ANESTHESIA FOR A GERIATRIC PATIENT WITH HEART DISEASE



- Slides: 22
ANESTHESIA FOR A GERIATRIC PATIENT WITH HEART DISEASE DR. BALAVENKAT, DR. KALYANASUNDARAM, DR. SUDARSHAN, DR. VENKATACHELLAM, DR. MAHES H
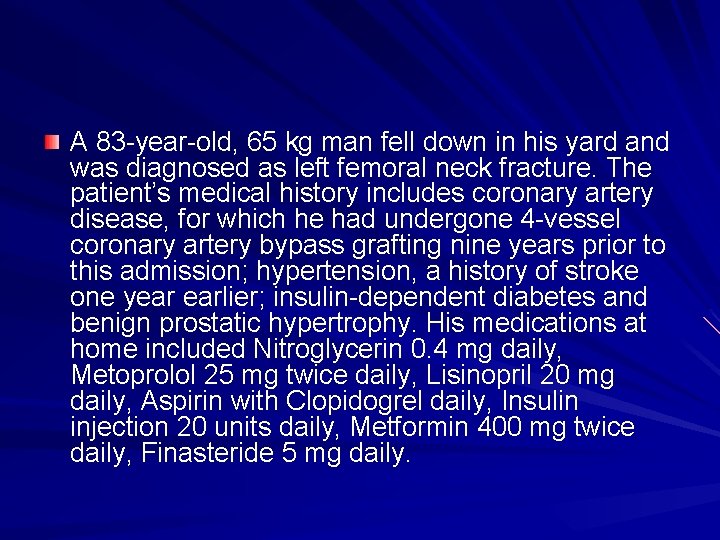
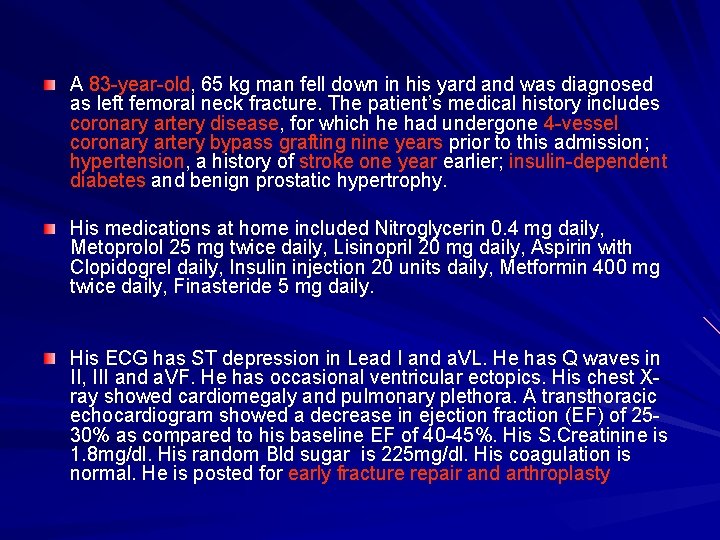
A 83 -year-old, 65 kg man fell down in his yard and was diagnosed as left femoral neck fracture. The patient’s medical history includes coronary artery disease, for which he had undergone 4 -vessel coronary artery bypass grafting nine years prior to this admission; hypertension, a history of stroke one year earlier; insulin-dependent diabetes and benign prostatic hypertrophy. His medications at home included Nitroglycerin 0. 4 mg daily, Metoprolol 25 mg twice daily, Lisinopril 20 mg daily, Aspirin with Clopidogrel daily, Insulin injection 20 units daily, Metformin 400 mg twice daily, Finasteride 5 mg daily.
His ECG has ST depression in Lead I and a. VL. He has Q waves in II, III and a. VF. He has occasional ventricular ectopics. His chest X-ray showed cardiomegaly and pulmonary plethora. A transthoracic echocardiogram showed a decrease in ejection fraction. EF is 25 -30% as compared to his baseline EF of 40 -45%. His S. Creatinine is 1. 8 mg/dl. His random Bld sugar is 225 mg/dl. His coagulation is normal. He is posted for early fracture repair and arthroplasty.
Dr. Sudarshan/Dr. Venkatachellam 1. What is the risk involved in this case? High or moderate ? 2. How do we stratify the risk in old age? Do they have an increased risk than their younger counterparts with same risk factors?
