PLAIN XRAY EVALUATION OF CONGENITALDR SK HEART DISEASE




- Slides: 95

PLAIN X-RAY EVALUATION OF CONGENITALDR. SK. HEART DISEASE SAMSUZ ZAMAN 3 rd YEAR PGT MEDICAL COLLEGE KOLKATA 1
INRODUCTION Chest x-ray is an important, cost effective & simple investigation to diagnose various heart diseases. Even though not the investigation of choice, it gives a lot of information regarding cardiac lesions. The erect , frontal chest radiograph in full inspiration with an exposure showing peripheral pulmonary vessels , rt & lt bronchi & location of aortic arch is most important. 2
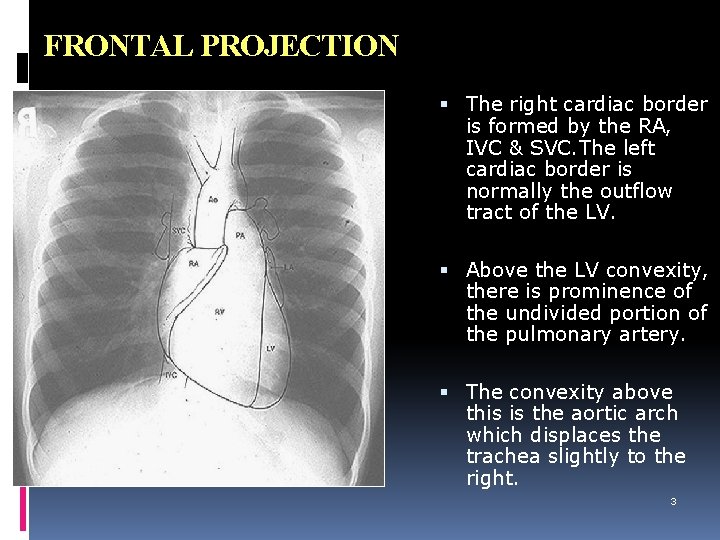
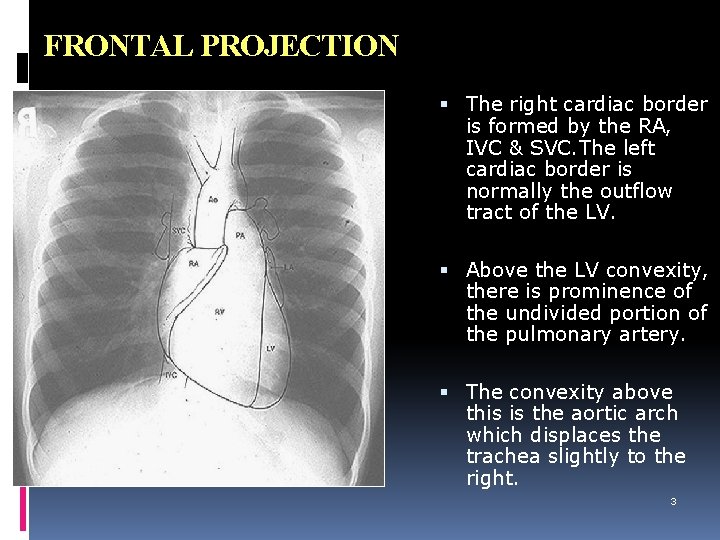
FRONTAL PROJECTION The right cardiac border is formed by the RA, IVC & SVC. The left cardiac border is normally the outflow tract of the LV. Above the LV convexity, there is prominence of the undivided portion of the pulmonary artery. The convexity above this is the aortic arch which displaces the trachea slightly to the right. 3
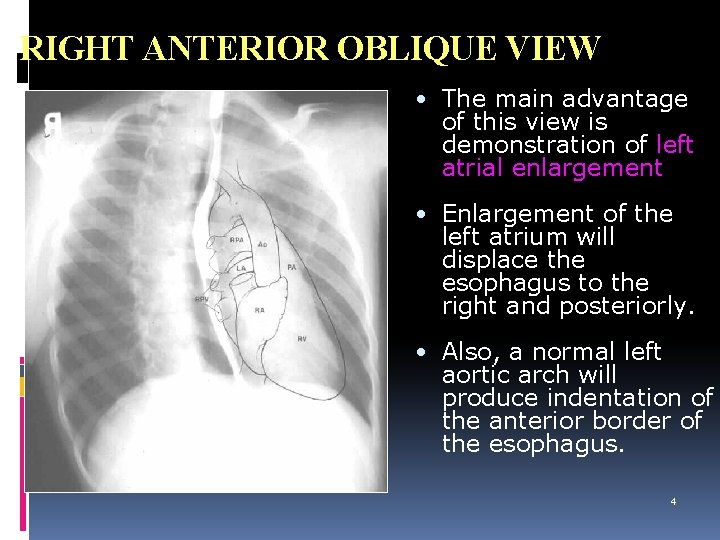
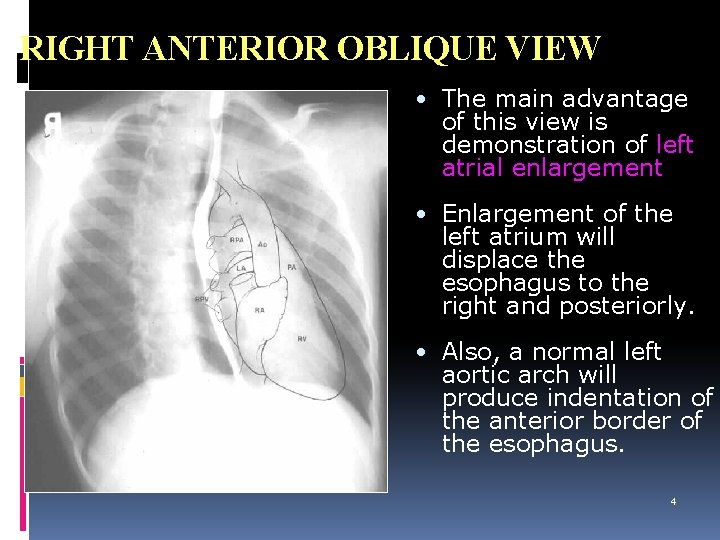
RIGHT ANTERIOR OBLIQUE VIEW • The main advantage of this view is demonstration of left atrial enlargement • Enlargement of the left atrium will displace the esophagus to the right and posteriorly. • Also, a normal left aortic arch will produce indentation of the anterior border of the esophagus. 4
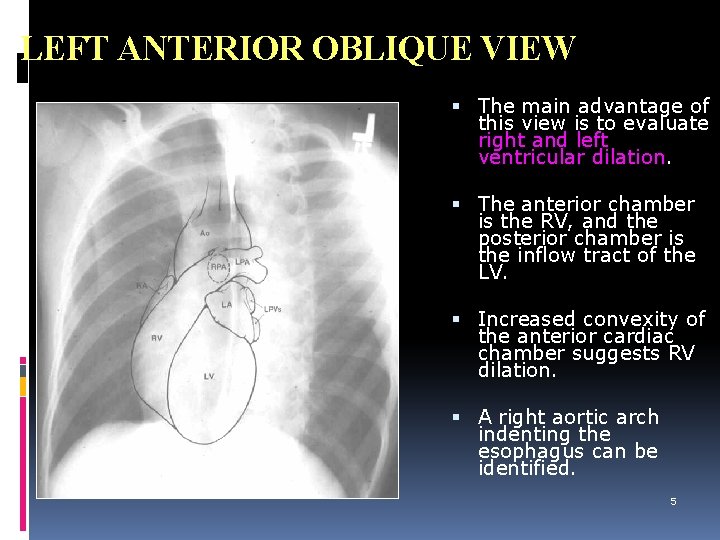
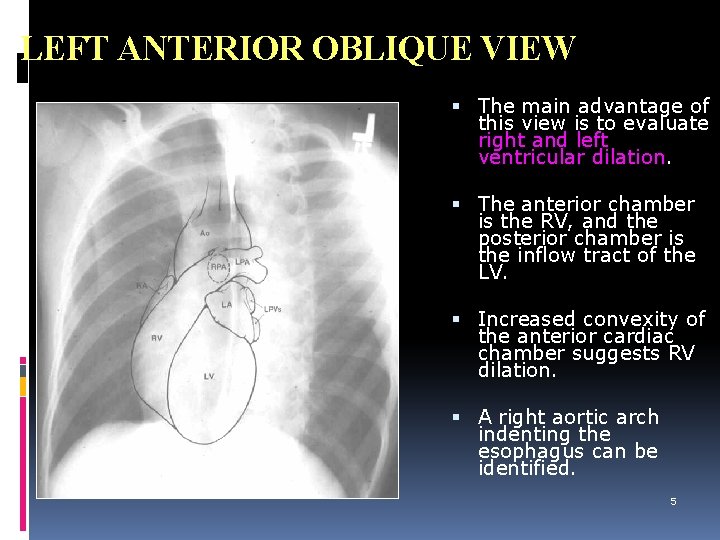
LEFT ANTERIOR OBLIQUE VIEW The main advantage of this view is to evaluate right and left ventricular dilation. The anterior chamber is the RV, and the posterior chamber is the inflow tract of the LV. Increased convexity of the anterior cardiac chamber suggests RV dilation. A right aortic arch indenting the esophagus can be identified. 5
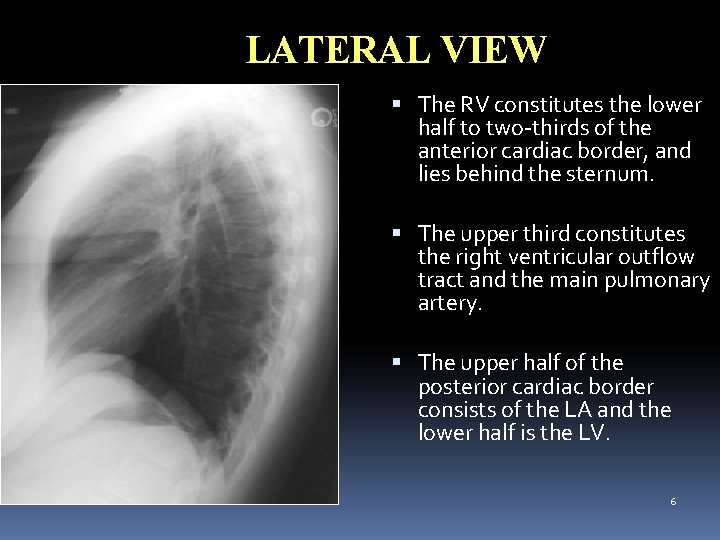
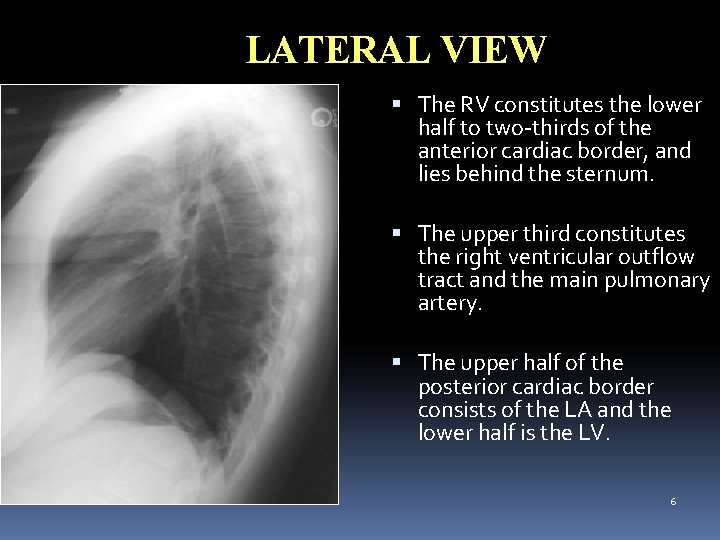
LATERAL VIEW The RV constitutes the lower half to two-thirds of the anterior cardiac border, and lies behind the sternum. The upper third constitutes the right ventricular outflow tract and the main pulmonary artery. The upper half of the posterior cardiac border consists of the LA and the lower half is the LV. 6
Congenital Heart diseases 75% of all CHD are not detected or do not have signs or symptom at infancy. Left to Right shunts , even large , rarely present with serious respiratory / cardiac difficulty in 1 st month of life. 7
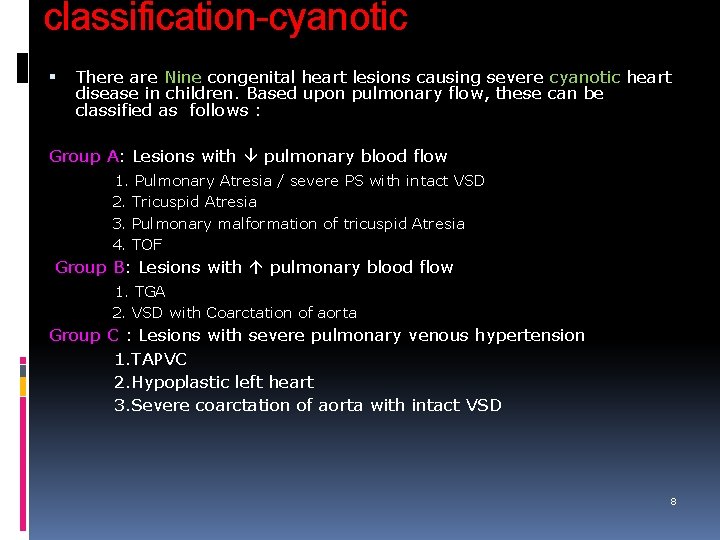
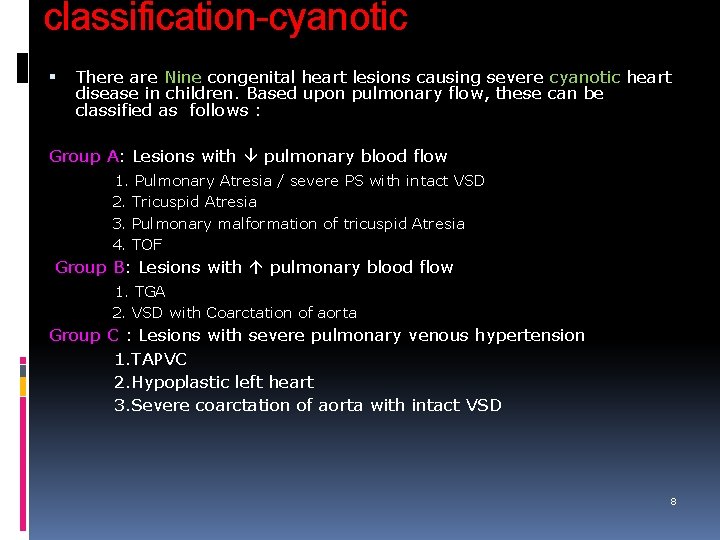
classification-cyanotic There are Nine congenital heart lesions causing severe cyanotic heart disease in children. Based upon pulmonary flow, these can be classified as follows : Group A: Lesions with pulmonary blood flow 1. Pulmonary Atresia / severe PS with intact VSD 2. Tricuspid Atresia 3. Pulmonary malformation of tricuspid Atresia 4. TOF Group B: Lesions with pulmonary blood flow 1. TGA 2. VSD with Coarctation of aorta Group C : Lesions with severe pulmonary venous hypertension 1. TAPVC 2. Hypoplastic left heart 3. Severe coarctation of aorta with intact VSD 8
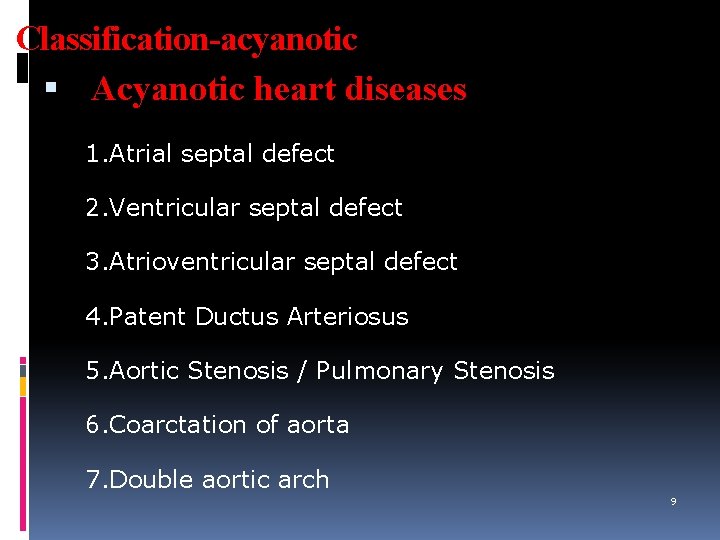
Classification-acyanotic Acyanotic heart diseases 1. Atrial septal defect 2. Ventricular septal defect 3. Atrioventricular septal defect 4. Patent Ductus Arteriosus 5. Aortic Stenosis / Pulmonary Stenosis 6. Coarctation of aorta 7. Double aortic arch 9
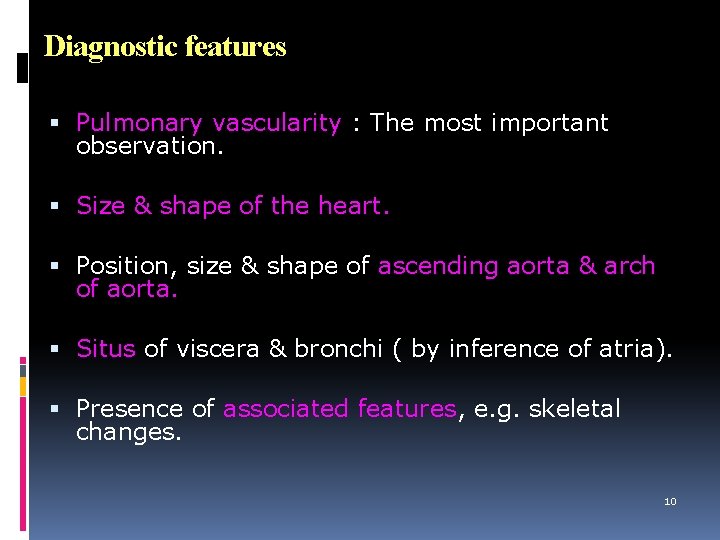
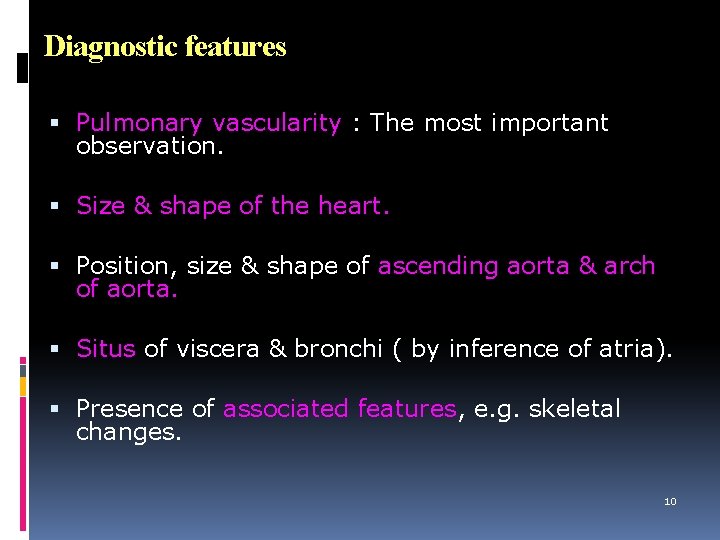
Diagnostic features Pulmonary vascularity : The most important observation. Size & shape of the heart. Position, size & shape of ascending aorta & arch of aorta. Situs of viscera & bronchi ( by inference of atria). Presence of associated features, e. g. skeletal changes. 10
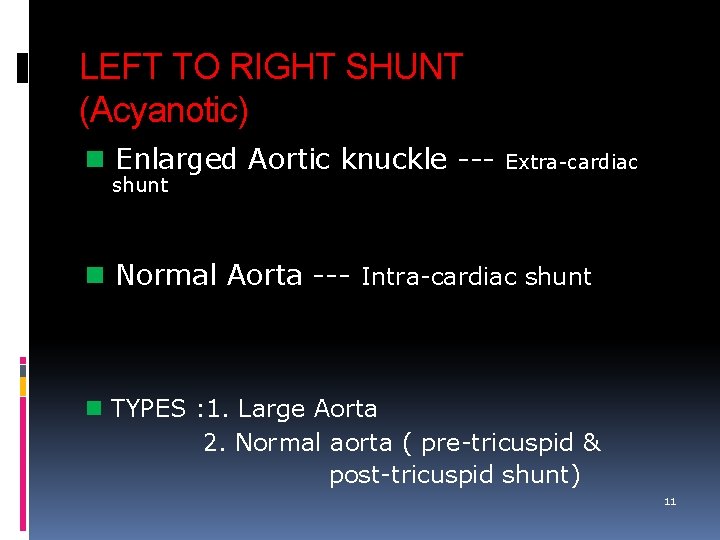
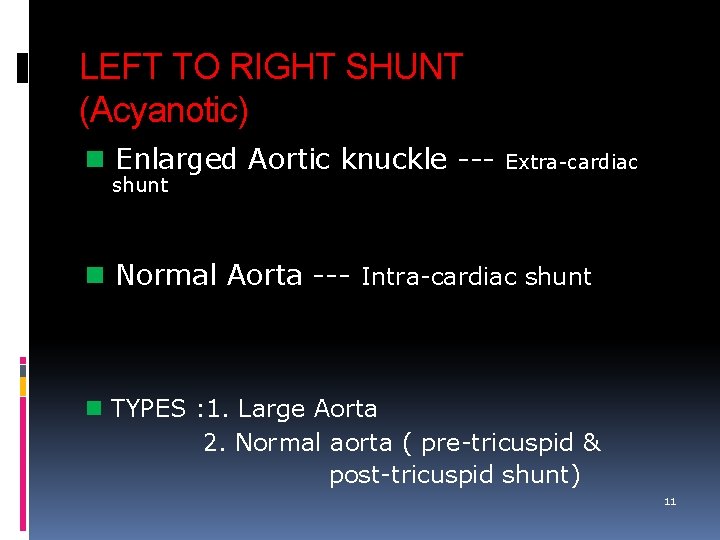
LEFT TO RIGHT SHUNT (Acyanotic) Enlarged Aortic knuckle --- Extra-cardiac shunt Normal Aorta --- Intra-cardiac shunt TYPES : 1. Large Aorta 2. Normal aorta ( pre-tricuspid & post-tricuspid shunt) 11
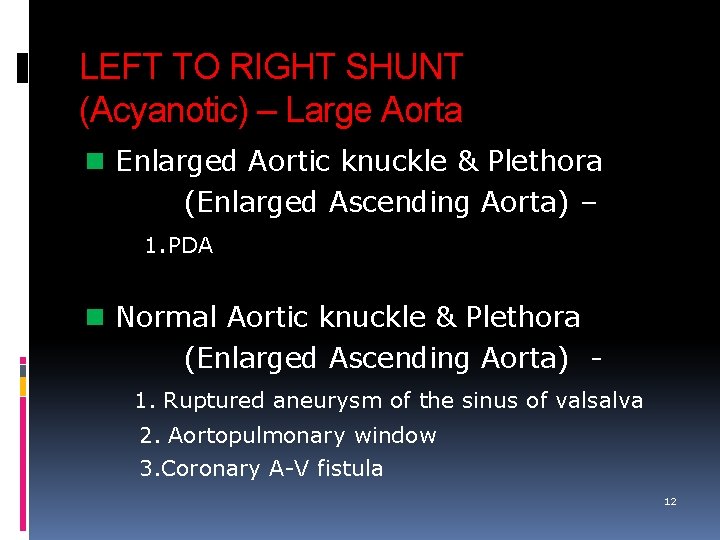
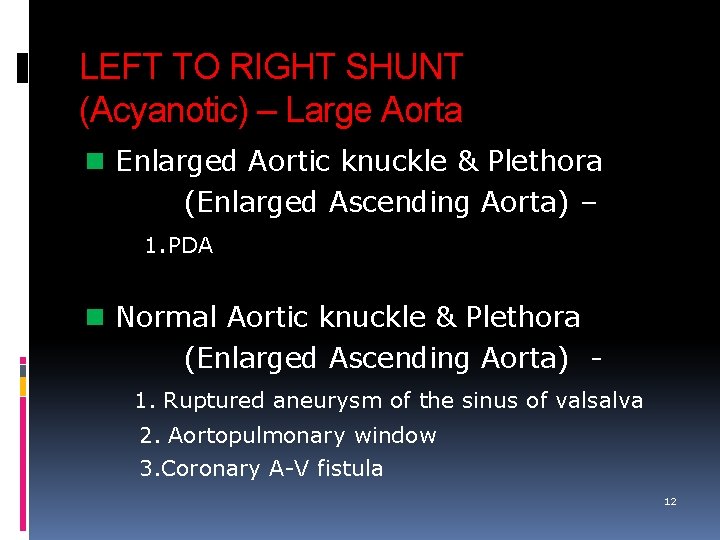
LEFT TO RIGHT SHUNT (Acyanotic) – Large Aorta Enlarged Aortic knuckle & Plethora (Enlarged Ascending Aorta) – 1. PDA Normal Aortic knuckle & Plethora (Enlarged Ascending Aorta) 1. Ruptured aneurysm of the sinus of valsalva 2. Aortopulmonary window 3. Coronary A-V fistula 12
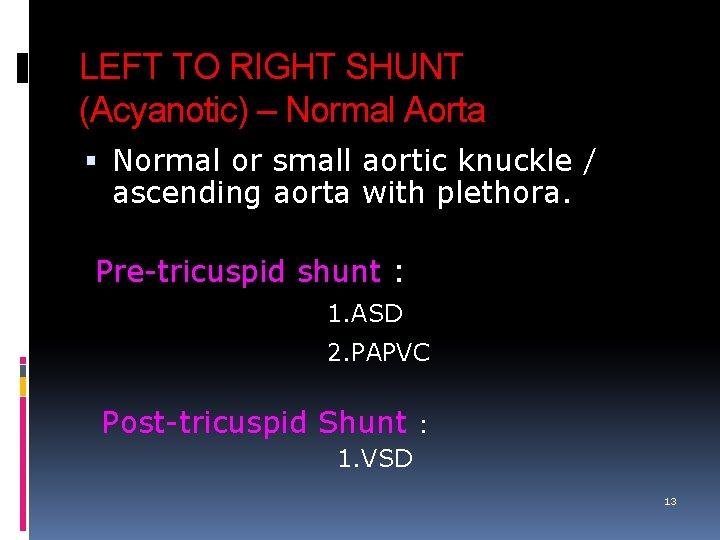
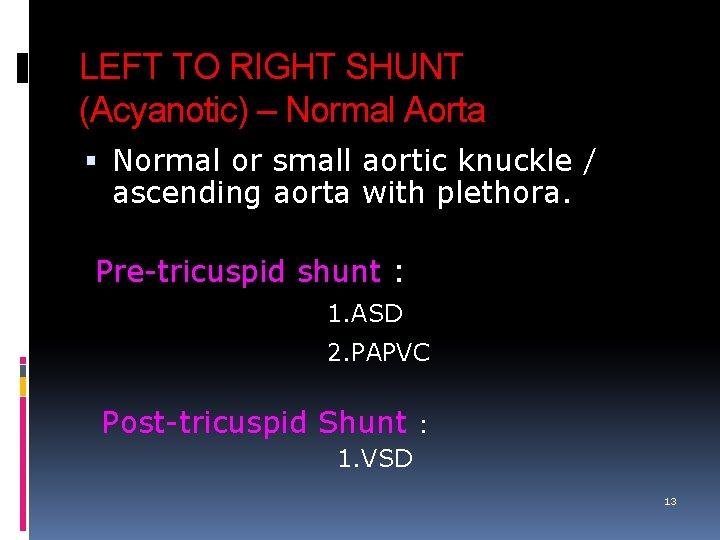
LEFT TO RIGHT SHUNT (Acyanotic) – Normal Aorta Normal or small aortic knuckle / ascending aorta with plethora. Pre-tricuspid shunt : 1. ASD 2. PAPVC Post-tricuspid Shunt : 1. VSD 13

RIGHT TO LEFT SHUNT Cyanosis 14
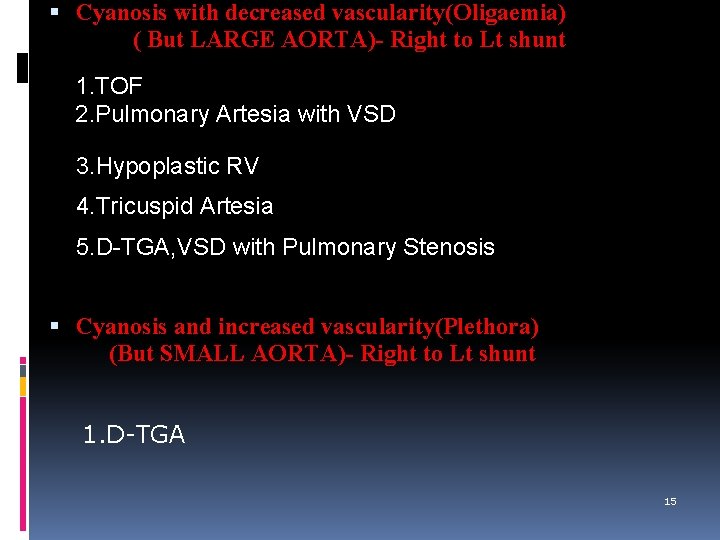
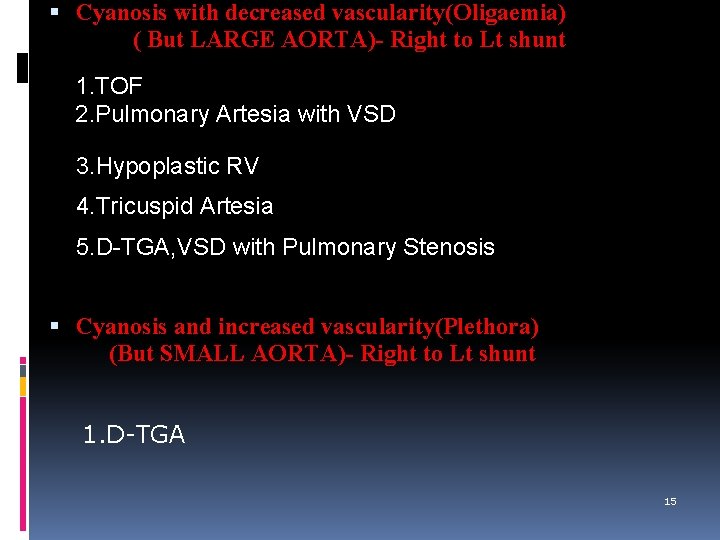
Cyanosis with decreased vascularity(Oligaemia) ( But LARGE AORTA)- Right to Lt shunt 1. TOF 2. Pulmonary Artesia with VSD 3. Hypoplastic RV 4. Tricuspid Artesia 5. D-TGA, VSD with Pulmonary Stenosis Cyanosis and increased vascularity(Plethora) (But SMALL AORTA)- Right to Lt shunt 1. D-TGA 15
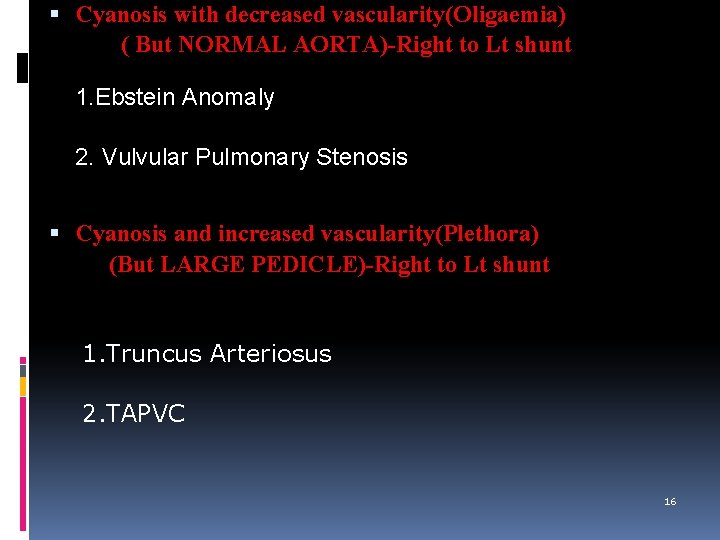
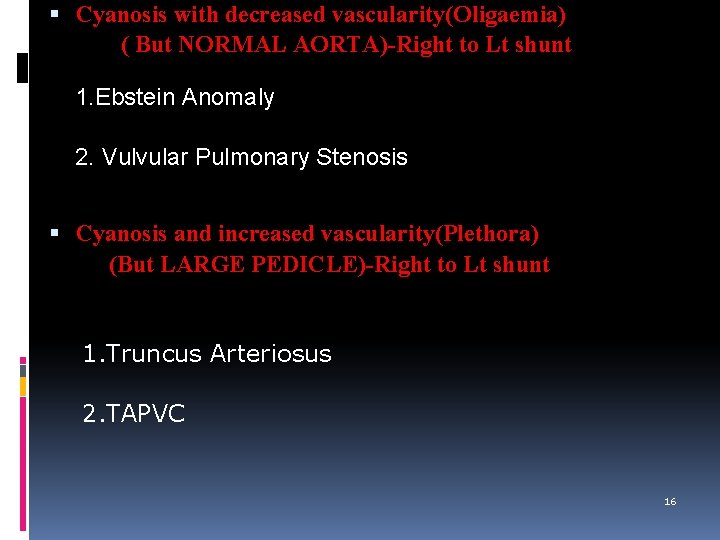
