Fractures of the Humeral Shaft Gregory L De

- Slides: 35
Fractures of the Humeral Shaft Gregory L. De. Silva, MD Associate Professor, University of Arizona
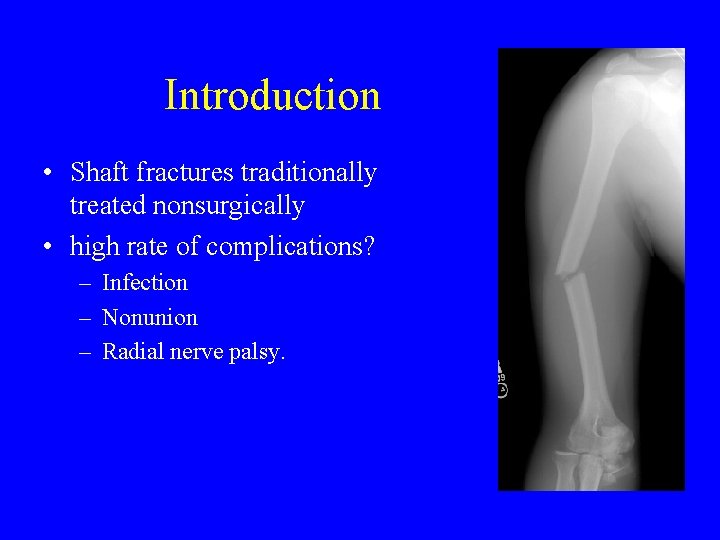
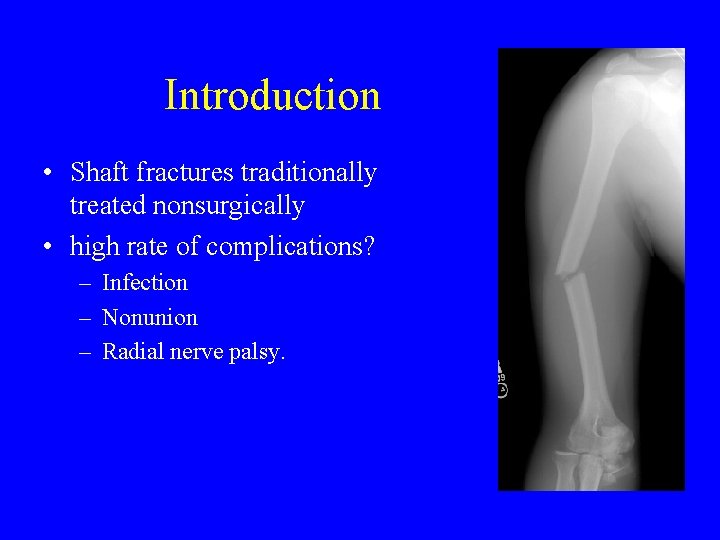
Introduction • Shaft fractures traditionally treated nonsurgically • high rate of complications? – Infection – Nonunion – Radial nerve palsy.
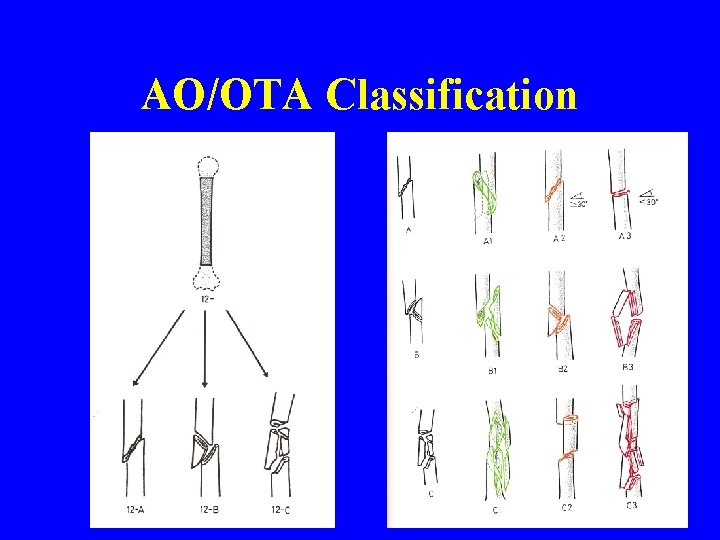
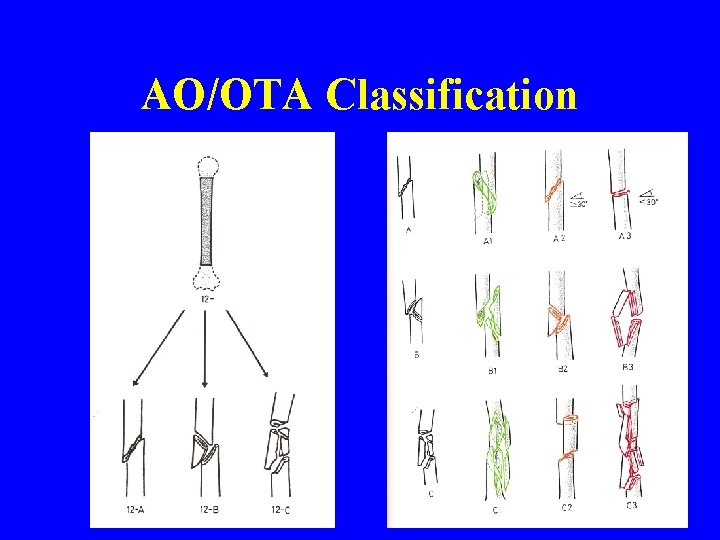
AO/OTA Classification
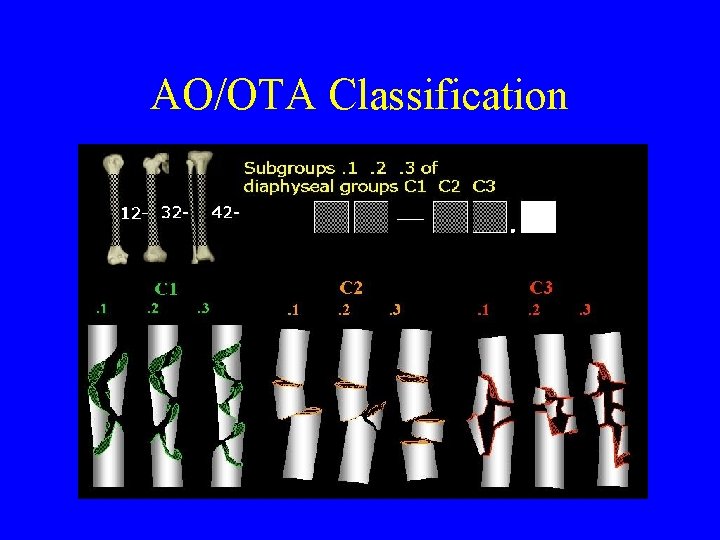
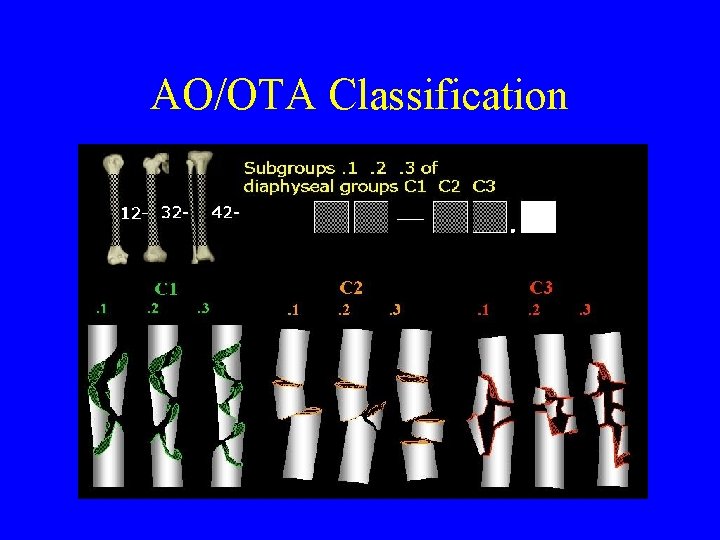
AO/OTA Classification
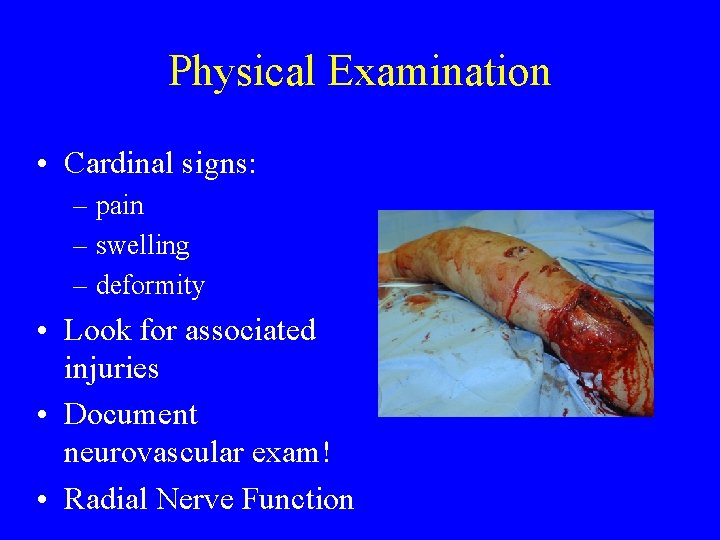
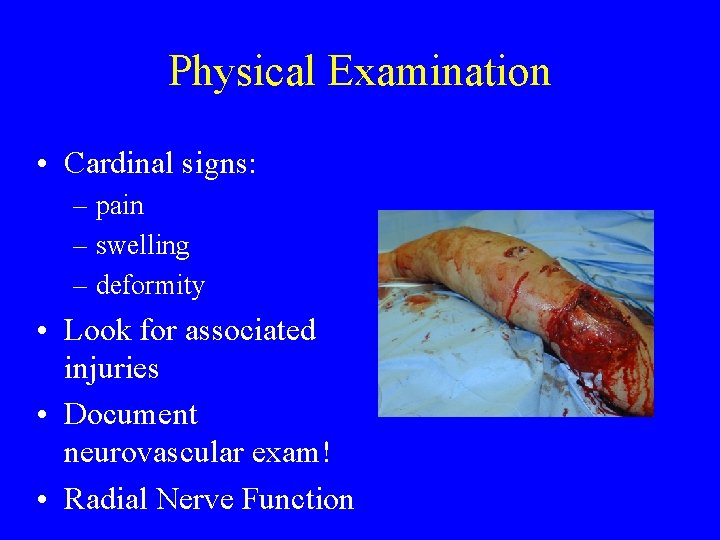
Physical Examination • Cardinal signs: – pain – swelling – deformity • Look for associated injuries • Document neurovascular exam! • Radial Nerve Function
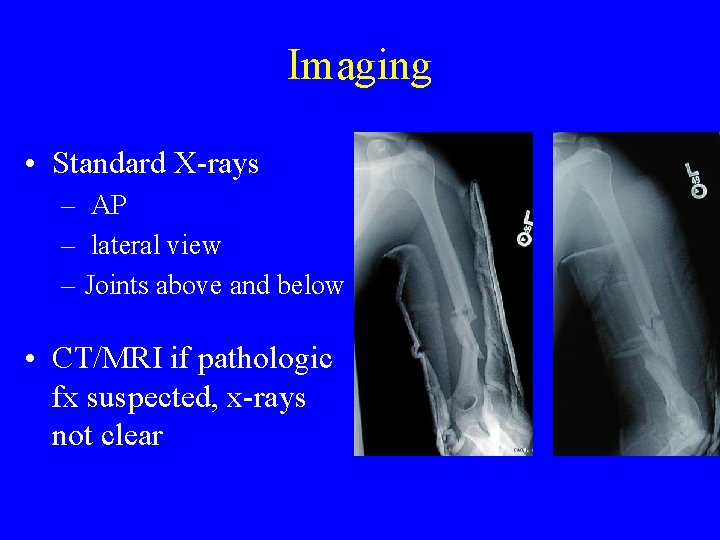
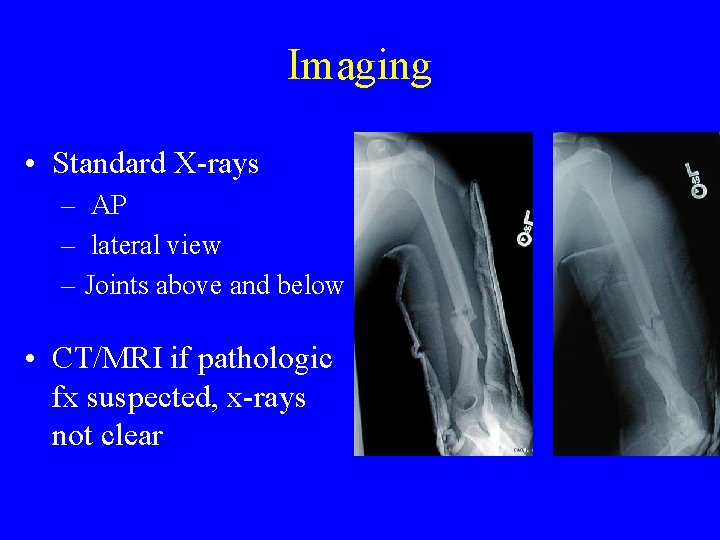
Imaging • Standard X-rays – AP – lateral view – Joints above and below • CT/MRI if pathologic fx suspected, x-rays not clear
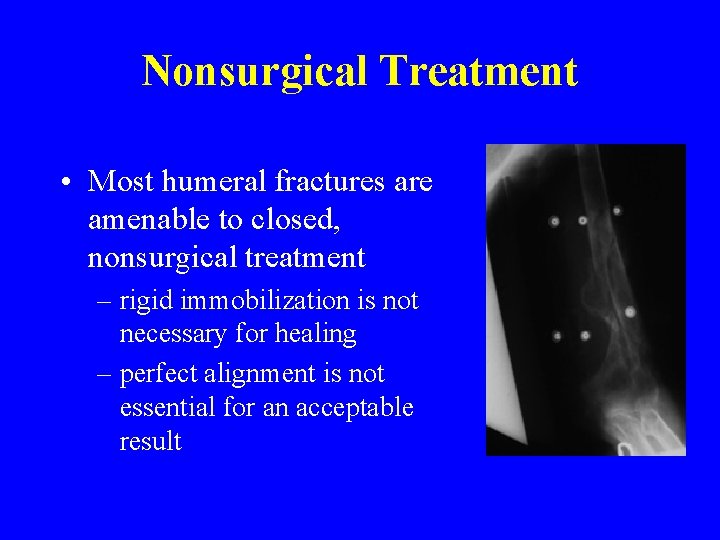
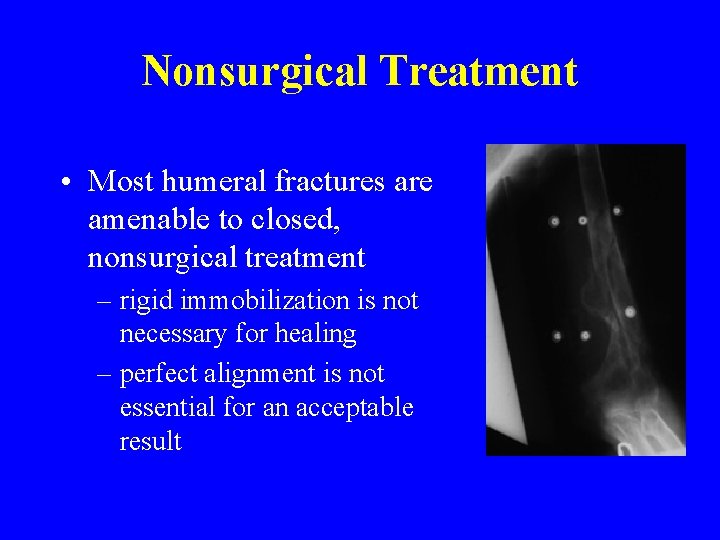
