Respiratory Emergencies Respiratory Emergencies Interact Respiratory distress Impending









- Slides: 40

Respiratory Emergencies
Respiratory Emergencies Interact! • Respiratory distress / Impending or overt respiratory failure is the most frequent reason for admission in a PICU • Which is the most frequent anatomical abnormality in the respiratory tract causing distress/failure? Airway / Parenchyma / Interstitium / Pleura
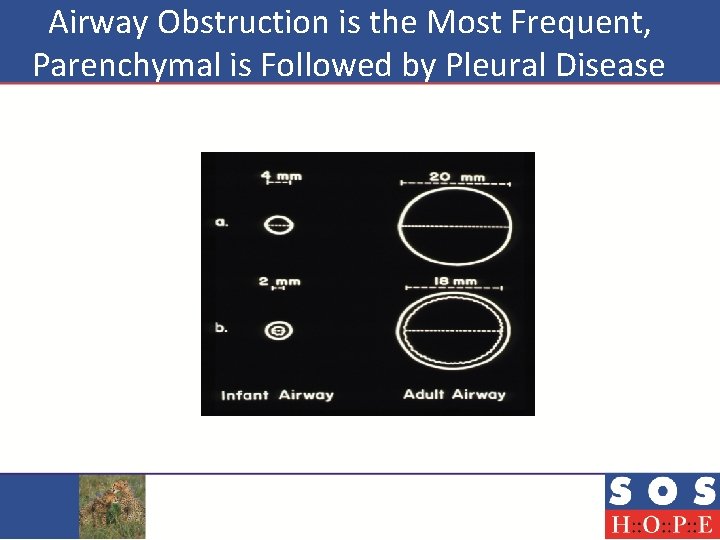
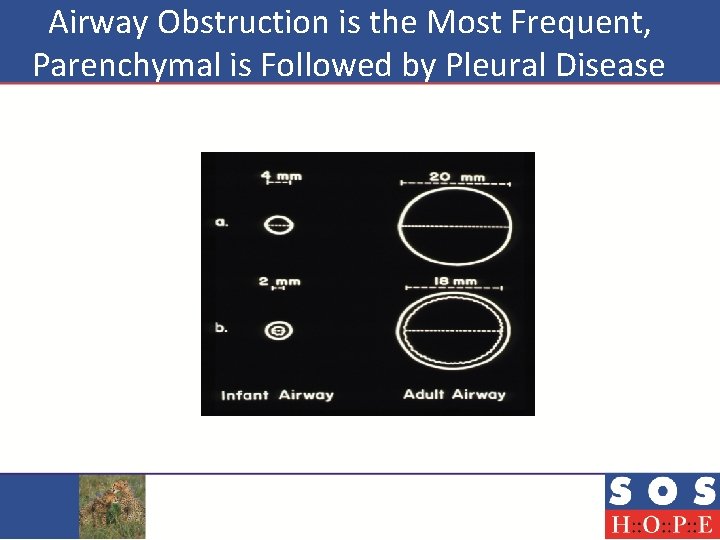
Airway Obstruction is the Most Frequent, Parenchymal is Followed by Pleural Disease
Case 1 • 3 year old boy brought with noisy breathing from 3 days • He has been nebulized for this kind of breathing in the past • He wakes up at night due to this and coughs

Case 1 Interact!
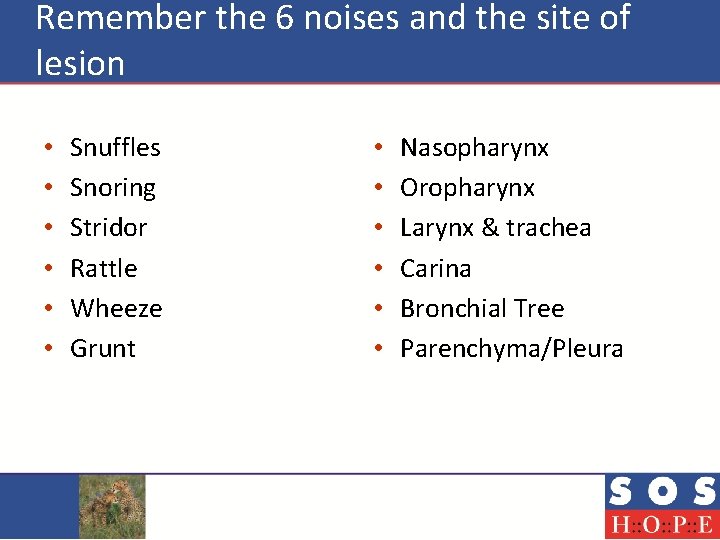
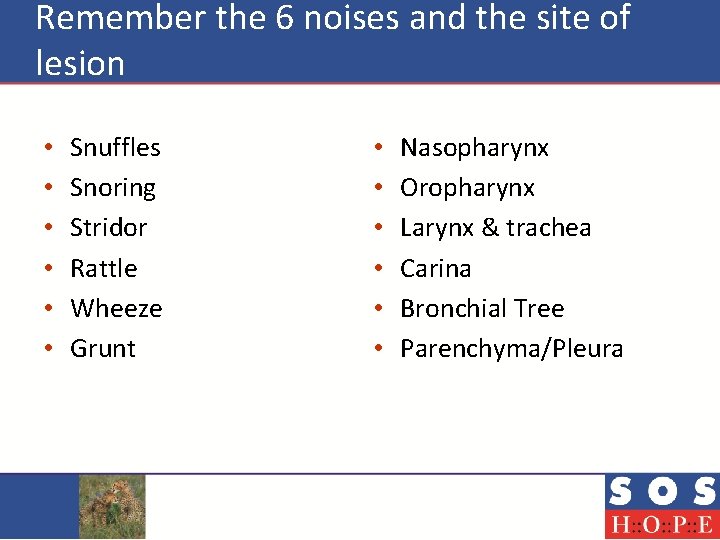
Remember the 6 noises and the site of lesion • • • Snuffles Snoring Stridor Rattle Wheeze Grunt • • • Nasopharynx Oropharynx Larynx & trachea Carina Bronchial Tree Parenchyma/Pleura

Case 2 - 15 month old with noisy breathing Interact!