Cyanosis with decreased vascularity(Oligaemia) ( But NORMAL AORTA)-Right to Lt shunt 1. Ebstein Anomaly 2. Vulvular Pulmonary Stenosis Cyanosis and increased vascularity(Plethora) (But LARGE PEDICLE)-Right to Lt shunt 1. Truncus Arteriosus 2. TAPVC 16
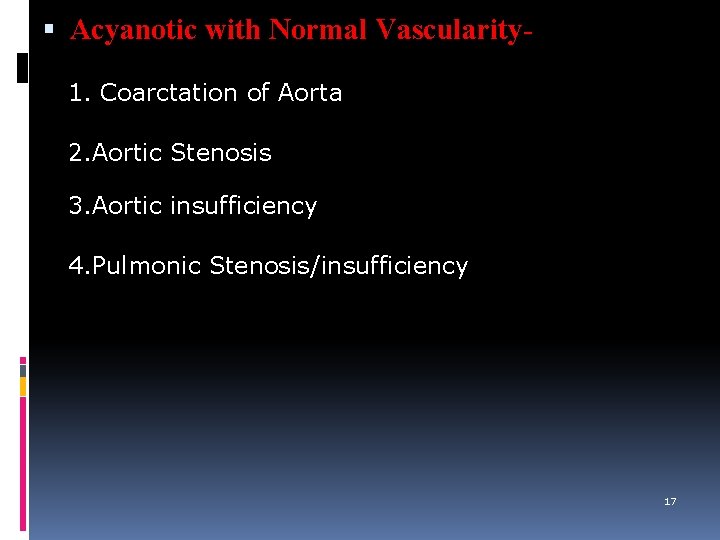
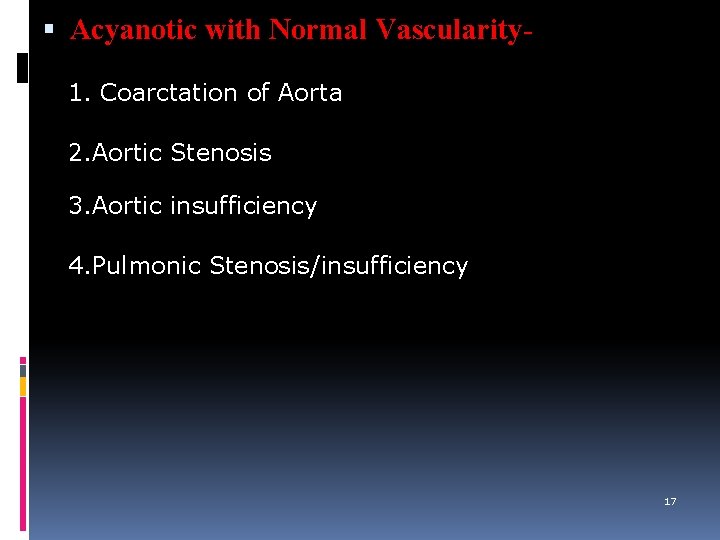
Acyanotic with Normal Vascularity 1. Coarctation of Aorta 2. Aortic Stenosis 3. Aortic insufficiency 4. Pulmonic Stenosis/insufficiency 17
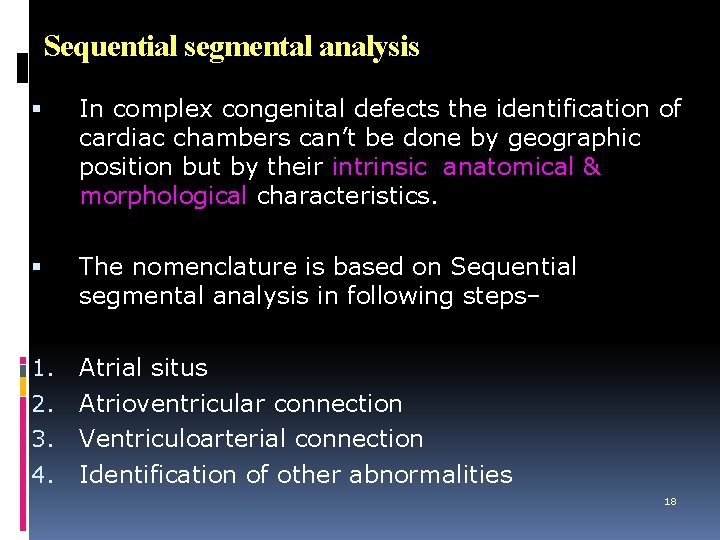
Sequential segmental analysis In complex congenital defects the identification of cardiac chambers can’t be done by geographic position but by their intrinsic anatomical & morphological characteristics. The nomenclature is based on Sequential segmental analysis in following steps– 1. Atrial situs Atrioventricular connection Ventriculoarterial connection Identification of other abnormalities 2. 3. 4. 18
How the heart chambers are named Anatomic right atrium is on the side of the trilobed lung and liver & the anatomic left atrium is on the side of the bilobed lung and spleen. The atrial appendages are the best method of atrial identification. Rt atrial appd. is triangular with a wide base ‘Dog ear configuration’. Terminal crest & pectinate muscle is present within. Lt atrial appd. is a tubular structure. The AV valves belong to the anatomic ventricles not atria 19
The anatomic RV is the coarsely trabeculated with a muscular pulmonic infundibulum & a mid ventricular ‘Moderator band’. Outflow portion is separated from inflow tract by crista supraventricularis. The anatomic LV is the smooth-walled ventricle. Fibrous continuity between: mitral valve anterior leaflet and aortic valve. The pulmonic valve is part of pulmonary artery not anatomic RV & the aortic valve is part of aorta not anatomic LV. The aorta & pulmonary arteries are identified by their typical branching patterns. 20
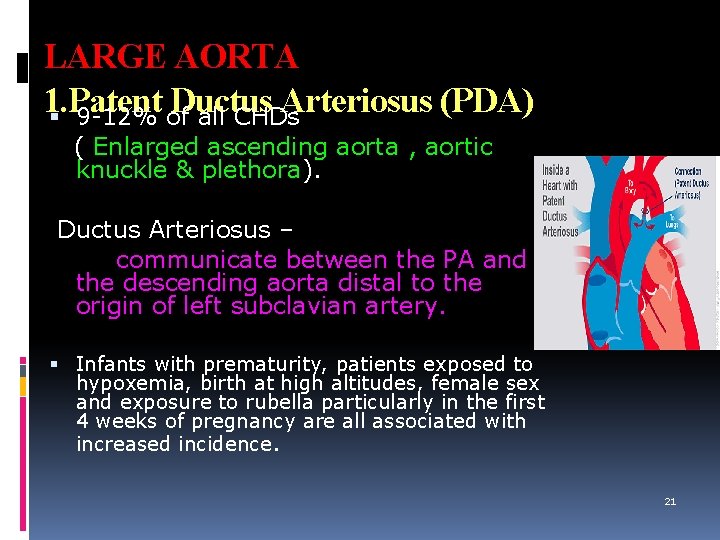
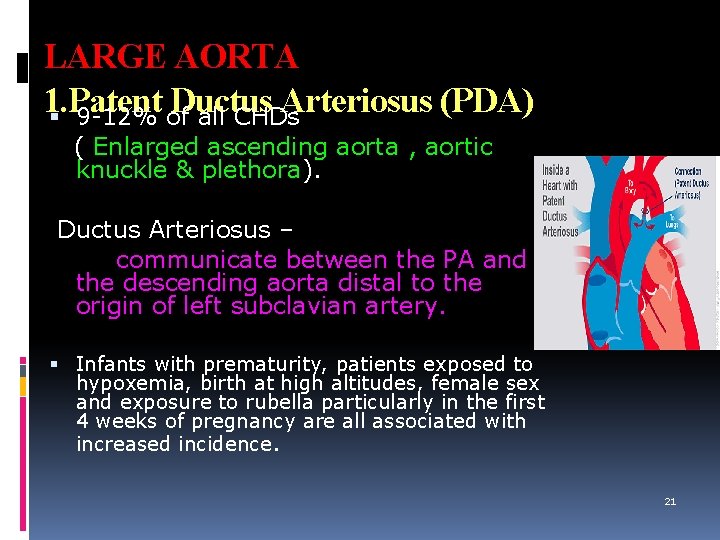
LARGE AORTA 1. Patent Ductus Arteriosus (PDA) 9 -12% of all CHDs ( Enlarged ascending aorta , aortic knuckle & plethora). Ductus Arteriosus – communicate between the PA and the descending aorta distal to the origin of left subclavian artery. Infants with prematurity, patients exposed to hypoxemia, birth at high altitudes, female sex and exposure to rubella particularly in the first 4 weeks of pregnancy are all associated with increased incidence. 21
X-ray findings A small PDA may be asymptomatic & not detected on X-ray. Sometimes seen as an inconspicuous soft convexity b/w aortic knob & PA. In mod to large PDA : ( L R shunt – blood shift from aorta to PA – more blood at PA & pulmonary circulation causing plethora – more blood at pulmonary vein – more blood at LA – more blood at LV – more blood at aorta – enlarged ascending aorta - large aortic knuckle due to shifting of blood occours distal to left subclavian artery) LA, LV, PA & its branches(plethora) , ascending aorta & aortic knuckle are enlarged. The main PA may become calcified s/o chronic PAH PDA with reversal exhibits reduced pulmonary vascularity , dilatation of pulmonary trunk, a normal LV & hypertrophied RV. 22
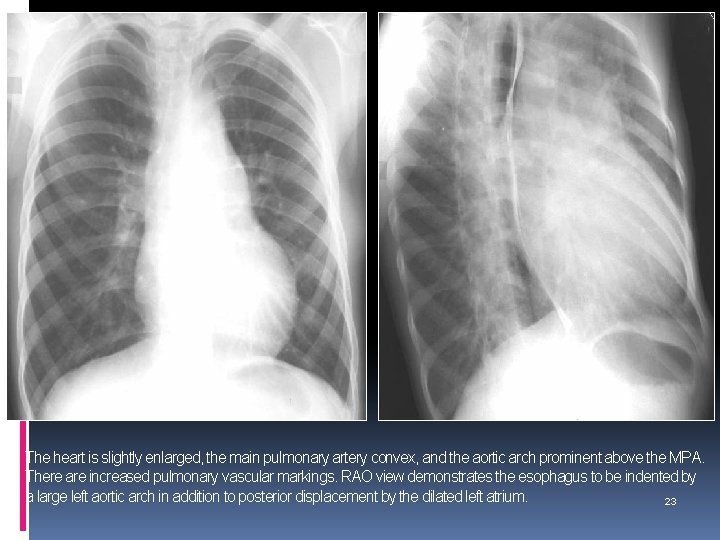
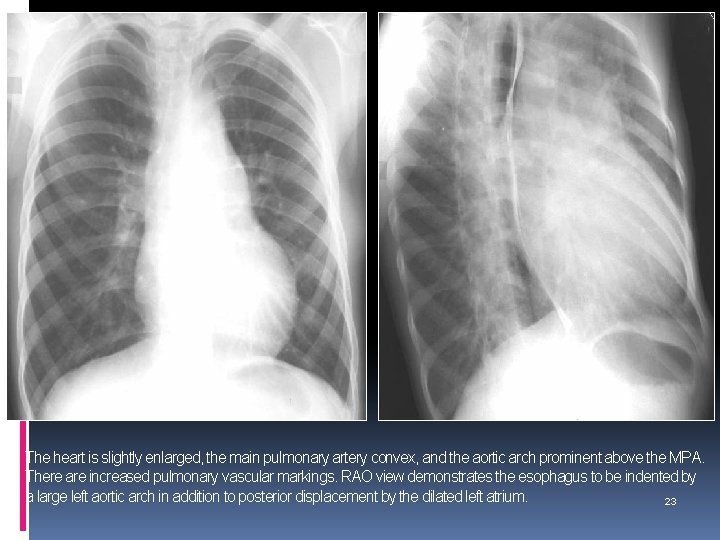
The heart is slightly enlarged, the main pulmonary artery convex, and the aortic arch prominent above the MPA. There are increased pulmonary vascular markings. RAO view demonstrates the esophagus to be indented by a large left aortic arch in addition to posterior displacement by the dilated left atrium. 23
…LARGE AORTA If the ascending aorta is enlarged disproportionate to the aortic knuckle, the L R shunt is at the aortic root level (Enlarged ascending aorta & plethora but normal aortic knuckle). TYPES : 1. Ruptured aneurysm of the sinus of valsalva(RSOV) 2. Aortopulmonary window 3. Coronary A-V fistula 24
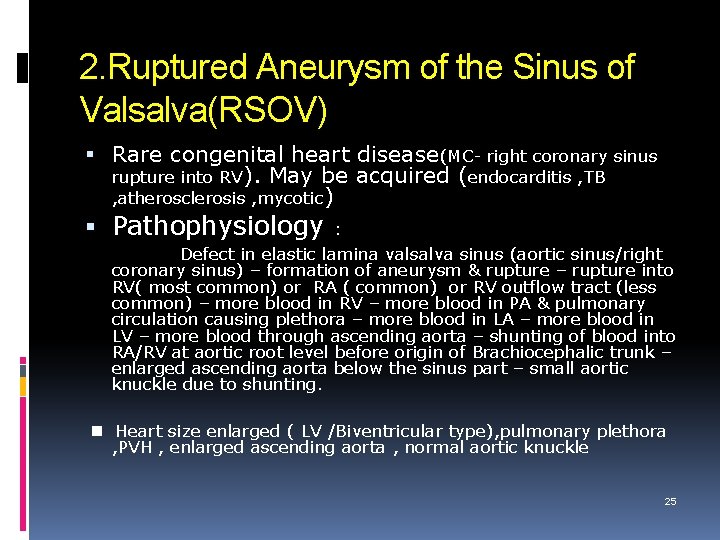
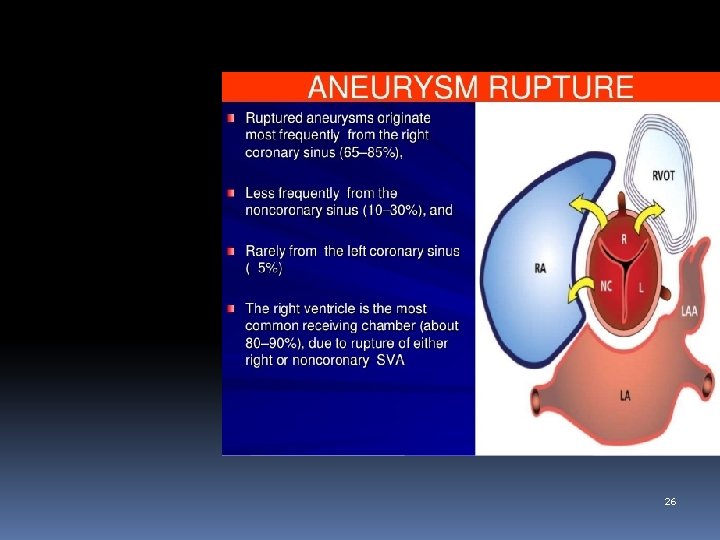
2. Ruptured Aneurysm of the Sinus of Valsalva(RSOV) Rare congenital heart disease(MC- right coronary sinus rupture into RV). May be acquired (endocarditis , TB , atherosclerosis , mycotic) Pathophysiology : Defect in elastic lamina valsalva sinus (aortic sinus/right coronary sinus) – formation of aneurysm & rupture – rupture into RV( most common) or RA ( common) or RV outflow tract (less common) – more blood in RV – more blood in PA & pulmonary circulation causing plethora – more blood in LA – more blood in LV – more blood through ascending aorta – shunting of blood into RA/RV at aortic root level before origin of Brachiocephalic trunk – enlarged ascending aorta below the sinus part – small aortic knuckle due to shunting. Heart size enlarged ( LV /Biventricular type), pulmonary plethora , PVH , enlarged ascending aorta , normal aortic knuckle 25
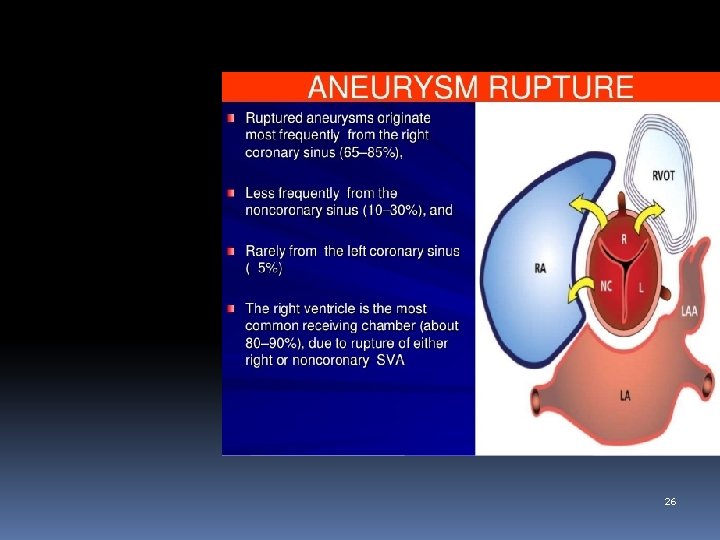
26
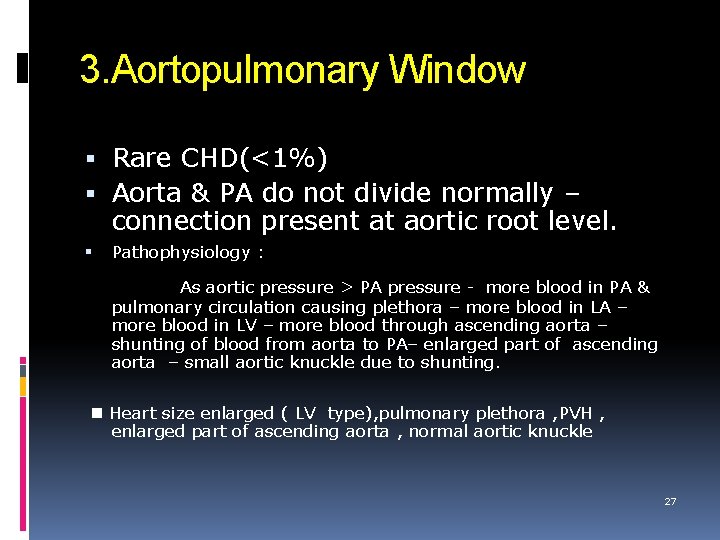
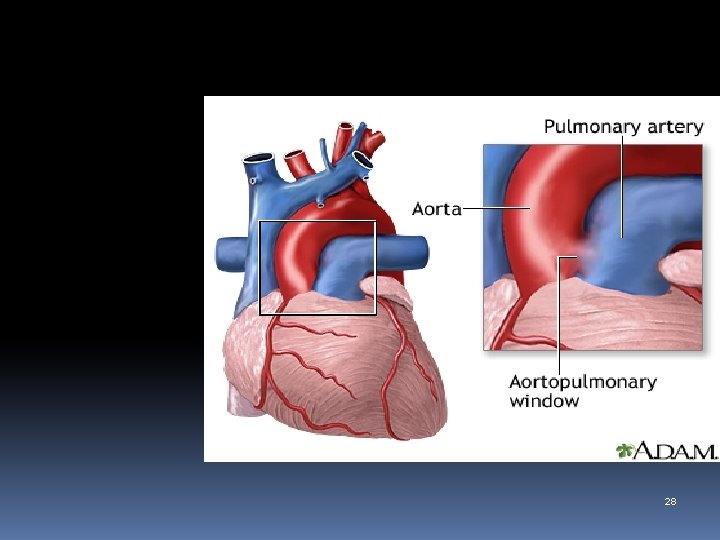
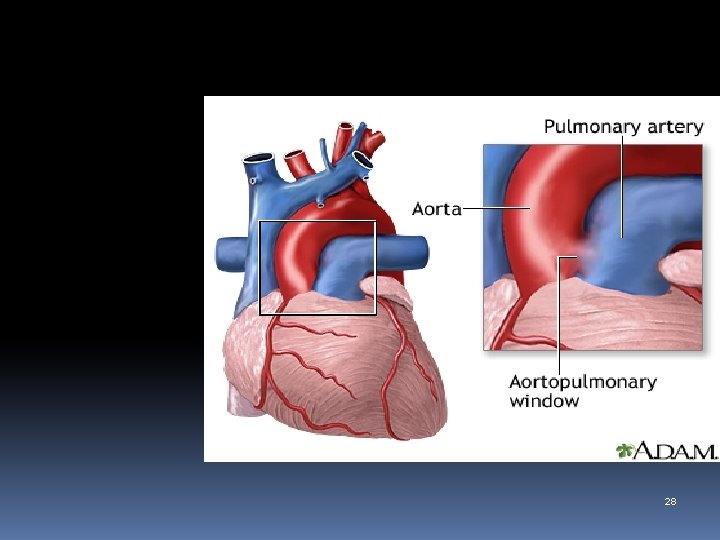
3. Aortopulmonary Window Rare CHD(<1%) Aorta & PA do not divide normally – connection present at aortic root level. Pathophysiology : As aortic pressure > PA pressure - more blood in PA & pulmonary circulation causing plethora – more blood in LA – more blood in LV – more blood through ascending aorta – shunting of blood from aorta to PA– enlarged part of ascending aorta – small aortic knuckle due to shunting. Heart size enlarged ( LV type), pulmonary plethora , PVH , enlarged part of ascending aorta , normal aortic knuckle 27
28
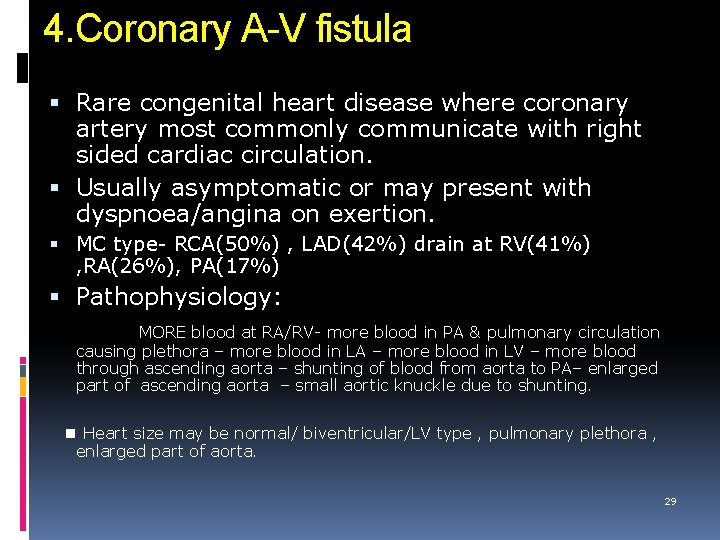
4. Coronary A-V fistula Rare congenital heart disease where coronary artery most commonly communicate with right sided cardiac circulation. Usually asymptomatic or may present with dyspnoea/angina on exertion. MC type- RCA(50%) , LAD(42%) drain at RV(41%) , RA(26%), PA(17%) Pathophysiology: MORE blood at RA/RV- more blood in PA & pulmonary circulation causing plethora – more blood in LA – more blood in LV – more blood through ascending aorta – shunting of blood from aorta to PA– enlarged part of ascending aorta – small aortic knuckle due to shunting. Heart size may be normal/ biventricular/LV type , pulmonary plethora , enlarged part of aorta. 29
Normal aorta , L R shunt , pre-tricuspid 1. Atrial Septal Defect (ASD) 6 -8% of all CHDs. The most common CHD detected in adults. An ASD is defined as any communication within the atrial septum which results in shunting between the atria. Holt-Oram syndrome is as/d with autosomal dominant inherited ASDs with absent or hypoplastic radii, and ECG findings of 1 st degree AV block and RBBB. 30
Classification Patent foramen ovale -25 -30% of normal hearts has incomplete fusion of septum primum & secundum with a potential for right to left shunt. Ostium secundum defect - 80% of all ASDs. located in the fossa ovalis. Ostium primum defect - prev. Regarded as ASD but actually is an AVSD. Sinus venosus defect - found at the junction of caval veins & the right atrium. Pathophysiology : LA pressure>RA pressure – more blood in RA/RV – more blood through PA causing plethora(more on right side) – normal aorta 31
X-ray findings (Pulmonary Plethora – normal aorta – acyanotic ) Cardiomegaly with enlargement of RA & RV- pulmonary plethora – normal aorta. Gross enlargement of pulmonary artery (calcified in chronic cases). Ampullary sign : bulging of SVC in sinus venosus defect 32
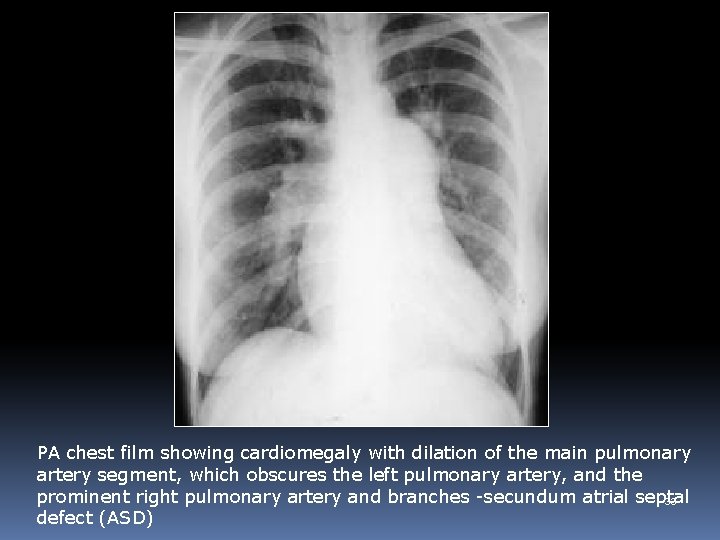
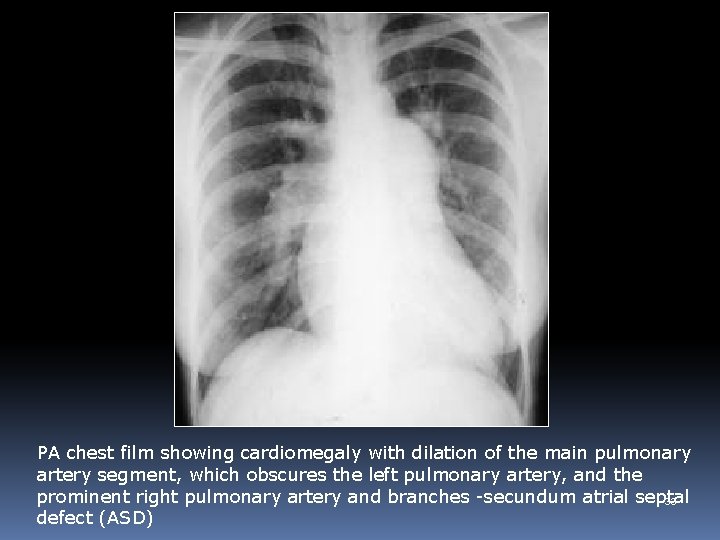
PA chest film showing cardiomegaly with dilation of the main pulmonary artery segment, which obscures the left pulmonary artery, and the prominent right pulmonary artery and branches -secundum atrial septal 33 defect (ASD)
Normal aorta , L R shunt , pre-tricuspid 2. Partial anomalous pulmonary venous connection (PAPVC) Rare congenital anomaly in which some pulmonary veins (not all) drain into systemic circulation rather than in the left atrium. Types : Supra-cardiac : Veins drain into right SVC(MC) , persistent left SVC , brachiocephalic vein. Cardiac : Veins drain into RA , coronary sinus Infra-cardiac : veins drain into portal vein, hepatic vein , IVC ( scimitar syndrome) mixed : combination of two or more 34
PAPVC cont. . . Right sided PAPVC common – children. Left sided PAPVC common – adult. Left upper lobe vein anomaly MC. Association – ASD (40%). Abnormal vein rarely identified except scimitar sydrome . Suspected radiographic features of ASD with abnormally enlarged shadow of SVC or abnormally directed pulmonary veins. Pathophysiology : Abnormally directed pulmonary veins in SVC/RA/IVC – more blood in RA – more blood in RV – enlarged PA causing plethora – normal aorta 35
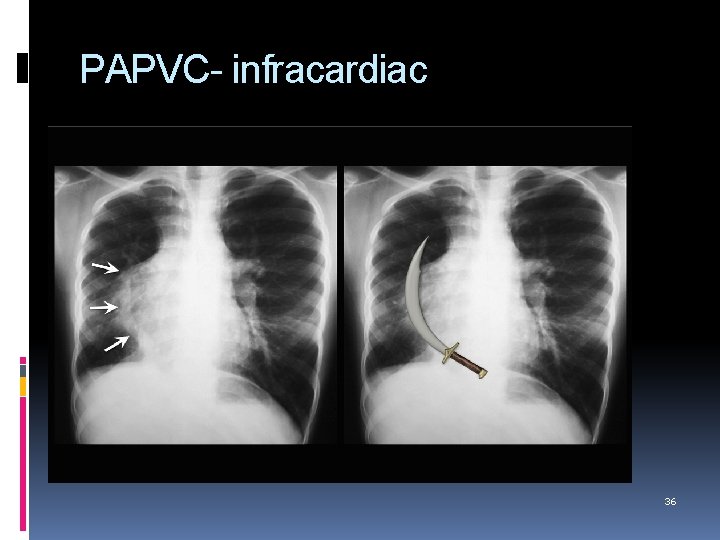
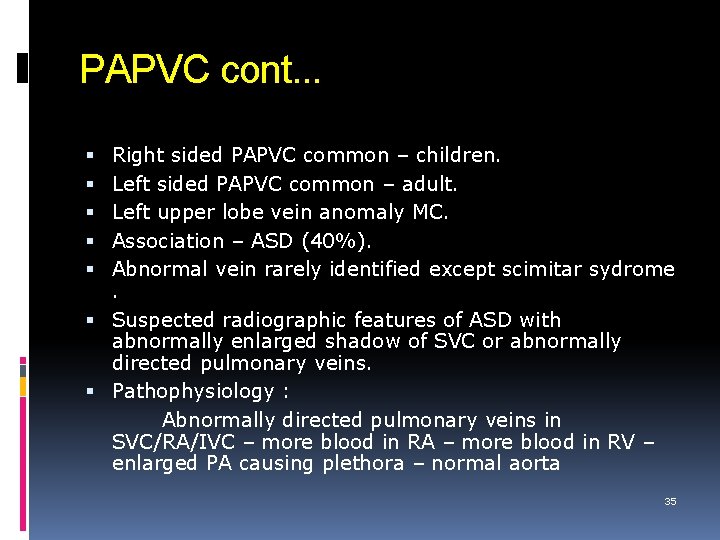
PAPVC- infracardiac 36
Normal aorta, L R shunt , Post-tricuspid 1. Ventricular Septal Defect (VSD) VSDs represent the commonest , acyanotic form of CHDs. Classification: Supracristal VSD (type I): occur beneath the pulmonary valve and communicate with the RV outflow tract. Perimembranous VSD (type II): (80% ) occur infracristal. 3 groups related to anatomical position; Perimembranous inlet, perimembranous trabecular (commonest) perimembranous outlet. 37
AV canal VSD (type III): (10%) occur beneath the tricuspid valve, in the posterior region of the septum. Muscular VSD (type IV): occur within the muscular septum and are subclassified as inlet, trabecular and infundibular. Trabecular defects may be multiple and described as Swiss cheese defects. Small membranous defects close spontaneously but muscular defects rarely do. COA & AS are most important ASD cardiac anomaly. Left to right shunt through VSD – more blood in RV – more blood through PA causing plethora & PAH –normal aorta. Cardiomegaly with LV / Bi-ventriculer configuration with 38 plethora & PAH.
X-ray findings Small defects show normal sized heart and PA & its branches. Large defects are associated with Hyperinflated lung fields with flat hemidiaphragms. Enlargement of LA & volume overload of LV. RA enlargement indicates CHF. Increase in size of PA & branches. Small sized aorta. 39
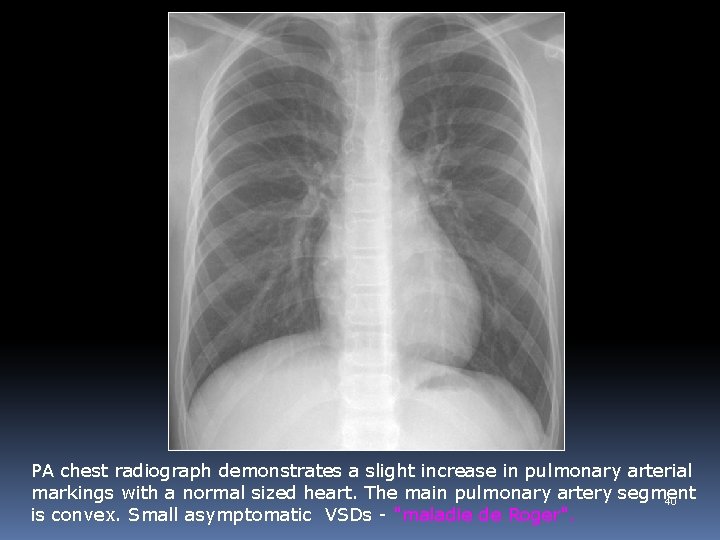
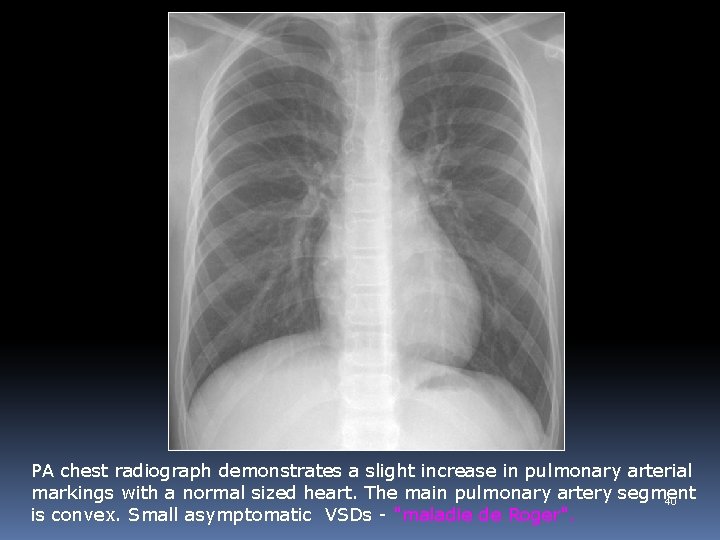
PA chest radiograph demonstrates a slight increase in pulmonary arterial markings with a normal sized heart. The main pulmonary artery segment 40 is convex. Small asymptomatic VSDs - "maladie de Roger".
