Chest Pain and Cardiac Emergencies 2015 Chest Pain










- Slides: 34

Chest Pain and Cardiac Emergencies 2015


Chest Pain and Cardiac Emergencies Welcome Chest Pain Certainty Simulation
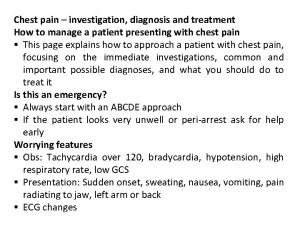
Introduction • Chest Pain is common – 6 potentially lethal causes to remember – Traditional approach (*full Hx) may be suboptimal • Assessment and Management should focus on – ABCDEFG and ECG – IV access, M. O. N. A. (may not be right anymore) – Senior review (#8500/mobile or Medical Registrar)
Approach – Traditional vs. Emergency Life Threats Serious Causes Benign Causes (Common)

Lethal Causes • • • Myocardial Infarction (MI) Pulmonary Embolism (PE) Aortic Dissection (AD) Pneumothorax (Tension Pneumothorax) Pneumonia and Sepsis Oesophageal Perforation

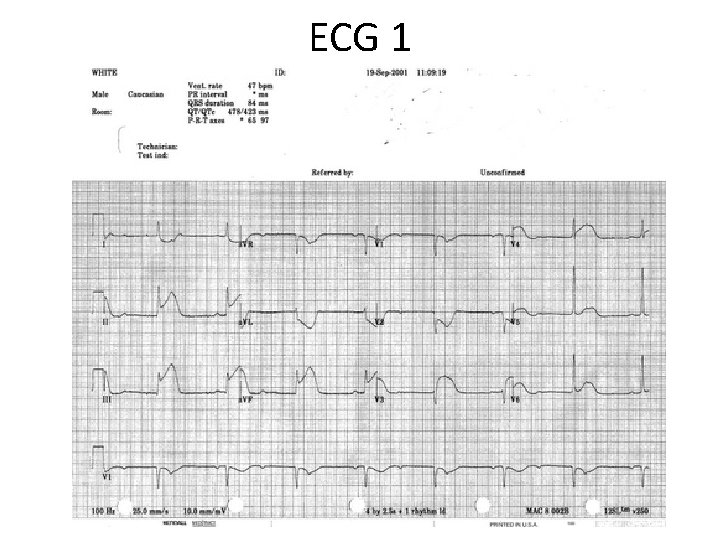
Myocardial Infarction and the Acute Coronary Syndromes ECG
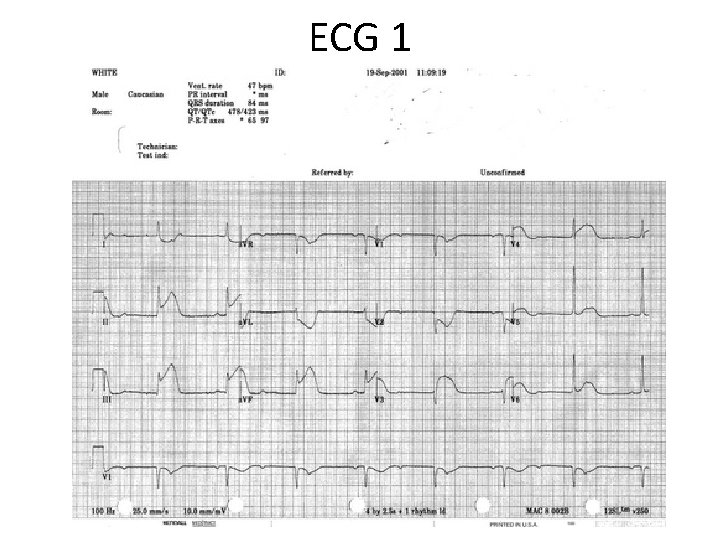
ECG 1

Acute Coronary Syndrome Assessment
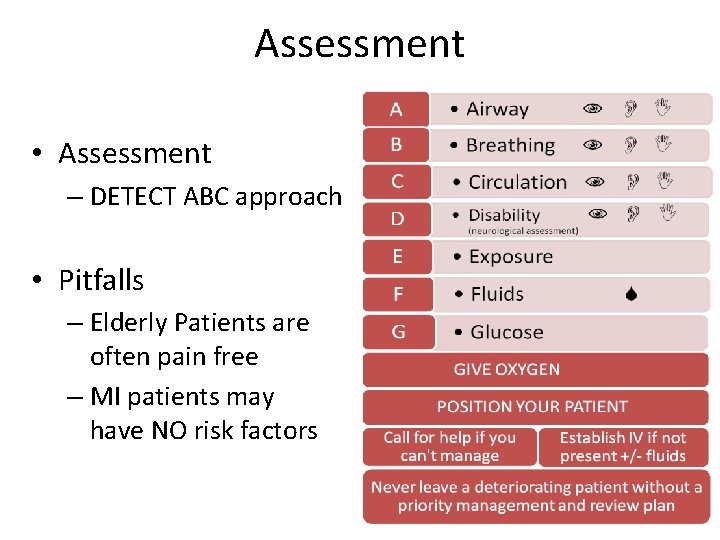
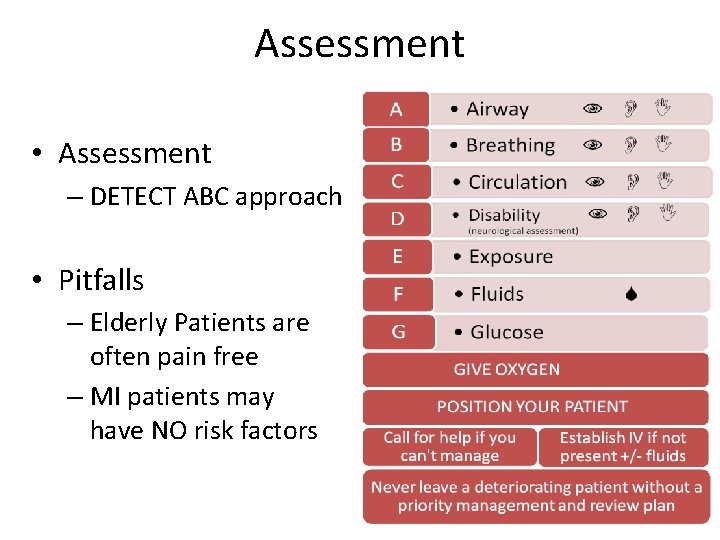
Assessment • Assessment – DETECT ABC approach • Pitfalls – Elderly Patients are often pain free – MI patients may have NO risk factors
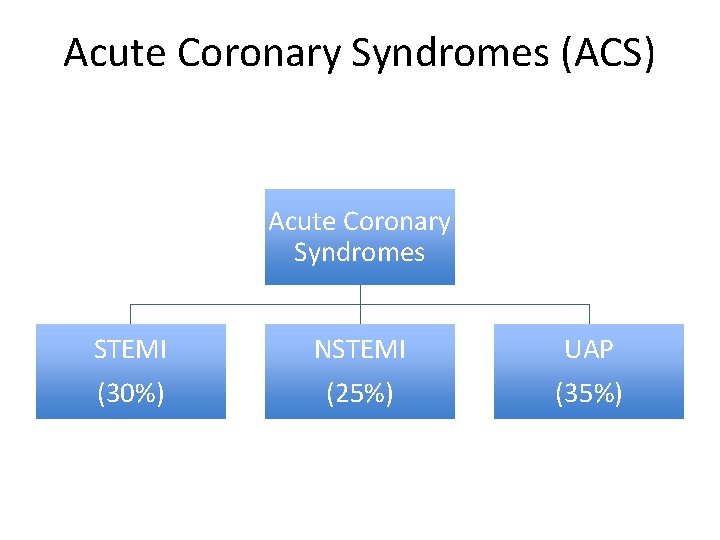
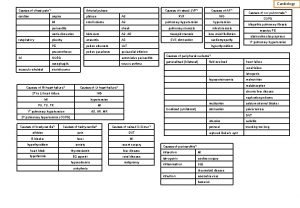
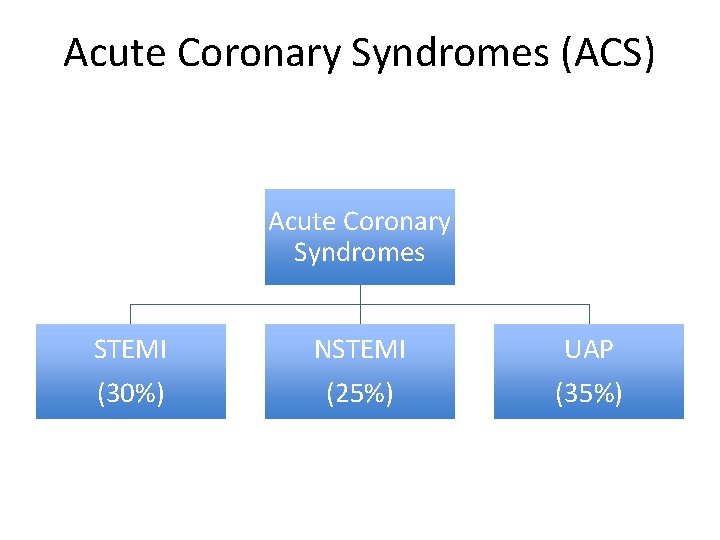
Acute Coronary Syndromes (ACS) Acute Coronary Syndromes STEMI (30%) NSTEMI (25%) UAP (35%)
Atypical = Typical

Acute Coronary Syndrome Management
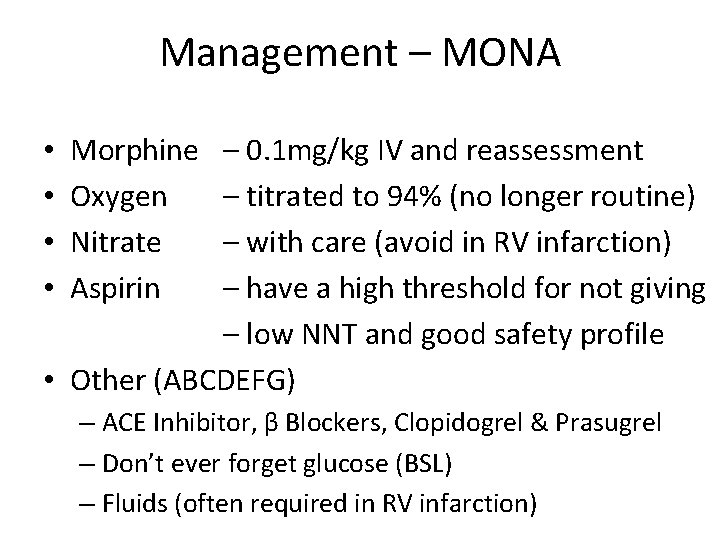
Management – MONA – 0. 1 mg/kg IV and reassessment – titrated to 94% (no longer routine) – with care (avoid in RV infarction) – have a high threshold for not giving – low NNT and good safety profile • Other (ABCDEFG) • • Morphine Oxygen Nitrate Aspirin – ACE Inhibitor, β Blockers, Clopidogrel & Prasugrel – Don’t ever forget glucose (BSL) – Fluids (often required in RV infarction)

Management DOCUMENT YOUR PLAN CLEARLY
Referral – “ISBAR” COMMUNICATE Page 8500 and/or Cath Lab Team (STEMI) Your Registrar Consultant (in hours) Medical Registrar (out of hours) EFFICIENTLY Intro - I am Andrew the Intern covering A 5 C Situation and Background - I have Mrs Smith who is in hospital with abdominal pain that AND CLEARLY was thought to be from Gallstones – she now has Chest pain & ST Elevation in AVF, II and III • Assessment – obs Response – review • • •
Management • Resuscitation, Specific (MONA) and Supportive • Disposition – Catheter Laboratory – Cardiac Unit (A 5 a, A 5 c) – CCU (A 5 b) – Cardiothoracics (C 3 c and D 3 c) – Respiratory Ward - PE and Pneumothorax (B 5 a) – ICU (E 3 a and E 3 b) – Home & follow up (e. g. EST, Cardiac CT, MIBI, Echo)
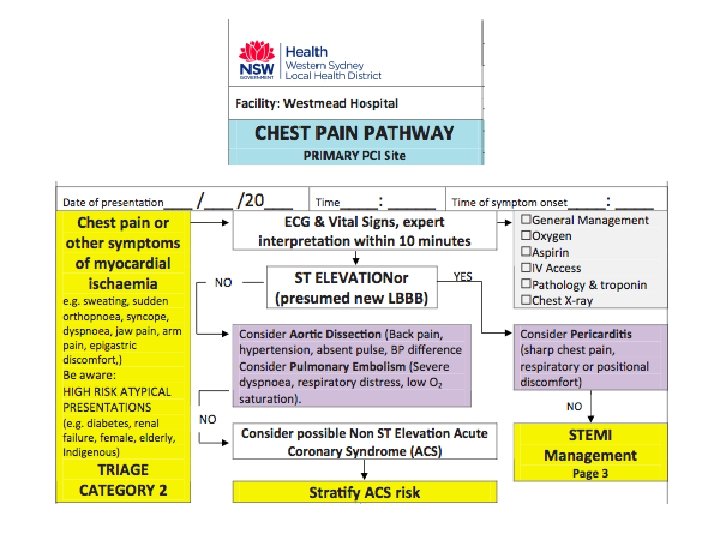
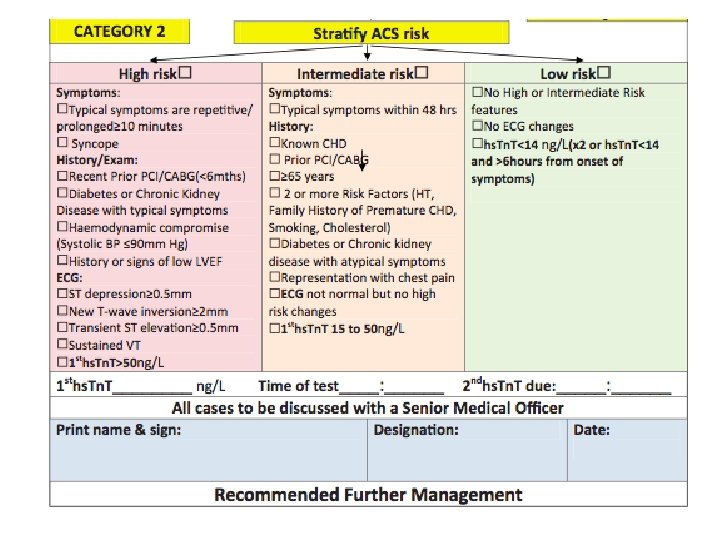
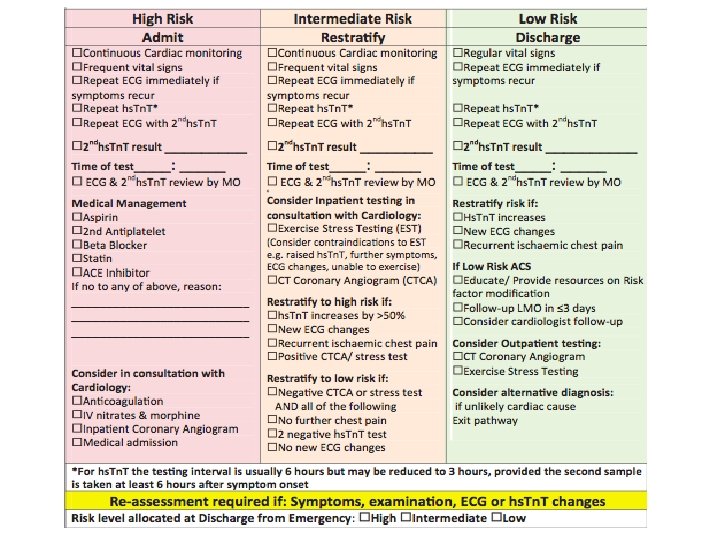
Chest Pain Risk Stratification and State Policy
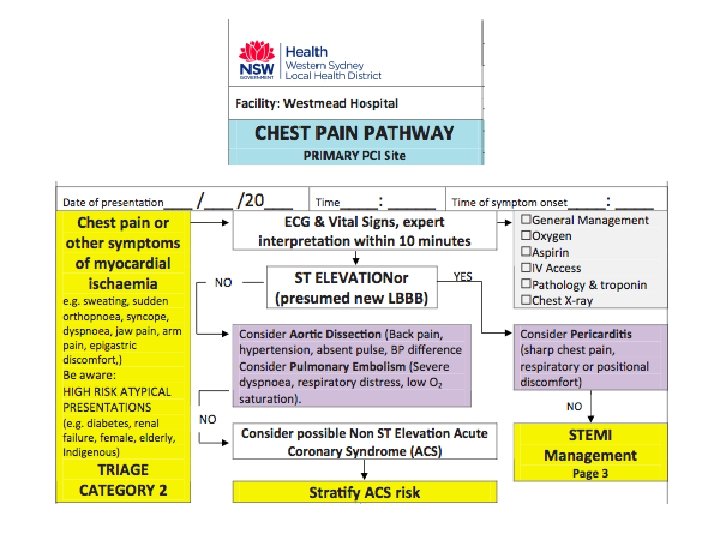
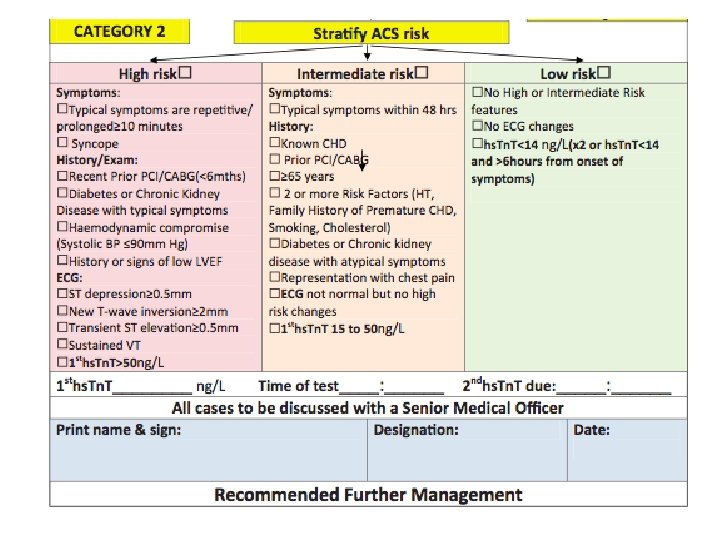
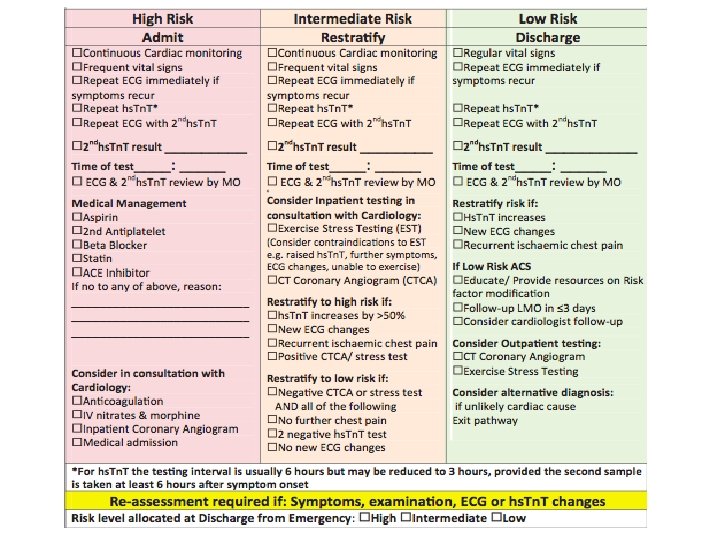
ALL PROTOCOLS ARE ON ED INTRANET

Other Causes of Chest Pain
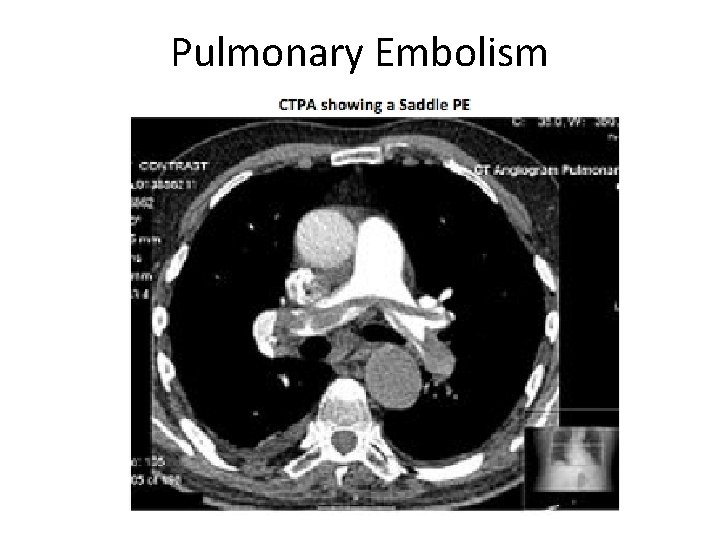
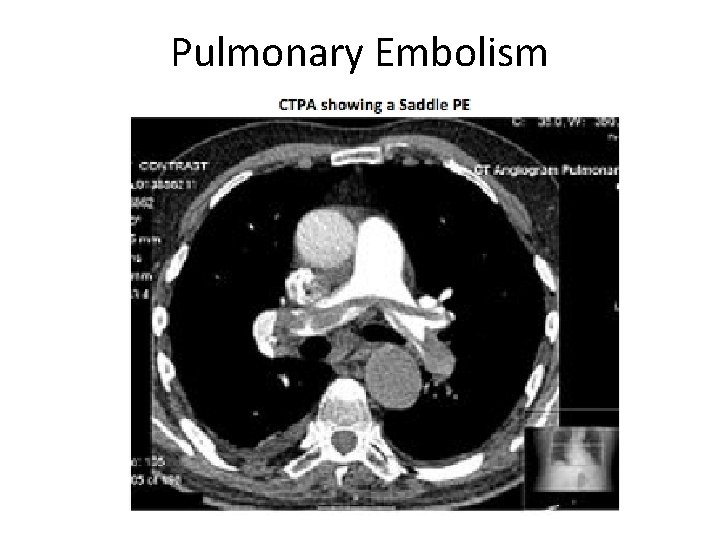
Pulmonary Embolism
Aortic Dissection • Uncommon 5/100, 000 • Overall Mortality is 27% in hospital, 1% per hour and >90% untreated • Ratio of MI to Dissection is 3000: 5 (so it is often missed and treated as MI) • Risk Factors – Hypertension, Cardiothoracic Surgery, Collagen Vascular Disease • Stanford – A & B (‘A’ proximal involvement) • CXR and BP both arms have limited value!
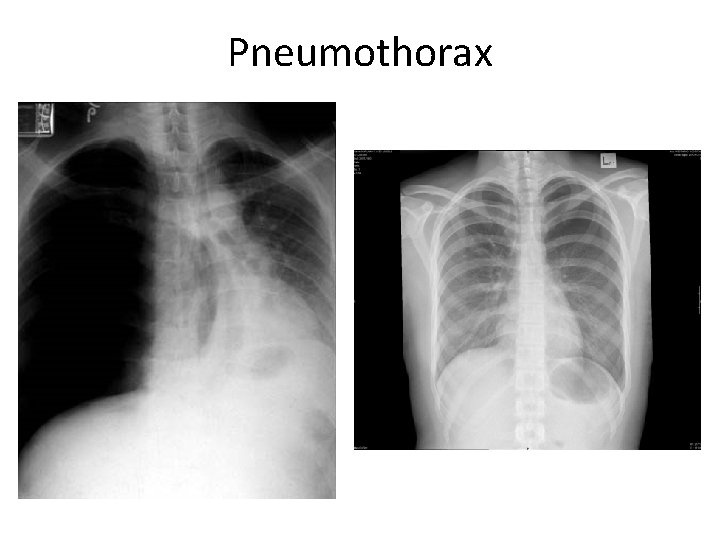
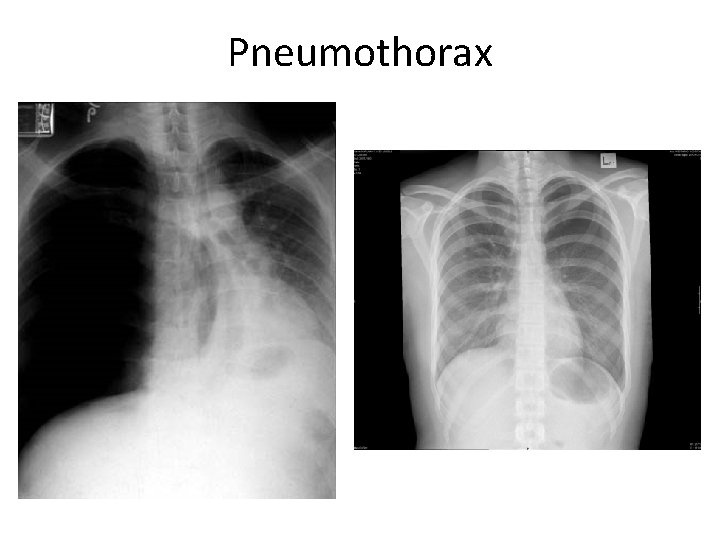
Pneumothorax

Arrhythmia Recognition and Management
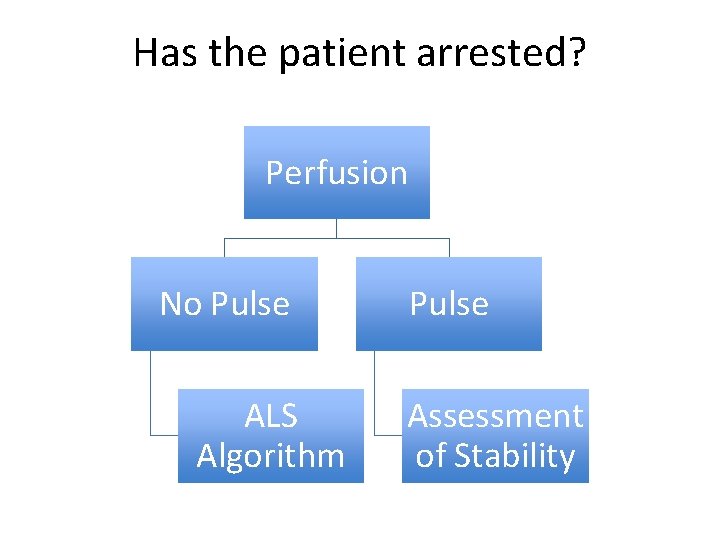
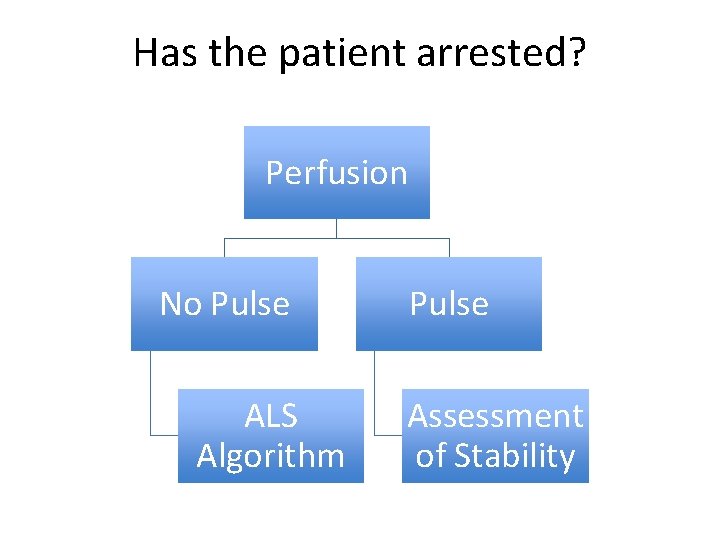
Has the patient arrested? Perfusion No Pulse ALS Algorithm Pulse Assessment of Stability
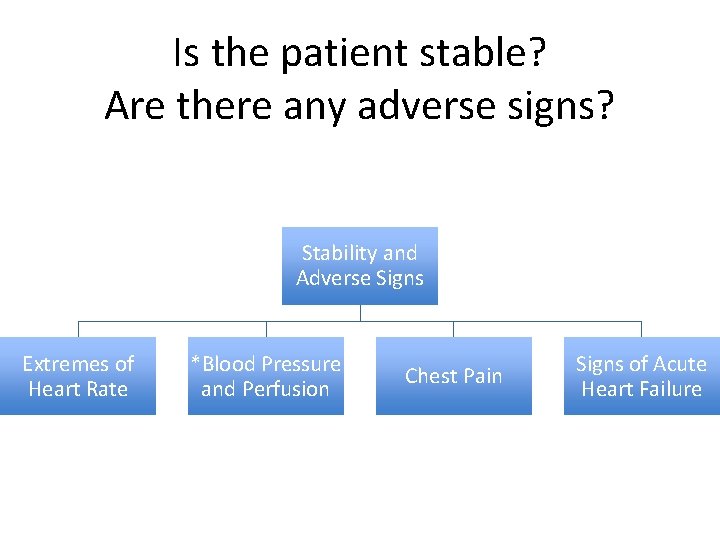
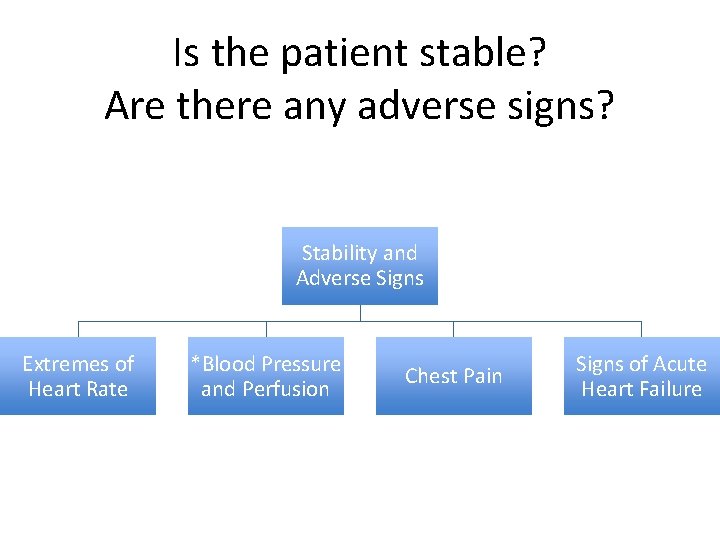
Is the patient stable? Are there any adverse signs? Stability and Adverse Signs Extremes of Heart Rate *Blood Pressure and Perfusion Chest Pain Signs of Acute Heart Failure
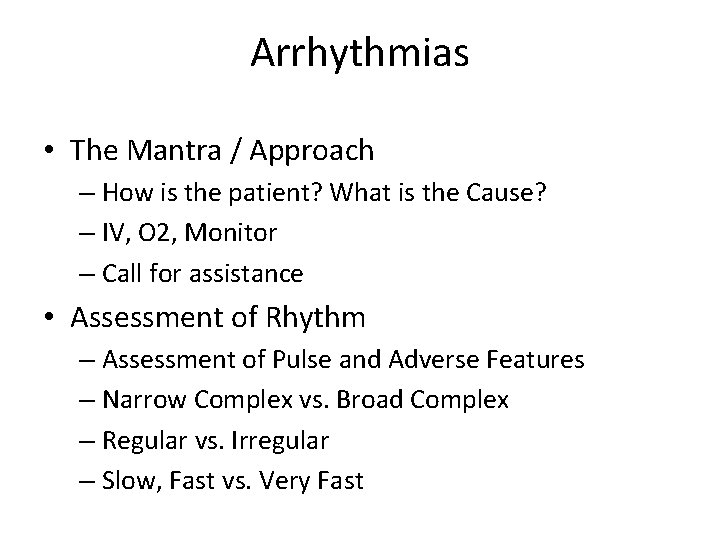
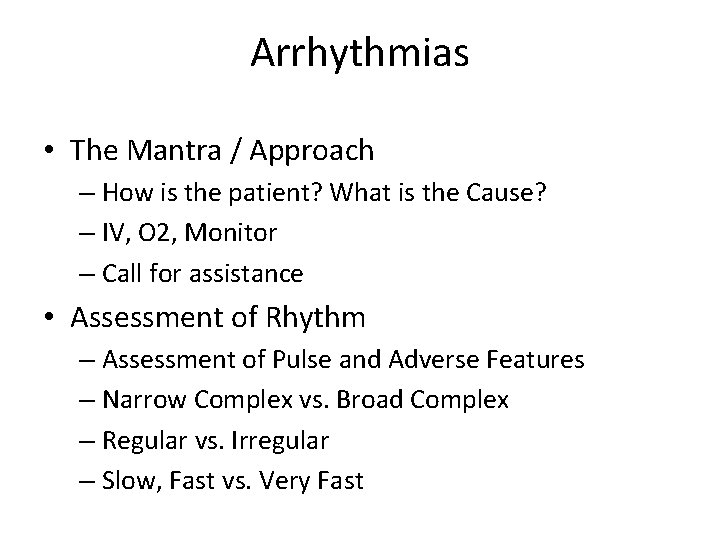
Arrhythmias • The Mantra / Approach – How is the patient? What is the Cause? – IV, O 2, Monitor – Call for assistance • Assessment of Rhythm – Assessment of Pulse and Adverse Features – Narrow Complex vs. Broad Complex – Regular vs. Irregular – Slow, Fast vs. Very Fast
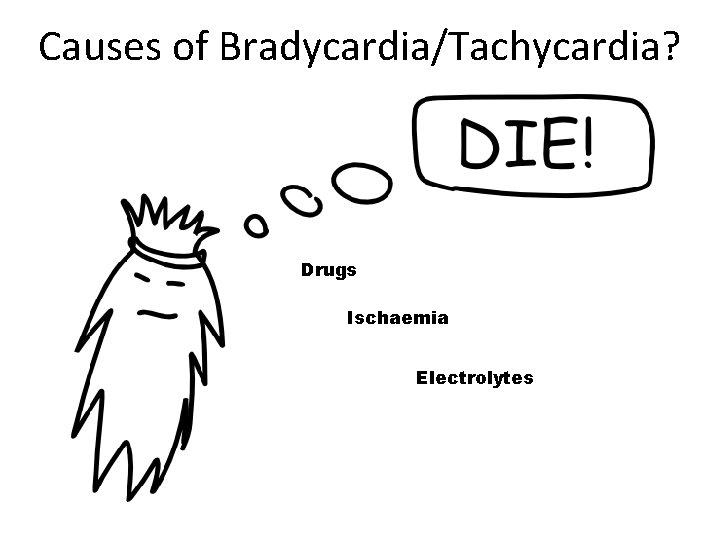
Causes of Bradycardia/Tachycardia? Drugs Ischaemia Electrolytes
Take Home • • • 6 lethal causes ‘Atypical = Typical’ (Non-cardiac = Non-cardiac) A – G approach Serial ECGs Call for senior help Call for help (ALS team) for patients with adverse signs including refractory chest pain, shock, extremes of heart rate and cardiac failure
 Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Funnel chest
Funnel chest Typical chest pain
Typical chest pain Mason liker
Mason liker Chest pain in pediatrics
Chest pain in pediatrics Ctas triage
Ctas triage Petmac chest pain
Petmac chest pain 50 shades of chest pain
50 shades of chest pain Retrosternal chest pain
Retrosternal chest pain Nursing care plan for angina
Nursing care plan for angina Causes chest pain
Causes chest pain örebro musculoskeletal pain screening questionnaire
örebro musculoskeletal pain screening questionnaire Referred back pain chart
Referred back pain chart Mad pain and martian pain
Mad pain and martian pain Vomiting during period sign of pregnancy
Vomiting during period sign of pregnancy Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 28 lesson 1
Chapter 28 lesson 1 Period vs pregnancy
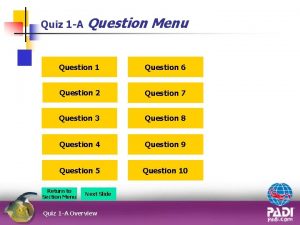
Period vs pregnancy I should take a local orientation dive whenever i
I should take a local orientation dive whenever i Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Environmental emergencies emt
Environmental emergencies emt Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies During a psychiatric emergency the emt should be able to
During a psychiatric emergency the emt should be able to Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Oncological emergencies wikipedia
Oncological emergencies wikipedia Gems diamond geriatric assessment
Gems diamond geriatric assessment Chapter 13 handling emergencies
Chapter 13 handling emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies Psychiatric emergencies
Psychiatric emergencies Qut security emergency extension number
Qut security emergency extension number