All these Children have Airway Obstruction • How do you triage such children? • Triage of these children will depend on 1. 2. The severity of obstruction The cause of obstruction which will give clue to the rate of narrowing
Principles of Stabilizing a Child with Airway Obstruction • Keep the child comfortable on the mothers lap • Do not stress the child, throat evaluation should be done only when facilities for providing airway access is available • Supplemental Humidified oxygen in a non threatening way

Croup--When do you call it mild? Looks Fine Barking cough Stridor on crying No accessory muscle use • No tachypnea • Saturations Normal • • • Symptomatic treatment +/- single dose of oral steroids • Parental education on symptoms and signs of worsening even at night
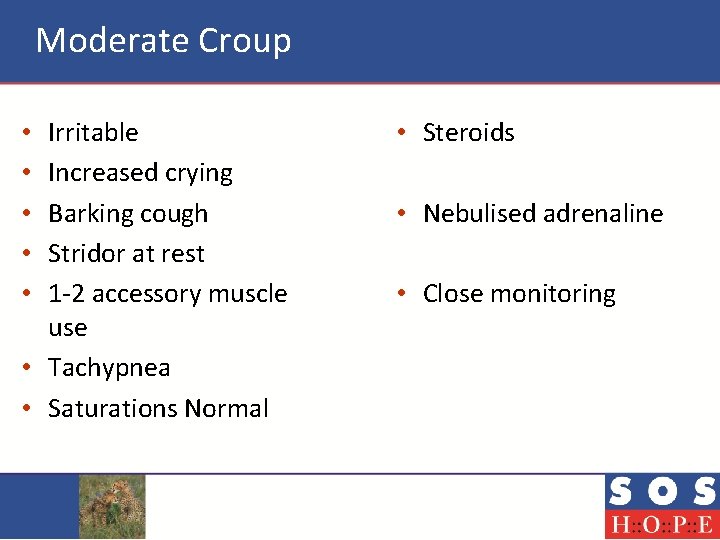
Moderate Croup Irritable Increased crying Barking cough Stridor at rest 1 -2 accessory muscle use • Tachypnea • Saturations Normal • • • Steroids • Nebulised adrenaline • Close monitoring
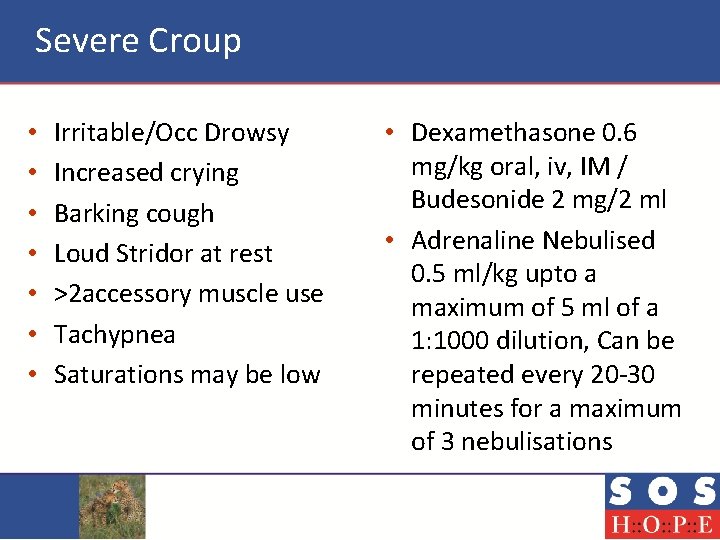
