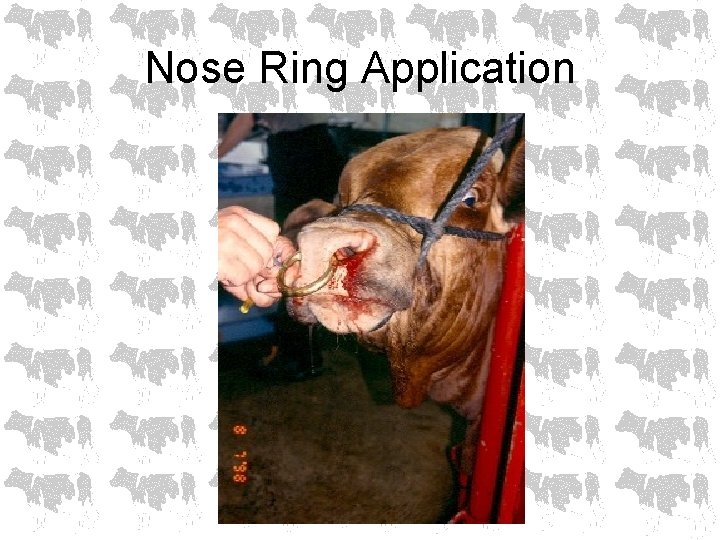
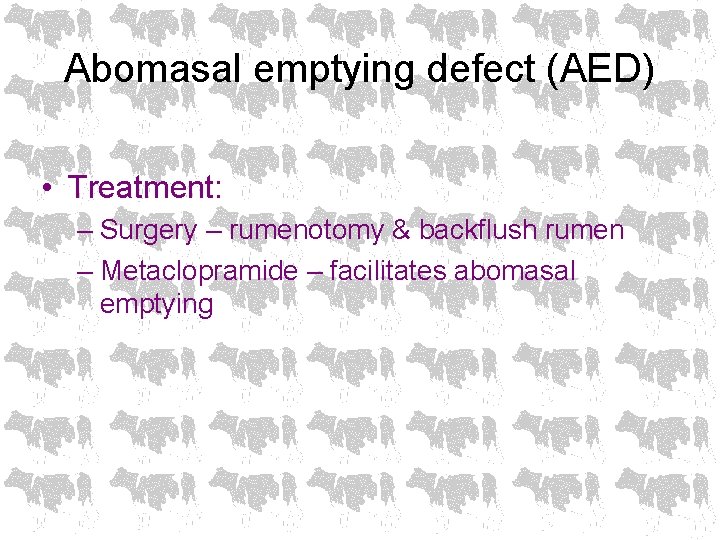
Nose Ring Application Nose Ring Application Nose Ring

- Slides: 70
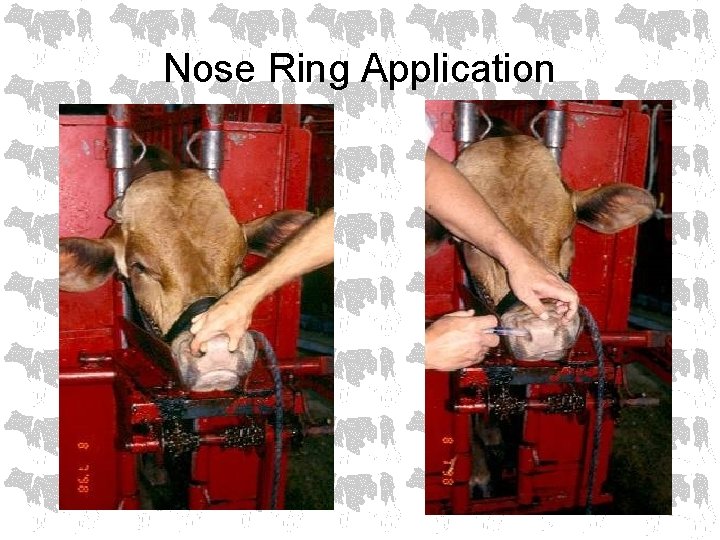
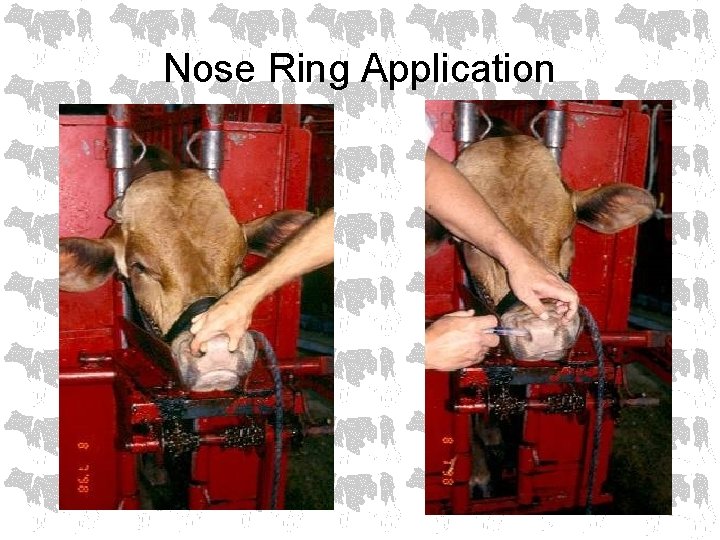
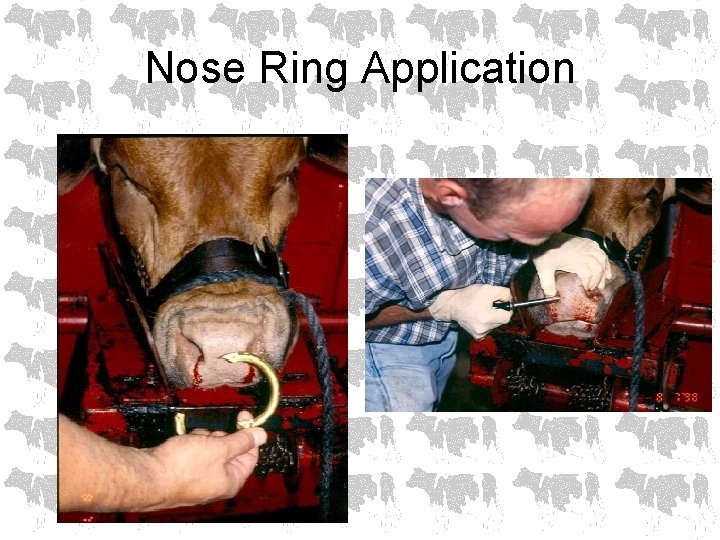
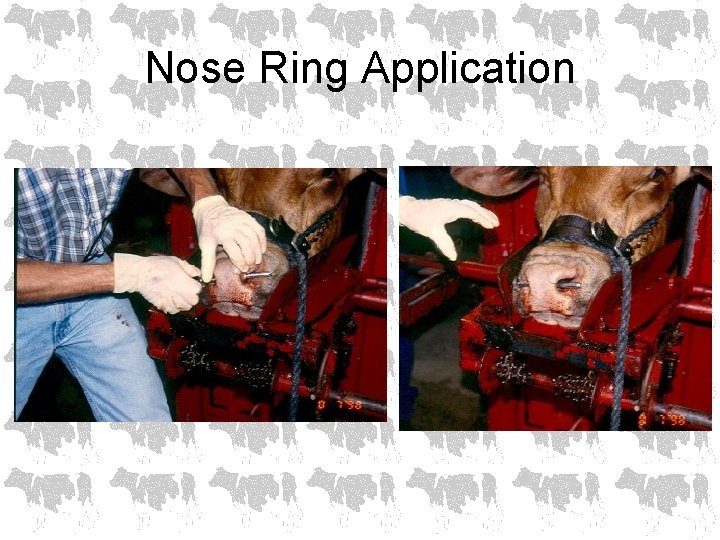
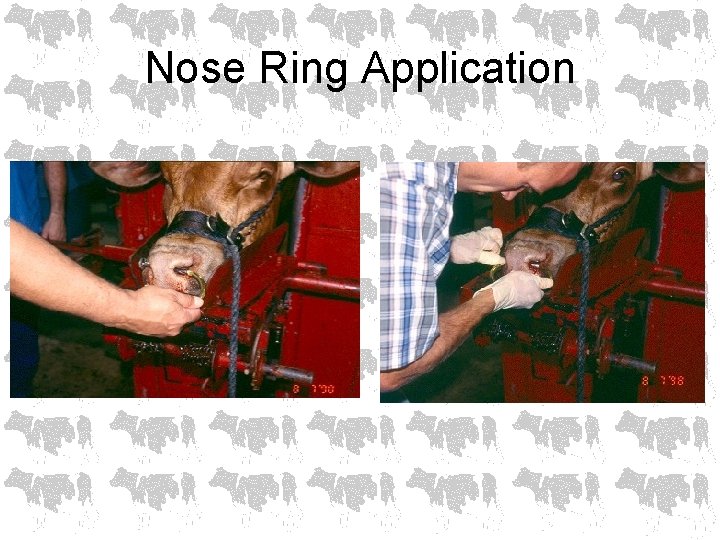
Nose Ring Application
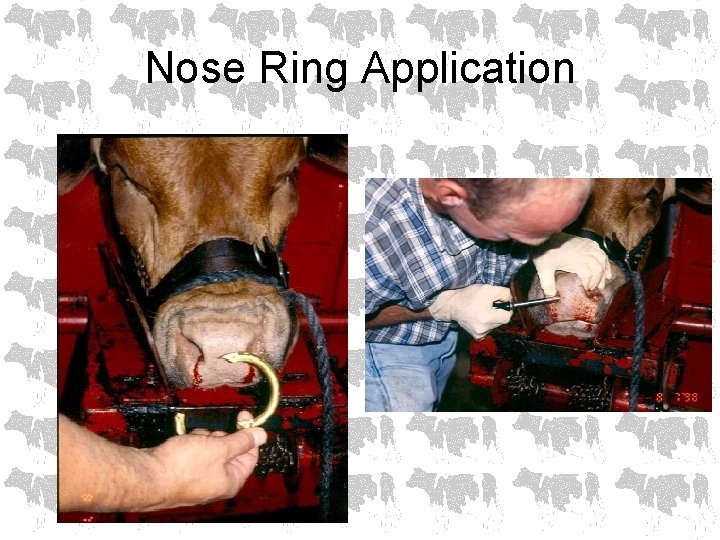
Nose Ring Application
Nose Ring Application
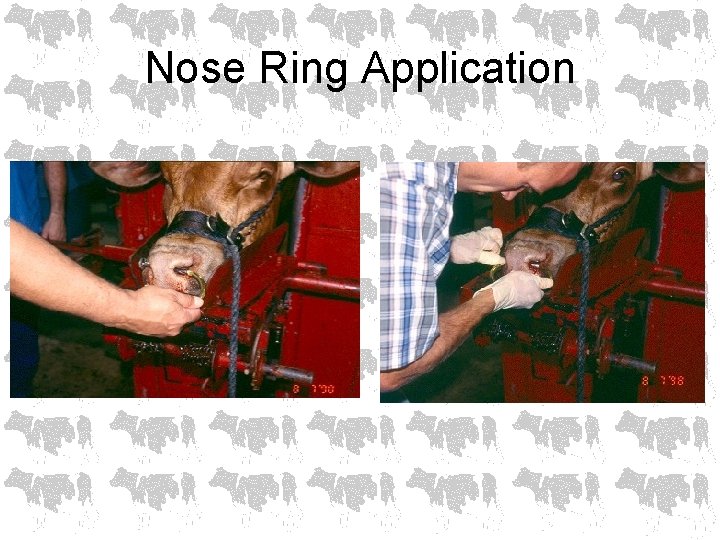
Nose Ring Application
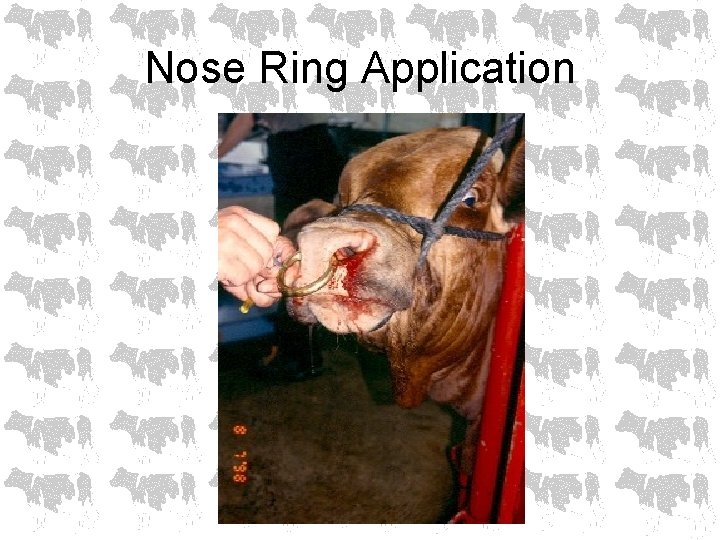
Nose Ring Application
Diseases of the Forestomachs M. S. Gill, D. V. M. , M. S.
Ruminant Carbohydrate Engorgement • • • Grain overload Lactic acidosis Carbohydrate intoxication Grain engorgement Founder
History • Access to highly fermentable feedstuffs – by unaccustomed animals, or – in larger than normal amounts • May involve several animals in herd • Rapid clinical course
Clinical findings • • Abdominal pain Dehydration (6 -12 %) Diarrhea – fluid, fetid Splashy rumen, bloat Depression Lameness Scleral injection
Clinical findings • Elevated temp initially, may be subnormal when presented • HR = 80 -140 bpm • RR elevated (blow off CO 2) • Rumen fluid analysis – p. H < 5 – sour odor – protozoa dead, predominance of gram +
Clinical findings • • • Metabolic acidosis PCV protein Elevated BUN, creatinine, phosphorous Increased anion gap Decreased calcium
