Proximal humeral fractures AO Trauma Advanced Principles Course
- Slides: 48
Proximal humeral fractures AO Trauma Advanced Principles Course
Learning objectives • • • Describe anatomical landmarks and surgical approaches Outline techniques for reducing 2 -, 3 -, and 4 -part fractures Explain the key issues in the treatment of proximal humeral fractures Evaluate relative indications for internal fixation and arthroplasty Discuss expected outcomes and rehabilitation List key outcome publications
Unique problems • Anatomy: • Bone + soft tissue = complex • Rotator cuff critical for function • • • Fracture classification—difficult Vascular supply—avascular necrosis (AVN) a potential problem Demographics: • Elderly with poor bone and low functional demand • Young patients with good bone stock and high functional demand
Other facts about this fracture Systematic reviews demonstrate: • Assessment of fracture type is difficult • Wide range of treatments exist • Evidence does not support any specific operative treatment choice Most surgeons are convinced “they” know the “correct” treatment
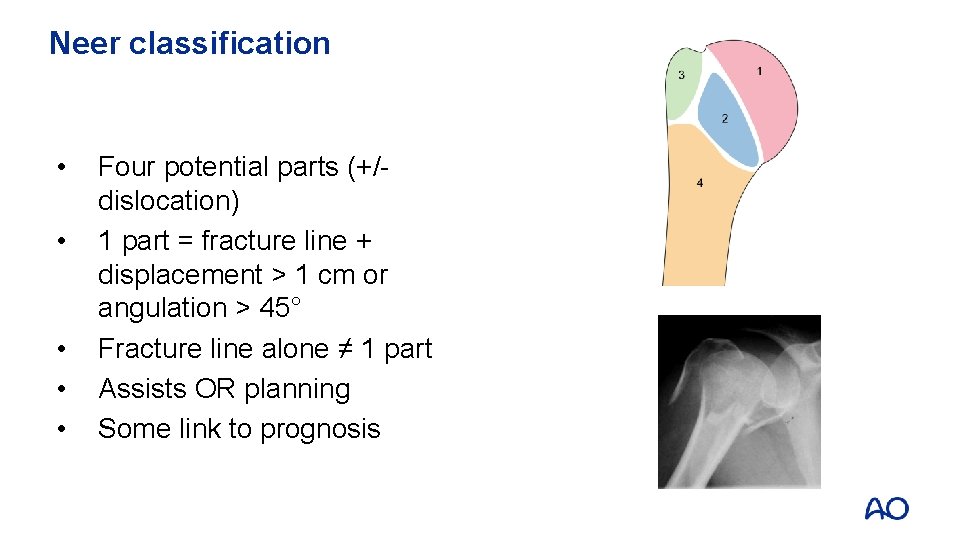
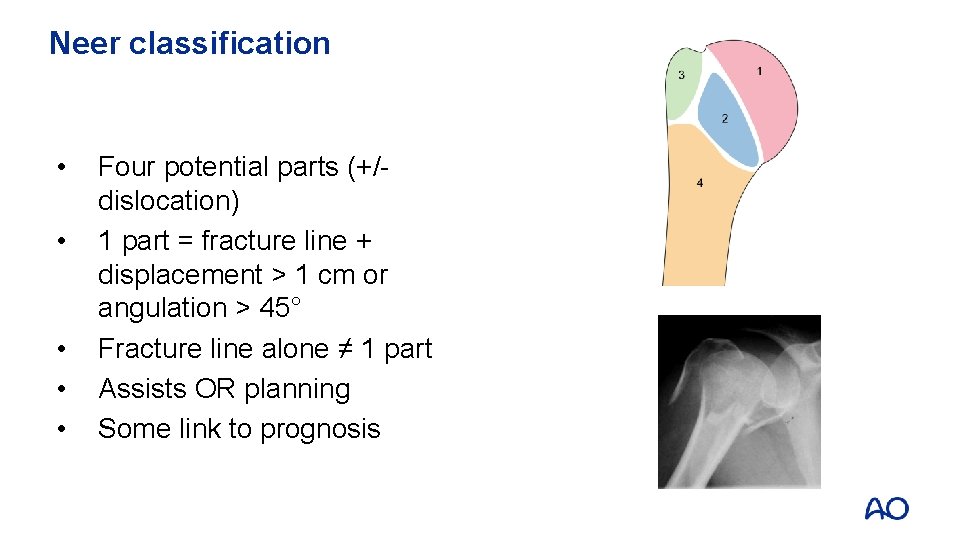
Neer classification • • • Four potential parts (+/dislocation) 1 part = fracture line + displacement > 1 cm or angulation > 45° Fracture line alone ≠ 1 part Assists OR planning Some link to prognosis
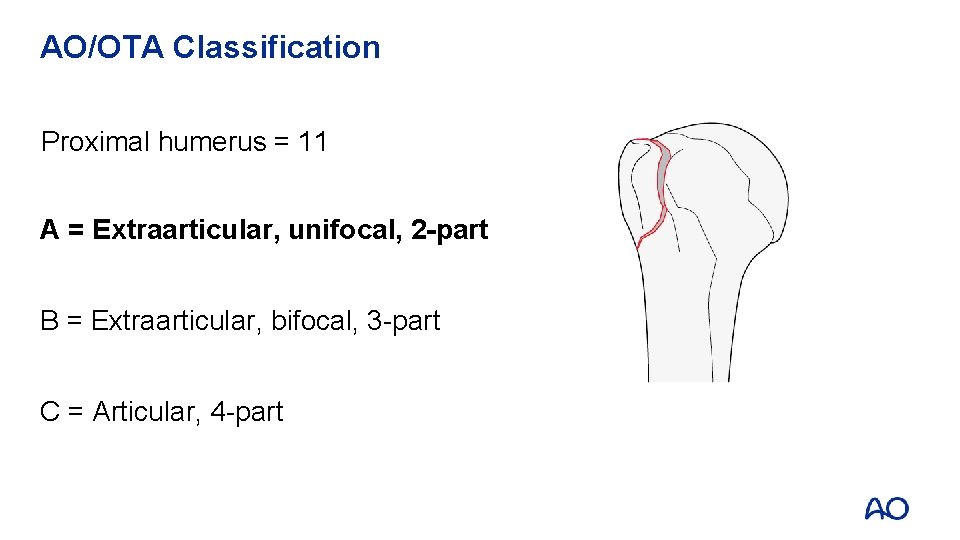
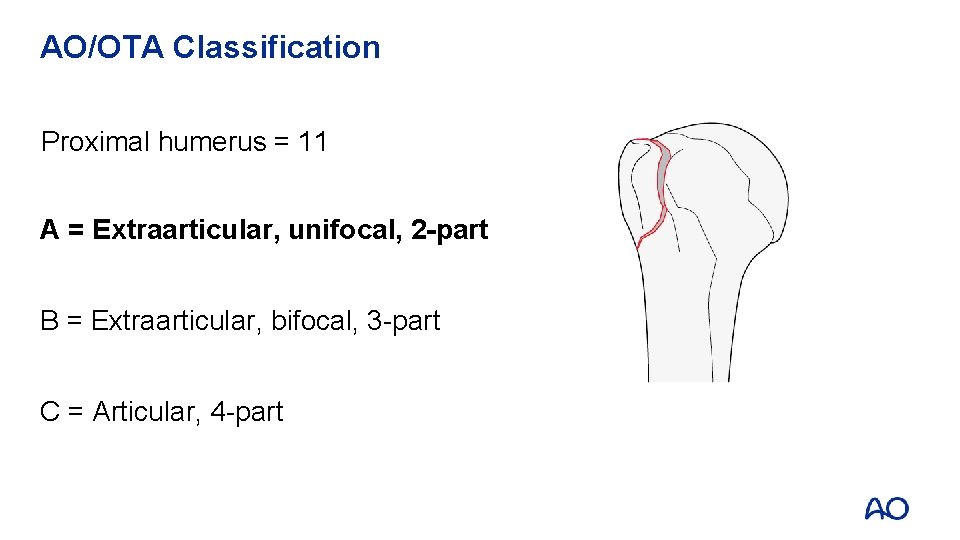
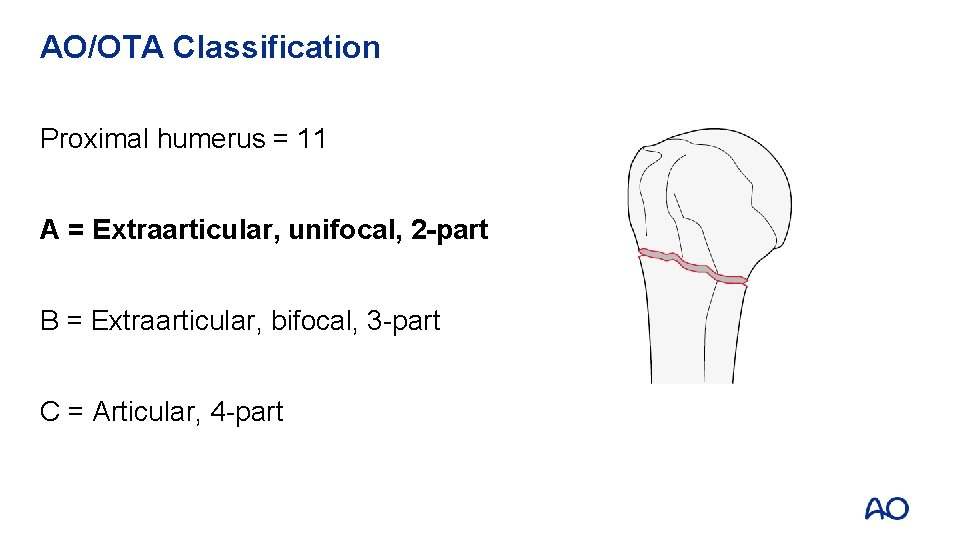
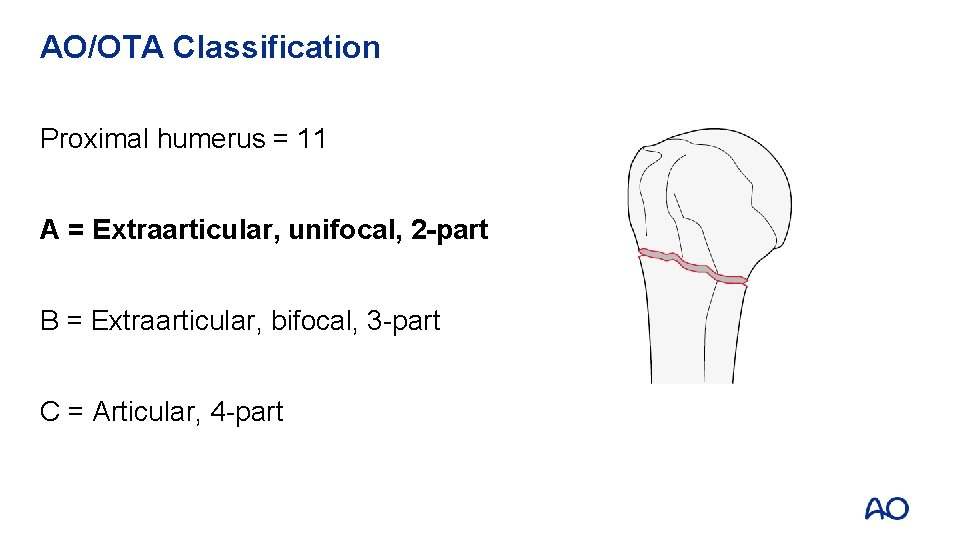
AO/OTA Classification Proximal humerus = 11 A = Extraarticular, unifocal, 2 -part B = Extraarticular, bifocal, 3 -part C = Articular, 4 -part A 1
AO/OTA Classification Proximal humerus = 11 A = Extraarticular, unifocal, 2 -part B = Extraarticular, bifocal, 3 -part C = Articular, 4 -part A 2