Severe Croup • • Irritable/Occ Drowsy Increased crying Barking cough Loud Stridor at rest >2 accessory muscle use Tachypnea Saturations may be low • Dexamethasone 0. 6 mg/kg oral, iv, IM / Budesonide 2 mg/2 ml • Adrenaline Nebulised 0. 5 ml/kg upto a maximum of 5 ml of a 1: 1000 dilution, Can be repeated every 20 -30 minutes for a maximum of 3 nebulisations
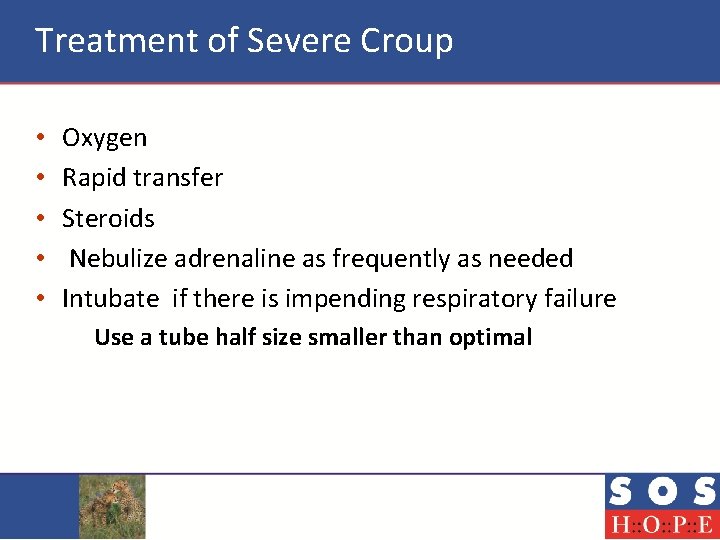
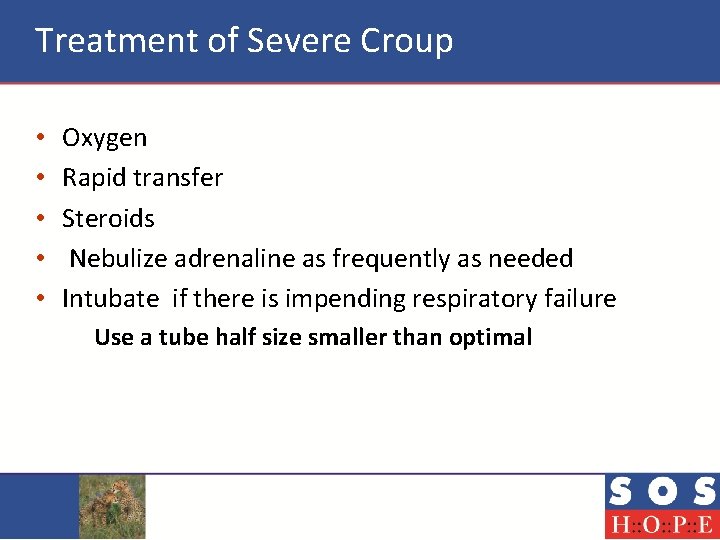
Treatment of Severe Croup • • • Oxygen Rapid transfer Steroids Nebulize adrenaline as frequently as needed Intubate if there is impending respiratory failure Use a tube half size smaller than optimal

Case 3 Interact!
3 Year Old Boy • Acute episode of cough with wheeze • Multiple episodes in the past
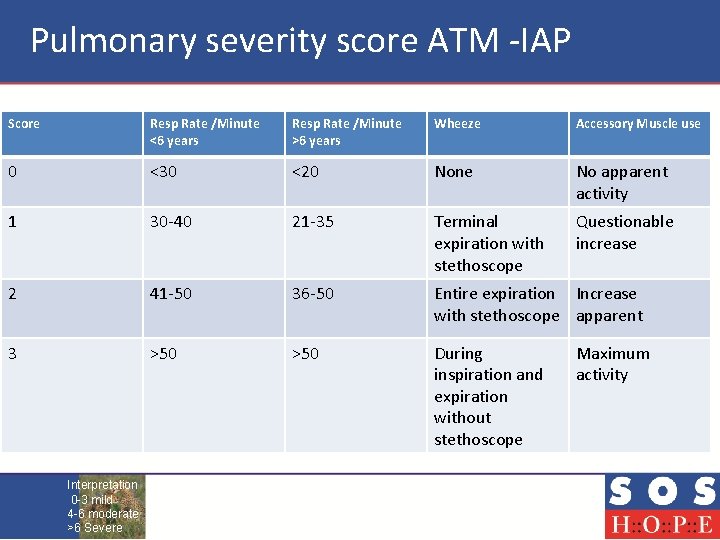
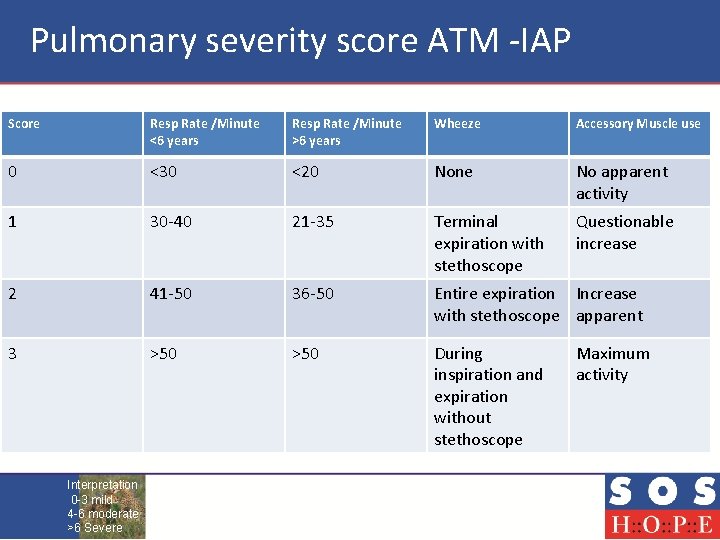
Pulmonary severity score ATM -IAP Score Resp Rate /Minute <6 years Resp Rate /Minute >6 years Wheeze Accessory Muscle use 0 <30 <20 None No apparent activity 1 30 -40 21 -35 Terminal expiration with stethoscope Questionable increase 2 41 -50 36 -50 Entire expiration Increase with stethoscope apparent 3 >50 During inspiration and expiration without stethoscope Interpretation 0 -3 mild 4 -6 moderate >6 Severe Maximum activity
