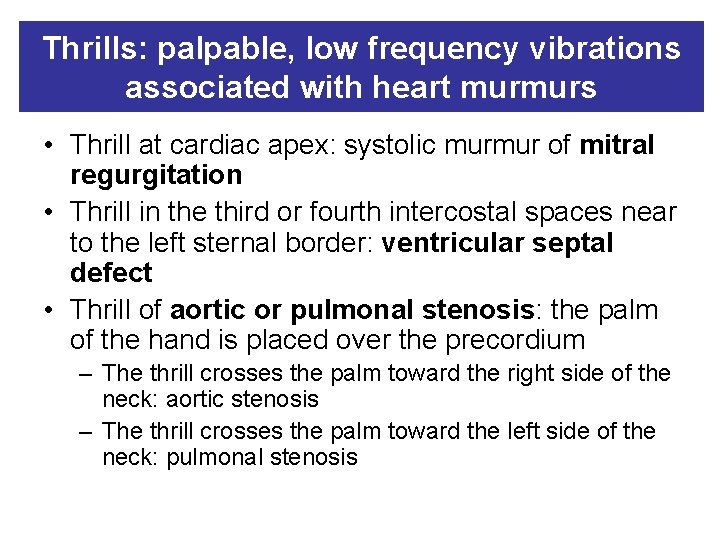
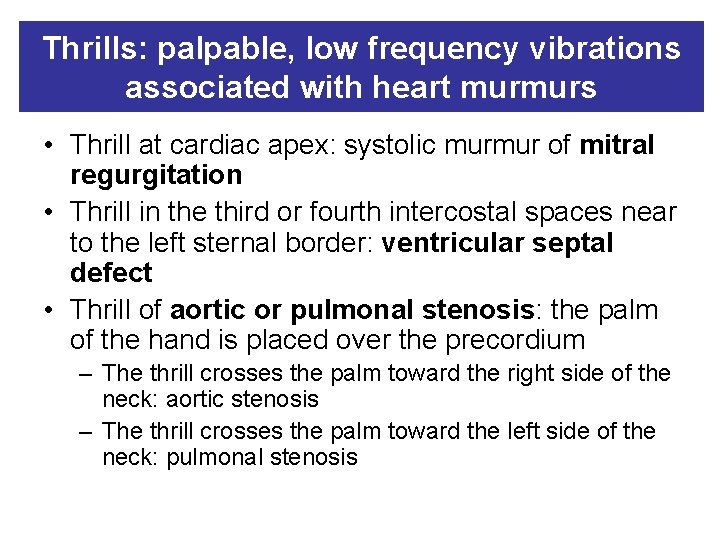
Thrills: palpable, low frequency vibrations associated with heart murmurs • Thrill at cardiac apex: systolic murmur of mitral regurgitation • Thrill in the third or fourth intercostal spaces near to the left sternal border: ventricular septal defect • Thrill of aortic or pulmonal stenosis: the palm of the hand is placed over the precordium – The thrill crosses the palm toward the right side of the neck: aortic stenosis – The thrill crosses the palm toward the left side of the neck: pulmonal stenosis
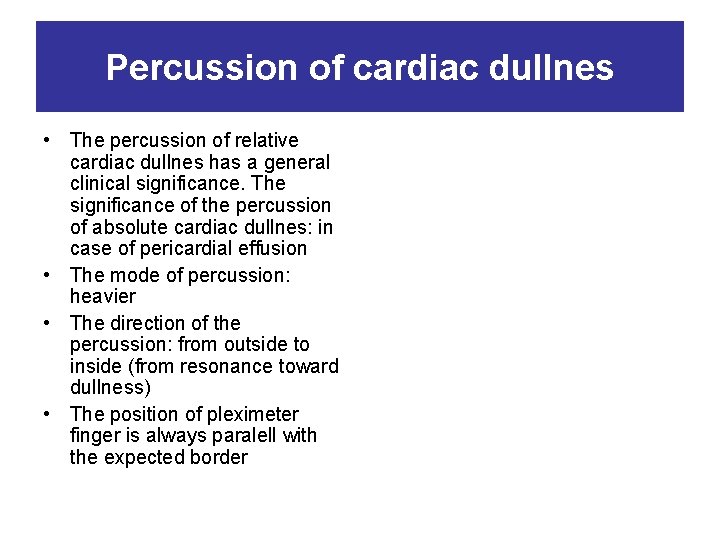
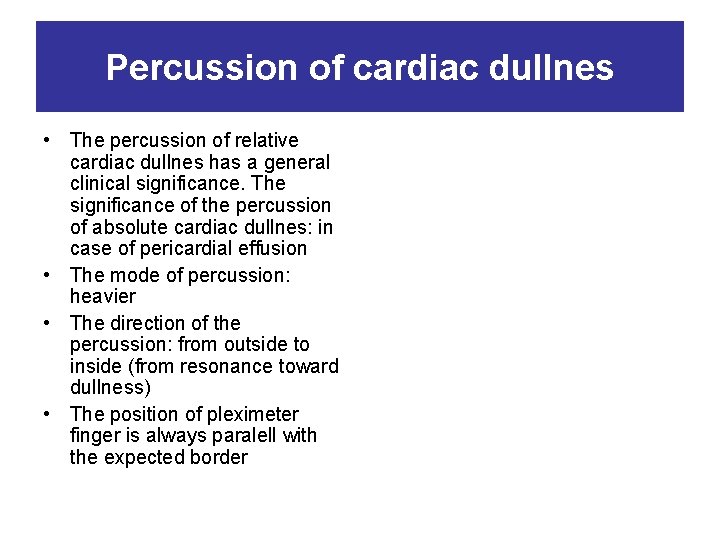
Percussion of cardiac dullnes • The percussion of relative cardiac dullnes has a general clinical significance. The significance of the percussion of absolute cardiac dullnes: in case of pericardial effusion • The mode of percussion: heavier • The direction of the percussion: from outside to inside (from resonance toward dullness) • The position of pleximeter finger is always paralell with the expected border
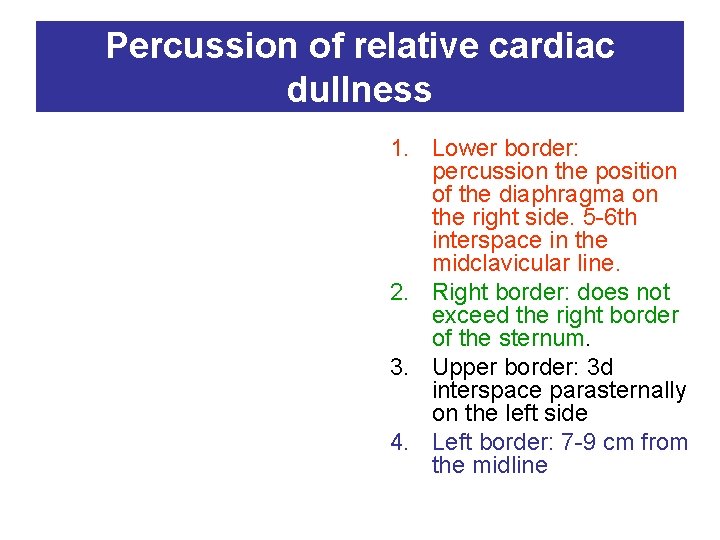
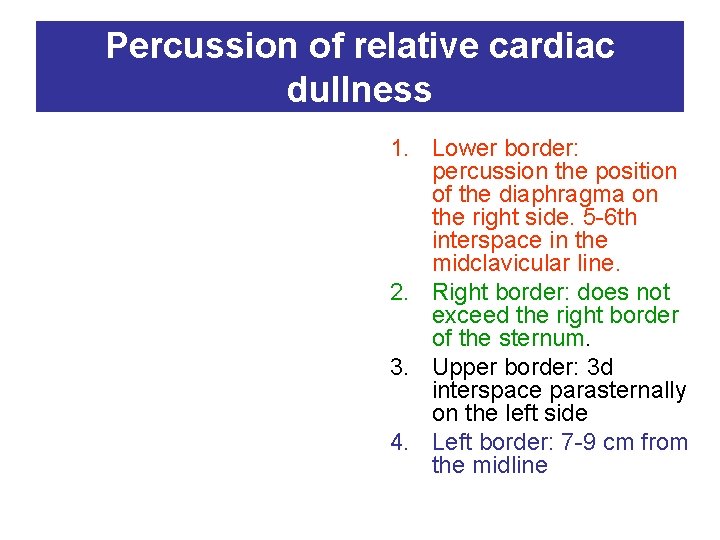
