Chest pain investigation diagnosis and treatment How to
![• Radiation (radiating to left arm, neck, jaw [ACS]; back [pancreatitis, aortic dissection]) • Radiation (radiating to left arm, neck, jaw [ACS]; back [pancreatitis, aortic dissection])](https://slidetodoc.com/presentation_image_h2/3c8fa8b4c305ad2a5f0cb3362d612ef9/image-26.jpg)
- Slides: 30
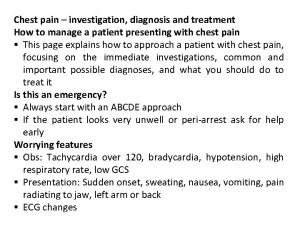
Chest pain – investigation, diagnosis and treatment How to manage a patient presenting with chest pain § This page explains how to approach a patient with chest pain, focusing on the immediate investigations, common and important possible diagnoses, and what you should do to treat it Is this an emergency? § Always start with an ABCDE approach § If the patient looks very unwell or peri-arrest ask for help early Worrying features § Obs: Tachycardia over 120, bradycardia, hypotension, high respiratory rate, low GCS § Presentation: Sudden onset, sweating, nausea, vomiting, pain radiating to jaw, left arm or back § ECG changes
Common Heart: Myocardial infarction or acute coronary syndromes (STEMI, NSTEMI, unstable angina), pericarditis Lungs: Pulmonary embolism, pneumonia, pneumothorax GI: Reflux and peptic ulcer disease Musculoskeletal (rule out others first) Uncommon but important Aortic dissection Cardiac tamponade Sickle-cell crisis
History • Presenting complaint: site of onset and radiation, quality (heavy, aching, sharp, tearing), intensity (scale of 1– 10), time of onset, duration, associated symptoms (sweating, nausea, palpitations, breathlessness), exacerbating or relieving factors (breathing, position, exertion, eating), recent trauma or exertion, similarity to previous episodes • Past medical history : cardiac or respiratory problems, diabetes, reflux • Drug history: cardiac or respiratory medications, antacids • Family history: IHD (esp under 60 years old), premature cardiac death • Social history: smoking, exercise tolerance
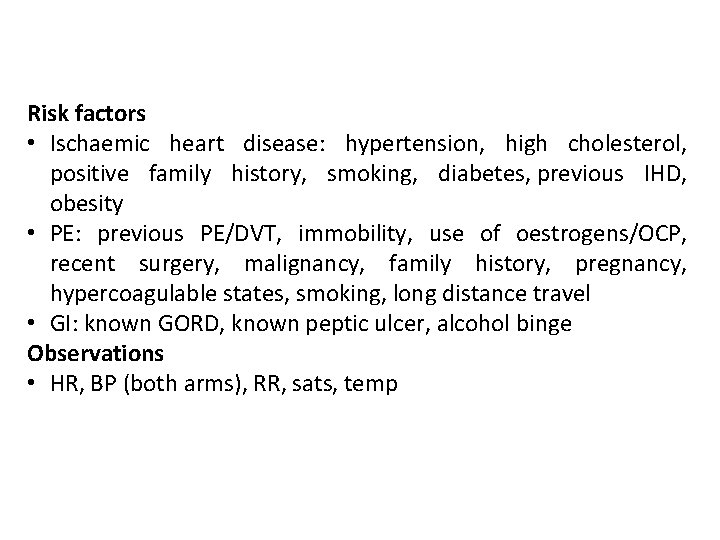
Risk factors • Ischaemic heart disease: hypertension, high cholesterol, positive family history, smoking, diabetes, previous IHD, obesity • PE: previous PE/DVT, immobility, use of oestrogens/OCP, recent surgery, malignancy, family history, pregnancy, hypercoagulable states, smoking, long distance travel • GI: known GORD, known peptic ulcer, alcohol binge Observations • HR, BP (both arms), RR, sats, temp
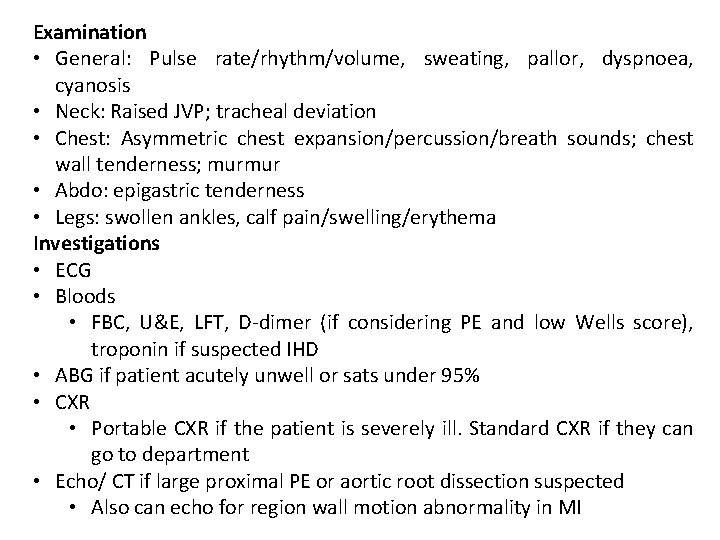
