Infectious Emergencies Medical Emergencies Infections Infectious Emergencies Systems

























- Slides: 142
Infectious Emergencies Medical Emergencies Infections
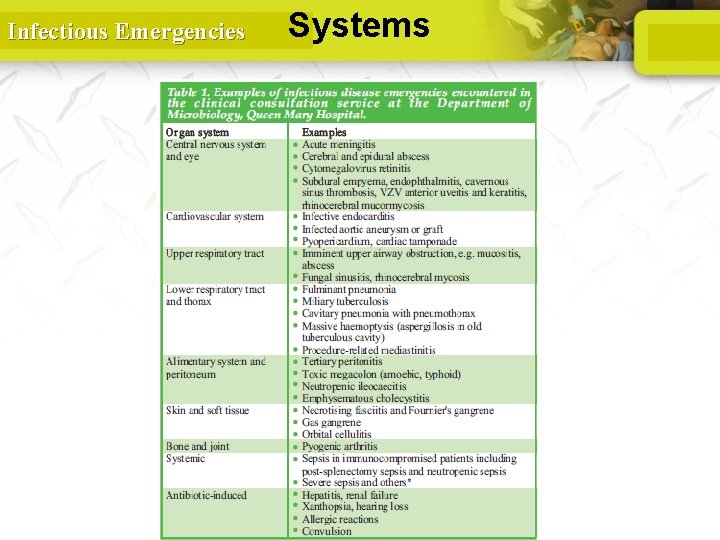
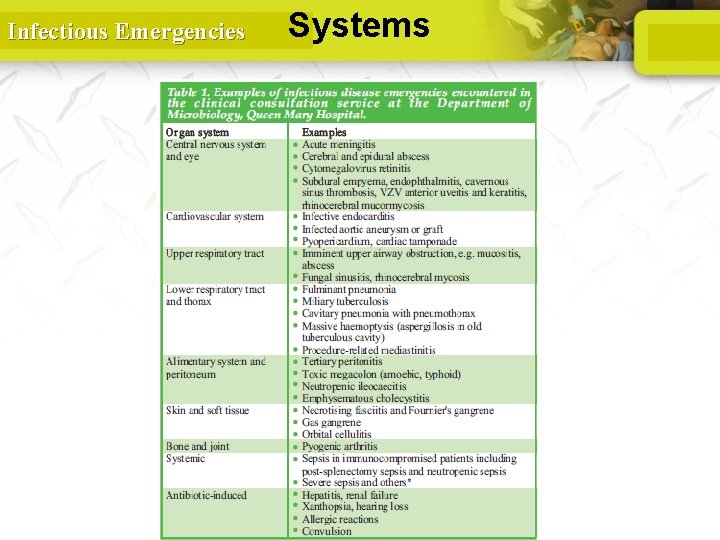
Infectious Emergencies Systems 2
Infectious Emergencies Medical Emergencies- Infections • • • Sepsis Bacterial Meningitis Infectious endocarditis Pneumonia Necrotizing Fascitiis Gastroenteritis -Food poisoning 3
Infectious Emergencies SEPSIS
Infectious Emergencies Sepsis • Sepsis is a clinical syndrome that complicates severe infection. • It is characterized by the cardinal signs of inflammation (vasodilation, leukocyte accumulation, increased microvascular permeability) occurring in tissues that are remote from the infection. 5

Infectious Emergencies SEPSIS • Severe sepsis accounts for 20% of all admissions to intensive care units (ICUs) • The leading cause of death in noncardiac ICUs Intensive Care Med (2010) 36: 222– 231
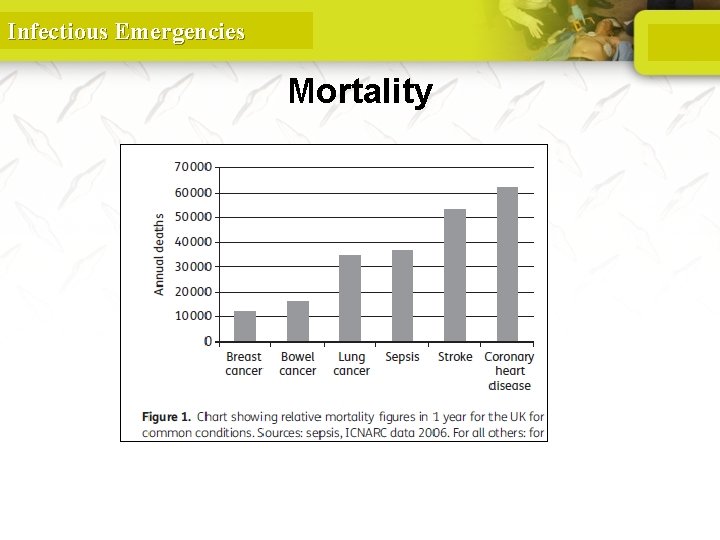
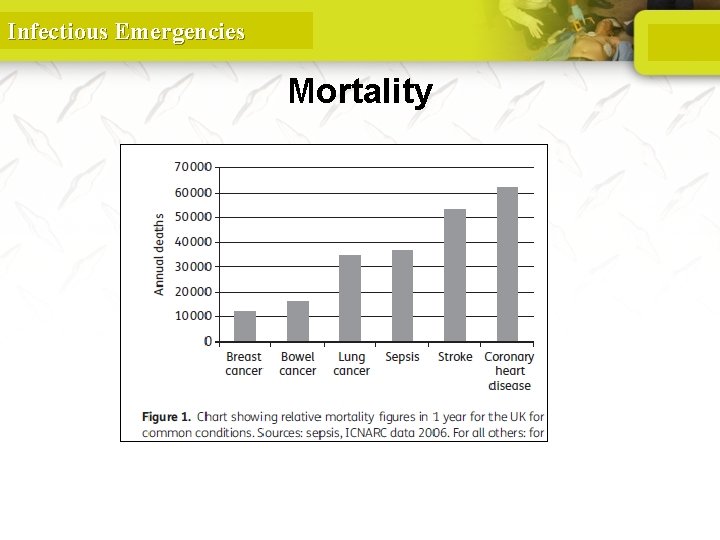
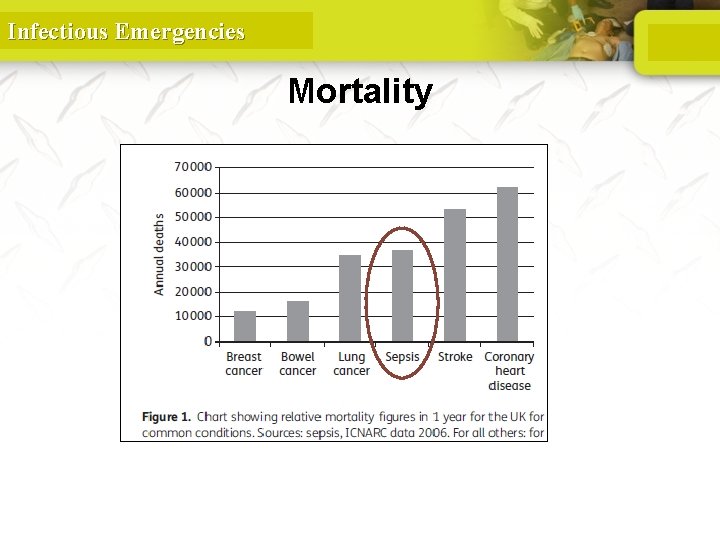
Infectious Emergencies Mortality
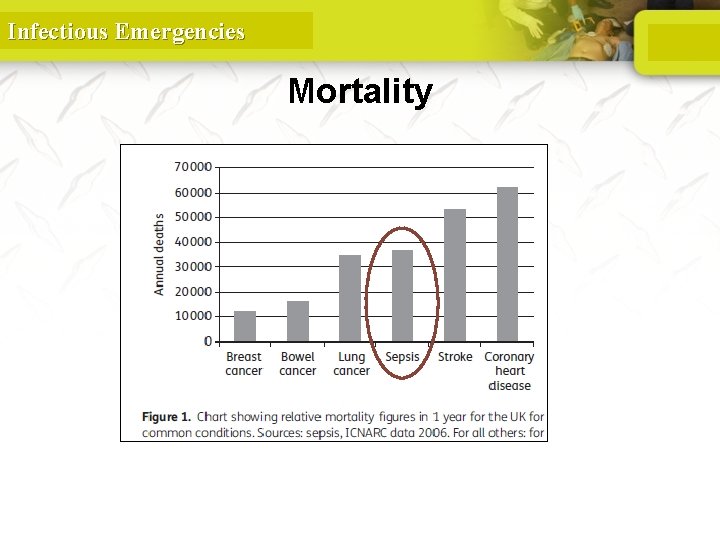
Infectious Emergencies Mortality
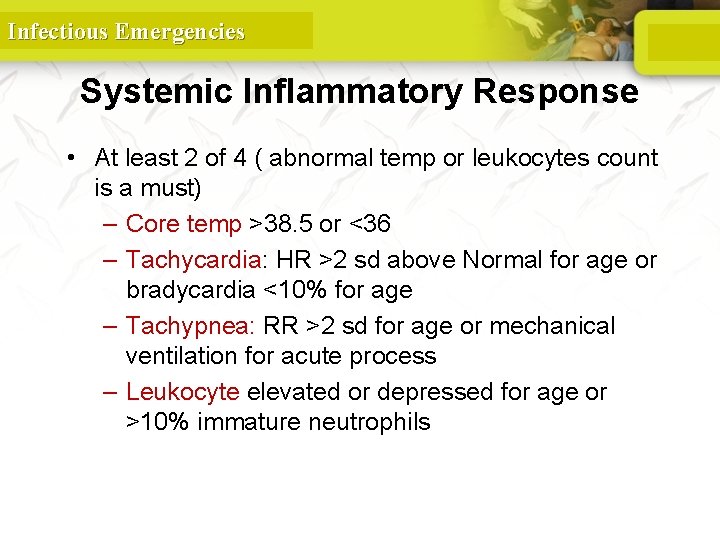
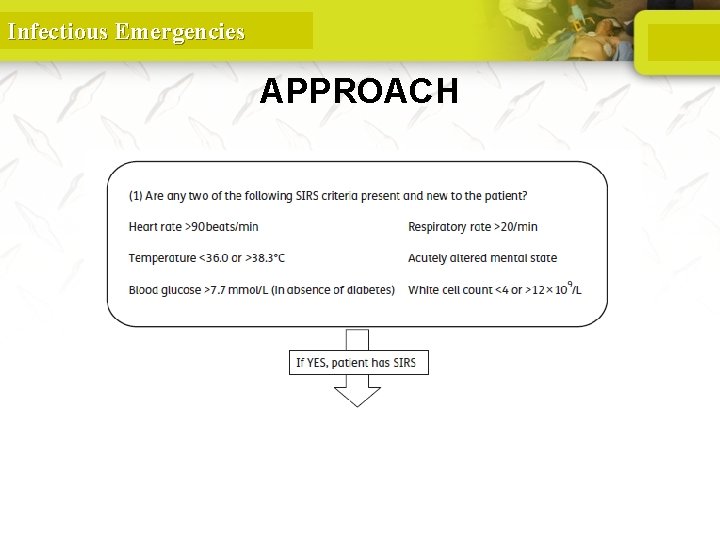
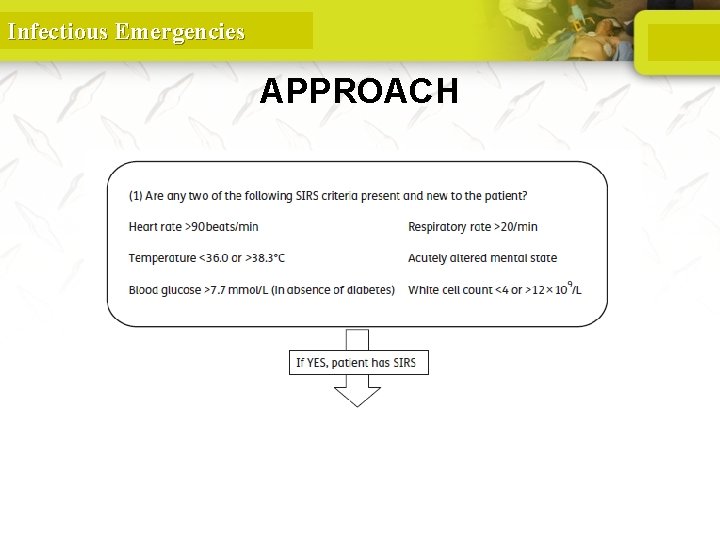
Infectious Emergencies Systemic Inflammatory Response • At least 2 of 4 ( abnormal temp or leukocytes count is a must) – Core temp >38. 5 or <36 – Tachycardia: HR >2 sd above Normal for age or bradycardia <10% for age – Tachypnea: RR >2 sd for age or mechanical ventilation for acute process – Leukocyte elevated or depressed for age or >10% immature neutrophils 9
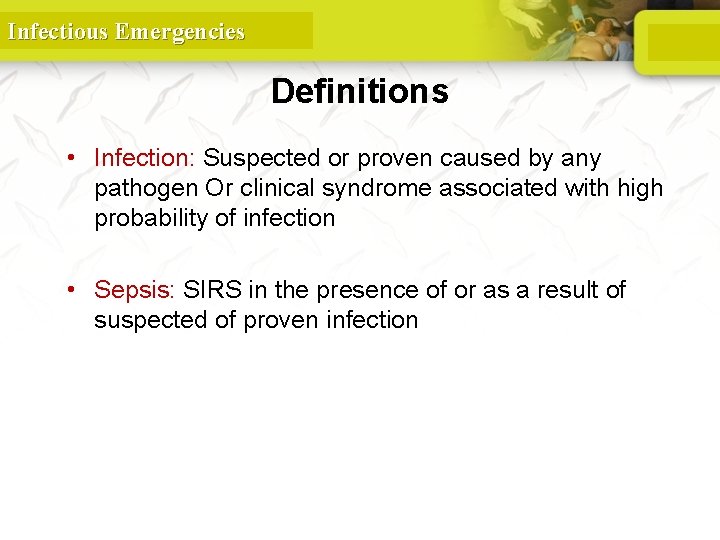
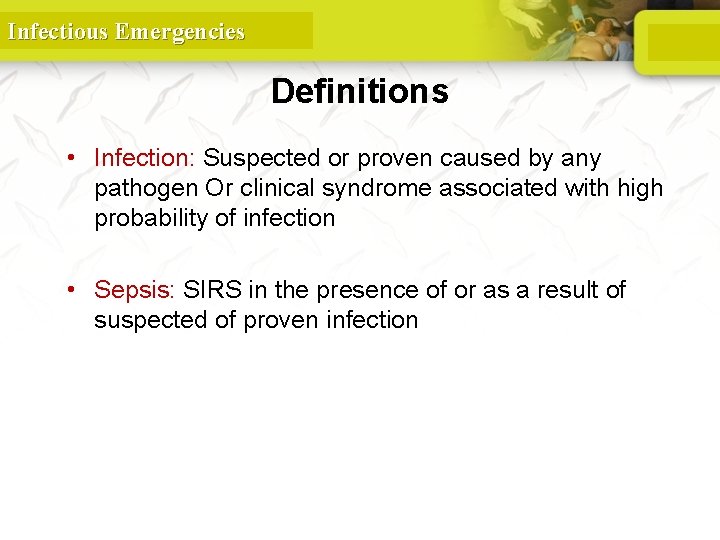
Infectious Emergencies Definitions • Infection: Suspected or proven caused by any pathogen Or clinical syndrome associated with high probability of infection • Sepsis: SIRS in the presence of or as a result of suspected of proven infection 10
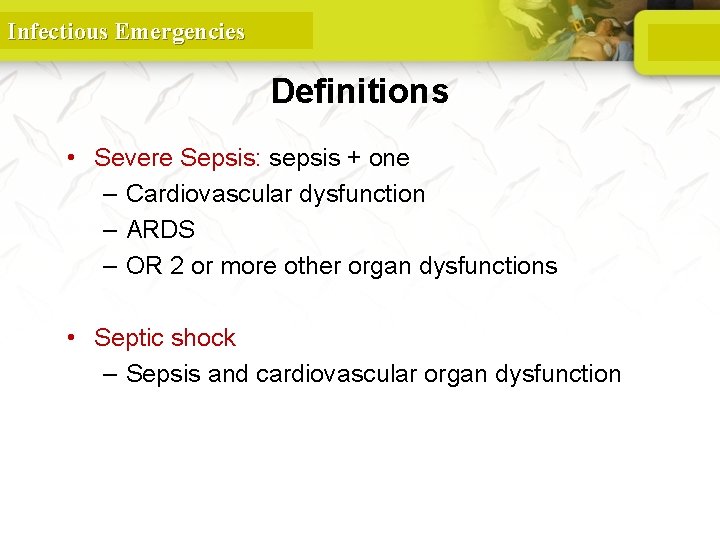
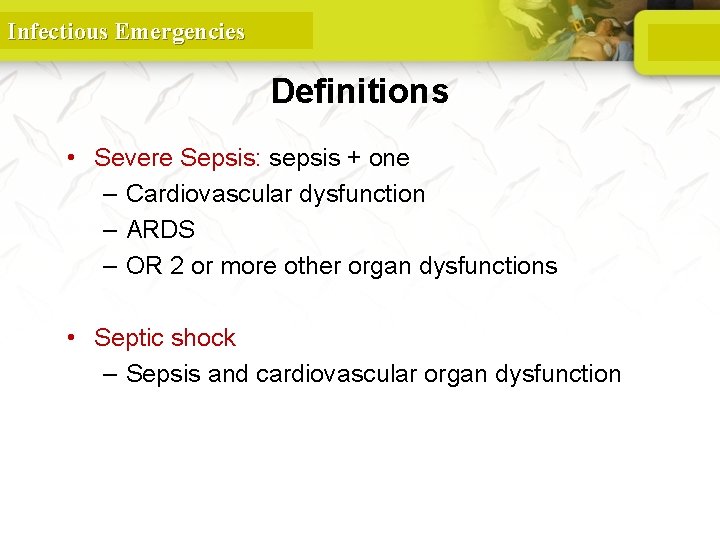
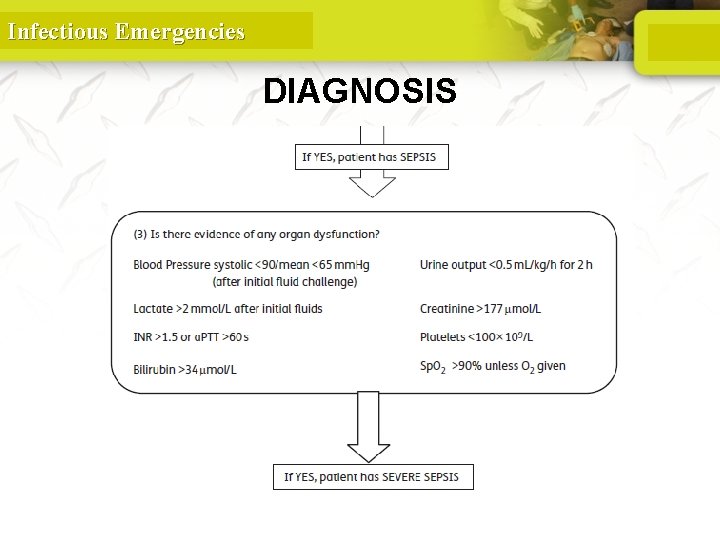
Infectious Emergencies Definitions • Severe Sepsis: sepsis + one – Cardiovascular dysfunction – ARDS – OR 2 or more other organ dysfunctions • Septic shock – Sepsis and cardiovascular organ dysfunction 11
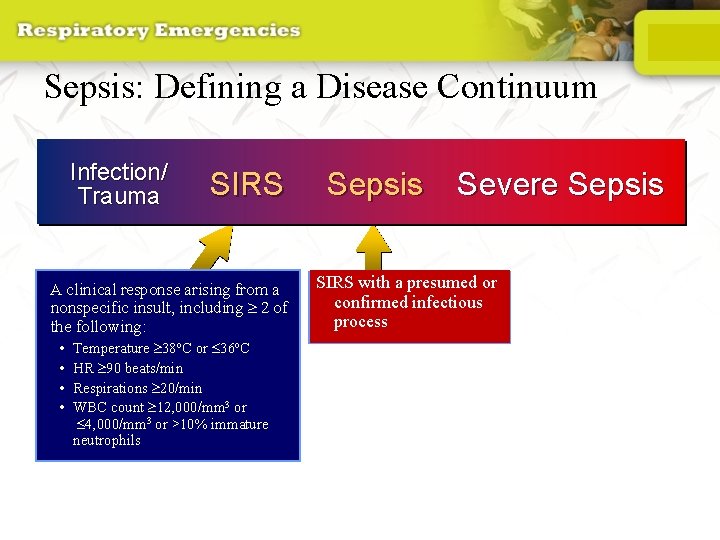
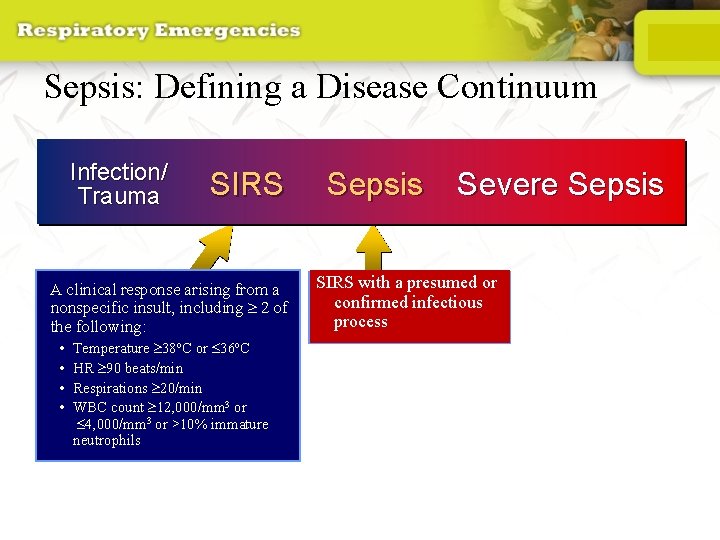
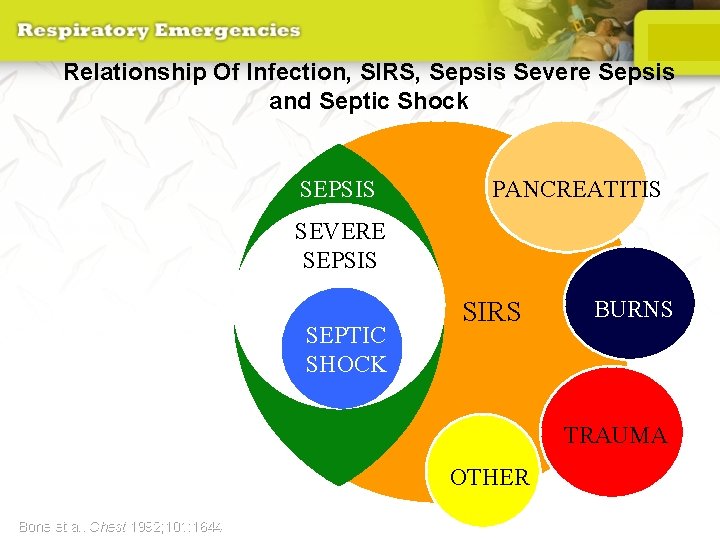
Sepsis: Defining a Disease Continuum Infection/ Trauma SIRS A clinical response arising from a nonspecific insult, including 2 of the following: • • Temperature 38 o. C or 36 o. C HR 90 beats/min Respirations 20/min WBC count 12, 000/mm 3 or 4, 000/mm 3 or >10% immature neutrophils Adapted from: Bone RC, et al. Chest 1992; 101: 1644 Opal SM, et al. Crit Care Med 2000; 28: S 81 Sepsis Severe Sepsis SIRS with a presumed or confirmed infectious process SIRS = Systemic Inflammatory Response Syndrome 12
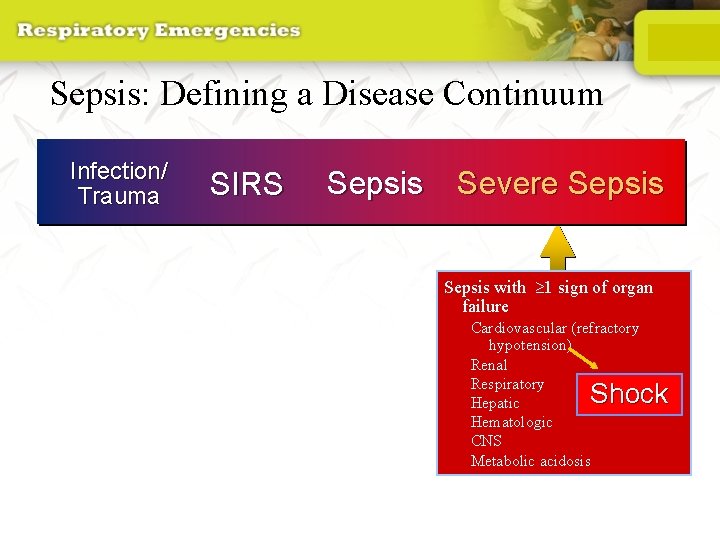
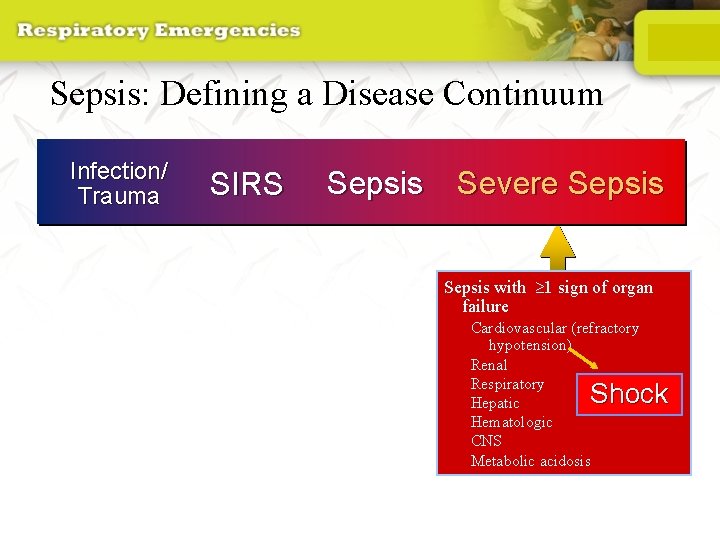
Sepsis: Defining a Disease Continuum Infection/ Trauma SIRS Sepsis Severe Sepsis with 1 sign of organ failure Cardiovascular (refractory hypotension) Renal Respiratory Hepatic Hematologic CNS Metabolic acidosis Shock Bone et al. Chest 1992; 101: 1644; Wheeler and Bernard. N Engl J Med 1999; 340: 207 13
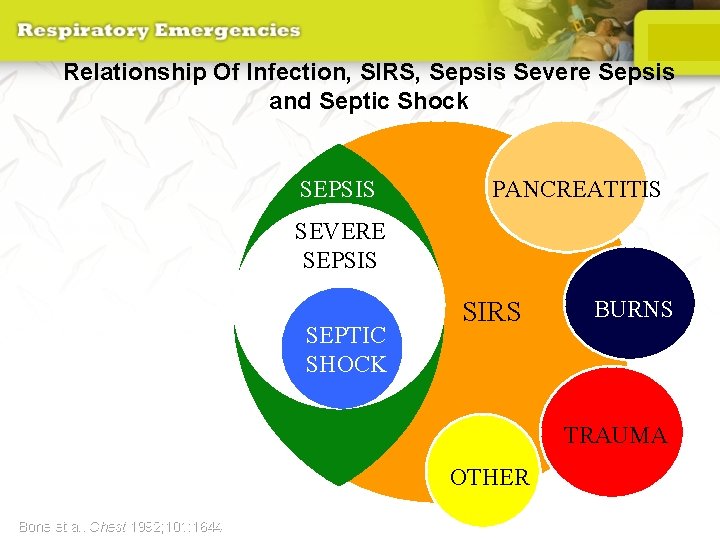
Relationship Of Infection, SIRS, Sepsis Severe Sepsis and Septic Shock SEPSIS PANCREATITIS SEVERE SEPSIS INFECTION SEPTIC SHOCK BURNS SIRS TRAUMA OTHER Bone et al. Chest 1992; 101: 1644 14
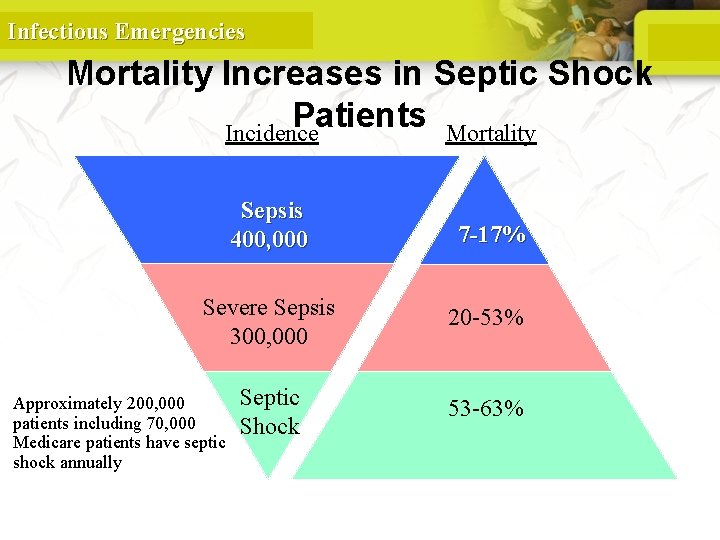
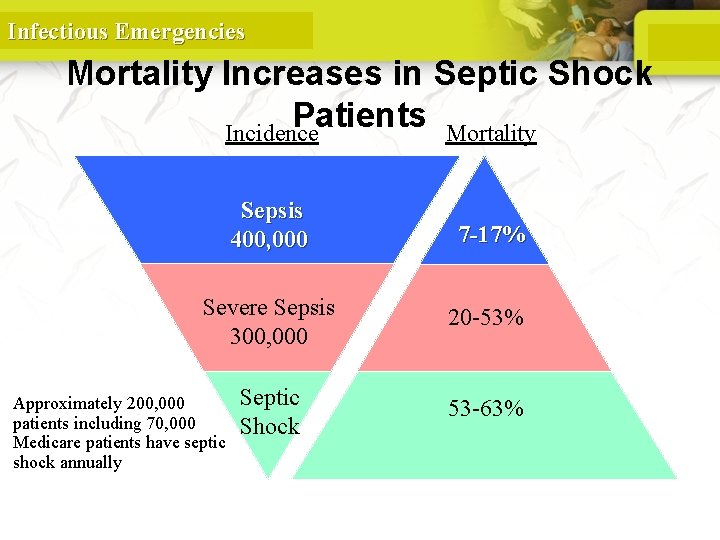
Infectious Emergencies Mortality Increases in Septic Shock Patients Incidence Mortality Sepsis 400, 000 7 -17% Severe Sepsis 300, 000 20 -53% Septic Shock 53 -63% Approximately 200, 000 patients including 70, 000 Medicare patients have septic shock annually Balk, R. A. Crit Care Clin 2000; 337: 52 15
Infectious Emergencies APPROACH