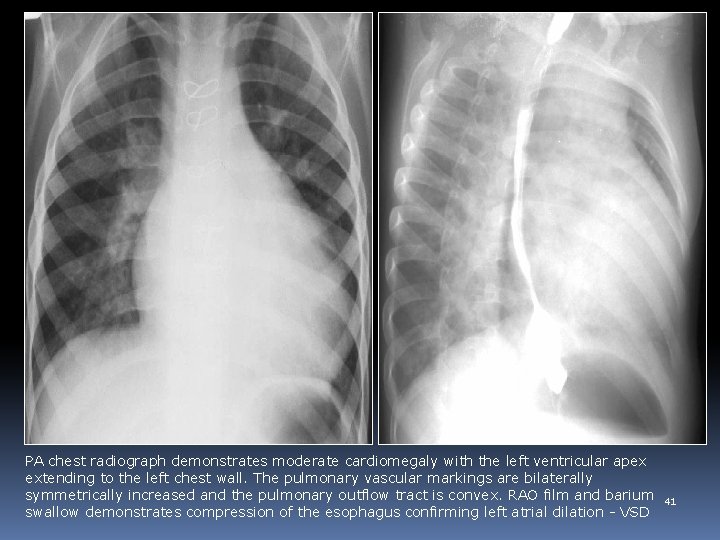
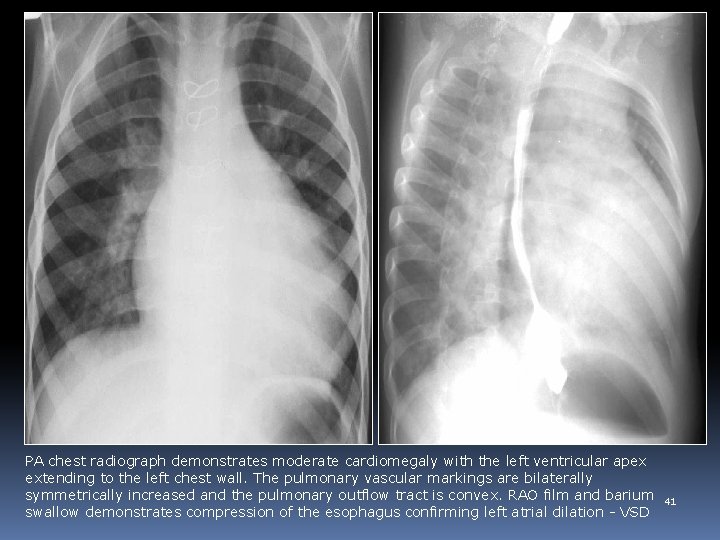
PA chest radiograph demonstrates moderate cardiomegaly with the left ventricular apex extending to the left chest wall. The pulmonary vascular markings are bilaterally symmetrically increased and the pulmonary outflow tract is convex. RAO film and barium swallow demonstrates compression of the esophagus confirming left atrial dilation - VSD 41
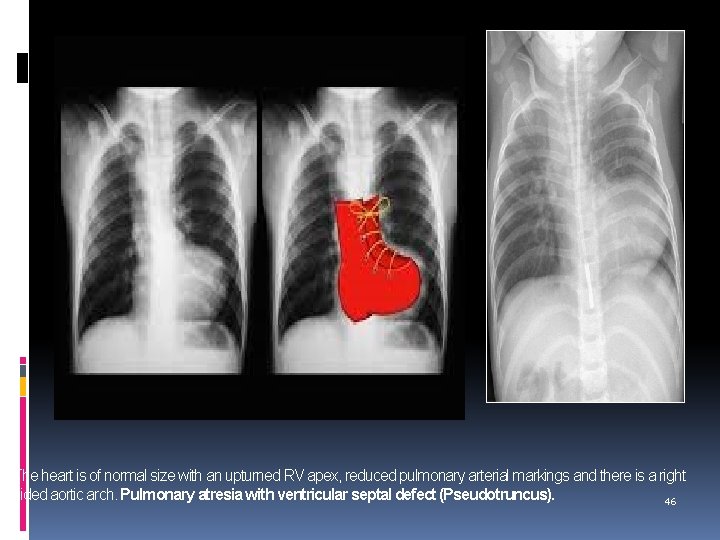
Large aorta, Rt to Lt shunt , pulmonary oligaemia 1. Tetralogy of Fallot ( TOF) TOF is the commonest cyanotic CHD after age of 2 years. Pathophysiology : PS(small pulmonary conus) with VSD causing pulmonary oligaemia – Rt to Lt shunt causing cyanosismore blood in LV- more blood in aorta – large aorta. Pseudotruncus Arteriosus : Tetralogy with pulmonary Atresia. Pentalogy of Fallot : Tetralogy with ASD Association: 1. Right sided aortic arch(25%) 2. Anamalous coronary artery 3. AVSD 4. MS / AS 5. Absent pulmonary artery ( lt>rt) 6. Rib notching may be due to collateral 7. Cardiomegaly - in PR/TR , absent pulmonary valve, 42
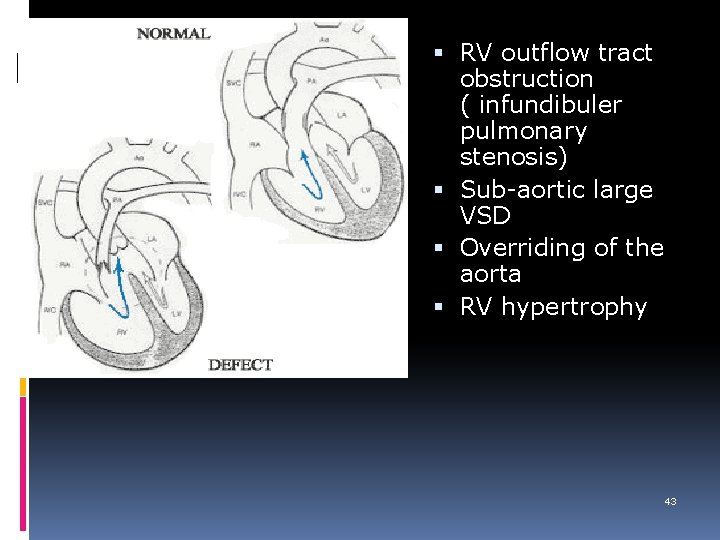
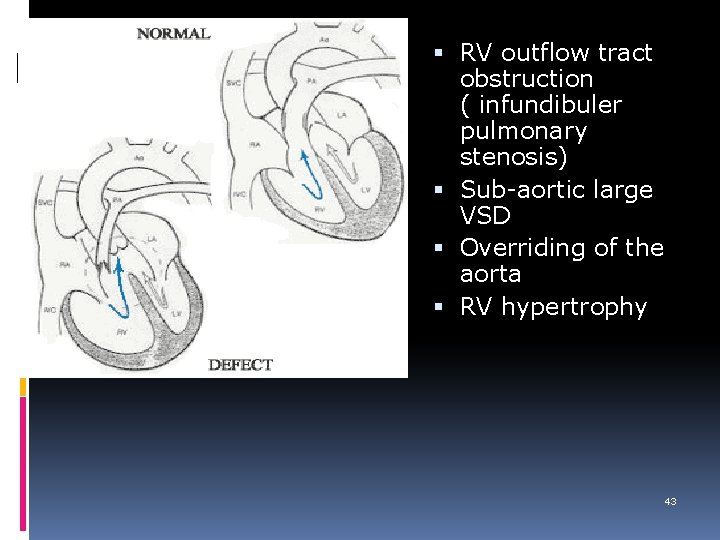
RV outflow tract obstruction ( infundibuler pulmonary stenosis) Sub-aortic large VSD Overriding of the aorta RV hypertrophy 43
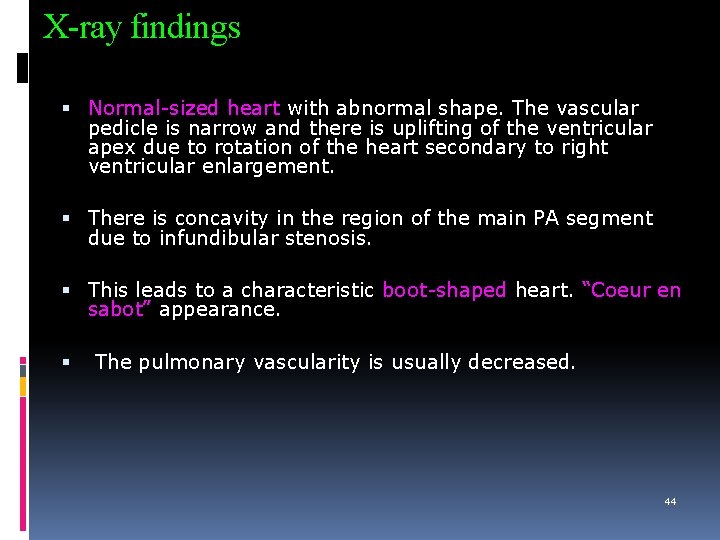
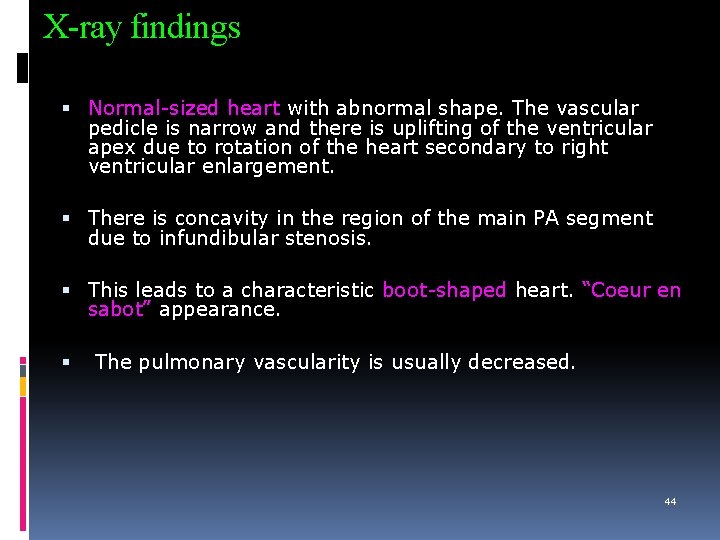
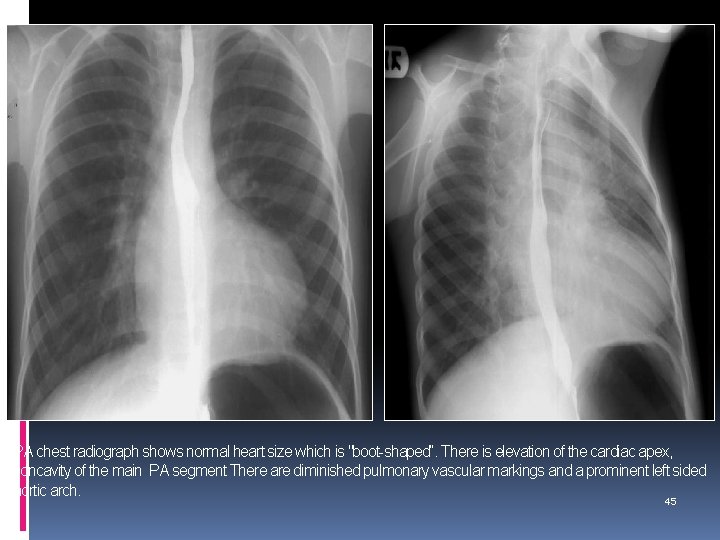
X-ray findings Normal-sized heart with abnormal shape. The vascular pedicle is narrow and there is uplifting of the ventricular apex due to rotation of the heart secondary to right ventricular enlargement. There is concavity in the region of the main PA segment due to infundibular stenosis. This leads to a characteristic boot-shaped heart. “Coeur en sabot” appearance. The pulmonary vascularity is usually decreased. 44
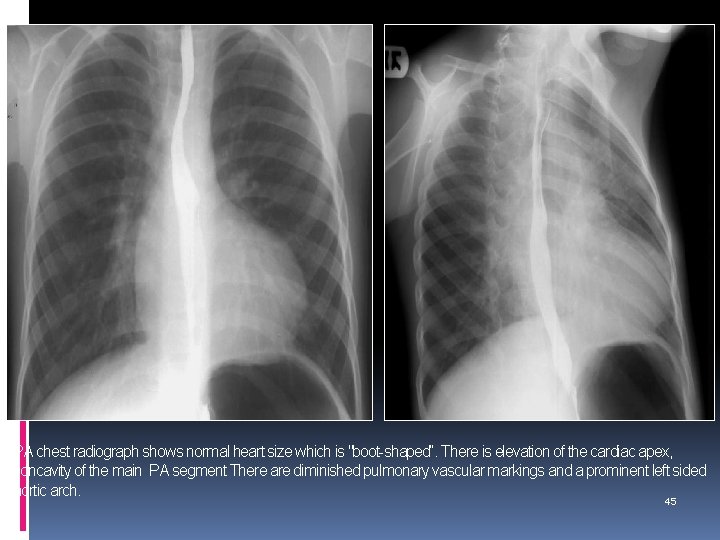
PA chest radiograph shows normal heart size which is "boot-shaped“. There is elevation of the cardiac apex, concavity of the main PA segment There are diminished pulmonary vascular markings and a prominent left sided aortic arch. 45
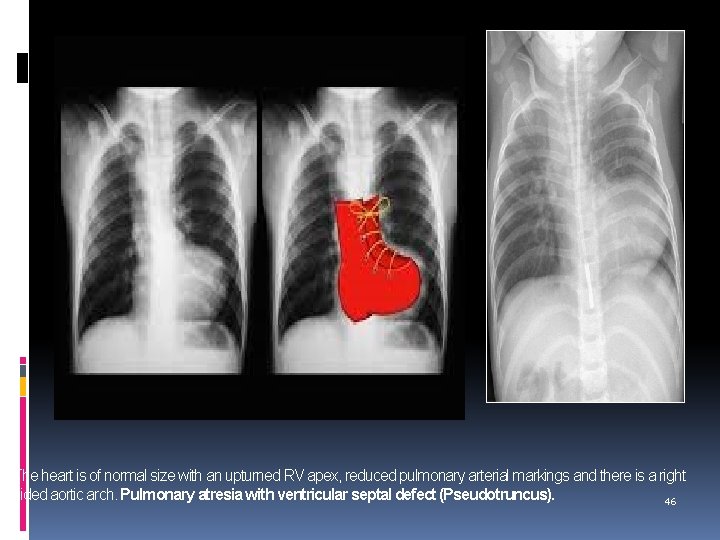
The heart is of normal size with an upturned RV apex, reduced pulmonary arterial markings and there is a right sided aortic arch. Pulmonary atresia with ventricular septal defect (Pseudotruncus). 46
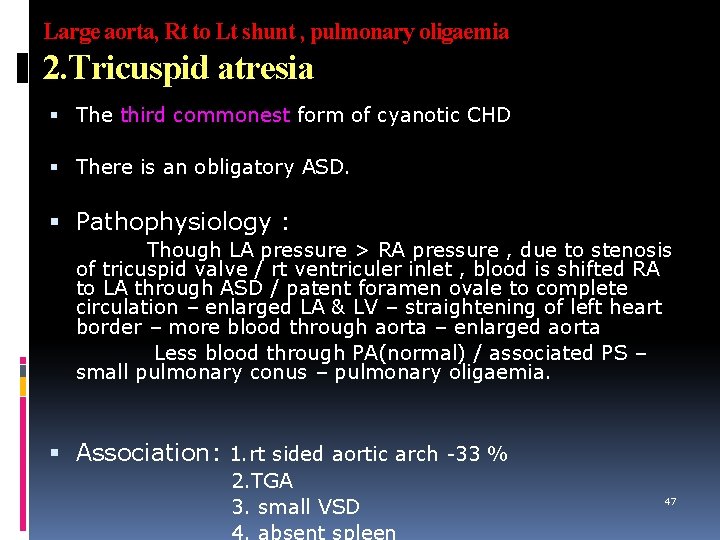
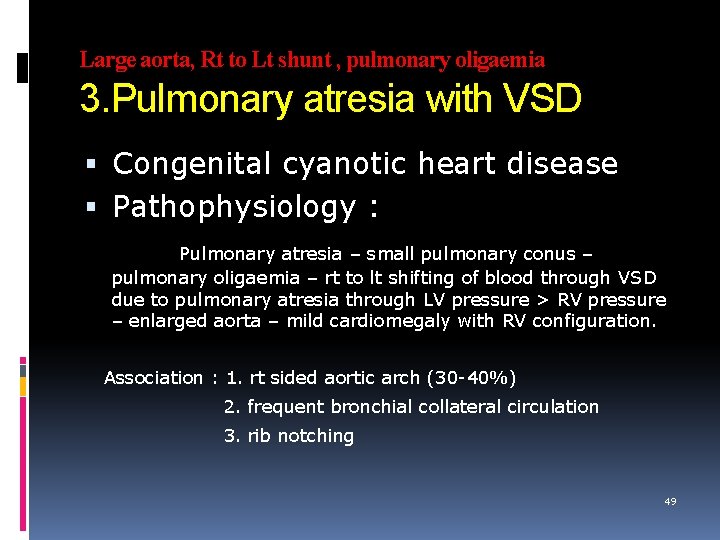
Large aorta, Rt to Lt shunt , pulmonary oligaemia 2. Tricuspid atresia The third commonest form of cyanotic CHD There is an obligatory ASD. Pathophysiology : Though LA pressure > RA pressure , due to stenosis of tricuspid valve / rt ventriculer inlet , blood is shifted RA to LA through ASD / patent foramen ovale to complete circulation – enlarged LA & LV – straightening of left heart border – more blood through aorta – enlarged aorta Less blood through PA(normal) / associated PS – small pulmonary conus – pulmonary oligaemia. Association: 1. rt sided aortic arch -33 % 2. TGA 3. small VSD 47
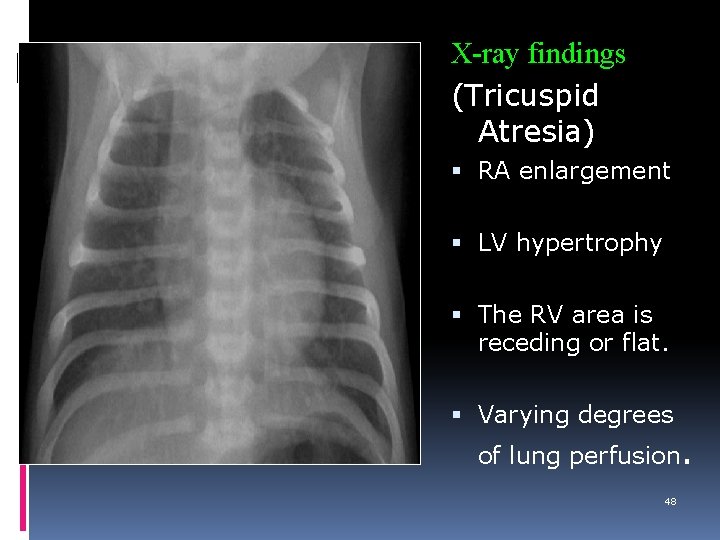
X-ray findings (Tricuspid Atresia) RA enlargement LV hypertrophy The RV area is receding or flat. Varying degrees of lung perfusion. 48
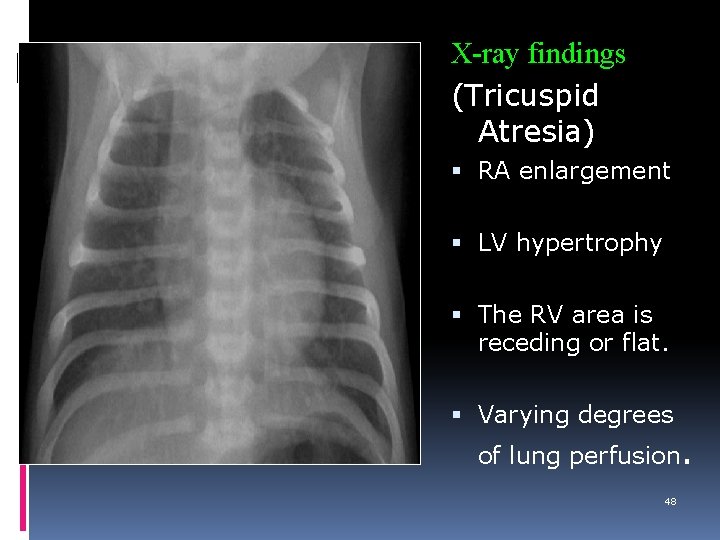
Large aorta, Rt to Lt shunt , pulmonary oligaemia 3. Pulmonary atresia with VSD Congenital cyanotic heart disease Pathophysiology : Pulmonary atresia – small pulmonary conus – pulmonary oligaemia – rt to lt shifting of blood through VSD due to pulmonary atresia through LV pressure > RV pressure – enlarged aorta – mild cardiomegaly with RV configuration. Association : 1. rt sided aortic arch (30 -40%) 2. frequent bronchial collateral circulation 3. rib notching 49
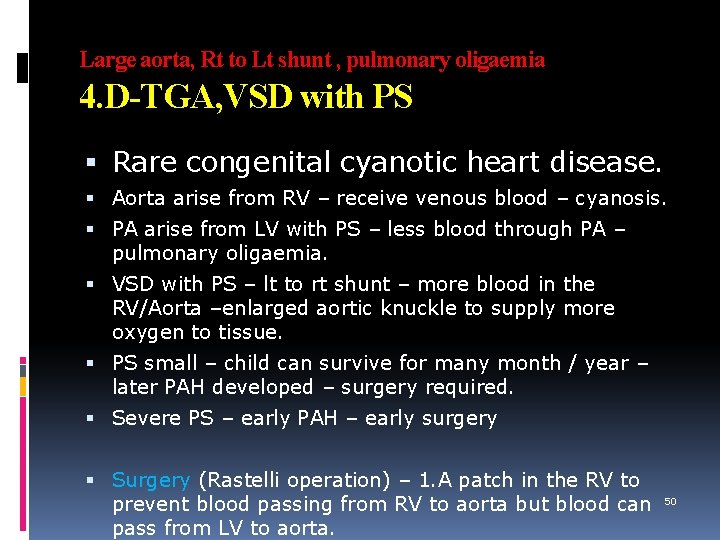
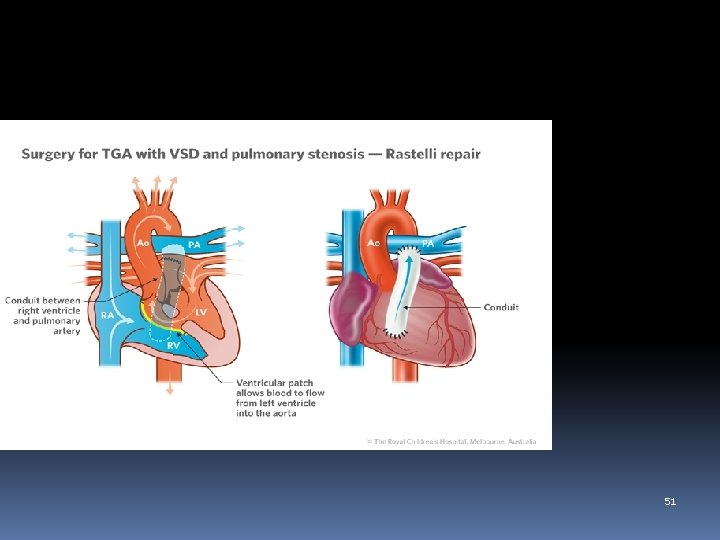
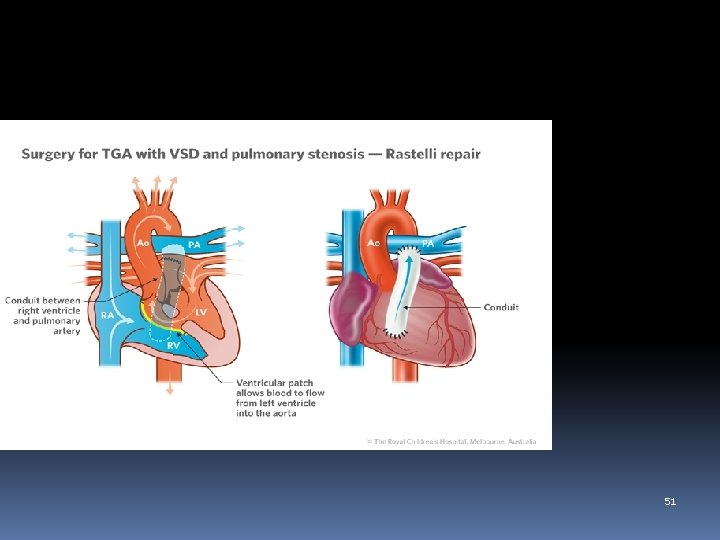
Large aorta, Rt to Lt shunt , pulmonary oligaemia 4. D-TGA, VSD with PS Rare congenital cyanotic heart disease. Aorta arise from RV – receive venous blood – cyanosis. PA arise from LV with PS – less blood through PA – pulmonary oligaemia. VSD with PS – lt to rt shunt – more blood in the RV/Aorta –enlarged aortic knuckle to supply more oxygen to tissue. PS small – child can survive for many month / year – later PAH developed – surgery required. Severe PS – early PAH – early surgery Surgery (Rastelli operation) – 1. A patch in the RV to prevent blood passing from RV to aorta but blood can 50 pass from LV to aorta.
