Chapter 17 Neurologic Emergencies Introduction 1 of 3


































- Slides: 96
Chapter 17 Neurologic Emergencies
Introduction (1 of 3) • Stroke is the fifth-leading cause of death and the leading cause of adult disability in the United States. • Common in geriatric patients.
Introduction (2 of 3) • Contributing factors for stroke. • New treatments are available for stroke patients.

Introduction (3 of 3) • Seizures and altered mental status are other common neurological emergencies.

Anatomy and Physiology (1 of 5) • The brain is the body’s computer. • Controls breathing, speech, and all other body functions • Three major parts: brain stem, cerebellum, and cerebrum – Cerebrum is the largest part.

Anatomy and Physiology (2 of 5) © Jones & Bartlett Learning.

Anatomy and Physiology (3 of 5) • The brain stem controls the most basic functions. • The cerebellum controls muscle and body coordination.
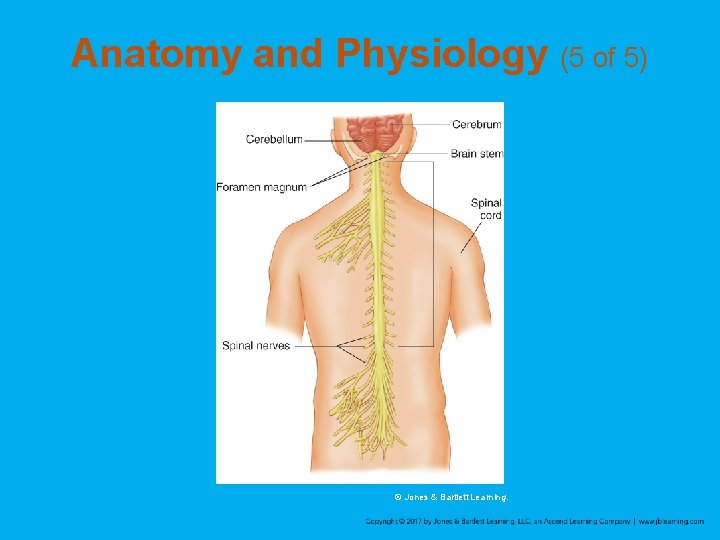
Anatomy and Physiology (4 of 5) • Messages sent to and from the brain travel through nerves. – Twelve cranial nerves – Spinal nerves
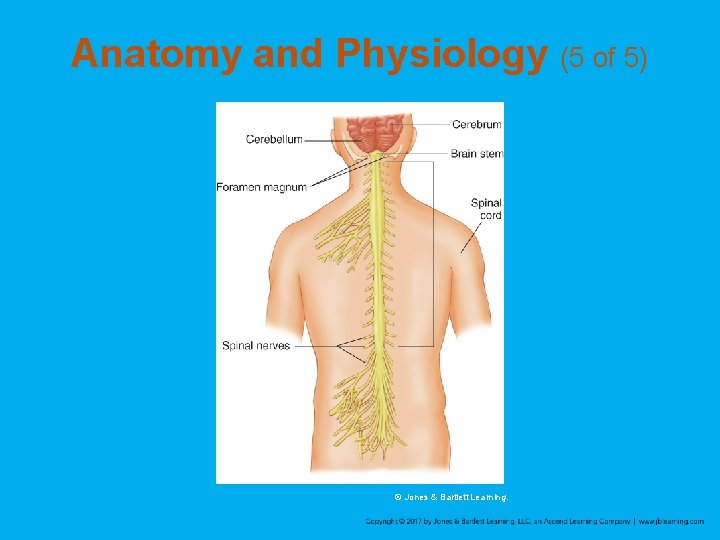
Anatomy and Physiology (5 of 5) © Jones & Bartlett Learning.
Pathophysiology • Many different disorders can cause brain dysfunction. – Can affect the patient’s level of consciousness, speech, and voluntary muscle control • The brain is sensitive to changes in oxygen, glucose, and temperature. – Significant change in any one of these levels will result in a neurologic change
Headache (1 of 5) • One of the most common complaints • Can be a symptom of another condition or a neurologic condition on its own • Only a small percentage of headaches are caused by a serious medical condition.

Headache (2 of 5) • Tension headaches – Caused by muscle contractions in the head and neck – Attributed to stress – Pain is usually described as squeezing, dull, or as an ache. – Usually do not require medical attention