Pathogenesis • Excess CHO ingestion, VFAs, rumen p. H, rumen motility, Strep bovis proliferates producing lactic acid, further p. H (4 -5) • Acid resistant Lactobacillus spp. proliferate producing lactic acid
Pathogenesis • Lactic acid accumulation in the rumen osmolarity of the rumen fluid drawing more body water into the rumen (creates the “splashy rumen”) • Loss of body water causes dehydration contributing to acidosis • Lactic acid is absorbed from rumen as well as from small intestine & profound lactic acidosis develops
Pathogenesis • Acidic rumen p. H damages mucosal surfaces in the forestomachs & intestine • Blood vessels thrombose & sections of rumen mucosa & submucosa slough allowing bacteria to invade • Bacteria travel to liver via portal circulation & cause liver abscesses • Mycotic ruminitis may develop
Pathogenesis • Histamine levels increase • Ethanol, methanol, tyramine, tryptamine production contribute to CNS depression • Thiaminase production may result in development of polio • Death of Gram – bacteria can cause endotoxin release
What feeds can cause carbohydrate engorgement? • Cereal grains • Industrial byproducts (brewers grains, sugars) • Fruits • Tubers (potatoes, sugar beets)
What feeds can cause carbohydrate engorgement? • Finely ground feeds with large surface area promote rapid fermentation • Hay and grass are not highly fermentable due to cellulose and large particle size • Corn silage usually not a problem because much of CHO already reduced to VFAs in ensiling process and also due to large particle size