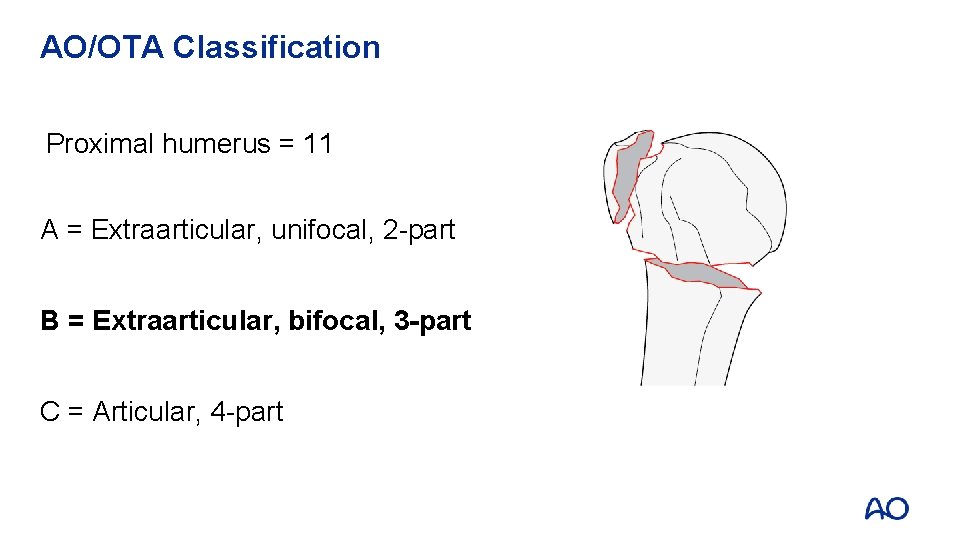
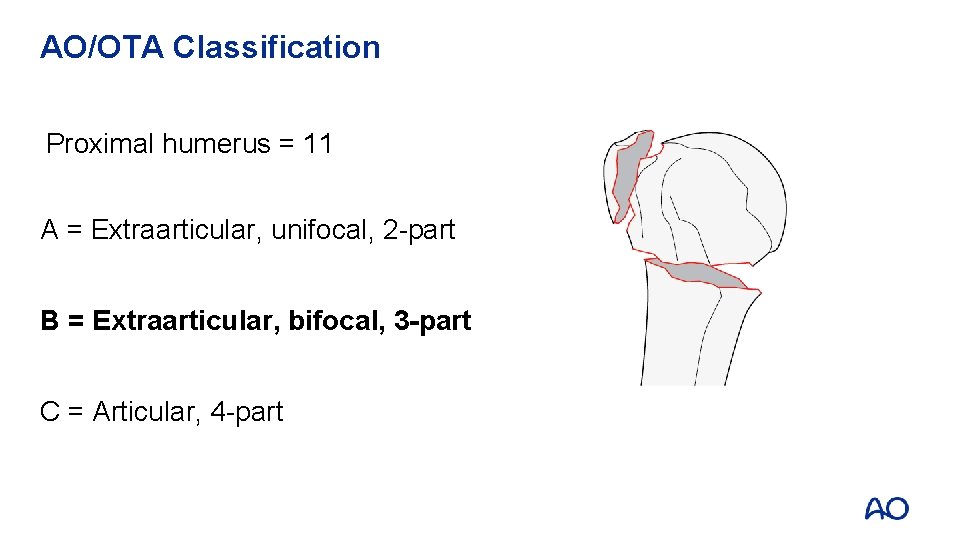
AO/OTA Classification Proximal humerus = 11 A = Extraarticular, unifocal, 2 -part B = Extraarticular, bifocal, 3 -part C = Articular, 4 -part B 1
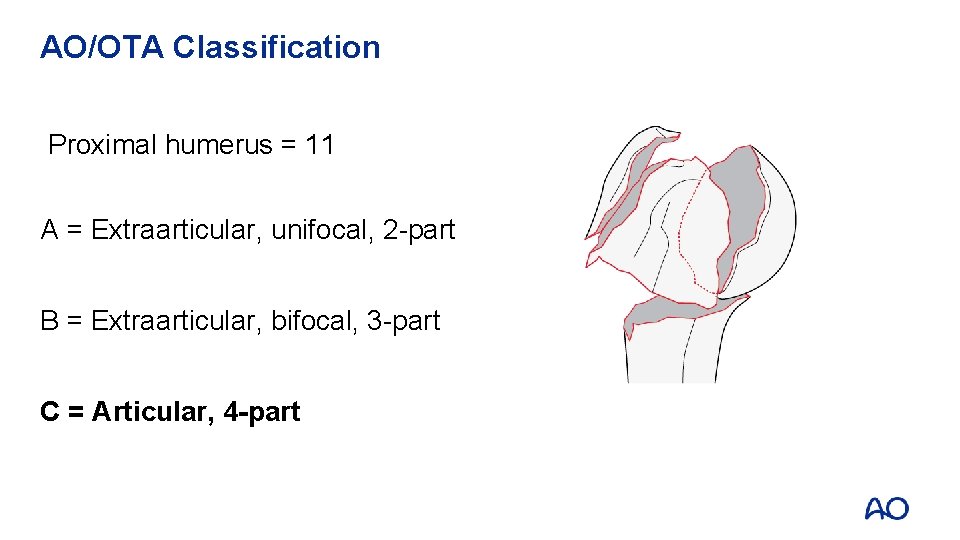
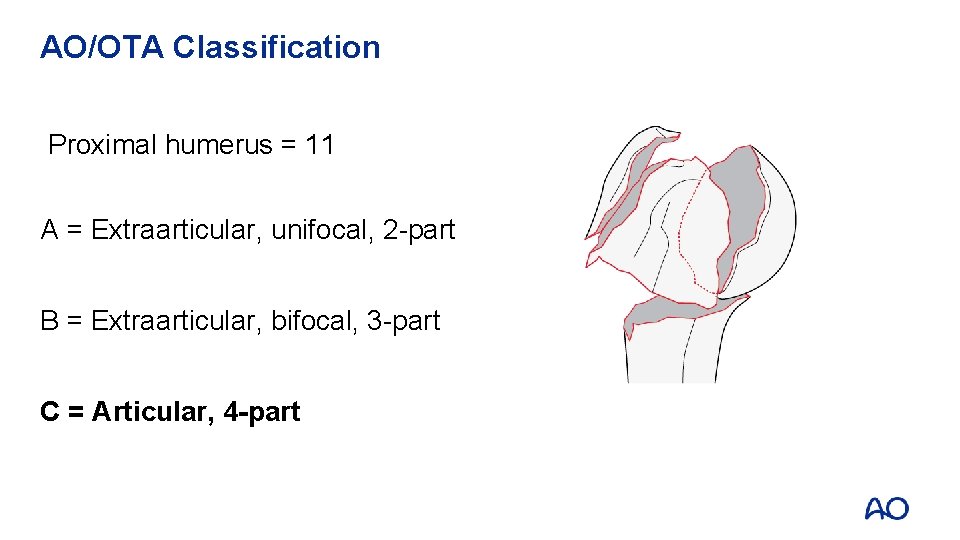
AO/OTA Classification Proximal humerus = 11 A = Extraarticular, unifocal, 2 -part B = Extraarticular, bifocal, 3 -part C = Articular, 4 -part C 1
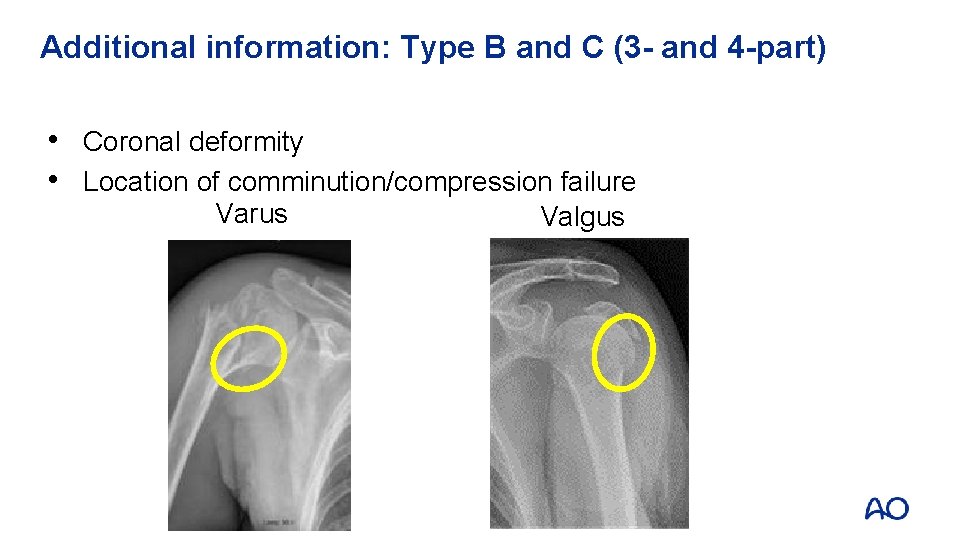
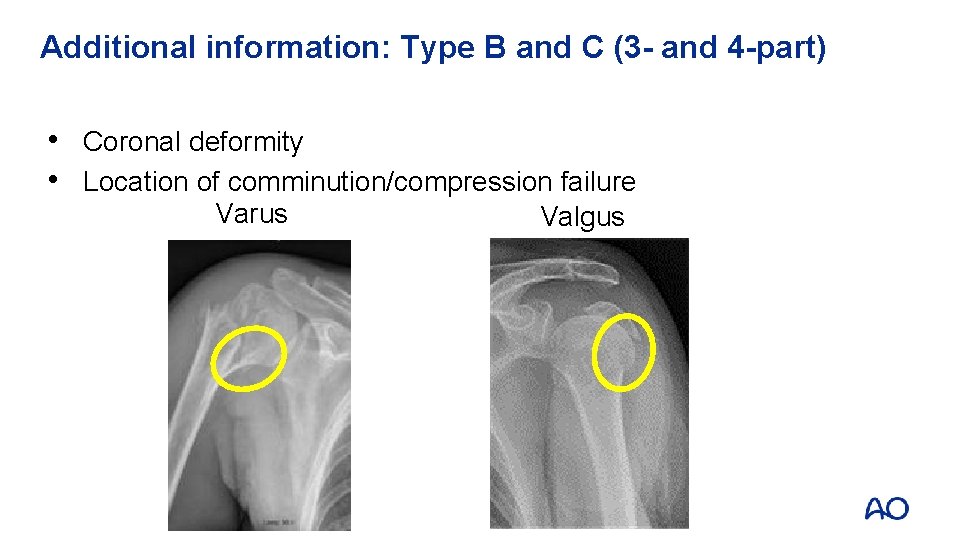
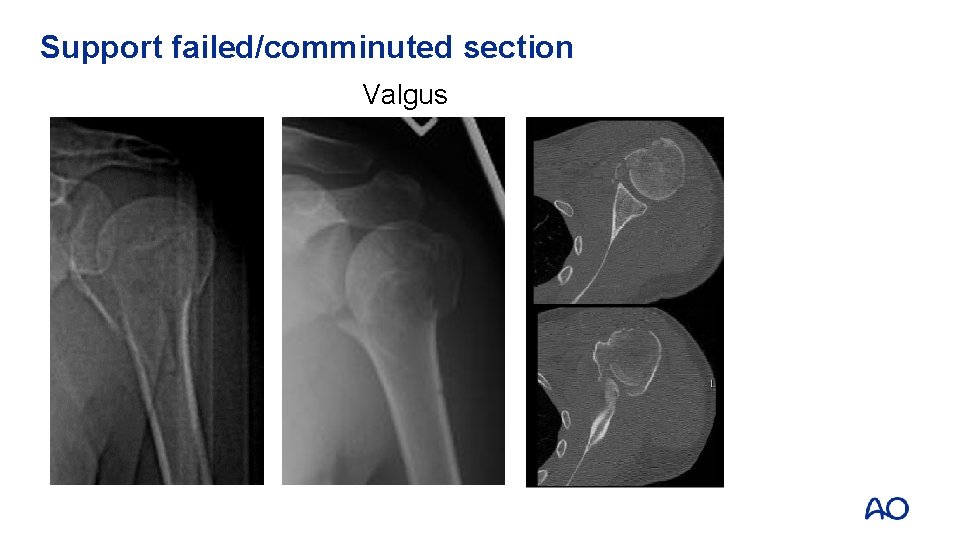
Additional information: Type B and C (3 - and 4 -part) • Coronal deformity • Location of comminution/compression failure Varus Valgus
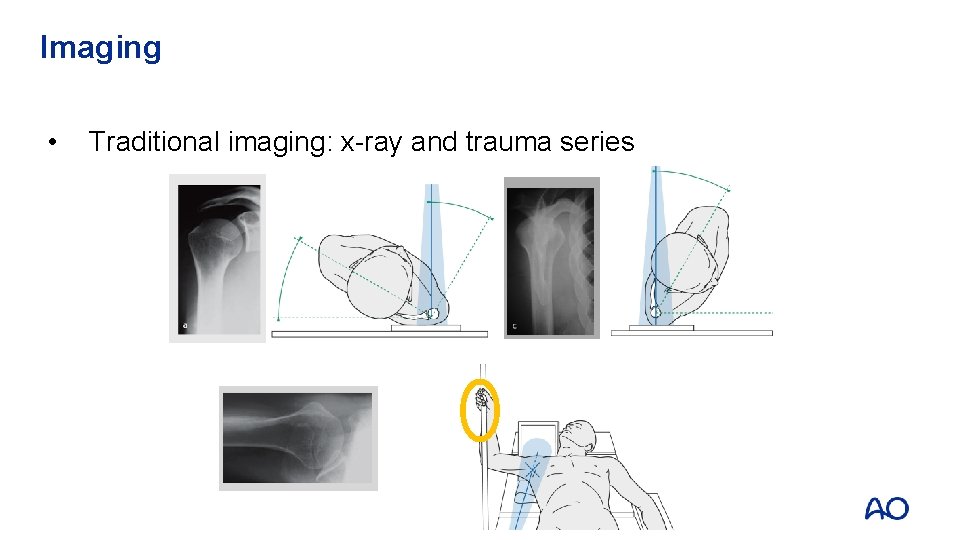
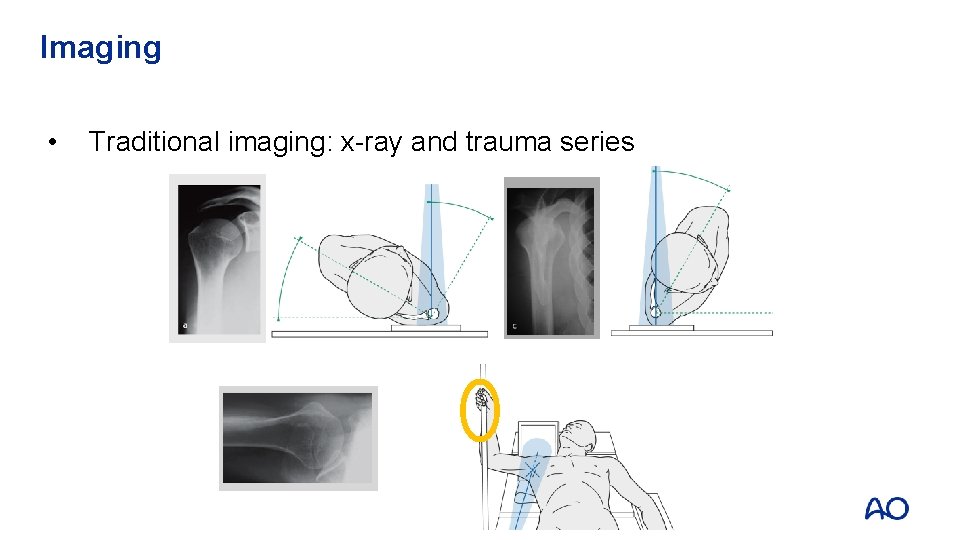
Imaging • Traditional imaging: x-ray and trauma series
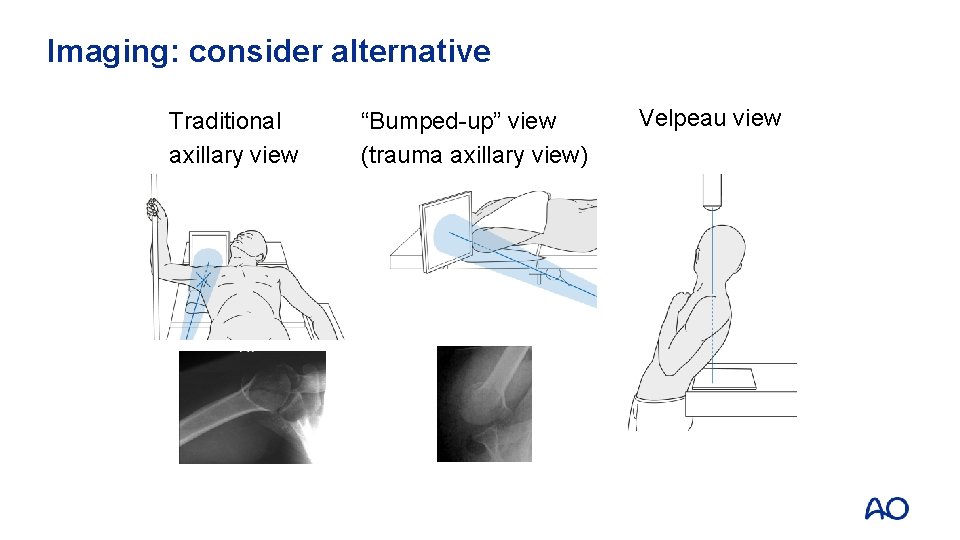
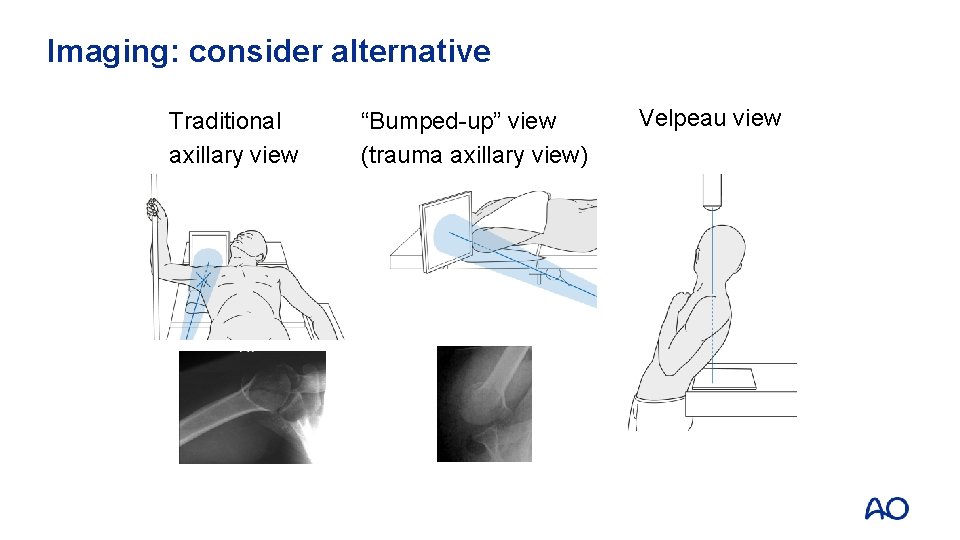
Imaging: consider alternative Traditional axillary view “Bumped-up” view (trauma axillary view) Velpeau view
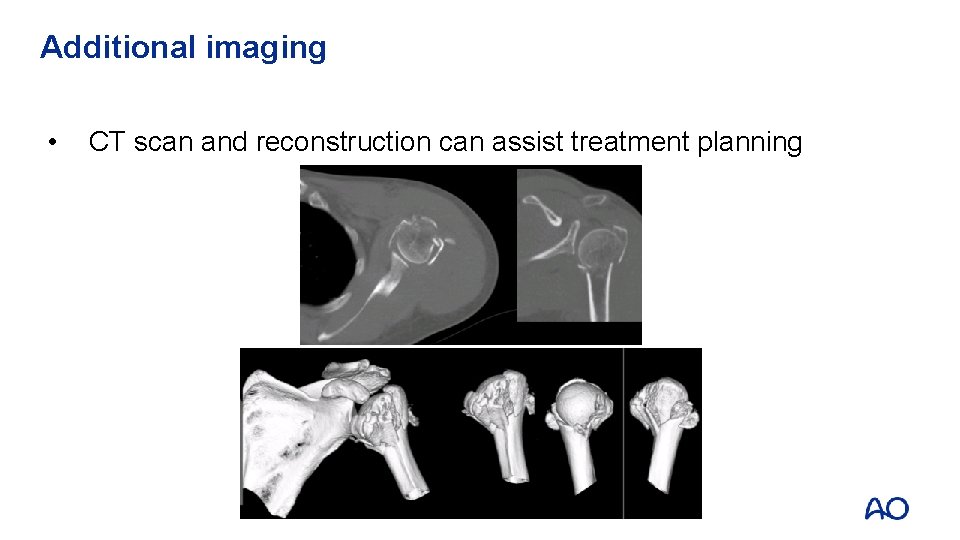
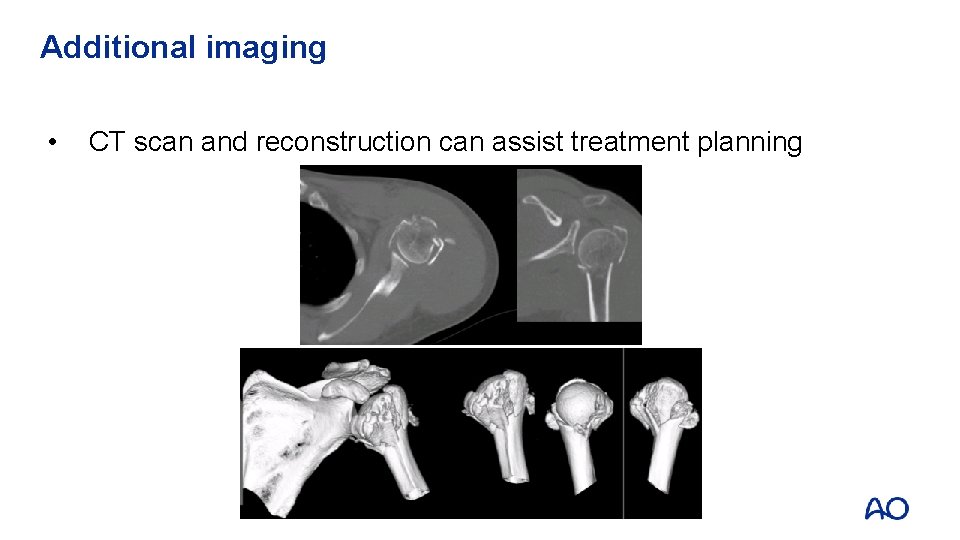
Additional imaging • CT scan and reconstruction can assist treatment planning
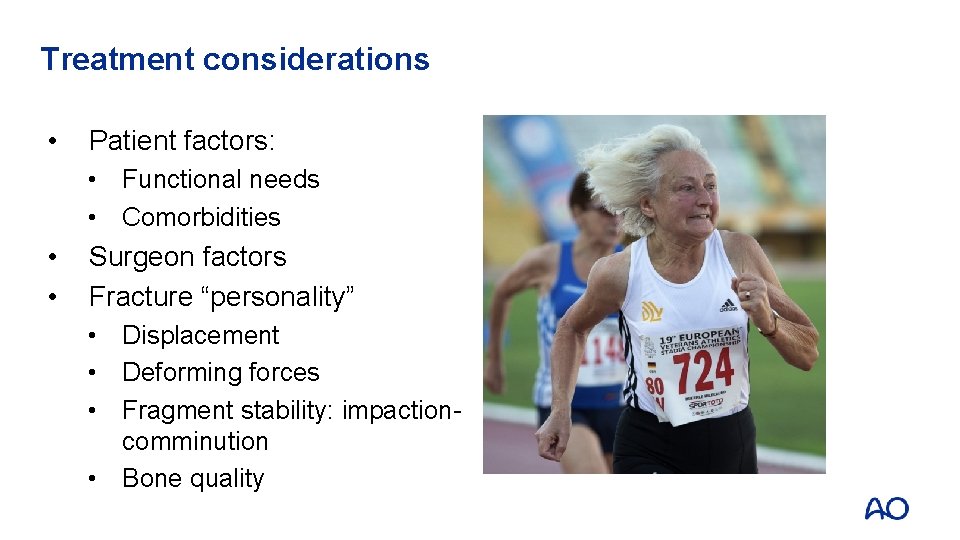
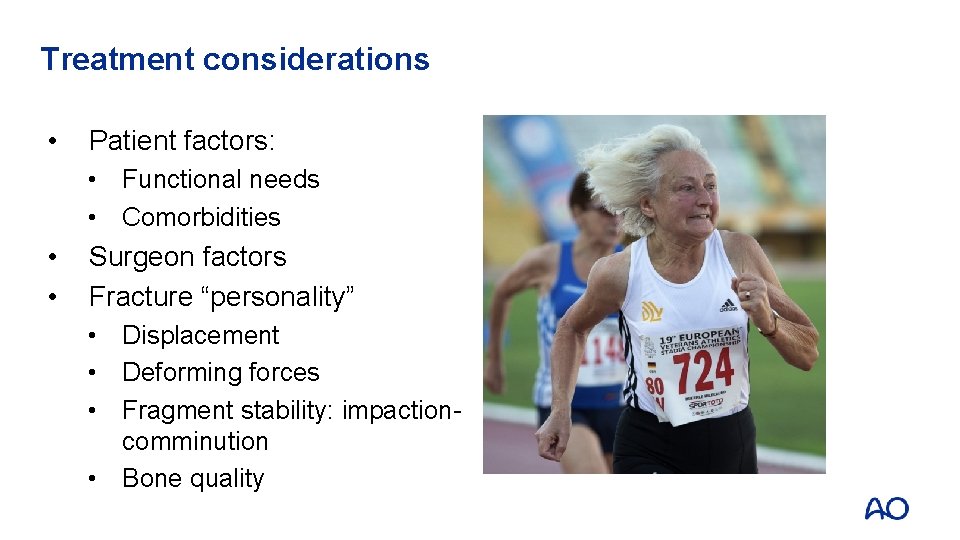
Treatment considerations • Patient factors: • Functional needs • Comorbidities • • Surgeon factors Fracture “personality” • Displacement • Deforming forces • Fragment stability: impactioncomminution • Bone quality
Treatment goals • • Pain control Restore function • Restore and maintain bony/soft tissue anatomy • Initiate early rehabilitation
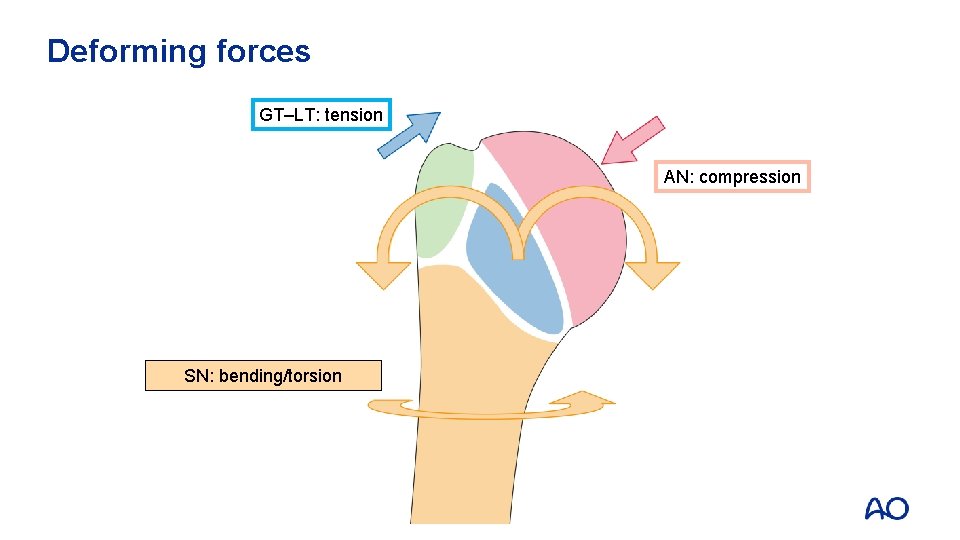
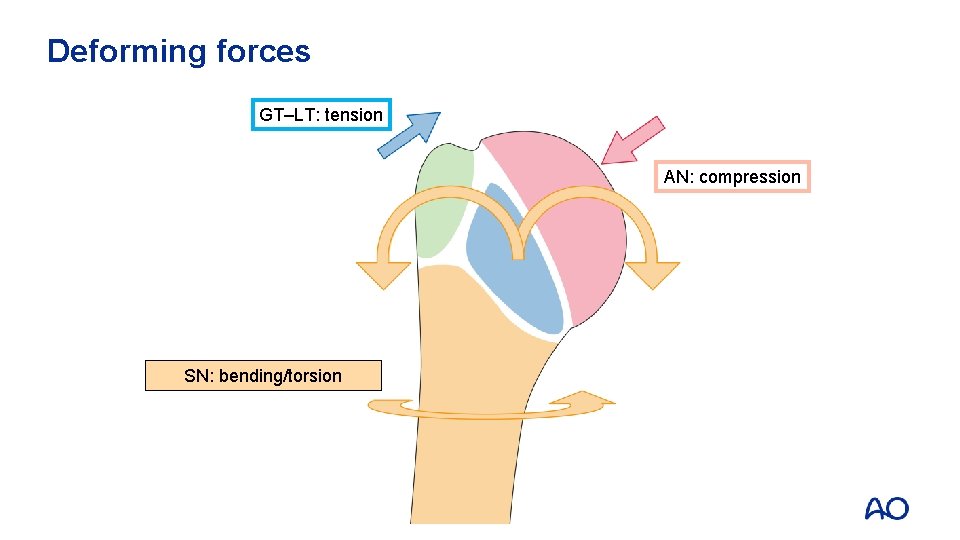
Deforming forces GT–LT: tension AN: compression SN: bending/torsion
