Section 2 Trauma What is trauma trauma n
- Slides: 26
Section 2: Trauma
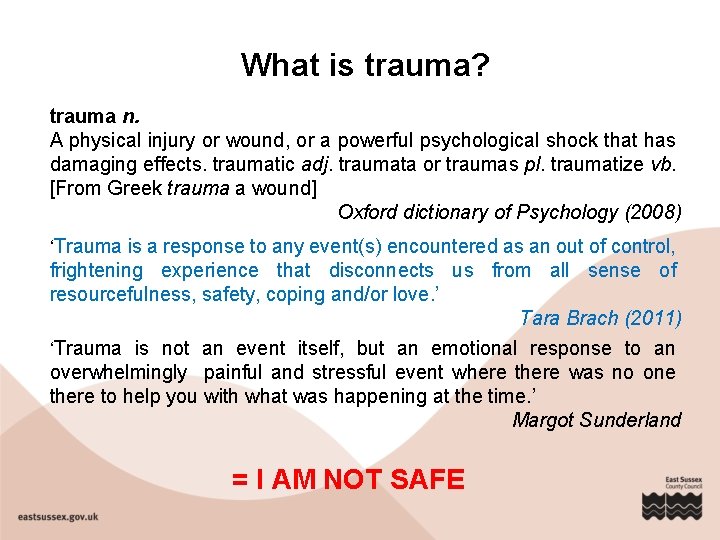
What is trauma? trauma n. A physical injury or wound, or a powerful psychological shock that has damaging effects. traumatic adj. traumata or traumas pl. traumatize vb. [From Greek trauma a wound] Oxford dictionary of Psychology (2008) ‘Trauma is a response to any event(s) encountered as an out of control, frightening experience that disconnects us from all sense of resourcefulness, safety, coping and/or love. ’ Tara Brach (2011) ‘Trauma is not an event itself, but an emotional response to an overwhelmingly painful and stressful event where there was no one there to help you with what was happening at the time. ’ Margot Sunderland = I AM NOT SAFE
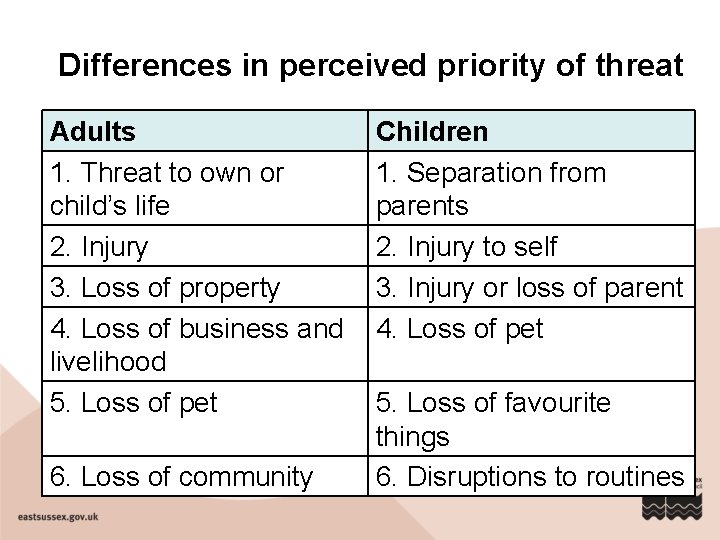
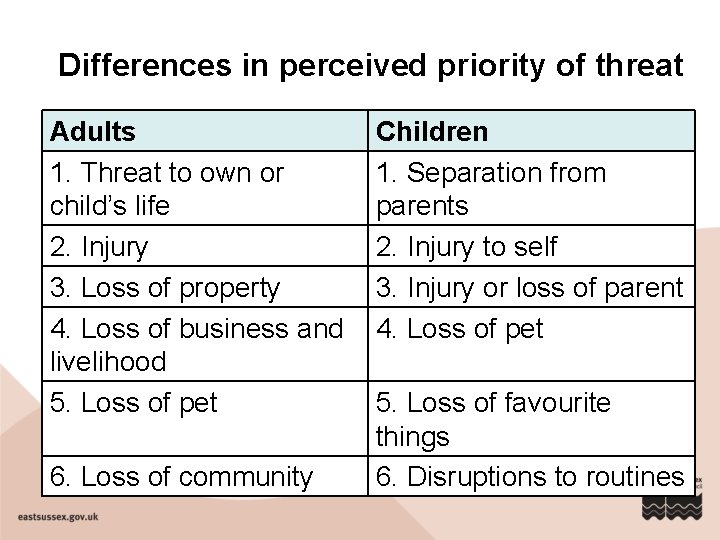
Differences in perceived priority of threat Adults 1. Threat to own or child’s life 2. Injury 3. Loss of property 4. Loss of business and livelihood 5. Loss of pet 6. Loss of community Children 1. Separation from parents 2. Injury to self 3. Injury or loss of parent 4. Loss of pet 5. Loss of favourite things 6. Disruptions to routines
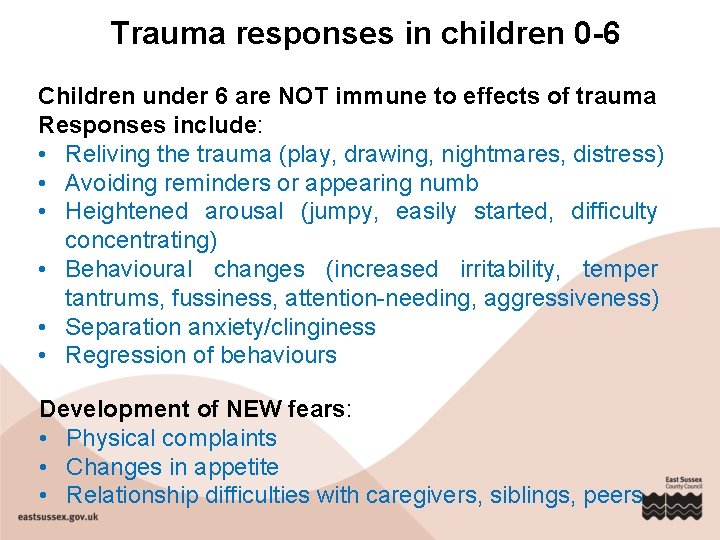
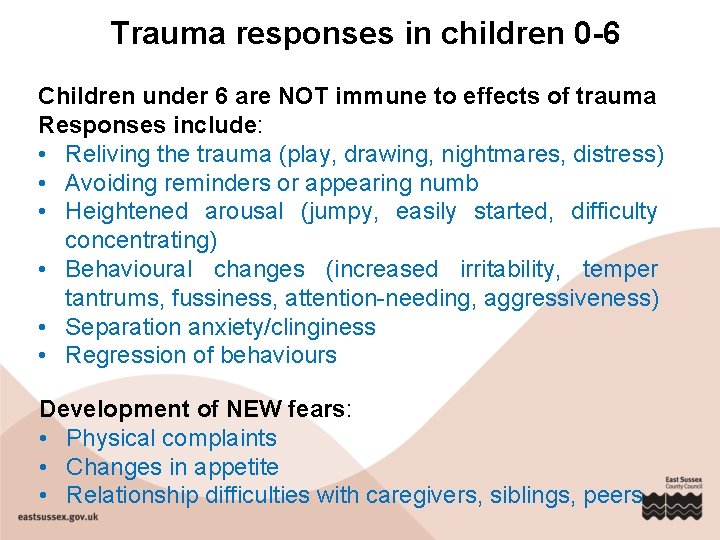
Trauma responses in children 0 -6 Children under 6 are NOT immune to effects of trauma Responses include: • Reliving the trauma (play, drawing, nightmares, distress) • Avoiding reminders or appearing numb • Heightened arousal (jumpy, easily started, difficulty concentrating) • Behavioural changes (increased irritability, temper tantrums, fussiness, attention-needing, aggressiveness) • Separation anxiety/clinginess • Regression of behaviours Development of NEW fears: • Physical complaints • Changes in appetite • Relationship difficulties with caregivers, siblings, peers
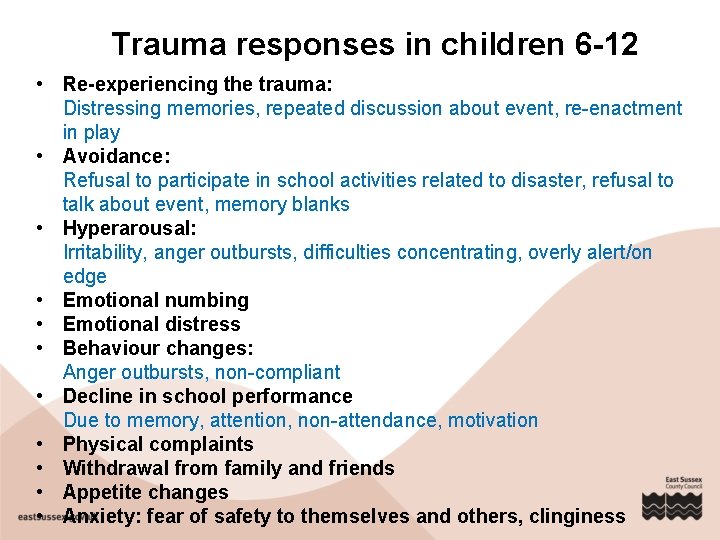
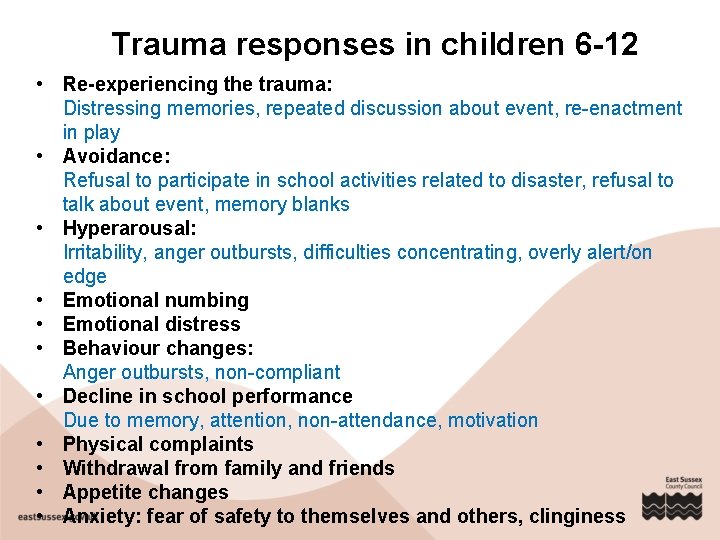
Trauma responses in children 6 -12 • Re-experiencing the trauma: Distressing memories, repeated discussion about event, re-enactment in play • Avoidance: Refusal to participate in school activities related to disaster, refusal to talk about event, memory blanks • Hyperarousal: Irritability, anger outbursts, difficulties concentrating, overly alert/on edge • Emotional numbing • Emotional distress • Behaviour changes: Anger outbursts, non-compliant • Decline in school performance Due to memory, attention, non-attendance, motivation • Physical complaints • Withdrawal from family and friends • Appetite changes • Anxiety: fear of safety to themselves and others, clinginess
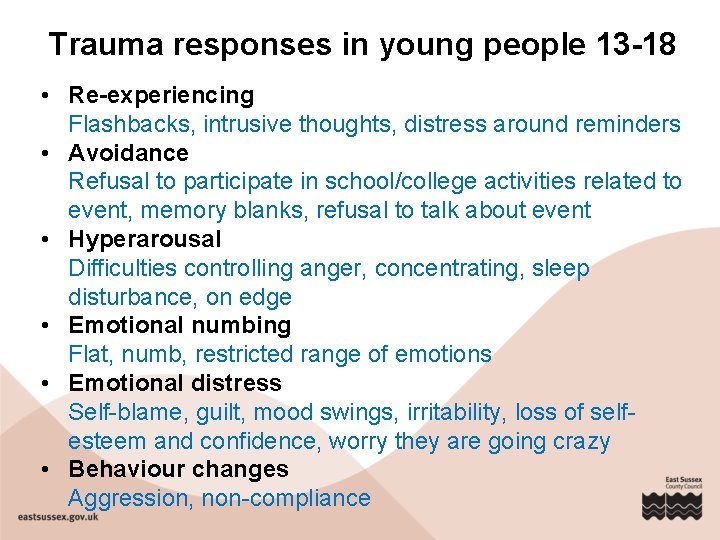
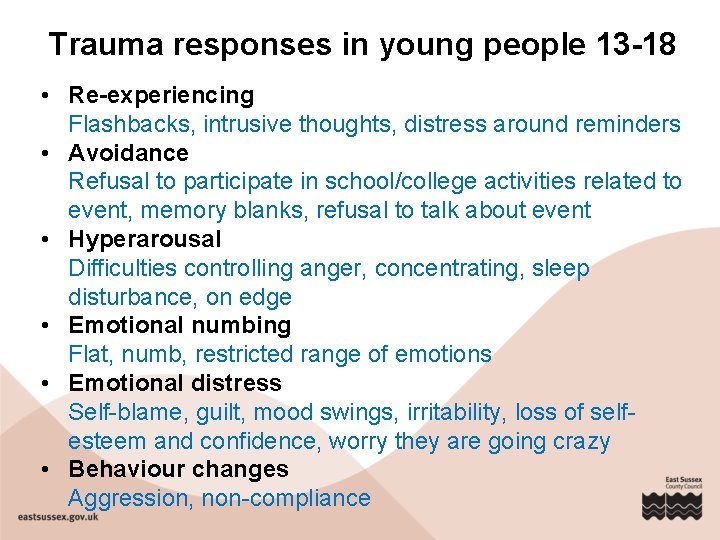
Trauma responses in young people 13 -18 • Re-experiencing Flashbacks, intrusive thoughts, distress around reminders • Avoidance Refusal to participate in school/college activities related to event, memory blanks, refusal to talk about event • Hyperarousal Difficulties controlling anger, concentrating, sleep