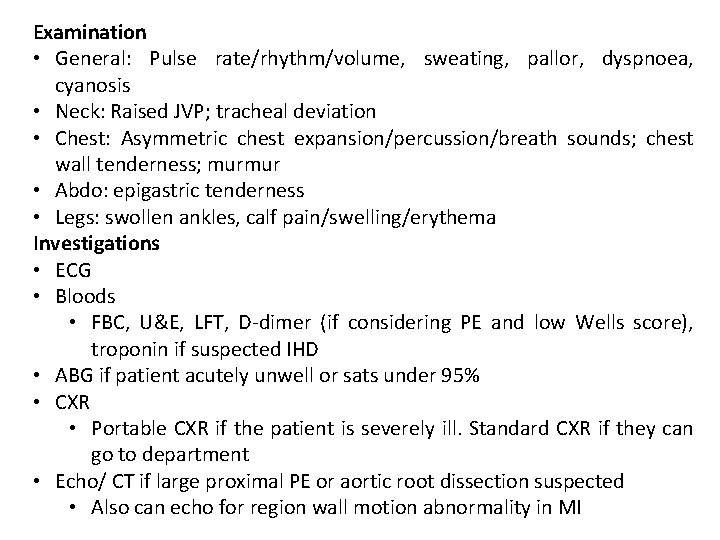
Examination • General: Pulse rate/rhythm/volume, sweating, pallor, dyspnoea, cyanosis • Neck: Raised JVP; tracheal deviation • Chest: Asymmetric chest expansion/percussion/breath sounds; chest wall tenderness; murmur • Abdo: epigastric tenderness • Legs: swollen ankles, calf pain/swelling/erythema Investigations • ECG • Bloods • FBC, U&E, LFT, D-dimer (if considering PE and low Wells score), troponin if suspected IHD • ABG if patient acutely unwell or sats under 95% • CXR • Portable CXR if the patient is severely ill. Standard CXR if they can go to department • Echo/ CT if large proximal PE or aortic root dissection suspected • Also can echo for region wall motion abnormality in MI
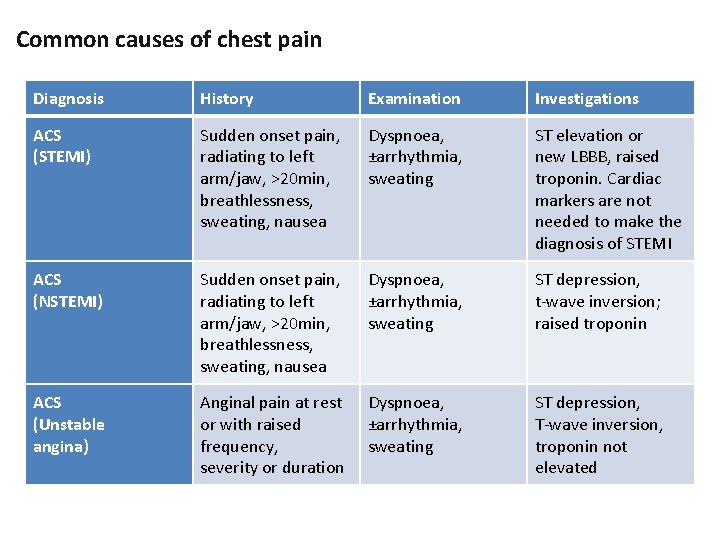
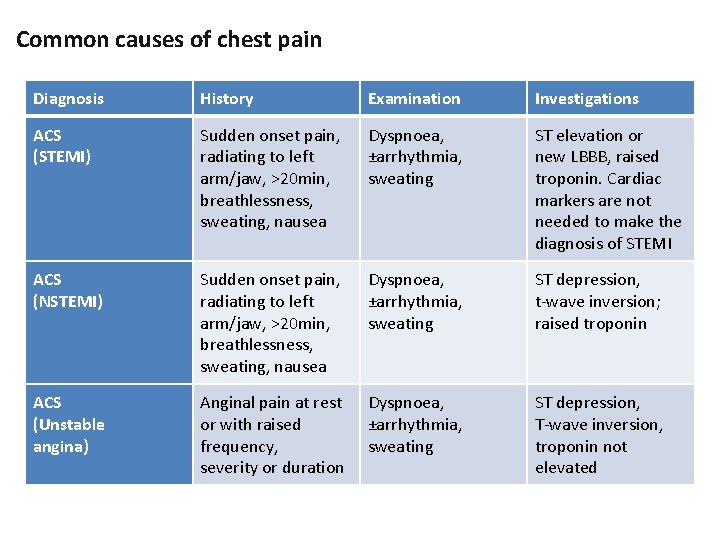
Common causes of chest pain Diagnosis History Examination Investigations ACS (STEMI) Sudden onset pain, radiating to left arm/jaw, >20 min, breathlessness, sweating, nausea Dyspnoea, ±arrhythmia, sweating ST elevation or new LBBB, raised troponin. Cardiac markers are not needed to make the diagnosis of STEMI ACS (NSTEMI) Sudden onset pain, radiating to left arm/jaw, >20 min, breathlessness, sweating, nausea Dyspnoea, ±arrhythmia, sweating ST depression, t-wave inversion; raised troponin ACS (Unstable angina) Anginal pain at rest or with raised frequency, severity or duration Dyspnoea, ±arrhythmia, sweating ST depression, T-wave inversion, troponin not elevated
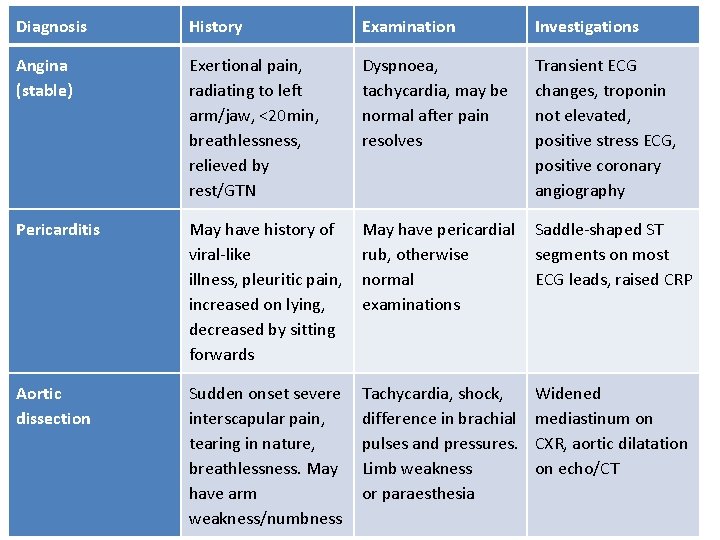
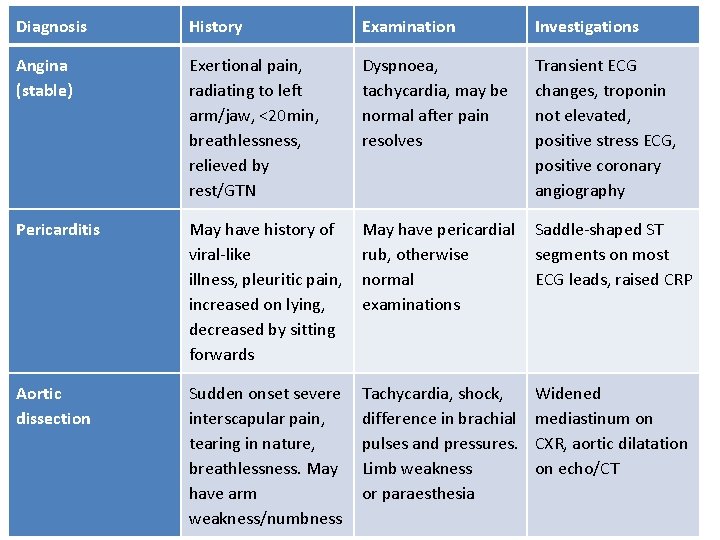
Diagnosis History Examination Investigations Angina (stable) Exertional pain, radiating to left arm/jaw, <20 min, breathlessness, relieved by rest/GTN Dyspnoea, tachycardia, may be normal after pain resolves Transient ECG changes, troponin not elevated, positive stress ECG, positive coronary angiography Pericarditis May have history of viral-like illness, pleuritic pain, increased on lying, decreased by sitting forwards May have pericardial rub, otherwise normal examinations Saddle-shaped ST segments on most ECG leads, raised CRP Aortic dissection Sudden onset severe interscapular pain, tearing in nature, breathlessness. May have arm weakness/numbness Tachycardia, shock, difference in brachial pulses and pressures. Limb weakness or paraesthesia Widened mediastinum on CXR, aortic dilatation on echo/CT
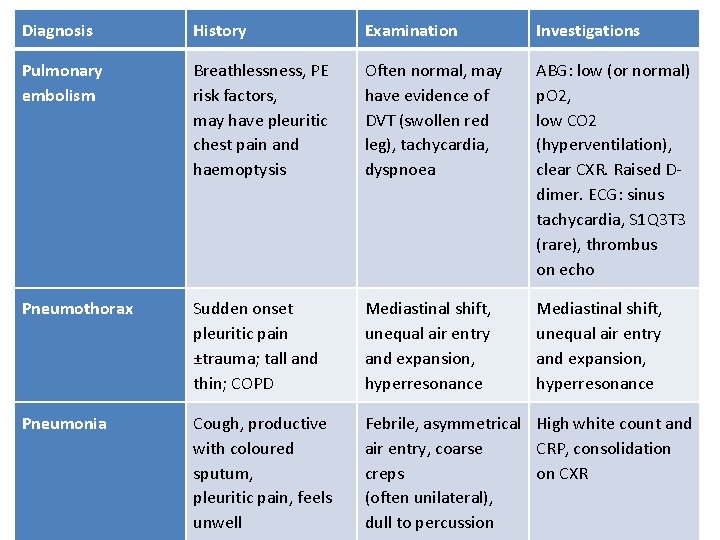
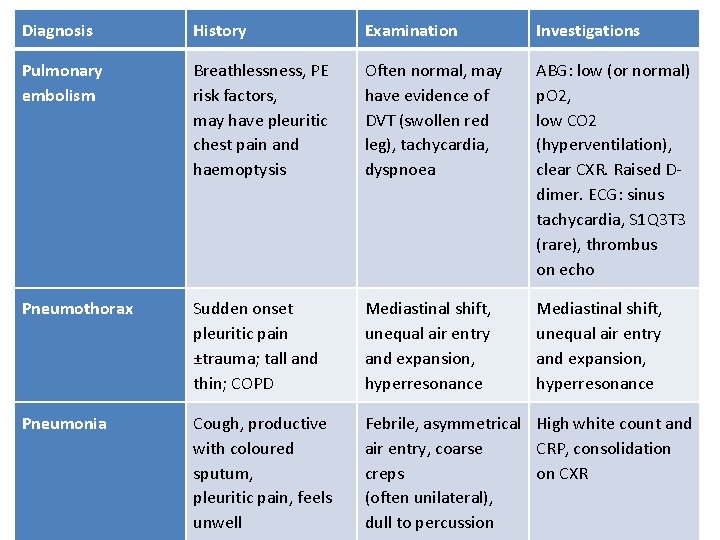