Headache (3 of 5) • Migraine headaches – Thought to be caused by changes in the blood vessel size in the base of the brain. – Pain is usually described as pounding, throbbing, and pulsating. – Often associated with nausea and vomiting and may be preceded by visual changes. – Can last for several hours or days.
Headache (4 of 5) • Sinus headaches – Caused by pressure that results from accumulated fluid in the sinuses
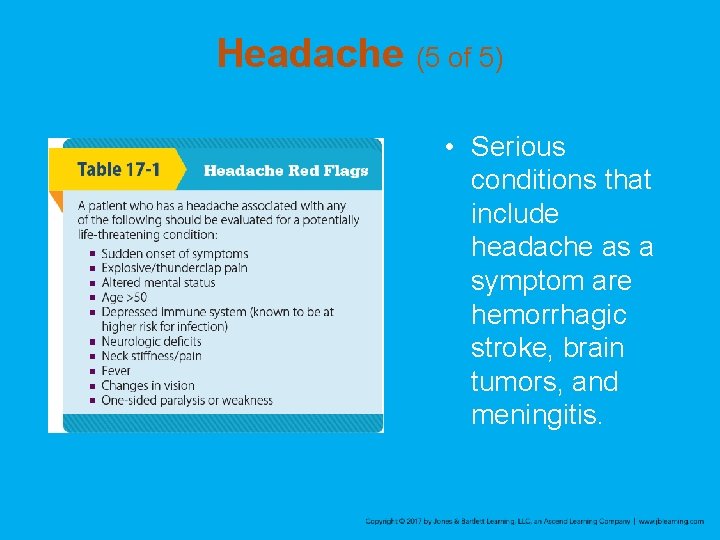
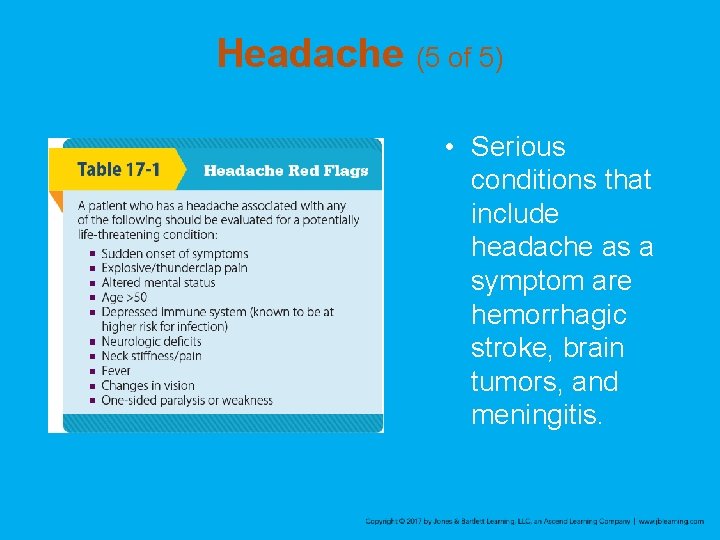
Headache (5 of 5) • Serious conditions that include headache as a symptom are hemorrhagic stroke, brain tumors, and meningitis.
Stroke • Also called a cerebrovascular accident (CVA) • Interruption of blood flow to an area within the brain • Results in the loss of brain function
Ischemic Stroke (1 of 2) • Most common, accounting for more than 80% of strokes • Results from thrombosis or an embolus • Symptoms may range from nothing at all to complete paralysis. • Atherosclerosis in the blood vessels is often the cause.

Ischemic Stroke (2 of 2) © Jones & Bartlett Learning.
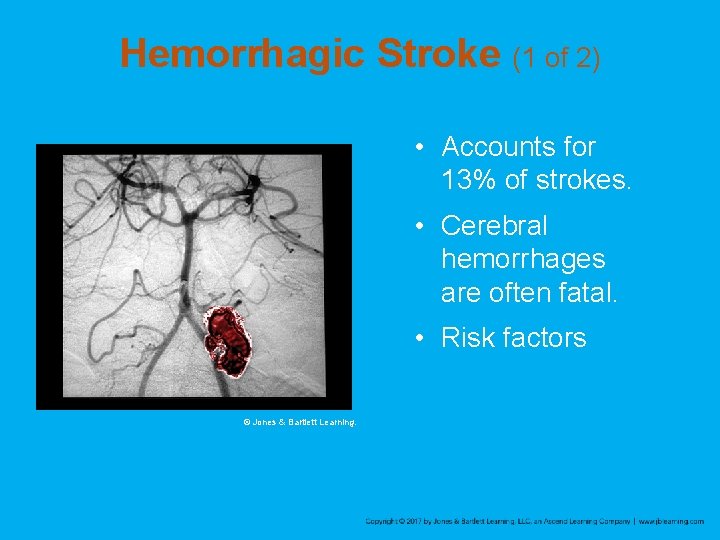
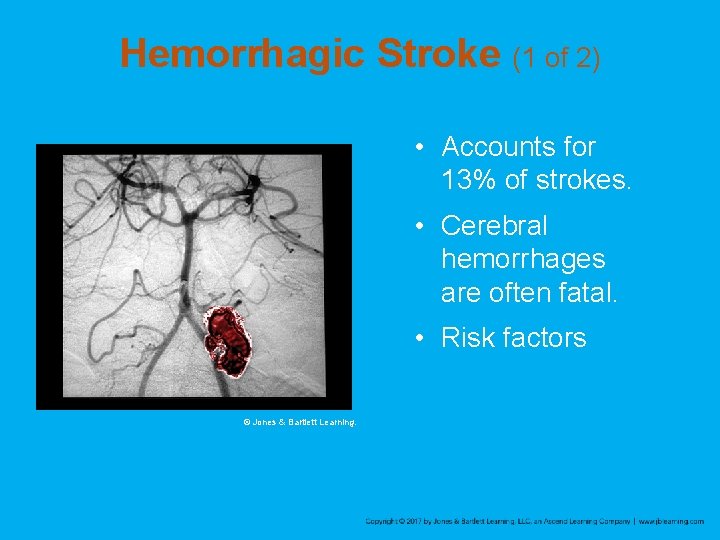
Hemorrhagic Stroke (1 of 2) • Accounts for 13% of strokes. • Cerebral hemorrhages are often fatal. • Risk factors © Jones & Bartlett Learning.
Hemorrhagic Stroke (2 of 2) • Berry aneurysms are a common cause of hemorrhagic strokes in healthy, young people. – Presents as the “worst headache of their life” – Causes a subarachnoid hemorrhage
Transient Ischemic Attack (TIA) • When stroke-like symptoms go away on their own in less than 24 hours, the event is called a TIA. • May be a warning sign of a larger stroke to come and is considered an emergency – About one third of patients who have a TIA will experience a stroke soon after. – All patients with a TIA should be evaluated by a physician.
Signs and Symptoms of Stroke (1 of 3) • Facial drooping • Sudden weakness or numbness in the face, arm, leg, or one side of body • Decreased or absent movement and sensation on one side of the body • Lack of muscle coordination (ataxia) or loss of balance • Sudden vision loss in one eye, blurred or double vision

Signs and Symptoms of Stroke (2 of 3) • Difficulty swallowing • Decreased level of responsiveness • Speech disorders • Difficulty expressing thoughts or inability to use the right words • Slurred speech (dysarthria) • Sudden and severe headache
Signs and Symptoms of Stroke (3 of 3) • Confusion • Dizziness • Weakness • Combativeness • Restlessness • Tongue deviation • Coma
Left Hemisphere • Stroke in the left cerebral hemisphere may cause aphasia. – Inability to produce or understand speech • Strokes that affect the left side of the brain can also cause paralysis of the right side of the body.

