Pain assessment management in frail older people withwithout


- Slides: 28
Pain assessment & management in frail older people with/without dementia Jo Hockley RN MSc Ph. D OBE Senior Research Fellow, Primary Palliative Care University of Edinburgh
Outline of my lecture Background on pain and older people in nursing care homes Remind us all of the BASICS of pain assessment What influences the pain threshold in older people Important aspects of pain assessment in older people With/without cognitive impairment Tools particularly used for people with advanced dementia
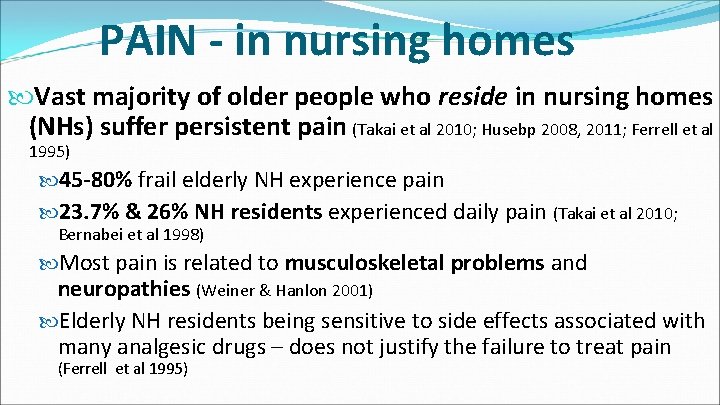
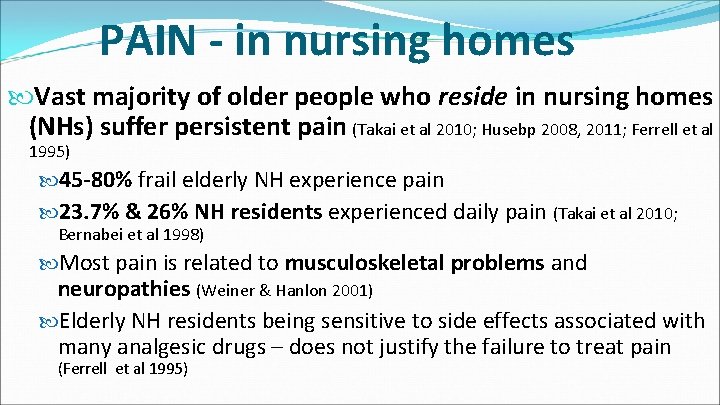
PAIN - in nursing homes Vast majority of older people who reside in nursing homes (NHs) suffer persistent pain (Takai et al 2010; Husebp 2008, 2011; Ferrell et al 1995) 45 -80% frail elderly NH experience pain 23. 7% & 26% NH residents experienced daily pain (Takai et al 2010; Bernabei et al 1998) Most pain is related to musculoskeletal problems and neuropathies (Weiner & Hanlon 2001) Elderly NH residents being sensitive to side effects associated with many analgesic drugs – does not justify the failure to treat pain (Ferrell et al 1995)
