PEDIATRIC CHEST PAIN EMS REGION 8 JANUARY 2017















- Slides: 81
PEDIATRIC CHEST PAIN EMS REGION 8 JANUARY 2017 CE

OBJECTIVES • Discuss the most common causes of chest pain in pediatric patients • Differentiate cardiac from non cardiac chest pain • Discuss evaluation of the pediatric patient who has chest pain

INTRODUCTION 1. SME video of the month: Dr. Mark Cichon 2. Review of Pediatric Cardiac SOPs 3. Scenarios
DR. CICHON VIDEO • January 2017 CE final
PEDIATRIC CHEST PAIN • One of the most common reasons for a child to visit a pediatrician or the Emergency Department • Various disorders may cause chest pain in children and adolescents – Cardiac – Gastrointestinal – Respiratory – Psychogenic – Idiopathic
PEDIATRIC CHEST PAIN • Pediatric chest pain is classified into cardiac or non cardiac chest pain • Most episodes of chest pain in children have non cardiac causes • Good history taking and physical exam are important • Be suspicious if child is colicky, has palpitations, light headedness, syncope, seizure or exertional symptoms
PEDIATRIC CHEST PAIN • Age is a consideration when assessing chest pain in a child • Young children may interpret a wide range of symptoms or chest sensations as pain • Adolescents are more likely to have musculoskeletal or psychogenic causes
NON-CARDIAC CHEST PAIN • Causes of non-cardiac chest pain – Musculoskeletal – Costochondritis – Tietze syndrome – Non-specific or idiopathic chest wall pain – Slipping rib syndrome – Trauma or muscle overuse – Xiphoid pain – Sickle cell vaso-occulsive crisis
NON-CARDIAC CHEST PAIN • Pulmonary or airway related causes – Asthma – Bronchitis – Pleuritis – Pneumonia – Pulmonary embolism – Pneumothorax – Acute chest syndrome
NON-CARDIAC CHEST PAIN • Gastrointestinal causes – Gastroesophageal reflux – Esophageal spasm – Peptic ulcer disease – Drug induced esophagitis/gastritis – Cholecystitis
NON-CARDIAC CHEST PAIN • Miscellaneous causes – Panic disorder – Hyperventilation
MUSCULOSKELETAL PAIN • AKA chest wall pain • The most common cause of chest pain in children and adolescents • The prevalence is between 15% and 31%
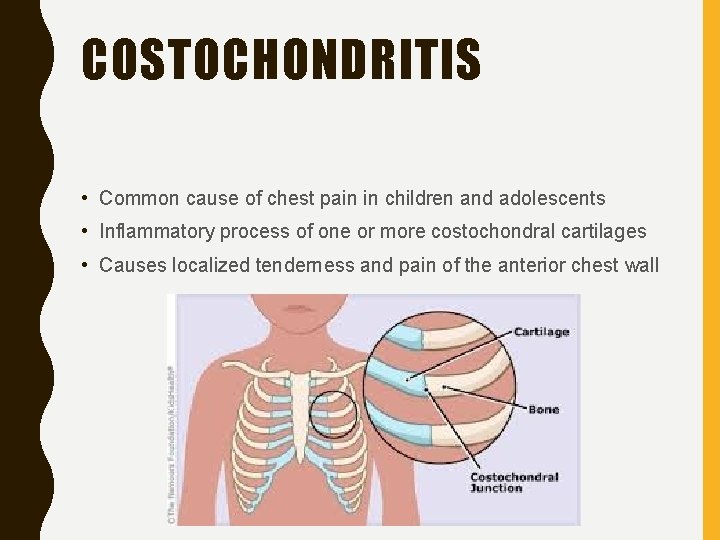
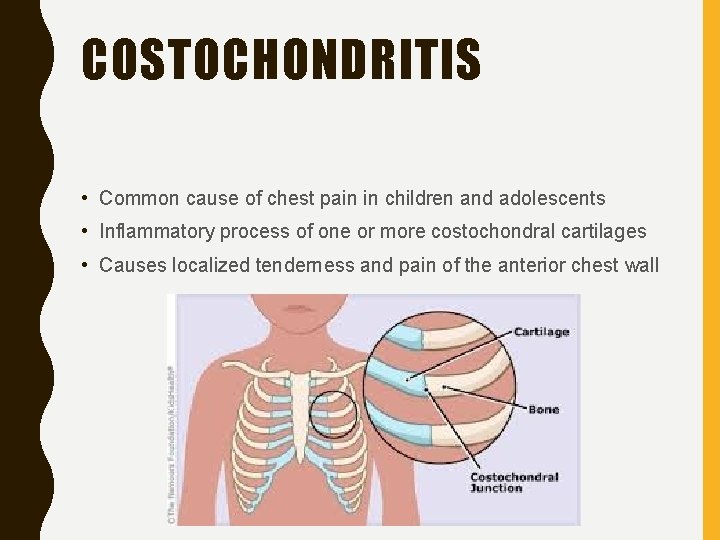
COSTOCHONDRITIS • Common cause of chest pain in children and adolescents • Inflammatory process of one or more costochondral cartilages • Causes localized tenderness and pain of the anterior chest wall
COSTOCHONDRITIS • Unilateral, sharp, stabbing pain • Occurs along the upper two or more contiguous costochondral joints • Exacerbated by deep breathing • Pain lasts for a few seconds to a few minutes • Chest wall tenderness can be reproduced by palpation over the affected area
COSTOCHONDRITIS • Most cases are idiopathic • Other causes – Costochondral irritation due to trauma – Aggressive exercise resulting in strain of the costochondral cartilage – Prior upper respiratory tract infection with cough causing stretching and strain to the cartilage, resulting in local irritation and pain • Cartilage involved is either inflamed or fractured
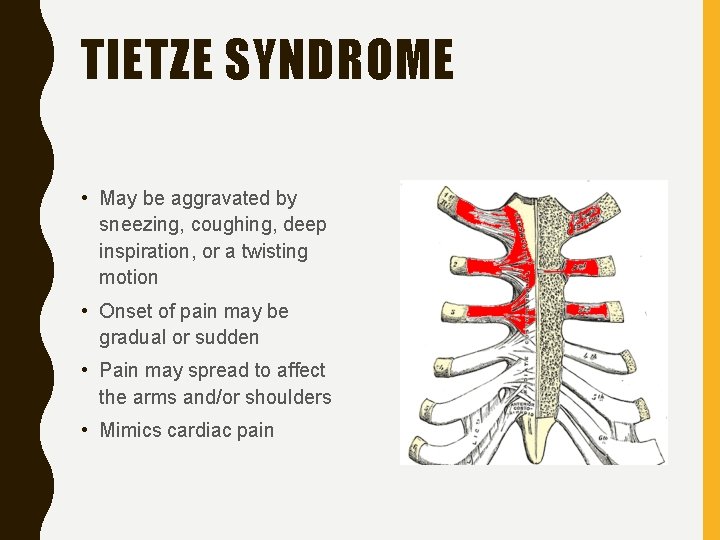
TIETZE SYNDROME • First described in 1921 by German surgeon Alexander Tietze • Rare inflammatory disorder • Specific inflammation of the first two or three costochondral articulations
TIETZE SYNDROME • Chest pain and swelling of the cartilage of one or more of the upper ribs • Specifically where the ribs attach to the sternum • Usually characterized by involvement of a single joint along with signs of inflammation such as warmth, swelling, tenderness
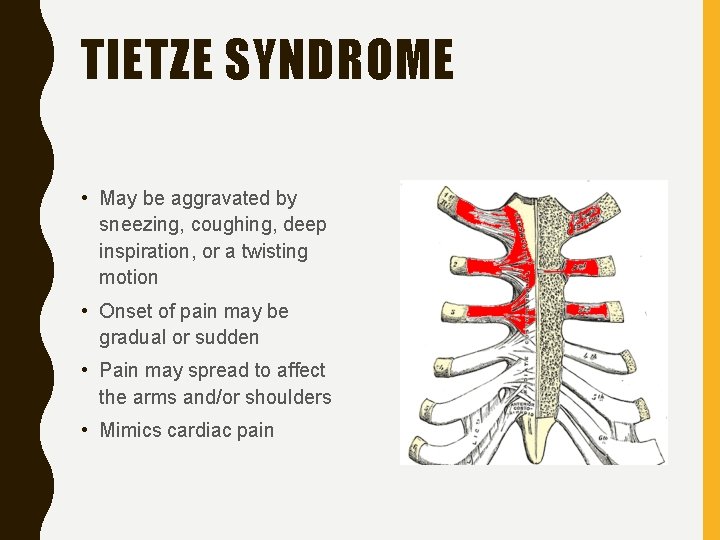
TIETZE SYNDROME • May be aggravated by sneezing, coughing, deep inspiration, or a twisting motion • Onset of pain may be gradual or sudden • Pain may spread to affect the arms and/or shoulders • Mimics cardiac pain
SLIPPING-RIB SYNDROME • Also known as lower rib pain syndrome • Occurs infrequently in children • Characterized by intense pain in the lower chest or upper abdominal area • Caused by trauma or dislocation of the 8 th, 9 th and 10 th ribs • Impinges on the intercostal nerves