Nonsurgical Treatment • Most humeral fractures are amenable to closed, nonsurgical treatment – rigid immobilization is not necessary for healing – perfect alignment is not essential for an acceptable result
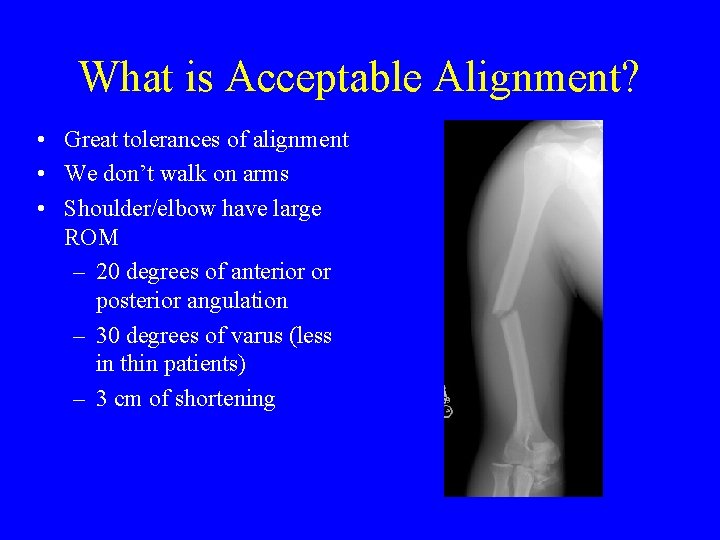
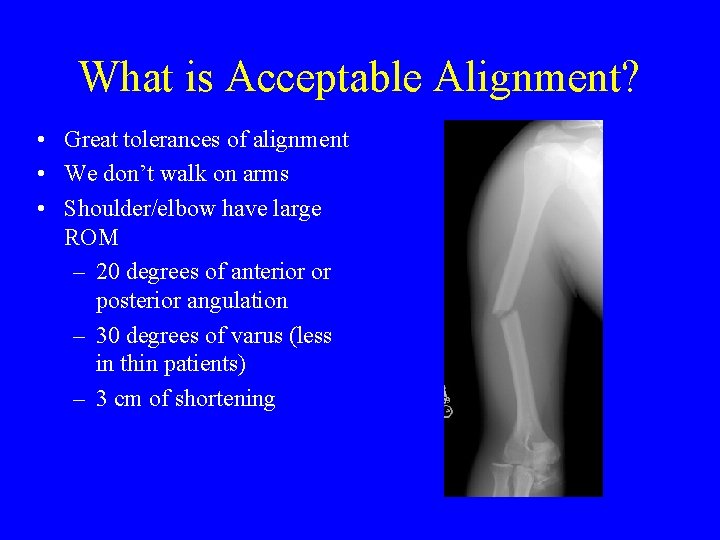
What is Acceptable Alignment? • Great tolerances of alignment • We don’t walk on arms • Shoulder/elbow have large ROM – 20 degrees of anterior or posterior angulation – 30 degrees of varus (less in thin patients) – 3 cm of shortening
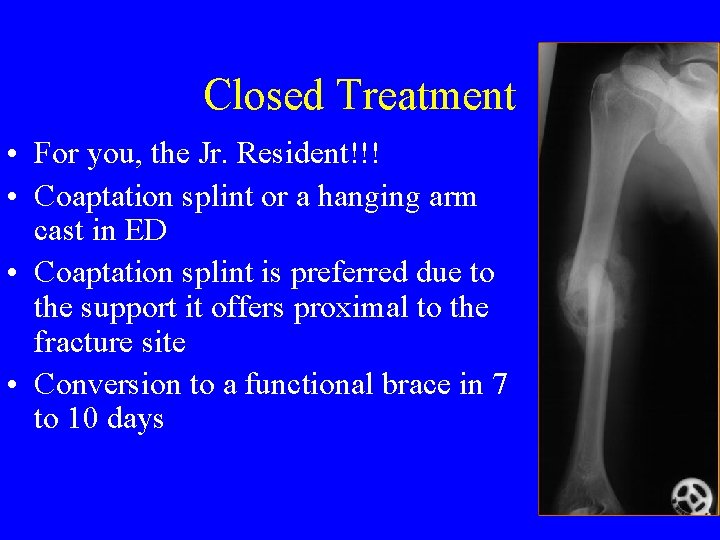
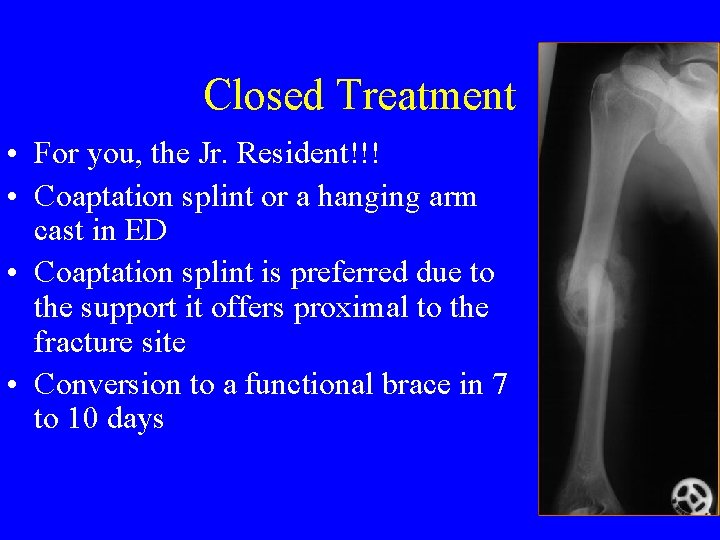
Closed Treatment • For you, the Jr. Resident!!! • Coaptation splint or a hanging arm cast in ED • Coaptation splint is preferred due to the support it offers proximal to the fracture site • Conversion to a functional brace in 7 to 10 days
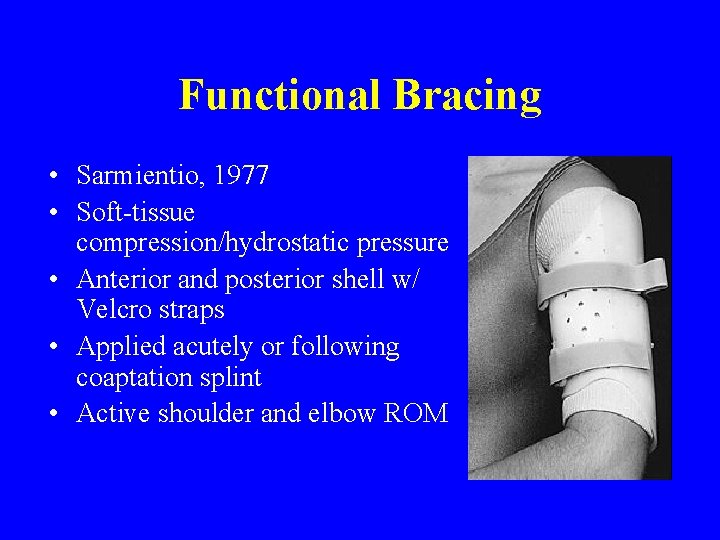
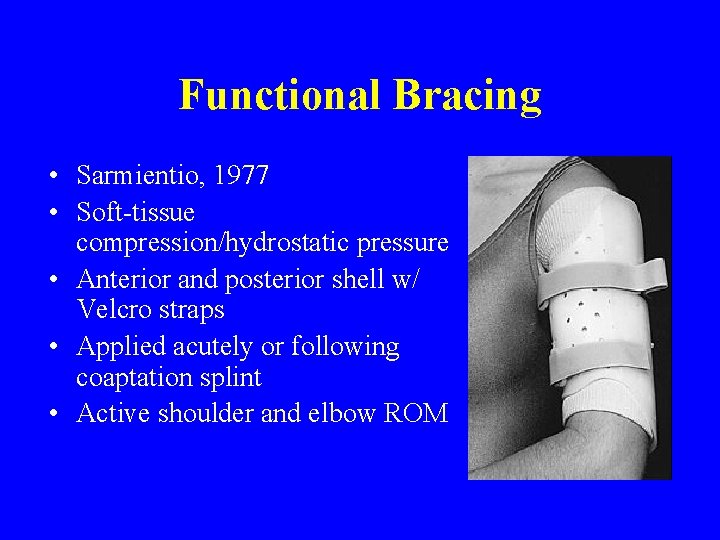
Functional Bracing • Sarmientio, 1977 • Soft-tissue compression/hydrostatic pressure • Anterior and posterior shell w/ Velcro straps • Applied acutely or following coaptation splint • Active shoulder and elbow ROM
