Patella Fractures Extensor Mechanism Injuries Lisa K Cannada













- Slides: 67
Patella Fractures & Extensor Mechanism Injuries Lisa K. Cannada, MD Revised: October 2008; May 2011
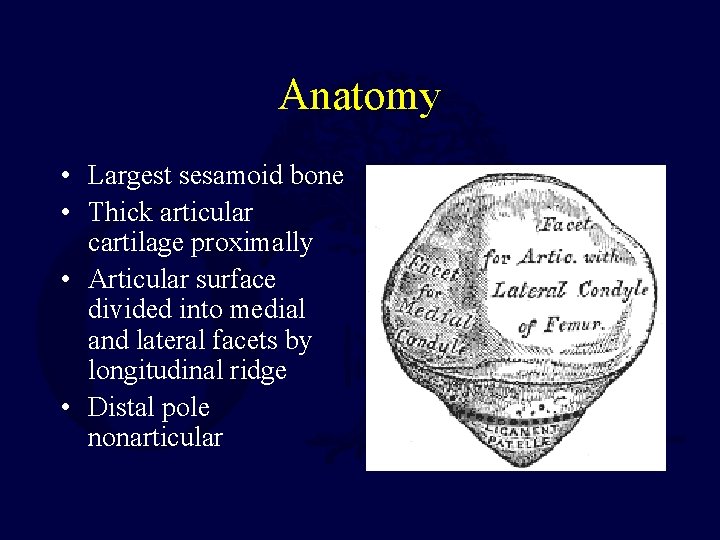
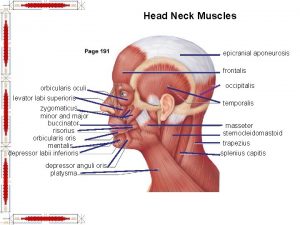
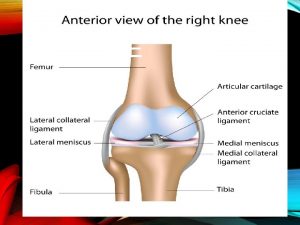
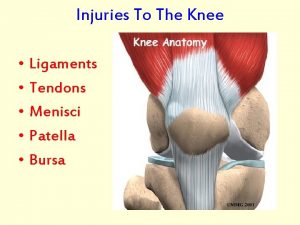
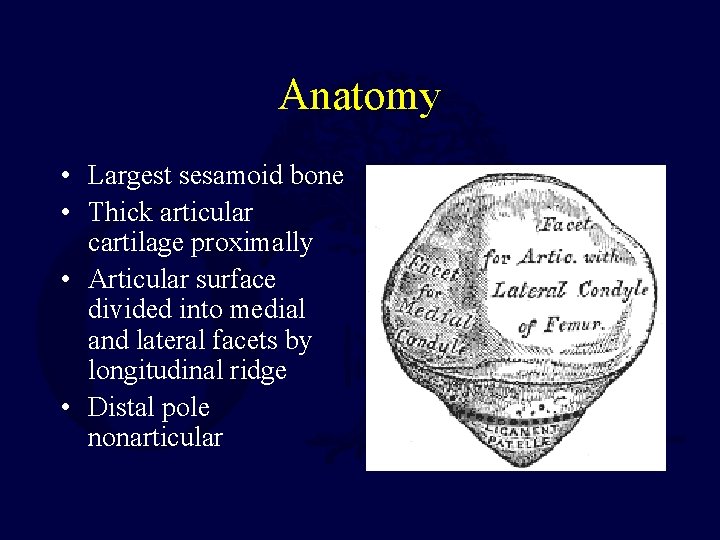
Anatomy • Largest sesamoid bone • Thick articular cartilage proximally • Articular surface divided into medial and lateral facets by longitudinal ridge • Distal pole nonarticular
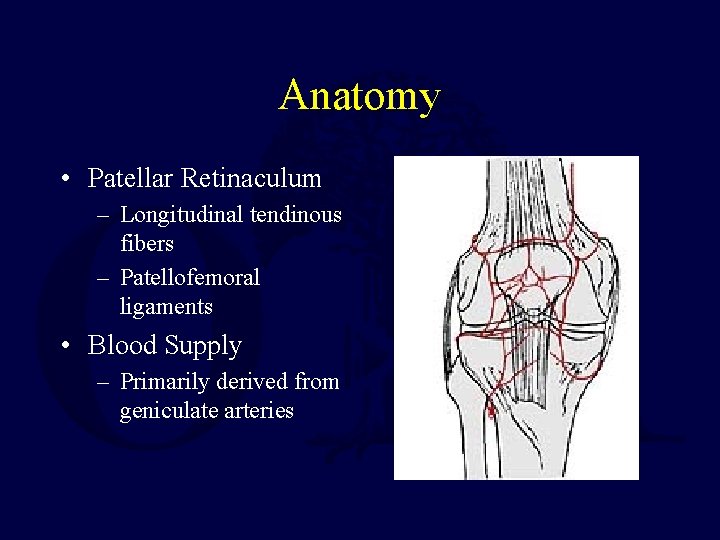
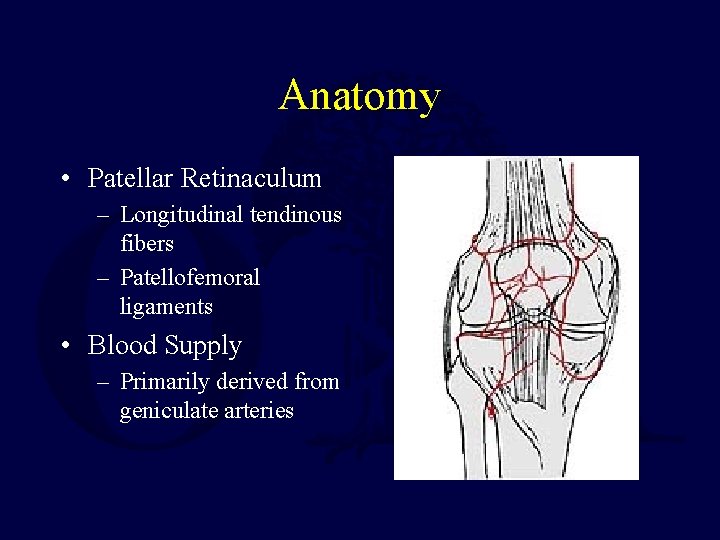
Anatomy • Patellar Retinaculum – Longitudinal tendinous fibers – Patellofemoral ligaments • Blood Supply – Primarily derived from geniculate arteries
Biomechanics • The patella undergoes approximately 7 cm of translation from full flexion to extension • Only 13 -38% of the patellar surface is in contact with the femur throughout its range of motion
Biomechanics • The patella increases the moment arm about the knee – Contributes up to 30% improvement in lever arm • Patella withstands compressive forces greater than 7 X body weight with squatting
Biomechanics • 2 X Torque: – Extend final 15° – Than to extend from a fully flexed position to 15 degrees of flexion
Physical Examination • Pain, swelling, contusions, lacerations and/or abrasions at the site of injury – Can determine timing of operative intervention • Palpable defect • Assessment of ability to extend the knee – Cannot perform a straight leg raise with no extensor lag
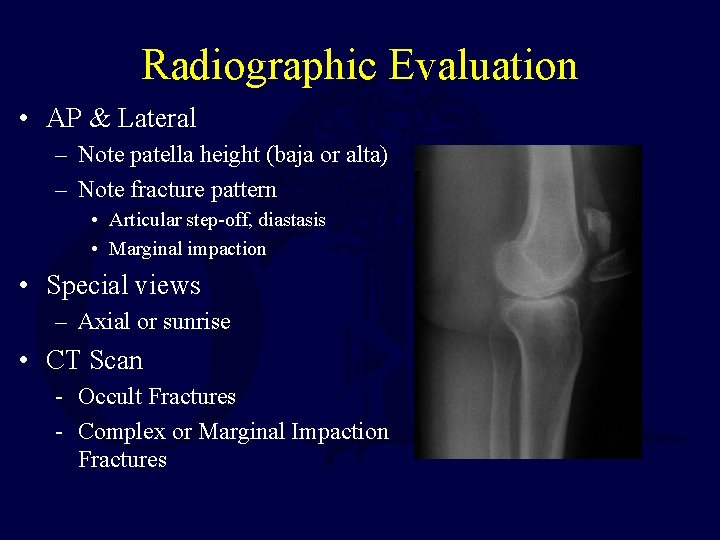
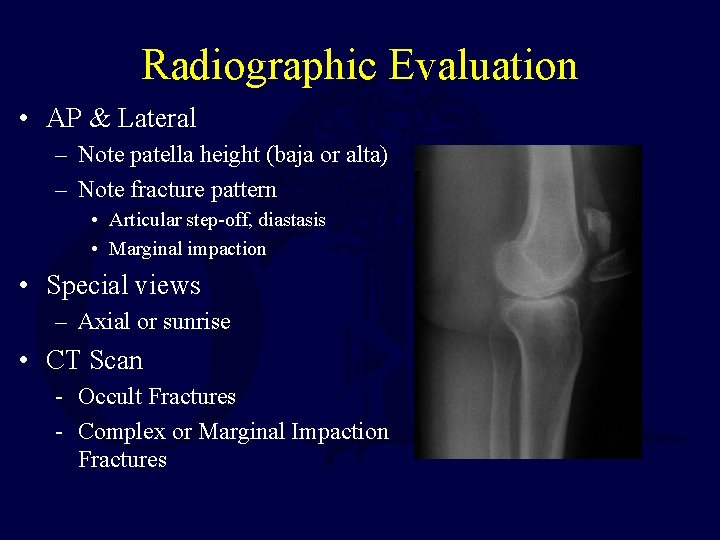
Radiographic Evaluation • AP & Lateral – Note patella height (baja or alta) – Note fracture pattern • Articular step-off, diastasis • Marginal impaction • Special views – Axial or sunrise • CT Scan - Occult Fractures - Complex or Marginal Impaction Fractures
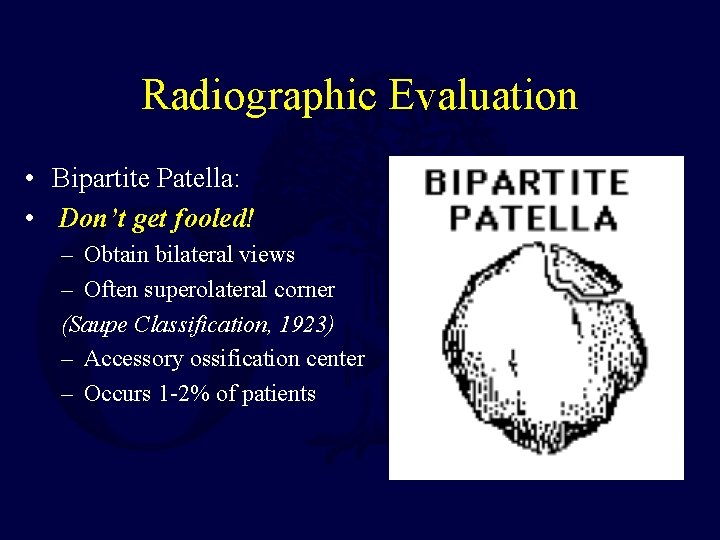
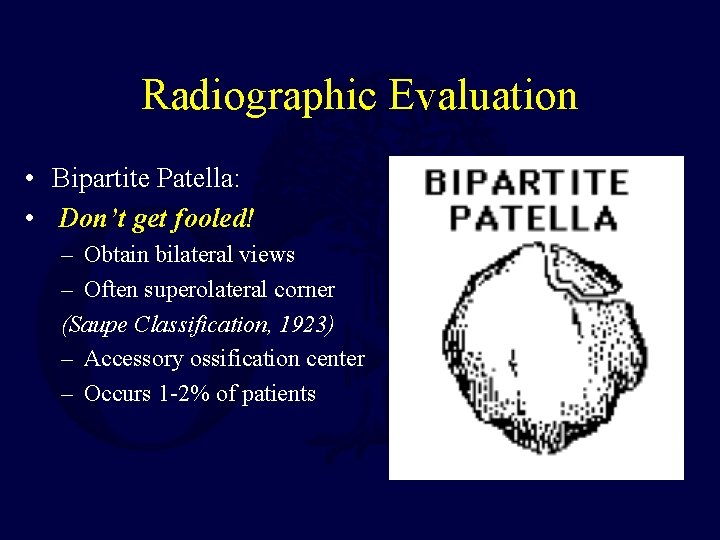
