Radiological Category Chest Principal Modality Chest Radiography Secondary










- Slides: 25
Radiological Category: Chest Principal Modality: Chest Radiography Secondary Modality: CT Case Report # 0903 Submitted by: J. Caleb Richards, M. D. Faculty reviewer: Emma Ferguson, M. D University of Texas at Houston Date accepted: 15 March 2012
Case History • 3 -year-old male with cough


Test Your Diagnosis Which feature(s) is(are) present? a. Alveolar opacity b. Rib splaying c. Paraspinal mass d. Ectatic aortic arch

FINDINGS • Left paraspinal mass • Rib splaying

Case History • A CT was performed


Test Your Diagnosis What is the most likely diagnosis? a. Chondrosarcoma b. Thoracic neuroblastoma c. Bronchogenic cyst d. Paraspinal abscess e. Thoracic aortic aneurysm

FINDINGS • CT confirms the posterior mediastinal mass with areas of calcification
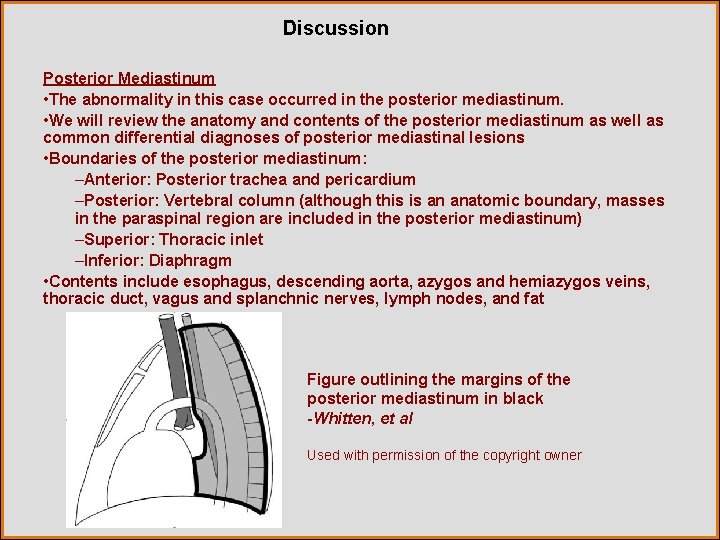
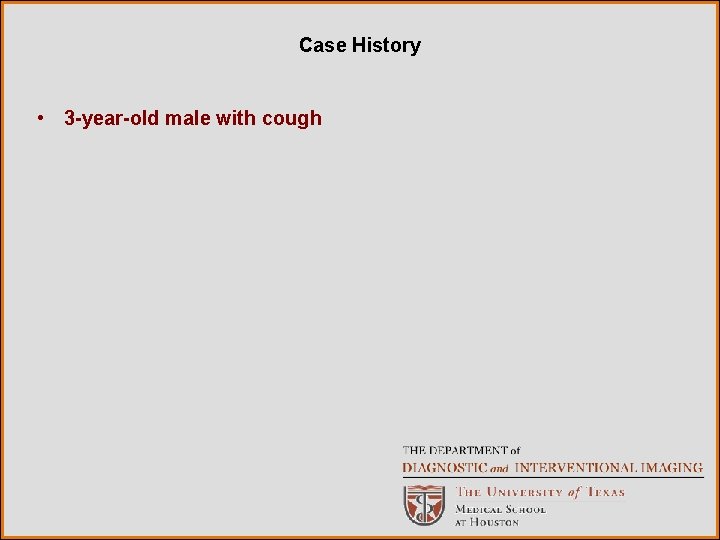
Discussion Posterior Mediastinum • The abnormality in this case occurred in the posterior mediastinum. • We will review the anatomy and contents of the posterior mediastinum as well as common differential diagnoses of posterior mediastinal lesions • Boundaries of the posterior mediastinum: –Anterior: Posterior trachea and pericardium –Posterior: Vertebral column (although this is an anatomic boundary, masses in the paraspinal region are included in the posterior mediastinum) –Superior: Thoracic inlet –Inferior: Diaphragm • Contents include esophagus, descending aorta, azygos and hemiazygos veins, thoracic duct, vagus and splanchnic nerves, lymph nodes, and fat Figure outlining the margins of the posterior mediastinum in black -Whitten, et al Used with permission of the copyright owner