Infectious Emergencies DIAGNOSIS
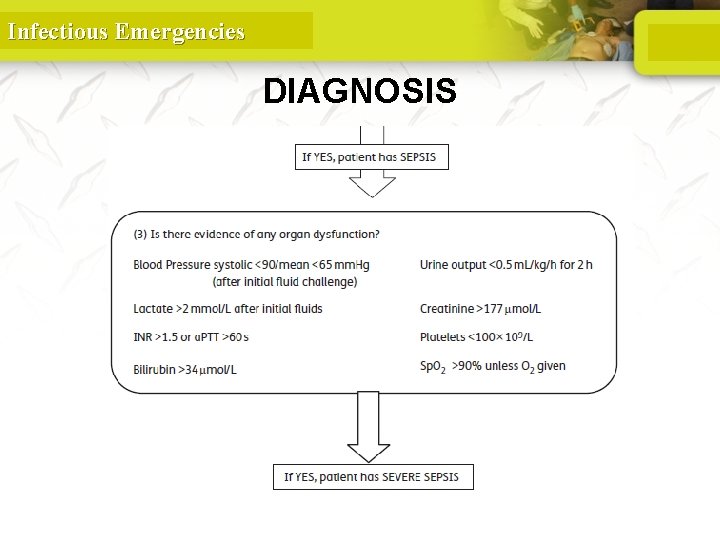
Infectious Emergencies DIAGNOSIS
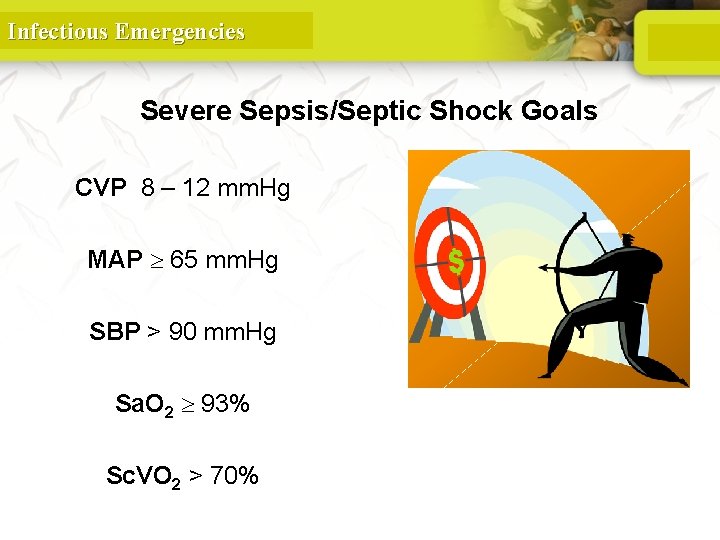
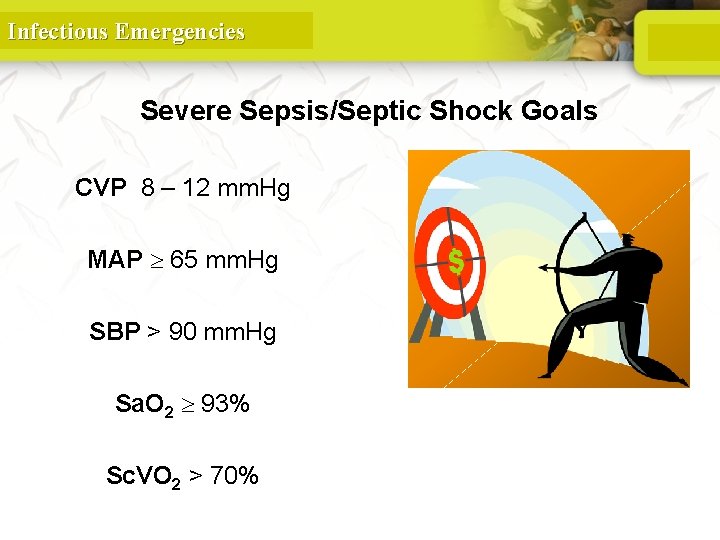
Infectious Emergencies Severe Sepsis/Septic Shock Goals CVP 8 – 12 mm. Hg MAP 65 mm. Hg SBP > 90 mm. Hg Sa. O 2 93% Sc. VO 2 > 70%
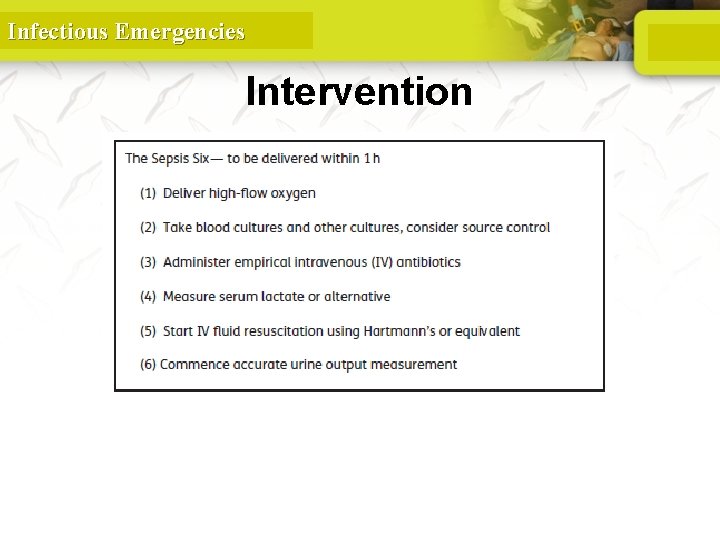
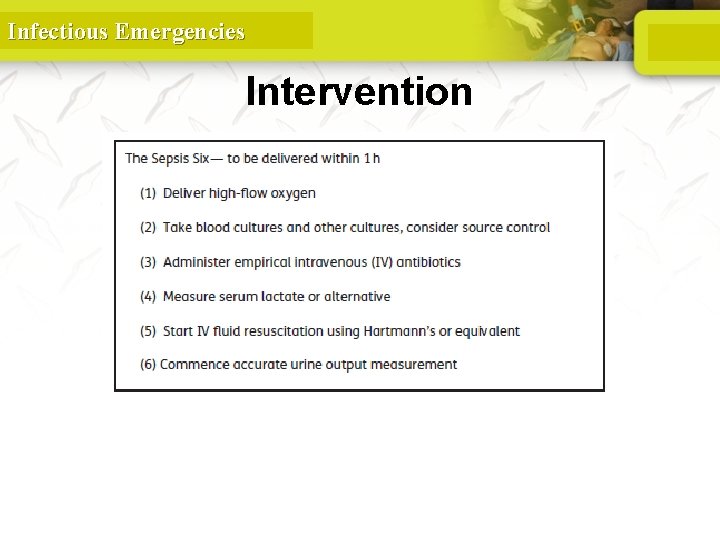
Infectious Emergencies Intervention
Infectious Emergencies Sepsis Resuscitation Emergency Department (ED) and Intensive Care Unit (ICU)

Infectious Emergencies Sepsis Resuscitation Bundle • Serum lactate measured • Blood cultures obtained prior to antibiotic administration • From the time of presentation, broad-spectrum antibiotics administered: – within 3 hours for ED admissions – within 1 hour for non-ED ICU admissions • In the event of hypotension and/or lactate > 4 mmol/L (36 mg/dl): – Deliver an initial minimum of 20 -30 ml/kg of crystalloid (or colloid equivalent) – Apply vasopressors for hypotension not responding to initial fluid resuscitation to maintain MAP > 65 mm. Hg • In the event of persistent hypotension despite fluid resuscitation (septic shock) and/or lactate > 4 mmol/L (36 mg/dl): – Achieve central venous pressure (CVP) of > 8 mm. Hg – Achieve central venous oxygen saturation (Scv. O 2) of > 70% Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
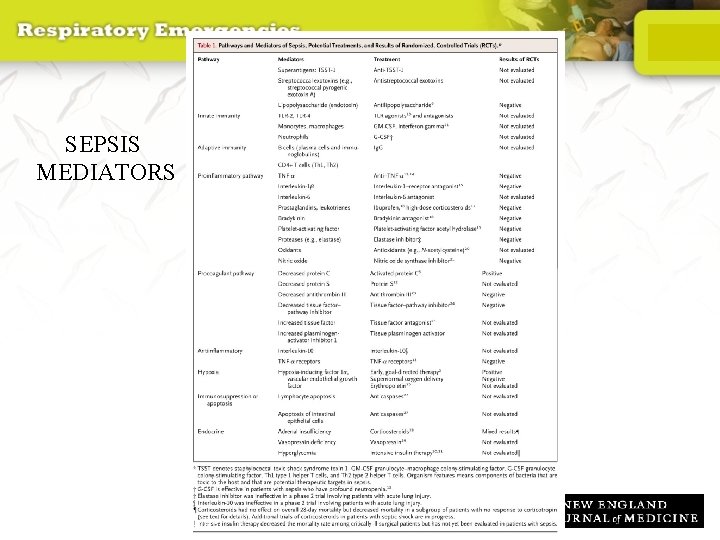
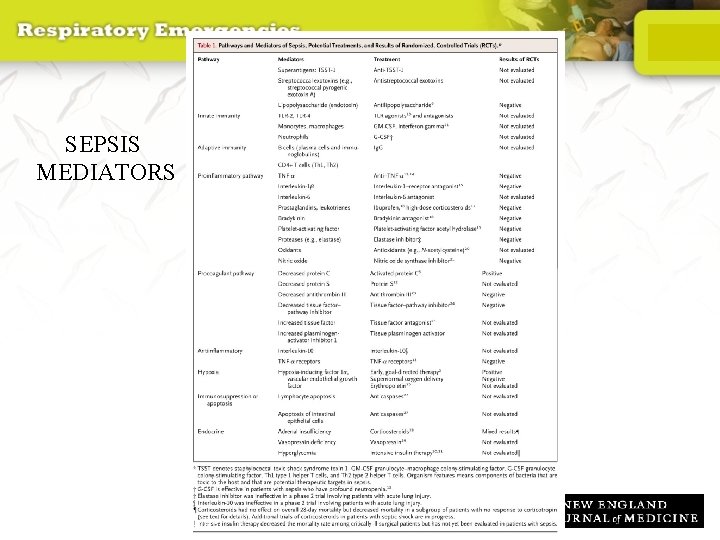
SEPSIS MEDIATORS 23 Russell J. N Engl J Med 2006; 355: 1699 -1713
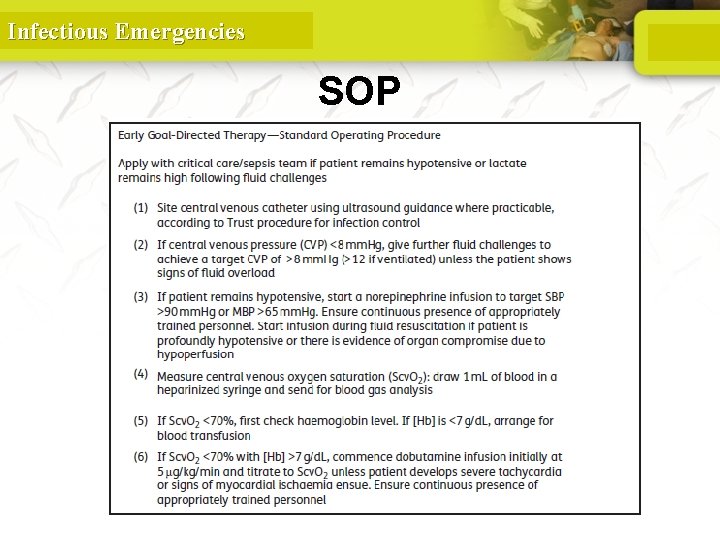
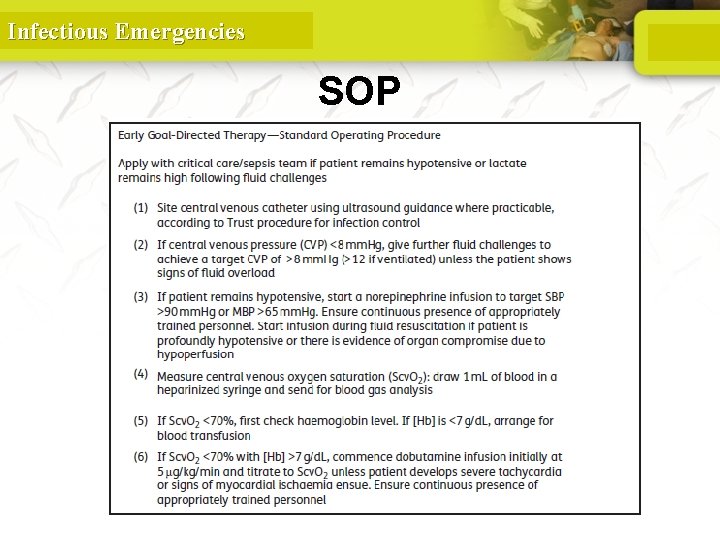
Infectious Emergencies SOP
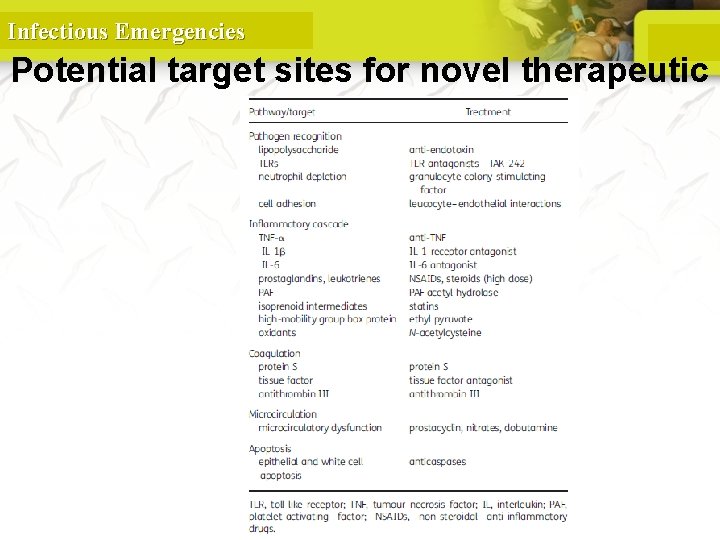
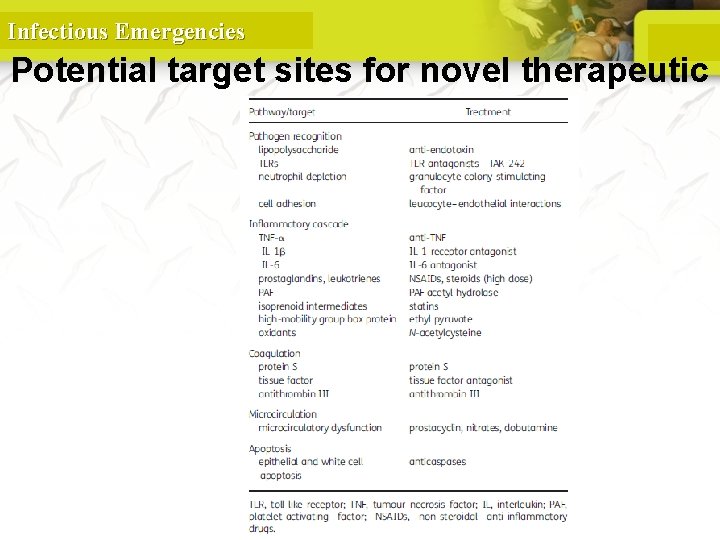
Infectious Emergencies Potential target sites for novel therapeutic agents

Infectious Emergencies MENINGITIS
Infectious Emergencies Meningitis is a clinical syndrome characterized by inflammation of the meninges
Infectious Emergencies Classification • Depending on the duration of symptoms, meningitis may be classified as acute or chronic. • Acute meningitis denotes the evolution of symptoms within hours to several days, while chronic meningitis has an onset and duration of weeks to months. • The duration of symptoms of chronic meningitis is characteristically at least 4 weeks.
Infectious Emergencies Classification • Meningitis can also be classified according to its etiology.
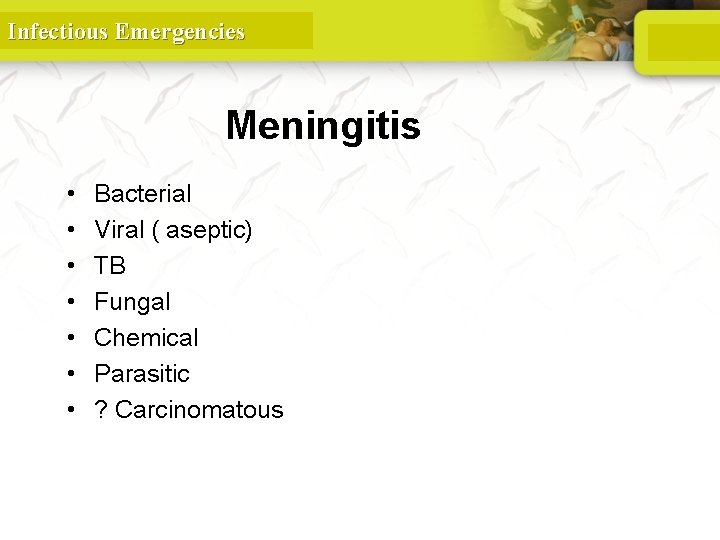
Infectious Emergencies Meningitis • • Bacterial Viral ( aseptic) TB Fungal Chemical Parasitic ? Carcinomatous
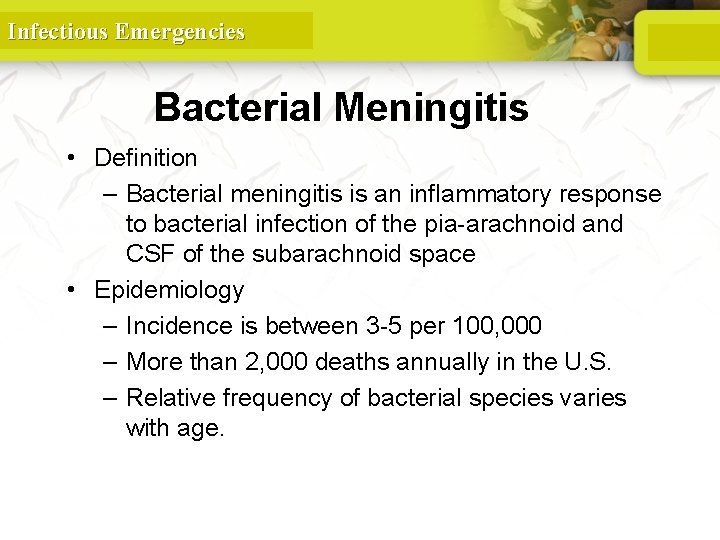
Infectious Emergencies Bacterial Meningitis • Definition – Bacterial meningitis is an inflammatory response to bacterial infection of the pia-arachnoid and CSF of the subarachnoid space • Epidemiology – Incidence is between 3 -5 per 100, 000 – More than 2, 000 deaths annually in the U. S. – Relative frequency of bacterial species varies with age.

