Trauma from occlusion v Every tissue in the

- Slides: 56
Trauma from occlusion
v Every tissue in the human body has got the ability to adapt according to the functional, physiologic and environmental changes occurring in and around it or to it. This adaptive capacity of a tissue creates a range so that when the tissue is stressed to its limit or within the limit, still functions without any pathology occurring in it. But when this range or limit is crossed or over stressed – tissue injury or pathology occurs. The adaptive capacity or the range forms an inherent margin of safety for that particular tissue.
v. E. g. v Skin, Mucosa → Stress → Keratinization → Still increased stress/irritation leads to → Malignant change
v Just like any other tissue in the body even the periodontal tissue has got an inherent margin of safety to occlulsal forces, but when these forces exceed the adaptive capacity of the periodontium tissue injury results. This tissue injury is referred to as trauma from occlusion and the occlusion which produces/causes such an injury is known as traumatic occlusion
v WHO 1978: v Damage in the periodontium caused by stress on the teeth produced directly or indirectly by teeth of opposing jaw. v AAP 1986: v An injury to the attachment apparatus as a result of excessive force.
classification 1 a) Acute b) Chronic 2 a) Primary b) Secondary
Criteria: The main criteria that determines whether the occlusion is traumatic or not is not how the teeth occlude. Ø Any occlusion that produces injury is traumatic Ø An occlusion esthetically and anatomically acceptable might be functionally traumatic and other hand highly mal occlusion might be nontraumatic. Ø
Acute v This results from an abrupt change in occlusion/occlusal force such as produced by Biting on hard object Over hang Over filling Faculty restoration/prosthesis
v The teeth might exhibit signs of acute trauma. pain, sensitivity to percussion, mobility etc. v The injury, mobility heals after removal of the irritant, removal of overfilling/prosthesis. If the condition is not treated then the condition might worsen and might lead to a chronic lesion. Sometimes cemental tears have also been found to occur with acute trauma.