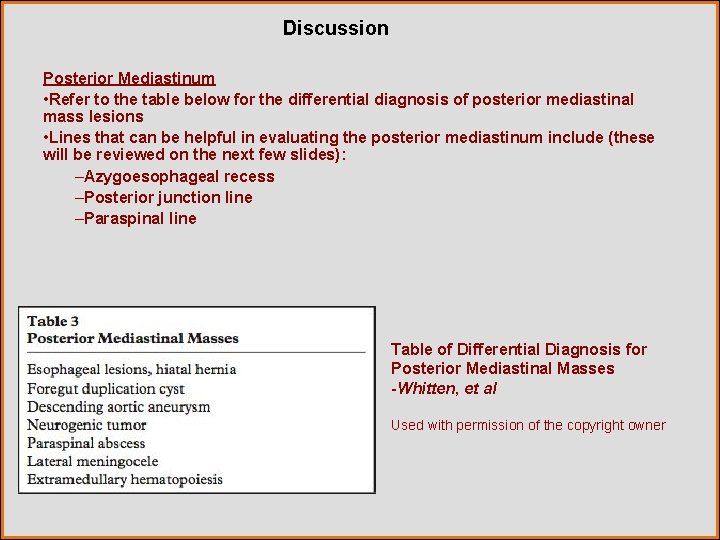
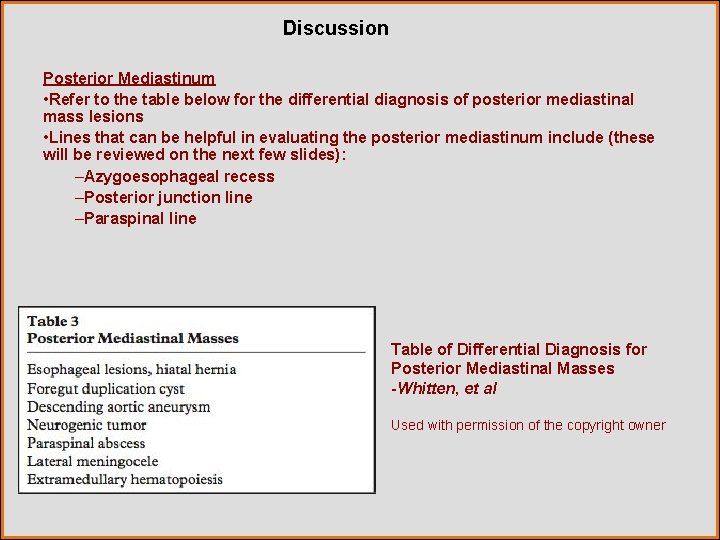
Discussion Posterior Mediastinum • Refer to the table below for the differential diagnosis of posterior mediastinal mass lesions • Lines that can be helpful in evaluating the posterior mediastinum include (these will be reviewed on the next few slides): –Azygoesophageal recess –Posterior junction line –Paraspinal line Table of Differential Diagnosis for Posterior Mediastinal Masses -Whitten, et al Used with permission of the copyright owner
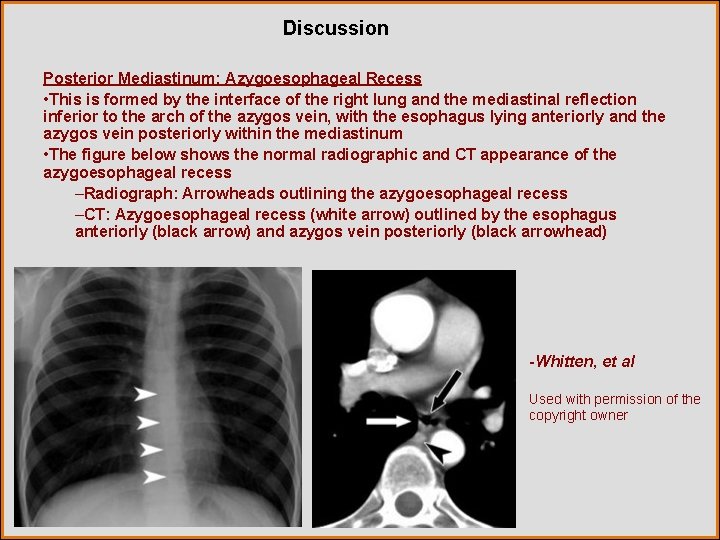
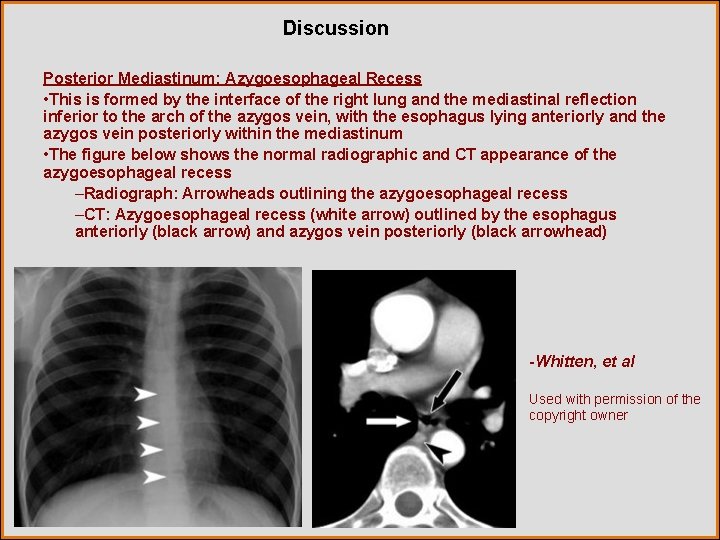
Discussion Posterior Mediastinum: Azygoesophageal Recess • This is formed by the interface of the right lung and the mediastinal reflection inferior to the arch of the azygos vein, with the esophagus lying anteriorly and the azygos vein posteriorly within the mediastinum • The figure below shows the normal radiographic and CT appearance of the azygoesophageal recess –Radiograph: Arrowheads outlining the azygoesophageal recess –CT: Azygoesophageal recess (white arrow) outlined by the esophagus anteriorly (black arrow) and azygos vein posteriorly (black arrowhead) -Whitten, et al Used with permission of the copyright owner
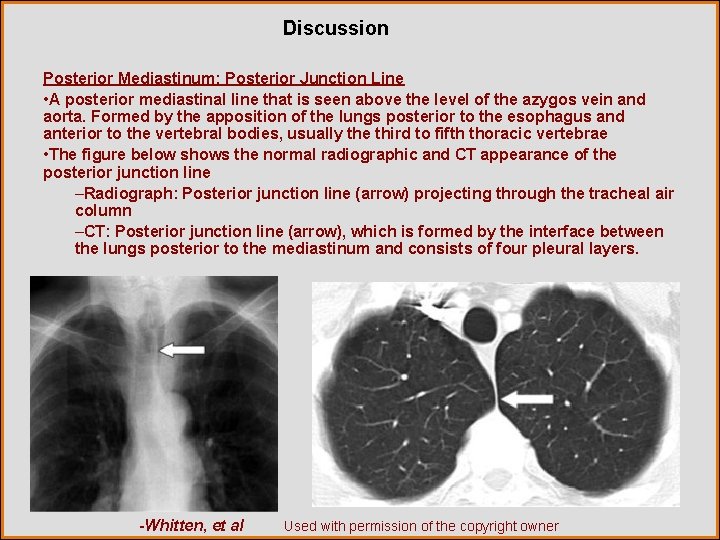
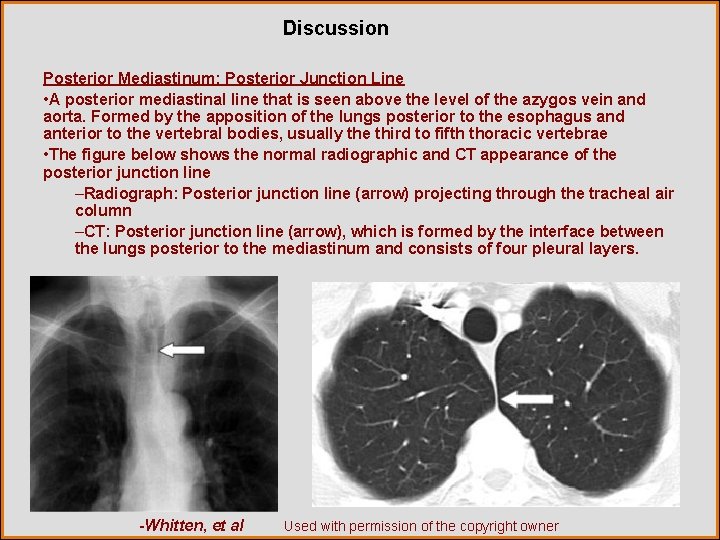