Diagnosis History Examination Investigations Pulmonary embolism Breathlessness, PE risk factors, may have pleuritic chest pain and haemoptysis Often normal, may have evidence of DVT (swollen red leg), tachycardia, dyspnoea ABG: low (or normal) p. O 2, low CO 2 (hyperventilation), clear CXR. Raised Ddimer. ECG: sinus tachycardia, S 1 Q 3 T 3 (rare), thrombus on echo Pneumothorax Sudden onset pleuritic pain ±trauma; tall and thin; COPD Mediastinal shift, unequal air entry and expansion, hyperresonance Pneumonia Cough, productive with coloured sputum, pleuritic pain, feels unwell Febrile, asymmetrical High white count and air entry, coarse CRP, consolidation creps on CXR (often unilateral), dull to percussion
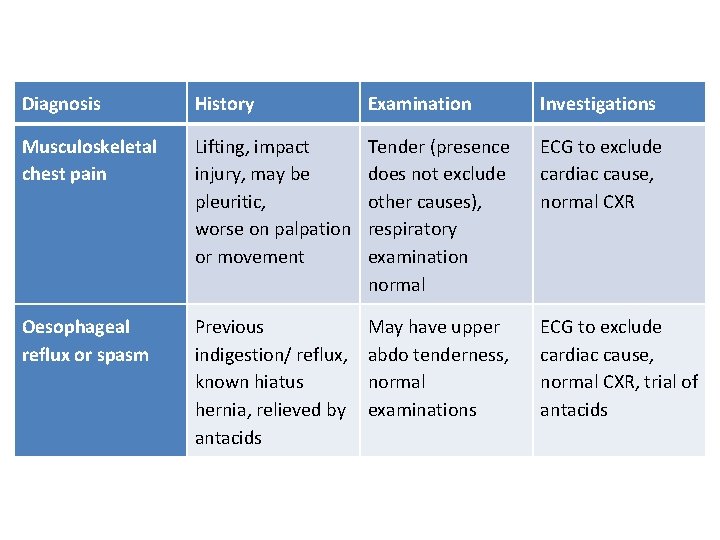
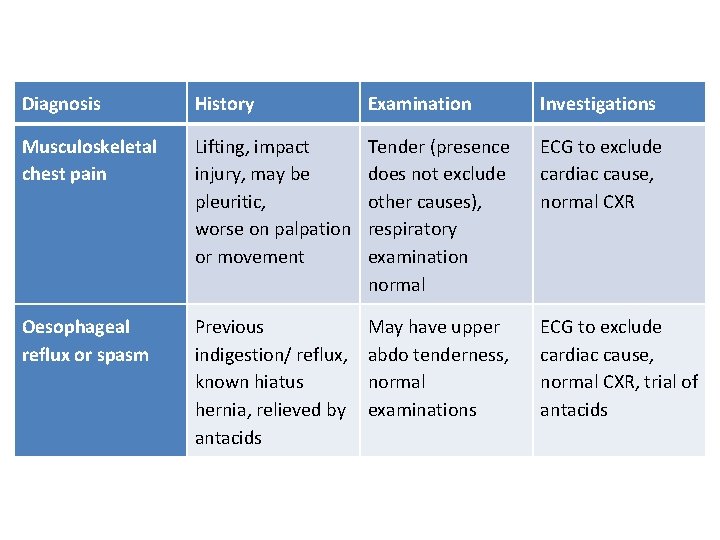
Diagnosis History Examination Investigations Musculoskeletal chest pain Lifting, impact injury, may be pleuritic, worse on palpation or movement Tender (presence does not exclude other causes), respiratory examination normal ECG to exclude cardiac cause, normal CXR Oesophageal reflux or spasm Previous indigestion/ reflux, known hiatus hernia, relieved by antacids May have upper abdo tenderness, normal examinations ECG to exclude cardiac cause, normal CXR, trial of antacids
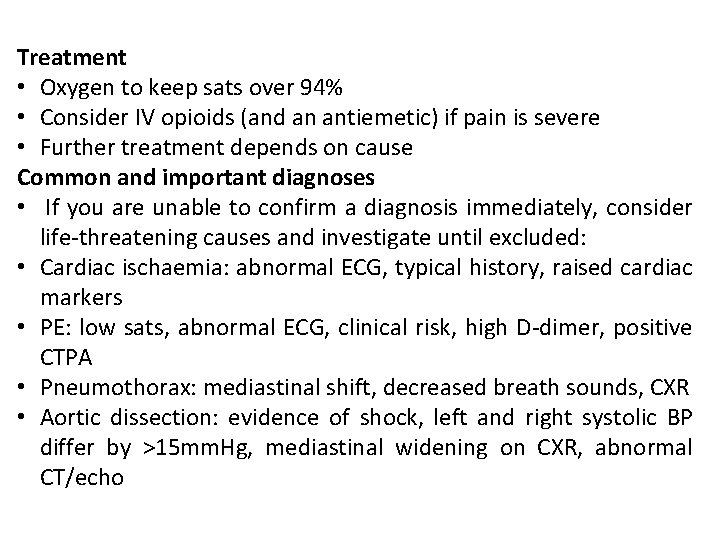
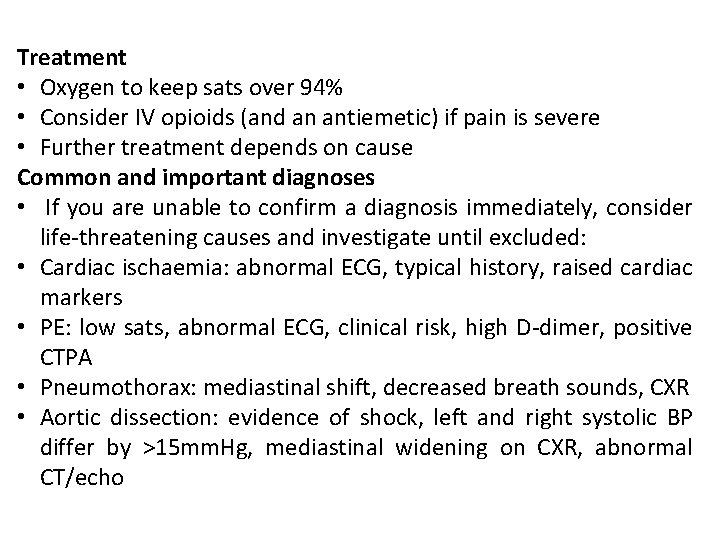
Treatment • Oxygen to keep sats over 94% • Consider IV opioids (and an antiemetic) if pain is severe • Further treatment depends on cause Common and important diagnoses • If you are unable to confirm a diagnosis immediately, consider life-threatening causes and investigate until excluded: • Cardiac ischaemia: abnormal ECG, typical history, raised cardiac markers • PE: low sats, abnormal ECG, clinical risk, high D-dimer, positive CTPA • Pneumothorax: mediastinal shift, decreased breath sounds, CXR • Aortic dissection: evidence of shock, left and right systolic BP differ by >15 mm. Hg, mediastinal widening on CXR, abnormal CT/echo
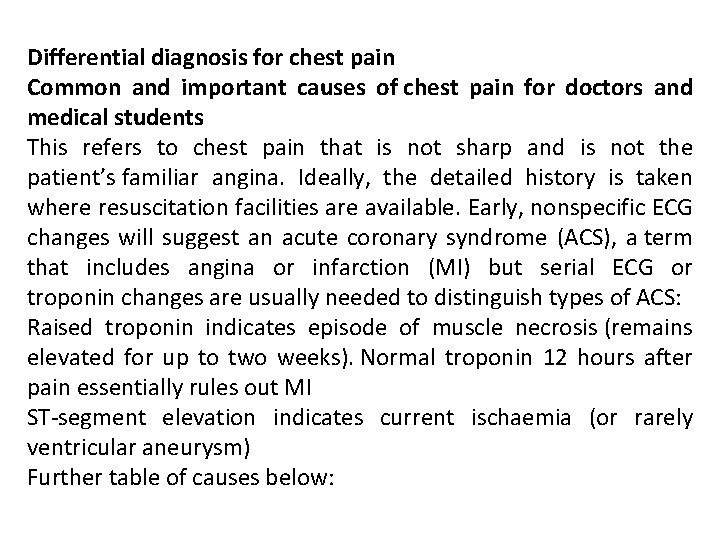
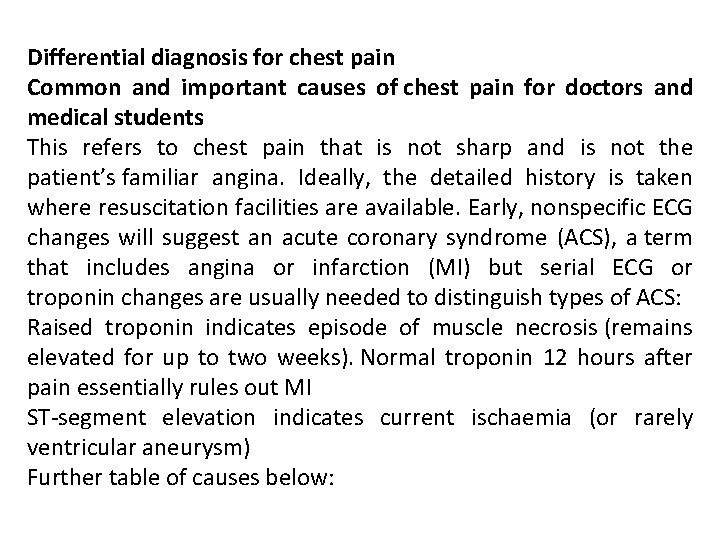
Differential diagnosis for chest pain Common and important causes of chest pain for doctors and medical students This refers to chest pain that is not sharp and is not the patient’s familiar angina. Ideally, the detailed history is taken where resuscitation facilities are available. Early, nonspecific ECG changes will suggest an acute coronary syndrome (ACS), a term