Slipping Rib Syndrome
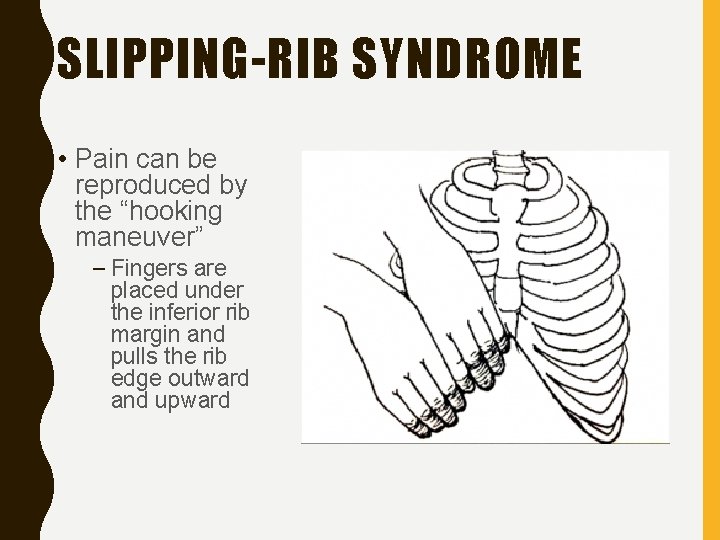
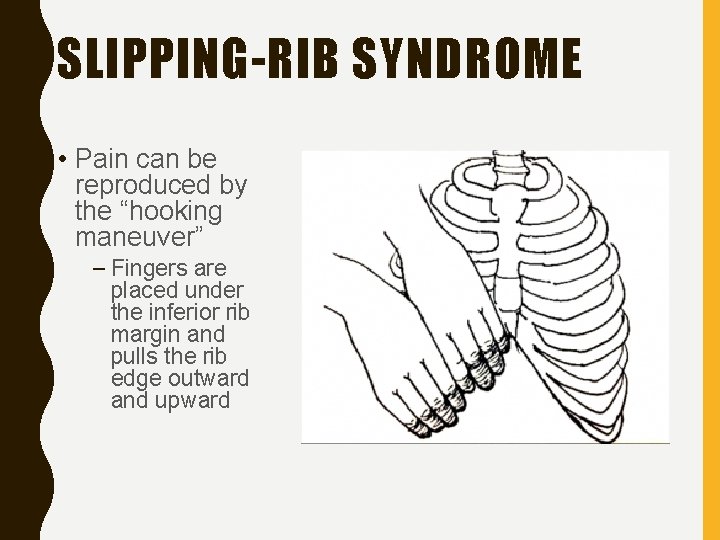
SLIPPING-RIB SYNDROME • Pain can be reproduced by the “hooking maneuver” – Fingers are placed under the inferior rib margin and pulls the rib edge outward and upward
PRECORDIAL CATCH SYNDROME • AKA Texidor’s twinge • Affects children more than adults • Most commonly affects children aged 6 -12 years • Characterized by sudden, sharp and localized chest pains lasting a few seconds to a few minutes along the lower left sternal border • Pain usually occurs while at rest • Most common sites for pain: left sternal border, right anterior chest, flanks
PRECORDIAL CATCH SYNDROME • Cause is unknown, but not cardiac or pericardial in nature • Has been associated with poor posture and may be caused by a pinched nerve • Exacerbated with inspiration, often leading to shallow breathing in an effort to alleviate pain
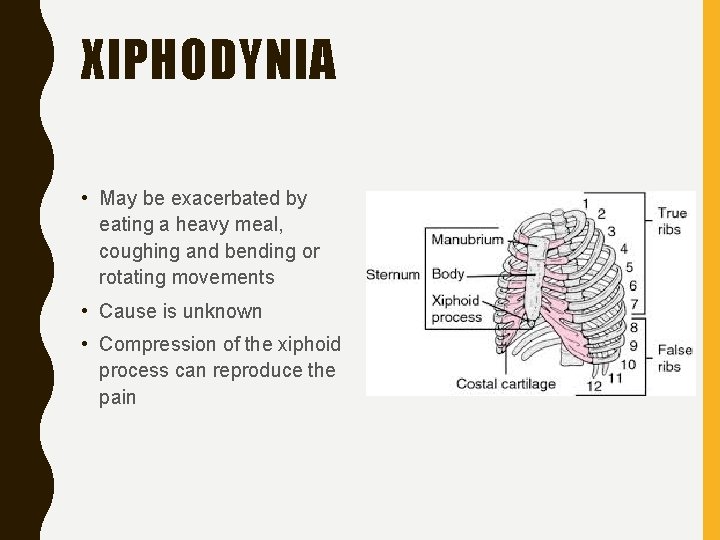
XIPHODYNIA • AKA hypersensitive xiphoid syndrome • Musculoskeletal disorder capable of producing symptoms that mimic several common abdominal and thoracic diseases • Pain or discomfort is localized over xiphoid process of the sternum
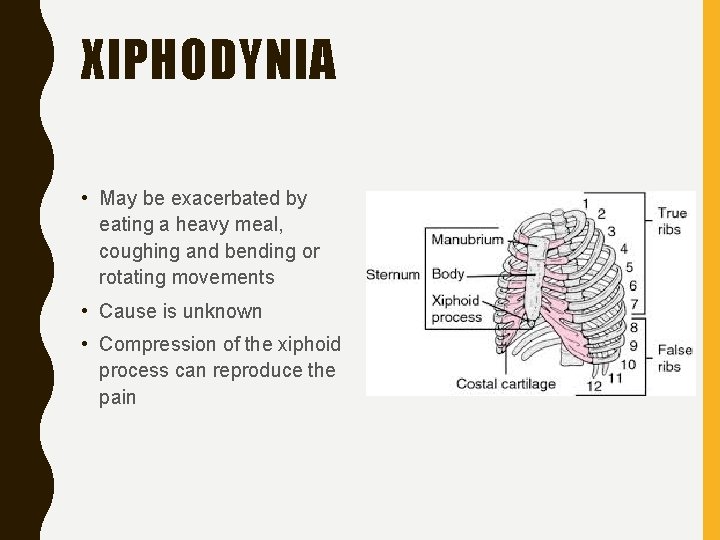
XIPHODYNIA • May be exacerbated by eating a heavy meal, coughing and bending or rotating movements • Cause is unknown • Compression of the xiphoid process can reproduce the pain
XIPHODYNIA • Symptoms include: § Cardiac chest pain § Epigastric pain § Nausea vomiting, diarrhea § Pain radiating into the back, neck, shoulders, arms and chest wall • Treatment is analgesics, topical heat and cold or an injection of local anesthetic and steroids
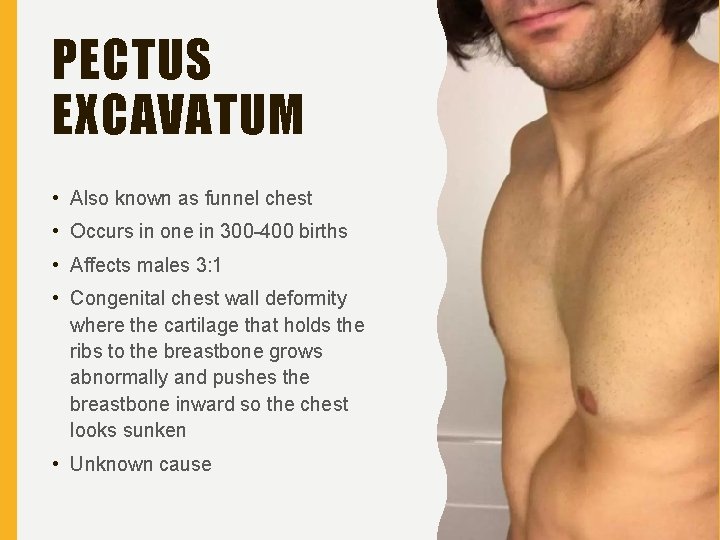
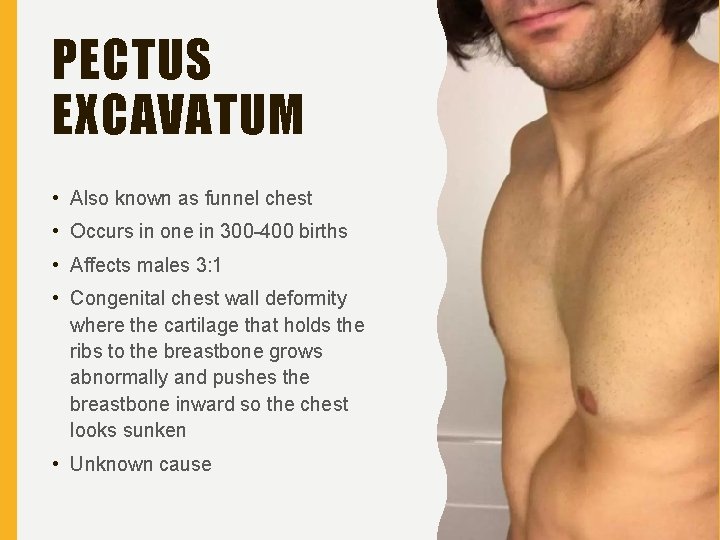
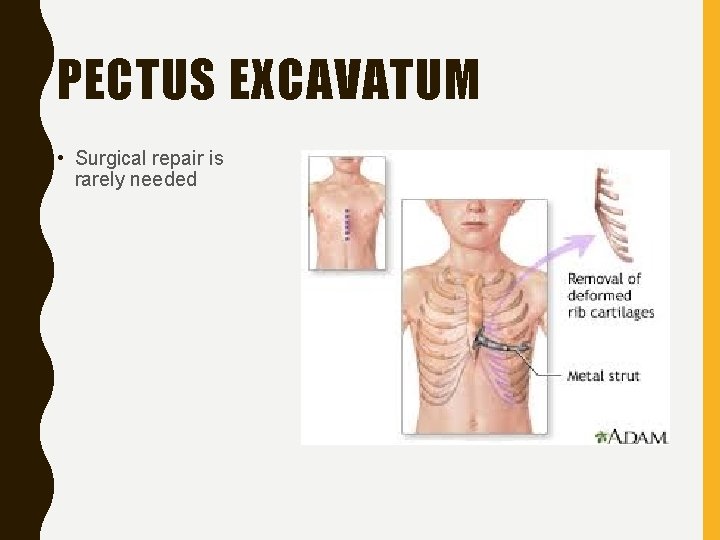
PECTUS EXCAVATUM • Also known as funnel chest • Occurs in one in 300 -400 births • Affects males 3: 1 • Congenital chest wall deformity where the cartilage that holds the ribs to the breastbone grows abnormally and pushes the breastbone inward so the chest looks sunken • Unknown cause