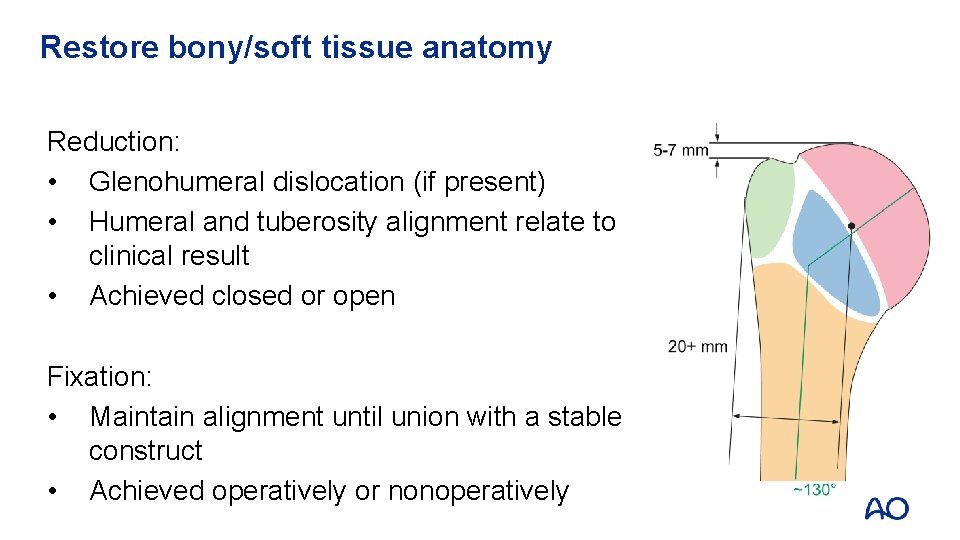
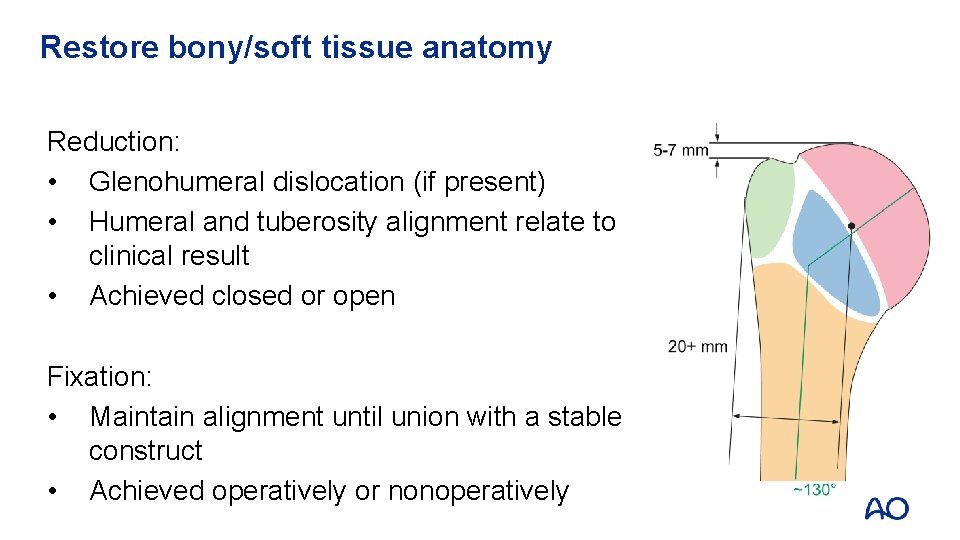
Restore bony/soft tissue anatomy Reduction: • Glenohumeral dislocation (if present) • Humeral and tuberosity alignment relate to clinical result • Achieved closed or open Fixation: • Maintain alignment until union with a stable construct • Achieved operatively or nonoperatively
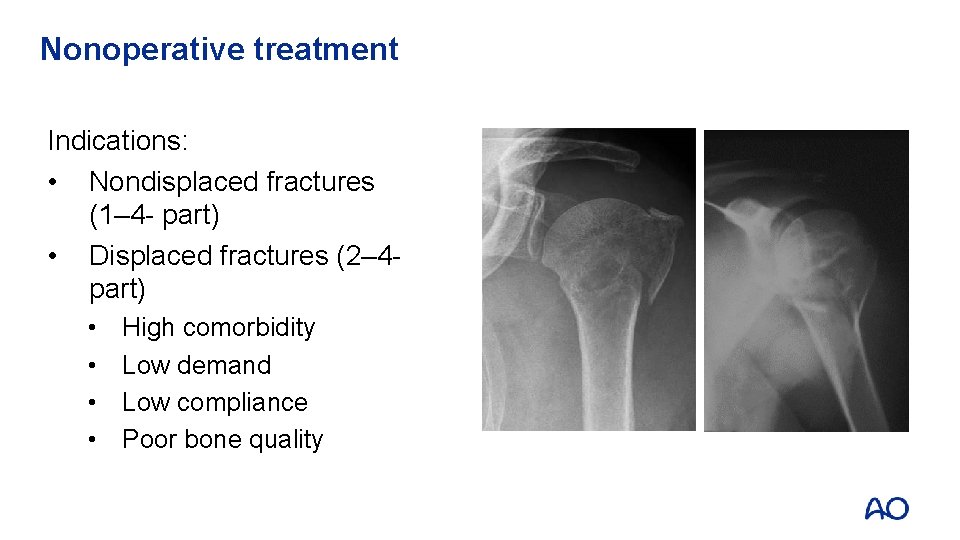
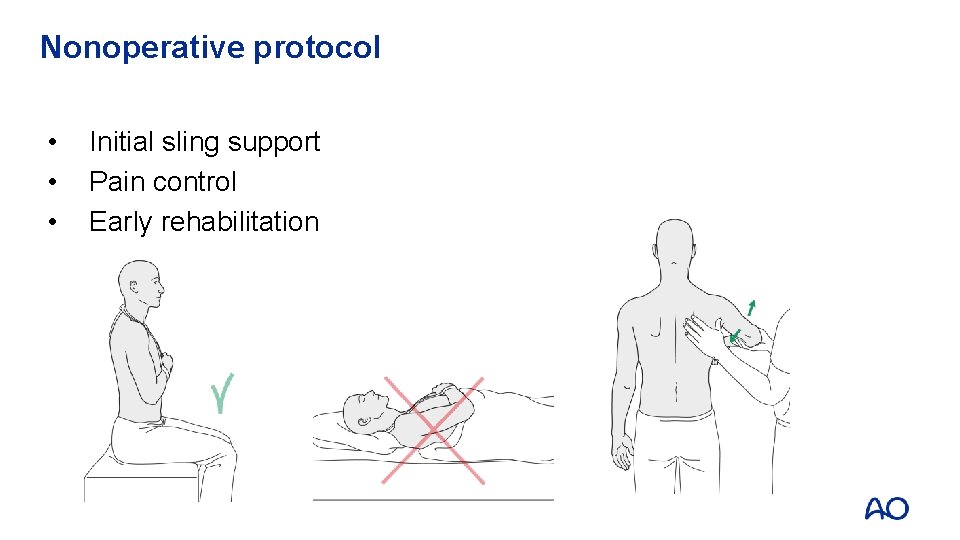
Nonoperative treatment Indications: • Nondisplaced fractures (1– 4 - part) • Displaced fractures (2– 4 part) • • High comorbidity Low demand Low compliance Poor bone quality
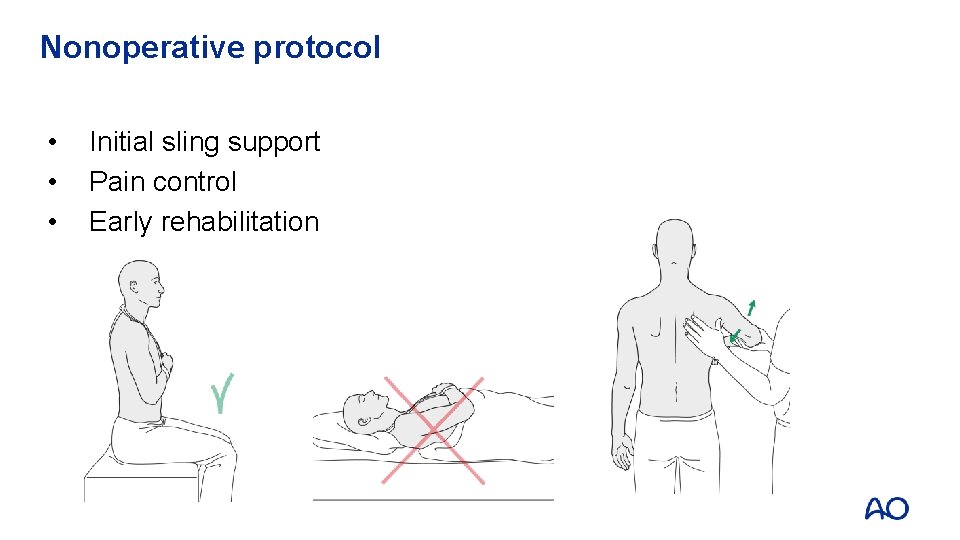
Nonoperative protocol • • • Initial sling support Pain control Early rehabilitation
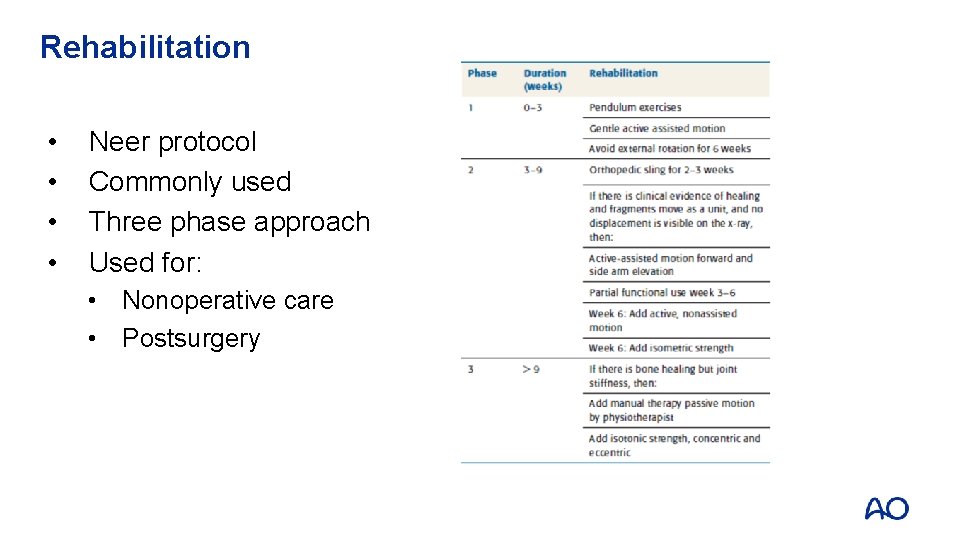
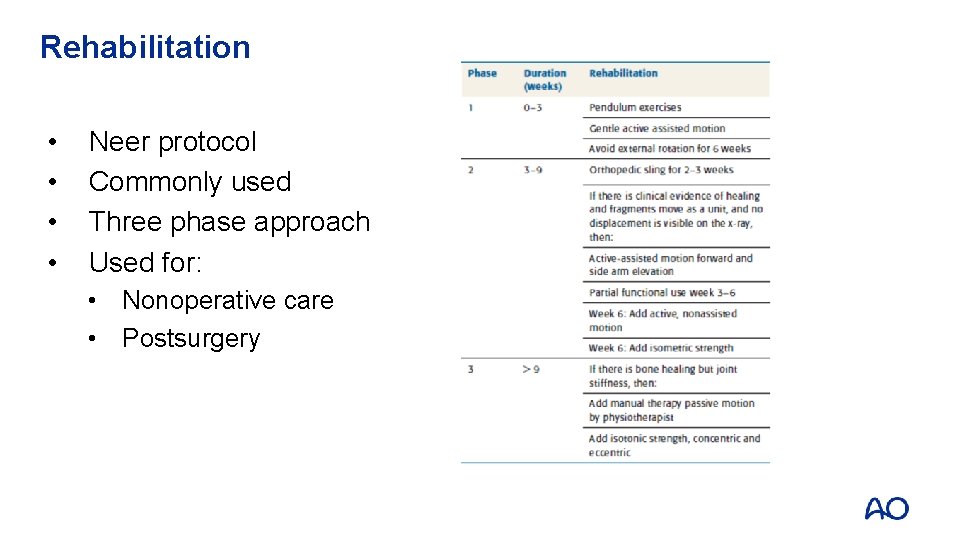
Rehabilitation • • Neer protocol Commonly used Three phase approach Used for: • Nonoperative care • Postsurgery
Nonoperative outcome • • • Simple A 2, A 3 Multifragmentary but nondisplaced Standardized therapy regimen About 75% are good to excellent results Best when therapy starts less than 14 days post injury
Operative versus nonoperative treatment for 2 -part proximal humerus fracture: A multicenter randomized controlled trial (RCT) • 88 patients aged 60 years or older • Displaced 2 -part PHF into 2 groups (conservative vs ORIF) • We recorded the disabilities of arm, shoulder, and hand (DASH) score, other measures of shoulder function and quality of life, and complications at 2 -year follow-up. • No significant or clinically important between-group differences in all outcomes. Published: July 18, 2019 https: //doi. org/10. 1371/journal. pmed. 1002855
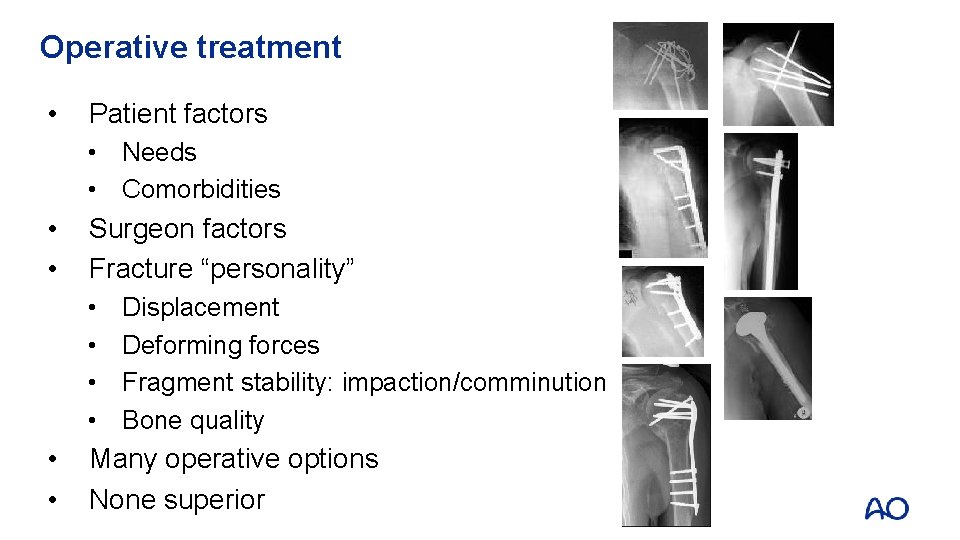
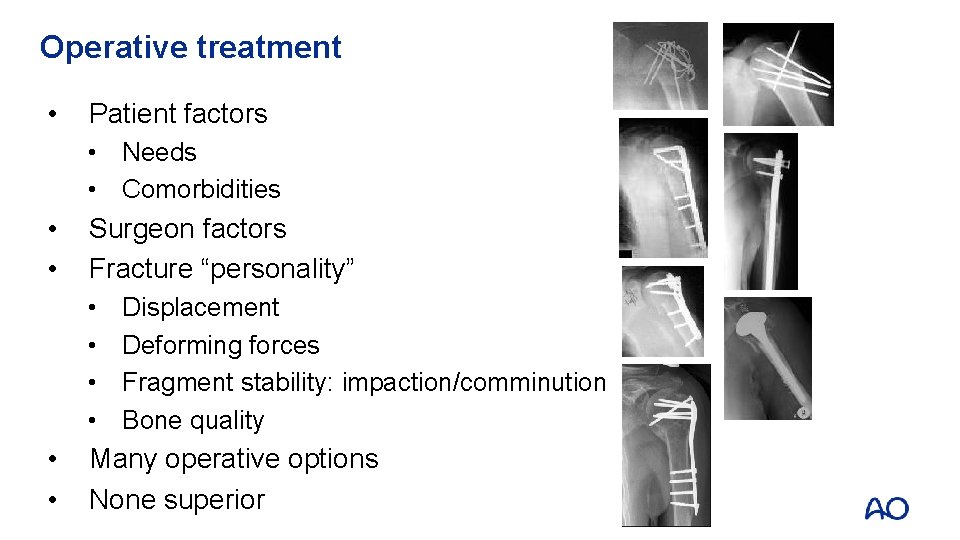
