Pain Science PAIN DRAWING PAIN DRAWING PAIN DRAWING


- Slides: 52
Pain Science
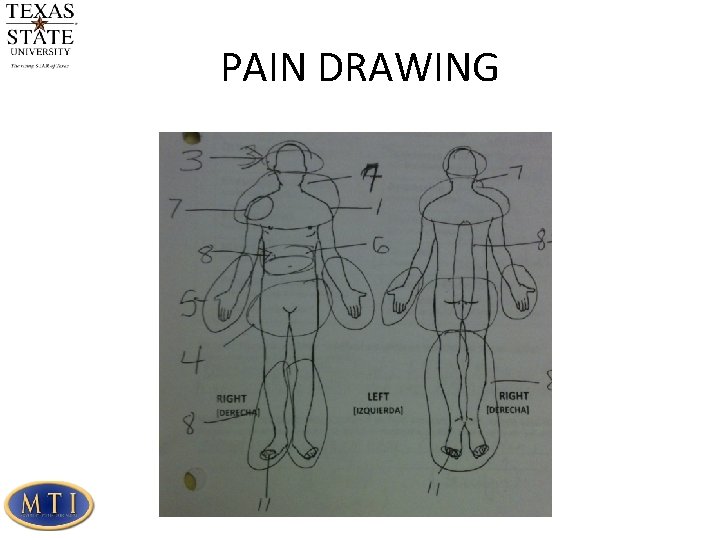
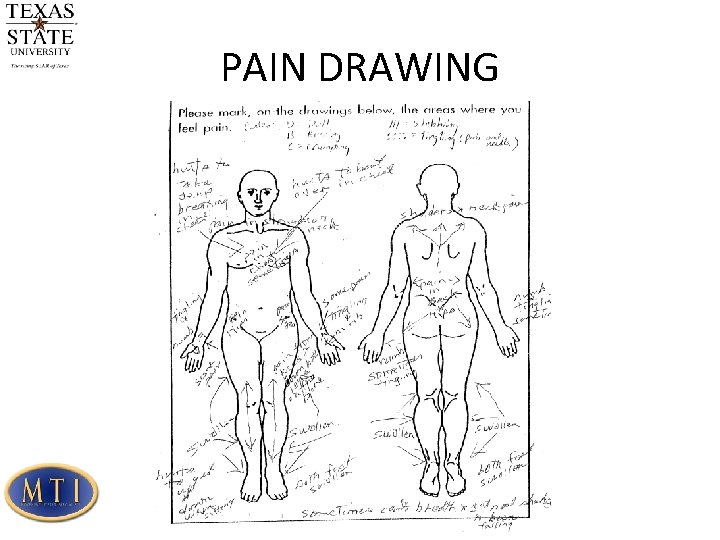
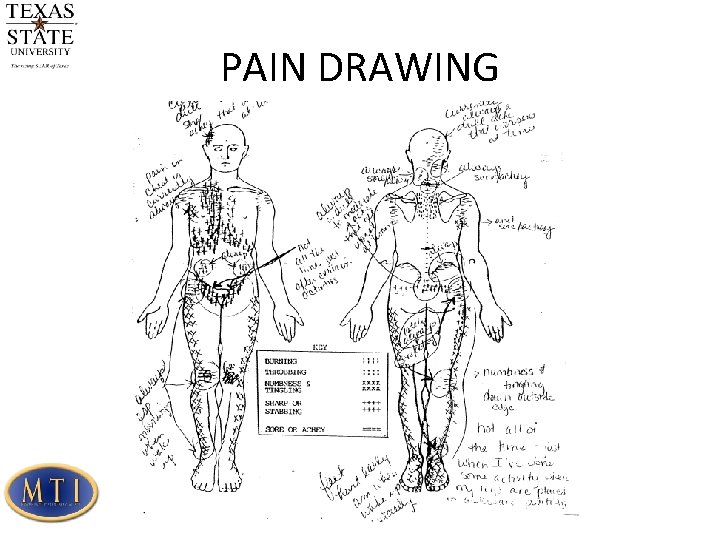
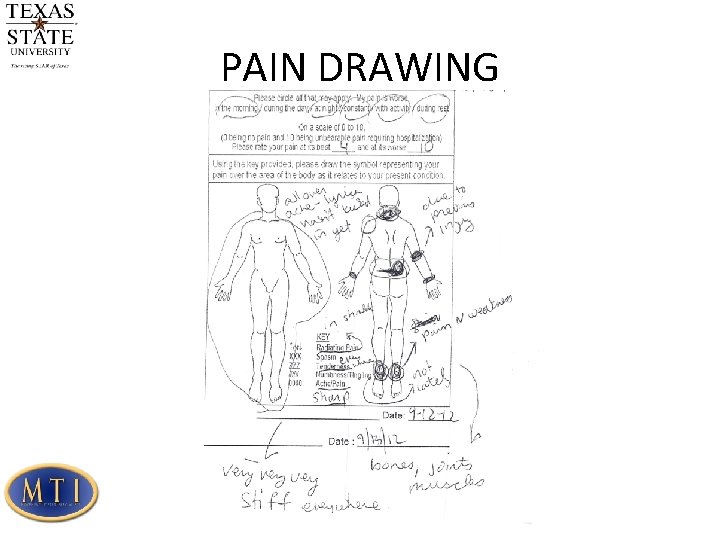
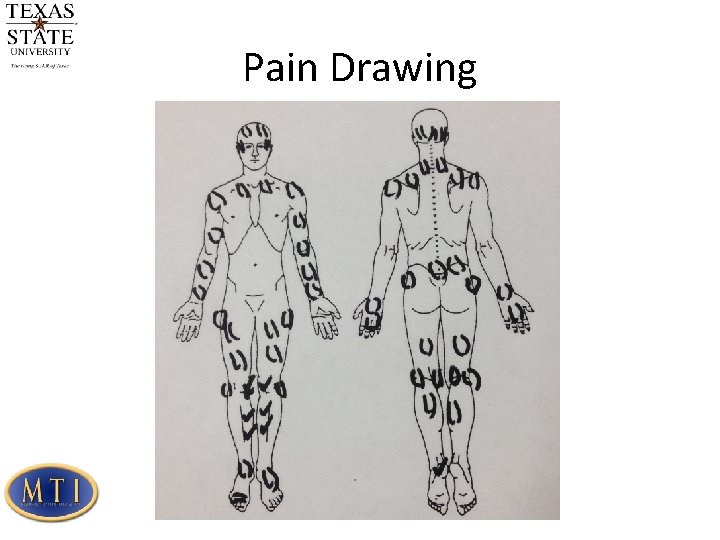
PAIN DRAWING
PAIN DRAWING
PAIN DRAWING
PAIN DRAWING
Pain Drawing
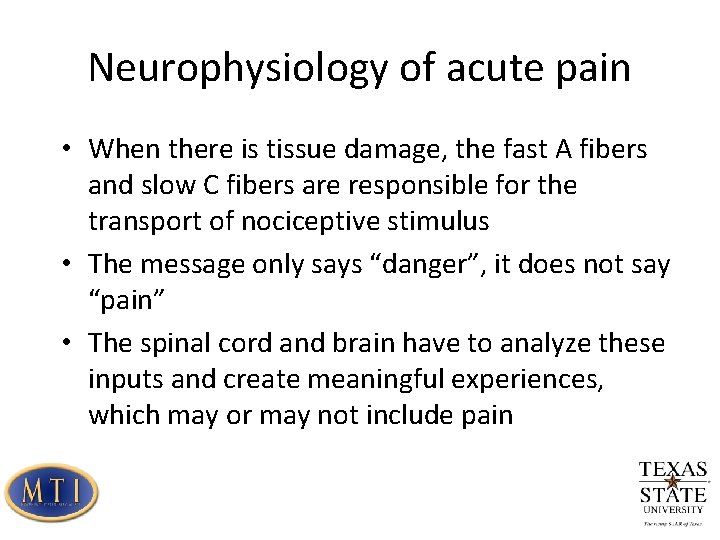
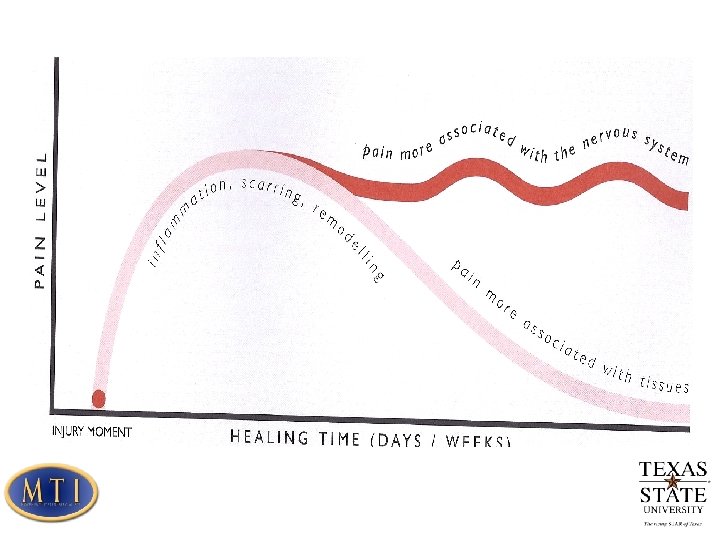
Neurophysiology of acute pain • When there is tissue damage, the fast A fibers and slow C fibers are responsible for the transport of nociceptive stimulus • The message only says “danger”, it does not say “pain” • The spinal cord and brain have to analyze these inputs and create meaningful experiences, which may or may not include pain
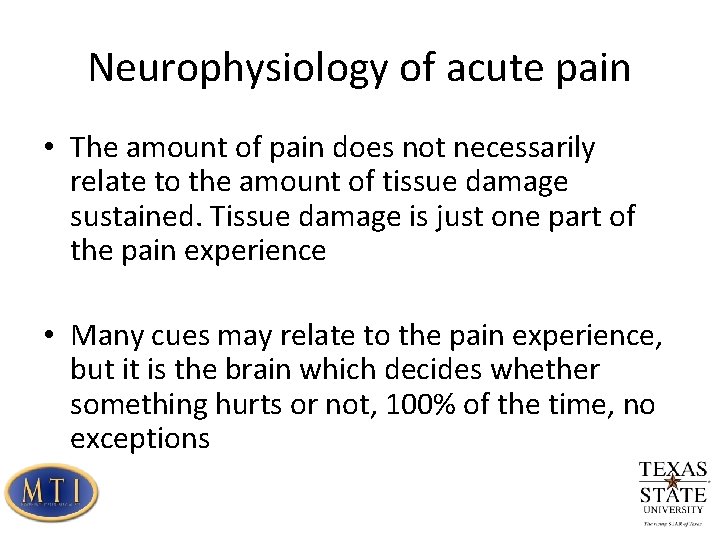
Neurophysiology of acute pain • The amount of pain does not necessarily relate to the amount of tissue damage sustained. Tissue damage is just one part of the pain experience • Many cues may relate to the pain experience, but it is the brain which decides whether something hurts or not, 100% of the time, no exceptions
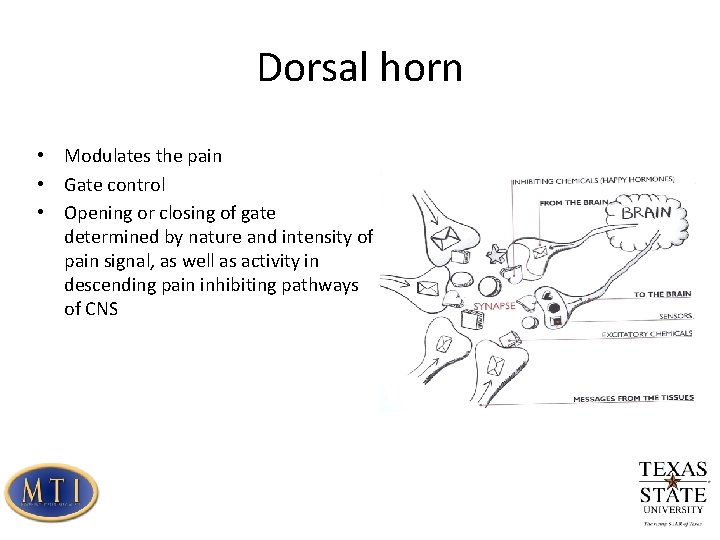
Dorsal horn • Modulates the pain • Gate control • Opening or closing of gate determined by nature and intensity of pain signal, as well as activity in descending pain inhibiting pathways of CNS
The adaptable nervous system • When impulses keep arriving at dorsal horn, the neurons adapt to meet that demand • This begins within seconds of the demand increasing • The neuron increases its sensitivity to incoming excitatory chemicals: primary hyperalgesia
Primary hyperalgesia • More nociceptor receptors are added • Increased responsiveness of nociceptor receptors • Protective action to prevent further use and damage of injured tissue • The danger message neuron increases its sensitivity to the incoming excitatory chemicals. This leads to hyperalgesia and allodynia • Hyperalgesia: things that used to hurt, now hurt more • Allodynia: things that didn’t hurt before, now hurt