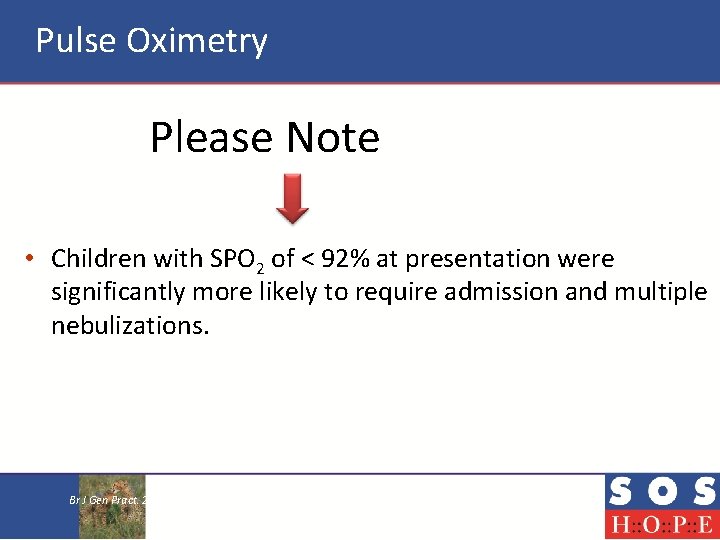
Pulse Oximetry Please Note • Children with SPO 2 of < 92% at presentation were significantly more likely to require admission and multiple nebulizations. Br J Gen Pract. 2005 July 1; 55(516): 501– 502.

How do you Stabilize? Interact! • Aerosol Therapy with MDI with spacer is better than nebulizer in office setting Agree / Disagree ?
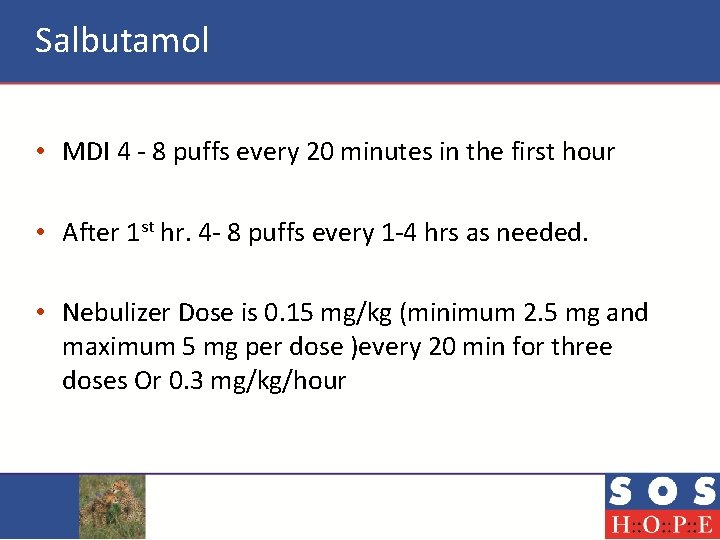
Salbutamol • MDI 4 - 8 puffs every 20 minutes in the first hour • After 1 st hr. 4 - 8 puffs every 1 -4 hrs as needed. • Nebulizer Dose is 0. 15 mg/kg (minimum 2. 5 mg and maximum 5 mg per dose )every 20 min for three doses Or 0. 3 mg/kg/hour
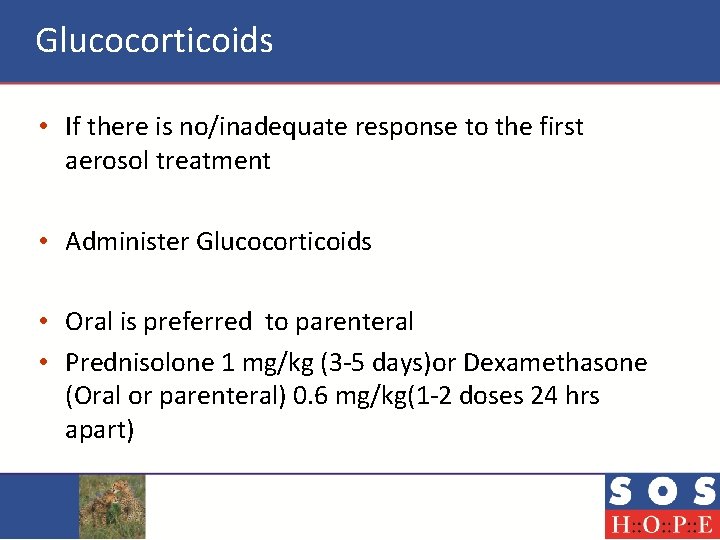
Glucocorticoids • If there is no/inadequate response to the first aerosol treatment • Administer Glucocorticoids • Oral is preferred to parenteral • Prednisolone 1 mg/kg (3 -5 days)or Dexamethasone (Oral or parenteral) 0. 6 mg/kg(1 -2 doses 24 hrs apart)
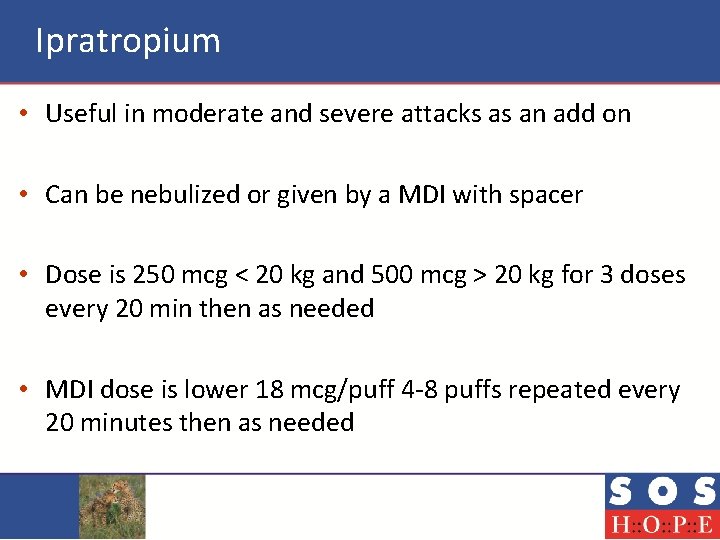
