Open Fractures Dr Sukhpal Singh Definition These are



- Slides: 75

Open Fractures Dr. Sukhpal Singh
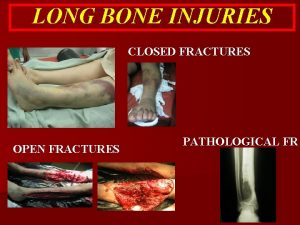
Definition • These are the fractures in which there is breach in the soft tissue envelope over or near the fracture, such that fracture haematoma communicates with external environment.
History • Egyptians 1 st time recognised he need for coverage over fracture wounds to minimise morbidity. • Hippocrates favoured the debridement of purulent material. • Galen considered purulence as necessary “Laudable pus” & considered it as essential for healing. • Ambroise Parè also favoured the debridement as the mainstay of treatment of open
History • Desault (coined the term ‘debridement) in 18 th century reiterated this belief by advising debridement of dead necrotic material. • Still in the 19 th century, prior to aseptic technique & antibiotics, emergency amputation was the life saving measure after open fracture.
History • Last century, high mortality with open fractures of long bones • WWI, mortality of open femur fractures > 70% • By the WWI the main principle of treatment was debridement and stabilization & all healing by secondary intention. • 1939 Trueta “closed treatment of war fractures” – Included open wound treatment and then enclosure of the extremity in a cast – “Greatest danger of infection lay in muscle, not bone”
History • During the WW-II use of local antibiotics like sulfonamides was started for wound treatment. • Use of PCN on the battlefield quickly reduced the rate of wound sepsis.
History • Advances shifted the focus – Preservation of life and limb preservation of function and prevention of complications • However, amputation rates still exceed 50% in the most severe open tibial fractures assoc with vascular injury.
Epidemiology • More than 4. 5 million open fractures occur per year in India. (IJO)
Etiology • Generally a result of high energy mechanisms which cause greater soft tissue disruption that leaves the wound more susceptible to infection by contaminating bacteria. • The energy is stored in soft and hard tissues until the strength of respective material is exceeded. • Comminuted pieces may acquire high velocity after which they propel into the surrounding soft tissues and cause additional damage. • More severe injury, limb absorbs energy releases in explosion tears the skin momentary vacuum sucks foreign material into the wound depth. • Soft tissue damage enormous muscle swelling compartment syndrome (more in open injuries) of the intact compartments
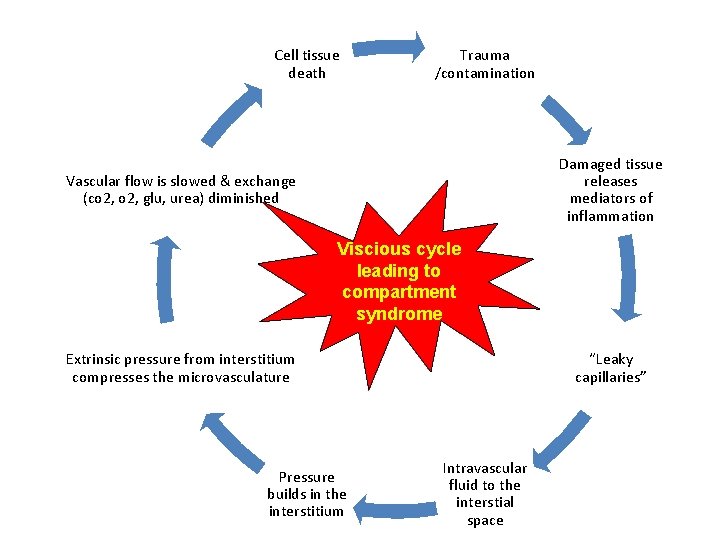
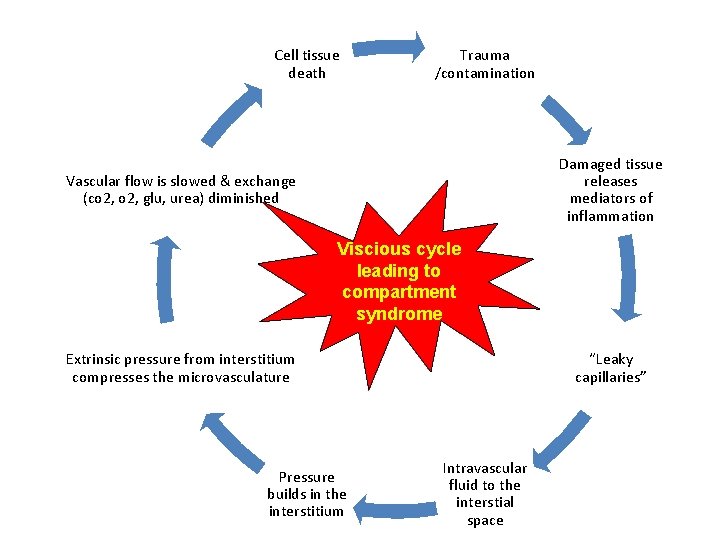
Cell tissue death Trauma /contamination Damaged tissue releases mediators of inflammation Vascular flow is slowed & exchange (co 2, glu, urea) diminished Viscious cycle leading to compartment syndrome Extrinsic pressure from interstitium compresses the microvasculature Pressure builds in the interstitium “Leaky capillaries” Intravascular fluid to the interstial space
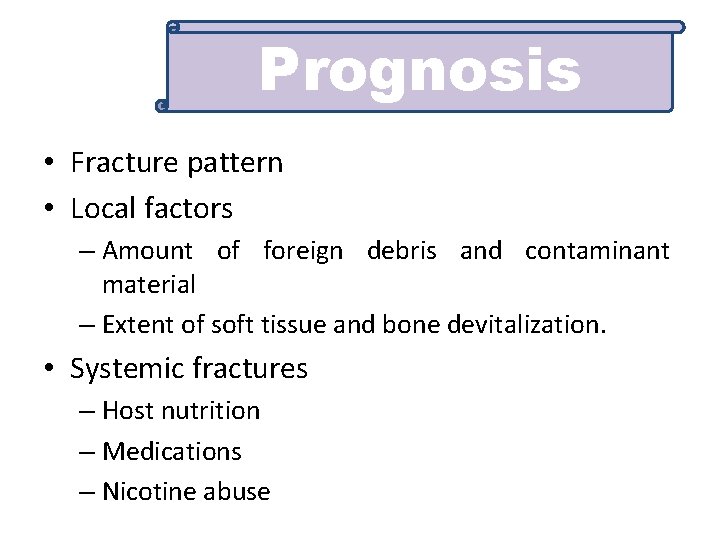
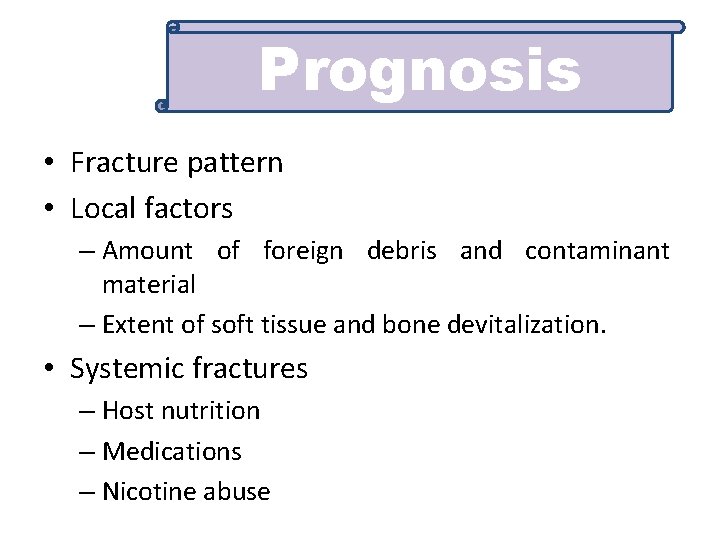
Prognosis • Fracture pattern • Local factors – Amount of foreign debris and contaminant material – Extent of soft tissue and bone devitalization. • Systemic fractures – Host nutrition – Medications – Nicotine abuse
