Pain relates to Chapter 9 Pain in the





- Slides: 67
Pain (relates to Chapter 9, “Pain, ” in the textbook)
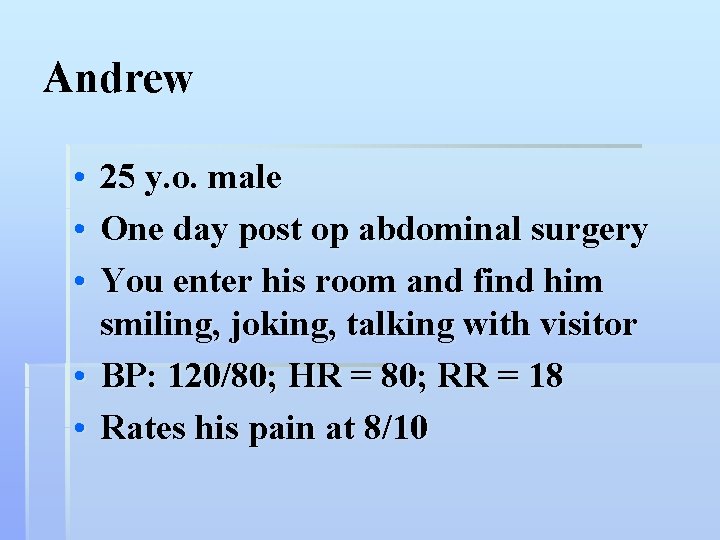
Andrew • 25 y. o. male • One day post op abdominal surgery • You enter his room and find him smiling, joking, talking with visitor • BP: 120/80; HR = 80; RR = 18 • Rates his pain at 8/10
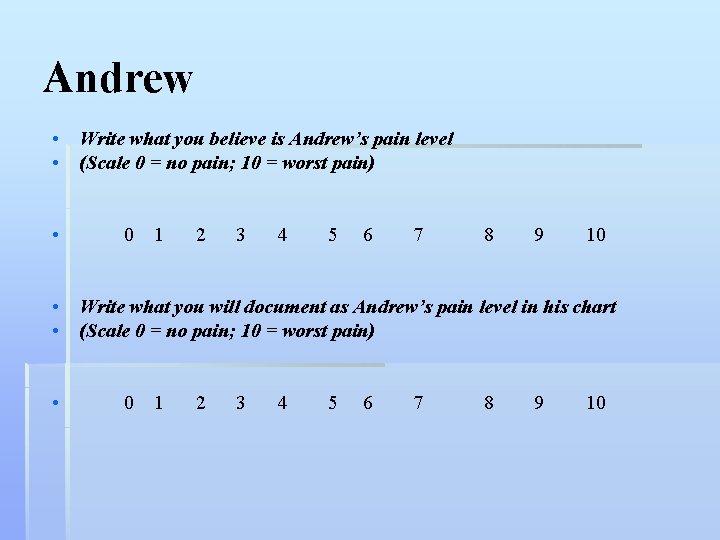
Andrew • Write what you believe is Andrew’s pain level • (Scale 0 = no pain; 10 = worst pain) • 0 1 2 3 4 5 6 7 8 9 10 • Write what you will document as Andrew’s pain level in his chart • (Scale 0 = no pain; 10 = worst pain) • 0 1 2 3 4 5 6 7 8 9 10
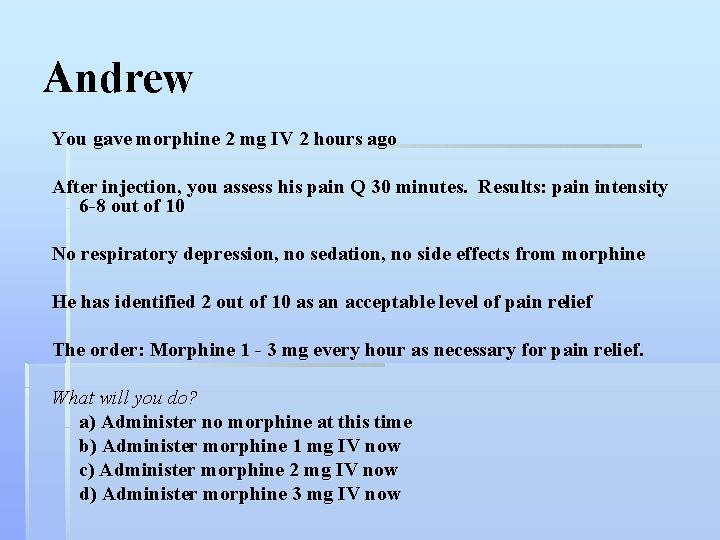
Andrew You gave morphine 2 mg IV 2 hours ago After injection, you assess his pain Q 30 minutes. Results: pain intensity 6 -8 out of 10 No respiratory depression, no sedation, no side effects from morphine He has identified 2 out of 10 as an acceptable level of pain relief The order: Morphine 1 - 3 mg every hour as necessary for pain relief. What will you do? a) Administer no morphine at this time b) Administer morphine 1 mg IV now c) Administer morphine 2 mg IV now d) Administer morphine 3 mg IV now
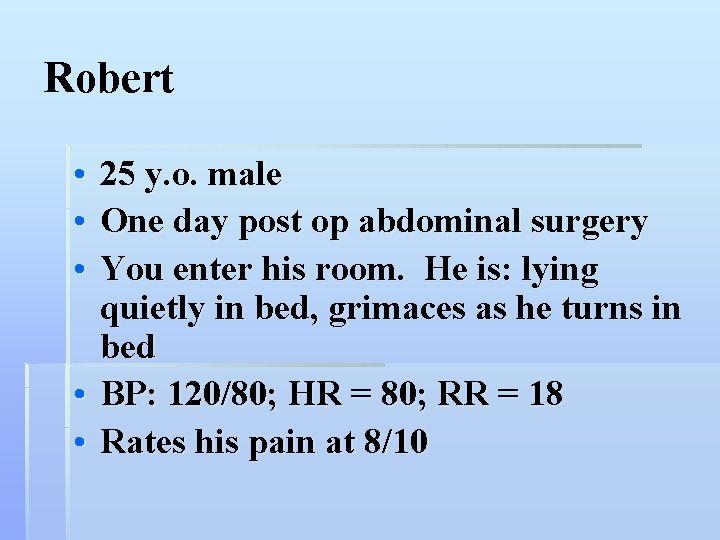
Robert • • • 25 y. o. male One day post op abdominal surgery You enter his room. He is: lying quietly in bed, grimaces as he turns in bed • BP: 120/80; HR = 80; RR = 18 • Rates his pain at 8/10
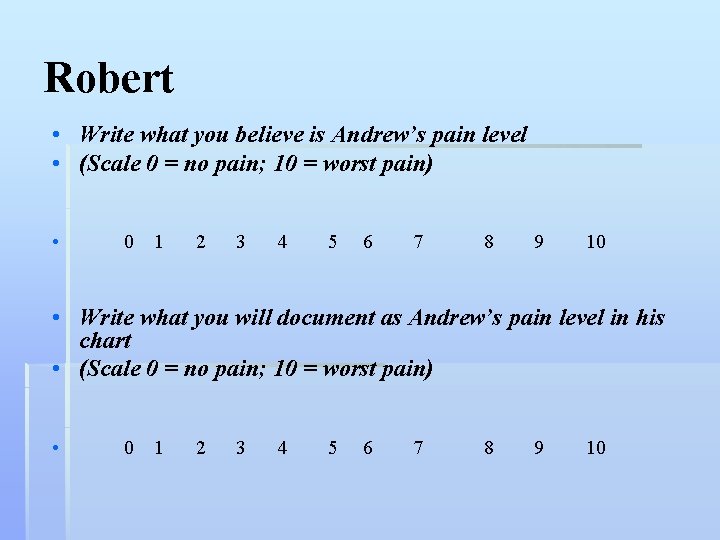