Radiographic Evaluation • Bipartite Patella: • Don’t get fooled! – Obtain bilateral views – Often superolateral corner (Saupe Classification, 1923) – Accessory ossification center – Occurs 1 -2% of patients
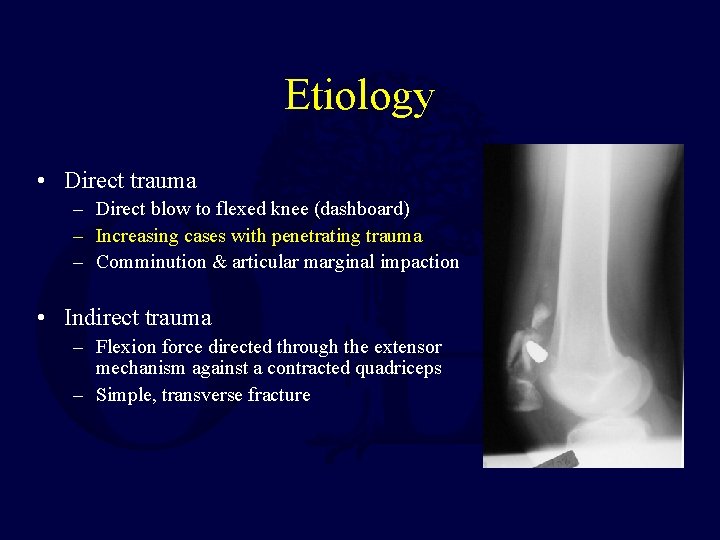
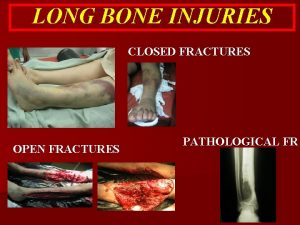
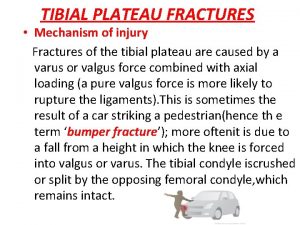
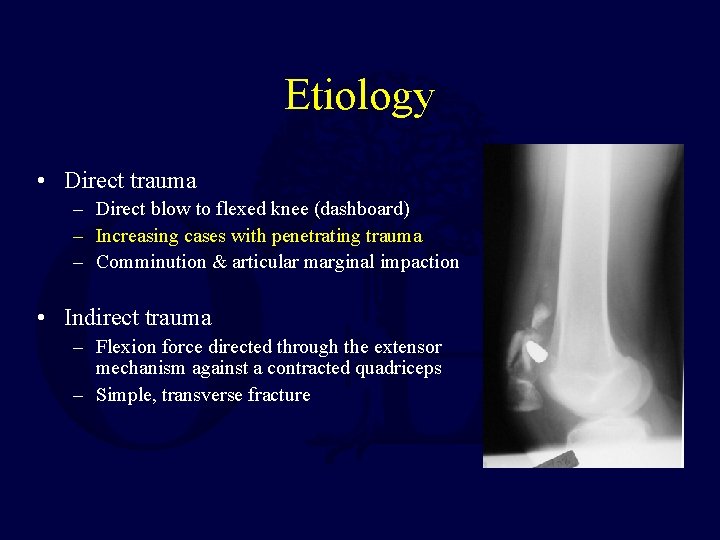
Etiology • Direct trauma – Direct blow to flexed knee (dashboard) – Increasing cases with penetrating trauma – Comminution & articular marginal impaction • Indirect trauma – Flexion force directed through the extensor mechanism against a contracted quadriceps – Simple, transverse fracture
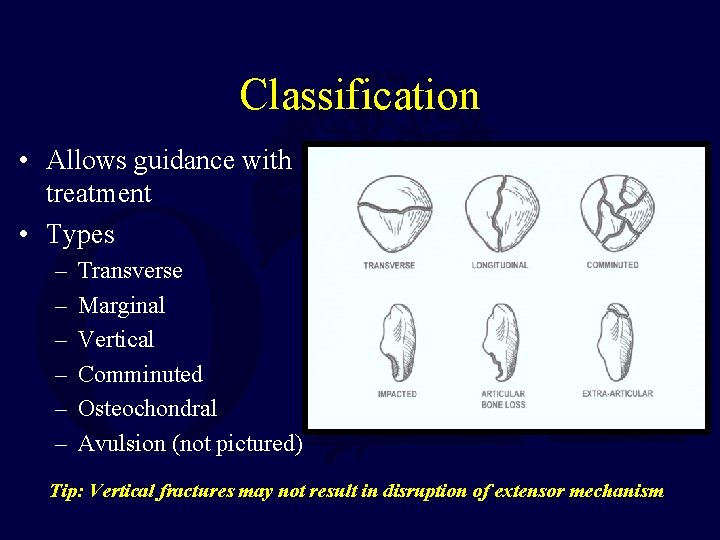
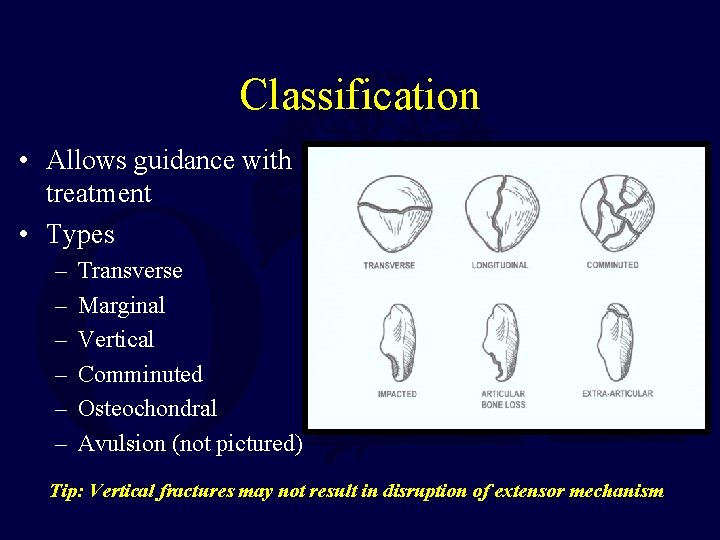
Classification • Allows guidance with treatment • Types – – – Transverse Marginal Vertical Comminuted Osteochondral Avulsion (not pictured) Tip: Vertical fractures may not result in disruption of extensor mechanism
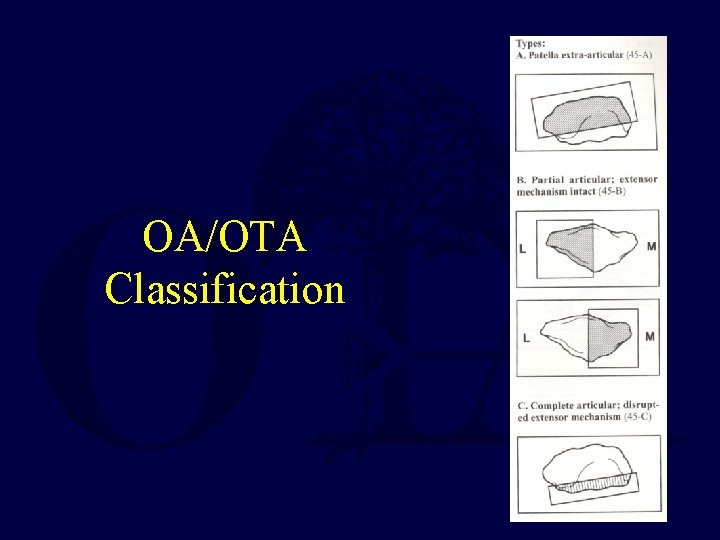
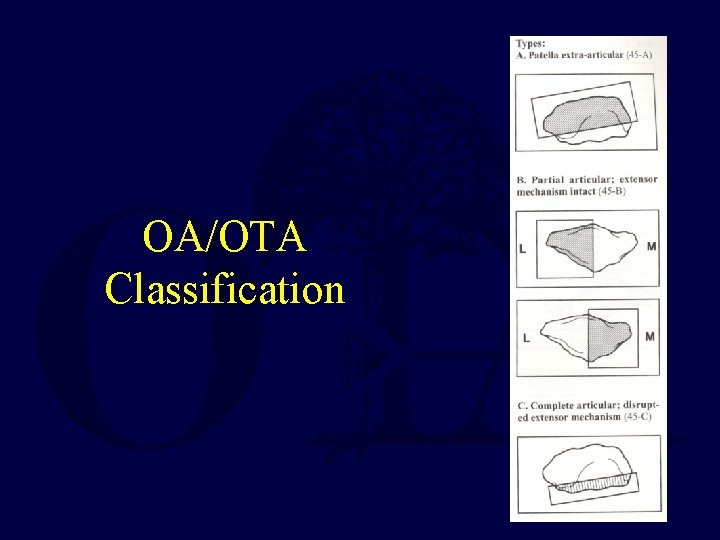
OA/OTA Classification
Nonoperative Treatment • Indicated for minimally or nondisplaced fractures – < 2 mm of articular step-off & < 3 mm of diastasis with an intact extensor mechanism (extensor retinaculum) – If difficulty assessing, consider intra-articular injection of local anesthetic to better assess ability to extend • Consider for minimally displaced fractures in low demand patients (evaluate comorbidities & function) • Patients with a extensive medical comorbidities

Nonoperative Treatment • Long leg cylinder cast for 4 -6 weeks – May consider a knee immobilizer or hinged knee brace for the elderly/low demand • Immediate weight-bearing as tolerated • Rehabilitation includes range of motion exercises with gradual quadriceps strengthening • Protect eccentric contraction 3 months

Operative Treatment • Goals – Preserve extensor function – Restore articular congruency • Preoperative Setup – Tourniquet (debatable) • Prior to inflation, gently flex the knee • Approach – Longitudinal midline incision recommended – Transverse approach alternative (dotted lines) – potentially higher risk wound problems, can limit initiation of ROM – Consider future surgeries!