Discussion Posterior Mediastinum: Posterior Junction Line • A posterior mediastinal line that is seen above the level of the azygos vein and aorta. Formed by the apposition of the lungs posterior to the esophagus and anterior to the vertebral bodies, usually the third to fifth thoracic vertebrae • The figure below shows the normal radiographic and CT appearance of the posterior junction line –Radiograph: Posterior junction line (arrow) projecting through the tracheal air column –CT: Posterior junction line (arrow), which is formed by the interface between the lungs posterior to the mediastinum and consists of four pleural layers. -Whitten, et al Used with permission of the copyright owner
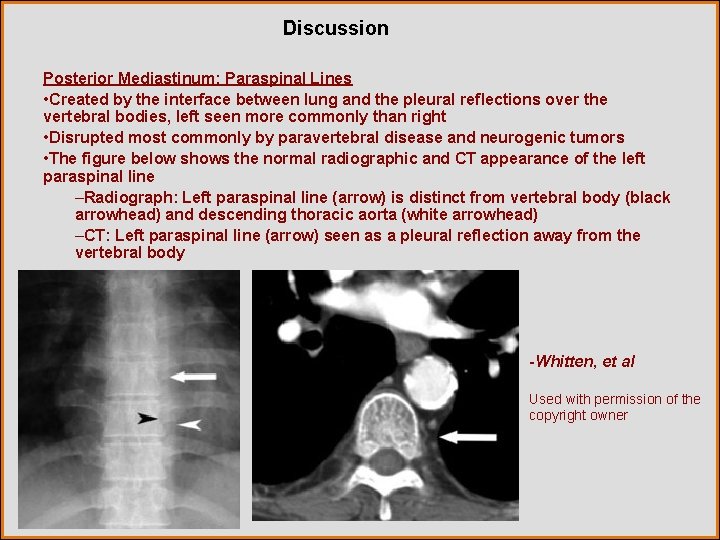
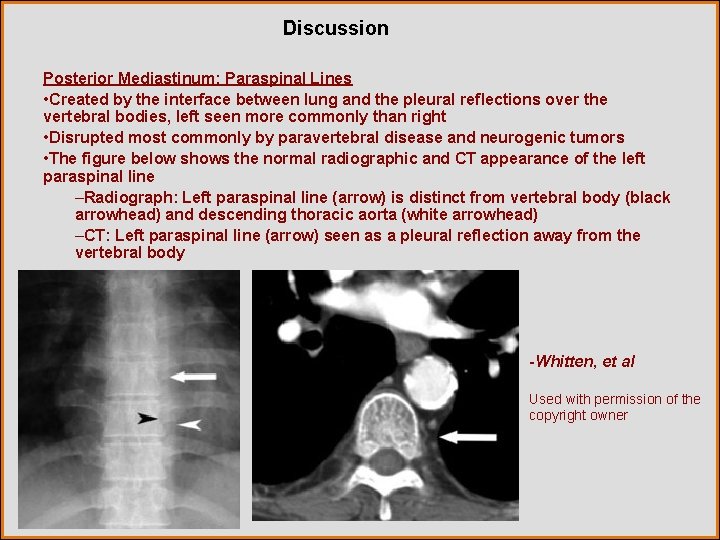
Discussion Posterior Mediastinum: Paraspinal Lines • Created by the interface between lung and the pleural reflections over the vertebral bodies, left seen more commonly than right • Disrupted most commonly by paravertebral disease and neurogenic tumors • The figure below shows the normal radiographic and CT appearance of the left paraspinal line –Radiograph: Left paraspinal line (arrow) is distinct from vertebral body (black arrowhead) and descending thoracic aorta (white arrowhead) –CT: Left paraspinal line (arrow) seen as a pleural reflection away from the vertebral body -Whitten, et al Used with permission of the copyright owner
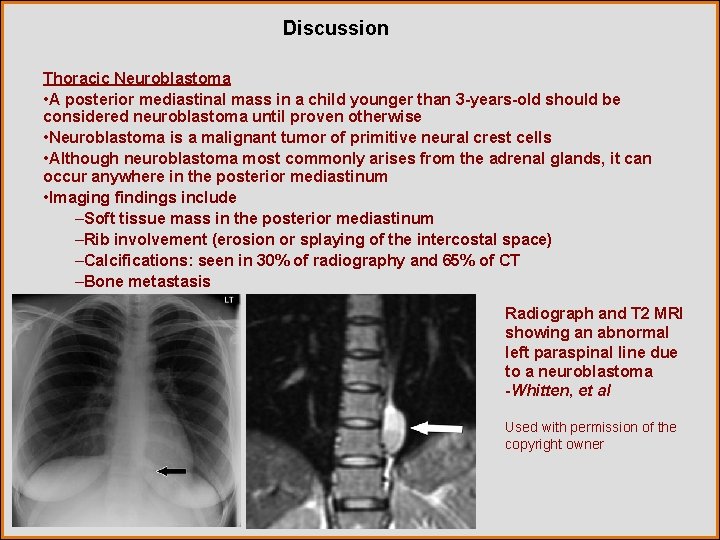
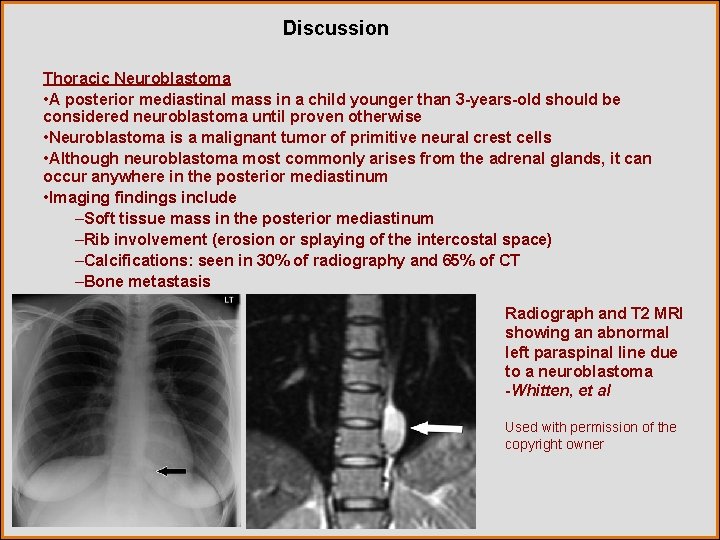