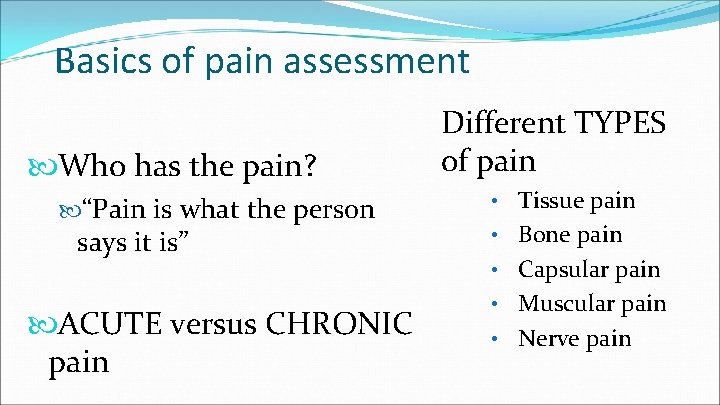
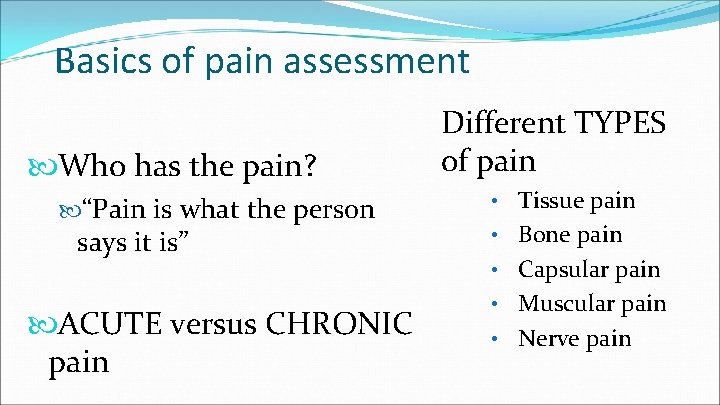
Basics of pain assessment Who has the pain? “Pain is what the person says it is” ACUTE versus CHRONIC pain Different TYPES of pain • Tissue pain • Bone pain • Capsular pain • Muscular pain • Nerve pain
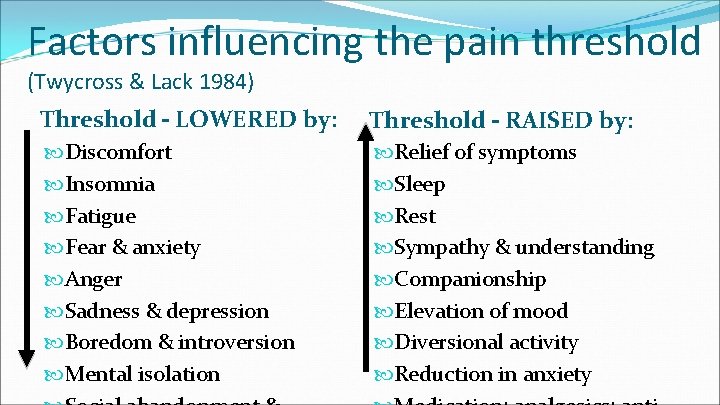
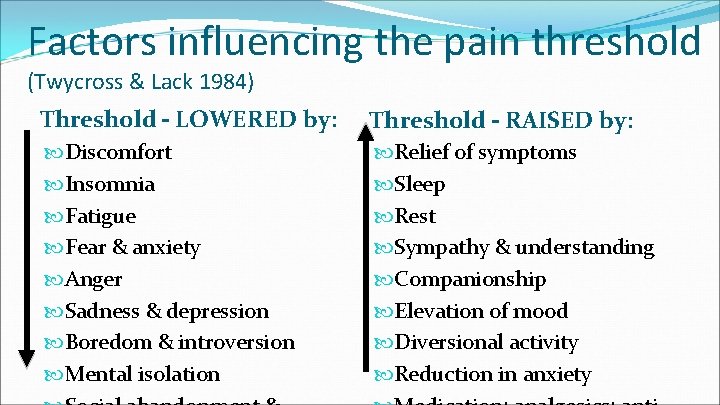
Factors influencing the pain threshold (Twycross & Lack 1984) Threshold – LOWERED by: Threshold – RAISED by: Discomfort Insomnia Fatigue Fear & anxiety Anger Sadness & depression Boredom & introversion Mental isolation Relief of symptoms Sleep Rest Sympathy & understanding Companionship Elevation of mood Diversional activity Reduction in anxiety
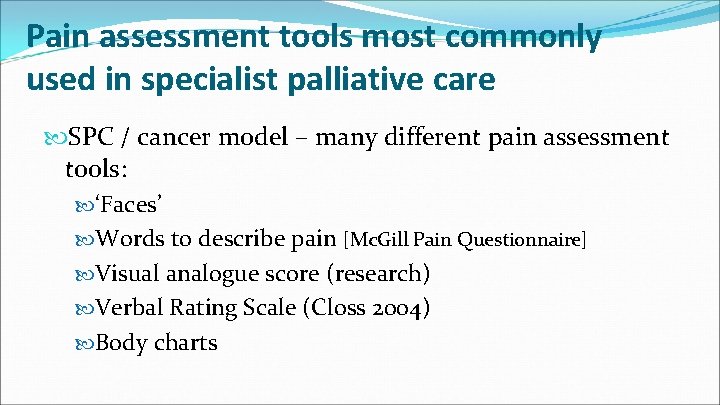
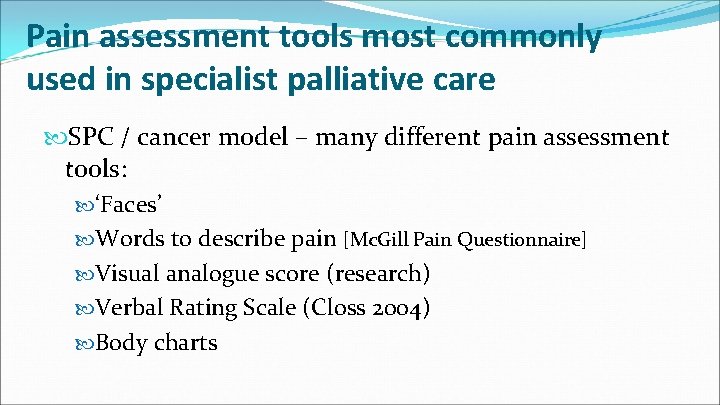
Pain assessment tools most commonly used in specialist palliative care SPC / cancer model – many different pain assessment tools: ‘Faces’ Words to describe pain [Mc. Gill Pain Questionnaire] Visual analogue score (research) Verbal Rating Scale (Closs 2004) Body charts