Robert • Write what you believe is Andrew’s pain level • (Scale 0 = no pain; 10 = worst pain) • 0 1 2 3 4 5 6 7 8 9 10 • Write what you will document as Andrew’s pain level in his chart • (Scale 0 = no pain; 10 = worst pain) • 0 1 2 3 4 5 6 7 8 9 10
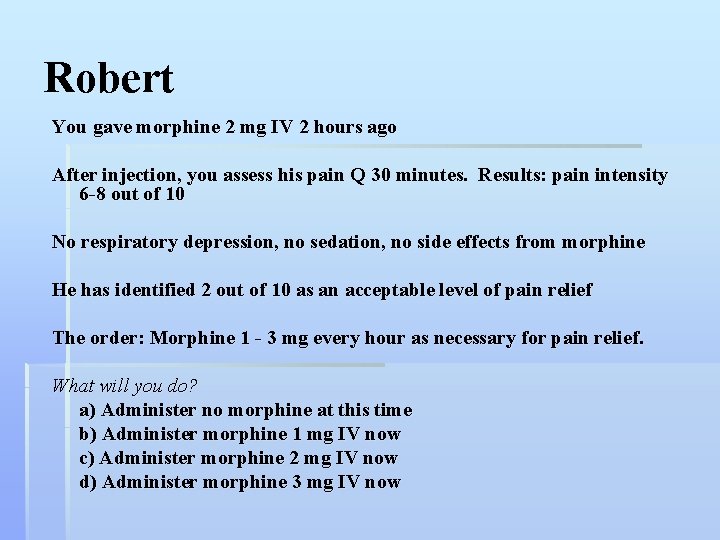
Robert You gave morphine 2 mg IV 2 hours ago After injection, you assess his pain Q 30 minutes. Results: pain intensity 6 -8 out of 10 No respiratory depression, no sedation, no side effects from morphine He has identified 2 out of 10 as an acceptable level of pain relief The order: Morphine 1 - 3 mg every hour as necessary for pain relief. What will you do? a) Administer no morphine at this time b) Administer morphine 1 mg IV now c) Administer morphine 2 mg IV now d) Administer morphine 3 mg IV now
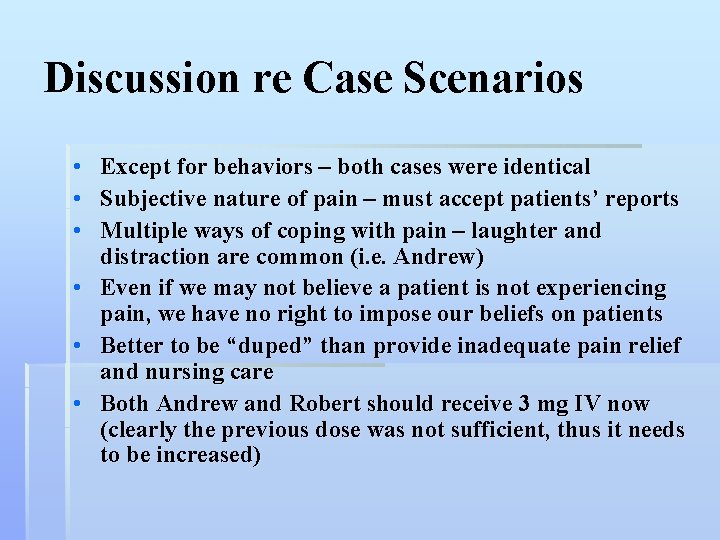
Discussion re Case Scenarios • Except for behaviors – both cases were identical • Subjective nature of pain – must accept patients’ reports • Multiple ways of coping with pain – laughter and distraction are common (i. e. Andrew) • Even if we may not believe a patient is not experiencing pain, we have no right to impose our beliefs on patients • Better to be “duped” than provide inadequate pain relief and nursing care • Both Andrew and Robert should receive 3 mg IV now (clearly the previous dose was not sufficient, thus it needs to be increased)
Discussion from Mc. Caffery • Clock watchers • Other “suspect” behaviors
Pain • Whatever the person experiencing the pain says it is, existing wherever the person says it does (Mc. Caffery) • An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage
Pain • A major reasons for seeking health care • Nurses have a central role in pain assessment and management
Pain • A subjective experience • Patient’s experience and self-report is essential • Self-report can be problematic when dealing with special populations • Nonverbal information such as behaviors can also aid the assessment of pain
Nursing Roles • Assessing pain and communicating this information to other health care providers • Ensuring the initiation of adequate pain relief measures • Evaluating the effectiveness of these interventions
Nociception • Nociception is the activation of the primary afferent nerves with peripheral terminals (free nerve endings) that respond differently to noxious (tissue-damaging) stimuli • Nociceptors function primarily to sense and transmit pain signals
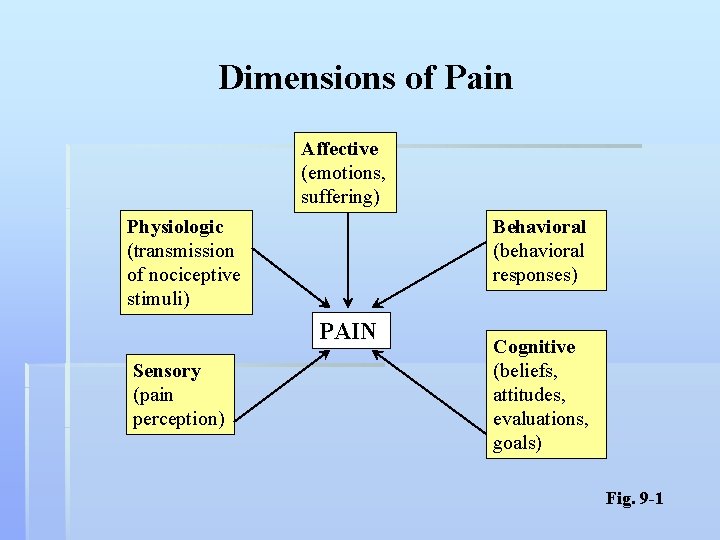
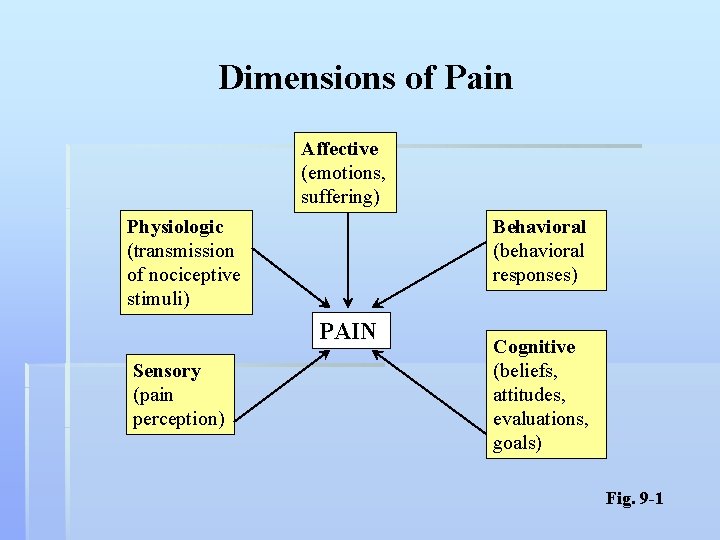
Dimensions of Pain Affective (emotions, suffering) Physiologic (transmission of nociceptive stimuli) Behavioral (behavioral responses) PAIN Sensory (pain perception) Cognitive (beliefs, attitudes, evaluations, goals) Fig. 9 -1
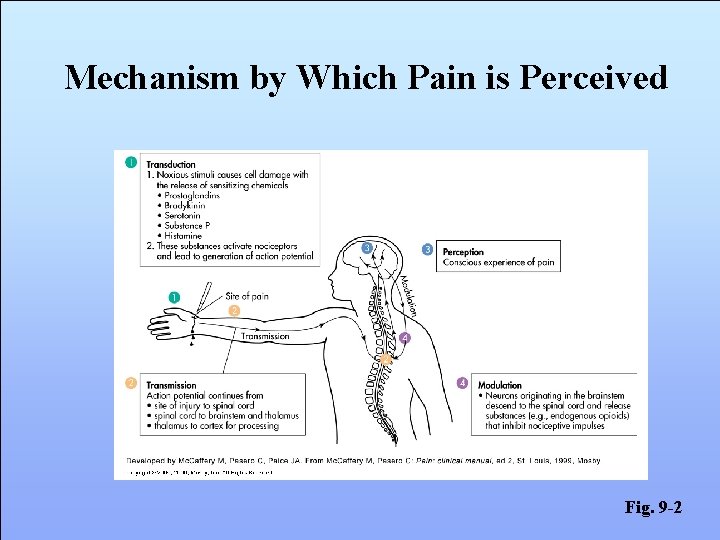
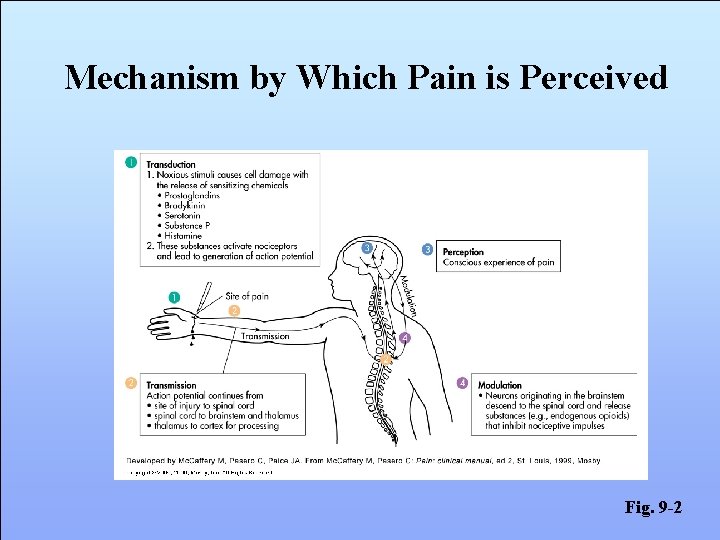
Mechanism by Which Pain is Perceived Fig. 9 -2
Medications Interrupt the Pathway • Transduction (e. g. , NSAIDS, local anesthetics) • Transmission (e. g. , opioids) • Perception (e. g. , opioids, adjuvants, NSAIDS) • Modulation (e. g. , tricyclic antidepressants)