Discussion Thoracic Neuroblastoma • A posterior mediastinal mass in a child younger than 3 -years-old should be considered neuroblastoma until proven otherwise • Neuroblastoma is a malignant tumor of primitive neural crest cells • Although neuroblastoma most commonly arises from the adrenal glands, it can occur anywhere in the posterior mediastinum • Imaging findings include –Soft tissue mass in the posterior mediastinum –Rib involvement (erosion or splaying of the intercostal space) –Calcifications: seen in 30% of radiography and 65% of CT –Bone metastasis Radiograph and T 2 MRI showing an abnormal left paraspinal line due to a neuroblastoma -Whitten, et al Used with permission of the copyright owner

Discussion Thoracic Neuroblastoma • Most commonly are seen in the inferior mediastinum, although can occur in the superior mediastinum (as in our case) • Mean age of presentation is 22 months • Younger presentation is associated with better prognosis • Metastasizes most commonly to liver and bone • Skin metastasis may present as multiple bluish or purple masses resembling blueberries (this appearance has been given the eponym “blueberry muffin” syndrome) Blueberry muffin syndrome in an 8 -month-old female with neuroblastoma -Longergan, et al Used with permission of the copyright owner

Discussion Bronchogenic Cyst • Are part of the family of foregut duplication cysts: bronchogenic, enteric, and neurenteric cysts • Result from abnormal ventral budding of the tracheobronchial tree between the 26 th and 40 th days of gestation • May occur in the mediastinum or in lung parenchyma, although mediastinal