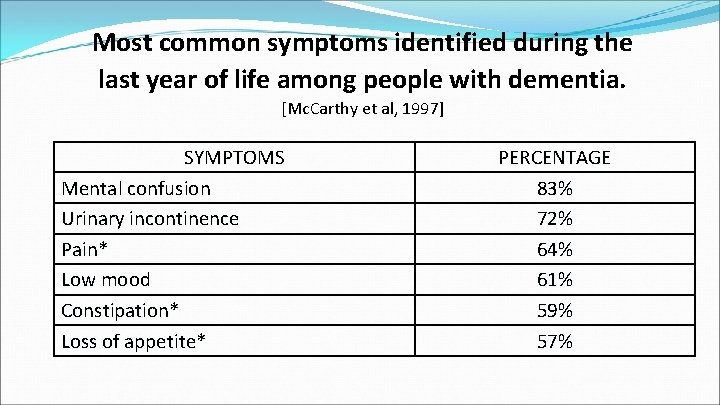
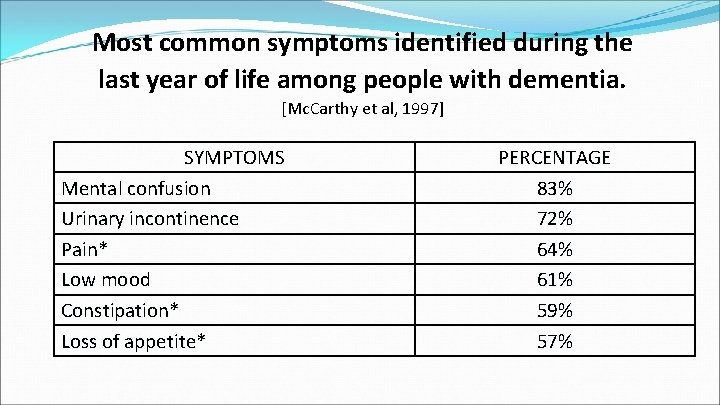
Most common symptoms identified during the last year of life among people with dementia. [Mc. Carthy et al, 1997] SYMPTOMS Mental confusion Urinary incontinence Pain* Low mood Constipation* Loss of appetite* PERCENTAGE 83% 72% 64% 61% 59% 57%
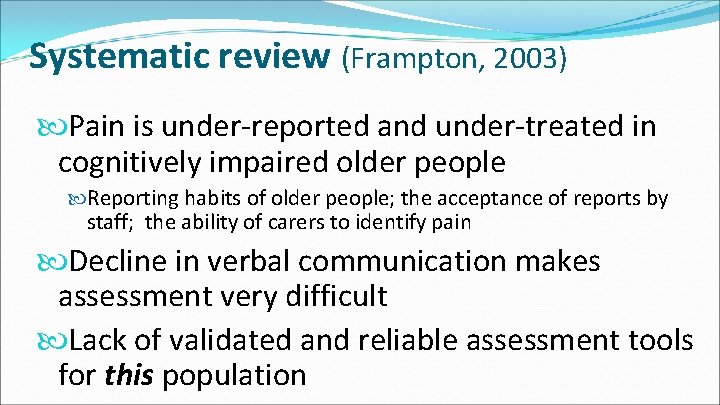
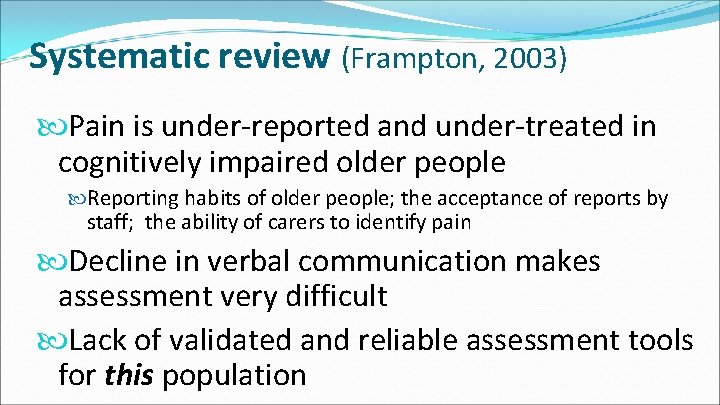
Systematic review (Frampton, 2003) Pain is under-reported and under-treated in cognitively impaired older people Reporting habits of older people; the acceptance of reports by staff; the ability of carers to identify pain Decline in verbal communication makes assessment very difficult Lack of validated and reliable assessment tools for this population
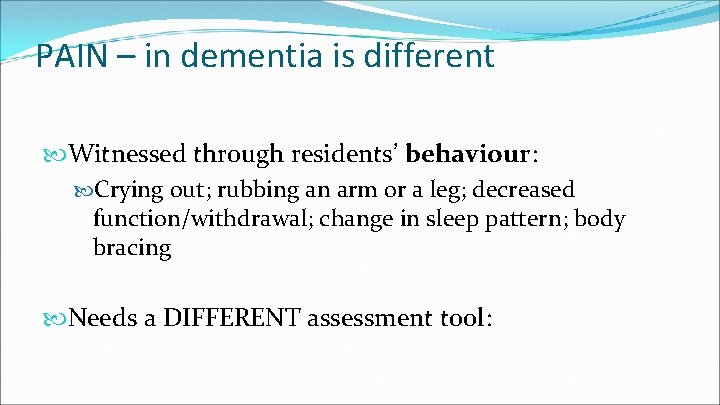
PAIN – in dementia is different Witnessed through residents’ behaviour: Crying out; rubbing an arm or a leg; decreased function/withdrawal; change in sleep pattern; body bracing Needs a DIFFERENT assessment tool:
