CHEST TRAUMA Victor Politi M D FACP Medical











- Slides: 179
CHEST TRAUMA Victor Politi, M. D. , FACP Medical Director, SVCMC Physician Assistant Program
Statistics • Each year there are nearly 150, 000 accidental deaths in the United States • 25% of these deaths are a direct result of thoracic trauma • An additional 25% of traumatic deaths have chest injury as a contributing factor
Statistics • Chest injuries are the second leading cause of trauma deaths each year. • Most thoracic injuries (90% of blunt trauma and 70% to 85% of penetrating trauma) can be managed without surgery.
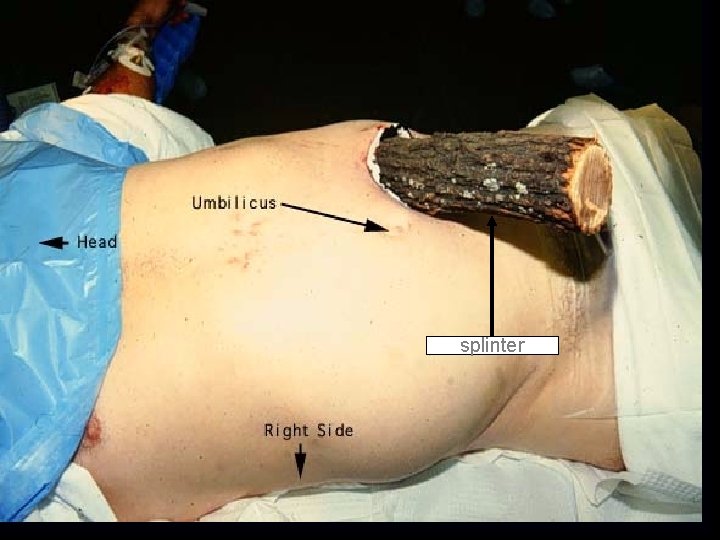
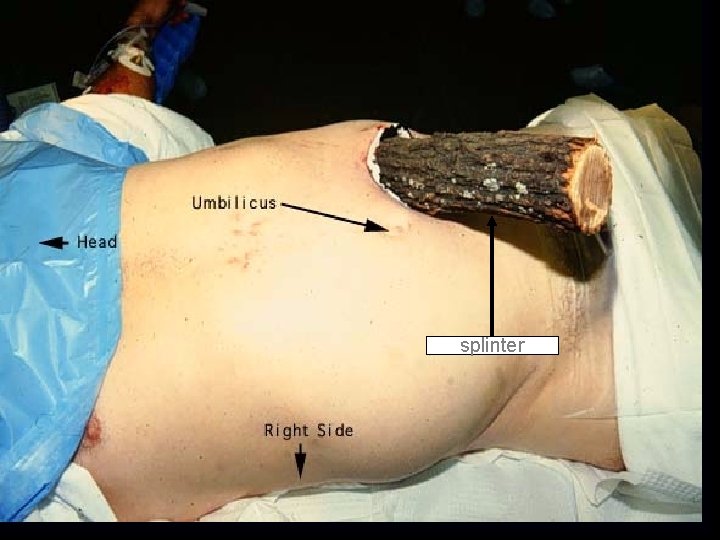
splinter

CAUSES OF THORACIC TRAUMA • • Falls 3 times the height of the patient Blast Injuries overpressure, plasma forced into alveoli • Blunt Trauma • Penetrating trauma
Incidence of Chest Trauma • Cause 1 of 4 American trauma deaths • Contributes to another 1 of 4 • Many die after reaching hospital - could be prevented if recognized • <10% of blunt chest trauma needs surgery • 1/3 of penetrating trauma needs surgery • Most life-saving procedures do NOT require a thoracic surgeon
Classifications of Chest Injuries • • Skeletal injury Pulmonary injury Heart and great vessel injury Diaphragmatic injury
Classification Mechanism of Injury • Blunt thoracic injuries • Forces distributed over a large area – Deceleration – Compression
Classification Mechanism of Injury • Penetrating thoracic injuries – Forces are distributed over a small area. – Organs injured are usually those that lie along the path of the penetrating object

Injury Patterns • General types – Open injuries – Closed injuries
Injury Patterns • • • Cardiovascular Pleural and pulmonary Mediastinal Diaphragmatic Esophageal Penetrating cardiac trauma Blast injury Confined spaces Shock wave Thoracic cage
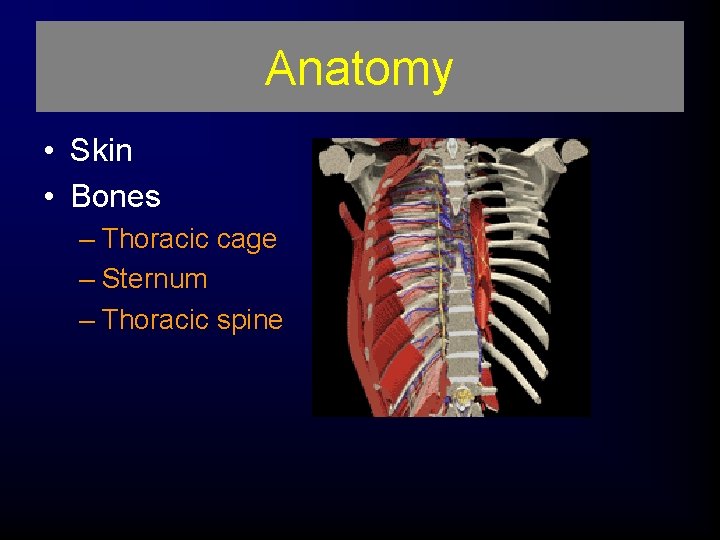
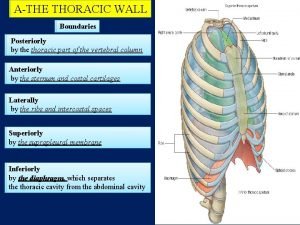
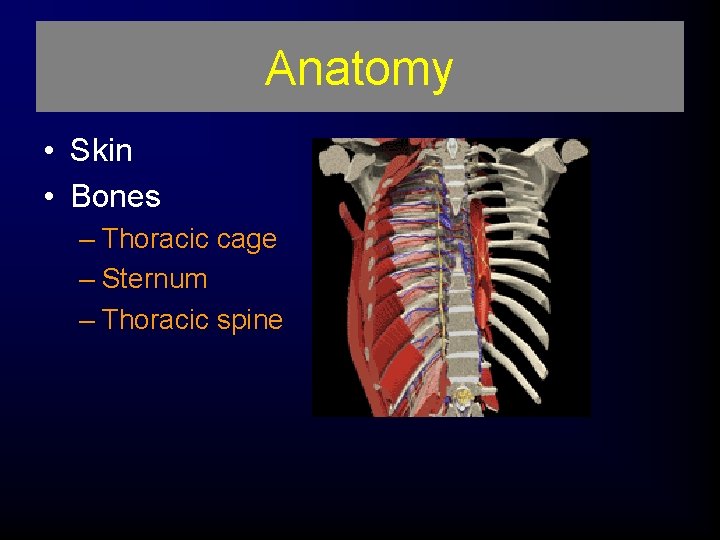
Anatomy • Skin • Bones – Thoracic cage – Sternum – Thoracic spine