Ipratropium • Useful in moderate and severe attacks as an add on • Can be nebulized or given by a MDI with spacer • Dose is 250 mcg < 20 kg and 500 mcg > 20 kg for 3 doses every 20 min then as needed • MDI dose is lower 18 mcg/puff 4 -8 puffs repeated every 20 minutes then as needed
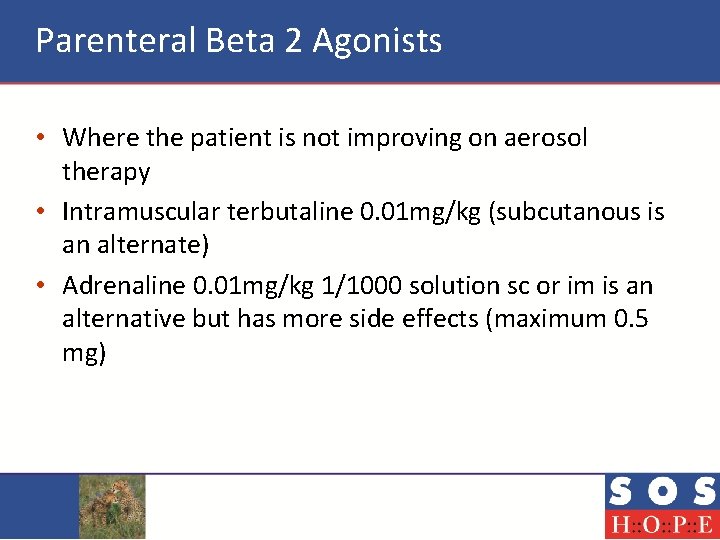
Parenteral Beta 2 Agonists • Where the patient is not improving on aerosol therapy • Intramuscular terbutaline 0. 01 mg/kg (subcutanous is an alternate) • Adrenaline 0. 01 mg/kg 1/1000 solution sc or im is an alternative but has more side effects (maximum 0. 5 mg)
Magnesium Sulphate • In patients who have received salbutamol, ipratropium and glucocorticoids and who are still significantly symptomatic • IV magnesium sulphate 50 mg/kg administered over 20 minutes with cardiorespiratory monitoring
Key Issues in Transport in Severe Exacerbations • • • Oxygen Airway Vascular access Nebulisation/MDI with aerosol Position Communication For Transport details Refer SOS-HOPE APP

Case 4 Interact!
Case 4 • S - an 8 month old infant presented with fever cough and breathlessness of 1 day • On examination he is febrile , toxic resp rate is 65, moderate intercostal and subcostal retractions, has significant grunt, HR is 140/min cap refill is < 2 secs and his saturation is 92%