Secondary hyperalgesia • Refers to adaptations in CNS • Increased responsiveness of dorsal horn neurons • Increased stimulus-response in all tissues innervated by involved segment • Results in pain complaints in areas other than where primary tissue damage took place
Ignition nodes • Not just one pain center in the brain • There are many, and include clusters of nodes used for movement, sensation, memory and emotions • Pain “borrows” from these parts to express itself • In chronic pain, these nodes are hijacked or enslaved by the pain experience
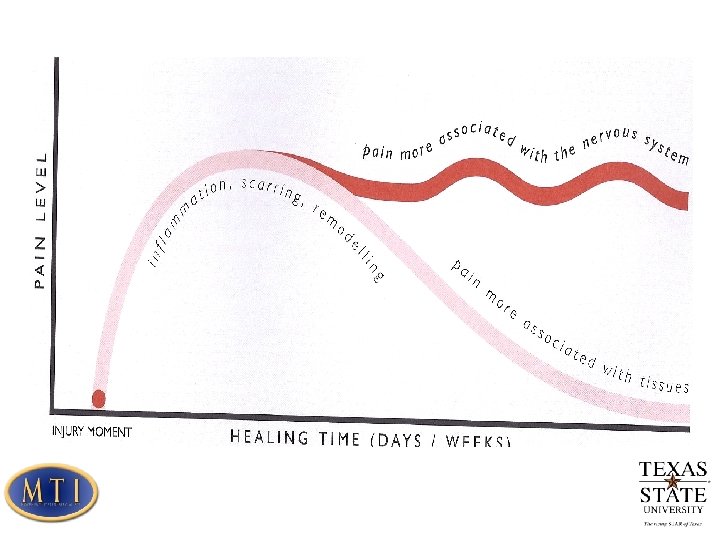
Neurophysiology of chronic pain • Central sensitization is the hall mark of chronic pain • Defined as augmentation of responsiveness of central neurons to input from receptors • Central sensitization requires functional changes in the CNS
Central Sensitization • Altered sensory processing in the brain • Malfunctioning of the descending antinociceptive mechanisms • Increased activity of pain facilitatory pathways • Your brain is tricked in a way. It is operating on faulty information about the condition of your tissues
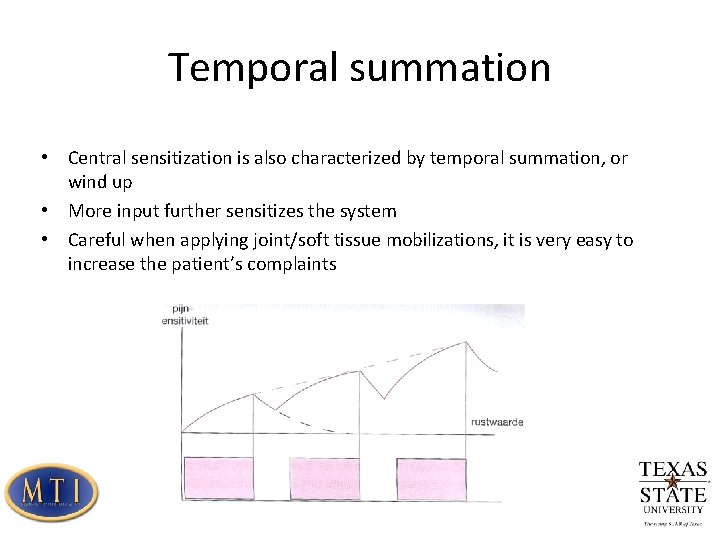
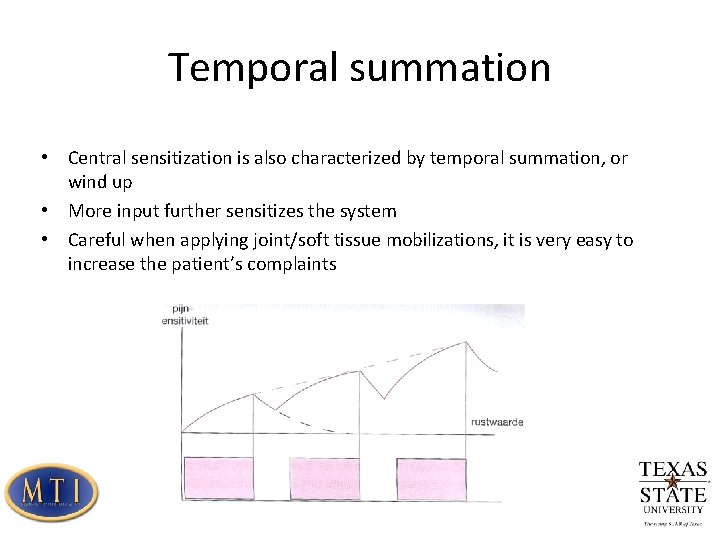
Temporal summation • Central sensitization is also characterized by temporal summation, or wind up • More input further sensitizes the system • Careful when applying joint/soft tissue mobilizations, it is very easy to increase the patient’s complaints
Central Sensitization • The amount of pain experienced by the patient does not necessarily relate to the amount of tissue damage sustained • Example: arthritic changes in the spine, disc bulges • If there is no pain, it means that changes in the tissue are not perceived by your brain as a threat • It is the brain which decides if something hurts or not, 100%