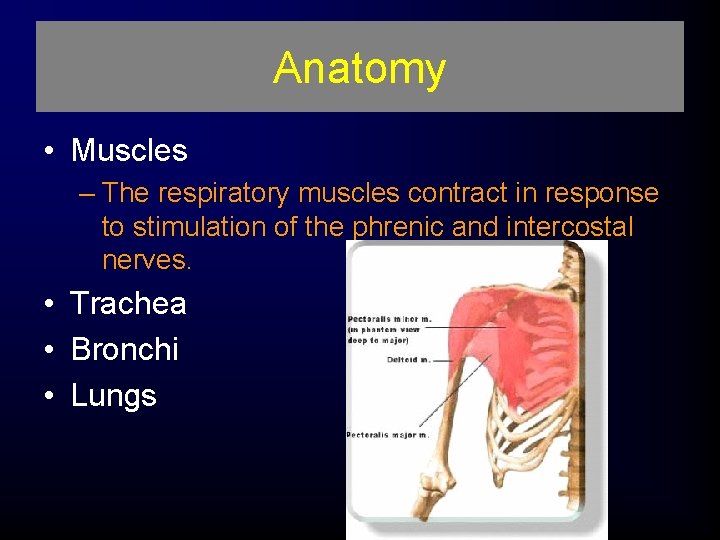
Anatomy • Muscles – The respiratory muscles contract in response to stimulation of the phrenic and intercostal nerves. • Trachea • Bronchi • Lungs

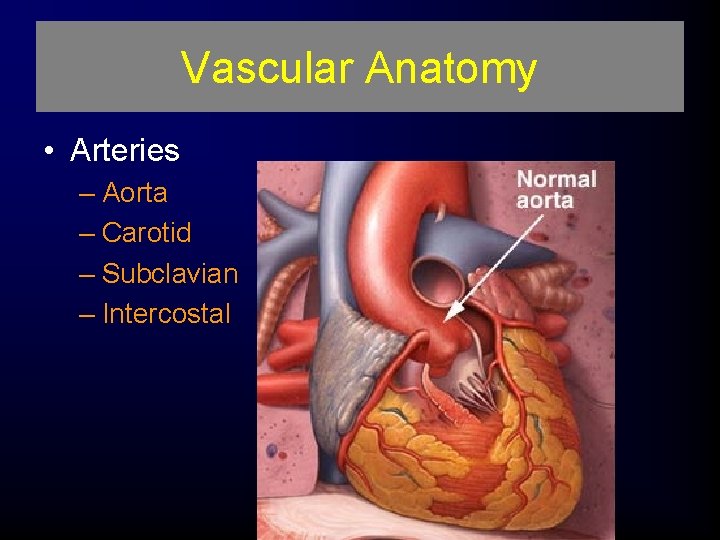
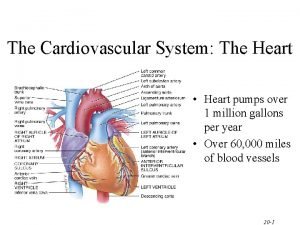
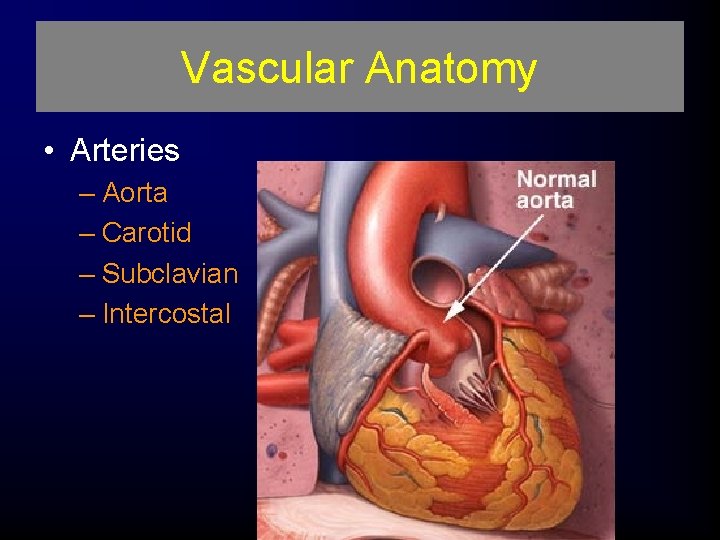
Vascular Anatomy • Arteries – Aorta – Carotid – Subclavian – Intercostal

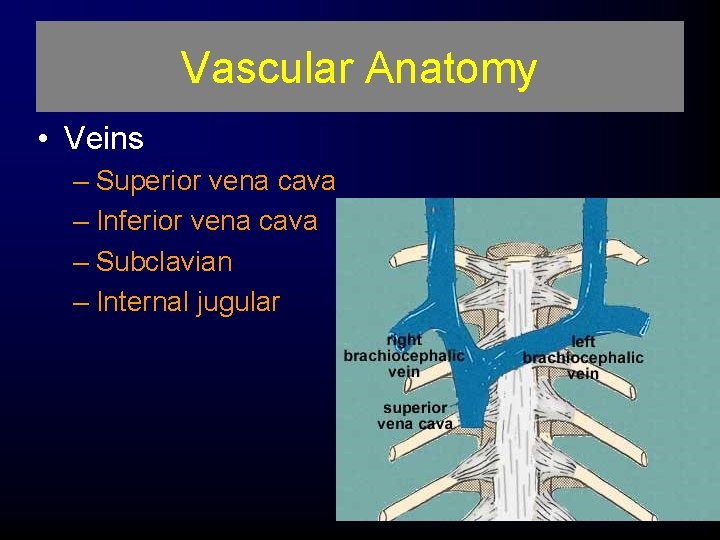
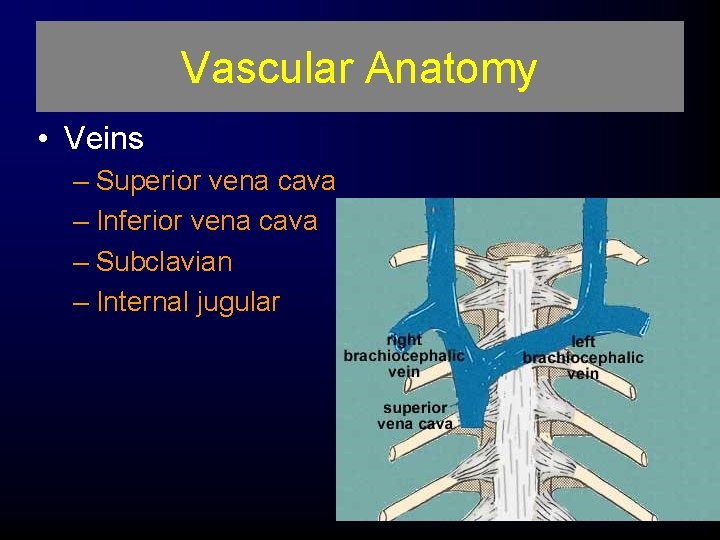
Vascular Anatomy • Veins – Superior vena cava – Inferior vena cava – Subclavian – Internal jugular
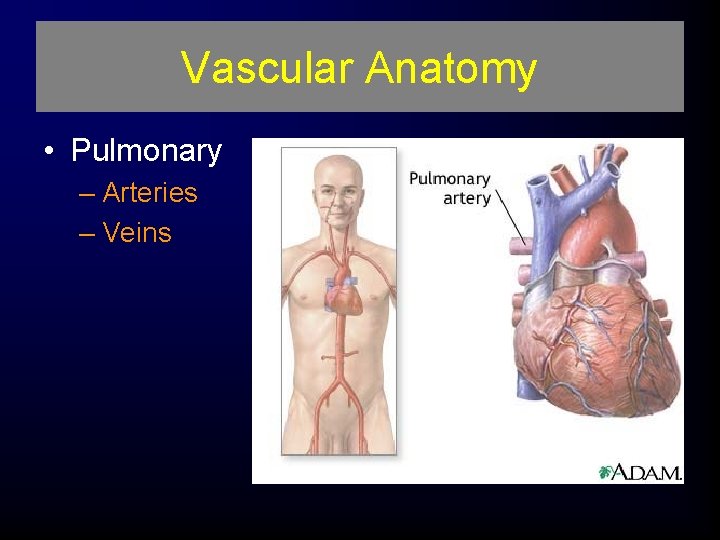
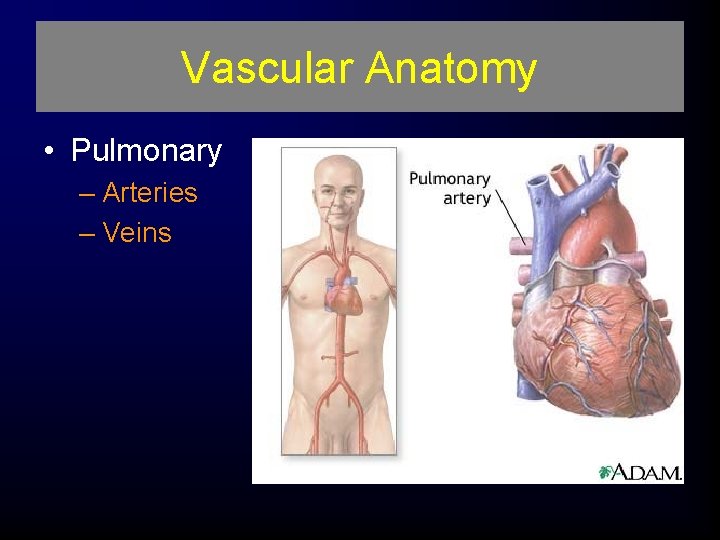
Vascular Anatomy • Pulmonary – Arteries – Veins
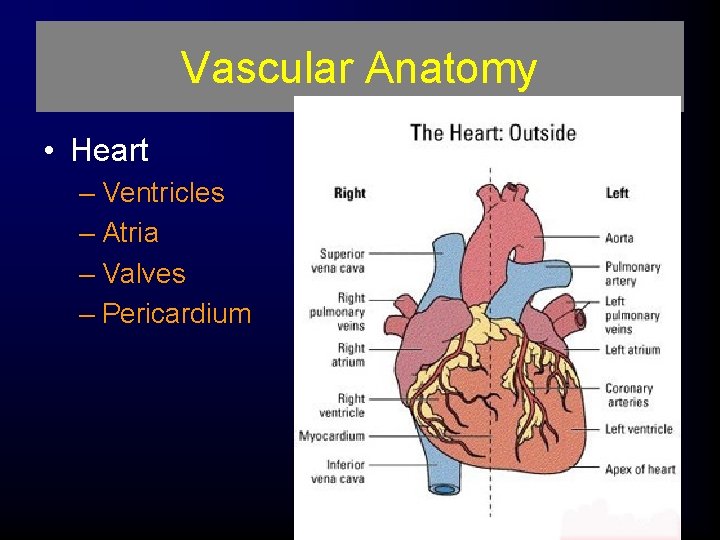
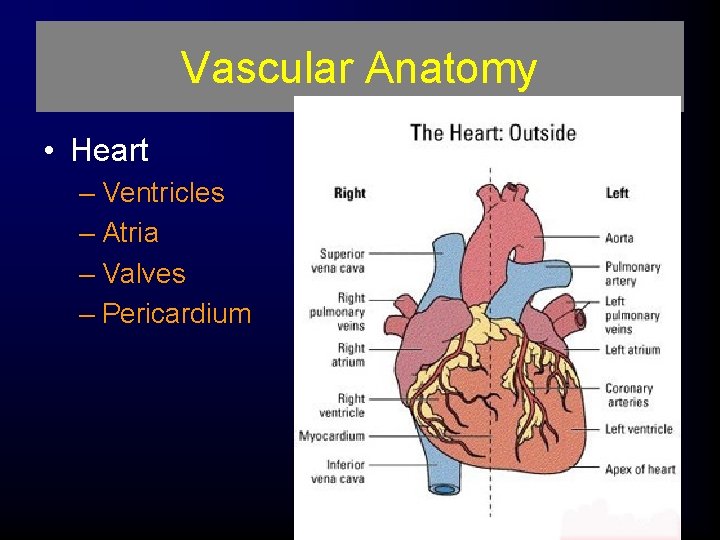
Vascular Anatomy • Heart – Ventricles – Atria – Valves – Pericardium
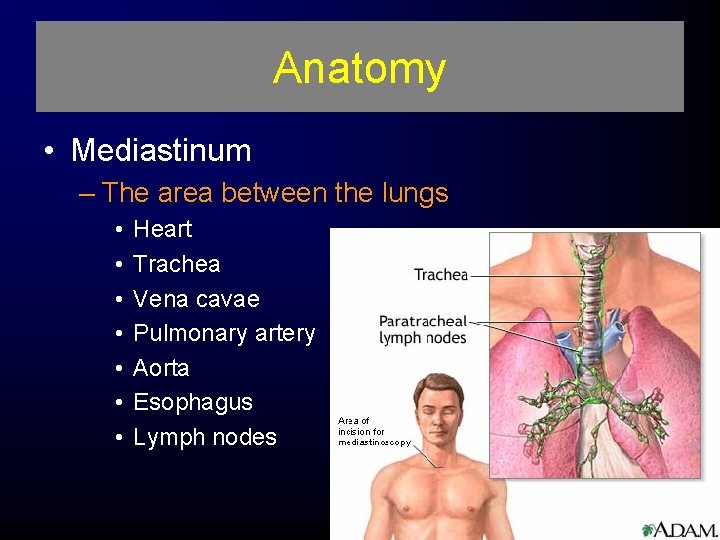
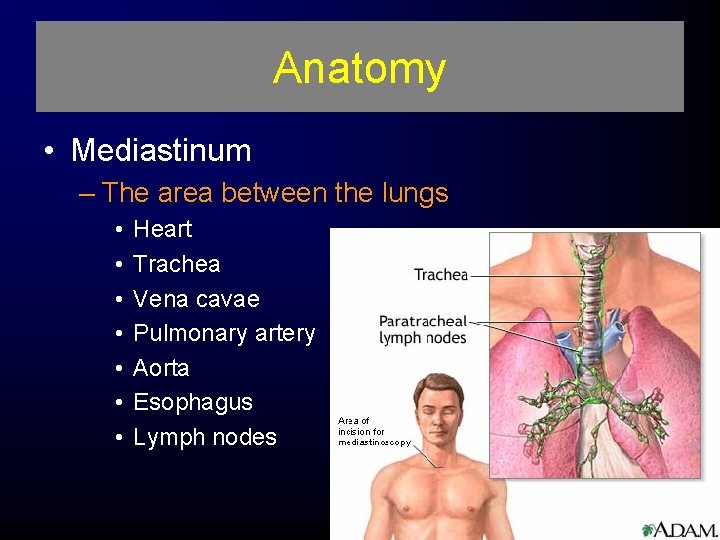
Anatomy • Mediastinum – The area between the lungs • • Heart Trachea Vena cavae Pulmonary artery Aorta Esophagus Lymph nodes
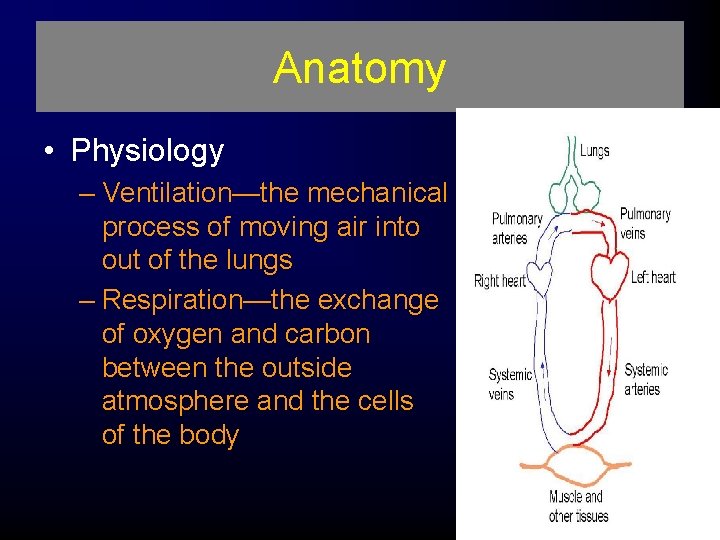
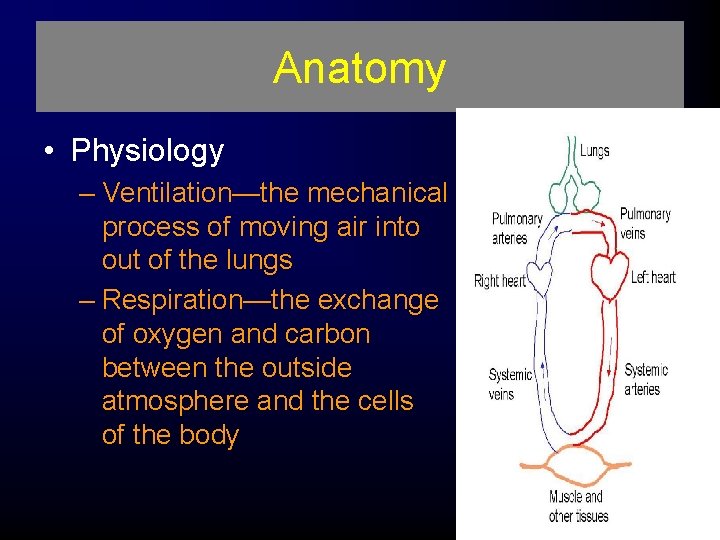
Anatomy • Physiology – Ventilation—the mechanical process of moving air into out of the lungs – Respiration—the exchange of oxygen and carbon between the outside atmosphere and the cells of the body and dioxide
Pathophysiology • Impairments in cardiac output – Blood loss – Increased intrapleural pressures – Blood in the pericardial sac – Myocardial valve damage – Vascular disruption
Pathophysiology • Impairments in cardiac output – Blood loss – Increased intrapleural pressures – Blood in the pericardial sac – Myocardial valve damage – Vascular disruption
Pathophysiology • Impairments in gas exchange – Atelectasis – Contused lung tissue – Disruption of the respiratory tract
Chest Trauma Initial Evaluation • Hypoxia and hypoventilation are the primary killers of acute trauma patients. • Assessment of ventilation is therefore given high priority in the primary survey as the second 'B' or Breathing stage.