PECTUS EXCAVATUM • Appearance varies widely from mild to severe with significant asymmetry between sides • Maybe noticed at birth with progressive worsening as the child grows • Chest pain is a frequent symptom • Moderate-to-severe cases: • Shortness of breath • Chest pain • Exercise intolerance
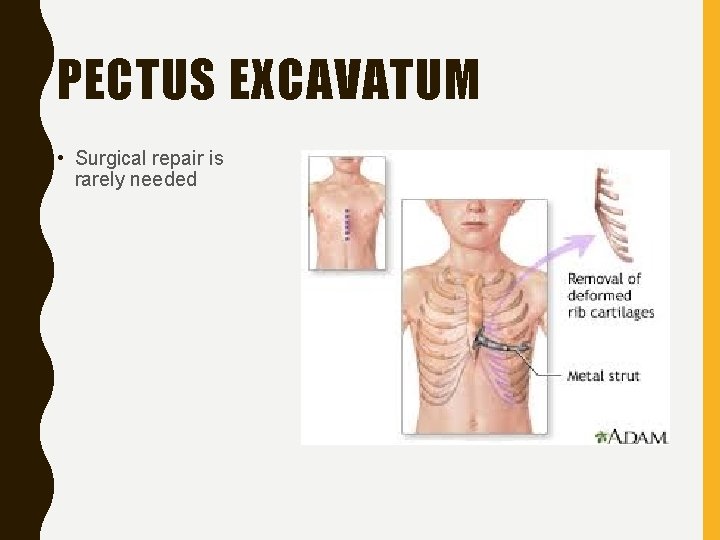
PECTUS EXCAVATUM • Surgical repair is rarely needed
SCENARIO • You are called to the local pre-school for the 4 -year-old complaining of pain. When asked where it hurts, she points to her right chest along the rib cage. Teacher informs you the girl just returned to school after being out for several days with viral respiratory illness.
SCENARIO • S- when asked to take a deep breath, she cries and says it hurts • A- none known • M- ibuprofen for fever • P- Viral respiratory illness • L- breakfast • E- Playing with other kids on playground and complained of pain
SCENARIO • Vital signs: – Pulse 98 – BP 100/60 – RR 24, shallow – Sp. O 2 95% on RA • Skin warm, flushed, dry • Breath sounds diminished on right side • Treatment? • Possible causes
PULMONARY CAUSES • Prevalence of chest pain due to respiratory causes is about 211% • Pneumonia and asthma are common causes of acute pediatric chest pain • Exercise induced asthma frequently causes chest pain in the pediatric population • Any respiratory condition with chronic cough may also cause chest pain due to muscle strain
PLEURODYNIA • Acute illness with marked paroxysmal spasms of the muscles of the chest and abdomen • Acute onset of pain • Pain is severe, intense and excruciating, lasting seconds to a minute • Severe attacks can cause difficulty in breathing • Thoracic pain occurs over lower ribs and is unilateral

PLEURODYNIA • Pain can also occur over front, back and substernal area • Between attacks, child may have constant dull pleuritic pain • Persists for about 5 days • Associated with symptoms related to a viral infection (URI)
EXERCISE-INDUCED ASTHMA • Most common pulmonary cause of chest pain • AKA exercise induced bronchoconstriction • Frequently results in chest pain • Caused by loss of heat and/or water from lungs during exercise
EXERCISE-INDUCED ASTHMA • Dryness of the air, rather than the temperature, is the most likely trigger • Quickly breathing dry air dehydrates the bronchial tubes, causing them to narrow and restrict airflow

EXERCISE-INDUCED ASTHMA • 90% of people with asthma have EIB but not everyone with EIB has asthma • Common symptoms include: § Shortness of breath or wheezing § Decreased endurance § Chest tightness or pain § Cough § Sore throat

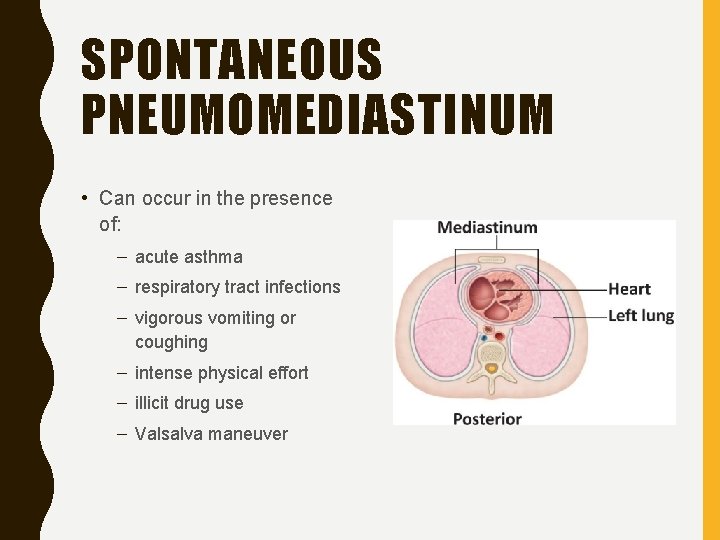
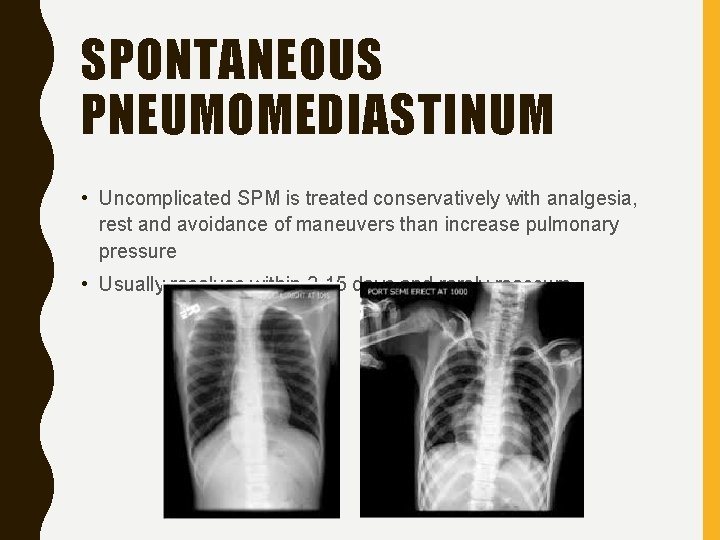
SPONTANEOUS PNEUMOMEDIASTINUM • Presence of gas in the mediastinum in the absence of trauma • Caused by alveolar rupture and dissection of air into the mediastinum
SPONTANEOUS PNEUMOMEDIASTINUM • Initial peak in incidence during late infancy and early childhood due to high prevalence of respiratory infections in this age group • Thought to be caused by increased pressure within obstructed airways • Second peak during adolescence: – Tall, thin males
SPONTANEOUS PNEUMOMEDIASTINUM • Approximately 25 -90% of children with SPM present with chest pain • Pain is retrosternal and pleuritic in nature • Presence of subcutaneous emphysema • Pain increases during deep inspiration and dyspnea • Pain may radiate to neck, shoulders, and arms
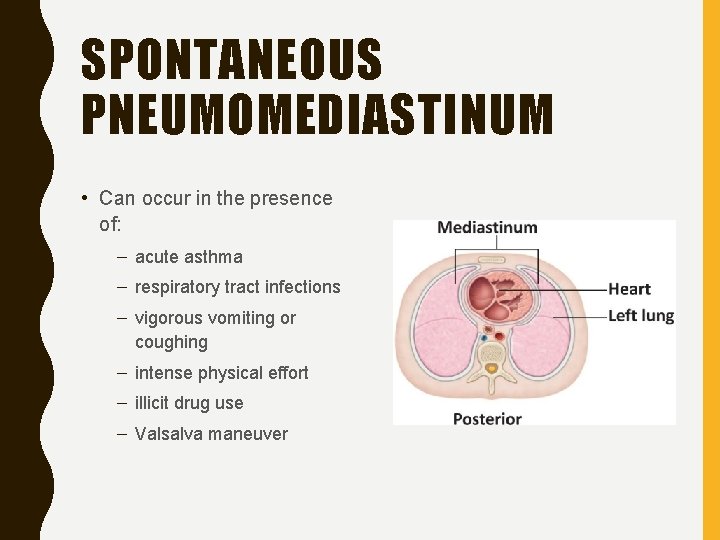
SPONTANEOUS PNEUMOMEDIASTINUM • Can occur in the presence of: – acute asthma – respiratory tract infections – vigorous vomiting or coughing – intense physical effort – illicit drug use – Valsalva maneuver
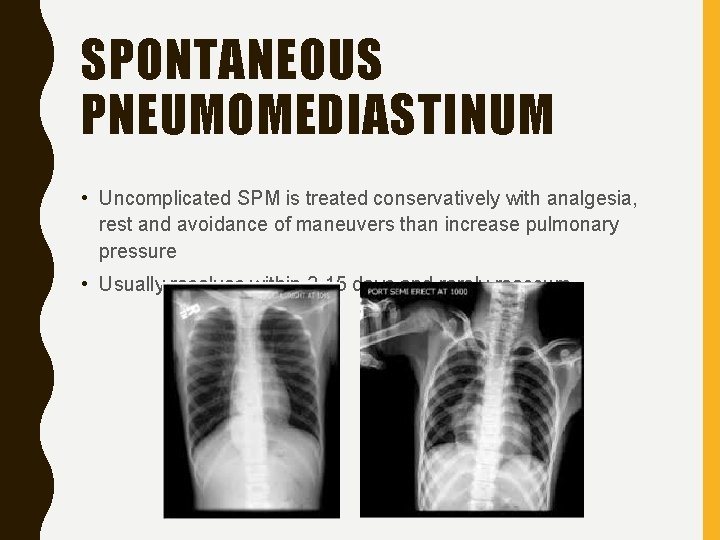
SPONTANEOUS PNEUMOMEDIASTINUM • Uncomplicated SPM is treated conservatively with analgesia, rest and avoidance of maneuvers than increase pulmonary pressure • Usually resolves within 2 -15 days and rarely reoccurs
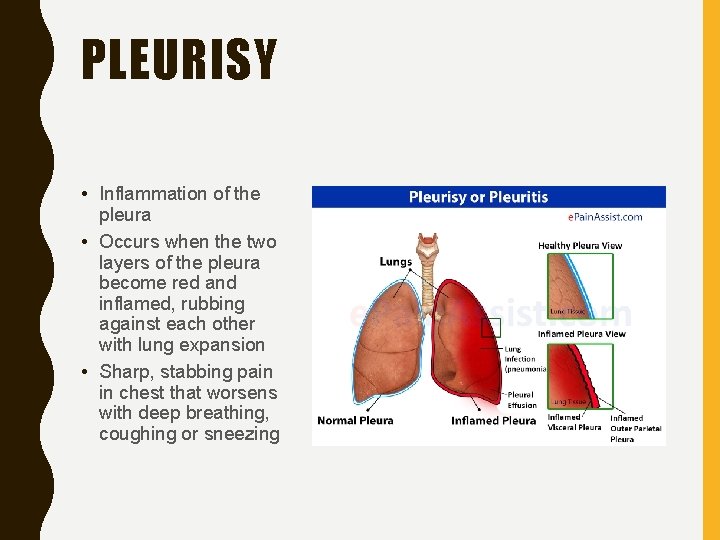
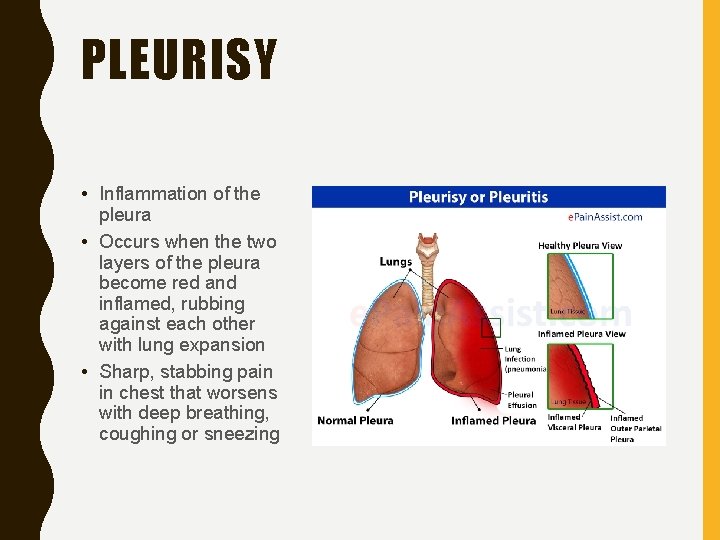
PLEURISY • Inflammation of the pleura • Occurs when the two layers of the pleura become red and inflamed, rubbing against each other with lung expansion • Sharp, stabbing pain in chest that worsens with deep breathing, coughing or sneezing
PLEURISY • Symptoms usually occur on one side of the chest • May extend to shoulder and belly • Eases when you hold your breath or press on the painful area • Treatment depends on the cause
SCENARIO • Called for the 5 -year-old male in acute respiratory distress. Upon arrival parents rush you into bedroom to find the patient unresponsive and apneic. • Your crew begins resuscitation while you gather additional information.
SCENARIO • • S- Difficulty breathing then unresponsive A- Penicillin M- Tylenol with Codeine for pain P- Cerebral palsy. Surgery 2 weeks ago for tendon lengthening. Bilateral casts • L- Breakfast • E- Patient has been home from hospital for 4 days with nursing and physical therapy coming twice daily. Pain was sudden onset upon waking up this morning when patient’s position was changed.
SCENARIO • Vital signs: – Pulse: Absent – Respirations: Absent – BP: N/A – Oxygen saturation at 70% • What are your next steps? • Possible causes?
PULMONARY EMBOLISM • Rare in pediatric population and may not be considered as cause • Risk factors – Obesity – Immobility – Central venous catheters – Malignancy – Congenital heart disease – Lupus – Recent surgery or trauma