Classification of Pain • Acute • Chronic
Acute Pain • Sudden onset • < 3 months or as long as it takes for normal healing to occur • Mild-to-severe pain • Generally can identify a precipitating event or illness (e. g. , surgery)
Acute Pain • Course of pain ↓ over time and goes away as recovery occurs • Includes postoperative pain, labor pain, pain from trauma • Treatment includes analgesics for symptom control and treatment of the underlying cause
Acute Pain • Manifestations reflect sympathetic nervous system activation • ↑ heart rate • ↑ respiratory rate • ↑ blood pressure • Pain control with eventual elimination is treatment goal
Chronic Pain • Gradual or sudden onset • > 3 month duration; may start as acute injury or event but continues past the normal recovery time • May not know cause of pain
Chronic Pain • Typically pain does not go away; characterized by periods of waxing and waning • Mostly behavioral manifestations • ↓ physical movement/activity • Fatigue • Withdrawal from others and social interaction
Chronic Pain • Can be disabling and is often accompanied by anxiety and depression • Treatment goals • Pain control to the extent possible • Focus on enhancing function and quality of life
Assessment of Pain: PQRST P = Provoking/Palliating factors • What precipitates/provokes the pain? What makes it worse? • What makes it better (palliates)? Q = Quality • What does it feel like? Ask open-end questions. R = Region/radiation • Where is the pain? Does it travel or radiate?