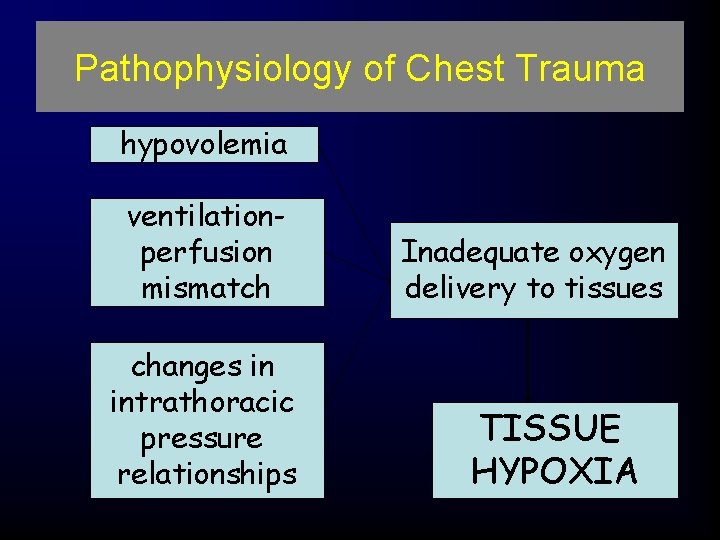
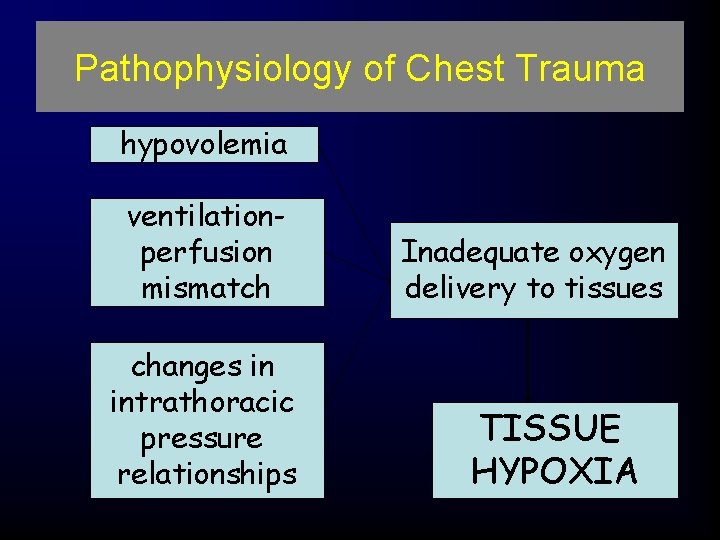
Pathophysiology of Chest Trauma hypovolemia ventilationperfusion mismatch changes in intrathoracic pressure relationships Inadequate oxygen delivery to tissues TISSUE HYPOXIA
Pathophysiology of Chest Trauma • • Tissue hypoxia Hypercarbia Respiratory acidosis - inadequate ventilation Metabolic acidosis - tissue hypoperfusion (e. g. , shock)
Chest Trauma Initial Evaluation • Life-threatening injuries should be identified and treated immediately. • Injuries may develop over time, and become life-threatening during the course of a resuscitation. • Re-assessment and evaluation is therefore extremely important, especially if the patient's condition deteriorates.
Chest Trauma - Initial Evaluation Mechanism of Injury • Mechanism of injury is important in so far as blunt and penetrating injuries have different pathophysiologies and clinical courses. • Most blunt injuries are managed nonoperatively or with simple interventions like intubation and ventilation and chest tube insertion.
Chest Trauma - Initial Evaluation Mechanism of Injury • Diagnosis of blunt injuries may be more difficult and require additional investigations such as CT scanning. • Patients with penetrating trauma may deteriorate rapidly, and recover much faster than patients with blunt injury.
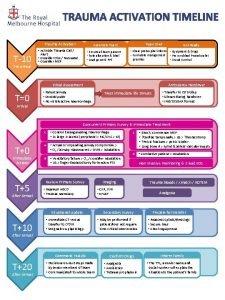
Initial assessment and management • • Primary survey Resuscitation of vital functions Detailed secondary survey Definitive care
Initial assessment and management • Hypoxia is most serious problem - early interventions aimed at reversing • Immediate life-threatening injuries treated quickly and simply - usually with a tube or a needle • Secondary survey guided by high suspicion for specific injuries
6 Immediate Life Threats • Airway obstruction • Tension pneumothorax • Open pneumothorax “sucking chest wound” • Massive hemothorax • Flail chest • Cardiac tamponade
6 Potential Life Threats • • Pulmonary contusion Myocardial contusion Traumatic aortic rupture Traumatic diaphragmatic rupture • Tracheobronchial tree injury - larynx, trachea, bronchus • Esophageal trauma
6 Other Frequent Injuries • • • Subcutaneous emphysema Traumatic asphyxia Simple pneumothorax Hemothorax Scapula fracture Rib fractures
Chest Trauma – Initial Evaluation Primary Survey • Monitoring – Oxygen Saturation – End-tidal CO 2 (if intubated) • Diagnostic Studies – Chest X-ray – FAST ultrasound – Arterial Blood Gas • Interventions – Chest drain – ED Thoracotomy
Chest Trauma – Initial Evaluation Secondary Survey • The secondary survey is a more detailed and complete examination, aimed at identifying all injuries and planning further investigation and treatment. • Chest injuries identified on secondary survey and its adjuncts are: – – – Rib fractures and flail chest Pulmonary contusion Simple pneumothorax Simple haemothorax Blunt aortic injury Blunt myocardial injury
Primary Survey • Airway • Breathing • Circulation
Chest Trauma – Initial Evaluation Physical examination • Physical examination is the primary tool for diagnosis of acute thoracic trauma. – However, in the noisy ER or in the pre-hospital arena, an adequate physical examination may be very difficult. • Even under ideal conditions, signs of significant thoracic injury may be subtle or even absent. – It is important also to understand that these conditions develop over time.
Chest Trauma – Initial Evaluation Physical examination • With the advantages of rapid prehospital transport many of these conditions will not have fully developed by the time the patient reaches the emergency department. • While the initial primary survey may identify some of these conditions, an initial normal examination does not exclude any of them, and serial examinations and use of diagnostic adjuncts is important.
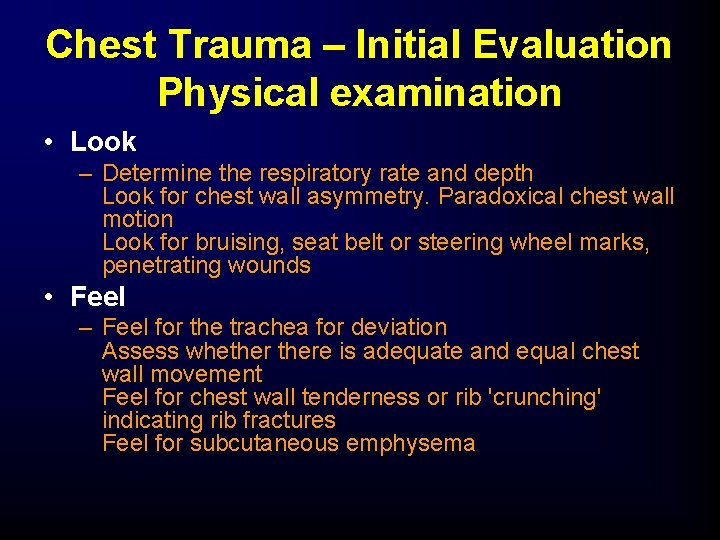
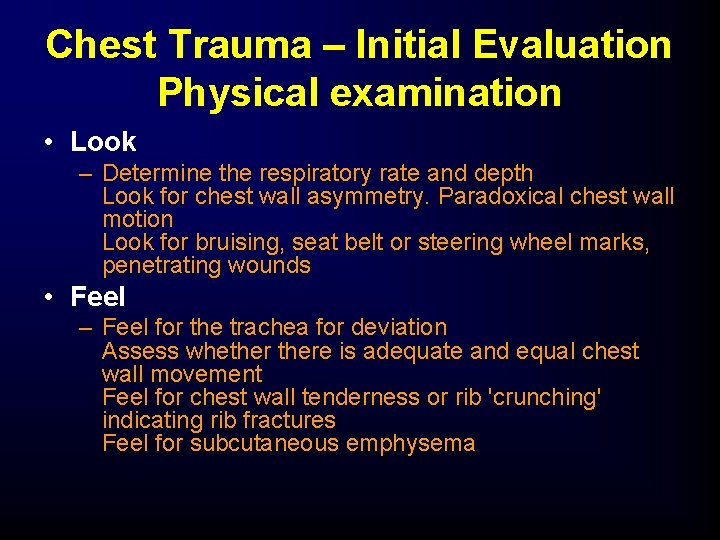
Chest Trauma – Initial Evaluation Physical examination • Look – Determine the respiratory rate and depth Look for chest wall asymmetry. Paradoxical chest wall motion Look for bruising, seat belt or steering wheel marks, penetrating wounds • Feel – Feel for the trachea for deviation Assess whethere is adequate and equal chest wall movement Feel for chest wall tenderness or rib 'crunching' indicating rib fractures Feel for subcutaneous emphysema
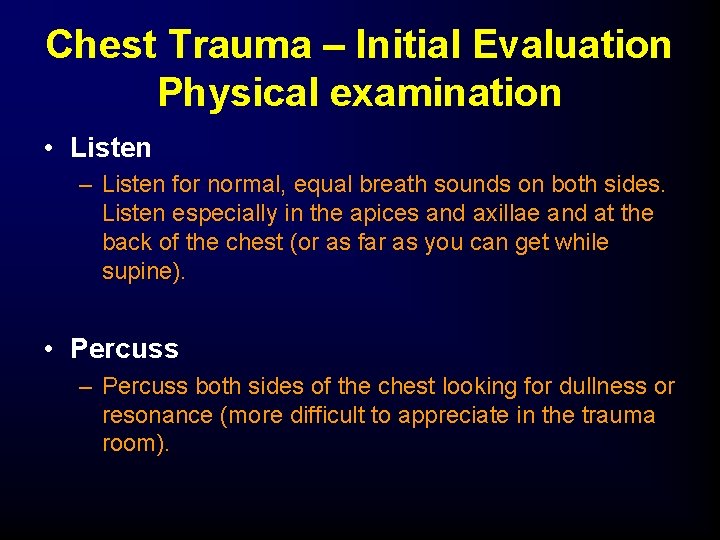
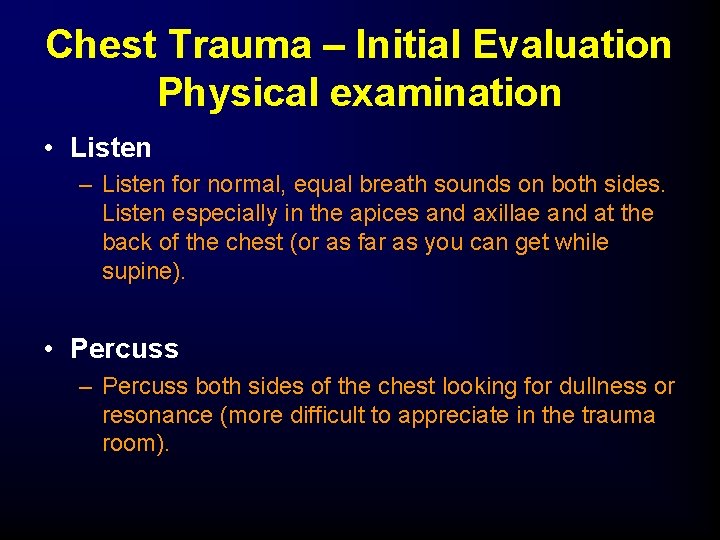
Chest Trauma – Initial Evaluation Physical examination • Listen – Listen for normal, equal breath sounds on both sides. Listen especially in the apices and axillae and at the back of the chest (or as far as you can get while supine). • Percuss – Percuss both sides of the chest looking for dullness or resonance (more difficult to appreciate in the trauma room).