disturbance, on edge • Emotional numbing Flat, numb, restricted range of emotions • Emotional distress Self-blame, guilt, mood swings, irritability, loss of selfesteem and confidence, worry they are going crazy • Behaviour changes Aggression, non-compliance
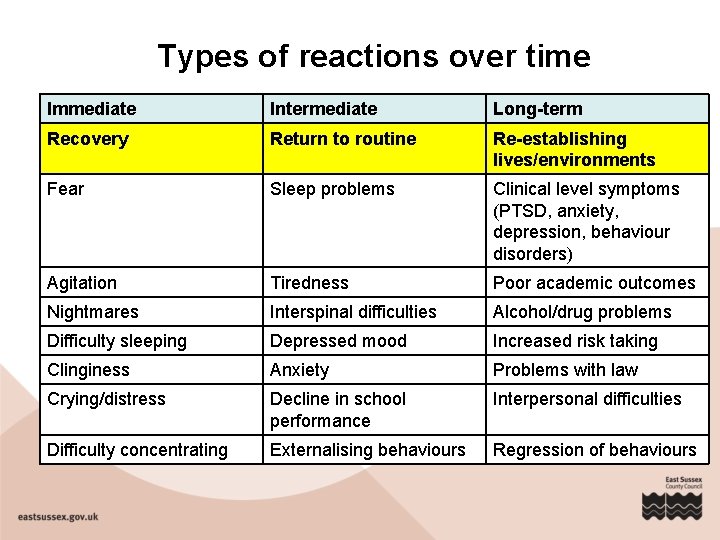
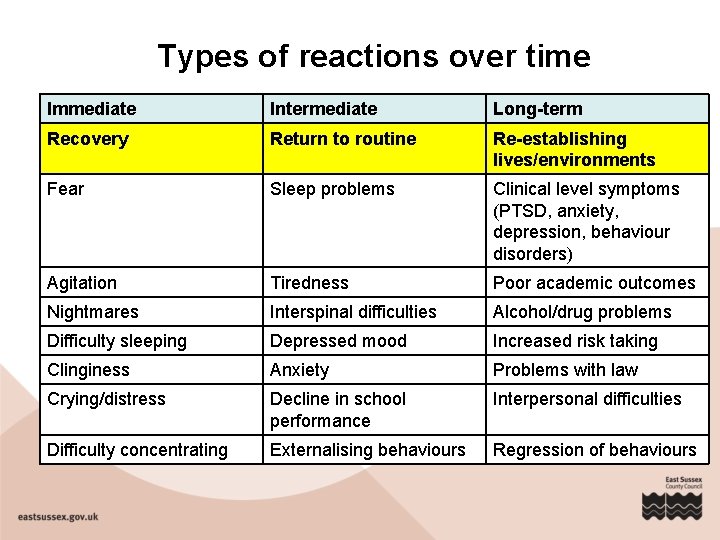
Types of reactions over time Immediate Intermediate Long-term Recovery Return to routine Re-establishing lives/environments Fear Sleep problems Clinical level symptoms (PTSD, anxiety, depression, behaviour disorders) Agitation Tiredness Poor academic outcomes Nightmares Interspinal difficulties Alcohol/drug problems Difficulty sleeping Depressed mood Increased risk taking Clinginess Anxiety Problems with law Crying/distress Decline in school performance Interpersonal difficulties Difficulty concentrating Externalising behaviours Regression of behaviours
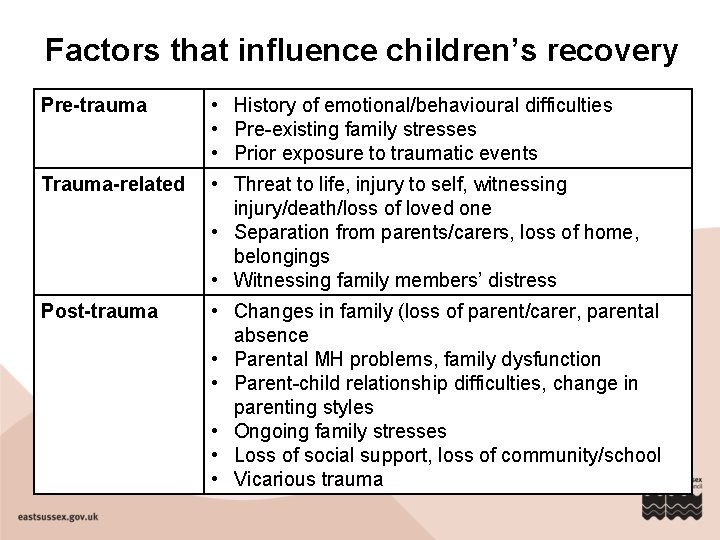
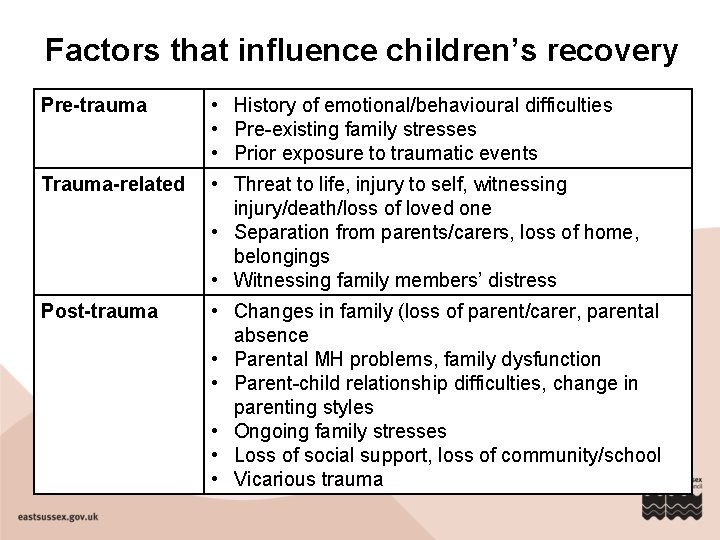
Factors that influence children’s recovery Pre-trauma • History of emotional/behavioural difficulties • Pre-existing family stresses • Prior exposure to traumatic events Trauma-related • Threat to life, injury to self, witnessing injury/death/loss of loved one • Separation from parents/carers, loss of home, belongings • Witnessing family members’ distress Post-trauma • Changes in family (loss of parent/carer, parental absence • Parental MH problems, family dysfunction • Parent-child relationship difficulties, change in parenting styles • Ongoing family stresses • Loss of social support, loss of community/school • Vicarious trauma
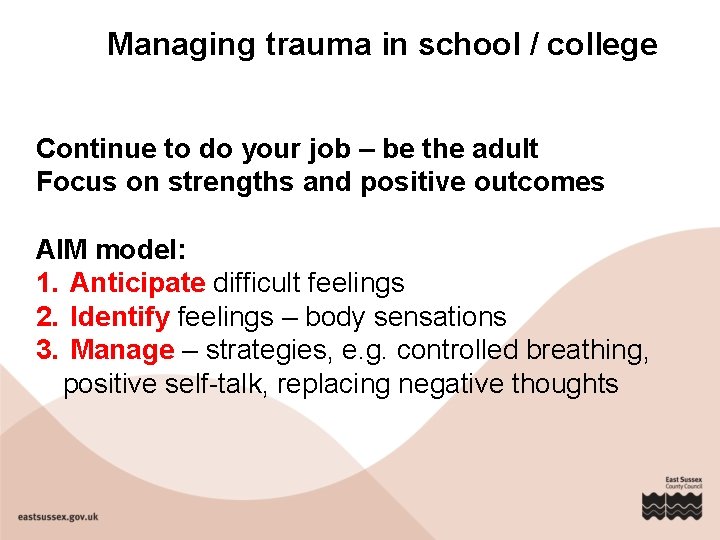
Managing trauma in school / college Continue to do your job – be the adult Focus on strengths and positive outcomes AIM model: 1. Anticipate difficult feelings 2. Identify feelings – body sensations 3. Manage – strategies, e. g. controlled breathing, positive self-talk, replacing negative thoughts
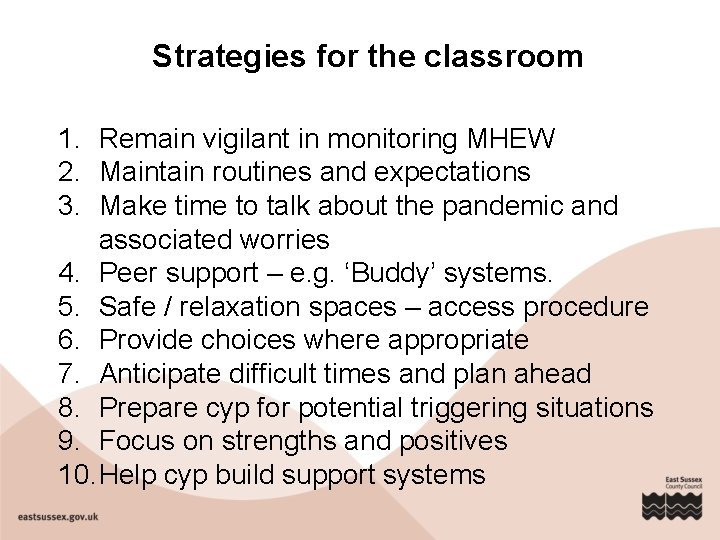
Strategies for the classroom 1. Remain vigilant in monitoring MHEW 2. Maintain routines and expectations 3. Make time to talk about the pandemic and associated worries 4. Peer support – e. g. ‘Buddy’ systems. 5. Safe / relaxation spaces – access procedure 6. Provide choices where appropriate 7. Anticipate difficult times and plan ahead 8. Prepare cyp for potential triggering situations 9. Focus on strengths and positives 10. Help cyp build support systems
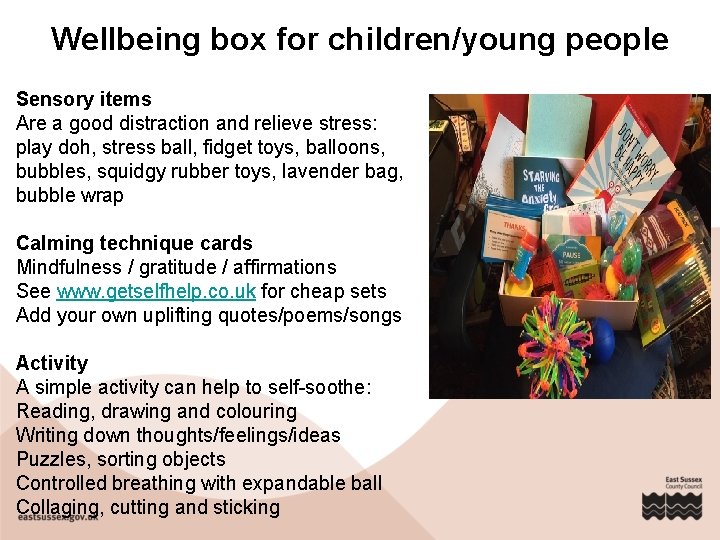
Wellbeing box for children/young people Sensory items Are a good distraction and relieve stress: play doh, stress ball, fidget toys, balloons, bubbles, squidgy rubber toys, lavender bag, bubble wrap Calming technique cards Mindfulness / gratitude / affirmations See www. getselfhelp. co. uk for cheap sets Add your own uplifting quotes/poems/songs Activity A simple activity can help to self-soothe: Reading, drawing and colouring Writing down thoughts/feelings/ideas Puzzles, sorting objects Controlled breathing with expandable ball Collaging, cutting and sticking