Operative treatment • Patient factors • Needs • Comorbidities • • Surgeon factors Fracture “personality” • • • Displacement Deforming forces Fragment stability: impaction/comminution Bone quality Many operative options None superior
Operative indications • • Open fracture Associated dislocation Displaced tuberosity fractures Displaced/unstable 2 -part fractures 3/4 -part fractures (young/active patients) 4 -part valgus-impacted fractures In the elderly, the indications for surgery are relative
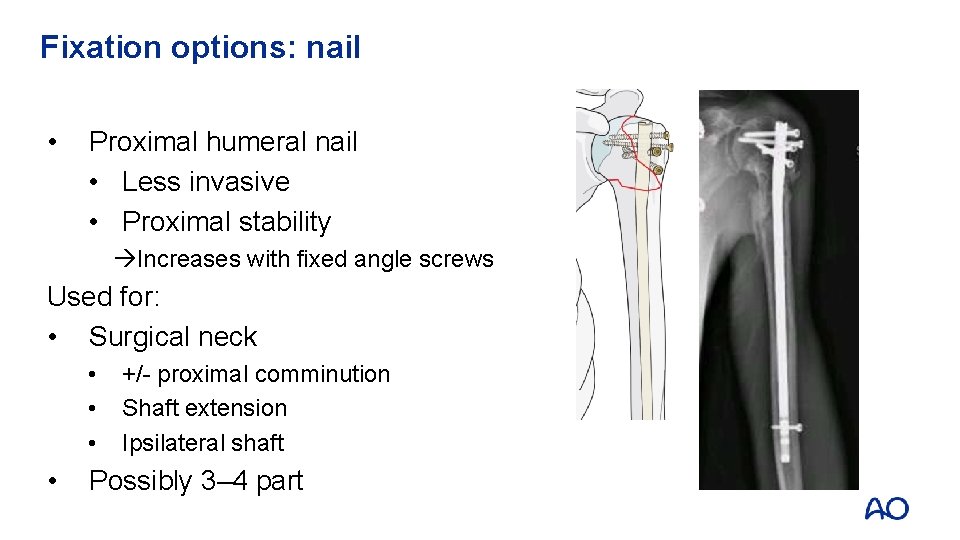
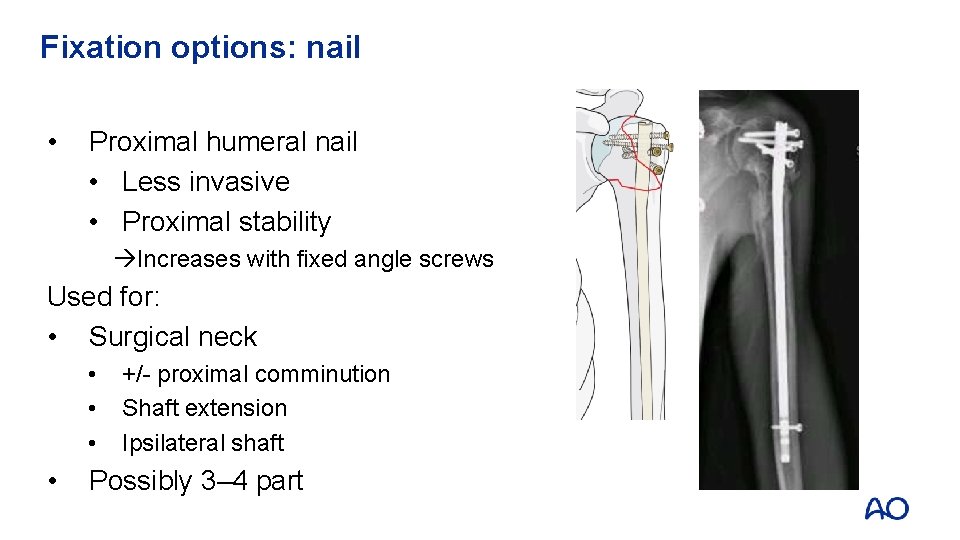
Fixation options: nail • Proximal humeral nail • Less invasive • Proximal stability Increases with fixed angle screws Used for: • Surgical neck • • +/- proximal comminution Shaft extension Ipsilateral shaft Possibly 3– 4 part
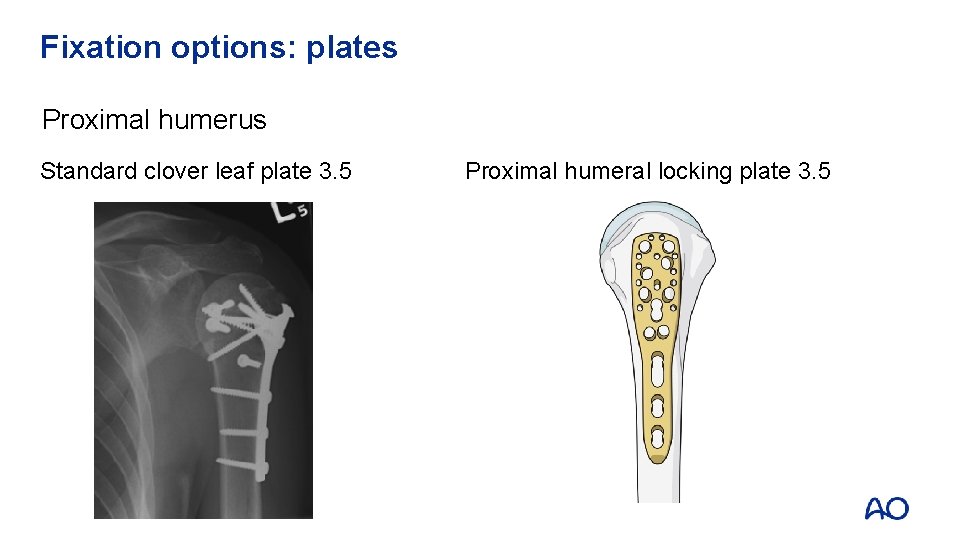
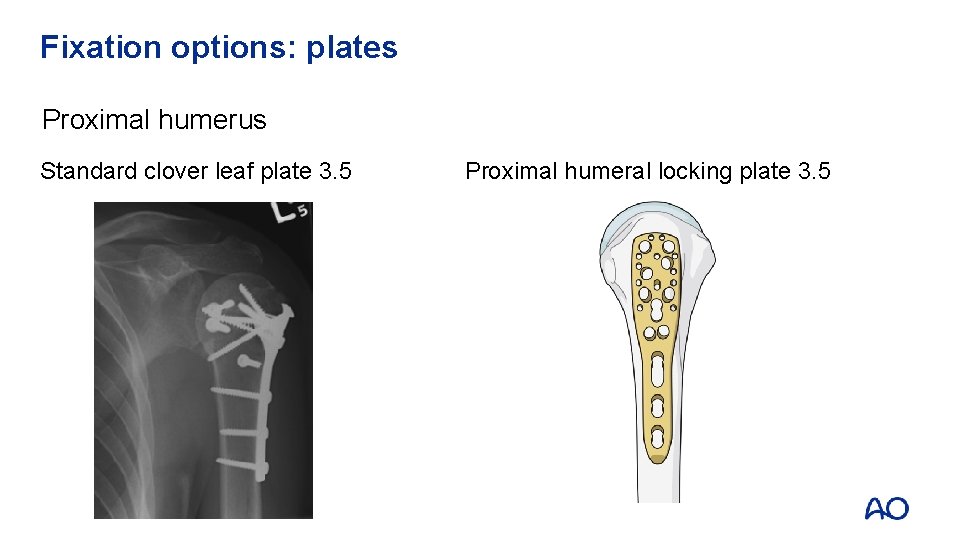
Fixation options: plates Proximal humerus Standard clover leaf plate 3. 5 Proximal humeral locking plate 3. 5
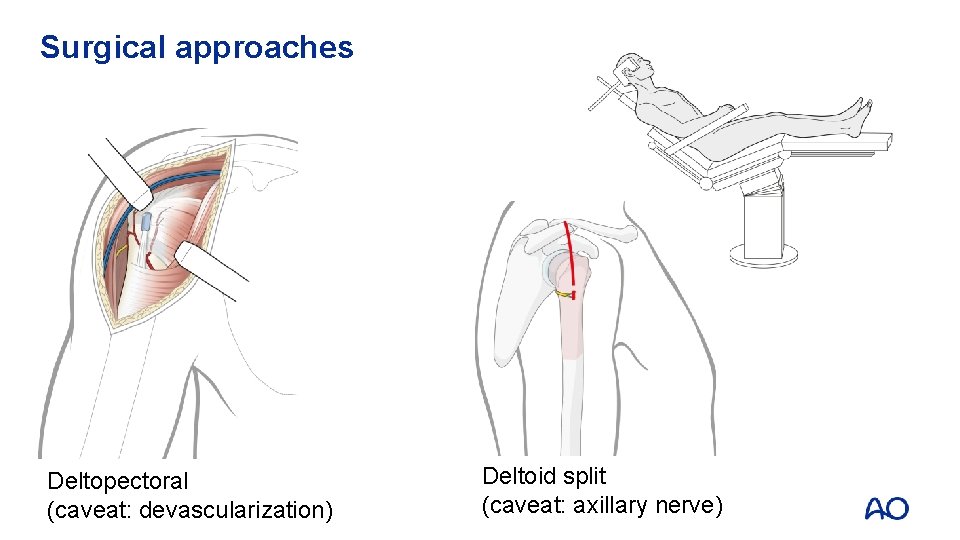
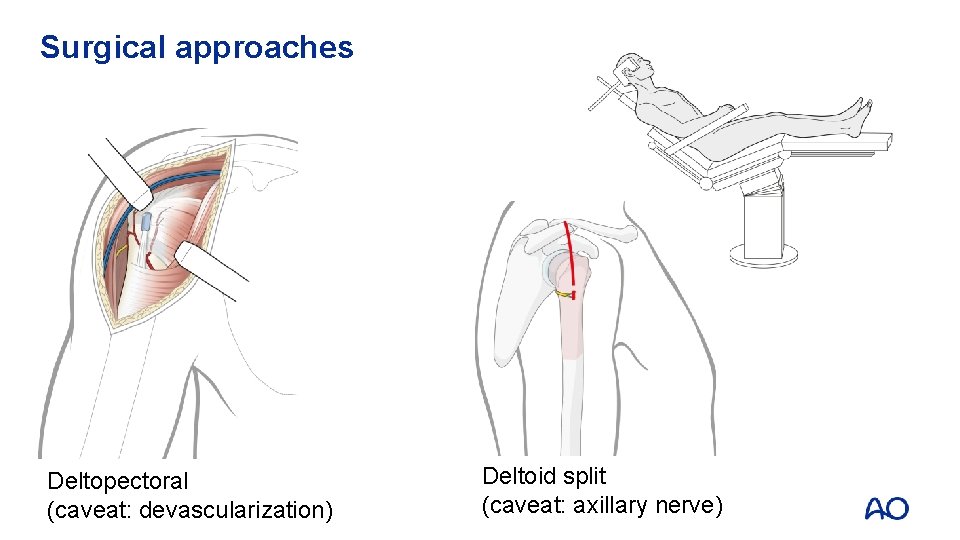
Surgical approaches Deltopectoral (caveat: devascularization) Deltoid split (caveat: axillary nerve)
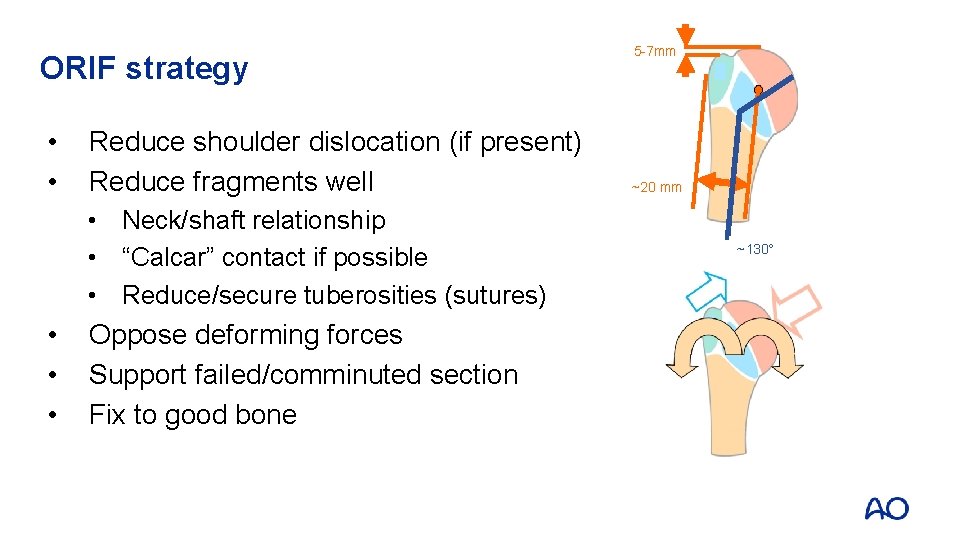
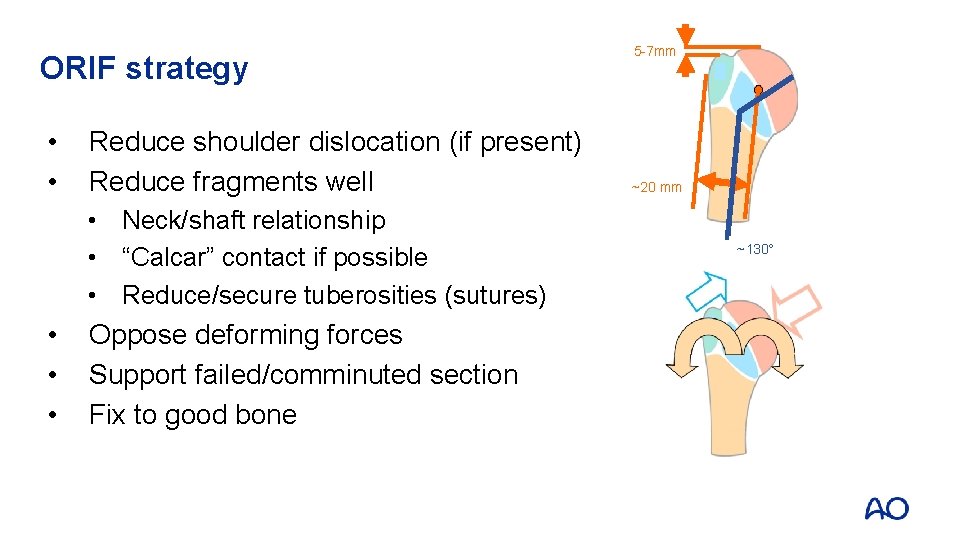
ORIF strategy • • Reduce shoulder dislocation (if present) Reduce fragments well • Neck/shaft relationship • “Calcar” contact if possible • Reduce/secure tuberosities (sutures) • • • Oppose deforming forces Support failed/comminuted section Fix to good bone 5 -7 mm ~20 mm ~130
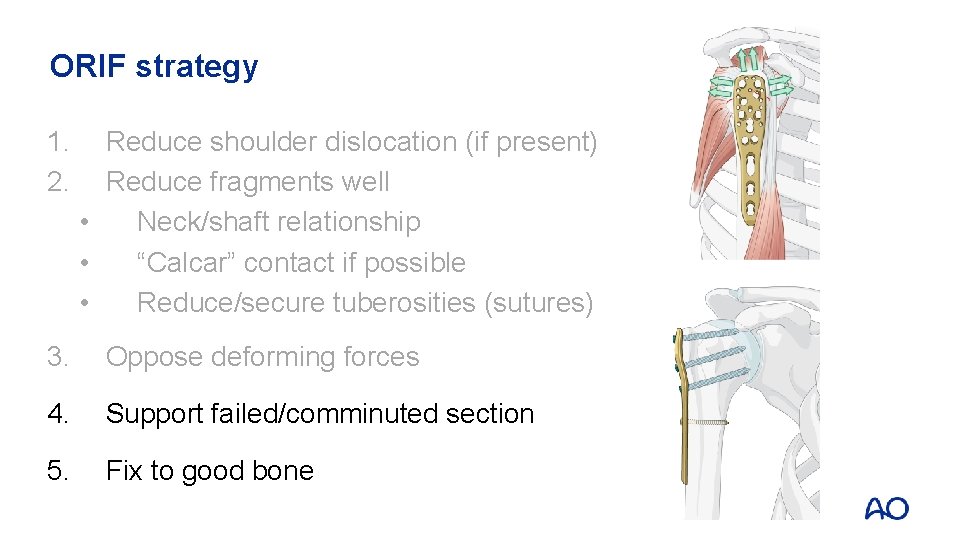
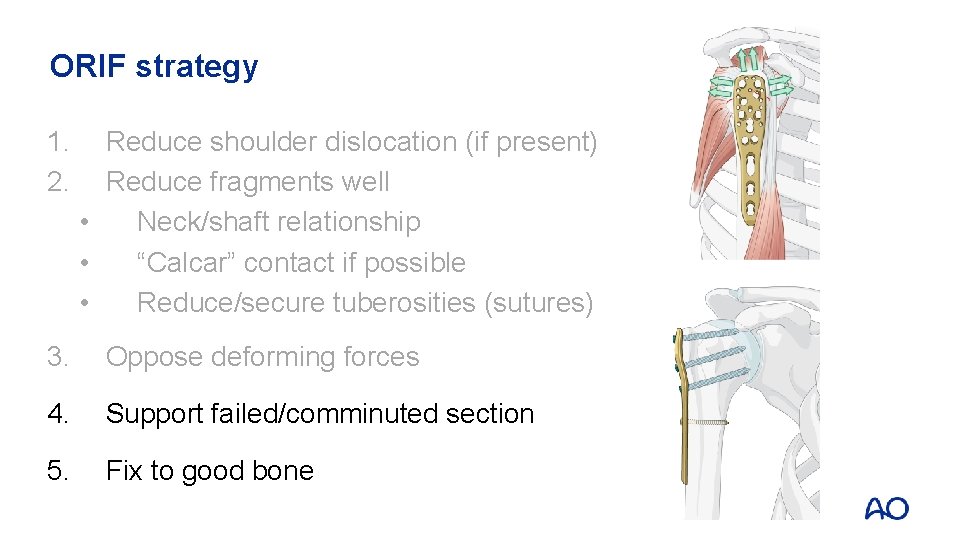
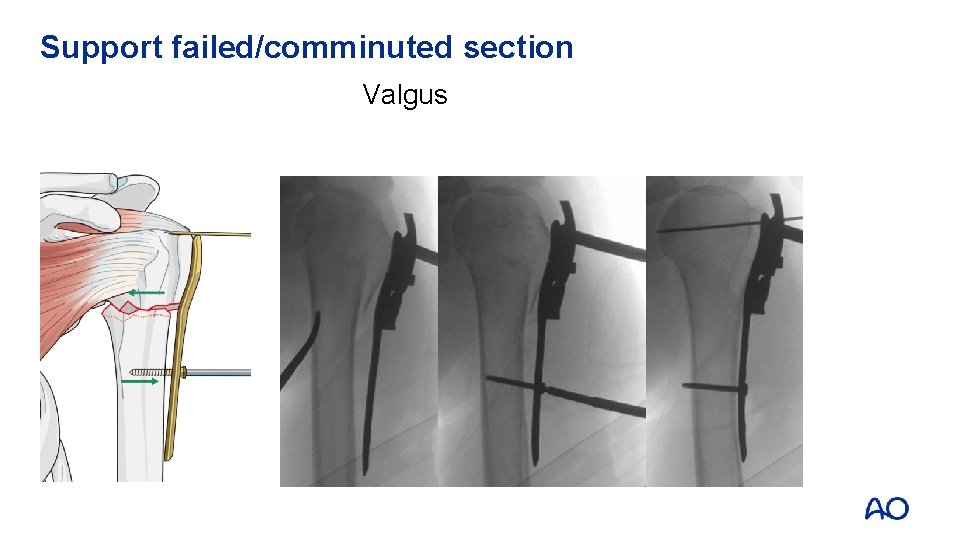
ORIF strategy 1. 2. Reduce shoulder dislocation (if present) Reduce fragments well • Neck/shaft relationship • “Calcar” contact if possible • Reduce/secure tuberosities (sutures) 3. Oppose deforming forces 4. Support failed/comminuted section 5. Fix to good bone