Right Hemisphere • Strokes that affect the right side of the brain cause paralysis of the left side of the body. • Patients can understand language and speak, but their words may be slurred. • Patients may be oblivious to their problem (neglect). • Patients with a problem affecting the back part of the cerebrum may neglect certain parts of their vision. • Neglect and lack of pain cause many patients to delay seeking help.
Bleeding in the Brain • Patients may have high blood pressure. – May be the cause of the bleeding. – May be caused by the bleeding, as a compensatory response. • A trend of an increasing blood pressure is an important sign. • Significant drops may occur as the patient’s condition worsens.
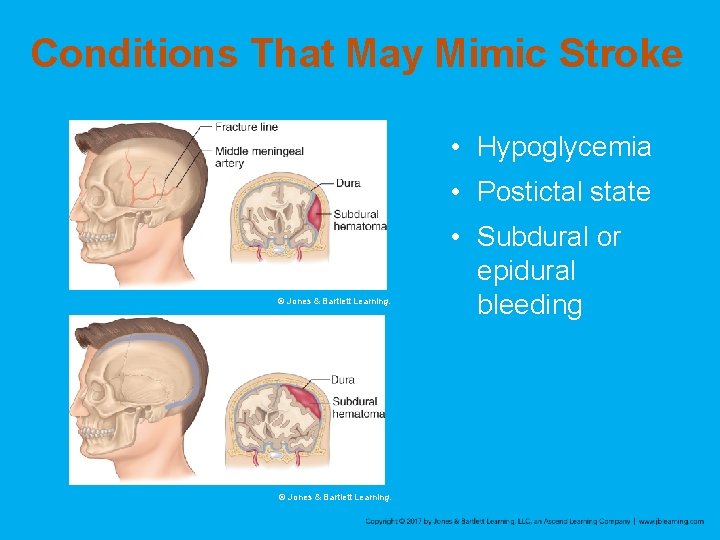
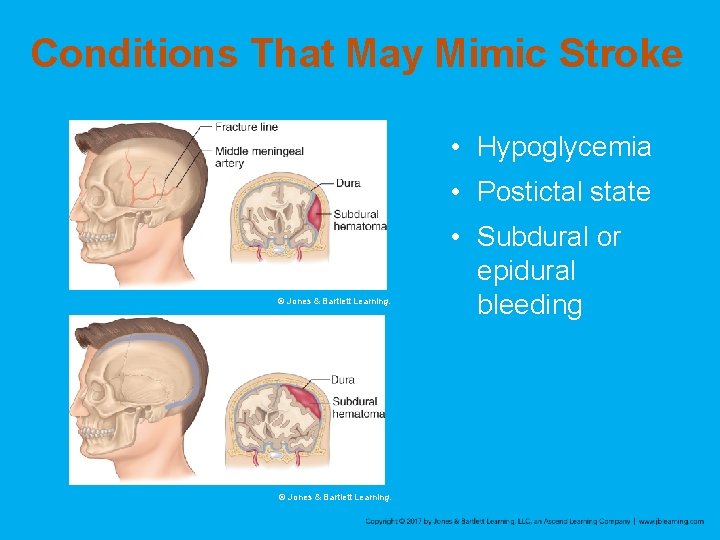
Conditions That May Mimic Stroke • Hypoglycemia • Postictal state © Jones & Bartlett Learning. • Subdural or epidural bleeding

Seizures • A seizure is a neurologic episode caused by a surge of electrical activity in the brain. • In the United States, it is estimated that 2 to 3 million people have epilepsy.
Generalized (Tonic-Clonic) Seizure • Results from abnormal electrical discharges from large areas of the brain. – Usually involves both hemispheres • Characterized by unconsciousness and a generalized, severe twitching of all muscles. – Lasts several minutes or longer
Absence Seizure • Does not involve any changes in motor activity. • Characterized by a brief lapse of consciousness in which the patient seems to stare and not respond.

Partial (Focal) Seizure (1 of 2) • Simple partial seizure – No change in the patient’s level of consciousness – May have numbness, weakness, dizziness, visual changes, or unusual smells and tastes – May cause some twitching or brief paralysis
Partial (Focal) Seizure (2 of 2) • Complex partial seizure – Altered mental status – Results from abnormal discharges from the temporal lobe of the brain – Characterized by lip smacking, eye blinking, isolated jerking – Patients also may experience unpleasant smells or visual hallucinations, exhibit uncontrolled fear, or perform repetitive physical behavior.
Aura • Patients may experience an aura prior to a seizure.