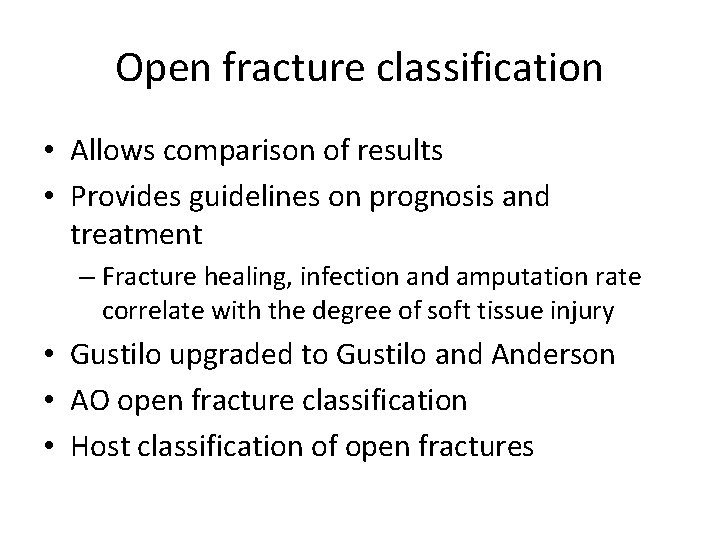
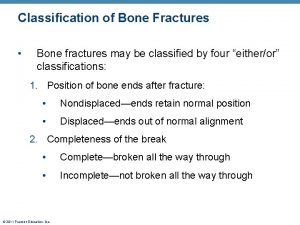
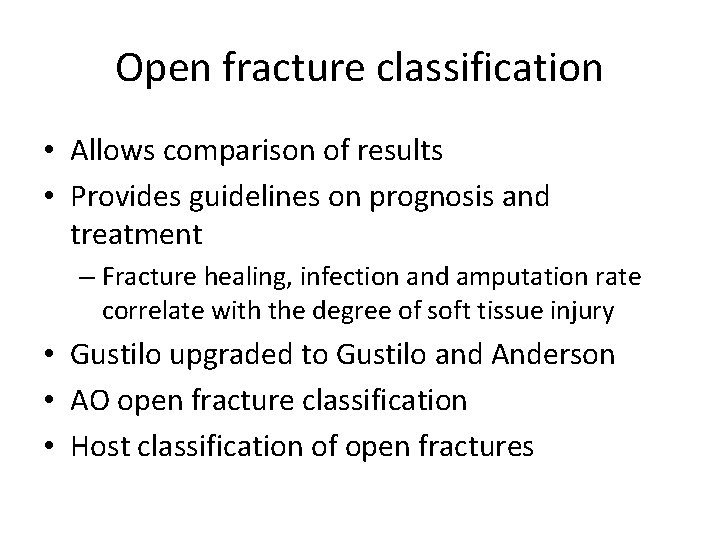
Open fracture classification • Allows comparison of results • Provides guidelines on prognosis and treatment – Fracture healing, infection and amputation rate correlate with the degree of soft tissue injury • Gustilo upgraded to Gustilo and Anderson • AO open fracture classification • Host classification of open fractures
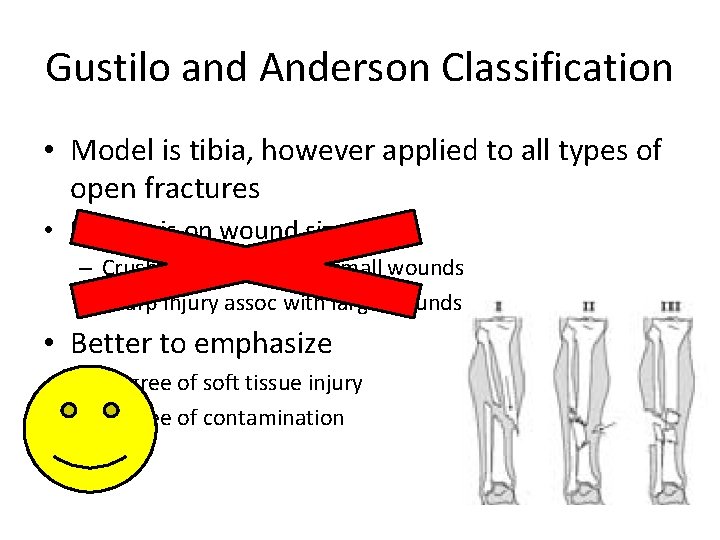
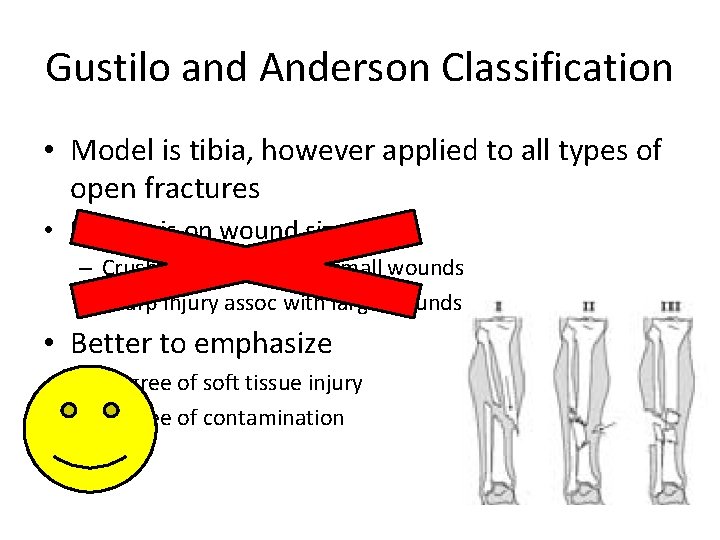
Gustilo and Anderson Classification • Model is tibia, however applied to all types of open fractures • Emphasis on wound size – Crush injury assoc with small wounds – Sharp injury assoc with large wounds • Better to emphasize – Degree of soft tissue injury – Degree of contamination
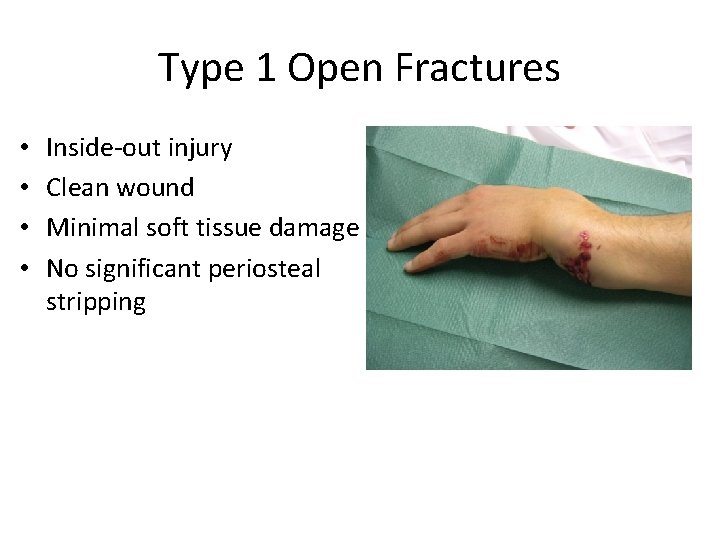
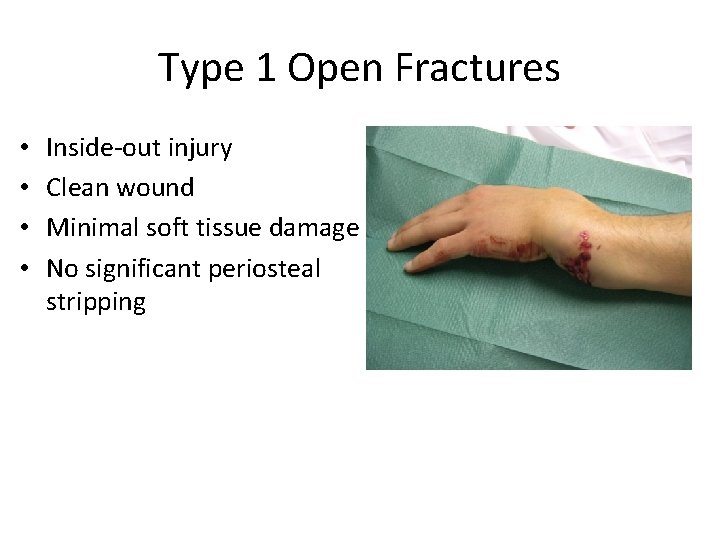
Type 1 Open Fractures • • Inside-out injury Clean wound Minimal soft tissue damage No significant periosteal stripping
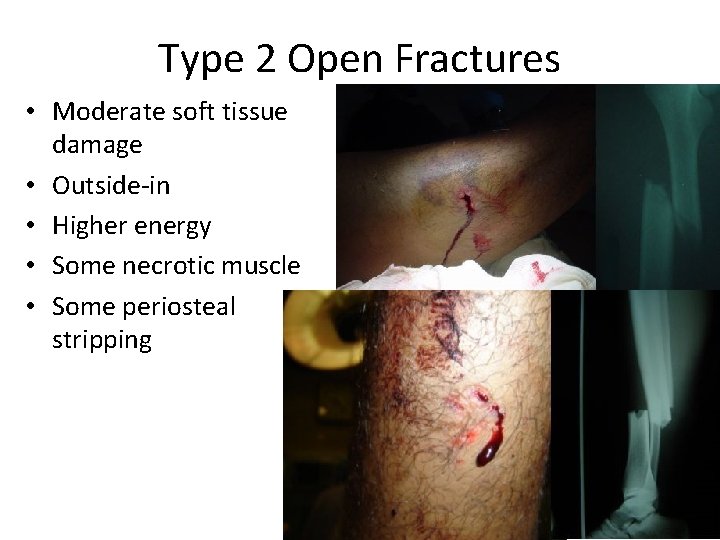
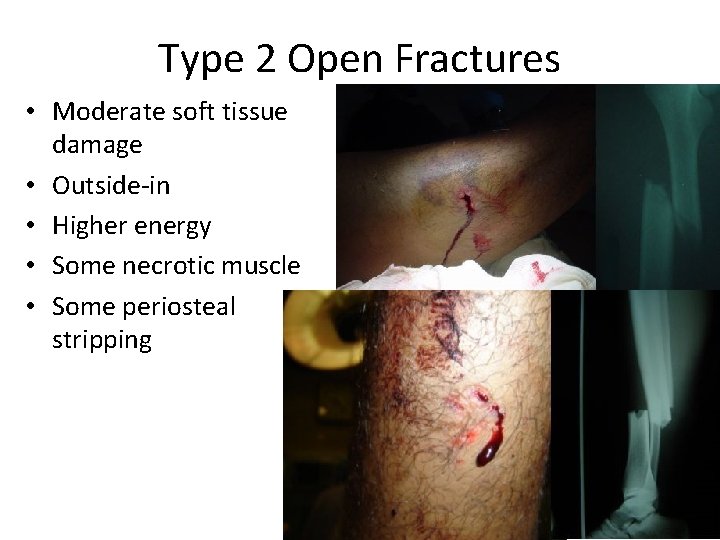
Type 2 Open Fractures • Moderate soft tissue damage • Outside-in • Higher energy • Some necrotic muscle • Some periosteal stripping
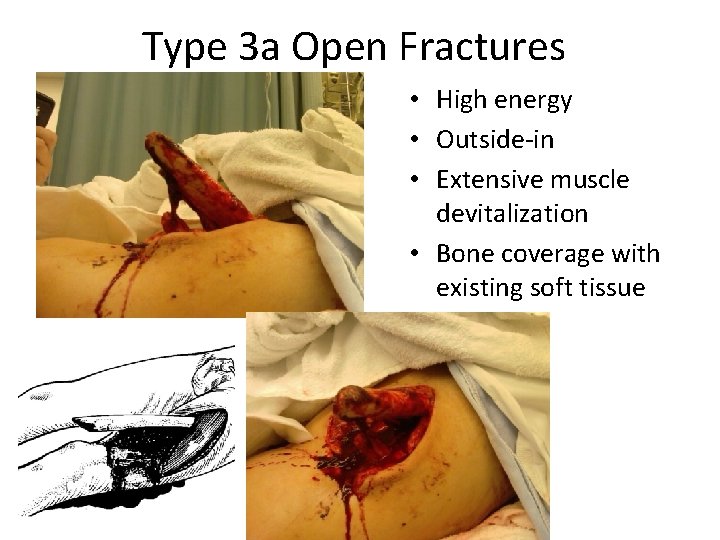
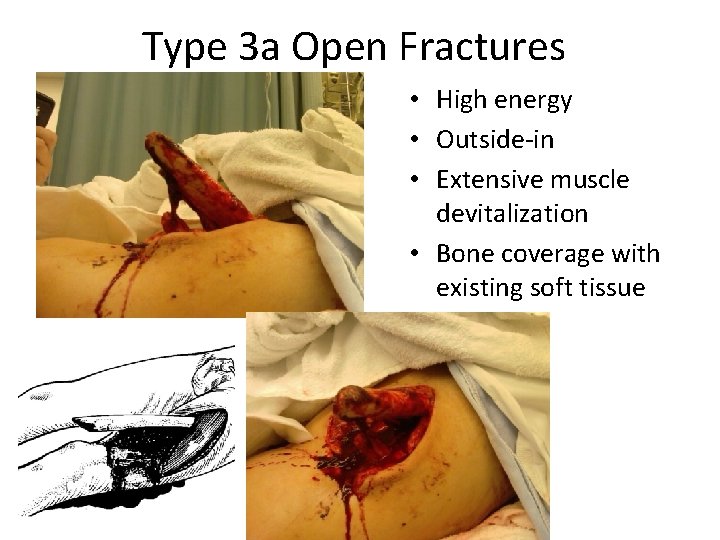
Type 3 a Open Fractures • High energy • Outside-in • Extensive muscle devitalization • Bone coverage with existing soft tissue
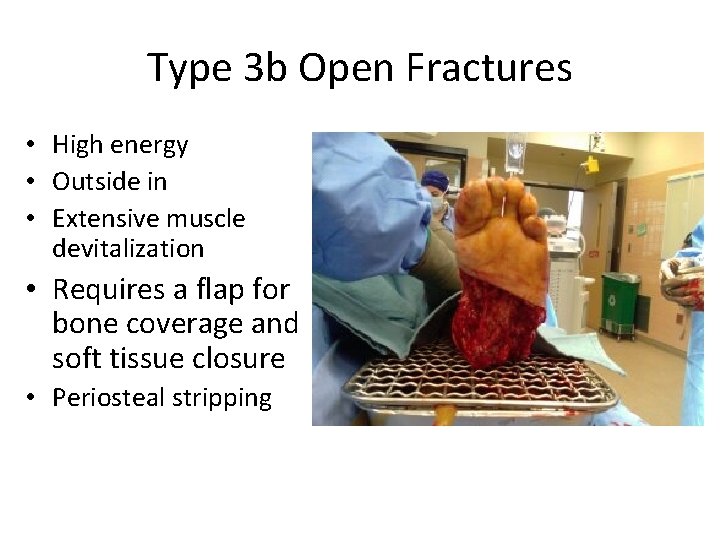
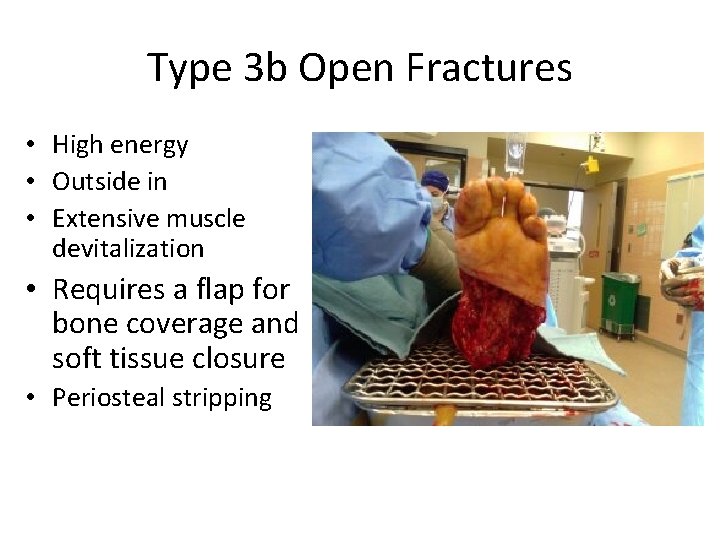
Type 3 b Open Fractures • High energy • Outside in • Extensive muscle devitalization • Requires a flap for bone coverage and soft tissue closure • Periosteal stripping
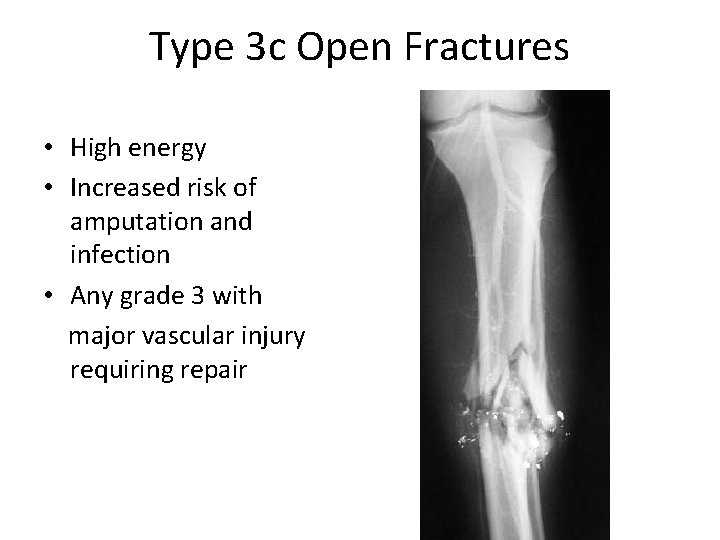
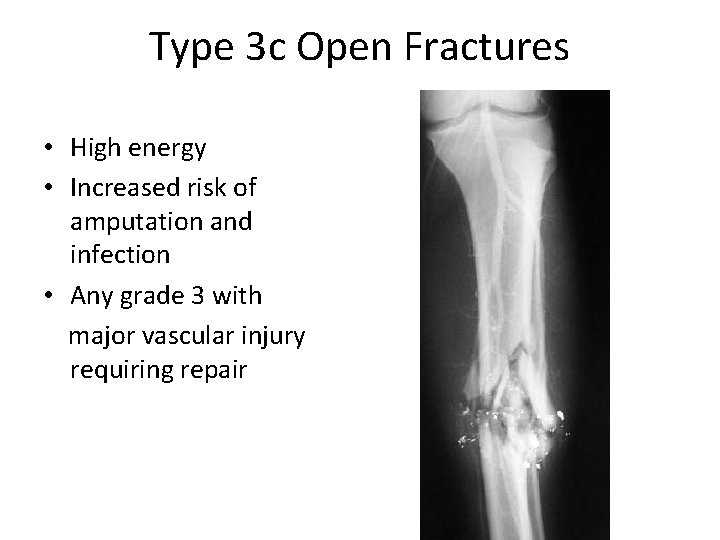
Type 3 c Open Fractures • High energy • Increased risk of amputation and infection • Any grade 3 with major vascular injury requiring repair
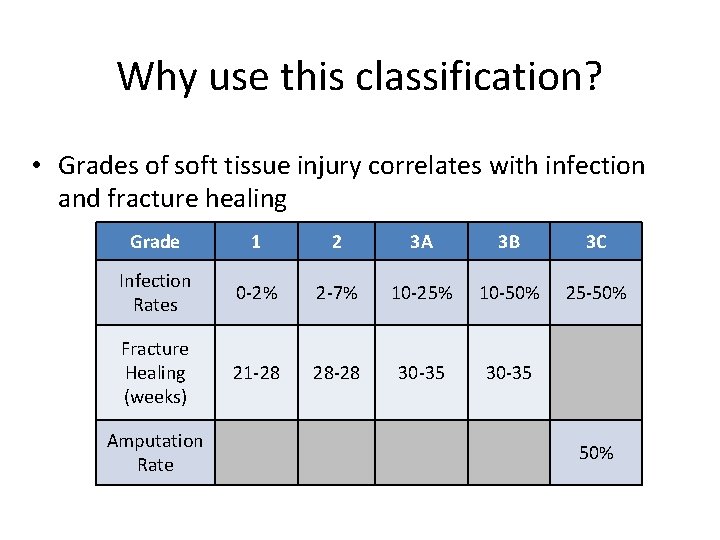
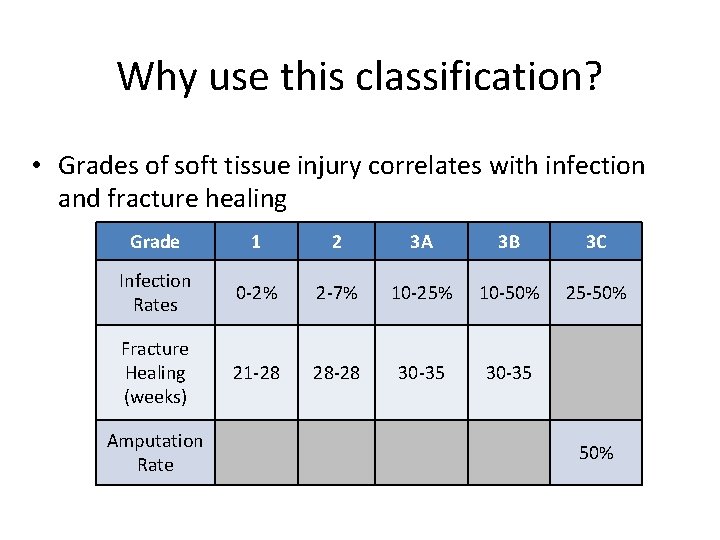
Why use this classification? • Grades of soft tissue injury correlates with infection and fracture healing Grade 1 2 3 A 3 B 3 C Infection Rates 0 -2% 2 -7% 10 -25% 10 -50% 25 -50% Fracture Healing (weeks) 21 -28 28 -28 30 -35 Amputation Rate 50%
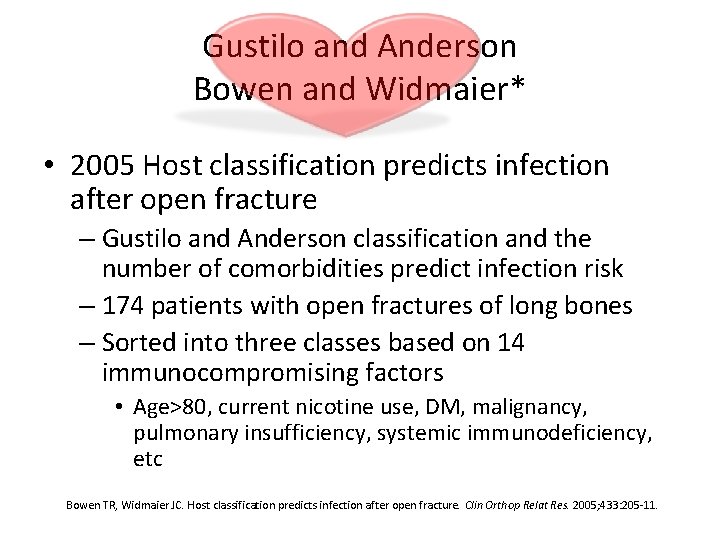
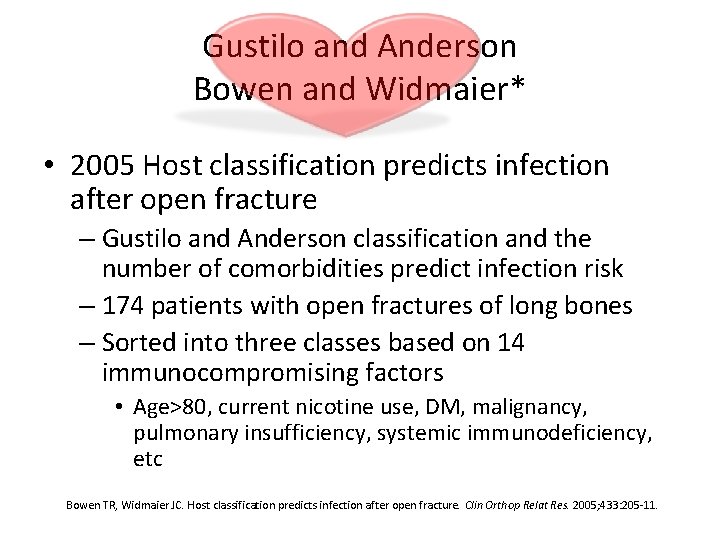
Gustilo and Anderson Bowen and Widmaier* • 2005 Host classification predicts infection after open fracture – Gustilo and Anderson classification and the number of comorbidities predict infection risk – 174 patients with open fractures of long bones – Sorted into three classes based on 14 immunocompromising factors • Age>80, current nicotine use, DM, malignancy, pulmonary insufficiency, systemic immunodeficiency, etc Bowen TR, Widmaier JC. Host classification predicts infection after open fracture. Clin Orthop Relat Res. 2005; 433: 205 -11.
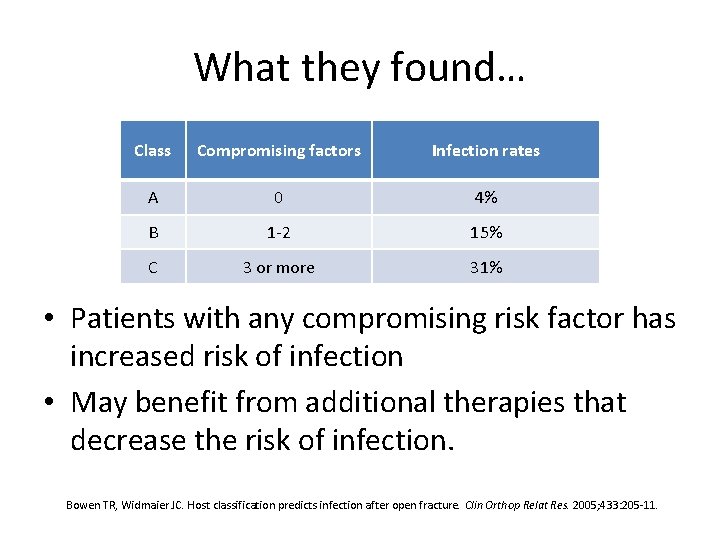
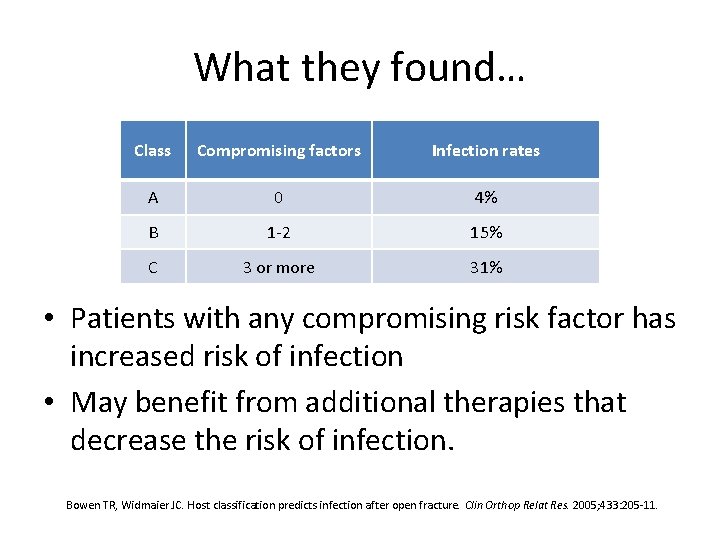
What they found… Class Compromising factors Infection rates A 0 4% B 1 -2 15% C 3 or more 31% • Patients with any compromising risk factor has increased risk of infection • May benefit from additional therapies that decrease the risk of infection. Bowen TR, Widmaier JC. Host classification predicts infection after open fracture. Clin Orthop Relat Res. 2005; 433: 205 -11.
