Ischemic Heart Disease IHD coronary Heart Disease Introduction


- Slides: 23
Ischemic Heart Disease (IHD – coronary Heart Disease) Introduction to Primary Care: a course of the Center of Post Graduate Studies in FM PO Box 27121 – Riyadh 11417 Tel: 4912326 – Fax: 4970847 1 1
objectives: At the end of this session the trainee will be able to • be able to discuss the burden of IHD. • describe essential elements in history taking & examination • develop a differential diagnosis of chest pain. • describe appropriate diagnostic testing for chest pain. • discuss modifiable & non modifiable risk factors for cardiac disease. • describe the use of investigation in the evaluation of a patient with chest pain. • appropriatly use of specialty referral.
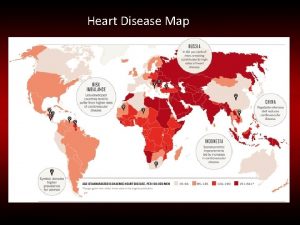
Prevalence of IHD • Heart diseases responsible for overal deaths in the Saudi population: – IHD : 17% – Hypertensive heart disease 9% – CVA : 4% 18 th scientific session of the Saudi Heart Association. 2007 http: //www. highbeam. com/doc/1 G 1 -158905180. html
History taking in CAD • Patient characteristics (Name, age, sex, occupation) • Pain (duration, location, intensity, nature, aggravating factors • Associated symptoms (Dyspnea, syncope…. etc) • Past history (HPN, DM, COPD. . ETC) • Family history (coronary artery disease , pneumothorax) • Drug history (antiangina, anti diabetic. . etc) • Life style (Diet, exercise, alcohol, smoking ) • Psychosocial (ICE, anxiety, stress )
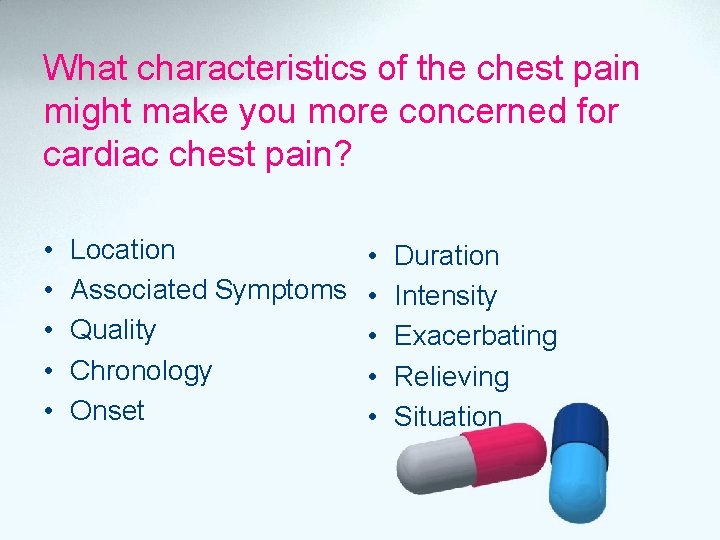
What characteristics of the chest pain might make you more concerned for cardiac chest pain? • • • Location Associated Symptoms Quality Chronology Onset • • • Duration Intensity Exacerbating Relieving Situation
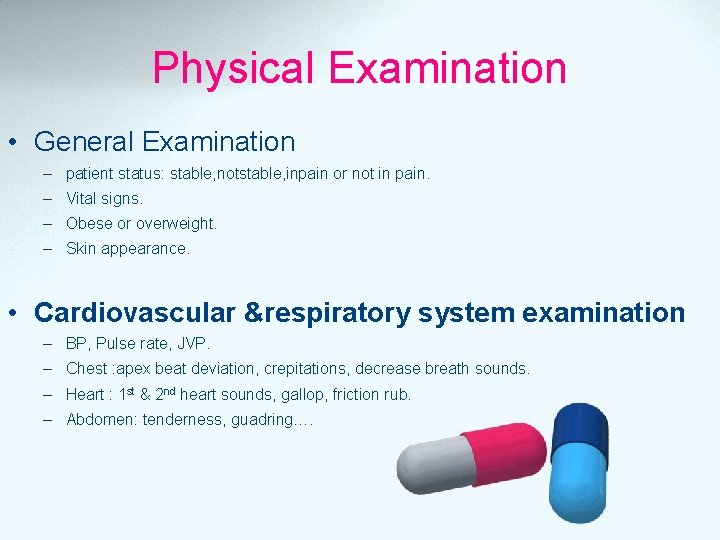
Physical Examination • General Examination – patient status: stable, notstable, inpain or not in pain. – Vital signs. – Obese or overweight. – Skin appearance. • Cardiovascular &respiratory system examination – BP, Pulse rate, JVP. – Chest : apex beat deviation, crepitations, decrease breath sounds. – Heart : 1 st & 2 nd heart sounds, gallop, friction rub. – Abdomen: tenderness, guadring….
