CHEST TRAUMA Sept 42003 Todd Ring Gord Mc



- Slides: 115

CHEST TRAUMA Sept 4/2003 Todd Ring Gord Mc. Neil
Overview n n Approach to patient with chest trauma Pulmonary injuries: – – – n n Management of occult pneumothorax OR intervention for hemothorax Imaging of pulmonary contusion Traumatic aortic injury: imaging modalities Blunt and penetrating cardiac injury – Role of ED Thoracotomy n n Chest wall and other injuries Gord’s chest trauma cases
Epidemiology n n n 2 nd commonest cause of traumatic death after head injuries (USA = 16, 000 deaths per year) 25% of all trauma related deaths 10 % mortality 5 – 10 % of pediatric trauma admissions but higher mortalilty – – – 5% mortality when isolated 25 % mortality with head or abdominal trauma 40 % mortality when head, abdominal and chest injury
Initial Management and Assessment n n ABC’s Six Immediately Life Threatening Injuries: – – – n n airway obstruction flail chest tension pneumothorax open peumothorax massive hemothorax cardiac tamponade All can be identified in the primary survey CXR not necessary to make the diagnosis
Secondary Survey n n n More detailed examination including reassessment of items covered in primary survey Appropriate investigations: CXR, pulse oximeter, EKG, ABG Identify “potentially” lethal chest injuries – simple pneumothorax, hemothorax, pulmonnary contusion, tracheobronchial tree injury, blunt cardiac injury, traumatic aortic injury, diaphragmatic injury, wounds transversing the mediastinum
Classification 1) Chest wall injuries 50% – rib fractures, flail chest, sternal fractures 2) Pulmonary injuries 25% – pulmonary contusion, hemothorax, pneumothorax, tracheo-bronchial disruption 3) Cardiovascular injuries 20% – myocardial contusion, aortic disruption, cardiac rupture/tamponade 4) Other 5% – esophageal/diaphragmatic injuries
Mr. C. Tube 22 yo male driver MVC. Unrestrained found 10 feet from vehicle. GCS 8 at scene. Intubated for airway protection. Hemodynamically stable. CXR normal. CT head and spine normal. CT abdomen demonstrates small pneumothoracies, no abdominal pathology. – What features on supine CXR useful in identifying pneumothoracies? – Does this patient require a chest tube? – Does he require antibiotic prophylaxis if he gets a chest tube?
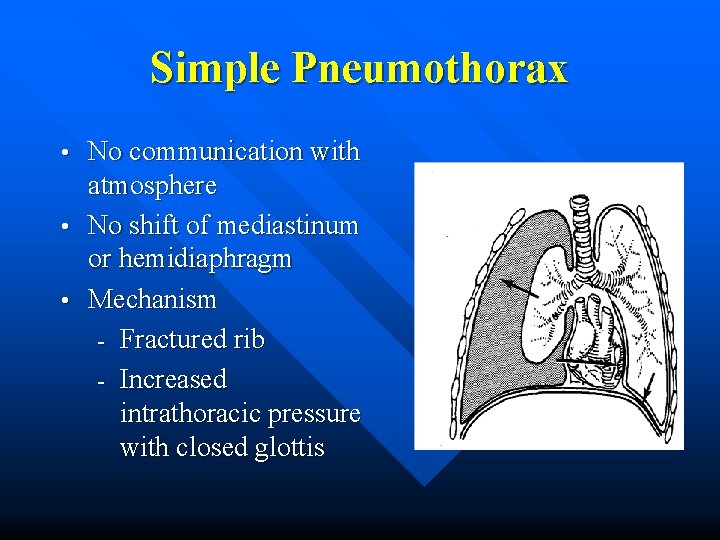
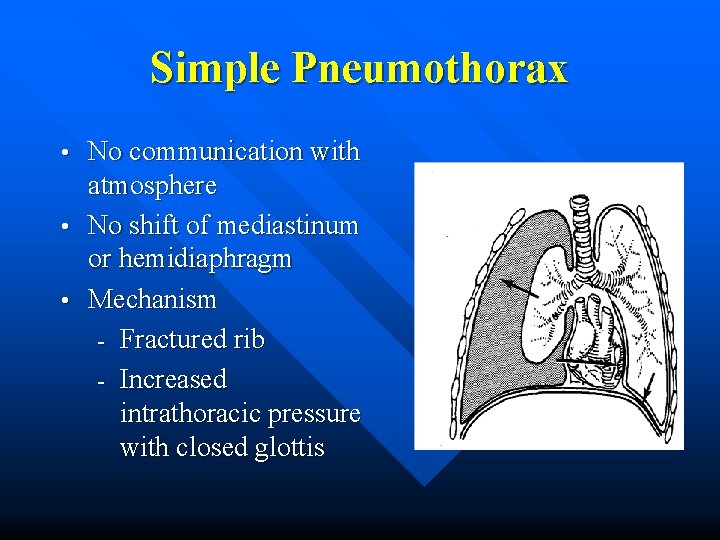
Simple Pneumothorax No communication with atmosphere • No shift of mediastinum or hemidiaphragm • Mechanism - Fractured rib - Increased intrathoracic pressure with closed glottis •
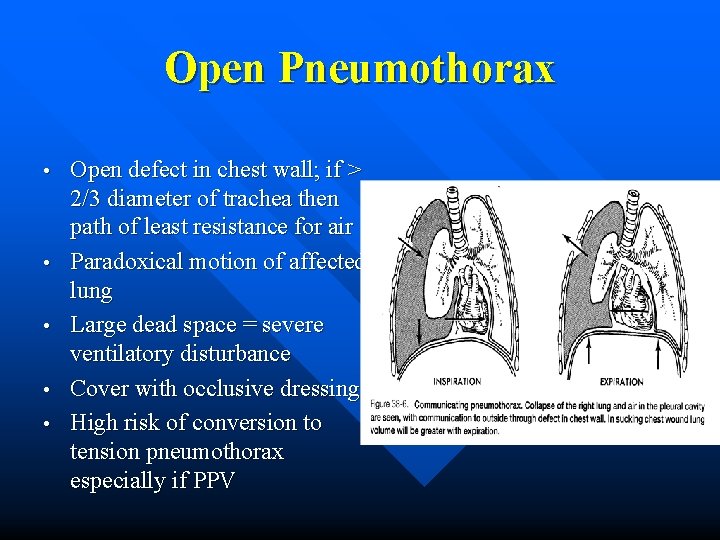
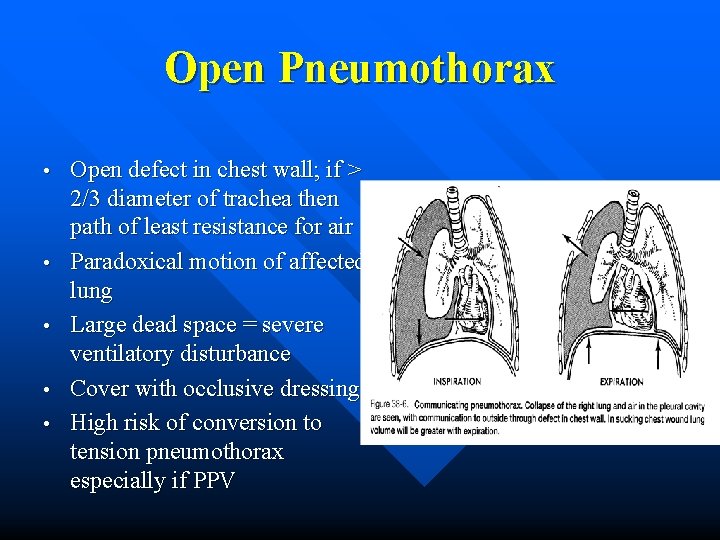
Open Pneumothorax • • • Open defect in chest wall; if > 2/3 diameter of trachea then path of least resistance for air Paradoxical motion of affected lung Large dead space = severe ventilatory disturbance Cover with occlusive dressing High risk of conversion to tension pneumothorax especially if PPV
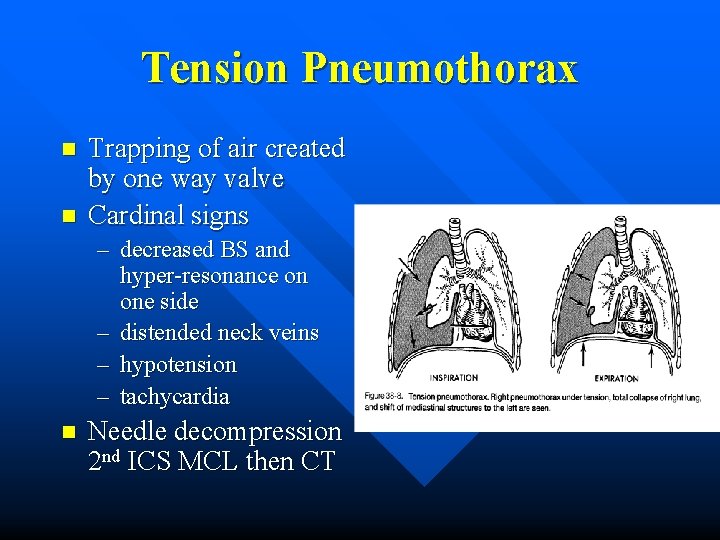
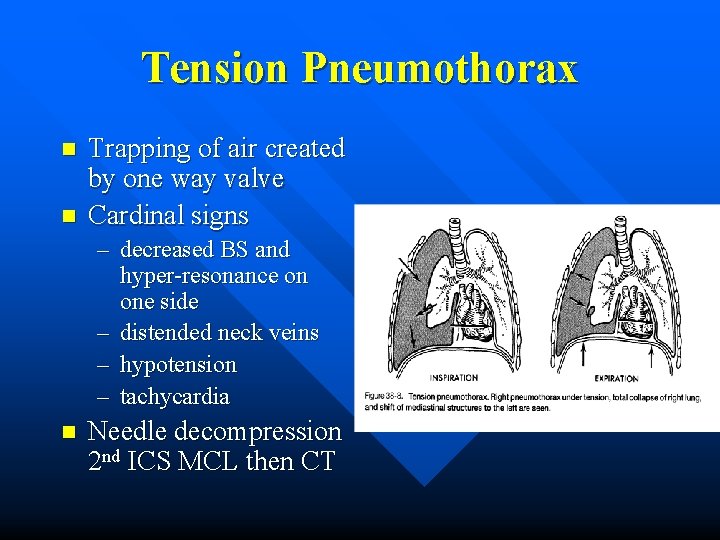
Tension Pneumothorax n n Trapping of air created by one way valve Cardinal signs – decreased BS and hyper-resonance on one side – distended neck veins – hypotension – tachycardia n Needle decompression 2 nd ICS MCL then CT
Pneumothorax on CXR Frequently missed (20 -30%) on initial trauma CXR (small size or supine position) n If pneumothorax suspected: n – sit patient up – expiration film – repeat in 3 hours – +/- indication for CT chest
Pneumothorax on Supine Film n Deep sulcus sign – deep lucent costophrenic sulcus Depression of involved hemidiaphragm n Hyperlucency in lower chest n Double diaphragm sign n – Seen at interface of dorsal and ventral pneumothorax with anterior and posterior aspects of hemidiaphragm
Pneumothoarx on CXR Estimation of size of pneumothorax n Generally inaccurate – varies with inspiratory effort and shift of mediastinum n – From lateral chest wall (~4 th rib) 1 cm = 10%, 2 cm = 20% – Generally intervention is indicated if >20%
Treatment of Occult Pneumothoracies Occult pneumothoracies are often missed on CXR and found on abdominal CT scans—do these patients need chest tubes? • Brasel et al. conducted a prospective, randomized trial comparing CT to observation in 39 patients with pneumothoracies from blunt chest trauma (including 9 patients in each group with PPV) • there was no difference in overall complication rate (progression of pneumo or resp. distress) - no patient had respiratory distress related to the OPTX or required emergent CT - Brasel et al. Treatment of occult pneumothoraces from blunt trauma. Journal of Trauma-Injury Infection & Critical Care. 46(6): 987 -90
Occult Pneumothorax in MV Patients n Enderson et al. studied forty trauma patients with occult pneumothorax who were prospectively randomized to management with CT (n = 19) or observation (n = 21) in MV patients – 8 of 21 patients observed had progression of their pneumothoraces on PPV with 3 developing tension pneumothorax – no patients with CT suffered major complications – hospital and ICU stays were not increased by CT – they concluded that patients with occult pneumothorax on PPV should undergo tube thoracostomy Enderson et al. Tube thoracostomy for occult pneumothorax: a prospective randomized study of its use. Journal of Trauma-Injury Infection & Critical Care. 35(5): 726 -9
Chest Tube Indications • • • Traumatic cause of pneumothorax Moderate-to-large pneumothorax Respiratory distress Increasing size with conservative therapy Recurrence after removal of chest tube Patient requires ventilation Hemothorax Bilateral pneumothorax (regardless of size) Tension pneumothorax Marx: Rosen's Emergency Medicine: Concepts and Clinical Practice, 5 th ed. , Copyright © 2002 Mosby, Inc.
Chest Tube Complications • Complications: - • neurovascular bundle damage, intrapulmonary insertion, subcutaneous emphysema, bronchopleural fistula Bailey et al. performed a retrospective case series of all trauma patients who underwent chest tube over a one year period to determine rates of complications in trauma patients 57 CT’s placed in 47 patients with no insertional complications and only one major complication - they concluded no need to decrease rates of CT - Bailey et al. Complications of tube thoracostomy in trauma. Journal of Accident & Emergency Medicine. 17(2): 111 -4, 2000 Mar.
Antibiotic Prophylaxis in Patients with Chest Tubes n n Reported incidence of empyema 1. 6 – 26 % after chest tube Mandal et al. recommend antibiotics for emergent or urgent thoracotomy, shotgun blast to chest wall, lung contusion with hemoptysis, exploratory lap, or open long bone fracture – 5474 patients followed protocol with only 1. 6% developed empyema Mandal et al. Post traumatic empyema. Risk factor analysis. Arch Surg 1997; 132: 647 -651.
Antibiotics con’t… n Richardson’s review article from 7 RTC’s comparing antibiotics vs. none – Infection rate in placebo 20. 9% vs. 4. 5 % in treatment Richardson. Thoracic infection after trauma. Chest Surg. Clin NA. 1997; 7: 401 -426 n n No infectious complications in hemothoracies > 500 cc (often thought to be nidus for infection) Staph aureus most common pathogen; gram negative, anaerobes also pathogens
Air Travel Following Pneumothorax n n Aerospace Medicine Association recommends waiting 2 -3 weeks after radiographic resolution of pneumothorax prior to air travel Cheatham et al. conducted a prospective study of air travel following pneumothorax – 12 patients who flew 14 days after pneumothorax resolved had no symptoms – 2 patients who flew within 14 days; one patient developed symptoms Cheatham et al. Air travel following traumatic pneumothorax. When is it safe? Am Surg. 1999; 65: 1, 160 -4.
“Stick-em up!” 41 year old male, “minding his own business, ” single GSW to R chest by small caliber handgun. Tachycardic. BP 90/50. Decreased BS to R chest. CXR opacification of R lung. CT on R initial drainage 1000 cc. – Does this patient require immediate OR?