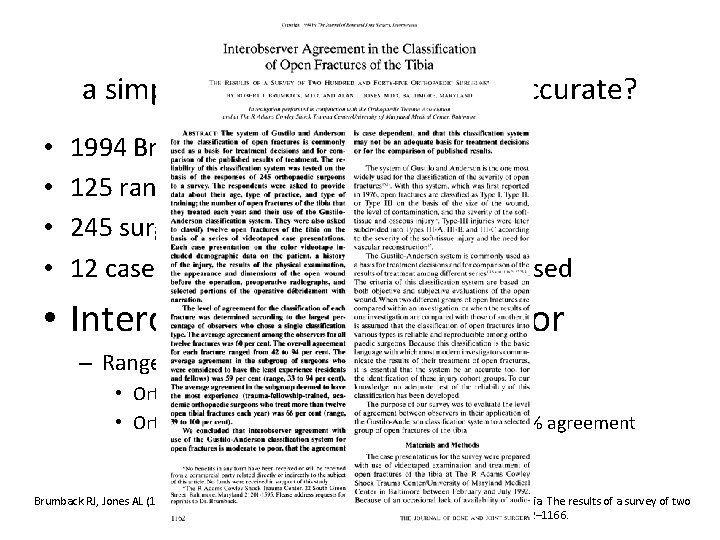
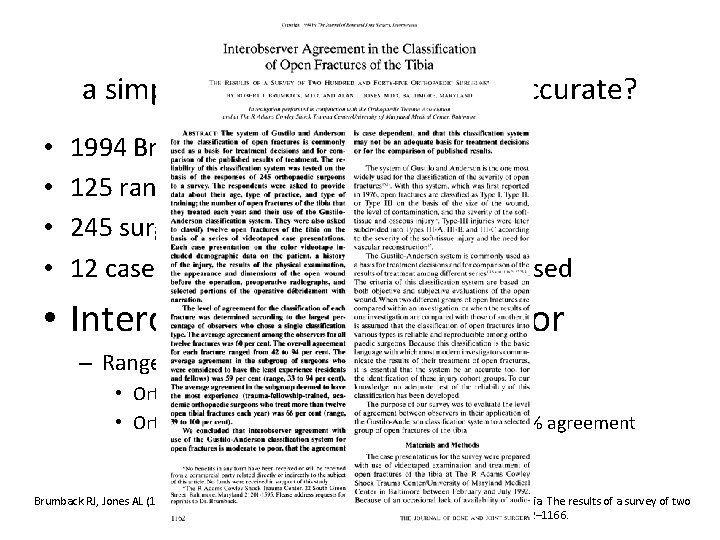
Gustilo Classification: a simple and useful tool, but is it accurate? • • 1994 Brumback et al. 125 randomized open fractures 245 surgeons of various levels of training 12 cases of open tibia fractures, videos used • Interobserver agreement poor – Range 42 -94% for each fracture • Ortho attendings - 59% agreement • Ortho Trauma Fellowship trained attendings - 66% agreement Brumback RJ, Jones AL (1994) Interobserver agreement in the classification of open fractures of the tibia. The results of a survey of two hundred and forty-five orthopaedic surgeons. J Bone and Joint Am; 76(8): 1162– 1166.
So………. • Fracture type should not be classified in the ER • Most reliably done in the OR at the completion of primary wound care and debridement
Microbiology • Most acute infections are caused by pathogens acquired in the hospital • 1976 Gustilo and Anderson – most infections in their study of 326 open fxs developed secondarily • When left open for >2 wks, wounds were prone to nocosomial contaminants such as Pseudomonas and other GN bacteria • Currently most open fracture infections are caused by GNR and GP staph Gustilo RB, Anderson JT: Prevention of Infection in the Treatment of One Thousand Twenty-five Open Fractures of Long Bones; JBJS, 58(4): 453 -458, June 1976
Nocosomial infection? !!!! • Only 18% of infections were caused by the same organism initially isolated in the perioperative cultures* • Carsenti-Etesse et al. 1999 Cover the wounds quickly – 92% of open fracture infections were caused by bacteria acquired while the patient was in the hospital** *Patzakis MJ, Wilkins J, Moore TM: Considerations in reducing the infection rate in open tibial fractures. Clin Orthop Relat Res. 1983 Sep; (178): 36 -41. *Patzakis MJ, Bains RS, Lee J, Shepherd L, Singer G, Ressler R, Harvey F, Holtom P: Prospective, randomized, double-blind study comparing single antibiotic therapy, ciprofloxacin, to combo antibiotic therapy in open fracture wounds. J Orthop Trauma. 2000 Nov; 14(8): 529 -33. **Carsenti-Etesse H, Doyon F, Desplaces N, Gagey O, Tancrede C, Pradier C, Dunais B, Dellamonica P. Epidemiology of bacterial infection during management of open leg fractures. Eur J Clin Microbiol Infect Dis. 1999; 18: 315 -23.
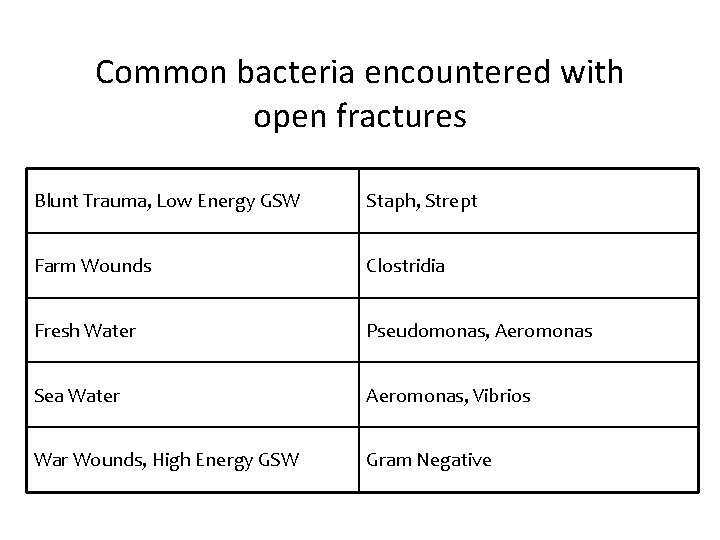
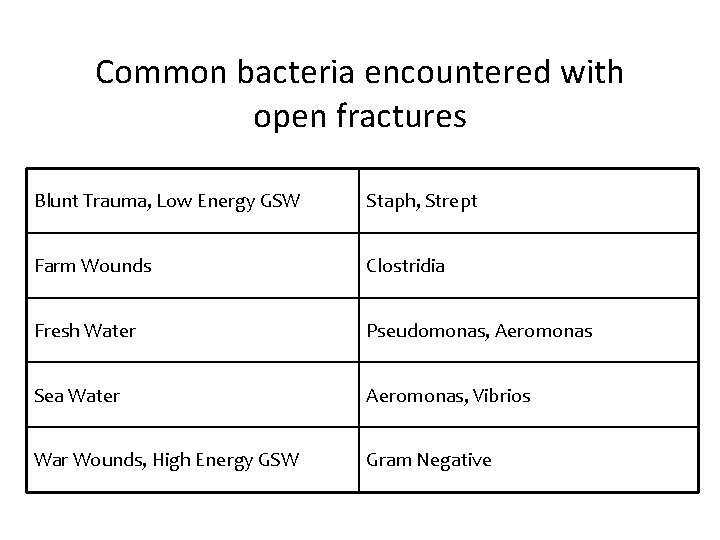
Common bacteria encountered with open fractures Blunt Trauma, Low Energy GSW Staph, Strept Farm Wounds Clostridia Fresh Water Pseudomonas, Aeromonas Sea Water Aeromonas, Vibrios War Wounds, High Energy GSW Gram Negative
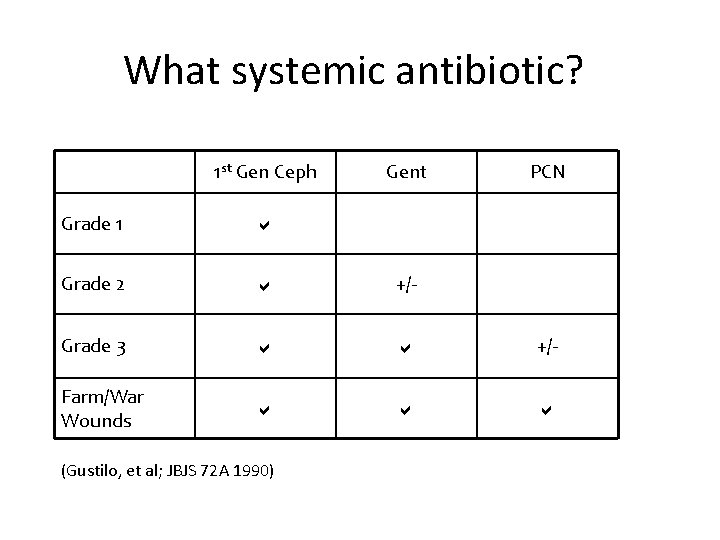
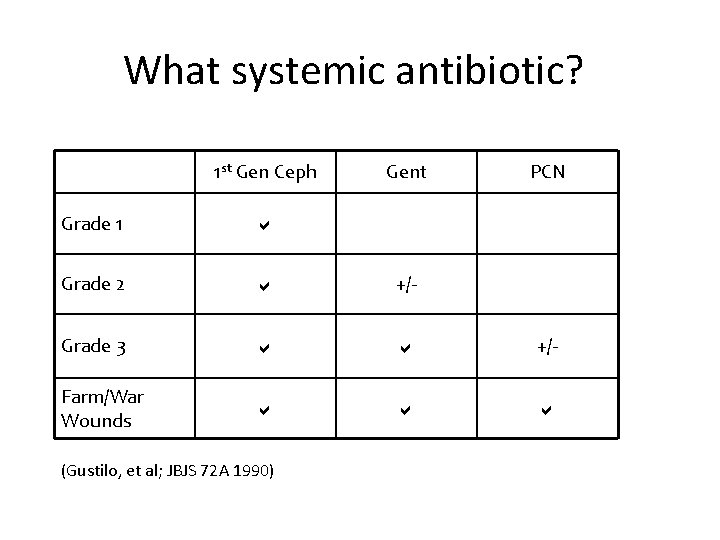
What systemic antibiotic? 1 st Gen Ceph Gent PCN Grade 1 Grade 2 +/- Grade 3 +/- Farm/War Wounds (Gustilo, et al; JBJS 72 A 1990)
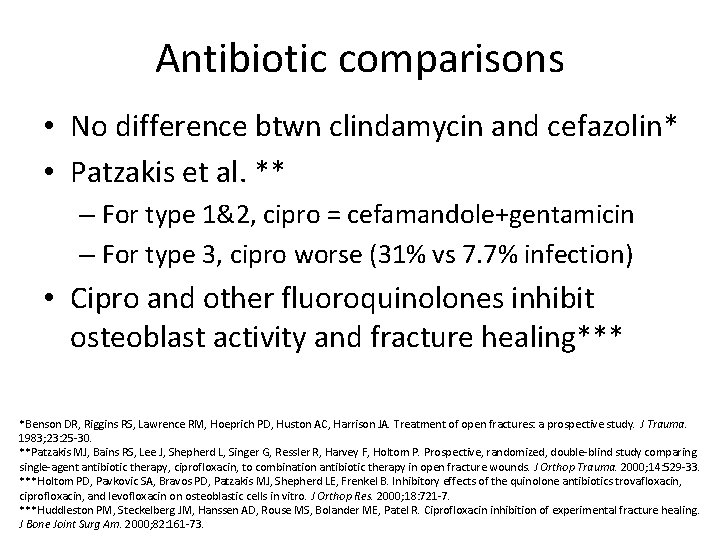
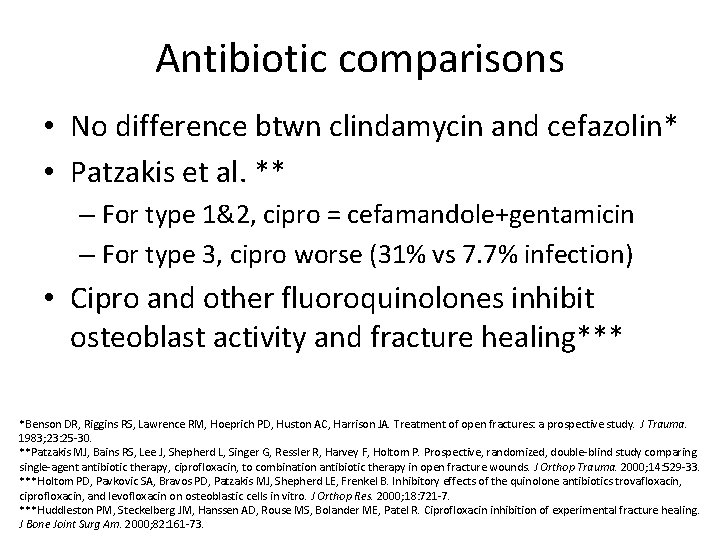
Antibiotic comparisons • No difference btwn clindamycin and cefazolin* • Patzakis et al. ** – For type 1&2, cipro = cefamandole+gentamicin – For type 3, cipro worse (31% vs 7. 7% infection) • Cipro and other fluoroquinolones inhibit osteoblast activity and fracture healing*** *Benson DR, Riggins RS, Lawrence RM, Hoeprich PD, Huston AC, Harrison JA. Treatment of open fractures: a prospective study. J Trauma. 1983; 23: 25 -30. **Patzakis MJ, Bains RS, Lee J, Shepherd L, Singer G, Ressler R, Harvey F, Holtom P. Prospective, randomized, double-blind study comparing single-agent antibiotic therapy, ciprofloxacin, to combination antibiotic therapy in open fracture wounds. J Orthop Trauma. 2000; 14: 529 -33. ***Holtom PD, Pavkovic SA, Bravos PD, Patzakis MJ, Shepherd LE, Frenkel B. Inhibitory effects of the quinolone antibiotics trovafloxacin, ciprofloxacin, and levofloxacin on osteoblastic cells in vitro. J Orthop Res. 2000; 18: 721 -7. ***Huddleston PM, Steckelberg JM, Hanssen AD, Rouse MS, Bolander ME, Patel R. Ciprofloxacin inhibition of experimental fracture healing. J Bone Joint Surg Am. 2000; 82: 161 -73.
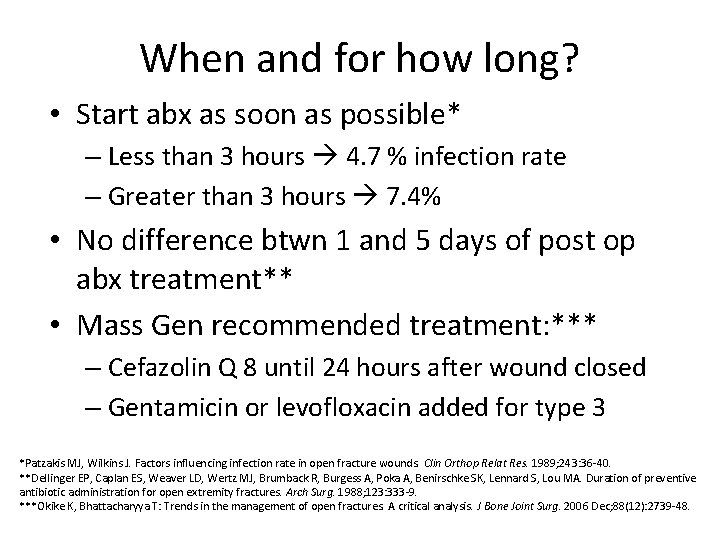
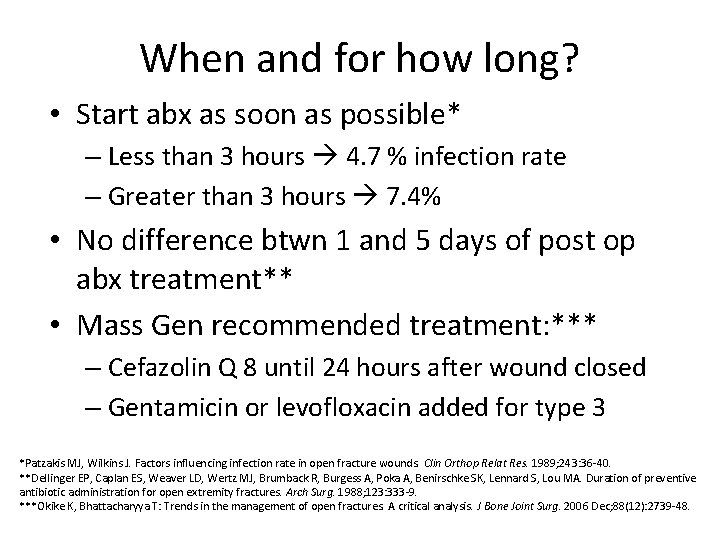
When and for how long? • Start abx as soon as possible* – Less than 3 hours 4. 7 % infection rate – Greater than 3 hours 7. 4% • No difference btwn 1 and 5 days of post op abx treatment** • Mass Gen recommended treatment: *** – Cefazolin Q 8 until 24 hours after wound closed – Gentamicin or levofloxacin added for type 3 *Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res. 1989; 243: 36 -40. **Dellinger EP, Caplan ES, Weaver LD, Wertz MJ, Brumback R, Burgess A, Poka A, Benirschke SK, Lennard S, Lou MA. Duration of preventive antibiotic administration for open extremity fractures. Arch Surg. 1988; 123: 333 -9. ***Okike K, Bhattacharyya T: Trends in the management of open fractures. A critical analysis. J Bone Joint Surg. 2006 Dec; 88(12): 2739 -48.
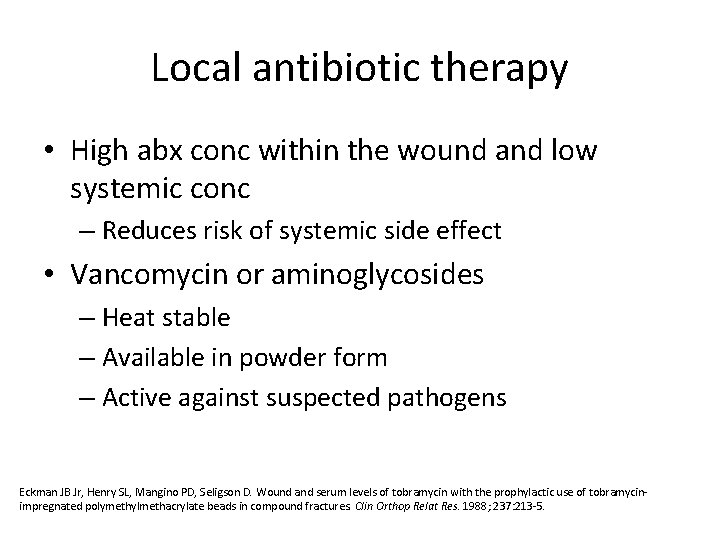
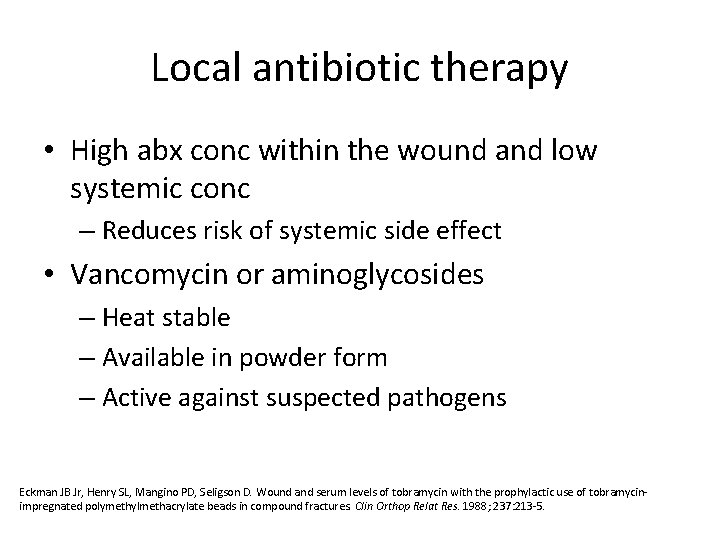
Local antibiotic therapy • High abx conc within the wound and low systemic conc – Reduces risk of systemic side effect • Vancomycin or aminoglycosides – Heat stable – Available in powder form – Active against suspected pathogens Eckman JB Jr, Henry SL, Mangino PD, Seligson D. Wound and serum levels of tobramycin with the prophylactic use of tobramycinimpregnated polymethylmethacrylate beads in compound fractures. Clin Orthop Relat Res. 1988; 237: 213 -5.