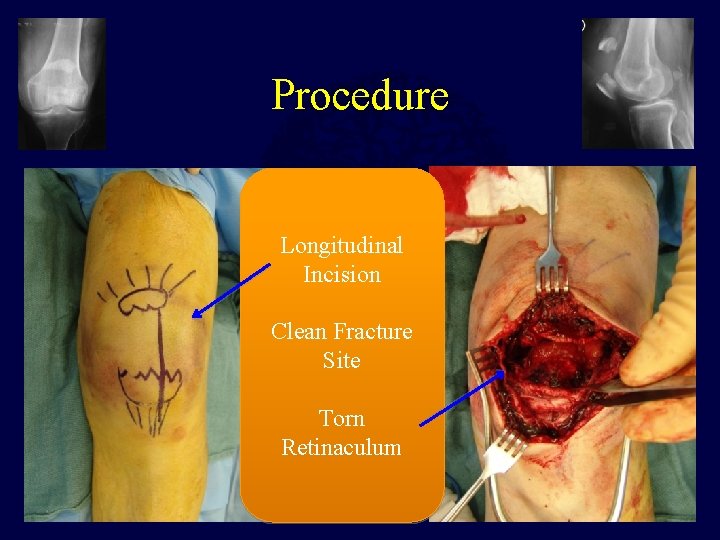
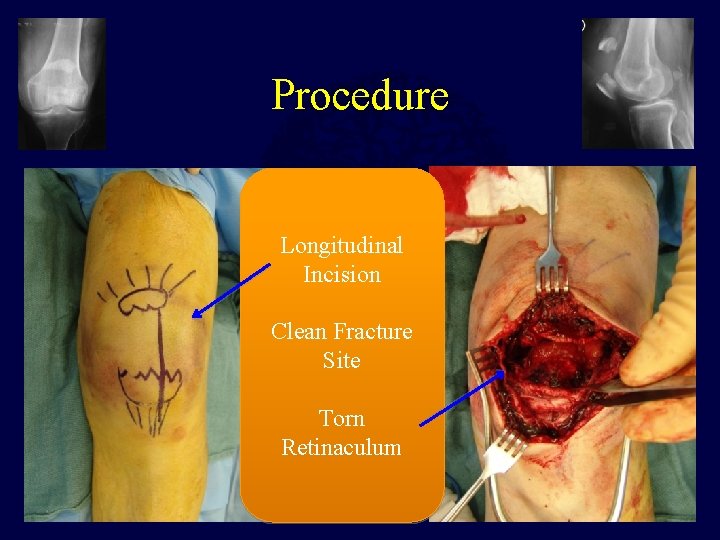
Procedure Longitudinal Incision Clean Fracture Site Torn Retinaculum
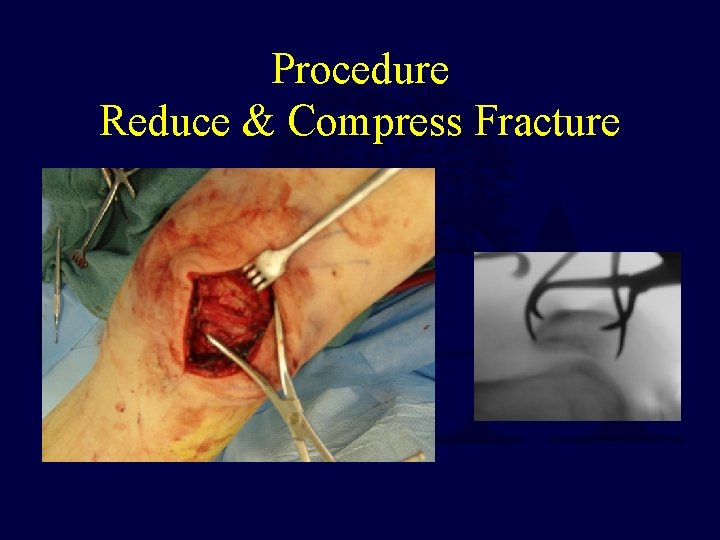
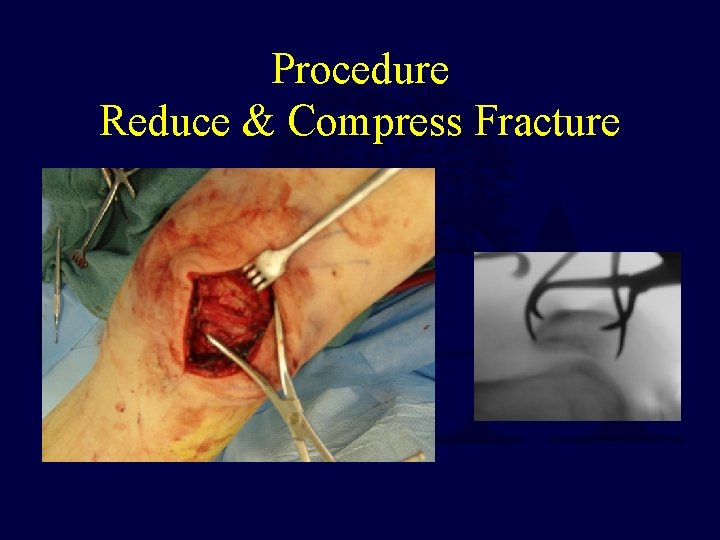
Procedure Reduce & Compress Fracture

Operative Techniques • K-wires w/ tension band wiring (TBW) • Lag-screw fixation • Cannulated lag-screw with TBW (tension band screw – TBS) • Partial patellectomy • Total Patellectomy
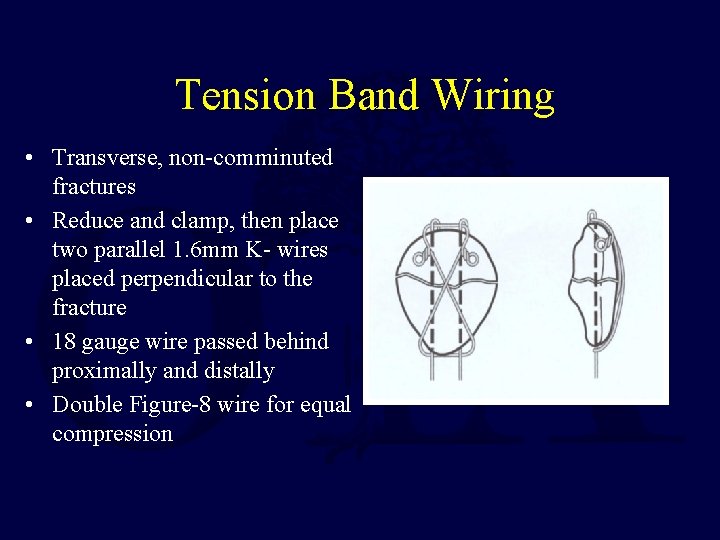
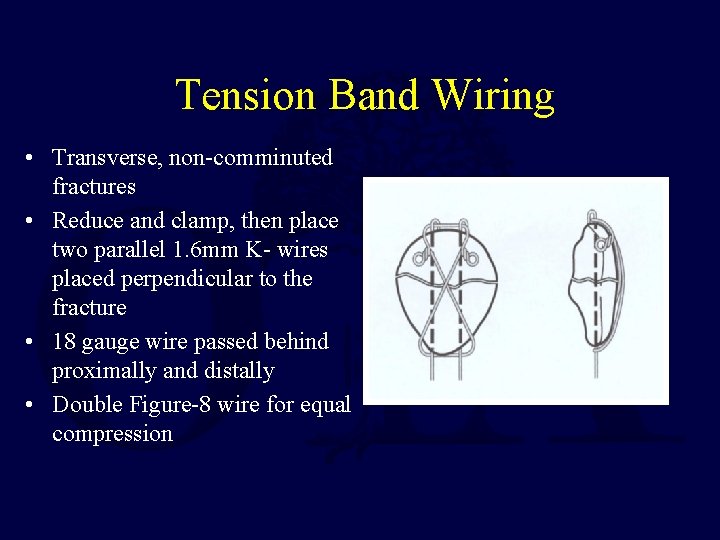
Tension Band Wiring • Transverse, non-comminuted fractures • Reduce and clamp, then place two parallel 1. 6 mm K- wires placed perpendicular to the fracture • 18 gauge wire passed behind proximally and distally • Double Figure-8 wire for equal compression
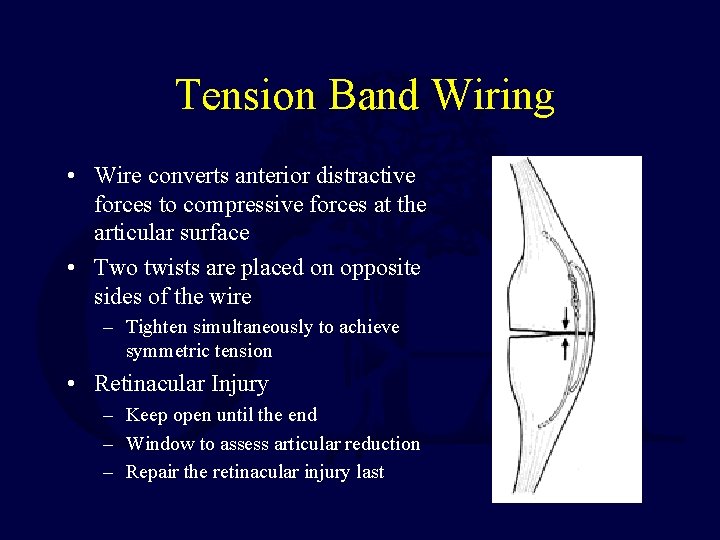
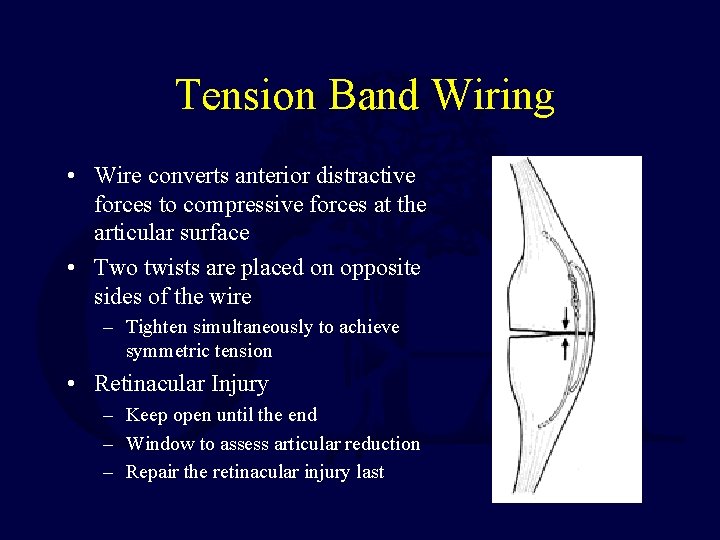
Tension Band Wiring • Wire converts anterior distractive forces to compressive forces at the articular surface • Two twists are placed on opposite sides of the wire – Tighten simultaneously to achieve symmetric tension • Retinacular Injury – Keep open until the end – Window to assess articular reduction – Repair the retinacular injury last
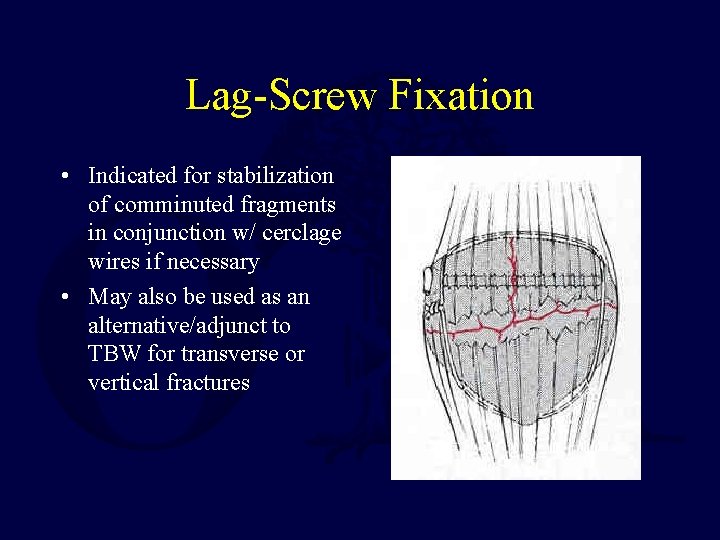
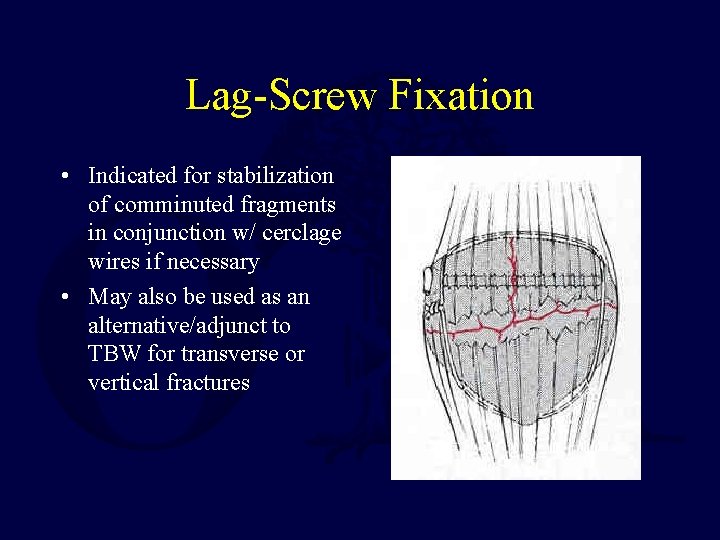
Lag-Screw Fixation • Indicated for stabilization of comminuted fragments in conjunction w/ cerclage wires if necessary • May also be used as an alternative/adjunct to TBW for transverse or vertical fractures
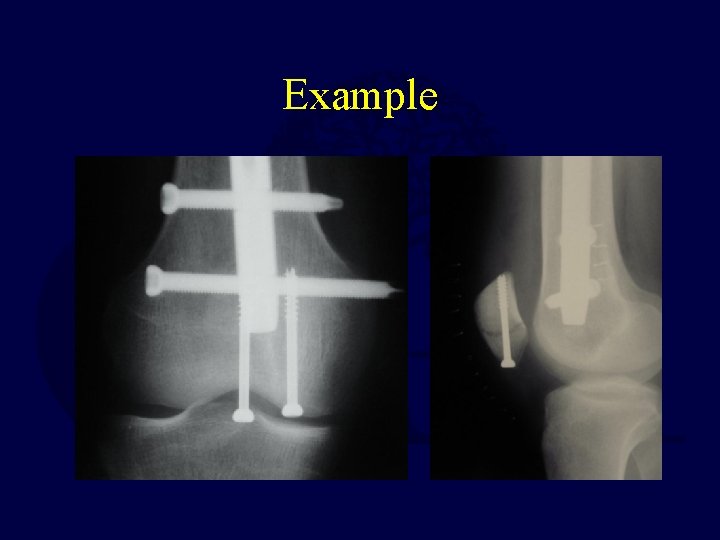
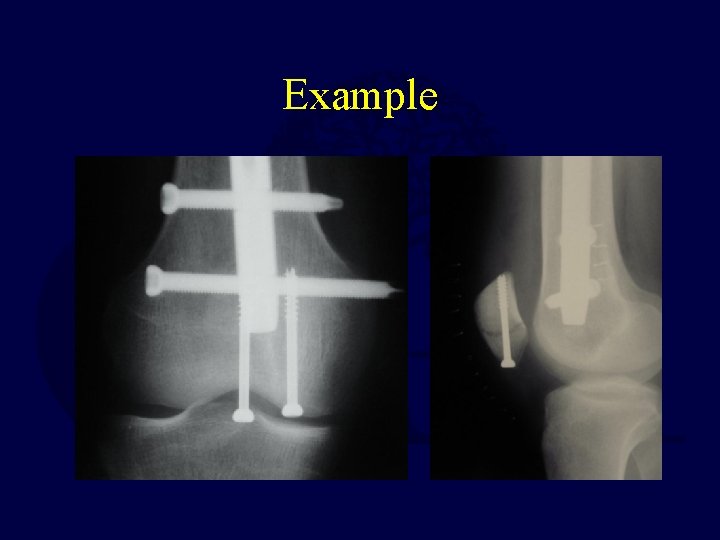
Example
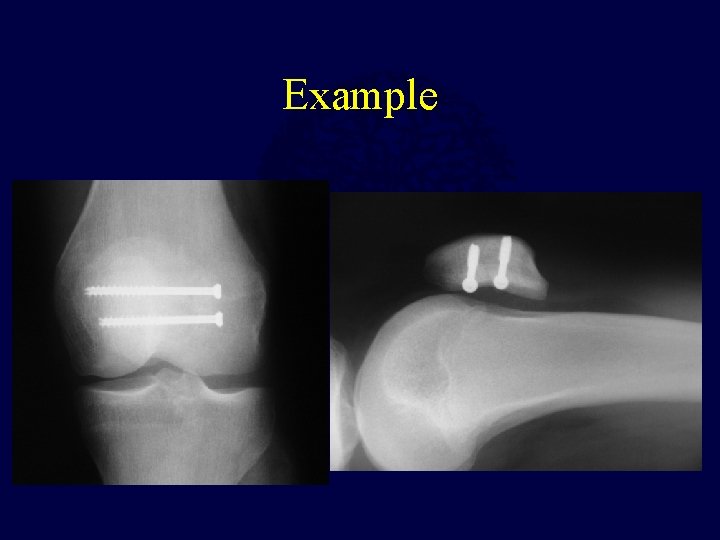
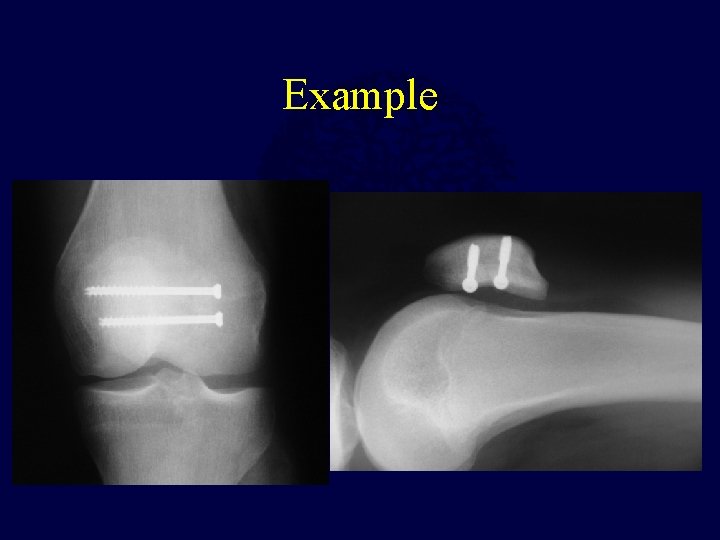
Example
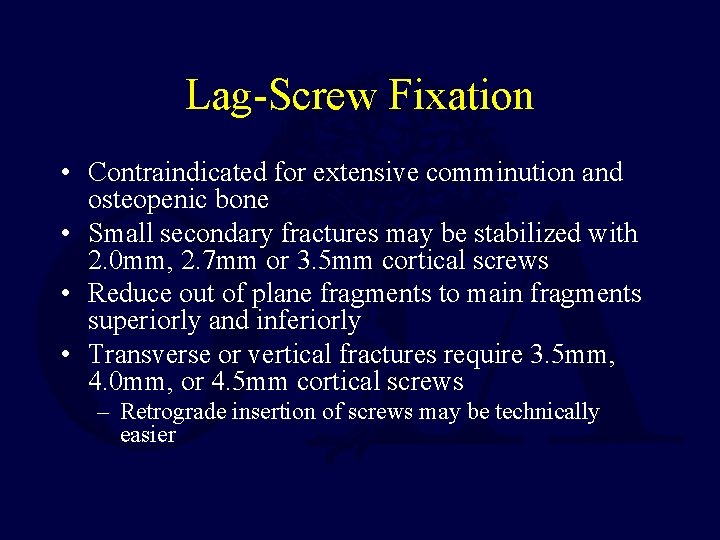
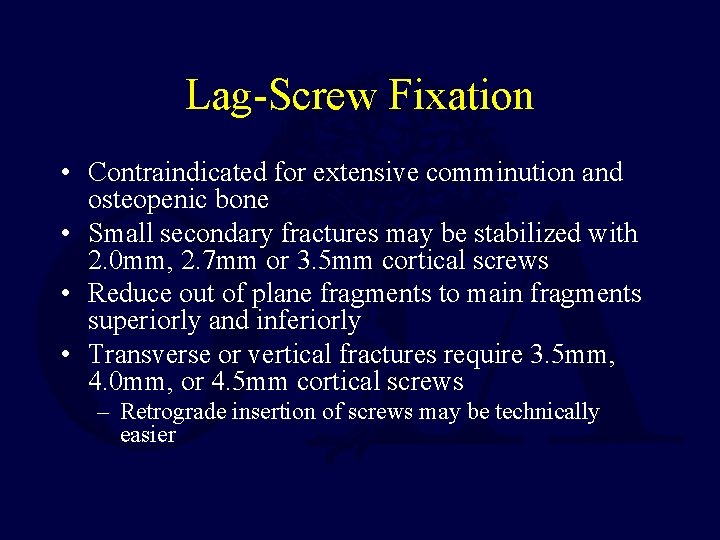
Lag-Screw Fixation • Contraindicated for extensive comminution and osteopenic bone • Small secondary fractures may be stabilized with 2. 0 mm, 2. 7 mm or 3. 5 mm cortical screws • Reduce out of plane fragments to main fragments superiorly and inferiorly • Transverse or vertical fractures require 3. 5 mm, 4. 0 mm, or 4. 5 mm cortical screws – Retrograde insertion of screws may be technically easier
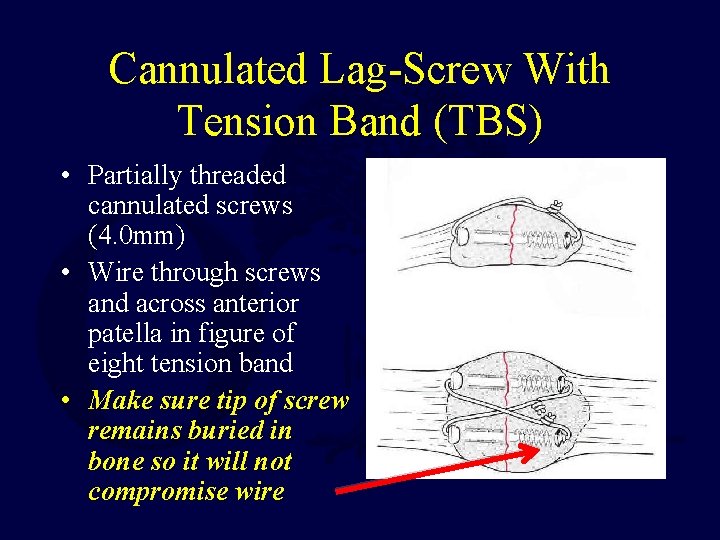
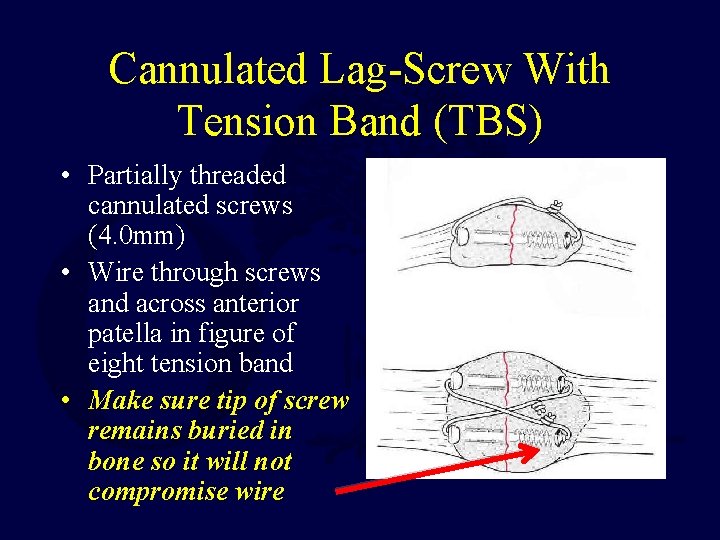
Cannulated Lag-Screw With Tension Band (TBS) • Partially threaded cannulated screws (4. 0 mm) • Wire through screws and across anterior patella in figure of eight tension band • Make sure tip of screw remains buried in bone so it will not compromise wire

Cannulated Lag-Screw With Tension Band • More stable construct – Screws and tension band wire combination eliminates both possible separation seen at the fracture site with K wire/TBW and screw failure due to excessive three point bending
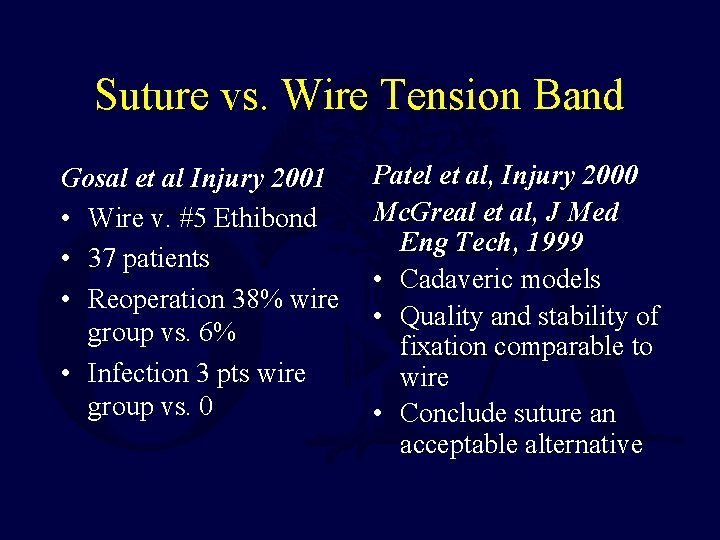
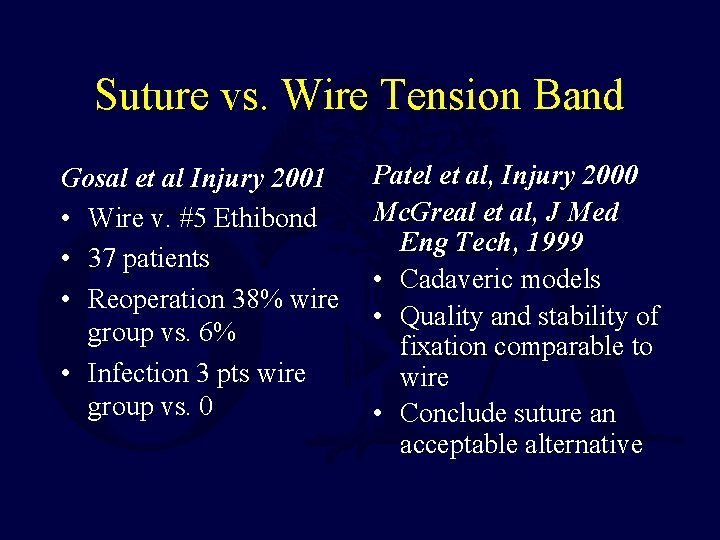