Generalized Seizure (1 of 2) • Characterized by sudden loss of consciousness, chaotic muscle movement and tone, and apnea • Most seizures last 3 to 5 minutes. • Followed by a postictal state
Absence Seizure • Formerly called petit mal • Last for seconds • Patient fully recovers with a brief lapse of memory of the event.
Status Epilepticus • Seizures that continue every few minutes without the person regaining consciousness or last longer than 30 minutes.
Causes of Seizures (1 of 2) • Congenital • Structural • Metabolic • Febrile • Epileptic seizures usually can be controlled with medications

Causes of Seizures (2 of 2) © Jones & Bartlett Learning.
The Importance of Recognizing Seizures • Recognize when a seizure is occurring and whether this episode differs from previous ones. • Identify other problems associated with the seizure.

The Postictal State • Following the seizure, a patient’s muscles relax and the breathing becomes labored. • Patients may present with hemiparesis, lethargy, or confusion. • If the patient’s condition does not improve, consider other problems such as infection or hypoglycemia.
Syncope • Seizures are often mistaken for syncope. – Differences between seizures and syncope
Altered Mental Status • Aside from stroke and seizures, the most common neurologic emergency • Common causes
Causes of AMS (1 of 2) • Hypoglycemia – Patients can have signs and symptoms that mimic stroke and seizures. • Delirium – A symptom, not a disease – Presents as a new complaint – Temporary state often with a physical or mental cause – Can be reversed with proper treatment – Signs and symptoms
Causes of AMS (2 of 2) • Other causes of AMS – Unrecognized head injury – Severe intoxication – Psychological disorders – Medication complications – Infections, particularly those involving the brain or bloodstream

Patient Assessment (1 of 7) • Scene size-up • Primary assessment – All patients with an altered mental status should receive high-flow oxygen. – Hyperventilation may have several negative consequences. • History taking
Patient Assessment (2 of 7) • Secondary assessment – Vital signs – Patients with intracranial bleeding may have increased pressure compressing the brain. – Can slow the pulse and cause erratic respirations – Blood pressure is usually high. – Changes in pupil size and reactivity indicate significant bleeding and pressure on the brain. – Check blood glucose levels.
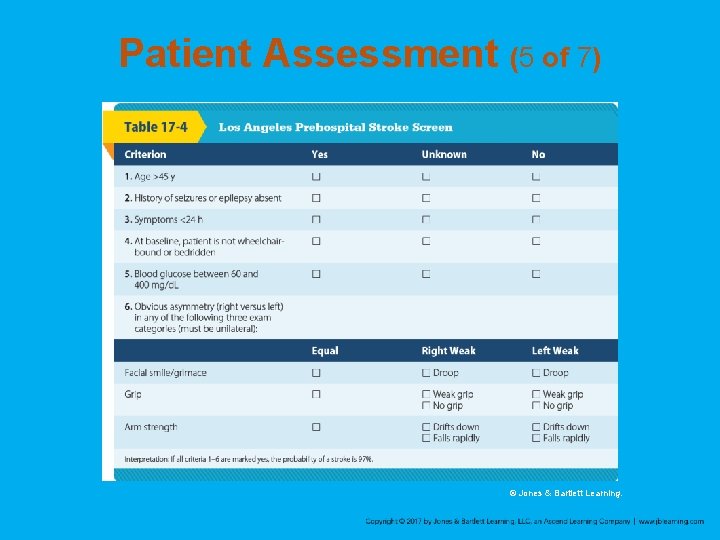
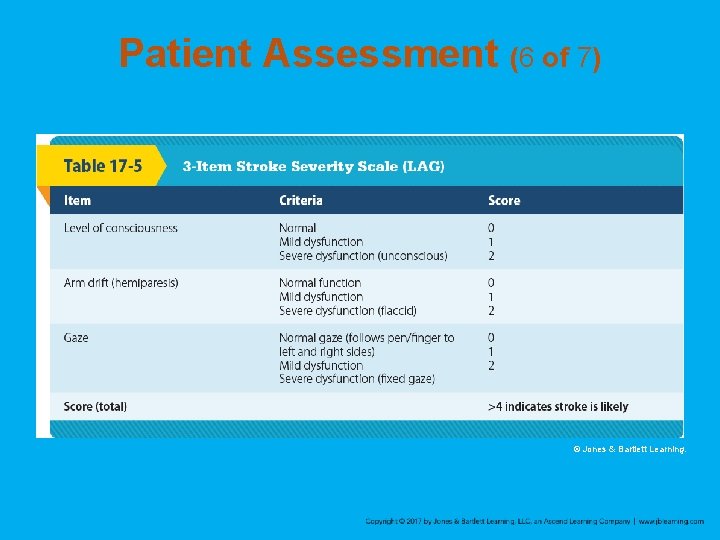
Patient Assessment (3 of 7) • Secondary assessment (cont’d) – Stroke Assessment • • • Cincinnati Prehospital Stroke Scale Los Angeles Prehospital Stroke Screen 3 -Item Stroke Severity Scale (LAG) FAST mnemonic Glasgow Coma Scale (GCS) score • Reassessment