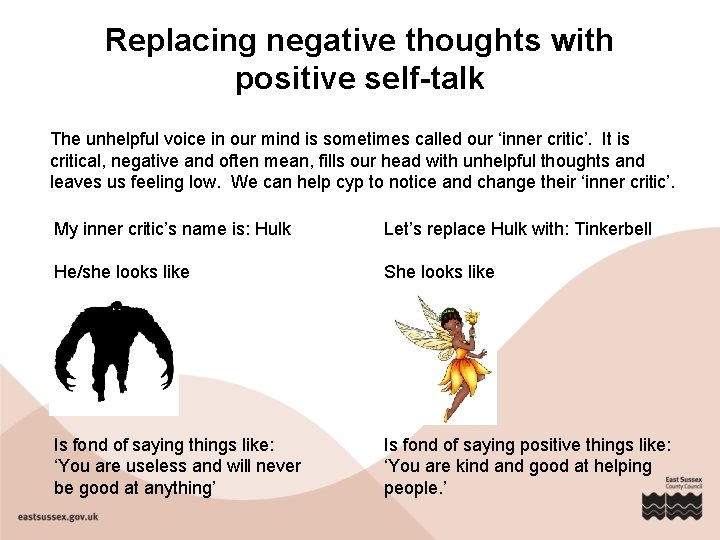
Replacing negative thoughts with positive self-talk The unhelpful voice in our mind is sometimes called our ‘inner critic’. It is critical, negative and often mean, fills our head with unhelpful thoughts and leaves us feeling low. We can help cyp to notice and change their ‘inner critic’. My inner critic’s name is: Hulk Let’s replace Hulk with: Tinkerbell He/she looks like She looks like Is fond of saying things like: ‘You are useless and will never be good at anything’ Is fond of saying positive things like: ‘You are kind and good at helping people. ’
Gather more information Talk to the cyp • Create a safe environment ‘You’ve been through a lot. Everyone reacts differently to events like this and it’s normal to find it difficult to talk about. ’ • Convey understanding • Ask general, then specific questions (careful not to push) ‘How have things been going for you since X? ’ ‘I’ve noticed that you’ve stopped doing some things that you used to enjoy. Can you tell me about that? ’ • Show the cyp you are listening (check understanding) ‘So it seems like things have been a bit difficult at home since X and that Mum and Dad are also feeling a bit stressed. Is that right? ’ • Acknowledge emotions as real and distressing • Focus on strengths and positive coping…. .