that includes angina or infarction (MI) but serial ECG or troponin changes are usually needed to distinguish types of ACS: Raised troponin indicates episode of muscle necrosis (remains elevated for up to two weeks). Normal troponin 12 hours after pain essentially rules out MI ST-segment elevation indicates current ischaemia (or rarely ventricular aneurysm) Further table of causes below:
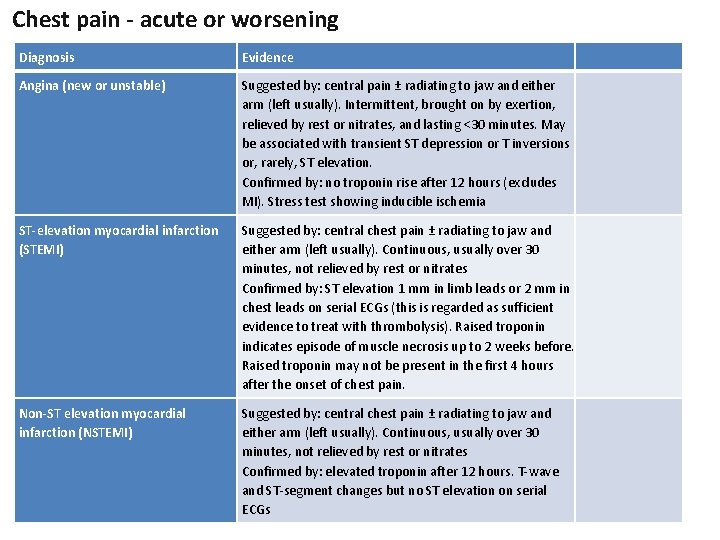
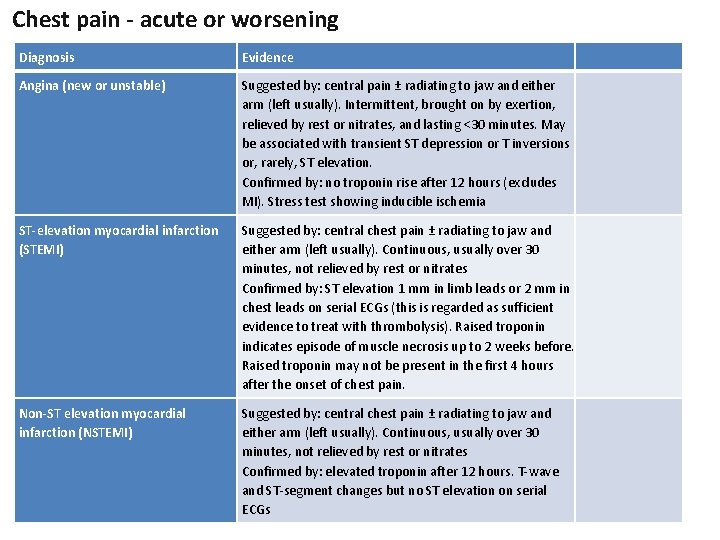
Chest pain - acute or worsening Diagnosis Evidence Angina (new or unstable) Suggested by: central pain ± radiating to jaw and either arm (left usually). Intermittent, brought on by exertion, relieved by rest or nitrates, and lasting <30 minutes. May be associated with transient ST depression or T inversions or, rarely, ST elevation. Confirmed by: no troponin rise after 12 hours (excludes MI). Stress test showing inducible ischemia ST-elevation myocardial infarction (STEMI) Suggested by: central chest pain ± radiating to jaw and either arm (left usually). Continuous, usually over 30 minutes, not relieved by rest or nitrates Confirmed by: ST elevation 1 mm in limb leads or 2 mm in chest leads on serial ECGs (this is regarded as sufficient evidence to treat with thrombolysis). Raised troponin indicates episode of muscle necrosis up to 2 weeks before. Raised troponin may not be present in the first 4 hours after the onset of chest pain. Non-ST elevation myocardial infarction (NSTEMI) Suggested by: central chest pain ± radiating to jaw and either arm (left usually). Continuous, usually over 30 minutes, not relieved by rest or nitrates Confirmed by: elevated troponin after 12 hours. T-wave and ST-segment changes but no ST elevation on serial ECGs
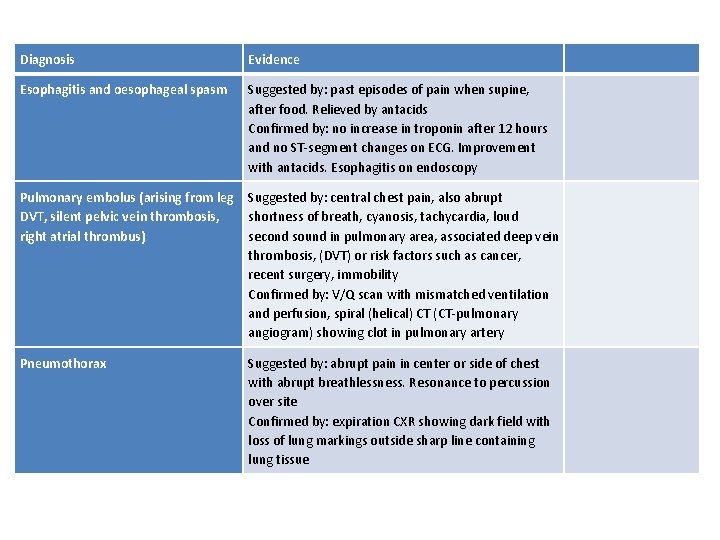
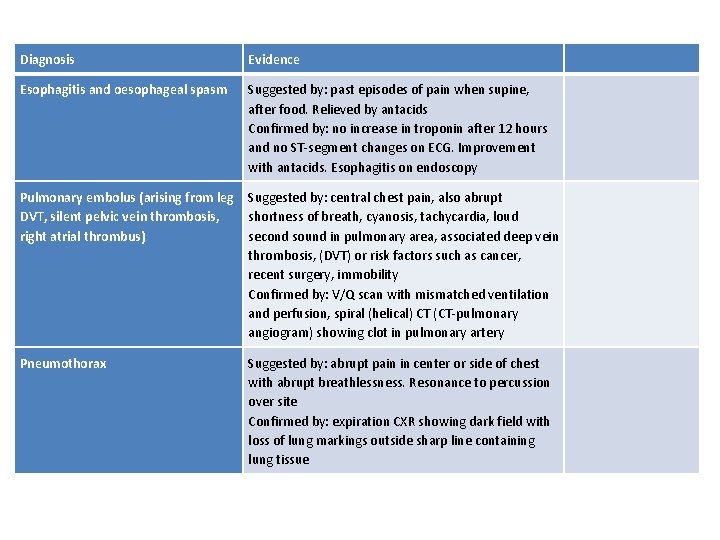
Diagnosis Evidence Esophagitis and oesophageal spasm Suggested by: past episodes of pain when supine, after food. Relieved by antacids Confirmed by: no increase in troponin after 12 hours and no ST-segment changes on ECG. Improvement with antacids. Esophagitis on endoscopy Pulmonary embolus (arising from leg DVT, silent pelvic vein thrombosis, right atrial thrombus) Suggested by: central chest pain, also abrupt shortness of breath, cyanosis, tachycardia, loud second sound in pulmonary area, associated deep vein thrombosis, (DVT) or risk factors such as cancer, recent surgery, immobility Confirmed by: V/Q scan with mismatched ventilation and perfusion, spiral (helical) CT (CT-pulmonary angiogram) showing clot in pulmonary artery Pneumothorax Suggested by: abrupt pain in center or side of chest with abrupt breathlessness. Resonance to percussion over site Confirmed by: expiration CXR showing dark field with loss of lung markings outside sharp line containing lung tissue
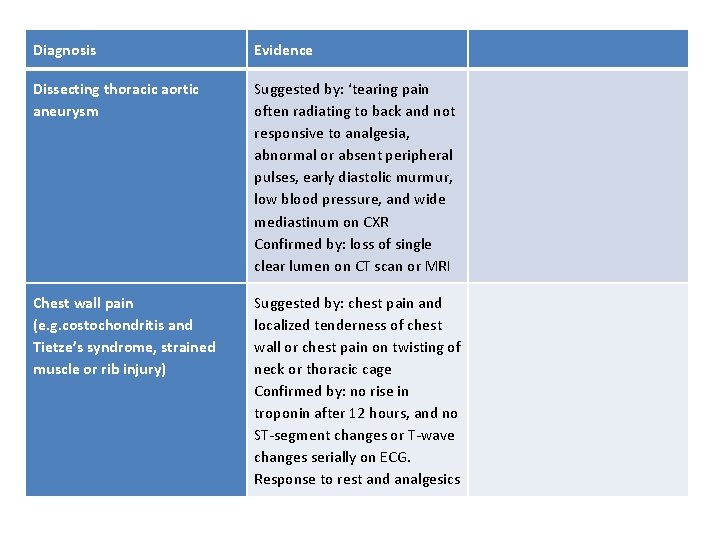
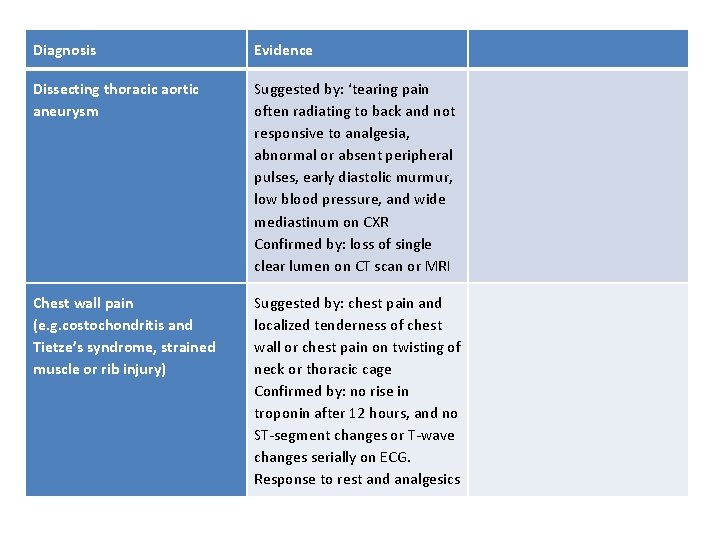
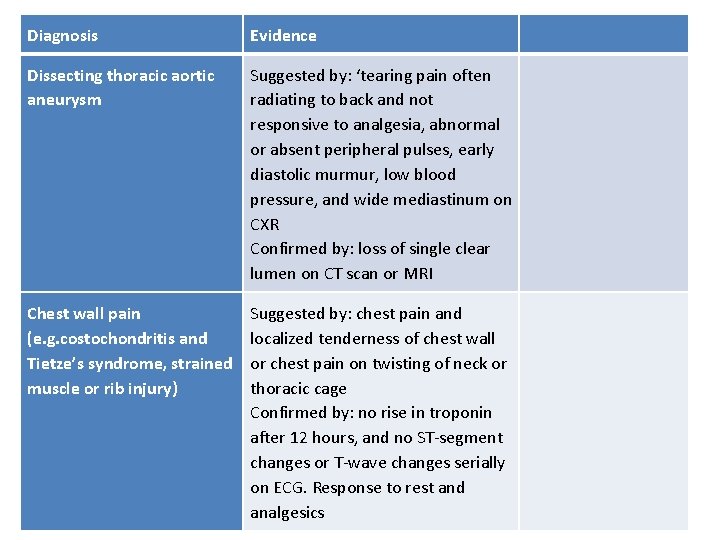
Diagnosis Evidence Dissecting thoracic aortic aneurysm Suggested by: ‘tearing pain often radiating to back and not responsive to analgesia, abnormal or absent peripheral pulses, early diastolic murmur, low blood pressure, and wide mediastinum on CXR Confirmed by: loss of single clear lumen on CT scan or MRI Chest wall pain (e. g. costochondritis and Tietze’s syndrome, strained muscle or rib injury) Suggested by: chest pain and localized tenderness of chest wall or chest pain on twisting of neck or thoracic cage Confirmed by: no rise in troponin after 12 hours, and no ST-segment changes or T-wave changes serially on ECG. Response to rest and analgesics
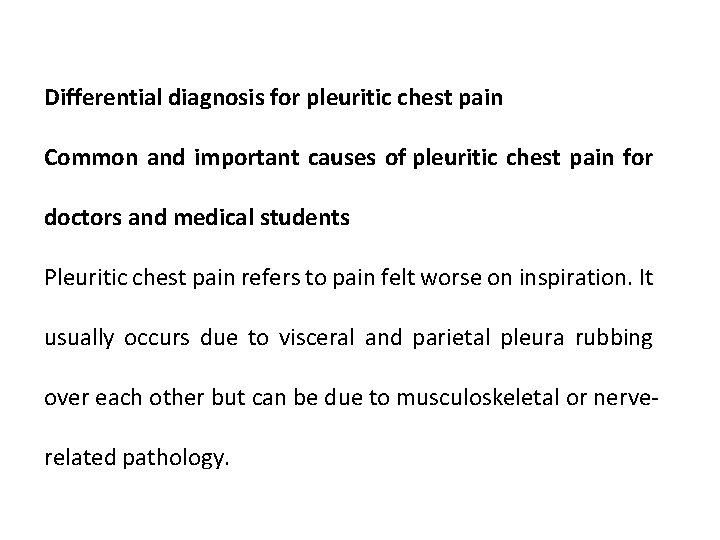
Differential diagnosis for pleuritic chest pain Common and important causes of pleuritic chest pain for doctors and medical students Pleuritic chest pain refers to pain felt worse on inspiration. It usually occurs due to visceral and parietal pleura rubbing over each other but can be due to musculoskeletal or nerverelated pathology.
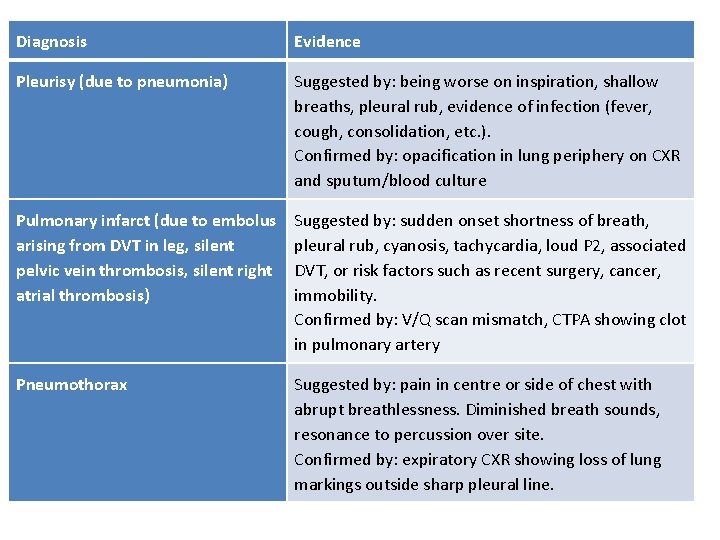
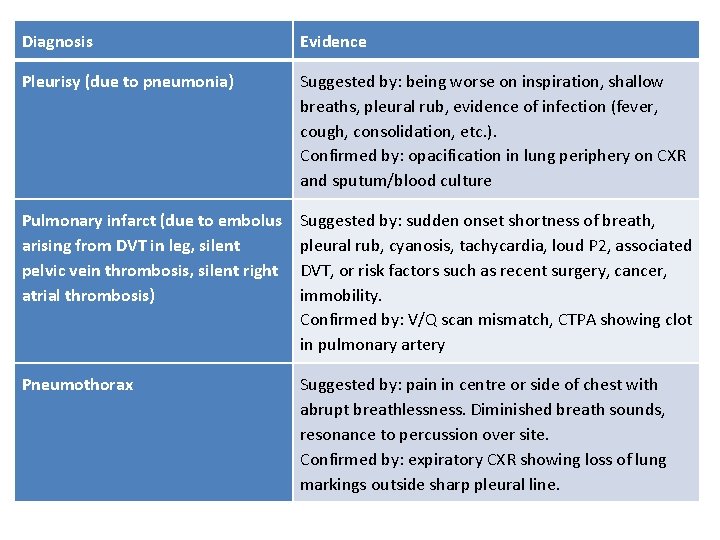
Diagnosis Evidence Pleurisy (due to pneumonia) Suggested by: being worse on inspiration, shallow breaths, pleural rub, evidence of infection (fever, cough, consolidation, etc. ). Confirmed by: opacification in lung periphery on CXR and sputum/blood culture Pulmonary infarct (due to embolus arising from DVT in leg, silent pelvic vein thrombosis, silent right atrial thrombosis) Suggested by: sudden onset shortness of breath, pleural rub, cyanosis, tachycardia, loud P 2, associated DVT, or risk factors such as recent surgery, cancer, immobility. Confirmed by: V/Q scan mismatch, CTPA showing clot in pulmonary artery Pneumothorax Suggested by: pain in centre or side of chest with abrupt breathlessness. Diminished breath sounds, resonance to percussion over site. Confirmed by: expiratory CXR showing loss of lung markings outside sharp pleural line.
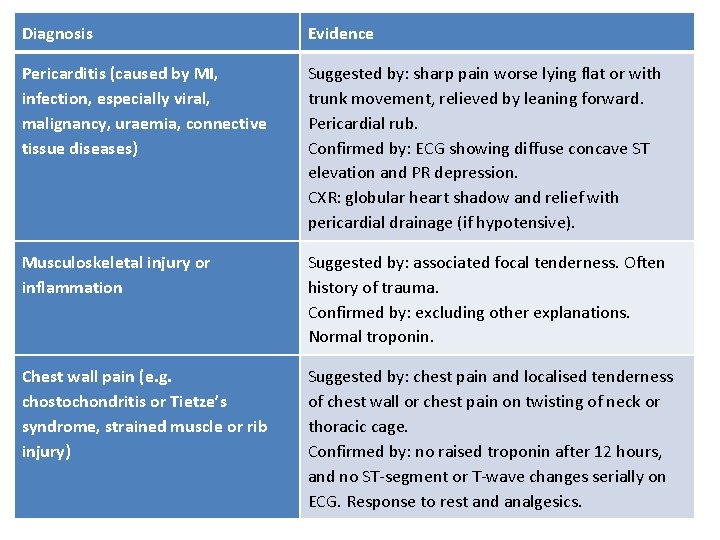
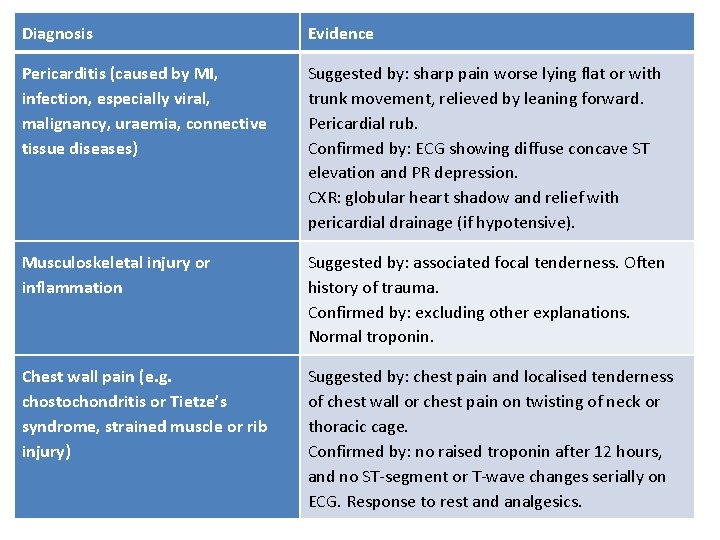
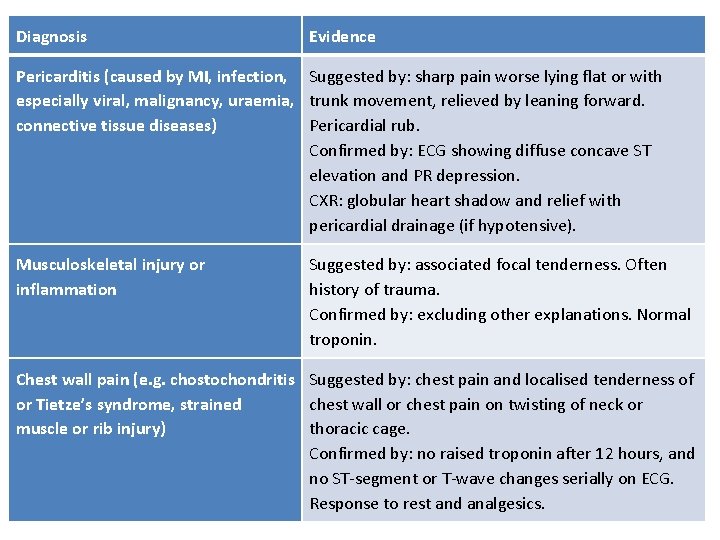
Diagnosis Evidence Pericarditis (caused by MI, infection, especially viral, malignancy, uraemia, connective tissue diseases) Suggested by: sharp pain worse lying flat or with trunk movement, relieved by leaning forward. Pericardial rub. Confirmed by: ECG showing diffuse concave ST elevation and PR depression. CXR: globular heart shadow and relief with pericardial drainage (if hypotensive). Musculoskeletal injury or inflammation Suggested by: associated focal tenderness. Often history of trauma. Confirmed by: excluding other explanations. Normal troponin. Chest wall pain (e. g. chostochondritis or Tietze’s syndrome, strained muscle or rib injury) Suggested by: chest pain and localised tenderness of chest wall or chest pain on twisting of neck or thoracic cage. Confirmed by: no raised troponin after 12 hours, and no ST-segment or T-wave changes serially on ECG. Response to rest and analgesics.
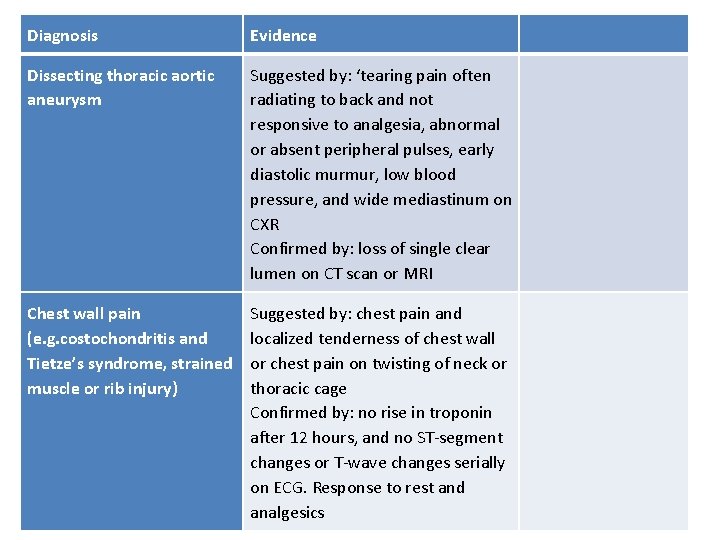
Diagnosis Evidence Dissecting thoracic aortic aneurysm Suggested by: ‘tearing pain often radiating to back and not responsive to analgesia, abnormal or absent peripheral pulses, early diastolic murmur, low blood pressure, and wide mediastinum on CXR Confirmed by: loss of single clear lumen on CT scan or MRI Chest wall pain (e. g. costochondritis and Tietze’s syndrome, strained muscle or rib injury) Suggested by: chest pain and localized tenderness of chest wall or chest pain on twisting of neck or thoracic cage Confirmed by: no rise in troponin after 12 hours, and no ST-segment changes or T-wave changes serially on ECG. Response to rest and analgesics
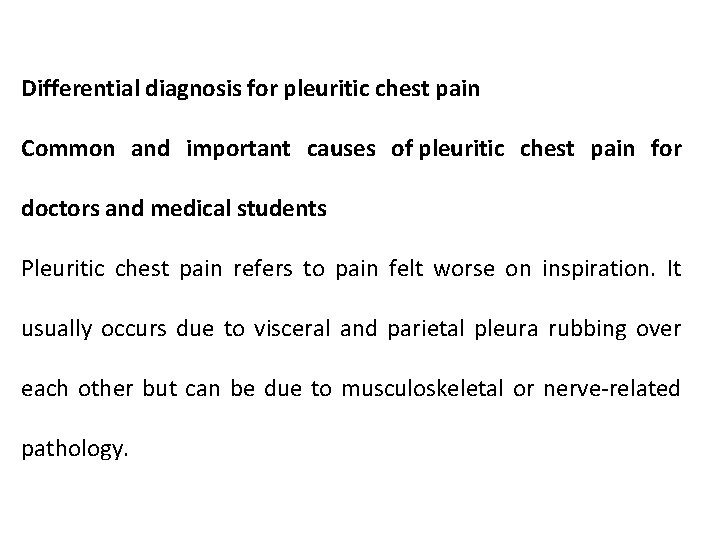
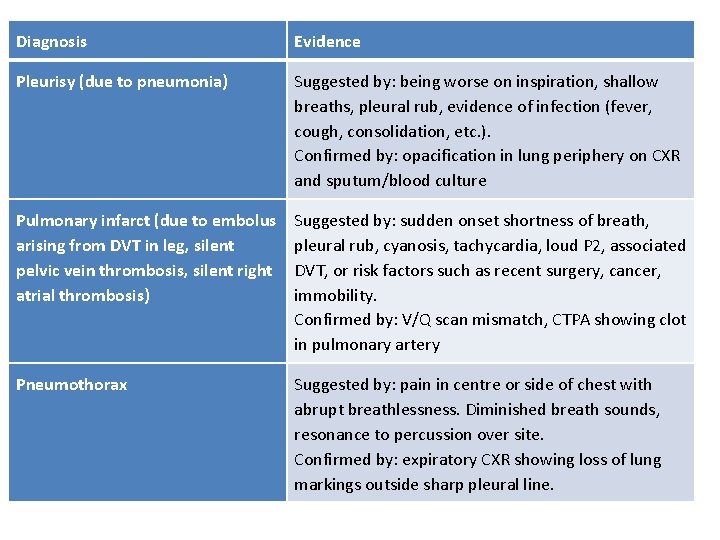
Differential diagnosis for pleuritic chest pain Common and important causes of pleuritic chest pain for doctors and medical students Pleuritic chest pain refers to pain felt worse on inspiration. It usually occurs due to visceral and parietal pleura rubbing over each other but can be due to musculoskeletal or nerve-related pathology.