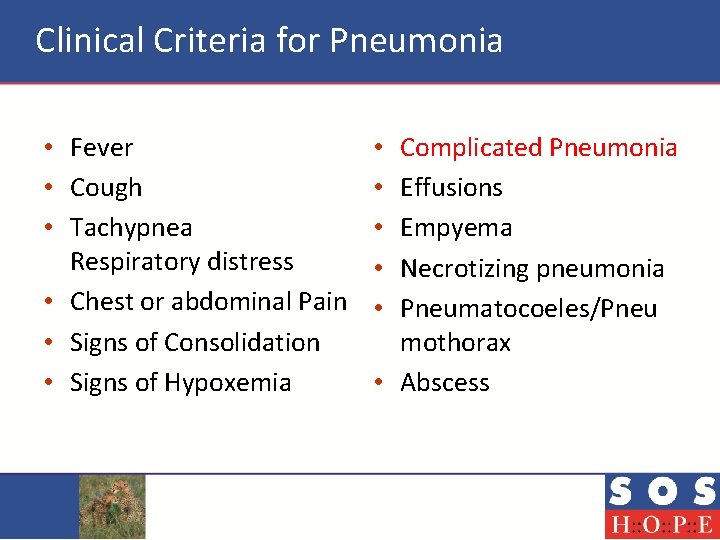
Clinical Criteria for Pneumonia • Fever • Cough • Tachypnea Respiratory distress • Chest or abdominal Pain • Signs of Consolidation • Signs of Hypoxemia Complicated Pneumonia Effusions Empyema Necrotizing pneumonia Pneumatocoeles/Pneu mothorax • Abscess • • •
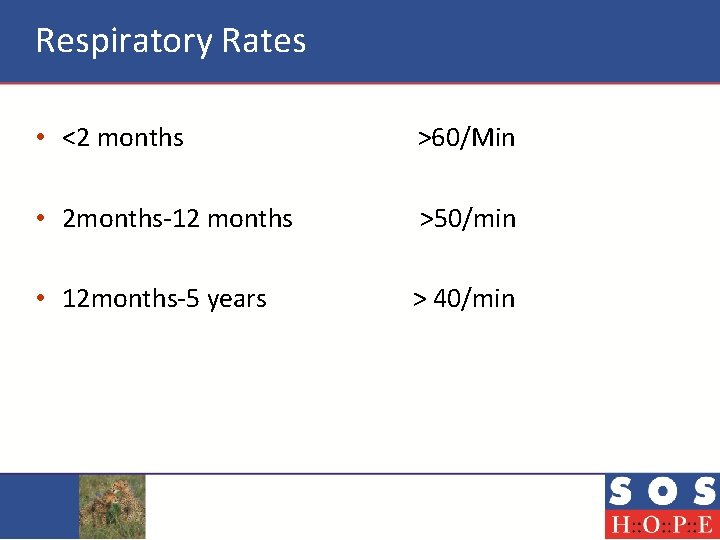
Respiratory Rates • <2 months >60/Min • 2 months-12 months >50/min • 12 months-5 years > 40/min
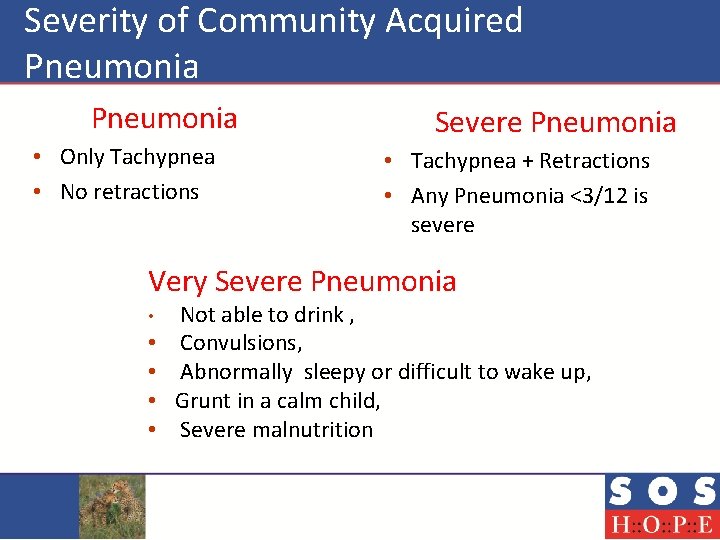
Severity of Community Acquired Pneumonia Severe Pneumonia • Only Tachypnea • No retractions • Tachypnea + Retractions • Any Pneumonia <3/12 is severe Very Severe Pneumonia • • • Not able to drink , Convulsions, Abnormally sleepy or difficult to wake up, Grunt in a calm child, Severe malnutrition
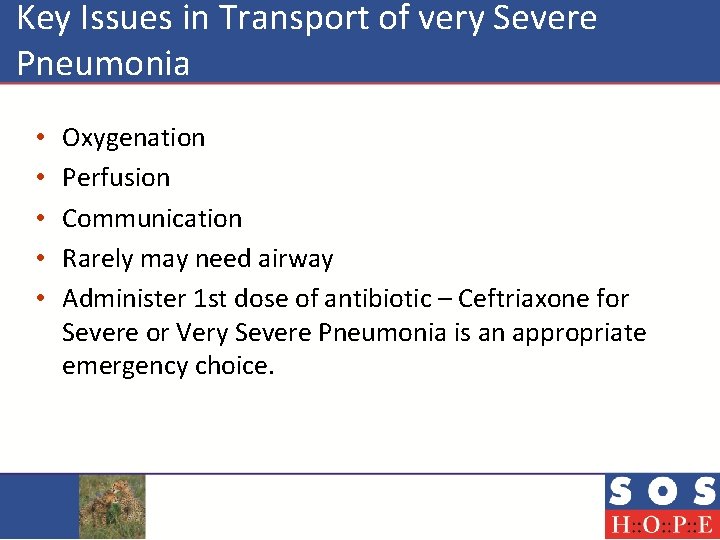
Key Issues in Transport of very Severe Pneumonia • • • Oxygenation Perfusion Communication Rarely may need airway Administer 1 st dose of antibiotic – Ceftriaxone for Severe or Very Severe Pneumonia is an appropriate emergency choice.
Case 5 Interact!