Diagnosis • • History Clinical signs and clinical findings Rumen fluid analysis CBC, chem panel, blood gas
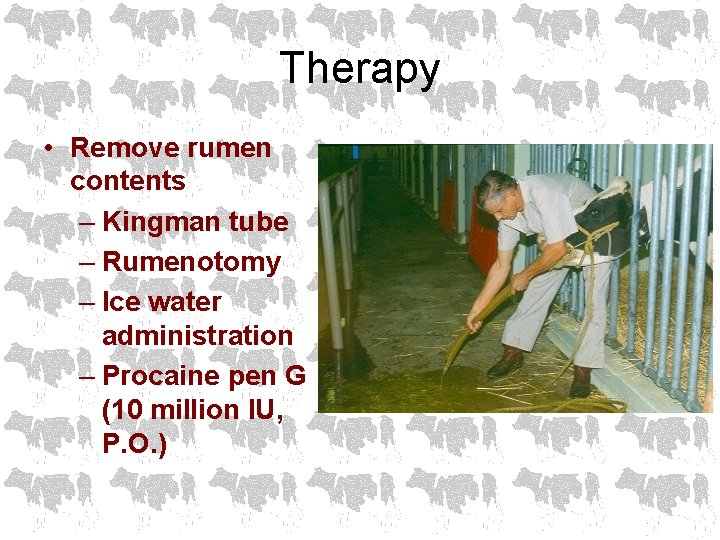
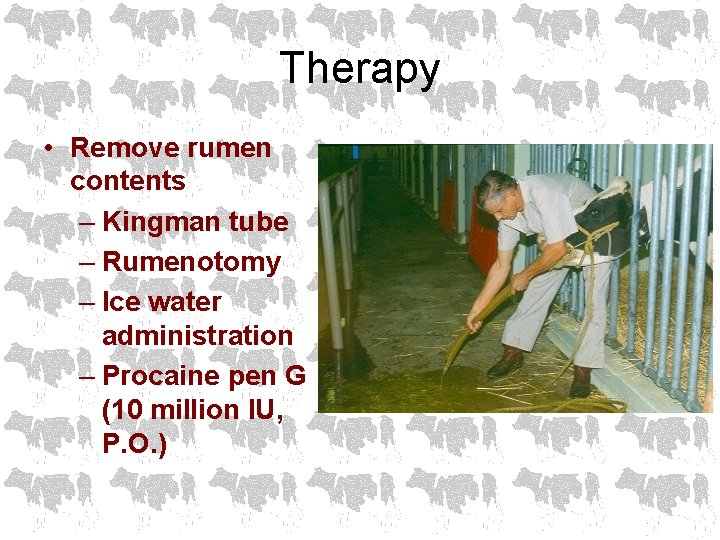
Therapy • Remove rumen contents – Kingman tube – Rumenotomy – Ice water administration – Procaine pen G (10 million IU, P. O. )
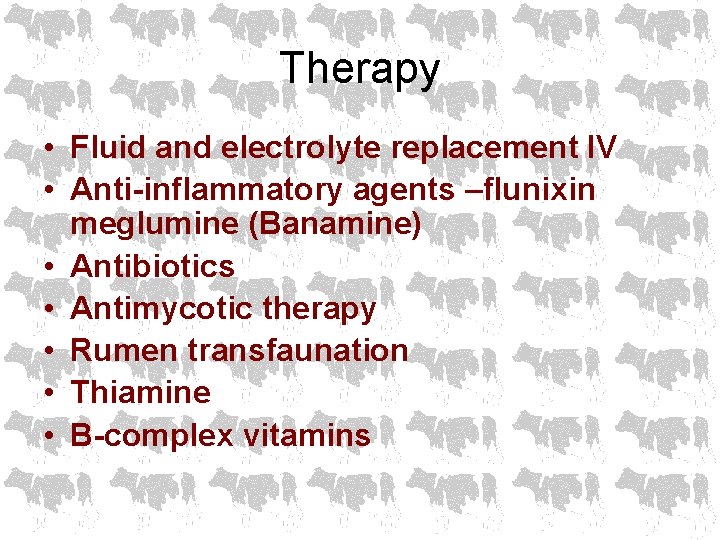
Therapy • Fluid and electrolyte replacement IV • Anti-inflammatory agents –flunixin meglumine (Banamine) • Antibiotics • Antimycotic therapy • Rumen transfaunation • Thiamine • B-complex vitamins
Client education • Make dietary changes very gradually – Addition of antibiotics, HCO 3 -, and ionophore antibiotics to the feed have been beneficial but do not replace good management • Rumen adaptation may take 6 weeks
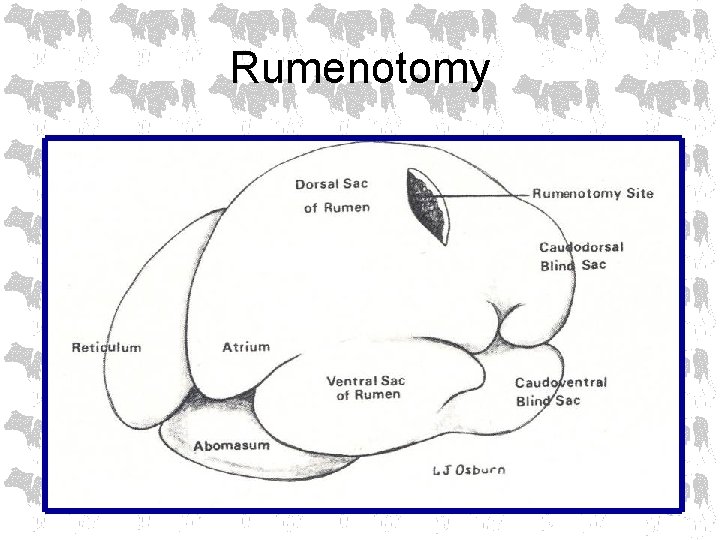
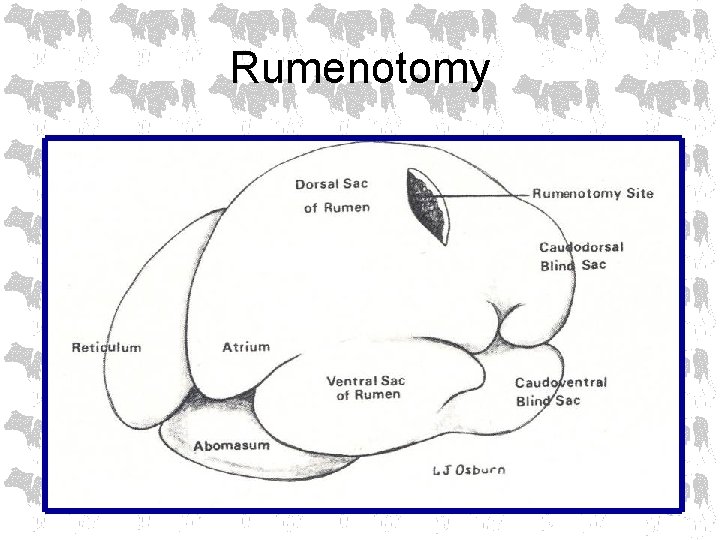
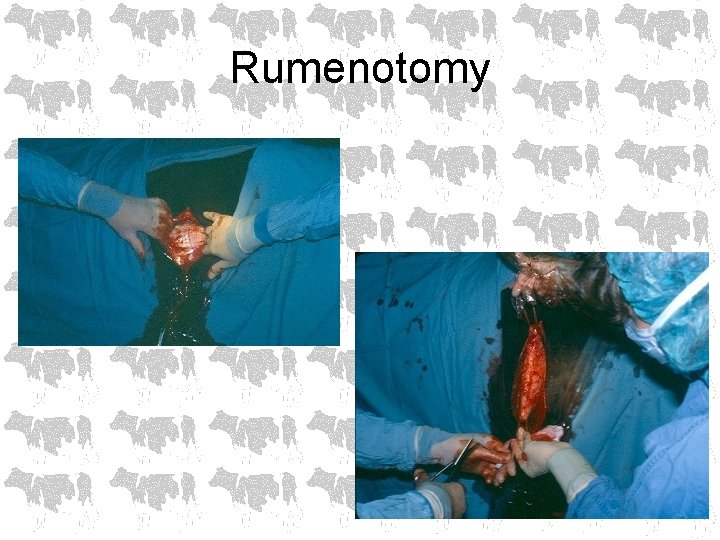
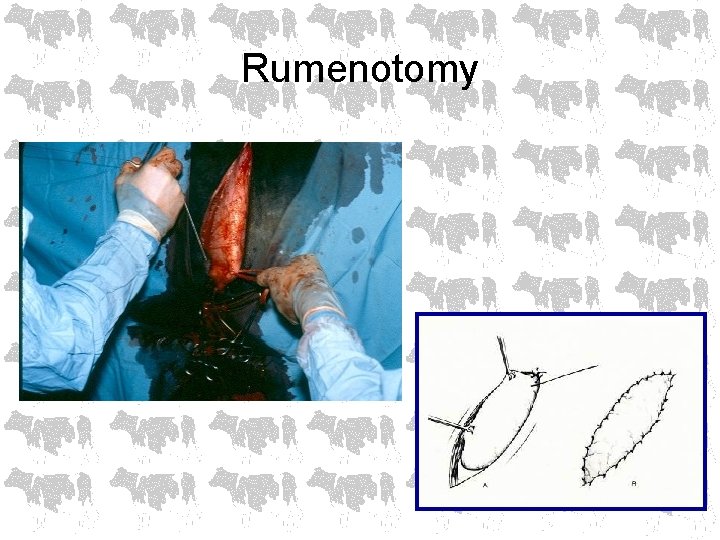
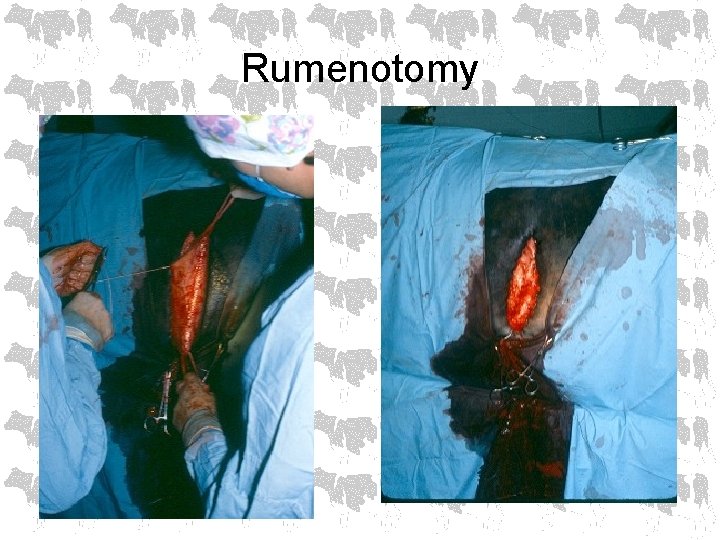
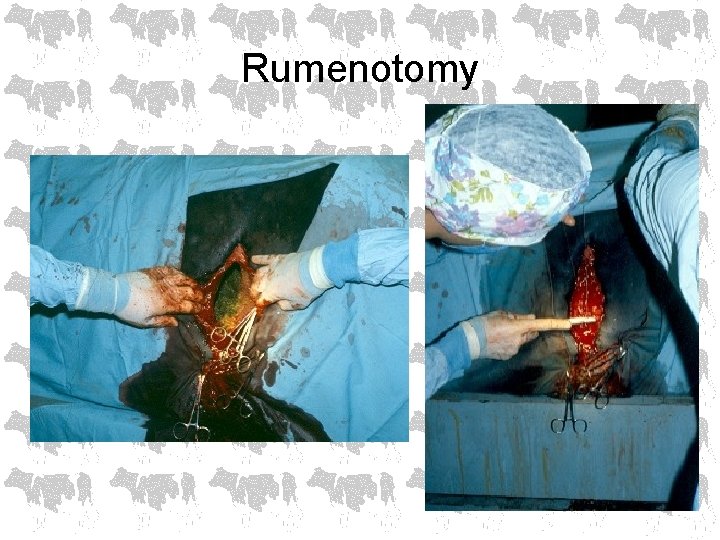
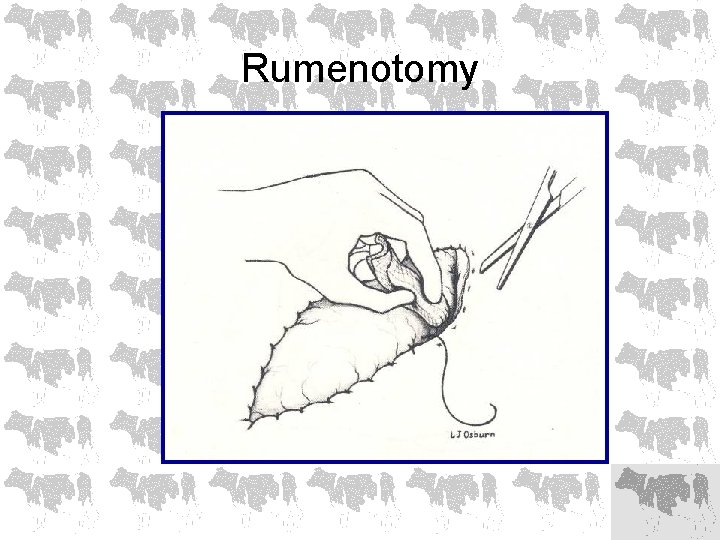
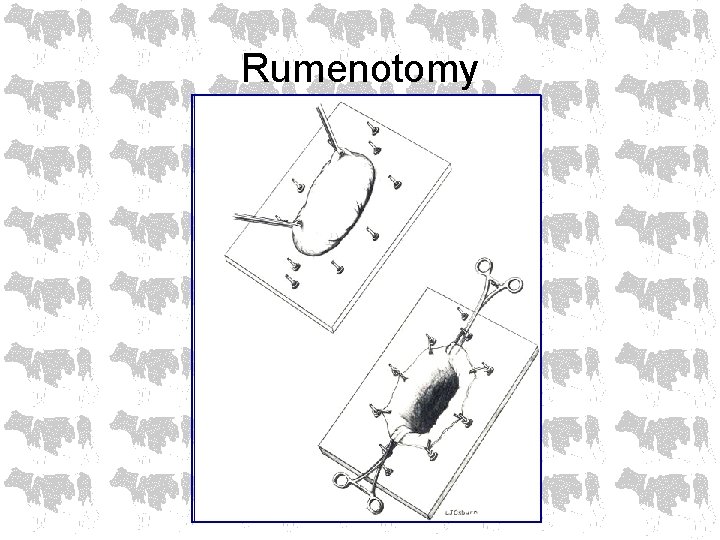
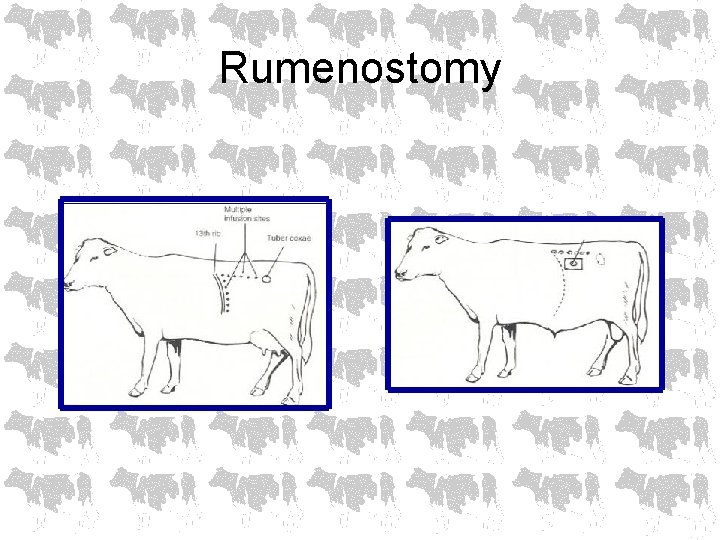
Rumenotomy
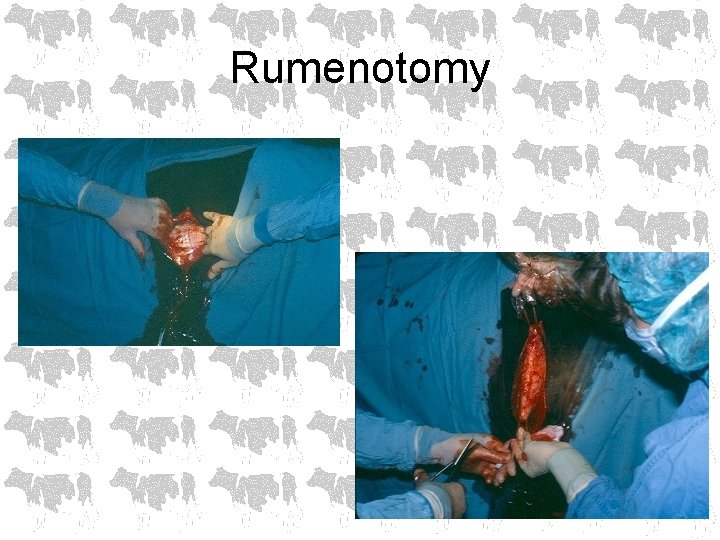
Rumenotomy
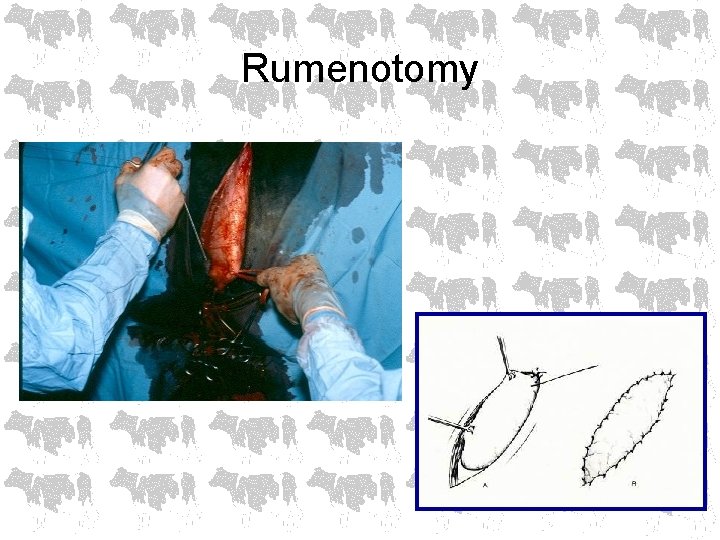
Rumenotomy
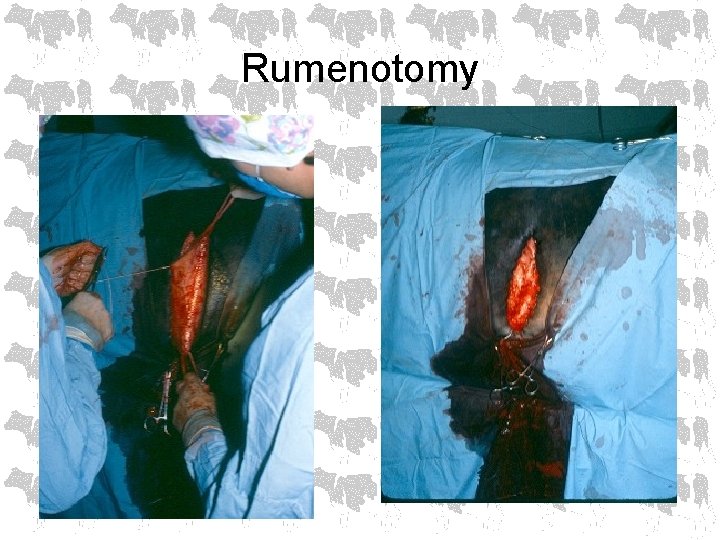
Rumenotomy
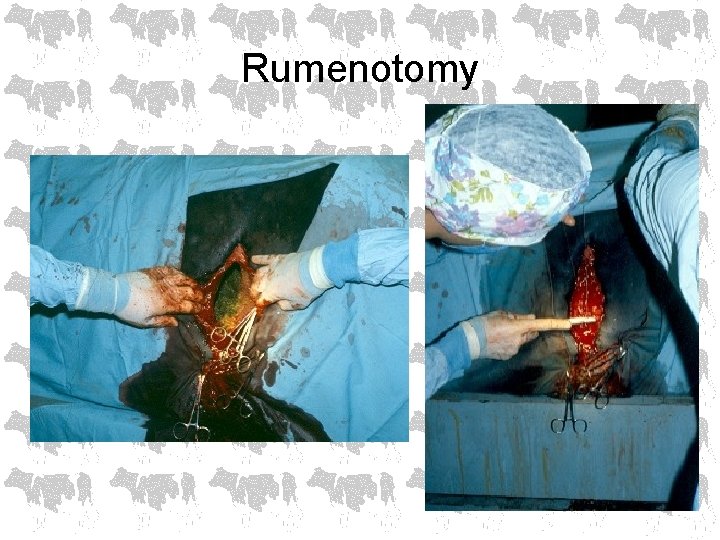
Rumenotomy
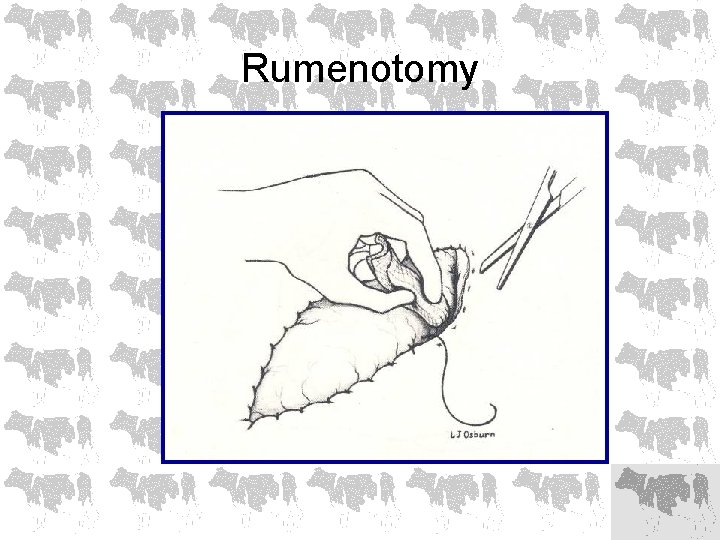
Rumenotomy