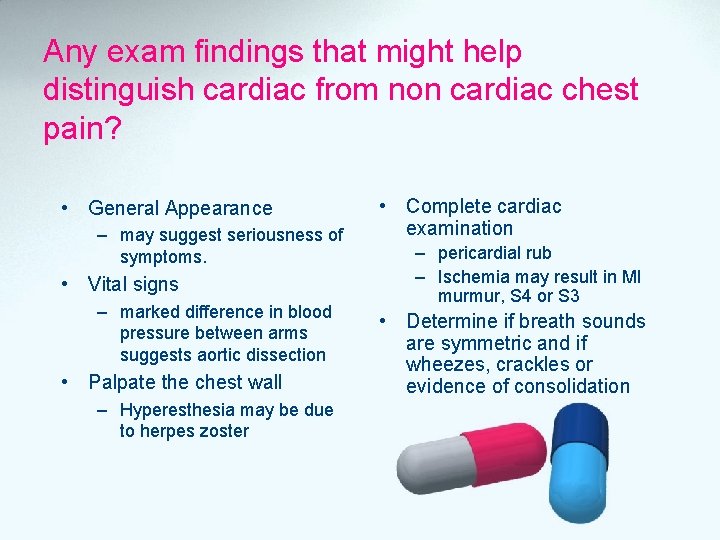
Any exam findings that might help distinguish cardiac from non cardiac chest pain? • General Appearance – may suggest seriousness of symptoms. • Vital signs – marked difference in blood pressure between arms suggests aortic dissection • Palpate the chest wall – Hyperesthesia may be due to herpes zoster • Complete cardiac examination – pericardial rub – Ischemia may result in MI murmur, S 4 or S 3 • Determine if breath sounds are symmetric and if wheezes, crackles or evidence of consolidation
What would be the differential diagnosis for chest pain?