Suture vs. Wire Tension Band Gosal et al Injury 2001 • Wire v. #5 Ethibond • 37 patients • Reoperation 38% wire group vs. 6% • Infection 3 pts wire group vs. 0 Patel et al, Injury 2000 Mc. Greal et al, J Med Eng Tech, 1999 • Cadaveric models • Quality and stability of fixation comparable to wire • Conclude suture an acceptable alternative
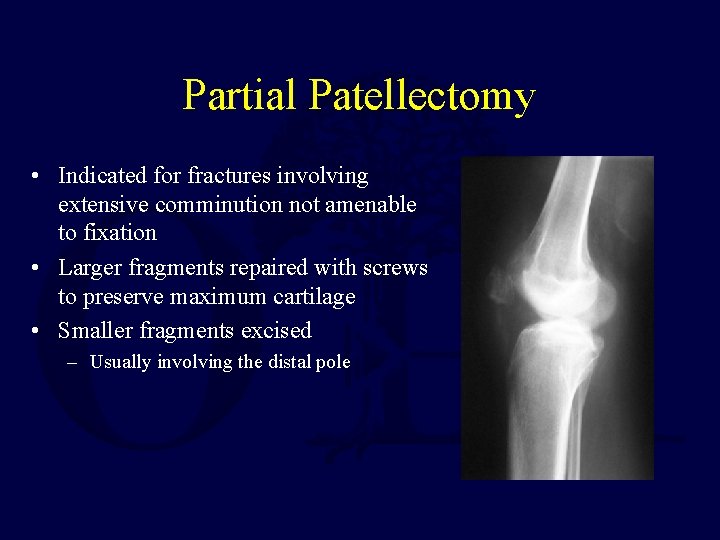
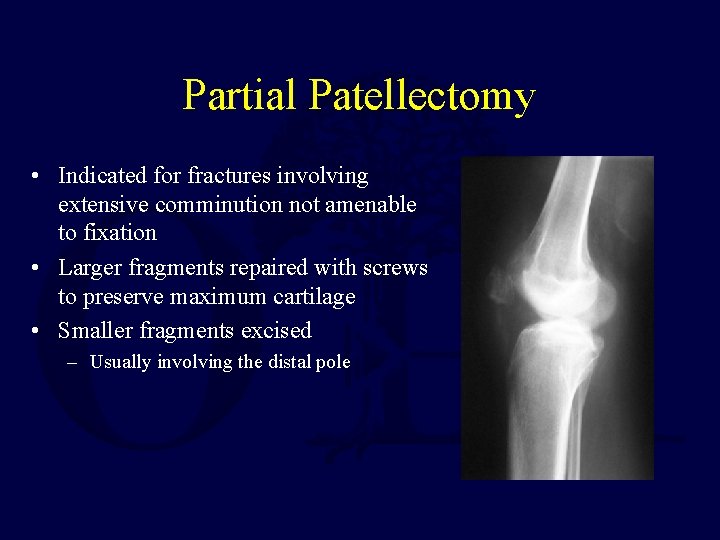
Partial Patellectomy • Indicated for fractures involving extensive comminution not amenable to fixation • Larger fragments repaired with screws to preserve maximum cartilage • Smaller fragments excised – Usually involving the distal pole

Partial Patellectomy • Tendon is attached to fragment with nonabsorbable suture passed through drill holes in the fragment – Drill holes should be near the articular surface to prevent tilting of the patella • Load sharing wire passed through drill holes in the tibial tubercle and patella may be used to protect the repair and facilitate early range of motion

Total Patellectomy • Indicated for displaced, comminuted fractures not amenable to reconstruction • Bone fragments sharply dissected • Defect may be repaired through a variety of techniques • Usually results in extensor lag (30°) and loss of strength (30%) – H Kaufer, JBJS
Postoperative Management • Immobilization with knee brace, WBAT in extension • Early range of motion – Based on intraoperative assessment of repair & bone quality – Active flexion with passive extension • Quadriceps strengthening – Begin when there is radiographic evidence of healing, usually around 6 weeks • Modify depending upon fracture, osteoporosis, comorbidities, tenuous fixation and/or wounds at risk

Complications • Knee Stiffness – Most common complication • Infection – Rare, depends on soft tissue compromise • Loss of Fixation – Hardware failure in up to 20% of cases • Osteoarthritis – May result from articular damage or incongruity • Nonunion < 1% with surgical repair • Painful hardware – Removal required in approximately 15%
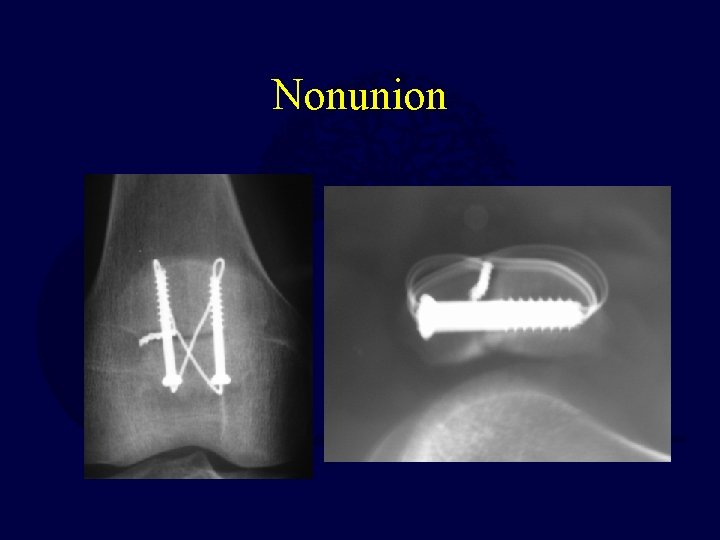
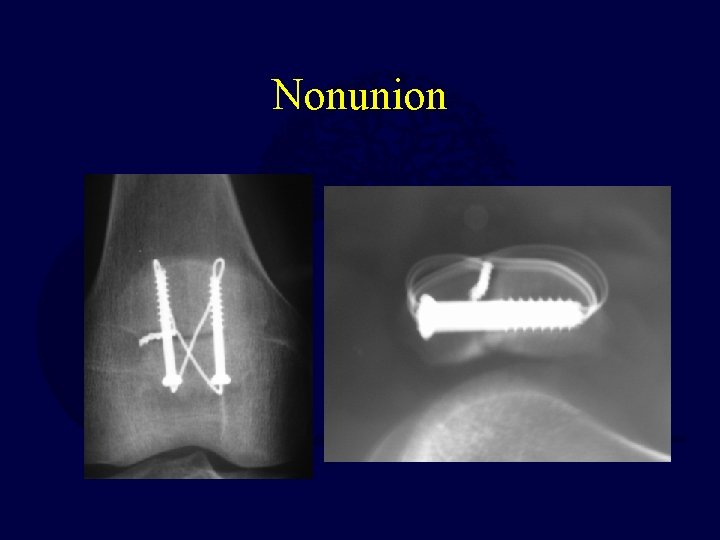
Nonunion
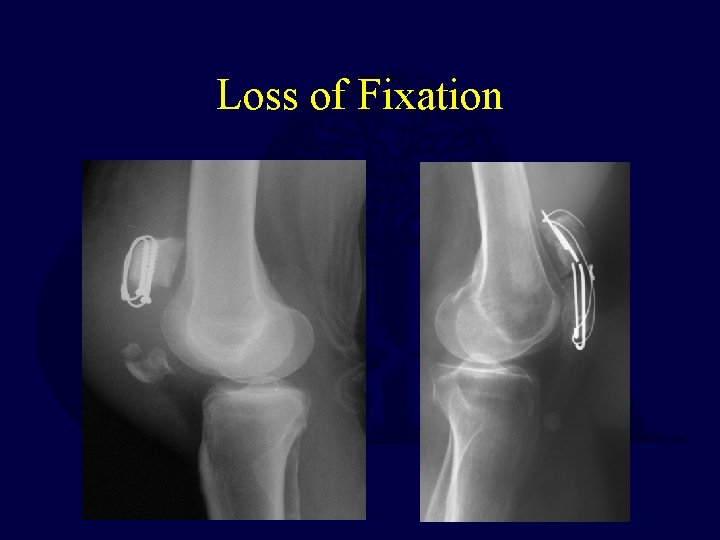
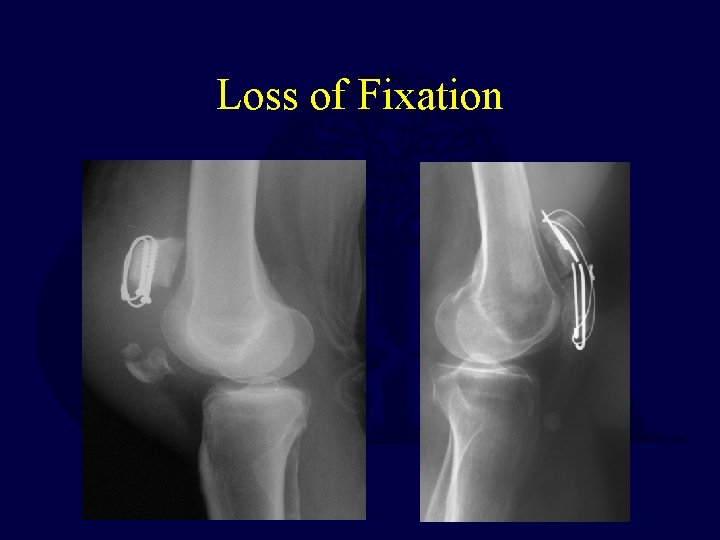
Loss of Fixation
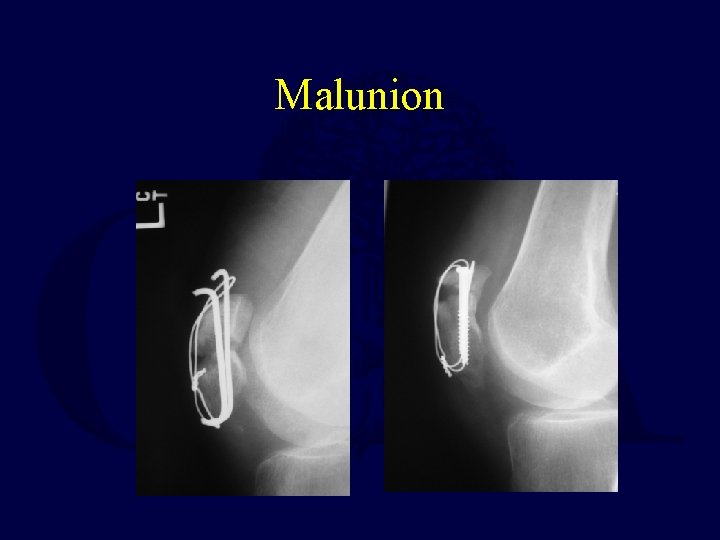
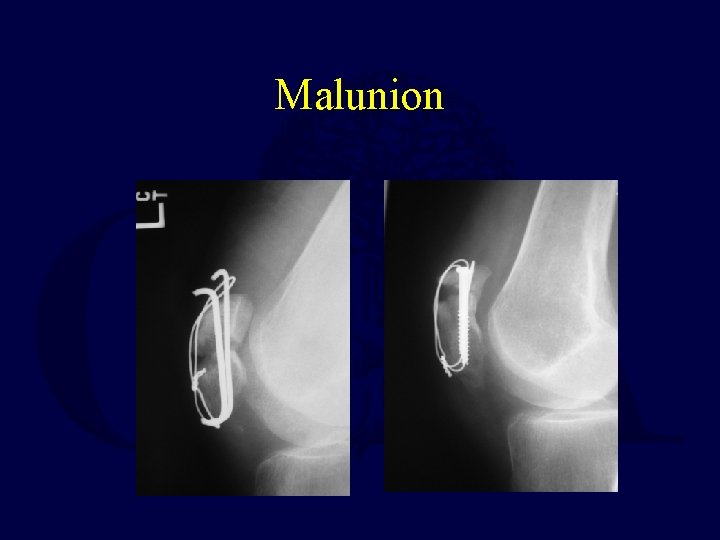
Malunion
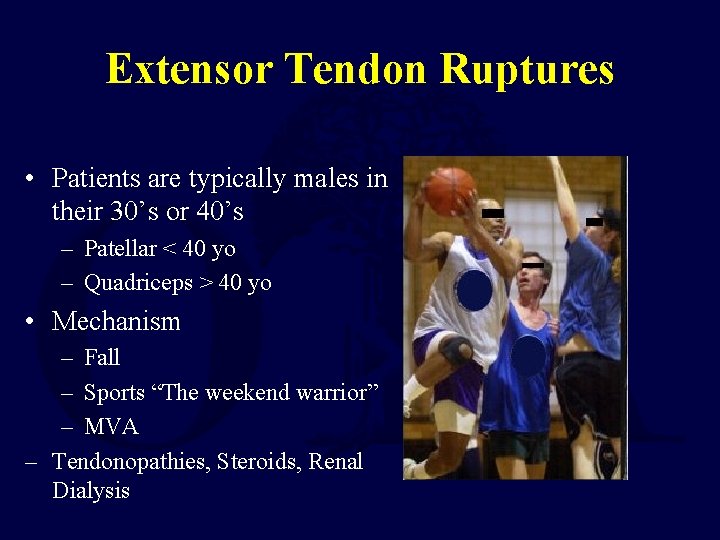
Extensor Tendon Ruptures • Patients are typically males in their 30’s or 40’s – Patellar < 40 yo – Quadriceps > 40 yo • Mechanism – Fall – Sports “The weekend warrior” – MVA – Tendonopathies, Steroids, Renal Dialysis
Quadriceps Tendon Rupture • Typically occurs in patients > 40 years old • Usually 0 -2 cm above the superior pole • Level often associated with age – Rupture occurs at the bone-tendon junction in majority of patients > 40 years old – Rupture occurs at midsubstance in majority of patients < 40 years old
Quadriceps Tendon Ruptures • Risk Factors – – – Chronic tendonitis Anabolic steroid use Local steroid injection Inflammatory arthropathy Chronic renal failure Systemic disease