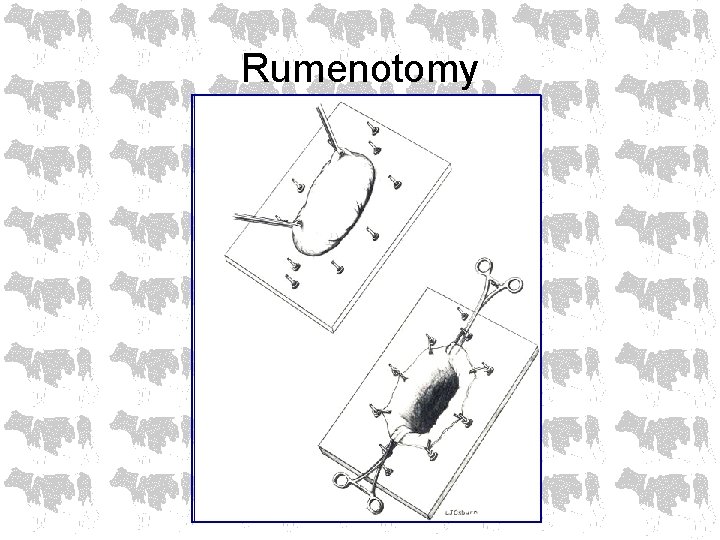
Rumenotomy
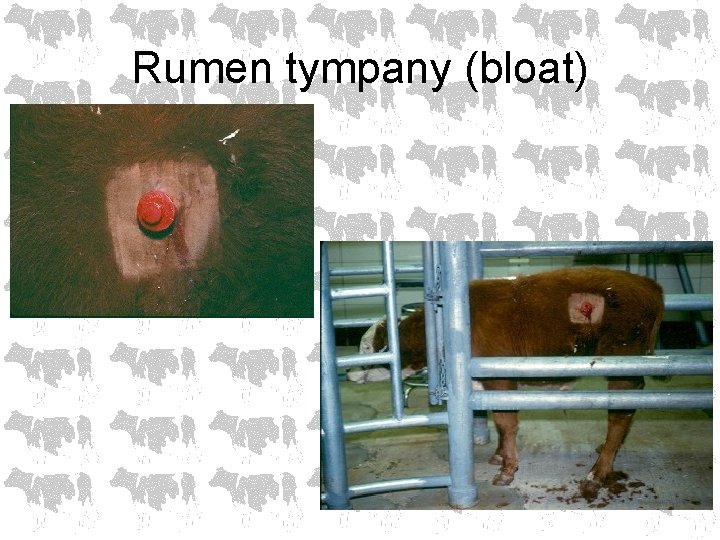
Rumen tympany (bloat) • Gas production is a normal occurrence during rumen fermentation • Bloat occurs if eructation is prevented for any reason
Clinical findings • • Distended left paralumbar fossa Discomfort (grunting, colic) Open-mouth breathing Anorexia Salivation Anxious Depressed terminally Sudden death
Types of bloat • Primary – Eructation normal but gas cannot be expelled • frothy bloat – legumes or grain (Strep bovis) • Secondary – Failure of eructation • • • esophageal FB’s vagus indigestion positional hypocalcemia pharyngitis
Diagnosis • History • Clinical findings
THERAPY • Free gas bloat – Pass a stomach tube (carefully) either nasogastric or orogastric – If positional, roll cow into sternal recumbency – Force exercise – If hypocalcemia, administer calcium – Rumen stimulents – Rumen trocharization for emergencies only

THERAPY • Frothy bloat – Reduce surface tension • • Poloxalene – 2 oz. Household detergent (Tide 2 -3 oz. ) Mineral oil Dioctyl sodium sulfosuccinate (DSS) *All of the above reduce surface tension allowing consolidation of tiny bubbles into a free gas bloat which can be eructated or relieved via tube
THERAPY • Chronic bloat – typically free gas bloat associated with high grain diets that may cause a permanent shift in microflora – Increase fiber in diet & reduce grain – Rumen transfaunation – Temporary rumenostomy in severe cases • May be 2° to another problem such as vagus indigestion
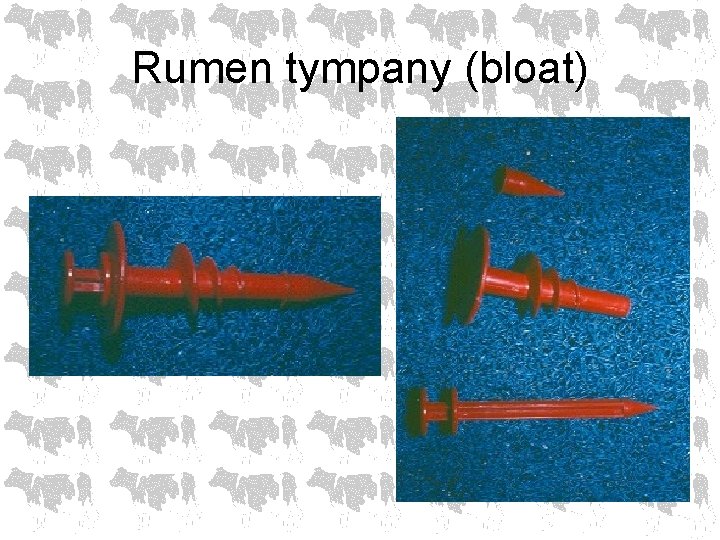
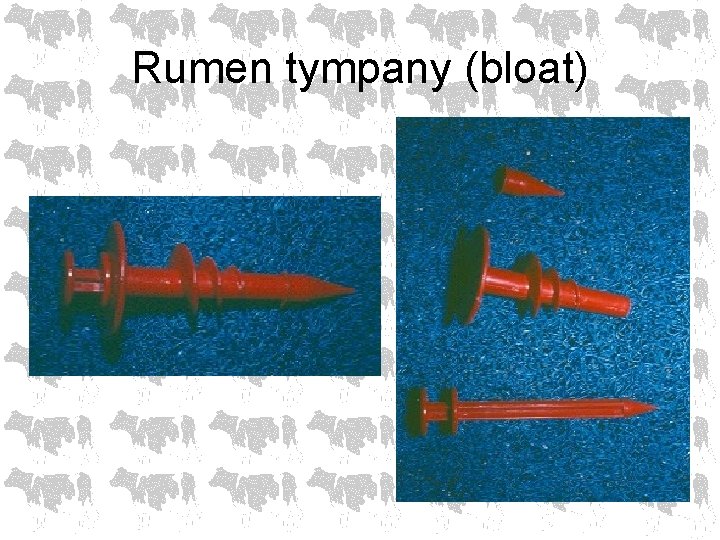
Rumen tympany (bloat)
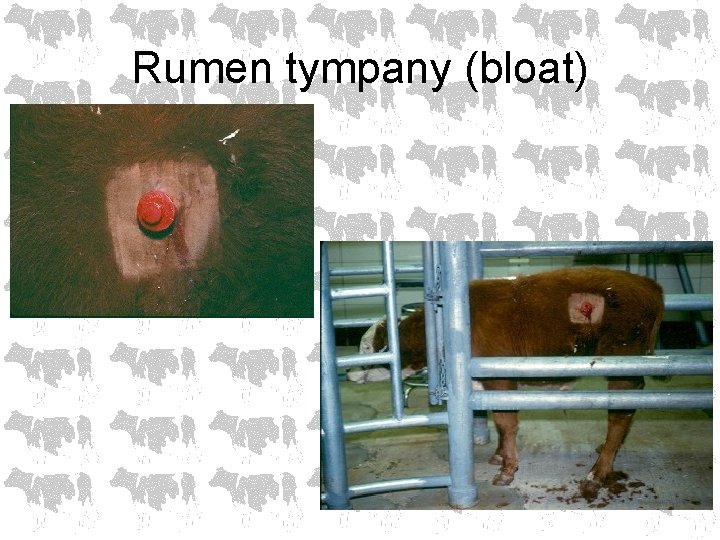
Rumen tympany (bloat)
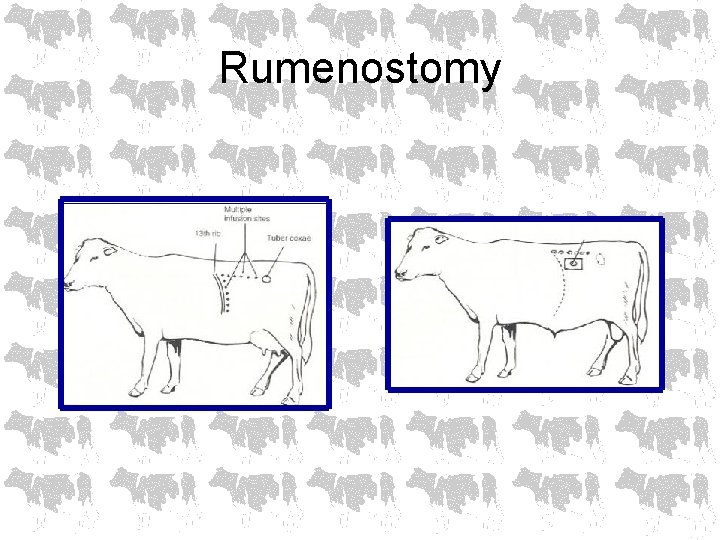
Rumenostomy
Client education • • Slow adaptation to grain Limit legume grazing Poloxalene in feed, molasses, salt or block Maintain sufficient long stem hay (fiber) in ration to stimulate good rumen motility
Rumenitis, rumen parakeratosis, chronic rumen acidosis • Long-term ingestion of high grain, low roughage diet • Poor appetite • Poor weight gain • Chronic laminitis
Rumenitis, rumen parakeratosis, chronic rumen acidosis • Clinical findings – Hypomotile rumen – Elevated liver enzymes – Rumen protozoa, gram + bacteria
Rumenitis, rumen parakeratosis, chronic rumen acidosis • Chronic exposure to high grain diet • Low rumen p. H (5. 0 -5. 5) • Increased propionic & butyric acid which stimulates proliferation of rumen papillae epithelium and even parakeratosis • Fine particle size, less cud chewing, less saliva buffering rumen contents • Damage to rumen leads to liver abscesses
Rumenitis, rumen parakeratosis, chronic rumen acidosis • Treatment includes increasing proportion of long stem hay in the diet
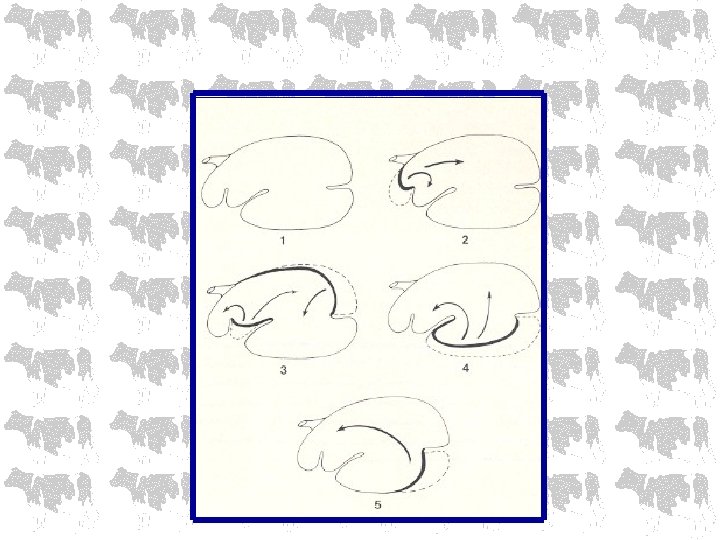
Vagus indigestion syndrome • Motor disturbances which impair passage of ingesta from the reticulorumen and/or abomasum into the lower GI tract
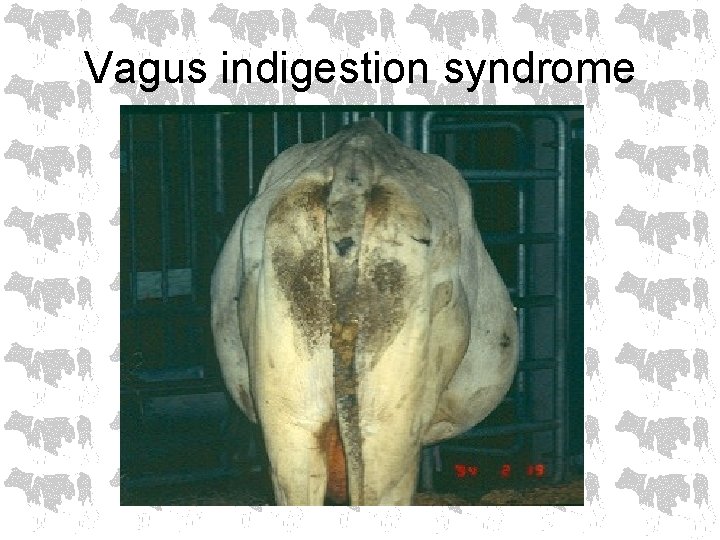