PULMONARY EMBOLISM • Non-specific symptoms – Tachypnea – Tachycardia – Fever – Pleuritic chest pain – Shortness of breath
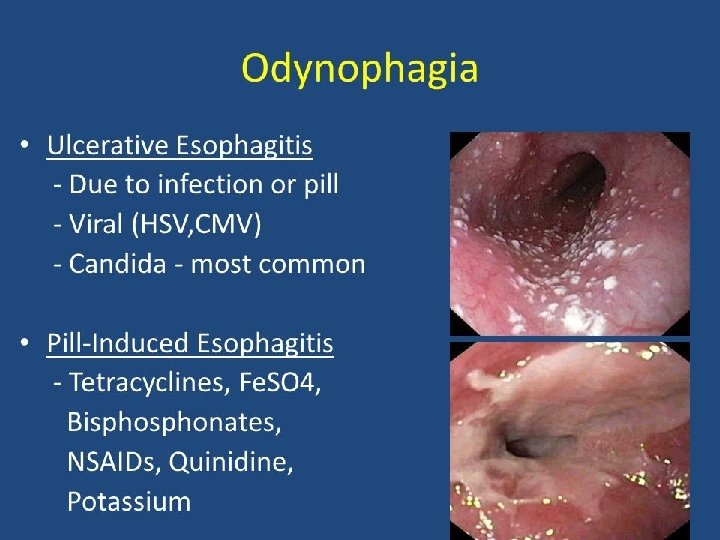
GI CAUSES OF CHEST PAIN • Prevalence of chest pain due to gastrointestinal causes is about 8% • Common causes: – Gastroesophageal reflux – Peptic ulcer disease – Esophageal spasm – Cholecystitis – Drug-induced esophagitis

GI CAUSES OF CHEST PAIN • Symptoms – Pain often recurrent or epigastric but may also be mid sternal – Typically burning or sharp in nature – May be exacerbated with eating or posture – Can be associated with heartburn, water brash or dysphagia