Patient Assessment (4 of 7) © Jones & Bartlett Learning.
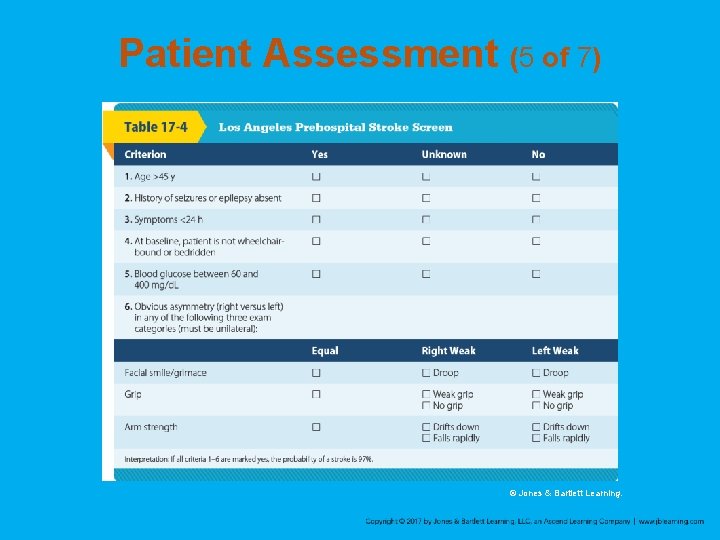
Patient Assessment (5 of 7) © Jones & Bartlett Learning.
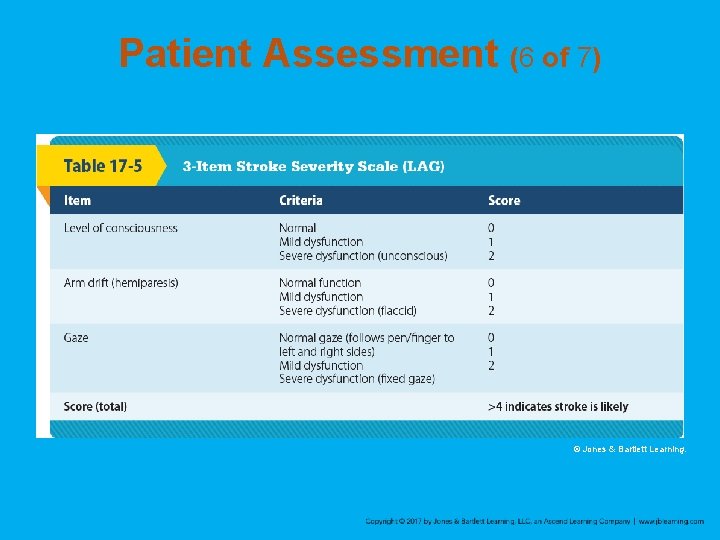
Patient Assessment (6 of 7) © Jones & Bartlett Learning.

Patient Assessment (7 of 7) © Jones & Bartlett Learning.

Emergency Medical Care: General (1 of 2) • For suspected stroke patients, physicians in the ED need to determine whethere is bleeding in the brain. • Notify the hospital regarding the last time the patient was known to be without their current signs and symptoms of stroke.

Emergency Medical Care: General (2 of 2) • Patients who have had a seizure require definitive evaluation and treatment in the hospital. • Patients having a seizure: – – Protect them from harm. Maintain a clear airway by suctioning. Provide oxygen as quickly as possible. If head or neck trauma is suspected, provide spinal immobilization.

Emergency Medical Care: Headache • You should be concerned if the patient complains of: – A sudden-onset, severe headache – A sudden headache with fever, seizures, AMS, or following trauma • Migraine
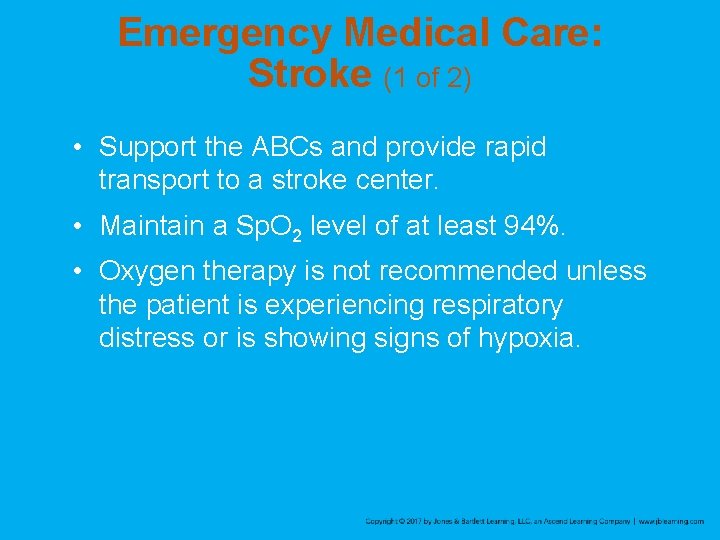
Emergency Medical Care: Stroke (1 of 2) • Support the ABCs and provide rapid transport to a stroke center. • Maintain a Sp. O 2 level of at least 94%. • Oxygen therapy is not recommended unless the patient is experiencing respiratory distress or is showing signs of hypoxia.
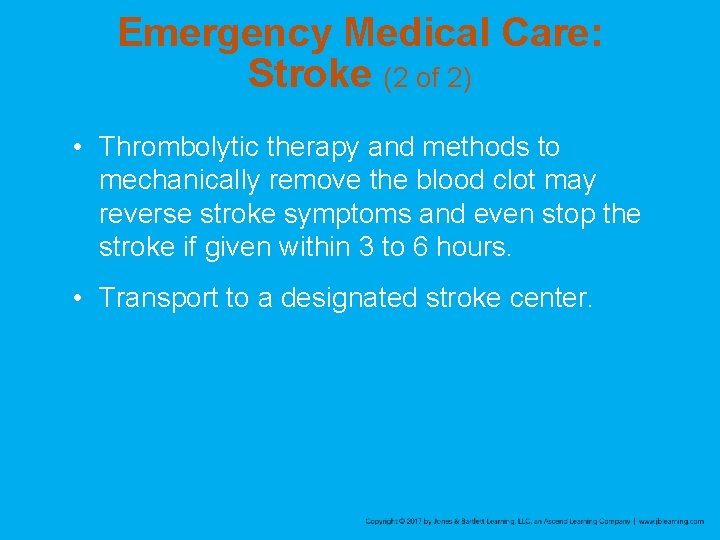
Emergency Medical Care: Stroke (2 of 2) • Thrombolytic therapy and methods to mechanically remove the blood clot may reverse stroke symptoms and even stop the stroke if given within 3 to 6 hours. • Transport to a designated stroke center.