Percussion of relative cardiac dullness 1. Lower border: percussion the position of the diaphragma on the right side. 5 -6 th interspace in the midclavicular line. 2. Right border: does not exceed the right border of the sternum. 3. Upper border: 3 d interspace parasternally on the left side 4. Left border: 7 -9 cm from the midline
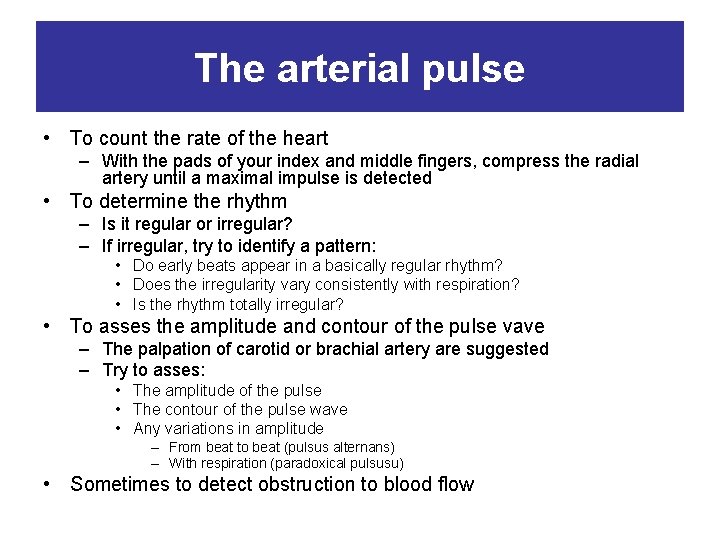
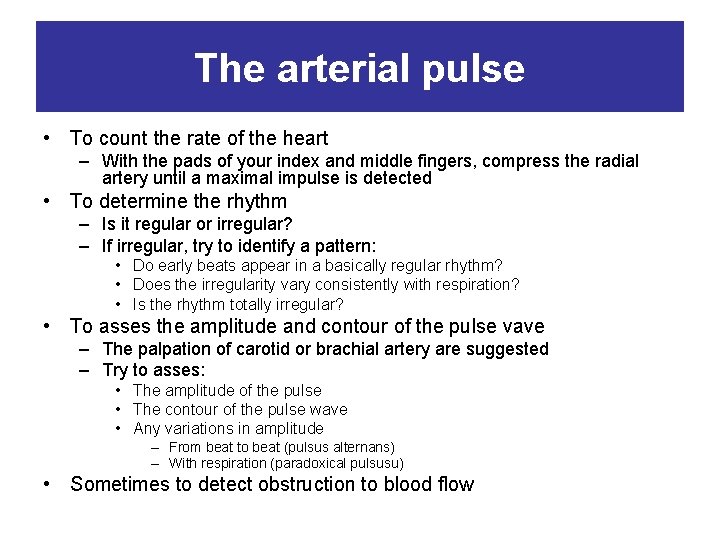
The arterial pulse • To count the rate of the heart – With the pads of your index and middle fingers, compress the radial artery until a maximal impulse is detected • To determine the rhythm – Is it regular or irregular? – If irregular, try to identify a pattern: • Do early beats appear in a basically regular rhythm? • Does the irregularity vary consistently with respiration? • Is the rhythm totally irregular? • To asses the amplitude and contour of the pulse vave – The palpation of carotid or brachial artery are suggested – Try to asses: • The amplitude of the pulse • The contour of the pulse wave • Any variations in amplitude – From beat to beat (pulsus alternans) – With respiration (paradoxical pulsusu) • Sometimes to detect obstruction to blood flow
Techniques of examination of carotid artery Your thumb should press just inside the medial border of the relaxed sternomastoid muscle, at the level of cricoid cartilage • Avoid pressing on the carotid sinus – at the level of the top of thyroid cartilage • Do not press on the both carotids at the same time
Palpation of peripheral arterial pulses • Brachial pulse: – Flex the elbow slightly, and with the thumb of your opposite hand palpate the artery just medial to the biceps tendon at the antecubital crease • Radial pulse: – palpate on the flexor surface of the wrist laterally • Femoral pulse: – Press deeply, below the inguinal ligament and about midway between the anterior superior iliac spine and the symphysis pubis • Popliteal pulse: – The patient’s knee should be somewhat flexed, the leg relaxed. Place the fingertips of both hands so that they just meet in the midline behind the knee and press them deeply into the popliteal fossa. • Dorsalis pedis pulse: – Feel the dorsum of foot just lateral to the extensor tendon of the great toe • Tibialis posterior pulse: – Curve your finger behind and slightly below the medial malleolus of the ankle
Examples of abnormalaties of arterial pulse • Decrease or absent of arterial pulse – indicates partial or complete occlusion proximally, most commonly due to arteriosclerosis obliterans • Exaggerated or widened pulse suggest pathologic dilatation of artery • Sudden arterial occlusion (embolism or thrombosis) causes pain and numbness. The limb distal to the occlusion becomes cold, pale, and pulseless.