Chronic v Chronic trauma from occlusion is the more common form and is of great significance. v Chronic trauma from occlusion is produced over a period of time by tooth wear, migration, extrusion of teeth etc. compounded with habits such as bruxism and clenching.
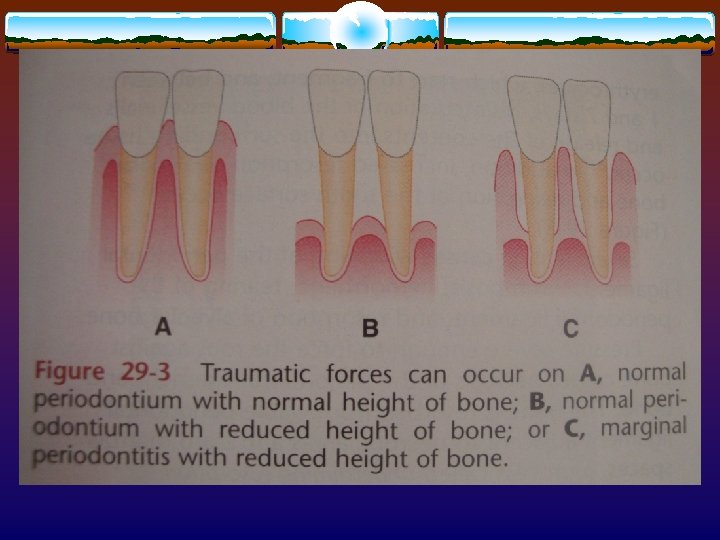
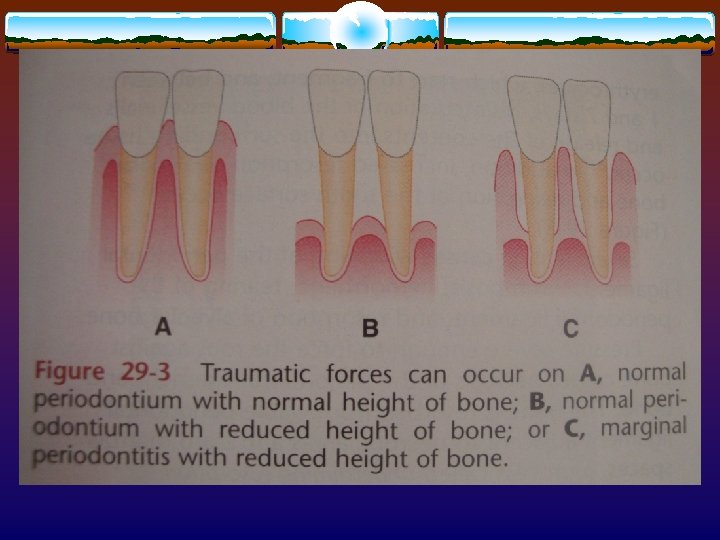
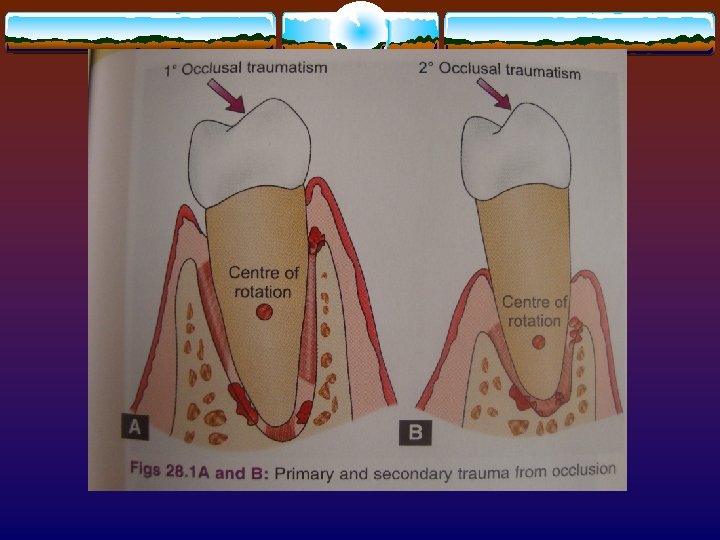
Primary Trauma from Occlusion v Primary form includes a tissue reaction or damage elicited around a tooth with normal height of periodontium. v The changes in the periodontium are because of changing occlusal forces and the local alterations to which a tooth is subjected from occlusion. :
For example 1 High filling. 2 Improper prosthesis. 3 Drifting of teeth into areas of missing teeth. 4 Orthodontic movement of teeth into functional unacceptable positions.
v there is no alteration in the connective tissue attachment level and do not initiate pocket formation.
Secondary Trauma from Occlusion v Secondary form is related to situations in which occlusal forces cause injury in a periodontium of a reduced height. This occurs when the adaptive capacity of the periodontium to withstand occlusal forces is impaired by bone loss resulting from marginal inflammation.
The result is that there is more force/Unit area of attachment. Thus the periodontium becomes vulnerable to injury and previously well tolerated forces become traumatic.
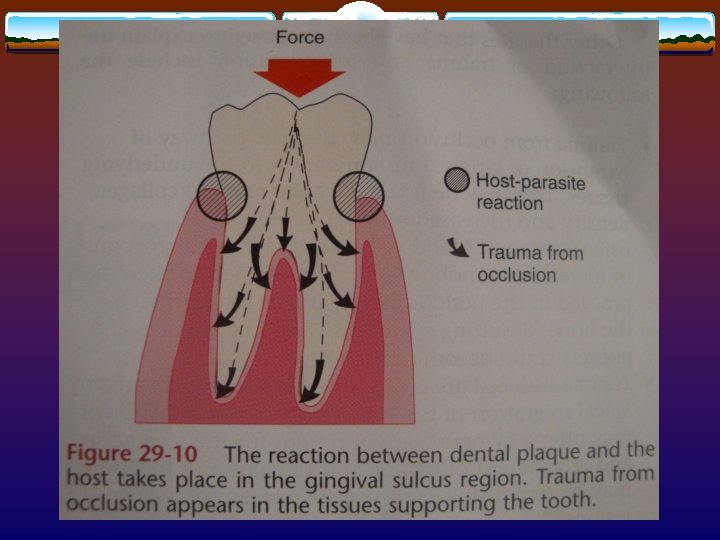
Trauma From Occlusion and Plaque Associated Periodontitis v Way back in 1901 Karolyi postulated that an interaction existed between trauma from occlusion and alveolar pyorrhea. Various opinions have been postulated for and against the same, over the years. v Box and Stone (1938) in experiments done on monkeys and sheep they showed that TFO is and etiologic factor in a variety of periodontal disease in which there is vertical bone loss in associated teeth
v Presently there are 2 main concepts on the relationship between TFO and periodontal disease given by: Glickman (1965, 1967) and 2. Waerhaug’s (1979) these concepts were based on studies done on human autopsy material. 1.