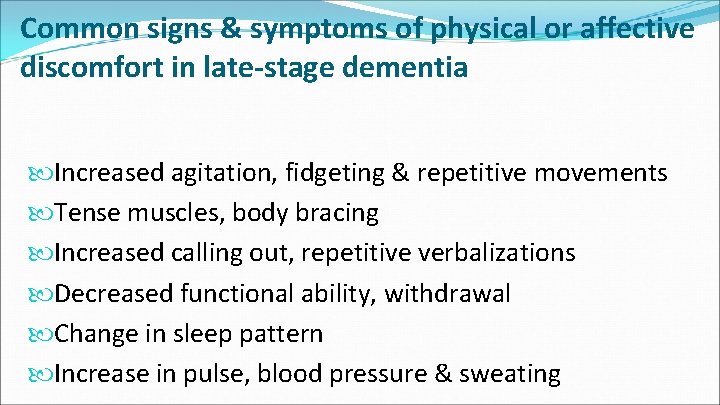
Common signs & symptoms of physical or affective discomfort in late-stage dementia Increased agitation, fidgeting & repetitive movements Tense muscles, body bracing Increased calling out, repetitive verbalizations Decreased functional ability, withdrawal Change in sleep pattern Increase in pulse, blood pressure & sweating
BEHAVOURAL ASSESSMENT TOOLS Verbal rating scale (Closs 2004) PAINAD (Volicer & Hurley 2015) DOLOPLUS 2 Scale (Lefebvre-Chapiro S. 2001) Abbey Scale (Abbey 2002) Dis. DAT - Disability Distress Assessment Tool (Regnard, 2003)
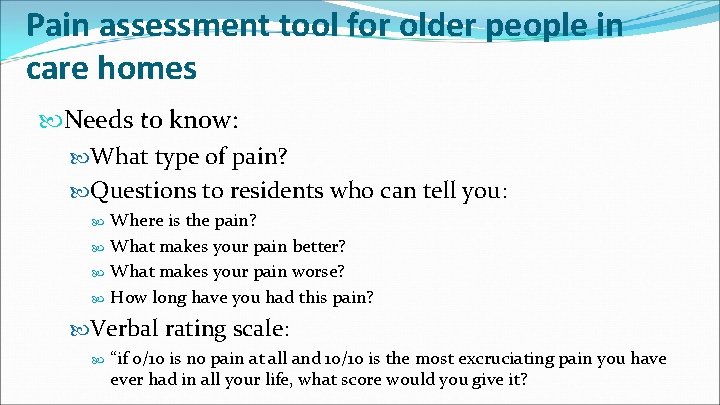
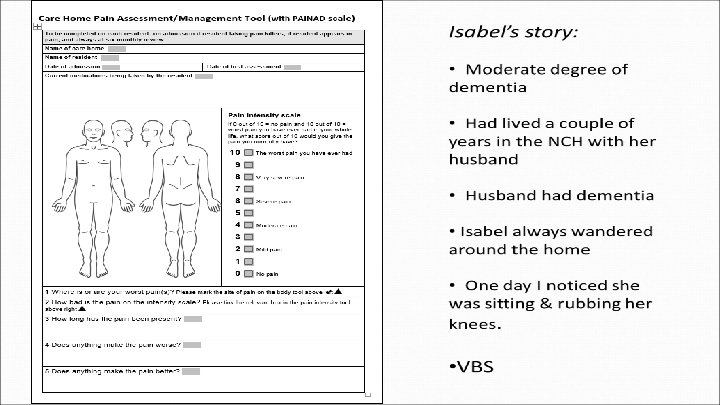
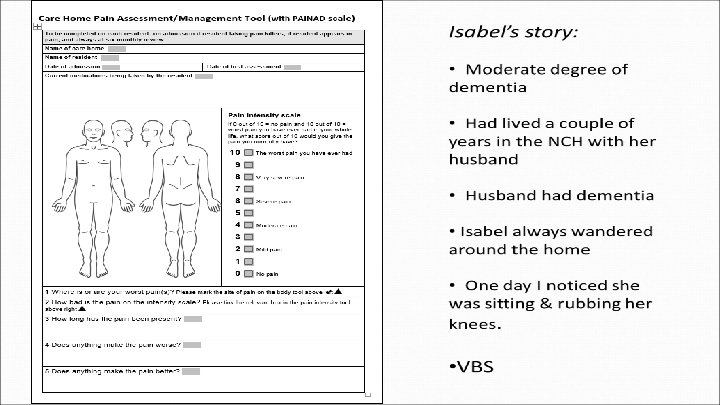
Pain assessment tool for older people in care homes Needs to know: What type of pain? Questions to residents who can tell you: Where is the pain? What makes your pain better? What makes your pain worse? How long have you had this pain? Verbal rating scale: “if 0/10 is no pain at all and 10/10 is the most excruciating pain you have ever had in all your life, what score would you give it?