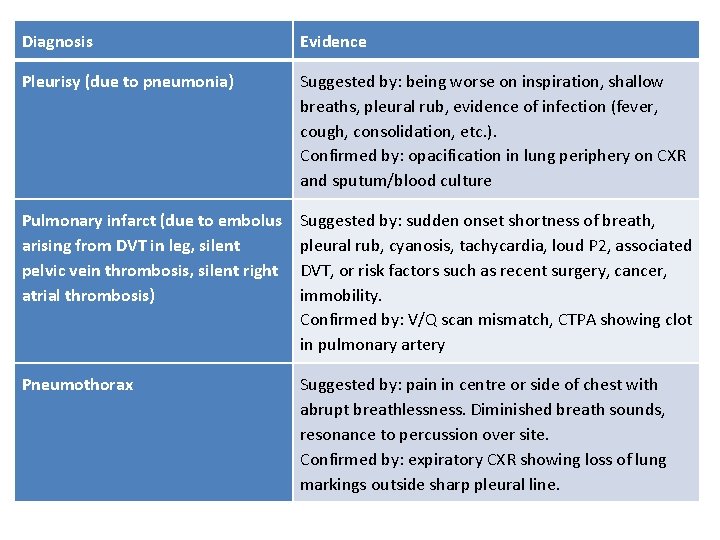
Diagnosis Evidence Pleurisy (due to pneumonia) Suggested by: being worse on inspiration, shallow breaths, pleural rub, evidence of infection (fever, cough, consolidation, etc. ). Confirmed by: opacification in lung periphery on CXR and sputum/blood culture Pulmonary infarct (due to embolus arising from DVT in leg, silent pelvic vein thrombosis, silent right atrial thrombosis) Suggested by: sudden onset shortness of breath, pleural rub, cyanosis, tachycardia, loud P 2, associated DVT, or risk factors such as recent surgery, cancer, immobility. Confirmed by: V/Q scan mismatch, CTPA showing clot in pulmonary artery Pneumothorax Suggested by: pain in centre or side of chest with abrupt breathlessness. Diminished breath sounds, resonance to percussion over site. Confirmed by: expiratory CXR showing loss of lung markings outside sharp pleural line.
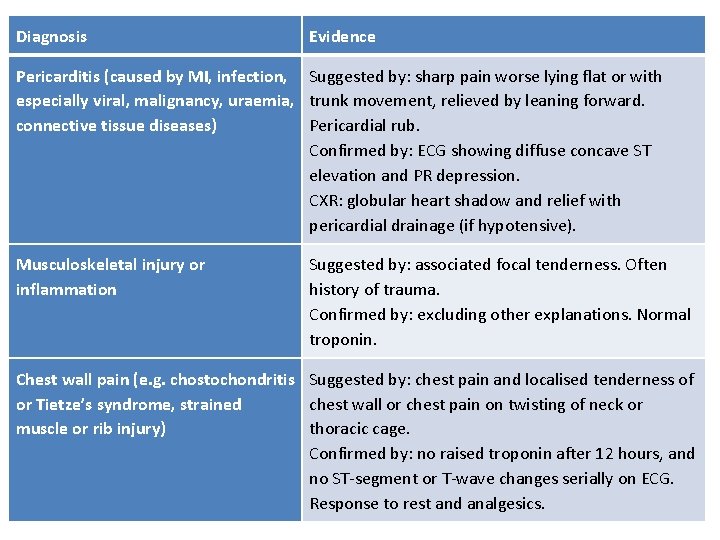
Diagnosis Evidence Pericarditis (caused by MI, infection, Suggested by: sharp pain worse lying flat or with especially viral, malignancy, uraemia, trunk movement, relieved by leaning forward. connective tissue diseases) Pericardial rub. Confirmed by: ECG showing diffuse concave ST elevation and PR depression. CXR: globular heart shadow and relief with pericardial drainage (if hypotensive). Musculoskeletal injury or inflammation Suggested by: associated focal tenderness. Often history of trauma. Confirmed by: excluding other explanations. Normal troponin. Chest wall pain (e. g. chostochondritis Suggested by: chest pain and localised tenderness of or Tietze’s syndrome, strained chest wall or chest pain on twisting of neck or muscle or rib injury) thoracic cage. Confirmed by: no raised troponin after 12 hours, and no ST-segment or T-wave changes serially on ECG. Response to rest and analgesics.
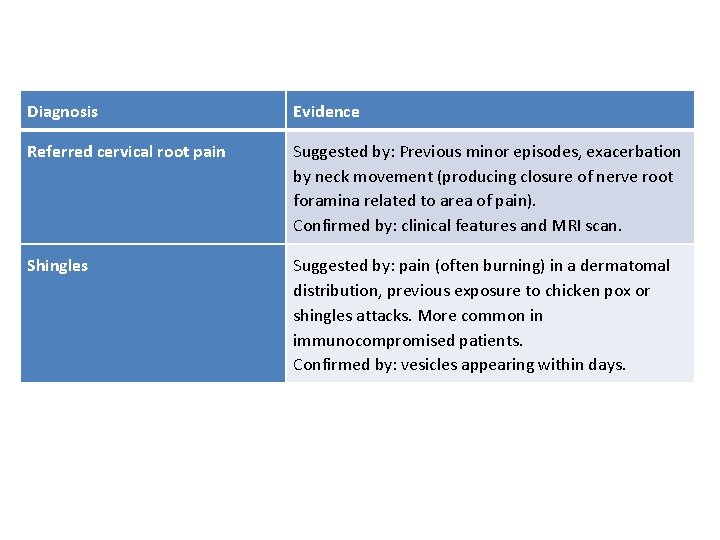
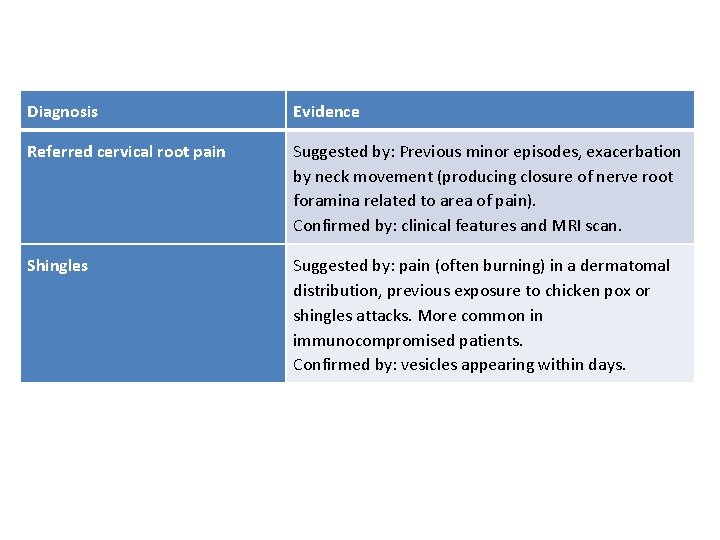
Diagnosis Evidence Referred cervical root pain Suggested by: Previous minor episodes, exacerbation by neck movement (producing closure of nerve root foramina related to area of pain). Confirmed by: clinical features and MRI scan. Shingles Suggested by: pain (often burning) in a dermatomal distribution, previous exposure to chicken pox or shingles attacks. More common in immunocompromised patients. Confirmed by: vesicles appearing within days.
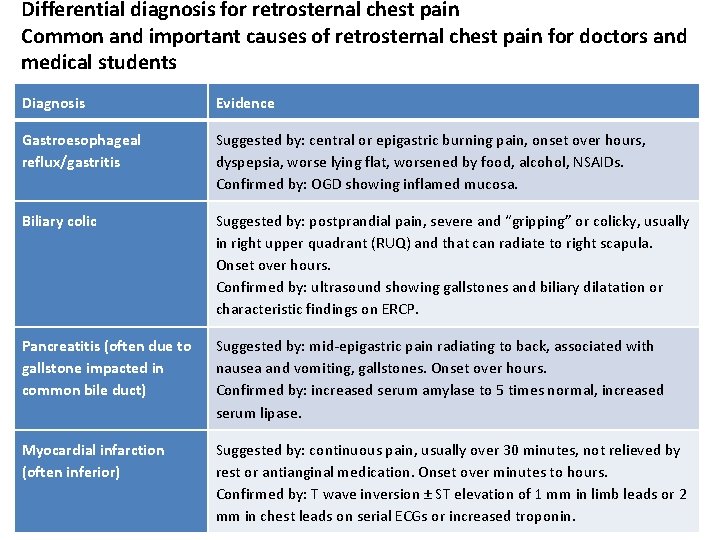
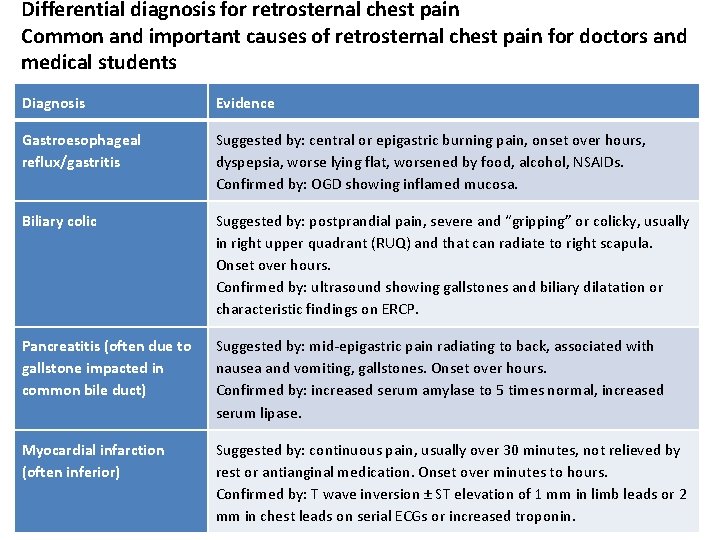
Differential diagnosis for retrosternal chest pain Common and important causes of retrosternal chest pain for doctors and medical students Diagnosis Evidence Gastroesophageal reflux/gastritis Suggested by: central or epigastric burning pain, onset over hours, dyspepsia, worse lying flat, worsened by food, alcohol, NSAIDs. Confirmed by: OGD showing inflamed mucosa. Biliary colic Suggested by: postprandial pain, severe and “gripping” or colicky, usually in right upper quadrant (RUQ) and that can radiate to right scapula. Onset over hours. Confirmed by: ultrasound showing gallstones and biliary dilatation or characteristic findings on ERCP. Pancreatitis (often due to gallstone impacted in common bile duct) Suggested by: mid-epigastric pain radiating to back, associated with nausea and vomiting, gallstones. Onset over hours. Confirmed by: increased serum amylase to 5 times normal, increased serum lipase. Myocardial infarction (often inferior) Suggested by: continuous pain, usually over 30 minutes, not relieved by rest or antianginal medication. Onset over minutes to hours. Confirmed by: T wave inversion ± ST elevation of 1 mm in limb leads or 2 mm in chest leads on serial ECGs or increased troponin.
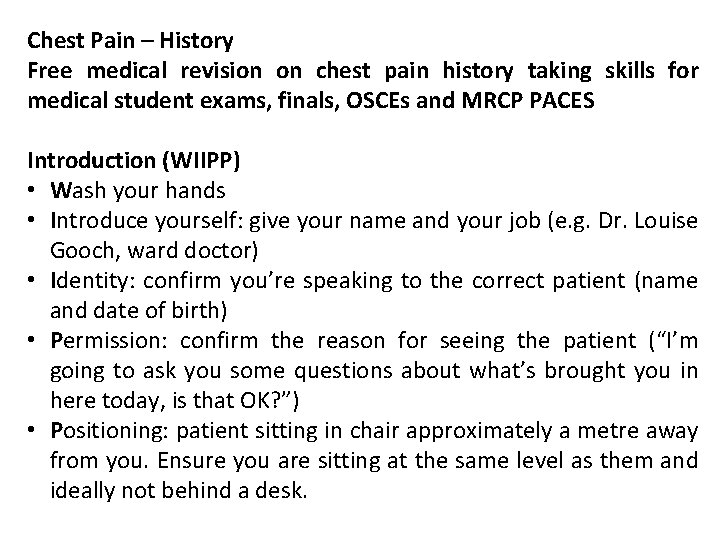
Chest Pain – History Free medical revision on chest pain history taking skills for medical student exams, finals, OSCEs and MRCP PACES Introduction (WIIPP) • Wash your hands • Introduce yourself: give your name and your job (e. g. Dr. Louise Gooch, ward doctor) • Identity: confirm you’re speaking to the correct patient (name and date of birth) • Permission: confirm the reason for seeing the patient (“I’m going to ask you some questions about what’s brought you in here today, is that OK? ”) • Positioning: patient sitting in chair approximately a metre away from you. Ensure you are sitting at the same level as them and ideally not behind a desk.
Presenting Complaint and History of Presenting Complaint • Chest pain is an excellent example of when to use the mnemonic “SOCRATES”: • Site (central or left sided chest pain, retrosternal pain, epigastric pain) • Onset (sudden onset, how quickly it progressed, relation to exertion [if related to exertion, is it always related to exertion or occasionally at rest]) • Character (crushing, heavy, tight, pleuritic [worst with breathing], burning) • Some patients may struggle to explain the character of their pain. If this the case, give them a list of options (e. g. tight, sharp, dull or burning)
![Radiation radiating to left arm neck jaw ACS back pancreatitis aortic dissection • Radiation (radiating to left arm, neck, jaw [ACS]; back [pancreatitis, aortic dissection])](https://slidetodoc.com/presentation_image_h2/3c8fa8b4c305ad2a5f0cb3362d612ef9/image-26.jpg)
• Radiation (radiating to left arm, neck, jaw [ACS]; back [pancreatitis, aortic dissection]) • Alleviating factors (rest, glycerol trinitrate [GTN – suggestive of ACS]; sitting forward [pericarditis]) • Timing (relation to exertion or food; any positional element) • Exacerbating factors • Arm movement, pressing on chest (suggests musculoskeletal) • Exercise, effort (suggest cardiac) • Severity scale (1 -10) • Associated symptoms • Acute coronary syndrome (shortness of breath, sweating, nausea) • Other cardiac symptoms (palpitations, peripheral oedema, paroxysmal nocturnal dyspnoea, orthopnoea) • Abdominal (heartburn, burping, previous history of gastroesophageal reflux) • Psychosomatic (anxiety, history of panic attacks) • Constitutional symptoms (fever, coryza)
Past Medical History Vascular disease in any organ • Cardiac • Angina; previous mycardial infarction; previous angioplasty or coronary artery bypass graft surgery (CABG); stents (how many, bare metal or drug-eluting) • Peripheral • Claudication, previous peripheral vascular disease • Neurological • Previous stroke, transient ischemic attack
Risk factors for cardiovascular disease • Hypertension • Hypercholesterolemia • Diabetes • Smoking • Family history (heart attack under 60 years old, familial hypercholesterolemia) Risk factors for DVT/PE • Recent surgery (under three months), malignancy, immobility • Inherited coagulopathy (e. g. protein C or S deficiency) • Relevant medications (e. g. oral contraceptive pill / hormone replacement therapy) Risk factors for pneumothorax • Tall, thin men in particular • Known connection tissue disease (e. g. Marfans) • Smoking history
Drug History Full drug history including recreational and over-the-counter (OTC) medications. In particular: Cardiac medications Beta-blockers, diuretics, antiplatelet agents, GTN spray Gastric irritants Non steroidal anti inflammatories (NSAIDs), steroids, bisphonates Procoagulant medications Oral contraceptive pill, hormone replacement therapy (HRT) Recreational drug use Cocaine (common cause of coronary artery spasm in young people)
Social history Smoking history (pack years) Alcohol intake (units per week) Lifestyle / exercise
 Stabbing pain in chest
Stabbing pain in chest Typical chest pain
Typical chest pain Typical chest pain
Typical chest pain Chest pain in pediatrics
Chest pain in pediatrics Emergency severity index
Emergency severity index Petmac chest pain
Petmac chest pain 50 shades of chest pain
50 shades of chest pain Retrosternal chest pain
Retrosternal chest pain Nursing care plan on angina pectoris
Nursing care plan on angina pectoris Causes chest pain
Causes chest pain örebro musculoskeletal pain screening questionnaire
örebro musculoskeletal pain screening questionnaire Sympathetic trunk
Sympathetic trunk Mad pain martian pain
Mad pain martian pain Pregnant or period
Pregnant or period What is the nursing process
What is the nursing process Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Second phase of nursing process
Second phase of nursing process Nursing process objectives
Nursing process objectives Charting identification chapter 28
Charting identification chapter 28 Tongue position classification
Tongue position classification Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Chapter 28 oral diagnosis and treatment planning
Chapter 28 oral diagnosis and treatment planning Symptoms before period
Symptoms before period Alarm signs of pud
Alarm signs of pud Anterior knee pain ddx
Anterior knee pain ddx Percussion abdominal assessment
Percussion abdominal assessment Pain treatment satisfaction scale
Pain treatment satisfaction scale Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Rash on upper chest and back
Rash on upper chest and back Chest and back muscles
Chest and back muscles Head and chest circumference chart
Head and chest circumference chart