Central Sensitization • Instead of a clear view of what is happening in the tissues, the dorsal horn becomes a “magnifier” or “distorter” • The brain is being told there is more damage at the tissues then there really is. • Brain responses such as movement, thoughts, autonomic and endocrine responses are now based on faulty information about the health of the tissues
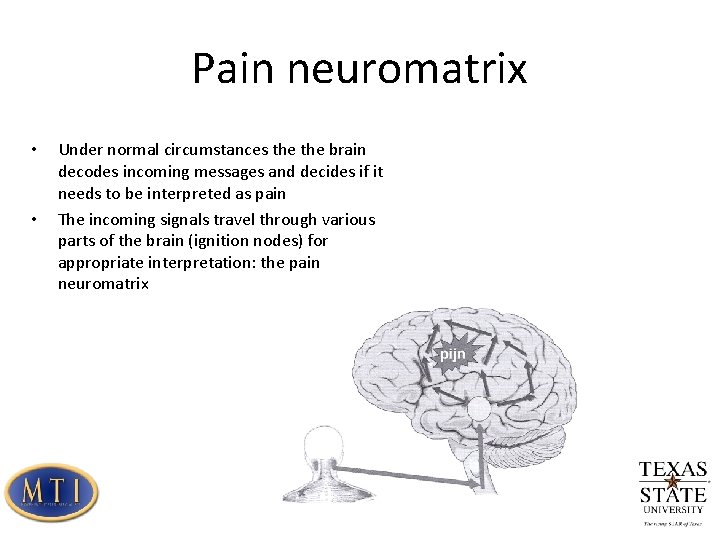
Pain neuromatrix • • Under normal circumstances the brain decodes incoming messages and decides if it needs to be interpreted as pain The incoming signals travel through various parts of the brain (ignition nodes) for appropriate interpretation: the pain neuromatrix
Pain Neuromatrix changes with chronic pain • Different brain patterns • Increased activity in certain parts of the brain • Increased manufacture of sensors in pain ignition nodes • Increased manufacture of chemicals that activate these sensors
RESULT • Potentially non threatening signals will be interpreted as threatening • Nociceptive signals will generate longer and more intense pain sensation
Neurotag • The constant activation of pain ignition nodes. • Chronic pain leads to persistent changes in endocrine- , immune-, motor- and nervous systems. They can combine to perpetuate the pain tune: the neurotag
In patients with chronic pain, descending pain inhibition fails, and is linked to psychological factors • • • Catastrophising Fear of movement Passive coping Hypervigilance Fear Depression
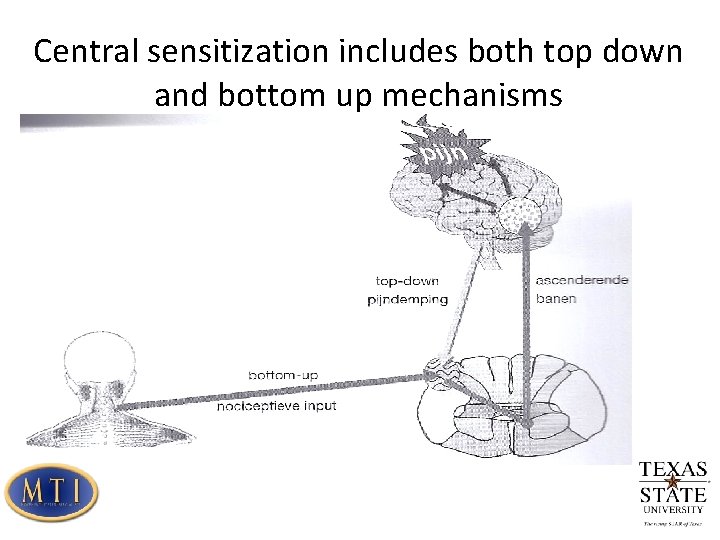
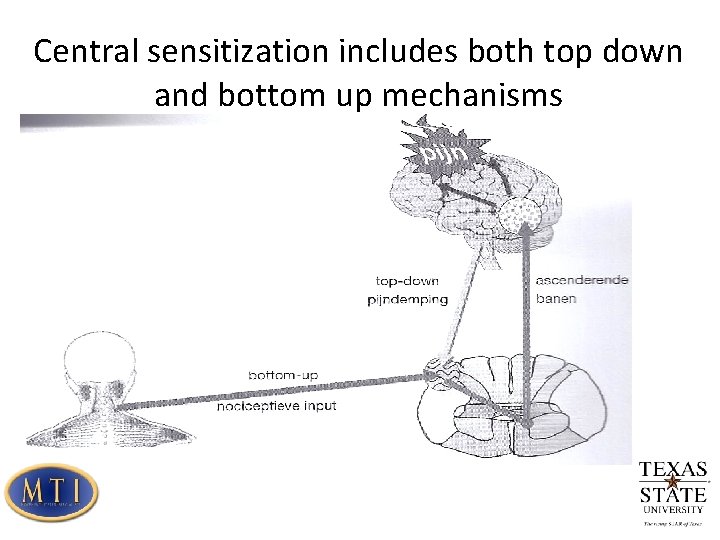
Central sensitization includes both top down and bottom up mechanisms
When does the brain decide if there is pain, or not? • You will have pain when the brain concludes there is more credible evidence of danger related to your body than there is credible evidence of safety related to your body.
Credible evidence of danger • Hearing that “there is nothing wrong with you so your pain is probably not real” • Believing you might end up in a wheelchair • Receiving a diagnosis that sounds bad without knowing what it really means • Going to the same place where you first injured your body
Credible evidence of safety • Being aware of a scientifically proven path to recovery • Making an appointment to see a good health professional • Knowing that your are not the only person to be in this situation • Having a local anaesthetic that blocks danger messages being sent to your spinal cord and brain • Loving support
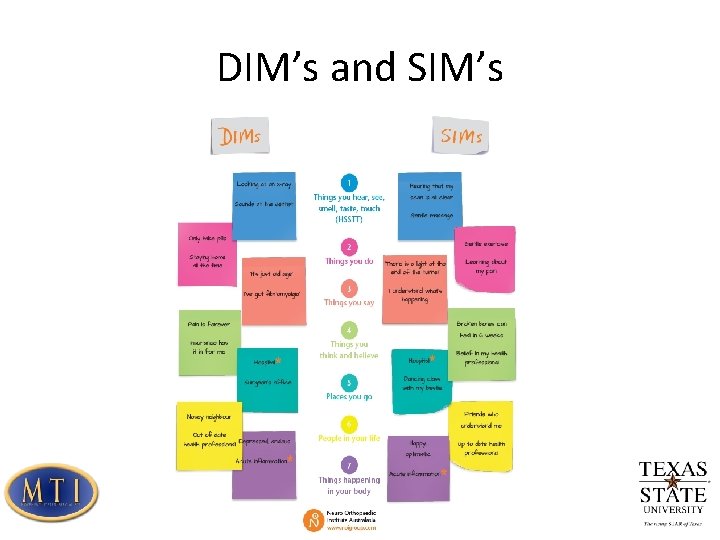
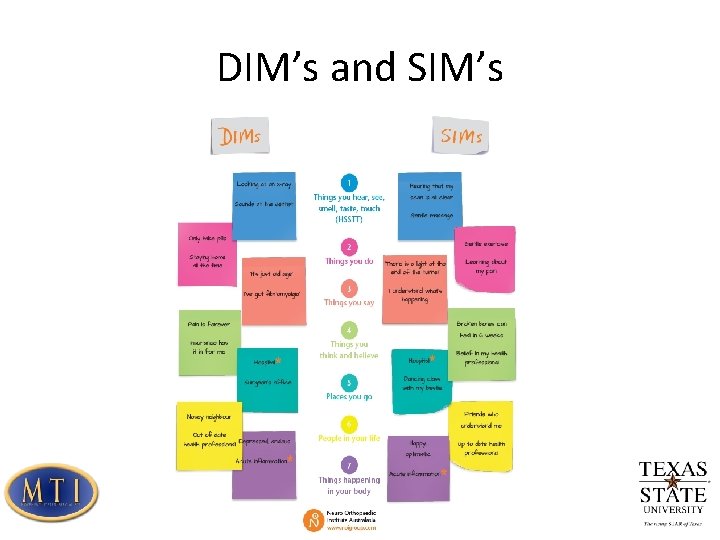
DIM’s and SIM’s
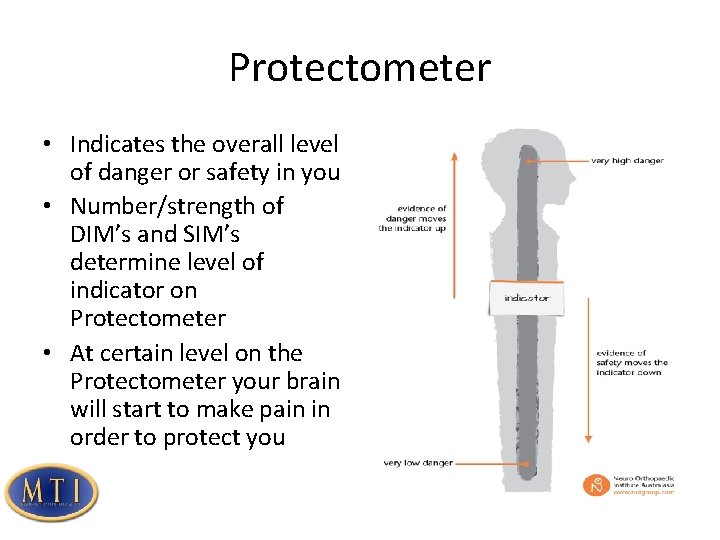
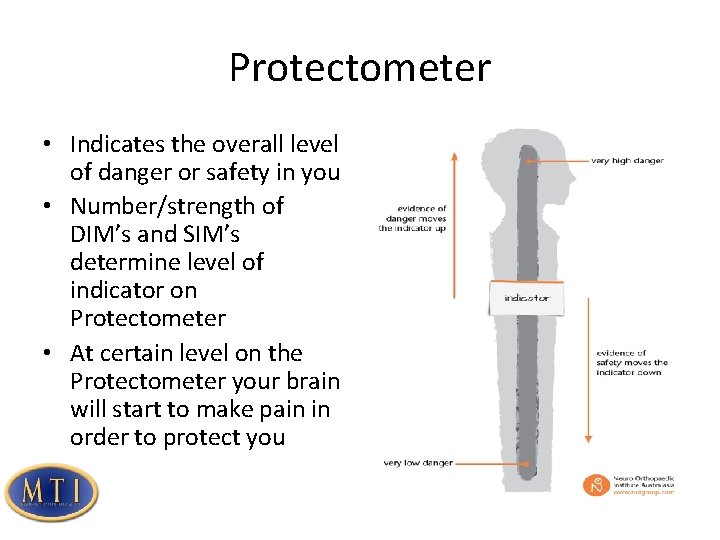
Protectometer • Indicates the overall level of danger or safety in you • Number/strength of DIM’s and SIM’s determine level of indicator on Protectometer • At certain level on the Protectometer your brain will start to make pain in order to protect you
Recognizing Central Sensitization • Increase in complexity of the clinical picture • Increase in unrelated symptoms • More difficult clinical reasoning process • Decreased odds of a favorable rehabilitation outcome
Central sensitization is characteristic for the following disorders • Chronic whiplash • Fibromyalgia • Irritable bowel syndrome • Chronic fatigue syndrome
Central sensitization is frequently present in a subgroup of dx • Chronic low back pain • Subacute whiplash • TMJ disorders • Rheumatoid arthritis • Chronic headaches • Osteoarthritis
History • general intolerance to physical and emotional stresses • sensitivity to bright lights (having to wear sunglasses inside), smells, loud noises (having to turn the radio down even when the volume is low already), hot/cold and touch. • fatigue • sleep disturbances • unrefreshing sleep • concentration difficulties • swollen feeling • tingling and numbness • When 2 -3 are present, it warrants further investigation
Clinical Examination • Pressure pain threshold • Sensitivity to cold, heat, vibration • Joint endfeel • Brachial plexus provocation test • Exercise response
Analyzing treatment response Central sensitization may not be present at the start of the treatment, but may become apparent during the rehab process. Therapy itself can become a stressor Other factors indicative of central sensitization: • non responders • post exertional malaise • decreased pain threshold during hands on treatment Consider the presence of central sensitization in poor treatment outcomes, but keep in mind that not all poor treatment outcomes are due to central sensitization
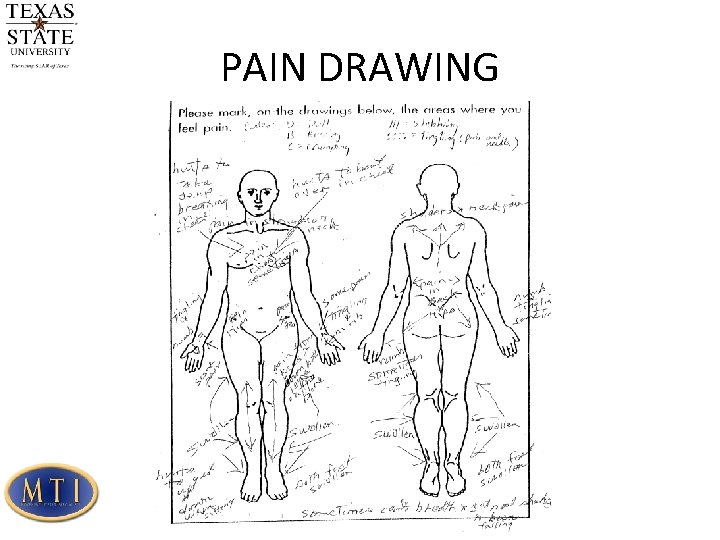
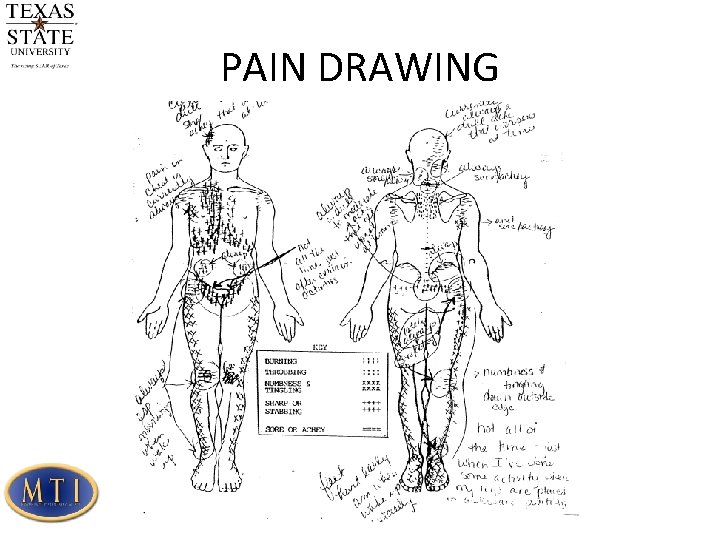
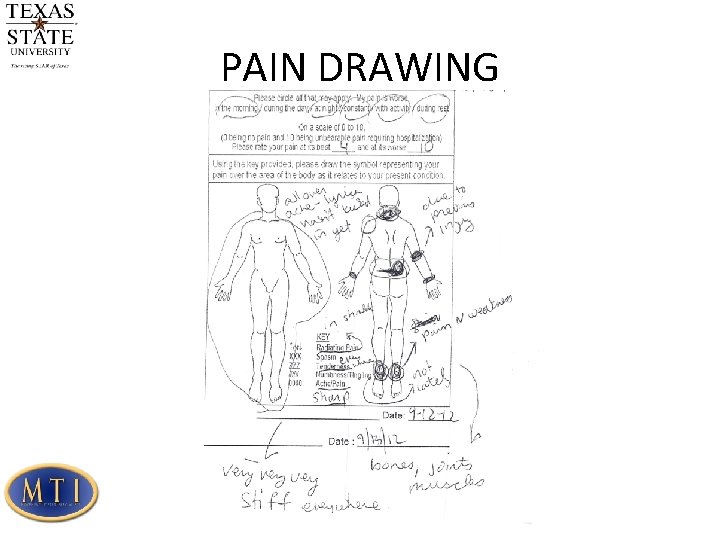
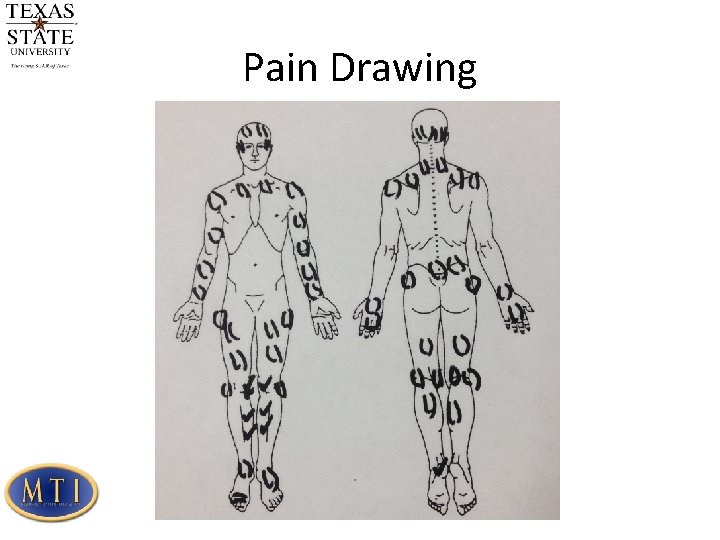
Pain Drawing Pain drawing describes the pain, but it can tell us about their psychological state and nervous system involvement as well Sheer quantity Addition of comments Excessive detail Do not overinterpret the pain drawing First clue that you should assess the patient in more depth Most patients with an exaggerated pain drawing are distressed, but 50% of patients in distress have a normal pain drawing
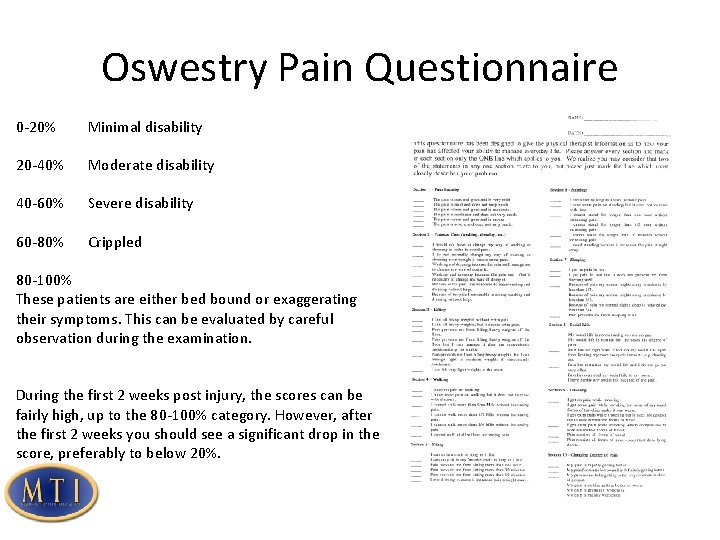
Oswestry Pain Questionnaire 0 -20% Minimal disability 20 -40% Moderate disability 40 -60% Severe disability 60 -80% Crippled 80 -100% These patients are either bed bound or exaggerating their symptoms. This can be evaluated by careful observation during the examination. During the first 2 weeks post injury, the scores can be fairly high, up to the 80 -100% category. However, after the first 2 weeks you should see a significant drop in the score, preferably to below 20%.
Yellow Flags Psychosocial risk factors that contribute to the development of chronic back pain and disability: • • • Patient believes that LBP is harmful and disabling Decreased activity levels and fear avoidance behavior Tendency to low mood and withdrawal from social activity Expectation of passive treatment Working more than one job Working overtime on a regular basis Job dissatisfaction Sickness benefits Compensation/litigation The current consensus is that psychosocial issues rarely cause acute pain, but are more important than physical features in determining which patients proceed on to chronicity and which patients can be helped. Screen early
Fear Avoidance Beliefs Patients who believe that physical activity may aggravate their pain, whether from past experience or because of their understanding of the pain, will expect and fear more pain if they are active. This is all a matter of fears and expectations about what may happen. Waddell found that low back disability depends more on fear avoidance than on pain or physical pathology. Fear of pain may be more disabling than pain itself Research has demonstrated a strong relationship between elevated fear avoidance beliefs and chronic disability due to LBP
FABQ A research study by Fritz and George in 2002 shows that the FABQ work subscale may be able to serve as a useful screening tool to identify increased risk form prolonged work absence A score of 29 or less has a negative LR of 0. 08 A score >34 has a positive LR of 3. 33 Reliability for the FABQ is. 77 for back pain Fritz JM and George, SZ. Identifying psychosocial variables in patients with acute work related low back pain: the importance of fear avoidance beliefs. Phys Ther Vol 82 No 10 2002
Consensus Guidelines Exclude serious disease (red flags) Avoid over investigation, labeling and over medication Continue with regular activities Early return to work Simple symptomatic measures Educate the patient that LBP is common, frequently recurrent, but acute attacks are usually brief and self-limiting Physical demanding work is one factor influencing LBP, but often not the most important Prevention and case management needs to be directed at both physical and psychosocial factors.
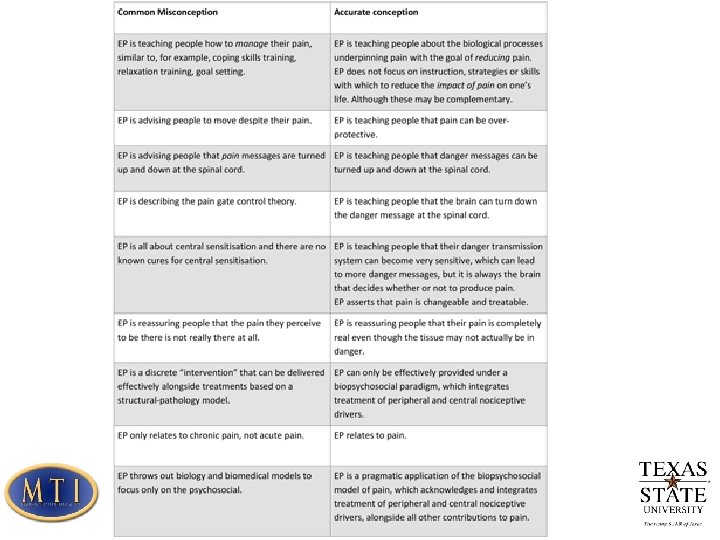
Pain Education Increase the knowledge of the neurophysiological mechanisms of chronic pain Provide insight in the role of biopsychosocial issues in chronic pain It is not totally clear yet what the most effective form of pain education is. Just handing out pain education booklets is insufficient to change illness perception. A combination of individual education sessions, a tailor made exercise program and written material appears to be more effective Focus on detailed explanation of pain physiology, and altering maladaptive responses to pain Patients in general have a poor understanding of the neurophysiology of pain, and providing education can significantly improve this knowledge. A study by Mosely directly related neurophysiology pain education to increased ROM, improved motor control and increased SLR
First session Explain mechanisms of central sensitization. Explain treatment rationale and discuss practical issues of treatment. Goal: Alter the patient’s knowledge about their pain state and re-conceptualize pain (i. e. a patient with chronic whiplash who is convinced the initial trauma caused such severe cervical damage that somehow remained invisible to modern medical imaging) Simply providing education about fear avoidance and the need for graded activity is unlikely to be beneficial. Detailed pain physiology education is required to re-conceptualize pain and to convince the patient that the hypersensitivity of the nervous system, rather than local tissue damage is the cause of their symptoms.
First session Topics to be included: • Characteristics of acute vs. chronic pain • Purpose of acute pain • How acute pain originates in the nervous system • How pain becomes chronic (plasticity of nervous system, modulation, modification and central sensitization) • Potential sustaining factors of central sensitization: emotion, stress, illness perception, pain cognition and pain behavior. • At the end of the session give them the neurophysiology of pain test, which they need to complete prior to the next session.

Neurophysiology of Pain Test
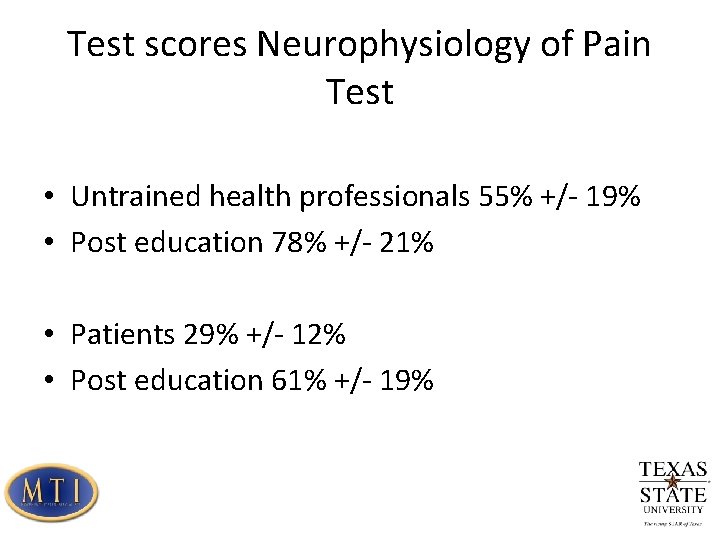
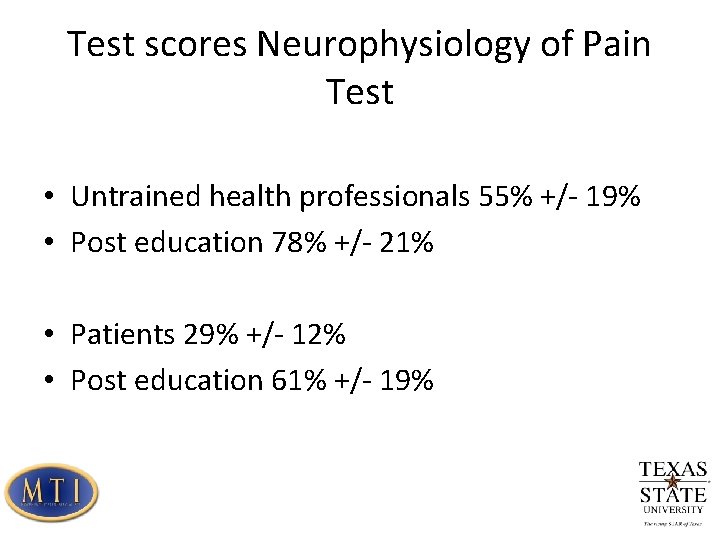
Test scores Neurophysiology of Pain Test • Untrained health professionals 55% +/- 19% • Post education 78% +/- 21% • Patients 29% +/- 12% • Post education 61% +/- 19%
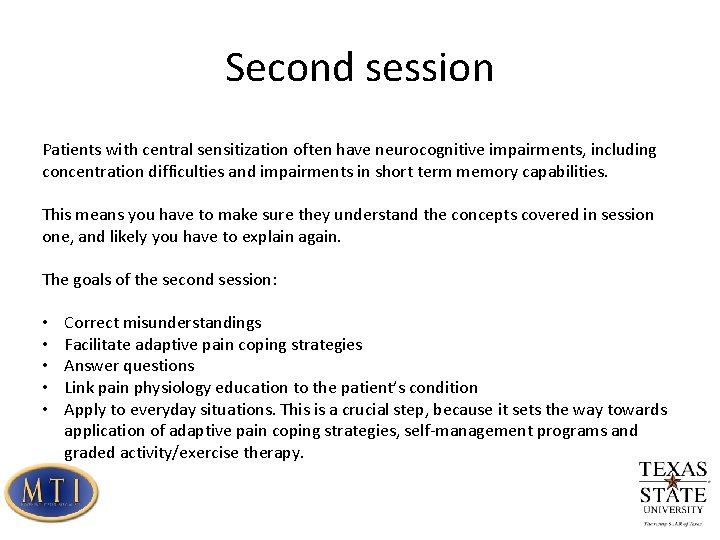
Second session Patients with central sensitization often have neurocognitive impairments, including concentration difficulties and impairments in short term memory capabilities. This means you have to make sure they understand the concepts covered in session one, and likely you have to explain again. The goals of the second session: • • • Correct misunderstandings Facilitate adaptive pain coping strategies Answer questions Link pain physiology education to the patient’s condition Apply to everyday situations. This is a crucial step, because it sets the way towards application of adaptive pain coping strategies, self-management programs and graded activity/exercise therapy.

Second session, new goals • Stop ruminating and worrying about pain • Reduce stress • Increase physical activity levels • Decrease hypervigilance (constant screening of body to assess for pain)
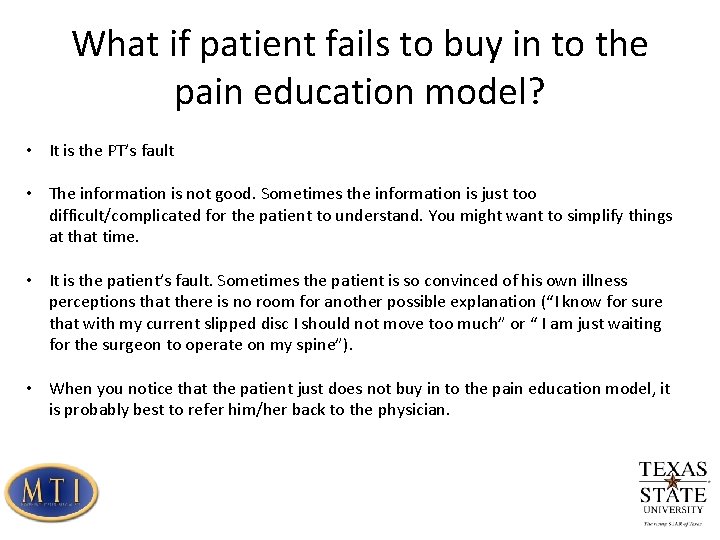
What if patient fails to buy in to the pain education model? • It is the PT’s fault • The information is not good. Sometimes the information is just too difficult/complicated for the patient to understand. You might want to simplify things at that time. • It is the patient’s fault. Sometimes the patient is so convinced of his own illness perceptions that there is no room for another possible explanation (“I know for sure that with my current slipped disc I should not move too much” or “ I am just waiting for the surgeon to operate on my spine”). • When you notice that the patient just does not buy in to the pain education model, it is probably best to refer him/her back to the physician.
Perils of Pain Education • Pain education is difficult • Don’t try to dumb it down • Don’t follow the Pain Education with “traditional treatments” • Think differently and more broadly
 Favorite subject is science
Favorite subject is science Lewis mad pain and martian pain
Lewis mad pain and martian pain Period cramps vs early pregnancy cramps
Period cramps vs early pregnancy cramps Pms vs pregnancy symptoms
Pms vs pregnancy symptoms Social science vs natural science
Social science vs natural science Branches of science
Branches of science Natural science vs physical science
Natural science vs physical science Applied science vs pure science
Applied science vs pure science Rapid change
Rapid change Science fusion online
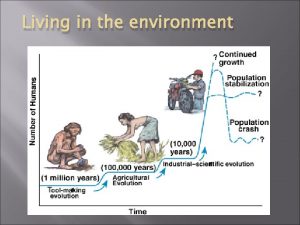
Science fusion online Rule of 70 population growth
Rule of 70 population growth Julie lundquist
Julie lundquist Hard science and soft science
Hard science and soft science Tripod science drawing
Tripod science drawing Pictorial drawing in engineering drawing
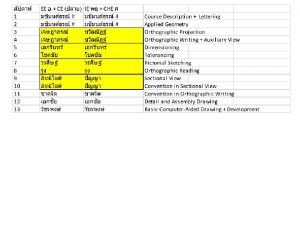
Pictorial drawing in engineering drawing Engineering drawing standards
Engineering drawing standards Spline shaft technical drawing
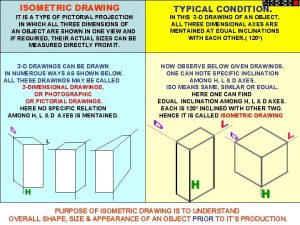
Spline shaft technical drawing Isometric axis
Isometric axis Introduction of drafting
Introduction of drafting Artistic drawing vs technical drawing
Artistic drawing vs technical drawing While drawing isometric view/drawing scale is reduced by
While drawing isometric view/drawing scale is reduced by Vena oesophageales
Vena oesophageales Systematic review in history taking
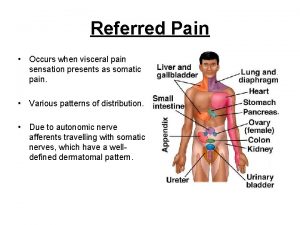
Systematic review in history taking Referred pain definition
Referred pain definition Par ton corps tu nous donnes la vie
Par ton corps tu nous donnes la vie Societal impact of pain
Societal impact of pain Moshe schein
Moshe schein University hospital of pisa
University hospital of pisa Pain management okc soonercare
Pain management okc soonercare I see every round as it rips through his life
I see every round as it rips through his life When was remains written
When was remains written Prostate referred pain
Prostate referred pain Actigramme exemple
Actigramme exemple Cpot pain scale
Cpot pain scale Example of pico question
Example of pico question Chest pain in pediatrics
Chest pain in pediatrics Pqrst pain assessment
Pqrst pain assessment Unpleasant sensory
Unpleasant sensory Internal medicine jeopardy questions and answers
Internal medicine jeopardy questions and answers Non-opioid
Non-opioid Stony brook pain management
Stony brook pain management Opqrst
Opqrst Painad
Painad Pain score assessment
Pain score assessment Pain scale ruler kkm
Pain scale ruler kkm Ms pain points
Ms pain points Npass pain scale
Npass pain scale Coat hanger pain
Coat hanger pain Larry leeman
Larry leeman Pain de vie corps ressuscité
Pain de vie corps ressuscité Digestion chimique
Digestion chimique Nccpc pain scale
Nccpc pain scale Iv site complications
Iv site complications