Dr. Kalyanasundaram/Dr. Balavenkat 3. Should we have to optimize him before taking him up for surgery? 4. What more information is needed? What should be done for optimization of his risk?
Dr. Sudarshan/Dr. Venkatachellam 5. How do we manage his medications? 6. What are the anesthetic concerns in this case?
Dr. Balavenkat/Dr. Venkatachellam 7. What kind of anesthetic is preferred? Regional or General? Does the type of anesthesia influence the outcomes? 8. Does the degree of monitoring influence the outcomes in this patient
Dr. Sudarshan/Dr. Kalyanasundaram 9. What postop complications can be expected in this patient? 10. How should we manage postop pain in this patient?

Panel discussion
A 83 -year-old, 65 kg man fell down in his yard and was diagnosed as left femoral neck fracture. The patient’s medical history includes coronary artery disease, for which he had undergone 4 -vessel coronary artery bypass grafting nine years prior to this admission; hypertension, a history of stroke one year earlier; insulin-dependent diabetes and benign prostatic hypertrophy. His medications at home included Nitroglycerin 0. 4 mg daily, Metoprolol 25 mg twice daily, Lisinopril 20 mg daily, Aspirin with Clopidogrel daily, Insulin injection 20 units daily, Metformin 400 mg twice daily, Finasteride 5 mg daily. His ECG has ST depression in Lead I and a. VL. He has Q waves in II, III and a. VF. He has occasional ventricular ectopics. His chest Xray showed cardiomegaly and pulmonary plethora. A transthoracic echocardiogram showed a decrease in ejection fraction (EF) of 2530% as compared to his baseline EF of 40 -45%. His S. Creatinine is 1. 8 mg/dl. His random Bld sugar is 225 mg/dl. His coagulation is normal. He is posted for early fracture repair and arthroplasty
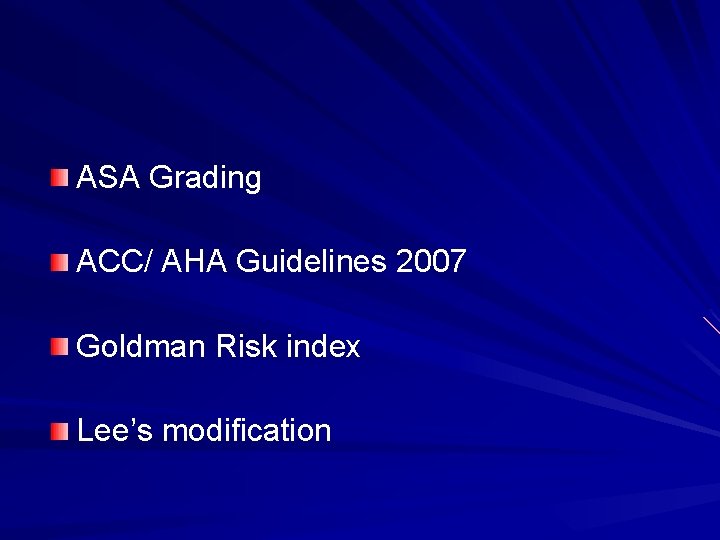
ASA Grading ACC/ AHA Guidelines 2007 Goldman Risk index Lee’s modification
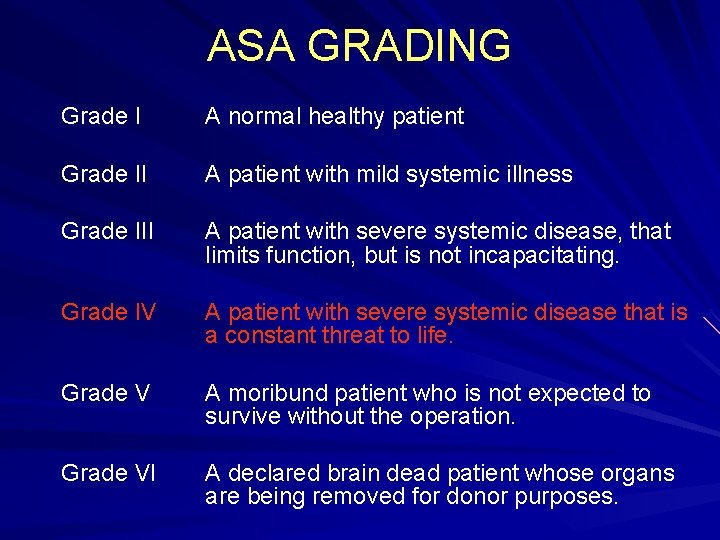
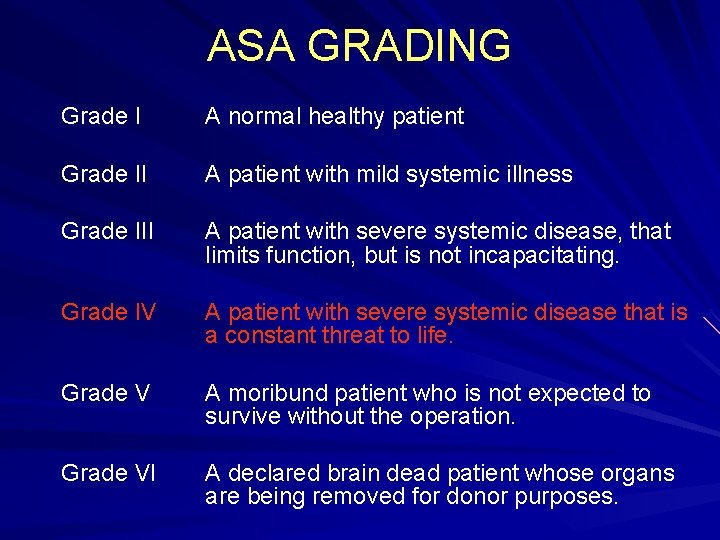