v In studies done on human autopsy material they assessed: 1. Lesions histopathologically 2. The presence and apical extensions of the microbial plaque 3. Mobility of teeth involved and 4 Occlusal scrutiny of the sites involved
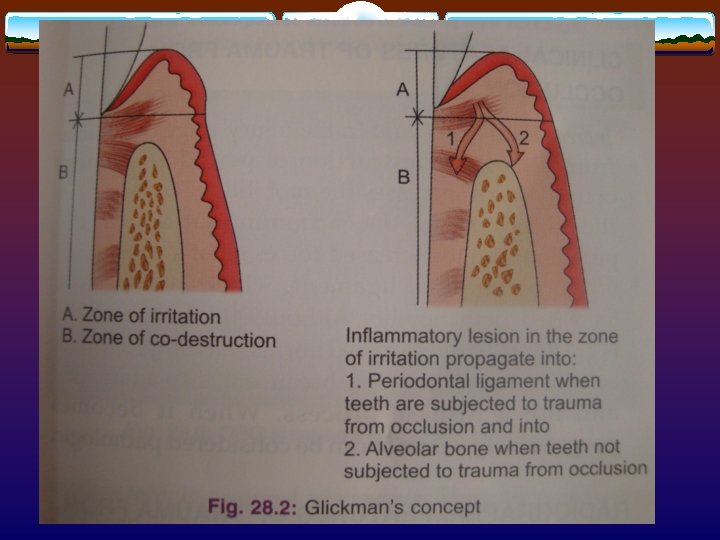
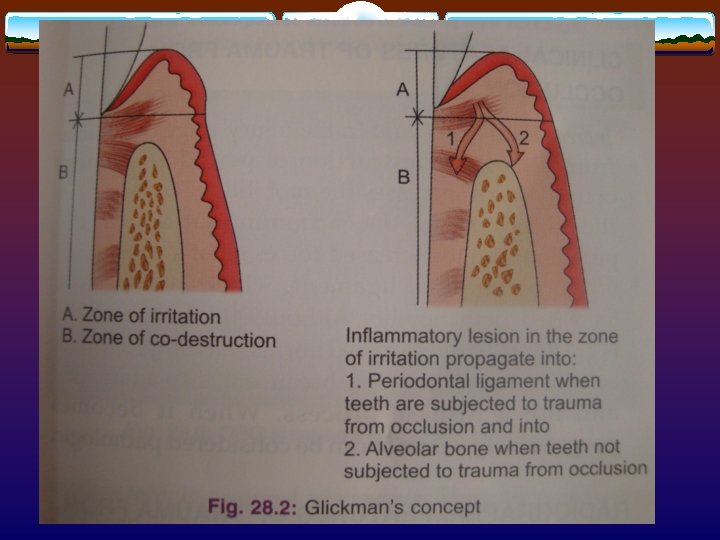
GLICKMAN’S CONCEPTS 1965, 1967: v We know that the normal path of progression of periodontal diseases is: v Gingiva → Alveolar bone → PDL v He said that trauma altered this path of spread of infection to: v Gingiva → PDL → Alveolar bone
v This said that the spread of infection and tissue destruction in a traumatized tooth was different than for a non-traumatized tooth. v Instead of even destruction of alveolar bone and PDL with suprabony pockets, with horizontal bone loss, the regions exposed to trauma developangular defects and infrabony pockets.