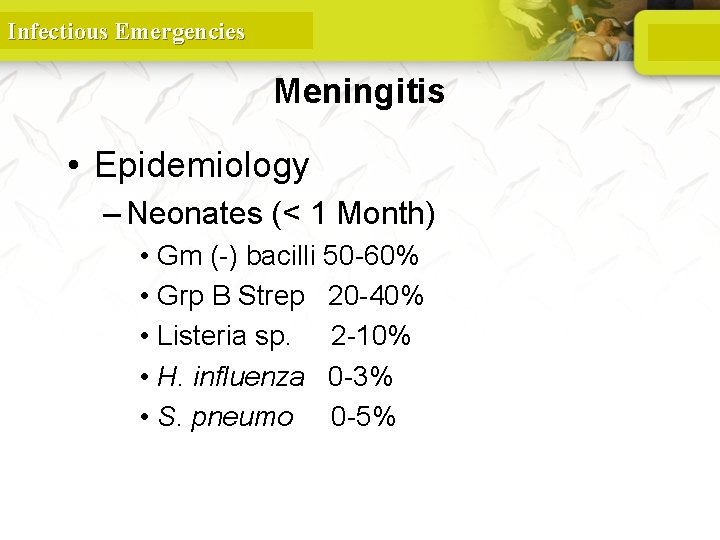
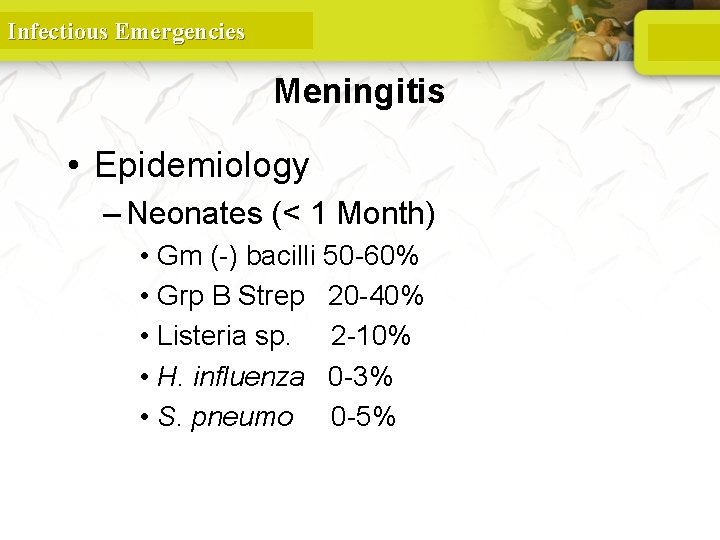
Infectious Emergencies Meningitis • Epidemiology – Neonates (< 1 Month) • Gm (-) bacilli 50 -60% • Grp B Strep 20 -40% • Listeria sp. 2 -10% • H. influenza 0 -3% • S. pneumo 0 -5%
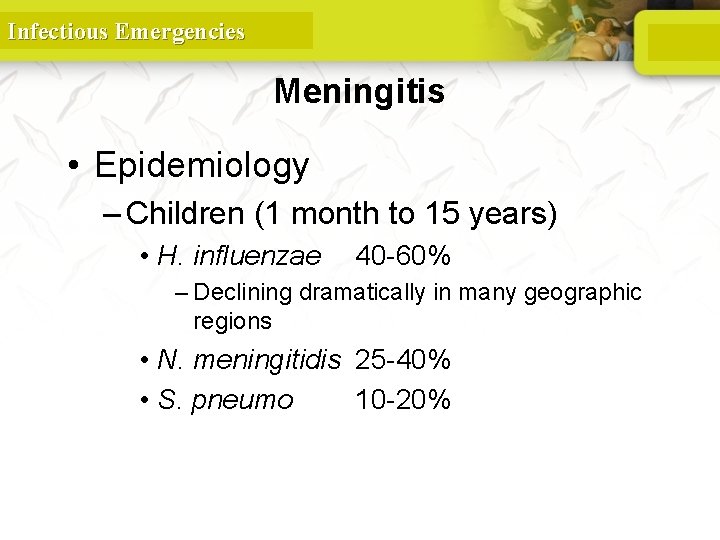
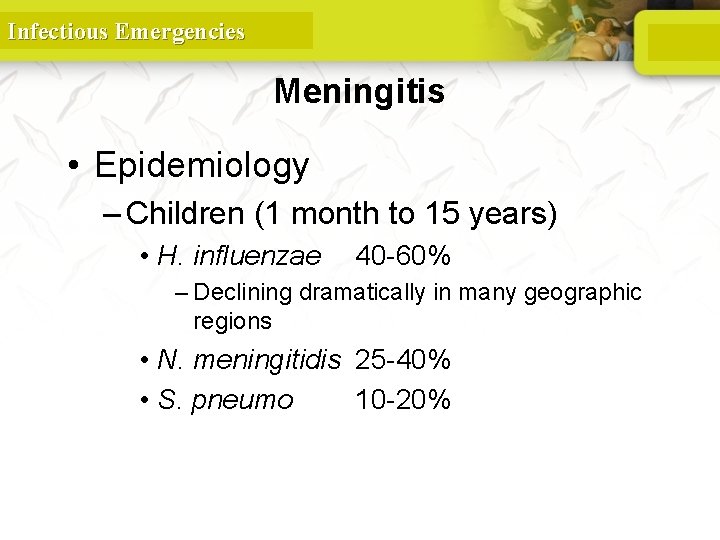
Infectious Emergencies Meningitis • Epidemiology – Children (1 month to 15 years) • H. influenzae 40 -60% – Declining dramatically in many geographic regions • N. meningitidis 25 -40% • S. pneumo 10 -20%
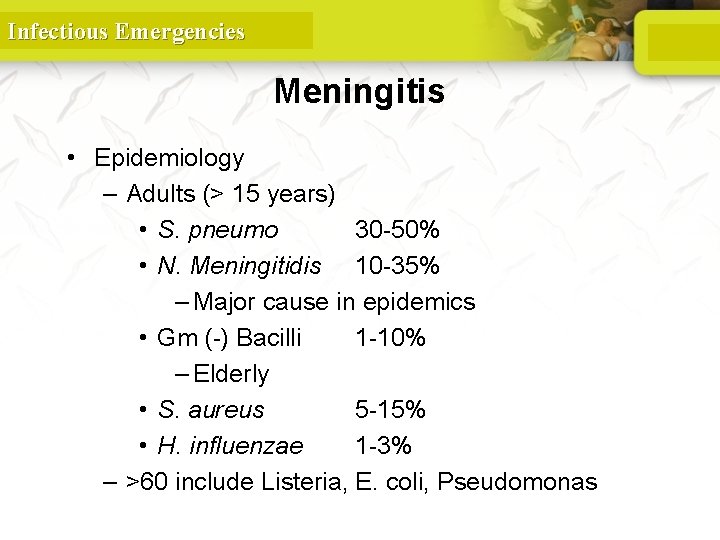
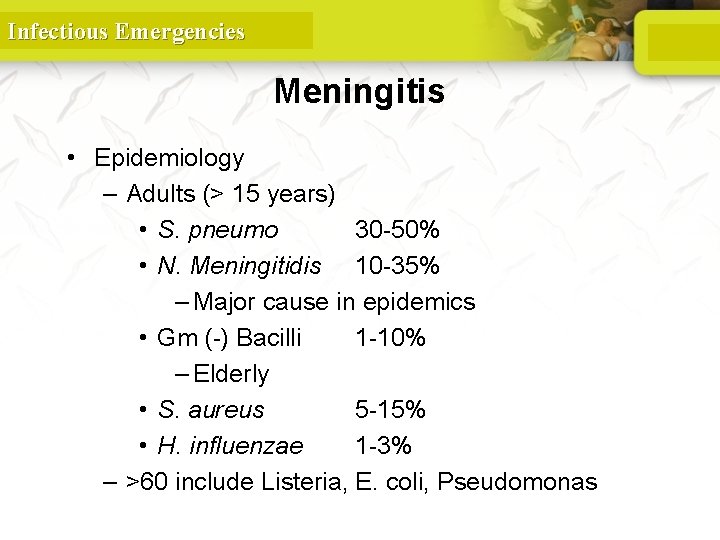
Infectious Emergencies Meningitis • Epidemiology – Adults (> 15 years) • S. pneumo 30 -50% • N. Meningitidis 10 -35% – Major cause in epidemics • Gm (-) Bacilli 1 -10% – Elderly • S. aureus 5 -15% • H. influenzae 1 -3% – >60 include Listeria, E. coli, Pseudomonas
Infectious Emergencies Meningitis • Pathogenesis – Majority of cases are hematogenous in origin – Organisms have virulence factors that allow bypassing of normal defenses • Proteases • Polysaccharidases
Infectious Emergencies Meningitis • Pathology and Pathogenesis – Sequential steps allow the pathogen into the CSF • Nasopharyngeal colonization • Nasopharyngeal epithelial cell invasion • Bloodstream invasion • Bacteremia with intravascular survival • Crossing of the BBB and entry into the CSF • Survival and replication in the subarachnoid space

Nasopharynx -> blood -> subarachnoid space

Infectious Emergencies Pathophysiology of Bacterial Meningitis • Bacterial colonization within the subarachnoid space • Initiation of inflammatory response which leads to: – Endothelial damage – Disruption of the blood-brain barrier • On a larger scale, this results in: – Cerebral edema • Cytotoxic • Vasogenic • Interstitial – Increased ICP
Infectious Emergencies Meningitis • Pathology and Pathogenesis – Key advances in the pathophysiology of meningitis include the pivotal role of cytokines (eg, tumor necrosis factor-alpha [TNF-alpha], interleukin [IL]– 1), chemokines (IL-8), and other proinflammatory molecules in the pathogenesis of pleocytosis and neuronal damage during bacterial meningitis. – Increased CSF concentrations of TNF-alpha, IL-1, IL-6, and IL-8 are characteristic findings in patients with bacterial meningitis

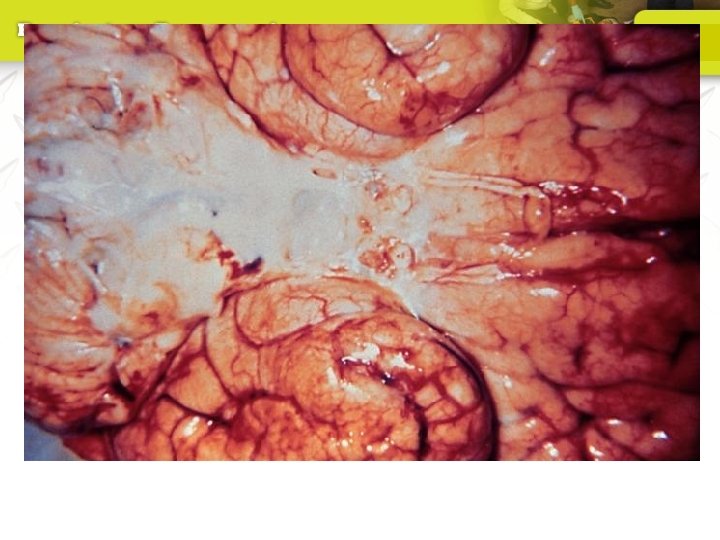
Infectious Emergencies Meningitis • Pathology – Hallmark • Exudate in the subarachnoid space • Accumulation of exudate in the dependent areas of the brain • Large numbers of PMN’s • Within 2 -3 days inflammation in the walls of the small and medium-sized blood vessels • Blockage of normal CSF pathways and blockage of the normal absorption may lead to obstructive hydrocephalus
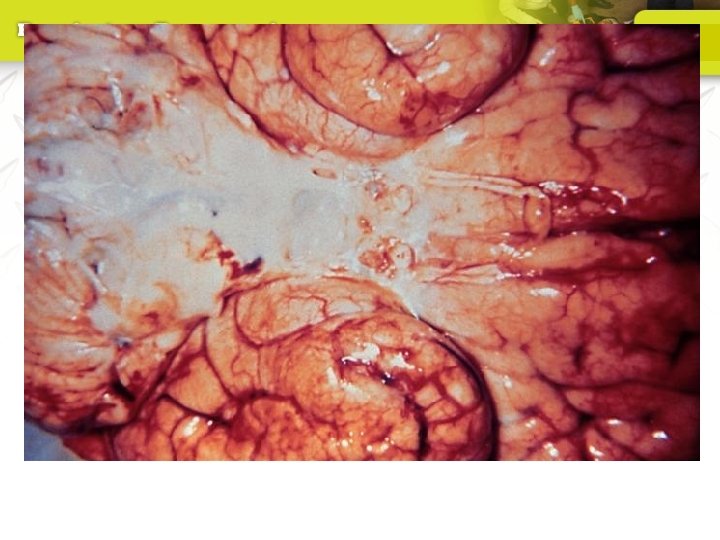
Infectious Emergencies Meningitis • Overall, the net result is vascular endothelial injury and increased BBB permeability leading to the entry of many blood components into the subarachnoid space. • This contributes to vasogenic edema and elevated CSF protein levels. • In response to the cytokines and chemotactic molecules, neutrophils migrate from the bloodstream and penetrate the damaged BBB, producing the profound neutrophilic pleocytosis characteristic of bacterial meningitis.
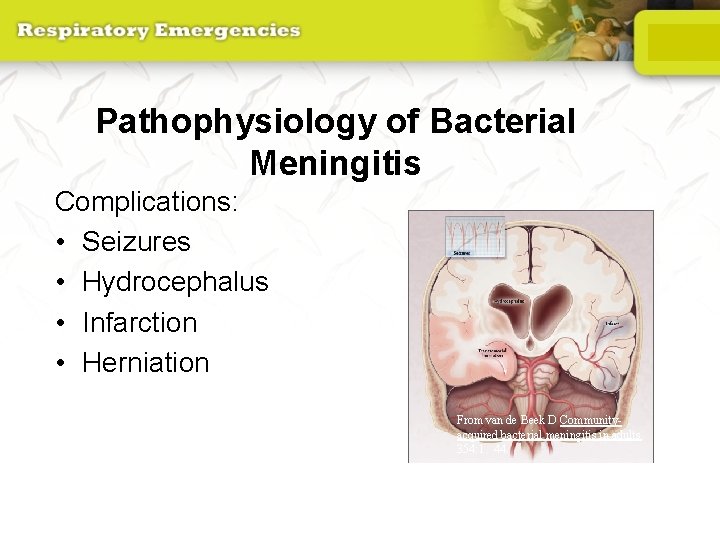
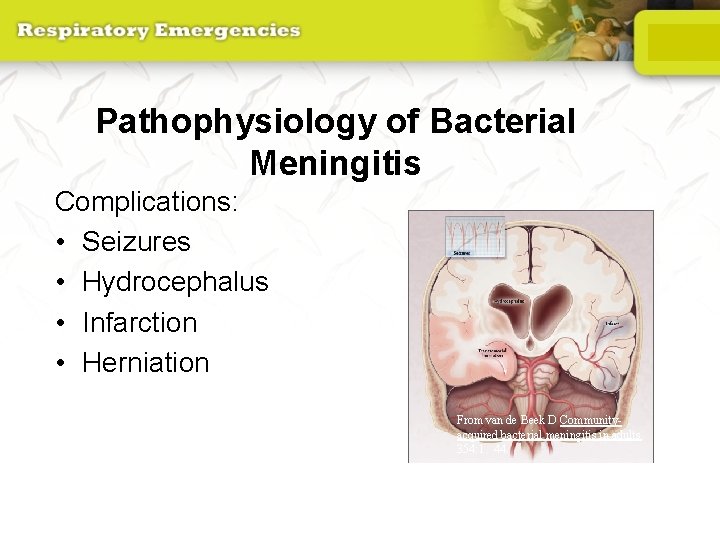
Pathophysiology of Bacterial Meningitis Complications: • Seizures • Hydrocephalus • Infarction • Herniation From van de Beek D Communityacquired bacterial meningitis in adults. 354: 1. 44.
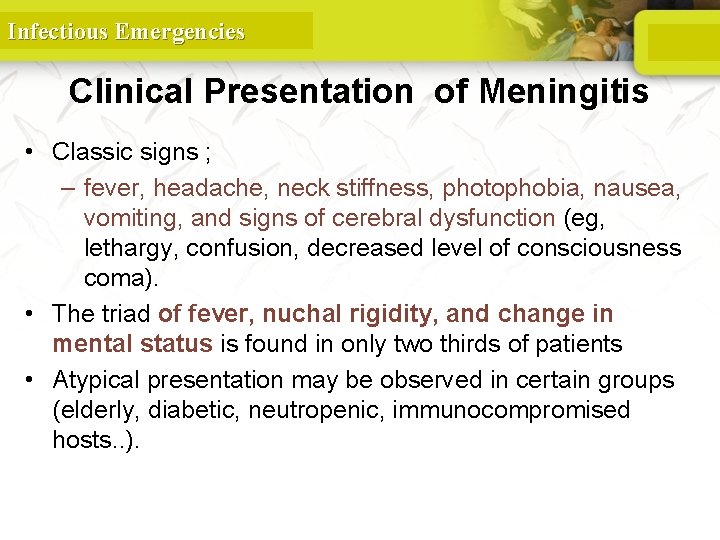
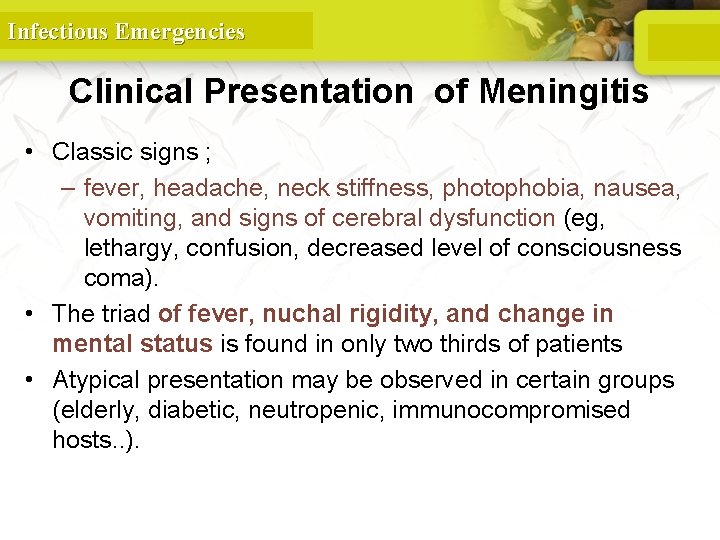
Infectious Emergencies Clinical Presentation of Meningitis • Classic signs ; – fever, headache, neck stiffness, photophobia, nausea, vomiting, and signs of cerebral dysfunction (eg, lethargy, confusion, decreased level of consciousness coma). • The triad of fever, nuchal rigidity, and change in mental status is found in only two thirds of patients • Atypical presentation may be observed in certain groups (elderly, diabetic, neutropenic, immunocompromised hosts. . ).
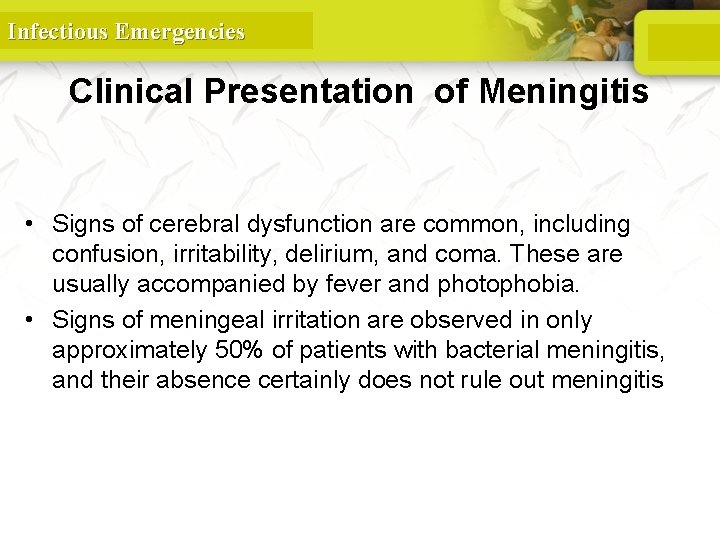
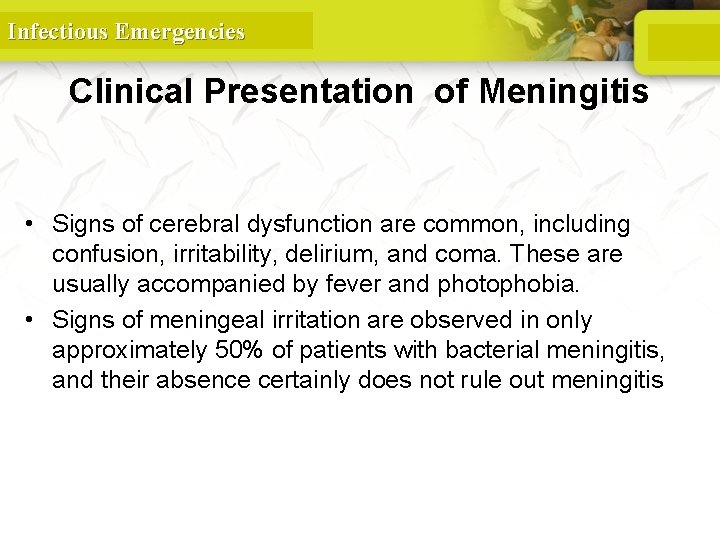
Infectious Emergencies Clinical Presentation of Meningitis • Signs of cerebral dysfunction are common, including confusion, irritability, delirium, and coma. These are usually accompanied by fever and photophobia. • Signs of meningeal irritation are observed in only approximately 50% of patients with bacterial meningitis, and their absence certainly does not rule out meningitis
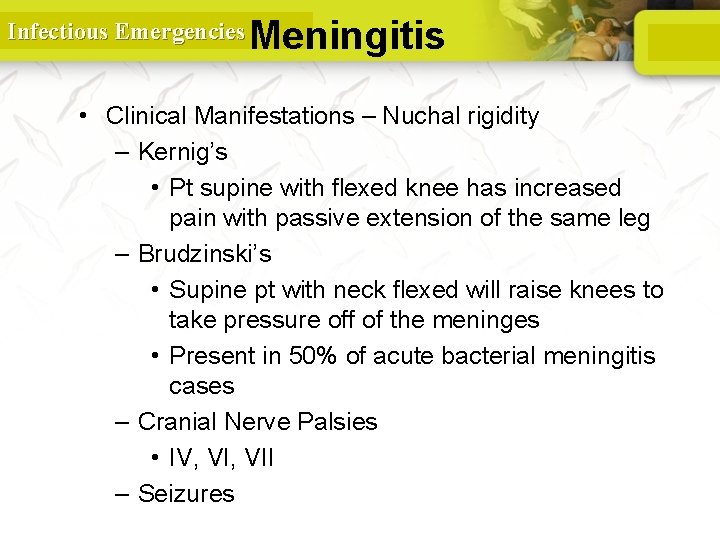
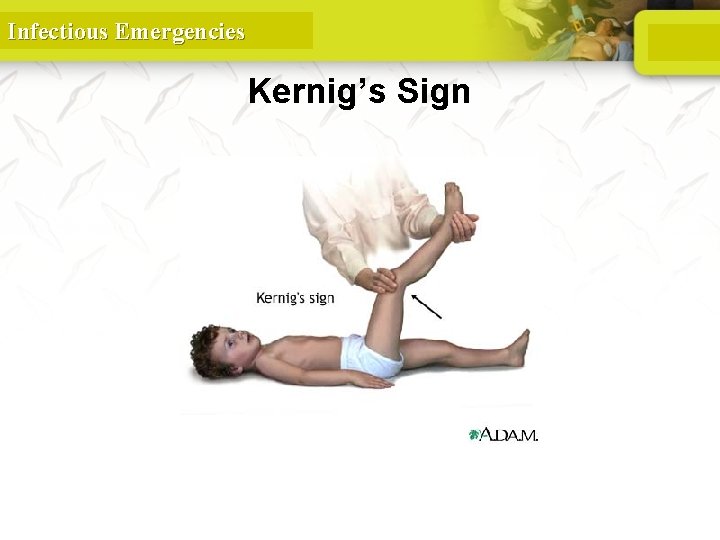
Infectious Emergencies Meningitis • Clinical Manifestations – Nuchal rigidity – Kernig’s • Pt supine with flexed knee has increased pain with passive extension of the same leg – Brudzinski’s • Supine pt with neck flexed will raise knees to take pressure off of the meninges • Present in 50% of acute bacterial meningitis cases – Cranial Nerve Palsies • IV, VII – Seizures