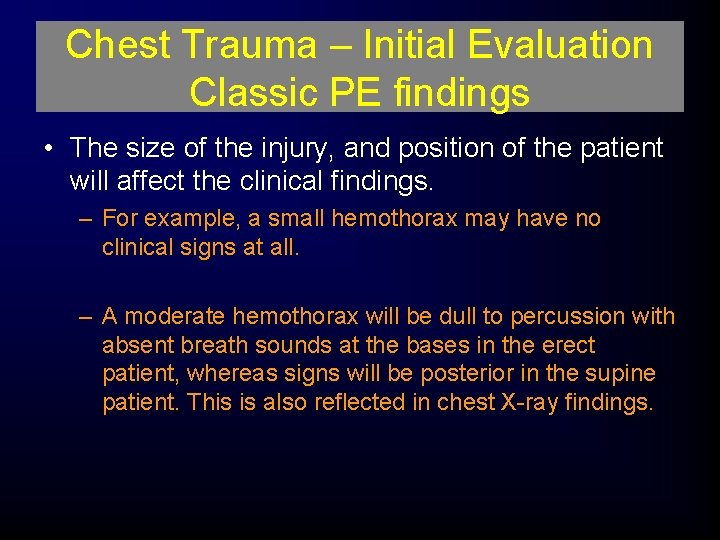
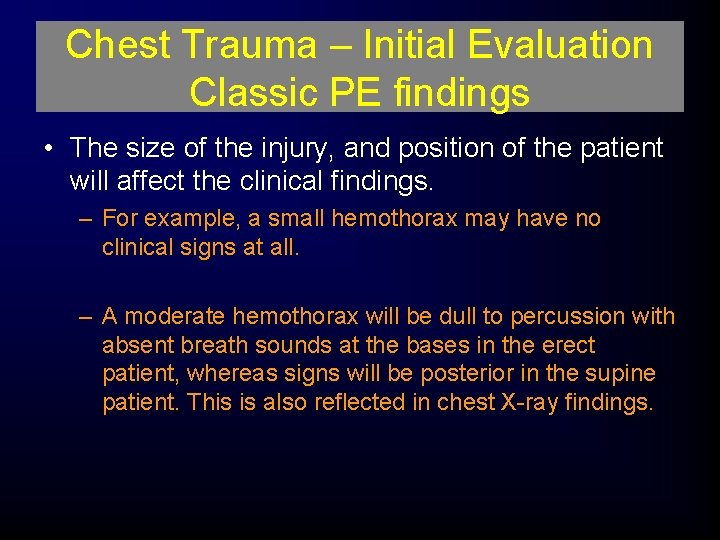
Chest Trauma – Initial Evaluation Classic PE findings • The size of the injury, and position of the patient will affect the clinical findings. – For example, a small hemothorax may have no clinical signs at all. – A moderate hemothorax will be dull to percussion with absent breath sounds at the bases in the erect patient, whereas signs will be posterior in the supine patient. This is also reflected in chest X-ray findings.
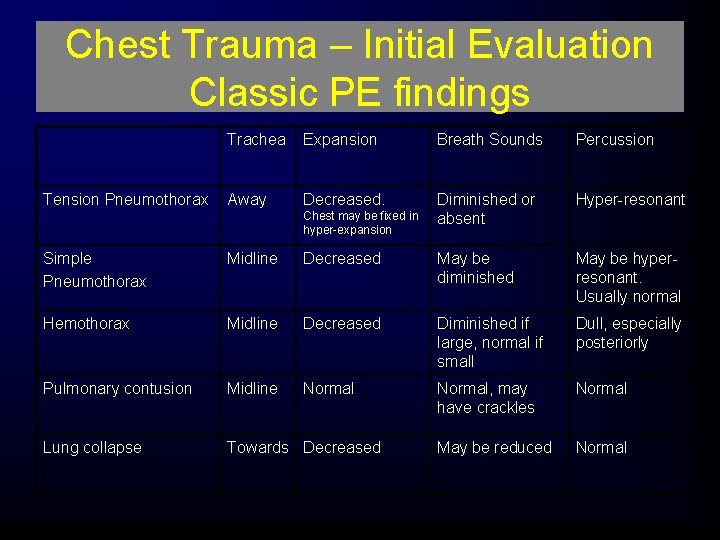
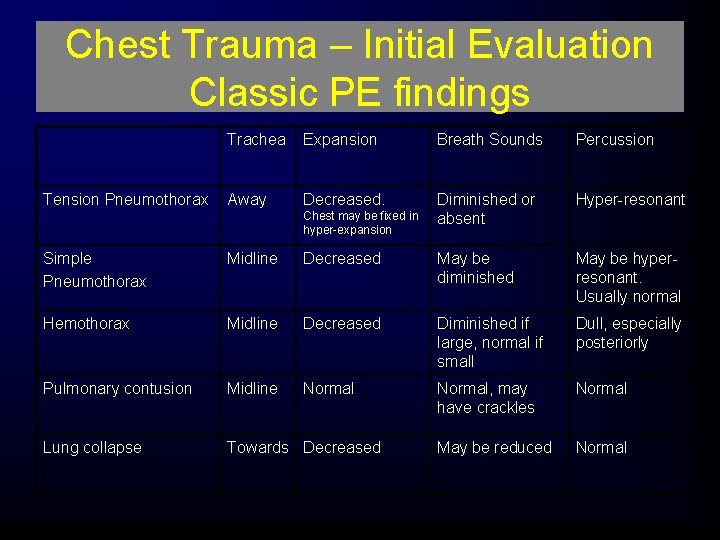
Chest Trauma – Initial Evaluation Classic PE findings Tension Pneumothorax Trachea Expansion Breath Sounds Percussion Away Decreased. Diminished or absent Hyper-resonant Chest may be fixed in hyper-expansion Simple Pneumothorax Midline Decreased May be diminished May be hyperresonant. Usually normal Hemothorax Midline Decreased Diminished if large, normal if small Dull, especially posteriorly Pulmonary contusion Midline Normal, may have crackles Normal Lung collapse Towards Decreased May be reduced Normal
Chest Trauma – Initial Evaluation • Note- a collapsed lung on one side can mimic a tension pneumothorax on the other side. – This is a common error, usually occurring when a tracheal tube has been incorrectly placed in the right main bronchus, obstructing the right upper lobe bronchus. – This leads to collapse of the right upper lobe and shift of the trachea to the right. – The left chest appears hype-resonant compared to the left, and breath sounds may be difficult to determine. – The patient may end up with an unnecessary chest drain.
Chest Trauma – Initial Evaluation • Oxygen saturation – Pulse oximetry allows continuous, noninvasive assessment of arterial hemoglobin oxygen saturation. – Continuous oxygen saturation monitoring should be used during the resuscitation of all trauma patients.
Chest Trauma – Initial Evaluation • End-tidal carbon dioxide – End-tidal carbon dioxide monitoring (ETCO 2) should be used in all intubated trauma patients. – ETCO 2 is the only definitive method of confirming placement of a tracheal tube. – Other methods, such as watching for chest wall movement and listening to breath sounds or for air in the stomach are inaccurate, especially in the setting of the trauma resuscitation room. – ETCO 2 also allows for the estimation of the arterial Pa. CO 2 level, and for its continuous montioring. – This is important for all mechanically ventilated patients and vital for patients with traumatic brain injury.
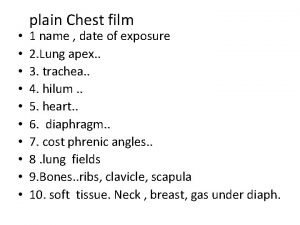
Chest Trauma – Initial Evaluation • Chest X-ray – The plain antero-posterior chest radiograph remains the standard initial evaluation for the evaluation of chest trauma. – Although the indications and techniques are slightly different for blunt and penetrating trauma.
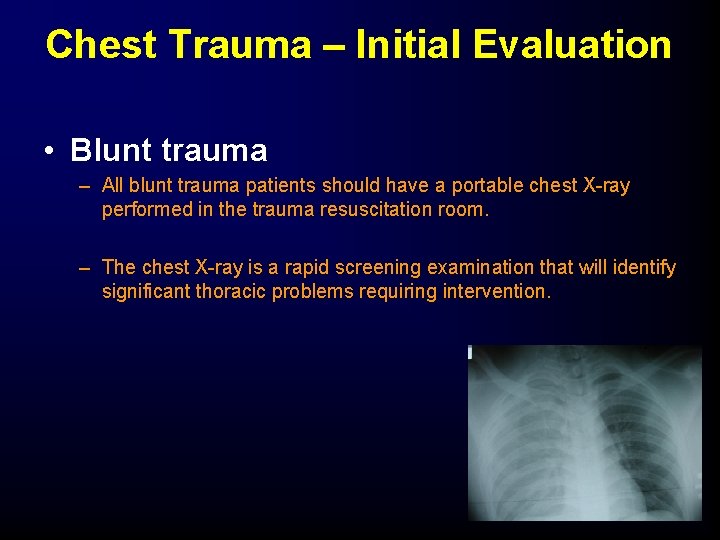
Chest Trauma – Initial Evaluation • Blunt trauma – All blunt trauma patients should have a portable chest X-ray performed in the trauma resuscitation room. – The chest X-ray is a rapid screening examination that will identify significant thoracic problems requiring intervention.
Chest Trauma – Initial Evaluation • Blunt trauma – Chest radiographs in blunt trauma patients are taken in the supine position, as unstable spinal fractures have not been ruled out at this stage. – Chest films should be slightly over-penetrated to allow better visualization of the thoracic spine, paraspinal lines and aortic outline.
Chest Trauma – Initial Evaluation • Penetrating trauma – Patients with a stab wound that may have violated the thoracic cavity or mediastinum should have a chest X-ray. – In practice, this means all patients with stab wounds between the neck and the umbilicus (front or back!).
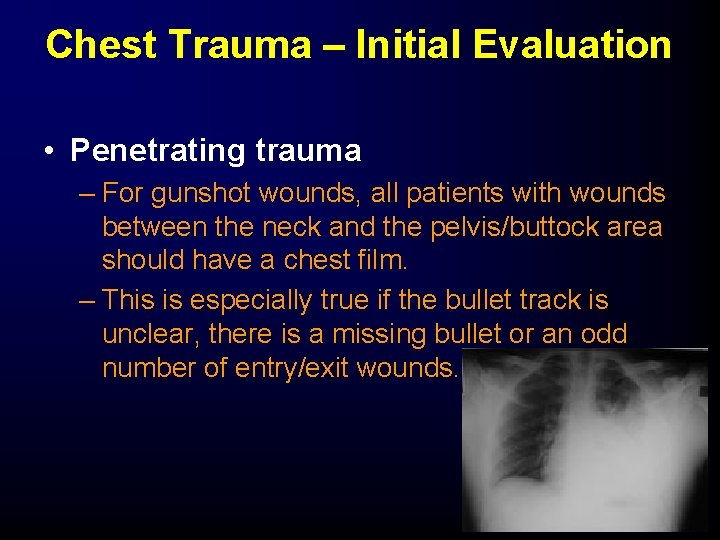
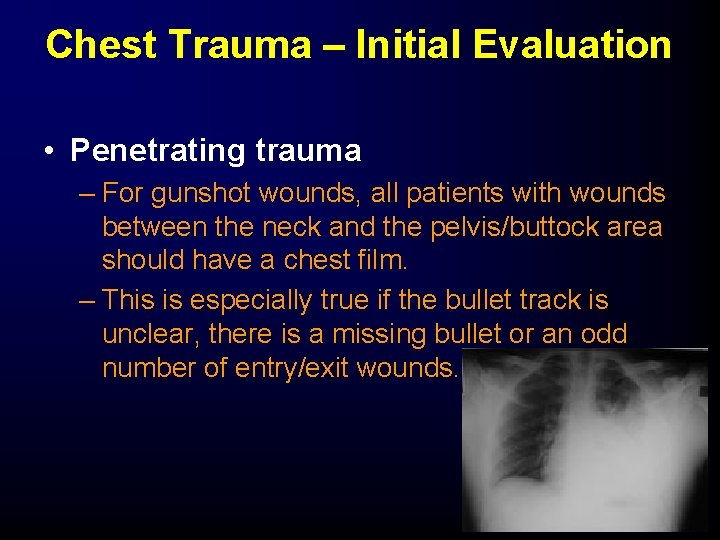
Chest Trauma – Initial Evaluation • Penetrating trauma – For gunshot wounds, all patients with wounds between the neck and the pelvis/buttock area should have a chest film. – This is especially true if the bullet track is unclear, there is a missing bullet or an odd number of entry/exit wounds.