Further action • Enlist additional support (colleagues, in-school support, counsellor, School Health) Check if there is an adult in school that the cyp would like to speak to • Follow your usual safeguarding protocols • Refer to additional support if: • Symptoms persist or worsen over time • Cyp shows significant decline in performance • Problems interfere with daily functioning or cause significant distress • Specific (ongoing or worsening) problems regulating emotions, e. g. difficulty controlling crying, anger, etc. • Significant and lasting changes in social functioning
Working with parents/carers • Check whether parent/carer agrees with concerns • Check if there any issues at home that may be contributing to cyp’s behaviour ‘Is there anything else going on at home, or with friends that might be making it difficult for X at the moment? ’ • Normalise difficulties and reassure family • Check how teacher and school/college can help the family ‘It seems like X is having some difficulties at the moment. If you think you might find it useful to have some help, I can help you find an appropriate person/service. ’ • Provide information/advice on additional support
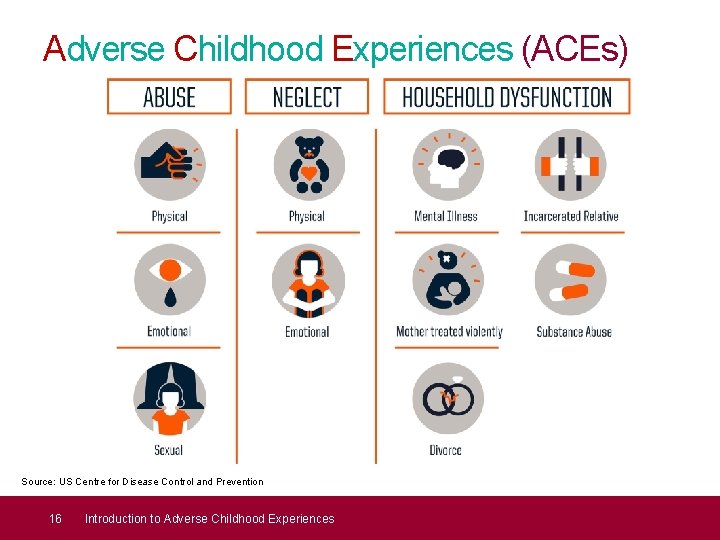
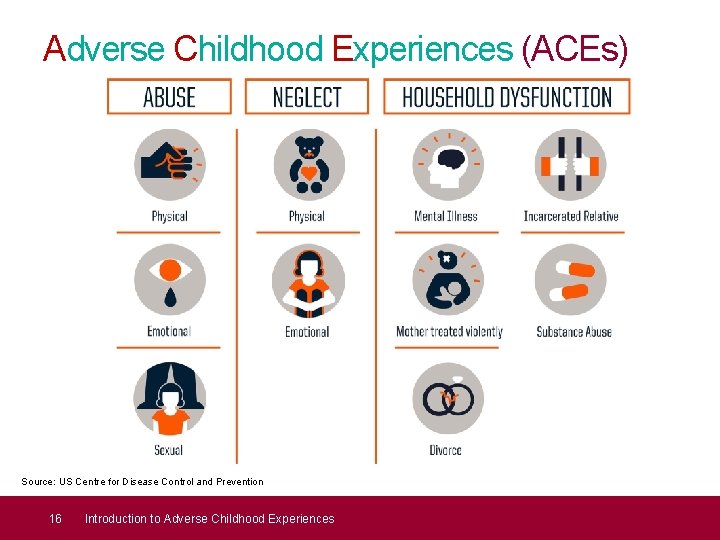
Adverse Childhood Experiences (ACEs) Source: US Centre for Disease Control and Prevention 16 Introduction to Adverse Childhood Experiences
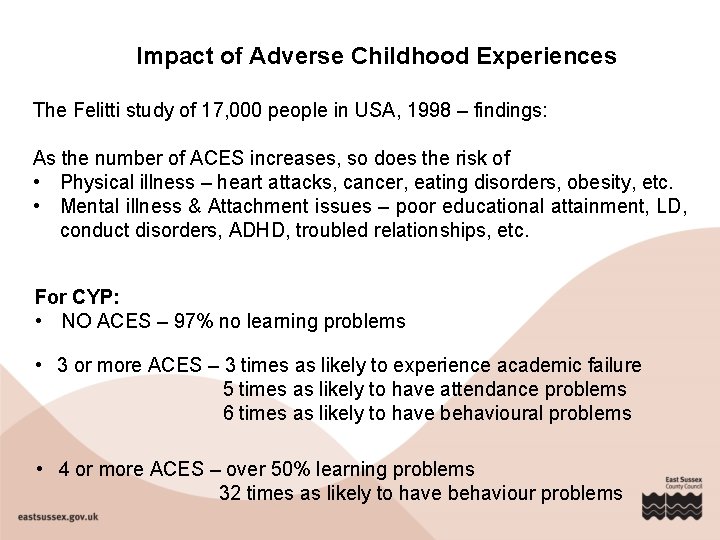
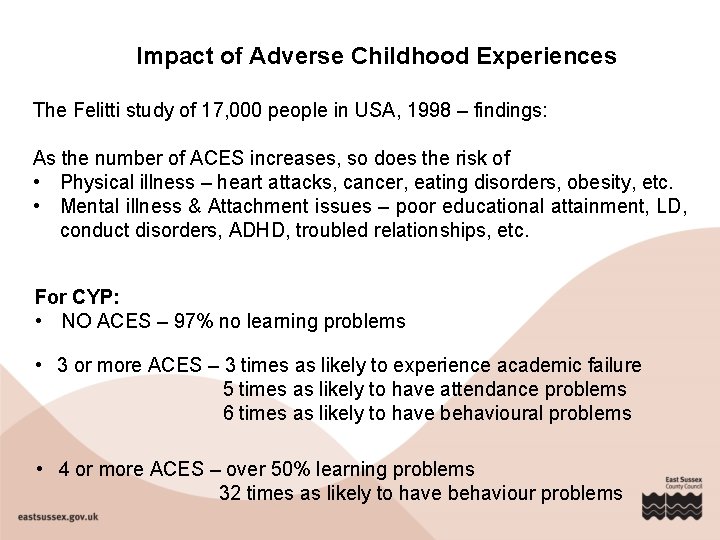