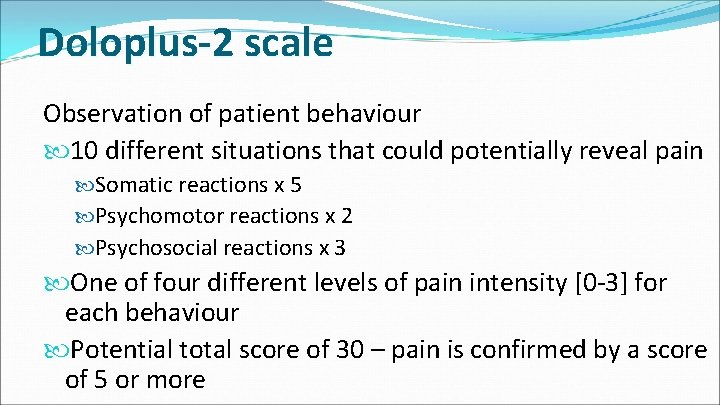
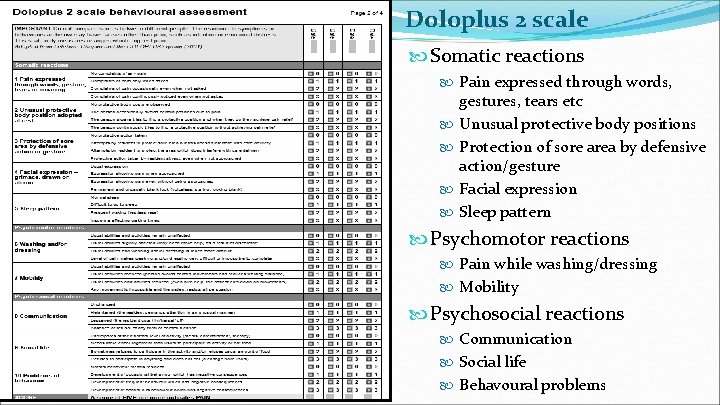
Doloplus-2 scale Observation of patient behaviour 10 different situations that could potentially reveal pain Somatic reactions x 5 Psychomotor reactions x 2 Psychosocial reactions x 3 One of four different levels of pain intensity [0 -3] for each behaviour Potential total score of 30 – pain is confirmed by a score of 5 or more
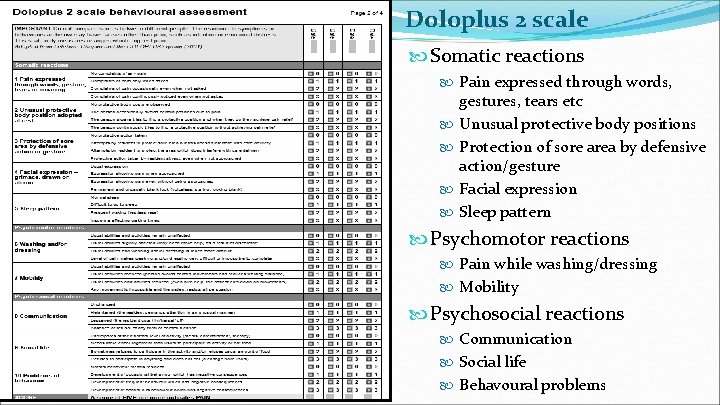
Doloplus 2 scale Somatic reactions Pain expressed through words, gestures, tears etc Unusual protective body positions Protection of sore area by defensive action/gesture Facial expression Sleep pattern Psychomotor reactions Pain while washing/dressing Mobility Psychosocial reactions Communication Social life Behavoural problems
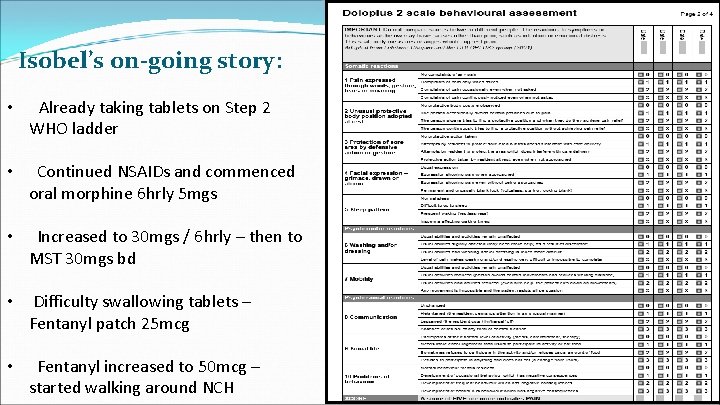
Isobel’s on-going story: • Already taking tablets on Step 2 WHO ladder • Continued NSAIDs and commenced oral morphine 6 hrly 5 mgs • Increased to 30 mgs / 6 hrly – then to MST 30 mgs bd • Difficulty swallowing tablets – Fentanyl patch 25 mcg • Fentanyl increased to 50 mcg – started walking around NCH
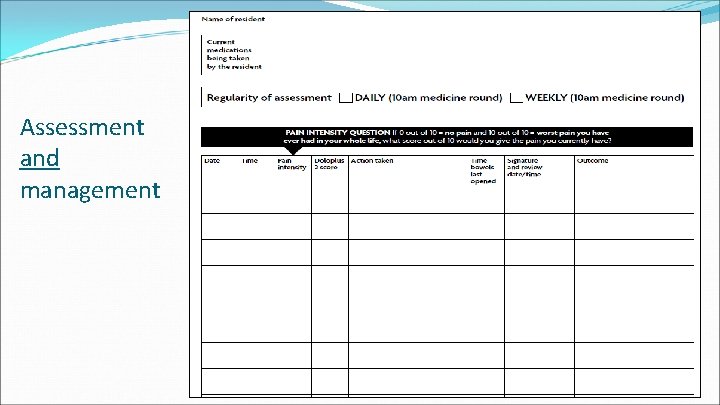
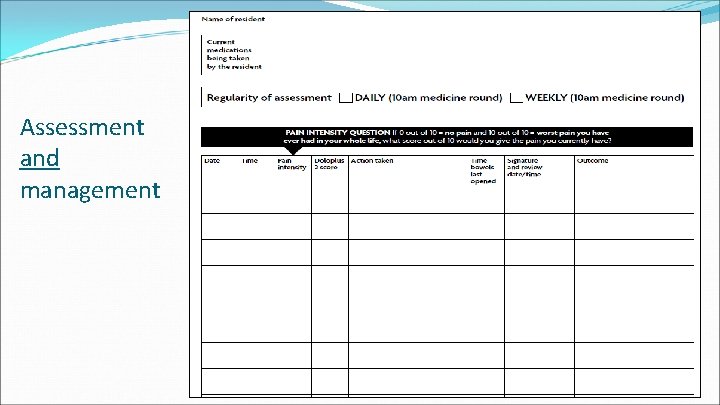
Assessment and management
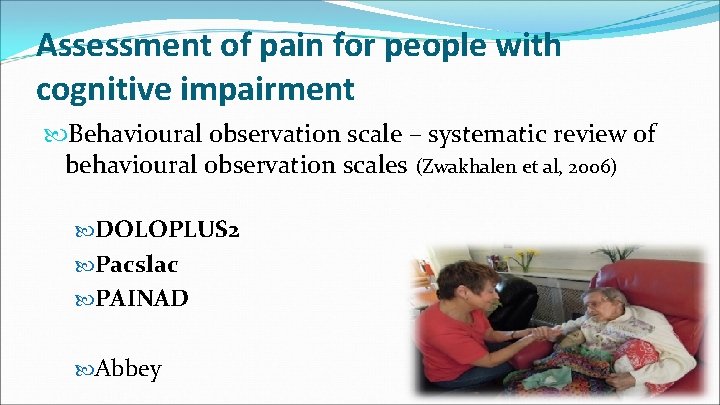
Assessment of pain for people with cognitive impairment Behavioural observation scale – systematic review of behavioural observation scales (Zwakhalen et al, 2006) DOLOPLUS 2 Pacslac PAINAD Abbey
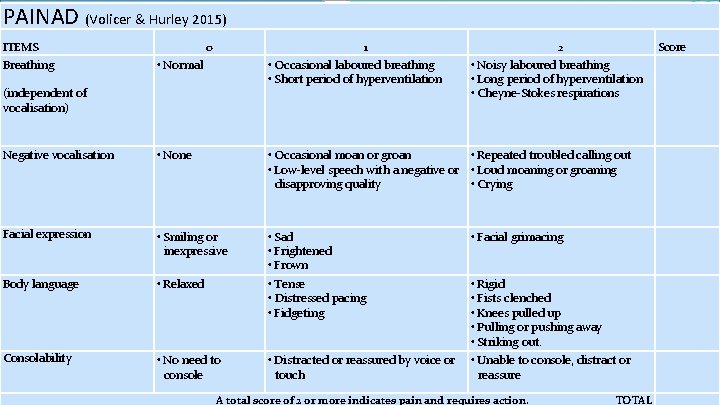
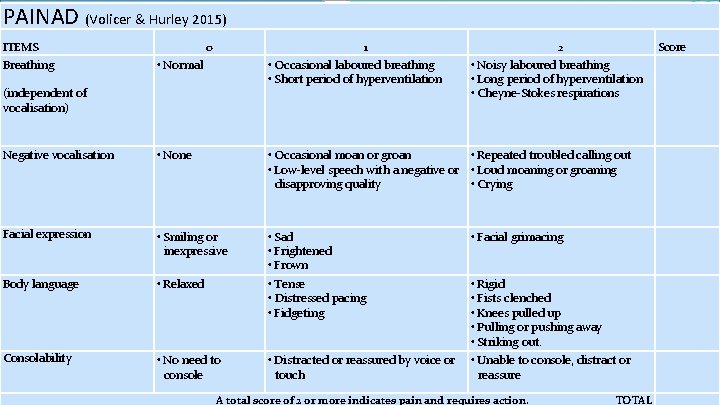