51
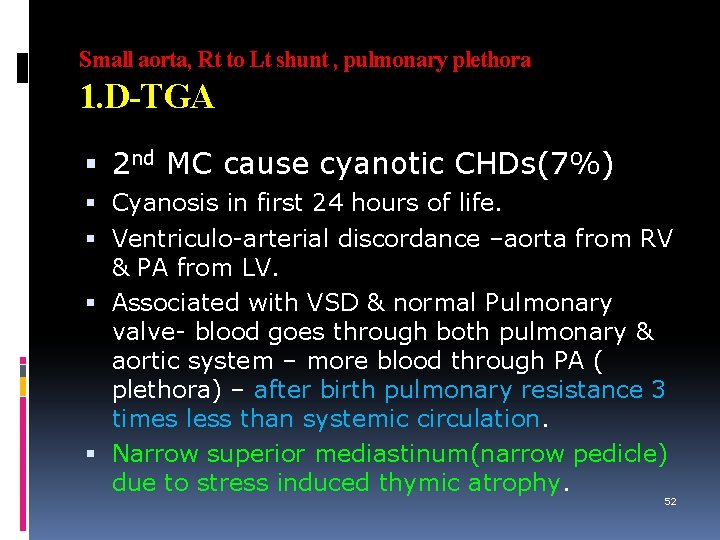
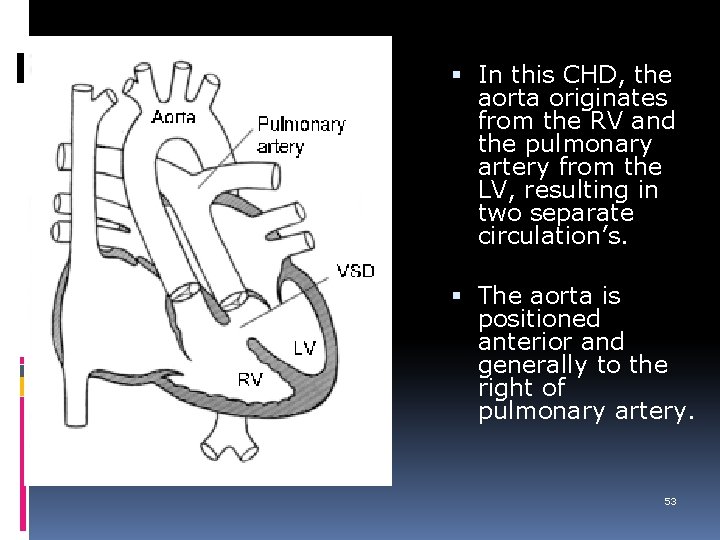
Small aorta, Rt to Lt shunt , pulmonary plethora 1. D-TGA 2 nd MC cause cyanotic CHDs(7%) Cyanosis in first 24 hours of life. Ventriculo-arterial discordance –aorta from RV & PA from LV. Associated with VSD & normal Pulmonary valve- blood goes through both pulmonary & aortic system – more blood through PA ( plethora) – after birth pulmonary resistance 3 times less than systemic circulation. Narrow superior mediastinum(narrow pedicle) due to stress induced thymic atrophy. 52
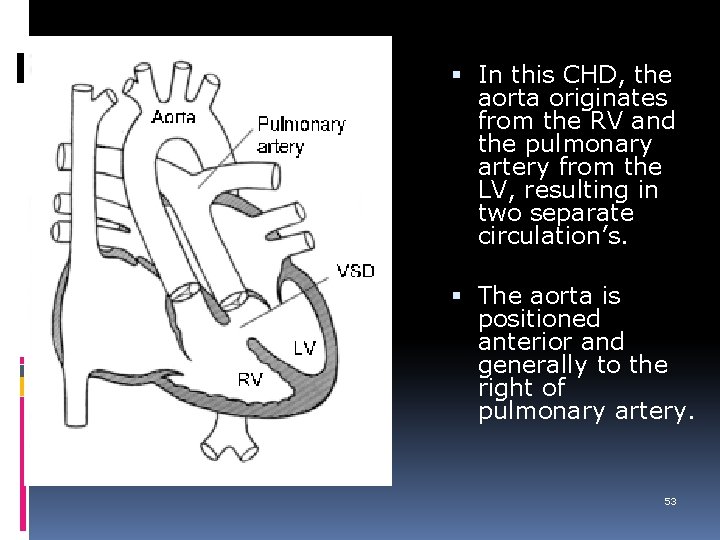
In this CHD, the aorta originates from the RV and the pulmonary artery from the LV, resulting in two separate circulation’s. The aorta is positioned anterior and generally to the right of pulmonary artery. 53
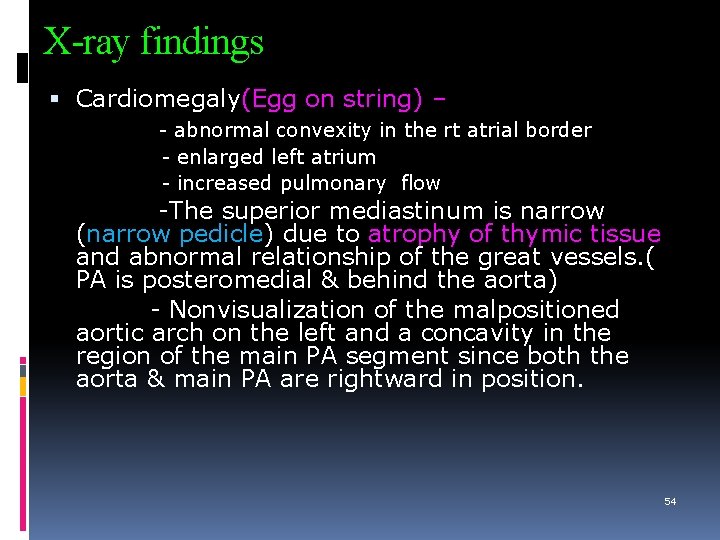
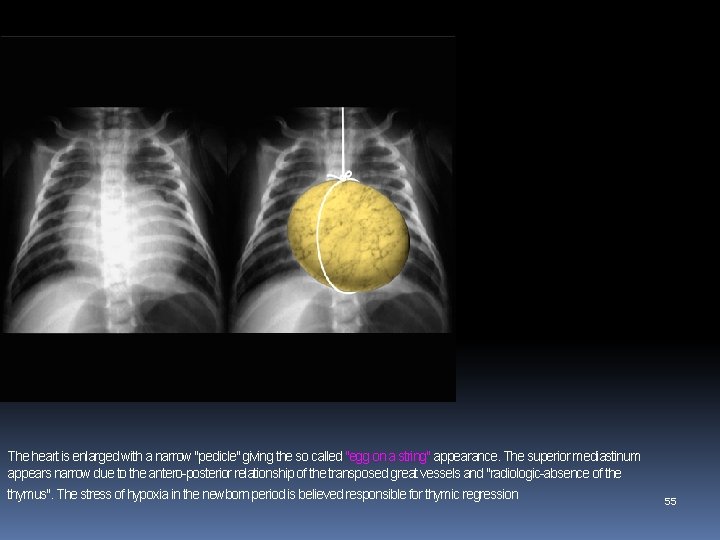
X-ray findings Cardiomegaly(Egg on string) – - abnormal convexity in the rt atrial border - enlarged left atrium - increased pulmonary flow -The superior mediastinum is narrow (narrow pedicle) due to atrophy of thymic tissue and abnormal relationship of the great vessels. ( PA is posteromedial & behind the aorta) - Nonvisualization of the malpositioned aortic arch on the left and a concavity in the region of the main PA segment since both the aorta & main PA are rightward in position. 54
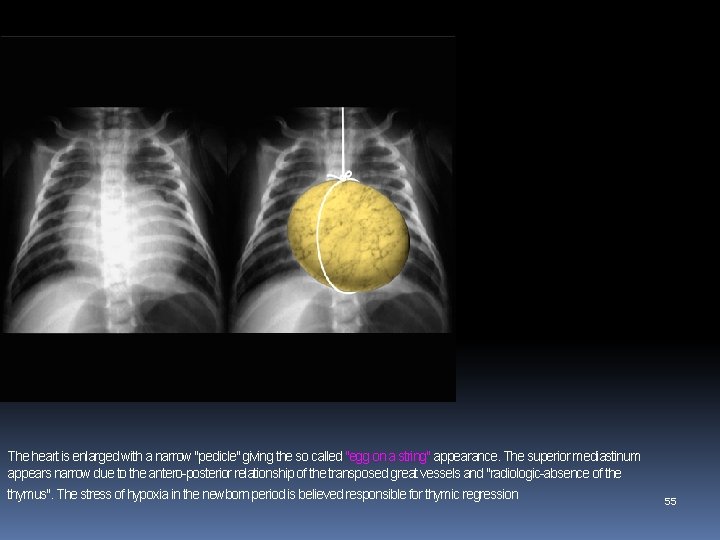
The heart is enlarged with a narrow "pedicle" giving the so called "egg on a string" appearance. The superior mediastinum appears narrow due to the antero-posterior relationship of the transposed great vessels and "radiologic-absence of the thymus". The stress of hypoxia in the newborn period is believed responsible for thymic regression 55
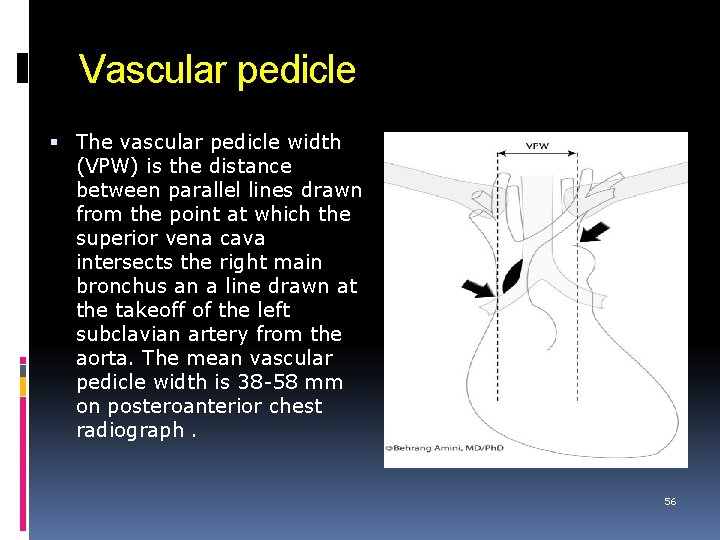
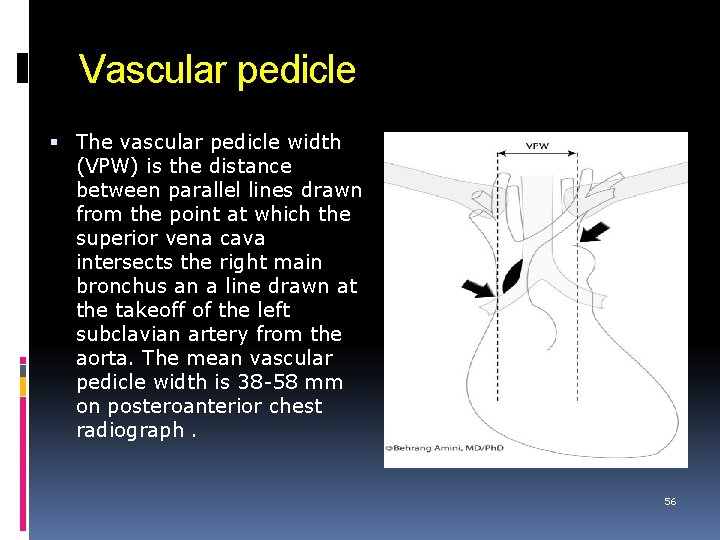
Vascular pedicle The vascular pedicle width (VPW) is the distance between parallel lines drawn from the point at which the superior vena cava intersects the right main bronchus an a line drawn at the takeoff of the left subclavian artery from the aorta. The mean vascular pedicle width is 38 -58 mm on posteroanterior chest radiograph. 56
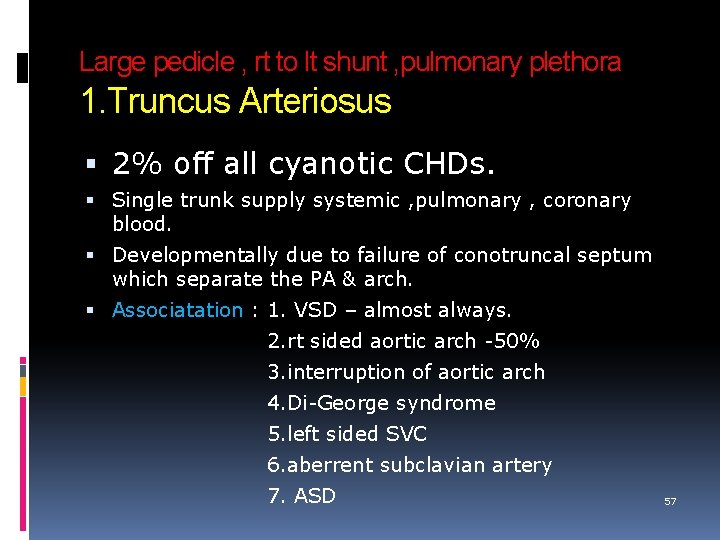
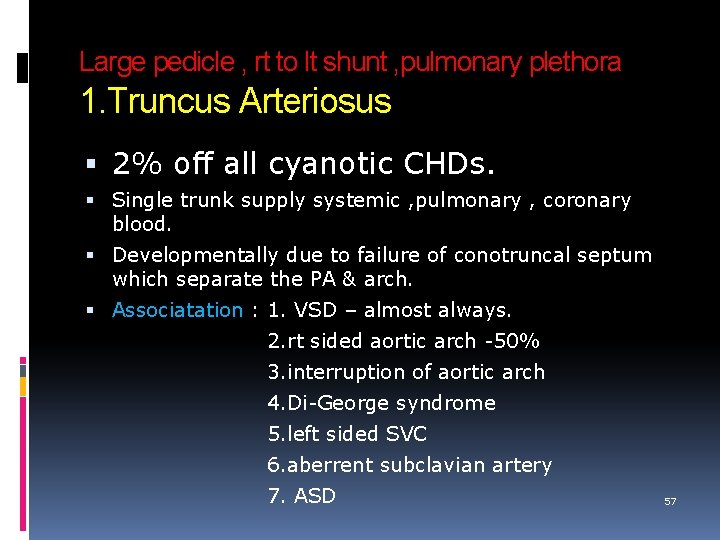
Large pedicle , rt to lt shunt , pulmonary plethora 1. Truncus Arteriosus 2% off all cyanotic CHDs. Single trunk supply systemic , pulmonary , coronary blood. Developmentally due to failure of conotruncal septum which separate the PA & arch. Associatation : 1. VSD – almost always. 2. rt sided aortic arch -50% 3. interruption of aortic arch 4. Di-George syndrome 5. left sided SVC 6. aberrent subclavian artery 7. ASD 57

Truncus Arteriosus cont… Classification: According to origin of pulmonary Artery ( Collett & Edward) Type I: a short main pulmonary artery segment arise from the aorta which then branches into both pulmonary arteries (MC -80%) Type II: both branch pulmonary arteries arise from the posterior common arterial trunk close to each other Type III: the branch pulmonary arteries arise from either side of the truncus and are remote from each other. Type IV: this is considered a form of pulmonary atresia. 58
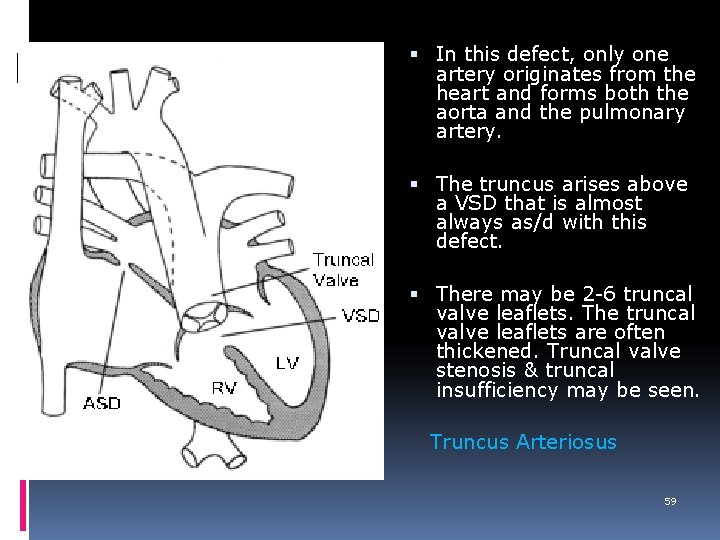
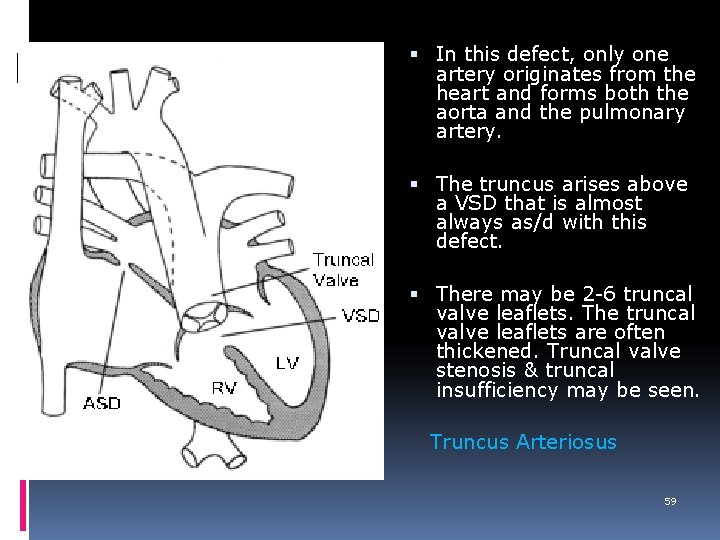
In this defect, only one artery originates from the heart and forms both the aorta and the pulmonary artery. The truncus arises above a VSD that is almost always as/d with this defect. There may be 2 -6 truncal valve leaflets. The truncal valve leaflets are often thickened. Truncal valve stenosis & truncal insufficiency may be seen. Truncus Arteriosus 59
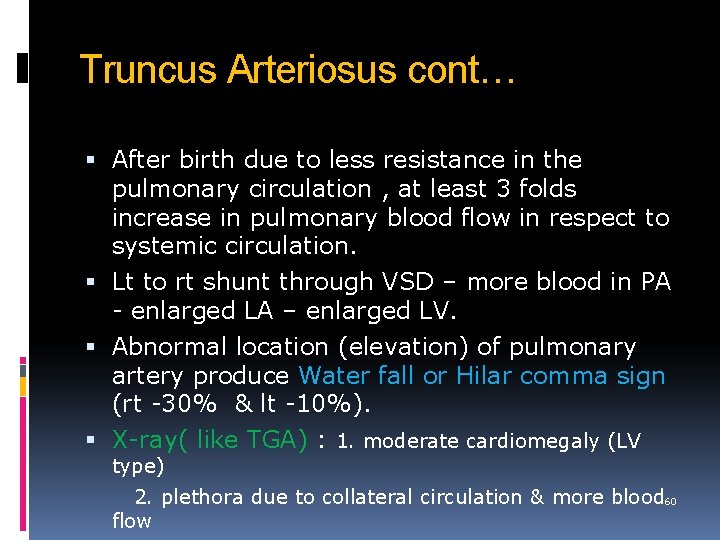
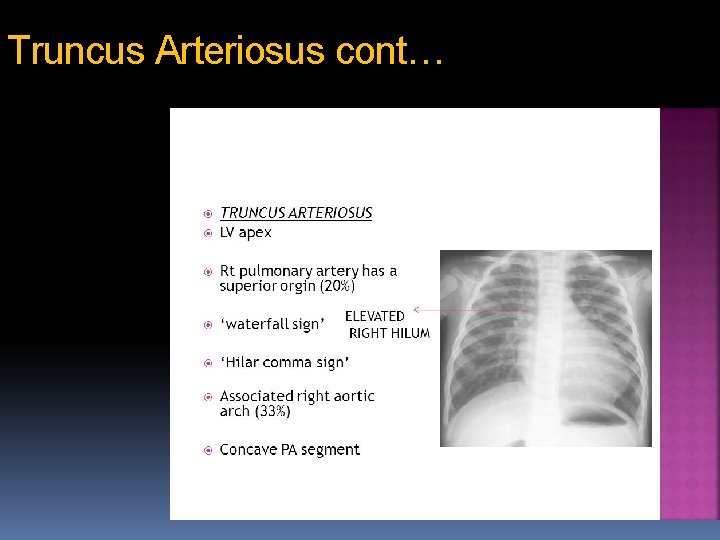
Truncus Arteriosus cont… After birth due to less resistance in the pulmonary circulation , at least 3 folds increase in pulmonary blood flow in respect to systemic circulation. Lt to rt shunt through VSD – more blood in PA - enlarged LA – enlarged LV. Abnormal location (elevation) of pulmonary artery produce Water fall or Hilar comma sign (rt -30% & lt -10%). X-ray( like TGA) : 1. moderate cardiomegaly (LV type) 2. plethora due to collateral circulation & more blood 60 flow
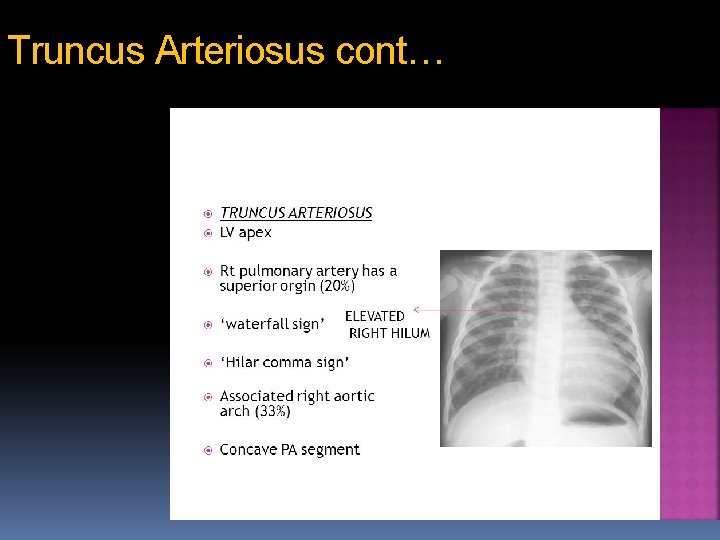
Truncus Arteriosus cont… 61
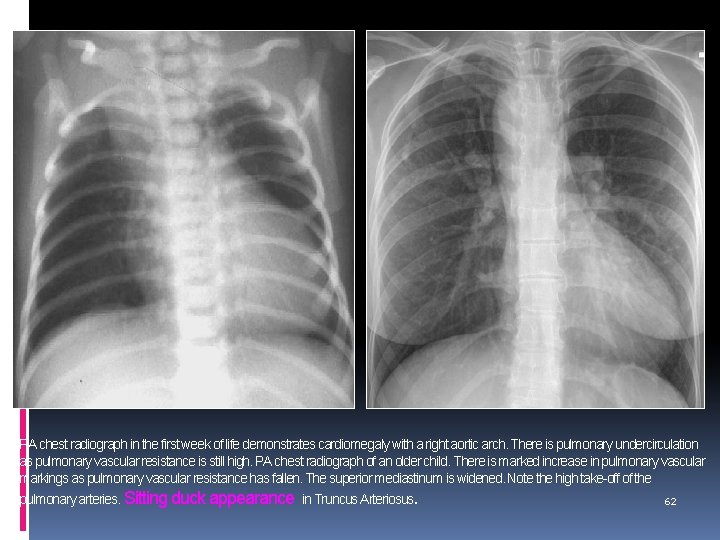
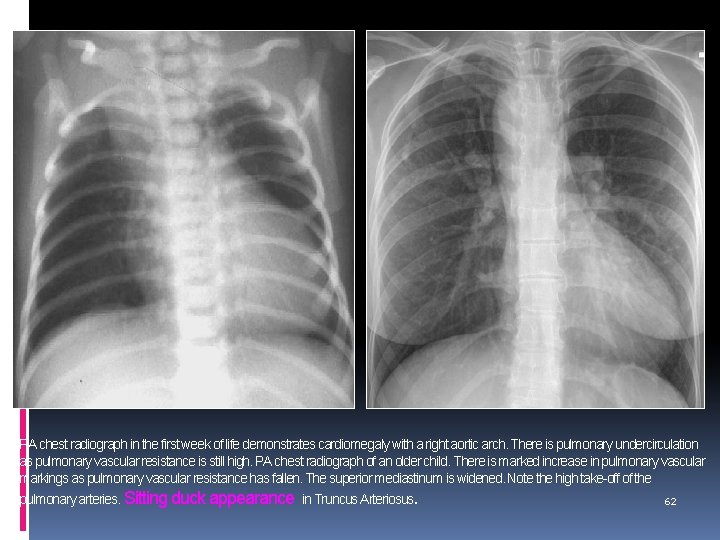
PA chest radiograph in the first week of life demonstrates cardiomegaly with a right aortic arch. There is pulmonary undercirculation as pulmonary vascular resistance is still high. PA chest radiograph of an older child. There is marked increase in pulmonary vascular markings as pulmonary vascular resistance has fallen. The superior mediastinum is widened. Note the high take-off of the pulmonary arteries. Sitting duck appearance in Truncus Arteriosus. 62