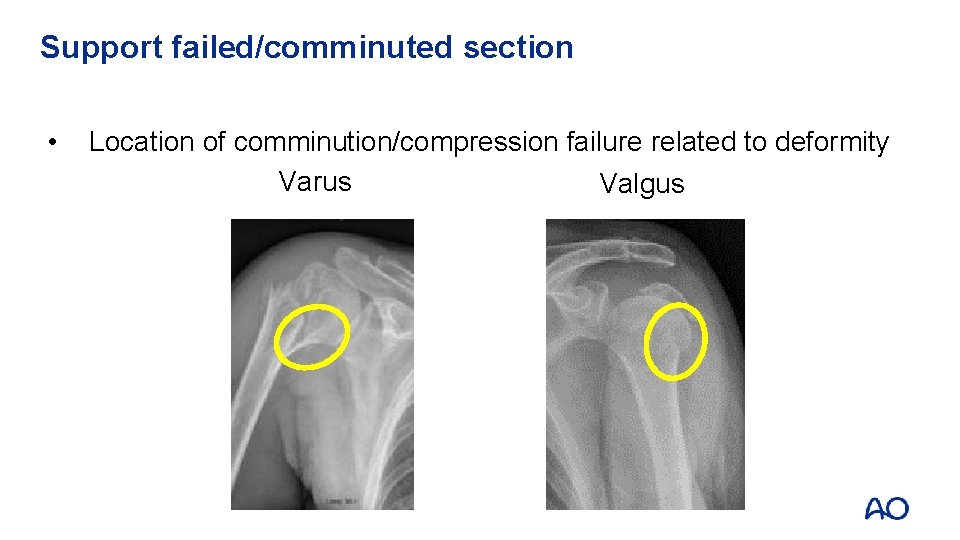
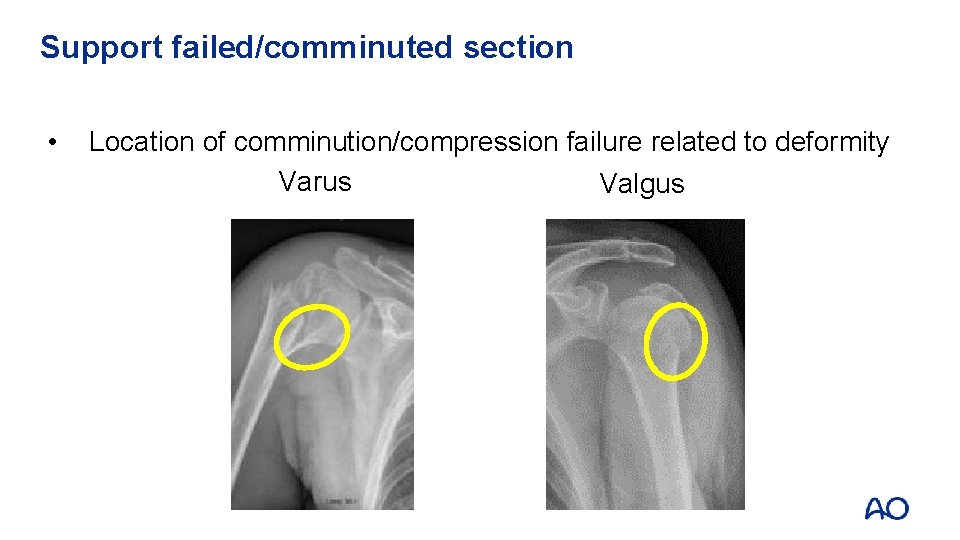
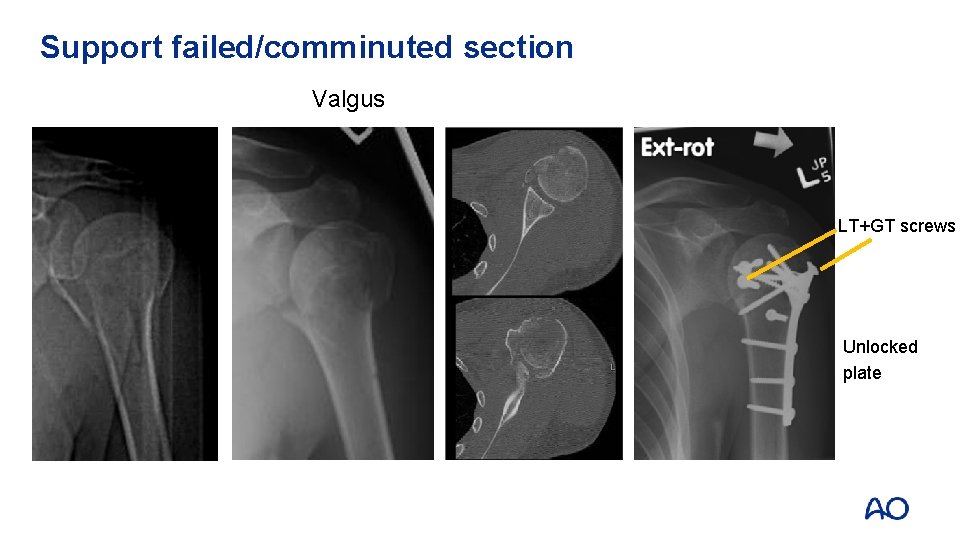
Support failed/comminuted section • Location of comminution/compression failure related to deformity Varus Valgus
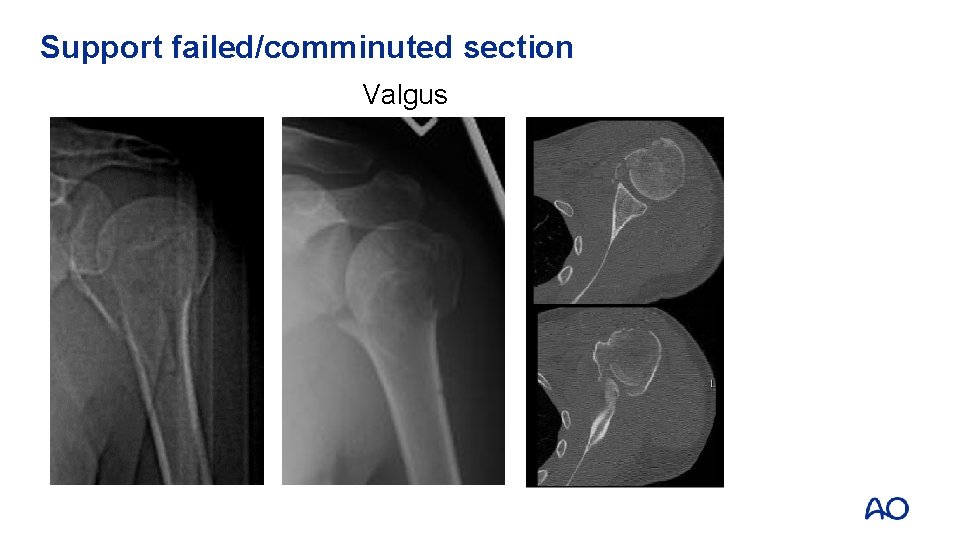
Support failed/comminuted section Valgus
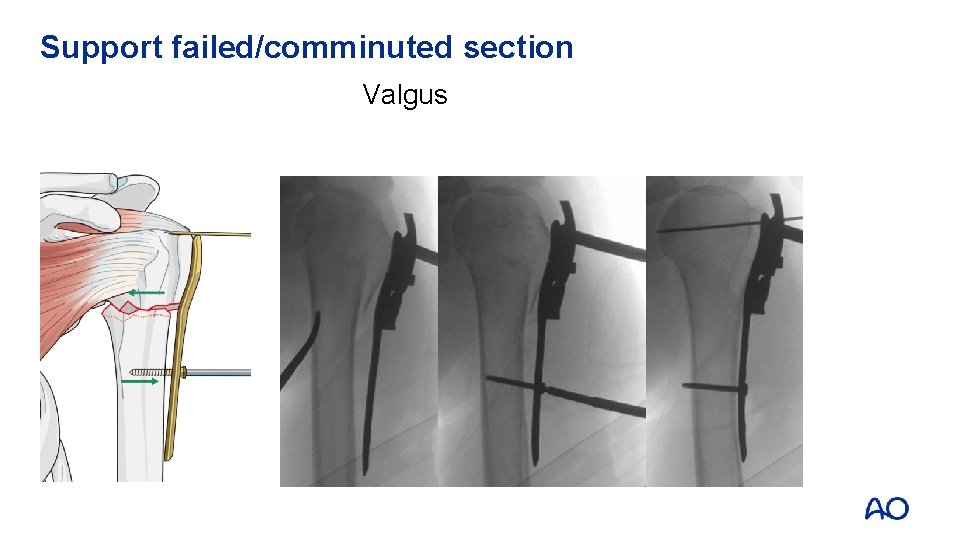
Support failed/comminuted section Valgus
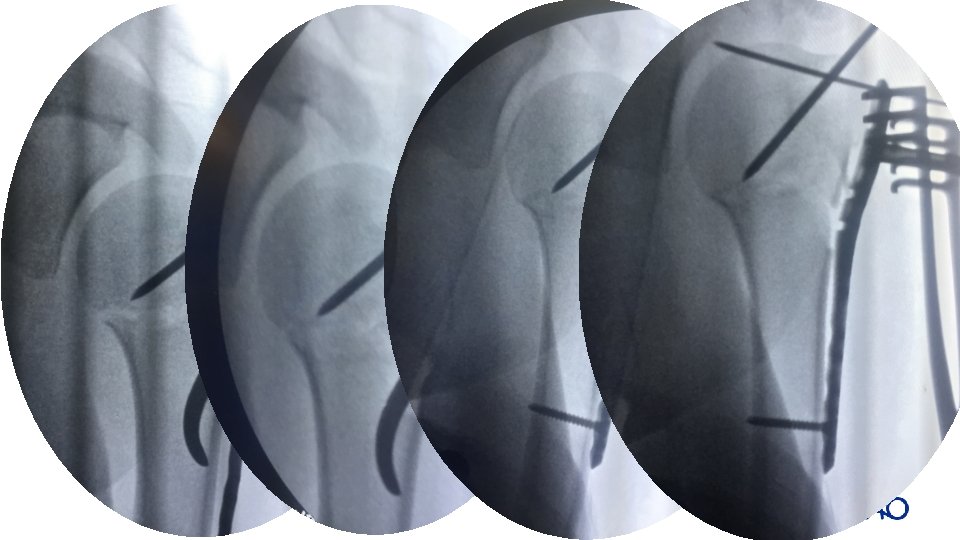
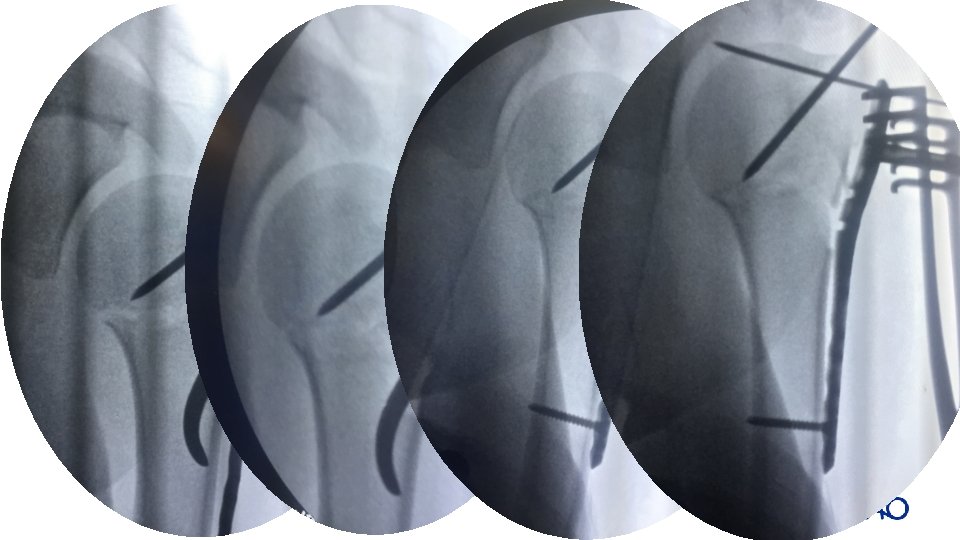
Reduction • • • Use direct or indirect Minimally invasive reduction could be achieved with K-wire joystick manipulation If not, go for open reduction
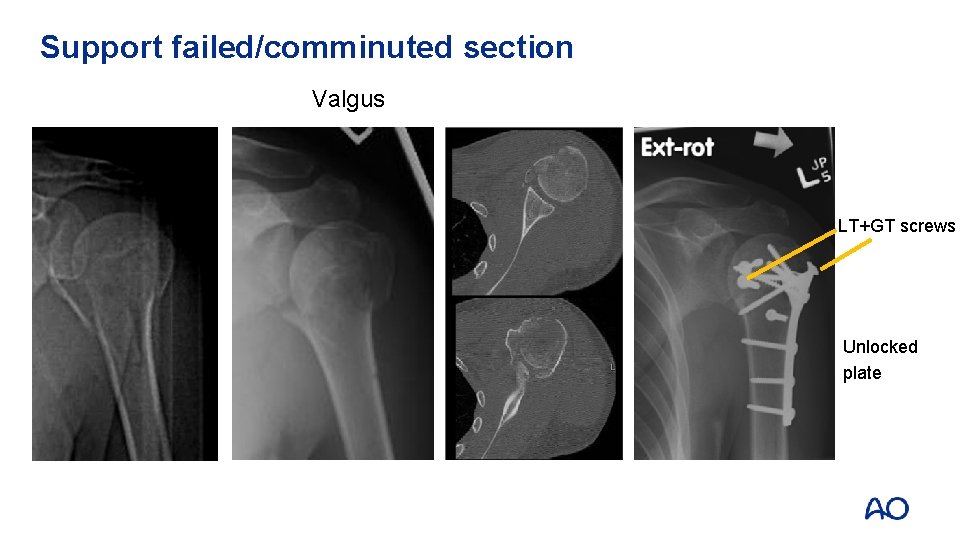
Support failed/comminuted section Valgus LT+GT screws Unlocked plate
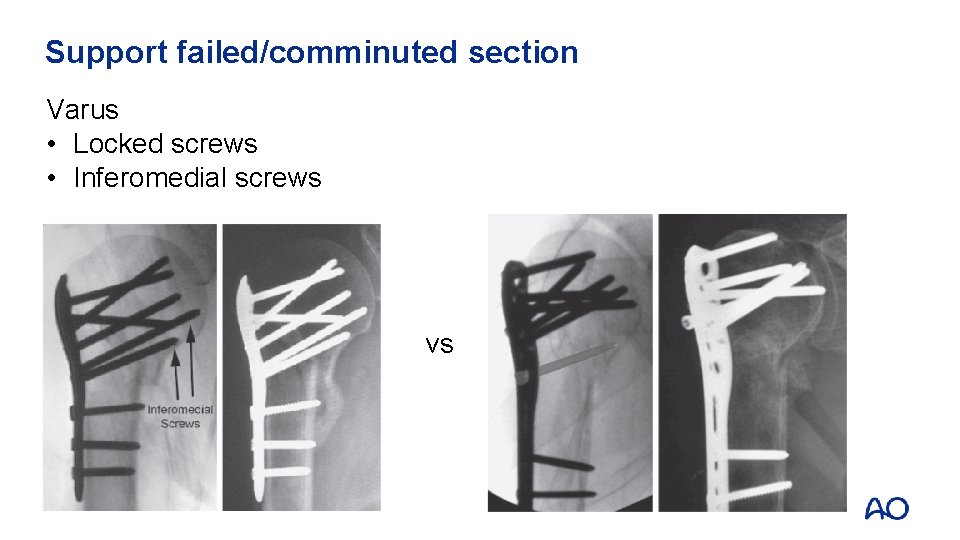
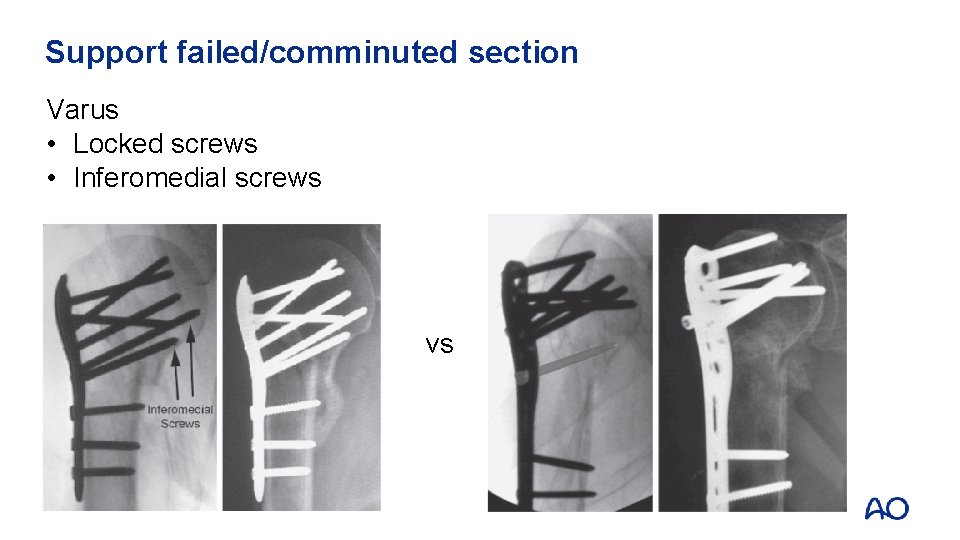
Support failed/comminuted section Varus • Locked screws • Inferomedial screws vs
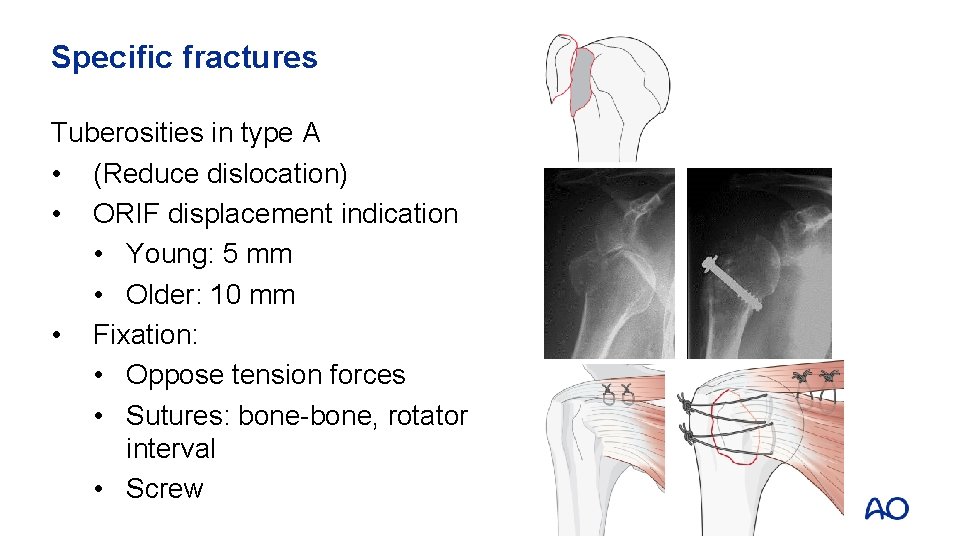
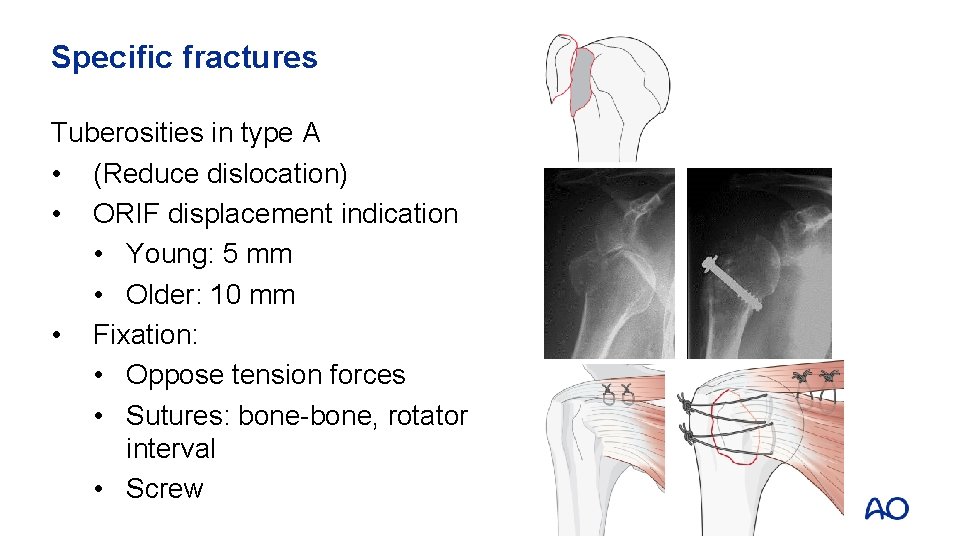
Specific fractures Tuberosities in type A • (Reduce dislocation) • ORIF displacement indication • Young: 5 mm • Older: 10 mm • Fixation: • Oppose tension forces • Sutures: bone-bone, rotator interval • Screw
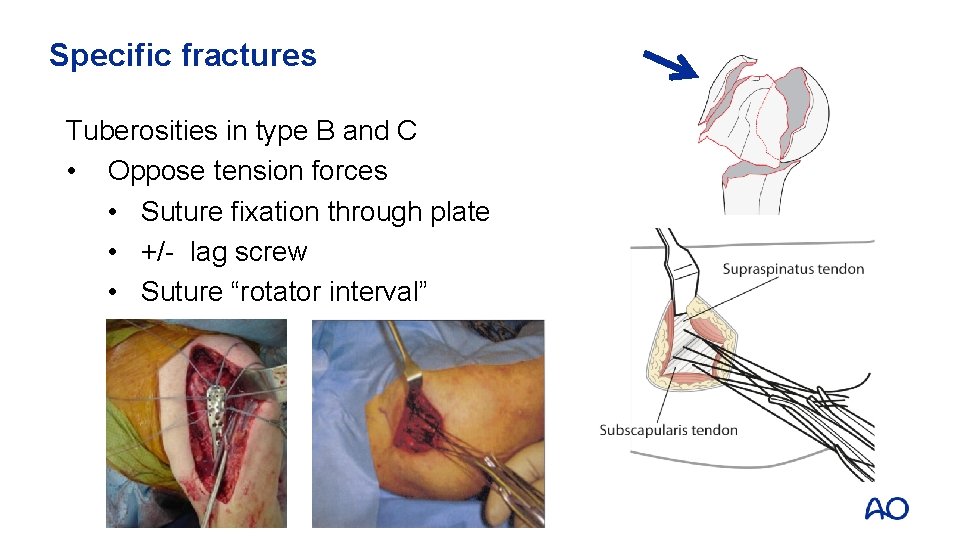
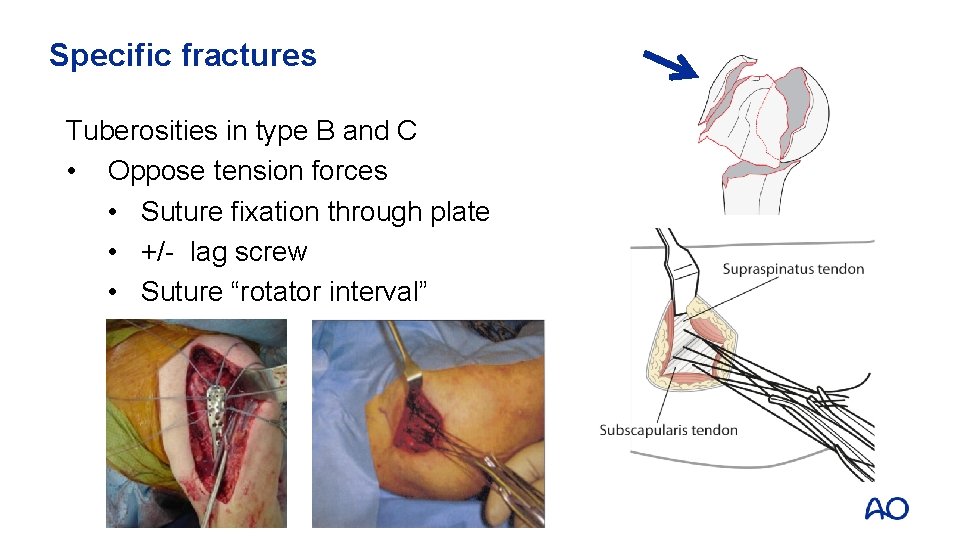
Specific fractures Tuberosities in type B and C • Oppose tension forces • Suture fixation through plate • +/- lag screw • Suture “rotator interval”
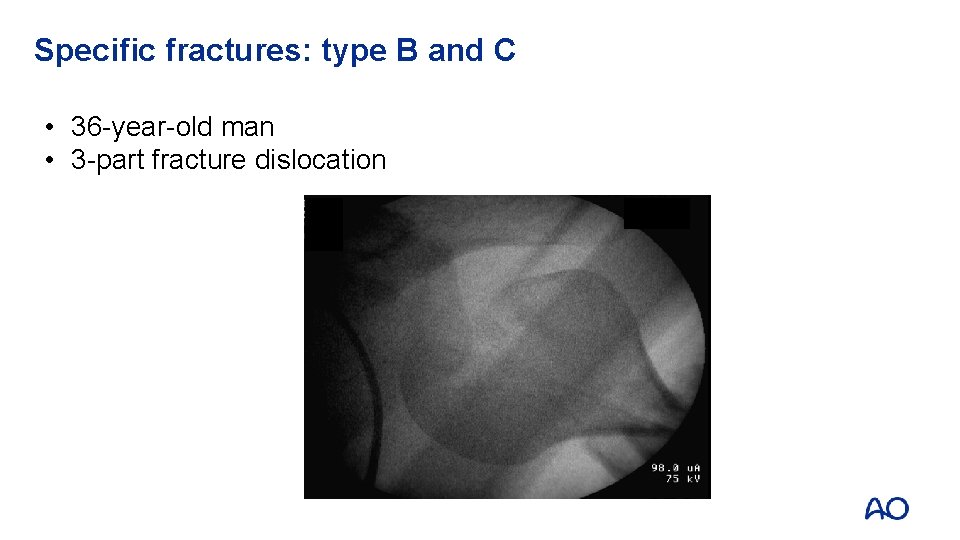
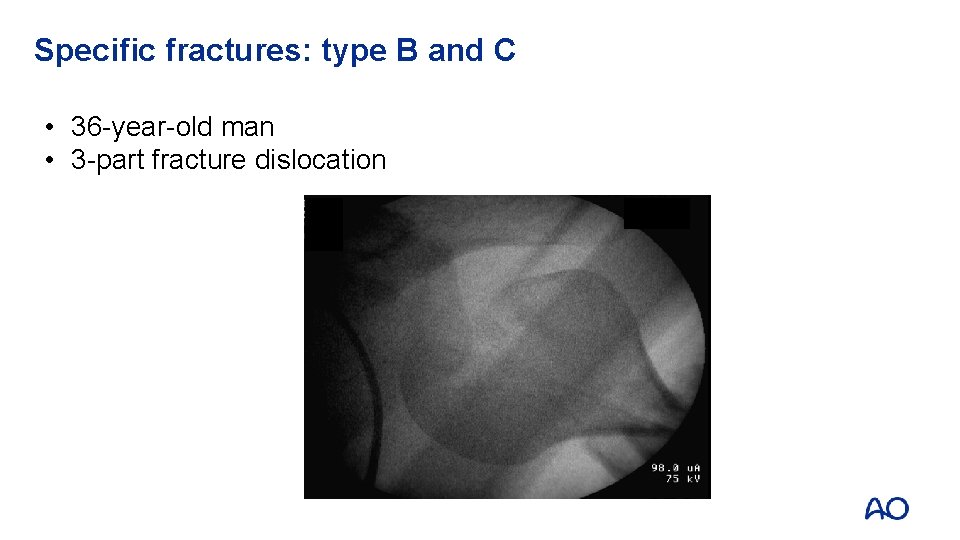
Specific fractures: type B and C • 36 -year-old man • 3 -part fracture dislocation
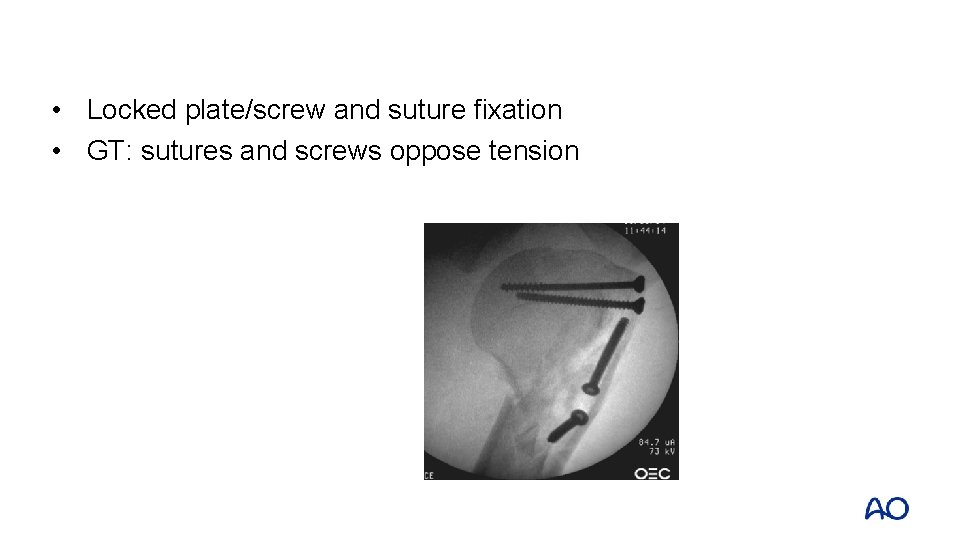
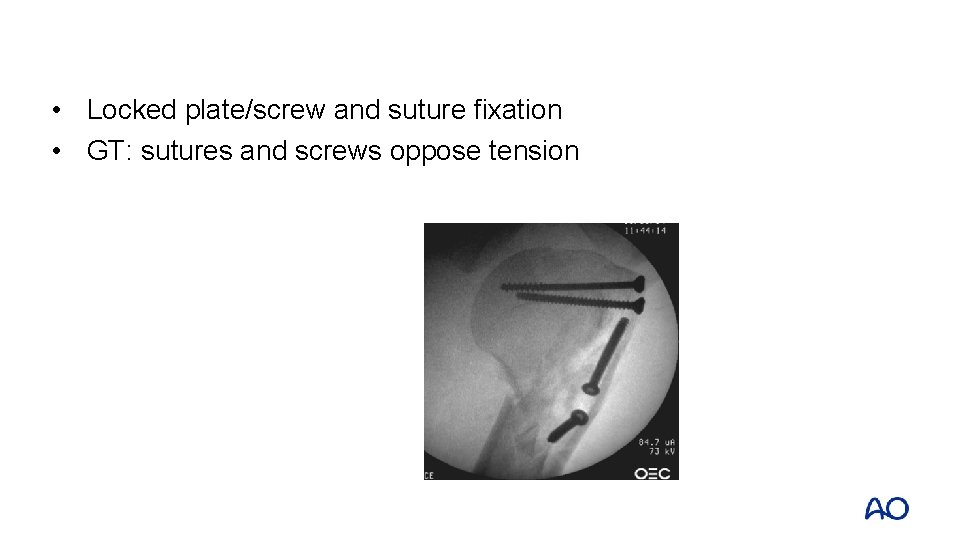
• Locked plate/screw and suture fixation • GT: sutures and screws oppose tension
