Respiratory Emergencies Victor Politi M D FACP Medical





- Slides: 87
Respiratory Emergencies Victor Politi, M. D. , FACP Medical Director Physican Assistant Program

• Dyspnea • the sensation of breathlessness or inadequate breathing • the most common complaint of patients with cardiopulmonary diseases
• Dyspnea - common complaint/symptom • “shortness of breath” or “breathlessness” • Defined as abnormal/uncomfortable breathing • Multiple etiologies • 2/3 of cases - cardiac or pulmonary etiology
• When it becomes obvious to us that an individual IS breathing, and it's one of the first things that we noticed about this individual, then THAT needs to be one of the first things that we address. • Any patient who is presenting with some degree of respiratory effort is IN respiratory distress
• There is no one specific cause of dyspnea and no single specific treatment • Treatment varies according to patient’s condition • • chief complaint history exam laboratory & study results
Differential Diagnosis • Composed of four general categories • Cardiac • Pulmonary • Mixed cardiac or pulmonary • non-cardiac or non-pulmonary
Pulmonary Etiology • • • COPD Asthma Restrictive Lung Disorders Hereditary Lung Disorders Pneumonia Pneumothorax
Cardiac Etiology • • CHF CAD MI (recent or past history) Cardiomyopathy Valvular dysfunction Left ventricular hypertrophy Pericarditis Arrhythmias
Mixed Cardiac/Pulmonary Etiology • • COPD with pulmonary HTN and/or cor pulmonale Deconditioning Chronic pulmonary emboli Pleural effusion
Noncardiac or Nonpulmonary Etiology • • • Metabolic conditions (e. g. acidosis) Pain Trauma Neuromuscular disorders Functional (anxiety, panic disorders, hyperventilation) • Chemical exposure
Easily Performed Diagnostic Tests • Chest radiographs • Electrocardiograph • Screening spirometry
• In cases where test results inconclusive • complete PFTs • ABGs • EKG • Standard exercise treadmill testing/ or complete cardiopulmonary exercise testing • Consultation with pulmonologist/cardiologist may be useful
ABGs • • • Commonly used to evaluate acute dyspnea can provide information about altered p. H, hypercapnia, hypocapnia or hypoxemia normal ABGs do not exclude cardiac/pulmonary dx as cause of dyspnea • Remember- ABGs may be normal even in cases of acute dyspnea - ABGs do not evaluate breathing
PULSE OX • Rapid, widely available, noninvasive means of assessment in most clinical situations • insensitive (may be normal in acute dyspnea) • • The % of Oxygen saturation does not always correspond to Pa. O 2 The hemoglobin desaturation curve can be shifted depending on the p. H, temperature or arterial carbon monoxide or carbon dioxide levels
ASTHMA
What is Asthma • A Chronic disease of the airways that may cause: • Wheezing • Breathlessness • Chest tightness • Nighttime or early morning coughing

The bronchospasm characteristic of the acute asthmatic attack is typically reversible. It improves spontaneously or within minutes to hours of treatment
• Asthma can exist by itself or coexist with chronic bronchitis, emphysema, or bronchiectasis
Symptoms/Chief Complaint • • Progressive dyspnea Cough Chest tightness Wheezing/coughing
• The rapidly reversible airflow obstruction of asthma is mainly due to bronchial smooth muscle contraction
Focus of Therapy • • Pharmacologic manipulation of airway smooth muscle Do not overlook physiologic impairment caused by mucous production and mucosal edema Bronchospasm can be reversed in minutes Airflow obstruction due to mucous plugging and inflammatory changes in bronchial walls may not resolve for days/weeks • may lead to atelectasis, infectious bronchitis, pneumonitis
Asthma Triggers • • Immunologic reaction Viral respiratory/sinus infections change in temperature/humidity Drugs/Chemicals • aspirin, NSAIDS • • Exercise GE reflux Laughing/coughing Environmental factors • strong odors, pollutants, dust, fumes
Patient Exam • Wheezing • may be audible w/o stethoscope • • • Use of accessory muscles of inspiration diaphragmatic fatigue Paradoxical respirations • - reflect impending ventilatory failure • Altered mental status • lethargy, exhaustion, agitation, confusion
Patient Exam • • • Hypersonance to percussion decreased intensity of breath sounds prolongation of expiratory phase w or w/o wheezing
Patient Exam • The intensity of the wheeze may not correlate with the severity of airflow obstruction • “quiet chest” - very severe airflow obstruction
Asthma Treatment • • Nebulized B-adrenergic drugs Corticosteroids Nebulized anticholinergics Magnesium sulfate Oxygen Long acting beta-agonists Inhaled steroids
Managing Asthma: • Indications of a severe attack: • Breathless at rest • hunched forward • talking in words rather than sentences • Agitated • Peak flow rate less than 60% of normal
Treatment Goals of Severe Asthma • • • Improve airway function rapidly Avoid hypoxemia Prevent respiratory failure and death
COPD
COPD • • • Hallmark symptom - Dyspnea Chronic productive cough Minor hemoptysis pink puffer blue bloater
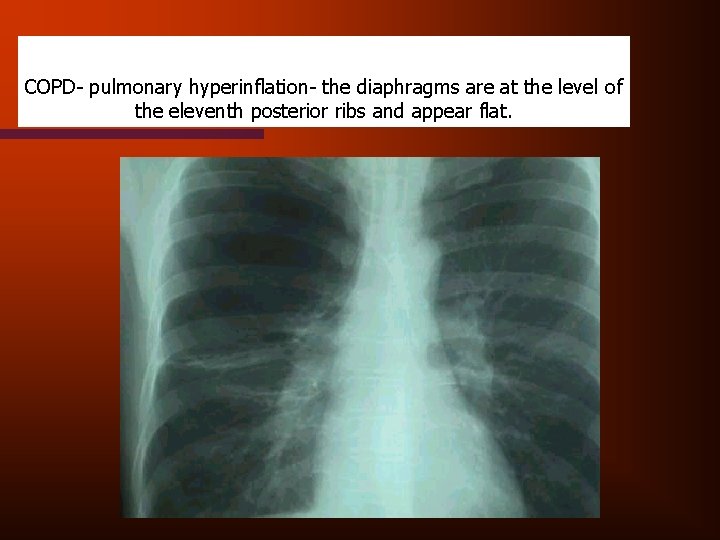
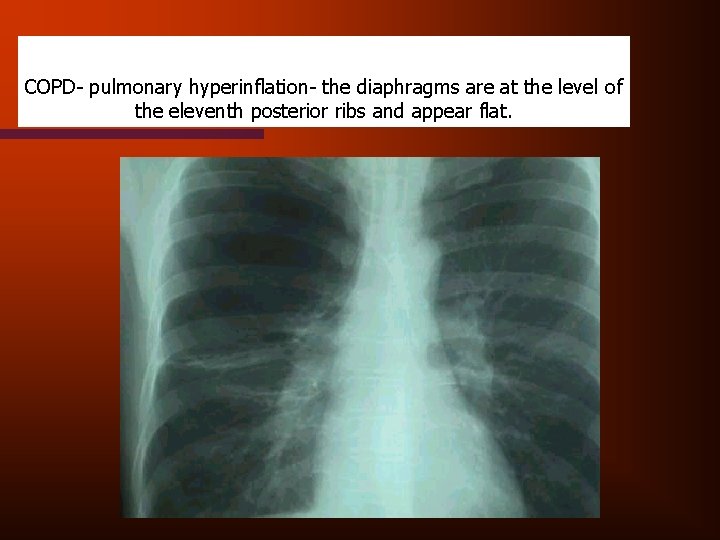
COPD- pulmonary hyperinflation- the diaphragms are at the level of the eleventh posterior ribs and appear flat.
COPD - Physical Findings • • Tachypnea Accessory respiratory muscle use Pursed lip exhalation Weight loss due to poor dietary intake and excessive caloric expenditure for work of breathing

Dominant Clinical Forms of COPD • • Pulmonary emphysema Chronic bronchitis • Most patients exhibit a mixture of symptoms and signs
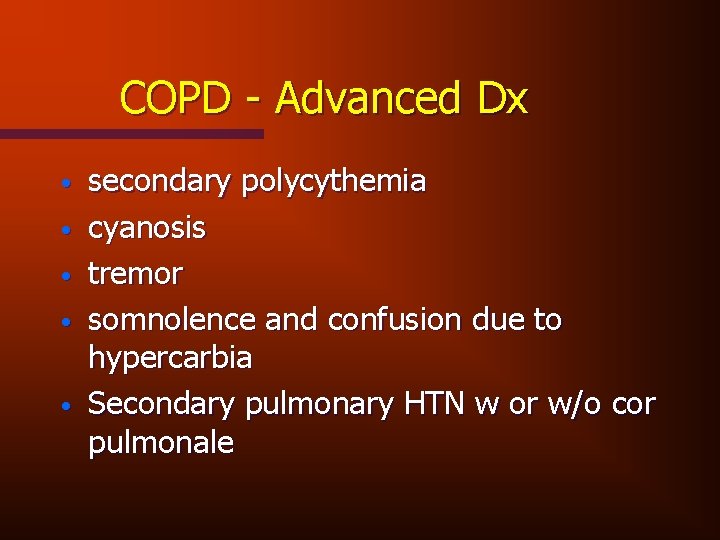
COPD - Advanced Dx • • • secondary polycythemia cyanosis tremor somnolence and confusion due to hypercarbia Secondary pulmonary HTN w or w/o cor pulmonale
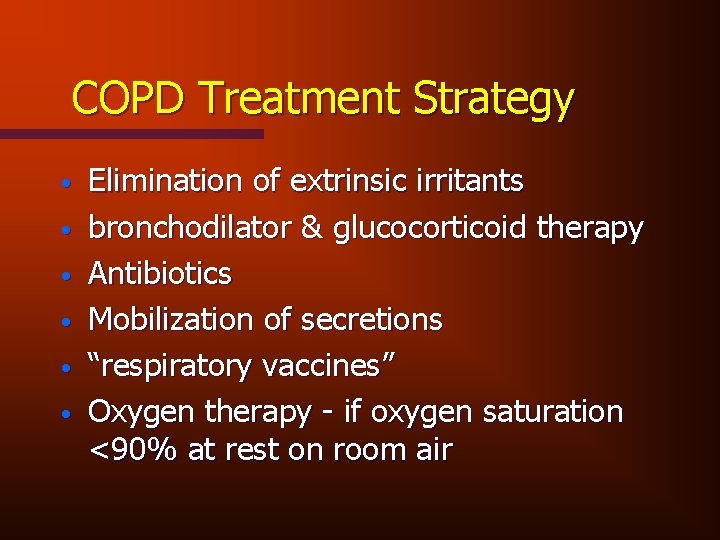
COPD Treatment Strategy • • • Elimination of extrinsic irritants bronchodilator & glucocorticoid therapy Antibiotics Mobilization of secretions “respiratory vaccines” Oxygen therapy - if oxygen saturation <90% at rest on room air
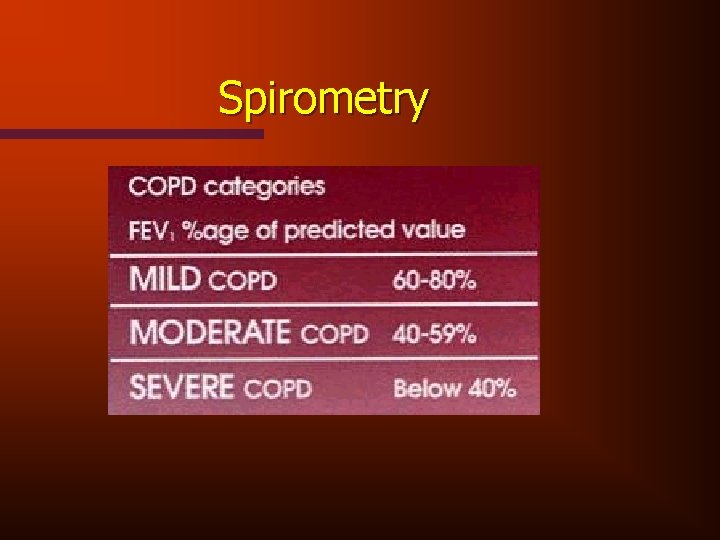
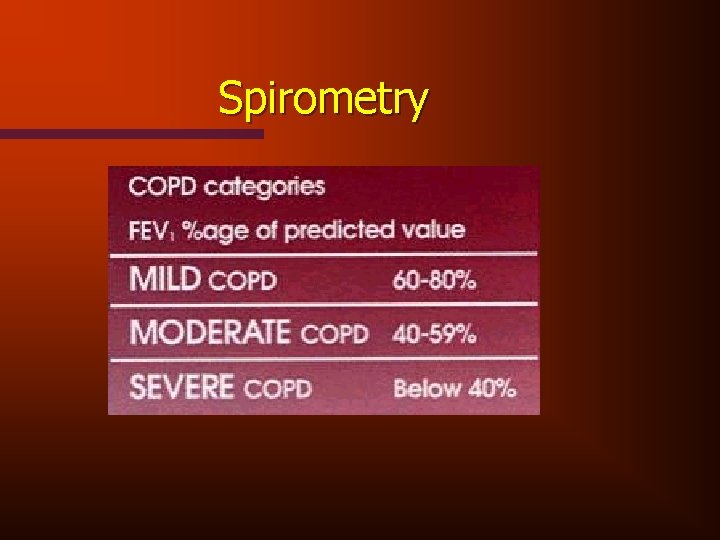
Spirometry

PNEUMONIA
• 6 th leading cause of death in the US • Respiratory viruses & mycoplasma responsible for greater than 1/3 of cases
Common types of respiratory infections • • Tracheobronchitis Pneumonia Effusions Empyema Abscess Cavitary lesions post-obstructive
Common Respiratory Viruses • • Influenza A & B Parainfluenza 1& 3 Respiratory Syncytial Virus Adenovirus Cytomegalovirus Herpes Simplex & Zoster/varicella Hanta Virus Infection
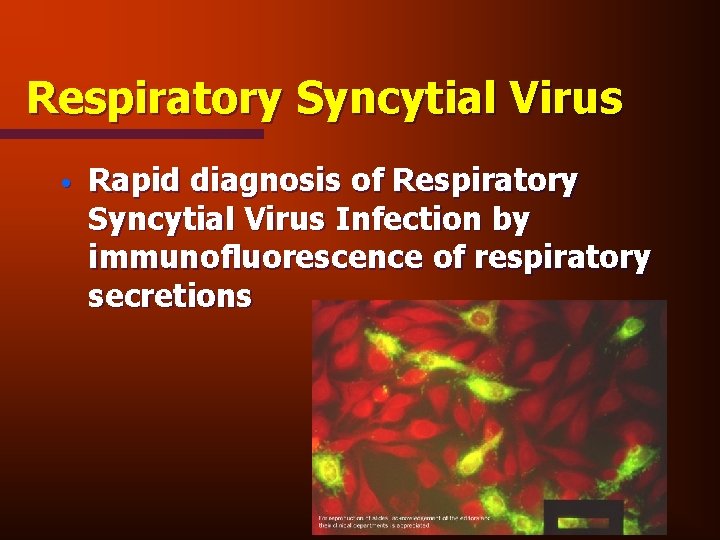
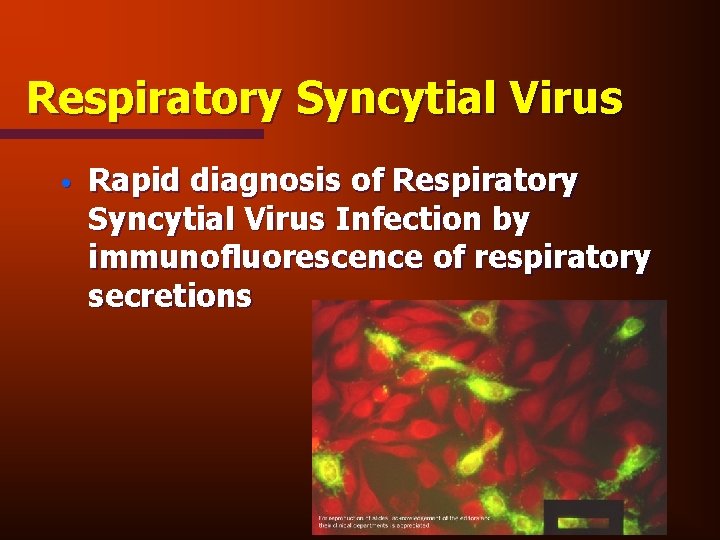
Respiratory Syncytial Virus • Rapid diagnosis of Respiratory Syncytial Virus Infection by immunofluorescence of respiratory secretions
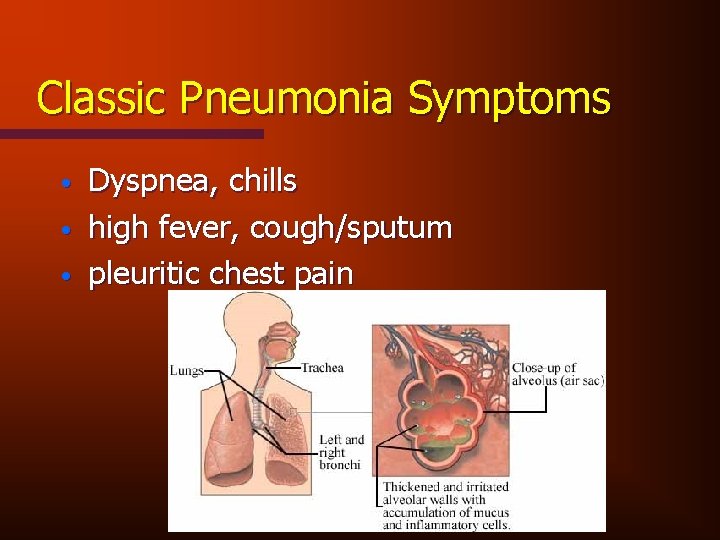
Classic Pneumonia Symptoms • • • Dyspnea, chills high fever, cough/sputum pleuritic chest pain
Viral Pneumonia - symptoms • • Chest Pain Fever Dyspnea Prodrome - malaise, upper respiratory symptoms, and other GI symptoms
Viral pneumonia Clinical Findings • • Minimal/variable Chest exam - may reveal wheezing Fine rales if heard can signify interstitial involvement Chest x-ray - patchy densities or interstitial involvement
Viral pneumonia Management /Prophylaxis • • • Supportive treatment - decrease severity of symptoms bed rest analgesics expectorants Patients w/ • airway obstruction - treat w/bronchodilators • secondary bacterial infection - antibiotics
Atypical Pneumonia • • • Accounts for 25% of community acquired pneumonias Mycoplasma/chlamyda/legionella can case extrapulmonary manifestations • meningitis, encephalitis, pericarditis, hepatitis, hemolytic anemia • typically bilateral infiltrates on chest x-ray • primarily effects younger persons
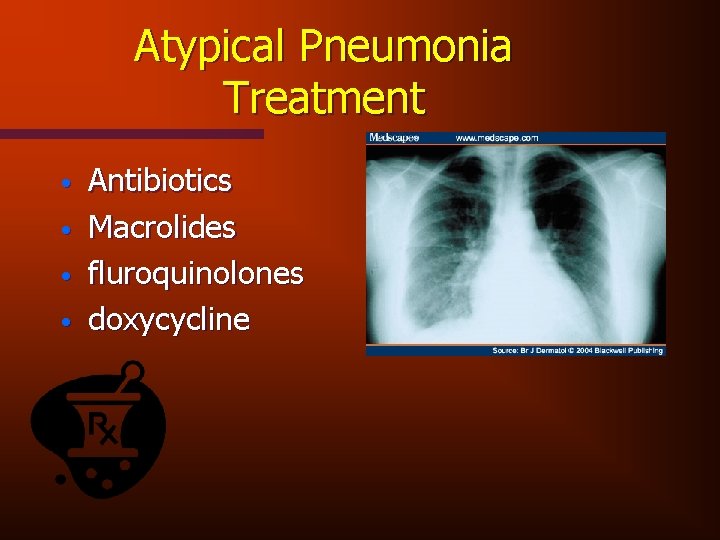
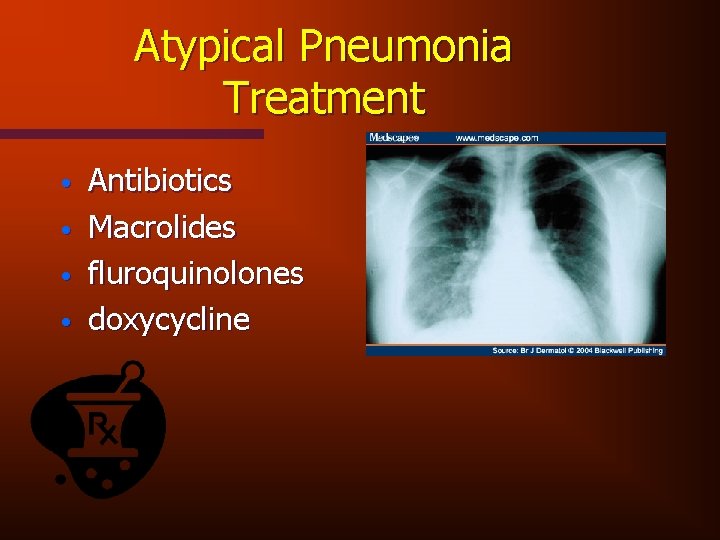
Atypical Pneumonia Treatment • • Antibiotics Macrolides fluroquinolones doxycycline

Bacterial pneumonia • • • 3. 3 million cases yearly in US responsible for 10% of hospital admissions unilateral infiltrate on x-ray high mortality in elderly population most common cause pneumococcal followed by haemophilus influenza
• Pneumococcus pneumonia accounts for up to 90% of all bacterial pneumonias • Patients with a chronic Dx are at an increased risk of contracting pneumonia
Bacterial pneumonia presentation • • acute shaking - chills tachypnea tachycardia malaise anorexia myalgias flank or back pain vomiting
Lab Tests • • WBC Chest X-ray Pulse Ox ABGs Sputum exam Blood cultures pleural fluid exam
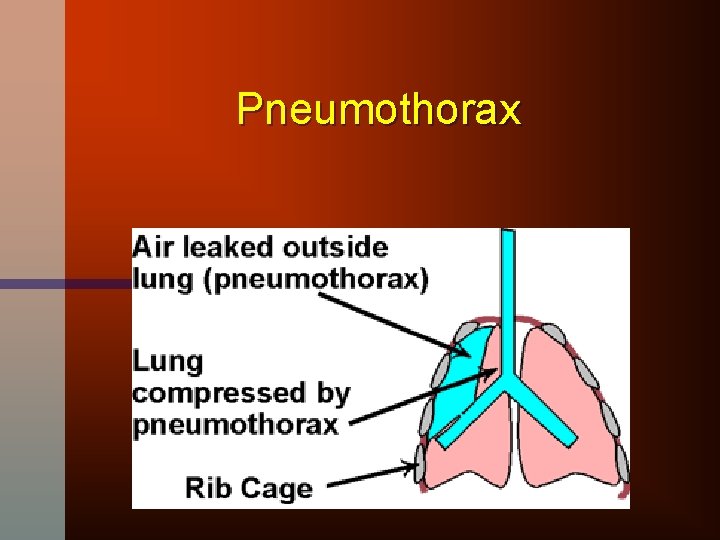
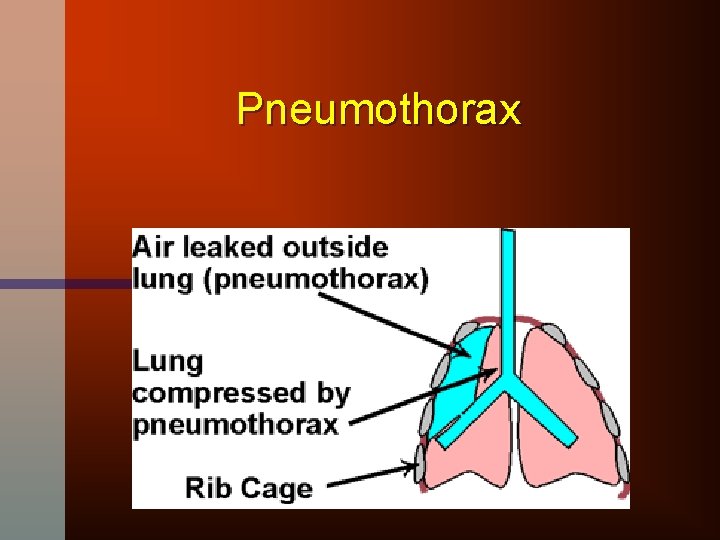
Pneumothorax
Causes of Spontaneous Pneumothorax • Pleural blebs • Bullae • Emphysema • Interstitial lung disease • Alpha 1 antitrypsin deficiency
Traumatic and Iatrogenic Causes • • Penetrating wounds Line placements Lung biopsies Mechanical ventilation
Two most common symptoms • • Dyspnea Chest pain
Physical Examination • • • Decreased breath sounds hyperresonance to percussion decreased tactile fremitus • In patients with emphysema - clinical findings may be subtle
Chest X-ray to Confirm Dx • 500 ml of air required to visualize pneumothorax on x-ray • Characterized by • hyperlucency and lack of lung markings at the periphery of the lung and appearance of fine line that represents the retraction of the visceral from the parietal pleura
Treatment Options • • • Observation - if pneumothorax involves < 15 -20% of hemithorax and patient relatively asymptomatic Tube thoracostomy Simple Aspiration
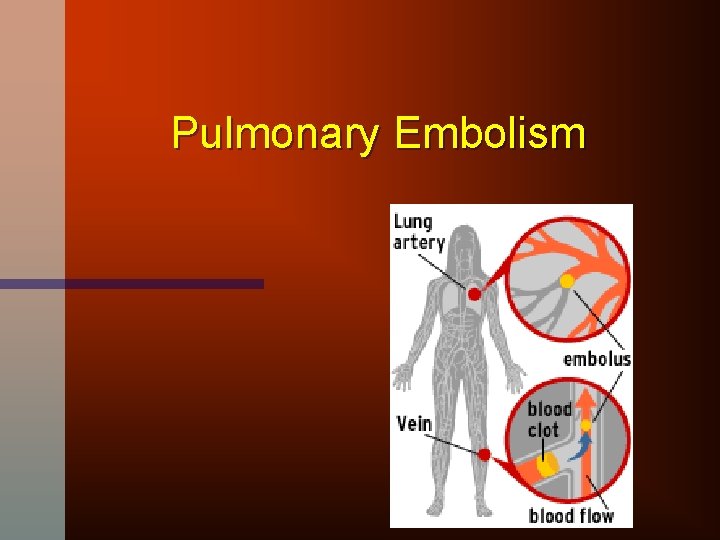
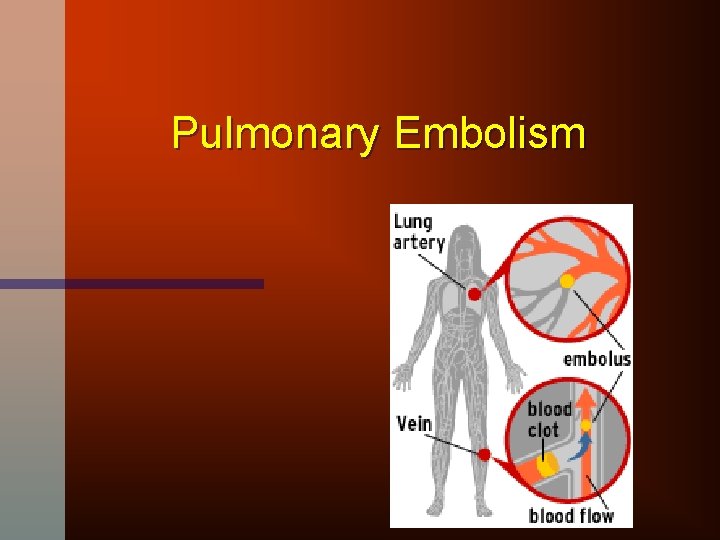
Pulmonary Embolism
PE History • PE is so common and deadly that the dx should be considered in any patient who presents with chest symptoms that cannot be proven to have another cause
PE Risk Markers • • Hypercoagulable states Prior hx of DVT or PE Recent surgery or pregnancy Prolonged immobolization Underlying malignancy smoking birth control pills trauma
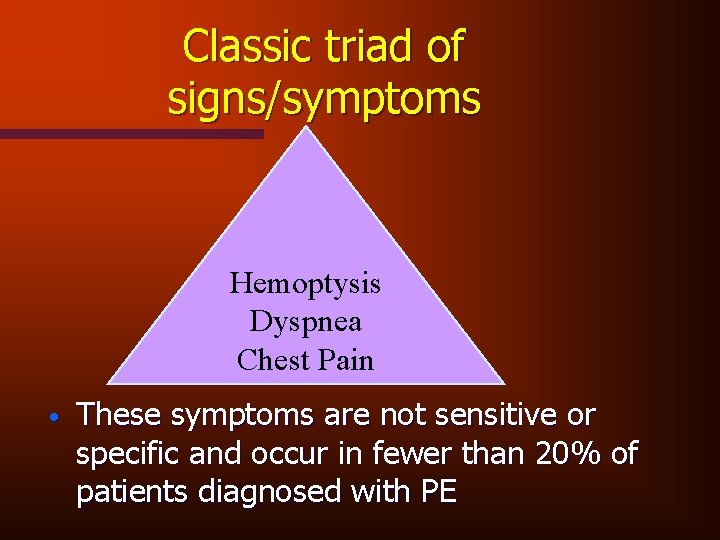
Classic triad of signs/symptoms Hemoptysis Dyspnea Chest Pain • These symptoms are not sensitive or specific and occur in fewer than 20% of patients diagnosed with PE
PE Physical Exam • • • Massive PE causes hypotension due to acute cor pulmonale Physical findings in early submassive PE may be completely normal Initially, abnomal findings are absent in most patients with PE
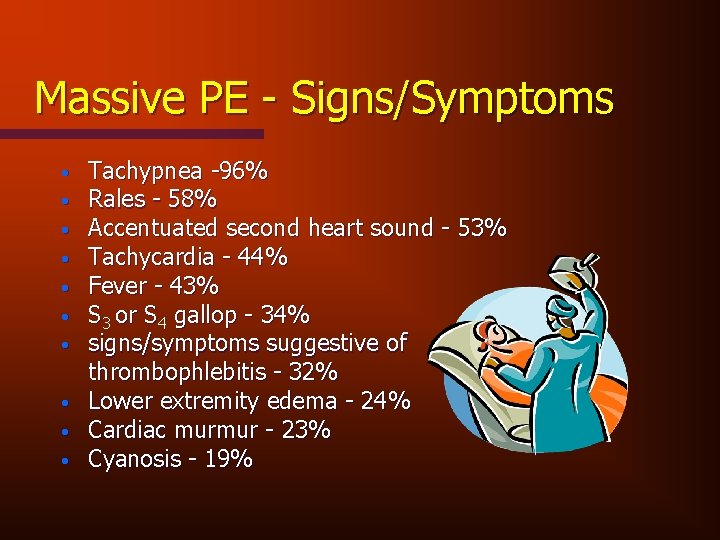
Massive PE - Signs/Symptoms • • • Tachypnea -96% Rales - 58% Accentuated second heart sound - 53% Tachycardia - 44% Fever - 43% S 3 or S 4 gallop - 34% signs/symptoms suggestive of thrombophlebitis - 32% Lower extremity edema - 24% Cardiac murmur - 23% Cyanosis - 19%
Massive PE Diagnostic Studies • • VQ scan Pulmonary angiography CT Echocardiography (TEE) Pulmonary artery catheterization Diagnostic algorithm D-dimer blood gases increased A-a gradient
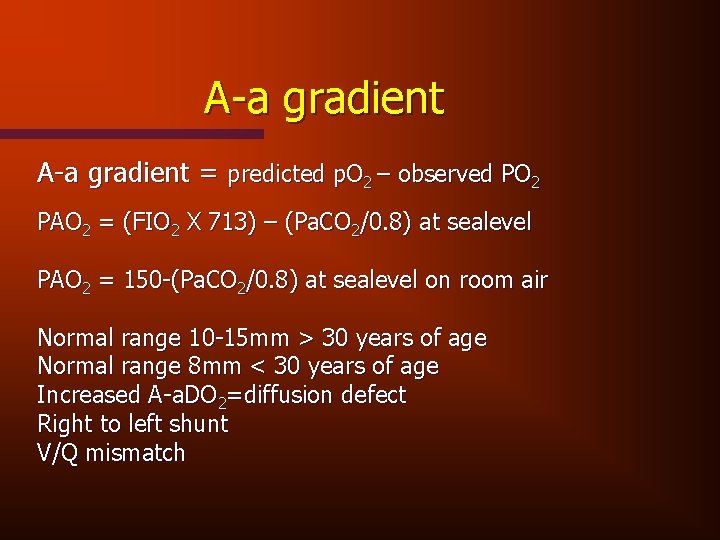
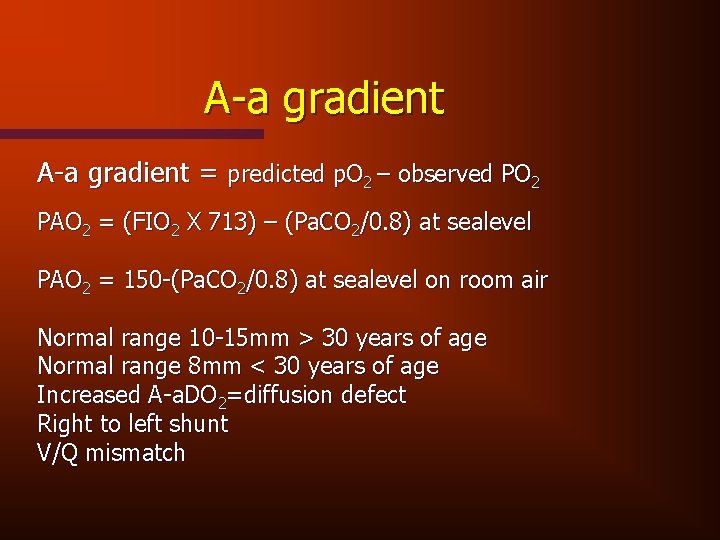
A-a gradient = predicted p. O 2 – observed PO 2 PAO 2 = (FIO 2 X 713) – (Pa. CO 2/0. 8) at sealevel PAO 2 = 150 -(Pa. CO 2/0. 8) at sealevel on room air Normal range 10 -15 mm > 30 years of age Normal range 8 mm < 30 years of age Increased A-a. DO 2=diffusion defect Right to left shunt V/Q mismatch
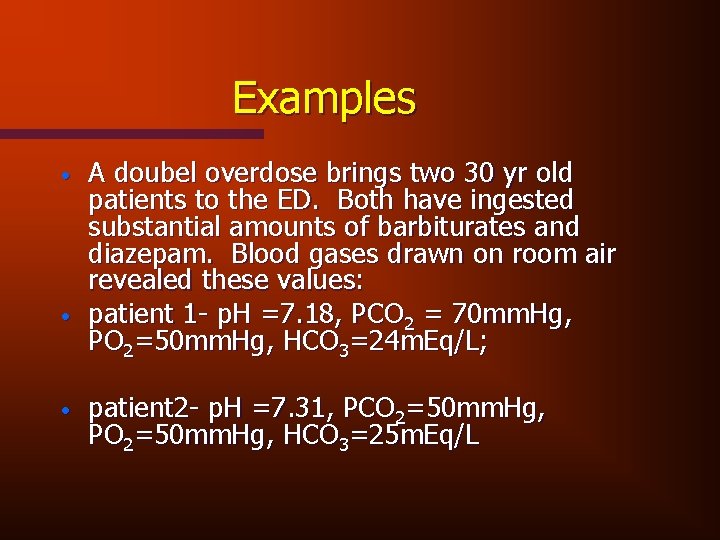
Examples • • • A doubel overdose brings two 30 yr old patients to the ED. Both have ingested substantial amounts of barbiturates and diazepam. Blood gases drawn on room air revealed these values: patient 1 - p. H =7. 18, PCO 2 = 70 mm. Hg, PO 2=50 mm. Hg, HCO 3=24 m. Eq/L; patient 2 - p. H =7. 31, PCO 2=50 mm. Hg, PO 2=50 mm. Hg, HCO 3=25 m. Eq/L
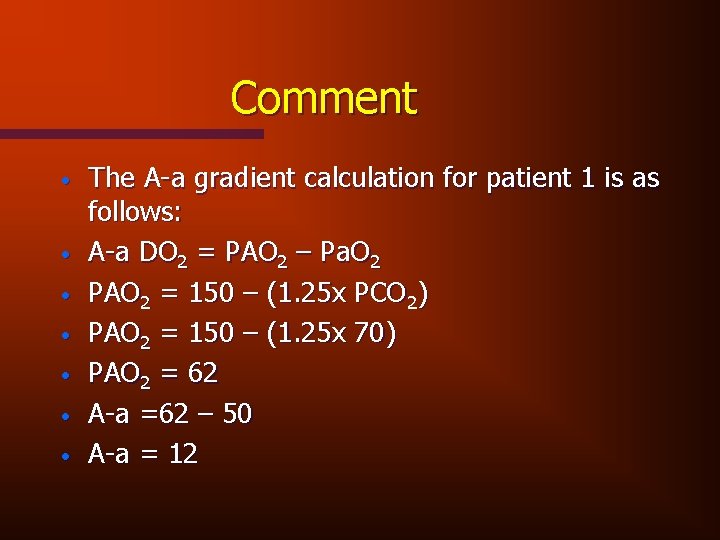
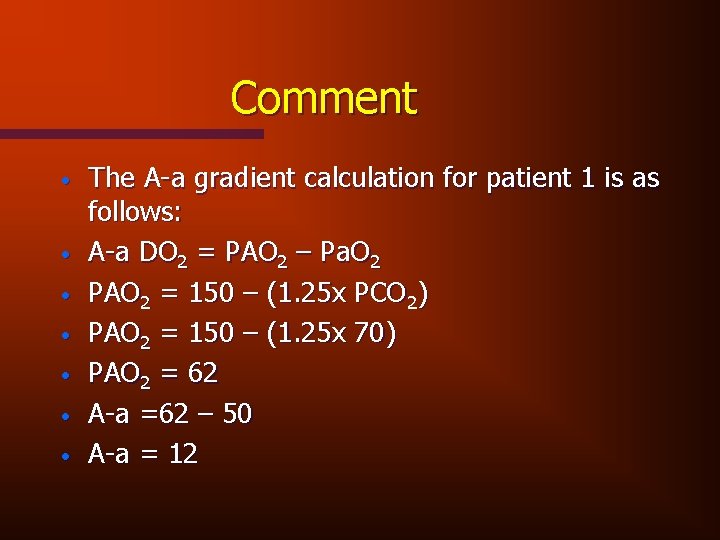
Comment • • The A-a gradient calculation for patient 1 is as follows: A-a DO 2 = PAO 2 – Pa. O 2 PAO 2 = 150 – (1. 25 x PCO 2) PAO 2 = 150 – (1. 25 x 70) PAO 2 = 62 A-a =62 – 50 A-a = 12
Comment • The calculation reveals a normal gradient, indicating that the etiology for hypoxemia and hypoventilation is extrinsic to the lung itself.
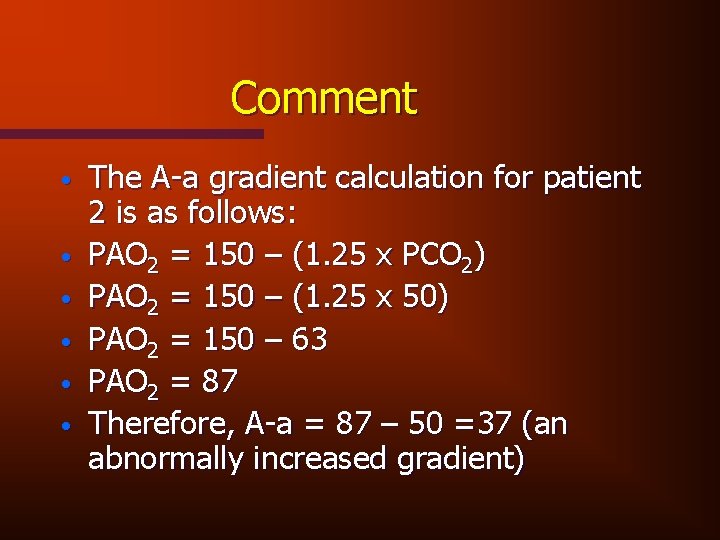
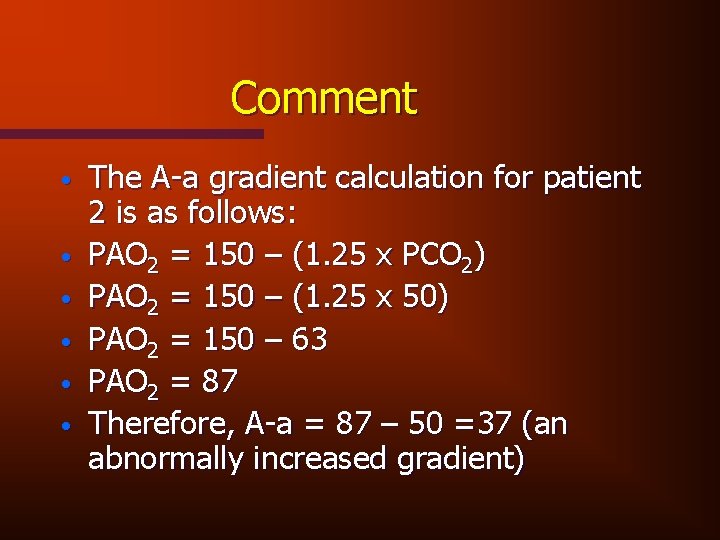
Comment • • • The A-a gradient calculation for patient 2 is as follows: PAO 2 = 150 – (1. 25 x PCO 2) PAO 2 = 150 – (1. 25 x 50) PAO 2 = 150 – 63 PAO 2 = 87 Therefore, A-a = 87 – 50 =37 (an abnormally increased gradient)
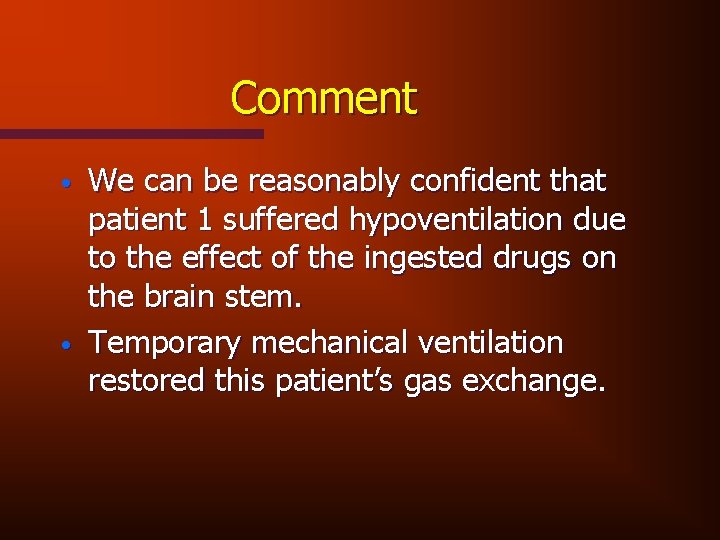
Comment • • We can be reasonably confident that patient 1 suffered hypoventilation due to the effect of the ingested drugs on the brain stem. Temporary mechanical ventilation restored this patient’s gas exchange.
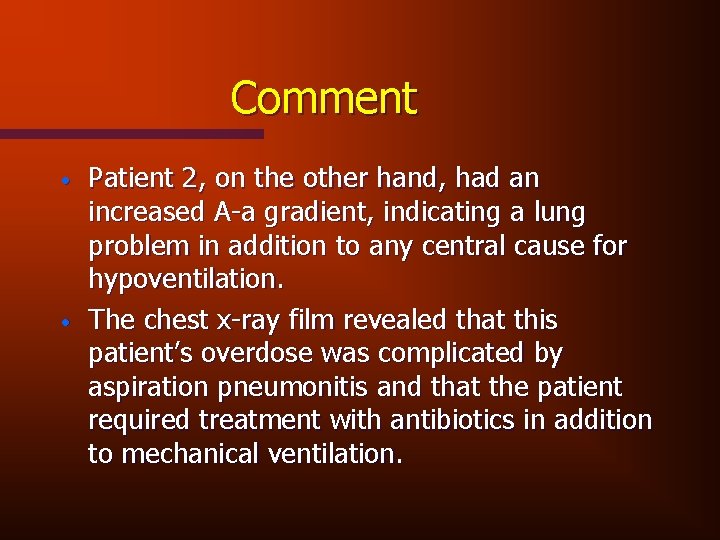
Comment • • Patient 2, on the other hand, had an increased A-a gradient, indicating a lung problem in addition to any central cause for hypoventilation. The chest x-ray film revealed that this patient’s overdose was complicated by aspiration pneumonitis and that the patient required treatment with antibiotics in addition to mechanical ventilation.
Treatment Strategies • • • Fluid administration anticoagulation Vena caval interruption Thrombolytics oxygen pulse ox
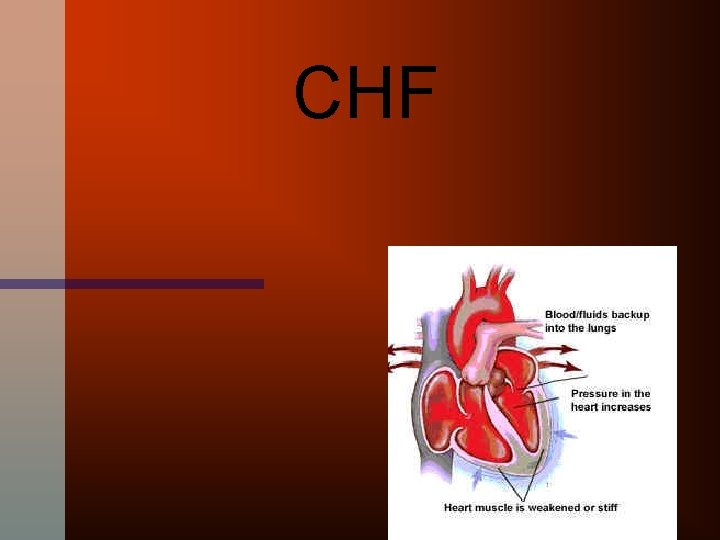
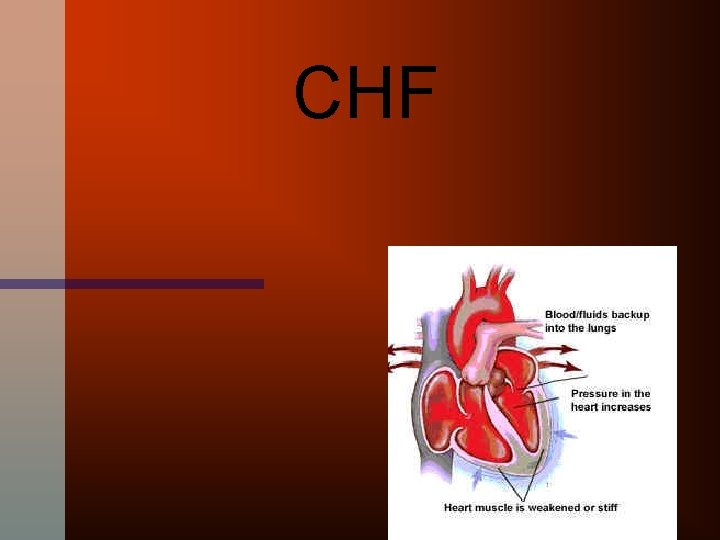
CHF
Left sided Failure • Blood/fluid back-up into the lungs result in • SOB • Fatigue • Cough (especially at night) • PND • orthopnea
Right sided Failure • Build-up of fluid in the veins • Edema of feet, legs and ankles • may effect liver/portal circulation and 3 rd spacing into soft tissue/ascites/pleural effusion
Causes of CHF • Variety of cardiac diseases • Most common cause of CHF - CAD • other causes - valvular heart dx, HTN, cardiomyopathies, myocarditis, renal dx, fluid overload, liver dx w/loss of protein and osmotic forces, high altitude and many others
Physical Findings • • • Peripheral edema JVD tachycardia tachypnea, using accessory muscles of respiration Skin - diaphoretic/cold/gray/cyanotic Wheezing/rales on ausculation Apical impulse displaced laterally ascites hepatosplenomegaly
Diagnostic Work-Up • • History Physical exam EKG Echo Chest x-ray BNP ABG/pulse ox
Treatment • • • Diuretics Digitalis Peripheral vasodilators/NTG Positive inotropic agents ACE inhibitors Beta blockers Oxygen MS 04 BNP
• Respiratory distress is FRIGHTENING! • Feelings of confinement, claustrophobia, restlessness, and anxiety accompany a realization that DEATH may be imminent. • All of this, in a patient that is, most likely, normally mentated and aware of what is happening. • If you never before had any reason to "dig deep" and draw out true human compassion for a patient, THIS IS THE TIME TO DO IT!
Questions ?
 Victor politi
Victor politi Victor politi
Victor politi Type i
Type i Victor politi
Victor politi Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Rachel politi
Rachel politi Conducting zone of the respiratory system
Conducting zone of the respiratory system Medical terminology for respiratory system
Medical terminology for respiratory system Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Immunologic emergencies
Immunologic emergencies Chapter 35 geriatric emergencies
Chapter 35 geriatric emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 17 neurologic emergencies
Chapter 17 neurologic emergencies Padi quiz 1 answers
Padi quiz 1 answers Chapter 13 handling emergencies
Chapter 13 handling emergencies Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies Psychiatric emergency
Psychiatric emergency Chapter 28 lesson 1
Chapter 28 lesson 1 Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies Chapter 22 psychiatric emergencies
Chapter 22 psychiatric emergencies Qut security contact number for emergencies
Qut security contact number for emergencies Pumberton sign
Pumberton sign Cartersville medical center medical records
Cartersville medical center medical records Greater baltimore medical center medical records
Greater baltimore medical center medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate California medical license application
California medical license application Torrance memorial hospital medical records
Torrance memorial hospital medical records Victor hugo desejo
Victor hugo desejo Msaludjujuy gestión ambulatoria
Msaludjujuy gestión ambulatoria Texte victor le maladroit
Texte victor le maladroit Motecuzoma ilhuicamina 179 turno matutino
Motecuzoma ilhuicamina 179 turno matutino Victor hugo anecdote
Victor hugo anecdote Victor hugo poema te deseo
Victor hugo poema te deseo Victor hugo knihy
Victor hugo knihy Victor quia victima
Victor quia victima Dr victor christiansen
Dr victor christiansen Victor jimmy arbulu martinez
Victor jimmy arbulu martinez Respiracion apneustica
Respiracion apneustica Victor douville
Victor douville Ift3355
Ift3355 Miguel bern
Miguel bern Casa tassel horta
Casa tassel horta Analogue and digital images
Analogue and digital images External conflicts in frankenstein
External conflicts in frankenstein Texto partidas e chegadas victor hugo
Texto partidas e chegadas victor hugo Victor insulators inc
Victor insulators inc Victor dimitri
Victor dimitri Partida e chegada (victor hugo)
Partida e chegada (victor hugo) Victor manuel ugalde saldivar
Victor manuel ugalde saldivar Victor hugo introduction
Victor hugo introduction Victor khomenko
Victor khomenko Victor farinelli
Victor farinelli En que coincide víctor y marisol
En que coincide víctor y marisol Victor babes university of medicine
Victor babes university of medicine Victor shia
Victor shia Les femmes sont sur la terre victor hugo
Les femmes sont sur la terre victor hugo Victor cairo arcelormittal
Victor cairo arcelormittal Victor luygg
Victor luygg Soleil couchants victor hugo
Soleil couchants victor hugo Con víctor
Con víctor Byronic hero qualities
Byronic hero qualities Victor chapela
Victor chapela Frankenstein chapter 24
Frankenstein chapter 24 Sessad victor duruy
Sessad victor duruy Greenberrg
Greenberrg Exposé sur victor hugo
Exposé sur victor hugo Victor carter-bey
Victor carter-bey Who is mr. kirwin and how does he treat victor?
Who is mr. kirwin and how does he treat victor? Victor hugo fabl
Victor hugo fabl Victor kuarsingh
Victor kuarsingh Victor brauner hitler
Victor brauner hitler Narrativa modernista
Narrativa modernista Poema desejo de victor hugo
Poema desejo de victor hugo O combien de marins
O combien de marins Viktor pestov
Viktor pestov Victor halvani
Victor halvani Oeuvres victor hugo
Oeuvres victor hugo Victor hess balloon experiment
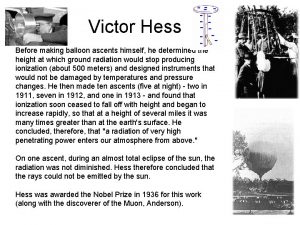
Victor hess balloon experiment Victor campbell nashville net worth
Victor campbell nashville net worth Dr victor de moya
Dr victor de moya Victor thompson nasa
Victor thompson nasa