Hemothorax • • • Accumulation of blood in pleural space Can cause severe hypovolemia, shock, and decrease vital capacity Generally due to injured lung parenchyma – usually self-limiting More severe bleeding from intercostal and internal mammary arteries Uncommonly from great vessels
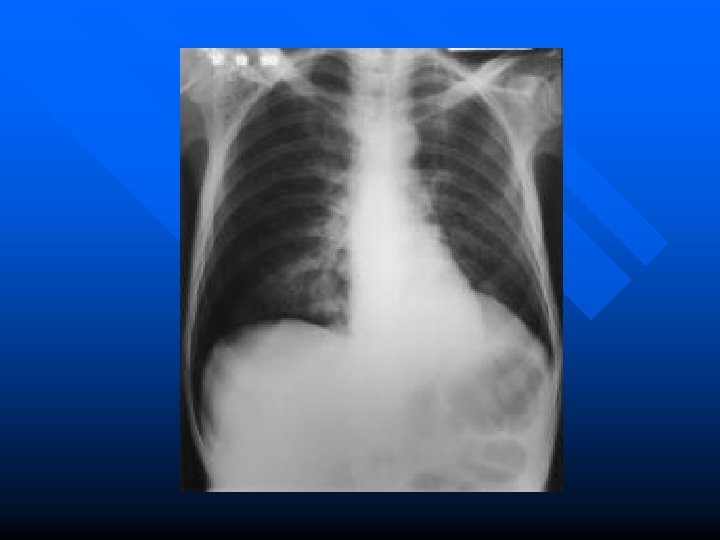
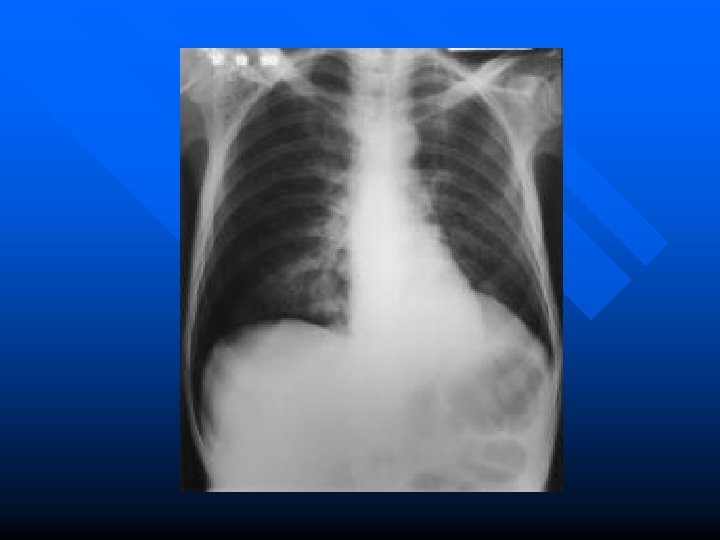
Xray in Hemothorax n n n Poor ability to predicit amount of blood in chest cavity using CXR 250 ml required to cause blunting of costophrenic angle on upright On supine film fluid layers posteriorly – increased density over hemithorax n 25 % of cases associated with pneumothorax – may see air fluid level on upright CXR n CT more sensitive than CXR but generally clinically insignificant if not visible on CXR
Treatment #38 chest tube at midaxillary line n BIG PROBLEM = BIG CUT = BIG TUBE n
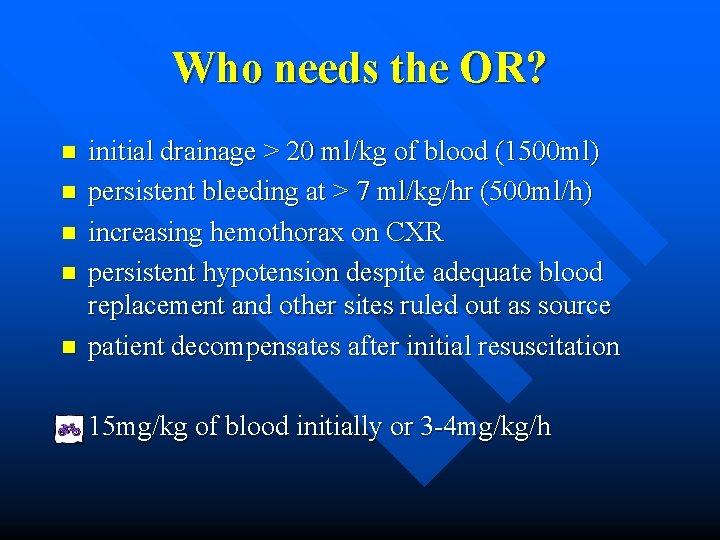
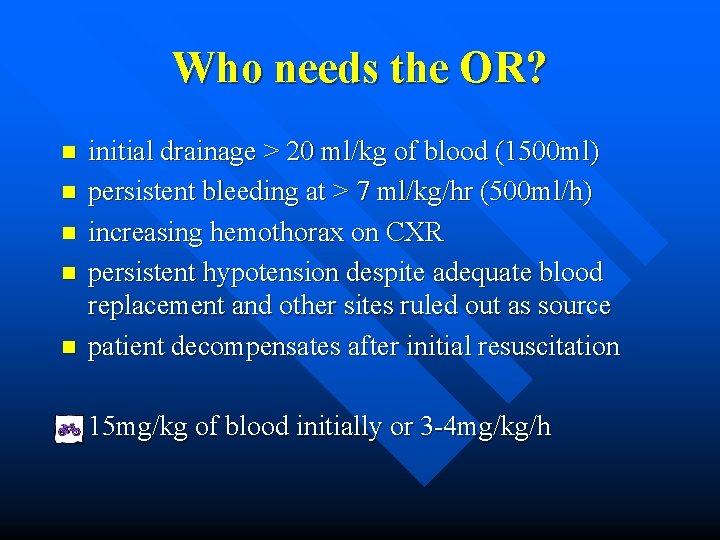
Who needs the OR? n n n initial drainage > 20 ml/kg of blood (1500 ml) persistent bleeding at > 7 ml/kg/hr (500 ml/h) increasing hemothorax on CXR persistent hypotension despite adequate blood replacement and other sites ruled out as source patient decompensates after initial resuscitation 15 mg/kg of blood initially or 3 -4 mg/kg/h
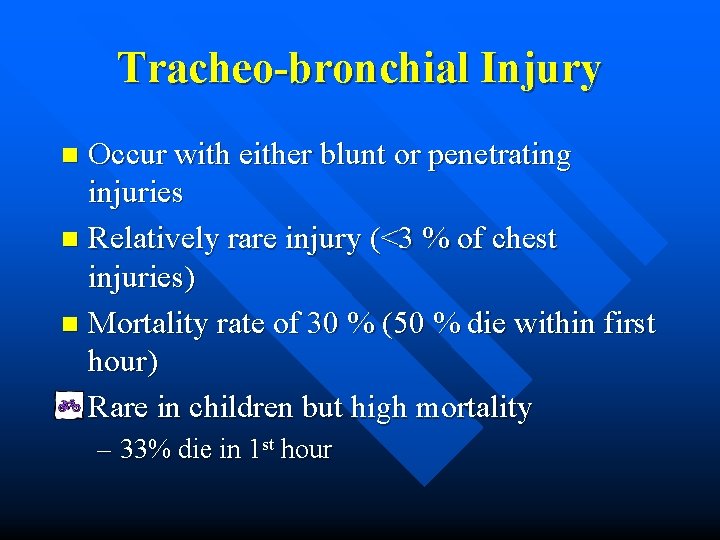
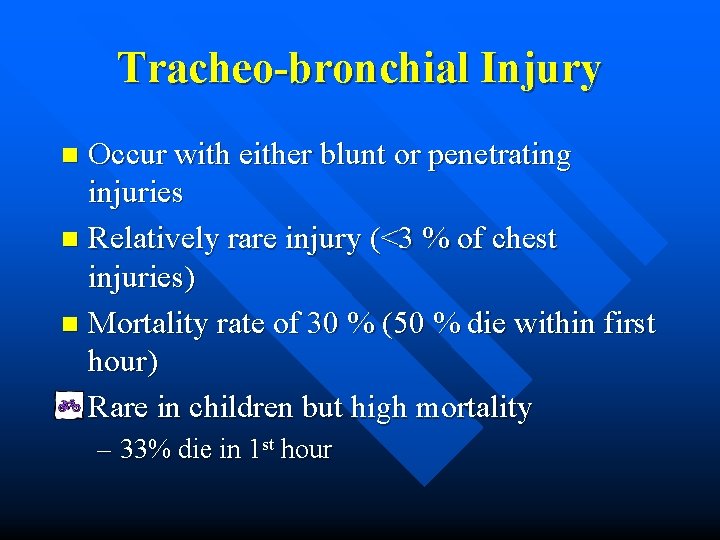
Tracheo-bronchial Injury Occur with either blunt or penetrating injuries n Relatively rare injury (<3 % of chest injuries) n Mortality rate of 30 % (50 % die within first hour) Rare in children but high mortality n – 33% die in 1 st hour
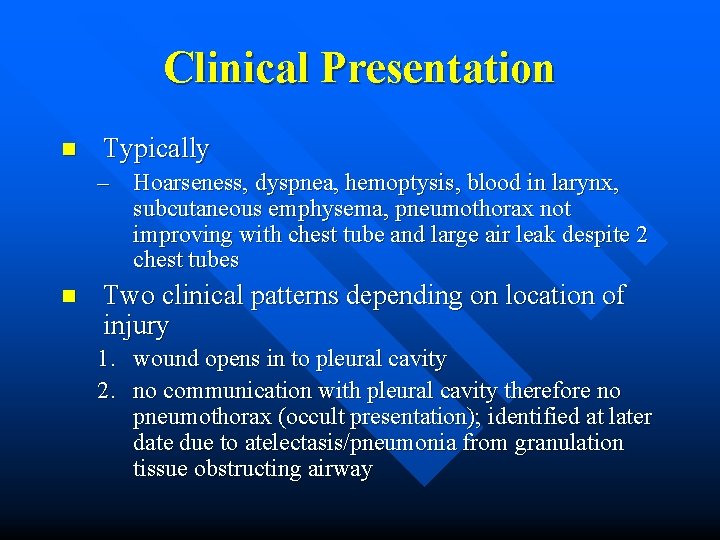
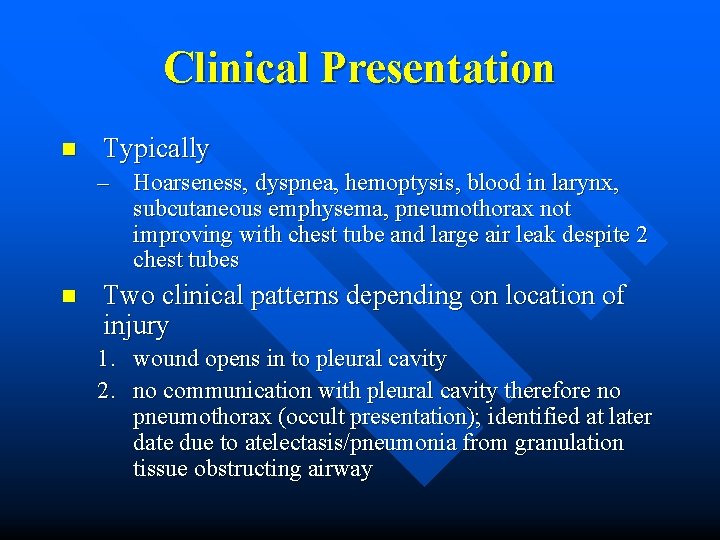
Clinical Presentation n Typically – Hoarseness, dyspnea, hemoptysis, blood in larynx, subcutaneous emphysema, pneumothorax not improving with chest tube and large air leak despite 2 chest tubes n Two clinical patterns depending on location of injury 1. wound opens in to pleural cavity 2. no communication with pleural cavity therefore no pneumothorax (occult presentation); identified at later date due to atelectasis/pneumonia from granulation tissue obstructing airway
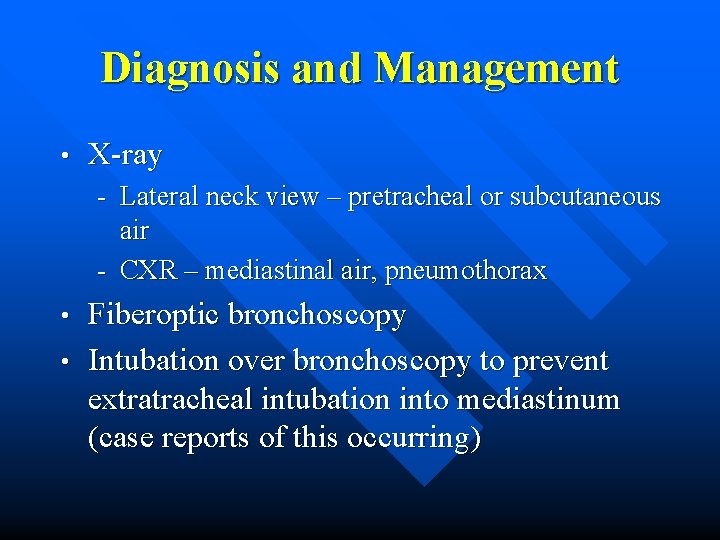
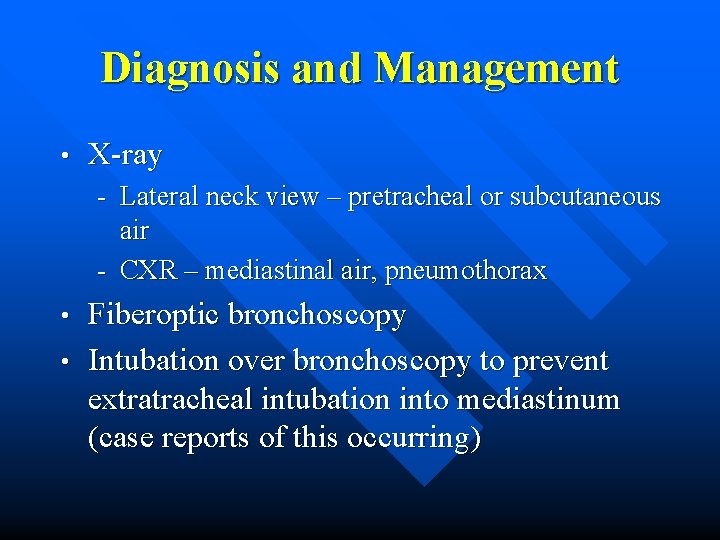
Diagnosis and Management • X-ray - Lateral neck view – pretracheal or subcutaneous air - CXR – mediastinal air, pneumothorax Fiberoptic bronchoscopy • Intubation over bronchoscopy to prevent extratracheal intubation into mediastinum (case reports of this occurring) •
Pulmonary Contusion n Most common injury following chest trauma Often in combination with other injuries such as rib fracture or flail chest Bleeding from laceration of lung parenchyma Most common thoracic injury in pediatric trauma Often isolated injury due to pliable chest wall
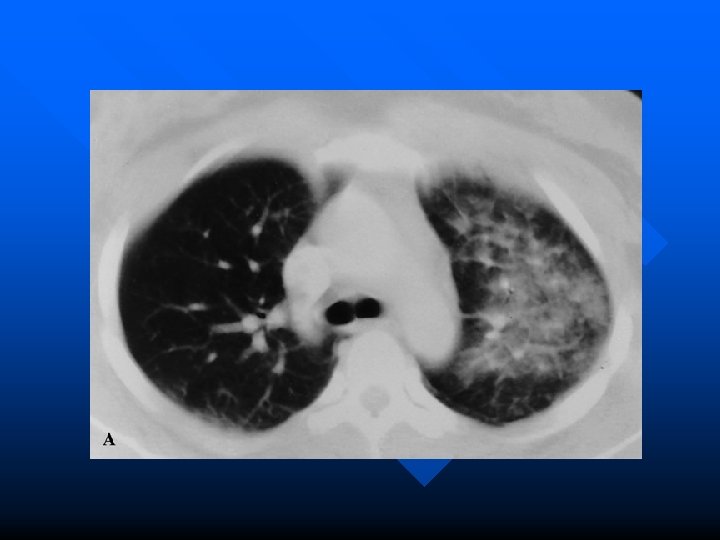
Imaging in Pulmonary Contusion n Contusion usually present on initial CXR and always appears within 6 hours Appear as patchy or diffuse airspace disease Can identify occult contusions on chest CT but clinically utility unclear – Guerro-Lopez et al. conducted a cohort study of 375 patients. One group received admission CT the other CXR. – Induced therapy changes in 30 % of patients but no effect on MV, ICU stay or mortality Guerrero-Lopez F, Vazquez-Mata G, Alcazar-Romero PP, et al. Evaluation of the utility of computed tomography in the initial assessment of the critical care patient with chest trauma. Crit Care Med 2000; 28: 1370 -5

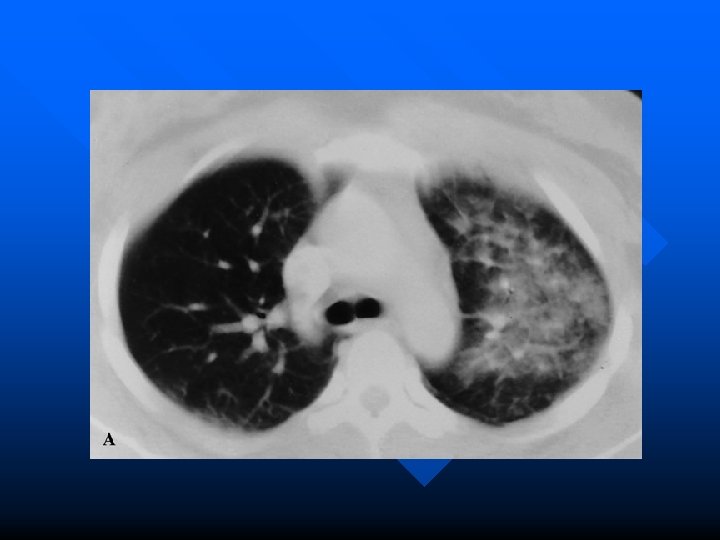
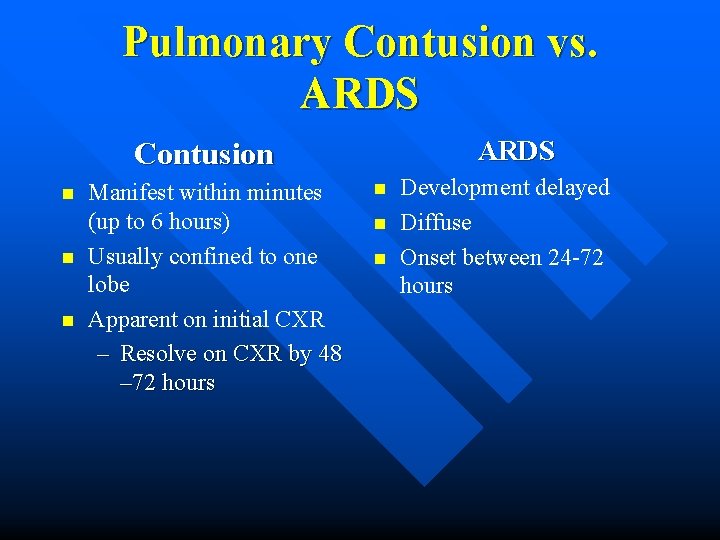
Pulmonary Contusion vs. ARDS Contusion n Manifest within minutes (up to 6 hours) Usually confined to one lobe Apparent on initial CXR – Resolve on CXR by 48 – 72 hours n n n Development delayed Diffuse Onset between 24 -72 hours
Management Hospitalize for observation n Chest physio/incentive spirometry/ analgesia/supplemental O 2 n In patients who remain hospitalized greater than 48 h and have progression of CXR finding should prompt suspicion of other diagnosises including ARDS or aspiration n
Mrs. Dee Sellaration 55 yo female. Driver of single vehicle MVC into telephone pole (approx 70 kph). Restrained. Airbag deployed. LOC at scene GCS 3. Intubated. Tachycardic but BP 90/50. – Findings on CXR to suggest TAI? – What is the next imaging study of choice? – How aggressive do you fluid resuscitate this patient?