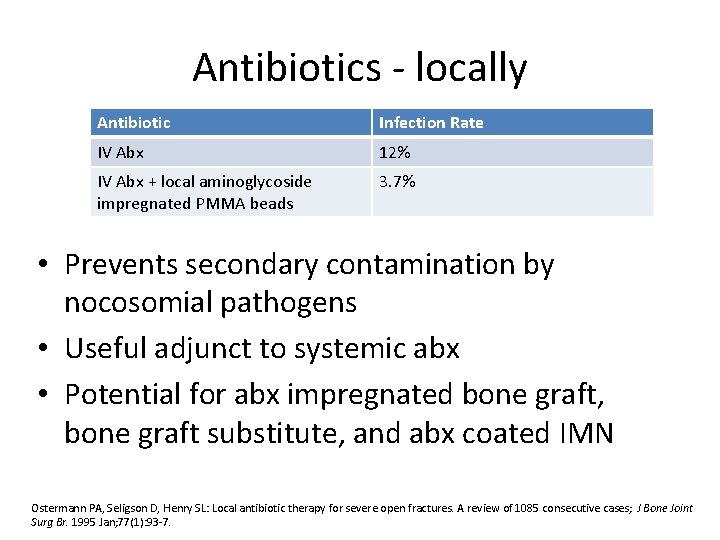
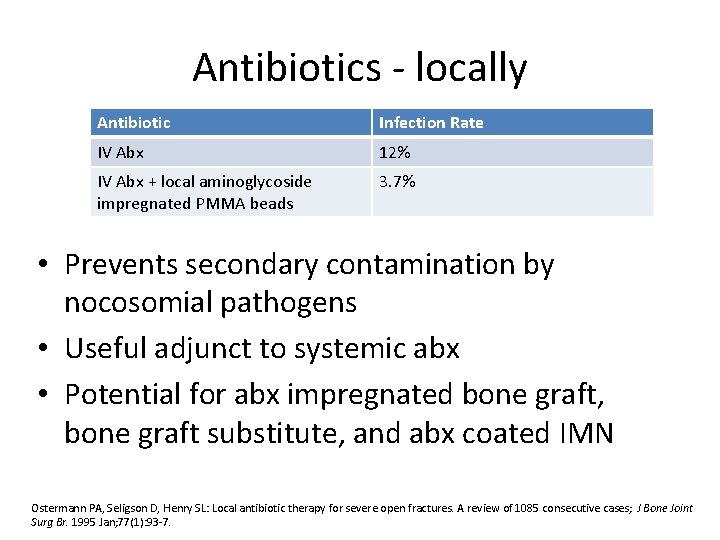
Antibiotics - locally Antibiotic Infection Rate IV Abx 12% IV Abx + local aminoglycoside impregnated PMMA beads 3. 7% • Prevents secondary contamination by nocosomial pathogens • Useful adjunct to systemic abx • Potential for abx impregnated bone graft, bone graft substitute, and abx coated IMN Ostermann PA, Seligson D, Henry SL: Local antibiotic therapy for severe open fractures. A review of 1085 consecutive cases; J Bone Joint Surg Br. 1995 Jan; 77(1): 93 -7.
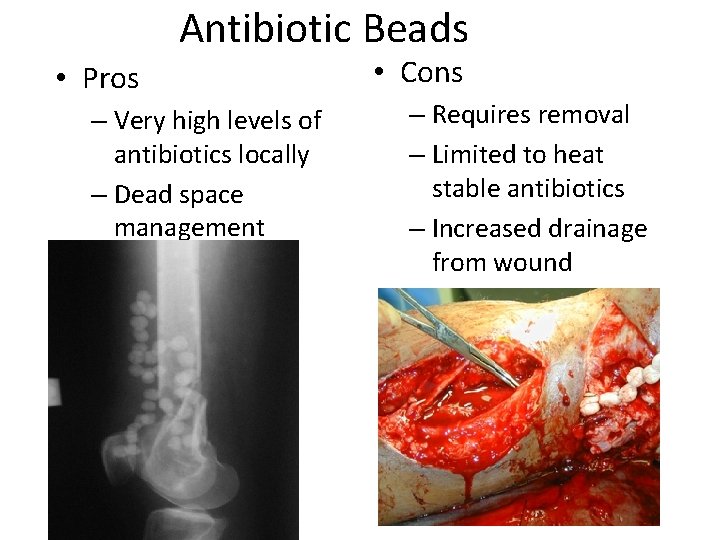
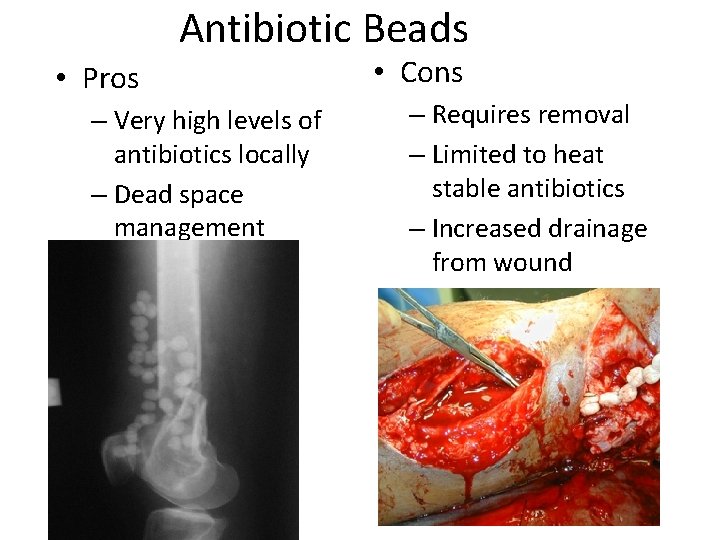
Antibiotic Beads • Pros – Very high levels of antibiotics locally – Dead space management • Cons – Requires removal – Limited to heat stable antibiotics – Increased drainage from wound

Goals of treatment • 1. preserve life • 2. preserve limb • 3. preserve function • Also…. – Prevent infection – Fracture stabilization – Soft tissue coverage
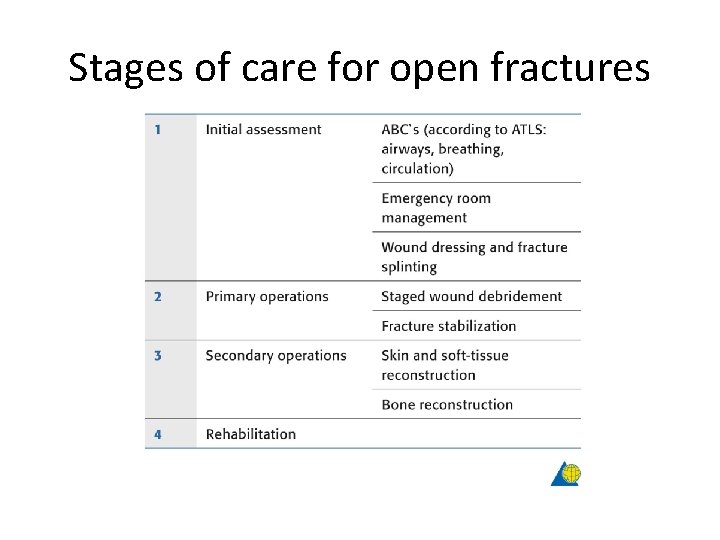
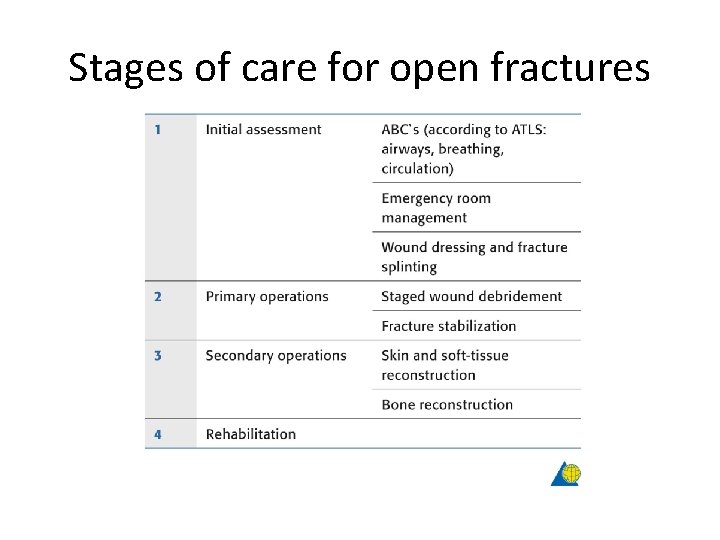
Stages of care for open fractures
Initial assessment & management • • ABC’s Assess entire patient Careful PE, neurovasc Abx and tetanus Local irrigation 1 -2 liters Sterile compressive dressings Realign fracture and splint Do not culture wound in the ED* – 8% of bugs grown caused deep infection – cultures were of no value and not to be done • Recheck pulse, motor and sensation Lee J. Efficacy of cultures in the management of open fractures. Clin Orthop Relat Res. 1997; 339: 71 -5.
Can I take pictures with my phone and send it to my senior? • Documents characteristics accurately • Prevents multiple examinations • Decreases contamination* • Communication via digital photography was more useful than verbal communication** • 1. 3 -megapixel camera is comparable with higher resolution cameras when viewing color images on computer desktop***
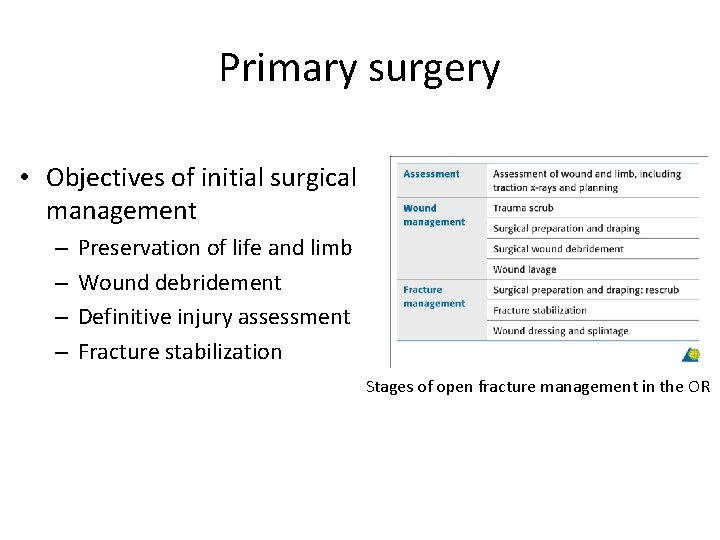
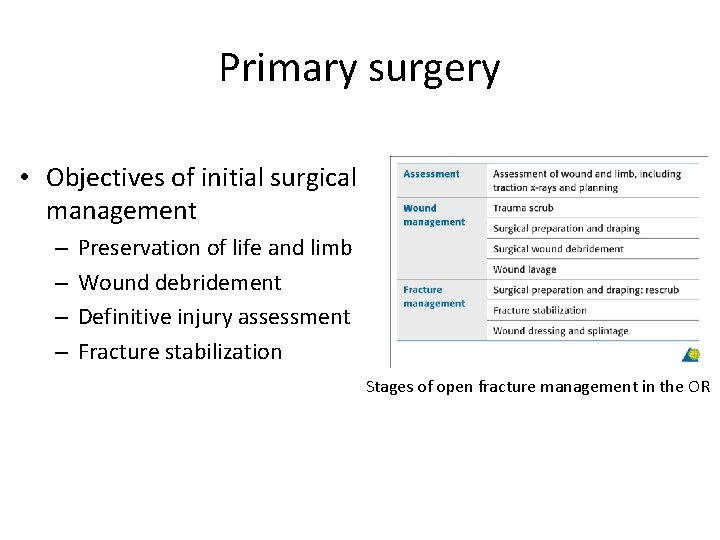
Primary surgery • Objectives of initial surgical management – – Preservation of life and limb Wound debridement Definitive injury assessment Fracture stabilization Stages of open fracture management in the OR
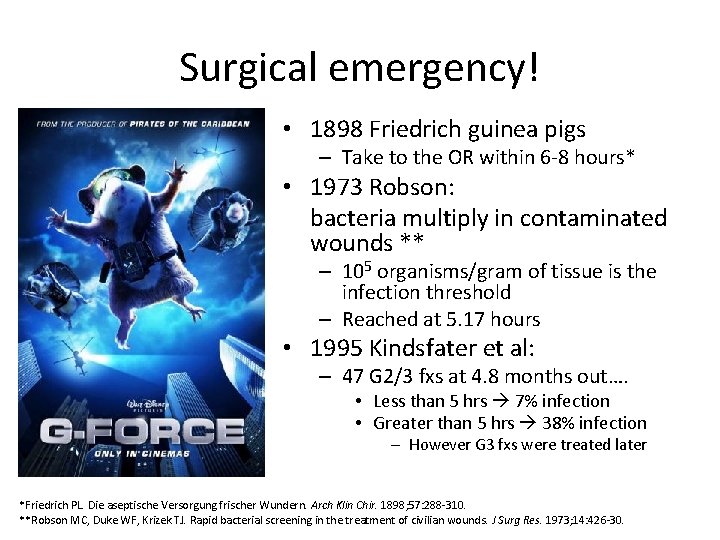
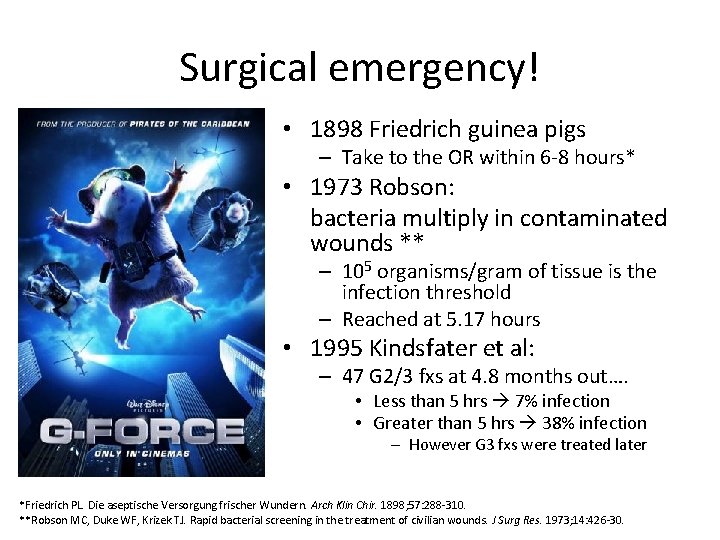
Surgical emergency! • 1898 Friedrich guinea pigs – Take to the OR within 6 -8 hours* • 1973 Robson: bacteria multiply in contaminated wounds ** – 105 organisms/gram of tissue is the infection threshold – Reached at 5. 17 hours • 1995 Kindsfater et al: – 47 G 2/3 fxs at 4. 8 months out…. • Less than 5 hrs 7% infection • Greater than 5 hrs 38% infection – However G 3 fxs were treated later *Friedrich PL. Die aseptische Versorgung frischer Wundern. Arch Klin Chir. 1898; 57: 288 -310. **Robson MC, Duke WF, Krizek TJ. Rapid bacterial screening in the treatment of civilian wounds. J Surg Res. 1973; 14: 426 -30.