Vagus indigestion syndrome • • • “Vague” signs Slow loss of production Slow weight loss Poor appetite Scant, pasty feces Abdominal enlargement - “papple” shape • Rumen hyper motility, bradycardia
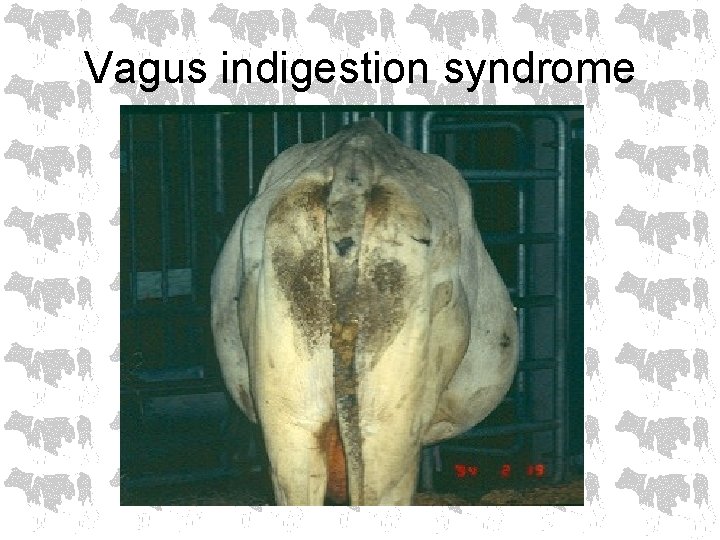
Vagus indigestion syndrome
Vagus indigestion syndrome • Classification: – Lesions anterior to cardia – Lesions at the reticulum – Lesions distal to the reticulum
Vagus indigestion syndrome • Treatment involves correction of underlying problem • Lymphosarcoma hopeless • Rumen lavage • Rumenotomy to remove contents & ‘shrink’ rumen or to treat reticular abscesses
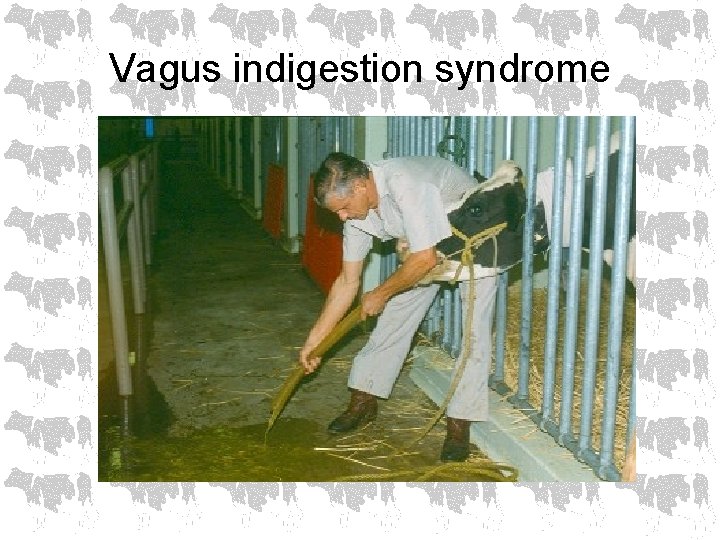
Vagus indigestion syndrome
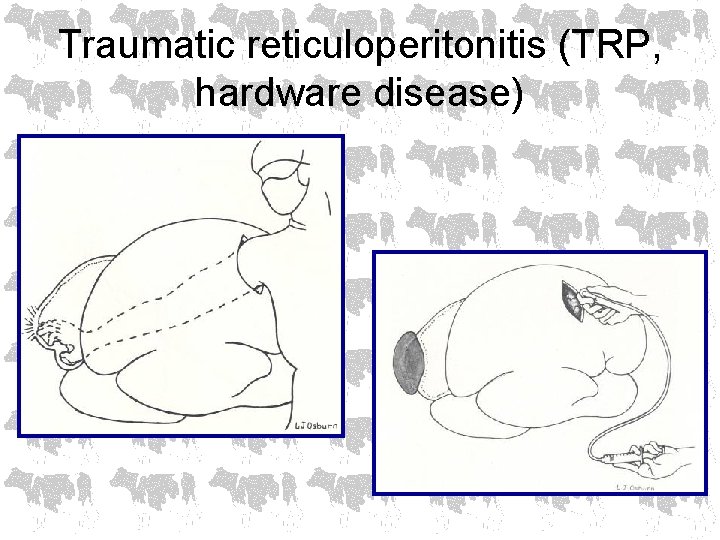
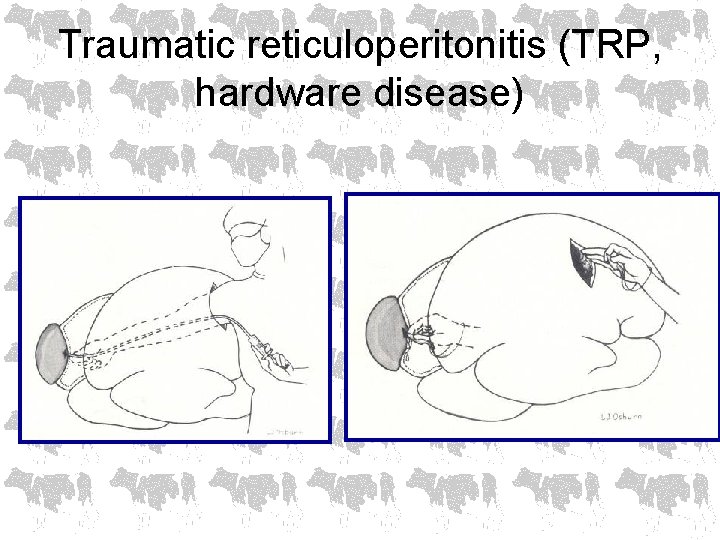
Traumatic reticuloperitonitis (TRP, hardware disease) • Sudden decrease in appetite & milk production • Anterior abdominal pain • Kyphosis • Low grade fever (103°) • Mild leukocytosis with neutrophilia • Hyperfibrinogenemia
Traumatic reticuloperitonitis (TRP, hardware disease) • Diagnostics – History – Clinical findings – Paracentesis – Reticular radiography – ultrasound
Traumatic reticuloperitonitis (TRP, hardware disease) • Medical treatment – Antibiotics – Magnet • Surgical treatment – Rumenotomy to approach reticulum
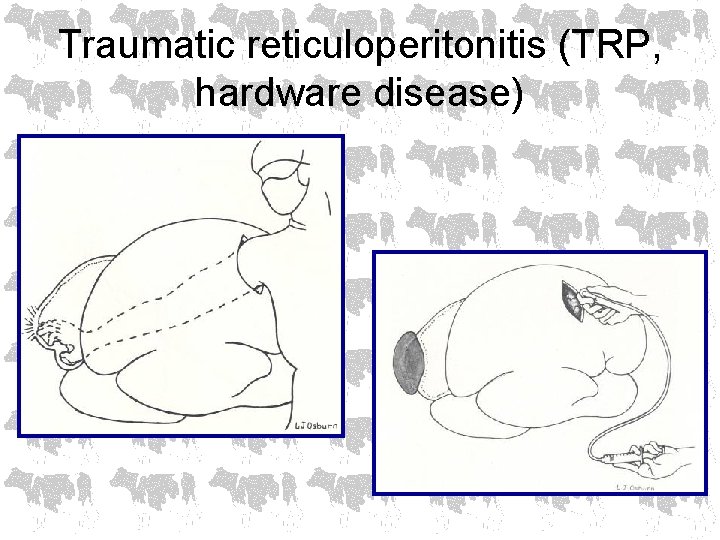
Traumatic reticuloperitonitis (TRP, hardware disease)
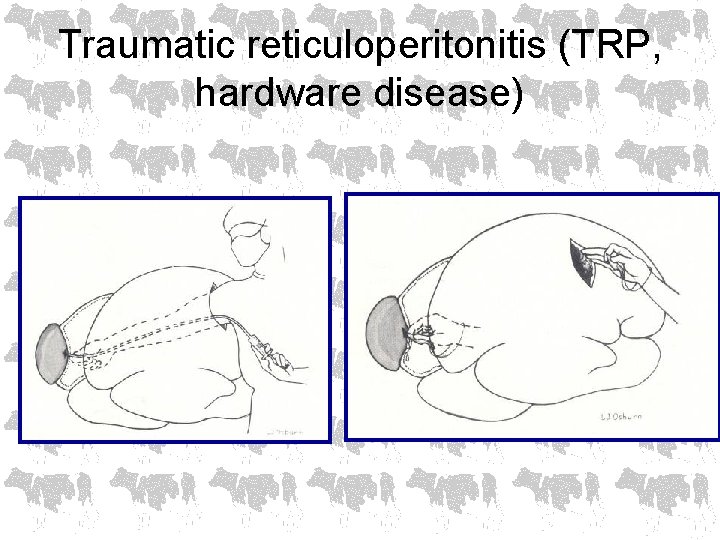
Traumatic reticuloperitonitis (TRP, hardware disease)