Emergency Medical Care: Seizure and AMS • The patient may be in a postictal state on your arrival. • Care for patients actively seizing. • Altered mental status
Review 1. A 41 -year-old man presents with slow, irregular breathing; hypotension; and dilated pupils. These signs MOST likely indicate dysfunction of the: A. brain stem. B. hypothalamus. C. cerebrum. D. cerebellum.
Review Answer: A Rationale: The brain stem is responsible for functions such as breathing, blood pressure, and pupil constriction. Brain stem dysfunction would result in abnormal findings with these functions.

Review (1 of 2) 1. A 41 -year-old man presents with slow, irregular breathing; hypotension; and dilated pupils. These signs MOST likely indicate dysfunction of the: A. brain stem. Rationale: Correct answer B. hypothalamus. Rationale: The hypothalamus causes changes to occur in the heart rate, body temperature, and thirst.
Review (2 of 2) 1. A 41 -year-old man presents with slow, irregular breathing; hypotension; and dilated pupils. These signs MOST likely indicate dysfunction of the: C. cerebrum. Rationale: The cerebrum causes changes to occur in emotion, thought, touch, and movement. D. cerebellum. Rationale: The cerebellum causes changes to occur in muscle control, body coordination, standing, walking, and writing.
Review 2. An acute ischemic stroke is caused by: A. a ruptured cerebral artery. B. increased intracranial pressure. C. an acute rise in a person’s blood pressure. D. a blocked cerebral artery.

Review Answer: D Rationale: There are two types of stroke— hemorrhagic and ischemic. A hemorrhagic stroke is caused by a ruptured cerebral artery (aneurysm), which causes bleeding within the brain and increased intracranial pressure. An ischemic stroke is caused by a blocked cerebral artery—either from a clot that grows locally (thrombus) or that travels to the brain from another part of the body (embolus).
Review (1 of 2) 2. An acute ischemic stroke is caused by: A. a ruptured cerebral artery. Rationale: This is known as a hemorrhagic stroke. B. increased intracranial pressure. Rationale: This can be caused by swelling, bleeding, or tumors.
Review (2 of 2) 2. An acute ischemic stroke is caused by: C. an acute rise in a person’s blood pressure. Rationale: This is known as a hypertensive crisis. D. a blocked cerebral artery. Rationale: Correct answer
Review 3. A 56 -year-old man experienced a sudden, severe headache and then became unresponsive. He has a history of high blood pressure. The MOST likely cause of his condition is a(n): A. hemorrhagic stroke. B. acute ischemic stroke. C. severe migraine headache. D. transient ischemic attack.
Review Answer: A Rationale: Hemorrhagic strokes are typically preceded by a sudden, severe headache (signals the rupture of a cerebral artery), after which the patient becomes unresponsive due to bleeding within the brain. Ischemic strokes and transient ischemic attacks generally do not cause a sudden, severe headache, and migraine headaches typically do not cause a loss of consciousness.

Review (1 of 2) 3. A 56 -year-old man experienced a sudden, severe headache and then became unresponsive. He has a history of high blood pressure. The MOST likely cause of his condition is a(n): A. hemorrhagic stroke. Rationale: Correct answer B. acute ischemic stroke. Rationale: This generally does not cause a sudden, severe headache.

Review (2 of 2) 3. A 56 -year-old man experienced a sudden, severe headache and then became unresponsive. He has a history of high blood pressure. The MOST likely cause of his condition is a(n): C. severe migraine headache. Rationale: This generally does not cause a loss of consciousness. D. transient ischemic attack. Rationale: This generally does not cause a sudden, severe headache.
Review 4. Unlike an ischemic stroke, a transient ischemic attack is characterized by all of the following, EXCEPT: A. symptoms that resolve within 24 hours. B. symptoms that persist for longer than 24 hours. C. weakness or paralysis to one side of the body. D. an acute onset of confusion and slurred speech.
Review Answer: B Rationale: Signs and symptoms of a transient ischemic attack (TIA) are usually identical to those of an acute ischemic stroke (eg, hemiparesis, slurred speech, confusion, facial droop). Unlike the ischemic stroke, however, the symptoms of a TIA usually resolve within 24 hours.

Review (1 of 2) 4. Unlike an ischemic stroke, a transient ischemic attack is characterized by all of the following EXCEPT: A. symptoms that resolve within 24 hours. Rationale: This is a sign of a transient ischemic attack. B. symptoms that persist for longer than 24 hours. Rationale: Correct answer
Review (2 of 2) 4. Unlike an ischemic stroke, a transient ischemic attack is characterized by all of the following EXCEPT: C. weakness or paralysis to one side of the body. Rationale: This is a sign of a transient ischemic attack. D. an acute onset of confusion and slurred speech. Rationale: This is a sign of a transient ischemic attack.
Review 5. A patient with a suspected stroke presents with slurred speech that is difficult for you to understand. This is referred to as: A. aphasia. B. dysphasia. C. dysphagia. D. dysarthria.

Review Answer: D Rationale: Dysarthria is defined as slurred, poorly articulated speech; it is common in stroke patients. Dysphasia is defined as difficulty speaking; the patient’s speech may or may not be slurred. Aphasia is the inability to speak. Dysphagia is defined as difficulty swallowing.
Review (1 of 2) 5. A patient with a suspected stroke presents with slurred speech that is difficult for you to understand. This is referred to as: A. aphasia. Rationale: Aphasia is the inability to produce or understand speech. B. dysphasia. Rationale: Dysphasia is difficulty in speaking.