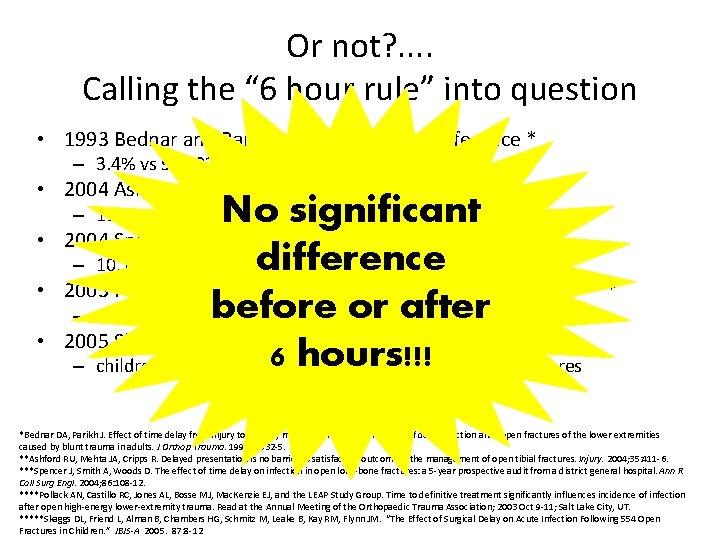
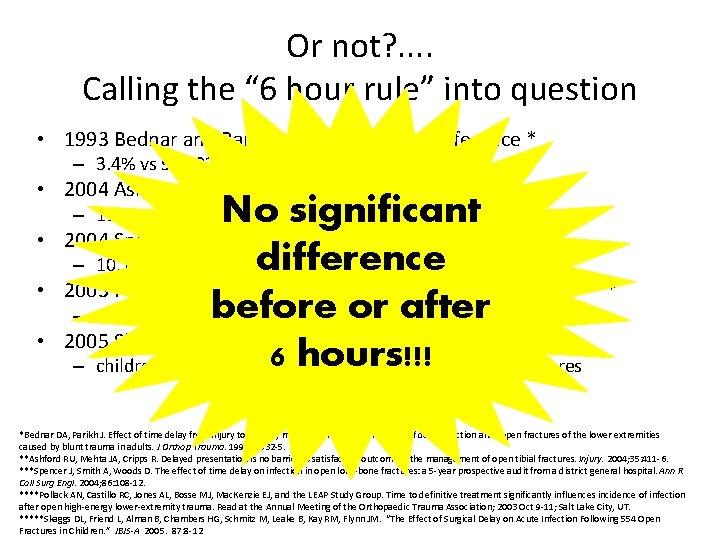
Or not? . . Calling the “ 6 hour rule” into question • 1993 Bednar and Parikh…. No significant difference * – 3. 4% vs 9%; 82 open femoral/tibial fxs • 2004 Ashford et al…. No significant difference ** No significant 2004 Spencer et al. . No significant difference *** difference – 10. 1% vs 10. 9%; 142 open long bone fxs from UK 2003 Pollack and the LEAP investigators…. No correlation**** before or after – 315 open long bone fxs 2005 Skaggs et al…. No significant difference ***** 6 hours!!! – children with all types of open fractures; 554 open fractures – 11% vs 17%; pts from the austrailian outback • • • *Bednar DA, Parikh J. Effect of time delay from injury to primary management on the incidence of deep infection after open fractures of the lower extremities caused by blunt trauma in adults. J Orthop Trauma. 1993; 7: 532 -5. **Ashford RU, Mehta JA, Cripps R. Delayed presentation is no barrier to satisfactory outcome in the management of open tibial fractures. Injury. 2004; 35: 411 -6. ***Spencer J, Smith A, Woods D. The effect of time delay on infection in open long-bone fractures: a 5 -year prospective audit from a district general hospital. Ann R Coll Surg Engl. 2004; 86: 108 -12. ****Pollack AN, Castillo RC, Jones AL, Bosse MJ, Mac. Kenzie EJ, and the LEAP Study Group. Time to definitive treatment significantly influences incidence of infection after open high-energy lower-extremity trauma. Read at the Annual Meeting of the Orthopaedic Trauma Association; 2003 Oct 9 -11; Salt Lake City, UT. *****Skaggs DL, Friend L, Alman B, Chambers HG, Schmitz M, Leake B, Kay RM, Flynn JM. “The Effect of Surgical Delay on Acute Infection Following 554 Open Fractures in Children. ” JBJS-A 2005. 87: 8 -12
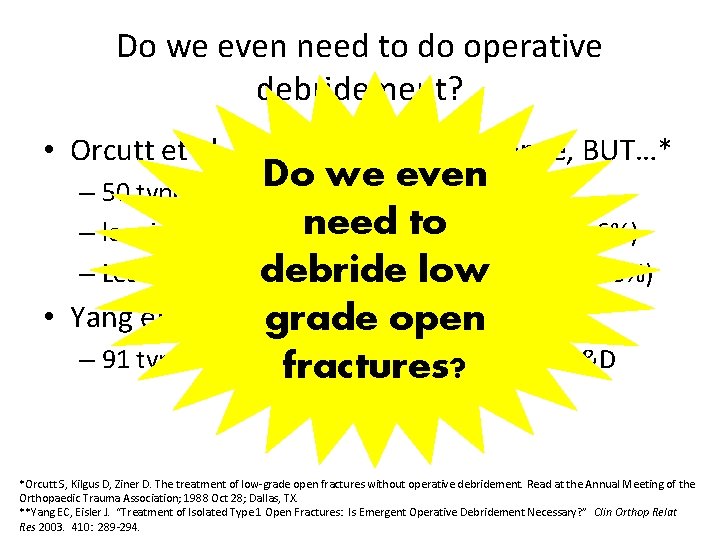
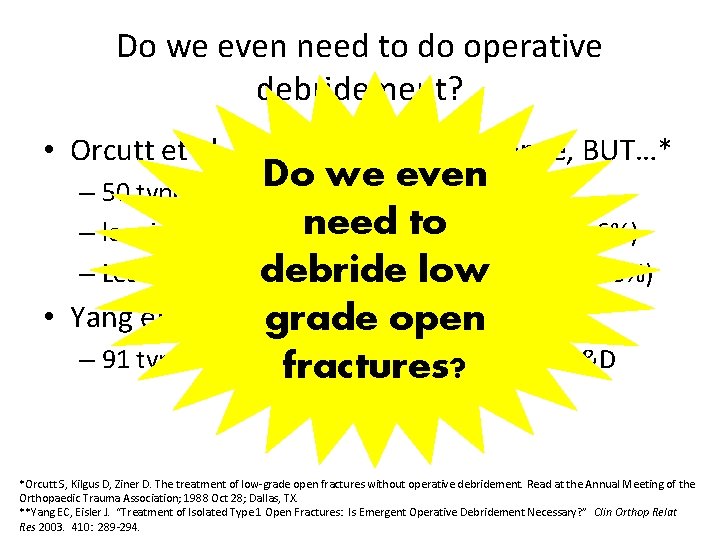
Do we even need to do operative debridement? • Orcutt et al. . . No significant difference, BUT…* Do we even – 50 type 1 &2 open fractures need to – less infection in nonoperative group (3% vs 6%) – Less delayed union in nonop group (10% vs 16%) debride low • Yang et al…. 0% infections ** grade open – 91 type 1 open fractures treated without I&D fractures? *Orcutt S, Kilgus D, Ziner D. The treatment of low-grade open fractures without operative debridement. Read at the Annual Meeting of the Orthopaedic Trauma Association; 1988 Oct 28; Dallas, TX. **Yang EC, Eisler J. “Treatment of Isolated Type 1 Open Fractures: Is Emergent Operative Debridement Necessary? ” Clin Orthop Relat Res 2003. 410: 289 -294.
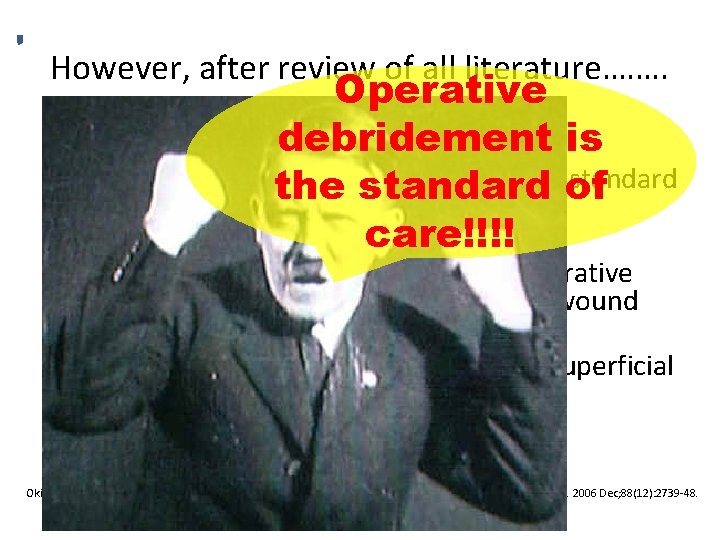
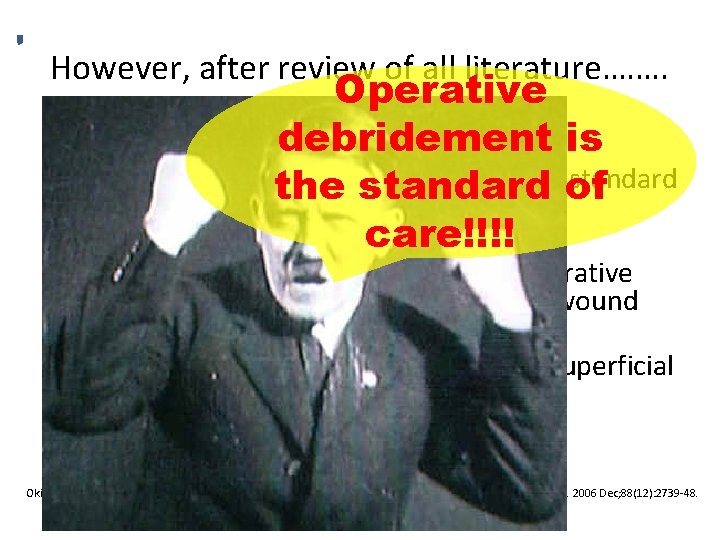
However, after review of all literature…. …. • • • Operative debridement is Okike et al. states…. “Thorough operative debridement is the standard of of care for all open fractures. ” care!!!! “Even if the benefits of formal I&D were insignificant for low grade fractures, operative debridement is still required for proper wound classification. ” • “Open fractures graded on the basis of superficial characteristics are often misclassified. ” • Huge risk not to explore and debride! Okike K, Bhattacharyya T: Trends in the management of open fractures. A critical analysis. J Bone Joint Surg Am. 2006 Dec; 88(12): 2739 -48.
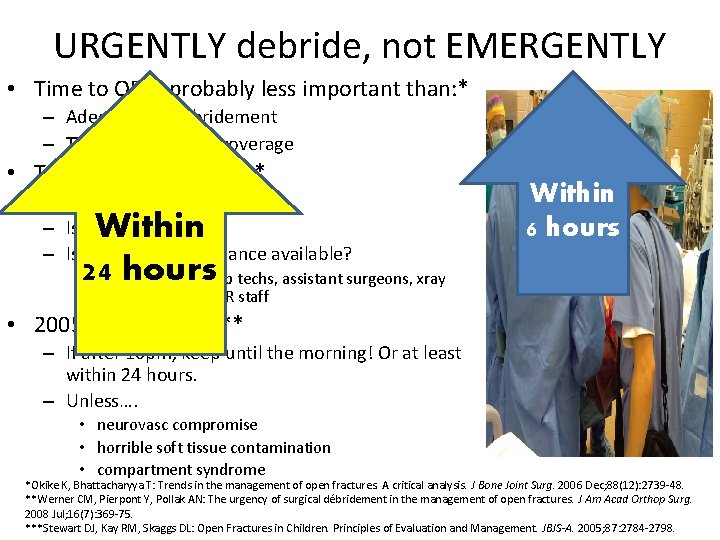
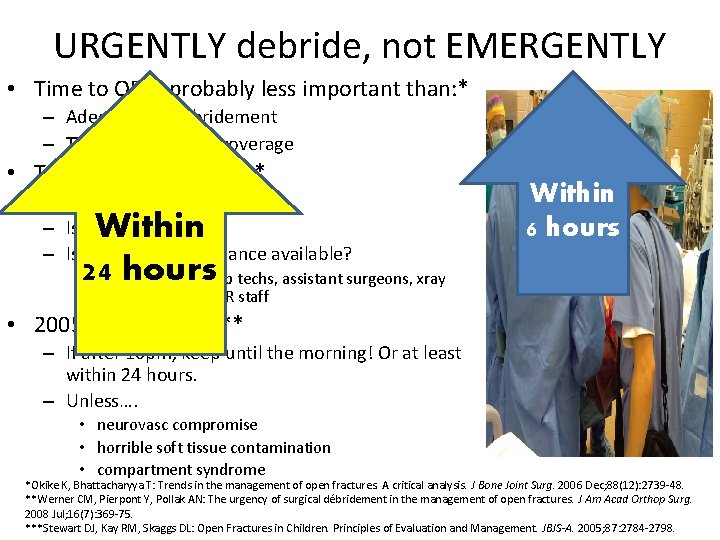
URGENTLY debride, not EMERGENTLY • Time to OR is probably less important than: * – Adequacy of debridement – Time to soft tissue coverage • Timing depends on…. ** – Is patient stable? – Is the OR prepared? – Is appropriate assistance available? Within hours • 24 Ortho trained scrub techs, assistant surgeons, xray Within 6 hours techs, and other OR staff • 2005 Skaggs et al: *** – If after 10 pm, keep until the morning! Or at least within 24 hours. – Unless…. • neurovasc compromise • horrible soft tissue contamination • compartment syndrome *Okike K, Bhattacharyya T: Trends in the management of open fractures. A critical analysis. J Bone Joint Surg. 2006 Dec; 88(12): 2739 -48. **Werner CM, Pierpont Y, Pollak AN: The urgency of surgical débridement in the management of open fractures. J Am Acad Orthop Surg. 2008 Jul; 16(7): 369 -75. ***Stewart DJ, Kay RM, Skaggs DL: Open Fractures in Children. Principles of Evaluation and Management. JBJS-A. 2005; 87: 2784 -2798.
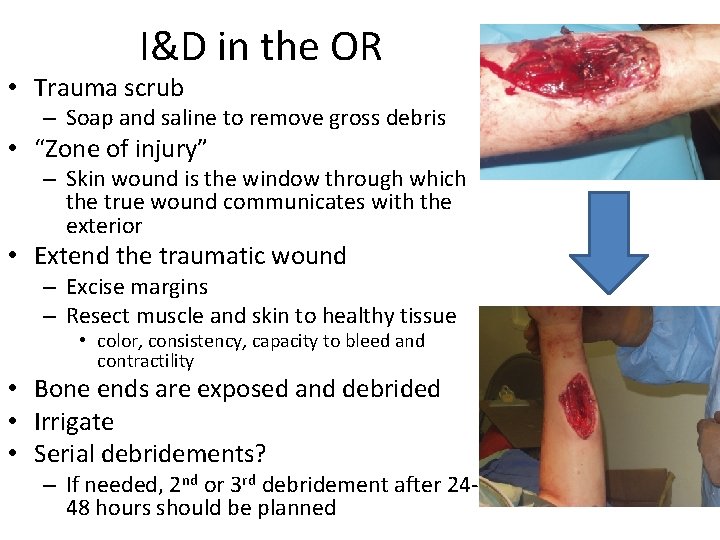
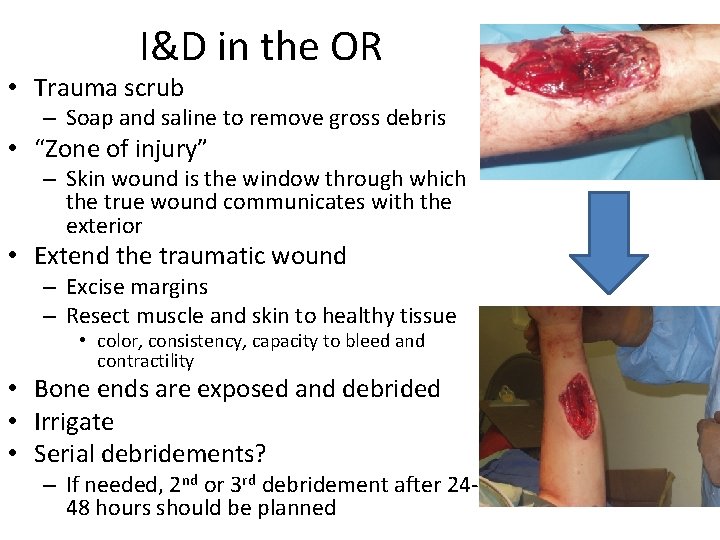
I&D in the OR • Trauma scrub – Soap and saline to remove gross debris • “Zone of injury” – Skin wound is the window through which the true wound communicates with the exterior • Extend the traumatic wound – Excise margins – Resect muscle and skin to healthy tissue • color, consistency, capacity to bleed and contractility • Bone ends are exposed and debrided • Irrigate • Serial debridements? – If needed, 2 nd or 3 rd debridement after 2448 hours should be planned
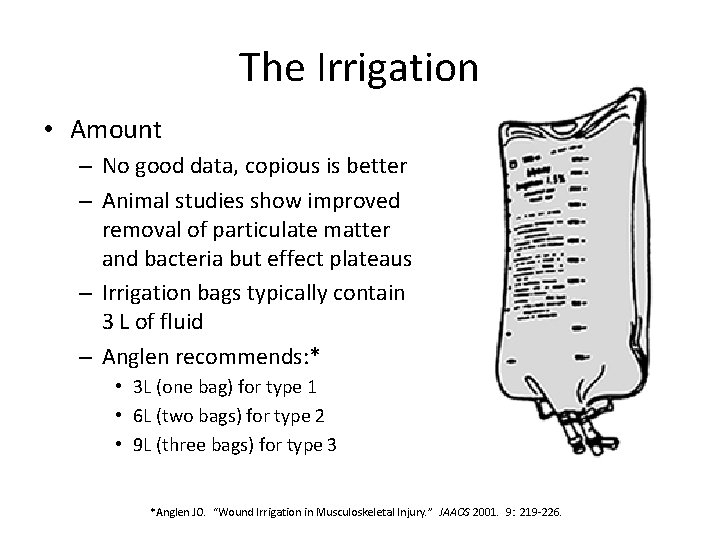
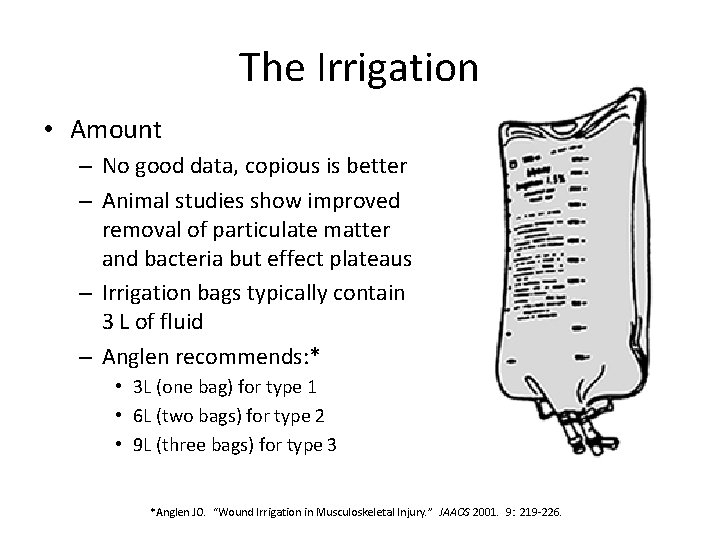
The Irrigation • Amount – No good data, copious is better – Animal studies show improved removal of particulate matter and bacteria but effect plateaus – Irrigation bags typically contain 3 L of fluid – Anglen recommends: * • 3 L (one bag) for type 1 • 6 L (two bags) for type 2 • 9 L (three bags) for type 3 *Anglen JO. “Wound Irrigation in Musculoskeletal Injury. ” JAAOS 2001. 9: 219 -226.