History • Sensation of a sudden pop while stressing the extensor mechanism (eccentric load) • Pain at the site of injury • Inability to extend the knee • Difficulty weight-bearing

Physical Exam • Effusion • Tenderness at the upper pole • Palpable defect above superior pole • Loss of extension • With partial tears, extension will be intact
Quadriceps Tendon Rupture Radiographic Evaluation • X-ray- AP, Lateral, and Tangential (Sunrise, Merchant) – Distal displacement of the patella (patella baja) • MRI – Useful when diagnosis is unclear Treatment • Nonoperative – Partial tears and strains • Operative – For complete ruptures
Operative Treatment • Reapproximation of tendon to bone using nonabsorbable sutures with tears at the muscle-tendon junction – Locking stitch (Bunnel, Krakow) with No. 5 ethibond passed through vertical bone tunnels – Repair tendon close to articular surface to avoid abnormal patellar tilting
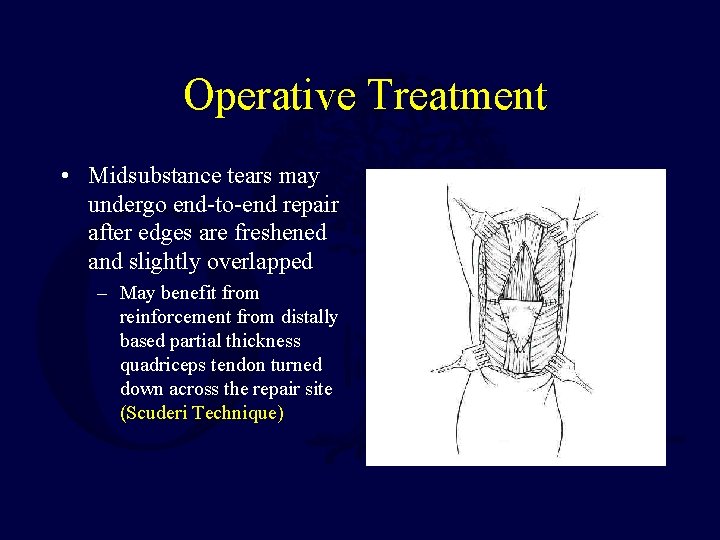
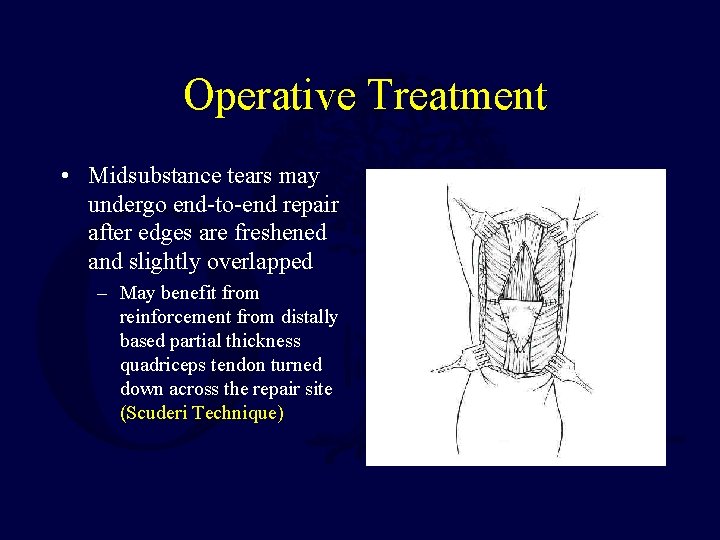
Operative Treatment • Midsubstance tears may undergo end-to-end repair after edges are freshened and slightly overlapped – May benefit from reinforcement from distally based partial thickness quadriceps tendon turned down across the repair site (Scuderi Technique)
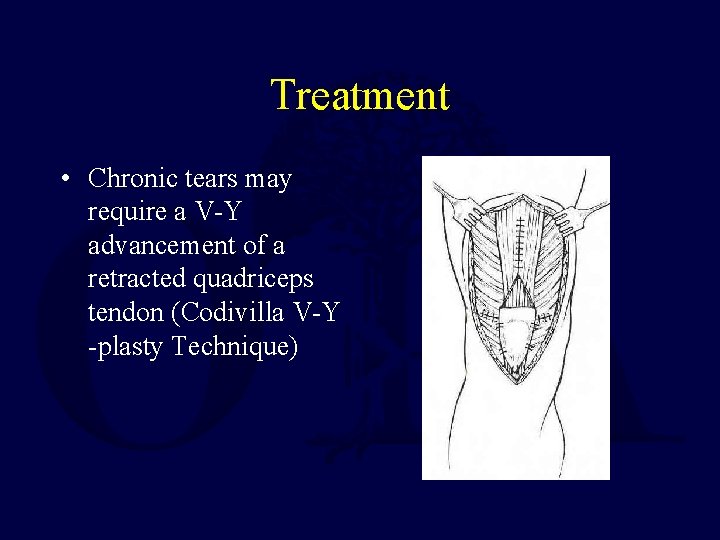
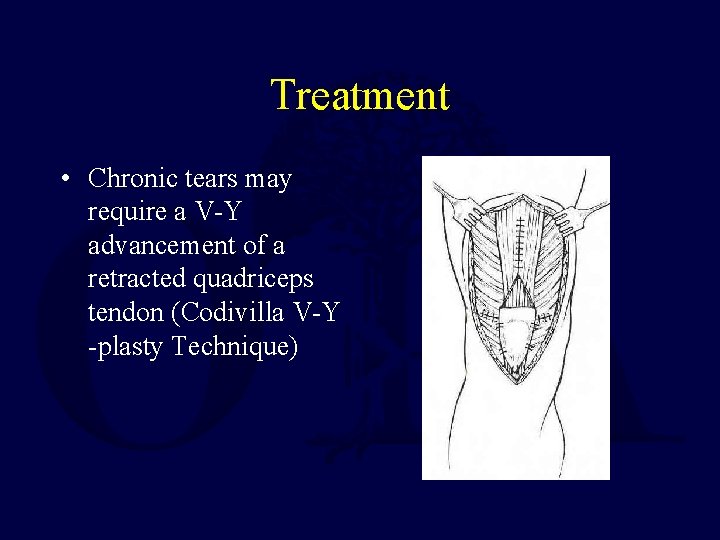
Treatment • Chronic tears may require a V-Y advancement of a retracted quadriceps tendon (Codivilla V-Y -plasty Technique)
Postoperative Management • Knee immobilizer, Hinged Knee Brace, or cylinder cast for 5 -6 weeks • Immediate weight-bearing as tolerated • At 2 -3 weeks, hinged knee brace starting with 45 degrees active range of motion with 10 -15 degrees of progression each week
Complications • Rerupture • Persistent quadriceps atrophy/weakness • Loss of motion • Infection
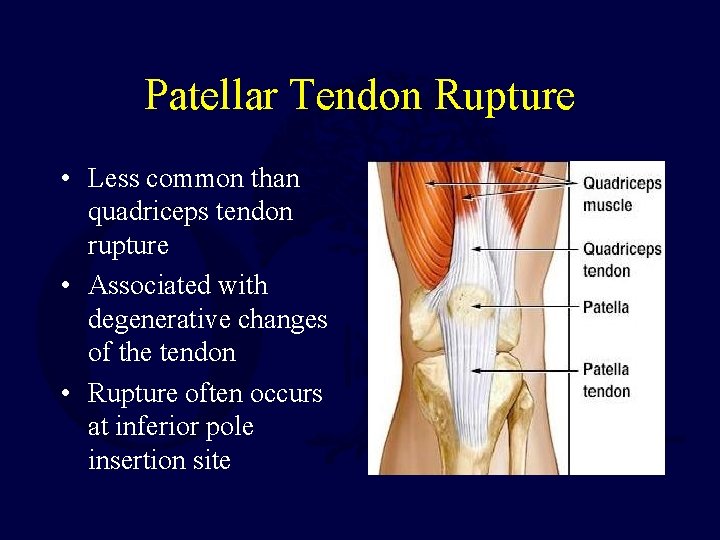
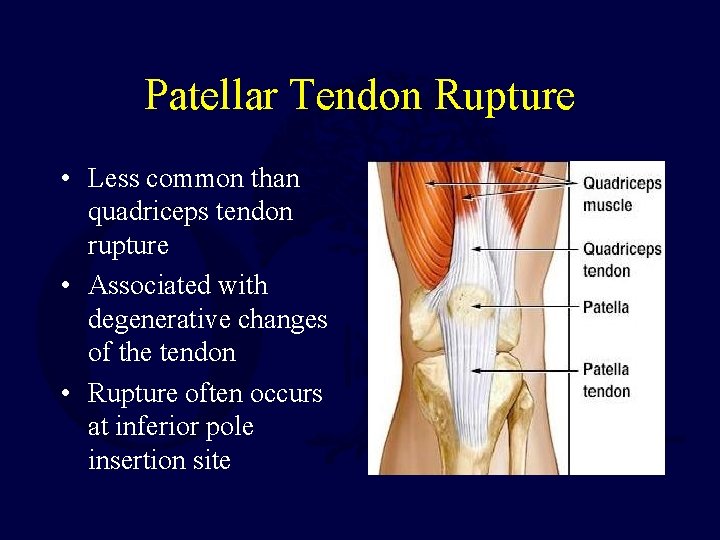
Patellar Tendon Rupture • Less common than quadriceps tendon rupture • Associated with degenerative changes of the tendon • Rupture often occurs at inferior pole insertion site
Patellar Tendon Rupture • Risk Factors – Rheumatoid arthritis – Systemic Lupus Erythematosus – Diabetes – Chronic Renal Failure – Systemic Corticosteroid Therapy – Local Steroid Injection – Chronic tendonitis
Anatomy • Patellar tendon – Averages 4 mm thick but widens to 5 -6 mm at the tibial tubercle insertion – Merges with the medial and lateral retinaculum – 90% type I collagen
Blood Supply • Fat pad vessels supply posterior aspect of tendon via inferior medial and lateral geniculate arteries • Retinacular vessels supply anterior portion of tendon via the inferior medial geniculate and recurrent tibial arteries • Proximal and distal insertion areas are relatively avascular and subsequently are a common site of rupture