Review (2 of 2) 5. A patient with a suspected stroke presents with slurred speech that is difficult for you to understand. This is referred to as: C. dysphagia. Rationale: Dysphagia is difficulty in swallowing. D. dysarthria. Rationale: Correct answer

Review 6. A type of seizure that is characterized by severe twitching of all the body’s muscles and lasts for several minutes or longer is called a(n): A. partial seizure. B. absence seizure. C. tonic-clonic seizure. D. generalized seizure.

Review Answer: D Rationale: Generalized seizures are characterized by generalized severe twitching of all of the body’s muscles; they often last for several minutes or longer. An absence seizure is characterized by a blank stare; generalized muscle twitching is absent.
Review (1 of 2) 6. A type of seizure that is characterized by severe twitching of all the body’s muscles and lasts for several minutes or longer is called a(n): A. partial seizure. Rationale: A partial seizure is broken down into simple (jerking of one part of the body) and complex (changes in behavior and emotion). B. absence seizure. Rationale: An absence seizure does not involve any changes in motor activity.

Review (2 of 2) 6. A type of seizure that is characterized by severe twitching of all the body’s muscles and lasts for several minutes or longer is called a(n): C. tonic-clonic seizure. Rationale: A tonic-clonic seizure exhibits muscle contraction and incontinence. D. generalized seizure. Rationale: Correct answer
Review 7. The MOST important reason for promptly transporting a stroke patient to the hospital is because: A. a transient ischemic attack can be ruled out. B. medications may be given to reverse the stroke. C. the clot in the coronary artery may be dissolved. D. he or she needs close blood pressure monitoring.

Review Answer: B Rationale: Fibrinolytic medications (clot busters) have been shown to reverse the symptoms of a stroke by dissolving the clot that is blocking the cerebral artery. However, for the patient to be eligible for this therapy, it must be initiated within 3 hours after the onset of symptoms. For this reason, prompt transport of the stroke patient is critical.
Review (1 of 2) 7. The MOST important reason for promptly transporting a stroke patient to the hospital is because: A. a transient ischemic attack can be ruled out. Rationale: In a TIA, stroke symptoms resolve (on their own) usually in less than 24 hours with no neurologic deficits. B. medications may be given to reverse the stroke. Rationale: Correct answer

Review (2 of 2) 7. The MOST important reason for promptly transporting a stroke patient to the hospital is because: C. the clot in the coronary artery may be dissolved. Rationale: The coronary artery is in the heart and not the brain. D. he or she needs close blood pressure monitoring. Rationale: Monitoring of a patient’s blood pressure is important, but dissolving the clot and stopping the progression of damage is more important.
Review 8. Which of the following are components of the Cincinnati Prehospital Stroke Scale? A. Arm drift, blood pressure, speech B. Speech, pupil response, arm drift C. Facial symmetry, speech, arm drift D. Pupil response, facial droop, speech
Review Answer: C Rationale: The three components of the Cincinnati Prehospital Stroke Scale are facial symmetry, speech, and arm drift. Both sides of the patient’s face should move symmetrically (equally) when he or she smiles. The patient’s speech should be easily understandable and without slurring. The patient should be able to hold both arms out in front of his or her body— with eyes closed and palms up—without one arm drifting down to his or her side.
Review 8. Which of the following are components of the Cincinnati Prehospital Stroke Scale? A. Arm drift, blood pressure, speech Rationale: The scale does not use blood pressure. B. Speech, pupil response, arm drift Rationale: The scale does not use pupil response. C. Facial symmetry, speech, arm drift Rationale: Correct answer D. Pupil response, facial droop, speech Rationale: The scale does not use pupil response.
Review 9. Your patient opens his eyes when you say his name, is making incomprehensible sounds, and withdraws when you pinch his earlobe. What is his GCS score? A. 9 B. 8 C. 11 D. 12
Review Answer: A Rationale: The Glasgow Coma Scale gives a score of 3 to a patient who opens his or her eyes in response to speech. “Incomprehensible sounds” has a score of 2, and “withdraws to pain” has a score of 4. When added together, this patient’s GCS score is 9.