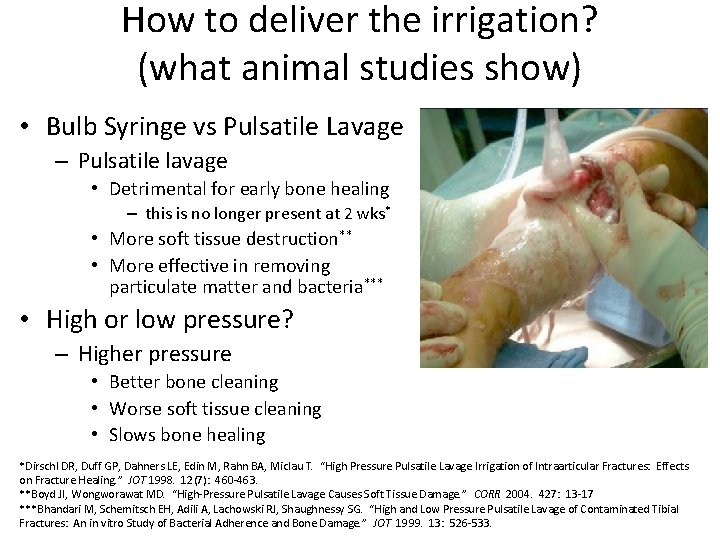
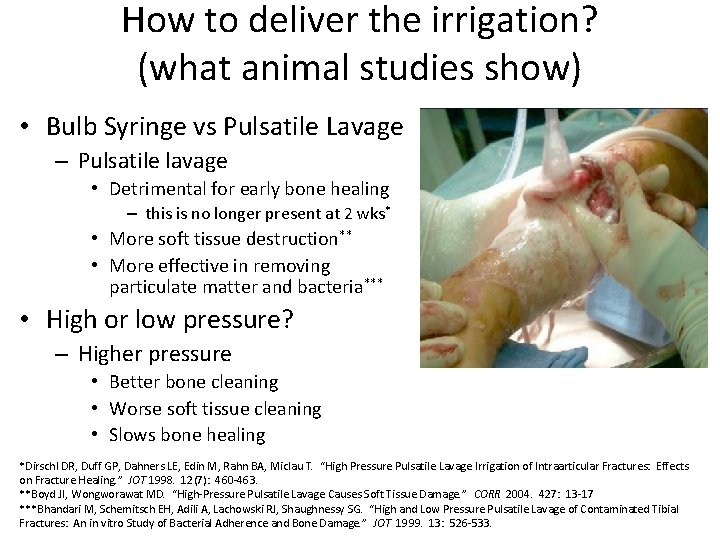
How to deliver the irrigation? (what animal studies show) • Bulb Syringe vs Pulsatile Lavage – Pulsatile lavage • Detrimental for early bone healing – this is no longer present at 2 wks* • More soft tissue destruction** • More effective in removing particulate matter and bacteria*** • High or low pressure? – Higher pressure • Better bone cleaning • Worse soft tissue cleaning • Slows bone healing *Dirschl DR, Duff GP, Dahners LE, Edin M, Rahn BA, Miclau T. “High Pressure Pulsatile Lavage Irrigation of Intraarticular Fractures: Effects on Fracture Healing. ” JOT 1998. 12(7): 460 -463. **Boyd JI, Wongworawat MD. “High-Pressure Pulsatile Lavage Causes Soft Tissue Damage. ” CORR 2004. 427: 13 -17 ***Bhandari M, Schemitsch EH, Adili A, Lachowski RJ, Shaughnessy SG. “High and Low Pressure Pulsatile Lavage of Contaminated Tibial Fractures: An in vitro Study of Bacterial Adherence and Bone Damage. ” JOT 1999. 13: 526 -533.
Antibiotics in the irrigation? • Antibiotics (bacitracin and/or neomycin) – Mixed results, controversial – Costly No proven – ? ? Causing resistance benefit! • bacitracin alone around $500/washout – Wound healing problems? – Few reported cases of anaphylaxis – Anglen: “No proven value in the care of open fracture wounds…some risk, albeit small. ” *Anglen JO. “Wound Irrigation in Musculoskeletal Injury. ” JAAOS 2001. 9: 219 -226.
Soaps in the irrigation? • Surfactants (i. e. Soaps) – Less bacteria adhesion – Emulsify and remove debris – No significant difference in infection or bone healing compared to bacitracin solution, but more wound healing problems in bacitracin group Anglen JO. “Comparison of Soap and Antibiotic Solutions for Irrigation of Lower-Limb Open Fracture Wounds: A Prospective, Randomized Study. ” JBJS-A 2005. 87(7): 1415 -1422.
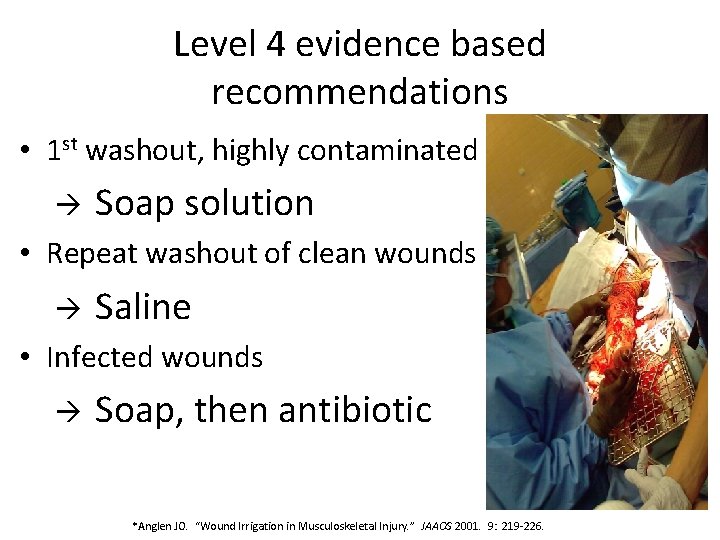
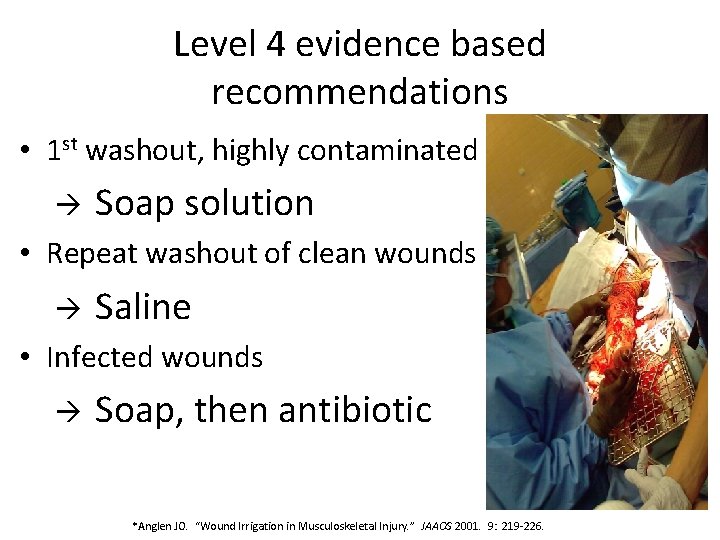
Level 4 evidence based recommendations • 1 st washout, highly contaminated Soap solution • Repeat washout of clean wounds Saline • Infected wounds Soap, then antibiotic *Anglen JO. “Wound Irrigation in Musculoskeletal Injury. ” JAAOS 2001. 9: 219 -226.
Wound closure after contaminated fracture • Timing and technique is controversial OPEN WOUND should be left OPEN! Dubunked! – Prevents anaerobic conditions in wound: Clostridium – Facilitates drainage – Allows repeat debridement Zalavras CG, Patzakis MJ: Open fractures: evaluation and management. J Am Acad Orthop Surg. 2003 May-Jun; 11(3): 212 -9.
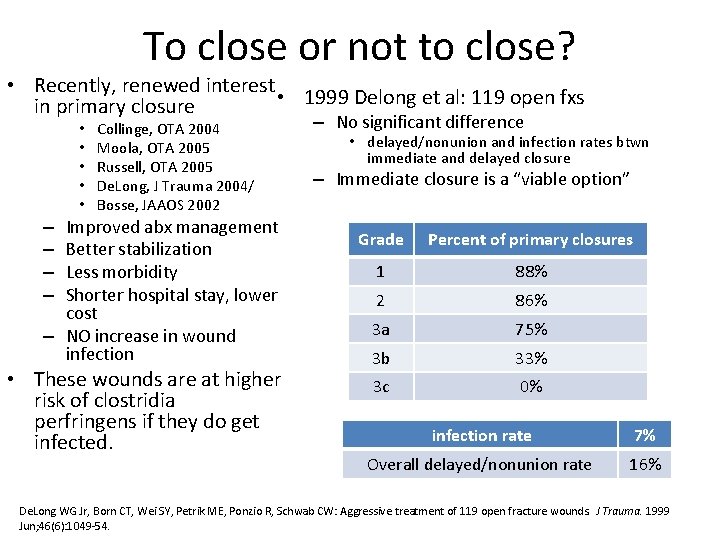
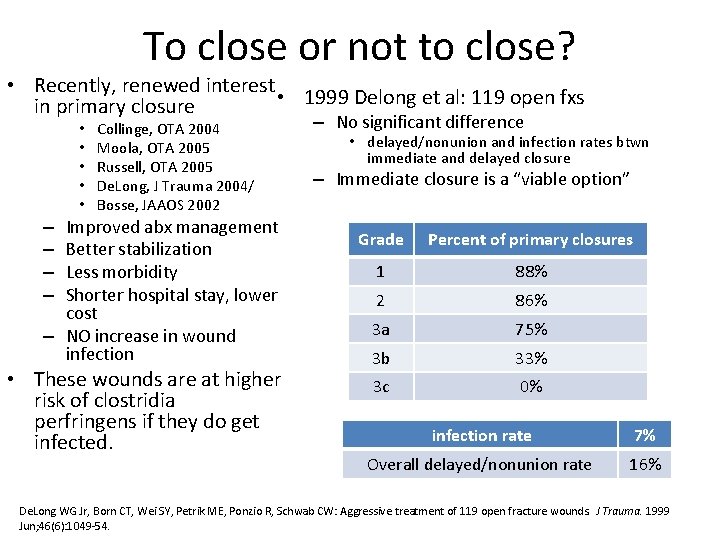
To close or not to close? • Recently, renewed interest • 1999 Delong et al: 119 open fxs in primary closure • • • Collinge, OTA 2004 Moola, OTA 2005 Russell, OTA 2005 De. Long, J Trauma 2004/ Bosse, JAAOS 2002 Improved abx management Better stabilization Less morbidity Shorter hospital stay, lower cost – NO increase in wound infection – – • These wounds are at higher risk of clostridia perfringens if they do get infected. – No significant difference • delayed/nonunion and infection rates btwn immediate and delayed closure – Immediate closure is a “viable option” Grade Percent of primary closures 1 88% 2 86% 3 a 75% 3 b 33% 3 c 0% infection rate 7% Overall delayed/nonunion rate 16% De. Long WG Jr, Born CT, Wei SY, Petrik ME, Ponzio R, Schwab CW: Aggressive treatment of 119 open fracture wounds. J Trauma. 1999 Jun; 46(6): 1049 -54.
Contraindications to primary closure • • • Inadequate debridement Gross contamination Farm related or freshwater immersion injuries Delay in treatment >12 hours Delay in giving abx Compromised host or tissue viability
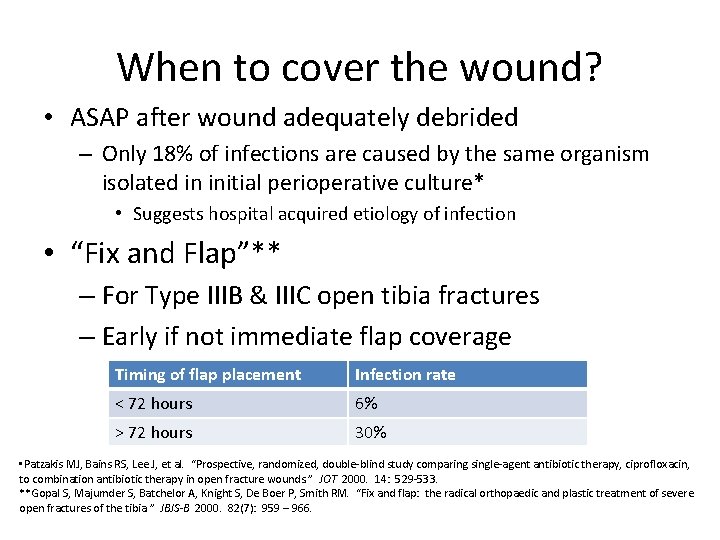
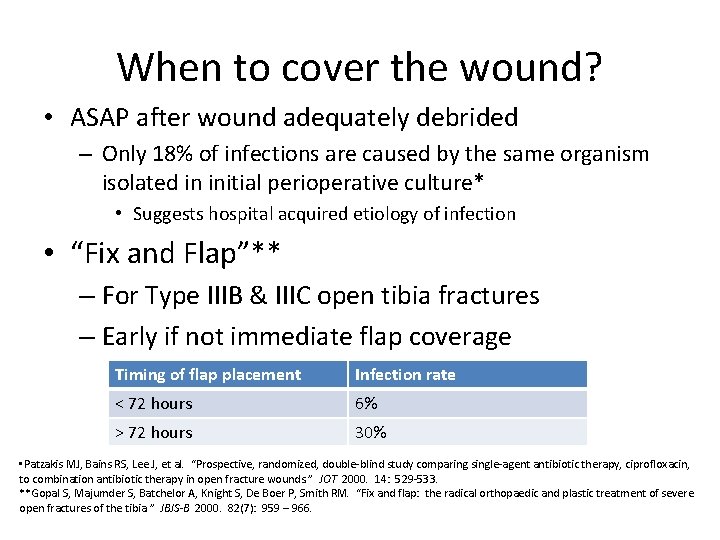
When to cover the wound? • ASAP after wound adequately debrided – Only 18% of infections are caused by the same organism isolated in initial perioperative culture* • Suggests hospital acquired etiology of infection • “Fix and Flap”** – For Type IIIB & IIIC open tibia fractures – Early if not immediate flap coverage Timing of flap placement Infection rate < 72 hours 6% > 72 hours 30% • Patzakis MJ, Bains RS, Lee J, et al. “Prospective, randomized, double-blind study comparing single-agent antibiotic therapy, ciprofloxacin, to combination antibiotic therapy in open fracture wounds. ” JOT 2000. 14: 529 -533. **Gopal S, Majumder S, Batchelor A, Knight S, De Boer P, Smith RM. “Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. ” JBJS-B 2000. 82(7): 959 – 966.
Dressings • Temporary closures – rubber bands • Wet to dry dressings • Semi-permeable membranes • Antibiotic bead pouch • VAC
VAC • Vacuum assisted wound closure – Recommended for temporary management – Mechanically induced negative pressure in a closed system – Removes fluid from extravascular space – Reduced edema – Improves microcirculation – Enhances proliferation of reparative granulation tissue • Open cell polyurethane foam dressing ensures an even distribution of negative pressure -Webb LX: New techniques in wound management: vacuum-assisted wound closure. J Am Acad Orthop Surg. 2002 Sep-Oct; 10(5): 303 -11. -Dedmond BT, Kortesis B, Punger K, Simpson J, Argenta A, Kulp B, Morykwas M, Webb L. “The use of Negative Pressure Wound Therapy in the Temporary Treatment of Soft Tissue Injuries associated with High Energy Open Tibial Shaft Fractures. ” JOT. 2007
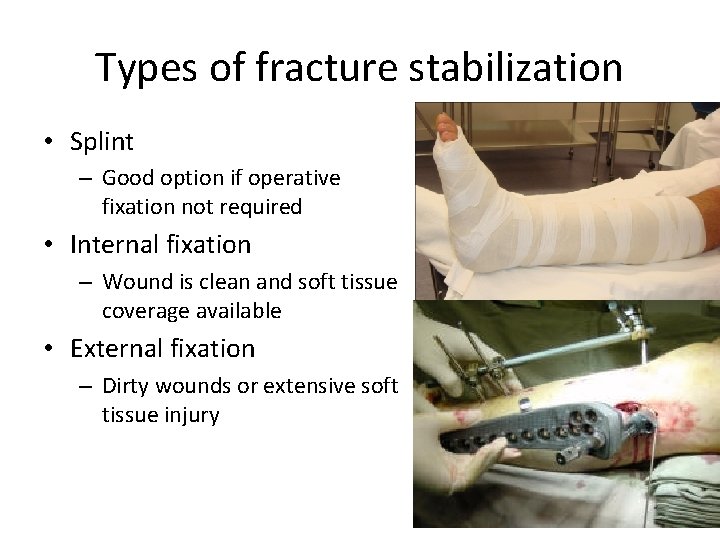
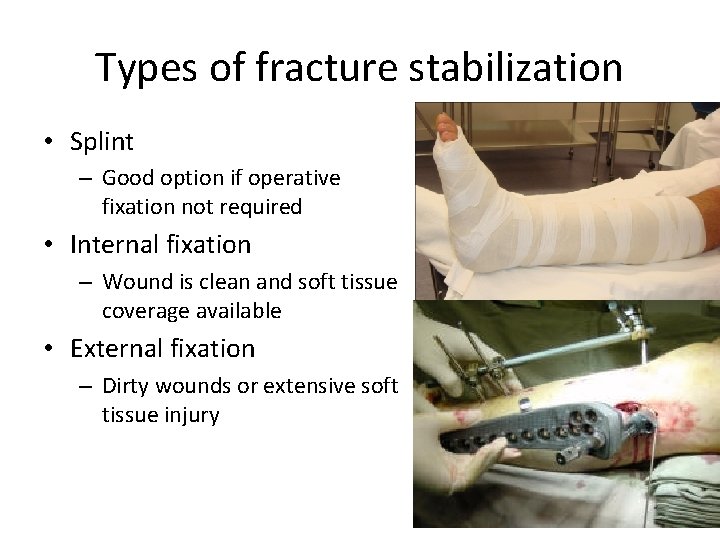
Types of fracture stabilization • Splint – Good option if operative fixation not required • Internal fixation – Wound is clean and soft tissue coverage available • External fixation – Dirty wounds or extensive soft tissue injury
Fracture stabilization • Gustilo type 1 injury can be treated the same way as a comparable closed fracture • Most cases involve surgical fixation • Outcome is similar to closed counterparts
Fracture stabilization • Gustilo type 2&3 usually displaced and unstable – dictate surgical fixation • Restore length, alignment, rotation and provide stability – ideal environment for soft tissue healing and reduces wound infection – reduces dead space and hematoma volume • Inflammatory response dampened • Exudates and edema is reduced • Tissue revascularization is encouraged
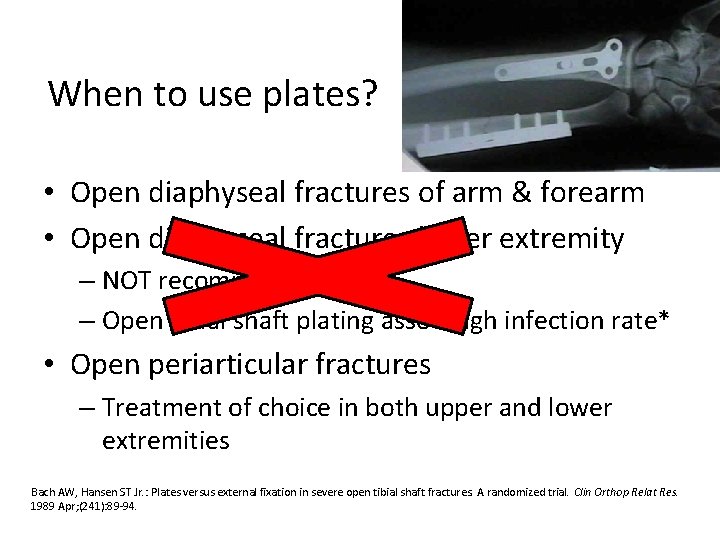
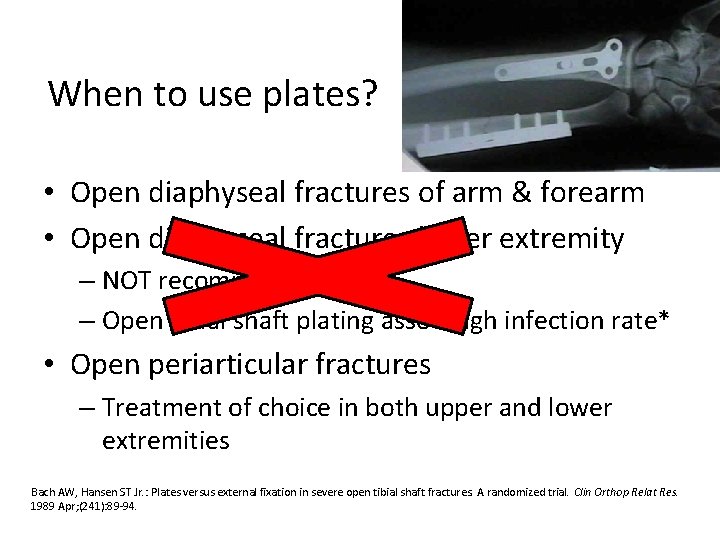
When to use plates? • Open diaphyseal fractures of arm & forearm • Open diaphyseal fractures lower extremity – NOT recommended – Open tibial shaft plating assoc high infection rate* • Open periarticular fractures – Treatment of choice in both upper and lower extremities Bach AW, Hansen ST Jr. : Plates versus external fixation in severe open tibial shaft fractures. A randomized trial. Clin Orthop Relat Res. 1989 Apr; (241): 89 -94.