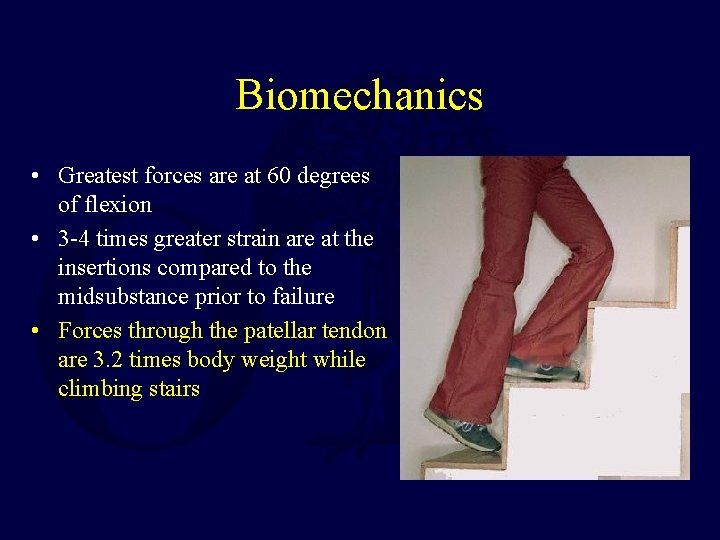
Biomechanics • Greatest forces are at 60 degrees of flexion • 3 -4 times greater strain are at the insertions compared to the midsubstance prior to failure • Forces through the patellar tendon are 3. 2 times body weight while climbing stairs
History • Often a report of forceful quadriceps contraction against a flexed knee • May experience and audible “pop” • Inability to weightbear or extend the knee
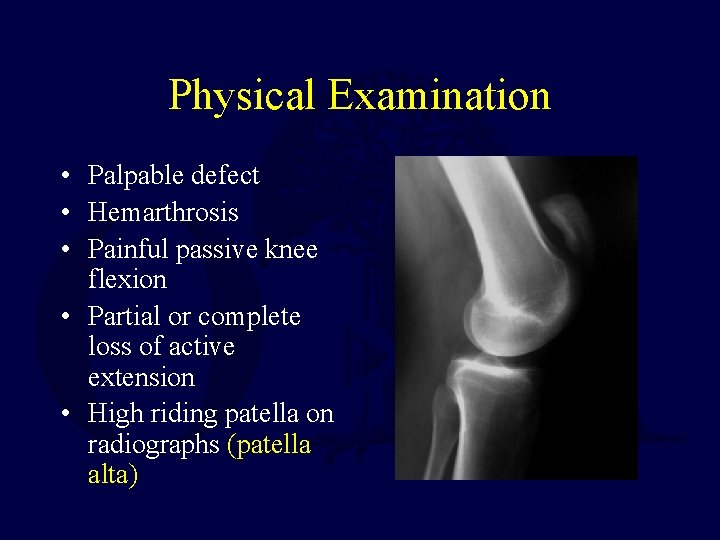
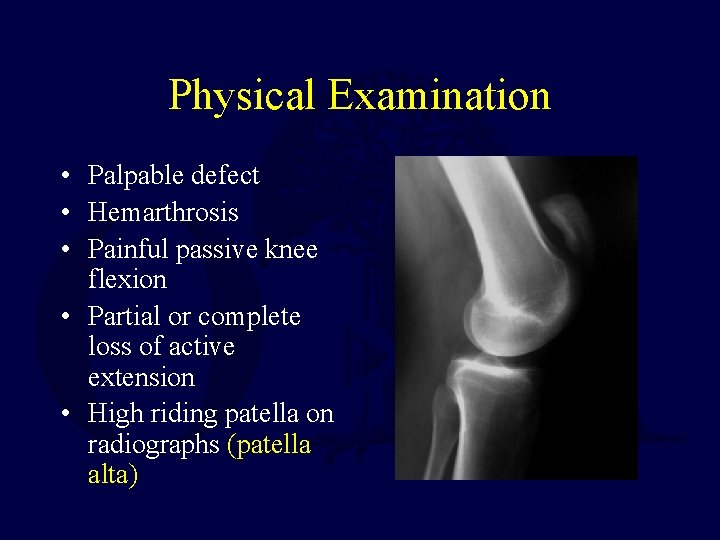
Physical Examination • Palpable defect • Hemarthrosis • Painful passive knee flexion • Partial or complete loss of active extension • High riding patella on radiographs (patella alta)
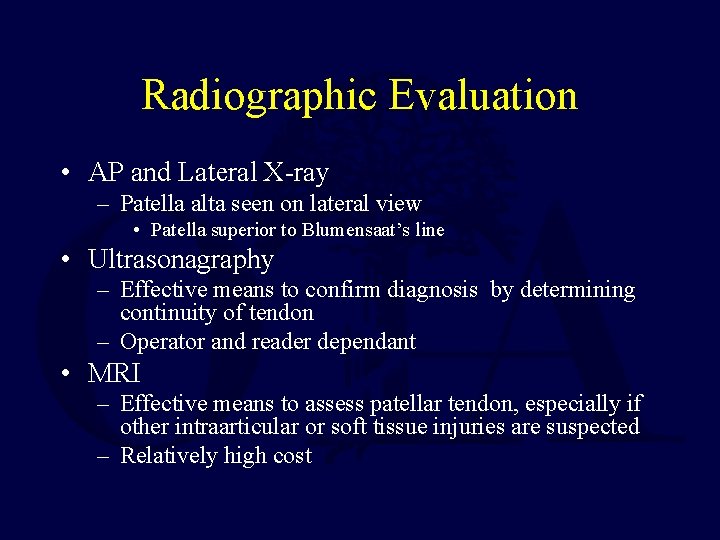
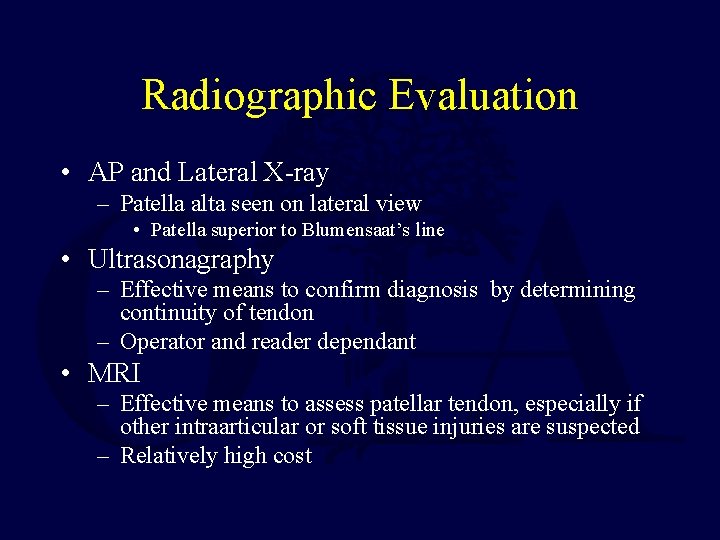
Radiographic Evaluation • AP and Lateral X-ray – Patella alta seen on lateral view • Patella superior to Blumensaat’s line • Ultrasonagraphy – Effective means to confirm diagnosis by determining continuity of tendon – Operator and reader dependant • MRI – Effective means to assess patellar tendon, especially if other intraarticular or soft tissue injuries are suspected – Relatively high cost
Classification • No widely accepted means of classification • Can be categorized by: – Location of tear • Proximal insertion most common – Timing between injury and surgery • Most important factor for prognosis • Acute: < 2 weeks • Chronic: > 2 weeks

Treatment • Surgical treatment is required for restoration of the extensor mechanism • Repairs categorized as early or delayed

Early Repair • Better overall outcome • Primary repair of the tendon • Surgical approach is through a midline incision – Incise just lateral to tibial tubercle as skin thicker with better blood supply to decrease wound complications • Patellar tendon rupture & retinacular tears are exposed • Frayed edges and hematoma are debrided
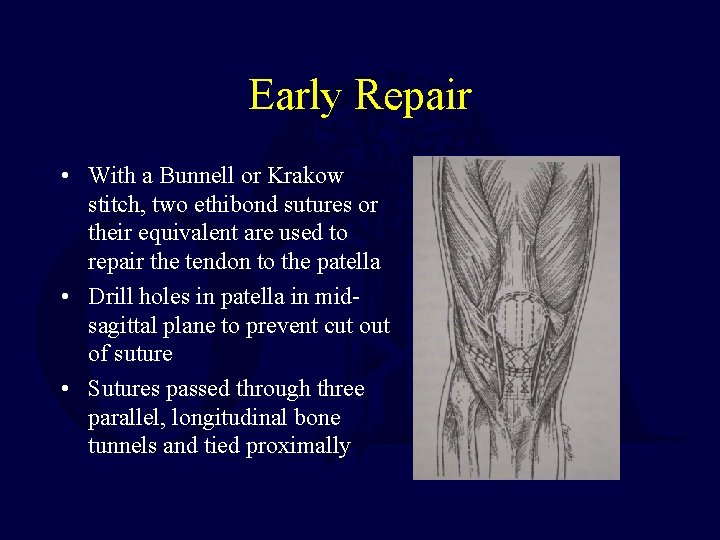
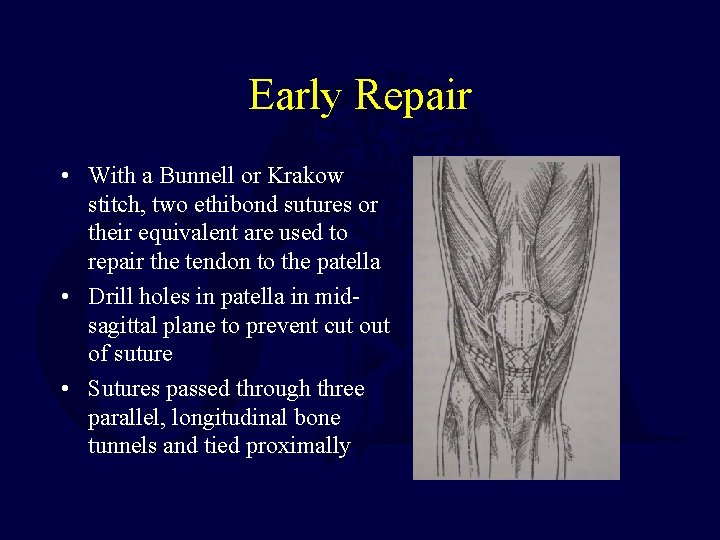
Early Repair • With a Bunnell or Krakow stitch, two ethibond sutures or their equivalent are used to repair the tendon to the patella • Drill holes in patella in midsagittal plane to prevent cut of suture • Sutures passed through three parallel, longitudinal bone tunnels and tied proximally
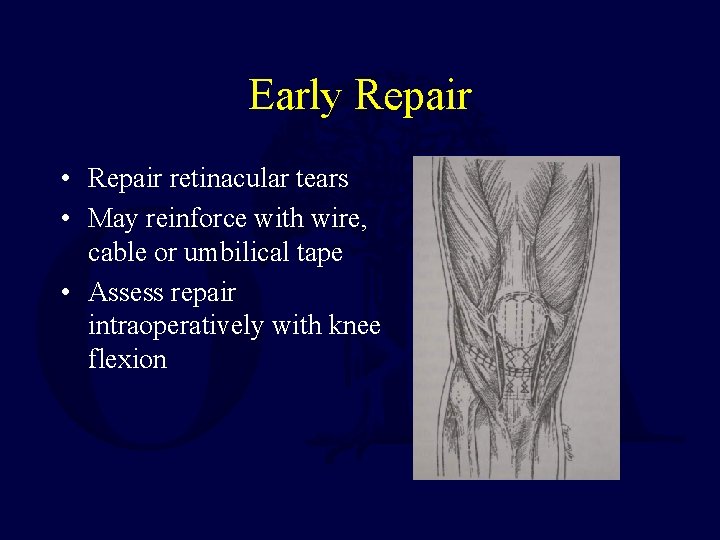
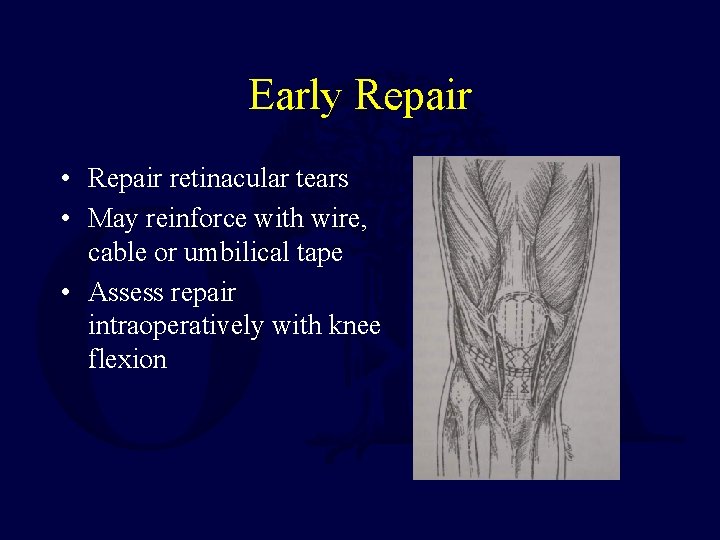
Early Repair • Repair retinacular tears • May reinforce with wire, cable or umbilical tape • Assess repair intraoperatively with knee flexion
Postoperative Management • Maintain hinged knee brace which is gradually increased as motion increases (tailor to the patient) • Immediate vs. delayed (3 weeks) weightbearing as tolerated • At 2 -3 weeks, hinged knee brace starting with 45 degrees active range of motion with 10 -15 degrees of progression each week • Immediate isometric quadriceps exercises • All restrictions are lifted after full range of motion and 90% of the contralateral quadriceps strength are obtained; usually at 4 -6 months