PAINAD (Volicer & Hurley 2015) ITEMS Breathing (independent of vocalisation) 0 1 • Occasional laboured breathing • Short period of hyperventilation • Normal 2 • Noisy laboured breathing • Long period of hyperventilation • Cheyne-Stokes respirations Score Negative vocalisation • None • Occasional moan or groan • Repeated troubled calling out • Low-level speech with a negative or • Loud moaning or groaning disapproving quality • Crying Facial expression • Smiling or inexpressive • Sad • Frightened • Frown • Facial grimacing Body language • Relaxed • Tense • Distressed pacing • Fidgeting • Rigid • Fists clenched • Knees pulled up • Pulling or pushing away • Striking out. Consolability • No need to console • Distracted or reassured by voice or touch • Unable to console, distract or reassure A total score of 2 or more indicates pain and requires action. TOTAL
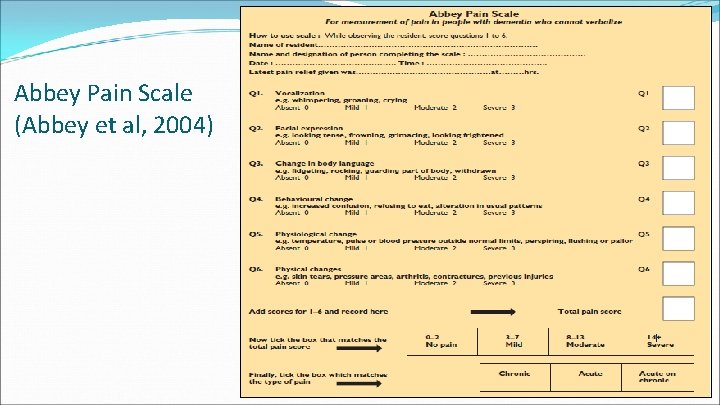
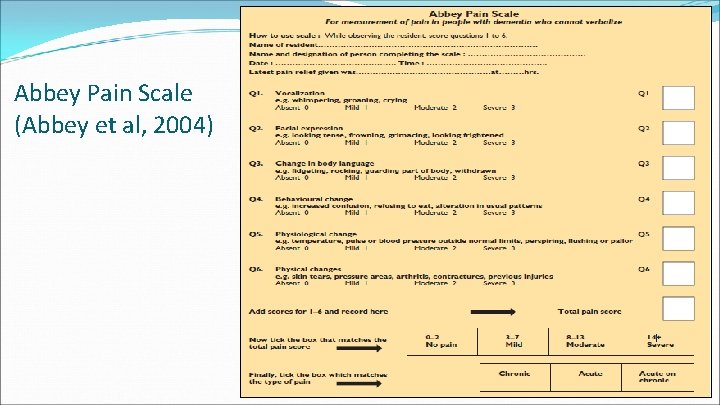
Abbey Pain Scale (Abbey et al, 2004)

Management of chronic pain in older people with dementia Start ‘low’ and ‘go slow’ Use the WHO analgesic ladder – especially Step 2 but remember that codeine is more nauseating than an opiate REGULAR analgesics + co-analgesics PLUS APERIENTS Softeners + pushers
Management of chronic pain in older people with dementia… contd/ Older people have a greater sensitivity to medication especially opiates/NSAIDs Start oral morphine at 2. 5 -5 mg/6 hrly Morphine is less nauseating than high dose codeine Collaborate with geriatrician – helps their knowledge and empowerment Use ‘long acting’ analgesics [ie MST or patches. Butrans/Transdec/Fentanyl patch] once pain control is properly assessed/titrated on quick release morphine NB Fentanyl patch 25 mcg is equivalent to Morphine 20 mgs/4 hrly
Rose’s story Very advanced dementia – used to like to have a doll to cuddle. I had known of her but never really chatted to her. Crying out – daughter arrived: o Arthritis since mid-20 s o Long term codeine / paracetamol medication regularly x 4 daily o Prescribed Quotiepine for ‘behavour’
