NPASS and the journey to improved documentation Team
- Slides: 9
NPASS and the journey to improved documentation Team Members: Elaine Trulis, RN, BSN – NICU Manager NICU Nursing Staff Patricia Hummel, RNC, MS, APN-NNP/PNP Marilyn Wager, RN, BS – Utilization Review Marianne Chybik, RNC, MSN – NICU Case Manager Marc Weiss, MD – NICU Medical Director
Opportunity Statement Inconsistency and lack of standardization of pain assessment in neonates – nationally a problem n Inconsistent documentation of pain scores with vital signs and after an intervention n Pain is considered the 5 th vital sign n
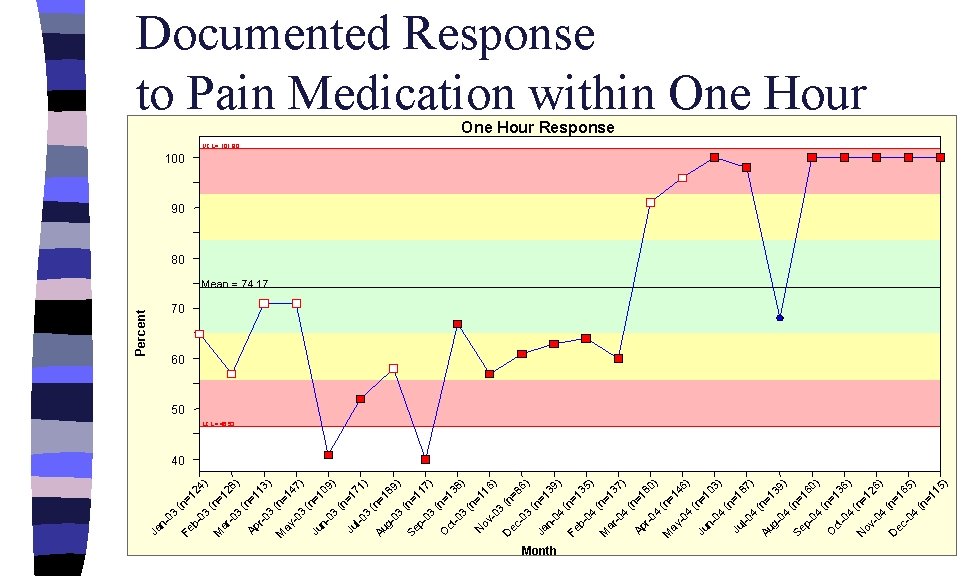
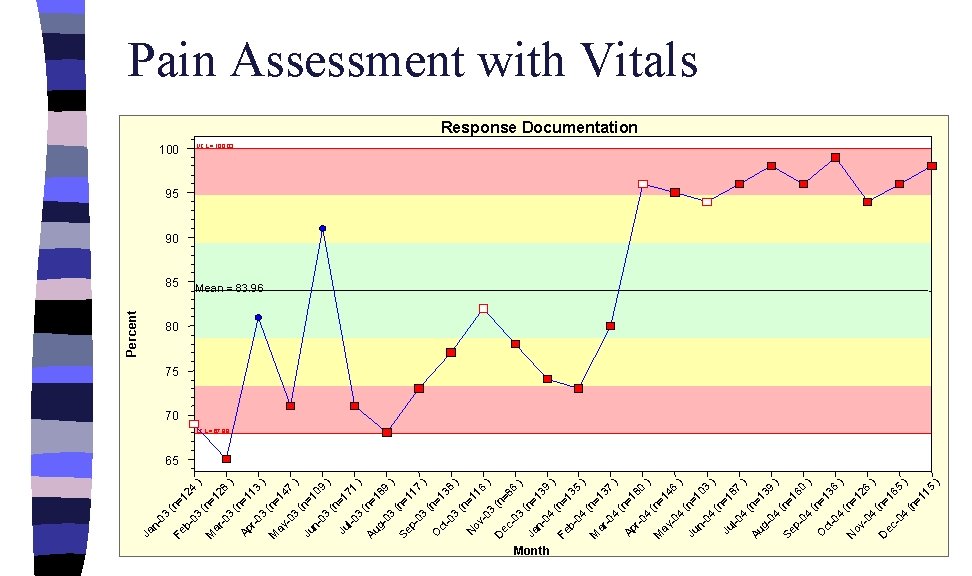
NICU QI Data n Pain Assessment with Vital Signs n Documented response to Pain Medication within One Hour n Data reflects scores given using the Neonatal Pain, Agitation and Sedation Scale
Most Likely Causes Identified n Lack of a standard pain assessment tool for neonates n Lack of familiarity with pain assessment tools n Flow sheet without a column for pain documentation