Chest Trauma – Initial Evaluation • Penetrating trauma – The chest-X-ray in penetrating trauma should be taken with the patient sitting upright if possible. – This will increase the sensitivity for detecting a small hemothorax, pneumothorax or diaphragm injury.
Chest Trauma – Initial Evaluation • FAST examination – Focused abdominal sonography for trauma (FAST) is a rapid ultrasound examination performed in the trauma resuscitation room looking specifically from blood - in the peritoneum, pericardium, or hemithorax. – Currently, FAST is indicated for all hemodynamically unstable blunt trauma patients. It may also have a role in some patients with penetrating trauma.
Chest Trauma – Initial Evaluation • Arterial Blood Gas analysis – Arterial blood gas analyses should be drawn on all intubated and ventilated trauma patients, and any patient with significant chest trauma or evidence of hemodynamic instability.
Chest Trauma – Initial Evaluation • As part of the secondary survey the chest is fully examined, front and back. • Special attention is paid to identifying any missed injuries or progression of previously identified injuries. • The examination is also directed by findings on the chest X-ray or by information from monitoring adjuncts.
Chest Trauma – Initial Evaluation • Further investigations may include: – – CT scan Angiography Oesophagoscopy / oesophagram Bronchoscopy • Definitive care may include: – Chest drain – Thoracotomy – Transfer to ICU area for ventilation / observation
Assessment Findings • Pulse – Deficit – Tachycardia – Bradycardia • Blood pressure – Narrowed pulse pressure – Hypertension – Hypotension – Pulsus paradoxus
Assessment Findings • Respiratory rate and effort – Tachypnea – Bradypnea – Labored – Retractions – Other evidence of respiratory distress
Assessment Findings • Skin – Diaphoresis – Pallor – Cyanosis – Open wounds – Ecchymosis – Other evidence of trauma
Assessment (Neck) • • Position of trachea Subcutaneous emphysema Jugular venous distention Penetrating wounds
Assessment (Chest) • • Contusions Tenderness Asymmetry Lung sounds – Absent or decreased – Unilateral – Bilateral – Location – Bowel sounds in hemothorax
Abnormal Percussion Finding • Hyperresonance–Air • Hyporesonance–Fluid
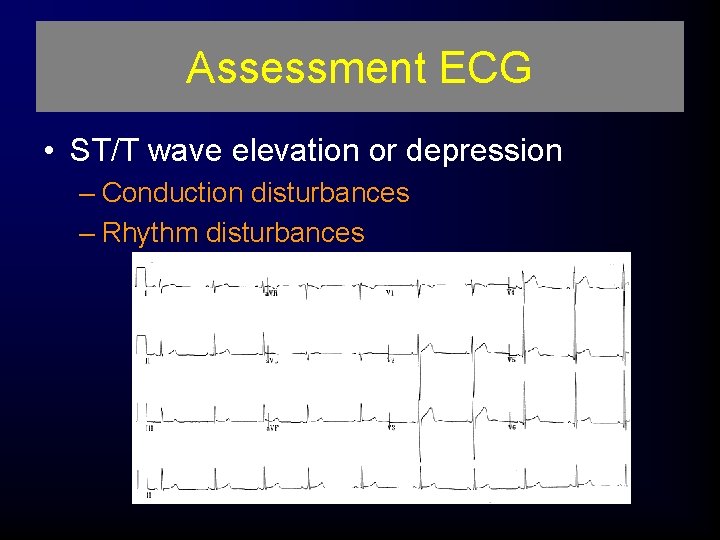
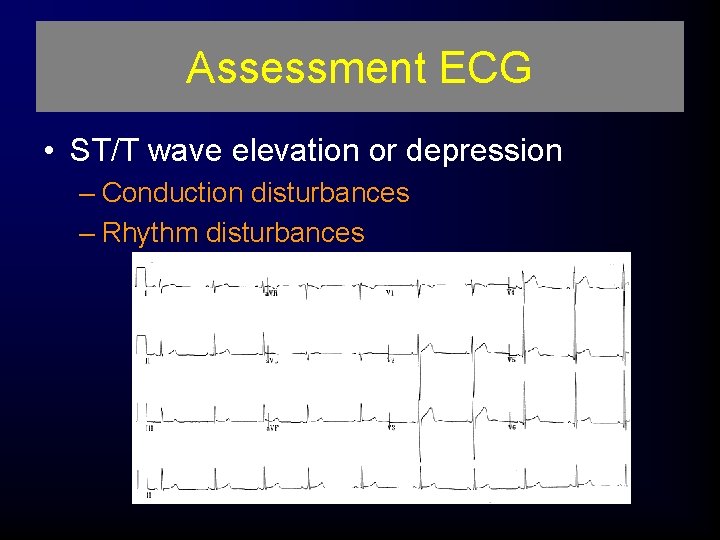
Assessment ECG • ST/T wave elevation or depression – Conduction disturbances – Rhythm disturbances
History • Dyspnea • Chest pain • Associated symptoms – Other areas of pain or discomfort – Symptoms before incident • Past history of cardiorespiratory disease • Use of restraint in motor vehicle crash
Management • Airway and ventilation – High-concentration oxygen – Pleural decompression – Endotracheal intubation – Needle cricothyrotomy – Surgical cricothyrotomy – Positive-pressure ventilation – Occlude open wounds – Stabilize chest wall
Circulation • Manage cardiac dysrhythmias • Intravenous access
Pharmacological • Analgesics • Antidysrhythmics
Nonpharmacological • Needle thoracostomy • Tube thoracostomy—in hospital management • Pericardiocentesis—in hospital
Skeletal Injury • Clavicular fractures – Clavicle the most commonly fractured bone – Isolated fracture of the clavicle seldom a significant injury • Common causes – Children who fall on their shoulders or outstretched arms – Athletes involved in contact sports
Skeletal Injury • Treatment – Usually accomplished with a sling and swathe or a clavicular strap that immobilizes the affected shoulder and arm – Usually heals well within 4 to 6 weeks • Signs and symptoms – Pain – Point tenderness – Evident deformity
Skeletal Injury • Complications – Injury to the subclavian vein or artery from bony fragment penetration, producing a hematoma or venous thrombosis (rare)
Rib Fractures • Incidence – Infrequent until adult life – Significant force required – Most often elderly patients
Rib Fractures Morbidity/Mortality • Can lead to serious consequences. • Older ribs are more brittle and rigid. • There may be associated underlying pulmonary or cardiovascular injury.
Rib Fractures Pathophysiology • Most often caused by blunt trauma— bowing effect with midshaft fracture • Ribs 3 to 8 are fractured most often (they are thin and poorly protected) • Respiratory restriction as a result of pain and splinting
Rib Fractures Pathophysiology • Intercostal vessel injury • Associated complications – First and second ribs are injured by severe trauma – Rupture of the aorta – Tracheobronchial tree injury – Vascular injury
Multiple Rib Fractures • • Atelectasis Hypoventilation Inadequate cough Pneumonia
Multiple Rib Fractures • Assessment findings – Localized pain – Pain that worsens with movement, deep breathing, coughing – Point tenderness • Most patients can localize the fracture by pointing to the area (confirmed by palpation). – Crepitus or audible crunch – Splinting on respiration
Multiple Rib Fractures Complications • Splinting, which leads to atelectasis and ventilation-perfusion mismatch (ventilated alveoli that are not perfused or perfused alveoli that are not ventilated)
Rib Fractures Management • Airway and ventilation – High-concentration oxygen – Positive-pressure ventilation – Encourage coughing and deep breathing • Pharmacological – Analgesics • Nonpharmacological – Non-circumferential splinting
Flail Chest • Incidence – Most common cause: vehicular crash – Falls from heights – Industrial accidents – Assault – Birth trauma
Flail Chest Morbidity/Mortality • Significant chest trauma • Mortality rates 20% to 40% due to associated injuries • Mortality increased with – – – Advanced age Seven or more rib fractures Three or more associated injuries Shock Head injuries
Flail Chest Pathophysiology • Two or more adjacent ribs fractured in two or more places producing a free-floating segment of chest wall Flail chest usually results from direct impact.
Flail Chest Pathophysiology • Respiratory failure due to: – Underlying pulmonary contusion • The blunt force of the injury typically produces an underlying pulmonary contusion. – Associated intrathoracic injury – Inadequate bellows action of the chest
Flail Chest Assessment Findings • • • Chest wall contusion Respiratory distress Paradoxical chest wall movement Pleuritic chest pain Crepitus Pain and splinting of affected side Tachypnea Tachycardia Possible bundle branch block on ECG
Flail Chest Management • Airway and ventilation – High-concentration oxygen. – Positive-pressure ventilation may be needed. • Reverses the mechanism of paradoxical chest wall movement • Restores the tidal volume • Reduces the pain of chest wall movement • Assess for the development of a pneumothorax – Evaluate the need for endotracheal intubation. – Stabilize the flail segment (controversial).
Sternal Fractures • Incidence – Occurs in 5% to 8% of all patients with blunt chest trauma – A deceleration compression injury – Steering wheel – Dashboard – A blow to the chest; massive crush injury – Severe hyperflexion of the thoracic cage
Sternal Fractures Morbidity/Mortality • 25% to 45% mortality rate • High association with myocardial or lung injury – Myocardial contusion – Myocardial rupture – Cardiac tamponade – Pulmonary contusion
Sternal Fractures Pathophysiology • Associated injuries cause morbidity and mortality. – Pulmonary and myocardial contusion – Flail chest • Seriously displaced sternal fractures may produce a flail chest. – Vascular disruption of thoracic vessels – Intra-abdominal injuries – Head injuries
Sternal Fractures Management • Airway and ventilation – High-concentration oxygen • Circulation—restrict fluids if pulmonary contusion suspected • Pharmacological—analgesics • Non-pharmacological—allow chest wall selfsplinting • Psychological support/communication strategies
Pulmonary Injury • Closed (simple) pneumothorax – Incidence • 10% to 30% in blunt chest trauma • Almost 100% with penetrating chest trauma – Morbidity/mortality • Extent of atelectasis • Associated injuries – Pathophysiology • Caused by the presence of air in the pleural space • A common cause of pneumothorax is a fractured rib that penetrates the underlying lung.
Closed (Simple) Pneumothorax • May occur in the absence of rib fractures from: – A sudden increase in intrathoracic pressure generated when the chest wall is compressed against a closed glottis (the paper-bag effect) • Results in an increase in airway pressure and ruptured alveoli, which lead to a pneumothorax • Small tears self-seal; larger ones may progress. • The trachea may tug toward the affected side. • Ventilation/perfusion mismatch.
Closed Pneumothorax Assessment Findings • • Tachypnea Tachycardia Respiratory distress Absent or decreased breath sounds on the affected side Hyperresonance Decreased chest wall movement Dyspnea Chest pain referred to the shoulder or arm on the affected side • Slight pleuritic chest pain
Closed Pneumothorax Management • Airway and ventilation – High-concentration oxygen. – Positive-pressure ventilation if necessary. – If respiration rate is <12 or >28 per minute, ventilatory assistance with a bag-valve mask may be indicated.