Examination of a veins • Are the veins unusually prominent? – The standing posture allows any varicosity to fill with blood and makes them visible • Is the swelling unilateral or bilateral? – Unilateral edema with venous distension suggest venous cause of edema – Local swelling, redness, warmth, and a subcutaneous cord suggest superficial thrombophlebitis – Painful, pale, swollen leg, together with tenderness of the femoral vein, suggest deep iliofemoral thrombosis – Calf tenderness and cords deep in the calf suggest deep vein thrombosis there • Brownish areas near the ankles – chronic venous insufficiency • Feel the thickness of the skin – Thickened skin in lymphedema and advanced venous insufficiency
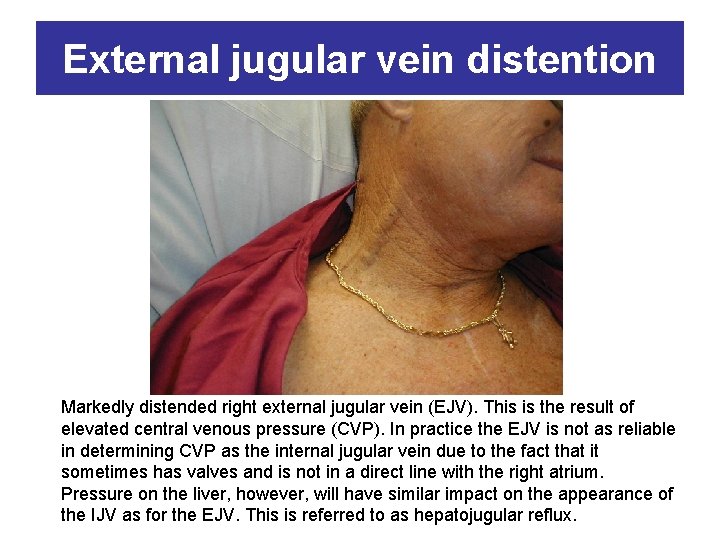
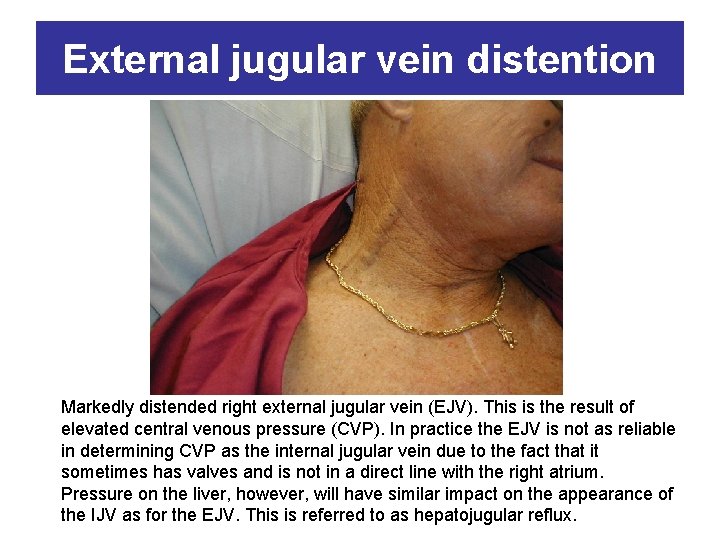
External jugular vein distention Markedly distended right external jugular vein (EJV). This is the result of elevated central venous pressure (CVP). In practice the EJV is not as reliable in determining CVP as the internal jugular vein due to the fact that it sometimes has valves and is not in a direct line with the right atrium. Pressure on the liver, however, will have similar impact on the appearance of the IJV as for the EJV. This is referred to as hepatojugular reflux.
 Heart vessels
Heart vessels In a great house there are vessels
In a great house there are vessels Right border of the relative cardiac dullness is formed by
Right border of the relative cardiac dullness is formed by Sheep heart labeled
Sheep heart labeled Heart to heart merrylands
Heart to heart merrylands Altar vestments and vessels
Altar vestments and vessels Lidded chalice like vessel
Lidded chalice like vessel These vessels have thicker walls and a heavier tunica media
These vessels have thicker walls and a heavier tunica media Lesson 12 blood and immune system
Lesson 12 blood and immune system Chapter 14 circulation and blood vessels
Chapter 14 circulation and blood vessels Liturgical objects
Liturgical objects Incisura anacrota
Incisura anacrota Type of blood system that has blood vessels and haemocoels
Type of blood system that has blood vessels and haemocoels Quizlet
Quizlet Types of capillaries
Types of capillaries Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton