Pain Management Why Treat Pain Animals feel pain






















- Slides: 66

Pain Management
Why Treat Pain? Animals feel pain just like us n Unethical not to address pain n Animal owner and public concerns n Many anesthetics have no analgesic effect n – Which do? n Pain results in poor anesthetic recovery
MYTHS “Anesthetics mask symptoms” “Patient will harm itself if there’s no pain” “Pain is difficult to assess”
The Truth! n Pain is BAD: – Decreased cardiovascular function – Decresed appetite – Slows wound healing – Decreased immune function » Greater chance of infection – Increased fear and anxiety
Use of Analgesics in Practice n Overall = poor – 13 -26% dog and cat spay/neuters receive analgesics – 50 -70% of non-neutering soft tissue surgery – >80% orthopedic surgery and severe trauma n Why not better? – – DEA / theft concerns Older vets not trained that way Older drugs dangerous Animals are stoic
Pain Perception n Pain sensor nerve fiber spinal cord brain n Neurotransmitters>> – – – Somatic ( superficial ) pain Visceral ( internal organ ) pain Bone pain
Classification of Pain n n Intensity (scale of 1 -10) Acute, sharp, sudden, short – Surgical pain – Responds well to drug tx n Chronic, dull, prolonged – Cancer or arthritis – Doesn’t always respond well to tx n n n Referred (from somewhere else) Hyperesthesia (increased sensitivity) Neuropathic (Nerve damage) – Poorly responsive
Degree and Type of Pain Depend On The procedure n The animal n – Pain is an individual experience » Tailor analgesic protocol to the patient n Analgesic administration – Timing – Dosage
Preemptive Analgesia n If the body doesn’t sense the pain during the procedure, the pain will be easier to deal with post-operatively – A patient in surgical anesthesia is not aware of pain, but the body is still responding sensitizes the nervous system
Preemptive Analgesia Results In Marked decrease in amount of analgesic medication needed post-operatively n Increased patient comfort n

Balanced Anesthesia Several anesthetic drugs are combined into anesthetic protocol n Include analgesic n Synergism n – Smaller dosages needed – Decreased potential for side effects
Monitoring Signs of Pain Facial Expression Vocalization Body Posture Abnormal Gait Decreased Activity Level Attitude Appetite Grooming Urination/Defecation Habits
Methods of Pain Control n Non-pharmacological methods: Endorphins = The body’s natural painkillers n Good nursing care n – Comfortable bedding » Clean and dry – Easy access to bathroom, food, water – TLC – Rotate recumbency – Allow time to sleep
Non-pharmacological Methods n Apply cold to site (acute- 1 st 24 hours) – Decreases inflammation – Numbs Apply heat to site (chronic) n Massage n Acupuncture/acupressure n Complementary methods n – Herbs, laser, magnetic, chiropractic
Pharmacologic Methods Opioids n 2 agonists n Steroids n NSAIDS n Local anesthetics n Chondroprotective drugs n
Opioids
Opiate Receptors MOA? 4 types of receptors: mu kappa sigma delta Should we be wondering why fraternities/sororities name themselves after receptors of pain? ?
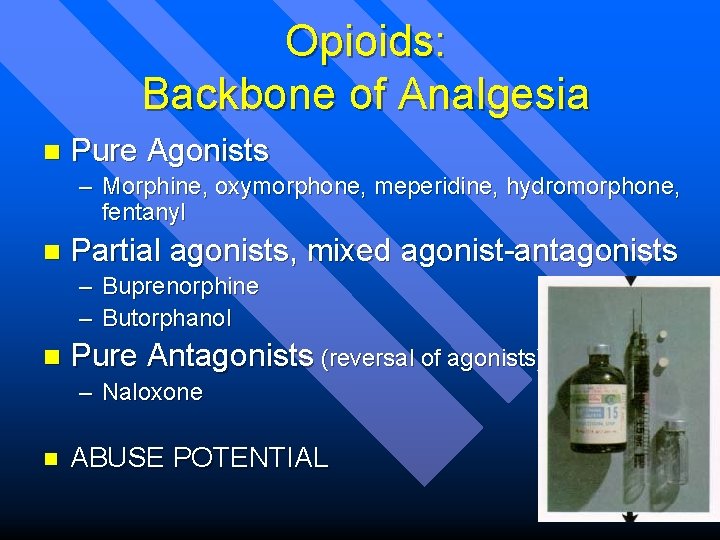
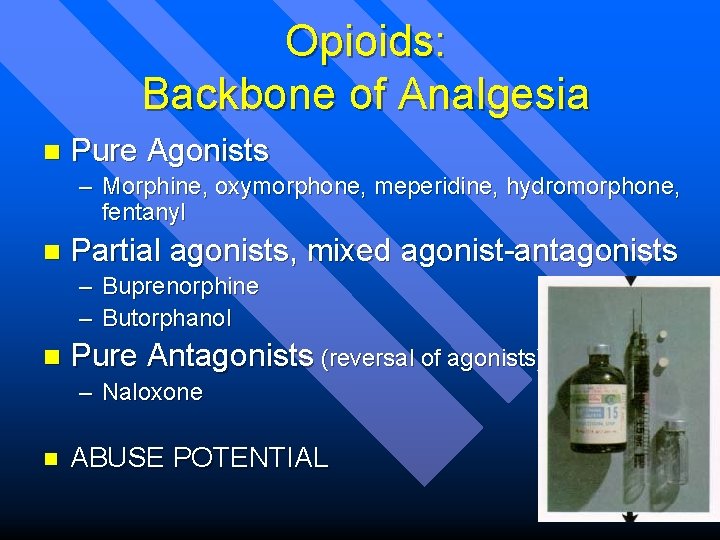
Opioids: Backbone of Analgesia n Pure Agonists – Morphine, oxymorphone, meperidine, hydromorphone, fentanyl n Partial agonists, mixed agonist-antagonists – Buprenorphine – Butorphanol n Pure Antagonists (reversal of agonists) – Naloxone n ABUSE POTENTIAL

Opioid Administration Systemic: IV, SQ, IM, CRI n Intra-articular injection n Local injection n Epidural injection n Transdermal fentanyl patch n
Opioid Effects n GOOD: – Great analgesia – Variable muscle relaxation – Sedation n BAD: – Respiratory depression – GI effects » Vomiting » Defecation followed by constipation
Opioids (other effects) n Excitement – Panting – Vocalization – Noise sensitivity n Depression of the cough center – Advantage for?

Fentanyl Patch n Lag time: – apply 6 -12 hours prior to surgery in cats, – 12 -24 hours in dogs n n Lasts about 3 days (up to 6 in cats) Variation in absorption rate – Dose of patch (in micrograms/hr) – Avoid heat sources n Excessive amounts can cause ataxia, sedation in dogs, excitement, disorientation, wide-eyed stare in cats – Remove patch, can reverse

Fentanyl Patch n n n Applied to dorsal neck or shoulders, lateral thorax Clip hair, clean skin with water only Do not cut patch – Can remove just part of backing if small animal n n Apply patch, hold firmly 2 minutes Bandage
Opioid Partial Agonists Buprenorphine n Buprenex® n 4 -8 hour duration n

Opioid Mixed Agonist-Antagonist Butorphanol n (Torbutrol®, Torbugesic®) n For mild to moderate pain n Duration 1 to 4 hours IM, SQ n n Less abuse potential than agonists
Opioid Antagonists n Naloxone Used to reverse opiates/opioids n Remember: Reverses analgesia too! n May not last as long as the agonist n – Relapse =“renarcotization” n Partial reversal with butorphanol possible

Alpha-2 Agonists “thiazines”
Alpha-2 Agonists n MOA? Engages receptors in CNS >> decrease norepinephrine n Examples: – Xylazine (Rompun®) – Medetomidine (Domitor®)

Xylazine: Good Things n Moderate analgesia n Potent sedative effect n Good muscle relaxation
Xylazine: Bad Things Bradycardia due to stimulation of the vagus nerve heart block n Profound cardiac disturbances! n – Sensitizes the heart to catecholamines Arrhythmias – Decreased cardiac output » Hypotension (BP decreases by 1/4 -1/3)
Xylazine: More Bad Things n Vomiting (sometimes used as emetic)
Xylazine: Reversal? n Yohimbine is reversal agent Mixed Alpha- antagonist (blocker) n Trade name “Yobine” n
Medetomidine n n n =DOMITOR® More specific to CNS alpha-2 receptors Alpha-2 so has reversal agent – (Antisedan®)
Steroids= corticosteroids, glucocoticoids • Examples: – Prednisone = Prednisolone – Dexamethasone – Betamethasone – Solu-Delta-Cortef – Solu-Medrol • Decrease pain by decreasing inflammation

Steroids: MOA inhibit phospholipase A 2>>> inhibits prostoglandin/leukotrienes Membrane Phospholipid Phospholipase A 2 Steroids inhibit here Arachidonic Acid COX-2 NSAIDS inhibit here “Bad” Prostaglandins Pain/Inflammation COX-1 Thromboxane “Platelets” “Good” Prostaglandins GI Protection Renal Blood Flow

Side Effects and Toxicity • Iatrogenic hyperadrenocorticism – “Cushings Dz” • • • Polyphagia PU/PD Glaucoma and cataracts Gastric ulceration Delayed wound healing Immunosuppression
More ! • • Insulin resistance Hepatopathy CNS: restlessness, seizure activity Infection
Non-Steroidal Anti-inflammatory Drugs ( NSAIDS ) n Aspirin Carprofen - Rimadyl ® Etodolac - Etogesic® Ketoprofen - Ketofen ® Phenylbutazone – “Bute” n Flunixin - Banamine ® n (Acetaminophen - Tylenol ®) n n
NSAIDS Most have effective somatic (superficial) analgesic effect n Some have good visceral analgesic effect also n All take 30 -60 minutes to take effect, even if injected n All have antiinflammatory properties n Reduce fevers n

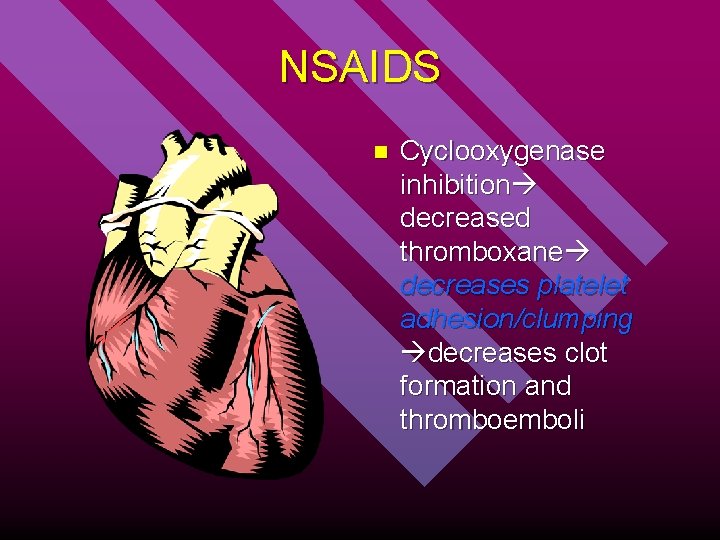
NSAIDS MOA: cyclooxygenase inhibitors >> prostaglandin inhibitors n Many side effects are due to “good” prostaglandin inhibition (COX 1): n – GI upset/ ulceration – Renal toxicity – Impaired platelet function