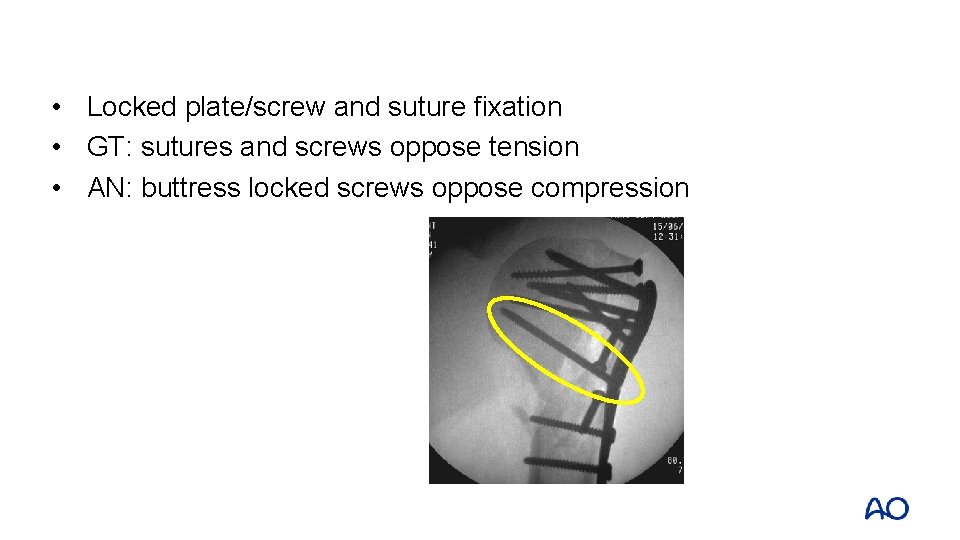
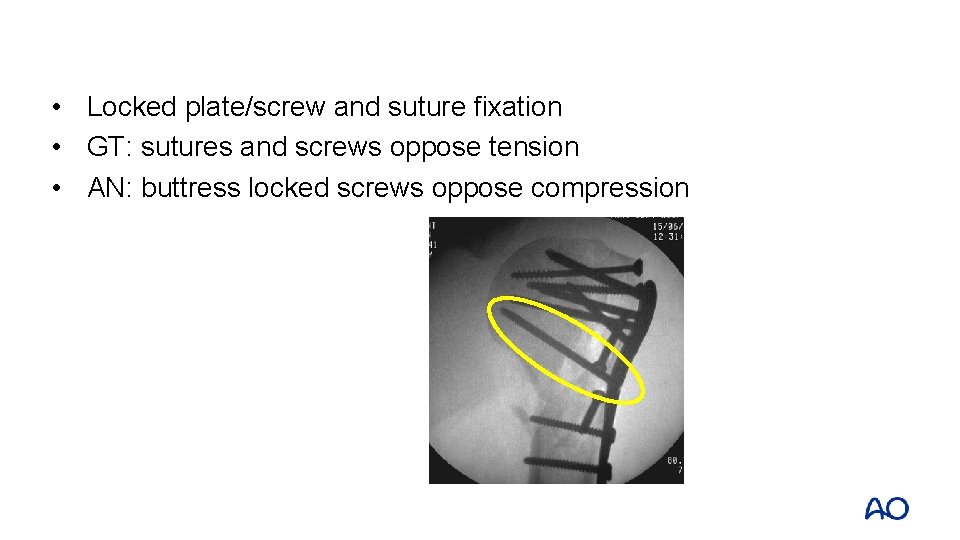
• Locked plate/screw and suture fixation • GT: sutures and screws oppose tension • AN: buttress locked screws oppose compression
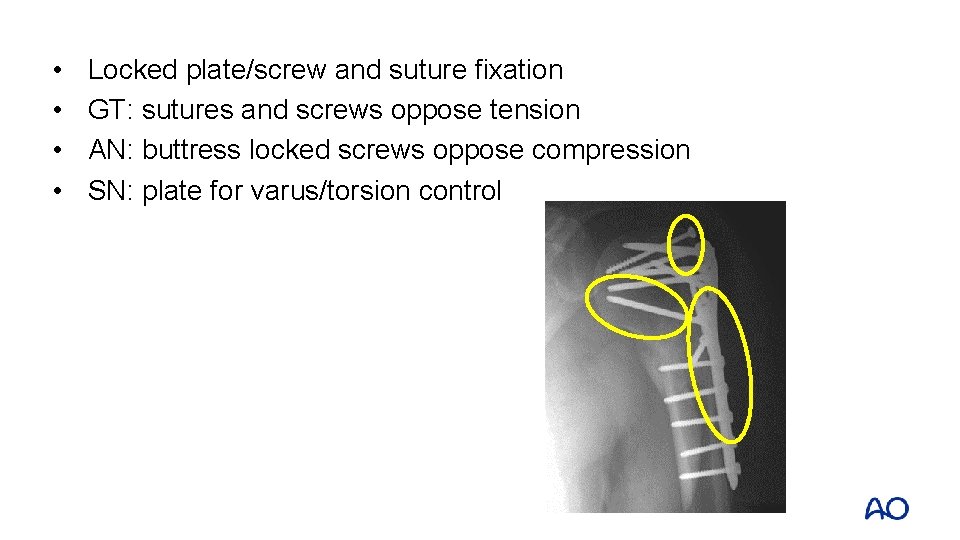
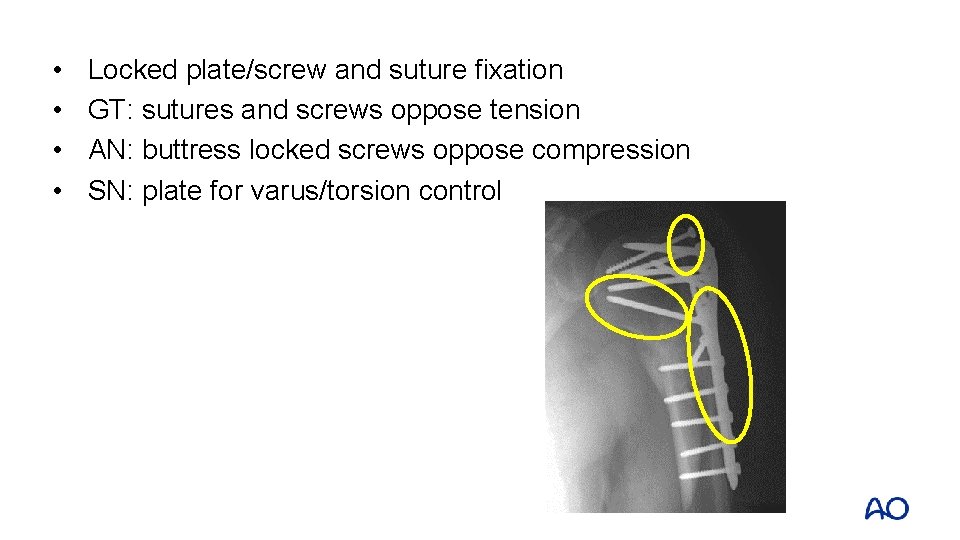
• • Locked plate/screw and suture fixation GT: sutures and screws oppose tension AN: buttress locked screws oppose compression SN: plate for varus/torsion control
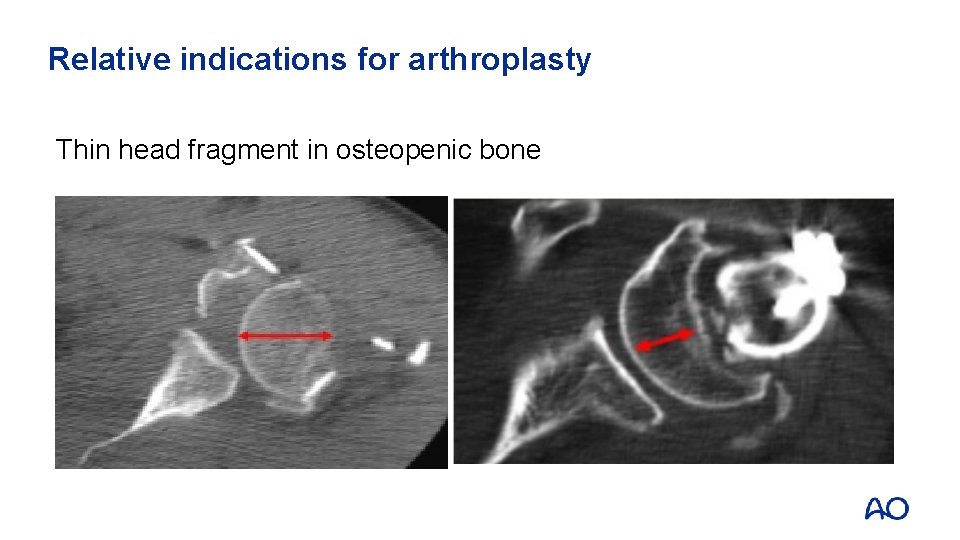
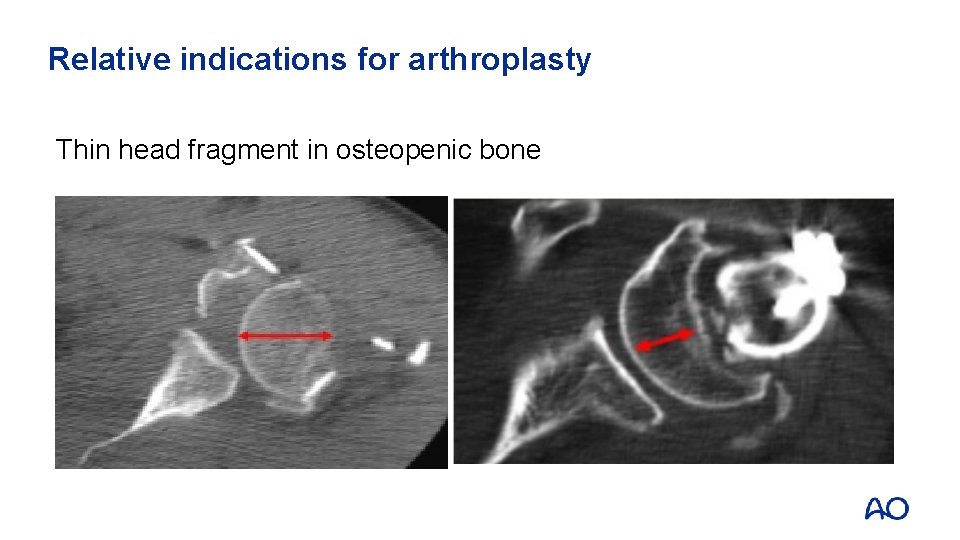
Relative indications for arthroplasty Thin head fragment in osteopenic bone
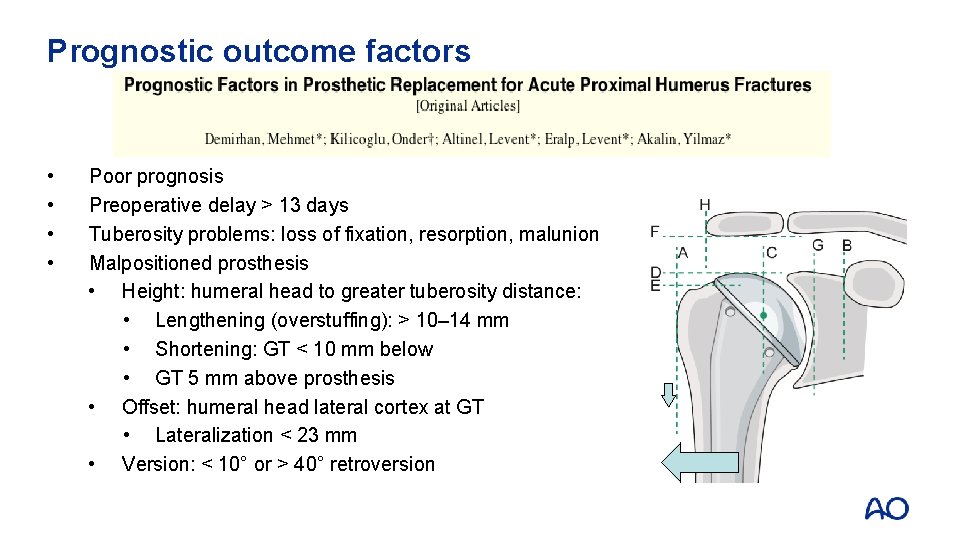
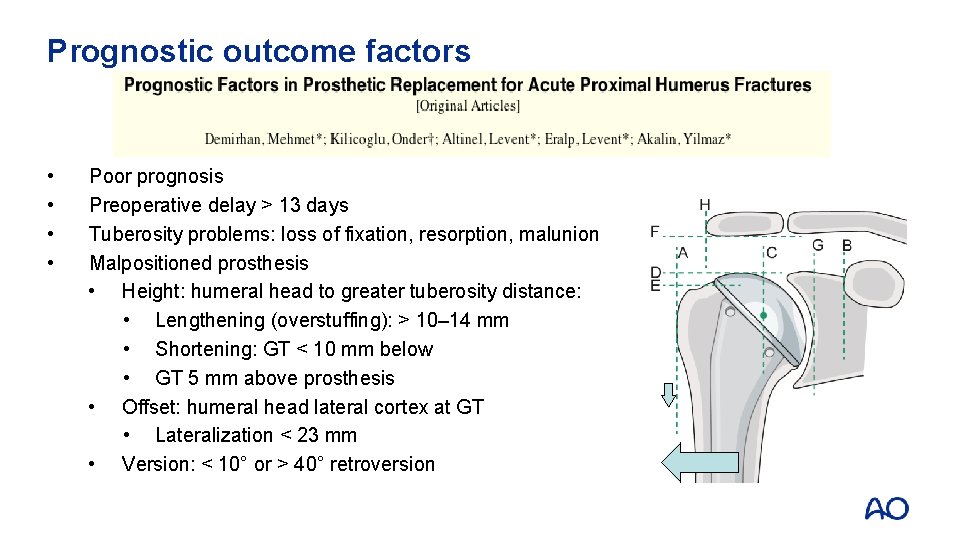
Prognostic outcome factors • • Poor prognosis Preoperative delay > 13 days Tuberosity problems: loss of fixation, resorption, malunion Malpositioned prosthesis • Height: humeral head to greater tuberosity distance: • Lengthening (overstuffing): > 10– 14 mm • Shortening: GT < 10 mm below • GT 5 mm above prosthesis • Offset: humeral head lateral cortex at GT • Lateralization < 23 mm • Version: < 10° or > 40° retroversion
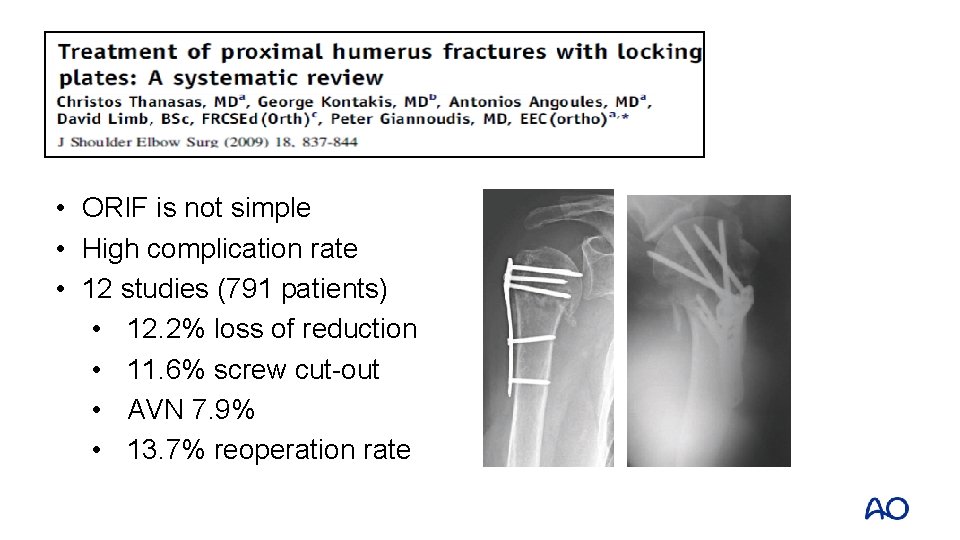
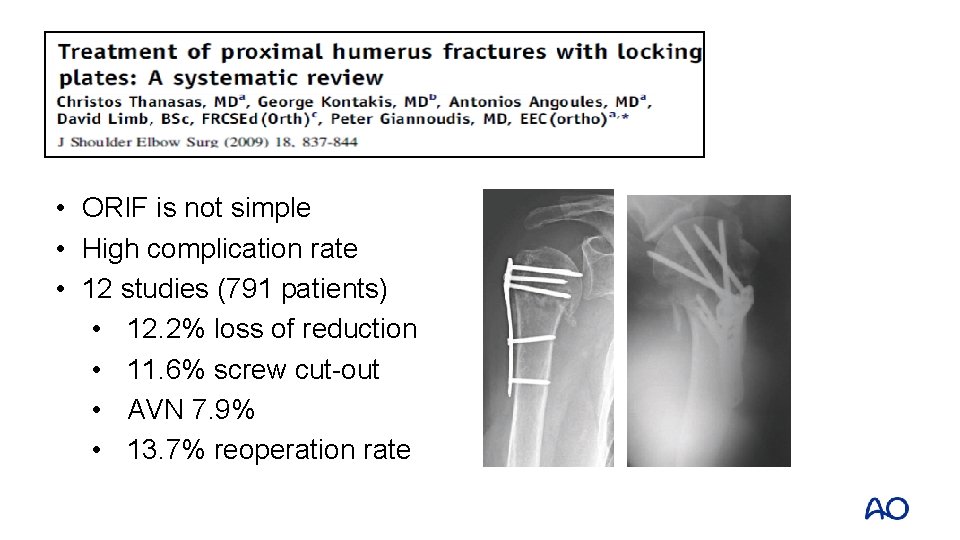
• ORIF is not simple • High complication rate • 12 studies (791 patients) • 12. 2% loss of reduction • 11. 6% screw cut-out • AVN 7. 9% • 13. 7% reoperation rate
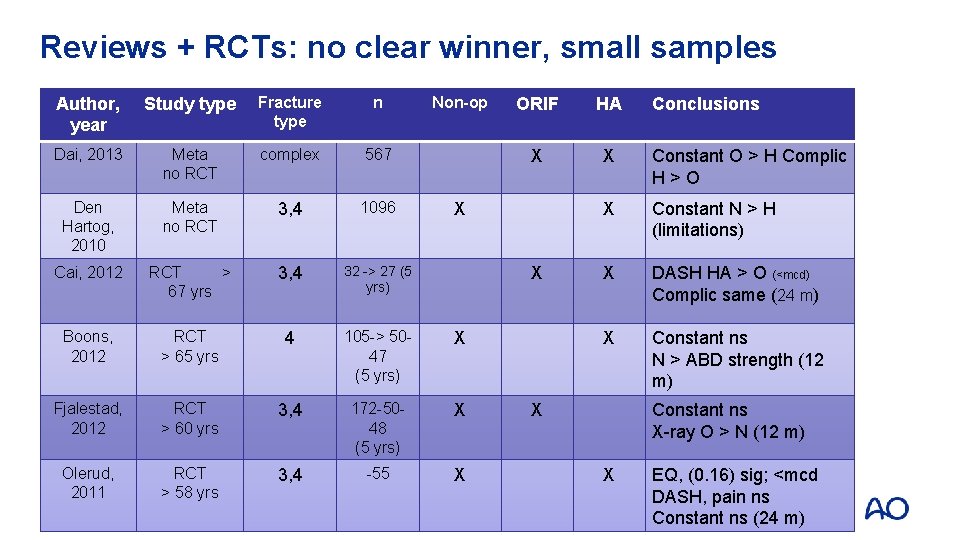
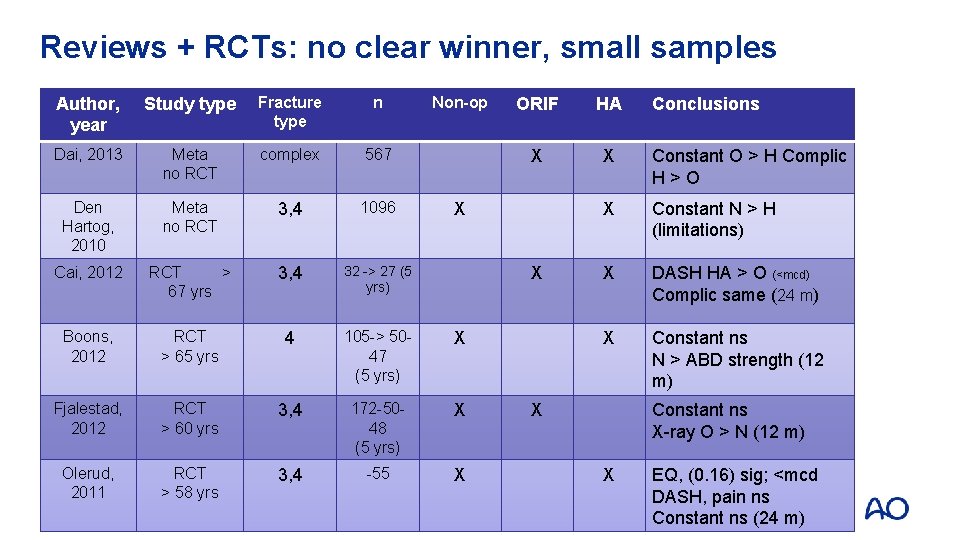
Reviews + RCTs: no clear winner, small samples Author, year Study type Fracture type n Non-op Dai, 2013 Meta no RCT complex 567 Den Hartog, 2010 Meta no RCT 3, 4 1096 Cai, 2012 RCT > 67 yrs 3, 4 32 -> 27 (5 yrs) Boons, 2012 RCT > 65 yrs 4 105 -> 5047 (5 yrs) X Fjalestad, 2012 RCT > 60 yrs 3, 4 172 -5048 (5 yrs) X Olerud, 2011 RCT > 58 yrs 3, 4 -55 X ORIF HA X X Constant O > H Complic H>O X Constant N > H (limitations) X DASH HA > O (<mcd) Complic same (24 m) X Constant ns N > ABD strength (12 m) X X X Conclusions Constant ns X-ray O > N (12 m) X EQ, (0. 16) sig; <mcd DASH, pain ns Constant ns (24 m)