ASA GRADING Grade I A normal healthy patient Grade II A patient with mild systemic illness Grade III A patient with severe systemic disease, that limits function, but is not incapacitating. Grade IV Grade VI A patient with severe systemic disease that is a constant threat to life. A moribund patient who is not expected to survive without the operation. A declared brain dead patient whose organs are being removed for donor purposes.
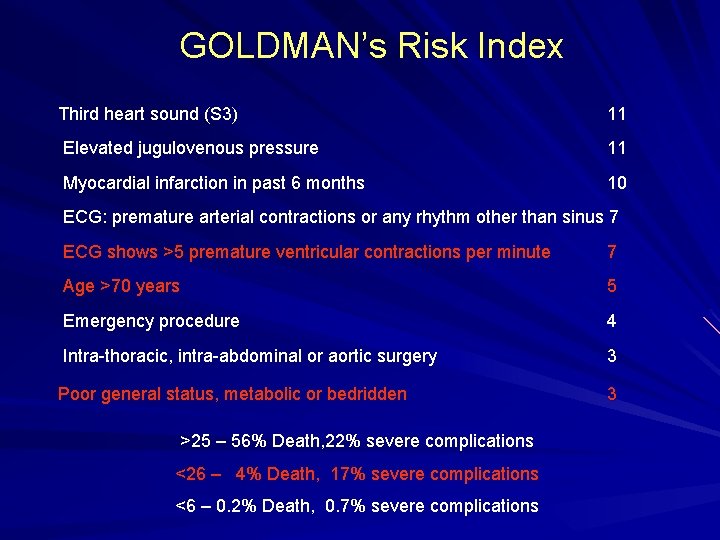
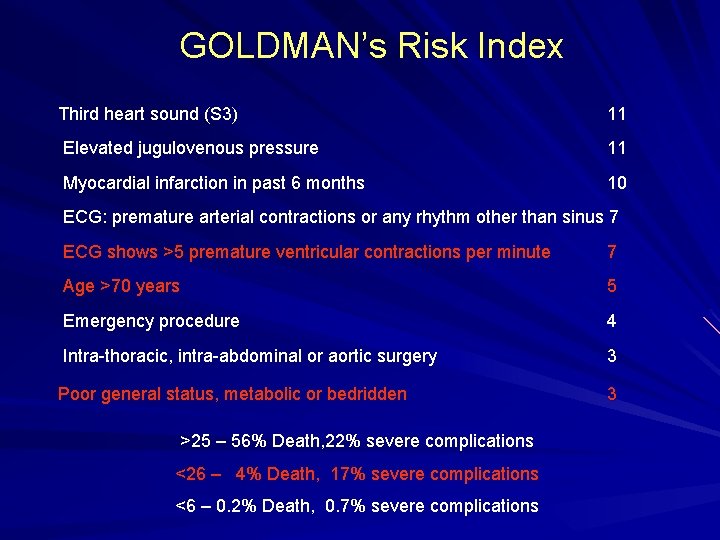
GOLDMAN’s Risk Index Third heart sound (S 3) 11 Elevated jugulovenous pressure 11 Myocardial infarction in past 6 months 10 ECG: premature arterial contractions or any rhythm other than sinus 7 ECG shows >5 premature ventricular contractions per minute 7 Age >70 years 5 Emergency procedure 4 Intra-thoracic, intra-abdominal or aortic surgery 3 Poor general status, metabolic or bedridden >25 – 56% Death, 22% severe complications <26 – 4% Death, 17% severe complications <6 – 0. 2% Death, 0. 7% severe complications 3
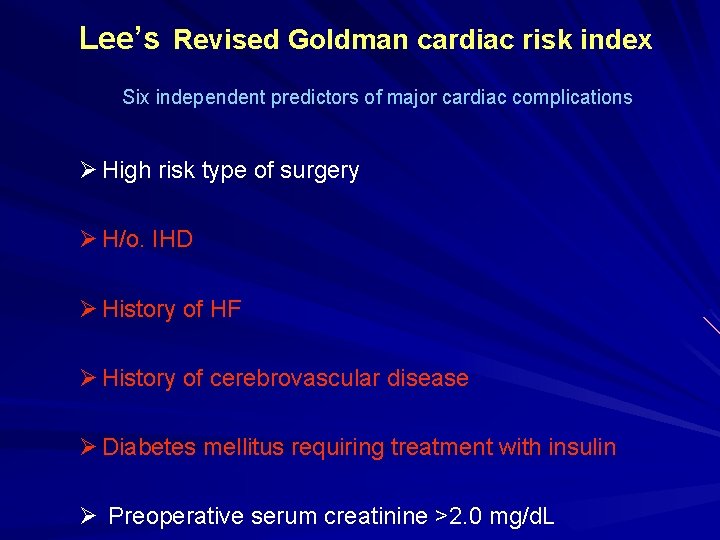
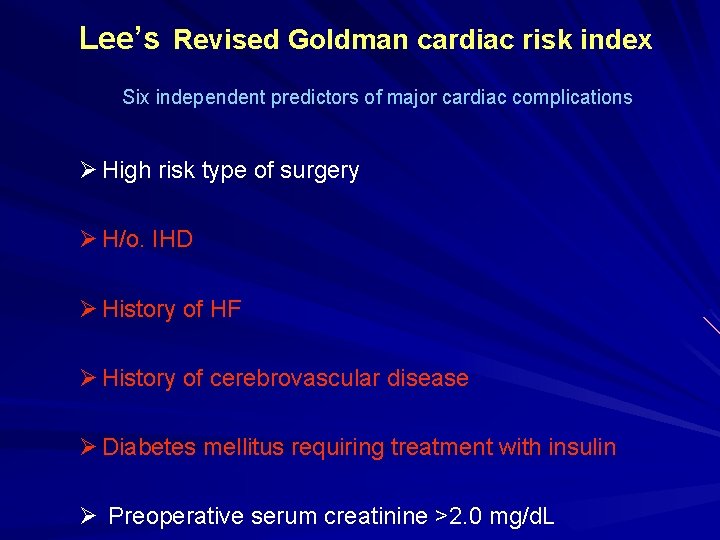
Lee’s Revised Goldman cardiac risk index Six independent predictors of major cardiac complications Ø High risk type of surgery Ø H/o. IHD Ø History of HF Ø History of cerebrovascular disease Ø Diabetes mellitus requiring treatment with insulin Ø Preoperative serum creatinine >2. 0 mg/d. L
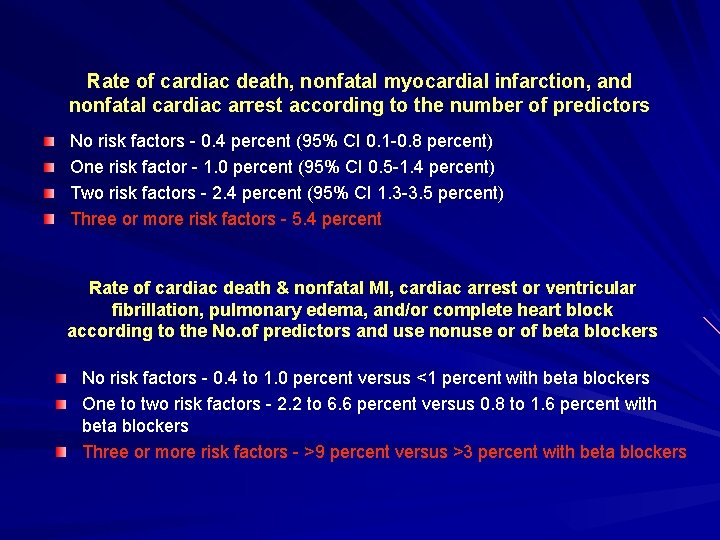
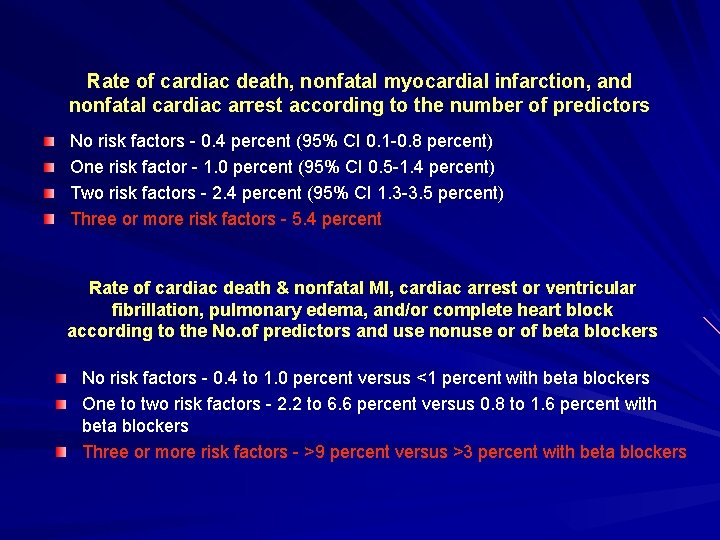
Rate of cardiac death, nonfatal myocardial infarction, and nonfatal cardiac arrest according to the number of predictors No risk factors - 0. 4 percent (95% CI 0. 1 -0. 8 percent) One risk factor - 1. 0 percent (95% CI 0. 5 -1. 4 percent) Two risk factors - 2. 4 percent (95% CI 1. 3 -3. 5 percent) Three or more risk factors - 5. 4 percent Rate of cardiac death & nonfatal MI, cardiac arrest or ventricular fibrillation, pulmonary edema, and/or complete heart block according to the No. of predictors and use nonuse or of beta blockers No risk factors - 0. 4 to 1. 0 percent versus <1 percent with beta blockers One to two risk factors - 2. 2 to 6. 6 percent versus 0. 8 to 1. 6 percent with beta blockers Three or more risk factors - >9 percent versus >3 percent with beta blockers