location is more common • Typically do not communicate with airway and do not contain air Radiograph showing a mass obliterating the posterior junction line. CT confirms posterior location and proved to be a bronchogenic cyst. -Whitten, et al Used with permission of the copyright owner
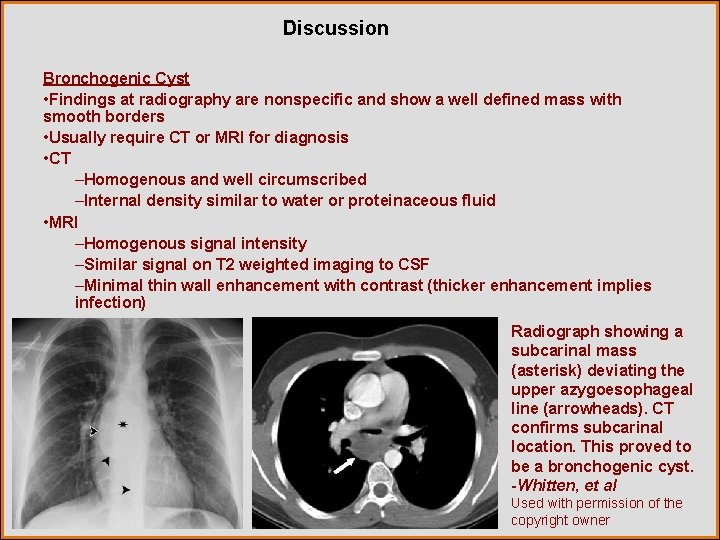
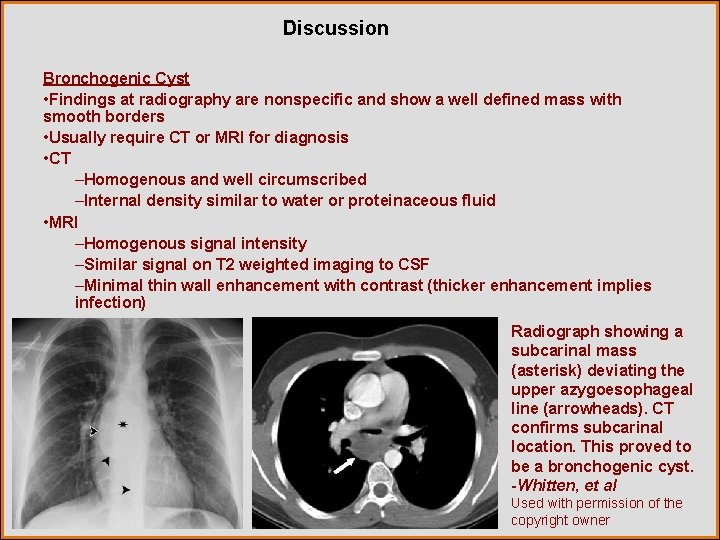
Discussion Bronchogenic Cyst • Findings at radiography are nonspecific and show a well defined mass with smooth borders • Usually require CT or MRI for diagnosis • CT –Homogenous and well circumscribed –Internal density similar to water or proteinaceous fluid • MRI –Homogenous signal intensity –Similar signal on T 2 weighted imaging to CSF –Minimal thin wall enhancement with contrast (thicker enhancement implies infection) Radiograph showing a subcarinal mass (asterisk) deviating the upper azygoesophageal line (arrowheads). CT confirms subcarinal location. This proved to be a bronchogenic cyst. -Whitten, et al Used with permission of the copyright owner
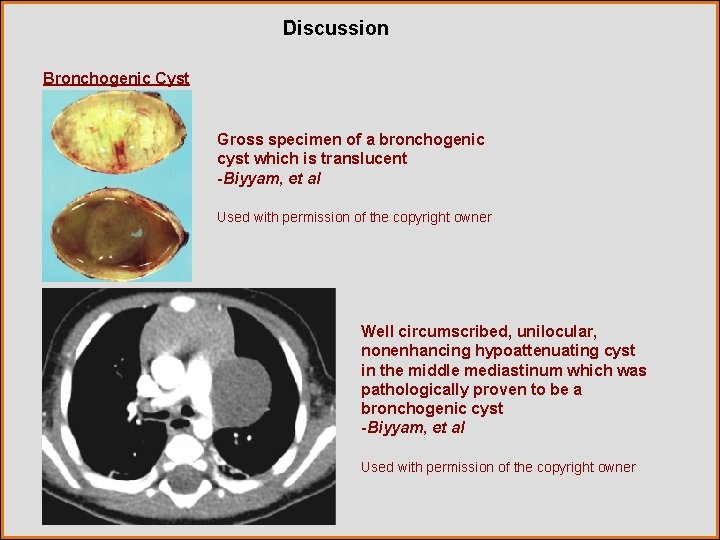
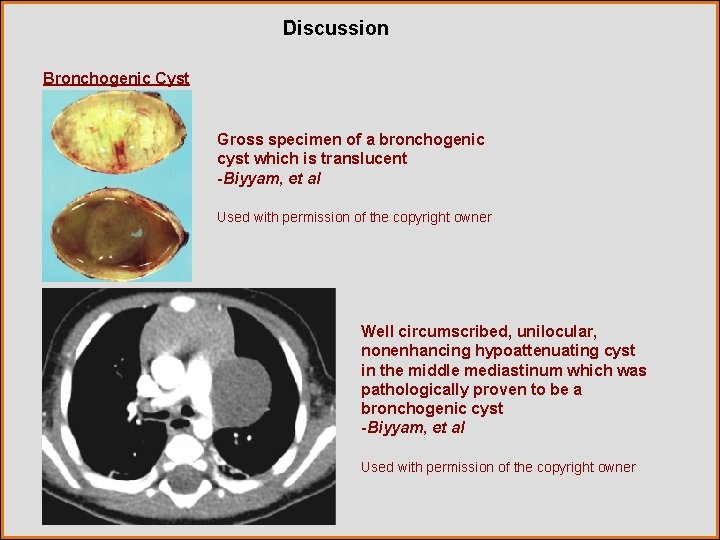
Discussion Bronchogenic Cyst Gross specimen of a bronchogenic cyst which is translucent -Biyyam, et al Used with permission of the copyright owner Well circumscribed, unilocular, nonenhancing hypoattenuating cyst in the middle mediastinum which was pathologically proven to be a bronchogenic cyst -Biyyam, et al Used with permission of the copyright owner
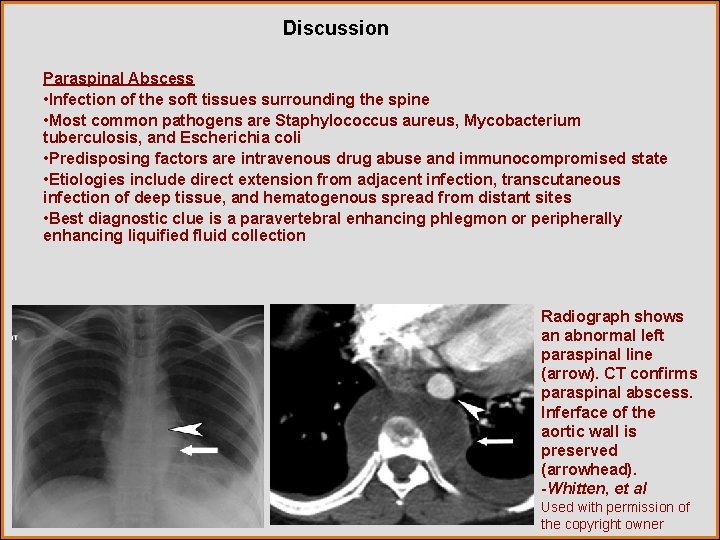
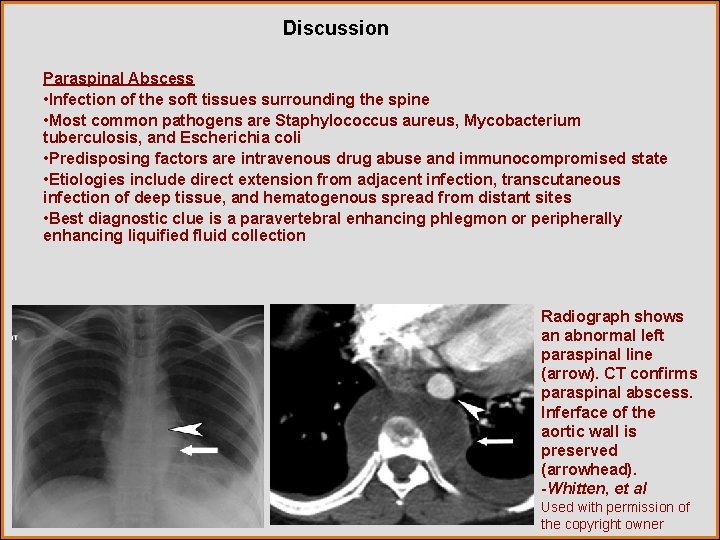