Abomasal ulcers • Occur in all ages of cattle • Associated with stress & high concentrate diets and lymphosarcoma in older animals • Four categories – Non-perforating with severe blood loss* – Perforating with localized peritonitis – Perforating with diffuse peritonitis* *life threatening
Abomasal ulcers • Diagnostics – Fecal occult blood – Abdominocentesis – WBC – leukocytosis with neutrophilia, high fibrinogen – Serology for BLV
Abomasal ulcers • Calves – Usually see perforation with peritonitis – May be associated with copper deficiency • Adults – 1/3 significant hemorrhage – 1/3 perforating with localized peritonitis – 1/3 perforating with diffuse peritonitis
Abomasal ulcers • Treatment – Dietary changes – Decrease stress – Avoid steroid & NSAID use – Treat concurrent problems – Blood transfusions – Antibiotics – GI protectants – H 2 antagonists
Clinical case • History: – Yearling BFM show heifer – History of mild abdominal pain – Mild bloat – Off feed – Change in feed in last week
• Clinical findings: – T – 103° – Leukocytosis, neutrophilia – Increased fibrinogen – Abdominocentesis • Protein > 3. 5 • WBC > 10, 000 • Neutrophilic inflammation
• Treatment: – Antibiotics – Decrease stress – Dietary change – hay, ryegrass, no grain – Rumen transfaunation – Avoid NSAIDS & steroids
Abomasal impaction • Causes: – Poor quality roughage for overwintering beef cows – Calves fed poor quality milk replacers – Animals on low fiber diets – Abomasal volvulus – Lymphosarcoma