Large pedicle , rt to lt shunt , pulmonary plethora 2. TAPVC Congenital cyanotic heart disease with abnormal drainage of pulmonary venous system. All systemic & pulmonary vein drain into RA , nothing drain into LA – small LA. For survival rt to lt shunt through mostly by patent foramen ovale / less commonly by ASD. 63
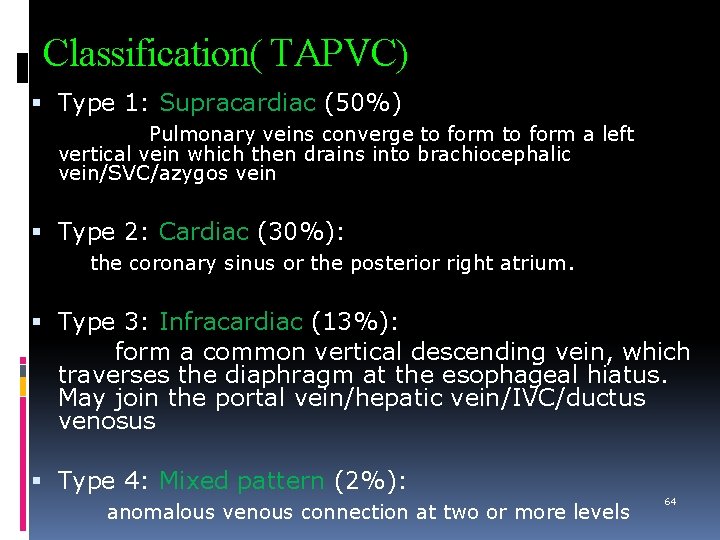
Classification( TAPVC) Type 1: Supracardiac (50%) Pulmonary veins converge to form a left vertical vein which then drains into brachiocephalic vein/SVC/azygos vein Type 2: Cardiac (30%): the coronary sinus or the posterior right atrium. Type 3: Infracardiac (13%): form a common vertical descending vein, which traverses the diaphragm at the esophageal hiatus. May join the portal vein/hepatic vein/IVC/ductus venosus Type 4: Mixed pattern (2%): 64 anomalous venous connection at two or more levels
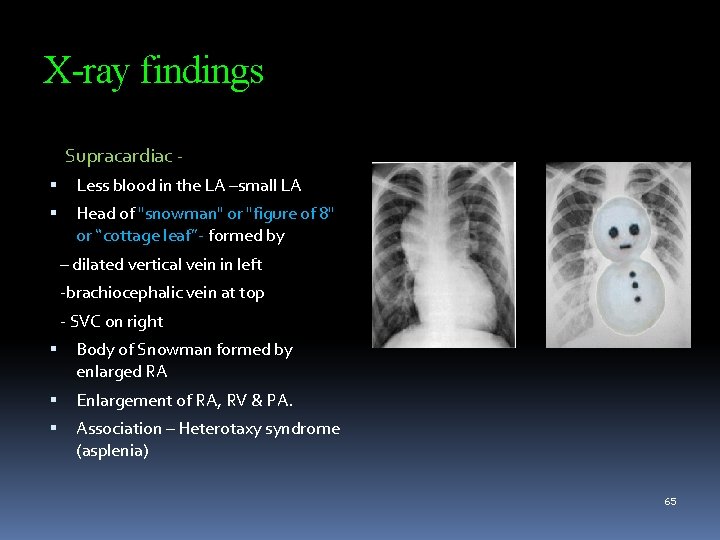
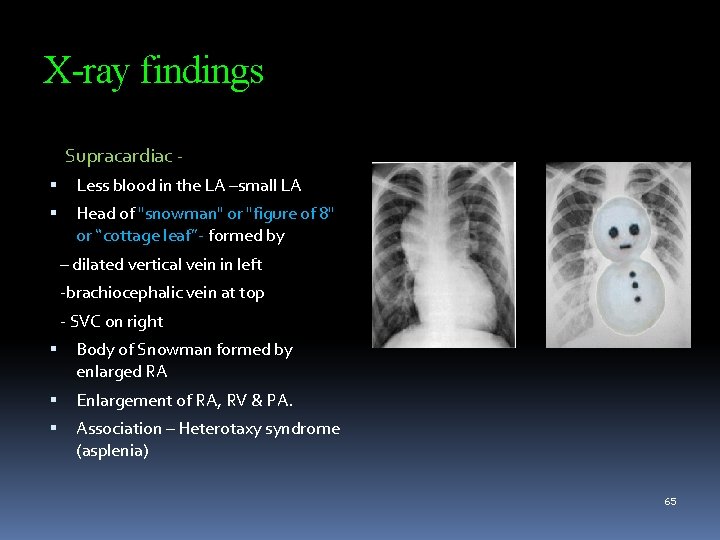
X-ray findings Supracardiac Less blood in the LA –small LA Head of "snowman" or "figure of 8" or “cottage leaf”- formed by – dilated vertical vein in left -brachiocephalic vein at top - SVC on right Body of Snowman formed by enlarged RA Enlargement of RA, RV & PA. Association – Heterotaxy syndrome (asplenia) 65
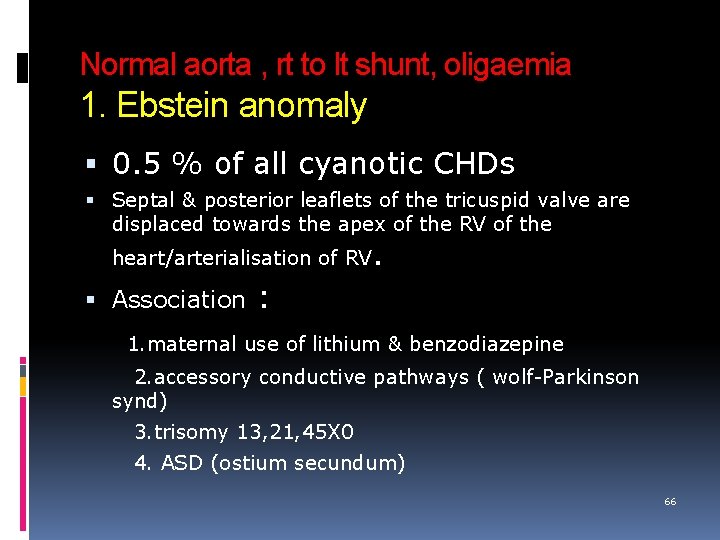
Normal aorta , rt to lt shunt, oligaemia 1. Ebstein anomaly 0. 5 % of all cyanotic CHDs Septal & posterior leaflets of the tricuspid valve are displaced towards the apex of the RV of the heart/arterialisation of RV. Association : 1. maternal use of lithium & benzodiazepine 2. accessory conductive pathways ( wolf-Parkinson synd) 3. trisomy 13, 21, 45 X 0 4. ASD (ostium secundum) 66
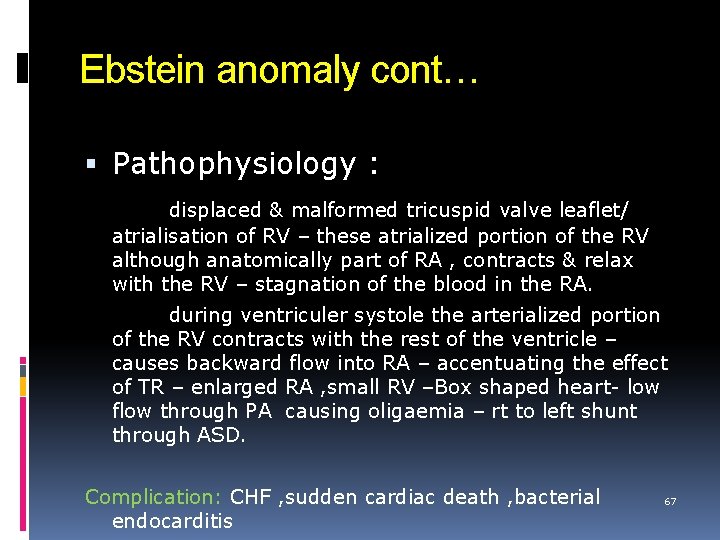
Ebstein anomaly cont… Pathophysiology : displaced & malformed tricuspid valve leaflet/ atrialisation of RV – these atrialized portion of the RV although anatomically part of RA , contracts & relax with the RV – stagnation of the blood in the RA. during ventriculer systole the arterialized portion of the RV contracts with the rest of the ventricle – causes backward flow into RA – accentuating the effect of TR – enlarged RA , small RV –Box shaped heart- low flow through PA causing oligaemia – rt to left shunt through ASD. Complication: CHF , sudden cardiac death , bacterial endocarditis 67
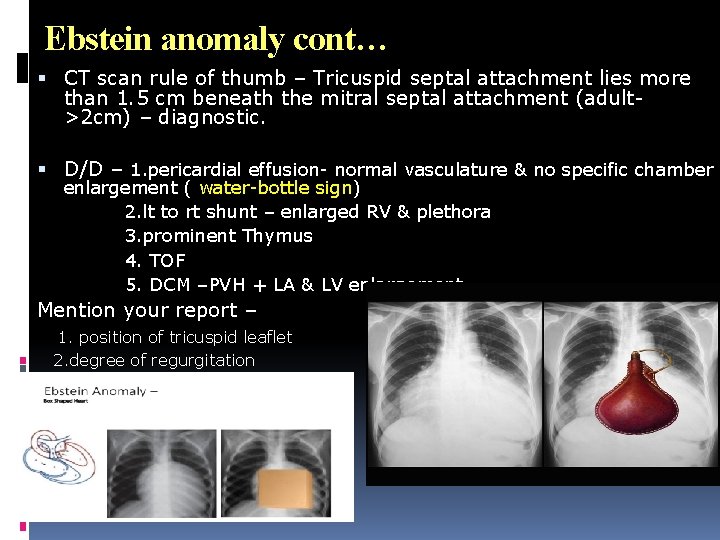
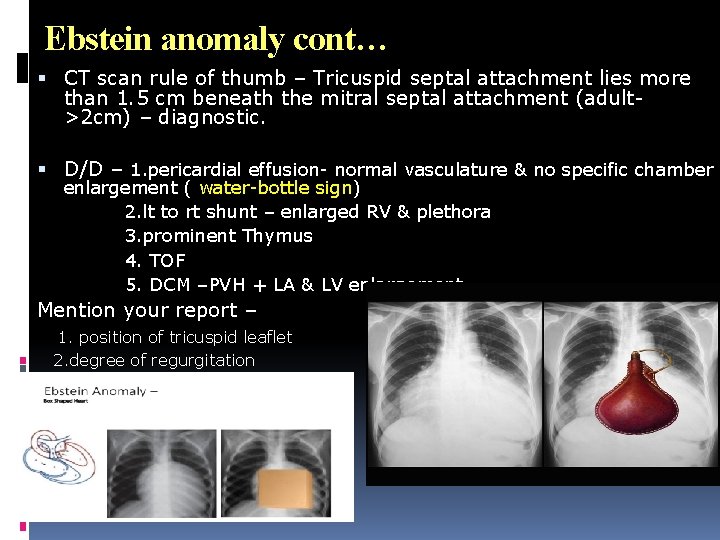
Ebstein anomaly cont… CT scan rule of thumb – Tricuspid septal attachment lies more than 1. 5 cm beneath the mitral septal attachment (adult- >2 cm) – diagnostic. D/D – 1. pericardial effusion- normal vasculature & no specific chamber enlargement ( water-bottle sign) 2. lt to rt shunt – enlarged RV & plethora 3. prominent Thymus 4. TOF 5. DCM –PVH + LA & LV enlargement Mention your report – 1. position of tricuspid leaflet 2. degree of regurgitation 3. RV volume & function 68
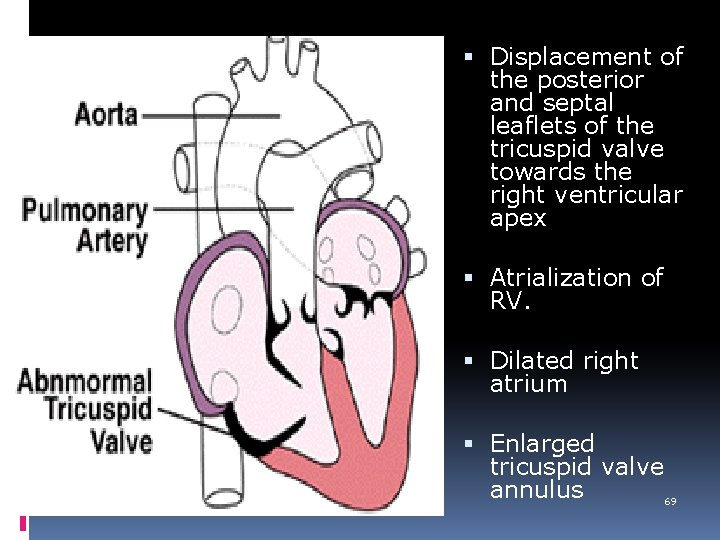
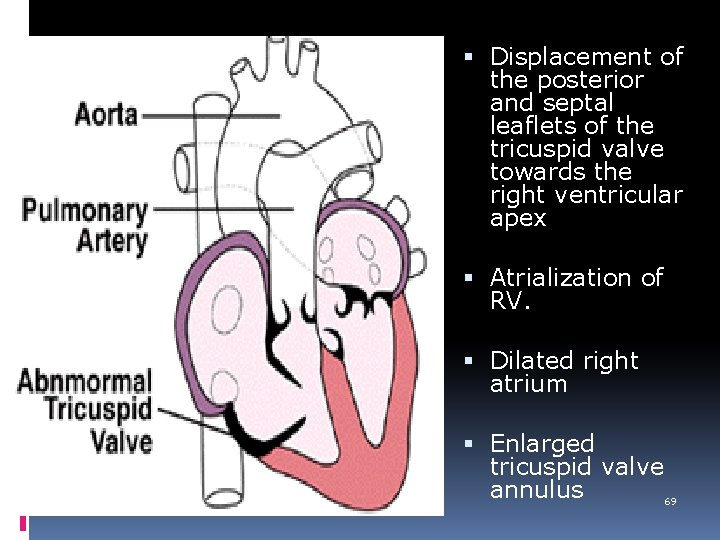
Displacement of the posterior and septal leaflets of the tricuspid valve towards the right ventricular apex Atrialization of RV. Dilated right atrium Enlarged tricuspid valve annulus 69
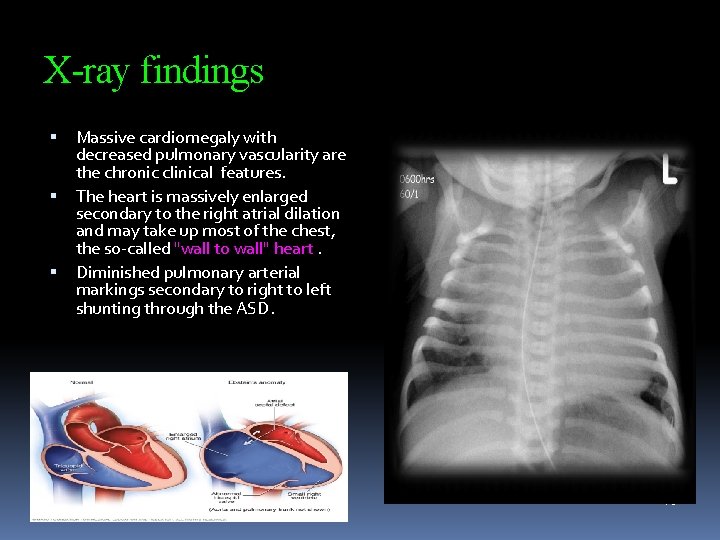
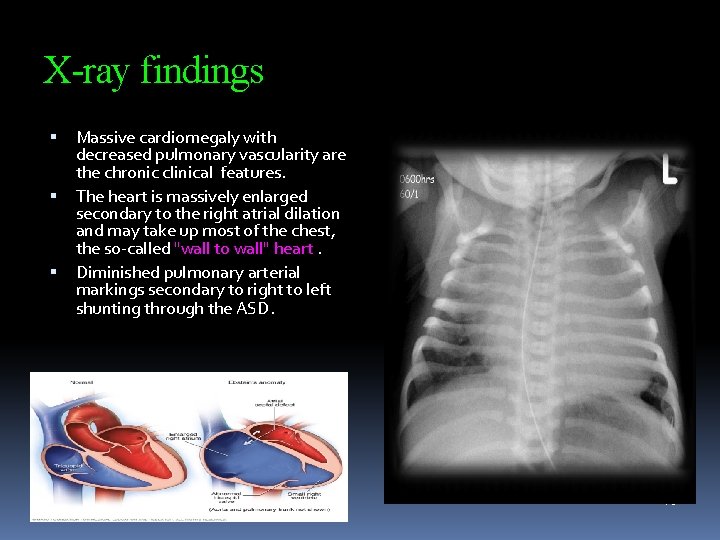
X-ray findings Massive cardiomegaly with decreased pulmonary vascularity are the chronic clinical features. The heart is massively enlarged secondary to the right atrial dilation and may take up most of the chest, the so-called "wall to wall" heart. Diminished pulmonary arterial markings secondary to right to left shunting through the ASD. 70
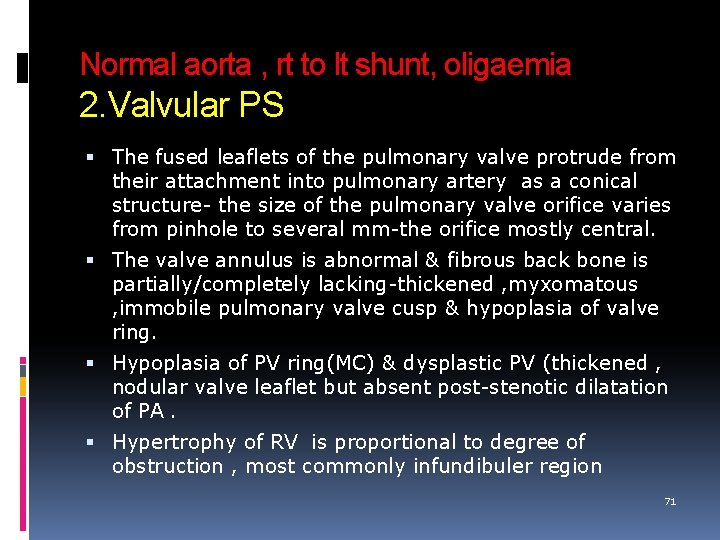
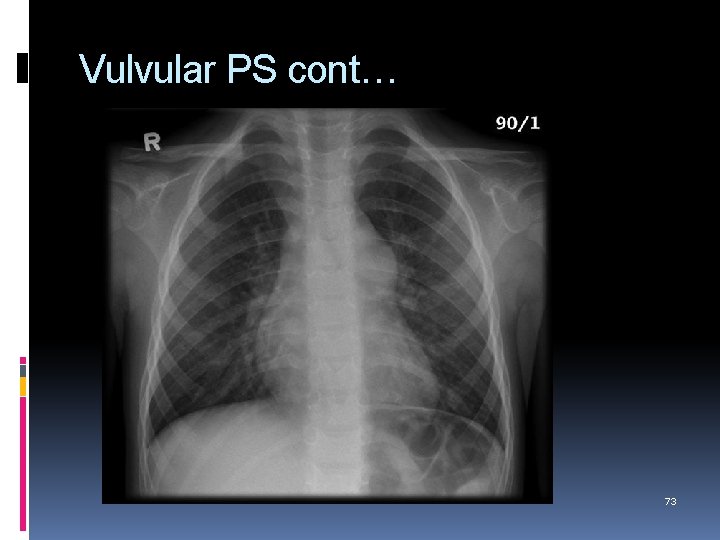
Normal aorta , rt to lt shunt, oligaemia 2. Valvular PS The fused leaflets of the pulmonary valve protrude from their attachment into pulmonary artery as a conical structure- the size of the pulmonary valve orifice varies from pinhole to several mm-the orifice mostly central. The valve annulus is abnormal & fibrous back bone is partially/completely lacking-thickened , myxomatous , immobile pulmonary valve cusp & hypoplasia of valve ring. Hypoplasia of PV ring(MC) & dysplastic PV (thickened , nodular valve leaflet but absent post-stenotic dilatation of PA. Hypertrophy of RV is proportional to degree of obstruction , most commonly infundibuler region 71
Valvular PS cont… RV dilated from mild to severe – RA enlargedrt to lt shunt through ASD/ Foramen ovale – LA, LV enlargement & cyanosis. The main PA is dilated due to high velocity jet after stenosis –peripheral oligaemia. Association : 1. ASD/ patent foramen ovale 2. Noonan syndrome 3. Turner syndrome 4. supravalvular PS-rubella & Williams 5. isolated 72
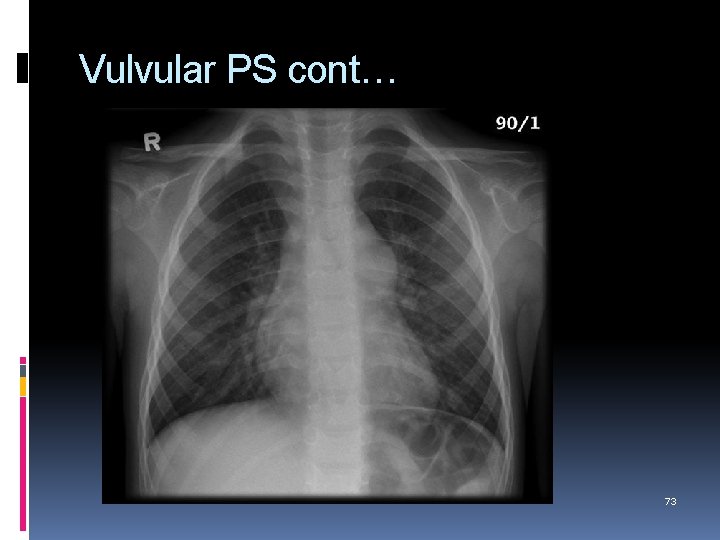
Vulvular PS cont… 73
Acyanotic with normal vascularity Coarctation of Aorta 5 -8% of all CHDs. Increased predisposition in girls with Turner’s syndrome (15 -20%). Adult/juxtaductal - short segment abrupt obstruction in the postductal region secondary to localized thickening of the aortic media. This typically occurs just distal to the ductus arteriosus. Infantile /preductal -diffuse narrowing or hypoplasia of the aorta just distal to brachiocephalic/innominate artery & proximal to the level of ductus but distal to origin of left subclavian artery. - blood supply to descending aorta through PDA Presentation- leg claudication , femoral pulse, pressure diff Associated anomalies : Bicuspid aortic valve (in up to 85%) 74 , VSD, Mitral valve lesions, truncus arteriosus and TGA
Coarctation cont… Rib notching: - mostly over 20 years age & rare < 5 years. -due to narrowing high flow noted proximal to this through subclavian artery- in long standing cases more blood passes through internal mammary artery , responsible formation of collateral in the intercostals region with intercostals branch of descending thoracic aorta causing rib notching (3 rd- 9 th rib) –bypass coarctation & supply descending thoracic aorta. - rib notching absent at 1 st-2 nd rib as these artery arise from directly from costocervical trunk & no intercostals artery drain in the descending thoracic aorta 75
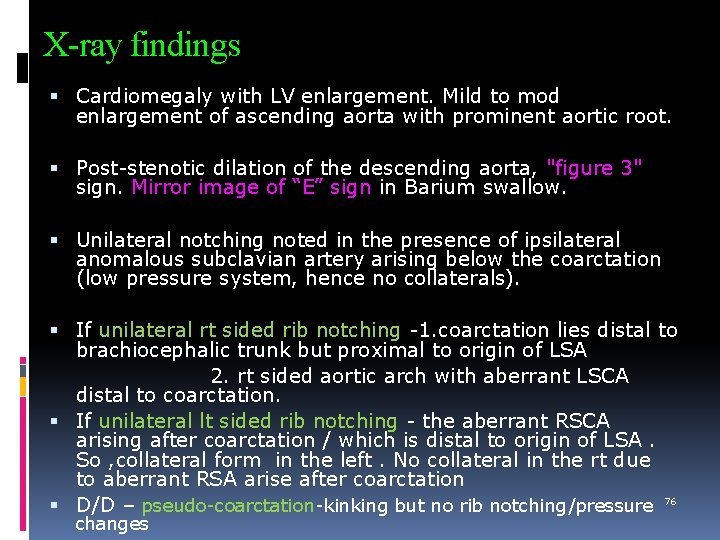
X-ray findings Cardiomegaly with LV enlargement. Mild to mod enlargement of ascending aorta with prominent aortic root. Post-stenotic dilation of the descending aorta, "figure 3" sign. Mirror image of “E” sign in Barium swallow. Unilateral notching noted in the presence of ipsilateral anomalous subclavian artery arising below the coarctation (low pressure system, hence no collaterals). If unilateral rt sided rib notching -1. coarctation lies distal to brachiocephalic trunk but proximal to origin of LSA 2. rt sided aortic arch with aberrant LSCA distal to coarctation. If unilateral lt sided rib notching - the aberrant RSCA arising after coarctation / which is distal to origin of LSA. So , collateral form in the left. No collateral in the rt due to aberrant RSA arise after coarctation D/D – pseudo-coarctation-kinking but no rib notching/pressure 76 changes
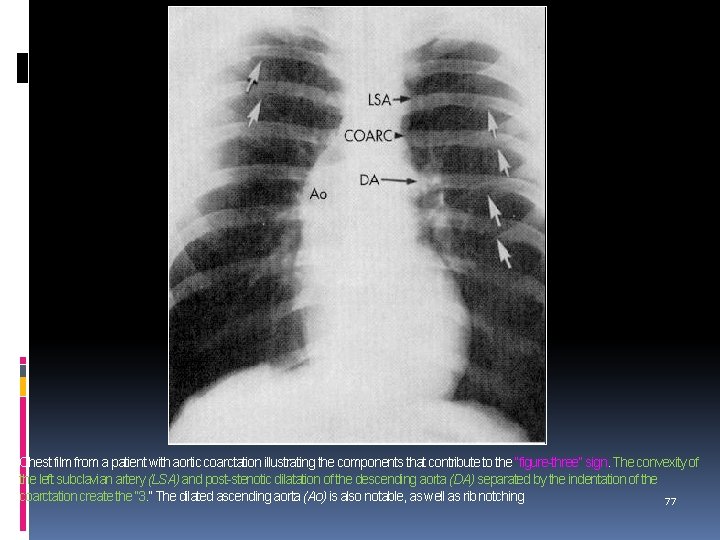
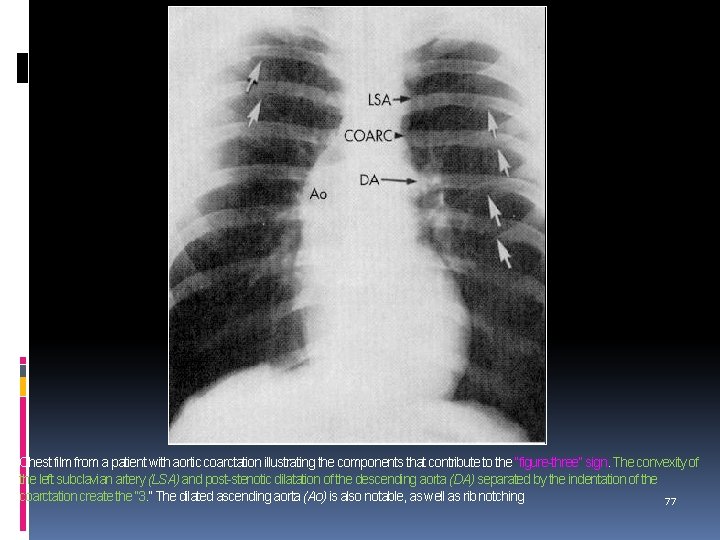
Chest film from a patient with aortic coarctation illustrating the components that contribute to the “figure-three” sign. The convexity of the left subclavian artery (LSA) and post-stenotic dilatation of the descending aorta (DA) separated by the indentation of the coarctation create the “ 3. ” The dilated ascending aorta (Ao) is also notable, as well as rib notching 77
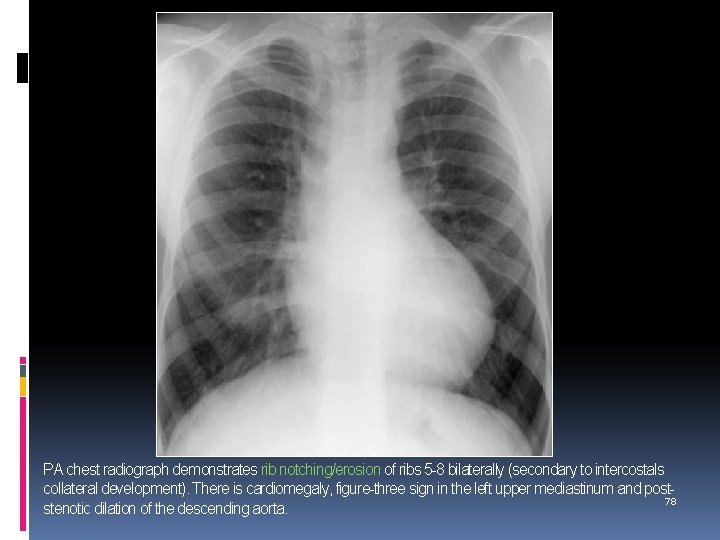
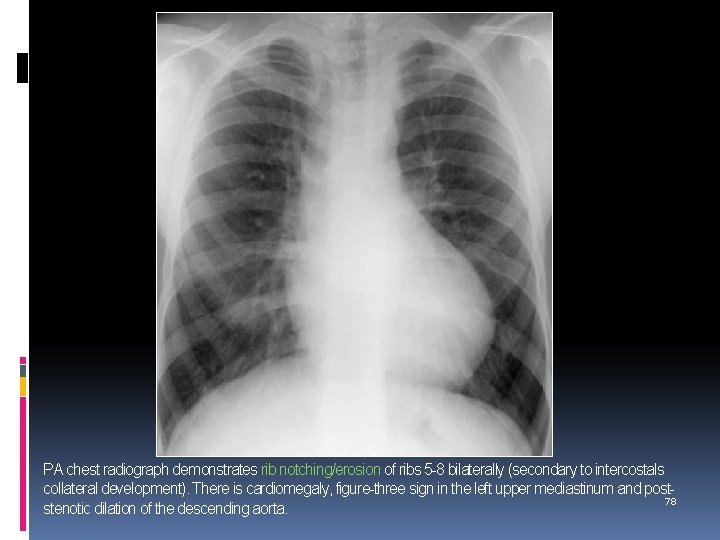
PA chest radiograph demonstrates rib notching/erosion of ribs 5 -8 bilaterally (secondary to intercostals collateral development). There is cardiomegaly, figure-three sign in the left upper mediastinum and post 78 stenotic dilation of the descending aorta.

Aortogram from a patient with coarctation. The coarctation is well visualized (upper arrow) beyond the origin of the left subclavian artery. A bicuspid aortic valve is also present (lower arrow) with a faint blush of aortic regurgitation (arrows) 79
Double aortic arch It is characterized by the persistence of both embryonic aortic arches. Each arch gives rise to an ipsilateral carotid and subclavian artery and there is no innominate artery. The ascending aorta divides into each arch anterior to the trachea and then form a common descending aorta completing a vascular ring, which encircles both the trachea and esophagus. The ductus arteriosus usually arises from the left-sided arch. Usually the right arch is dominant. The descending aorta is usually on the side of the spine opposite to the dominant arch. Associated anomalies : TOF, TGA, VSD Or ASD. 80
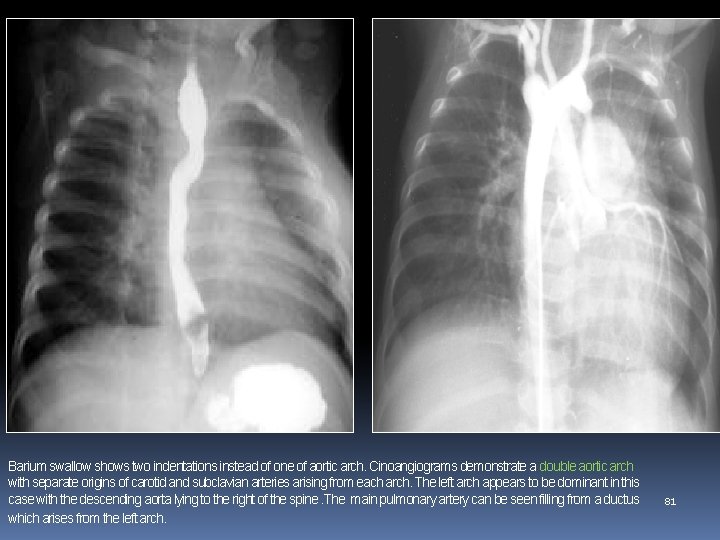
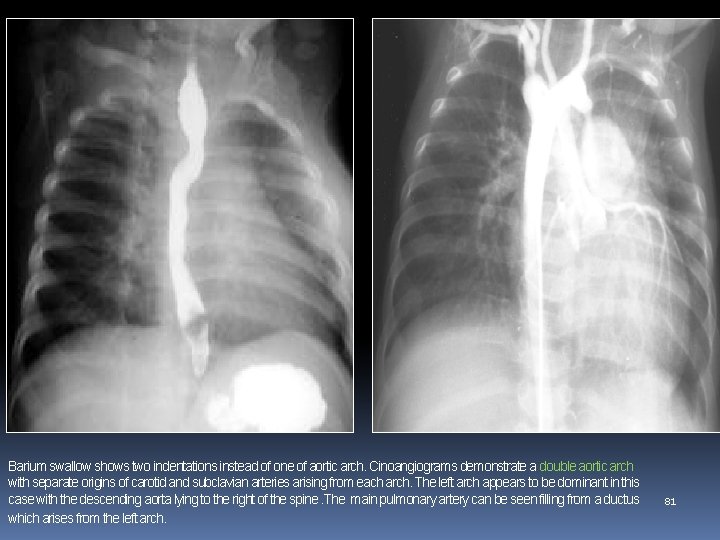
Barium swallow shows two indentations instead of one of aortic arch. Cinoangiograms demonstrate a double aortic arch with separate origins of carotid and subclavian arteries arising from each arch. The left arch appears to be dominant in this case with the descending aorta lying to the right of the spine. The main pulmonary artery can be seen filling from a ductus which arises from the left arch. 81
Corrected transposition/ventricular inversion, L-TGA This is characterised by atrioventicular discordance and ventriculoarterial discordance Hence the left atrium connects to the right ventricle which connects to the aorta. Associated anomalies: VSD (80%), PS (50%)’ Dextrocardia (25%) & AV valve abnormalities X-ray: the upper left heart border is straightened as a result of leftward displacement of the aorta. 82
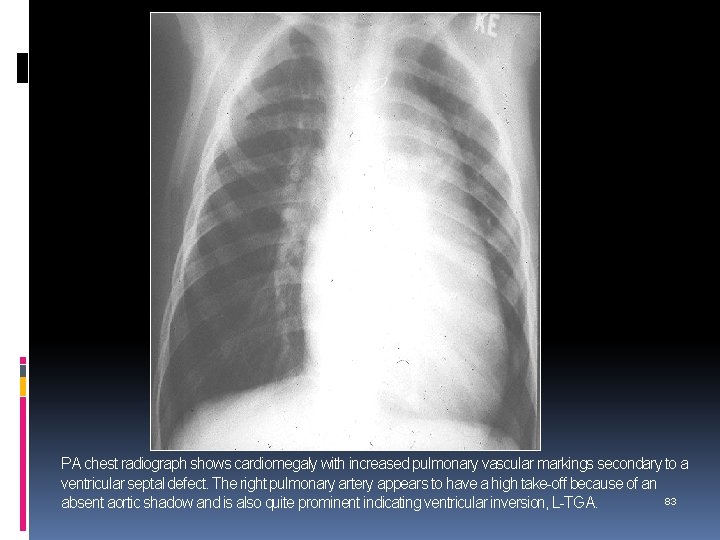
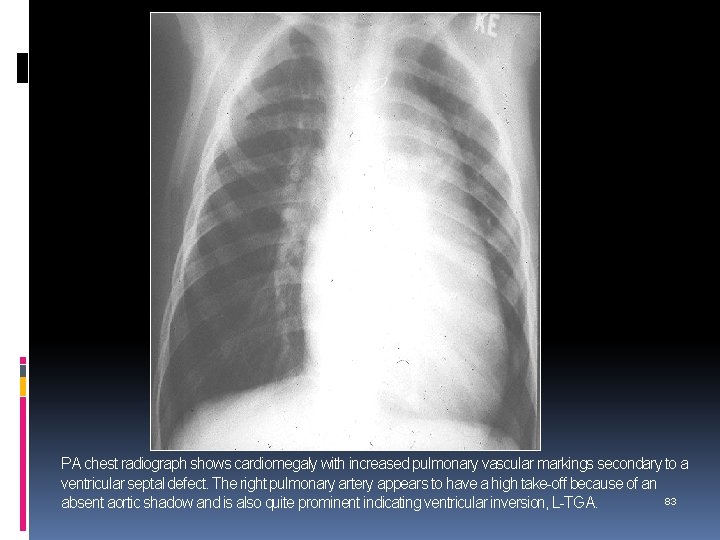
PA chest radiograph shows cardiomegaly with increased pulmonary vascular markings secondary to a ventricular septal defect. The right pulmonary artery appears to have a high take-off because of an 83 absent aortic shadow and is also quite prominent indicating ventricular inversion, L-TGA.
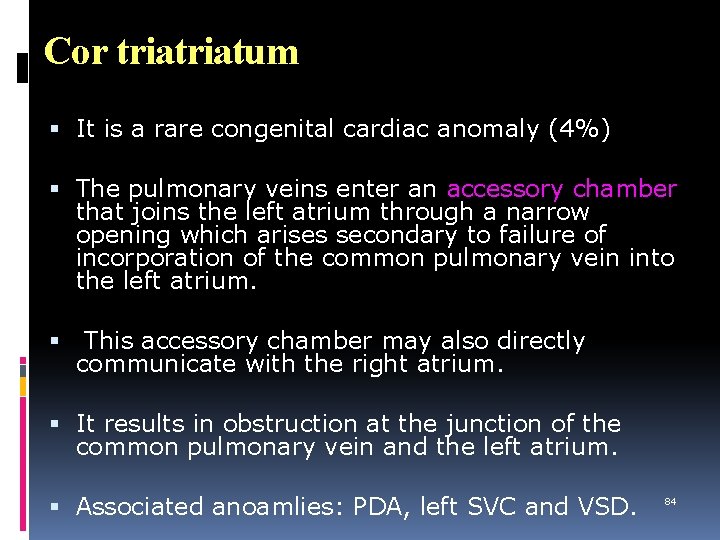
Cor triatum It is a rare congenital cardiac anomaly (4%) The pulmonary veins enter an accessory chamber that joins the left atrium through a narrow opening which arises secondary to failure of incorporation of the common pulmonary vein into the left atrium. This accessory chamber may also directly communicate with the right atrium. It results in obstruction at the junction of the common pulmonary vein and the left atrium. Associated anoamlies: PDA, left SVC and VSD. 84
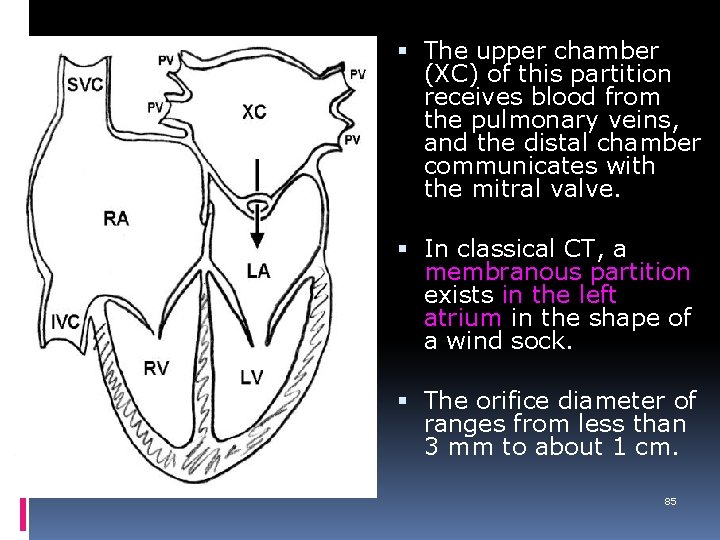
The upper chamber (XC) of this partition receives blood from the pulmonary veins, and the distal chamber communicates with the mitral valve. In classical CT, a membranous partition exists in the left atrium in the shape of a wind sock. The orifice diameter of ranges from less than 3 mm to about 1 cm. 85
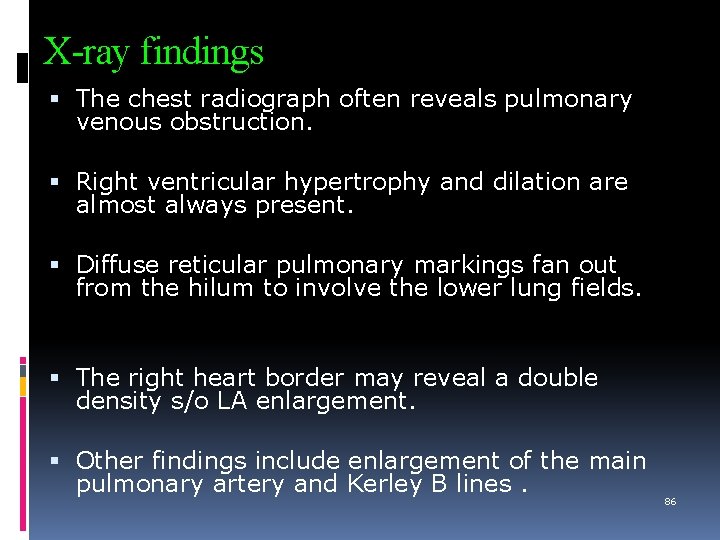
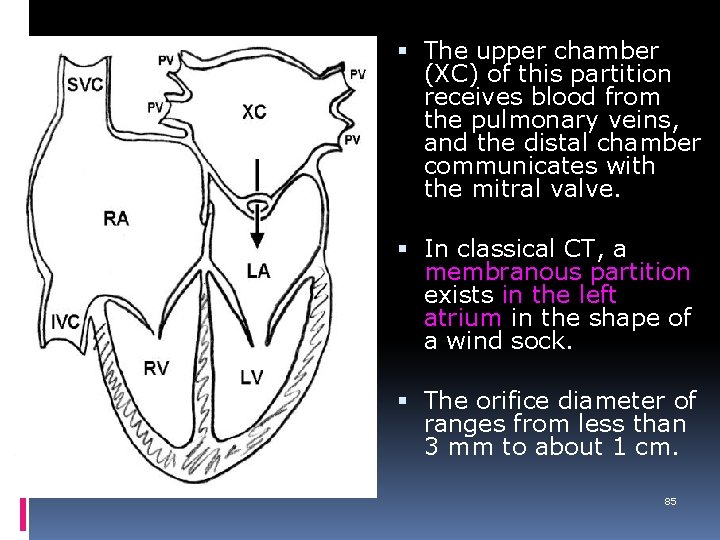
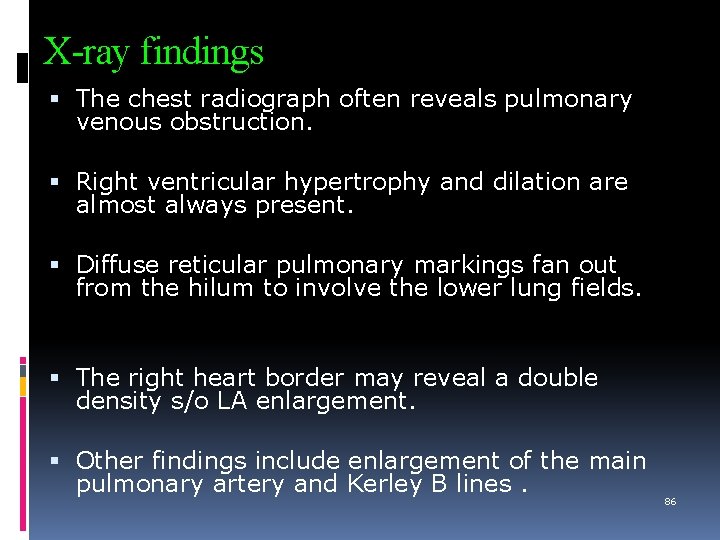
X-ray findings The chest radiograph often reveals pulmonary venous obstruction. Right ventricular hypertrophy and dilation are almost always present. Diffuse reticular pulmonary markings fan out from the hilum to involve the lower lung fields. The right heart border may reveal a double density s/o LA enlargement. Other findings include enlargement of the main pulmonary artery and Kerley B lines. 86
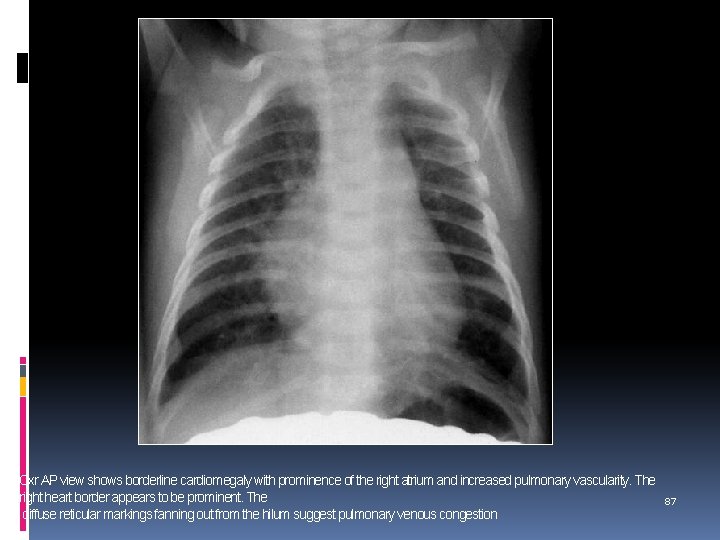
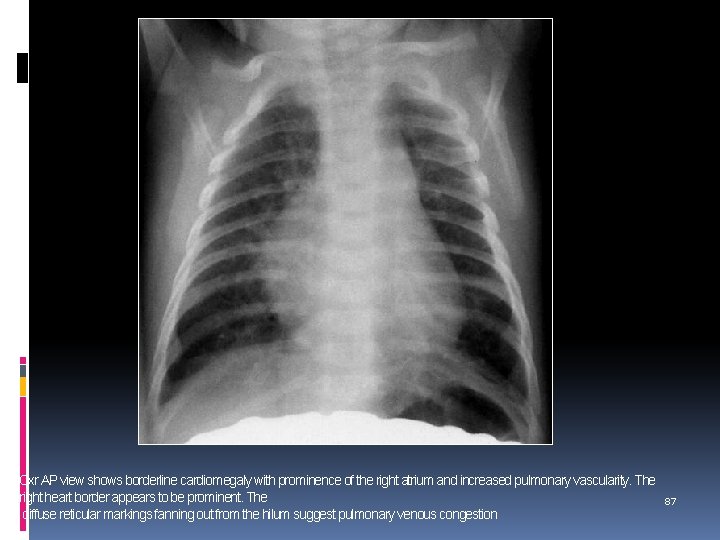
Cxr AP view shows borderline cardiomegaly with prominence of the right atrium and increased pulmonary vascularity. The right heart border appears to be prominent. The diffuse reticular markings fanning out from the hilum suggest pulmonary venous congestion 87
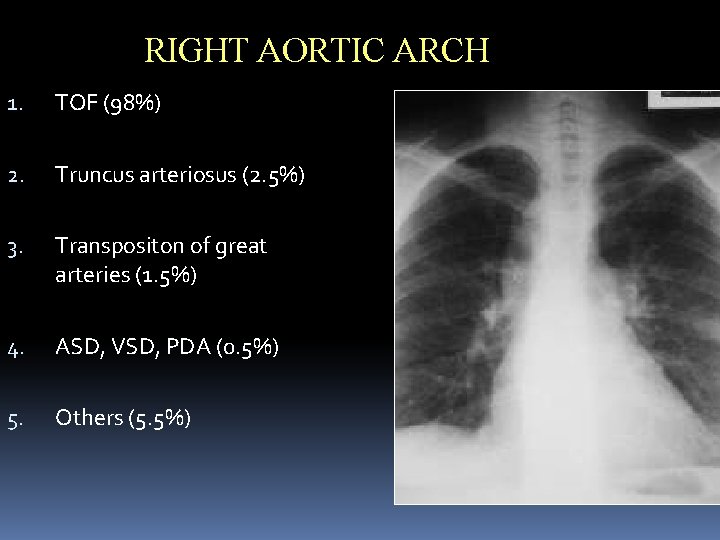
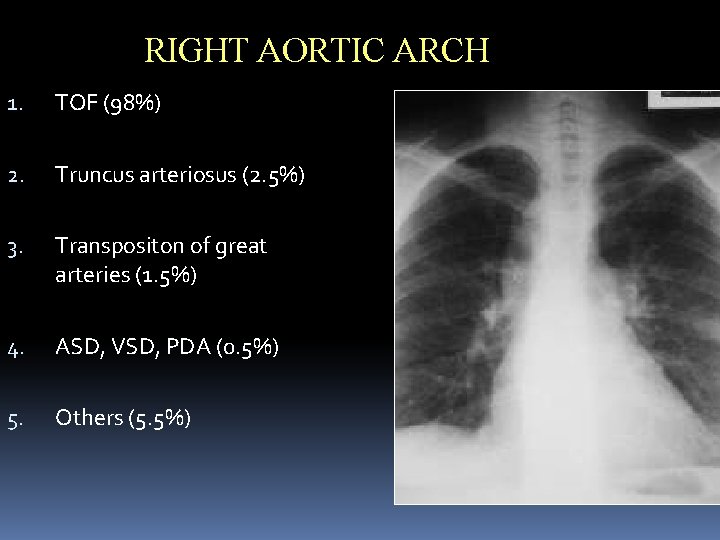
RIGHT AORTIC ARCH 1. TOF (98%) 2. Truncus arteriosus (2. 5%) 3. Transpositon of great arteries (1. 5%) 4. ASD, VSD, PDA (0. 5%) 5. Others (5. 5%) 88
Various shapes of heart Boot shaped - TOF, TA Egg shaped – TGA Figure of 8 / snowman app. – TAPVC Box shaped – Ebstein’s anomaly Water bottle – Pericardial effusion 89
Sitting duck app. – Truncus arteriosus Armoured heart – calcified pericardium Tear drop / strap like heart – Emphysema Quadrilateral heart – supine Xray Pancake heart – straight back synd. (compressed b/w sternum & vertebral column) 90
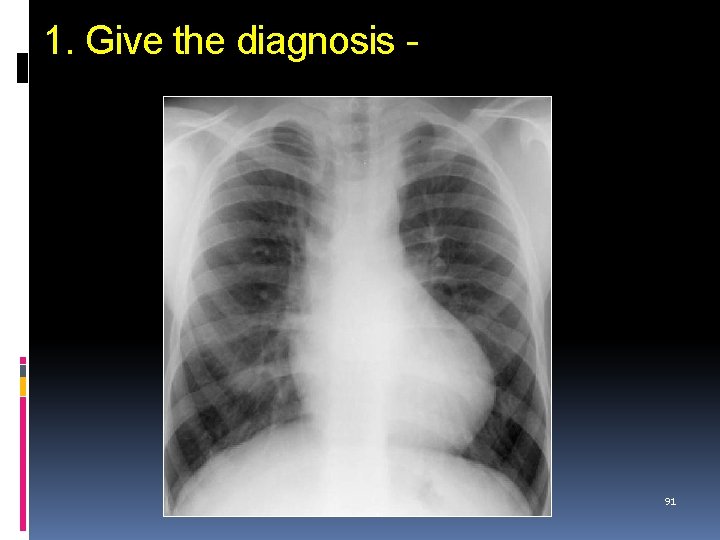
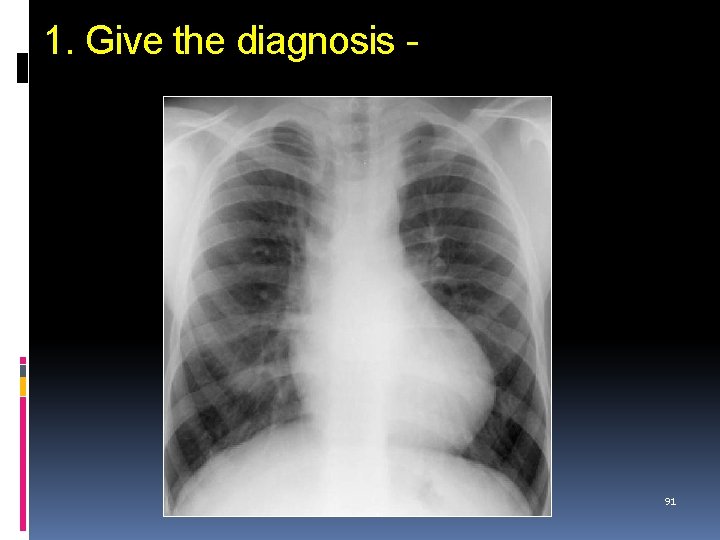
1. Give the diagnosis - 91
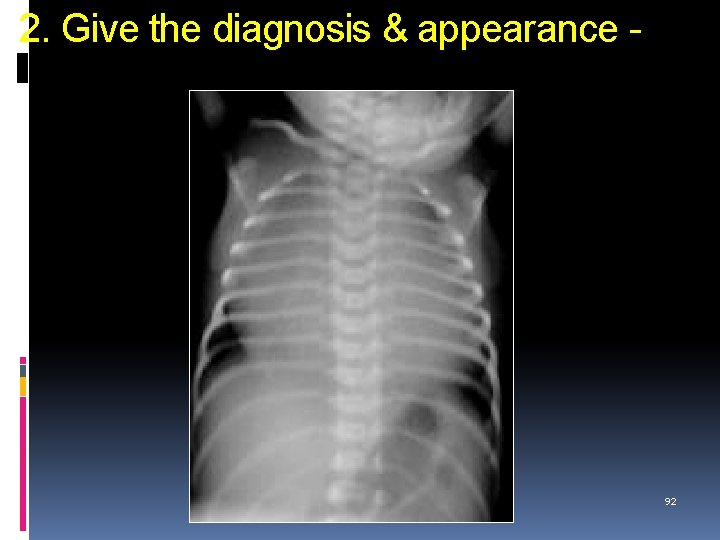
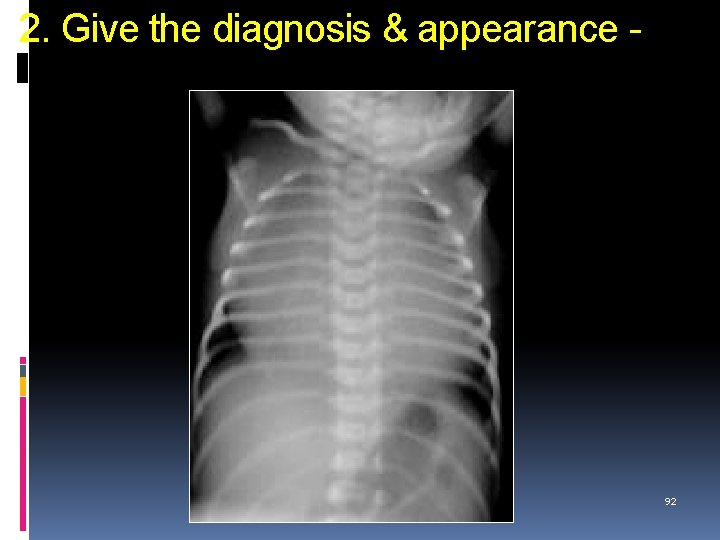
2. Give the diagnosis & appearance - 92
3. “Snowman” appearance of heart seen in- 93
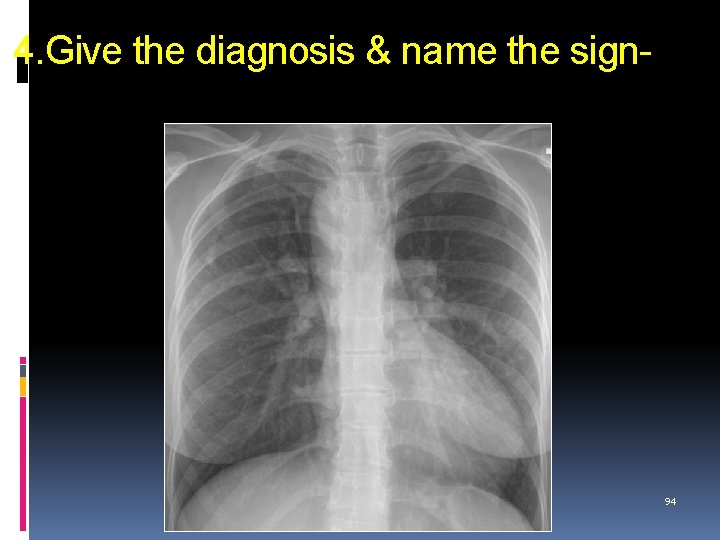
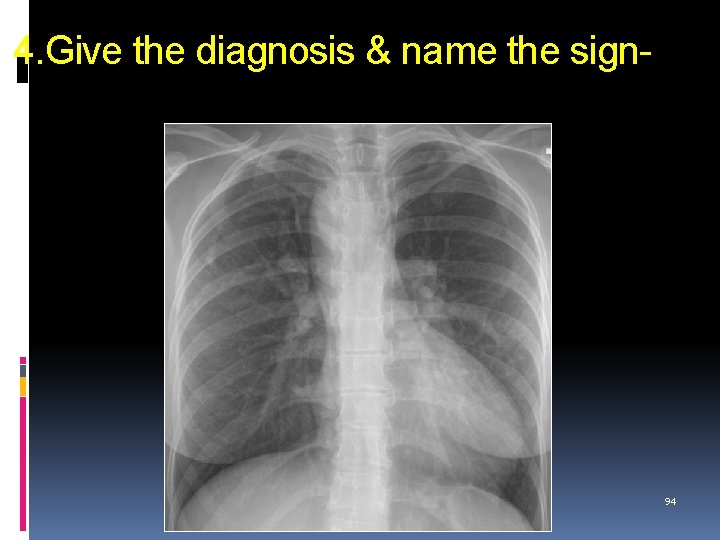
4. Give the diagnosis & name the sign- 94
95
 Communicable disease and non communicable disease
Communicable disease and non communicable disease Heart disease symptoms
Heart disease symptoms Pico question examples heart disease
Pico question examples heart disease Cyanotic congenital heart disease
Cyanotic congenital heart disease Footbal tatto
Footbal tatto 5 cyanotic congenital heart disease
5 cyanotic congenital heart disease Tga cxr
Tga cxr Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy Heart disease data
Heart disease data Ie
Ie Mitral regurgitation symptoms
Mitral regurgitation symptoms Lvvo heart
Lvvo heart Terrible t's cyanotic heart disease
Terrible t's cyanotic heart disease Causes of valvular heart disease
Causes of valvular heart disease Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Dopamine uses
Dopamine uses Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Causes of valvular heart disease
Causes of valvular heart disease Rheumatic heart disease
Rheumatic heart disease Causes of valvular heart disease
Causes of valvular heart disease Farah garmany
Farah garmany Fish mouth or buttonhole stenosis
Fish mouth or buttonhole stenosis Rhumatic fever criteria
Rhumatic fever criteria Coronary heart disease
Coronary heart disease Chronic coronary syndrome
Chronic coronary syndrome Rheumatic heart disease
Rheumatic heart disease Rheumatic heart disease causes
Rheumatic heart disease causes Heart disease
Heart disease Pac ecg
Pac ecg Nyha classification of heart disease
Nyha classification of heart disease Heart disease and stroke are the world's biggest killers
Heart disease and stroke are the world's biggest killers Chronic rheumatic heart disease
Chronic rheumatic heart disease Diploetic
Diploetic Purpose of lead foil sheet in the film packet
Purpose of lead foil sheet in the film packet Kub xray
Kub xray Xray xml editor
Xray xml editor Sza xray
Sza xray Jfk jr plane crash photos
Jfk jr plane crash photos Mary beth sanders
Mary beth sanders Rickets xray
Rickets xray Cvs x ray
Cvs x ray Lefort 3
Lefort 3 Occipito-frontal
Occipito-frontal Xray technique chart
Xray technique chart Emulsion peel in radiography
Emulsion peel in radiography X ray circuit diagram
X ray circuit diagram Xray lara
Xray lara Artifact
Artifact Spectrum xray
Spectrum xray Air under diaphragm
Air under diaphragm Noi toi poi doi meaning
Noi toi poi doi meaning Unilaterallt
Unilaterallt Xray file cabinet
Xray file cabinet Gimp xray
Gimp xray Darkroom equipment in radiography
Darkroom equipment in radiography Abnormal vq scan images
Abnormal vq scan images Prehistoric era
Prehistoric era Xray neck lateral view
Xray neck lateral view Xray laser
Xray laser Xray laser
Xray laser Triboluminescence xray
Triboluminescence xray Xray laser
Xray laser Xray spectrometer
Xray spectrometer Xray laser
Xray laser Xray laser
Xray laser X ray scrubs
X ray scrubs Xray laser
Xray laser Xray laser
Xray laser Xray laser
Xray laser Bga xray
Bga xray Pa caldwell facial bones positioning
Pa caldwell facial bones positioning The xray guy
The xray guy 68 xray
68 xray Double bubble sign
Double bubble sign Supine chest xray
Supine chest xray Reverse waters
Reverse waters Picker xray
Picker xray Ellis curve
Ellis curve Atom xray
Atom xray Silicon valley xray
Silicon valley xray Xray photoelectron spectroscopy
Xray photoelectron spectroscopy Who discovered xray
Who discovered xray Properties of xray
Properties of xray Pnuemothorax xray
Pnuemothorax xray Capacitor-discharge mobile x-ray units
Capacitor-discharge mobile x-ray units Xray uranus
Xray uranus Mdcis
Mdcis Mmc xray
Mmc xray Aryepiglotic
Aryepiglotic Compass gladstone park
Compass gladstone park Fadhl alakwaa
Fadhl alakwaa Croup xray steeple sign
Croup xray steeple sign Clubfoot clinical features
Clubfoot clinical features Braggs law definition
Braggs law definition