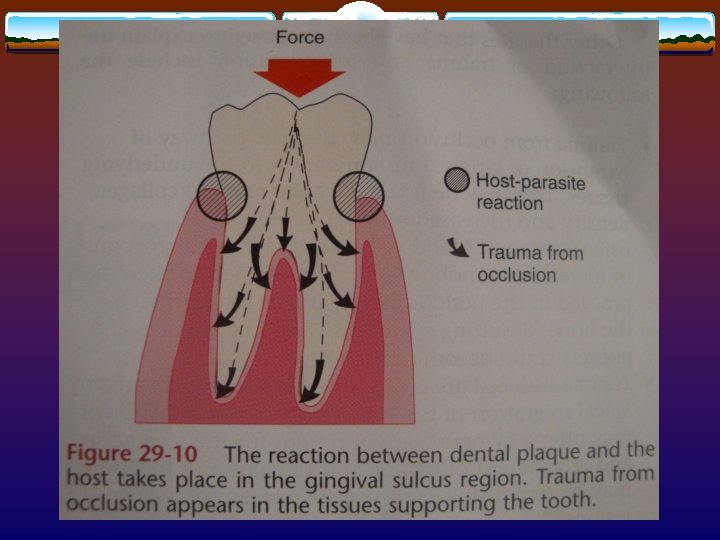
In order to understand this we divide the periodontium into 2 parts: Zone of irritation 2. Zone of co-destruction 1.
Zone of irritation: v This includes the marginal gingival and interdental gingiva. The soft tissue is bordered only one side by hard tissue i. e. the tooth and is not effected by the forces of occlusion. v This means that TFO does cause gingivitis. v Gingivitis is because of the plaque and its products v Tooth → Bone → PDL Horizontal bone loss
Zone of Co-destruction: v This zone includes the PDL, alveolar bone and root cementum. v This zone is separated from the zone of irritation by the supracrestal fibres. v This tissue is the seat of a lesion caused by TFO v The fibre bundles which separate the zones of Codestruction from zone of irritation can be affected in 2 directions:
1. 2. v v From the microbial plaque inflammatory lesion From trauma induced changes in zone of Codestruction Because of the action of the injurious agents from 2 different direction the fibres get oriented in a direction parallel to root surface. This facilitates the spread of infection from zone of irritation to directly into the PDL space rather than through alveolar bone.
v This alteration in “Normal” pathway leads to spread of plaque association inflammatory lesion and development of angular defects
WAERHAUG’S CONCEPT (1979): v This study was similar to Glickman’s but he also measured the distance between the subginginval plaque and 1. Periphery of the associated inflammatory cell infiltrate in the gingiva 2. Surface of the alveolar bone
v From this study he concluded that angular bony defects and infrabony pockets occur equally often at periodontal sites of teeth which are not affected by TFO as in traumatized teeth.
v This refutes the Glickman’s concept that TFO has a role in spreads of infection in the zone of codestruction. v The resorption of bone and pocketing are only because of plaque and its microbial effect. v This said that infrabony pockets occurred when the subgingival plaque reached an area apical to than the adjacent tooth and the volume of the alveolar bone surrounding the root is large.
Response of the Periodontium to Increased External Forces v When the periodontium is stressed to its limits, the tissue response occurs in 3 stages: 1. Injury 2. Repair 3. Adaptive remodeling of the periodontium
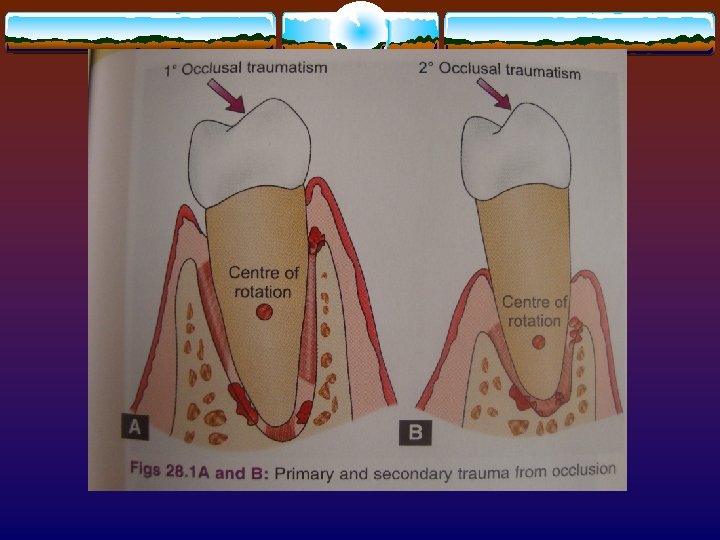
v Tissue injury is produced by excessive occlusal forces, the tissue then attempts to repair and restore the periodontium. This occurs if the forces are diminished or the tooth drifts away from the traumatizing forces. v If the offending force is chronic, the periodontium is remodelled to cushion its impact. The ligament is widened at the expense of the bone resulting in angular defects without periodontal pockets and the tooth becomes mobile.