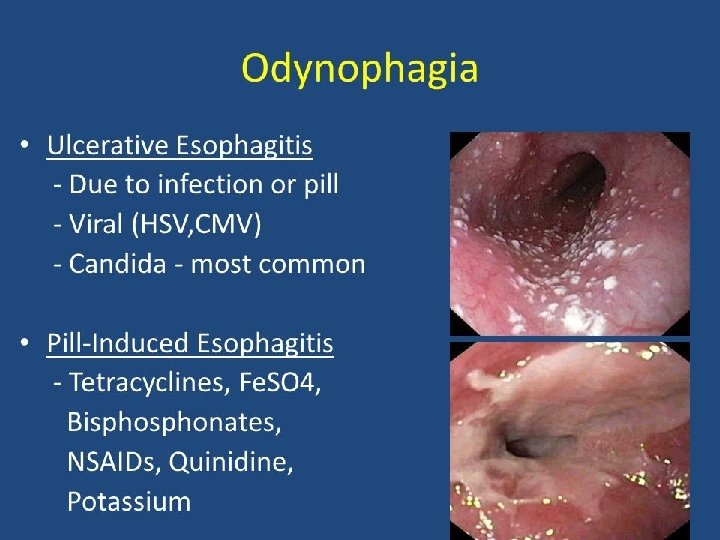
DRUG-INDUCED ESOPHAGITIS • Occurs in pediatric patients treated with tablets or capsules • Esophagitis most frequent esophageal disorder in children • 90% occurs after use of NSAIDS or antibiotics • Symptoms include chest pain, dysphagia and retrosternal pain • Usually self-limiting
PSYCHOGENIC • Psychogenic chest pain in older children can result from anxiety or a conversion disorder triggered by recent stressors in personal or family life • Approximately 1/3 of adolescents complaining of chest pain had a history of stressful events either in family or at school
PSYCHOGENIC • Often recurrent with particular stressors • History of anxiety or panic disorders and/or stressful life events • May be associated with hyperventilation • This may accompanied by difficulty in breathing, dizziness, paresthesias and chest pain
PSYCHOGENIC • Hyperventilation due to anxiety or a panic disorder can cause chest pain • May be accompanied by difficulty in breathing, dizziness or paresthesia
CARDIAC CAUSES OF CHEST PAIN • Chest pain due to a cardiac condition is rare • Infectious or inflammatory – Pericarditis: inflammation of the sac surrounding the heart – Myocarditis: a viral infection of the heart – Endocarditis: infection of inner lining of the heart • Coronary artery and structural abnormalities • Dissection, or tearing, of the aorta
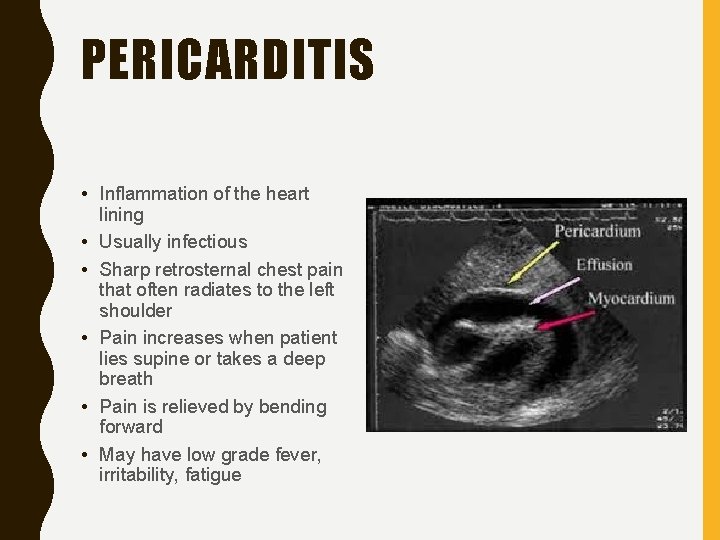
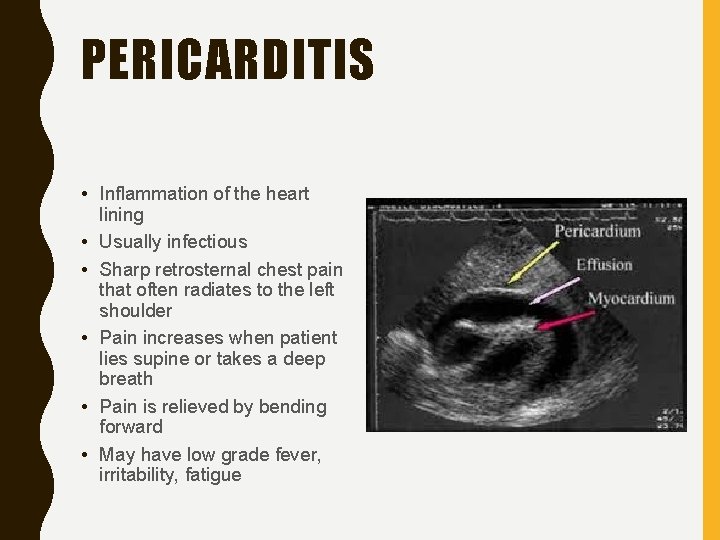
PERICARDITIS • Inflammation of the heart lining • Usually infectious • Sharp retrosternal chest pain that often radiates to the left shoulder • Pain increases when patient lies supine or takes a deep breath • Pain is relieved by bending forward • May have low grade fever, irritability, fatigue
ACUTE CHEST SYNDROME • Most common cause of sickle cell-related death • Second most common cause of hospitalizations in patients with sickle cell disease • Recurrent ACS events have been associated with chronic lung disease and early death
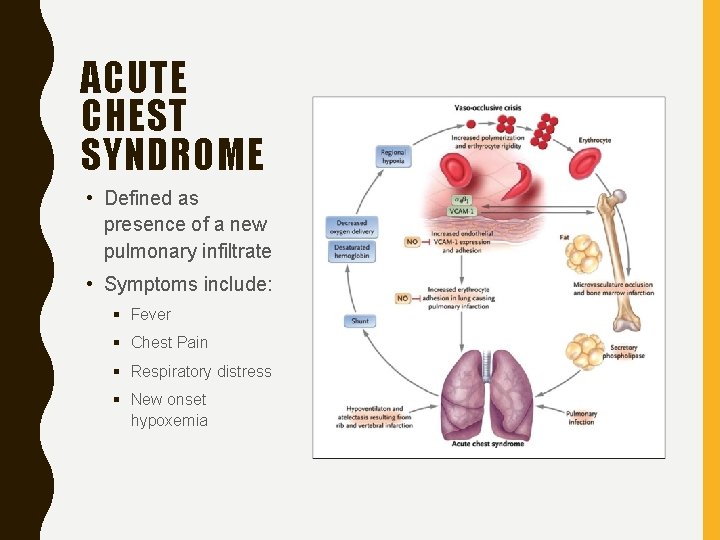
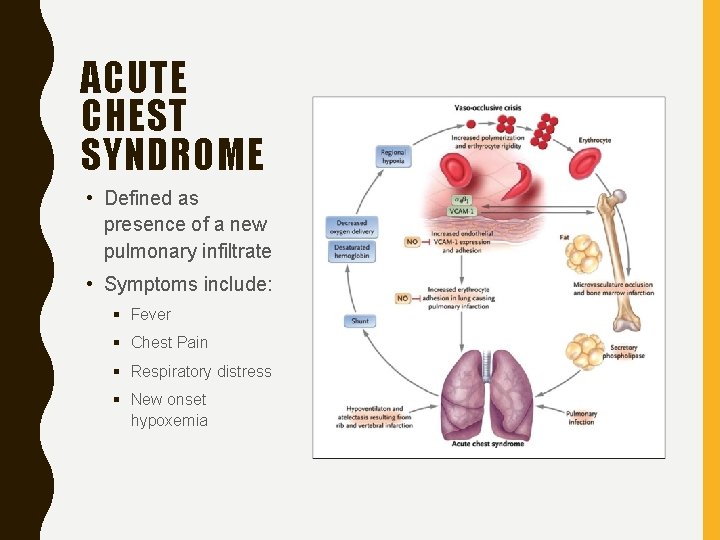
ACUTE CHEST SYNDROME • Defined as presence of a new pulmonary infiltrate • Symptoms include: § Fever § Chest Pain § Respiratory distress § New onset hypoxemia
ACUTE CHEST SYNDROME • Higher occurrence in winter months • Children more likely to have preceding febrile events • Peak incidence between ages of 2 and 4 years • Rarely seen in children < 2 years • Respiratory infections leading cause of ACS

MARFAN SYNDROME • Genetic connective tissue disorder • Affects 1 in 5, 000 • Male and female of all races and ethnic groups • 3 out of 4 people inherit it • Severity of condition varies • Features and related disorders can appear at any age


MARFAN SYNDROME • Additional signs – Heart problems especially those related to the aorta, mitral valve prolapse, and mitral regurgitation, heart murmur, arrhythmias – Chest pain when active – Sudden lung collapse – Eye problems including severe nearsightedness