Impact of Adverse Childhood Experiences The Felitti study of 17, 000 people in USA, 1998 – findings: As the number of ACES increases, so does the risk of • Physical illness – heart attacks, cancer, eating disorders, obesity, etc. • Mental illness & Attachment issues – poor educational attainment, LD, conduct disorders, ADHD, troubled relationships, etc. For CYP: • NO ACES – 97% no learning problems • 3 or more ACES – 3 times as likely to experience academic failure 5 times as likely to have attendance problems 6 times as likely to have behavioural problems • 4 or more ACES – over 50% learning problems 32 times as likely to have behaviour problems
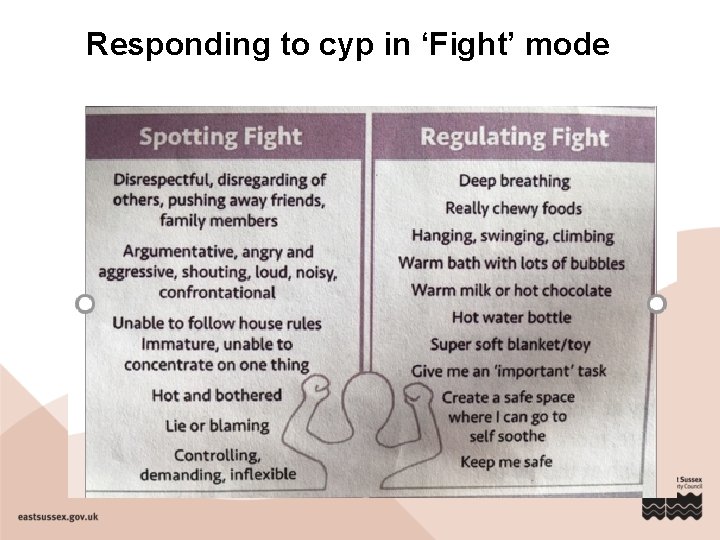
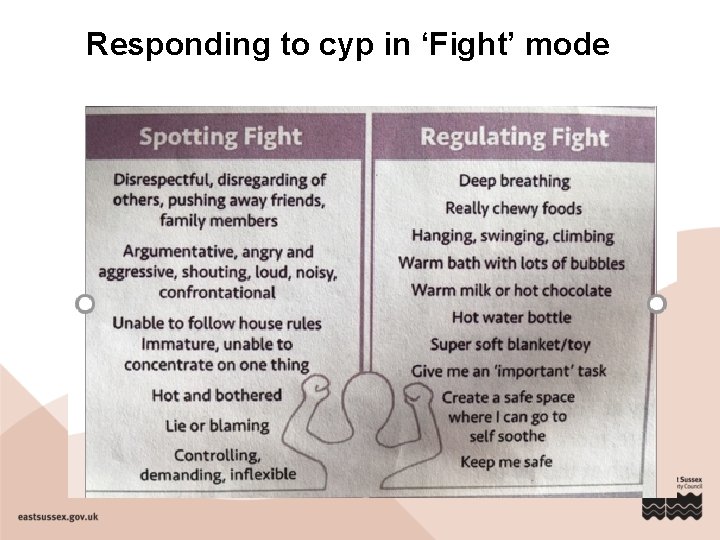
Responding to cyp in ‘Fight’ mode
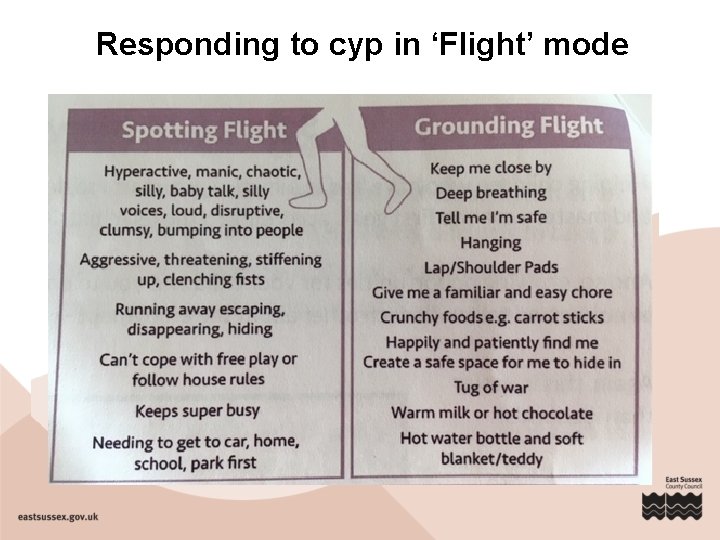
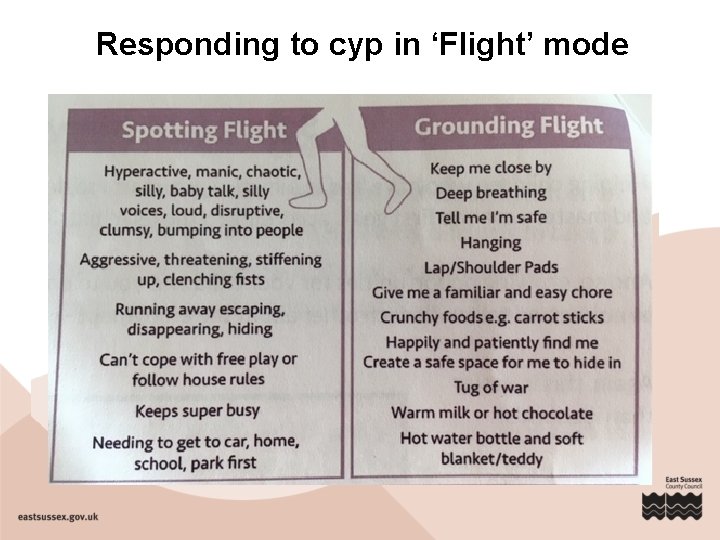
Responding to cyp in ‘Flight’ mode
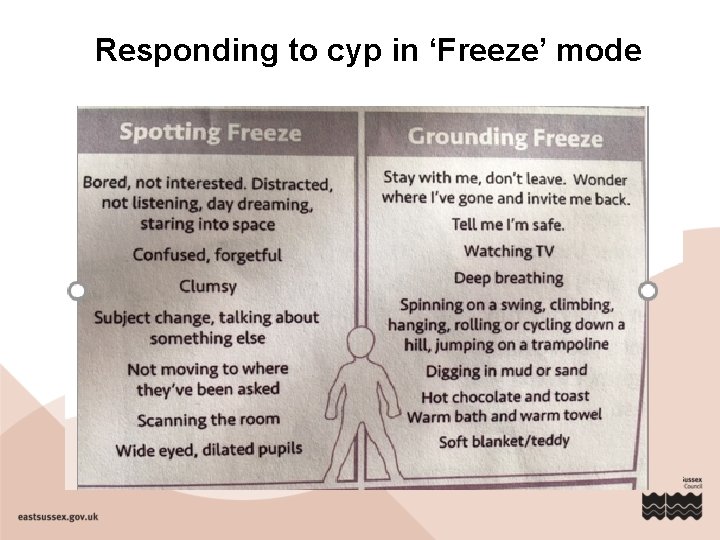
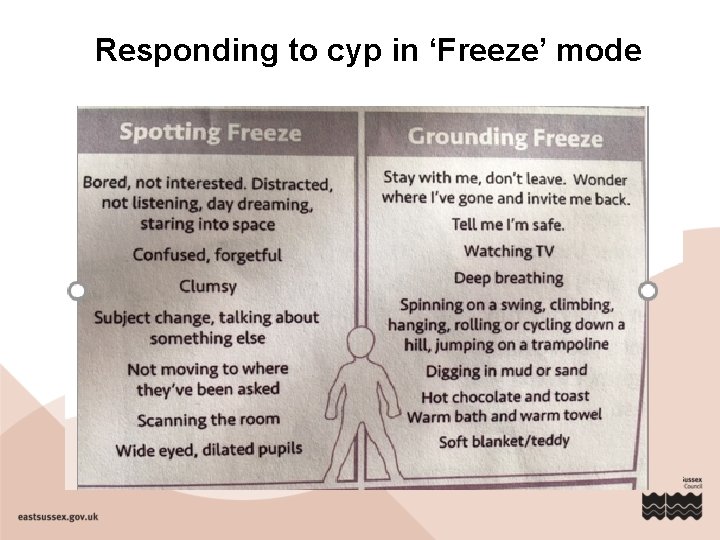
Responding to cyp in ‘Freeze’ mode
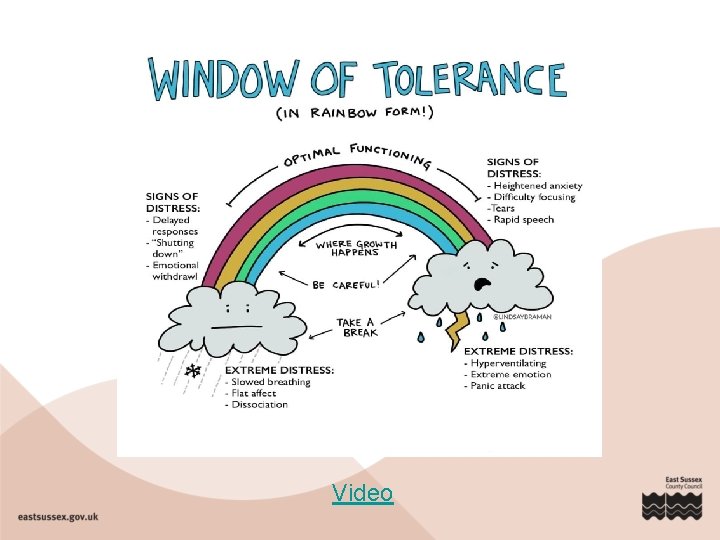
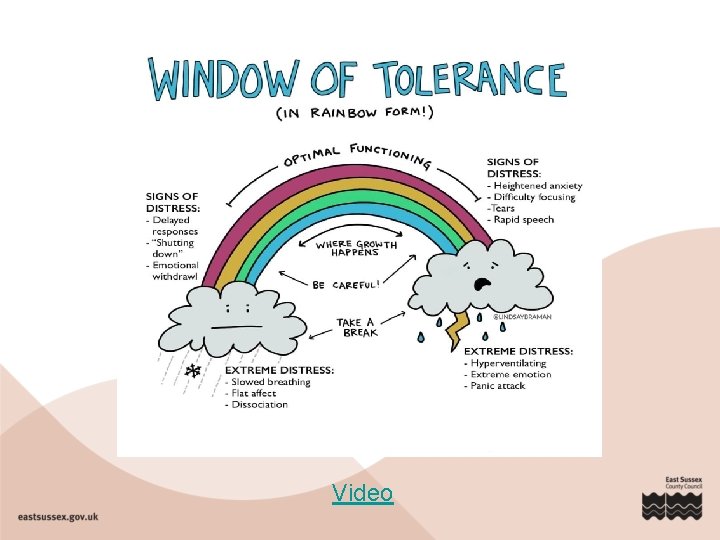
Video
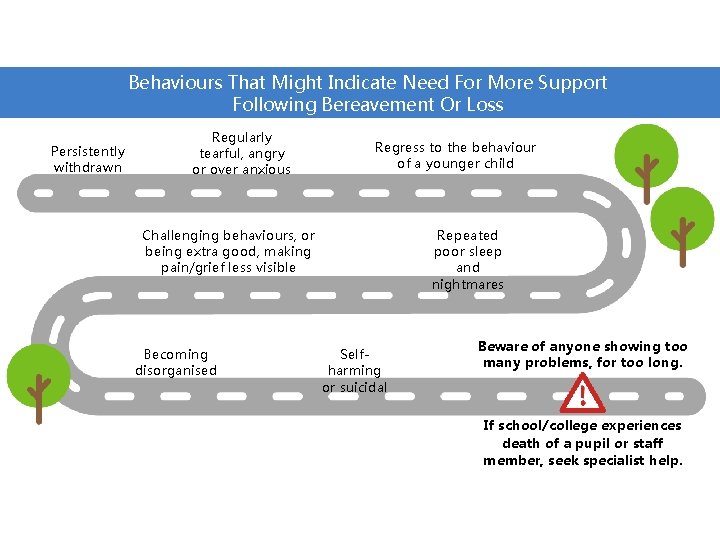
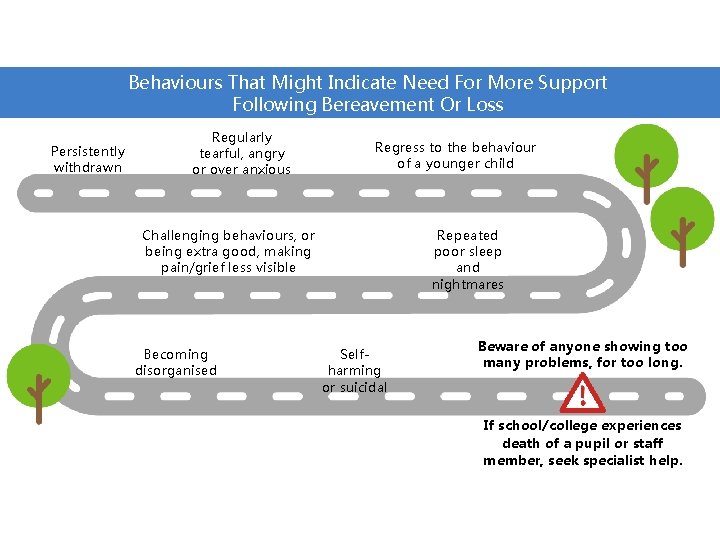
Behaviours That Might Indicate Need For More Support Following Bereavement Or Loss Persistently withdrawn Regularly tearful, angry or over anxious Regress to the behaviour of a younger child Repeated poor sleep and nightmares Challenging behaviours, or being extra good, making pain/grief less visible Becoming disorganised Selfharming or suicidal Beware of anyone showing too many problems, for too long. If school/college experiences death of a pupil or staff member, seek specialist help.
Vicarious trauma Staff who look after themselves are better able to manage cyp Staff distress = difficulty reacting in calm and constructive ways Tips for staff self-care • Monitor own reactions, emotions and needs • Seek help for trauma-related distress • Define your support system • Plan ahead: schedule relaxation/quiet time • Use positive coping strategies ü Breathing techniques, muscle relaxation, imagery ü Replace unhelpful thoughts with positive statements ü Use self-help resources: websites, apps, books • Maintain healthy habits • Schedule time for yourself, family and friends • Spend time with cyp who have NOT experienced traumatic stress
MHEW whole school programmes in East Sussex Therapeutic Thinking Overarching principles: de-escalation, consistency and teaching internal discipline; care and control, not punishment; reducing exclusions. ELSAs – Emotional Literacy Support Assistants – Educational Psychology Service Accredited* school support staff who plan and deliver evidence-based early intervention programmes to help a child recognise and manage their emotions. Action your Potential - neuroscience-based sessions. Currently commissioned by ESCC for selected schools. Mental Health First Aid Training Support from ESCC Children’s Services for a range of SEND and MHEW needs School Health Service, Children’s Social Care, CAMHS, MH Support Teams The Empowerment Approach - Independent Positive Behaviour Training