NSAIDS: MOA inhibit cyclooxygenase>>> inhibits prostoglandin/thromboxane Membrane Phospholipid Phospholipase A 2 Steroids inhibit here Arachidonic Acid COX-2 NSAIDS inhibit here “Bad” Prostaglandins Pain/Inflammation COX-1 Thromboxane “Platelets” Fever “Good” Prostaglandins GI Protection Renal Blood Flow
NSAIDS - Metabolism Metabolized by the liver n Variation in metabolism between species n Aspirin half-life 12 hours in dogs, 1 hour in horses, 38 hours in cats n Many NSAIDS toxic to cats due to inability to metabolize them n Acetaminophen is toxic in dogs AND cats! n
NSAIDS Inhibit Production of Protective GI Prostaglandins Erosion/ulceration of GI tract n Stomach upset n Inappetance n Vomiting n Diarrhea n Melena ? n
Prostaglandins in the Kidneys n Cause dilation of renal vasculature, allowing perfusion despite decreased blood pressure due to – – n n Shock Dehydration Blood loss Anesthesia Inhibition of prostaglandin production cause kidney cell death due to lack of perfusion Only an issue if decreased BP
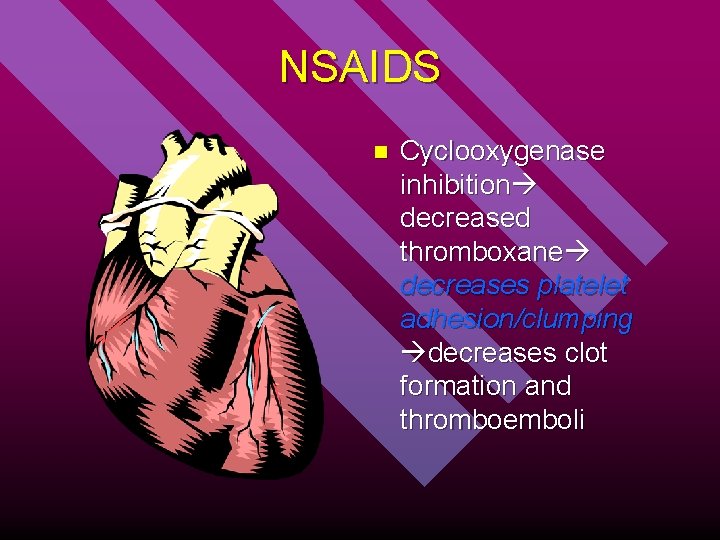
NSAIDS n Cyclooxygenase inhibition decreased thromboxane decreases platelet adhesion/clumping decreases clot formation and thromboemboli
TYPES of NSAIDs
Phenylbutazone COX 1 and 2 Inhibitor n Very Potent n Commonly used in horses n Not recommended in dogs n – GI side effects common – NEVER IN CATS!
Aspirin n COX 1 and 2 Inhibitor n Very short half-life in horses Commonly used in dogs n – Buffered only – With food n Use with caution in cats – – – Can’t metabolize well Half-life 38 hours Dosed every 48 -72 hours
Ibuprofen = “Advil” COX 1 + COX 2 Inhibitors Officially not recommended in dogs. most do OK if used like aspirin Neither Ibuprofen Nor Naproxen Is Recommended

Ketoprofen n n Ketofen® (COX 1 and COX 2) Licensed in horses Approved for use in dogs and cats in Canada, Europe Good analgesia, potent antipyretic Injectable – Limit use – Blood clotting
Flunixin meglumine Banamine® (COX 1 and COX 2) n Injectable n Horses n – Colic – Good analgesia n Dogs – GI side effects common, severe

Carprofen n n Rimadyl ® COX-2 inhibitor: “spares” “good” prostaglandins Fewer side effects DOGS ONLY Black labs… – 0. 06% of all dogs develop hepatic problems (rare) n BID Dosing

Etodolac n n Etogesic ® COX 1 and 2 Inhibition Once daily administration DOGS ONLY

Derramax Use in dogs n COX 2 Specific n SID dosing n $$ n

“Metacam” =Meloxicam COX-2 Specific n Use in dogs and cats n Liquid n Well tolerated n $$ n
NSAID Precautions n Use only 1 NSAID at a time n Never combine NSAIDS with glucocorticoids – Gastric Ulceration n Taper to lowest effective dose n Change to alternative NSAID if poor response
NSAID Contraindications Renal of hepatic dysfunction n Decreased circulating blood volume n Coagulopathies n GI disease n Pregnancy n

Local Anesthetics
Local Anesthetics n The “-caine” family: Lidocaine, bupivicaine, mepivicaine, proparicaine, tetracaine, etc. n MOA= Block nerve impulses by blocking Na+ channels in nerve membranes

Local Anesthetics Local infiltration of surgical site n Intravenous regional anesthesia n Intra-articular injection n Nerve blocks n Epidural n Topical on skin/ eye/ larynx n n http: //www. cvm. okstate. edu/courses/vmed 5412/Lect 23. asp
Commonly Used With Neuroleptanalgesic
Capsaicin n Hot peppers Excites then fatigues nerve transmission local analgesia Also get endorphin release

St. Johnswort n n Arthritic pain Hypericin – Stimulates neural inhibitory pathways analgesia

Chondroprotective Agents n Nutraceuticals – – Chondroitin sulfate Glucosamine Hyaluronic acid Building blocks for cartilage and synovial fluid Examples: (oral) Synovi, Glycoflex (injectable) Adequan Can be mixed with many other ingredients (MSM, Creatine) to enhance effects.
Antibiotic Analogy to understand pain control n n n Antibiotics prescribed based on clinical signs, not always based on culture and sensitivity Rely on return to normal function to confirm diagnosis If doesn’t help, add to or change drug protocol May need a loading dose May need a combination of drugs