Delayed Repair • > 6 weeks from initial injury • Often results in poorer outcome • Quadriceps contraction and patellar migration are encountered • Adhesions between the patella and femur may be present • Options include hamstring and fascia lata autograft augmentation of primary repair or Achilles tendon allograft
Postoperative Management • More conservative when compared to early repair • Bivalved cylinder cast for 6 weeks; may start passive range of motion • Active range of motion is started at 6 weeks

Complications • • • Knee stiffness Persistent extensor weakness Rerupture Infection Patella baja (Insall-Salvati ratio of < 0. 8)
References Patella Fractures: New • Hughes SC, Stott PM, Hearnden AJ, Ripley LG: A new and effective tension band braided polyester suture technique for transverse patellar fracture fixation. Injury 2007: 38: 212 -222. • Luna-Pizarro D, Amato D, Arellano F, Hernandez A, Lopez-Rojas P: Comparison of a technique using a new percutaneous osteosynthesis device with conventional open surgery for displaced patella fractures in a randomized controlled trial. J Orthop Trauma 2006; 20: 529 -535.
References Patella Fractures: Classic • Carpenter JE, Kasman R. Matthews LS: Fractures of the patella. Instr Course Lect 1994: 43: 97 -108. • Burvant JG, Thomas KA, Alexander R, Harris MB. Evaluation of methods of internal fixation of transverse patella fractures: A biomechanical study. J Orthop Trauma 1994; 8: 147 -153. • Einola S, Aho AJ, Kallio P. Patellectomy after fracture: long term follow-up results with special reference to functional disability. Acta Orthop Scand 1976: 47: 441 -447.
References: Extensor Mechanism Injuries • Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am 1981; 63: 932 -937. • Bhargava SP, Hynes MC, Dowell JK. Traumatic patella tendon rupture: early mobilization following surgical repair. Injury 2004; 35: 76 -79. • Konrath GA, Chen D, Lock T et al. Outcomes following repair of quadriceps tendon ruptures. J Orthop Trauma 1998; 12: 273 -279.

Thank You! lcannada@slu. edu If you would like to volunteer as an author for the Resident Slide Project or recommend updates to any of the following slides, please send an e-mail to ota@ota. org E-mail OTA about Questions/Comments Return to Lower Extremity Index
 Lisa cannada md
Lisa cannada md Tear drop fracture
Tear drop fracture Lisa cannada md
Lisa cannada md Patella fracture mechanism of injury
Patella fracture mechanism of injury Daniel tibia
Daniel tibia Activity 14-1 glass fracture patterns
Activity 14-1 glass fracture patterns Ilioposas
Ilioposas Water seal suction chest tube
Water seal suction chest tube Fracture bois vert
Fracture bois vert Classification of open fractures
Classification of open fractures Dr sukhpal singh
Dr sukhpal singh Gustilo anderson classification antibiotics