Infectious Emergencies Brudzinski’s Sign
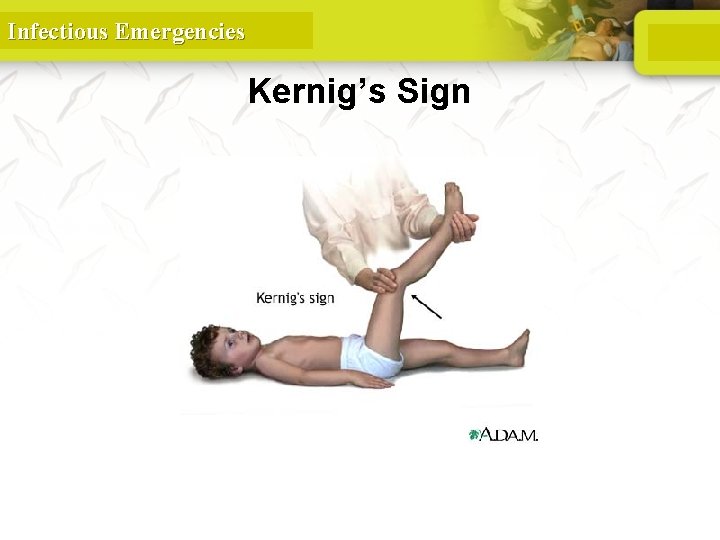
Infectious Emergencies Kernig’s Sign
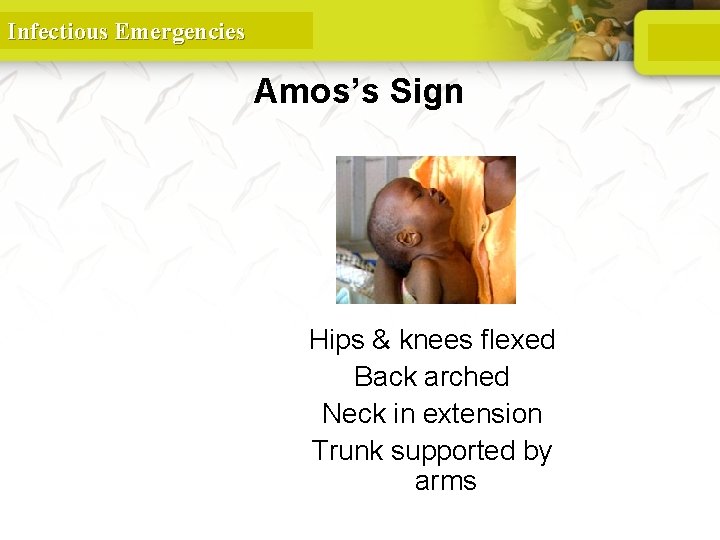
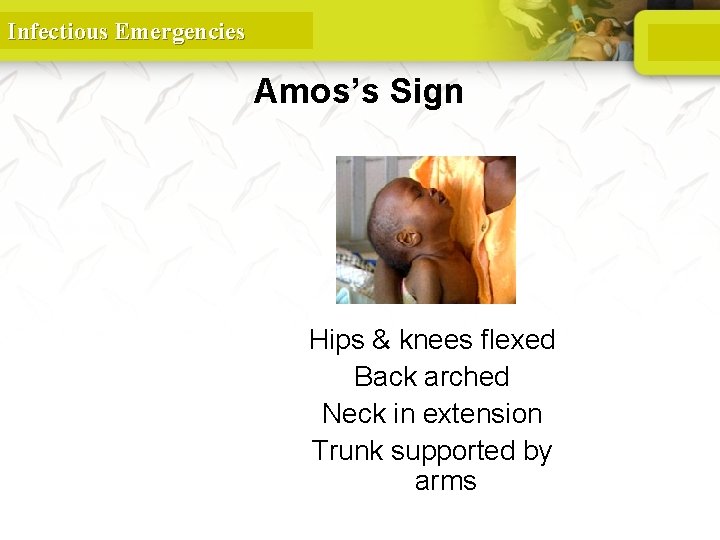
Infectious Emergencies Amos’s Sign Hips & knees flexed Back arched Neck in extension Trunk supported by arms
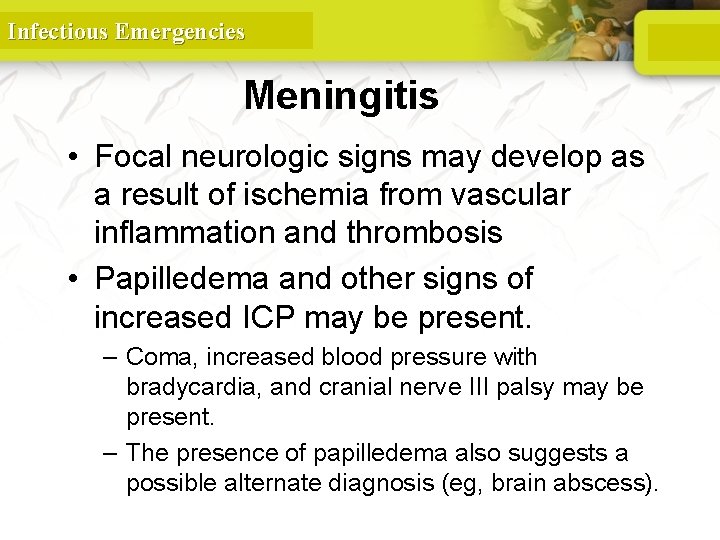
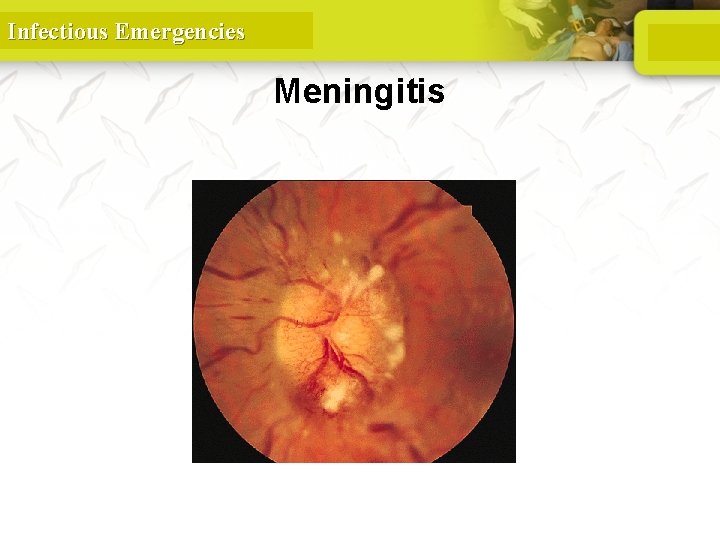
Infectious Emergencies Meningitis • Focal neurologic signs may develop as a result of ischemia from vascular inflammation and thrombosis • Papilledema and other signs of increased ICP may be present. – Coma, increased blood pressure with bradycardia, and cranial nerve III palsy may be present. – The presence of papilledema also suggests a possible alternate diagnosis (eg, brain abscess).
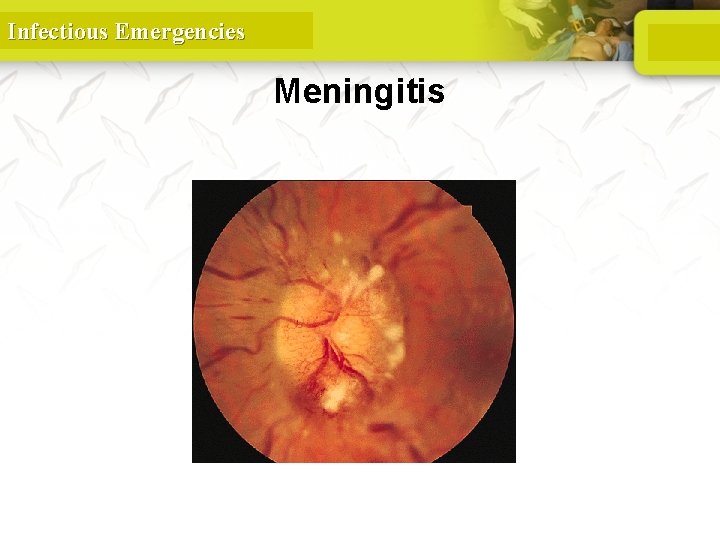
Infectious Emergencies Meningitis Papilledema
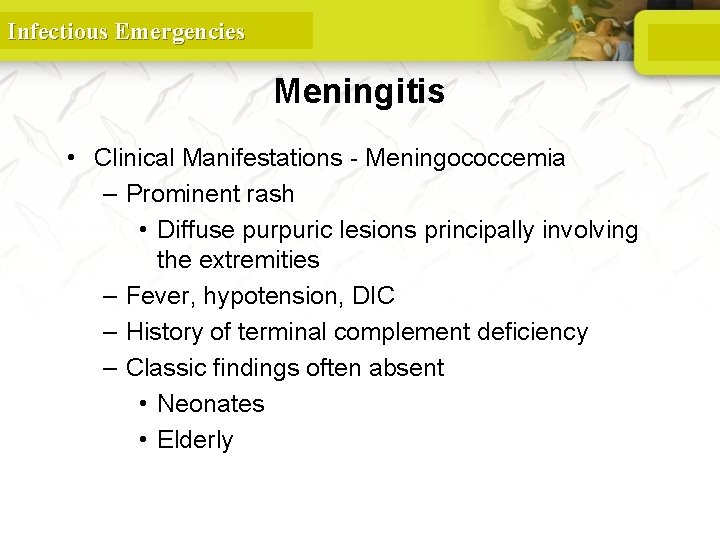
Infectious Emergencies Meningitis • Clinical Manifestations - Meningococcemia – Prominent rash • Diffuse purpuric lesions principally involving the extremities – Fever, hypotension, DIC – History of terminal complement deficiency – Classic findings often absent • Neonates • Elderly

Infectious Emergencies Meningitis
Infectious Emergencies Diagnosis of Meningitis • Diagnosis – Assess for increased ICP • Papilledema • Focal neurologic findings – Defer LP until CT scan or MRI obtained if any of above present – If suspect meningitis and awaiting neuroimaging • Obtain BC’s and start empiric Abx
Infectious Emergencies Diagnosis of Meningitis • • • Obtain CT scan before lumbar puncture in patients with: Immunucompromised state History of CNS disease New onset seizures Papilledema Altered level of consciousness Focal neurologic signs
Infectious Emergencies Diagnosis of Meningitis • Obtain blood cultures and give empiric antibiotics if LP is delayed
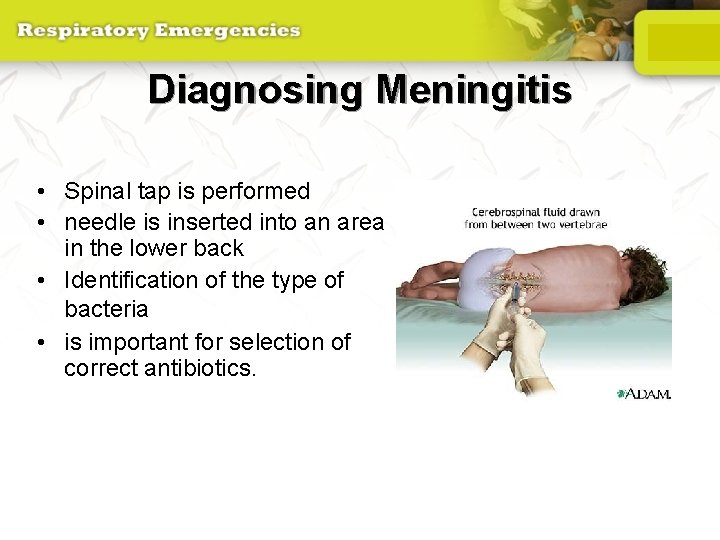
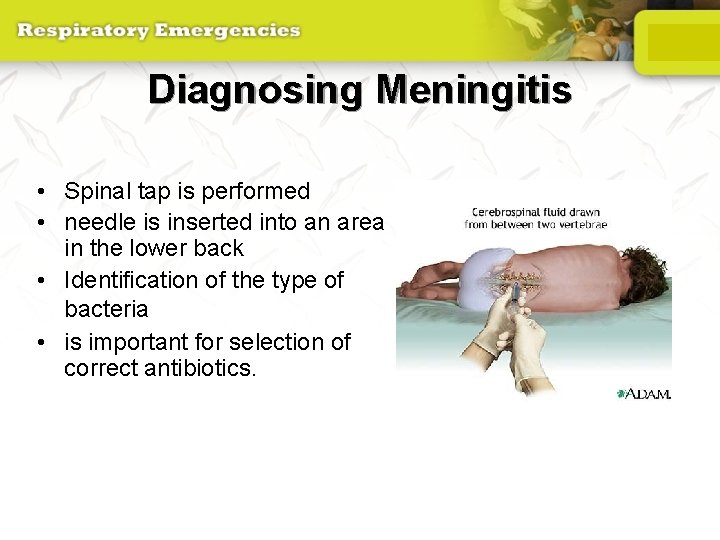
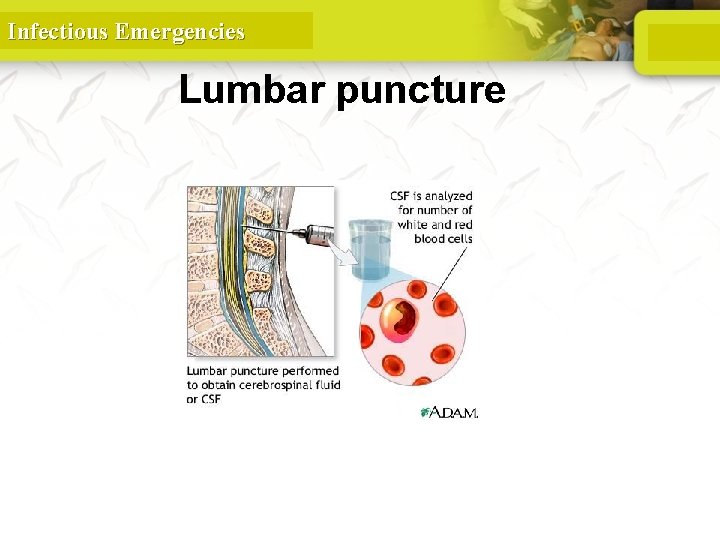
Diagnosing Meningitis • Spinal tap is performed • needle is inserted into an area in the lower back • Identification of the type of bacteria • is important for selection of correct antibiotics.
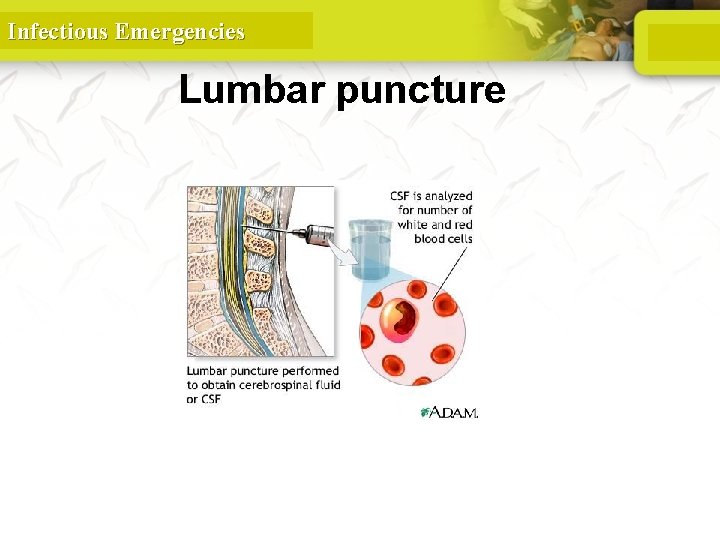
Infectious Emergencies Lumbar puncture
Infectious Emergencies
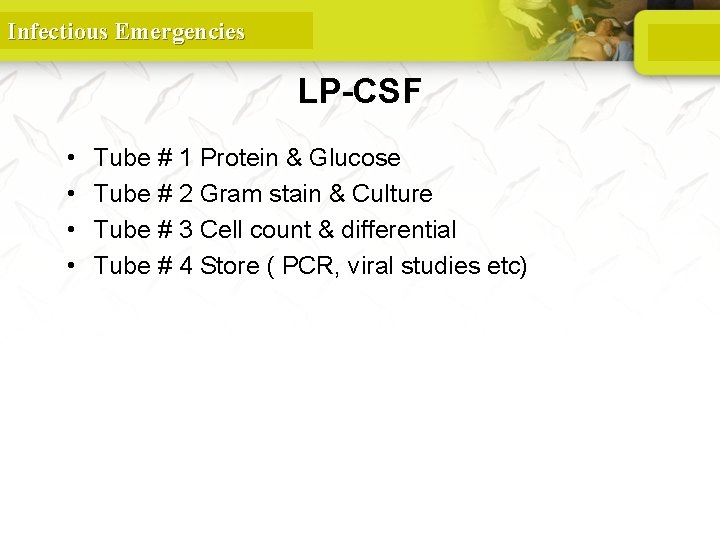
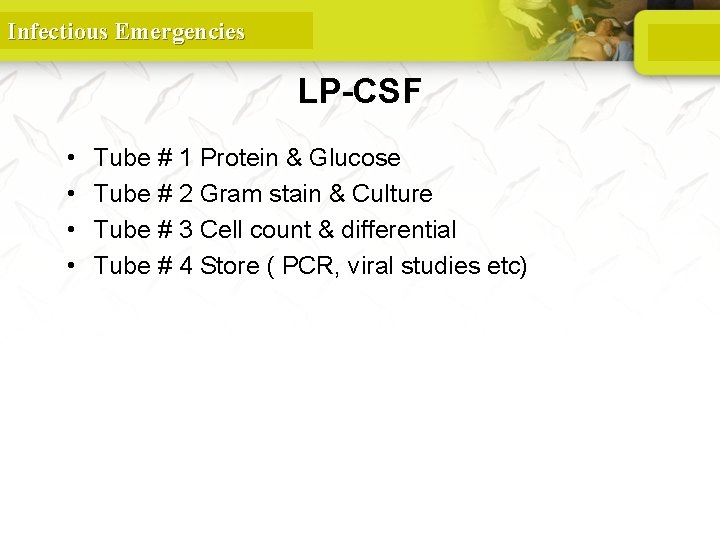
Infectious Emergencies LP-CSF • • Tube # 1 Protein & Glucose Tube # 2 Gram stain & Culture Tube # 3 Cell count & differential Tube # 4 Store ( PCR, viral studies etc)
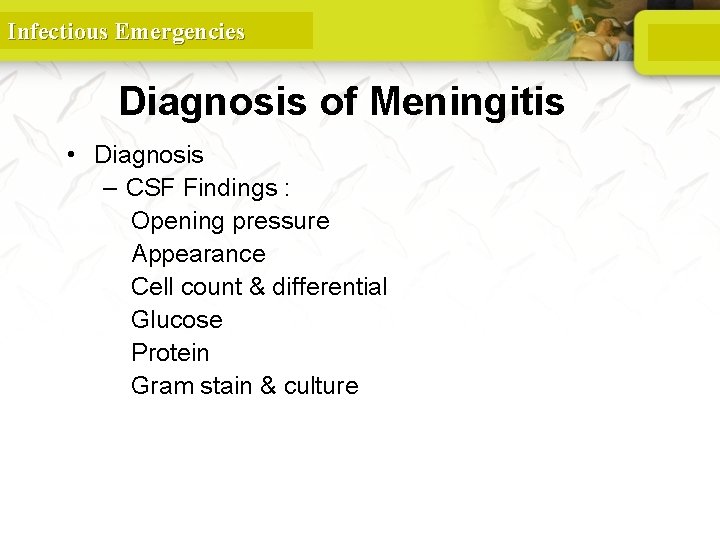
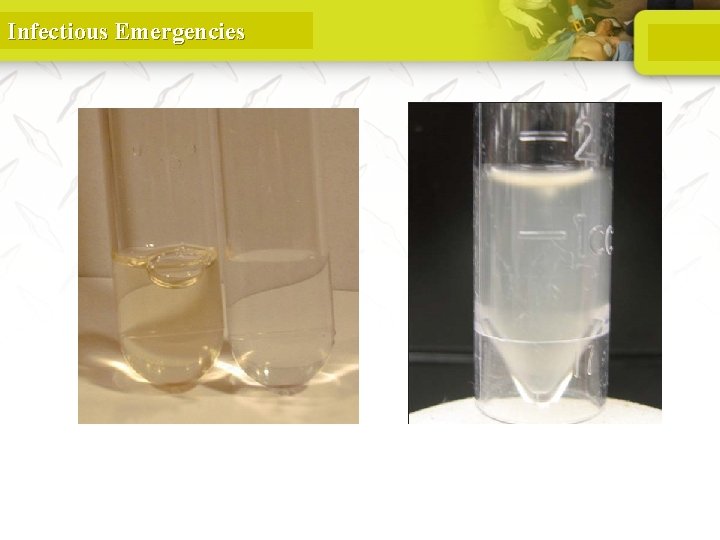
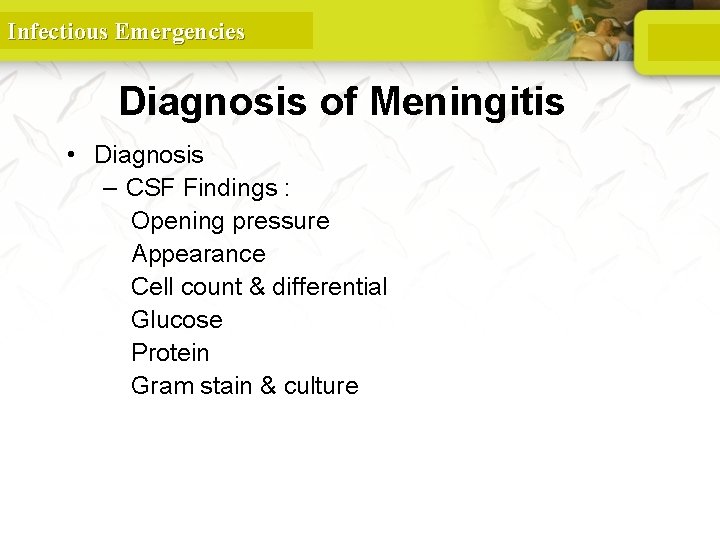
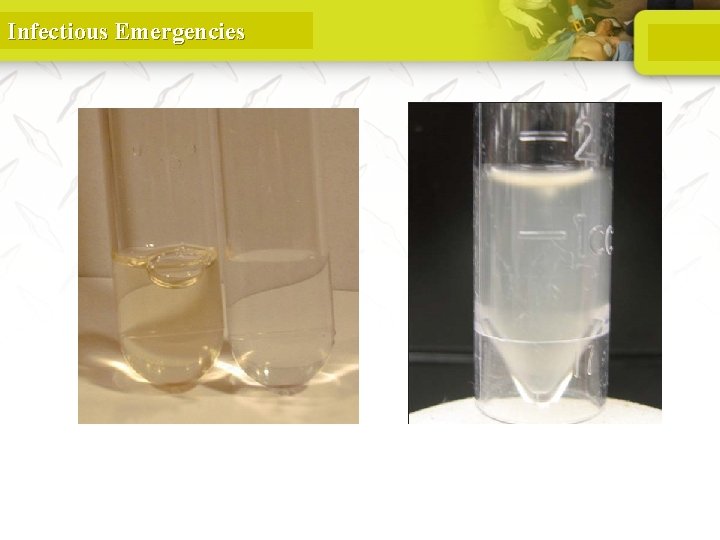
Infectious Emergencies Diagnosis of Meningitis • Diagnosis – CSF Findings : Opening pressure Appearance Cell count & differential Glucose Protein Gram stain & culture
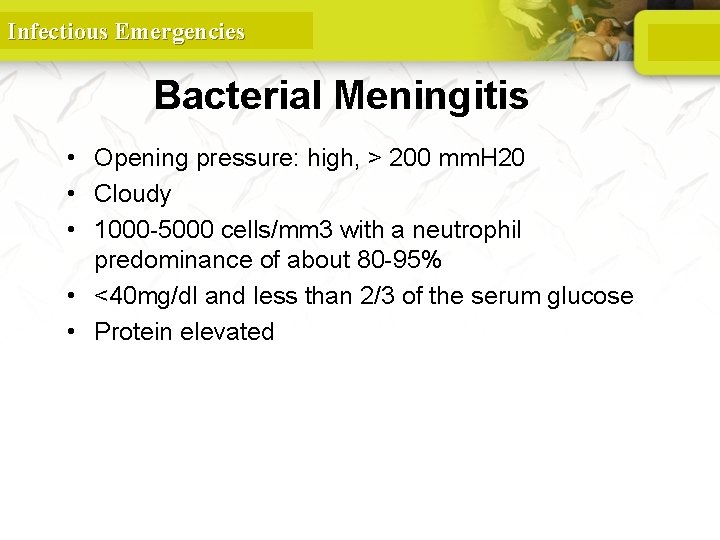
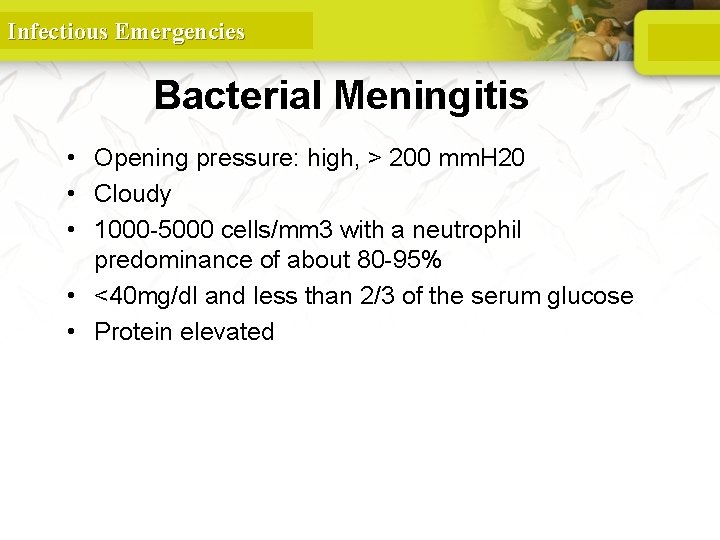
Infectious Emergencies Bacterial Meningitis • Opening pressure: high, > 200 mm. H 20 • Cloudy • 1000 -5000 cells/mm 3 with a neutrophil predominance of about 80 -95% • <40 mg/dl and less than 2/3 of the serum glucose • Protein elevated
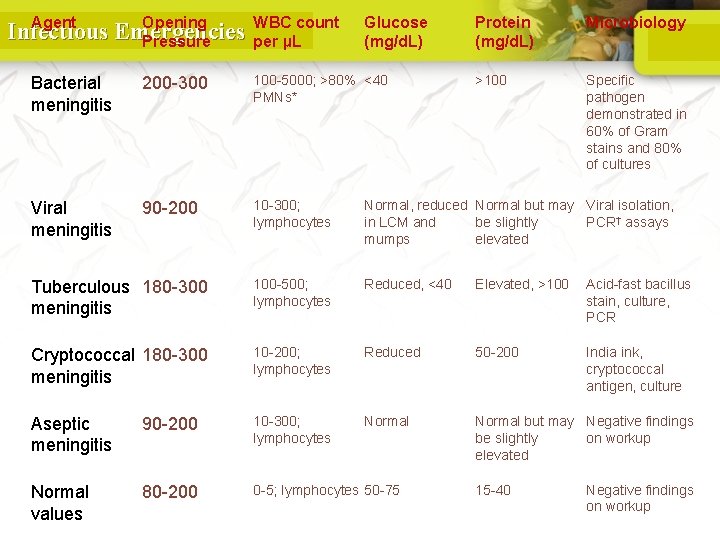
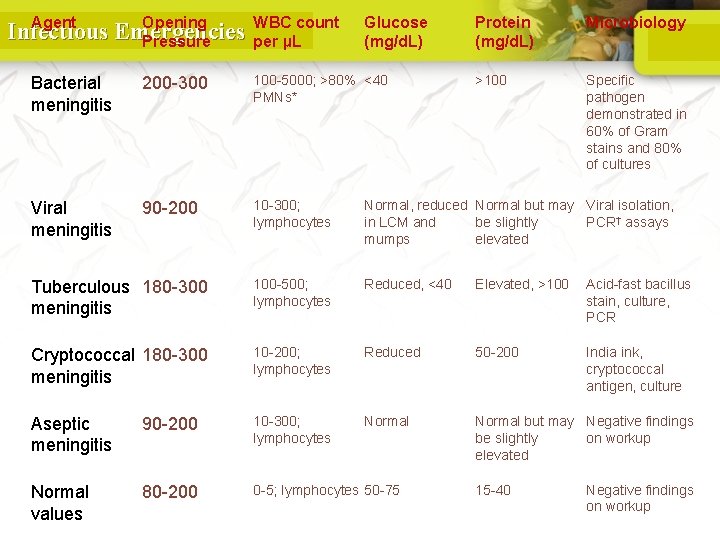
Agent Opening Infectious Emergencies Pressure WBC count per µL Glucose (mg/d. L) Protein (mg/d. L) Microbiology >100 Specific pathogen demonstrated in 60% of Gram stains and 80% of cultures Bacterial meningitis 200 -300 100 -5000; >80% <40 PMNs* Viral meningitis 90 -200 10 -300; lymphocytes Normal, reduced Normal but may Viral isolation, in LCM and be slightly PCR† assays mumps elevated Tuberculous 180 -300 meningitis 100 -500; lymphocytes Reduced, <40 Elevated, >100 Acid-fast bacillus stain, culture, PCR Cryptococcal 180 -300 meningitis 10 -200; lymphocytes Reduced 50 -200 India ink, cryptococcal antigen, culture Aseptic meningitis 90 -200 10 -300; lymphocytes Normal but may Negative findings be slightly on workup elevated Normal values 80 -200 0 -5; lymphocytes 50 -75 15 -40 Negative findings on workup
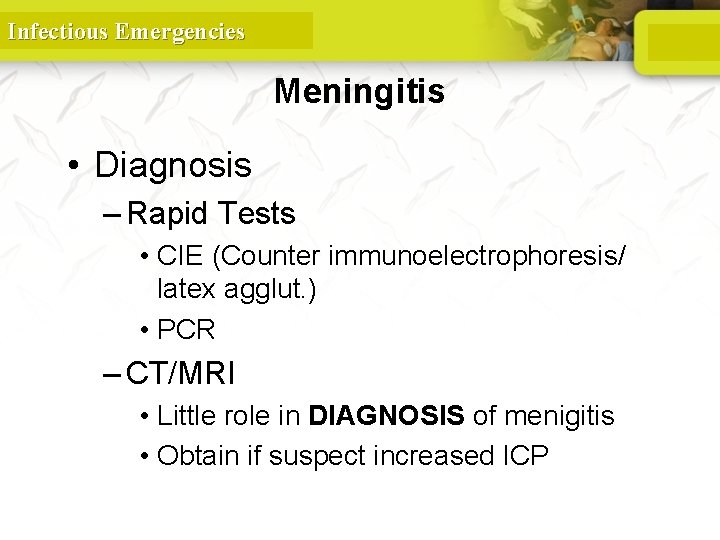
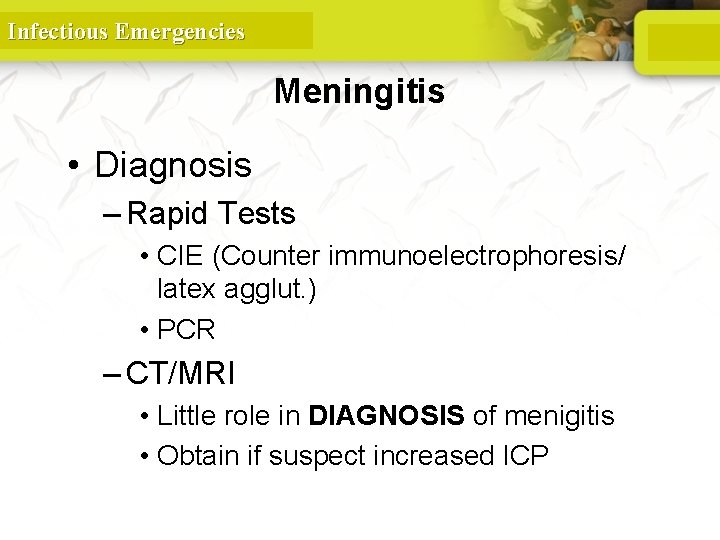
Infectious Emergencies Meningitis • Diagnosis – Rapid Tests • CIE (Counter immunoelectrophoresis/ latex agglut. ) • PCR – CT/MRI • Little role in DIAGNOSIS of menigitis • Obtain if suspect increased ICP
Infectious Emergencies Meningitis • Diagnosis – Additional Tests • CBC w/ diff • Blood cultures • CXR • Electrolytes and renal function
Infectious Emergencies Bacterial Cultures • “Gold standard” • Positive in 75 -85% who have not been treated with antibiotics
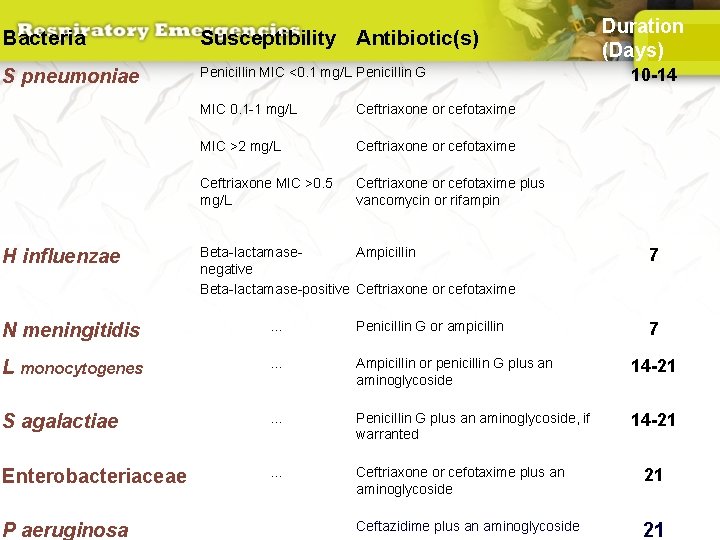
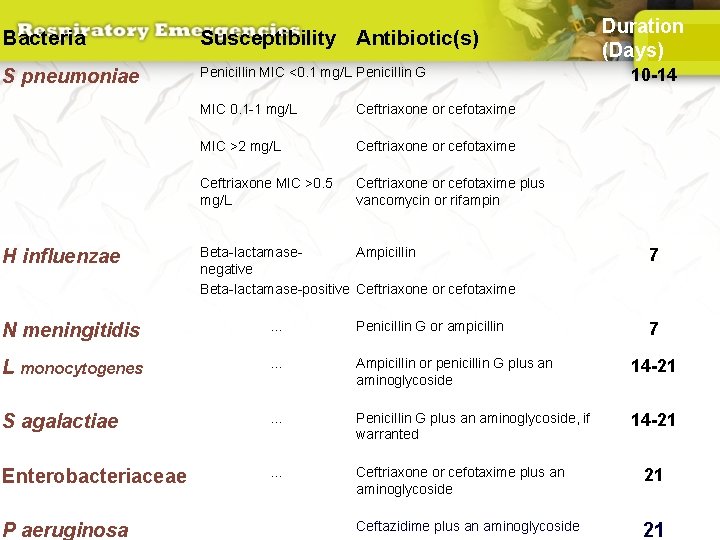
Bacteria Susceptibility Antibiotic(s) S pneumoniae Penicillin MIC <0. 1 mg/L Penicillin G H influenzae MIC 0. 1 -1 mg/L Ceftriaxone or cefotaxime MIC >2 mg/L Ceftriaxone or cefotaxime Ceftriaxone MIC >0. 5 mg/L Ceftriaxone or cefotaxime plus vancomycin or rifampin Beta-lactamase. Ampicillin negative Beta-lactamase-positive Ceftriaxone or cefotaxime Duration (Days) 10 -14 7 N meningitidis . . . Penicillin G or ampicillin L monocytogenes . . . Ampicillin or penicillin G plus an aminoglycoside 14 -21 S agalactiae . . . Penicillin G plus an aminoglycoside, if warranted 14 -21 Enterobacteriaceae . . . Ceftriaxone or cefotaxime plus an aminoglycoside 21 P aeruginosa . . . Ceftazidime plus an aminoglycoside 21 7
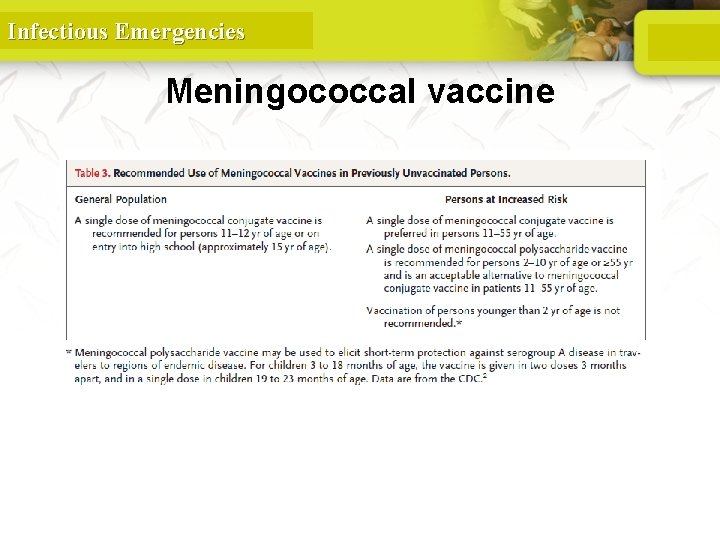
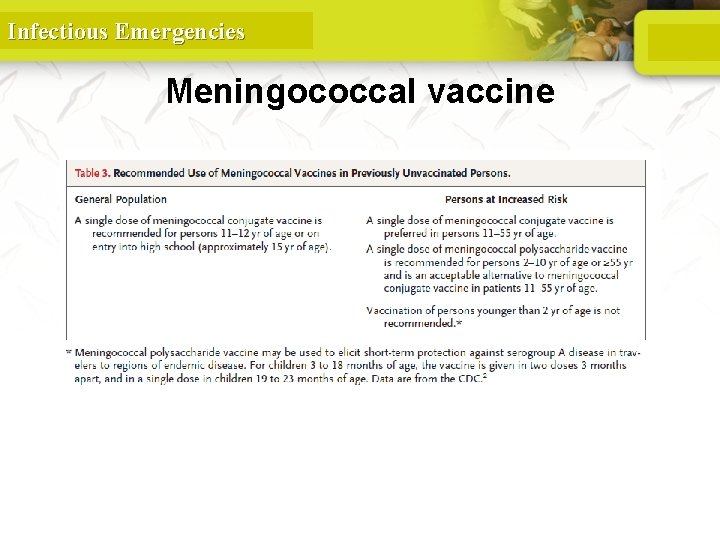
Infectious Emergencies Meningococcal vaccine
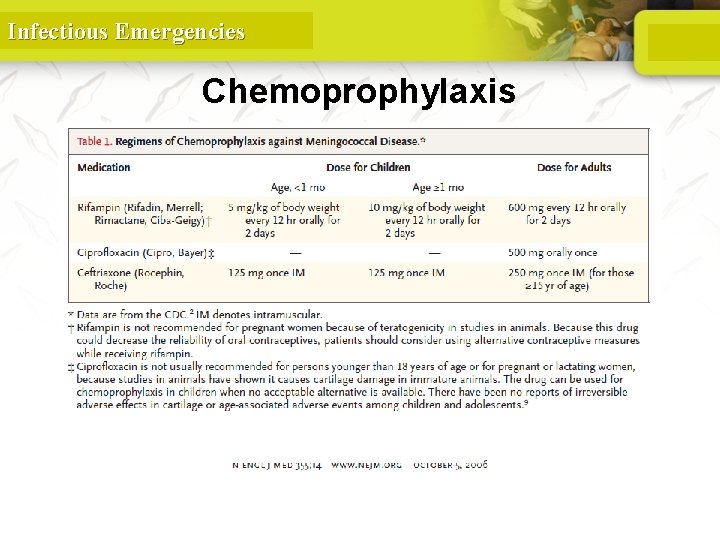
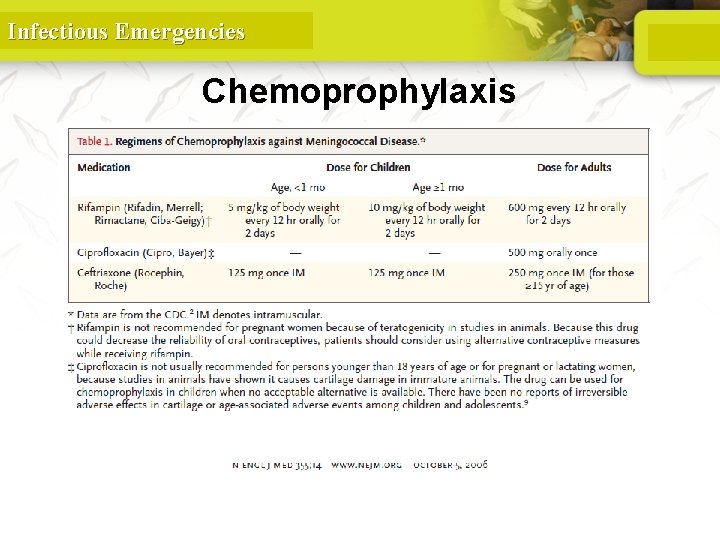
Infectious Emergencies Chemoprophylaxis
Infectious Emergencies INFECTIVE ENDOCARDITIS
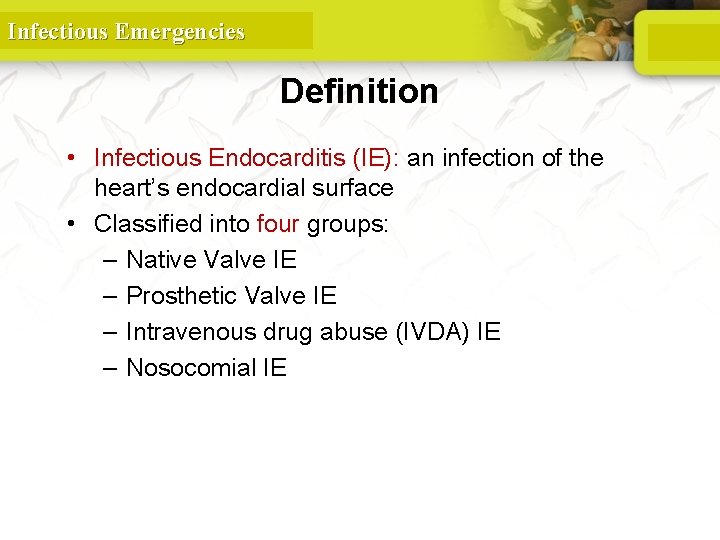
Infectious Emergencies Definition • Infectious Endocarditis (IE): an infection of the heart’s endocardial surface • Classified into four groups: – Native Valve IE – Prosthetic Valve IE – Intravenous drug abuse (IVDA) IE – Nosocomial IE
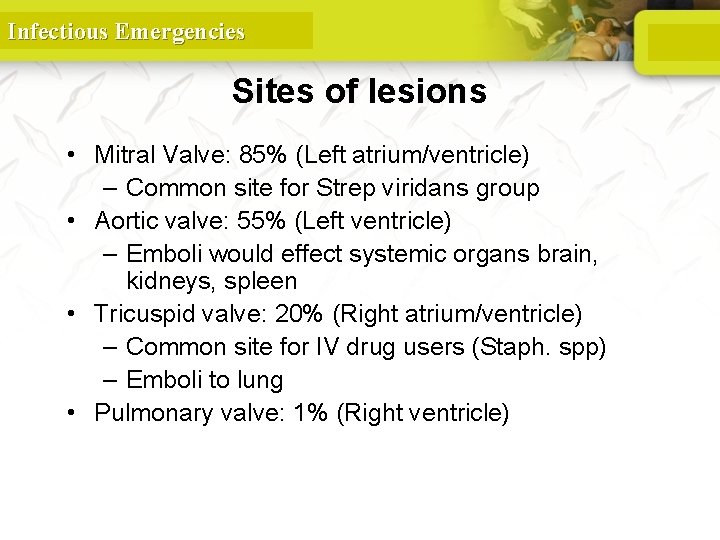
Infectious Emergencies Sites of lesions • Mitral Valve: 85% (Left atrium/ventricle) – Common site for Strep viridans group • Aortic valve: 55% (Left ventricle) – Emboli would effect systemic organs brain, kidneys, spleen • Tricuspid valve: 20% (Right atrium/ventricle) – Common site for IV drug users (Staph. spp) – Emboli to lung • Pulmonary valve: 1% (Right ventricle)
Infectious Emergencies Classification • Native valve endocarditis (NVE), acute and subacute • Prosthetic valve endocarditis (PVE), early and late • Intravenous drug abuse (IVDA) endocarditis – Other terms commonly used to classify types of IE include pacemaker IE and nosocomial IE (NIE).
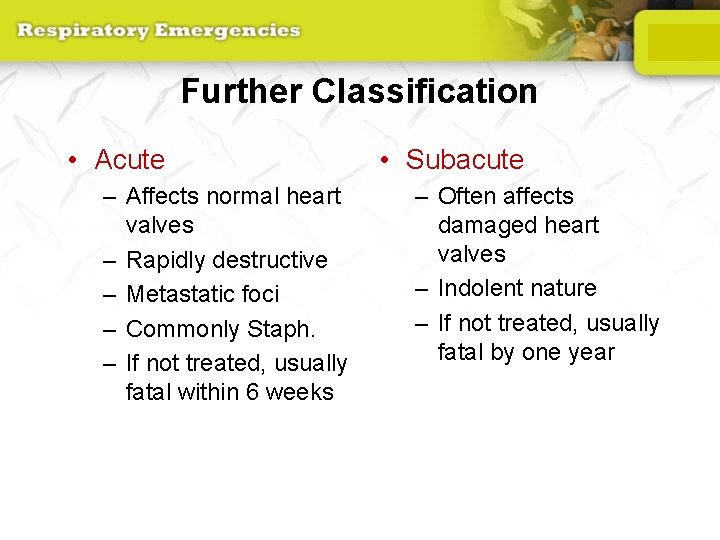
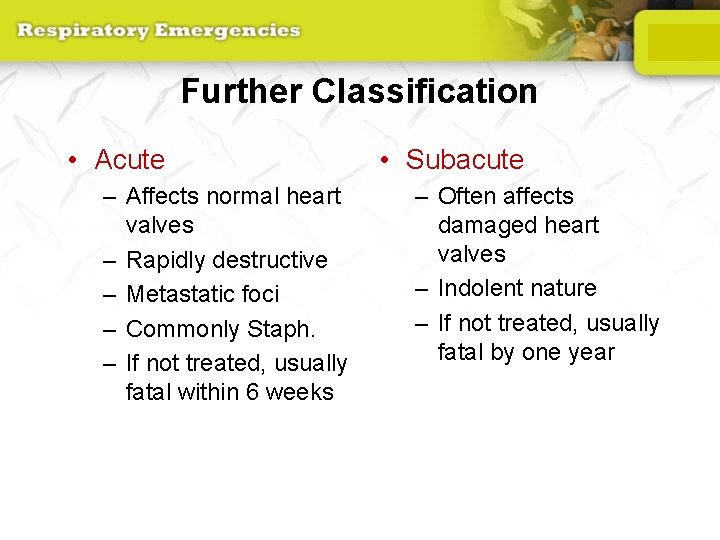
Further Classification • Acute – Affects normal heart valves – Rapidly destructive – Metastatic foci – Commonly Staph. – If not treated, usually fatal within 6 weeks • Subacute – Often affects damaged heart valves – Indolent nature – If not treated, usually fatal by one year
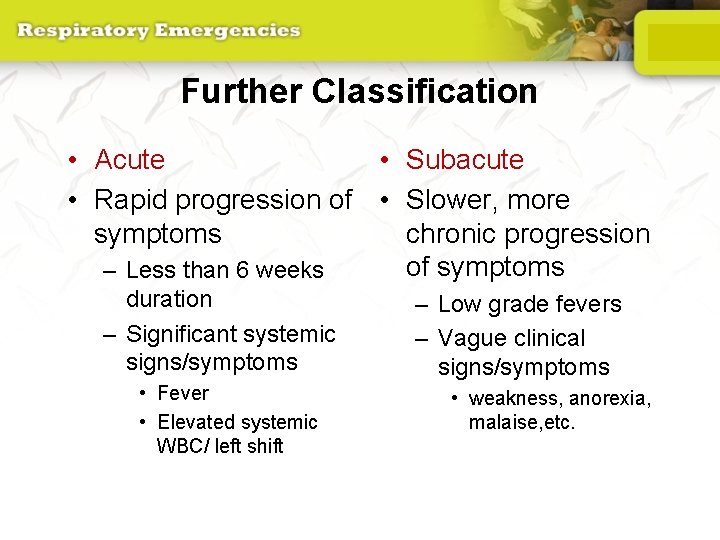
Further Classification • Acute • Subacute • Rapid progression of • Slower, more symptoms chronic progression of symptoms – Less than 6 weeks duration – Significant systemic signs/symptoms • Fever • Elevated systemic WBC/ left shift – Low grade fevers – Vague clinical signs/symptoms • weakness, anorexia, malaise, etc.

Infectious Emergencies European Heart Journal (2009
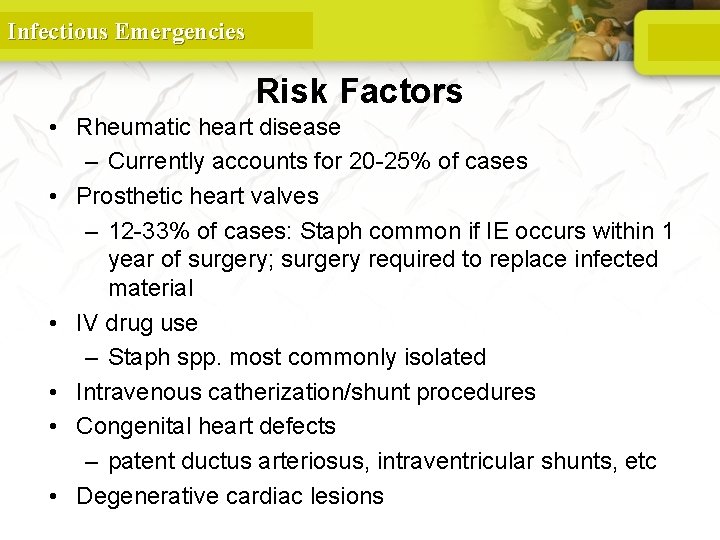
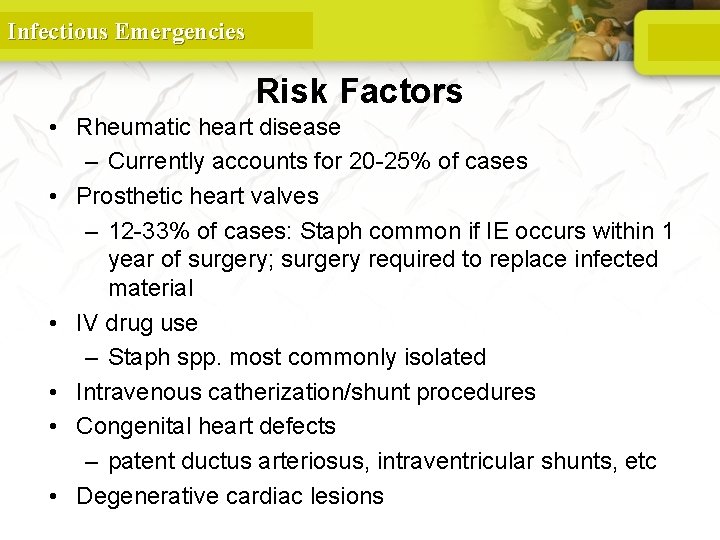
Infectious Emergencies Risk Factors • Rheumatic heart disease – Currently accounts for 20 -25% of cases • Prosthetic heart valves – 12 -33% of cases: Staph common if IE occurs within 1 year of surgery; surgery required to replace infected material • IV drug use – Staph spp. most commonly isolated • Intravenous catherization/shunt procedures • Congenital heart defects – patent ductus arteriosus, intraventricular shunts, etc • Degenerative cardiac lesions

Infectious Emergencies Infecting Organisms • Common bacteria – S. aureus – Streptococci – Enterococci • Not so common bacteria – Fungi – Pseudomonas – HACEK
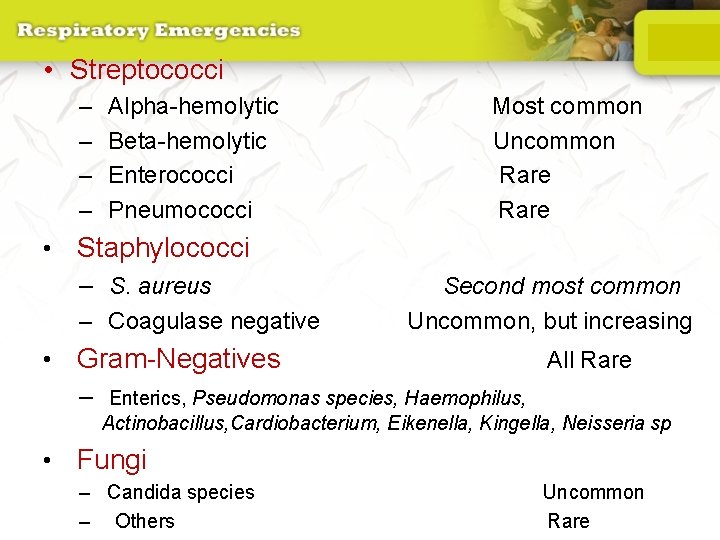
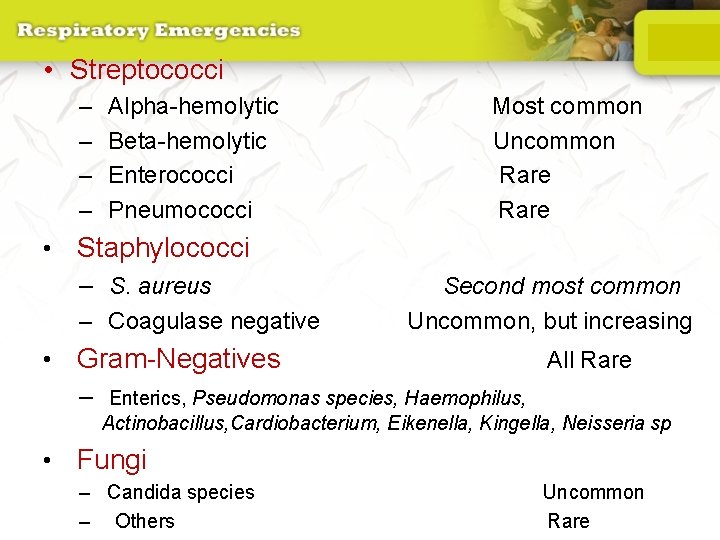
• Streptococci – – Alpha-hemolytic Beta-hemolytic Enterococci Pneumococci • Staphylococci – S. aureus – Coagulase negative Most common Uncommon Rare Second most common Uncommon, but increasing • Gram-Negatives All Rare – Enterics, Pseudomonas species, Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, Kingella, Neisseria sp • Fungi – Candida species – Others Uncommon Rare

Symptoms • Acute – High grade fever and chills – SOB – Arthralgias/ myalgias – Abdominal pain – Pleuritic chest pain – Back pain • Subacute – – – – Low grade fever Anorexia Weight loss Fatigue Arthralgias/ myalgias Abdominal pain N/V The onset of symptoms is usually ~2 weeks or less from the initiating bacteremia
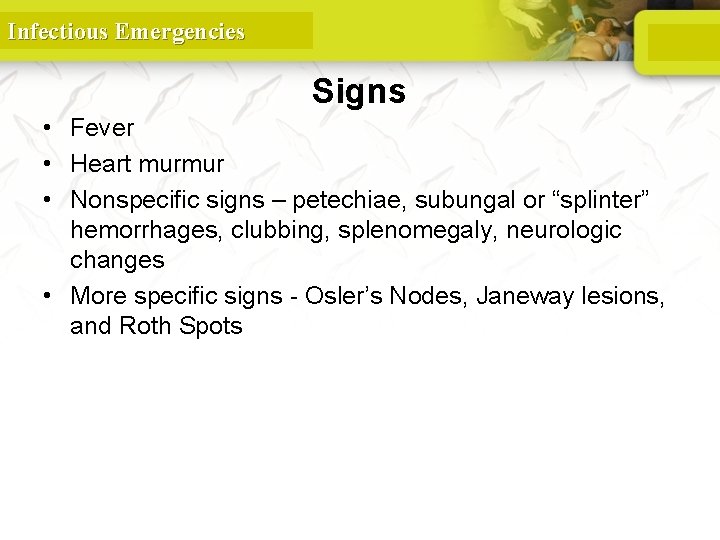
Infectious Emergencies Signs • Fever • Heart murmur • Nonspecific signs – petechiae, subungal or “splinter” hemorrhages, clubbing, splenomegaly, neurologic changes • More specific signs - Osler’s Nodes, Janeway lesions, and Roth Spots
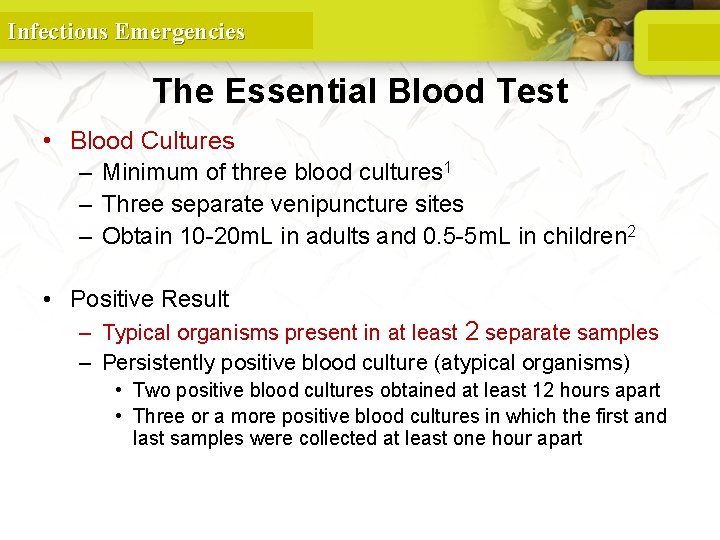
Infectious Emergencies The Essential Blood Test • Blood Cultures – Minimum of three blood cultures 1 – Three separate venipuncture sites – Obtain 10 -20 m. L in adults and 0. 5 -5 m. L in children 2 • Positive Result – Typical organisms present in at least 2 separate samples – Persistently positive blood culture (atypical organisms) • Two positive blood cultures obtained at least 12 hours apart • Three or a more positive blood cultures in which the first and last samples were collected at least one hour apart
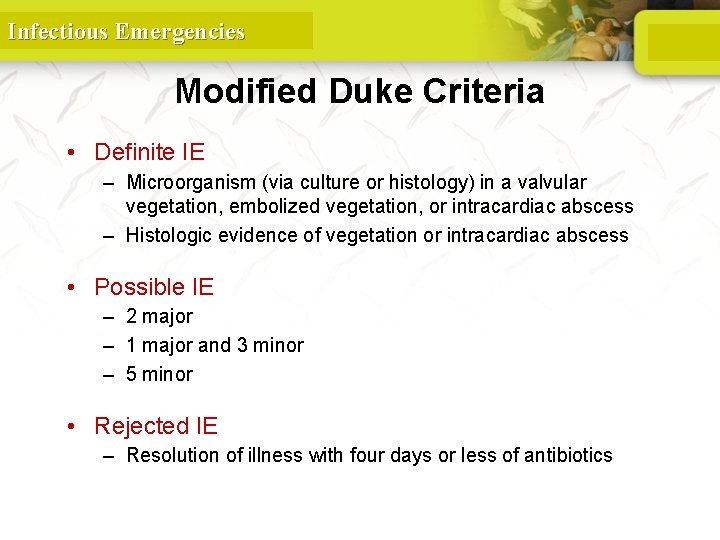
Infectious Emergencies Modified Duke Criteria • Definite IE – Microorganism (via culture or histology) in a valvular vegetation, embolized vegetation, or intracardiac abscess – Histologic evidence of vegetation or intracardiac abscess • Possible IE – 2 major – 1 major and 3 minor – 5 minor • Rejected IE – Resolution of illness with four days or less of antibiotics

Infectious Emergencies Guidelines on the prevention, diagnosis, and treatment of infective endocarditis European Heart Journal (2009)
Infectious Emergencies Treatment • Parenteral antibiotics – High serum concentrations to penetrate vegetations – Prolonged treatment to kill dormant bacteria clustered in vegetations • Surgery – Intracardiac complications • Surveillance blood cultures

Infectious Emergencies PNEUMONIA
Infectious Emergencies Infections of the Respiratory tract • Most common entry point for infections • Upper respiratory tract – nose, nasal cavity, sinuses, mouth, throat • Lower respiratory tract – Trachea, bronchioles, and alveoli in the lungs

Infectious Emergencies Respiratory System 90
Infectious Emergencies Pneumonia • Most deadly infectious disease in the U. S. • 6 th leading cause of death • Average mortality 14% • $20 billion/year in U. S. 1 • Community acquired pneumonia affects ~4 million patients and results in 10 million physician visits, • 1 million hospitalizations, and >50, 000 deaths annually File Chest 2004; 125: 1888 -1901
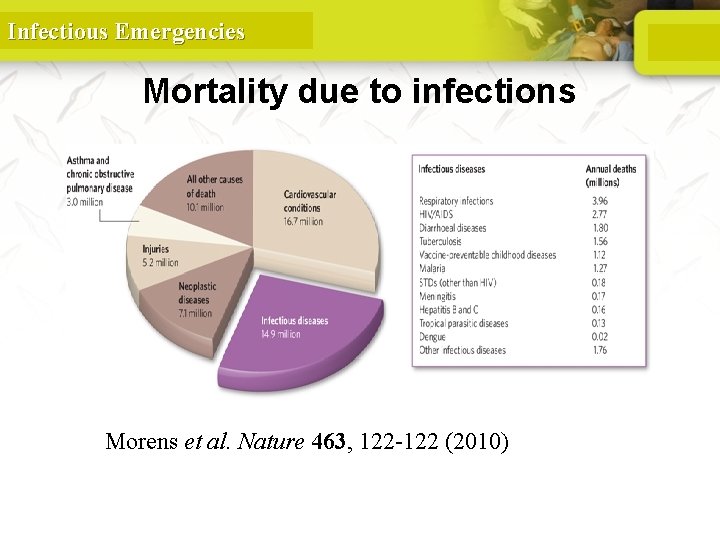
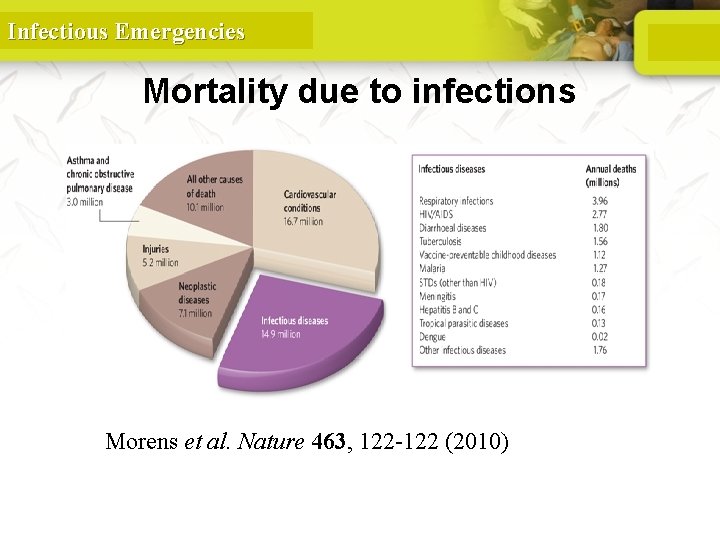
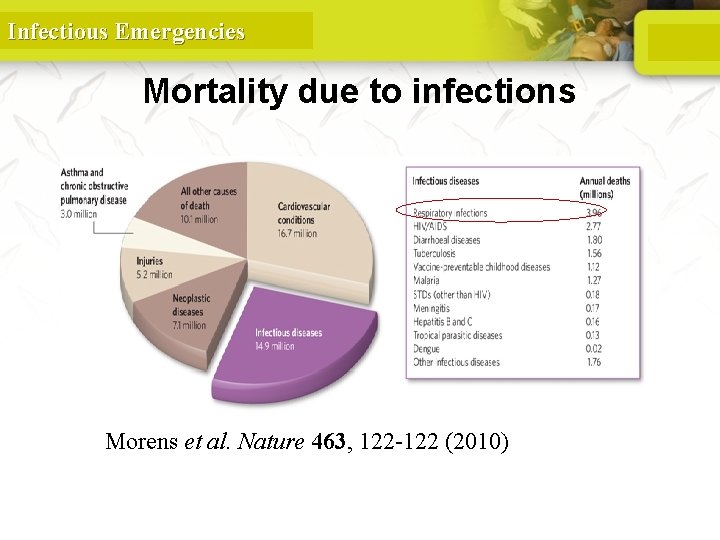
Infectious Emergencies Mortality due to infections DM Morens et al. Nature 463, 122 -122 (2010) doi: 10. 1038/nature 08554
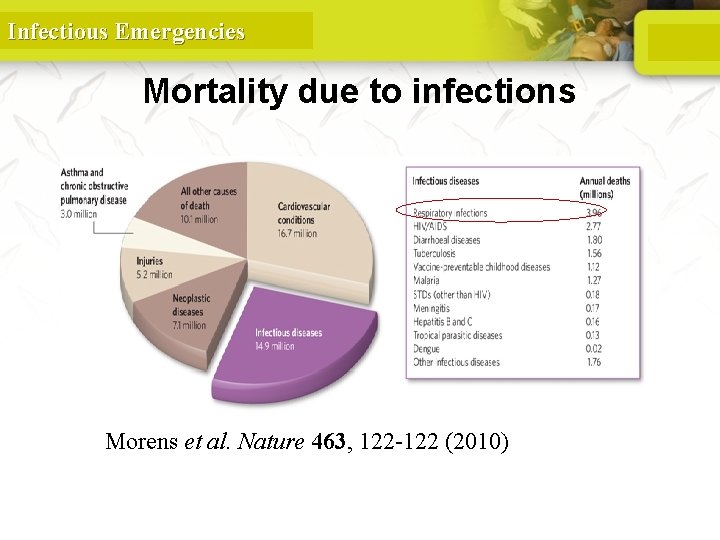
Infectious Emergencies Mortality due to infections DM Morens et al. Nature 463, 122 -122 (2010) doi: 10. 1038/nature 08554
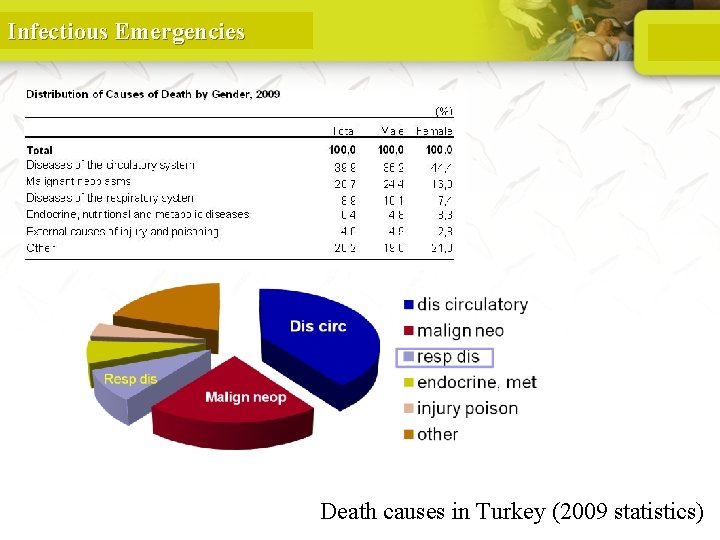
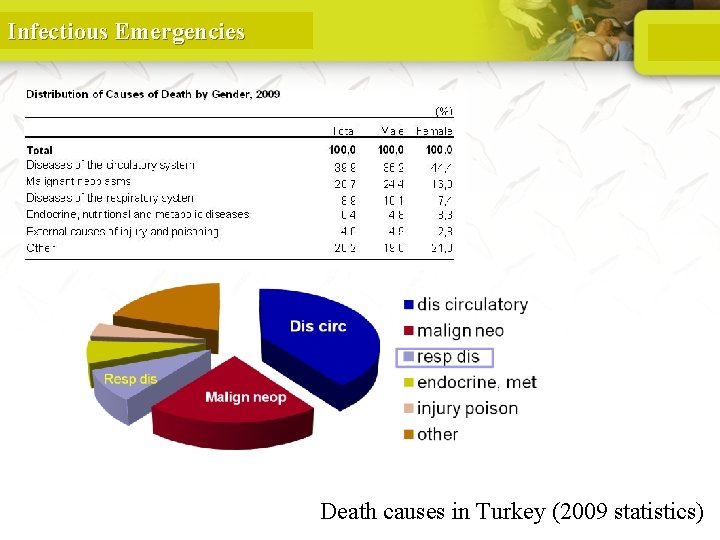
Infectious Emergencies 94 Death causes in Turkey (2009 statistics)
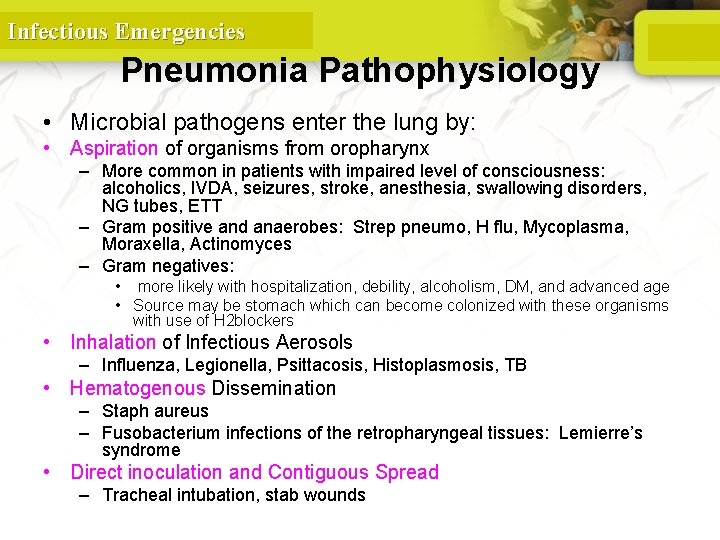
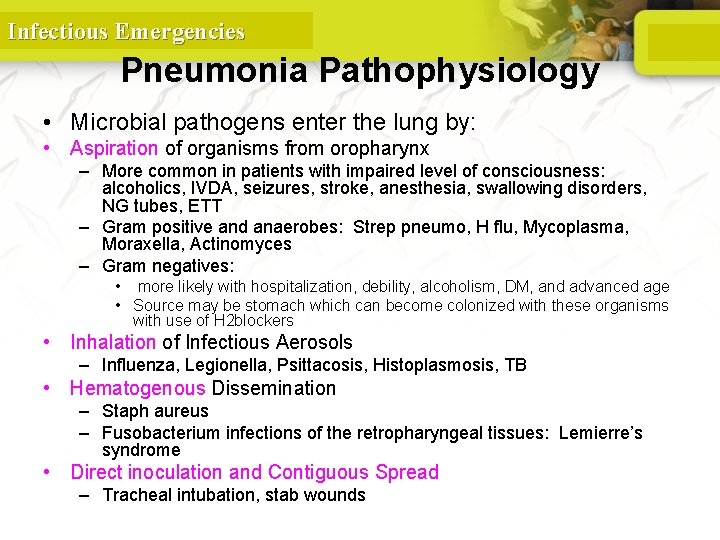
Infectious Emergencies Pneumonia Pathophysiology • Microbial pathogens enter the lung by: • Aspiration of organisms from oropharynx – More common in patients with impaired level of consciousness: alcoholics, IVDA, seizures, stroke, anesthesia, swallowing disorders, NG tubes, ETT – Gram positive and anaerobes: Strep pneumo, H flu, Mycoplasma, Moraxella, Actinomyces – Gram negatives: • more likely with hospitalization, debility, alcoholism, DM, and advanced age • Source may be stomach which can become colonized with these organisms with use of H 2 blockers • Inhalation of Infectious Aerosols – Influenza, Legionella, Psittacosis, Histoplasmosis, TB • Hematogenous Dissemination – Staph aureus – Fusobacterium infections of the retropharyngeal tissues: Lemierre’s syndrome • Direct inoculation and Contiguous Spread – Tracheal intubation, stab wounds

Infectious Emergencies Anatomy and Function of the Lung 96
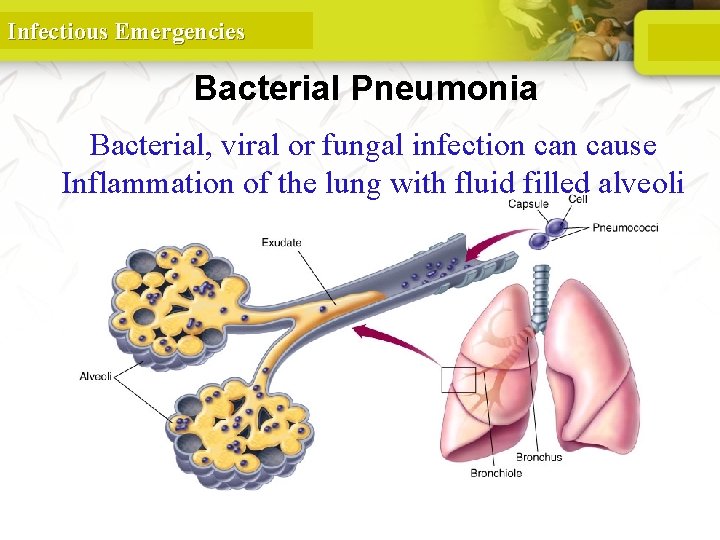
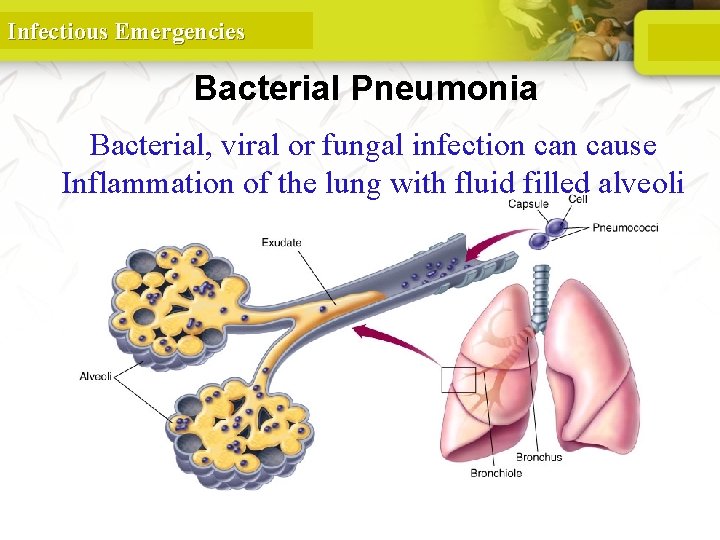
Infectious Emergencies Bacterial Pneumonia Bacterial, viral or fungal infection cause Inflammation of the lung with fluid filled alveoli

Infectious Emergencies Characteristics of Adequate Breathing • Normal rate and depth • Regular breathing pattern • Good breath sounds on both sides of the chest • Equal rise and fall of chest • Pink, warm, dry skin 98
Infectious Emergencies Characteristics of Inadequate Breathing • • • Pulmonary vessels become obstructed. Alveoli are damaged. Air passages are obstructed. Blood flow to the lungs is obstructed. Pleural space is filled. 99
Infectious Emergencies Signs of Inadequate Breathing • Slower than 12 breaths/min or faster than 20 breaths/min • Unequal chest expansion • Decreased breath sounds • Muscle retractions • Pale or cyanotic skin • Cool, damp (clammy) skin • Shallow or irregular respirations • Pursed lips • Nasal flaring 100
Infectious Emergencies Dyspnea • Shortness of breath or difficulty breathing • Patient may not be alert enough to complain of shortness of breath. 101
Infectious Emergencies Upper or Lower Airway Infection • Infectious diseases may affect all parts of the airway. • The problem is some form of obstruction to the air flow or the exchange of gases. 102
Infectious Emergencies Detailed Physical Exam • Performed only once life threats are addressed. • May not be able to do if busy treating airway or breathing problems. 103

Infectious Emergencies Ongoing Assessment • Carefully watch patients for shortness of breath. • Reassess vital signs. • Ask patient if treatment has made a difference. • Check for accessory muscle use. 104
Infectious Emergencies Clinical presentation • Pneumonia should be considered in any patient who has newly acquired respiratory symptoms: cough, sputum production, dyspnea, especially if accompanied by fever and abnormal breath sounds and crackles • In elderly or immunocompromised, pneumonia may present with confusion, failure to thrive, worsening of underlying chronic illness, falling
Infectious Emergencies Pneumonia Symptoms • “Typical” pneumonia: sudden onset of fever, cough productive of purulent sputum, pleuritic chest pain • “Atypical”: gradual onset, dry cough, prominence of extrapulmonary symptoms: headache, myalgias, fatigue, sore throat, nausea, vomiting • Includes diverse entities and has limited clinical value
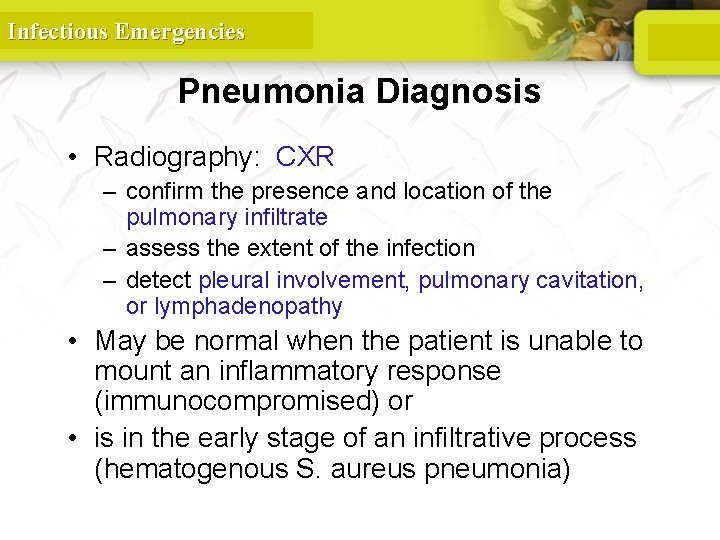
Infectious Emergencies Pneumonia Diagnosis • Radiography: CXR – confirm the presence and location of the pulmonary infiltrate – assess the extent of the infection – detect pleural involvement, pulmonary cavitation, or lymphadenopathy • May be normal when the patient is unable to mount an inflammatory response (immunocompromised) or • is in the early stage of an infiltrative process (hematogenous S. aureus pneumonia)
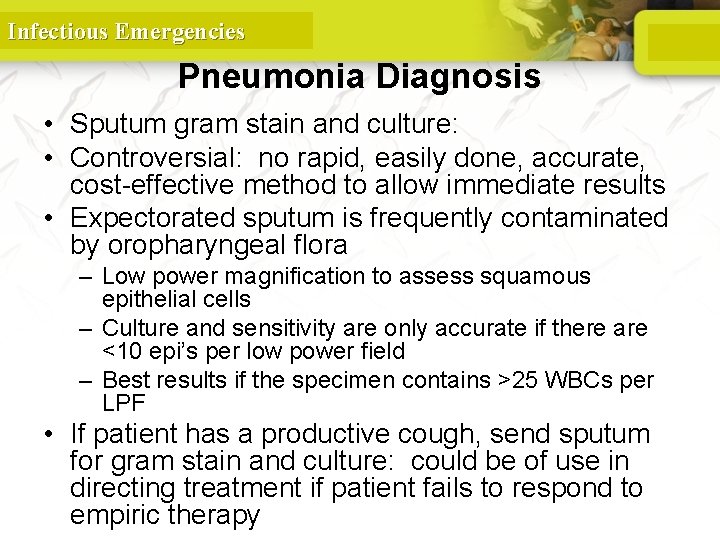
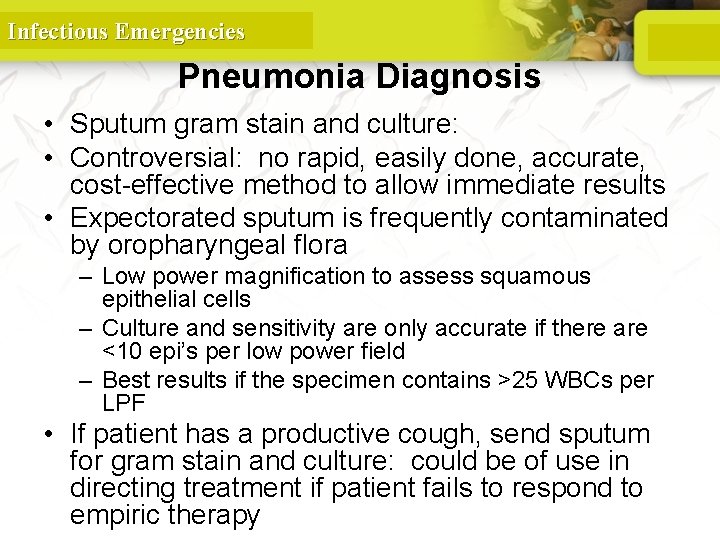
Infectious Emergencies Pneumonia Diagnosis • Sputum gram stain and culture: • Controversial: no rapid, easily done, accurate, cost-effective method to allow immediate results • Expectorated sputum is frequently contaminated by oropharyngeal flora – Low power magnification to assess squamous epithelial cells – Culture and sensitivity are only accurate if there are <10 epi’s per low power field – Best results if the specimen contains >25 WBCs per LPF • If patient has a productive cough, send sputum for gram stain and culture: could be of use in directing treatment if patient fails to respond to empiric therapy
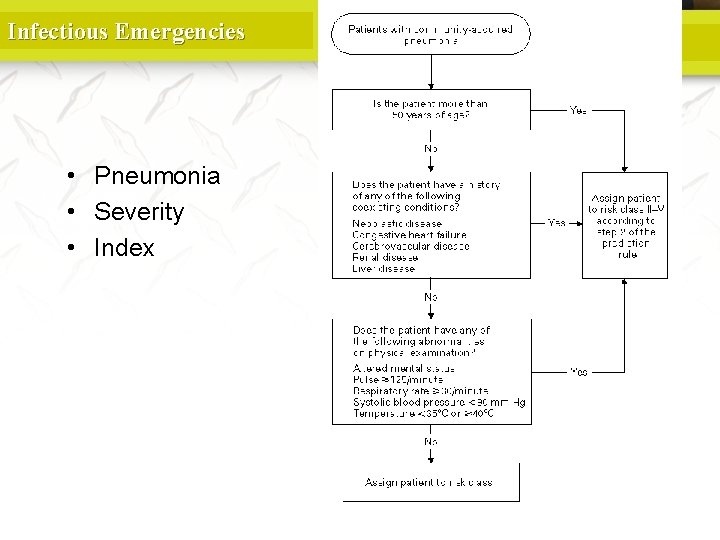
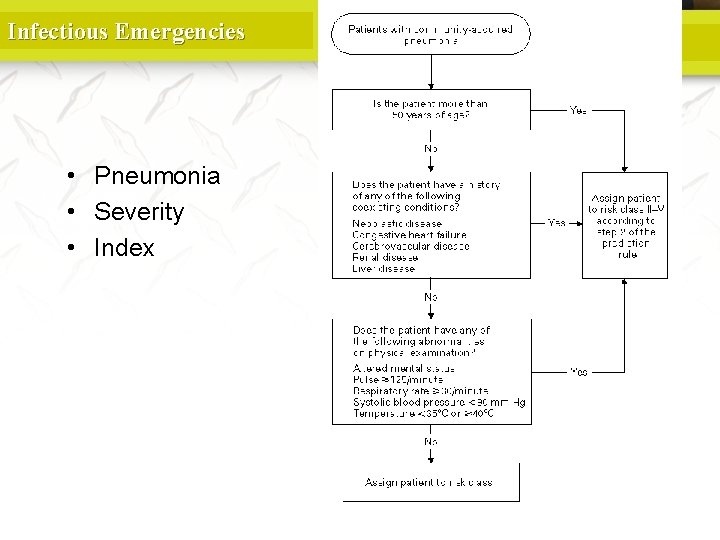
Infectious Emergencies • Pneumonia • Severity • Index
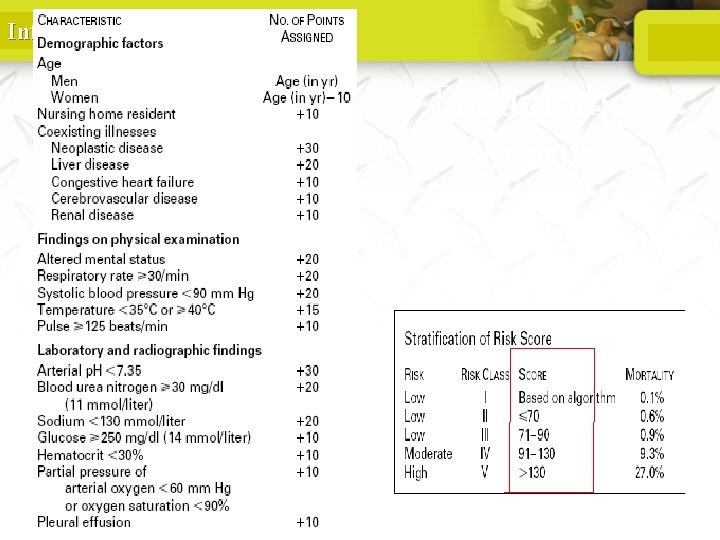
Infectious Emergencies Pneumonia Severity Index

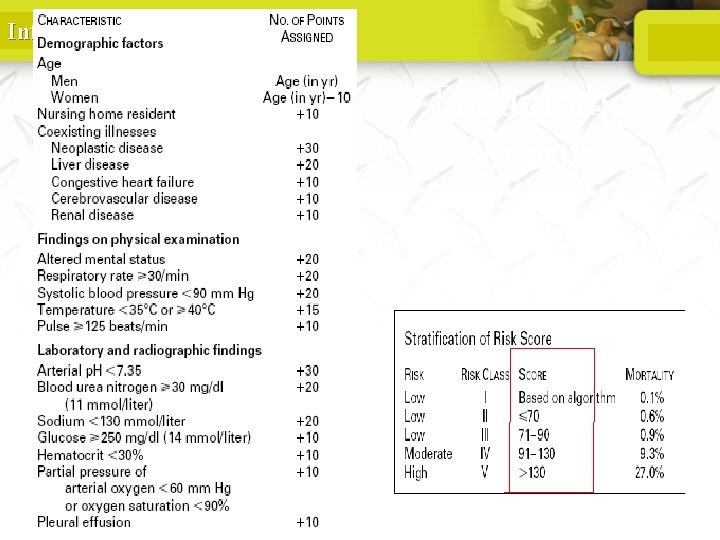
Infectious Emergencies PORT Score • • • Age 55 -10=45 CHF +10 RR +20 HR 124 +10 BUN +20 p. O 2 +10 115 Class IV Mortality 8 -9%
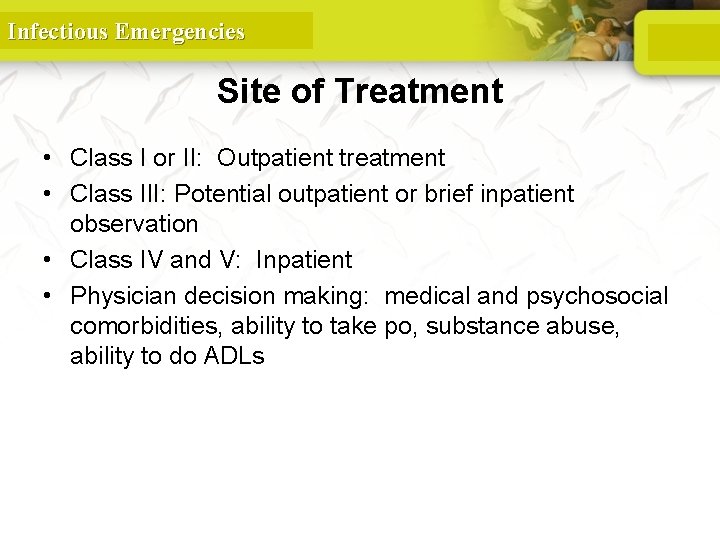
Infectious Emergencies Site of Treatment • Class I or II: Outpatient treatment • Class III: Potential outpatient or brief inpatient observation • Class IV and V: Inpatient • Physician decision making: medical and psychosocial comorbidities, ability to take po, substance abuse, ability to do ADLs
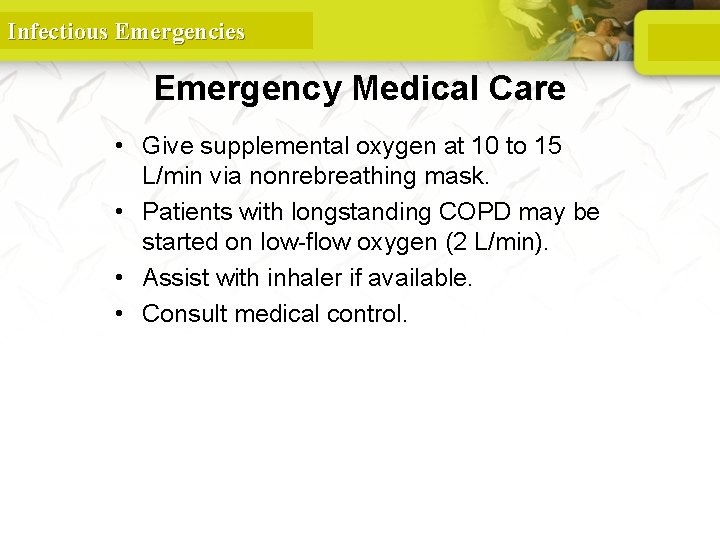
Infectious Emergencies Emergency Medical Care • Give supplemental oxygen at 10 to 15 L/min via nonrebreathing mask. • Patients with longstanding COPD may be started on low-flow oxygen (2 L/min). • Assist with inhaler if available. • Consult medical control. 113
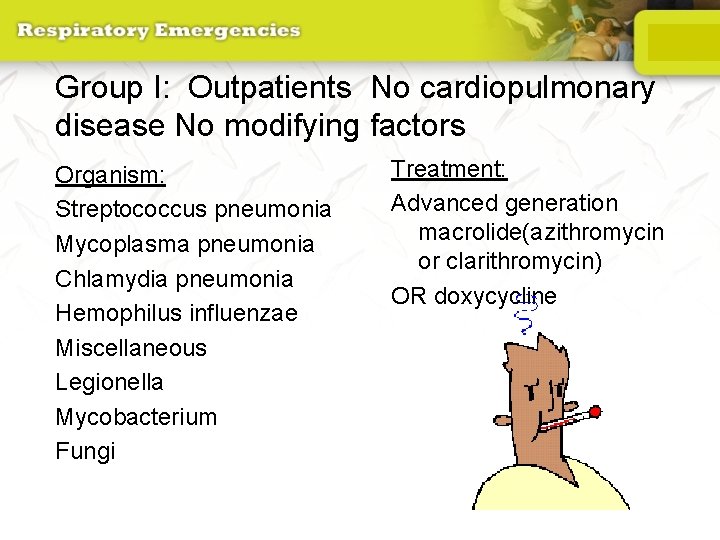
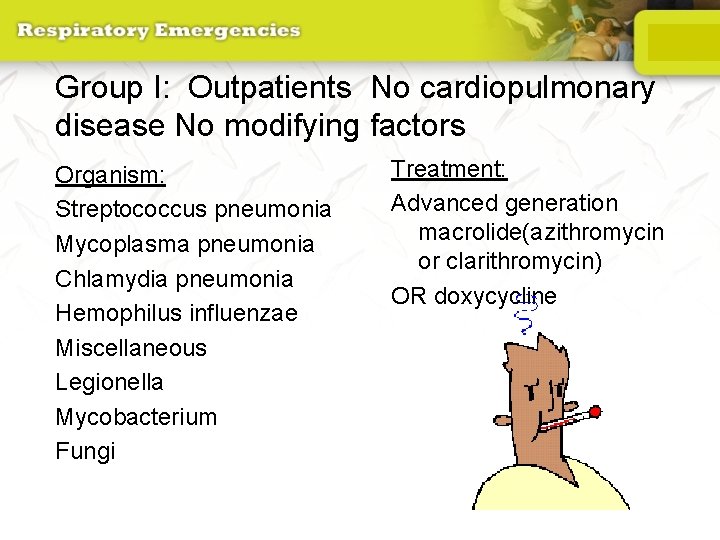
Group I: Outpatients No cardiopulmonary disease No modifying factors Organism: Streptococcus pneumonia Mycoplasma pneumonia Chlamydia pneumonia Hemophilus influenzae Miscellaneous Legionella Mycobacterium Fungi Treatment: Advanced generation macrolide(azithromycin or clarithromycin) OR doxycycline

Group II: Outpatient, with cardiopulmonary disease, and/or other modifying factors • • • Organism: Strep pneumonia Mycoplasma Chlamydia Mixed infection Hemophilus influenzae Enteric gram-negatives Viruses Miscellaneous Moraxella, Legionella, anaerobes, TB, fungi • Therapy: • B -lactam (oral cefpodoxime, cefuroxime, high-dose amoxicillin, amoxicillin/clavulanate or parenteral ceftriaxone PLUS • Macrolide or doxycycline OR • Antipneumococcal fluoroquinolone
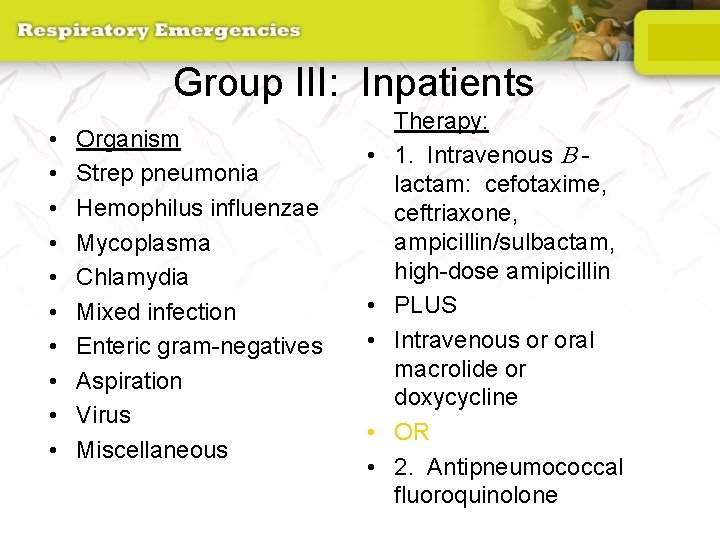
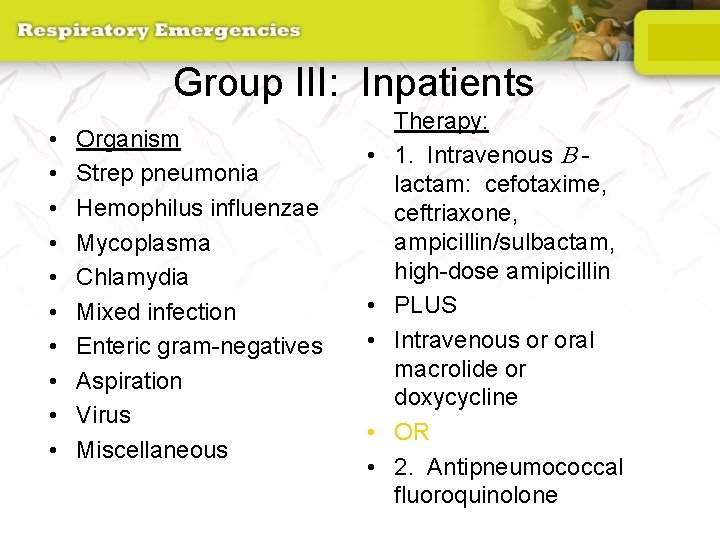
Group III: Inpatients • • • Organism Strep pneumonia Hemophilus influenzae Mycoplasma Chlamydia Mixed infection Enteric gram-negatives Aspiration Virus Miscellaneous • • • Therapy: 1. Intravenous B lactam: cefotaxime, ceftriaxone, ampicillin/sulbactam, high-dose amipicillin PLUS Intravenous or oral macrolide or doxycycline OR 2. Antipneumococcal fluoroquinolone
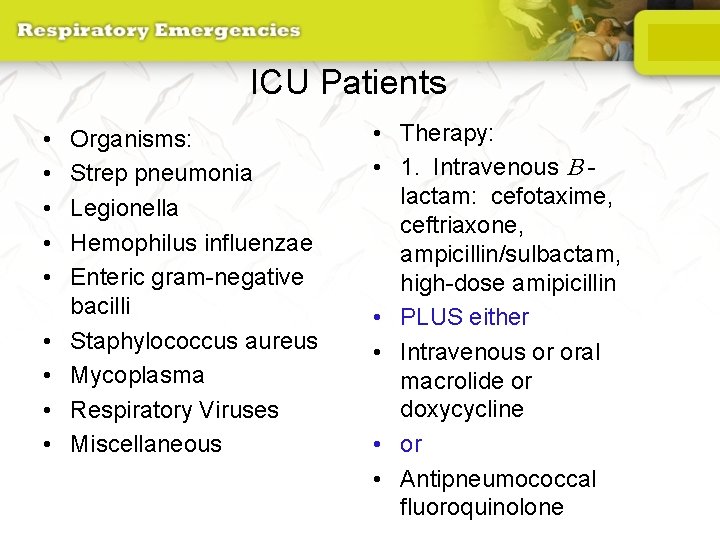
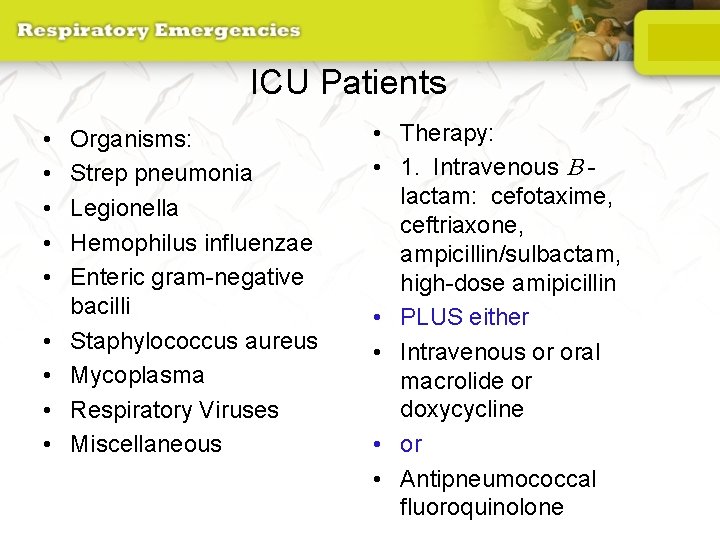
ICU Patients • • • Organisms: Strep pneumonia Legionella Hemophilus influenzae Enteric gram-negative bacilli Staphylococcus aureus Mycoplasma Respiratory Viruses Miscellaneous • Therapy: • 1. Intravenous B lactam: cefotaxime, ceftriaxone, ampicillin/sulbactam, high-dose amipicillin • PLUS either • Intravenous or oral macrolide or doxycycline • or • Antipneumococcal fluoroquinolone
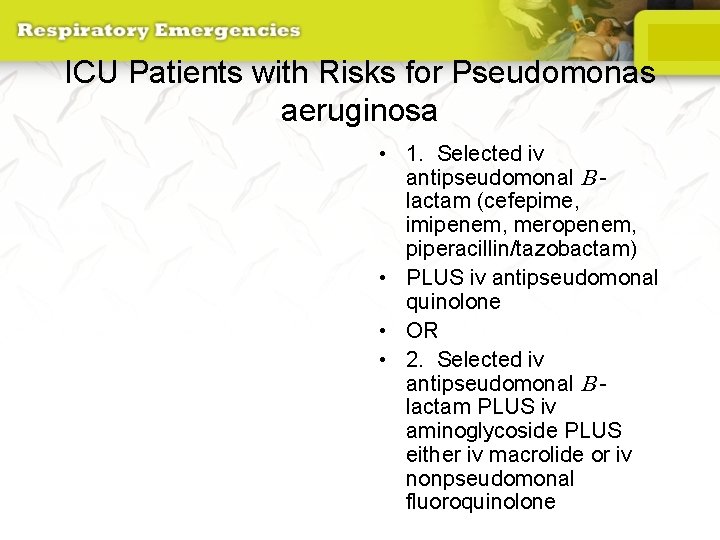
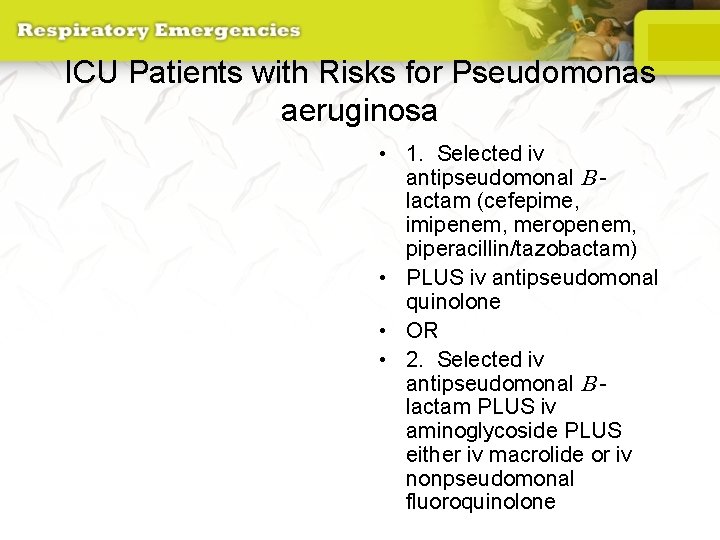
ICU Patients with Risks for Pseudomonas aeruginosa • 1. Selected iv antipseudomonal B lactam (cefepime, imipenem, meropenem, piperacillin/tazobactam) • PLUS iv antipseudomonal quinolone • OR • 2. Selected iv antipseudomonal B lactam PLUS iv aminoglycoside PLUS either iv macrolide or iv nonpseudomonal fluoroquinolone

Infectious Emergencies GASTROENTERITIS
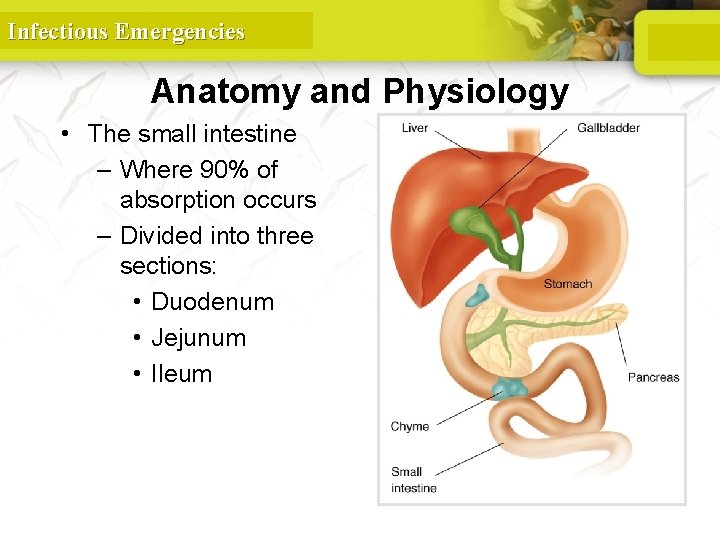
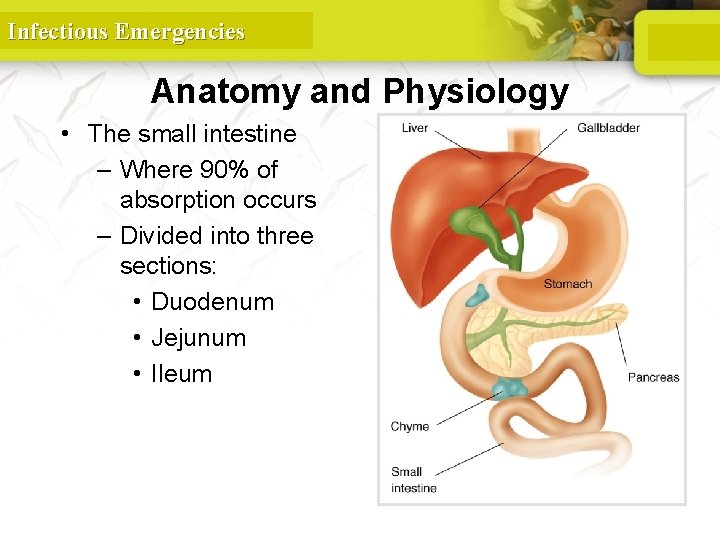
Infectious Emergencies Anatomy and Physiology • The small intestine – Where 90% of absorption occurs – Divided into three sections: • Duodenum • Jejunum • Ileum
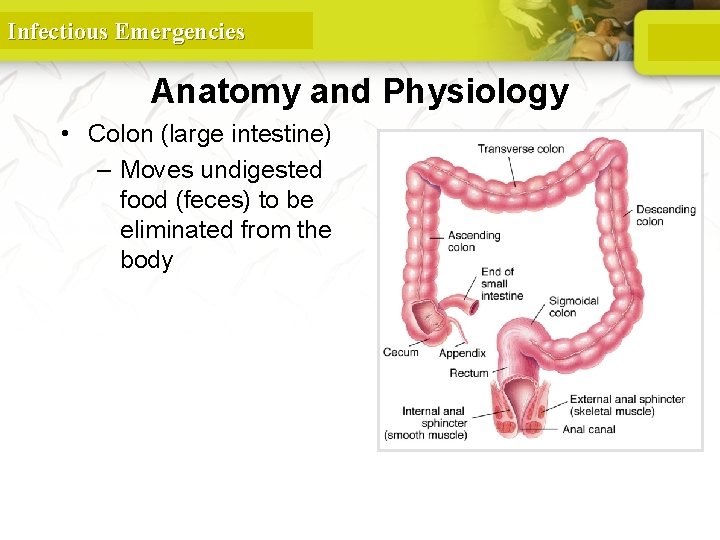
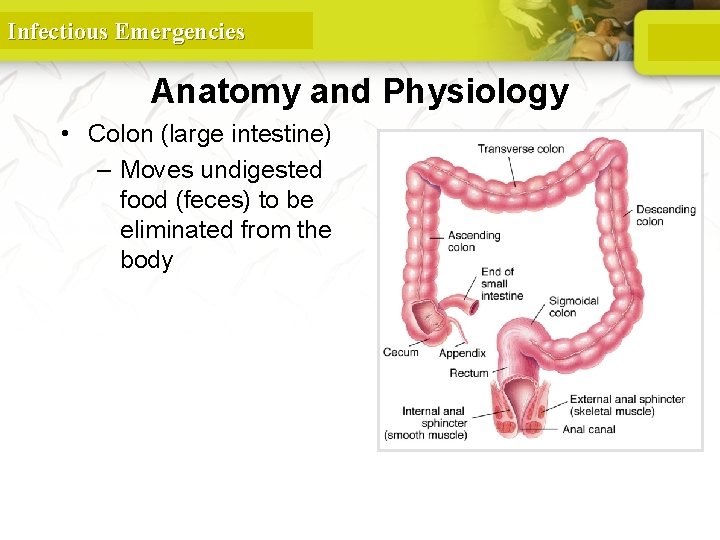
Infectious Emergencies Anatomy and Physiology • Colon (large intestine) – Moves undigested food (feces) to be eliminated from the body
Infectious Emergencies Anatomy and Physiology • The main role of the large intestine is to complete the reabsorption of water. • Bacterial digestion also occurs in the colon. • The journey from mouth to anus takes 8 to 72 hours.

Infectious Emergencies Introduction • GI problems are rarely life threatening. – Can lead to systemic problems if untreated
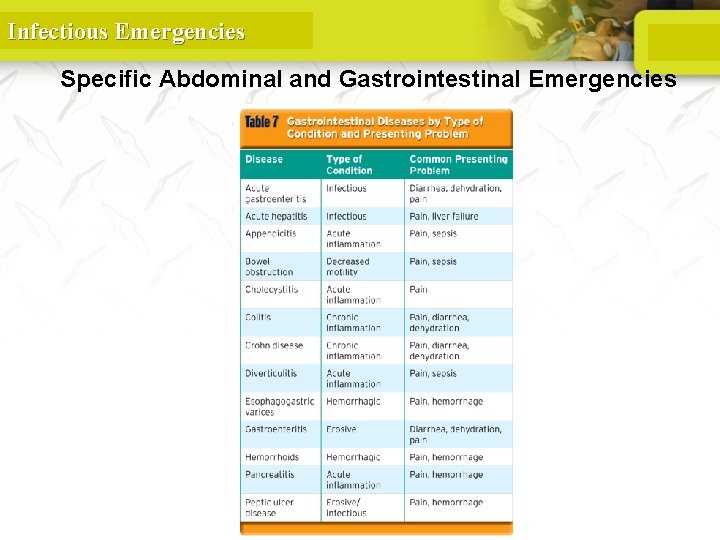
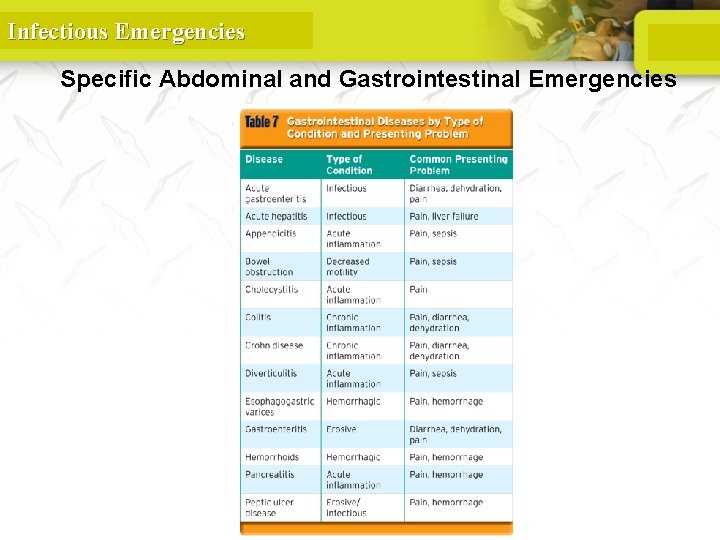
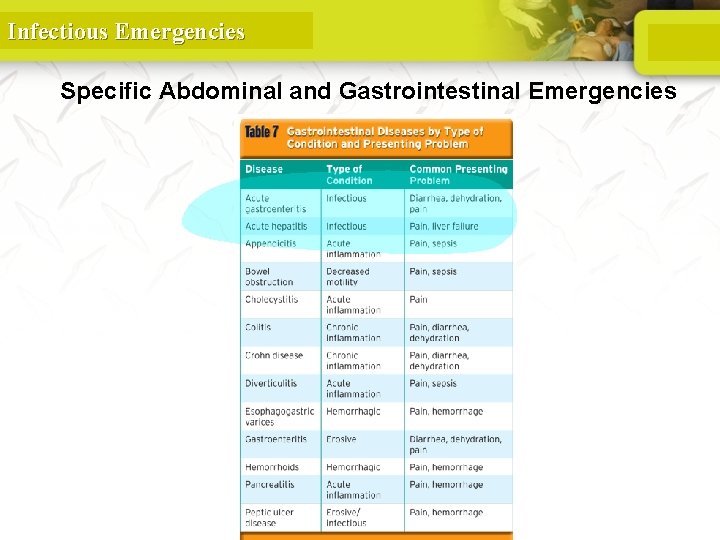
Infectious Emergencies Specific Abdominal and Gastrointestinal Emergencies
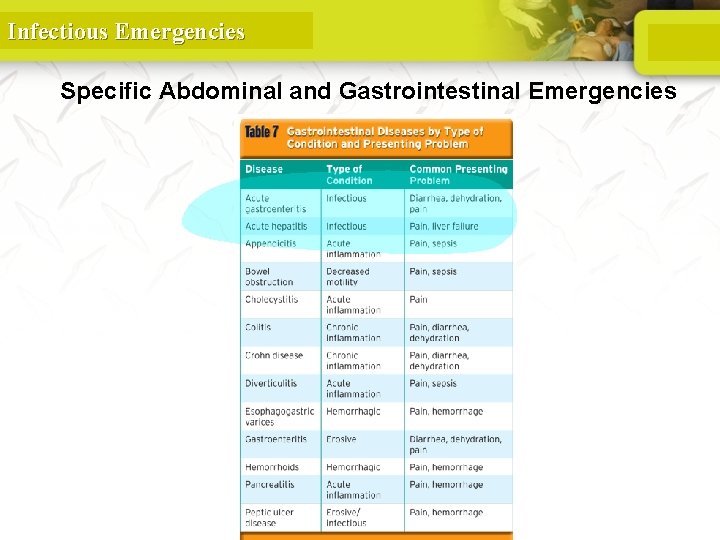
Infectious Emergencies Specific Abdominal and Gastrointestinal Emergencies
Infectious Emergencies Cholecystitis and Biliary Tract Disorders • Pathophysiology – Inflammation of the gallbladder • Choleangitis—inflammation of bile duct • Cholelithiasis—stones in the gallbladder • Cholecystitis—inflammation of the gallbladder • Acalculus cholecystitis—inflammation without gallstones
Infectious Emergencies Cholecystitis and Biliary Tract Disorders • Pathophysiology (cont’d) – May arise from decreased flow of biliary materials – Patient may present with: • Murphy sign • Nausea/vomiting • Jaundice

Infectious Emergencies Appendicitis • Pathophysiology – Fecal and other matter builds up in appendix. – Build-up of pressure will eventually cause the organ to rupture, resulting in: • Peritonitis • Sepsis • Death
Infectious Emergencies Appendicitis • Assessment – Stages of presentation • Early—periumbilical pain, nausea, vomiting • Ripe—pain in lower right quadrant • Rupture—decrease in pain (decrease in pressure) – Evaluate for peritonitis with Dunphy sign.
Infectious Emergencies Appendicitis • Management – Assess for septicemia. – Volume resuscitation • Use dopamine if crystalloids are not effective. – Administer pain and antinausea medications.
Infectious Emergencies Pancreatitis • Pathophysiology – Inflammation of the pancreas – Occurs when the tube carrying enzymes becomes blocked, leading to autodigestion – Can occur suddenly or over many months – May be single or episodic attacks

Infectious Emergencies Pancreatitis • Assessment – Signs and symptoms may include: • Sharp pain in the epigastric area or right upper abdomen • Pain radiating to the back • Muscle spasms
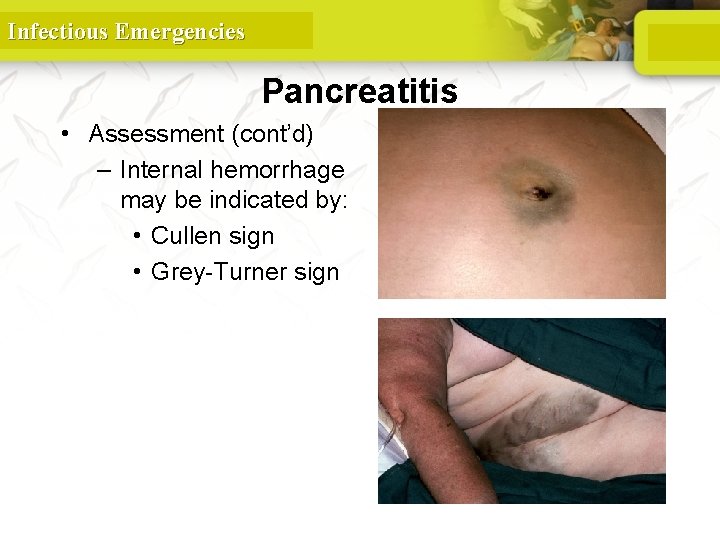
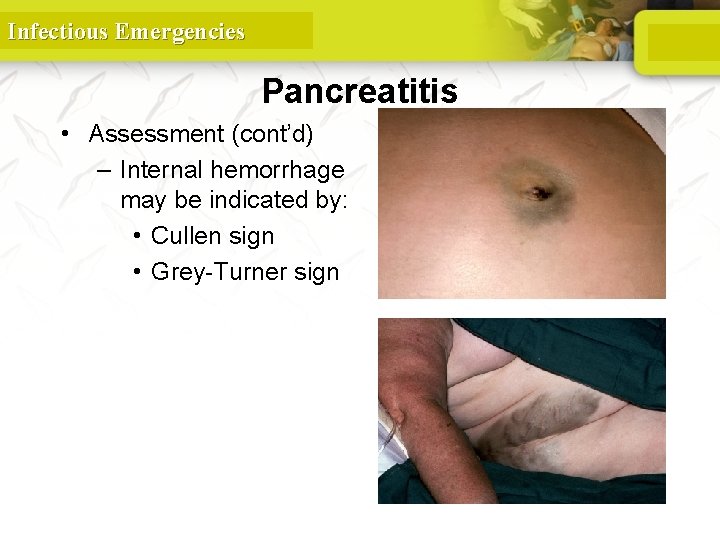
Infectious Emergencies © Wellcome Trust/Custom Medical Stock Photo • Assessment (cont’d) – Internal hemorrhage may be indicated by: • Cullen sign • Grey-Turner sign © Wellcome Trust/Custom Medical Stock Photo Pancreatitis
Infectious Emergencies Pancreatitis • Management – Directed by general management guidelines – Assess for signs of severe hemorrhage. – Meperidine is the choice for pain management.
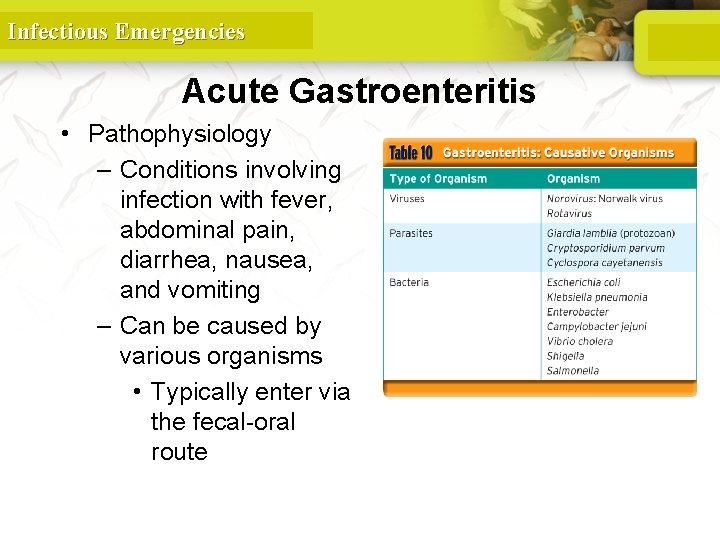
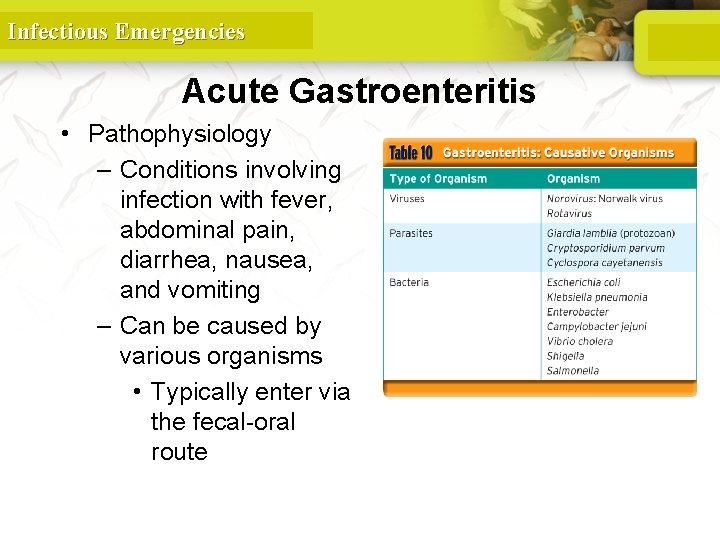
Infectious Emergencies Acute Gastroenteritis • Pathophysiology – Conditions involving infection with fever, abdominal pain, diarrhea, nausea, and vomiting – Can be caused by various organisms • Typically enter via the fecal-oral route
Infectious Emergencies Acute Gastroenteritis • Assessment – Symptoms may show anywhere from several hours to several days from contact – Can last two or three days, or several weeks
Infectious Emergencies Acute Gastroenteritis • Assessment (cont’d) – Signs and symptoms may include: • Diarrhea of various types • Nausea and vomiting • Anorexia – Assess for dehydration, hemodynamic instability, and electrolyte imbalance.
Infectious Emergencies Acute Gastroenteritis • Management – Determine the degree of fluid deficit. – Obtain orthostatic vital signs. – Analgesic and antiemetic medications – Teach patients about safe food and water use.
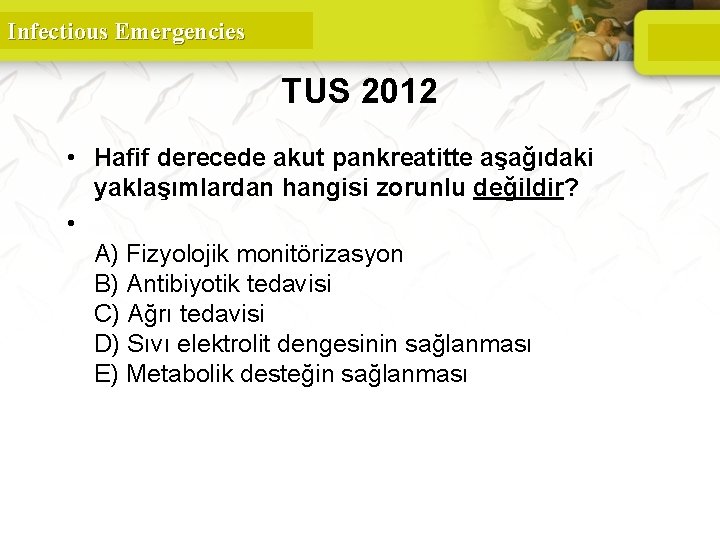
Infectious Emergencies TUS 2012 • Hafif derecede akut pankreatitte aşağıdaki yaklaşımlardan hangisi zorunlu değildir? • A) Fizyolojik monitörizasyon B) Antibiyotik tedavisi C) Ağrı tedavisi D) Sıvı elektrolit dengesinin sağlanması E) Metabolik desteğin sağlanması 139
Infectious Emergencies TUS 2012 • Hafif derecede akut pankreatitte aşağıdaki yaklaşımlardan hangisi zorunlu değildir? • A) Fizyolojik monitörizasyon B) Antibiyotik tedavisi C) Ağrı tedavisi D) Sıvı elektrolit dengesinin sağlanması E) Metabolik desteğin sağlanması 140
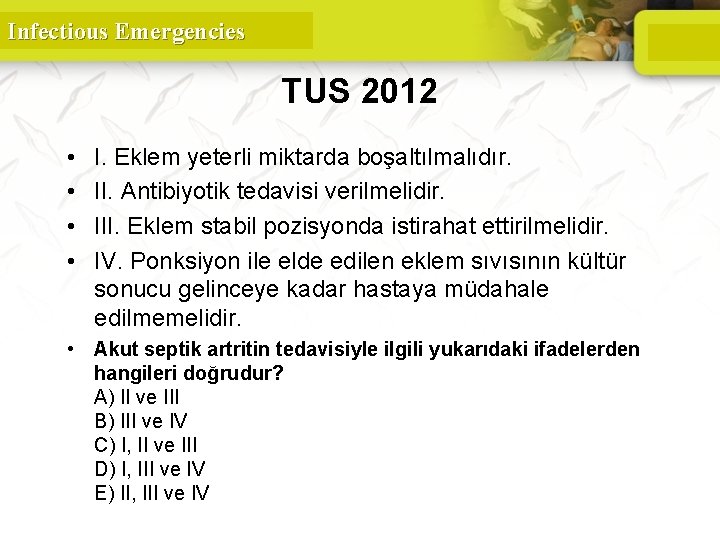
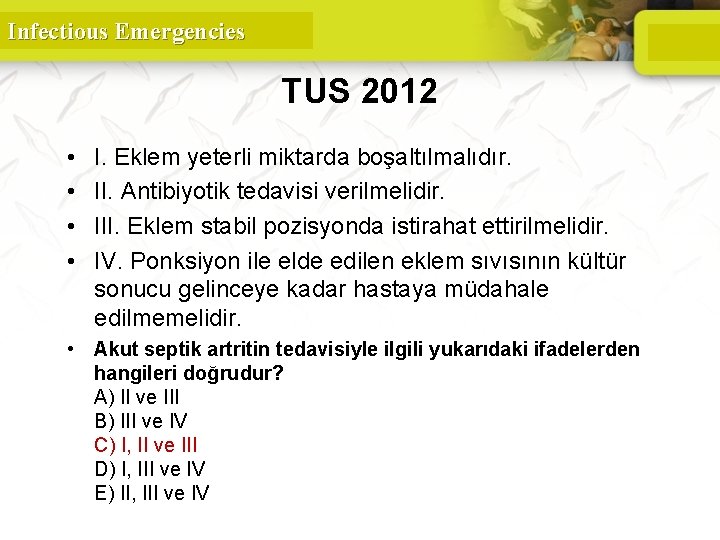
Infectious Emergencies TUS 2012 • • I. Eklem yeterli miktarda boşaltılmalıdır. II. Antibiyotik tedavisi verilmelidir. III. Eklem stabil pozisyonda istirahat ettirilmelidir. IV. Ponksiyon ile elde edilen eklem sıvısının kültür sonucu gelinceye kadar hastaya müdahale edilmemelidir. • Akut septik artritin tedavisiyle ilgili yukarıdaki ifadelerden hangileri doğrudur? A) II ve III B) III ve IV C) I, II ve III D) I, III ve IV E) II, III ve IV 141
Infectious Emergencies TUS 2012 • • I. Eklem yeterli miktarda boşaltılmalıdır. II. Antibiyotik tedavisi verilmelidir. III. Eklem stabil pozisyonda istirahat ettirilmelidir. IV. Ponksiyon ile elde edilen eklem sıvısının kültür sonucu gelinceye kadar hastaya müdahale edilmemelidir. • Akut septik artritin tedavisiyle ilgili yukarıdaki ifadelerden hangileri doğrudur? A) II ve III B) III ve IV C) I, II ve III D) I, III ve IV E) II, III ve IV 142
 Opportunistic infections
Opportunistic infections Methotrexate and yeast infections
Methotrexate and yeast infections Opportunistic infections
Opportunistic infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Cryptosporidiose
Cryptosporidiose Eye infections
Eye infections Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Genital infections
Genital infections Nosocomial infections
Nosocomial infections Classification of acute gingival infections
Classification of acute gingival infections Infectious waste management
Infectious waste management Infectious disease quality controls
Infectious disease quality controls Types of infection
Types of infection Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Stages of infectious disease
Stages of infectious disease Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious disease board review
Infectious disease board review Icd 10 morbus hansen
Icd 10 morbus hansen Smallest infectious agents
Smallest infectious agents Papillomitosis
Papillomitosis Infectious nucleic acid
Infectious nucleic acid University of washington
University of washington Infectious disease
Infectious disease Ebv
Ebv Hennepin county infectious disease manual
Hennepin county infectious disease manual Epidemiological triad
Epidemiological triad Whmis symbols skeleton hand
Whmis symbols skeleton hand Quizlet
Quizlet Infectious stunting syndrome
Infectious stunting syndrome California medical license for foreign medical graduates
California medical license for foreign medical graduates Gbmc infoweb
Gbmc infoweb Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial medical center medical records
Torrance memorial medical center medical records Cartersville medical center medical records
Cartersville medical center medical records I should take a local area orientation dive whenever i
I should take a local area orientation dive whenever i Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Environmental emergencies emt
Environmental emergencies emt Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies Chapter 22 psychiatric emergencies
Chapter 22 psychiatric emergencies Endocrine and hematologic emergencies
Endocrine and hematologic emergencies Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 28 lesson 1
Chapter 28 lesson 1 Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Dic labs
Dic labs Gems diamond geriatric assessment
Gems diamond geriatric assessment Chapter 13 handling emergencies
Chapter 13 handling emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 16 cardiovascular emergencies
Chapter 16 cardiovascular emergencies Psychiatric emergency
Psychiatric emergency Qut security emergency extension number
Qut security emergency extension number Immunologic emergencies
Immunologic emergencies Chapter 17 neurologic emergencies
Chapter 17 neurologic emergencies Alphabetical filing system for medical records
Alphabetical filing system for medical records Egton medical information systems
Egton medical information systems Medical office filing systems
Medical office filing systems Poc informatics
Poc informatics Decision support systems and intelligent systems
Decision support systems and intelligent systems Dicapine
Dicapine Embedded systems vs cyber physical systems
Embedded systems vs cyber physical systems Engineering elegant systems: theory of systems engineering
Engineering elegant systems: theory of systems engineering Wyndham houston - medical center hotel and suites
Wyndham houston - medical center hotel and suites Medical manuscript writing
Medical manuscript writing -in medical term suffix
-in medical term suffix Wootton medical centre
Wootton medical centre Woodlane medical centre doctors
Woodlane medical centre doctors Tifr medical section
Tifr medical section Flat thoracic spine
Flat thoracic spine Patient centered medical home conference
Patient centered medical home conference Queen anne medical electrolysis and laser
Queen anne medical electrolysis and laser Odo 268 swiss medical
Odo 268 swiss medical Chapter 11 medical terminology
Chapter 11 medical terminology Pte med school
Pte med school Ivf maribor
Ivf maribor Eponyms examples
Eponyms examples Umass memorial pharmacy residency
Umass memorial pharmacy residency 同善医院中医部医生
同善医院中医部医生 Tri-tech medical inc.
Tri-tech medical inc. Medical gas master alarm panel
Medical gas master alarm panel Tiu medical analysis
Tiu medical analysis Medical examiner vs coroner
Medical examiner vs coroner Medical terminology skeletal system
Medical terminology skeletal system Integrative medical clinic santa rosa
Integrative medical clinic santa rosa Respiratory sce question bank
Respiratory sce question bank Pomr charting
Pomr charting Pomr medical
Pomr medical Four pillars of medical ethics
Four pillars of medical ethics National board certification for medical interpreters
National board certification for medical interpreters The medical and dental defence union of scotland
The medical and dental defence union of scotland Medial lateral
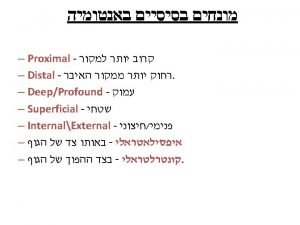
Medial lateral Code crimson in hospital
Code crimson in hospital Lesson 6 medical terminology
Lesson 6 medical terminology Medical terminology lesson 12
Medical terminology lesson 12 Positional asphyxia positions
Positional asphyxia positions Kelty medical practice
Kelty medical practice Royal london medical underwriting limits
Royal london medical underwriting limits Rop medical assisting
Rop medical assisting Makati medical center charity program
Makati medical center charity program Medical records committee functions
Medical records committee functions Medical device software fmea
Medical device software fmea Past medical history
Past medical history Chapter 18 psychological disorders
Chapter 18 psychological disorders Medical hard skills
Medical hard skills Preston medical library
Preston medical library Dvc pensioner tie up hospital
Dvc pensioner tie up hospital Bel retired officers association bangalore
Bel retired officers association bangalore Pakistan veterinary medical council
Pakistan veterinary medical council Signatura prescription
Signatura prescription Ion medical term suffix
Ion medical term suffix Dextro definition
Dextro definition Urethratresia definition
Urethratresia definition Swiss medical art
Swiss medical art Myorrhaphy adalah
Myorrhaphy adalah Pcma
Pcma Nelson medical practice
Nelson medical practice National ambulatory medical care survey
National ambulatory medical care survey Cin number medical
Cin number medical Osce medical
Osce medical Mdo kaiser
Mdo kaiser Axs medical
Axs medical Odsp medical review
Odsp medical review Khan academy medical terminology
Khan academy medical terminology Offshore medical check up
Offshore medical check up Method omop
Method omop Dependent intervention nursing
Dependent intervention nursing Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Prerequisites of gait
Prerequisites of gait Nemt brokers in texas
Nemt brokers in texas New mexico medical insurance pool
New mexico medical insurance pool Njdep medical waste generator registration
Njdep medical waste generator registration Greenhill medical centre
Greenhill medical centre Bmw according to nabh
Bmw according to nabh Sterilization
Sterilization Surgical asepsis hand washing
Surgical asepsis hand washing