Contraindications to Functional Bracing • Massive soft-tissue or bone loss • Unreliable or uncooperative patient • Inability to obtain and maintain acceptable fracture alignment • Fracture gap present - increases risk of nonunion
Surgical Treatment • Surgical intervention is preferable in specific cases – Injury Related Factors – Patient Related Factors
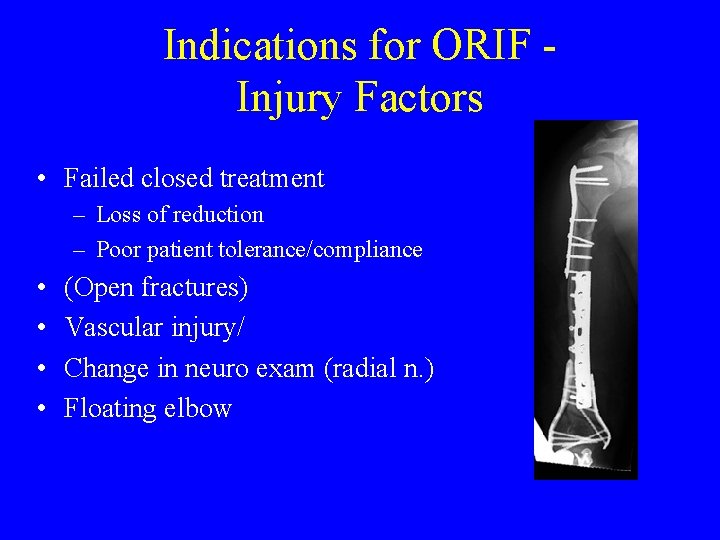
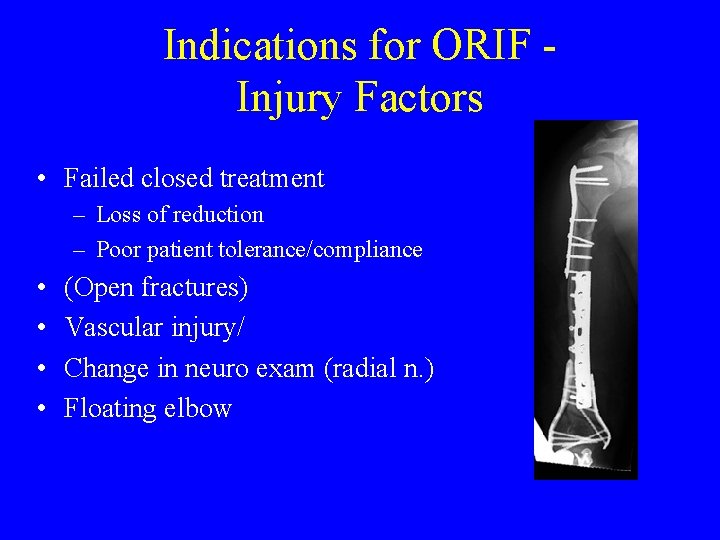
Indications for ORIF Injury Factors • Failed closed treatment – Loss of reduction – Poor patient tolerance/compliance • • (Open fractures) Vascular injury/ Change in neuro exam (radial n. ) Floating elbow
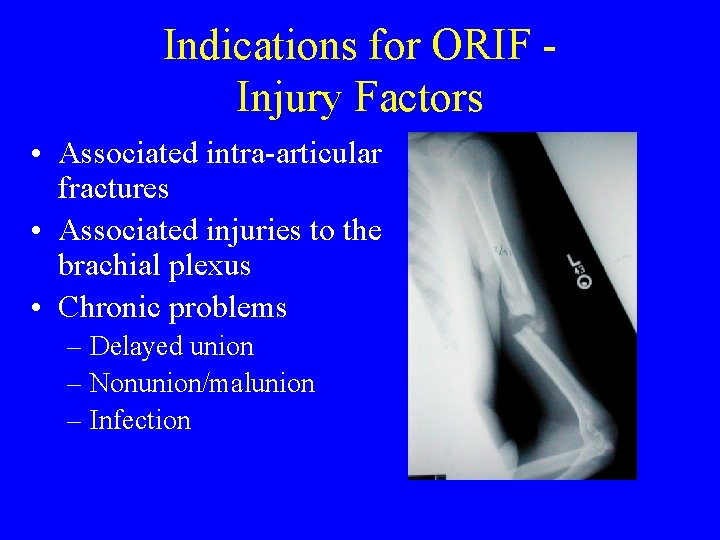
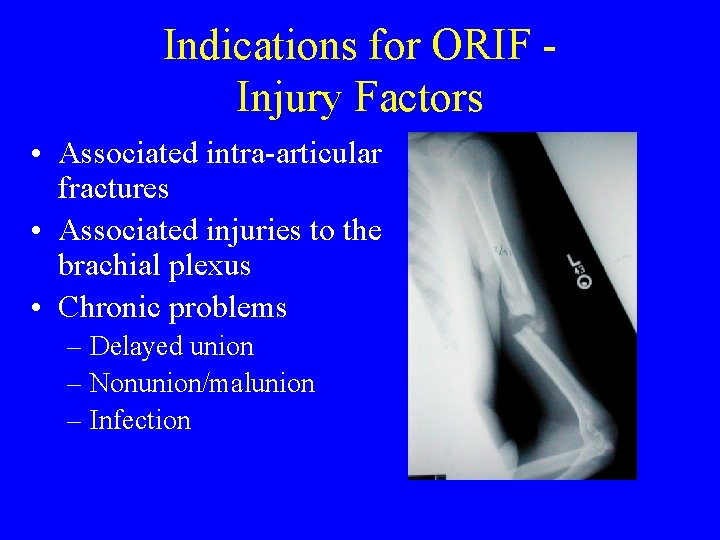
Indications for ORIF Injury Factors • Associated intra-articular fractures • Associated injuries to the brachial plexus • Chronic problems – Delayed union – Nonunion/malunion – Infection

Indications for ORIF Patient Factors • Polytrauma-requiring arm for mobilization – – Head injuries Burns Chest trauma Multiple fractures • Patient unable to be upright
Surgical Treatment • Plate osteosynthesis – Lag screws alone are not strong enough • IM fixation • External fixation