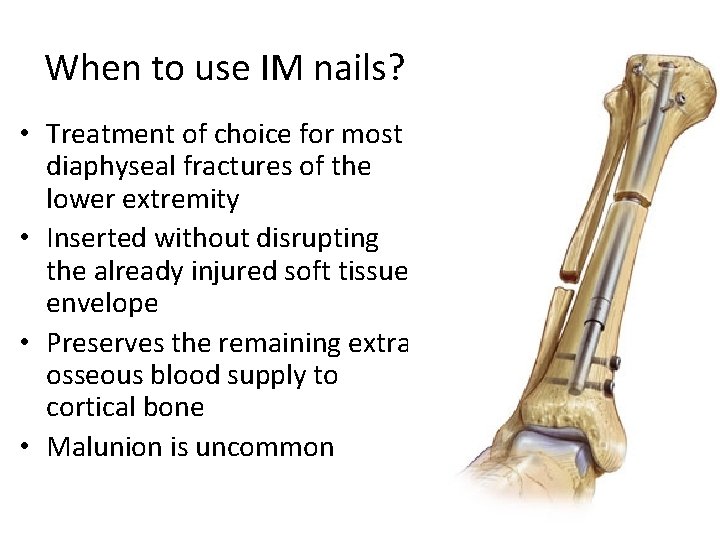
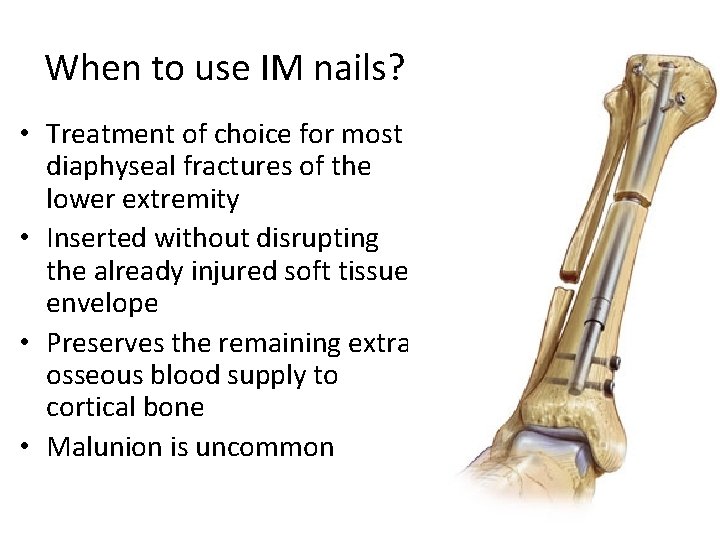
When to use IM nails? • Treatment of choice for most diaphyseal fractures of the lower extremity • Inserted without disrupting the already injured soft tissue envelope • Preserves the remaining extra osseous blood supply to cortical bone • Malunion is uncommon
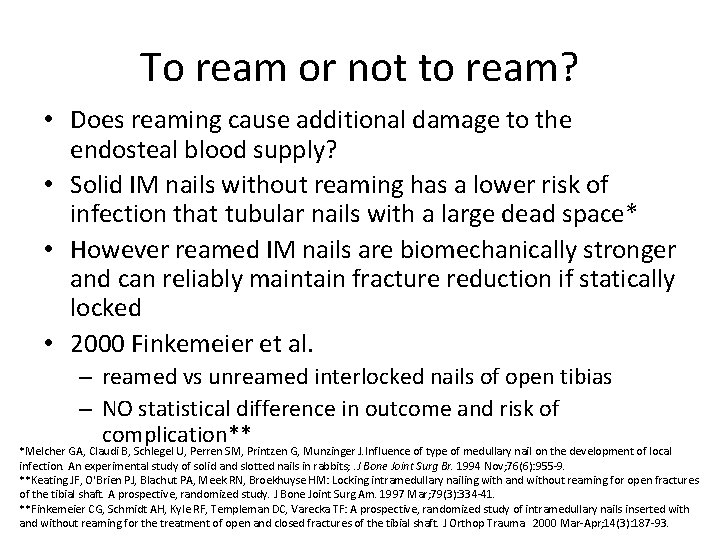
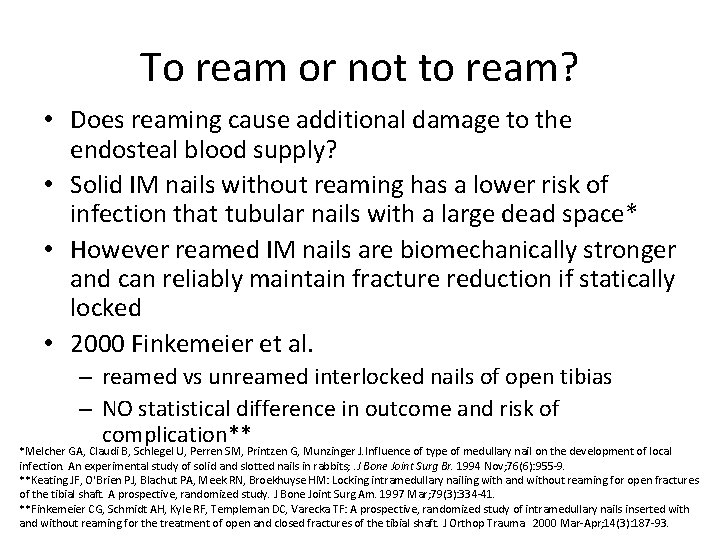
To ream or not to ream? • Does reaming cause additional damage to the endosteal blood supply? • Solid IM nails without reaming has a lower risk of infection that tubular nails with a large dead space* • However reamed IM nails are biomechanically stronger and can reliably maintain fracture reduction if statically locked • 2000 Finkemeier et al. – reamed vs unreamed interlocked nails of open tibias – NO statistical difference in outcome and risk of complication** *Melcher GA, Claudi B, Schlegel U, Perren SM, Printzen G, Munzinger J. Influence of type of medullary nail on the development of local infection. An experimental study of solid and slotted nails in rabbits; . J Bone Joint Surg Br. 1994 Nov; 76(6): 955 -9. **Keating JF, O'Brien PJ, Blachut PA, Meek RN, Broekhuyse HM: Locking intramedullary nailing with and without reaming for open fractures of the tibial shaft. A prospective, randomized study. J Bone Joint Surg Am. 1997 Mar; 79(3): 334 -41. **Finkemeier CG, Schmidt AH, Kyle RF, Templeman DC, Varecka TF: A prospective, randomized study of intramedullary nails inserted with and without reaming for the treatment of open and closed fractures of the tibial shaft. J Orthop Trauma. 2000 Mar-Apr; 14(3): 187 -93.
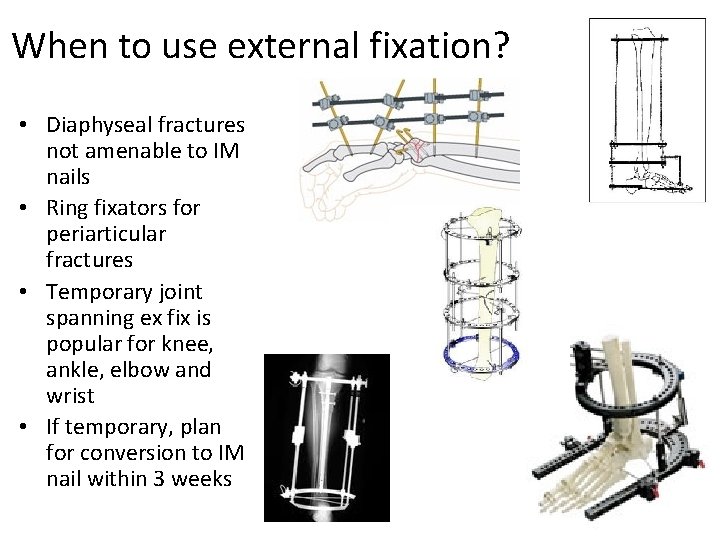
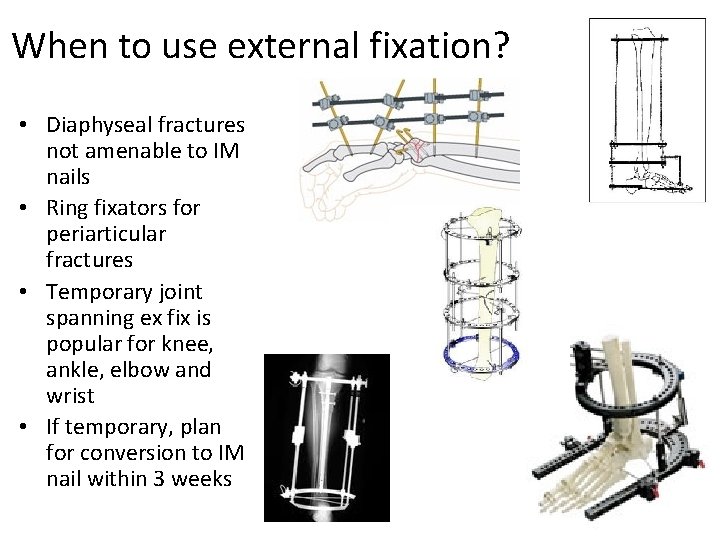
When to use external fixation? • Diaphyseal fractures not amenable to IM nails • Ring fixators for periarticular fractures • Temporary joint spanning ex fix is popular for knee, ankle, elbow and wrist • If temporary, plan for conversion to IM nail within 3 weeks
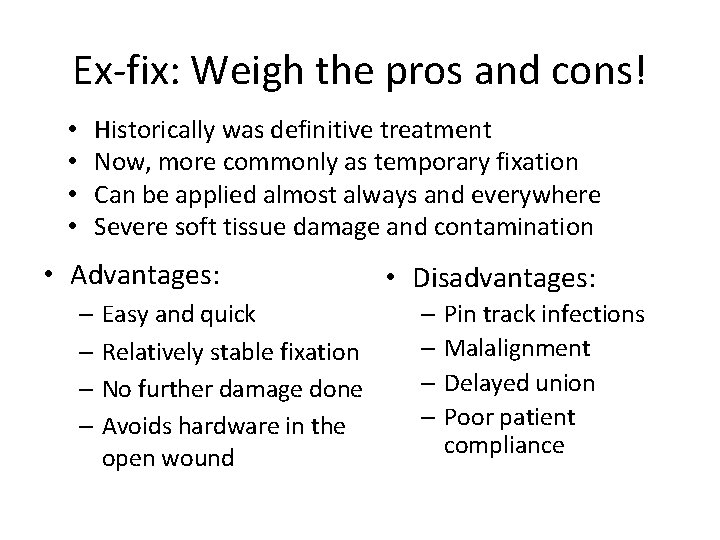
Ex-fix: Weigh the pros and cons! • • Historically was definitive treatment Now, more commonly as temporary fixation Can be applied almost always and everywhere Severe soft tissue damage and contamination • Advantages: – Easy and quick – Relatively stable fixation – No further damage done – Avoids hardware in the open wound • Disadvantages: – Pin track infections – Malalignment – Delayed union – Poor patient compliance
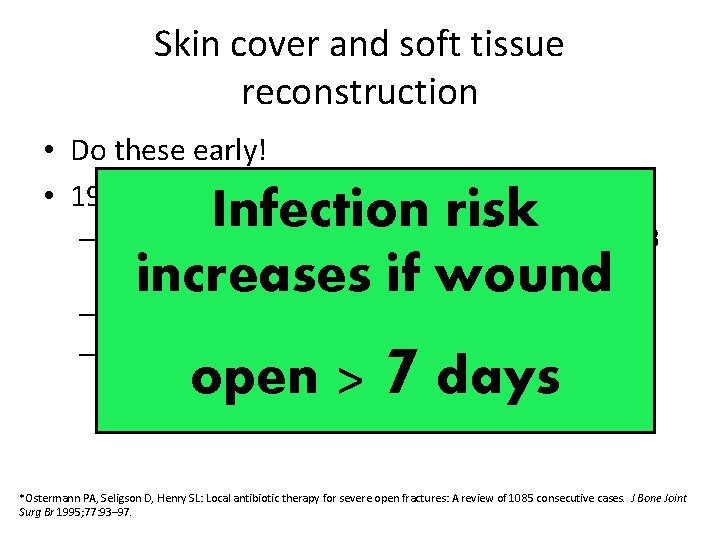
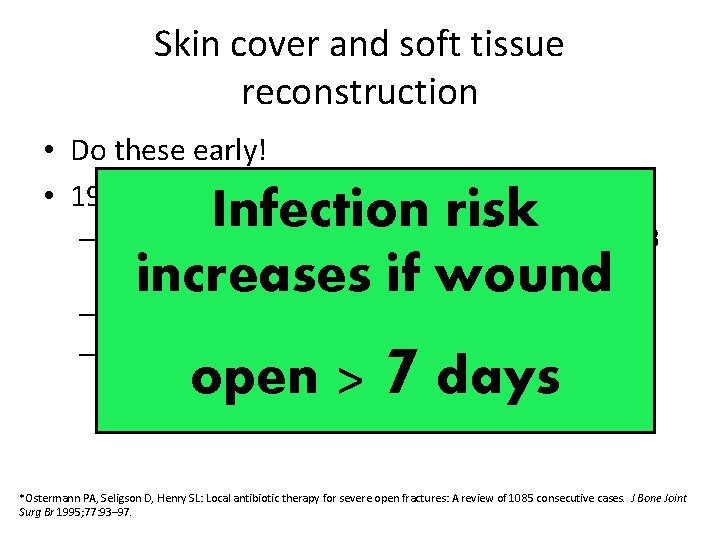
Skin cover and soft tissue reconstruction • Do these early! • 1994 Osterman et al. * Infection risk – Retrospective 1085 fractures, 115 G 2 and 239 G 3 • All treated with appropriate IV Abx and I&D increases if wound – No infection if wounds closed at 7. 6 days – Yes infection if wounds closed at 17. 9 days open > 7 days *Ostermann PA, Seligson D, Henry SL: Local antibiotic therapy for severe open fractures: A review of 1085 consecutive cases. J Bone Joint Surg Br 1995; 77: 93– 97.