Solutions Implemented n n n NPASS© tool developed, validity and reliability testing completed NICU staff educated on use of the tool Patient care flow sheet revised to include space for hourly pain documentation Audits conducted to monitor documentation Unit Pain Resource Nurses form a unit pain committee to facilitate education and use of the NPASS© tool
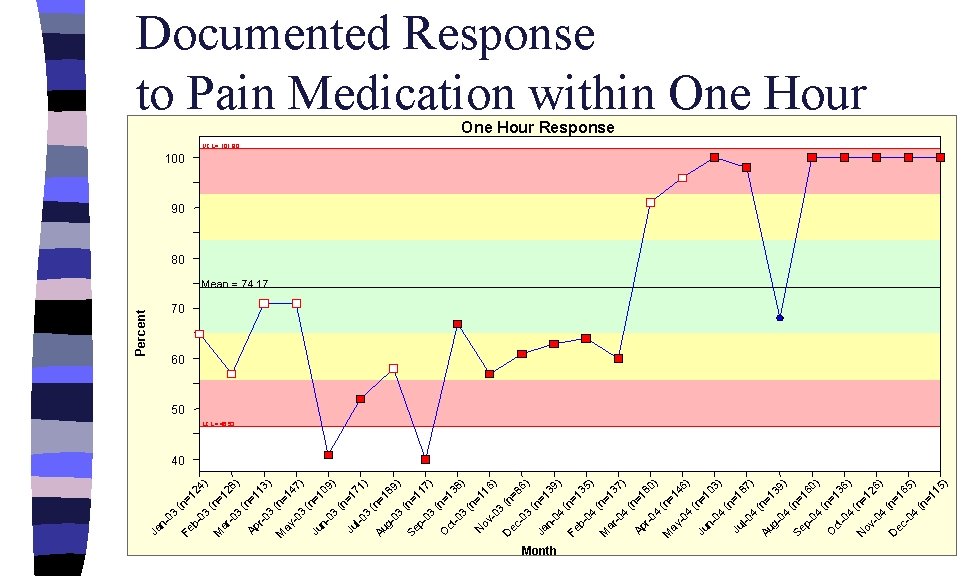
b 03 Fe (n =1 24 ) (n M =1 ar 28 -0 ) 3 (n Ap =1 13 r-0 ) 3 (n M =1 ay 47 -0 ) 3 (n Ju =1 n 09 03 ) (n =1 Ju 71 l-0 ) 3 (n Au =1 g 89 03 ) (n Se =1 p 17 03 ) (n O =1 ct 38 -0 ) 3 (n =1 N ov 16 -0 ) 3 ( D n= ec 86 -0 ) 3 (n Ja =1 n 39 04 ) ( n Fe =1 b 35 04 ) ( n M =1 ar 37 -0 ) 4 (n Ap =1 80 r-0 ) 4 (n M = ay 14 -0 6) 4 (n Ju =1 n 03 04 ) (n = Ju 18 l-0 7) 4 ( n Au =1 g 39 04 ) (n Se =1 p 60 04 ) (n O =1 ct 36 -0 ) 4 (n N = ov 12 -0 6) 4 ( n= D ec 16 -0 5) 4 (n =1 15 ) 03 n- Ja Percent Documented Response to Pain Medication within One Hour UCL = 101. 80 One Hour Response 100 90 80 Mean = 74. 17 70 60 50 LCL = 46. 53 40 Month
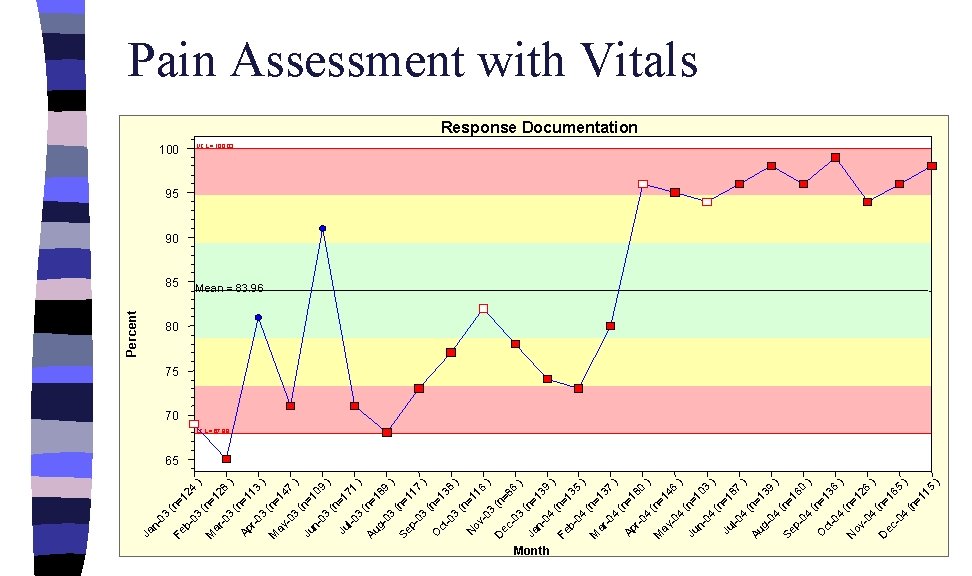