v Under these forces the tooth moves around an axis of rotation, which is located, in single rooted teeth at the junction between middle and apical 1/3 rd of the clinical root, which creates different degrees of pressure and tension and depend upon the type of the forces. v The furcation areas are the areas most susceptible to injury
v As a result of tissue injury there is a temporary depression in the mitotic activity and the rate of proliferation and differentiation of fibroblasts in collagen formation and in bone formation. v Once the forces are removed the tissues return to normal.
2. Repair: Repair is constantly occurring in normal periodontium and trauma stimulates the reparative activity. The damaged tissues are removed and new connective tissue cells, bone, fibres and cementum are formed in an attempt to restore the injured periodontium. v The forces remain traumatic only as long as the damage produced exceeds the reparative capacity of the tissues.

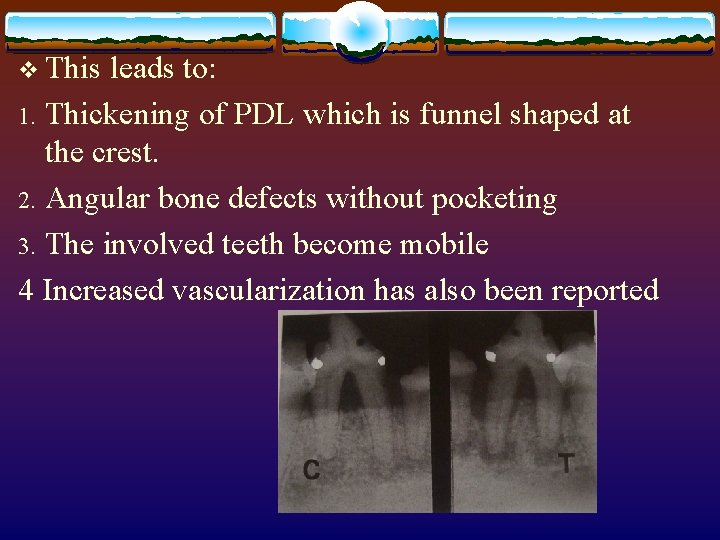
3. Adaptive Remodeling of the Periodontium: Force → Injury → Repair, v are at an equilibrium the active tissue injury will be at bay. But if the reparative capacity cannot keep up with the destruction caused by occlusion, the periodontium is remodelled in an effort to create a structural relationship in which the forces are no longer injurious.
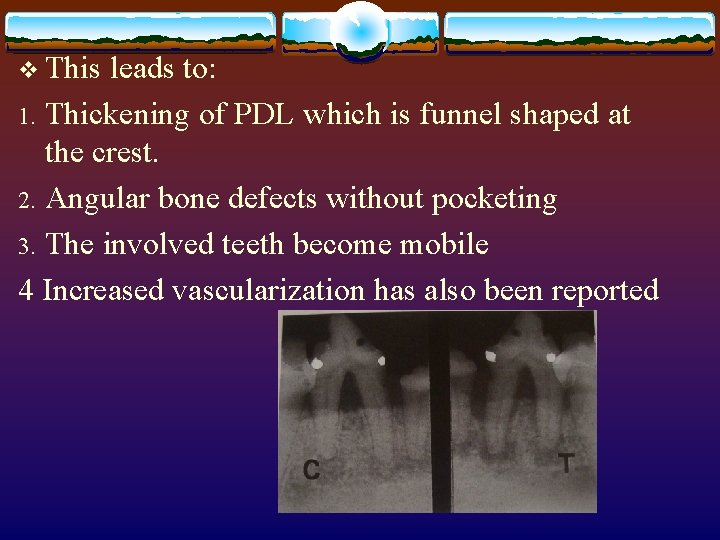
v This leads to: Thickening of PDL which is funnel shaped at the crest. 2. Angular bone defects without pocketing 3. The involved teeth become mobile 4 Increased vascularization has also been reported 1.