Take-home messages—treatment for young patients • Reduction is key to stability and outcome • Different surgical options to achieve stable fixation • Restoration of soft tissues • Strategy to allow early motion • Hemiarthroplasty only if unreconstructible and poor function
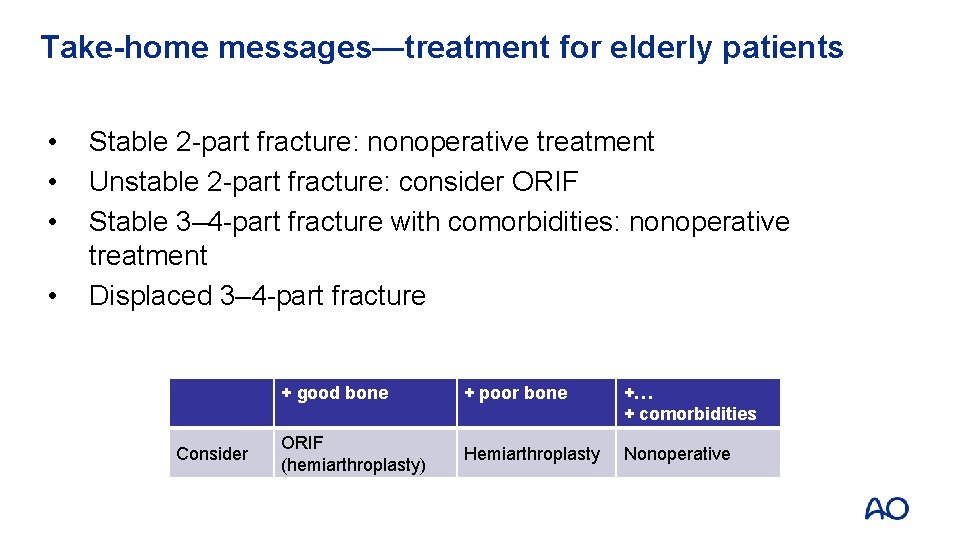
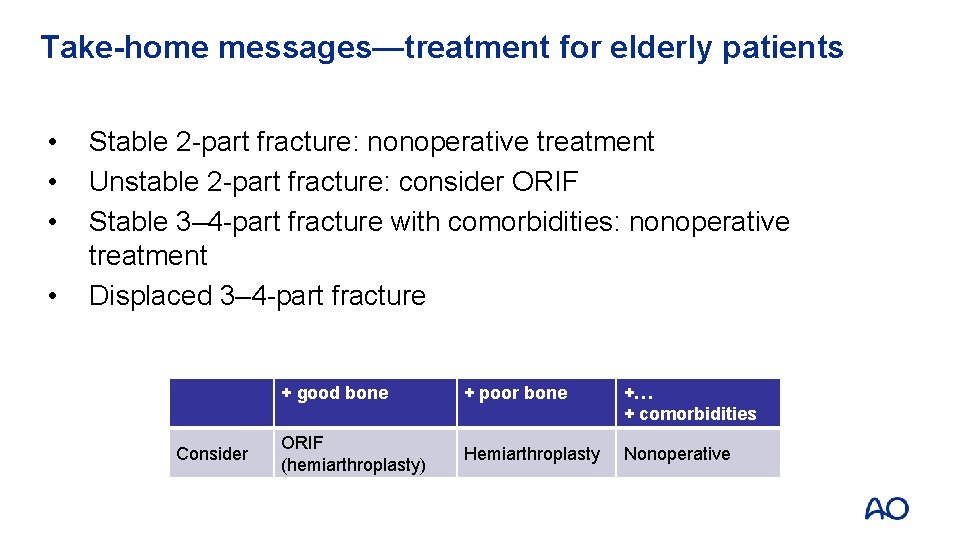
Take-home messages—treatment for elderly patients • • Stable 2 -part fracture: nonoperative treatment Unstable 2 -part fracture: consider ORIF Stable 3– 4 -part fracture with comorbidities: nonoperative treatment Displaced 3– 4 -part fracture Consider + good bone + poor bone +… + comorbidities ORIF (hemiarthroplasty) Hemiarthroplasty Nonoperative
 Radial artery in the hand
Radial artery in the hand Hiato aortico del diafragma
Hiato aortico del diafragma Expansion systolique des jugulaires
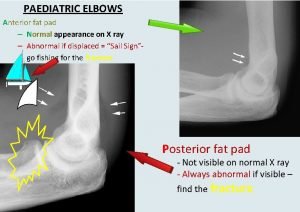
Expansion systolique des jugulaires Fat pad elbow
Fat pad elbow Cubital fossa contents
Cubital fossa contents Transverse humeral ligament
Transverse humeral ligament Desplazamientos
Desplazamientos Lig coraco humeral
Lig coraco humeral Ozdobená biskupská palica
Ozdobená biskupská palica Gonalgia derecha
Gonalgia derecha Pulso pedio y tibial
Pulso pedio y tibial Palette humérale anatomie
Palette humérale anatomie Facio escapulo humeral
Facio escapulo humeral Irving elbow dislocation
Irving elbow dislocation Radical fracture glass
Radical fracture glass Radial and concentric fractures
Radial and concentric fractures Gustilo anderson classification antibiotics
Gustilo anderson classification antibiotics Fracture sus et intercondylienne du coude
Fracture sus et intercondylienne du coude Les ischions
Les ischions Water seal chamber
Water seal chamber Bone cancer fractures
Bone cancer fractures Panfacial fractures sequencing
Panfacial fractures sequencing Daniel tibia
Daniel tibia Classification of open fractures
Classification of open fractures Classification of open fractures
Classification of open fractures Types of fractures with pictures
Types of fractures with pictures Types of fractures with pictures
Types of fractures with pictures Tubular shaft of a long bone
Tubular shaft of a long bone Youtube
Youtube Acetabulum ossification
Acetabulum ossification Types of glass fractures
Types of glass fractures Late complications of fractures
Late complications of fractures øpas
øpas Weber classification of ankle fractures
Weber classification of ankle fractures Memory forensics training
Memory forensics training Basic instructor course #1014
Basic instructor course #1014 Advanced land navigation
Advanced land navigation Introductory maxqda course
Introductory maxqda course Tcole advanced instructor course
Tcole advanced instructor course Tcole advanced instructor course
Tcole advanced instructor course Ao advanced course
Ao advanced course Half brick wall
Half brick wall Course number and title
Course number and title Course interne course externe
Course interne course externe Ao tibial shaft fracture
Ao tibial shaft fracture Advanced principles of fracture management
Advanced principles of fracture management Tibial fracture schatzker classification
Tibial fracture schatzker classification 321 riq
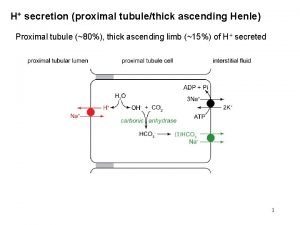
321 riq Selective reabsorption in the proximal convoluted tubule
Selective reabsorption in the proximal convoluted tubule