Discussion Paraspinal Abscess • Infection of the soft tissues surrounding the spine • Most common pathogens are Staphylococcus aureus, Mycobacterium tuberculosis, and Escherichia coli • Predisposing factors are intravenous drug abuse and immunocompromised state • Etiologies include direct extension from adjacent infection, transcutaneous infection of deep tissue, and hematogenous spread from distant sites • Best diagnostic clue is a paravertebral enhancing phlegmon or peripherally enhancing liquified fluid collection Radiograph shows an abnormal left paraspinal line (arrow). CT confirms paraspinal abscess. Inferface of the aortic wall is preserved (arrowhead). -Whitten, et al Used with permission of the copyright owner
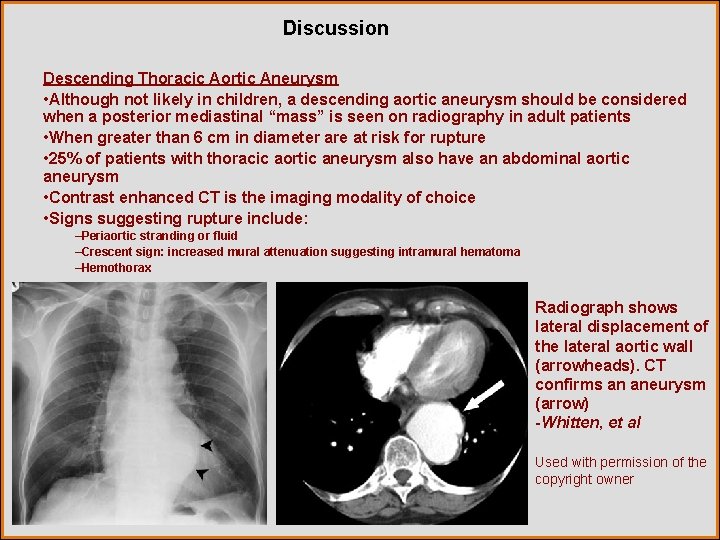
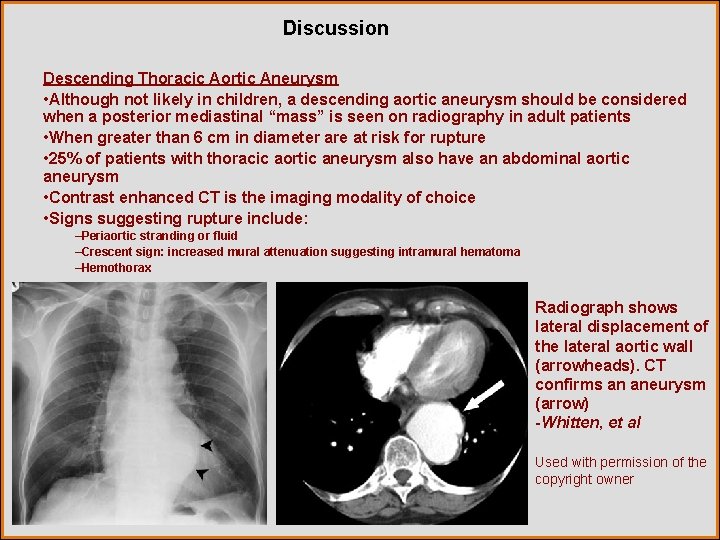
Discussion Descending Thoracic Aortic Aneurysm • Although not likely in children, a descending aortic aneurysm should be considered when a posterior mediastinal “mass” is seen on radiography in adult patients • When greater than 6 cm in diameter are at risk for rupture • 25% of patients with thoracic aortic aneurysm also have an abdominal aortic aneurysm • Contrast enhanced CT is the imaging modality of choice • Signs suggesting rupture include: –Periaortic stranding or fluid –Crescent sign: increased mural attenuation suggesting intramural hematoma –Hemothorax Radiograph shows lateral displacement of the lateral aortic wall (arrowheads). CT confirms an aneurysm (arrow) -Whitten, et al Used with permission of the copyright owner