Great Vessel Injury n Injury of high speed MVC – mortality 1947 < 1% – mortality now 15 % More frequent with penetrating trauma (90%) n Aorta most commonly injured; high mortality associated with this injury Rare in pediatrics—almost all secondary to MVC n
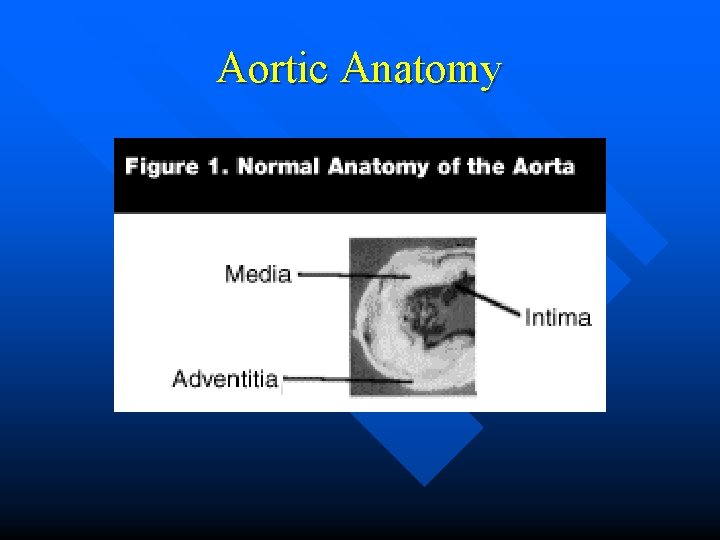
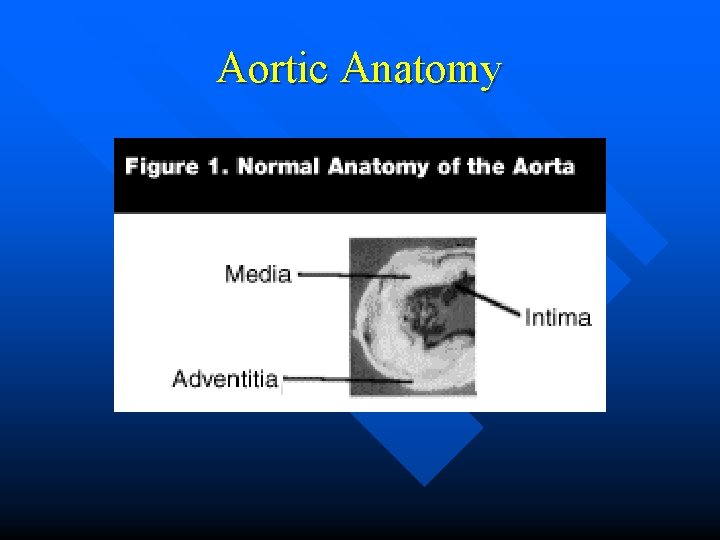
Aortic Anatomy
Pathologic Terminology Traumatic aortic injury: generic term that covers all of the below; should be used to describe the lesion until injury fully defined n Aortic traumatic rupture: full thickness disruption of the wall n Aortic traumatic tear: partial thickness tear limited to intima and muscularis n Aortic traumatic intimal tear: disruption of the intima n
Who cares about terminology? Most patients presenting to the ED with TAI have a partial thickness injury n Of those patients suffering a complete TAI n – 80 – 85 % exsanguinate at the scene, 15 -20% arrive in the ED alive – of these 50% exsanguinate in the first 24 hours; 80% by one week and 95% by four months – 2 – 5 % long term survivors
Risk factors for Aortic Injury n Dyer et al. conducted a prospective study of 1561 patients with suspected aortic injury over 5 year period – Only significant RF was high speed MVC (>60 kph) – No association for front vs. side impact, ejection, fatality, sudden deceleration, damage – No blunt TAI from fall < 10 feet – Concluded by recommended the liberal use of chest CT in blunt chest trauma Dryer et al. Thoracic Aortic Injury: How Predictive Is Mechanism and Is Chest Computed Tomography a Reliable Screening Tool? Journal of Trauma 2000; 48: 673 -683
Location, location. . . 55 - 65% involve proximal descending aorta n 10 -15% ascending aorta or arch n 12% distal n 13 -18% multiple sites n Patients with ascending aorta tears have a 70 -80% incidence of associated lethal injuries n – pericarditis, tamponade, aortic valve tear, coronary artery injury
Prehospital Management Good evidence to avoid military anti-shock trousers elevates BP n No effective in field therapy for injuries to the great vessels therefore “scoop and run” best pre-hospital management n ATLS recommends 1 -2 L fluid bolous for patients in shock to return BP to “normal” HOWEVER. . . n
Fluid Restriction in TAI n n n Bickell et al. conducted a prospective trial of penetrating torso trauma in patients with SBP < 90 Fluid restricted group received no fluid rescusitation until arrival at OR Control group received standard resuscitation – 203/289 (70 %) patients in restricted group survived to hospital d/c compared to 193/309 (62 %) of control group Bickell et al. Immediate versus Delayed Fluid Resuscitation for Hypotensive Patients with Penetrating Torso Injuries. NEJM 331: 1105 -1109
Clinical Presentation History n MVC: impact, duration of extraction, intrsuion, blood loss n Penetrating trauma: length of knife, firearm type, number of rounds fired and distance Physical Examination n Do not disregard the possibility of aortic injury based on patients clinical apperance
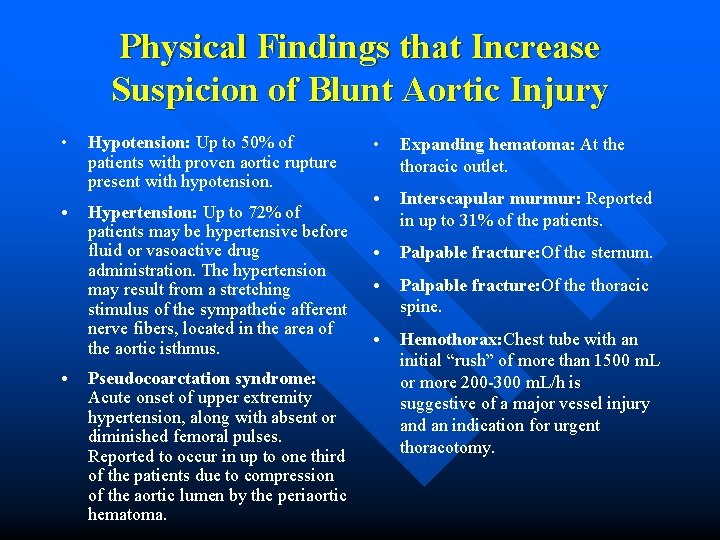
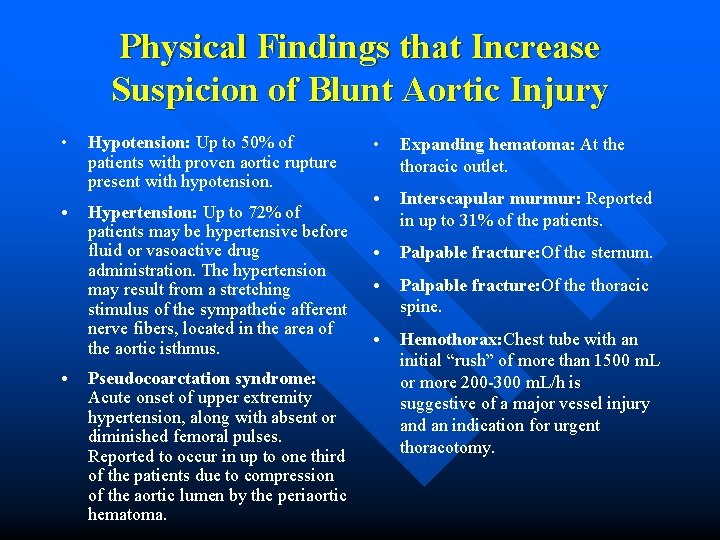
Physical Findings that Increase Suspicion of Blunt Aortic Injury • Hypotension: Up to 50% of patients with proven aortic rupture present with hypotension. • Hypertension: Up to 72% of patients may be hypertensive before fluid or vasoactive drug administration. The hypertension may result from a stretching stimulus of the sympathetic afferent nerve fibers, located in the area of the aortic isthmus. • Pseudocoarctation syndrome: Acute onset of upper extremity hypertension, along with absent or diminished femoral pulses. Reported to occur in up to one third of the patients due to compression of the aortic lumen by the periaortic hematoma. • Expanding hematoma: At the thoracic outlet. • Interscapular murmur: Reported in up to 31% of the patients. • Palpable fracture: Of the sternum. • Palpable fracture: Of the thoracic spine. • Hemothorax: Chest tube with an initial “rush” of more than 1500 m. L or more 200 -300 m. L/h is suggestive of a major vessel injury and an indication for urgent thoracotomy.