b 03 Fe (n =1 24 ) (n M =1 ar 28 -0 3 ) (n =1 Ap 13 r-0 3 ) (n M = ay 14 -0 7 3 ) ( n= Ju 10 n 9 03 ) (n =1 Ju 71 l-0 3 ) (n Au =1 g 89 03 ) (n Se =1 p 17 03 ) (n O =1 ct 38 -0 3 ) (n =1 N ov 16 -0 ) 3 (n D ec =8 -0 6 3 ) ( n= Ja 13 n 04 9 ) ( n= Fe 13 b 5 04 ) ( n= M 13 ar -0 7 4 ) (n Ap =1 80 r-0 4 ) (n M = ay 14 -0 6 4 ) ( n= Ju 10 n 3 04 ) (n =1 Ju 87 l-0 4 ) (n Au =1 g 39 04 ) (n Se =1 p 60 04 ) (n O =1 ct 36 -0 4 ) (n N = ov 12 -0 6 4 ) ( n= D ec 16 -0 5 4 ) (n =1 15 ) 03 n- Ja Percent Pain Assessment with Vitals 100 85 UCL = 100. 03 Response Documentation 95 90 Mean = 83. 96 80 75 70 LCL = 67. 89 65 Month
Results Pain scores are documented with all vital signs 99% of the time n Reassessment of pain after an intervention has improved from a low of 40% to 100% n n Staff is well versed on use of the NPASS© tool and includes a discussion of pain scores during multidisciplinary rounds and unit report
Next Steps Continue staff education n Expand use of the sedation score component of NPASS to assess individual patient response to opioids n Expand education and use of NPASS© tool to Respiratory Therapy staff n