Questions? ?
 Boundaries meme
Boundaries meme Pictures
Pictures Ject throw
Ject throw Factors that helped spread christianity
Factors that helped spread christianity Https//a-z-animals.com/animals
Https//a-z-animals.com/animals Consumer decomposer producer
Consumer decomposer producer Animals that eat both plants and animals
Animals that eat both plants and animals Animals that eat both plants and animals
Animals that eat both plants and animals Dont ask
Dont ask Why should i be discouraged
Why should i be discouraged Teaching bd
Teaching bd Where has everyone gone, leaving janie alone?
Where has everyone gone, leaving janie alone? Priveleges and immunities clause
Priveleges and immunities clause In the time of the butterflies chapter 10 quotes
In the time of the butterflies chapter 10 quotes The veldt questions and answers
The veldt questions and answers Why do you feel proud of mt everest and gautam buddha
Why do you feel proud of mt everest and gautam buddha Percy jackson
Percy jackson Why does joe think that janie is being ungrateful?
Why does joe think that janie is being ungrateful? Poe is a master at creating an eerie
Poe is a master at creating an eerie Madpain
Madpain What is breast tenderness in pregnancy
What is breast tenderness in pregnancy Period cramps vs early pregnancy cramps
Period cramps vs early pregnancy cramps Why did orwell use animals instead of people
Why did orwell use animals instead of people Why do desert animals have longer loop of henle
Why do desert animals have longer loop of henle Why do desert animals have longer loop of henle
Why do desert animals have longer loop of henle Macromolecule with nitrogen
Macromolecule with nitrogen Figure of speech of poem animals class 10
Figure of speech of poem animals class 10 Why do animals need a nervous system
Why do animals need a nervous system Why are big predatory animals rare
Why are big predatory animals rare Science class five
Science class five Aleppo and jericho are located in
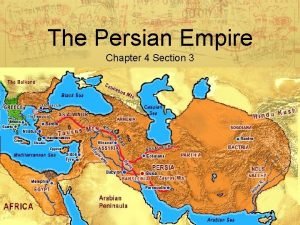
Aleppo and jericho are located in How did cyrus treat the people he conquered
How did cyrus treat the people he conquered Equation for number needed to treat
Equation for number needed to treat Invitation to treat
Invitation to treat What did juliet say she would rather do than marry paris
What did juliet say she would rather do than marry paris Which seedless plants have been used to treat bee stings
Which seedless plants have been used to treat bee stings Number needed to treat calculation
Number needed to treat calculation Offer
Offer How to treat laryngopharyngeal reflux
How to treat laryngopharyngeal reflux How to calculate number needed to treat
How to calculate number needed to treat Number needed to treat formula
Number needed to treat formula Numbers needed to treat
Numbers needed to treat Number needed to treat
Number needed to treat Invitation to treat
Invitation to treat Number needed to treat calculation
Number needed to treat calculation Mischief rule
Mischief rule Treat with sincerity
Treat with sincerity How does mercutio treat the nurse
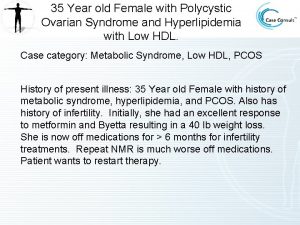
How does mercutio treat the nurse Is byetta used to treat pcos
Is byetta used to treat pcos Treat everyone with sincerity
Treat everyone with sincerity Social facilitation vs social loafing
Social facilitation vs social loafing Mole day treat ideas
Mole day treat ideas How to treat bursitis in the hip
How to treat bursitis in the hip Treat others the way you would like to be
Treat others the way you would like to be Treat with confidence
Treat with confidence St lucy's home raised by wolves characters
St lucy's home raised by wolves characters Fitz mayo
Fitz mayo Treat someone with contempt
Treat someone with contempt Epidydmis
Epidydmis Who put the blanket around scout's shoulders
Who put the blanket around scout's shoulders Intention to treat analysis
Intention to treat analysis Colours of halloween song
Colours of halloween song Who is mr. kirwin and how does he treat victor?
Who is mr. kirwin and how does he treat victor? The eraser game
The eraser game Treat the earth well
Treat the earth well Treat the earth well quote
Treat the earth well quote After realizing his own mistake the grasshopper felt
After realizing his own mistake the grasshopper felt