MARFAN SYNDROME • Requires individualized treatment plan depending on structures affected and severity • Medications typically not used to treat • If aorta affected, beta blockers may be utilized to prevent or slow the enlargement • Goal to prevent aortic dissection or rupture
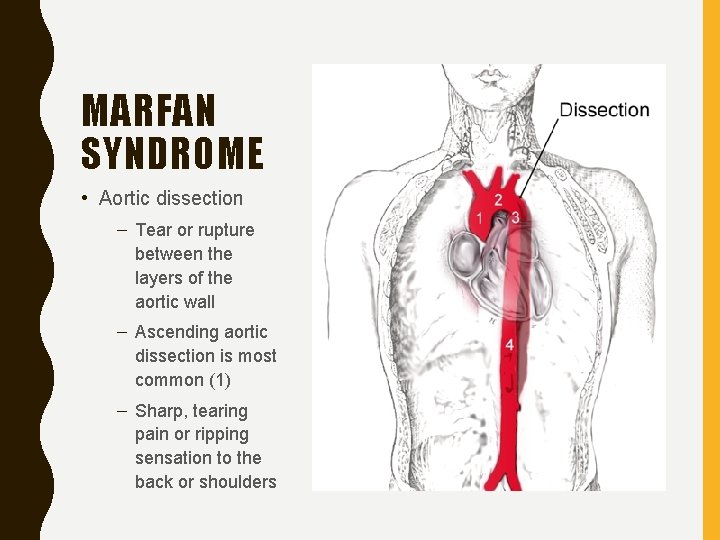
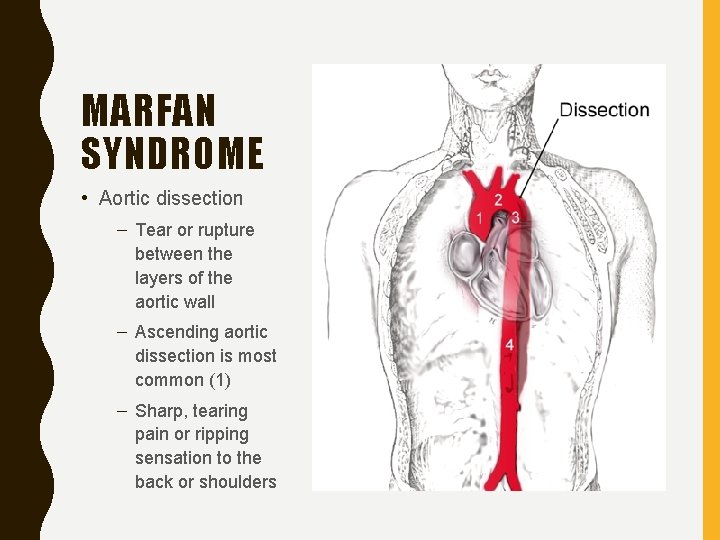
MARFAN SYNDROME • Aortic dissection – Tear or rupture between the layers of the aortic wall – Ascending aortic dissection is most common (1) – Sharp, tearing pain or ripping sensation to the back or shoulders
TACHARRHYTHMIAS • Supraventricular tachycardia • Wolff-Parkinson-White syndrome • Ventricular tachycardia • Symptoms may be mild or severe
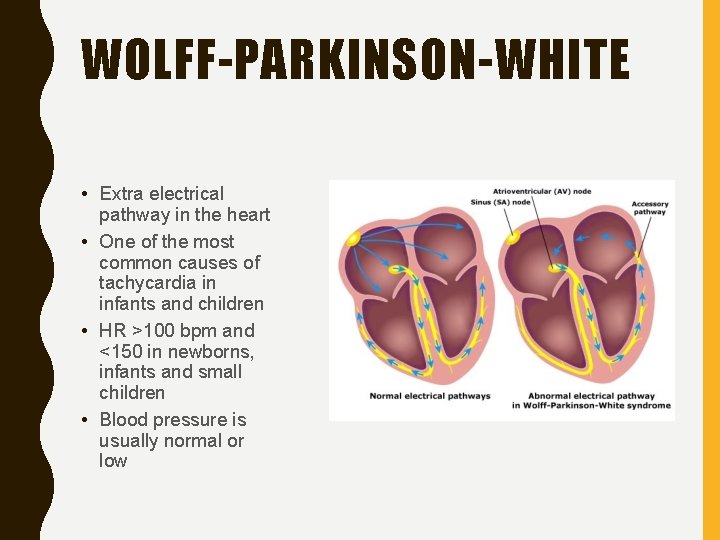
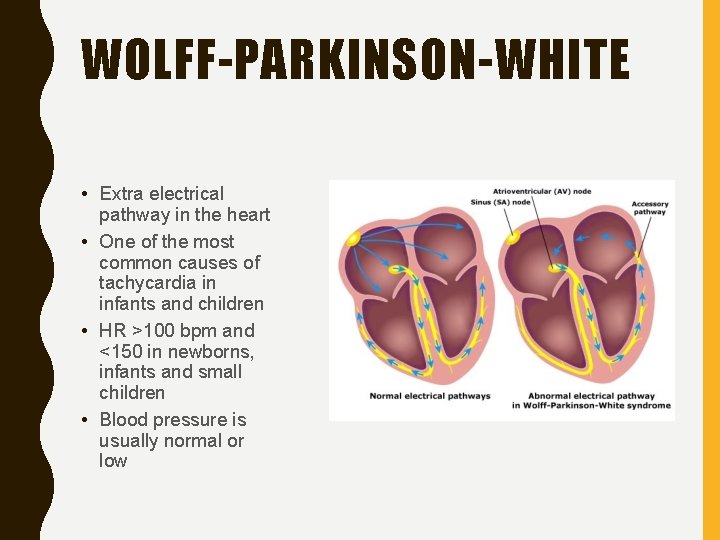
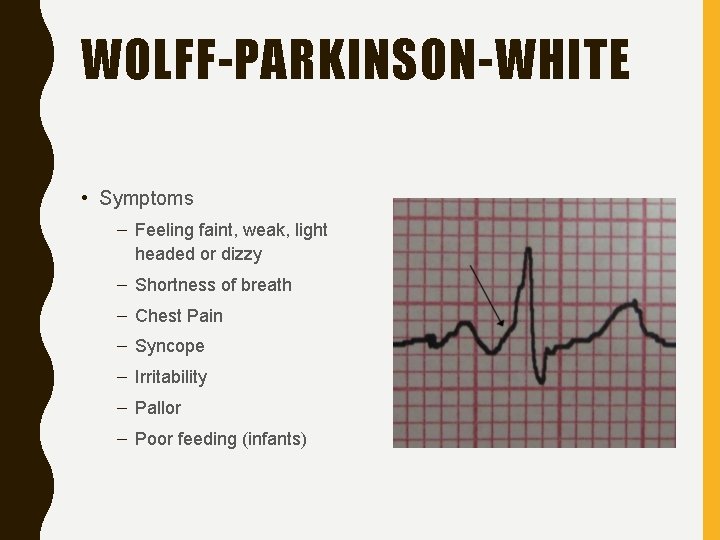
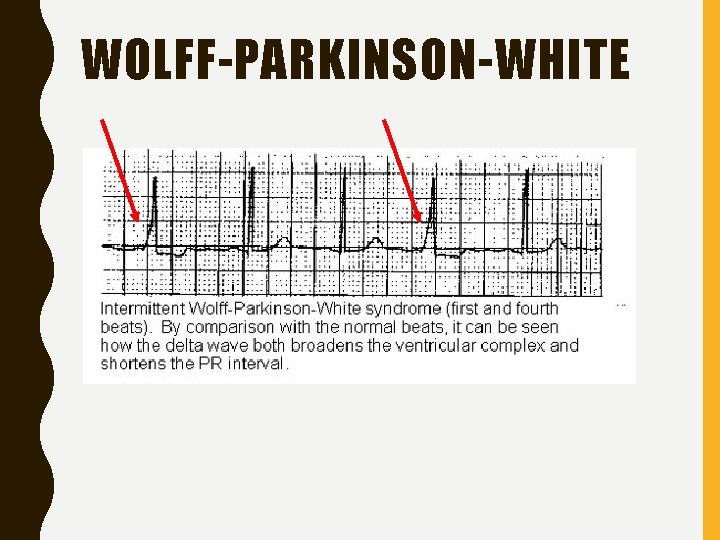
WOLFF-PARKINSON-WHITE • Extra electrical pathway in the heart • One of the most common causes of tachycardia in infants and children • HR >100 bpm and <150 in newborns, infants and small children • Blood pressure is usually normal or low
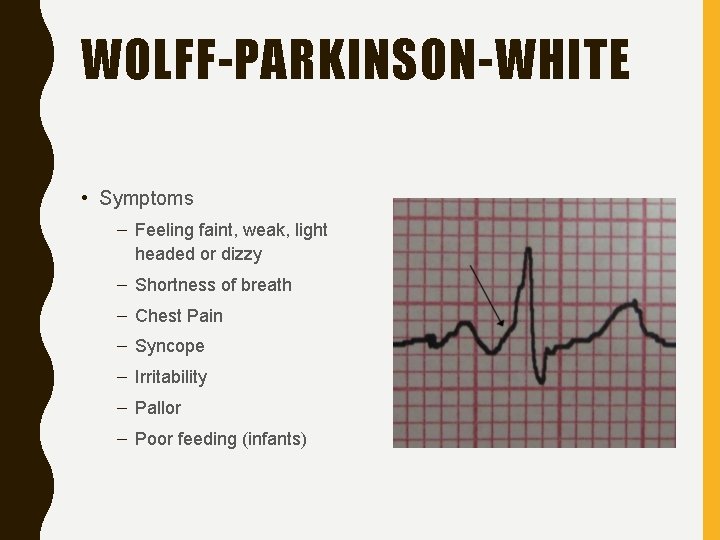
WOLFF-PARKINSON-WHITE • Symptoms – Feeling faint, weak, light headed or dizzy – Shortness of breath – Chest Pain – Syncope – Irritability – Pallor – Poor feeding (infants)
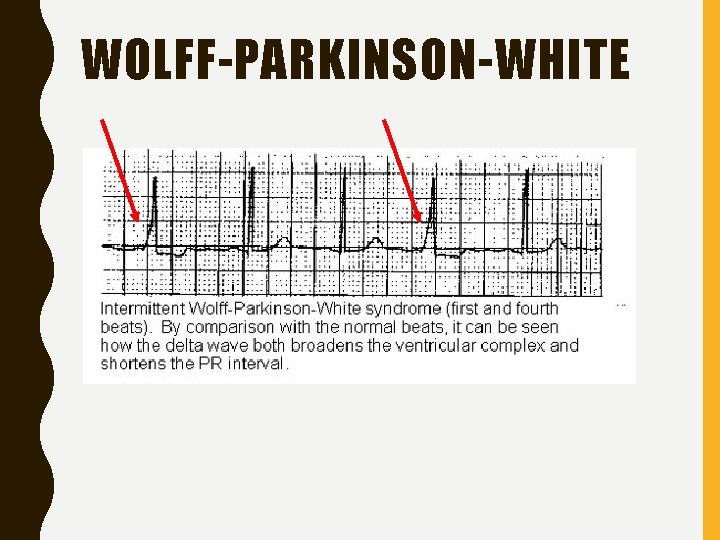
WOLFF-PARKINSON-WHITE
PULSE OXIMETRY SKILL OF THE MONTH
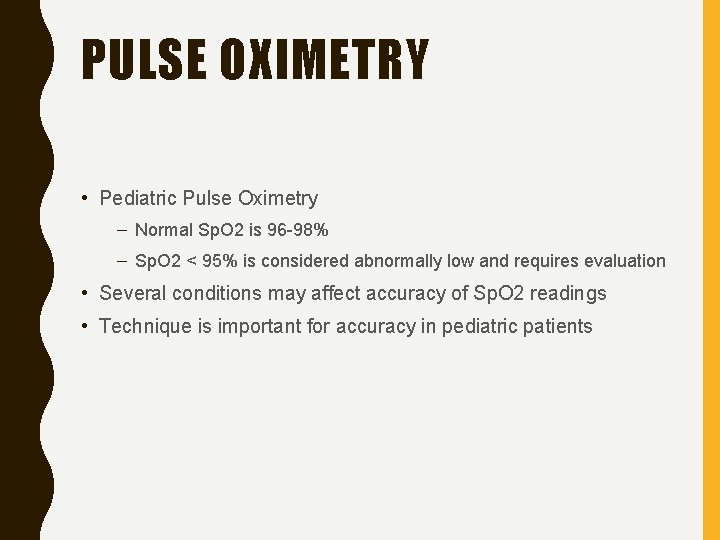
PULSE OXIMETRY • Pediatric Pulse Oximetry – Normal Sp. O 2 is 96 -98% – Sp. O 2 < 95% is considered abnormally low and requires evaluation • Several conditions may affect accuracy of Sp. O 2 readings • Technique is important for accuracy in pediatric patients
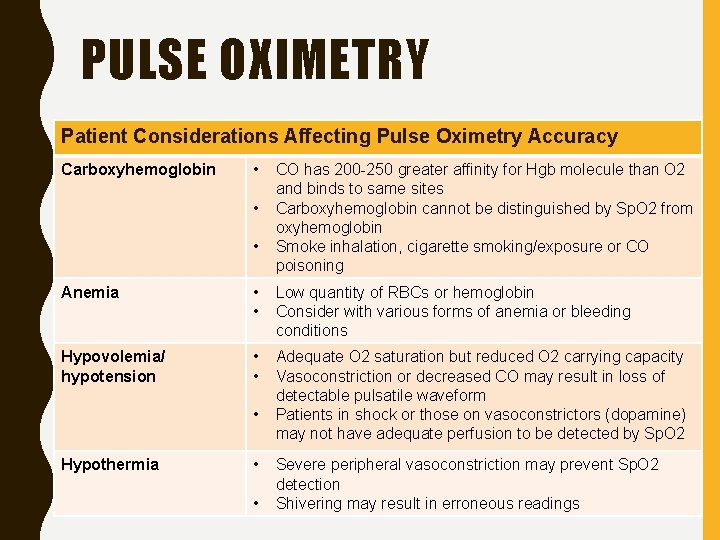
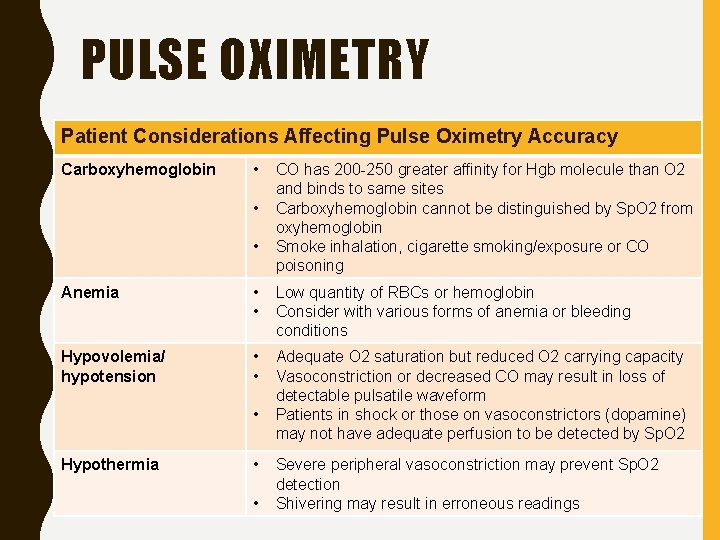
PULSE OXIMETRY Patient Considerations Affecting Pulse Oximetry Accuracy Carboxyhemoglobin • • • CO has 200 -250 greater affinity for Hgb molecule than O 2 and binds to same sites Carboxyhemoglobin cannot be distinguished by Sp. O 2 from oxyhemoglobin Smoke inhalation, cigarette smoking/exposure or CO poisoning Anemia • • Low quantity of RBCs or hemoglobin Consider with various forms of anemia or bleeding conditions Hypovolemia/ hypotension • • Adequate O 2 saturation but reduced O 2 carrying capacity Vasoconstriction or decreased CO may result in loss of detectable pulsatile waveform Patients in shock or those on vasoconstrictors (dopamine) may not have adequate perfusion to be detected by Sp. O 2 • Hypothermia • • Severe peripheral vasoconstriction may prevent Sp. O 2 detection Shivering may result in erroneous readings
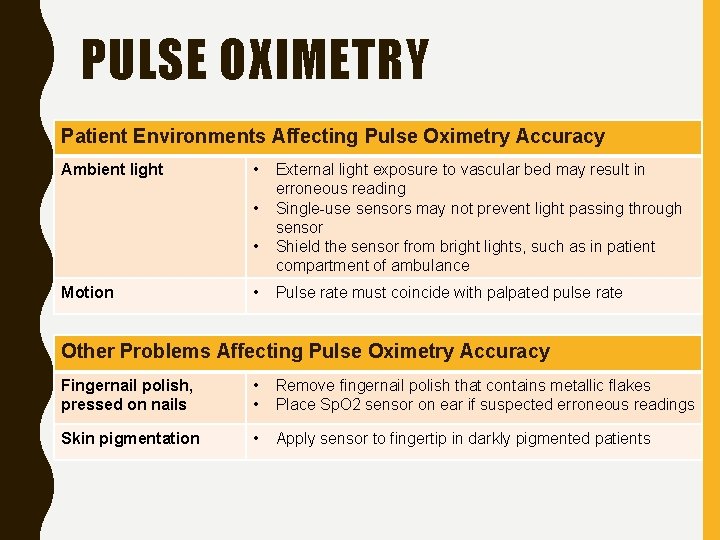
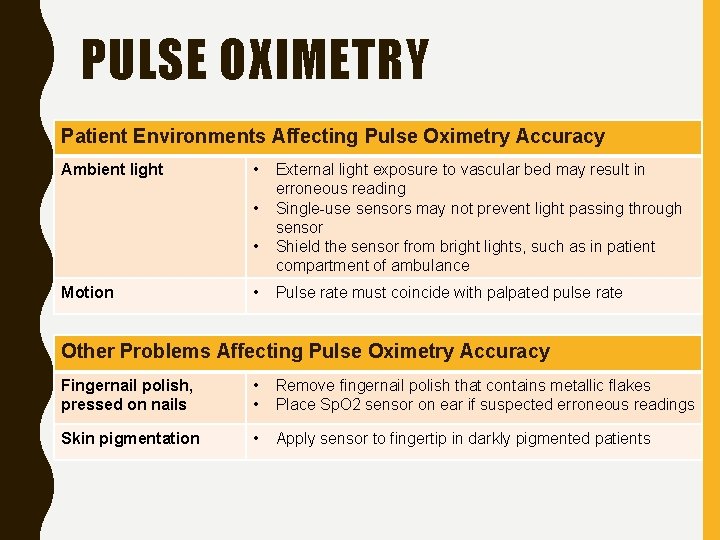
PULSE OXIMETRY Patient Environments Affecting Pulse Oximetry Accuracy Ambient light • • • Motion • External light exposure to vascular bed may result in erroneous reading Single-use sensors may not prevent light passing through sensor Shield the sensor from bright lights, such as in patient compartment of ambulance Pulse rate must coincide with palpated pulse rate Other Problems Affecting Pulse Oximetry Accuracy Fingernail polish, pressed on nails • • Remove fingernail polish that contains metallic flakes Place Sp. O 2 sensor on ear if suspected erroneous readings Skin pigmentation • Apply sensor to fingertip in darkly pigmented patients
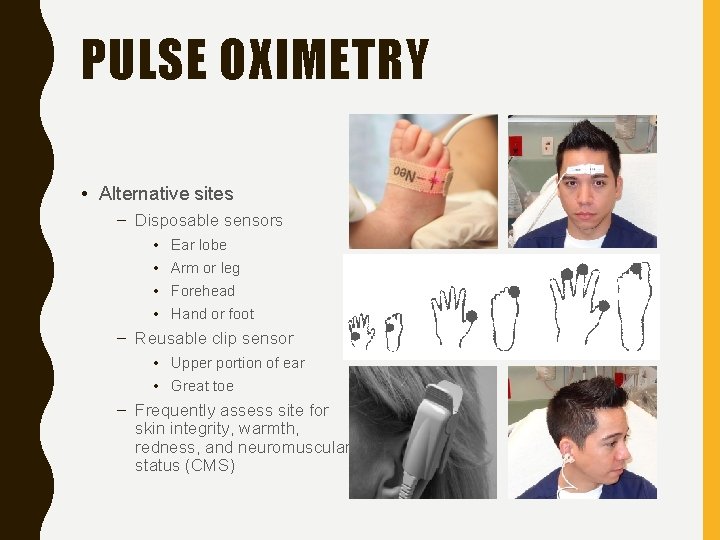
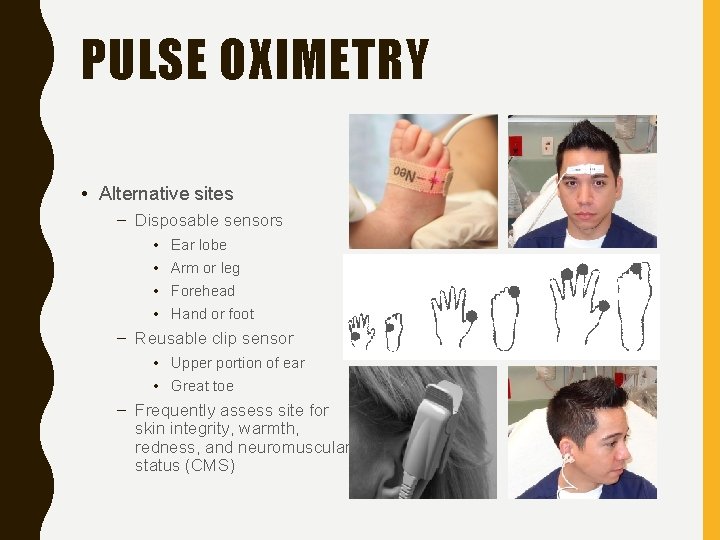
PULSE OXIMETRY • Alternative sites – Disposable sensors • • Ear lobe Arm or leg Forehead Hand or foot – Reusable clip sensor • Upper portion of ear • Great toe – Frequently assess site for skin integrity, warmth, redness, and neuromuscular status (CMS)
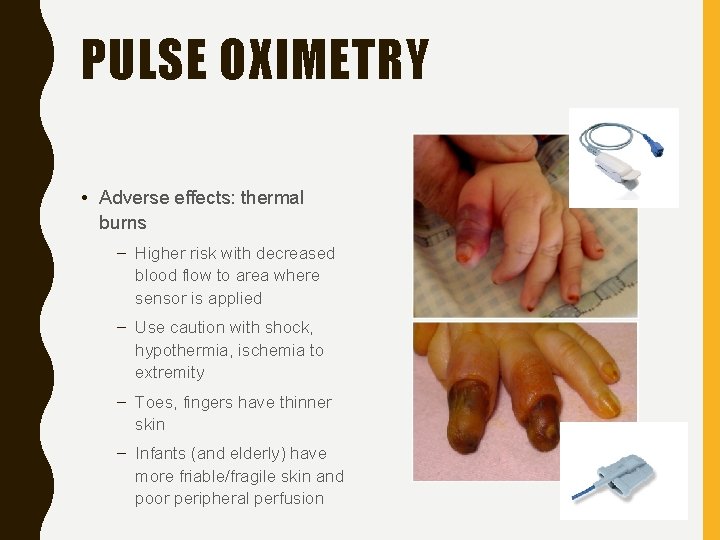
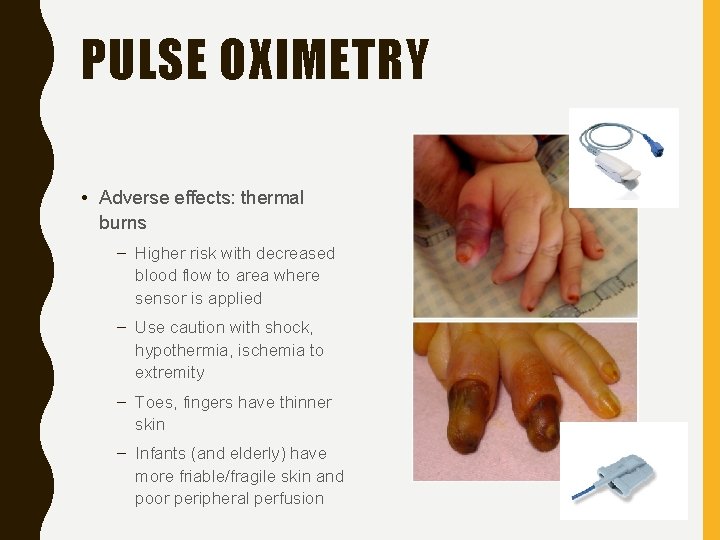
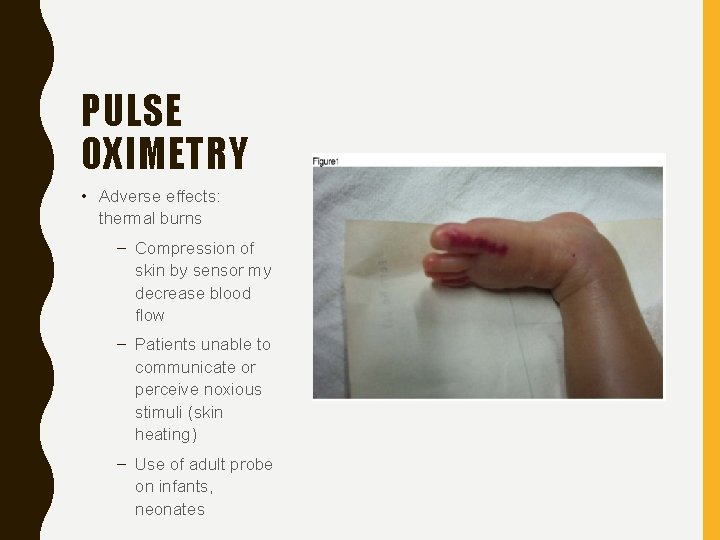
PULSE OXIMETRY • Adverse effects: thermal burns – Higher risk with decreased blood flow to area where sensor is applied – Use caution with shock, hypothermia, ischemia to extremity – Toes, fingers have thinner skin – Infants (and elderly) have more friable/fragile skin and poor peripheral perfusion
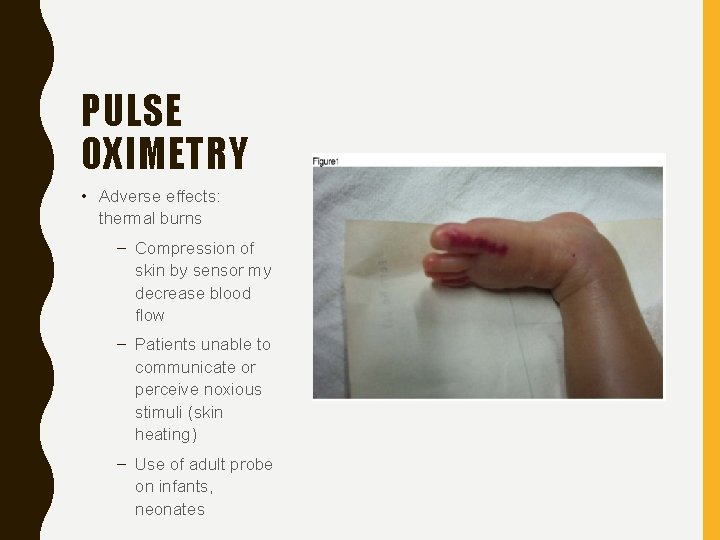
PULSE OXIMETRY • Adverse effects: thermal burns – Compression of skin by sensor my decrease blood flow – Patients unable to communicate or perceive noxious stimuli (skin heating) – Use of adult probe on infants, neonates