Assessment of Pain: PQRST S = Severity • VAS (Visual analogue scale) • Numerical scale (0 - 5; 0 - 10) • Descriptive scale (no pain, mild, moderate, severe, very severe, worst possible) • FACES pain rating scale - for children, non-verbal, language barriers T = Time/temporal factors • When did it begin? How long does it last? When does it occur? Does it come and go? Is it constant?
Assessing Pain in Cognitively Impaired/Non-verbal Adults • Self-report whenever possible: Often can use numerical scales if taught 0 - 5 scale may be easier Faces scale - 6 different facial images
Assessing Pain in Cognitively Impaired/Non-verbal Adults • Alternatives to self-report (from most to least useful) • Pathologic conditions or procedures known to cause discomfort • Behaviors • Facial expressions (frown, grimace, contract muscles around mouth/eyes) • physical movements (restless, fidget, resists movement, guarding, combativeness, hostile behavior) • Vocalizations (moan, groan, crying) • Proxy pain rating (family, friends, clinician) - only a guess • Physiological Measures (e. g. , HR, RR, BP- elevated) least helpful
Points to Remember: Special Considerations • Prevalence of pain increases with age • Pain is most under-treated among elderly • No reason to believe that age or cognitive impairment dulls sensitivity to pain • Make sure patient can see/use assessment tool (glasses, hearing aid, teach)
Factors affecting expression of pain • Age • pain wrongly accepted as part of aging • sign of weakness • don’t want to bother nurse • Gender • pain experience/perception may be different between genders • belief that men should be more stoic • Cultural Influences • Cause of pain (fate, lifestyle, punishment, witchcraft) • Emotional response and expression • Meaning of pain • Reports of intensity • How it should be treated/who treats it
Why People Deny Pain • Fear of Addiction • Discuss this common fear • Emphasize rarity of addiction when opioids used for pain (< 1%) • Fear of Developing Tolerance • Fear analgesic might not work when really needed • Emphasize can increase dose
Why People Deny Pain • Fear of Side Effects • Teach can treat and/or prevent these • Desire to be good patient/non-complainer • Explain importance of pain relief in preventing complications • Fear of Showing Weakness • Explain importance of pain relief for quality of life, maintaining control of life
Indicators of Denial of Pain • Known painful condition/procedure • Pain behaviors (grimacing, guarding, etc. ) • Family/friends suspect pain • If denial suspected • Identify concerns and discuss • Ultimately, must accept patient’s self-report
• Despite the prevalence of pain, many studies document inadequate pain management across care settings and patient populations
Consequences of Untreated Pain • Unnecessary suffering • Physical and psychosocial dysfunction • Impaired recovery from acute illness and surgery • Immuno-suppression • Sleep disturbances
Reasons for Under-Treatment of Pain • Inadequate professional knowledge • MDs under-prescribe; nurses under-administer • Fear of addiction by patients and practitioners • Lack of knowledge re difference between physical dependence, tolerance, addiction
Reasons for Under-Treatment of Pain • Inadequate assessment techniques • Inadequate use of assessment tools • Inadequate evaluation of effects of analgesia • Hesitance to believe self-reports • Lack of knowledge re cultural differences in pain expression • Pain management not a priority
Reasons for Under-Treatment of Pain • Inadequate Consumer knowledge • That most pain can be relieved • Fear of addiction/tolerance
Reasons for Under-Treatment of Pain • Communication Problems • Professionals • • Not a priority May not impress upon patients importance of achieving adequate pain control (reduces post-op complications, reduces hospital LOS, etc) • Consumers • Desire to be “good” patient; don’t want to “bother” nurse • Cultural variations in expression
Physical Dependence • May develop after using opioids for 1 -4 weeks or longer • If opioid stopped or antagonist is taken/given, withdrawal symptoms (mild -severe) occur • Yawning, chills, GI upset, tearing of eyes • May progress to muscle spasms, vomiting, diarrhea