Detsky and Goldman calculators http: //www. vasgbi. com/riskdetsky. htm

ACC/ AHA Guidelines 2007
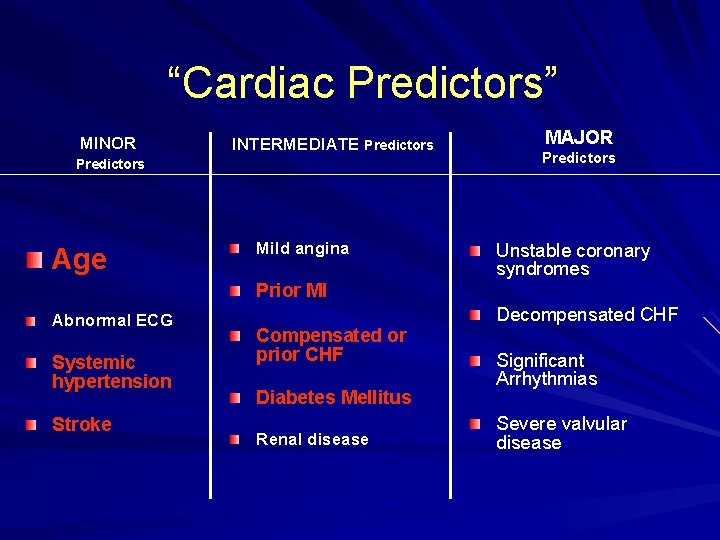
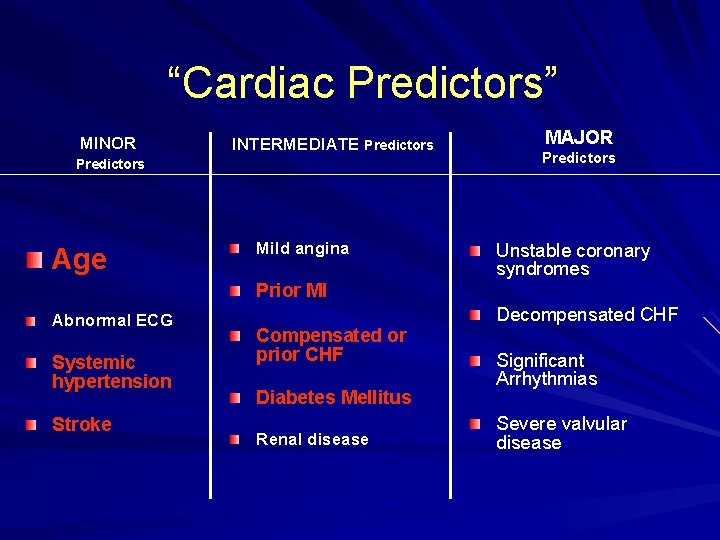
“Cardiac Predictors” MINOR INTERMEDIATE Predictors Age Mild angina Prior MI Abnormal ECG Systemic hypertension Stroke Compensated or prior CHF Diabetes Mellitus Renal disease MAJOR Predictors Unstable coronary syndromes Decompensated CHF Significant Arrhythmias Severe valvular disease
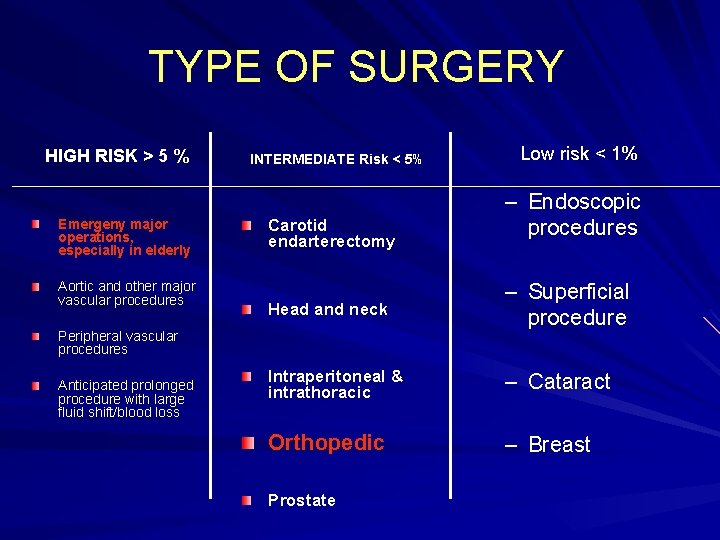
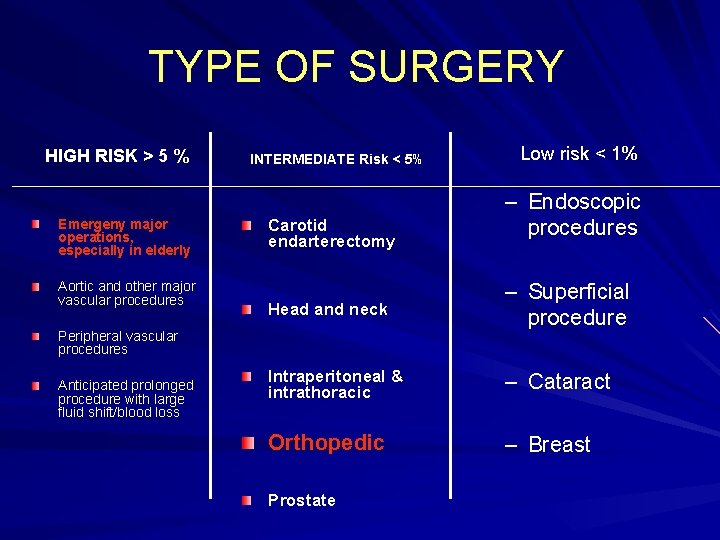
TYPE OF SURGERY HIGH RISK > 5 % Emergeny major operations, especially in elderly Aortic and other major vascular procedures INTERMEDIATE Risk < 5% Carotid endarterectomy – Endoscopic procedures Head and neck – Superficial procedure Intraperitoneal & intrathoracic – Cataract Orthopedic – Breast Peripheral vascular procedures Anticipated prolonged procedure with large fluid shift/blood loss Low risk < 1% Prostate
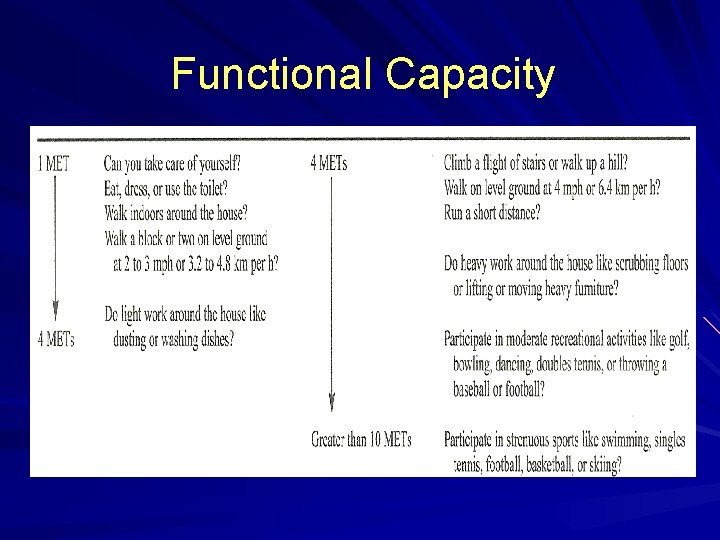
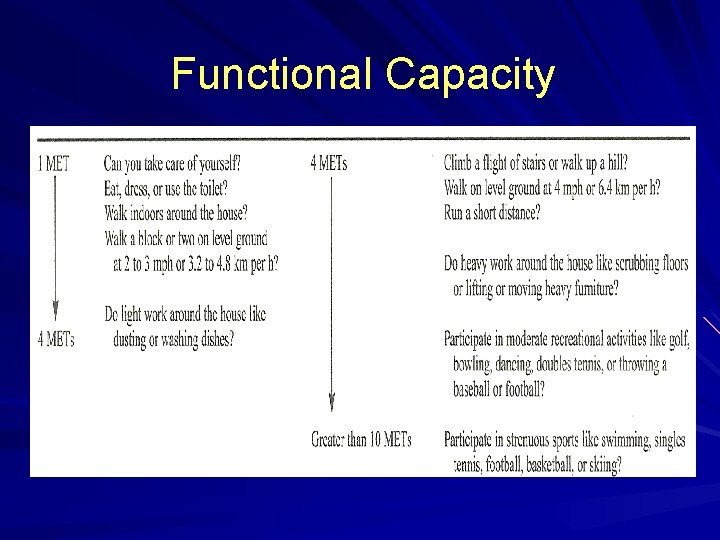
Functional Capacity
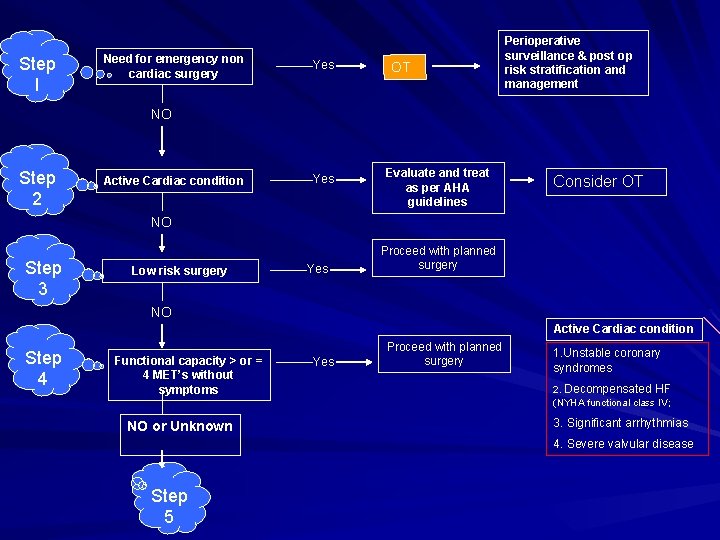
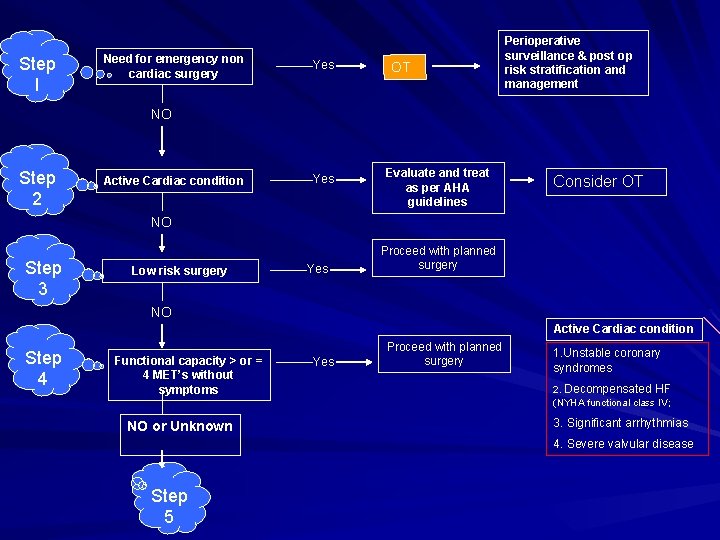
Step I Need for emergency non cardiac surgery Yes OT Perioperative surveillance & post op risk stratification and management NO Step 2 Active Cardiac condition Yes Evaluate and treat as per AHA guidelines Consider OT NO Step 3 Low risk surgery Yes Proceed with planned surgery NO Active Cardiac condition Step 4 Functional capacity > or = 4 MET’s without symptoms NO or Unknown Yes Proceed with planned surgery 1. Unstable coronary syndromes 2. Decompensated HF (NYHA functional class IV; 3. Significant arrhythmias 4. Severe valvular disease Step 5

History of CAD, or CVA Pulmonary STEP 5 Diabetes mellitus Renal impairment Hematologic disorders 3 or more risk factors Vascular 1 or 2 risk factors Intermediate risk Vascular No risk factors Intermediate risk Proceed with the planned surgery Consider testing if it will change management Proceed with planned surgery with HR Control or consider non invasive testing if it will change the management
 Patient 2 patient
Patient 2 patient Patient counselling for peptic ulcer disease
Patient counselling for peptic ulcer disease Bharathi viswanathan
Bharathi viswanathan Chronic coronary syndrome
Chronic coronary syndrome Feline
Feline Heart disease
Heart disease Causes of valvular heart disease
Causes of valvular heart disease Site:slidetodoc.com
Site:slidetodoc.com Chronic rheumatic heart disease
Chronic rheumatic heart disease Heart disease
Heart disease Ronaldo pictures
Ronaldo pictures Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pac vs pvc ecg
Pac vs pvc ecg Rheumatic heart disease
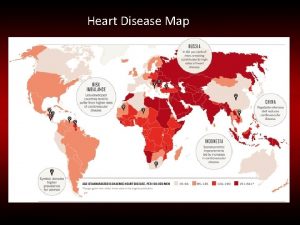
Rheumatic heart disease Heart disease data
Heart disease data Beau's lines autoimmune disease
Beau's lines autoimmune disease Heart disease symptoms
Heart disease symptoms Upper lobe diversion cxr
Upper lobe diversion cxr Terrible t's cyanotic heart disease
Terrible t's cyanotic heart disease Mitral facies
Mitral facies Tetralogy of fallot
Tetralogy of fallot Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Rheumatic heart disease
Rheumatic heart disease