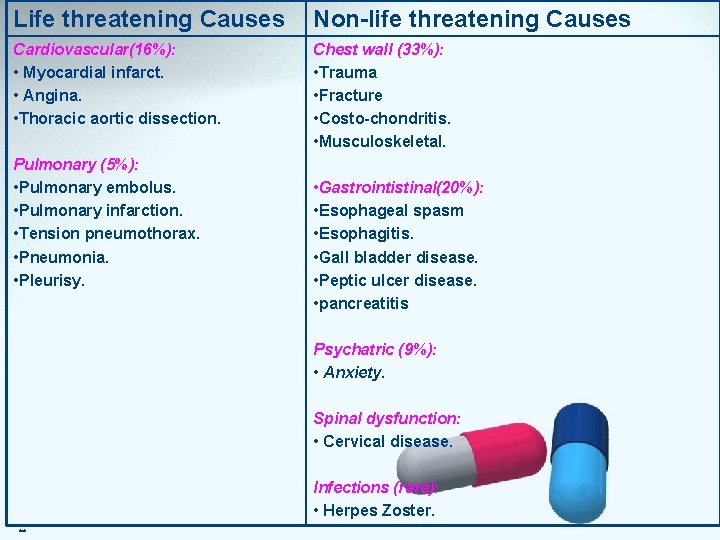
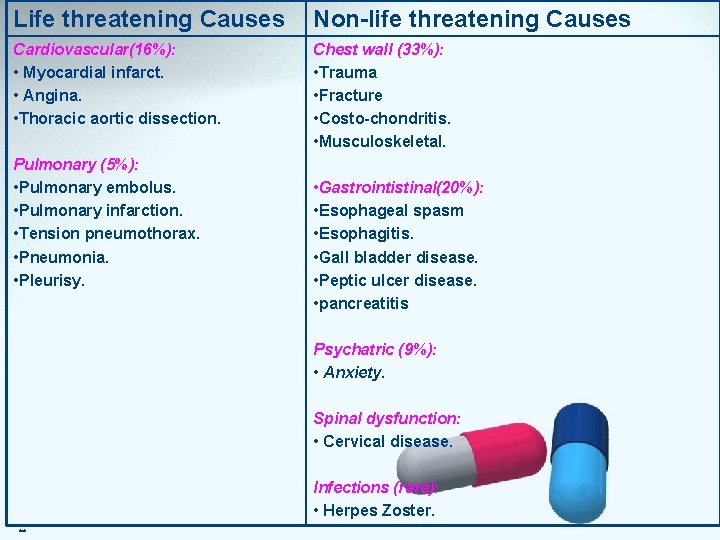
Life threatening Causes Non-life threatening Causes Cardiovascular(16%): • Myocardial infarct. • Angina. • Thoracic aortic dissection. Chest wall (33%): • Trauma • Fracture • Costo-chondritis. • Musculoskeletal. Pulmonary (5%): • Pulmonary embolus. • Pulmonary infarction. • Tension pneumothorax. • Pneumonia. • Pleurisy. • Gastrointistinal(20%): • Esophageal spasm • Esophagitis. • Gall bladder disease. • Peptic ulcer disease. • pancreatitis Psychatric (9%): • Anxiety. Spinal dysfunction: • Cervical disease. . . Infections (rare): • Herpes Zoster.
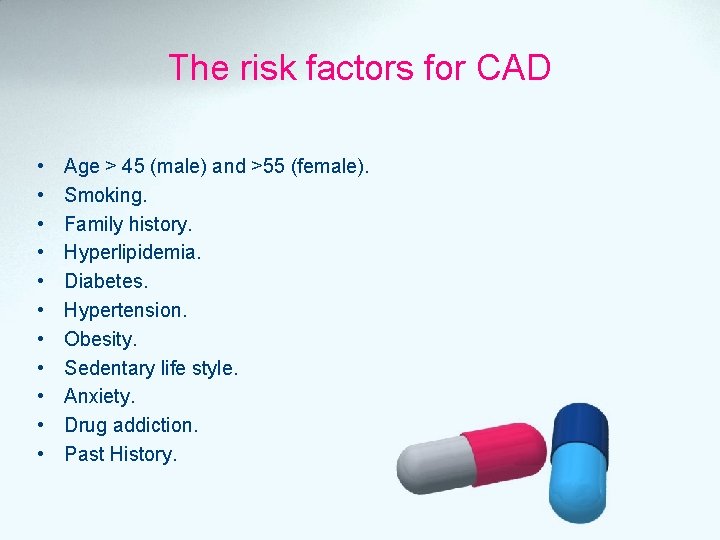
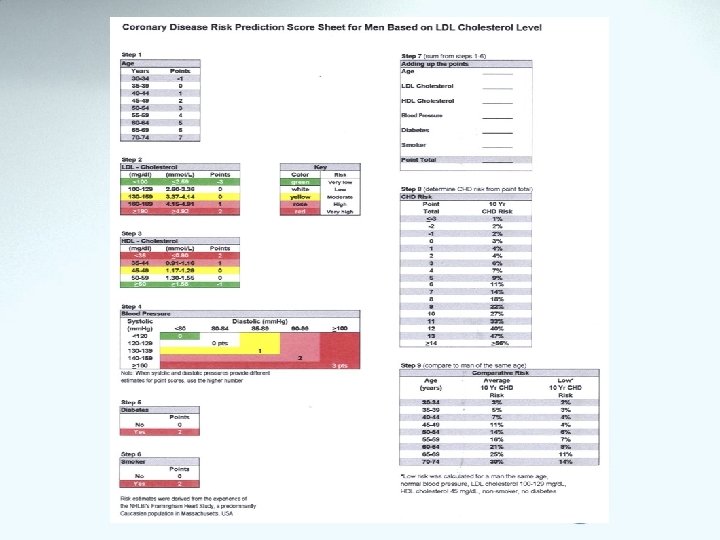
The risk factors for CAD • • • Age > 45 (male) and >55 (female). Smoking. Family history. Hyperlipidemia. Diabetes. Hypertension. Obesity. Sedentary life style. Anxiety. Drug addiction. Past History.
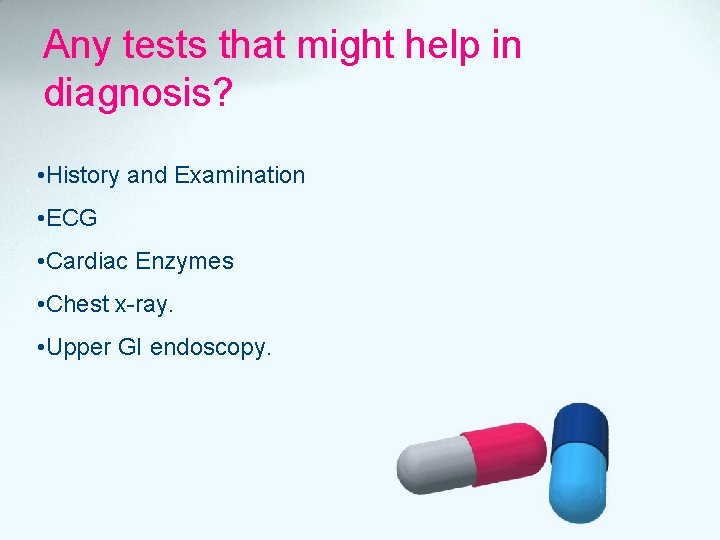
Any tests that might help in diagnosis? • History and Examination • ECG • Cardiac Enzymes • Chest x-ray. • Upper GI endoscopy.
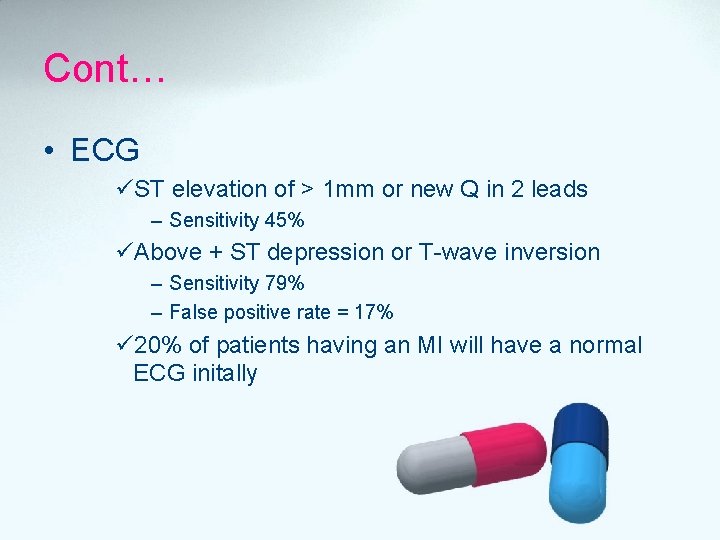
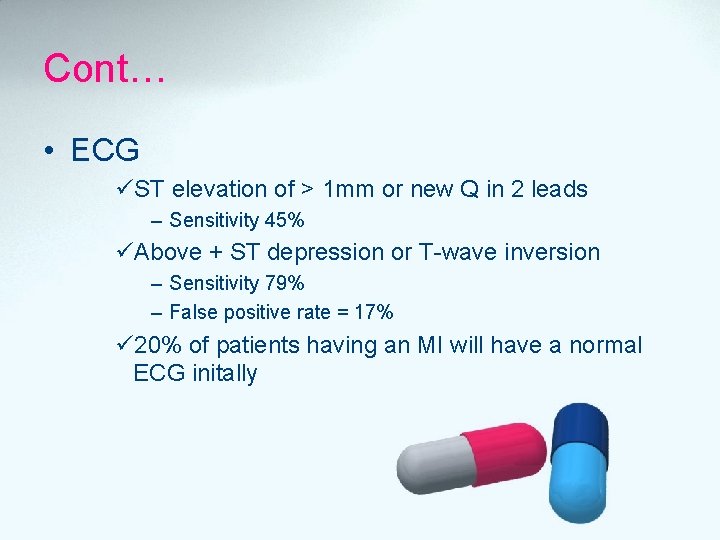
Cont… • ECG üST elevation of > 1 mm or new Q in 2 leads – Sensitivity 45% üAbove + ST depression or T-wave inversion – Sensitivity 79% – False positive rate = 17% ü 20% of patients having an MI will have a normal ECG initally

Cont… Cardiac enzymes: • Troponin, CK, myoglobin – 88 -90% sensitive at 4 -6 hours – 95 -100% sensitive 8 -12 hours Source: Am Heart J 1998 Aug; 136(2): 237 -44
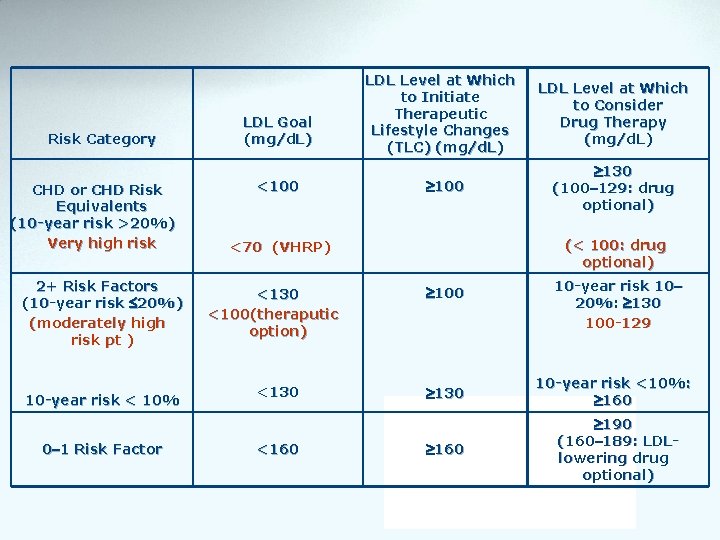
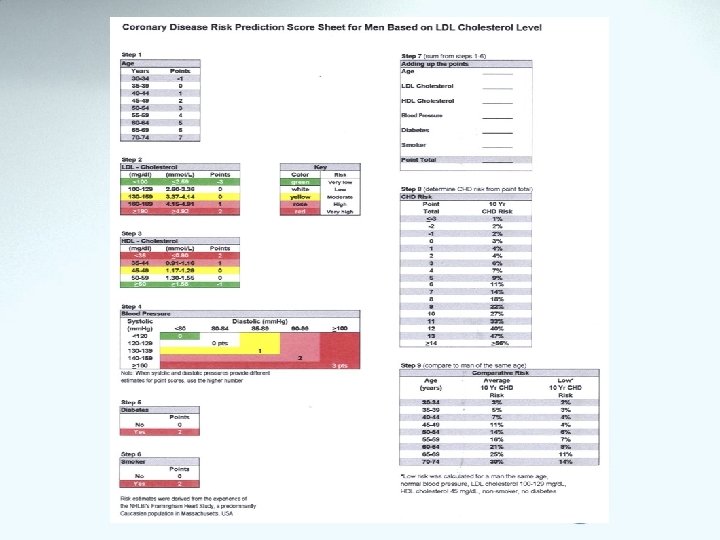
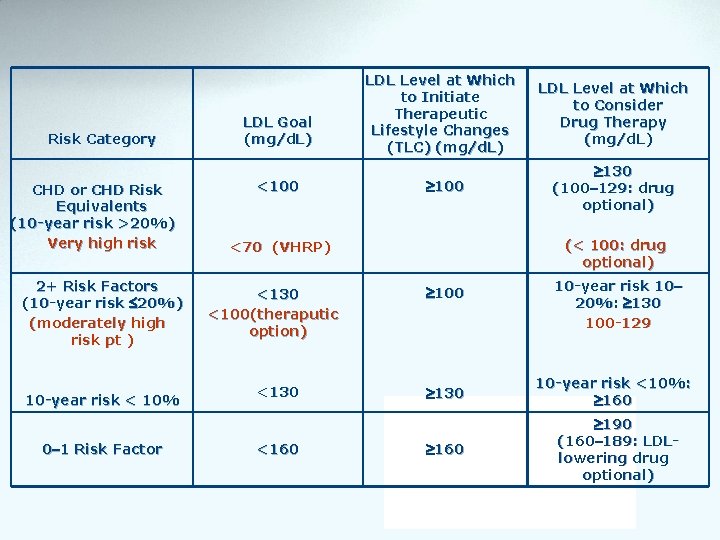
Risk Category CHD or CHD Risk Equivalents (10 -year risk >20%) Very high risk 2+ Risk Factors (10 -year risk 20%) (moderately high risk pt ) 10 -year risk < 10% 0– 1 Risk Factor LDL Goal (mg/d. L) <100 LDL Level at Which to Initiate Therapeutic Lifestyle Changes (TLC) (mg/d. L) 100 <130 <160 130 (100– 129: drug optional) (< 100: drug optional) <70 (VHRP) <130 <100(theraputic option) LDL Level at Which to Consider Drug Therapy (mg/d. L) 100 130 160 10 -year risk 10– 20%: 130 100 -129 10 -year risk <10%: 160 190 (160– 189: LDLlowering drug optional)
• Diabetes is regarded as a CHD Risk Equivalent • 10 -year risk for CHD 20% • High mortality with established CHD – High mortality with acute MI – High mortality post acute MI
Initial Approach • • ABC assessment 100% Oxygen Aspirine Nitroglycerine IV access Morphine Monitoring ECG quickly
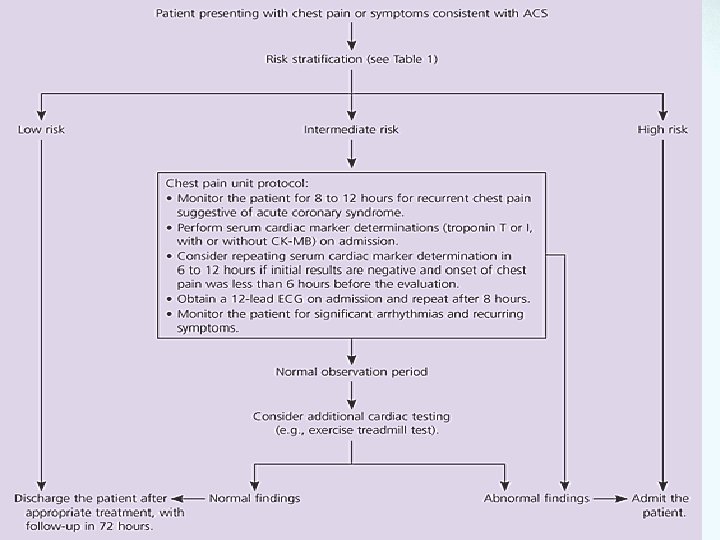
Action Plan
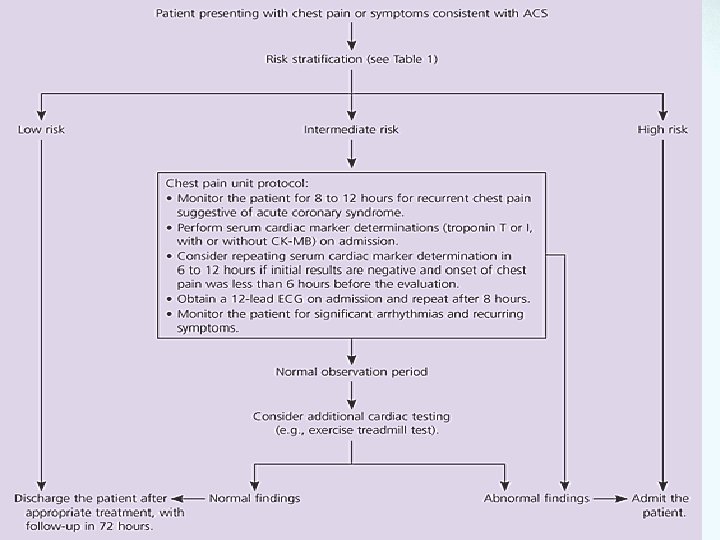
Action Plan Source: http: //www. aafp. org/afp/20050701/119. html
Referral Refer urgently all the serious conditions with chest pain: • • Cardiac causes. Esophageal spasm. Pulmonary embolism. Any other cases not responding to usual treatment.
Important Points • The likelihood of acute coronary syndrome (low, intermediate, high) should be determined in all patients who present with chest pain. • A 12 -lead ECG should be obtained within 10 minutes of presentation in patients with ongoing chest pain. • Cardiac markers (troponin T, troponin I, and/or creatine kinase. MB isoenzyme of creatine kinase) should be measured in any patient who has chest pain consistent with acute coronary syndrome. http: //www. aafp. org/afp/20050701/119. html
Important Points • A normal electrocardiogram does not rule out acute coronary syndrome. • When used by trained physicians, the Acute Cardiac Ischemia Time-Insensitive Predictive Instrument (a computerized, decision-making program built into the electrocardiogram machine) results in a significant reduction in hospital admissions of patients who do not have acute coronary syndrome. http: //www. aafp. org/afp/20050701/119. html

 Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Ischemic heart disease classification
Ischemic heart disease classification Heart disease
Heart disease Coronary heart disease
Coronary heart disease Ihd
Ihd Ihd
Ihd Ihd
Ihd Coronary artery disease
Coronary artery disease Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Coronary groove of heart
Coronary groove of heart Cardiovascular system crash course
Cardiovascular system crash course Coronary circulation of heart
Coronary circulation of heart Mechanism of ischemic stroke
Mechanism of ischemic stroke Cns ischemic response
Cns ischemic response Stroke protocol
Stroke protocol Hemorrhagic vs ischemic stroke symptoms
Hemorrhagic vs ischemic stroke symptoms Cns ischemic response
Cns ischemic response Cns ischemic response flow chart
Cns ischemic response flow chart Bainbridge reflex
Bainbridge reflex Tenecteplase ischemic stroke
Tenecteplase ischemic stroke Optic ischemic neuropathy
Optic ischemic neuropathy Ischemic bile duct injury
Ischemic bile duct injury Fossa ovalis
Fossa ovalis Pulmonary semilunar valve
Pulmonary semilunar valve