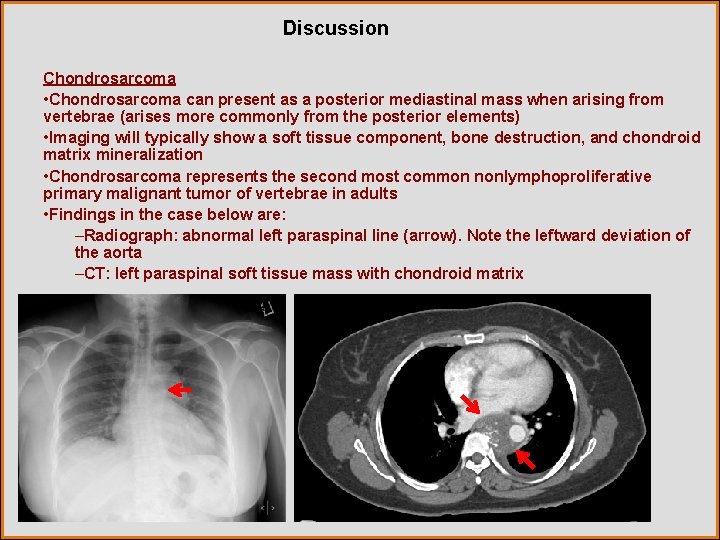
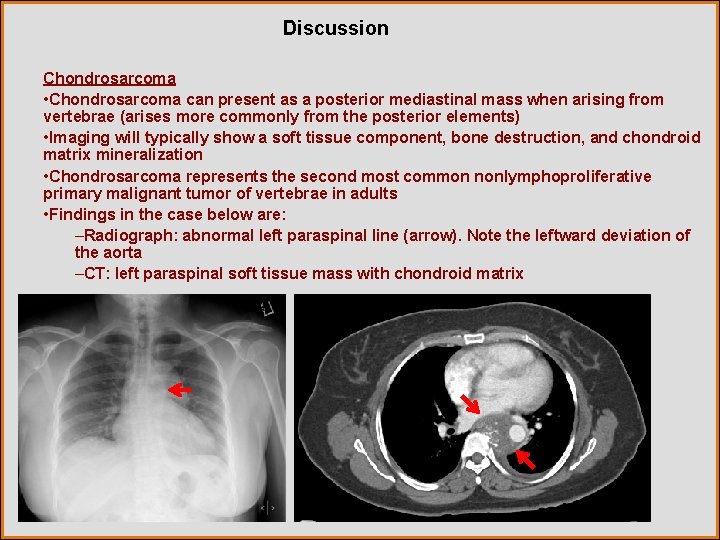
Discussion Chondrosarcoma • Chondrosarcoma can present as a posterior mediastinal mass when arising from vertebrae (arises more commonly from the posterior elements) • Imaging will typically show a soft tissue component, bone destruction, and chondroid matrix mineralization • Chondrosarcoma represents the second most common nonlymphoproliferative primary malignant tumor of vertebrae in adults • Findings in the case below are: –Radiograph: abnormal left paraspinal line (arrow). Note the leftward deviation of the aorta –CT: left paraspinal soft tissue mass with chondroid matrix
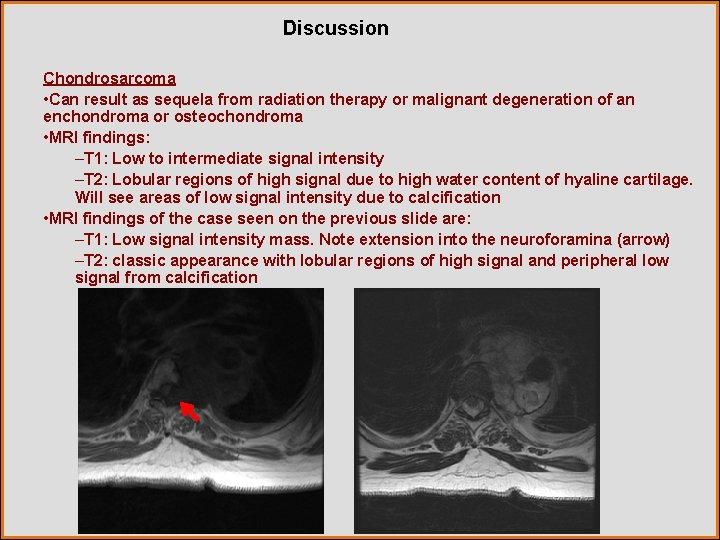
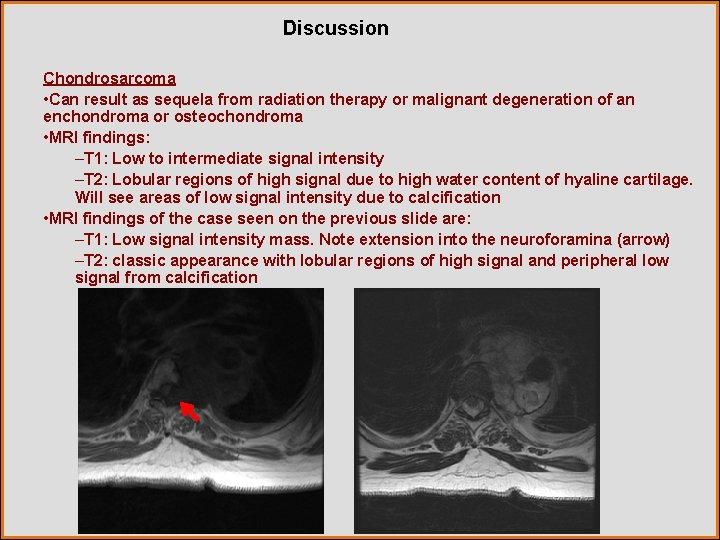
Discussion Chondrosarcoma • Can result as sequela from radiation therapy or malignant degeneration of an enchondroma or osteochondroma • MRI findings: –T 1: Low to intermediate signal intensity –T 2: Lobular regions of high signal due to high water content of hyaline cartilage. Will see areas of low signal intensity due to calcification • MRI findings of the case seen on the previous slide are: –T 1: Low signal intensity mass. Note extension into the neuroforamina (arrow) –T 2: classic appearance with lobular regions of high signal and peripheral low signal from calcification
Diagnosis Thoracic Neuroblastoma