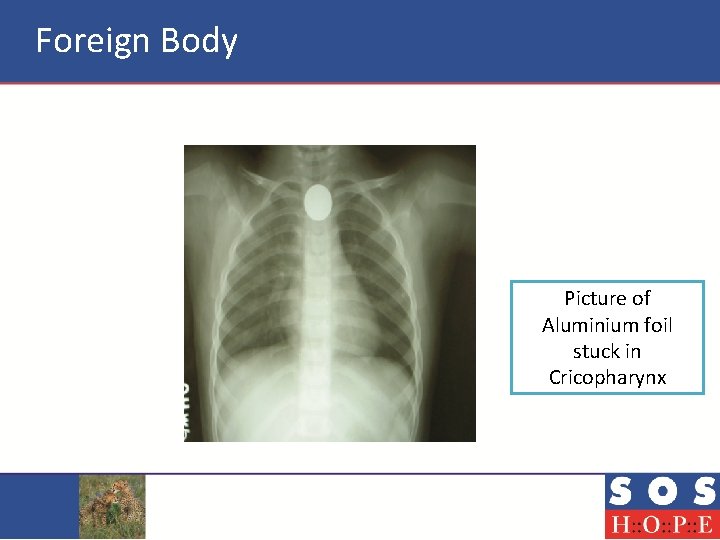
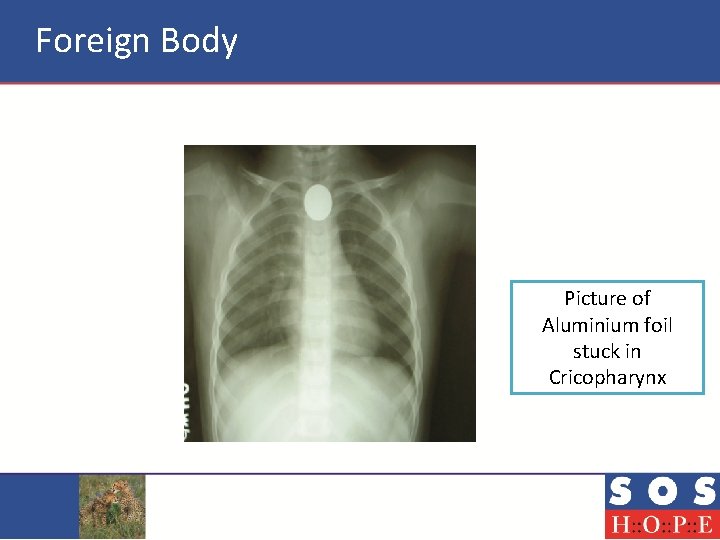
Foreign Body Picture of Aluminium foil stuck in Cricopharynx
Foreign Body • • Suspect choking caused by a foreign body if : The onset was very sudden There are no other signs of illness There are clues to alert the rescuer, for example a history of eating or playing with small items immediately prior to the onset of symptoms
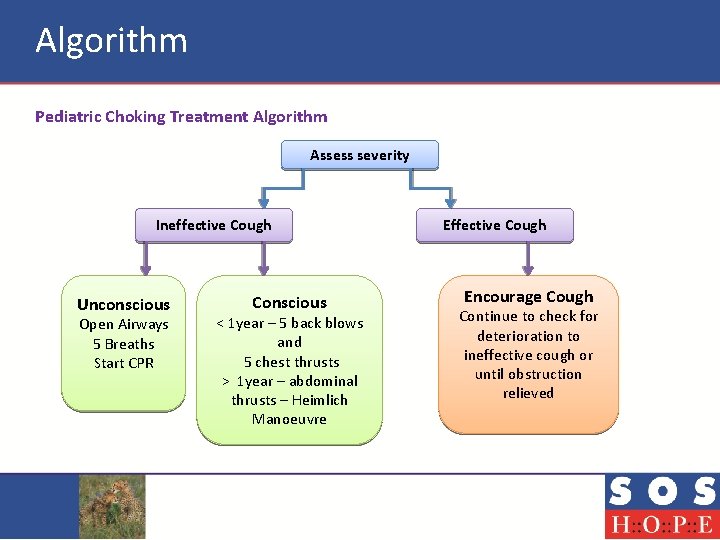
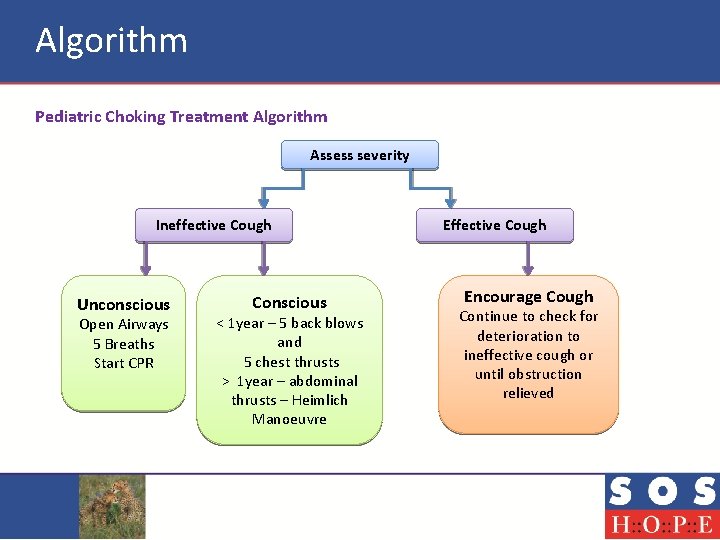
Algorithm Pediatric Choking Treatment Algorithm Assess severity Ineffective Cough Unconscious Open Airways 5 Breaths Start CPR Conscious < 1 year – 5 back blows and 5 chest thrusts > 1 year – abdominal thrusts – Heimlich Manoeuvre Effective Cough Encourage Cough Continue to check for deterioration to ineffective cough or until obstruction relieved
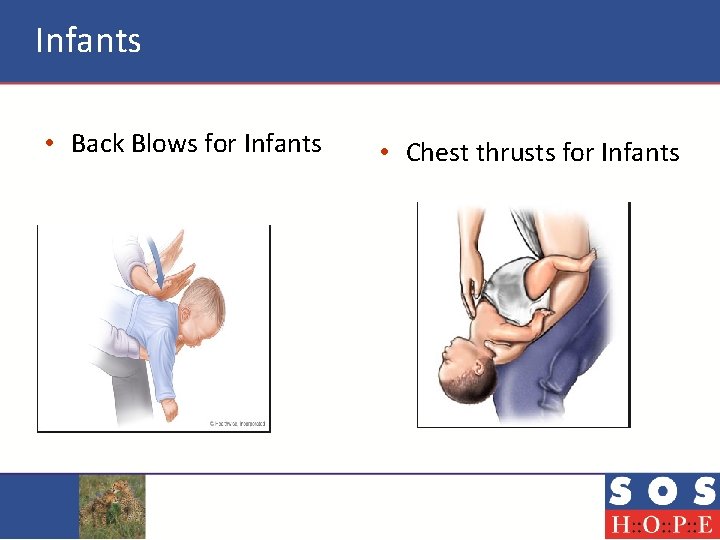
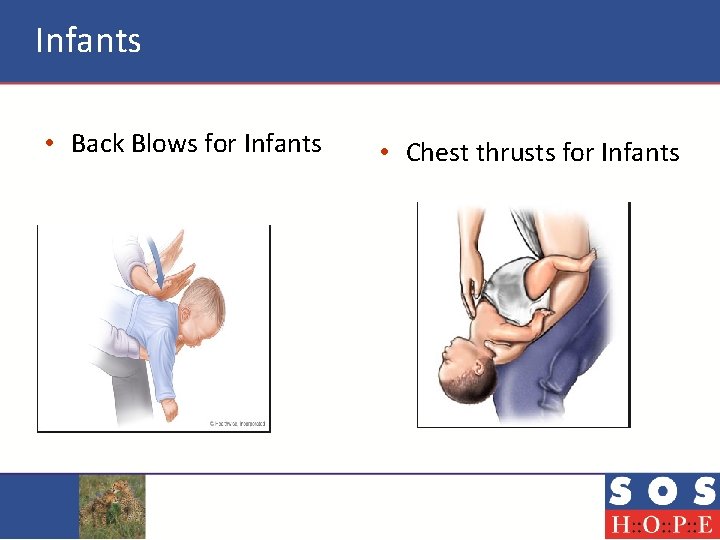
Infants • Back Blows for Infants • Chest thrusts for Infants

Heimlich Manoeuvre
Summary • Clinical evaluation should be with a focused history and clinical examination • Carefully count the respiratory rate for 1 minute, watch for breathing, respiratory sounds, and examine the chest • Measure the oxygen saturation, always have a pulse oximeter • Stabilise all patients with oxygen, airway and ensure they are breathing adequately
Summary • Keep a watch for subtle signs of hypoxia and deterioration • Make arrangements to shift optimally • Keep your office adequately stocked everyday, make sure the equipment is well maintained • Staff should be trained in triage, communication, maintaining equipment and medication and helping in an emergency

Your Opinion
 Respiratory distress
Respiratory distress Respiratory distress
Respiratory distress Respiratory distress nasal flaring
Respiratory distress nasal flaring Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Impending danger examples
Impending danger examples The impending crisis apush