Tolerance • May develop after using opioids for 1 -4 weeks or longer • Characterized by reduced effect of the opioid: • Reduced pain relief • Decrease in side effects, such as nausea, sedation, itching, or respiratory depression • Treat by increasing dose
Addiction • • • Psychological dependence Compulsive drug use Continued craving Opioids needed for other than pain relief An acquired disease of brain Rarely occurs when opioids used for pain relief • Of 24, 000 patients whose pain was treated with opioids, < 1% became addicted (7 of 24, 000 patients) • Fear of addiction is never a reason to withhold opioids from patients in pain
Pain Management and Substance Abusers • Discuss Mc. Caffery
Pain Treatment • All pain treatment is guided by the same underlying principles 1. The patient must always be believed 2. Every patient deserves adequate pain management 3. Set goals for comfort and function - e. g. , what pain rating would allow patient to do post-op recovery activities? - generally ratings > 3 -4 interferes with function
Pain Treatment 4. Prevent occurrence and recurrence - Predictable pain - give analgesic before - Pain around the clock (ATC) – analgesics ATC (wake patient for analgesic before the pain wakes patient) 4. All therapies must be evaluated to ensure they are meeting patient’s goals
Drug Therapy • • • Non-opioids Opioids Adjuvents Each works on pain in different ways (interrupt pathways in different points/ways), so can combine different types for maximal pain relief
Drug Therapy • See WHO Analgesic Ladder for management of pain (p. 142) • See Equi-analgesic chart (Mc. Caffery)
Non - Opioids Acetaminophen and NSAIDS • • General purpose analgesics Acute and chronic pain Especially for mild MS pain Also used in combination with adjuvants and opioids for moderate - severe pain • Have a ceiling effect - no more pain relief will be obtained beyond a certain dose
Non-Opioids • Acetaminophen (i. e. , Tylenol) • Analgesic action appears to be in CNS • Safest non-opioid for most patients, especially elderly • Does not increase bleeding time or cause ulcers • May cause hepatotoxicity (do not use in chronic liver disease or alcoholism) • Maximum daily dose: 4000 mg • Also an anti-pyretic (for fever) • Not an anti-inflammatory; not anti-platelet
Non-Opioids • NSAIDS • ASA/Aspirin, Ibuprofin/Motrin/Advil, Celebrex, Vioxx • Relieve pain at site of injury and act on CNS • Block prostaglandin production at site of injury • When NSAID doesn’t work: increase dose or try another type • NSAIDS are also • anti-inflammatory • anti-pyretics (for fever) • anti-platelet (prevent clotting)
Non- Opioids • NSAIDS • Common side effects • heartburn, GI ulceration, GI bleeding • risk of ulcers increases with increased dose • Increased bleeding time • Use cautiously in elderly - prone to GI problems, platelet dysfunction, renal problems
Opioids Two Categories • Morphine like (mu agonists) - largest group** • Agonist-antagonists
Opioids: Mu agonists • Examples: morphine, demerol, darvon • Bind to/activates mu opiod receptor sites in spinal cord, preventing transmission of pain impulses • Mainstay of acute and cancer pain treatment • No ceiling on dose (increasing does increases effect; no maximum dose); can increase dose until desired effect obtained or side effects are unacceptable/unmanageable • Relieves all types of pain • Routes: oral, IM (not recommended b/c unreliable absorption and painful), IV, rectal, topical
Opioids: Mu agonists • Side effects: • • • N&V Constipation (most common - prevent with laxatives) Itching Drowsiness Respiratory depression (generally not a problem if dosing is correct) • Monitor respiratory status • Most at risk are opioid naive • Naloxone (narcan) to revers effects of narcotics • Sedation/drowsiness (safety precautions very impt) • precedes resp depression, so can serve as a warning • See Mc. Caffery, Pg 18
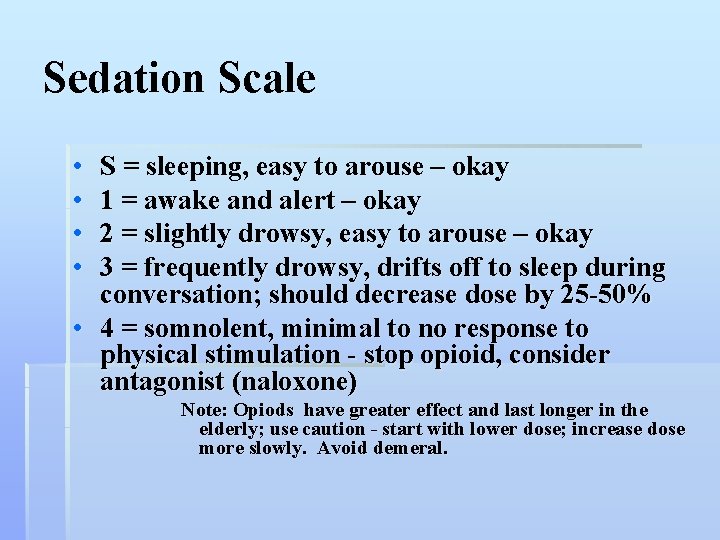
Sedation Scale • • S = sleeping, easy to arouse – okay 1 = awake and alert – okay 2 = slightly drowsy, easy to arouse – okay 3 = frequently drowsy, drifts off to sleep during conversation; should decrease dose by 25 -50% • 4 = somnolent, minimal to no response to physical stimulation - stop opioid, consider antagonist (naloxone) Note: Opiods have greater effect and last longer in the elderly; use caution - start with lower dose; increase dose more slowly. Avoid demeral.