Plate Osteosynthesis • The best functional results: use of plates and screws • Direct fracture reduction • Stable fixation of the humeral shaft • No violation of the rotator cuff • Visualization of radial nerve
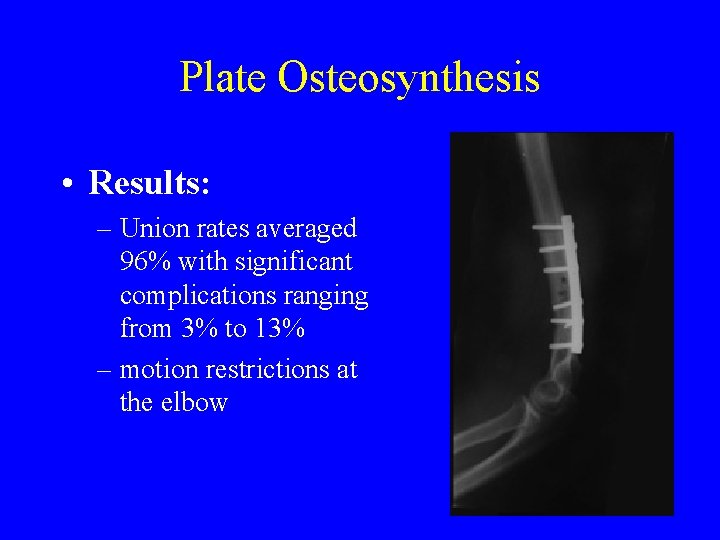
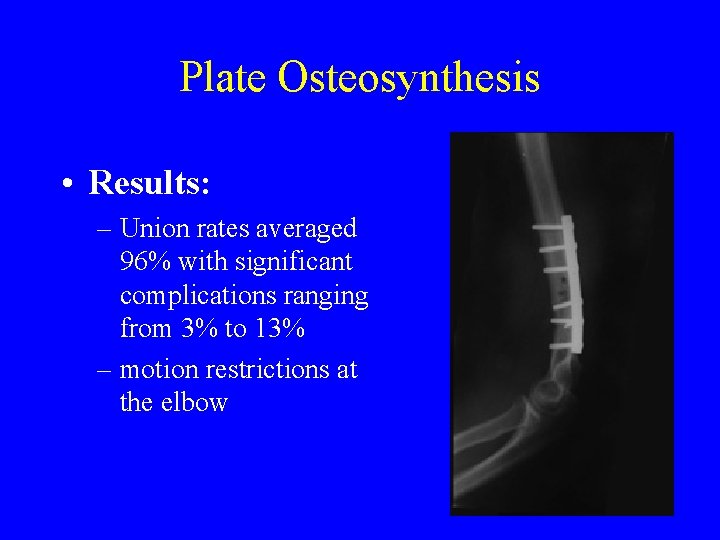
Plate Osteosynthesis • Results: – Union rates averaged 96% with significant complications ranging from 3% to 13% – motion restrictions at the elbow
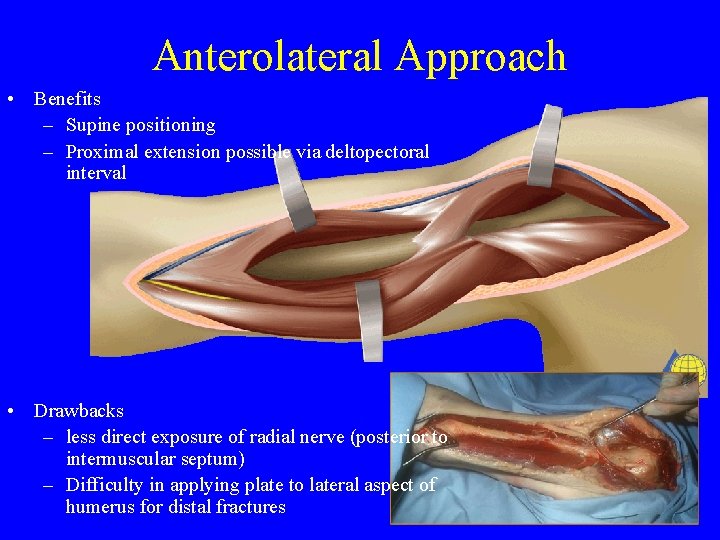
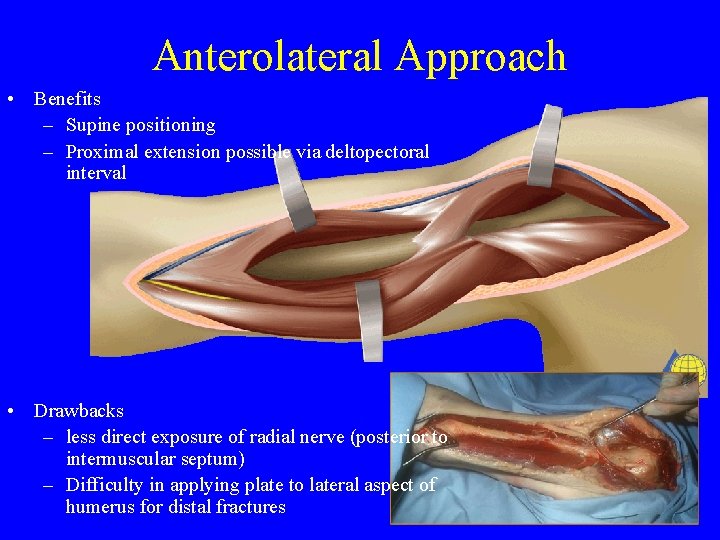
Anterolateral Approach • Benefits – Supine positioning – Proximal extension possible via deltopectoral interval • Drawbacks – less direct exposure of radial nerve (posterior to intermuscular septum) – Difficulty in applying plate to lateral aspect of humerus for distal fractures
Anterolateral Approach • For proximal and middle third fxs
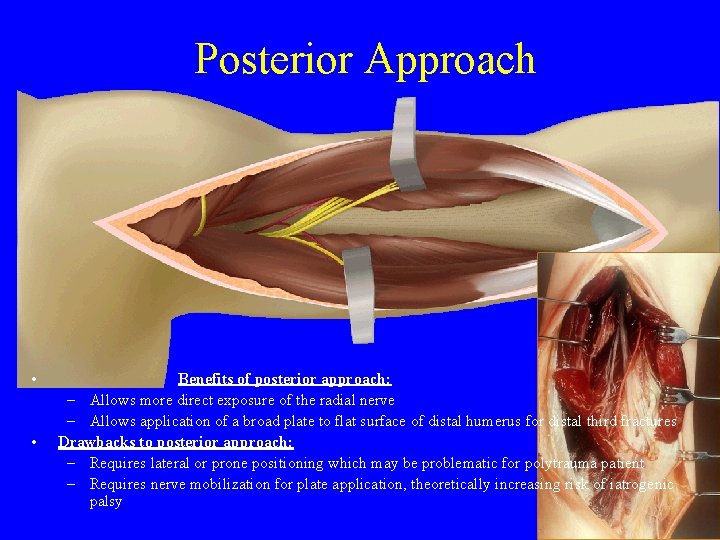
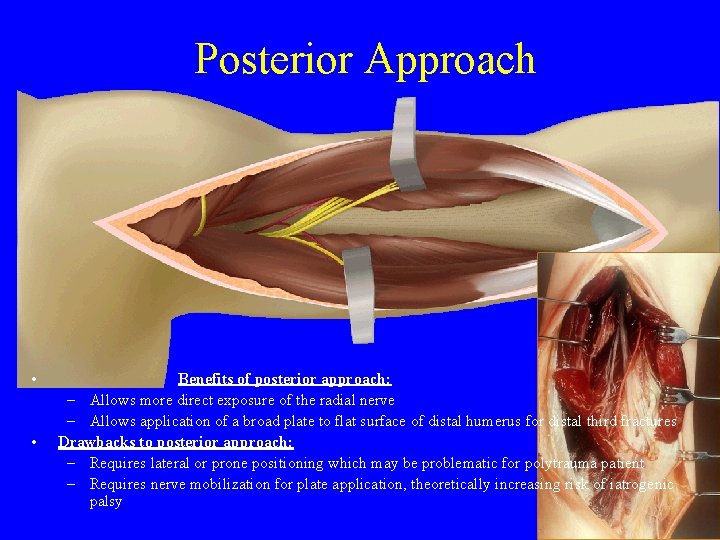
Posterior Approach • • Benefits of posterior approach: – Allows more direct exposure of the radial nerve – Allows application of a broad plate to flat surface of distal humerus for