The impending crisis apush Looming impending
Looming impending What is the conducting zone of the respiratory system
What is the conducting zone of the respiratory system Organizing students to interact with content
Organizing students to interact with content Competitive interaction
Competitive interaction Sergeant at arms in rotaract
Sergeant at arms in rotaract Humans built a dam out of rock materials
Humans built a dam out of rock materials Interact
Interact Teachstone class video library
Teachstone class video library How do similar (s-s or n-n) magnetic poles interact?
How do similar (s-s or n-n) magnetic poles interact? Example of coevolution
Example of coevolution Answer
Answer Tectonic plates interact at places called plate
Tectonic plates interact at places called plate Interact
Interact Oblate sheroid
Oblate sheroid Kesler science
Kesler science Raised by wolves
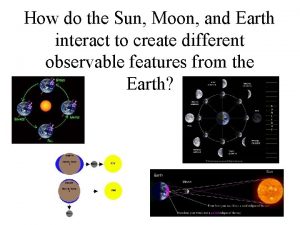
Raised by wolves How do the sun moon and earth interact
How do the sun moon and earth interact Action elements of dance
Action elements of dance Interact club handbook
Interact club handbook Body interact answers
Body interact answers How does biosphere interact with hydrosphere
How does biosphere interact with hydrosphere Interact
Interact Regularly and consciously interact with one another
Regularly and consciously interact with one another Why do magnets repel
Why do magnets repel How does biosphere interact with hydrosphere
How does biosphere interact with hydrosphere Interact
Interact Mm proposition ii with taxes
Mm proposition ii with taxes Willing hands dbt
Willing hands dbt Modified sims position for prolapsed cord
Modified sims position for prolapsed cord Paragraph about stress
Paragraph about stress Moral distress and burnout
Moral distress and burnout Konsep spiritual dalam keperawatan
Konsep spiritual dalam keperawatan Definisi psikologi klinis
Definisi psikologi klinis Damsel in distress archetype definition
Damsel in distress archetype definition