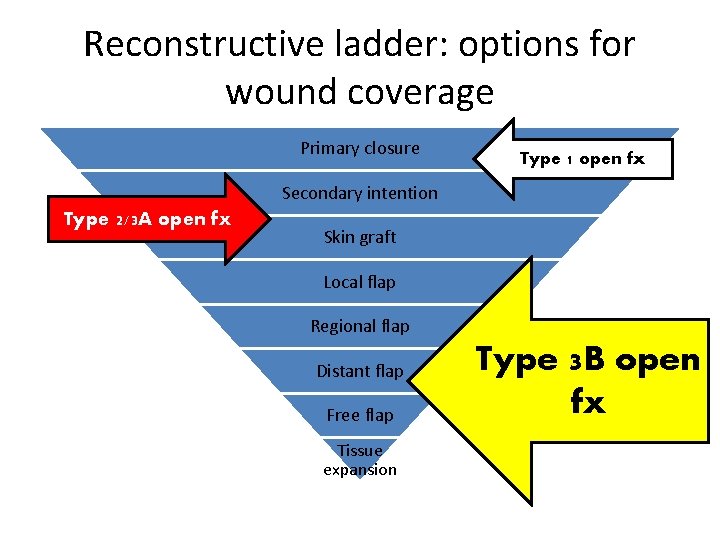
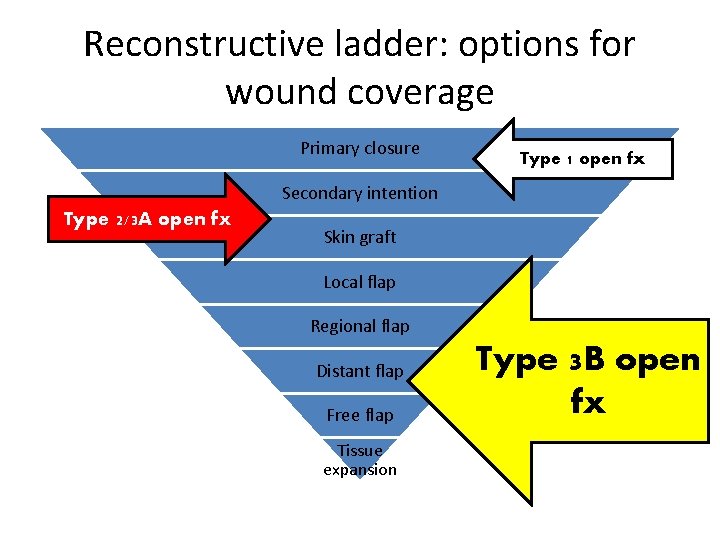
Reconstructive ladder: options for wound coverage Primary closure Type 1 open fx Secondary intention Type 2/3 A open fx Skin graft Local flap Regional flap Distant flap Free flap Tissue expansion Type 3 B open fx
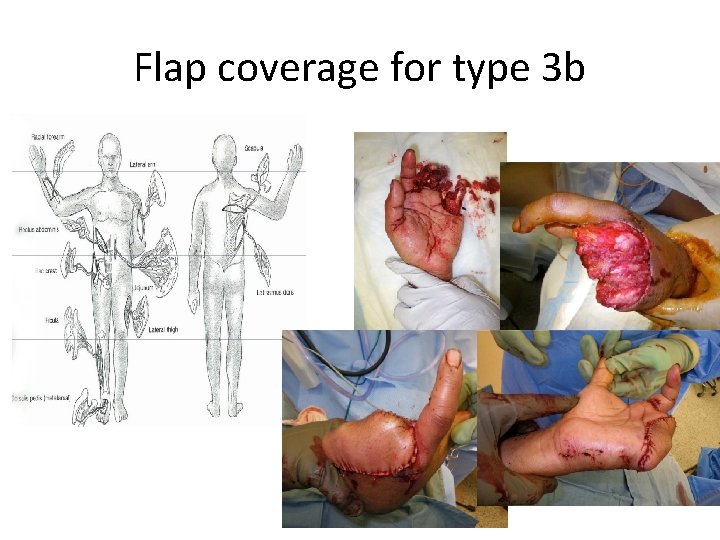
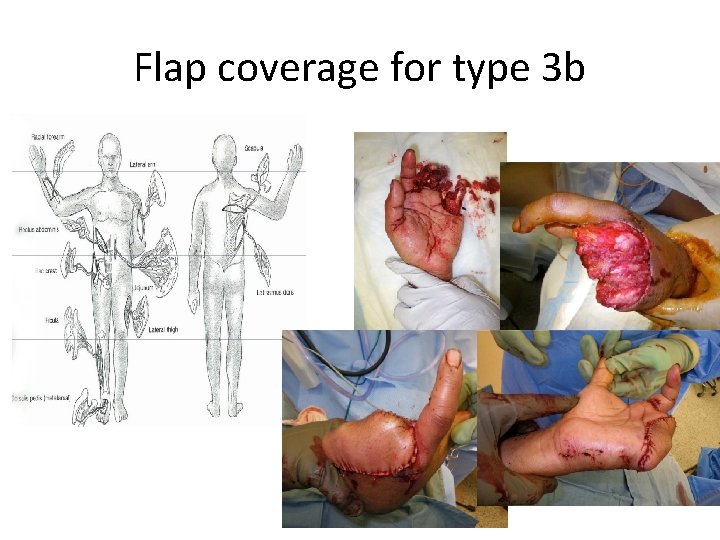
Flap coverage for type 3 b
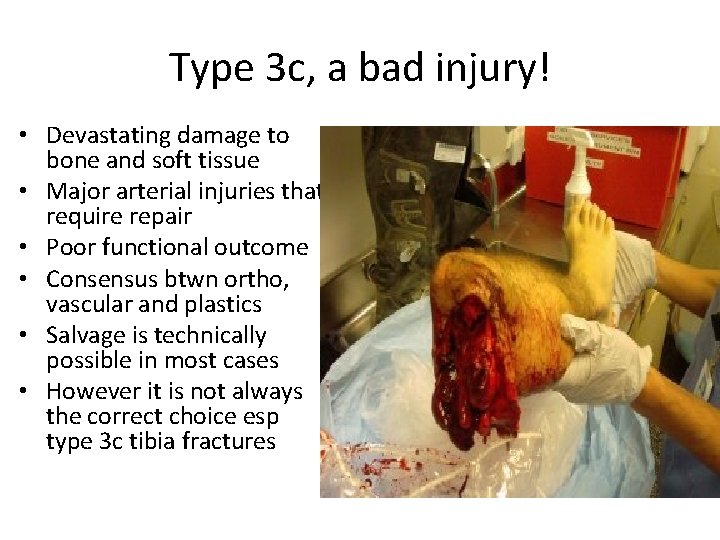
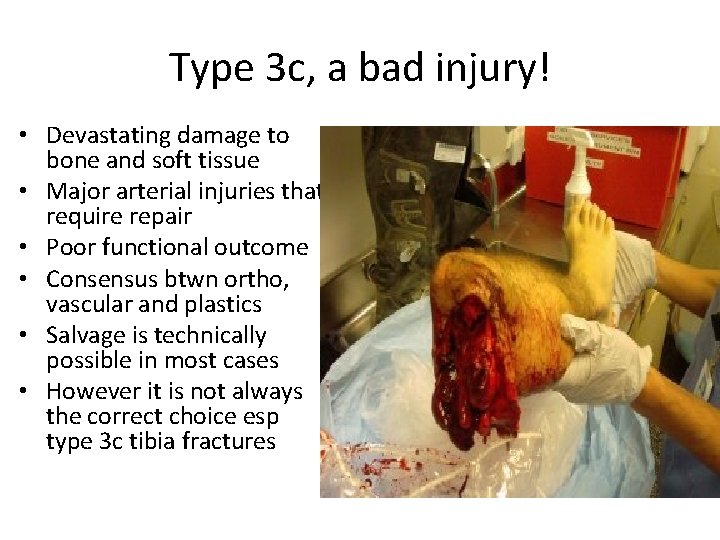
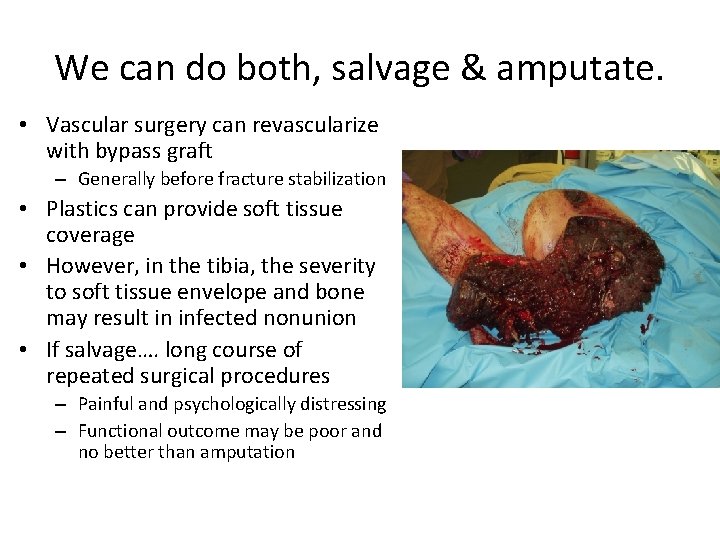
Type 3 c, a bad injury! • Devastating damage to bone and soft tissue • Major arterial injuries that require repair • Poor functional outcome • Consensus btwn ortho, vascular and plastics • Salvage is technically possible in most cases • However it is not always the correct choice esp type 3 c tibia fractures
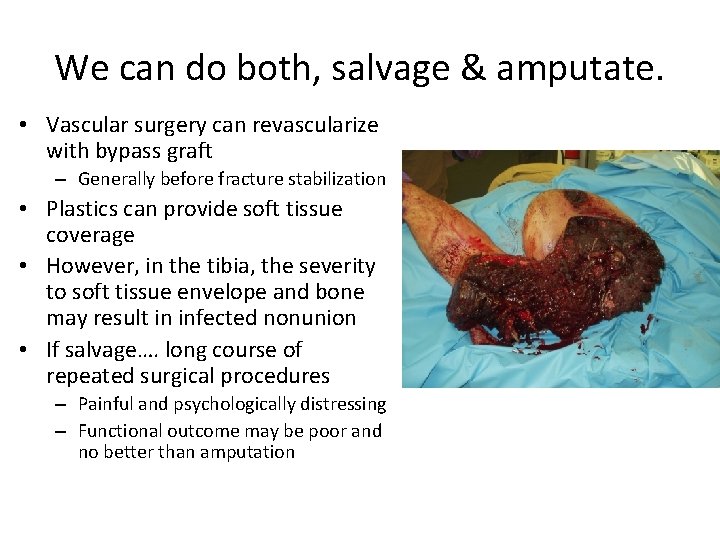
We can do both, salvage & amputate. • Vascular surgery can revascularize with bypass graft – Generally before fracture stabilization • Plastics can provide soft tissue coverage • However, in the tibia, the severity to soft tissue envelope and bone may result in infected nonunion • If salvage…. long course of repeated surgical procedures – Painful and psychologically distressing – Functional outcome may be poor and no better than amputation
How to decide, salvage or amputate? • Important factors in decision making: * – General condition of the patient (shock) – Warm ischemia time (>6 hours) – Age (>30 years) – Cut to crush ratio (blunt injuries has a large zone of crush) Howe HR Jr, Poole GV Jr, Hansen KJ, Clark T, Plonk GW, Koman LA, Pennell TC: Salvage of lower extremities following combined orthopedic and vascular trauma. A predictive salvage index. Am Surg. 1987 Apr; 53(4): 205 -8.
Gunshot injuries • Energy dissipated at impact = damage severity • High velocity rifles and close range shotguns – Worst, high energy of impact – Huge secondary cavitation – Secondary effects of shattered bone fragments • Bullets lodged in joints should be removed – avoid lead arthropathy and systemic lead poisoning
Low velocity GSW <2000 ft/sec • Low velocity handguns – Less severe, not treated like open fractures – Cavitation is not significant – Secondary missile effects are minimal – Bone fragments rarely stripped of soft tissue attachments and blood supply – Soft tissue injuries not severe and skin wounds are small
Low velocity GSW open fractures • Geisslar et al. * • Dickey et al. ** – No abx vs IV Ancef x 3 d • If neurovascular status – 67 low velocity GSW fxs normal, do local Treat open – Not requiring operative debridement fractures from low fixation • NO formal I&D needed – No difference in velocity GSW as • IV Abx infection rates closed fractures • Approach fx fixation as if closed **Dickey et al, J Ortho Trauma, 3; 6 -10, 1989 without Abx *Geisslar ett al, J Ortho Trauma, 4; 39 -41, 1990
Pitfalls and complications • Infection delayed union, nonunion, malunion and loss of function • Plan ahead to avoid delayed union and nonunion • Predict nonunion in severe injuries with bone loss – Bone grafting usually delayed 6 weeks when soft tissues have soundly healed – Autogenous bone grafting is usual strategy – Fibular transfer, free composite graft or distraction osteogenesis for complex defects – Recombinant human BMP in open tibia fracture reduces risk of delayed union
Advances… • BMPs – 40% decreased infection rate with BMP in type 3 open tibia fractures* • Antibiotic Laden Bone Graft** – Tobramycin-impregnated calcium sulfate pellets with demineralized bone matrix – Animal study: successful in preventing infection *BESTT Study Group, Govender S, Csimma C, Genant H, Valentin-Opran A. “Recombinant Human Bone Morphogenetic Protein-2 for Treatment of Open Tibial Fractures: A prospective, controlled, randomized study of four hundred and fifty patients. ” JBJS-A 2002. 84(12): 2123 -2134. **Beardmore AA, Brooks DE, Wenke JC, Thomas DB. “Effectiveness of local antibiotic delivery with an osteoinductive and osteoconductive bone-graft substitute. ” JBJS-A 2005. 87(1): 107 -112.
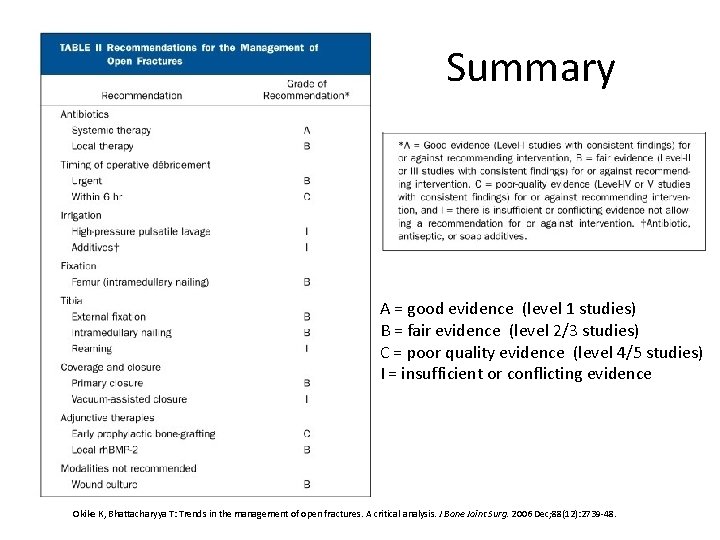
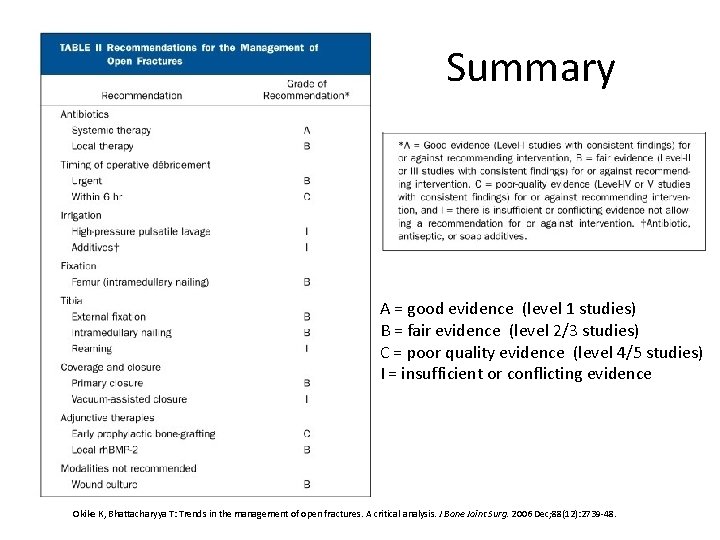
Summary A = good evidence (level 1 studies) B = fair evidence (level 2/3 studies) C = poor quality evidence (level 4/5 studies) I = insufficient or conflicting evidence Okike K, Bhattacharyya T: Trends in the management of open fractures. A critical analysis. J Bone Joint Surg. 2006 Dec; 88(12): 2739 -48.

Thank you
 Classification of open fractures
Classification of open fractures Antigentest åre
Antigentest åre Sukhpal ghuman
Sukhpal ghuman Duval algorithm
Duval algorithm Sarwan singh kundan singh
Sarwan singh kundan singh Daniel tibia
Daniel tibia Open fracture treatment
Open fracture treatment 영국 beis
영국 beis Irving olecranon fractures
Irving olecranon fractures Radial fracture glass definition
Radial fracture glass definition Activity 14-1 glass fracture patterns answer key
Activity 14-1 glass fracture patterns answer key Gustilo anderson classification antibiotics
Gustilo anderson classification antibiotics Fracture supracondylienne coude adulte
Fracture supracondylienne coude adulte Arc antérieur du bassin
Arc antérieur du bassin Chest tube landmarks
Chest tube landmarks Primary bone vs secondary bone
Primary bone vs secondary bone Panfacial fractures sequencing
Panfacial fractures sequencing Lisa cannada md
Lisa cannada md Canthatomy
Canthatomy Tubular shaft of a long bone
Tubular shaft of a long bone Ilioposas
Ilioposas Acetabular ossification
Acetabular ossification Types of glass fractures
Types of glass fractures Perkins timetable of fracture healing
Perkins timetable of fracture healing øpas
øpas Weber classification of ankle fractures
Weber classification of ankle fractures Off delay timer symbol
Off delay timer symbol Open hearts open hands
Open hearts open hands Sandeep singh jolly berlin
Sandeep singh jolly berlin Yatindra nath singh
Yatindra nath singh Singh song poem
Singh song poem Sexual harrasment prevention training
Sexual harrasment prevention training Dr ajit singh
Dr ajit singh Iqbal singh dhaliwal
Iqbal singh dhaliwal Linux operating system presentation
Linux operating system presentation Dr iqbal singh
Dr iqbal singh Navpreet singh iit kanpur
Navpreet singh iit kanpur Nimi singh
Nimi singh Basant kurre ias
Basant kurre ias Tanya singh husband
Tanya singh husband Guru gobind singh study circle books
Guru gobind singh study circle books Mannu singh vs umadat pandey
Mannu singh vs umadat pandey Muninder singh sambi
Muninder singh sambi Parkaranjot singh
Parkaranjot singh Parochialisation and universalisation
Parochialisation and universalisation Bro bakht singh birthday
Bro bakht singh birthday Kavita singh unc
Kavita singh unc Kavita singh uh
Kavita singh uh Sukhjit singh de anza
Sukhjit singh de anza Gurmeet singh manku
Gurmeet singh manku Daljeet singh banda
Daljeet singh banda Renal columns
Renal columns Dr nishi singh
Dr nishi singh Dr n k singh dhanbad
Dr n k singh dhanbad Raj singh ucr
Raj singh ucr Renural
Renural Garry singh iiris
Garry singh iiris Allama iqbal introduction
Allama iqbal introduction Manvinder singh jsa
Manvinder singh jsa Ca rajiv singh
Ca rajiv singh Janice singh
Janice singh Prasat muang singh
Prasat muang singh Nisha singh md
Nisha singh md Ram singh chauhan age
Ram singh chauhan age Chadah committee
Chadah committee Kartar singh committee recommendations
Kartar singh committee recommendations Gursharan singh tatla
Gursharan singh tatla Sultana daughter of boota singh
Sultana daughter of boota singh Warm chain in pediatrics
Warm chain in pediatrics Salil singh
Salil singh Devendra singh psychologist
Devendra singh psychologist Abhishek singh parihar
Abhishek singh parihar Summerpal singh gill
Summerpal singh gill Paroxysmal hemicrania
Paroxysmal hemicrania Lagrange polynomials
Lagrange polynomials Dr. vasu singh
Dr. vasu singh