Abomasal impaction • Clinical signs: – Takes weeks to develop – Decreased appetite – Firm, dry feces – Rumen enlargement, stasis – Poor BCS – Abomasal rupture may occur
Abomasal impaction • Differentials – Hydrops – Chronic peritonitis – Vagus indigestion – Omasal impaction
Abomasal impaction • Poor quality roughage is poorly digested so fibrous material passes to the abomasum creating accumulation of fibrous material in the abomasum which can not pass through • May develop post abomasal volvulus due to vagus nerve dysfunction
Abomasal impaction • • • Prognosis poor if advanced (slaughter) Fluid therapy*, laxatives, metaclopramide to early cases Terminate pregnancy Rumenotomy, backflush abomasal contents into rumen Place NG tube directly into abomasum for post-op medication *usually don’t develop metabolic alkalosis & hypochloremia
Abomasal emptying defect (AED) • • Suffolk sheep Anorexia, weight loss, abdominal enlargement Abomasum is enlarged and palpable DDx: – – – – Malnutrition Parasitism Dental attrition Johne’s Caseous lymphadenitis Neoplasia Chronic pneumonia
Abomasal emptying defect (AED) • Diagnostics – Increased rumen chloride (normal = 8 -15 m. Eq/L) – Ultrasound abomasum – normal diameter is 23”, with AED may see abomasal diameter of 6 -10” • Pathophysiology remains unknown
Abomasal emptying defect (AED) • Treatment: – Surgery – rumenotomy & backflush rumen – Metaclopramide – facilitates abomasal emptying