‘We face a big challenge in end-of-life care of older people, not because of demographics, but due to ignorance and prejudice among practitioners and the general public, failing to apply evidence to develop best practice and failing to spread good practice. ’ (Philp, 2003: 153)

Thank you! Any questions? jo. hockley@ed. ac. uk
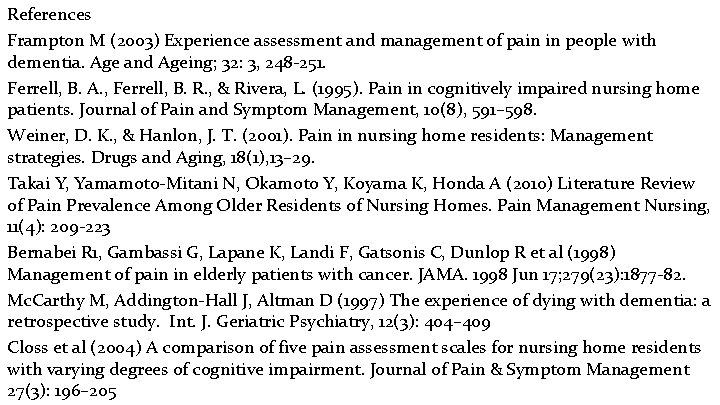
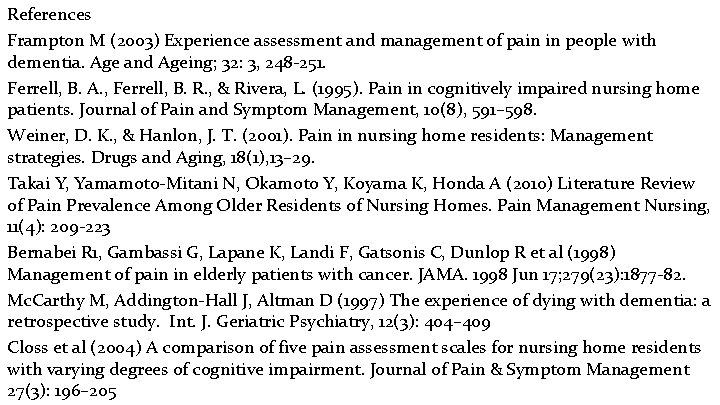
References Frampton M (2003) Experience assessment and management of pain in people with dementia. Age and Ageing; 32: 3, 248 -251. Ferrell, B. A. , Ferrell, B. R. , & Rivera, L. (1995). Pain in cognitively impaired nursing home patients. Journal of Pain and Symptom Management, 10(8), 591– 598. Weiner, D. K. , & Hanlon, J. T. (2001). Pain in nursing home residents: Management strategies. Drugs and Aging, 18(1), 13– 29. Takai Y, Yamamoto-Mitani N, Okamoto Y, Koyama K, Honda A (2010) Literature Review of Pain Prevalence Among Older Residents of Nursing Homes. Pain Management Nursing, 11(4): 209 -223 Bernabei R 1, Gambassi G, Lapane K, Landi F, Gatsonis C, Dunlop R et al (1998) Management of pain in elderly patients with cancer. JAMA. 1998 Jun 17; 279(23): 1877 -82. Mc. Carthy M, Addington-Hall J, Altman D (1997) The experience of dying with dementia: a retrospective study. Int. J. Geriatric Psychiatry, 12(3): 404– 409 Closs et al (2004) A comparison of five pain assessment scales for nursing home residents with varying degrees of cognitive impairment. Journal of Pain & Symptom Management 27(3): 196– 205
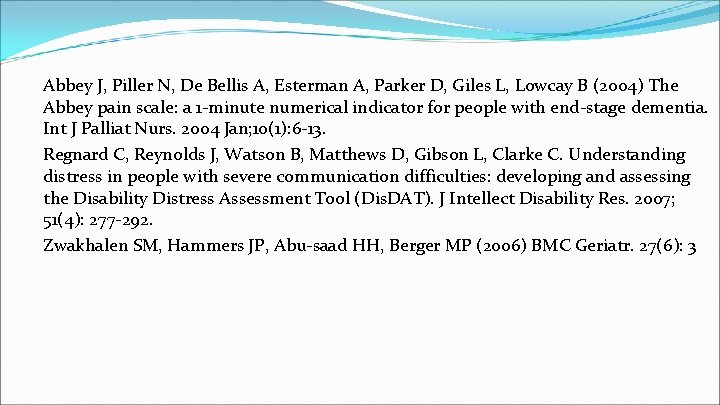
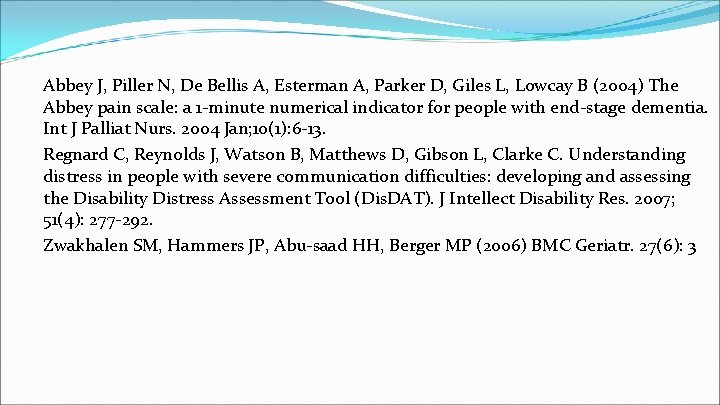