Review 9. Your patient opens his eyes when you say his name, is making incomprehensible sounds, and withdraws when you pinch his earlobe. What is his GCS score? A. 9 Rationale: Correct answer B. 8 Rationale: This is not the right score. C. 11 Rationale: This is not the right score. D. 12 Rationale: This is not the right score.
Review 10. If a patient complains of a severe migraine, how should she be transported? A. In a brightly lit ambulance so she can see while her vision is impaired B. With loud sirens so she can get to the hospital as soon as possible C. Without lights and sirens D. This patient should not be transported.
Review Answer: C Rationale: Treatment of a migraine headache is supportive; however, you should always assess the patient for other signs and symptoms that might indicate a more serious condition. Applying high-flow oxygen, if tolerated, may help ease the patient’s condition. When possible, provide a darkened and quiet environment because patients are sensitive to light and sound. Do not use lights and sirens during transport.
Review (1 of 2) 10. If a patient complains of a severe migraine, how should she be transported? A. In a brightly lit ambulance so she can see while her vision is impaired Rationale: Migraine patients are sensitive to light. B. With loud sirens so she can get to the hospital as soon as possible Rationale: Migraine patients are sensitive to loud noises.
Review (2 of 2) 10. If a patient complains of a severe migraine, how should she be transported? C. Without lights and sirens Rationale: Correct answer D. This patient should not be transported. Rationale: A migraine could indicate a more serious condition.
 Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Chapter 17 neurologic emergencies
Chapter 17 neurologic emergencies Management of patients with neurologic trauma
Management of patients with neurologic trauma Management of patients with neurologic trauma
Management of patients with neurologic trauma Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies A behavioral crisis is most accurately defined as
A behavioral crisis is most accurately defined as Endocrine and hematologic emergencies
Endocrine and hematologic emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 28 lesson 1
Chapter 28 lesson 1 Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Gems diamond geriatric assessment
Gems diamond geriatric assessment Chapter 13 handling emergencies
Chapter 13 handling emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies I should take a local area orientation dive whenever i
I should take a local area orientation dive whenever i Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Dic labs
Dic labs Psychiatric emergency
Psychiatric emergency Qut security contact number for emergencies
Qut security contact number for emergencies Immunologic emergencies
Immunologic emergencies Intro paragraph outline
Intro paragraph outline Levels of ecological organization
Levels of ecological organization Function of operation manager
Function of operation manager Introduction to management science chapter 9 solutions
Introduction to management science chapter 9 solutions Marine ecology
Marine ecology What is internet marketing 1
What is internet marketing 1 Chapter 9 review stoichiometry section 1
Chapter 9 review stoichiometry section 1 Chapter 9 introduction to waves
Chapter 9 introduction to waves Chaparral climograph
Chaparral climograph Chapter 3 research instrument example
Chapter 3 research instrument example 68k instruction set
68k instruction set A systematic study of the risks that you face.
A systematic study of the risks that you face. Chapter 24 body plans of animals with bilateral symmetry
Chapter 24 body plans of animals with bilateral symmetry Chapter 21 introduction to risk management
Chapter 21 introduction to risk management Chapter 19 section 1 introduction to protists
Chapter 19 section 1 introduction to protists Introduction to the structural units chapter 1 answers
Introduction to the structural units chapter 1 answers Chapter 1 learning exercises medical terminology
Chapter 1 learning exercises medical terminology Introduction to management science chapter 1 solutions
Introduction to management science chapter 1 solutions Chapter 1 introduction to management and organizations
Chapter 1 introduction to management and organizations New approaches to organizing hr
New approaches to organizing hr Human resources management chapter 1
Human resources management chapter 1 Chapter 1 introduction to human anatomy and physiology
Chapter 1 introduction to human anatomy and physiology Introduction to corporate finance
Introduction to corporate finance Introduction to accounting and business
Introduction to accounting and business Managers and management chapter 1
Managers and management chapter 1 Cyan medical term example
Cyan medical term example Introduction to triads and seventh chords
Introduction to triads and seventh chords Introduction to psychology chapter 1
Introduction to psychology chapter 1 A and b probability
A and b probability Introduction to materials science for engineers chapter 10
Introduction to materials science for engineers chapter 10 Introduction to accounting and business chapter 1
Introduction to accounting and business chapter 1 Colin dexter introduction
Colin dexter introduction Chapter 1 introduction to chemistry
Chapter 1 introduction to chemistry Chapter 8 introduction to metabolism
Chapter 8 introduction to metabolism Chapter 1 introduction to statistics
Chapter 1 introduction to statistics Ems system components
Ems system components Marketing research chapter 1
Marketing research chapter 1 Foundations in personal finance chapter 1
Foundations in personal finance chapter 1 Introduction to chemistry chapter 1
Introduction to chemistry chapter 1 The flow of food: an introduction
The flow of food: an introduction Introduction to accounting and business chapter 1
Introduction to accounting and business chapter 1 Introduction to business chapter 8
Introduction to business chapter 8 Chapter 7 study guide management and leadership
Chapter 7 study guide management and leadership Chapter 8 an introduction to metabolism
Chapter 8 an introduction to metabolism Chapter 4 prefixes medical terminology
Chapter 4 prefixes medical terminology An introduction to cost terms and purposes
An introduction to cost terms and purposes Chapter 1 the study of life
Chapter 1 the study of life Organizational behavior chapter 1
Organizational behavior chapter 1 Introduction to welding chapter 1
Introduction to welding chapter 1 Chapter 1 introduction to statistics
Chapter 1 introduction to statistics Non luminous flame
Non luminous flame Chapter 1 introduction to multimedia
Chapter 1 introduction to multimedia Chapter 1 introduction to medical terminology
Chapter 1 introduction to medical terminology Chapter 1 introduction to human anatomy and physiology
Chapter 1 introduction to human anatomy and physiology Introduction to health care agencies
Introduction to health care agencies Chapter 1 introduction to earth science
Chapter 1 introduction to earth science Chapter 1 introduction to corporate finance
Chapter 1 introduction to corporate finance Chapter 1 introduction to accounting
Chapter 1 introduction to accounting Physics chapter 1 introduction and mathematical concepts
Physics chapter 1 introduction and mathematical concepts Chapter 45 introduction to the clinical laboratory
Chapter 45 introduction to the clinical laboratory Introduction to public speaking chapter 1
Introduction to public speaking chapter 1 Computer programming chapter 1
Computer programming chapter 1 Introduction to materials science for engineers chapter 10
Introduction to materials science for engineers chapter 10 Chapter 22 introduction to plants worksheet answers
Chapter 22 introduction to plants worksheet answers Chapter 1 introduction to the structural units
Chapter 1 introduction to the structural units Introduction to the structural units
Introduction to the structural units Chapter 1 introduction to medical terminology
Chapter 1 introduction to medical terminology Chapter 1 introduction to corporate finance
Chapter 1 introduction to corporate finance Chapter 1 introduction to forensic science and the law
Chapter 1 introduction to forensic science and the law Chapter 1 introduction to corporate finance
Chapter 1 introduction to corporate finance Chapter 1 introduction to the dental profession
Chapter 1 introduction to the dental profession Percentile example
Percentile example Scytale
Scytale