distal third fractures Drawbacks to posterior approach: – Requires lateral or prone positioning which may be problematic for polytrauma patient – Requires nerve mobilization for plate application, theoretically increasing risk of iatrogenic palsy
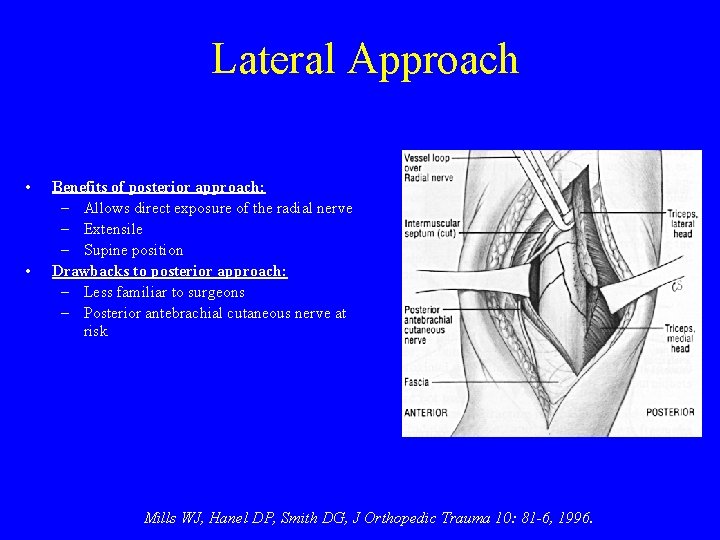
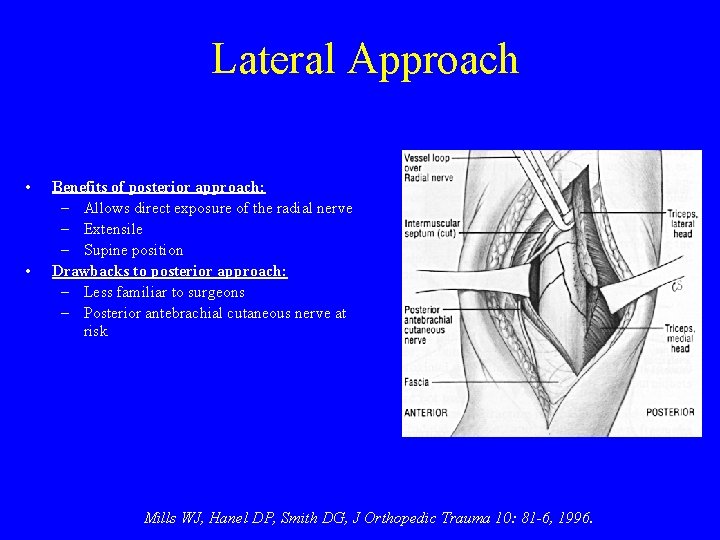
Lateral Approach • • Benefits of posterior approach: – Allows direct exposure of the radial nerve – Extensile – Supine position Drawbacks to posterior approach: – Less familiar to surgeons – Posterior antebrachial cutaneous nerve at risk Mills WJ, Hanel DP, Smith DG, J Orthopedic Trauma 10: 81 -6, 1996.
Medial Approach • True internervous interval • Not extensile proximally • Used in open fxs when wound medial?
Complications of Humeral Shaft Fractures • Radial nerve injury • Vascular injury • Nonunion
Radial Nerve Injury • Incidence varies from 1. 8% to 24% of shaft fractures • Primary - occurs @ injury • Secondary - occurs later during closed or open management • Management controversial
Radial Nerve Injury • Spontaneous recovery: ~90% • Even secondary palsies, have a high rate of spontaneous recovery • EMG and nerve conduction studies can help, (but not acutely!) • If no recovery, tendon transfers very reliable