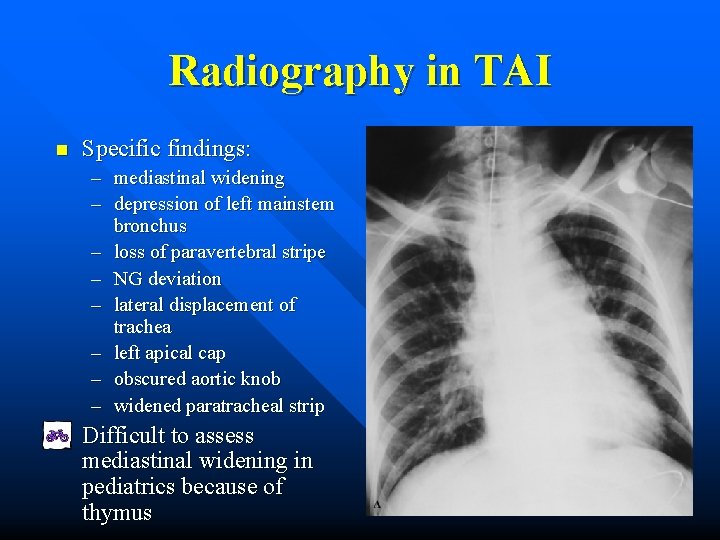
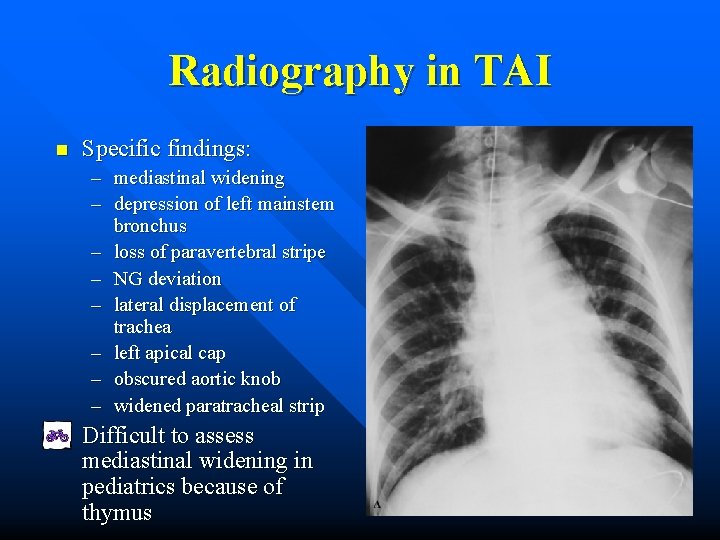
Radiography in TAI n Specific findings: – mediastinal widening – depression of left mainstem bronchus – loss of paravertebral stripe – NG deviation – lateral displacement of trachea – left apical cap – obscured aortic knob – widened paratracheal strip Difficult to assess mediastinal widening in pediatrics because of thymus
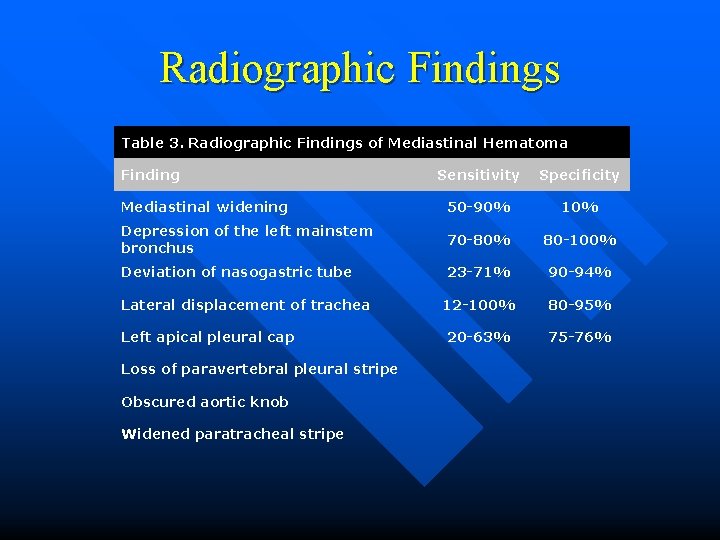
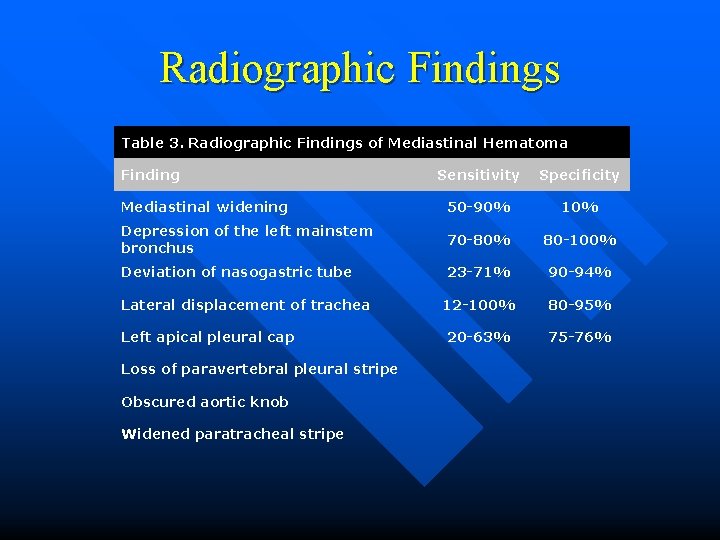
Radiographic Findings Table 3. Radiographic Findings of Mediastinal Hematoma Finding Sensitivity Specificity Mediastinal widening 50 -90% 10% Depression of the left mainstem bronchus 70 -80% 80 -100% Deviation of nasogastric tube 23 -71% 90 -94% 12 -100% 80 -95% 20 -63% 75 -76% Lateral displacement of trachea Left apical pleural cap Loss of paravertebral pleural stripe Obscured aortic knob Widened paratracheal stripe
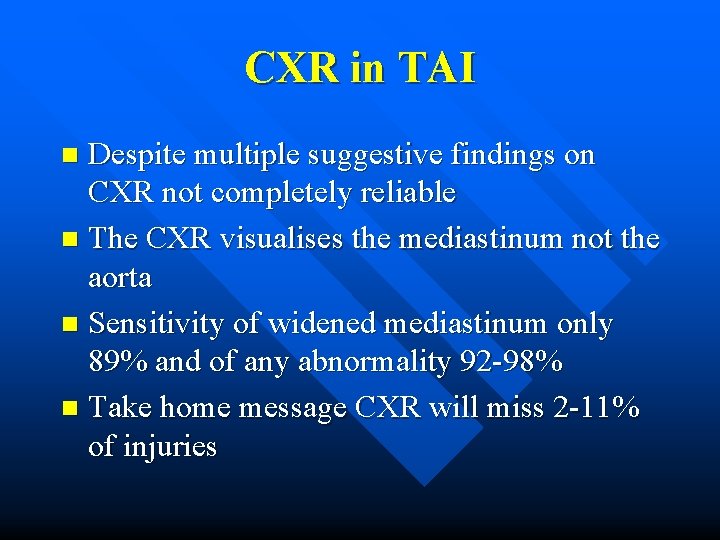
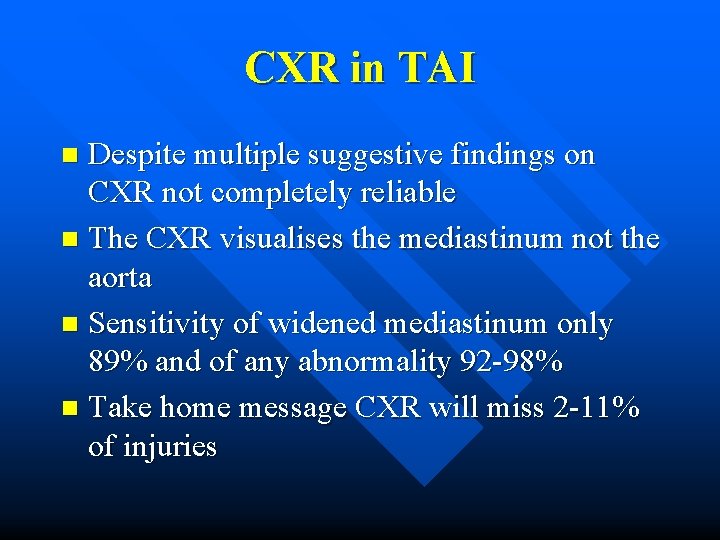
CXR in TAI Despite multiple suggestive findings on CXR not completely reliable n The CXR visualises the mediastinum not the aorta n Sensitivity of widened mediastinum only 89% and of any abnormality 92 -98% n Take home message CXR will miss 2 -11% of injuries n
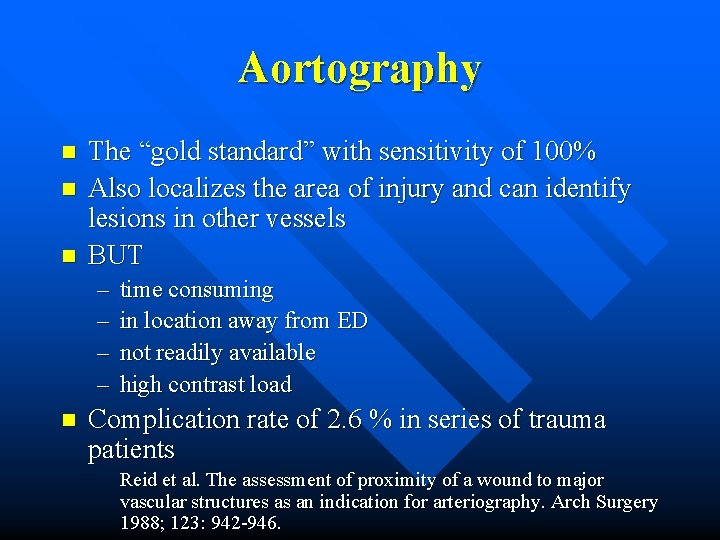
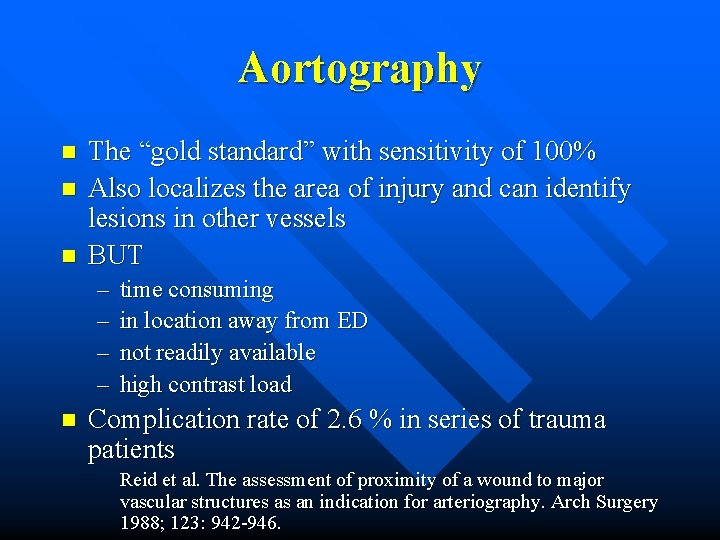
Aortography n n n The “gold standard” with sensitivity of 100% Also localizes the area of injury and can identify lesions in other vessels BUT – – n time consuming in location away from ED not readily available high contrast load Complication rate of 2. 6 % in series of trauma patients Reid et al. The assessment of proximity of a wound to major vascular structures as an indication for arteriography. Arch Surgery 1988; 123: 942 -946.
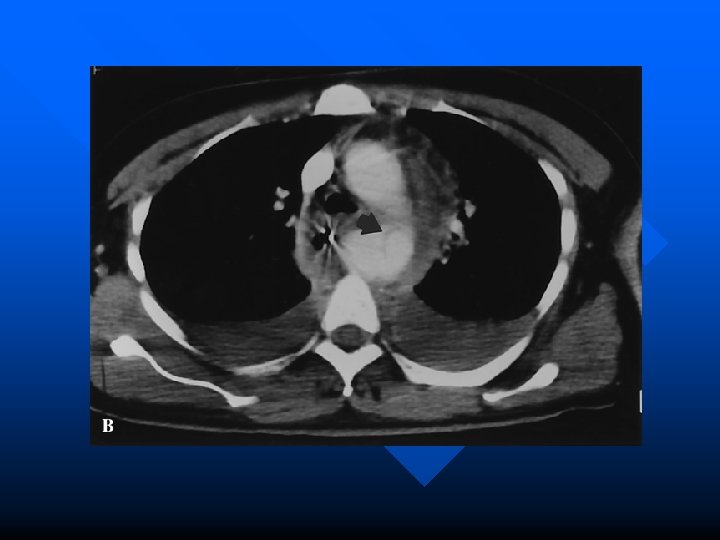
Chest CT n Many advantages over aortography – readily accessible in most urban ED’s – low complication rate – less contrast – fast – gives information about structures other than the aorta
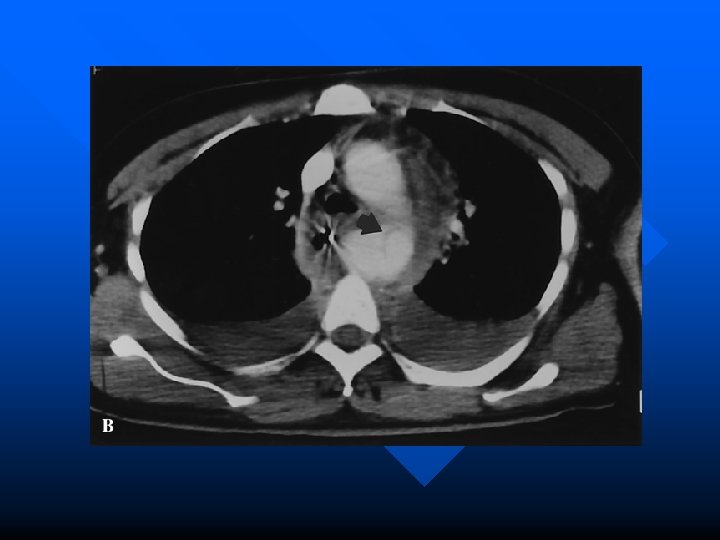
Evidence for CT in Blunt Trauma? n Early scanners (non-helical) were disappointing but new helical CT’s have sensitivities of 100% and specificity of 96 % Mirvis et al. Traumatic aortic injury. Diagnosis with contrast enhanced thoracic CT—five year experience at a major trauma center. Radiology 1990; 176: 181 -183 Garrant et al. Blunt traumatic aortic rupture. Detection with helical CT of the chest. Radiology 1995; 197: 125 -133. n Demetriades et al. concluded that “all trauma patients with high risk deceleration injuries undergo routine helical CT irrespective of CXR findings” Demetriades et al. Routine helical CT evaluation of the mediastinum in the high risk trauma patient. Arch Surg 1998; 133: 1084 -1088.
Helical CT in Penetrating Trauma n In stable patients with a GSW to the torso, CT can be used to follow the trajectory of the bullet thereby decreasing the need for exploratory surgery Grossman et al. Determining anatomical injury in selected torso gunshot wounds. J Trauma 1998; 446 -456
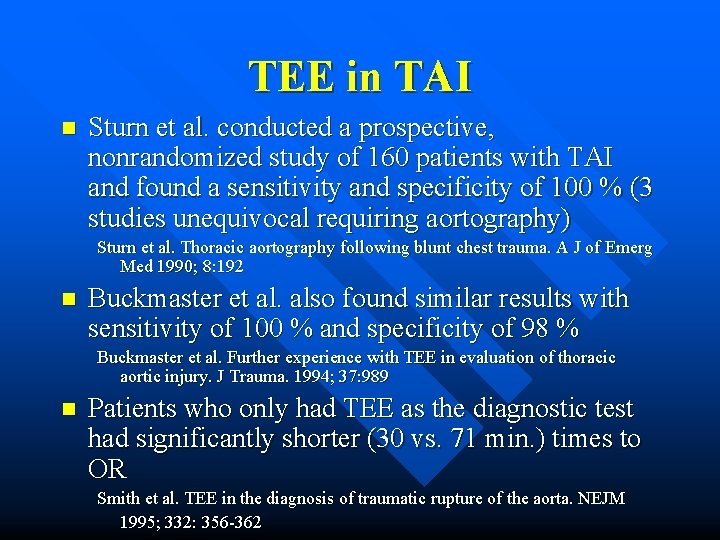
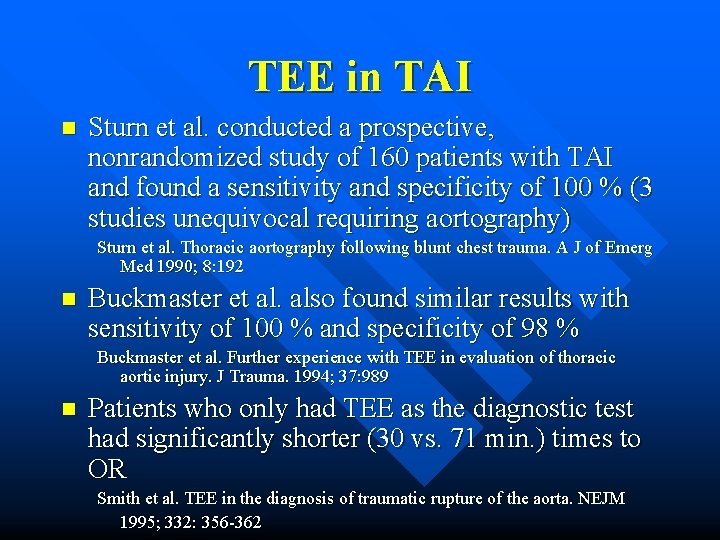
TEE in TAI n Sturn et al. conducted a prospective, nonrandomized study of 160 patients with TAI and found a sensitivity and specificity of 100 % (3 studies unequivocal requiring aortography) Sturn et al. Thoracic aortography following blunt chest trauma. A J of Emerg Med 1990; 8: 192 n Buckmaster et al. also found similar results with sensitivity of 100 % and specificity of 98 % Buckmaster et al. Further experience with TEE in evaluation of thoracic aortic injury. J Trauma. 1994; 37: 989 n Patients who only had TEE as the diagnostic test had significantly shorter (30 vs. 71 min. ) times to OR Smith et al. TEE in the diagnosis of traumatic rupture of the aorta. NEJM 1995; 332: 356 -362
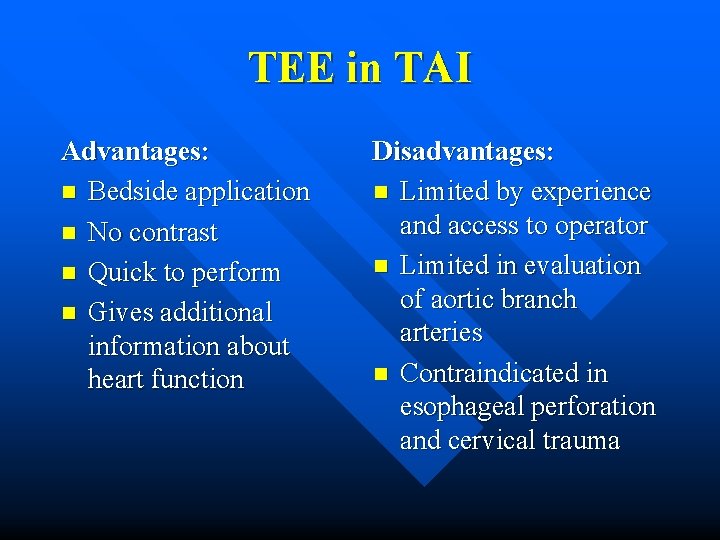
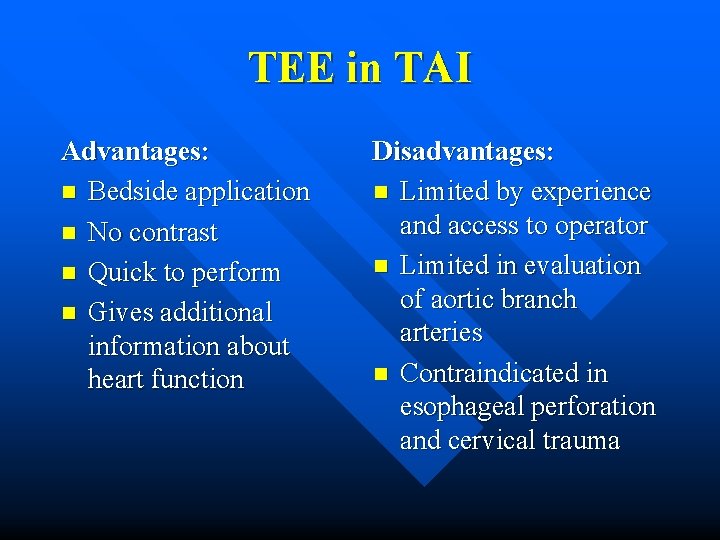
TEE in TAI Advantages: n Bedside application n No contrast n Quick to perform n Gives additional information about heart function Disadvantages: n Limited by experience and access to operator n Limited in evaluation of aortic branch arteries n Contraindicated in esophageal perforation and cervical trauma
The Bottom Line in Imagaing TAI n n n No clear algorithm to follow Variation from center to center Some centers use a widened mediastinum to prompt further investigation while others use mechanism of high velocity deceleration to advocate for aortography or helical CT In pediatrics making the diagnosis crucial as high survival rate (70 – 90 % once diagnosis made)
Management Pharmacologic management similar to aortic dissection n Maintain systolic blood pressure between 100 – 120 n Beta-blockers decrease pulse pressure and shear forces on the wall of the adventia n – esmolol preferred because short acting and titrateable n Addition of nitroprusside as needed
Non-operative Management Approach for patients with high intraoperative risk of death or injuries that are uniformly fatal n Giles et al. reported a case series of 42 patients with TAI n – 21 with immediate repair had a mortality rate of 19% vs. no deaths in 21 patients treated nonoperatively
Indications for Conservative Management of TAI n n n n Severe injury to the CNS Major burns with high infection risk Sepsis Contaminated open wounds with high risk of infection Severe respiratory insufficiency Hemodynamic instability Presence of a non-threatening lesion (an intimal defect only) False aneuryms
Mr. Al Kohol 43 yo male. Et. OH earlier in evening. Driving home, loses control of vehicle hits parked car head on (estimated speed 70 kph). Not wearing seat belt and no air bag. Hits steering wheel with chest. No LOC. Brought in by EMS complaining of chest pain. CXR and ECG normal. – What is the role of troponin in cardiac contusion? – Does this patient need admission?
Blunt Cardiac Trauma Result of high speed MVC with chest wall striking the steering column n Less commonly from falls, crush injury, blast and direct blows n Importance of diagnosis lies in recognition of associated fatal conditions n – dysrhythmias, CHF, cardiogenic shock, tamponade, cardiac rupture, intraventricular thrombi, coronary artery occlusion
Myocardial Concussion “Commotio cordis” n An acute form of blunt cardiac trauma that stuns the myocardium and results in a brief dysrrhythmia, hypotension and LOC n No long lasting histopathological changes n Death can result from an initial nonperfusing rhythm such as VF that results in cardiac arrest n
Myocardial Contusion Continuum from: concussions contusion infarct n Clinical picture varied and non-specific n – 73% have external signs of thoracic trauma – other associated injuries: pulmonary contusion, pneumothorax, hemothorax, external fracture, great vessel injury – sinus tachycardia most sensitive but least specific
Diagnosis Obvious at autopsy! n No true “gold standard” for making diagnosis n Normal ECG reassuring if no obvious clinical symptoms n Non-specific ECG findings include sinus tachy, PVC’s and PAC’s but also other conduction and rhythym disorders n
Troponin in Blunt Cardiac Trauma n Collins et al. conducted a prospective evaluation of all blunt trauma patients admitted with the possible diagnosis of blunt cardiac injury to exclude diagnosis of cardiac contusion – 72 patients enrolled, 40 normal ECG and Tnt, 16 abnormal ECG and normal troponin, 10 patients elevated Tnt 2 died, 1 poor LV function on echo, 8 d/c’d home – Concluded that normal Tnt exclude contusion and elevated Tnt should require ongoing monitoring…BUT… Collins et al. The usefulness of serum troponin levels in evaluating cardiac injury. American Surgeon. 67(9): 821 -5; discussion 825 -6, 2001 Sep.
Troponin in Blunt Cardiac Injury n Berchinant studied Tnt in 96 chest trauma patients of which 26 were diagnosed with myocardial contusion (echo and/or ECG) over 18 months – 23 % of patients with myocardial contusion had positive Tnt vs. 3 % of placebo – Sensitivity 23 %, specificity 97 % Berchinant et al. Evaluation of incidence, clinical significance, and prognostic value of circulating cardiac troponin. Journal of Trauma -Injury Infection & Critical Care. 48(5): 924 -31, 2000 May
Myocardial Rupture n n An acute perforation of the atria or ventricles Also includes pericardial rupture or laceration of the interventricualr or atrial septum, papillary muscle, chrodae, or valves MVC’s most common cause 0. 5 – 2 % of cases of chest trauma accounting for 5% mortality of all chest traumas
Clinical Presentation n Usually that of cardiac tamponade Less common hemothorax, hypotension, hypovolumeia suggesting pericardial rupture Diagnosis of shock and elevated JVP in blunt chest trauma patient = pericardial tamponade (also consider tension pneumothorax, RV contusion, SVC obstruction, ruptures tricuspid valve, chronic pulmnonary disease)
Management n EMS – scoop and run n ED – immediate decompression of tamponade and control of hemorrhage – emergency thoracotomy and percardiotomy then OR for definitive repair
Penetrating Cardiac Injury n Interpersonal violence vast majority of causes – GSW or SW n Two conditions may occur – exsanguinating hemorrhage: free communication with pleural space – cardiac tamponade: contained within the pericardium n n Those with exsanguination often die or will meet criteria for ED thoracotomy Those with tamponade provides some protection but require immediate attention
FAST Exam Focused Abdominal Sonography for Trauma n 4 windows: n – Pericaridial, perisplenic, perihepatic, pelvic n Purpose is for identification of hemopericardium and hemoperitoneum
FAST Exam in Penetrating Cardiac Injury n Rozycki et al. conducted a prospective multicenter trial of 261 patients to assess US identification of pericardial fluid – 100 % sensitive, 96. 9 % specific for identification of hemopericardium – Based on there findings recommend immediate OR for positive findings Rozycki et al. The role of US in patients with possible penetrating cardiac wounds. J Trauma 1999; 46: 543 -552
FAST Exam in Penetrating Cardiac Injury n Thourani et al conducted a retrospective chart review of 22 years for penetrating cardiac trauma at their institution; divided into two 11 year subgroups based on introduction of FAST exam – Current approaches impacting mortality are: shorter field time, more FAST exams in normotensive or moderately hypotensive patients and earlier OR – Mortality rate similar in both groups (25 %) but trend to better survivial in FAST group of normotensive and moderately hypotensive patients Thourani et al. Penetrating cardiac trauma at an uran trauma center. Am Surgeon 1999; 65: 811 -818
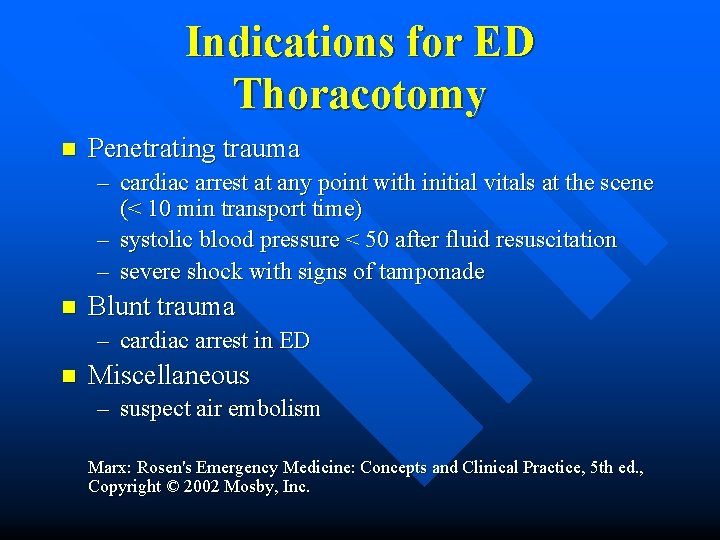
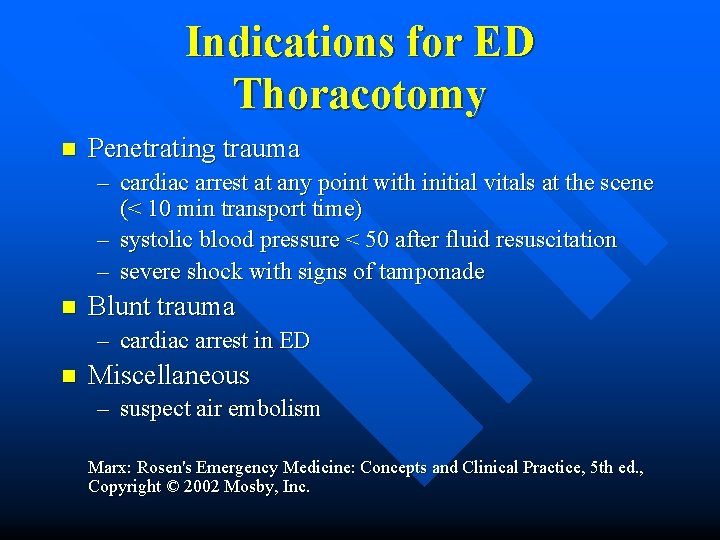
Indications for ED Thoracotomy n Penetrating trauma – cardiac arrest at any point with initial vitals at the scene (< 10 min transport time) – systolic blood pressure < 50 after fluid resuscitation – severe shock with signs of tamponade n Blunt trauma – cardiac arrest in ED n Miscellaneous – suspect air embolism Marx: Rosen's Emergency Medicine: Concepts and Clinical Practice, 5 th ed. , Copyright © 2002 Mosby, Inc.
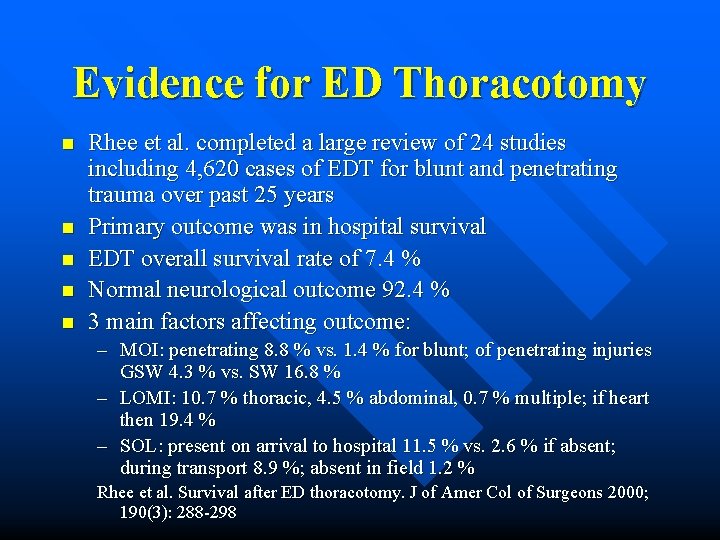
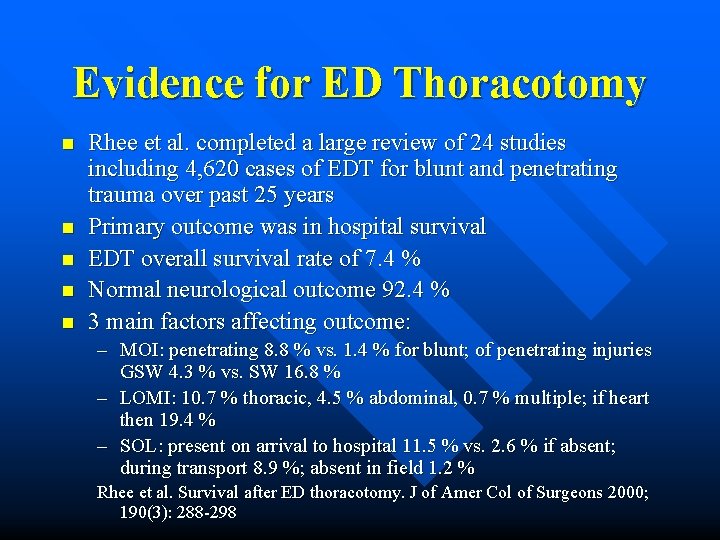
Evidence for ED Thoracotomy n n n Rhee et al. completed a large review of 24 studies including 4, 620 cases of EDT for blunt and penetrating trauma over past 25 years Primary outcome was in hospital survival EDT overall survival rate of 7. 4 % Normal neurological outcome 92. 4 % 3 main factors affecting outcome: – MOI: penetrating 8. 8 % vs. 1. 4 % for blunt; of penetrating injuries GSW 4. 3 % vs. SW 16. 8 % – LOMI: 10. 7 % thoracic, 4. 5 % abdominal, 0. 7 % multiple; if heart then 19. 4 % – SOL: present on arrival to hospital 11. 5 % vs. 2. 6 % if absent; during transport 8. 9 %; absent in field 1. 2 % Rhee et al. Survival after ED thoracotomy. J of Amer Col of Surgeons 2000; 190(3): 288 -298
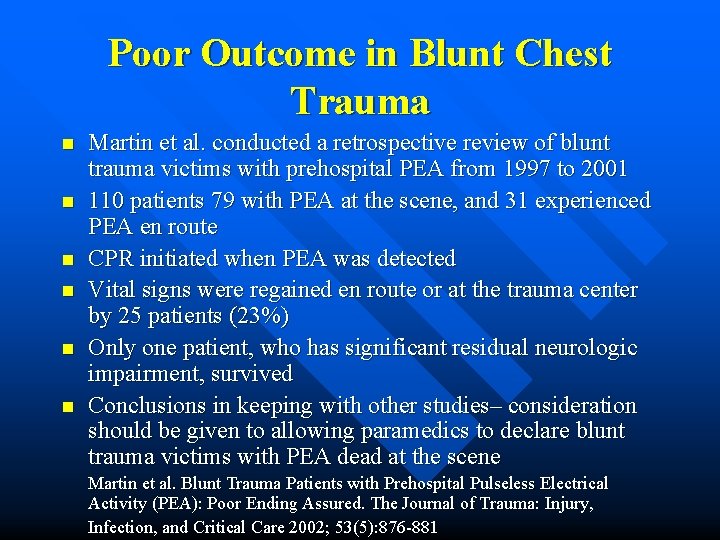
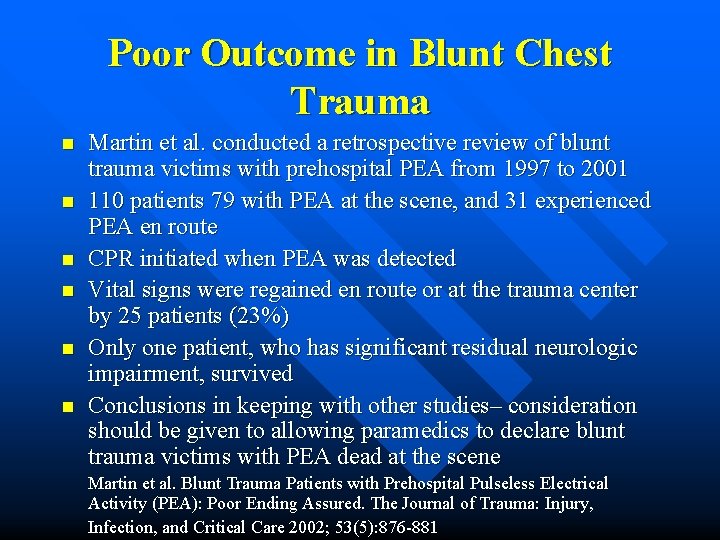
Poor Outcome in Blunt Chest Trauma n n n Martin et al. conducted a retrospective review of blunt trauma victims with prehospital PEA from 1997 to 2001 110 patients 79 with PEA at the scene, and 31 experienced PEA en route CPR initiated when PEA was detected Vital signs were regained en route or at the trauma center by 25 patients (23%) Only one patient, who has significant residual neurologic impairment, survived Conclusions in keeping with other studies– consideration should be given to allowing paramedics to declare blunt trauma victims with PEA dead at the scene Martin et al. Blunt Trauma Patients with Prehospital Pulseless Electrical Activity (PEA): Poor Ending Assured. The Journal of Trauma: Injury, Infection, and Critical Care 2002; 53(5): 876 -881
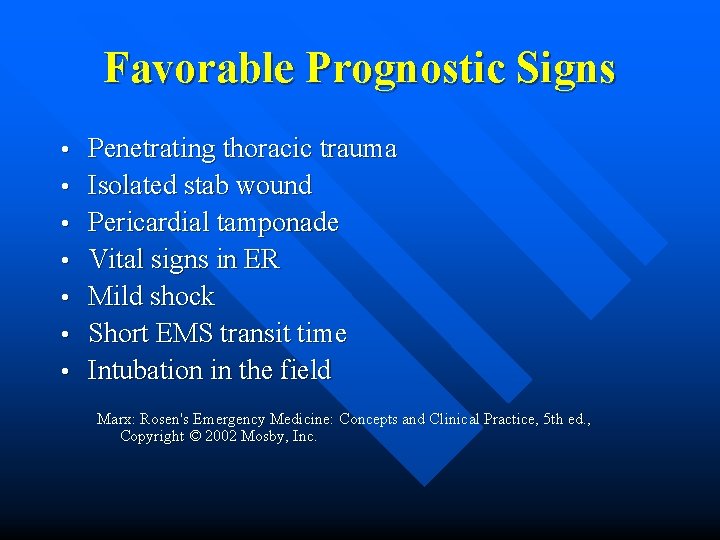
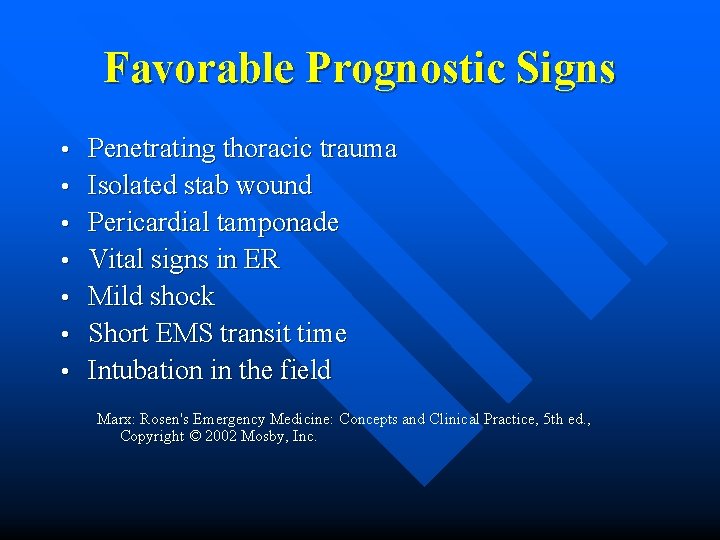
Favorable Prognostic Signs • • Penetrating thoracic trauma Isolated stab wound Pericardial tamponade Vital signs in ER Mild shock Short EMS transit time Intubation in the field Marx: Rosen's Emergency Medicine: Concepts and Clinical Practice, 5 th ed. , Copyright © 2002 Mosby, Inc.
Adverse Prognostic Factors • • Blunt thoracic trauma Gunshot wound Exsanguinating hemorrhage through pericardium No signs of life Extreme shock Prolonged EMS transit time Unsuccessful field intubation Asystole as initial cardiac rhythm Marx: Rosen's Emergency Medicine: Concepts and Clinical Practice, 5 th ed. , Copyright © 2002 Mosby, Inc.
Overall Survival Overall survival from EDT 4 - 16 % n Of patients with SW who reach the OR survival 70 - 80 % n Of patients with GSW who reach the OR survival 20 - 40% n
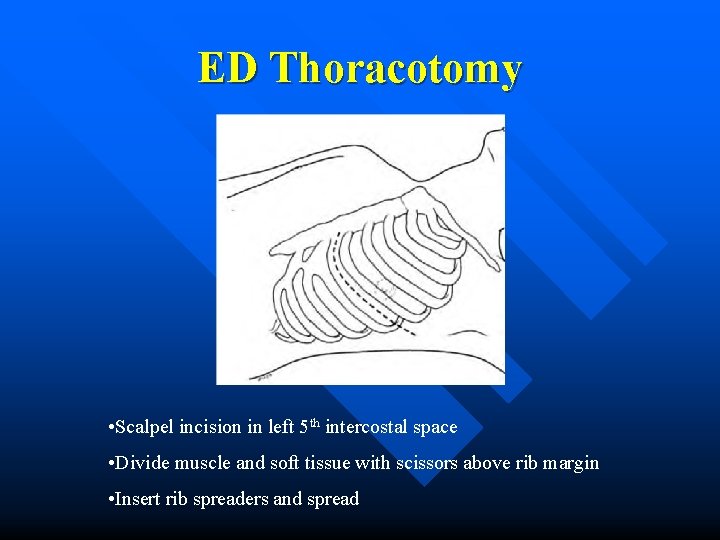
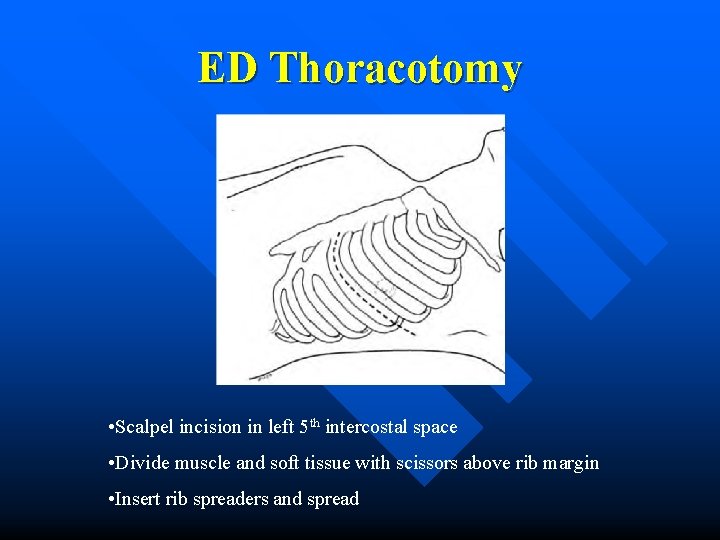
ED Thoracotomy • Scalpel incision in left 5 th intercostal space • Divide muscle and soft tissue with scissors above rib margin • Insert rib spreaders and spread
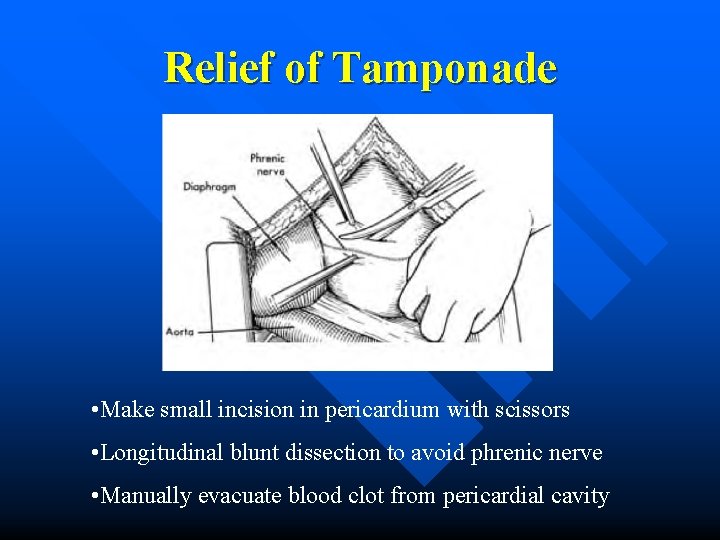
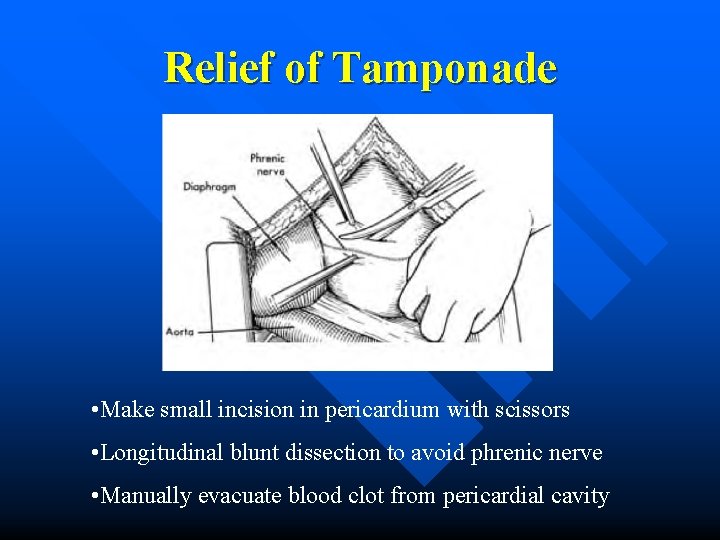
Relief of Tamponade • Make small incision in pericardium with scissors • Longitudinal blunt dissection to avoid phrenic nerve • Manually evacuate blood clot from pericardial cavity
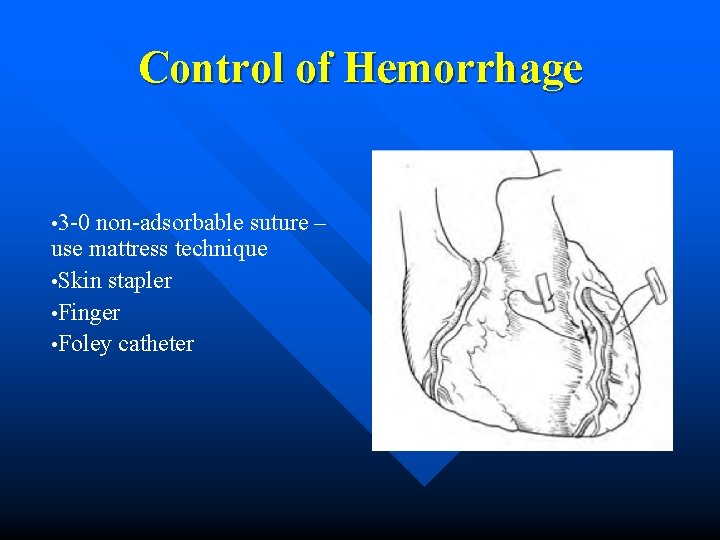
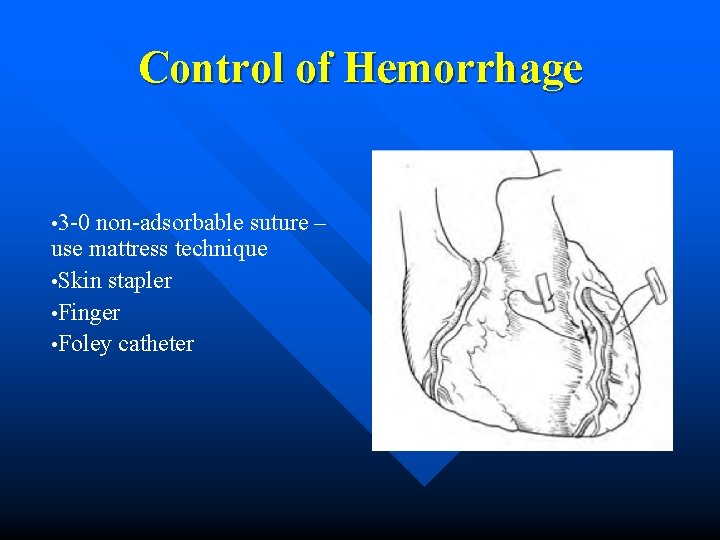
Control of Hemorrhage • 3 -0 non-adsorbable suture – use mattress technique • Skin stapler • Finger • Foley catheter
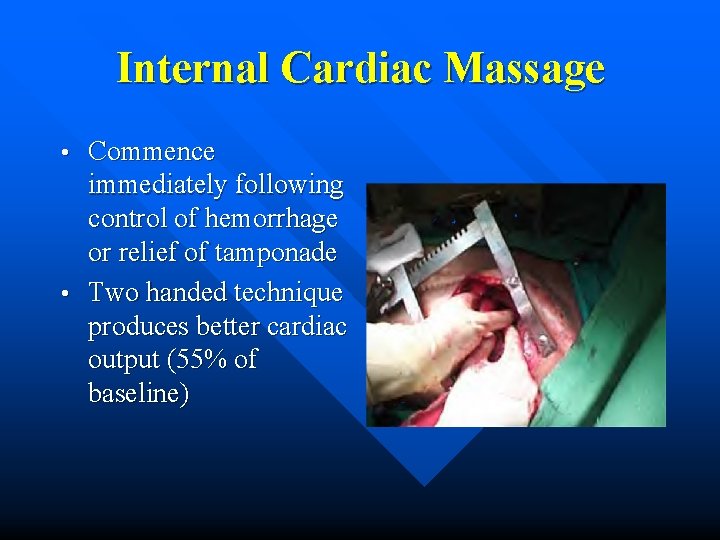
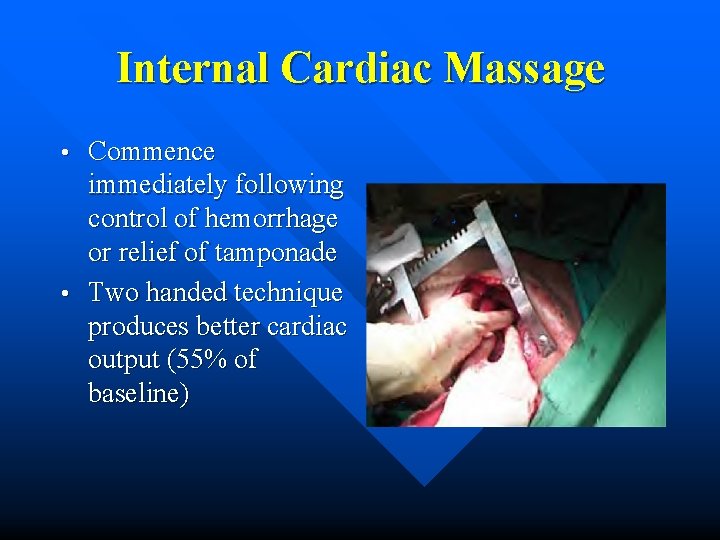
Internal Cardiac Massage Commence immediately following control of hemorrhage or relief of tamponade • Two handed technique produces better cardiac output (55% of baseline) •
Cardiac Tamponade 2% of patients with penetrating thoracic trauma develop cardiac tamponade n Rarely seen in blunt trauma n 60 - 80% of stab wounds to heart develop tamponade n 20% of GSW to heart n
Cardiac Tamponade Collection of blood in indispensable pericardium • 60 - 100 cc blood tolerated before decompensation begins (normal = 5 – 60 cc pericardial fluid) •
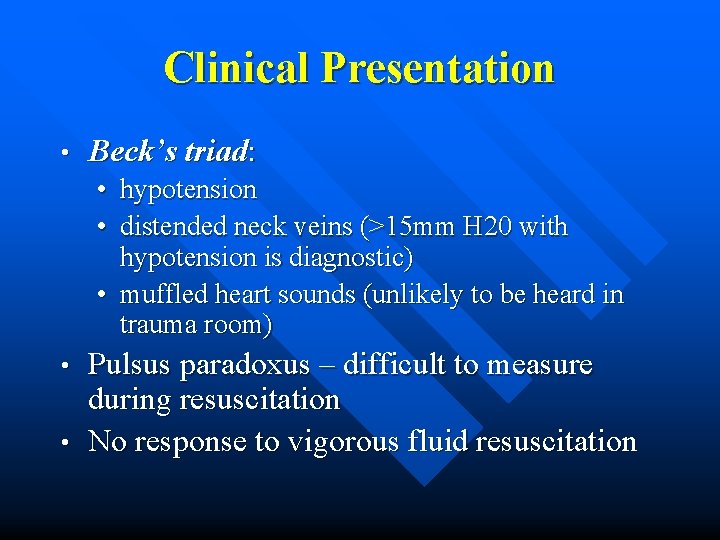
Clinical Presentation • Beck’s triad: • hypotension • distended neck veins (>15 mm H 20 with hypotension is diagnostic) • muffled heart sounds (unlikely to be heard in trauma room) Pulsus paradoxus – difficult to measure during resuscitation • No response to vigorous fluid resuscitation •
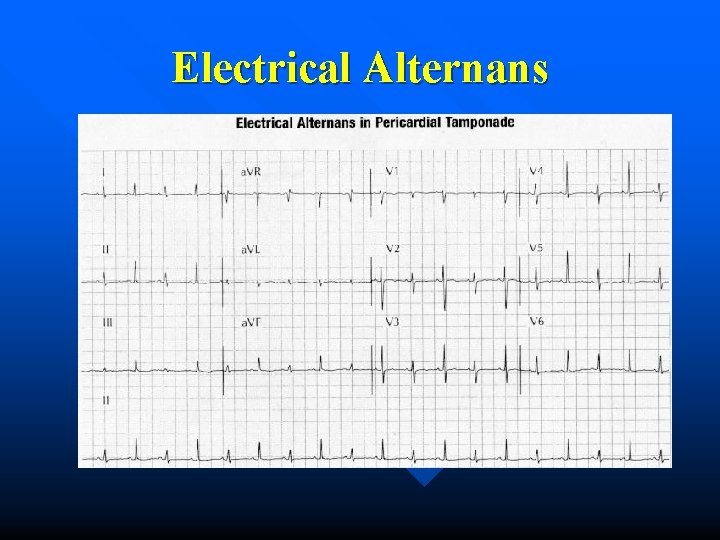
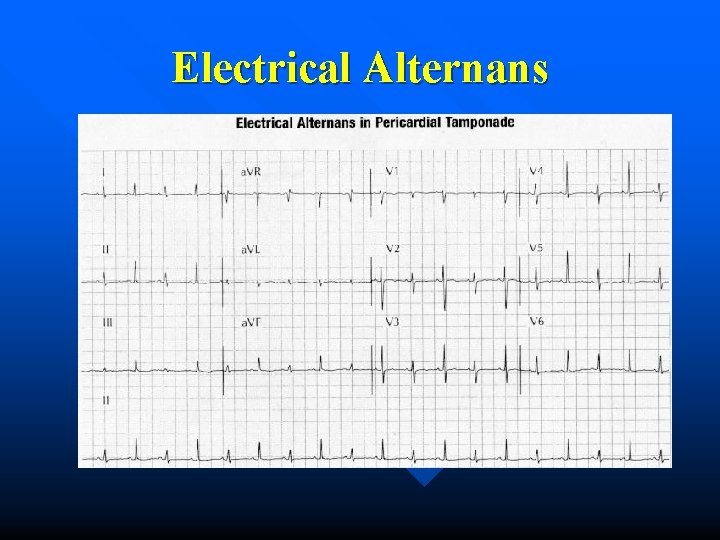
Electrical Alternans
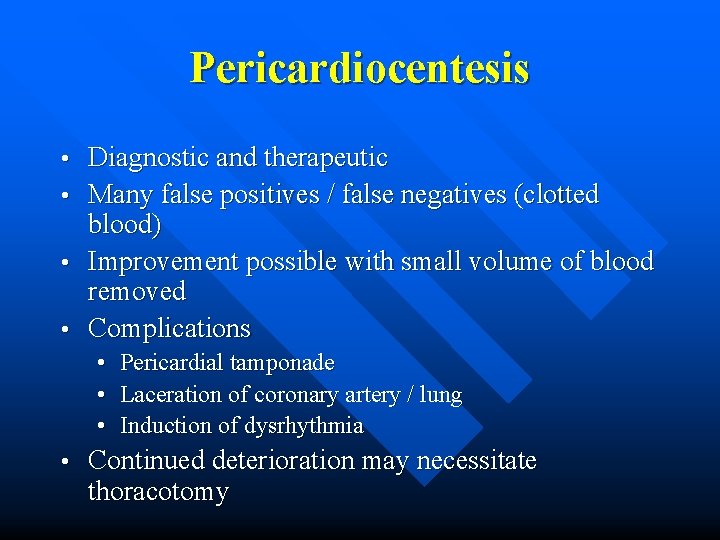
Pericardiocentesis Diagnostic and therapeutic • Many false positives / false negatives (clotted blood) • Improvement possible with small volume of blood removed • Complications • • Pericardial tamponade • Laceration of coronary artery / lung • Induction of dysrhythmia • Continued deterioration may necessitate thoracotomy
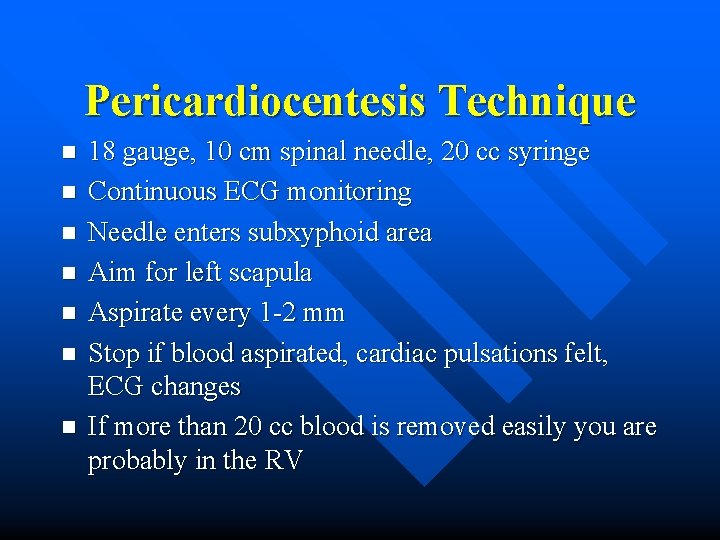
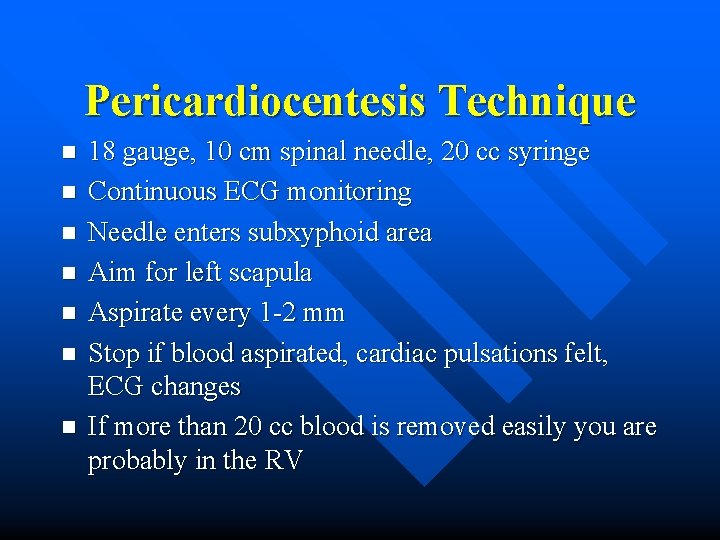