Mechanism v To understand the changes taking place within the periodontal tissues various experiments were carried out in different animal models.
1. Slightly excessive pressure v At sites of pressure: v There is increased vascularity → Increased permeability → Thrombosis → Disorganisation of cells and collagen fibres → If this is within limits then the vitality of the cells is maintained → Osteoclasts appear and resorb the bone. This is known as direct bone resorption.
At the sites of tension: Stretching of the periodontal ligament fibres ↓ Engorgement of vessels ↓ Increased blood flow ↓ Apposition of bone
2. Greater pressure: v At sites of pressure: v There is compression of the fibres → De-composition of fibres and death of cells → Necrosis of ligament. v Vascular changes in 30 mins. → Stasis of flow after 23 hrs. → Packing of RBC’s and fragmentation of RBC’s → (1 -7 days) Disintegration of the vessel wall → release of contents into surrounding tissues.
v Necrosis and hyalinization of the ligament → Osteoclasts appear from adjacent areas → Resorb bone. This is known as indirect resorption or Undermining resorption. v Areas of tension: v Tearing of fibres → Hemorrhage → Resorption of bone instead of formation.
v Severe pressure: v Causes the root to appose against the bone – leads to necrosis of the PDL and bone. When bone is resorbed by excessive occlusal forces the body tries to compensate for this by formation of bone and this compensatory mechanism is known as buttressing bone formation. v Bone is resorbed by the viable cells from the adjacent healthy PDL area and marrow spaces by undermining resorption/indirect resorption.
v Pressure and Tension → hypermobility of teeth → tilting of teeth → escape from forces → nullification → adaptation → stabilization of tooth.
v The buttressing bone formation is an important feature of reparative phase associated with TFO. Also seen in osteolytic tumors and carcinomas. v This buttressing formation can be either – 1 Central 2 Peripheral
v In central buttressing the endosteal cells deposit new bone, which restores the bony trabeculae and reduces the size of marrow spaces. v Peripheral buttressing occurs on buccal and lingual surfaces- “Lipping” v Some times cartilage like material is also deposited.
JIGGLING TYPE OF TRAUMA: v The fact that in humans like in other animals the trauma is not unilateral, the kind of direction of forces in humans has been described as JIGGLING type. This indicates forces acting from all sides something like torquing/shearing forces
Clinical and Radiographic Features
Clinical: 1. Increased mobility – injury stage - destruction of PDL fibres and because of widening of PDL space after remodeling – This mobility because of adaptation is normal and is not pathologic because it is an adaptation and not a disease, but if it becomes progressively mobile then it is considered to be pathologic. 2. Pain in acute cases.
3 Fremitus test – This is the clinical test done to check the presence of trauma in the anterior region. v Test: Place the moist finger on the labial surface of the upper anterior teeth and instruct the patient to bite with his back teeth. Feel for any vibrations on the finger.
v Grading: v I – When only vibration is felt and there is no mobility. v II – When the mobility of the teeth is felt but not clinically visible. v III – When there is overt, clinically visible mobility present. v To evaluate the TFO in posterior region it is advisable to do a cast mounting on an articulator.
Radiographic: i) Increased width of PDL space. ii) Thickening of lamina dura. iii) Vertical bone loss. iv) Root resorption.
Treatment: 1. 2. Coronoplasty Splinting
conclusion Trauma from occlusion does not initiate gingivitis or periodontal pockets, but it may act as an additional risk factor for the progression and severity of the disease.