Closed Pneumothorax Management • Nonpharmacological – Needle thoracostomy • Transport considerations – Position of comfort (usually partially sitting) unless contraindicated by possible spine injury
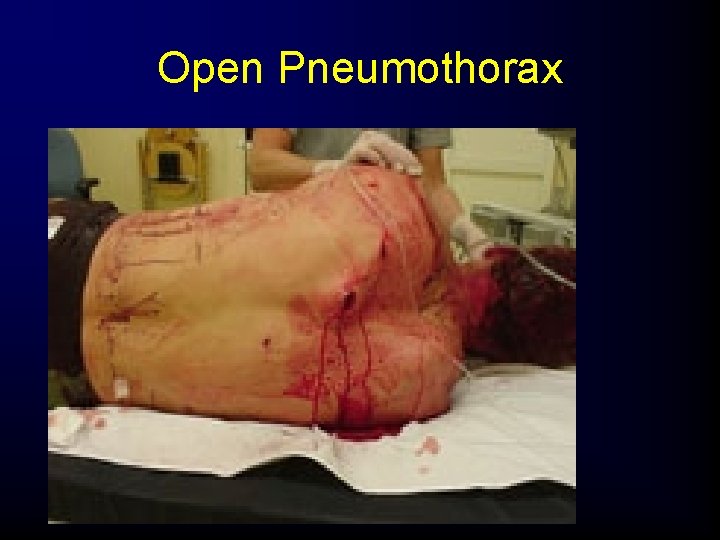
Open pneumothorax • Develops when penetration injury to the chest allows the pleural space to be exposed to atmospheric pressure "Sucking Chest Wound"
Open Pneumothorax • Incidence – Usually the result of penetrating trauma • • • Gunshot wounds Knife wounds Impaled objects Motor vehicle collisions Falls
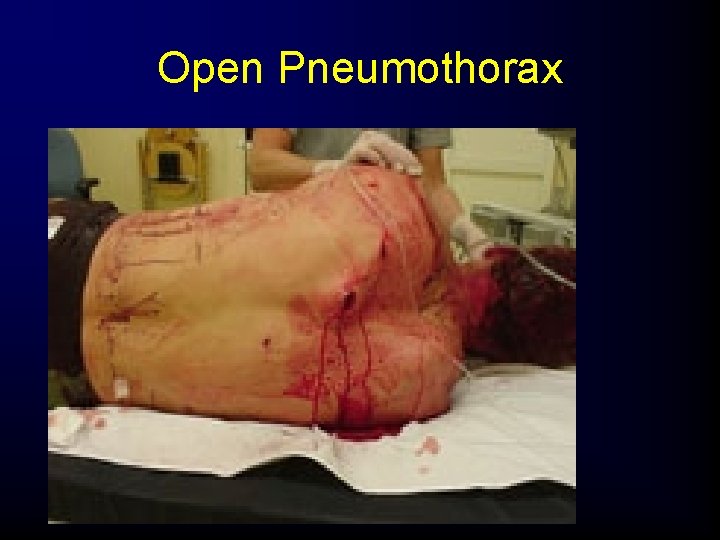
Open Pneumothorax
Open pneumothorax • WHAT MAY CAUSE A SCW? – Examples Include: GSW, Stab Wounds, Impaled Objects, Etc. . . • LARGE VS SMALL – Severity is directly proportional to the size of the wound • Atmospheric pressure forces air through the wound upon inspiration
Open Pneumothorax Morbidity/Mortality • Severity is directly proportional to the size of the wound. – Profound hypoventilation can result. – Death is related to delayed management.
Open Pneumothorax Pathophysiology • An open defect in the chest wall (>3 cm) – If the chest wound opening is greater than two -thirds the diameter of the trachea, air follows the path of least resistance through the chest wall with each inspiration. – As the air accumulates in the pleural space, the lung on the injured side collapses and begins to shift toward the uninjured side.
Open pneumothorax • Signs & Symptoms – Shortness of Breath (SOB) – Pain – Sucking or gurgling sound as air moves in and out of the pleural space through the wound
Open Pneumothorax Assessment Findings • To-and-fro air motion out of the defect • A defect in the chest wall • A penetrating injury to the chest that does not seal itself • A sucking sound on inhalation • Tachycardia • Tachypnea • Respiratory distress • Subcutaneous emphysema • Decreased breath sounds on the affected side
Open Pneumothorax • Breathing is rapid, shallow and laboured. There is reduced expansion of the hemithorax, accompanied by reduced breath sounds and an increased percussion note. • One or all of these signs may not be appreciated in a noisy ER.
Open Pneumothorax Management • Airway and ventilation: – High-concentration oxygen. – Positive-pressure ventilation if necessary. – Assist ventilations with a bag-valve device and intubation as necessary. – Monitor for the development of a tension pneumothorax. • Circulation—treat for shock with crystalloid infusion.
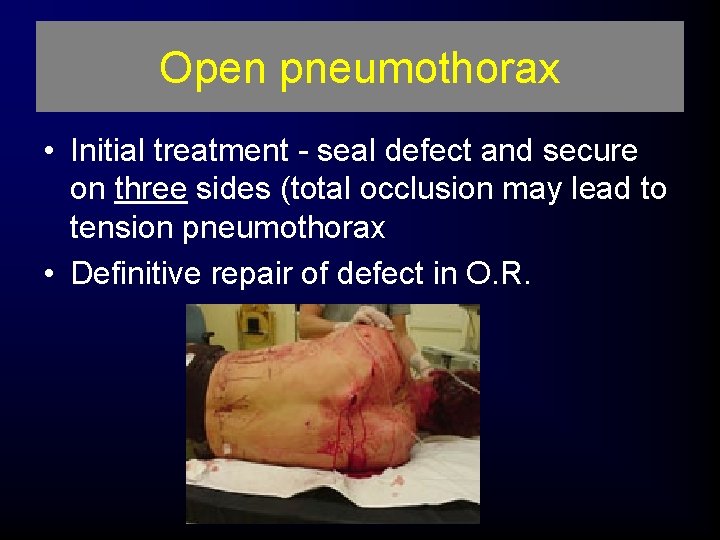
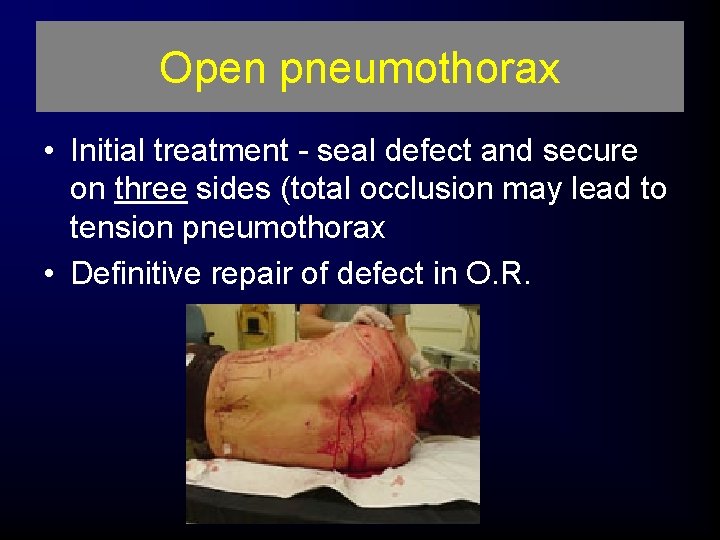
Open pneumothorax • Initial treatment - seal defect and secure on three sides (total occlusion may lead to tension pneumothorax • Definitive repair of defect in O. R.
Tension pneumothorax • Air within thoracic cavity that cannot exit the pleural space • Fatal if not immediately identified, treated, and reassessed for effective management
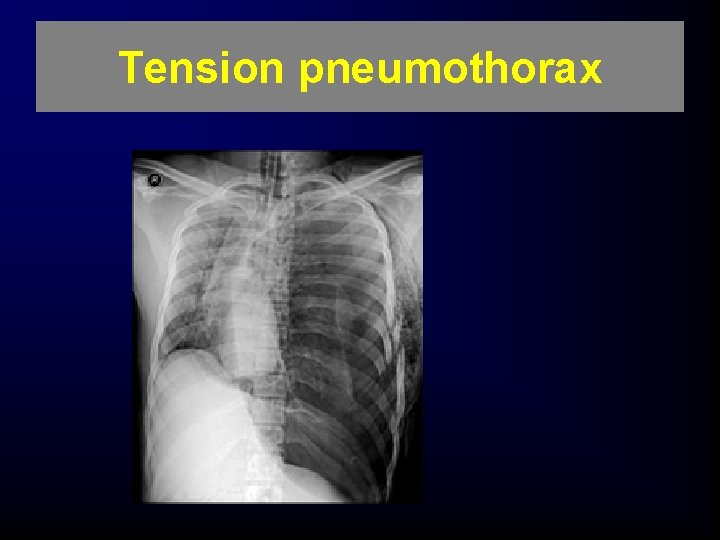
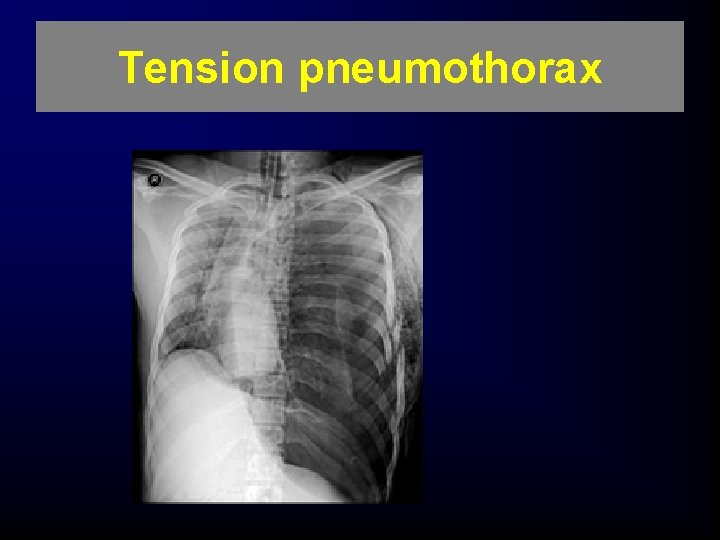
Tension pneumothorax
Tension Pneumothorax • Associated Injuries – A penetrating injury to the chest – Blunt trauma – Penetration by a rib fracture – Many other mechanisms of injury
Tension Pneumothorax Morbidity/Mortality • Profound hypoventilation can result. • Death is related to delayed management. • An immediate, life-threatening chest injury.
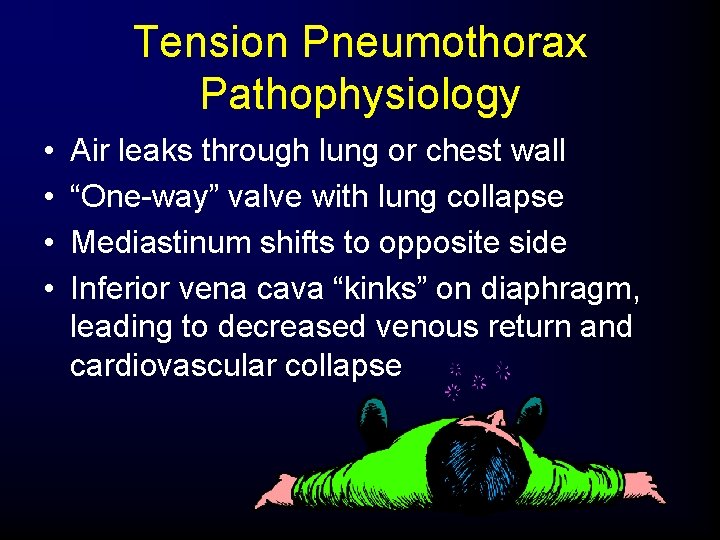
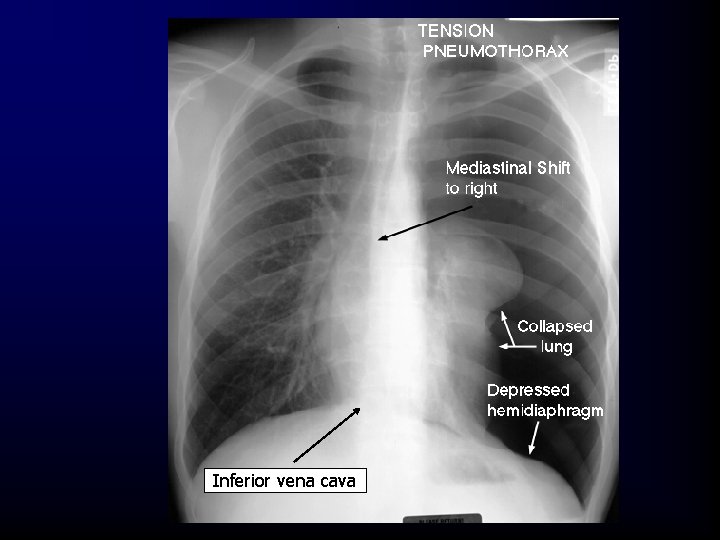
Tension Pneumothorax Pathophysiology • • Air leaks through lung or chest wall “One-way” valve with lung collapse Mediastinum shifts to opposite side Inferior vena cava “kinks” on diaphragm, leading to decreased venous return and cardiovascular collapse
Early Signs – Tension Pneumothorax • • • Extreme anxiety Cyanosis Increasing dyspnea Difficult ventilations while being assisted Tracheal deviation (a late sign) Hypotension Identification is the most difficult aspect of field care in a tension pneumothorax.
Tension Pneumothorax Assessment Findings • Bulging of the intercostal muscles • Subcutaneous emphysema • Jugular venous distention (unless hypovolemic) • Unequal expansion of the chest (tension does not fall with respiration) • Hyperresonnace to percussion
LATE S/S OF TENSION PNEUMOTHORAX • • Jugular Venous Distension (JVD) Tracheal Deviation Narrowing pulse pressure Signs of decompensating shock
MANAGEMENT OF TENSION PNEUMOTHORAX • Emergency care is directed at reducing the pressure in the pleural space. • Airway and ventilation: – High-concentration oxygen – Positive pressure ventilation if necessary • Circulation—relieve the tension pneumothorax to improve cardiac output.
Tension Pneumothorax Management • Nonpharmacological – Occlude open wound – Needle thoracostomy – Tube thoracostomy—in-hospital management Pleural decompression should only be employed if the patient demonstrates significant dyspnea and distinct signs and symptoms of tension pneumothorax.
Tension Pneumothorax Management • Tension pneumothorax associated with penetrating trauma – May occur when an open pneumothorax has been sealed with an occlusive dressing. – Pressure may be relieved by momentarily removing the dressing (air escapes with an audible release of air). After the pressure is released, the wound should be resealed.
Tension Pneumothorax Management • Tension pneumothorax associated with closed trauma – If the patient demonstrates significant dyspnea and distinct signs and symptoms of tension pneumothorax: • Provide thoracic decompression with either a large-bore needle or commercially available thoracic decompression kit. • Insert a 2 -inch 14 - or 16 -gauge hollow needle or catheter into the affected pleural space. – Usually the second intercostal space in the midclavicular line Insert the needle just above third rib to avoid the nerve, artery, and vein that lie just beneath each rib.
Tension pneumothorax • Tension pneumothorax is not an x-ray diagnosis - it MUST be recognized clinically • Treatment is decompression - needle into 2 nd intercostal space of mid-clavicular line followed by thoracotomy tube
Tension pneumothorax • The classic signs of a tension pneumothorax are deviation of the trachea away from the side with the tension, a hyper-expanded chest, an increased percussion note and a hyperexpanded chest that moves little with respiration. • The central venous pressure is usually raised, but will be normal or low in hypovolemic states.
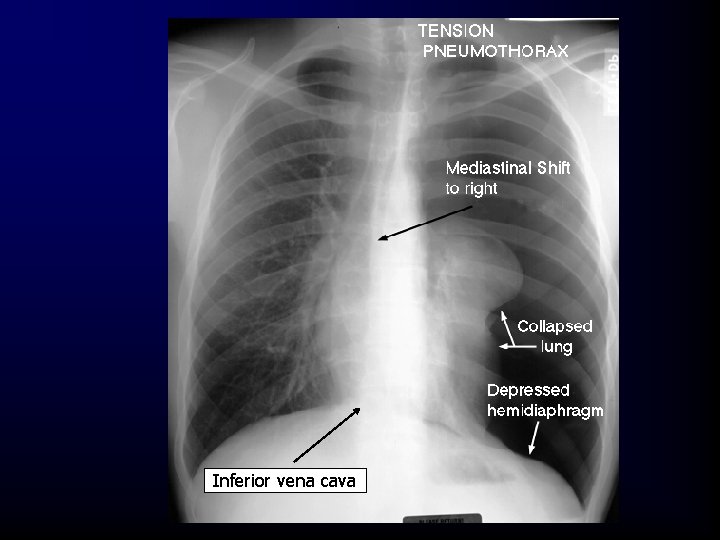
Inferior vena cava
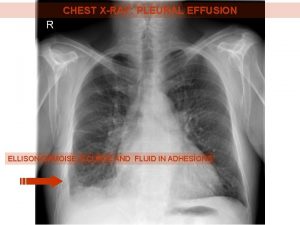
Hemothorax • If this condition is associated with pneumothorax, it is called a hemopneumothorax.
Hemothorax • Incidence – Associated with pneumothorax. – Blunt or penetrating trauma. – Rib fractures are frequent cause.
Hemothorax Morbidity/Mortality • A life-threatening injury that frequently requires urgent chest tube placement and/or surgery • Associated with great vessel or cardiac injury – 50% of these patients will die immediately. – 25% of these patients live 5 to 10 minutes. – 25% of these patients may live 30 minutes or longer.

Massive hemothorax • Rapid accumulation of >1500 cc blood in chest cavity • Hypovolemia & hypoxemia • Neck veins may be: – flat - from hypovolemia – distended - intrathoracic blood • Absent breath sounds, DULL to percussion



Hemothorax Assessment Findings • Tachypnea • Dyspnea • Cyanosis – Often not evident in hemorrhagic shock • Diminished or decreased breath sounds on the affected side
Hemothorax Assessment Findings • Hyporesonance (dullness on percussion) on the affected side • Hypotension • Narrowed pulse pressure • Tracheal deviation to the unaffected side (rare) • Pale, cool, moist skin
Hemothorax Management • Airway and ventilation – High-concentration oxygen – Positive-pressure ventilation if necessary – Ventilatory support with bag-valve mask, intubation, or both
Hemothorax Management • Circulation – Administer volume-expanding fluids to correct hypovolemia – Nonpharmacological—tube thoracostomy
Hemopneumothorax • Pathophysiology—pneumothorax with bleeding in the pleural space – Assessment—findings and management are the same as for hemothorax. – Management—management is the same as for hemothorax.
Pulmonary Contusion • A pulmonary contusion is the most common potentially lethal chest injury. • Incidence – Blunt trauma to the chest » The most common injury from blunt thoracic trauma. » 30% to 75% of patients with blunt trauma have pulmonary contusion. – Commonly associated with rib fracture – High-energy shock waves from explosion – High-velocity missile wounds – Rapid deceleration – A high incidence of extrathoracic injuries – Low velocity—ice pick
Pulmonary Contusion Morbidity/Mortality • May be missed due to the high incidence of other associated injuries Mortality—between 14% and 20%
Pulmonary Contusion Assessment Findings • • • Tachypnea Tachycardia Cough Hemoptysis Apprehension Respiratory distress Dyspnea Evidence of blunt chest trauma Cyanosis
Pulmonary Contusion Management • Airway and ventilation: – High-concentration oxygen – Positive-pressure ventilation if necessary • Circulation—restrict IV fluids (use caution restricting fluids in hypovolemic patients).
Traumatic Asphyxia • Incidence – A severe crushing injury to the chest and abdomen • Steering wheel injury • Conveyor belt injury • Compression of the chest under a heavy object
Traumatic Asphyxia Pathophysiology • A sudden compressional force squeezes the chest. • An increase in intrathoracic pressure forces blood from the right side of the heart into the veins of the upper thorax, neck, and face. • Jugular veins engorge and capillaries rupture.
Traumatic Asphyxia Assessment • Reddish-purple discoloration of the face and neck (the skin below the face and neck remains pink). • Jugular vein distention. • Swelling of the lips and tongue.
Traumatic Asphyxia Assessment – Swelling of the head and neck. – Swelling or hemorrhage of the conjunctiva (subconjunctival petechiae may appear). – Hypotension results once the pressure is released.
Traumatic Asphyxia Management • Airway and ventilation – Ensure an open airway. – Provide adequate ventilation. • Circulation – IV access. – Expect hypotension and shock once the compression is released.
Heart and Great Vessel Injury • Myocardial contusion (blunt myocardial injury) – Incidence • The most common cardiac injury after a blunt trauma to the chest • Occurs in 16% to 76% of blunt chest traumas • Usually results from motor vehicle collisions as the chest wall strikes the dashboard or steering column • Sternal and multiple rib fractures common
Heart and Great Vessel Injury Morbidity/Mortality • A significant cause of morbidity and mortality in the blunt trauma patient – Clinical findings are subtle and frequently missed due to: • Multiple injuries that direct attention elsewhere • Little evidence of thoracic injury • Lack of signs of cardiac injury on initial examination
Heart and Great Vessel Injury Assessment Findings • Retrosternal chest pain • ECG changes – Persistent tachycardia – ST elevation, T wave inversion – Right bundle branch block – Atrial flutter, fibrillation – Premature ventricular contractions – Premature atrial contractions
Heart and Great Vessel Injury Assessment Findings • • New cardiac murmur Pericardial friction rub (late) Hypotension Chest wall contusion and ecchymosis
Heart and Great Vessel Injury Management • Airway and ventilation—high-concentration oxygen • Circulation—IV access • Pharmacological – Antidysrhythmics – Vasopressors
Pericardial Tamponade • Incidence – Rare in blunt trauma – Penetrating trauma – Occurs in less than 2% of all chest traumas
Pericardial Tamponade Morbidity/Mortality • Gunshot wounds carry higher mortality than stab wounds. • Lower mortality rate if isolated tamponade is present.
Pericardial Tamponade Anatomy and Physiology • Pericardium – A tough fibrous sac that encloses heart – Attaches to the great vessels at the base of the heart – Two layers: • The visceral layer forms the epicardium. • The parietal layer is regarded as the sac itself.
Pericardial Tamponade Pathophysiology • A blunt or penetrating trauma may cause tears in the heart chamber walls, allowing blood to leak from the heart. – If the pericardium has been torn sufficiently, blood leaks into the thoracic cavity. If 150 to 200 m. L of blood enters the pericardial space acutely, pericardial tamponade develops.
Pericardial Tamponade Pathophysiology • Increased intrapericardial pressure: – Does not allow the heart to expand refill with blood – Results in a decrease in stroke volume and cardiac output • Myocardial perfusion decreases due to pressure effects on the walls of the heart and decreased diastolic pressures. • Ischemic dysfunction may result in infarction. • Removal of as little as 20 m. L of blood may drastically improve cardiac output.
Pericardial Tamponade Assessment Findings • • Tachycardia Respiratory distress Narrowed pulse pressure Cyanosis of the head, neck, and upper extremities
Pericardial Tamponade Assessment Findings • Beck’s triad – Narrowing pulse pressure – Neck vein distention – Muffled heart sounds
Pericardial Tamponade Assessment Findings • Kussmaul’s sign—a rise in venous pressure with inspiration when spontaneously breathing • ECG changes
Pericardial Tamponade Management • Airway and ventilation • Circulation—IV fluid challenge • Nonpharmacological pericardiocentesis
Traumatic Aortic Rupture • Incidence – Blunt trauma • Rapid deceleration in high-speed motor vehicle crashes • Falls from great heights • Crushing injuries 15% of all blunt trauma deaths
Traumatic Aortic Rupture Morbidity/Mortality • 80% to 90% of these patients die at the scene as a result of massive hemorrhage. – About 10% to 20% of these patients survive the first hour. • Bleeding is tamponaded by surrounding adventitia of the aorta and intact visceral pleura. • Of these, 30% have rupture within 6 hours.
Traumatic Aortic Rupture Pathophysiology • Patients who are normotensive should have limited replacement fluids to prevent an increase in pressure in the remaining aortic wall tissue.
Traumatic Aortic Rupture Assessment Findings • Upper-extremity hypertension with absent or decreased amplitude of femoral pulses – Thought to result from compression of the aorta by the expanding hematoma • Generalized hypertension – Secondary to increased sympathetic discharge • Retrosternal or interscapular pain
Traumatic Aortic Rupture Assessment Findings • About 25% have a harsh systolic murmur over the pericardium or interscapular region • Paraplegia with a normal cervical and thoracic spine (rare)
Traumatic Aortic Rupture Assessment Findings • • Dyspnea Dysphagia Ischemic pain of the extremities Chest wall contusion
Aortic Injury : Suspicion • Mechanism – Falls> 3 m – Major decelaration/acceleration • SIGNS – Neck hematoma – Assymetic pulse or BP – Radiofemoral delay – Severe searing pain
Aortic Injury: CXR Signs • • • Mediastinum > 8 cm Abnormal Aortic contour Opaque artopulmonary window Apical cap Mediastinal displacement Fracture of first rib or scapula



Traumatic Aortic Rupture Management • Airway and ventilation: – High-concentration oxygen – Ventilatory support with spinal precautions • Circulation—do not over-hydrate.
Diaphragmatic Rupture • Incidence • Penetrating trauma – Blunt trauma – Injuries to the diaphragm account for 1% to 8% of all blunt injuries. • 90% of injuries to the diaphragm are associated with high-speed motor vehicle crashes.
Diaphragmatic Rupture Anatomy Review • The diaphragm is a voluntary muscle that separates the abdominal cavity from the thoracic cavity. – The anterior portion attaches to the inferior portion of the sternum and the costal margin. – Attaches to the 11 th and 12 th ribs posteriorly. – The central portion is attached to the pericardium. – Innervated via the phrenic nerve.
Diaphragmatic Rupture • Rupture can allow intra-abdominal organs to enter the thoracic cavity, which may cause the following: – Compression of the lung with reduced ventilation – Decreased venous return – Decreased cardiac output – Shock
Diaphragmatic Rupture Pathophysiology • Can produce very subtle signs and symptoms • Bowel obstruction and strangulation • Restriction of lung expansion – Hypoventilation – Hypoxia • Mediastinal shift – Cardiac compromise – Respiratory compromise
Diaphragmatic Rupture Management • Airway and ventilation – High-concentration oxygen – Positive-pressure ventilation if necessary – Caution: positive-pressure may worsen the injury • Circulation—IV access • Nonpharmacological—do not place patient in Trendelenburg position
Diaphragmatic Rupture Assessment Findings • • • Tachypnea Tachycardia Respiratory distress Dullness to percussion Scaphoid abdomen (hollow or empty appearance) – If a large quantity of the abdominal contents are displaced into the chest • Bowel sounds in the affected hemithorax • Decreased breath sounds on the affected side • Possible chest or abdominal pain
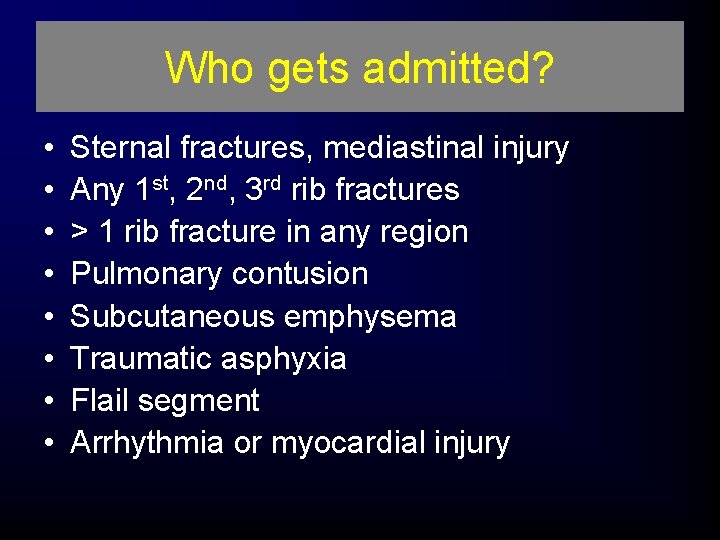
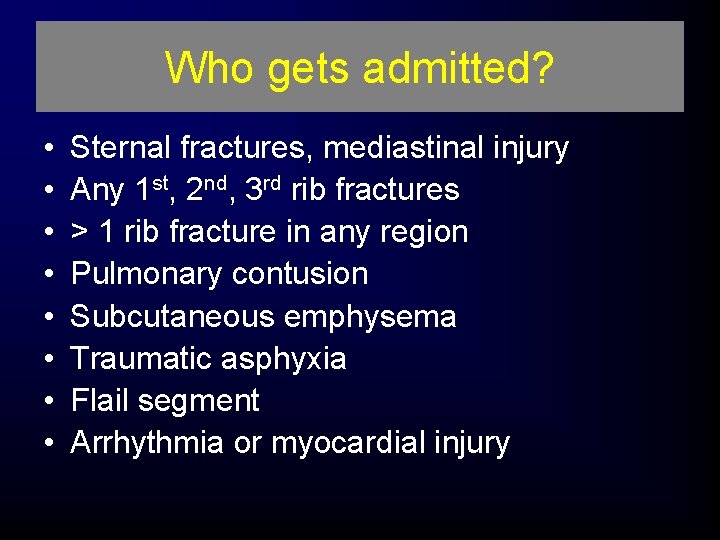
Who gets admitted? • • Sternal fractures, mediastinal injury Any 1 st, 2 nd, 3 rd rib fractures > 1 rib fracture in any region Pulmonary contusion Subcutaneous emphysema Traumatic asphyxia Flail segment Arrhythmia or myocardial injury
In Closing • Back to basics: ABCDE • If you suspect a major chest injury act swiftly • Ask for assistance early • Practice damage control when necessary • Problems with drains? Read the manual or call your friendly trauma tream
• QUESTIONS?
 Victor politi
Victor politi Victor politi
Victor politi Dr victor politi
Dr victor politi Victor politi
Victor politi Lethal six chest trauma
Lethal six chest trauma Rachel politi
Rachel politi Hepburn osteometric board
Hepburn osteometric board Torrance memorial map
Torrance memorial map Ptal california medical board
Ptal california medical board Cartersville medical center medical records
Cartersville medical center medical records Greater baltimore medical center medical records
Greater baltimore medical center medical records 12 lead ecg color code
12 lead ecg color code Tactile fremitus anterior
Tactile fremitus anterior Chest tube parts
Chest tube parts Dullness percussion sound
Dullness percussion sound Shield chest
Shield chest Petmac chest pain
Petmac chest pain Chest physiotherapy assignment
Chest physiotherapy assignment Chest abnormalities
Chest abnormalities Chest thightness
Chest thightness Sitting duck heart persistent truncus arteriosus
Sitting duck heart persistent truncus arteriosus Anterior respiratory assessment
Anterior respiratory assessment Table position
Table position Lung assessment landmarks
Lung assessment landmarks Supine chest xray
Supine chest xray Lobar pneumonia
Lobar pneumonia Mitral stenosis chest x ray
Mitral stenosis chest x ray General parasitology lecture notes
General parasitology lecture notes Thorax cavity
Thorax cavity Chest pain in pediatrics
Chest pain in pediatrics Tga cxr
Tga cxr Chest x ray lateral view positioning
Chest x ray lateral view positioning Barrel chest
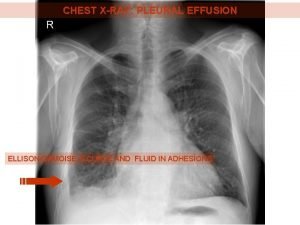
Barrel chest Pleural effusion ellis curve
Pleural effusion ellis curve Rash on upper chest and back
Rash on upper chest and back Uninterrupted suture
Uninterrupted suture The world overflowing like a treasure chest
The world overflowing like a treasure chest Heart sounds on chest
Heart sounds on chest Type of position in nursing
Type of position in nursing Nursing diagnosis for stable angina
Nursing diagnosis for stable angina Narmer king of egypt
Narmer king of egypt Petits triangle
Petits triangle Latent tb chest x ray
Latent tb chest x ray Deep chest muscles
Deep chest muscles Neck part of body
Neck part of body Thorax anatomy
Thorax anatomy The scarlet letter chapters 23-24
The scarlet letter chapters 23-24 Tension pneumothorax triad
Tension pneumothorax triad Knee chest position
Knee chest position What the vagus nerve controls
What the vagus nerve controls Chest wiggle factor
Chest wiggle factor How to read growth chart
How to read growth chart Chest pediatric pulmonary board review
Chest pediatric pulmonary board review Trauma tumpul thorax
Trauma tumpul thorax Chest ais
Chest ais Chest compressions
Chest compressions Chest fy
Chest fy Tactile fremitus
Tactile fremitus Clin chest med
Clin chest med Mitral stenosis chest x ray
Mitral stenosis chest x ray Flail chest paradoxical breathing
Flail chest paradoxical breathing Percussion of posterior thorax
Percussion of posterior thorax Timex fitness hrm
Timex fitness hrm Which side is your heart on
Which side is your heart on Barrel chest
Barrel chest Chest xray labelled
Chest xray labelled Where to place chest tube
Where to place chest tube Rickets forehead
Rickets forehead Triangle of safety chest tube
Triangle of safety chest tube ömpsq
ömpsq Typical chest pain
Typical chest pain Lateral knee chest position
Lateral knee chest position Causes chest pain
Causes chest pain Stabbing pain in chest
Stabbing pain in chest Fascia of thorax
Fascia of thorax Chest compression for infant 2 rescuer
Chest compression for infant 2 rescuer Internal thoracic vein
Internal thoracic vein Chest area name
Chest area name Tidaling
Tidaling Chest and back muscles
Chest and back muscles Barrel chest
Barrel chest Thorasic surgeon
Thorasic surgeon Shrine box/chest definition
Shrine box/chest definition Mason liker
Mason liker What is pigeon chest
What is pigeon chest Right lung lateral view
Right lung lateral view What is tactile fremitus
What is tactile fremitus Bilateral chest tubes
Bilateral chest tubes Renalia chest
Renalia chest Friction rub lung sounds
Friction rub lung sounds Ankylosing spondylitis
Ankylosing spondylitis Poppies poem context
Poppies poem context Whats a flail chest
Whats a flail chest Cvs x ray
Cvs x ray Flail chest symptoms
Flail chest symptoms Auscultate posterior thorax
Auscultate posterior thorax Chest wall tumors
Chest wall tumors Supine position
Supine position Open chest wound first aid
Open chest wound first aid Hila lung
Hila lung Retrosternal chest pain
Retrosternal chest pain Chronic bronchitis
Chronic bronchitis Ctas triage
Ctas triage Flail chest
Flail chest Mass
Mass Chest leads vs limb leads
Chest leads vs limb leads Transudate
Transudate Chest indrawing
Chest indrawing Pediatric life support algorithm
Pediatric life support algorithm Thoracic wall boundaries
Thoracic wall boundaries Seekers quorum chest
Seekers quorum chest Nbronchitis
Nbronchitis Pulmonary trauma
Pulmonary trauma Michael jackson chest
Michael jackson chest Sucking chest wound
Sucking chest wound Deadly dozen trauma
Deadly dozen trauma Water seal suction chest tube
Water seal suction chest tube 50 shades of chest pain
50 shades of chest pain Kronigs isthmus
Kronigs isthmus Fcps pulmonology
Fcps pulmonology Right middle lobe collapse
Right middle lobe collapse London chest günlük yaşam aktiviteleri ölçeği
London chest günlük yaşam aktiviteleri ölçeği Chest spring test positive
Chest spring test positive Chest oblique position
Chest oblique position Hypogammaglobulenemia
Hypogammaglobulenemia Funnel chest
Funnel chest Chest 2012
Chest 2012 Chest quadrants
Chest quadrants Audio compression test
Audio compression test Agnosist
Agnosist Barrel chest emphysema
Barrel chest emphysema Introduction to cpr
Introduction to cpr Blunt medical definition
Blunt medical definition Ample trauma
Ample trauma Tarn trauma
Tarn trauma Trauma acustico terapia
Trauma acustico terapia Glucocorticoides
Glucocorticoides Zone of irritation
Zone of irritation Ballistic trauma
Ballistic trauma Cinematica
Cinematica Jiggling type of trauma
Jiggling type of trauma Trauma institut mainz
Trauma institut mainz Seinsheimer classification
Seinsheimer classification Antemortem vs perimortem
Antemortem vs perimortem Trauma informed practice
Trauma informed practice Askep trauma mata
Askep trauma mata Ao trauma
Ao trauma Types of physical trauma
Types of physical trauma How to treat suspension trauma
How to treat suspension trauma Wikimedia
Wikimedia Trauma termico
Trauma termico Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma What is trauma
What is trauma Trauma informed legal advocacy
Trauma informed legal advocacy Facial trauma
Facial trauma How to do a trauma timeline
How to do a trauma timeline Vicarious trauma
Vicarious trauma Trauma informed practice
Trauma informed practice Tscc screening form
Tscc screening form Mike huggins
Mike huggins Trauma hepatico clasificacion
Trauma hepatico clasificacion Trauma awareness and treatment center utah
Trauma awareness and treatment center utah Signos duros y blandos de lesion vascular
Signos duros y blandos de lesion vascular Certified clinical trauma professional
Certified clinical trauma professional Trauma score
Trauma score Verstehensmodell
Verstehensmodell Trauma informed workplace
Trauma informed workplace Trauma healing centers
Trauma healing centers Biomekanika trauma
Biomekanika trauma Trauma status giesecke
Trauma status giesecke Ritmos de parada cardiorrespiratória
Ritmos de parada cardiorrespiratória Trauma symptom inventory tsi
Trauma symptom inventory tsi Trauma
Trauma Sns and pns
Sns and pns 4 r's trauma informed care
4 r's trauma informed care Trauma acronym
Trauma acronym Trauma who cares
Trauma who cares Trauma bonding quotes
Trauma bonding quotes Childhood trauma test
Childhood trauma test Ruptur ginjal grade
Ruptur ginjal grade