Pericardiocentesis Technique n n n n 18 gauge, 10 cm spinal needle, 20 cc syringe Continuous ECG monitoring Needle enters subxyphoid area Aim for left scapula Aspirate every 1 -2 mm Stop if blood aspirated, cardiac pulsations felt, ECG changes If more than 20 cc blood is removed easily you are probably in the RV
“He was trying to break up the fight…” 21 year old male, “brought fists to a knife fight. ” Stabbed once in the abdomen with “long” knife. Hemodynamically stable. Mild SOB but O 2 sat, vitals stable. CXR normal. To OR for laparotomy. Multiple abdominal lacerations including laceration of L diaphragm. – CXR findings suggestive of diaphragmatic injury? – Is there a role for DPL or CT scan?
Diaphragmatic Injuries n n n 1 -6% of people sustaining multiple trauma 55% from penetrating trauma and 45% from blunt trauma High speed blunt trauma to the diaphragm or direct injury to diaphragm from penetrating trauma Transmission of abdominal pressure through diaphragm Left sided traumatic hernias 3 -4 x’s more common – liver acts as buffer
Diaphragmatic Injuries Symptoms and signs variable and often over shadowed by associated injuries n 30 % missed in acute phase n Often not accompanied by herniation of abdominal viscera n
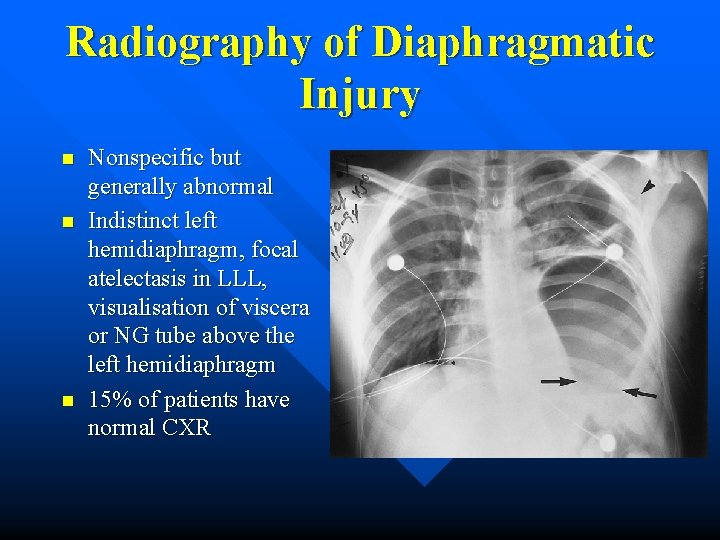
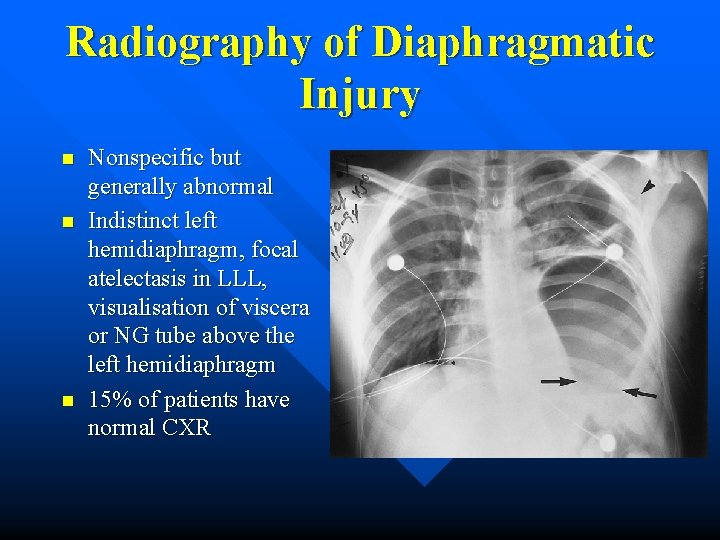
Radiography of Diaphragmatic Injury n n n Nonspecific but generally abnormal Indistinct left hemidiaphragm, focal atelectasis in LLL, visualisation of viscera or NG tube above the left hemidiaphragm 15% of patients have normal CXR
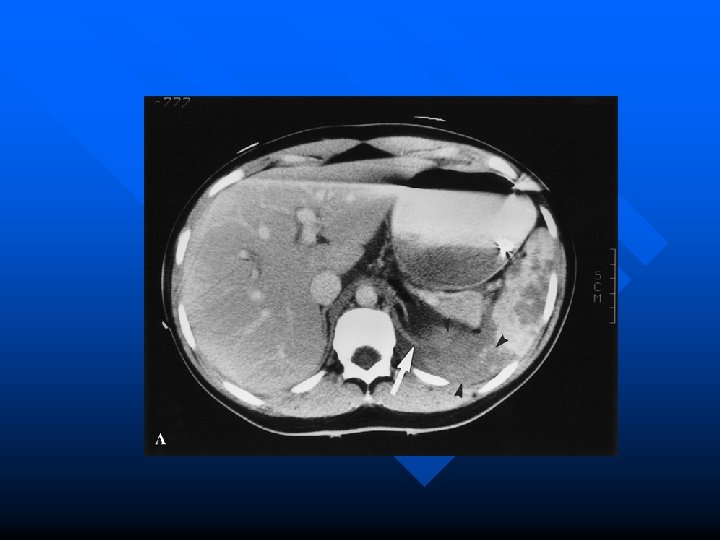
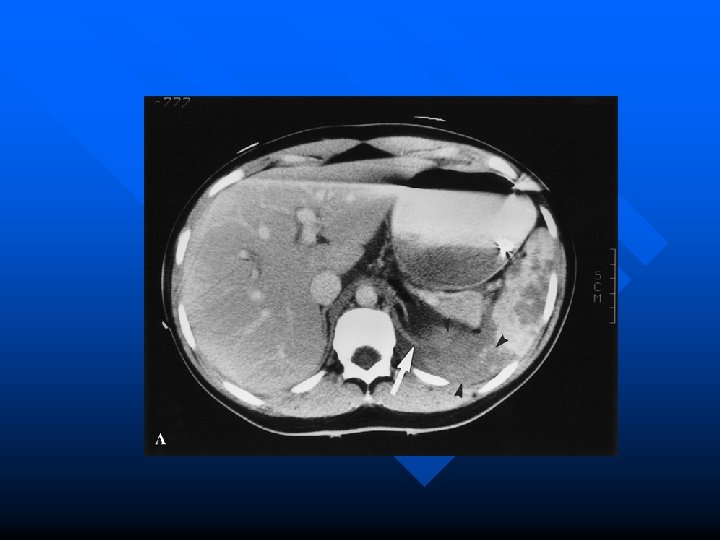
Investigation of Diaphragmatic Injury n DPL found unreliable – False negative rate of 34 % n n CT variable sensitivity 14 - 61% if no herniation of abdominal viscera and specificity of 76 – 99 % Most common finding is defect in hemi-diaphragm – Seen in approx. 70 % of ruptures – CT collar sign 100 % specific but only 30 % sensitive

Latent Phase Herniation can be intermittent making the diagnosis difficult n Requires serial examination if persistent symptoms n Contrast studies useful n
Esophageal Injury Result of blunt or penetrating trauma, barotrauma (blast), or ingestion of caustic material n Symptoms: chest, throat or neck pain, dysphagia or odynophagia n Signs: fever choking, subcutaneous emphysema, redness, swelling, shock n
Diagnosis Clinical: subcutaneous crepitus n Neck and CXR: air in cervical tissue or mediastinum or pleural effusions n Diagnosis made by esophogram using gastrografin initially then barium if no lesion identified n Endoscopy identifies 50 - 100% of injuries but can enlarge the perforation n
Management Surgical management is definitive treatment if patient is stable n If patient is not a suitable surgical candidate and continuing to have ongoing leak then treat with IV antibiotics, NG suction, parenteral nutrion n High mortality with medical management with mortality rate 50 % or greater if surgery delayed > 24 hours n
Rib Fractures n n n Ribs 4 -9 most commonly broken Ribs 1 -3 well protected – marker for severe intrathoracic injury Ribs 9 -12 mobile anteriorly – marker for intra-abdominal injury (liver, spleen, kidney) Rib Fractures less common in pediatric population because of chest wall compliance Rib fractures in children less than 3 yo need to rule out NAT
Rib Fractures n Single rib fracture – May limit ventilation and cough reflex secondary to pain – Conservative management n Multiple rib fractures – More force = more injuries – Look for flail chest, pneumothorax, hemothorax, and extrathoracic injuries (liver, spleen, kidney – 30% of patients with 9 -12 th rib fractures)
Rib Fractures n Clinical – Tenderness, bony crepitus, ecchymosis, muscle spasm n Radiological – best diagnosed using CXR but still miss 50% – CXR inadequate for evaluation of rib fractures, but valuable for seeing intrathoracic/ mediastinal injuries
Rib Views: Indications Fractures suspected, ribs 1 -2 n Fractures suspected, ribs 9 -12 n Multiple rib fractures n Elderly patient n Preexisting pulmonary disease n Suspected pathologic fractures n
Rib Fractures: Treatment Pain relief n Medication/intercostal nerve block/epidural n Deep breathing exercises n Do not use n – binders, belts, other restrictive devices as they promote atelectasis, pneumonia
Mr. Flail 65 yo male passenger in MVC. T-Bone collision at high speed. Restrained. No LOC. Complaining of L chest wall pain. Mild respiratory difficulty. RR 30. O 2 sat 95 % on 5 L. Tender on L chest wall. ? Palpable flail segment. CXR flail segment on L chest wall. – What are the indications for MV in flail chest? – Does this patient require prophylactic intubation?