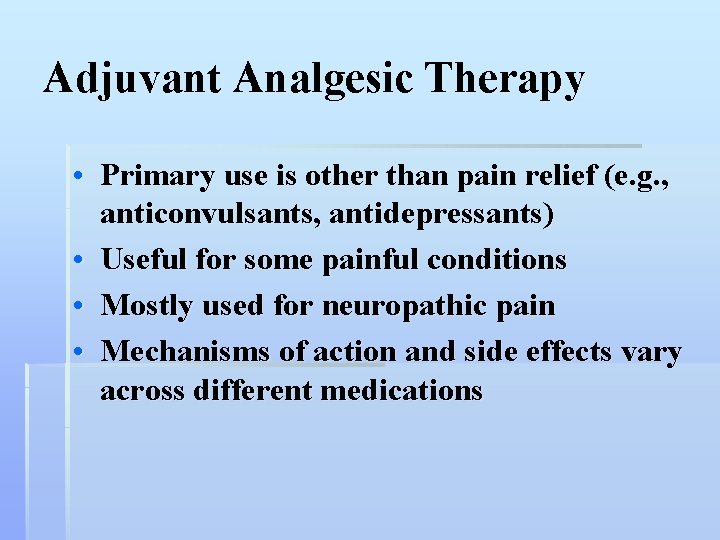
Adjuvant Analgesic Therapy • Primary use is other than pain relief (e. g. , anticonvulsants, antidepressants) • Useful for some painful conditions • Mostly used for neuropathic pain • Mechanisms of action and side effects vary across different medications
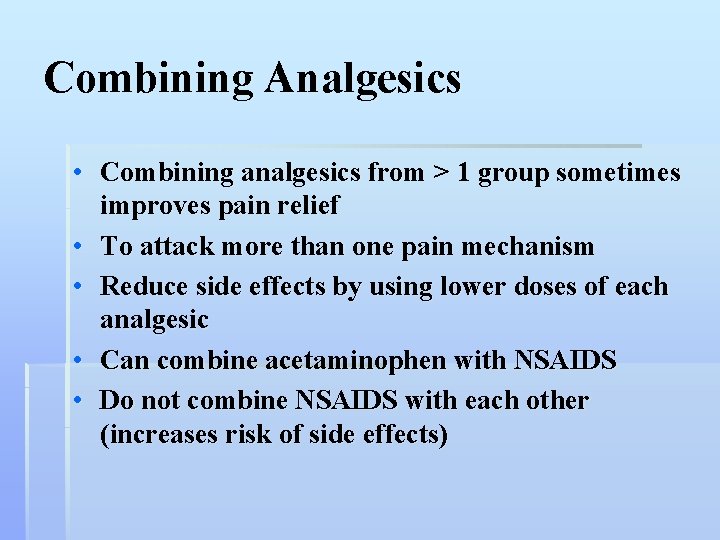
Combining Analgesics • Combining analgesics from > 1 group sometimes improves pain relief • To attack more than one pain mechanism • Reduce side effects by using lower doses of each analgesic • Can combine acetaminophen with NSAIDS • Do not combine NSAIDS with each other (increases risk of side effects)
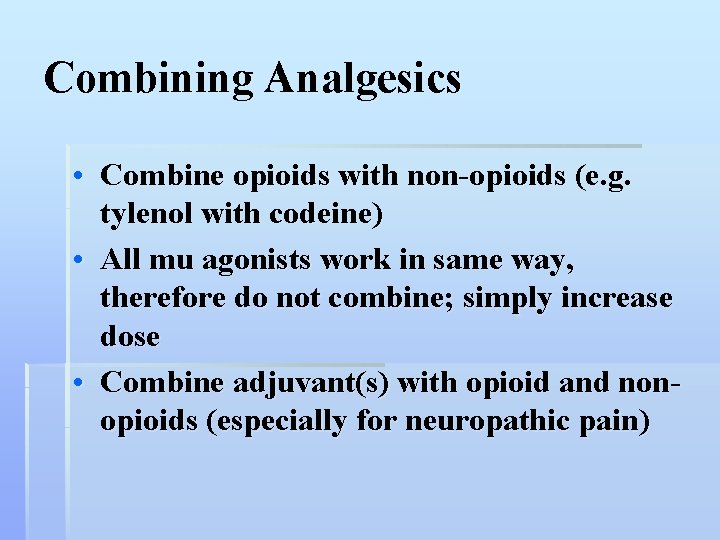
Combining Analgesics • Combine opioids with non-opioids (e. g. tylenol with codeine) • All mu agonists work in same way, therefore do not combine; simply increase dose • Combine adjuvant(s) with opioid and nonopioids (especially for neuropathic pain)
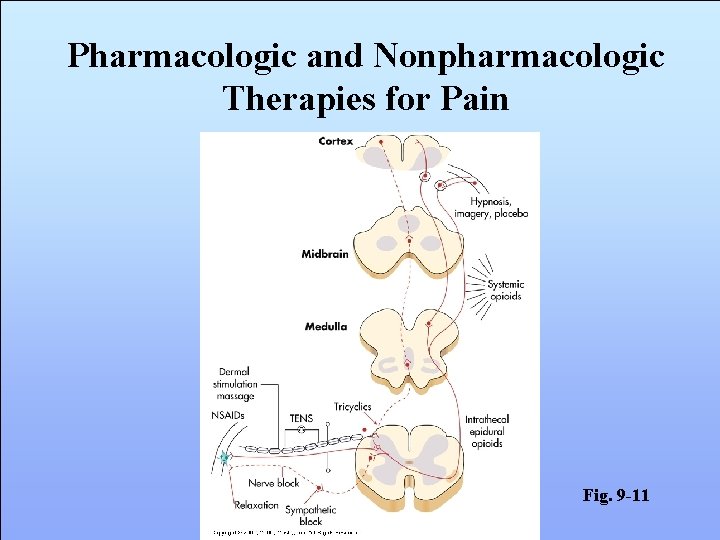
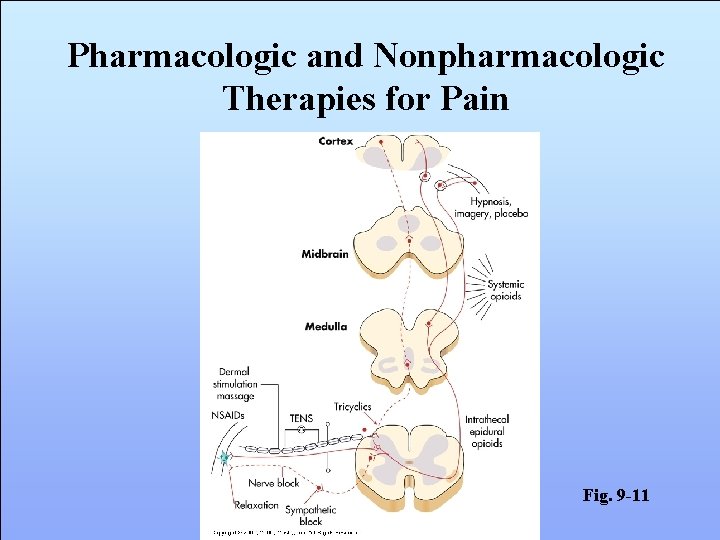
Pharmacologic and Nonpharmacologic Therapies for Pain Fig. 9 -11

Surgical Therapies • Performed for severe pain that is unresponsive to all otherapies • Nerve blocks • Used to reduce pain by interrupting transmission of nociceptive input • Neural blockade with local anesthetics is sometimes used for peri-operative pain • For intractable chronic pain when conservative therapies fail

Nonpharmacologic Therapy • Can reduce the dose of an analgesic required to control pain and thereby minimize side effects of drug therapy • Some strategies are believed to alter ascending nociceptive input or stimulate descending pain modulation mechanisms
Nonpharmacologic Therapy • Physical pain relief strategies • Acupuncture • Application of heat and cold • Exercise • Massage • Percutaneous electrical nerve stimulation (PENS)

Nonpharmacologic Therapy • Physical pain relief strategies (cont. ) • Transcutaneous electrical nerve stimulation (TENS) • Vibration

Nonpharmacologic Therapy • Cognitive therapies • Distraction • Hypnosis • Imagery • Relaxation
Placebos • Any medication that produces an effect b/c of its implicit/explicit intent and not b/c of its physical or chemical properties (e. g. , sugar pills, saline injections) • What does it mean when relief is obtained from placebos? • Are placebos ethical? (College of Nurses)

Nursing Diagnoses – Pain • • Activity intolerance Acute pain Anxiety Chronic pain Constipation Disturbed sleep pattern Disturbed thought process
Nursing Diagnoses – Pain • • Fatigue Fear Hopelessness Ineffective coping Ineffective role performance Powerlessness Social isolation