QUESTIONS?
 Tet spell
Tet spell Chest pediatric pulmonary board review
Chest pediatric pulmonary board review January 2016 chemistry regents answers
January 2016 chemistry regents answers Petmac chest pain
Petmac chest pain Causes chest pain
Causes chest pain Mason liker
Mason liker Dmagid
Dmagid ömpsq
ömpsq Chest pain in pediatrics
Chest pain in pediatrics Retrosternal chest pain
Retrosternal chest pain Stabbing pain in chest
Stabbing pain in chest What is referred pain
What is referred pain The canadian ed triage and acuity scale
The canadian ed triage and acuity scale Nursing care plan for angina
Nursing care plan for angina Typical vs atypical chest pain
Typical vs atypical chest pain Pms vs pregnancy symptoms
Pms vs pregnancy symptoms Pain x mad
Pain x mad Can u have period cramps and be pregnant
Can u have period cramps and be pregnant Polyhdramnion
Polyhdramnion Ece
Ece Site:slidetodoc.com
Site:slidetodoc.com January comes before february
January comes before february How many syllables in phenomenon
How many syllables in phenomenon January 24 1848
January 24 1848 9 months before january 26 2009
9 months before january 26 2009 June 2012 chemistry regents answers
June 2012 chemistry regents answers Character traits of respect
Character traits of respect Arvod cannot find work as a mall santa in january.
Arvod cannot find work as a mall santa in january. January 2012
January 2012 Spatial january
Spatial january An asset was purchased for $120 000 on january 1
An asset was purchased for $120 000 on january 1 January february spelling
January february spelling Sunday, tuesday, january, saturday
Sunday, tuesday, january, saturday February and march season
February and march season January 31 2006
January 31 2006 January 19, 1809
January 19, 1809 Meridel lesueur, new masses, january 1932.
Meridel lesueur, new masses, january 1932. Life of a plant by risa jordan
Life of a plant by risa jordan April 2006 calendar
April 2006 calendar 15 janvier 1929
15 janvier 1929 Mozart who was born on january
Mozart who was born on january Put in at on or in mozart was born in salzburg
Put in at on or in mozart was born in salzburg Hello song peter weatherall
Hello song peter weatherall Letter to senator robert wagner march 7 1934
Letter to senator robert wagner march 7 1934 Lipsume
Lipsume What is the theme for the month of january
What is the theme for the month of january January february march
January february march January 15, 1929
January 15, 1929 March april may june
March april may june January 19, 1809
January 19, 1809 Polytechnic hardware store
Polytechnic hardware store January 27, 1756
January 27, 1756 Ib physics hl grade boundaries
Ib physics hl grade boundaries 15 janvier 1929
15 janvier 1929 Zodiac for january 20
Zodiac for january 20 Your impolite tone surprises me
Your impolite tone surprises me 1st january 2018
1st january 2018 Blackberry devices working on january
Blackberry devices working on january Star life cycle from birth to death
Star life cycle from birth to death Kent chemistry reference table
Kent chemistry reference table 25 january scotland
25 january scotland Pro forma journal entries example
Pro forma journal entries example January 13 2006 calendar
January 13 2006 calendar January 10th 1776
January 10th 1776 25 january 1759
25 january 1759 Was born in salzburg austria on january 27 1756
Was born in salzburg austria on january 27 1756 January 29 2015
January 29 2015 Newton biography
Newton biography Months of the year december
Months of the year december Recumbent position used for
Recumbent position used for Wormhost chest worm locations
Wormhost chest worm locations Literary techniques in the scarlet letter
Literary techniques in the scarlet letter Chest area name
Chest area name Pleural effusion color chart
Pleural effusion color chart Pulse check in unresponsive victim
Pulse check in unresponsive victim Dullness percussion sound
Dullness percussion sound Head and chest circumference chart
Head and chest circumference chart Chest compressions
Chest compressions Paradoxical movement of the chest wall
Paradoxical movement of the chest wall Chest physiotherapy assignment
Chest physiotherapy assignment Flail chest adalah
Flail chest adalah Chest indrawing
Chest indrawing