References Biyyam, D et al. Congenital Lung Abnormalities: Embryologic Features, Prenatal Diagnosis, and Postnatal Radiologic-Pathologic Correlation. Radio. Graphics 2010; 30: 1721– 1738 Whitten, C et al. A Diagnostic Approach to Mediastinal Abnormalities. Radio. Graphics 2007; 27: 657– 671 Lee, E et al. Multidetector CT Evaluation of Congenital Lung Anomalies. Radiology 2008; 247: 632 -648 Lonergan et al. From the Archives of the AFIP: Neuroblastoma, Ganglioneuroblastoma, and Ganglioneuroma: Radiologic-Pathologic Correlation. Radio. Graphics 2002; 22: 911– 934
 Pa erate
Pa erate National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health Cardinality and modality
Cardinality and modality Cardinality and modality
Cardinality and modality Cardinality and modality
Cardinality and modality Tom arbuthnot
Tom arbuthnot Epistemic modality
Epistemic modality Diagnostics imaging
Diagnostics imaging What is modality in statistics
What is modality in statistics Stefan savi
Stefan savi Modality in software engineering
Modality in software engineering Modality in software engineering
Modality in software engineering Deontic and epistemic modality exercises
Deontic and epistemic modality exercises Modality in software engineering
Modality in software engineering Data modeling fundamentals
Data modeling fundamentals Modality
Modality High modality definition
High modality definition Pacs modality workstation
Pacs modality workstation Short wave diathermy definition
Short wave diathermy definition Exteroceptors
Exteroceptors Sodality vs modality
Sodality vs modality Modality
Modality Difference between fresnel and fraunhofer diffraction
Difference between fresnel and fraunhofer diffraction