Flail Chest > 2 adjacent ribs fractured at two points n Mortality 8 - 35% n Respiration adversely affected n – Free segment moves paradoxically – Frequently associated with underlying pulmonary contusion n Intubation and ventilation can splint and mask flail chest
Flail Chest: Management Observe for signs of underlying pulmonary injury/pathology • Conserstone of Rx: physiotherapy, analgesia, selective use of endotracheal intubation/MV, and observation for respiratory compromise •
Who needs MV in Flail Chest? n n Freedland et al. conducted a retrospective study to identify factors affecting outcome in 57 patients with flail chest Factors correlating with need for MV – ISS > 22, blood transfusion in 1 st 24 h, moderate to severe associated injuries n Factors correlating with adverse outcome (MV >2/52), death from sepsis or pneumonia – ISS >30, moderate or severe associated injuries or need for transfsuion Freeland M, et al. The management of flail chest injury: Factors affecting outcome. J Trauma. 1990; 30: 1460 -1468
Sternal Fracture n n Mechanism generally anterior blunt chest trauma Usually MVC – More likely with restrained passengers n Associated with – – – n myocardial contusion (1. 5 -6%) rib fractures (21%) spinal fractures (<10%) mediastinal hematoma no association with aortic rupture Isolated sternal fractures – low mortality (0. 7%)
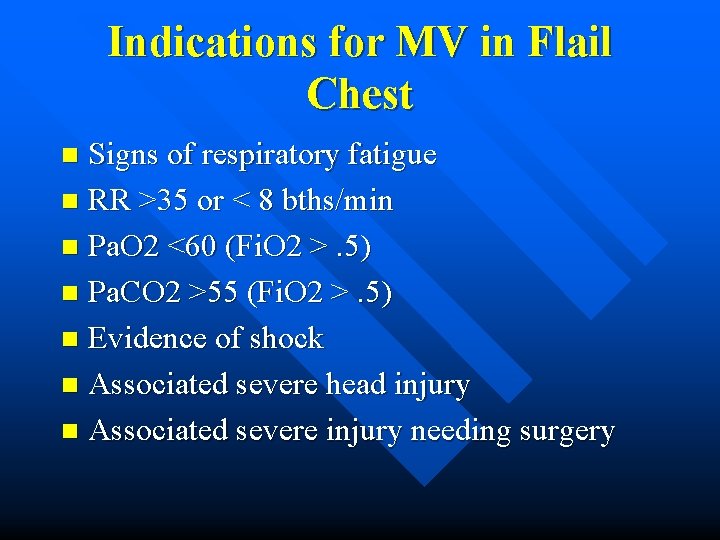
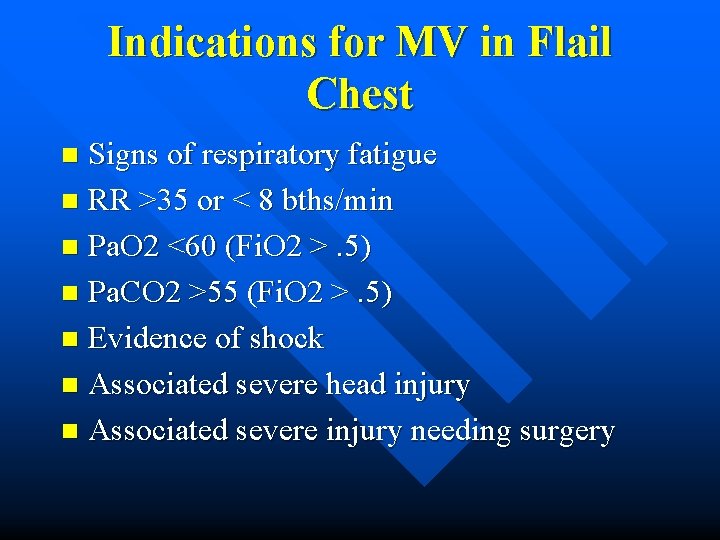
Indications for MV in Flail Chest Signs of respiratory fatigue n RR >35 or < 8 bths/min n Pa. O 2 <60 (Fi. O 2 >. 5) n Pa. CO 2 >55 (Fi. O 2 >. 5) n Evidence of shock n Associated severe head injury n Associated severe injury needing surgery n
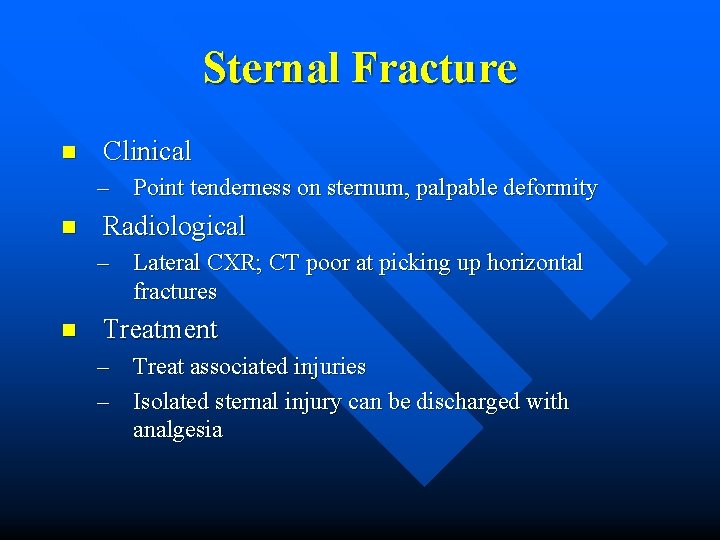
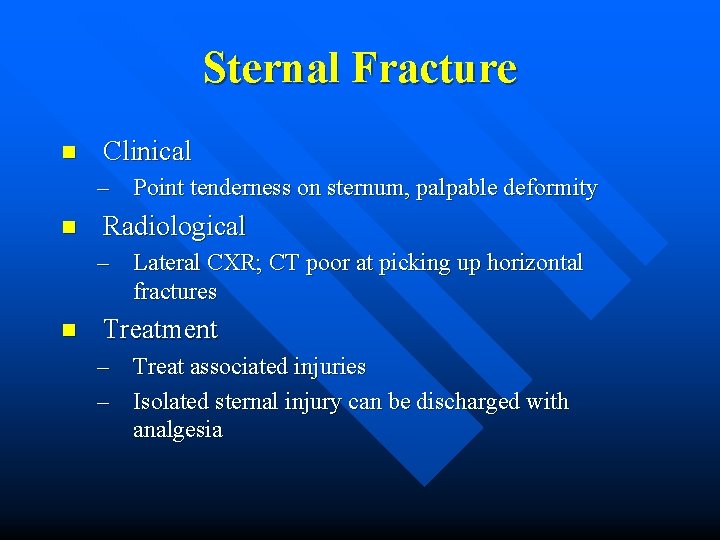
Sternal Fracture n Clinical – Point tenderness on sternum, palpable deformity n Radiological – Lateral CXR; CT poor at picking up horizontal fractures n Treatment – Treat associated injuries – Isolated sternal injury can be discharged with analgesia
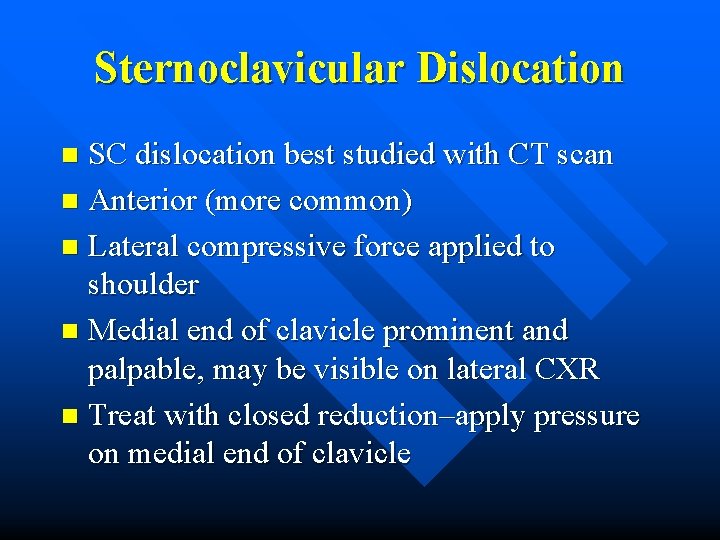
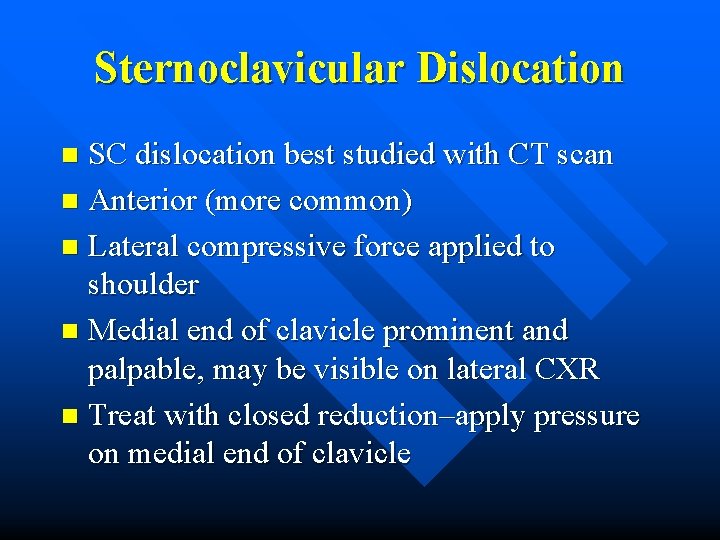
Sternoclavicular Dislocation SC dislocation best studied with CT scan n Anterior (more common) n Lateral compressive force applied to shoulder n Medial end of clavicle prominent and palpable, may be visible on lateral CXR n Treat with closed reduction–apply pressure on medial end of clavicle n
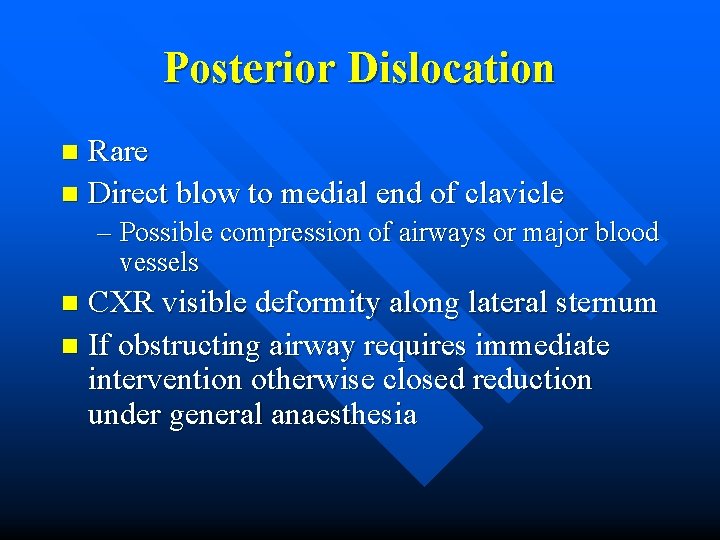
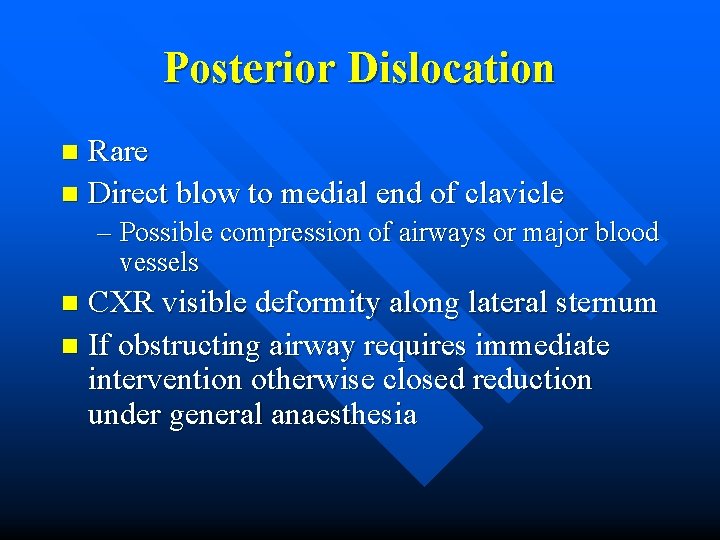
Posterior Dislocation Rare n Direct blow to medial end of clavicle n – Possible compression of airways or major blood vessels CXR visible deformity along lateral sternum n If obstructing airway requires immediate intervention otherwise closed reduction under general anaesthesia n