Abbey J, Piller N, De Bellis A, Esterman A, Parker D, Giles L, Lowcay B (2004) The Abbey pain scale: a 1 -minute numerical indicator for people with end-stage dementia. Int J Palliat Nurs. 2004 Jan; 10(1): 6 -13. Regnard C, Reynolds J, Watson B, Matthews D, Gibson L, Clarke C. Understanding distress in people with severe communication difficulties: developing and assessing the Disability Distress Assessment Tool (Dis. DAT). J Intellect Disability Res. 2007; 51(4): 277 -292. Zwakhalen SM, Hammers JP, Abu-saad HH, Berger MP (2006) BMC Geriatr. 27(6): 3
 Life is older older than the trees
Life is older older than the trees Epicran
Epicran Frail fract frag root words
Frail fract frag root words Cut grass lies frail
Cut grass lies frail Height he
Height he As people grow older
As people grow older Mad pain and martian pain
Mad pain and martian pain Breast pain in pregnancy
Breast pain in pregnancy Pms vs pregnancy
Pms vs pregnancy Pqrst pain assessment
Pqrst pain assessment Pqrst assessment
Pqrst assessment Pqrstu pain
Pqrstu pain Capa pain assessment tool
Capa pain assessment tool Wilda pain assessment
Wilda pain assessment Child pain scale
Child pain scale Comprehensive pain assessment
Comprehensive pain assessment Pqrst pain scale
Pqrst pain scale Pqrstu pain assessment
Pqrstu pain assessment What is pain
What is pain Jarvis chapter 11 pain assessment
Jarvis chapter 11 pain assessment Web accessibility for older users
Web accessibility for older users Tall strong younger sister
Tall strong younger sister Syncope in the older patient is
Syncope in the older patient is Td st annes
Td st annes Mental health and older adults
Mental health and older adults Dq98 form
Dq98 form Intellectual development in older adulthood
Intellectual development in older adulthood Older individuals who are blind program
Older individuals who are blind program Mental health and older adults
Mental health and older adults