Preferred Management of Fractures with Associated Radial Nerve Palsy • Indications for surgery: – Open fractures – Secondary palsies developing after a closed reduction
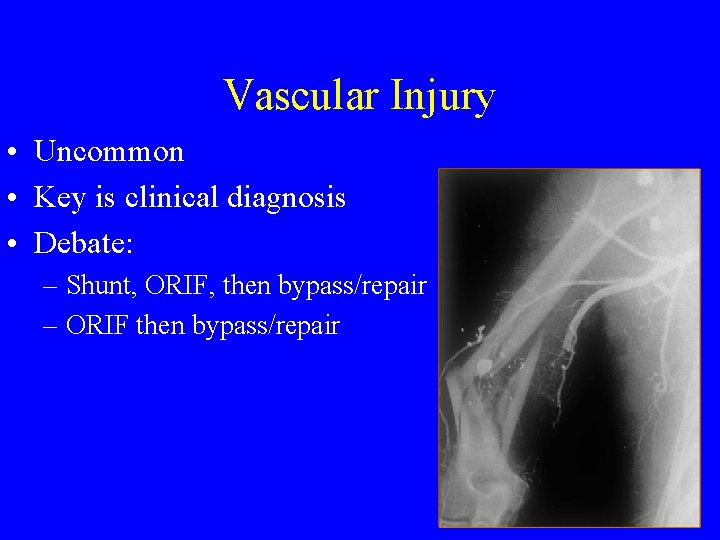
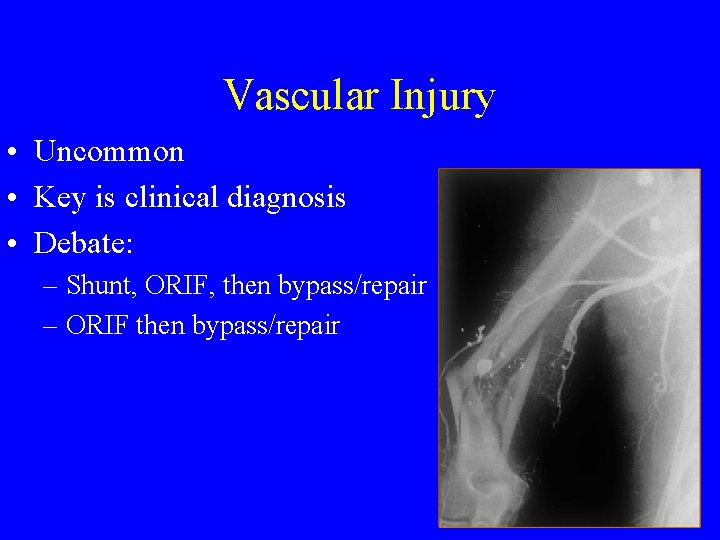
Vascular Injury • Uncommon • Key is clinical diagnosis • Debate: – Shunt, ORIF, then bypass/repair – ORIF then bypass/repair
Nonunion • Rate: 0% to 15%
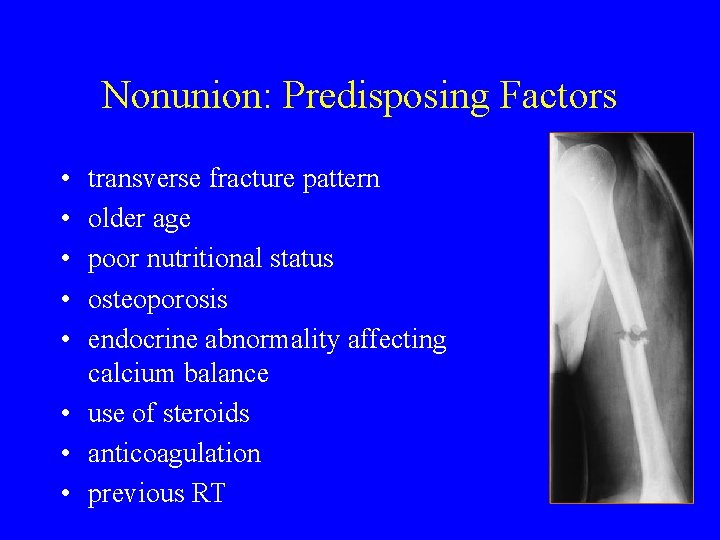
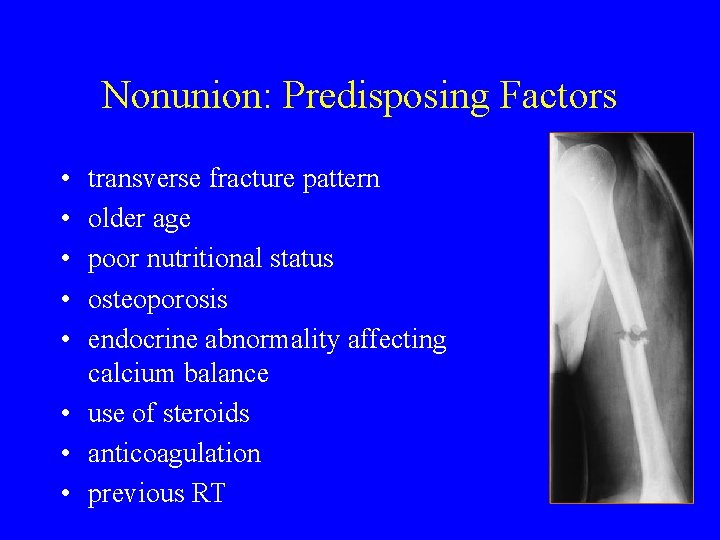
Nonunion: Predisposing Factors • • • transverse fracture pattern older age poor nutritional status osteoporosis endocrine abnormality affecting calcium balance • use of steroids • anticoagulation • previous RT
Nonunion: Surgical Treatment • Compression plate fixation for hypertrophic nonunions • Biologic stimulation + plate for atrophic nonunions
Nonunion: Surgical Treatment • Compression plate fixation for hypertrophic nonunions • Biologic stimulation + plate for atrophic nonunions