Gustilo anderson classification antibiotics Triradiate cartilage
Triradiate cartilage Primary bone vs secondary bone
Primary bone vs secondary bone Weber classification of ankle fractures
Weber classification of ankle fractures Olecranon bursitis irving
Olecranon bursitis irving Types of fractures with pictures
Types of fractures with pictures Classification fracture supracondylienne
Classification fracture supracondylienne Types of glass fractures
Types of glass fractures Panfacial fractures sequencing
Panfacial fractures sequencing Concentric fracture glass definition
Concentric fracture glass definition Types of fractures with pictures
Types of fractures with pictures Disjonction symphyse pubienne classification
Disjonction symphyse pubienne classification Late complications of fractures
Late complications of fractures Fascia cruris
Fascia cruris Extensor expansion
Extensor expansion Leg extensors
Leg extensors Palmar vs volar
Palmar vs volar Extensor: an accelerator for sparse tensor algebra
Extensor: an accelerator for sparse tensor algebra Keresztezett hajlító feszítő reflex
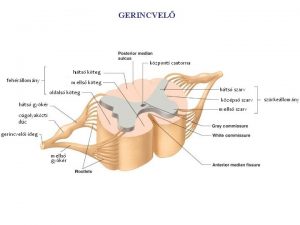
Keresztezett hajlító feszítő reflex Function of brachioradialis
Function of brachioradialis Flexor and extensor muscles
Flexor and extensor muscles Rigidity vs spasticity
Rigidity vs spasticity Peroneus tertius
Peroneus tertius Reflejo rotuliano
Reflejo rotuliano Extensor digitorum longus insertion
Extensor digitorum longus insertion Muscles crossing the shoulder joint
Muscles crossing the shoulder joint Plexus brachialis
Plexus brachialis Subanconeus
Subanconeus Lumbricals and interossei hand
Lumbricals and interossei hand Flexor digitorum profundus origin and insertion
Flexor digitorum profundus origin and insertion Abductor pollicis longus
Abductor pollicis longus Epicranial aponeurosis
Epicranial aponeurosis Foosh injury
Foosh injury Extensor posturing
Extensor posturing Musculo piriforme
Musculo piriforme Muskuli gluteal
Muskuli gluteal Flexor and extensor muscles
Flexor and extensor muscles Enfiye çukuru
Enfiye çukuru Innervation of flexor carpi radialis
Innervation of flexor carpi radialis Flexor pollicis longus origin and insertion
Flexor pollicis longus origin and insertion Forearm stretches
Forearm stretches 1st and 2nd lumbricals
1st and 2nd lumbricals Ulnar nerve muscles
Ulnar nerve muscles Crossed extensor reflex
Crossed extensor reflex Vestus intermedius
Vestus intermedius Brianna ochoa
Brianna ochoa Pronador largo
Pronador largo Dr nabil khouri
Dr nabil khouri Patellectomie partielle
Patellectomie partielle Atelectasis prefix and suffix
Atelectasis prefix and suffix Femur tibia patella
Femur tibia patella Patella bone
Patella bone Gurney's tubercle
Gurney's tubercle Radio rotule normale
Radio rotule normale Lamine rexed
Lamine rexed Patella tilt angle
Patella tilt angle Knee palpations
Knee palpations