Summary Humeral Shaft Fractures • • • Results very good for functional bracing Need to carefully document radial nerve exam Most radial nerves injuries recover Most prefer plates over nails Look for prospective study of immediate fixation vs. functional bracing
SWOTA : 2010 Resident Course - Fundamentals of Fracture Care PROXIMAL HUMERUS AND DIAPHYSEAL FRACTURES Helpfulness of Material A) Worst B) Bad C) OK D) Good COMMENTS Please E) Best
SWOTA : 2010 Resident Course - Fundamentals of Fracture Care PROXIMAL HUMERUS AND DIAPHYSEAL FRACTURES Quality of Presentation A) Worst B) Bad C) OK D) Good COMMENTS Please E) Best
 Fractura supra condilea
Fractura supra condilea Pulso pedio y tibial
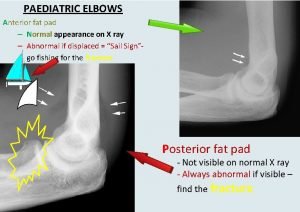
Pulso pedio y tibial Fat pad sign
Fat pad sign Lig coraco humeral
Lig coraco humeral A. profunda brachii
A. profunda brachii Palette humeral
Palette humeral Olecrannon fossa
Olecrannon fossa Humerál
Humerál Yugulares
Yugulares Facio escapulo humeral
Facio escapulo humeral Coracohumeral
Coracohumeral Gonalgia derecha
Gonalgia derecha Hypotension norme
Hypotension norme Classification of open fractures
Classification of open fractures Gustilo anderson classification antibiotics
Gustilo anderson classification antibiotics Olecranon bursitis irving
Olecranon bursitis irving Types of fractures with pictures
Types of fractures with pictures Types of glass fractures
Types of glass fractures Primary bone vs secondary bone
Primary bone vs secondary bone Classification of open fractures
Classification of open fractures Classification fracture supracondylienne
Classification fracture supracondylienne Radial glass fracture
Radial glass fracture Non union types
Non union types Acetabular fractures
Acetabular fractures Panfacial fractures sequencing
Panfacial fractures sequencing Lisa kasman
Lisa kasman Fracture de voilemier
Fracture de voilemier Bobine d andrieu
Bobine d andrieu Acetabular ossification
Acetabular ossification Classification of open fractures
Classification of open fractures How is glass made
How is glass made Types of fractures with pictures
Types of fractures with pictures Rapid bubbling in the water seal chamber
Rapid bubbling in the water seal chamber Weber classification of ankle fractures
Weber classification of ankle fractures Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau