Valvular Heart Disease Kenneth S Korr M D

- Slides: 32
Valvular Heart Disease Kenneth S. Korr M. D. Associate Professor of Medicine, Brown Medical School Director, Division of Cardiology The Miriam Hospital
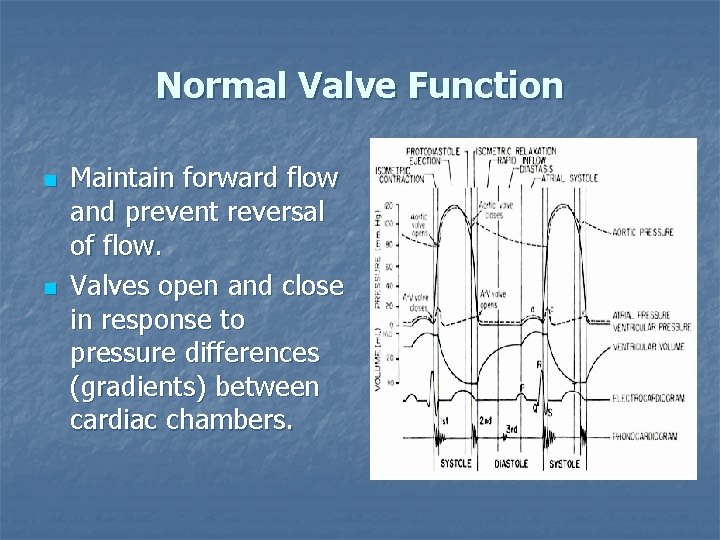
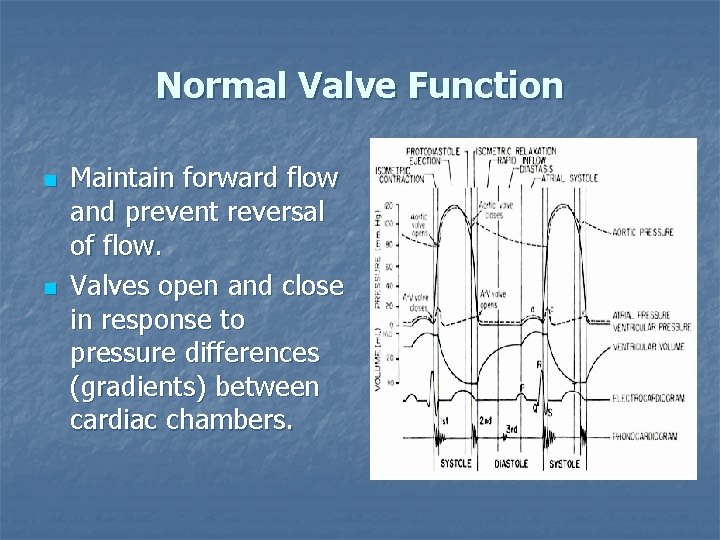
Normal Valve Function n n Maintain forward flow and prevent reversal of flow. Valves open and close in response to pressure differences (gradients) between cardiac chambers.
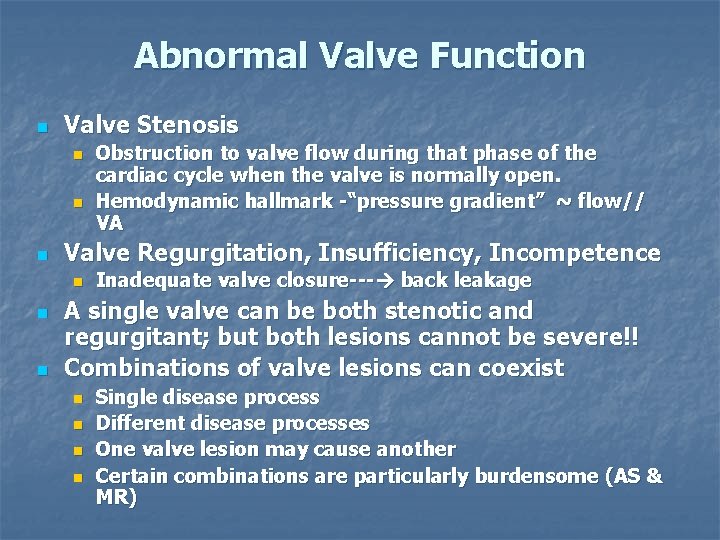
Abnormal Valve Function n Valve Stenosis n n n Valve Regurgitation, Insufficiency, Incompetence n n n Obstruction to valve flow during that phase of the cardiac cycle when the valve is normally open. Hemodynamic hallmark -“pressure gradient” ~ flow// VA Inadequate valve closure--- back leakage A single valve can be both stenotic and regurgitant; but both lesions cannot be severe!! Combinations of valve lesions can coexist n n Single disease process Different disease processes One valve lesion may cause another Certain combinations are particularly burdensome (AS & MR)
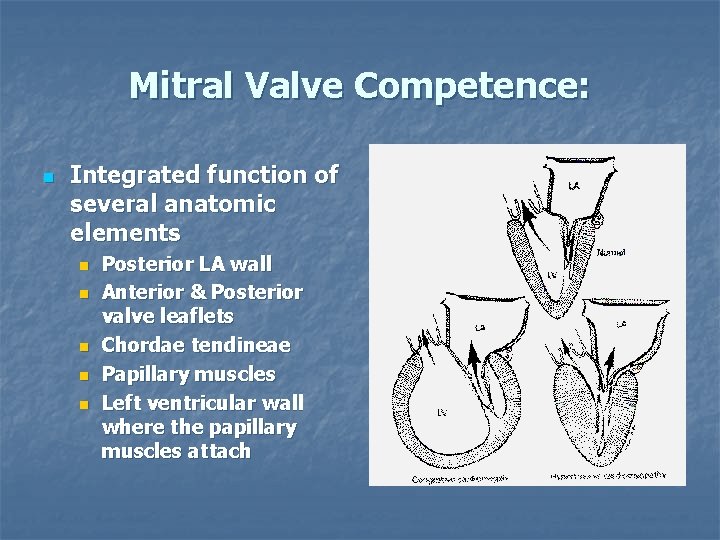
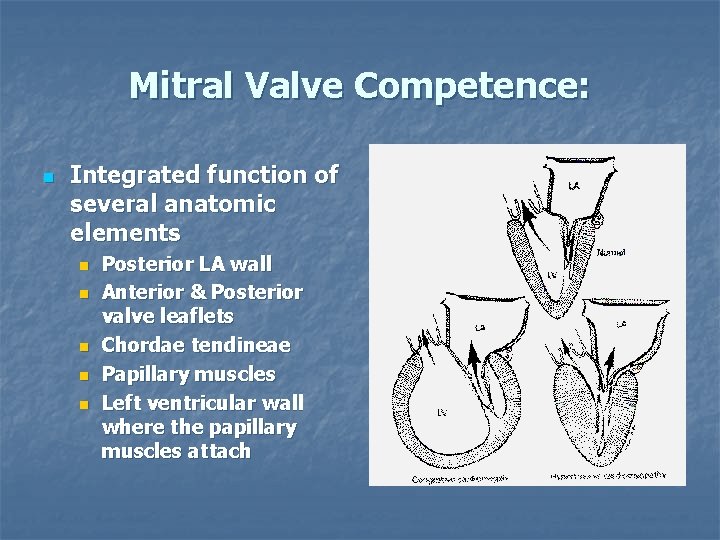
Mitral Valve Competence: n Integrated function of several anatomic elements n n n Posterior LA wall Anterior & Posterior valve leaflets Chordae tendineae Papillary muscles Left ventricular wall where the papillary muscles attach
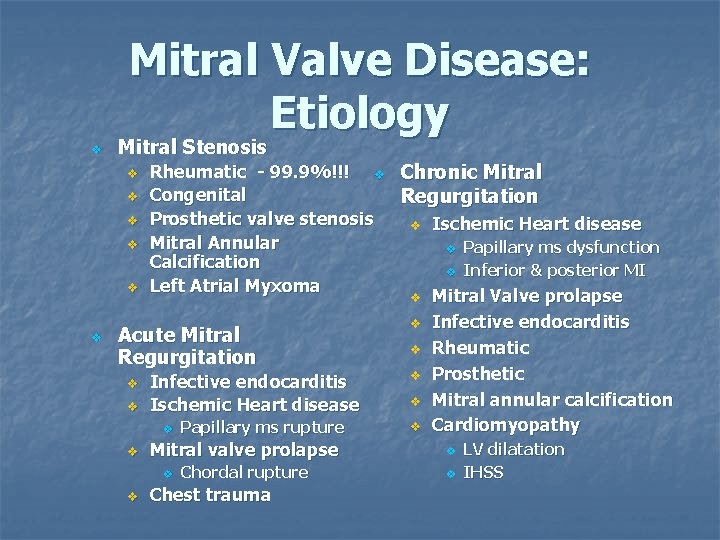
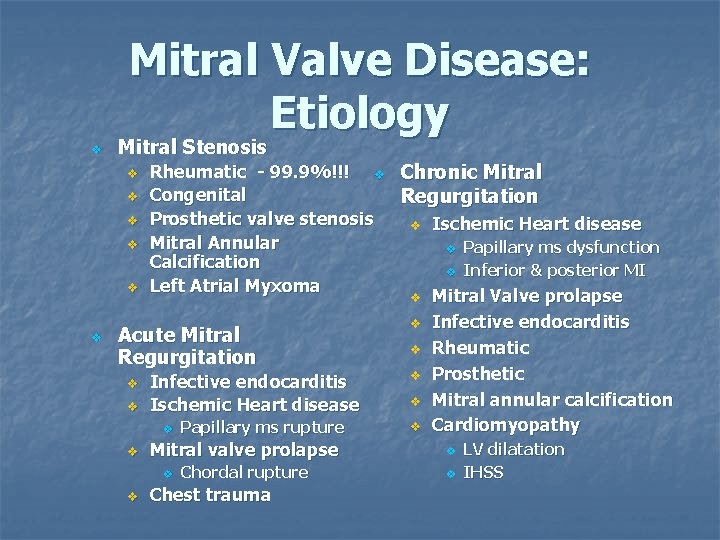
Mitral Valve Disease: Etiology v Mitral Stenosis v v v Rheumatic - 99. 9%!!! v Congenital Prosthetic valve stenosis Mitral Annular Calcification Left Atrial Myxoma Acute Mitral Regurgitation v v Infective endocarditis Ischemic Heart disease v v v Chordal rupture v Chest trauma Papillary ms dysfunction Inferior & posterior MI Mitral Valve prolapse Infective endocarditis Rheumatic Prosthetic Mitral annular calcification Cardiomyopathy Mitral valve prolapse v v Papillary ms rupture Chronic Mitral Regurgitation LV dilatation IHSS
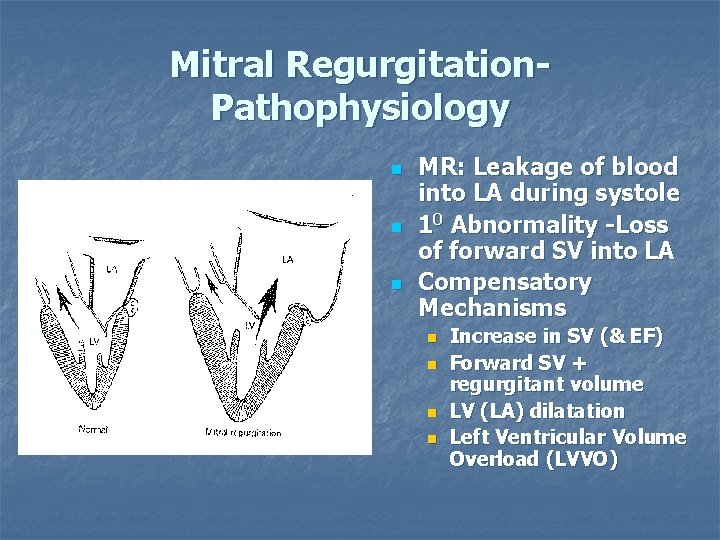
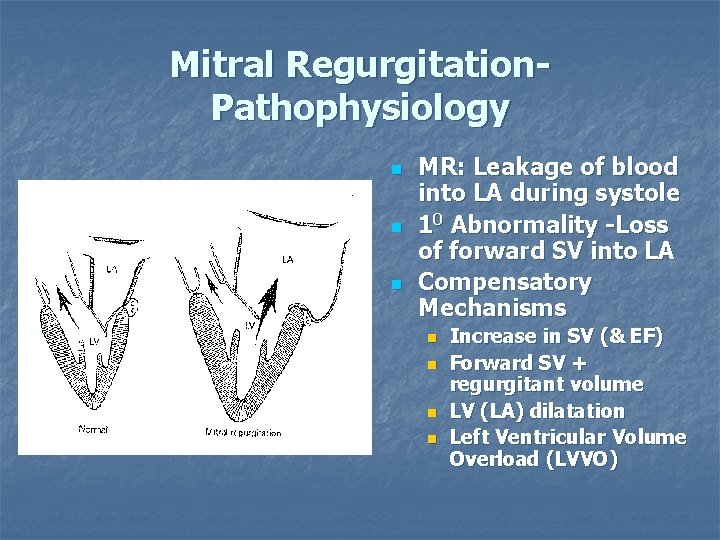
Mitral Regurgitation. Pathophysiology n n n MR: Leakage of blood into LA during systole 10 Abnormality -Loss of forward SV into LA Compensatory Mechanisms n n Increase in SV (& EF) Forward SV + regurgitant volume LV (LA) dilatation Left Ventricular Volume Overload (LVVO)
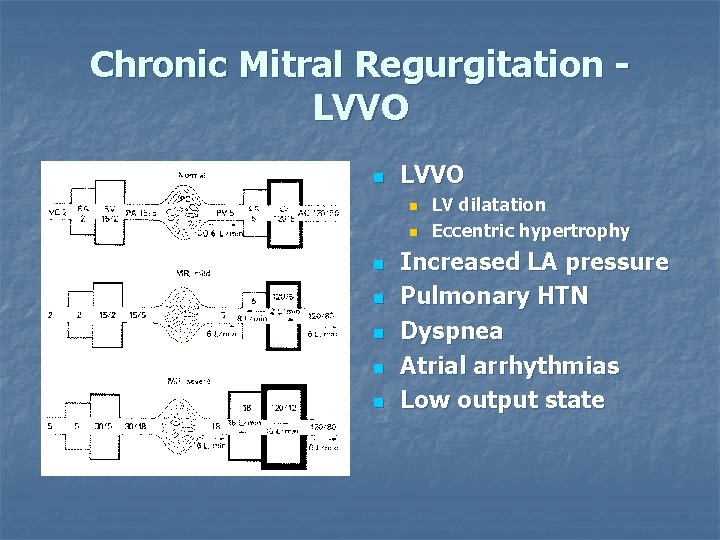
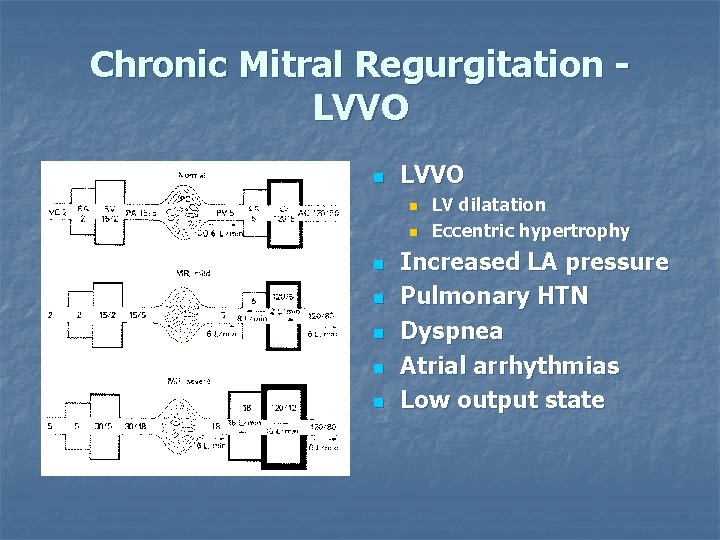
Chronic Mitral Regurgitation LVVO n n n n LV dilatation Eccentric hypertrophy Increased LA pressure Pulmonary HTN Dyspnea Atrial arrhythmias Low output state
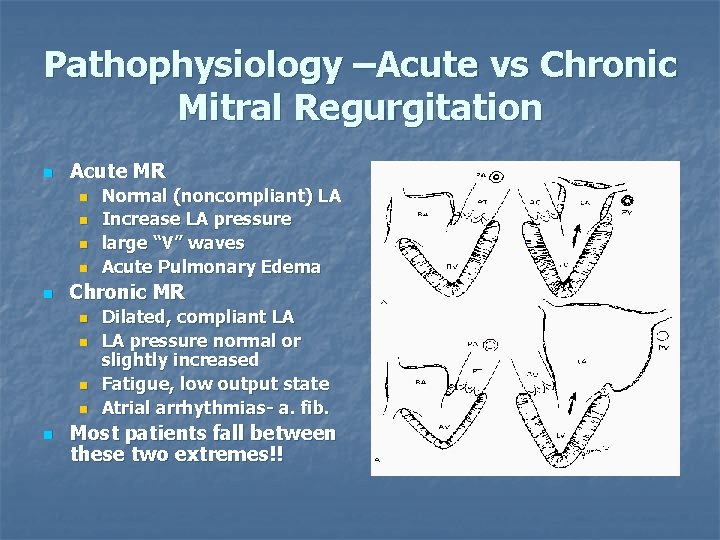
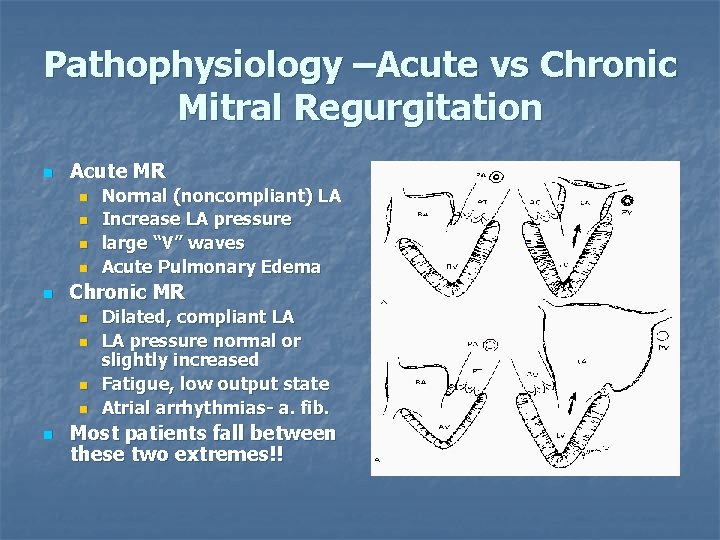
Pathophysiology –Acute vs Chronic Mitral Regurgitation n Acute MR n n n Chronic MR n n n Normal (noncompliant) LA Increase LA pressure large “V” waves Acute Pulmonary Edema Dilated, compliant LA LA pressure normal or slightly increased Fatigue, low output state Atrial arrhythmias- a. fib. Most patients fall between these two extremes!!
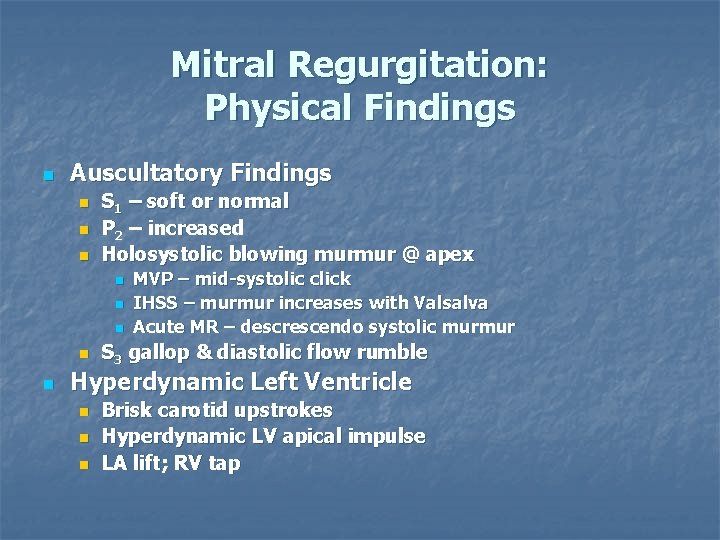
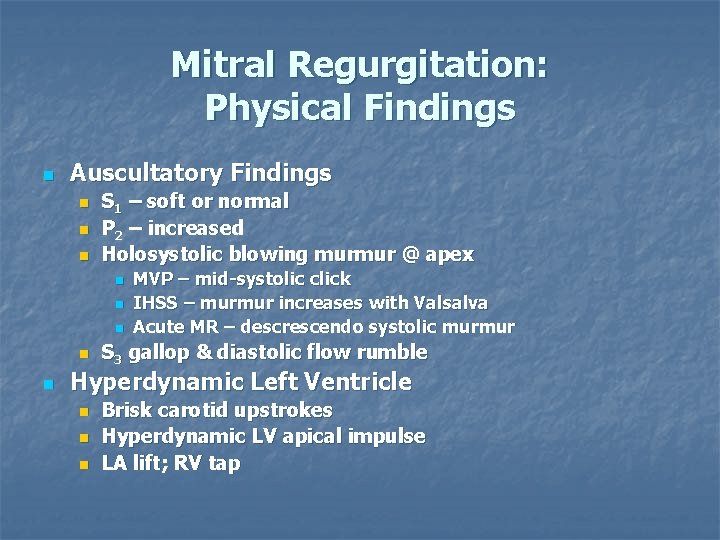
Mitral Regurgitation: Physical Findings n Auscultatory Findings n n n S 1 – soft or normal P 2 – increased Holosystolic blowing murmur @ apex n n n MVP – mid-systolic click IHSS – murmur increases with Valsalva Acute MR – descrescendo systolic murmur S 3 gallop & diastolic flow rumble Hyperdynamic Left Ventricle n n n Brisk carotid upstrokes Hyperdynamic LV apical impulse LA lift; RV tap
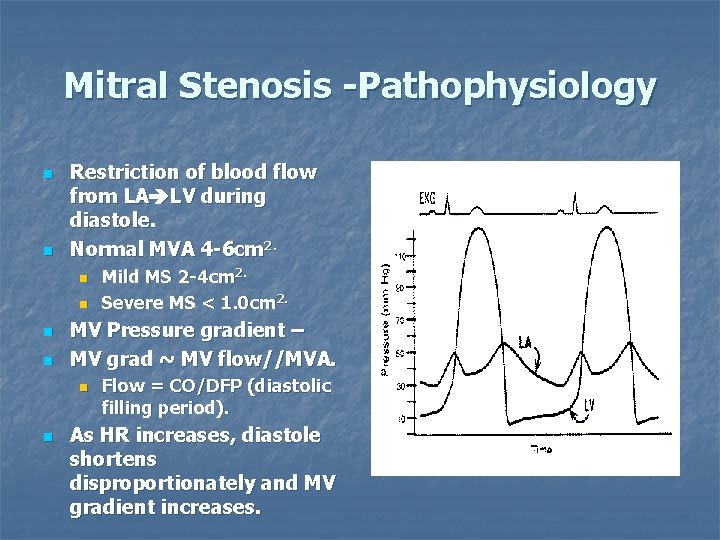
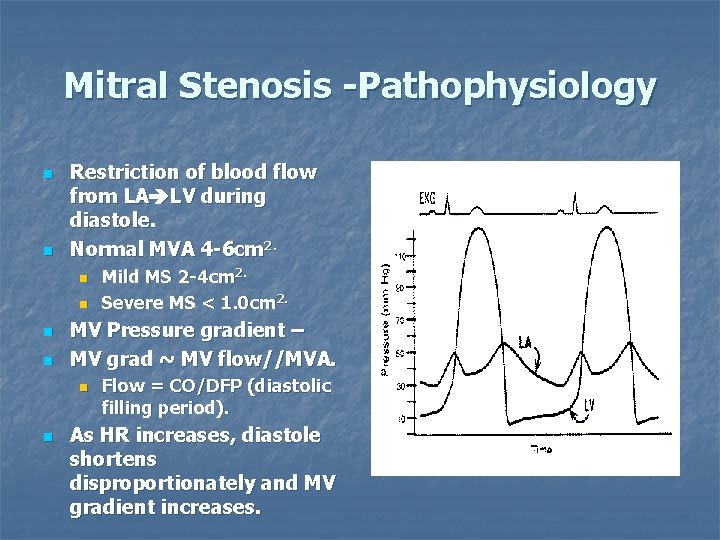
Mitral Stenosis -Pathophysiology n n Restriction of blood flow from LA LV during diastole. Normal MVA 4 -6 cm 2. n n MV Pressure gradient – MV grad ~ MV flow//MVA. n n Mild MS 2 -4 cm 2. Severe MS < 1. 0 cm 2. Flow = CO/DFP (diastolic filling period). As HR increases, diastole shortens disproportionately and MV gradient increases.
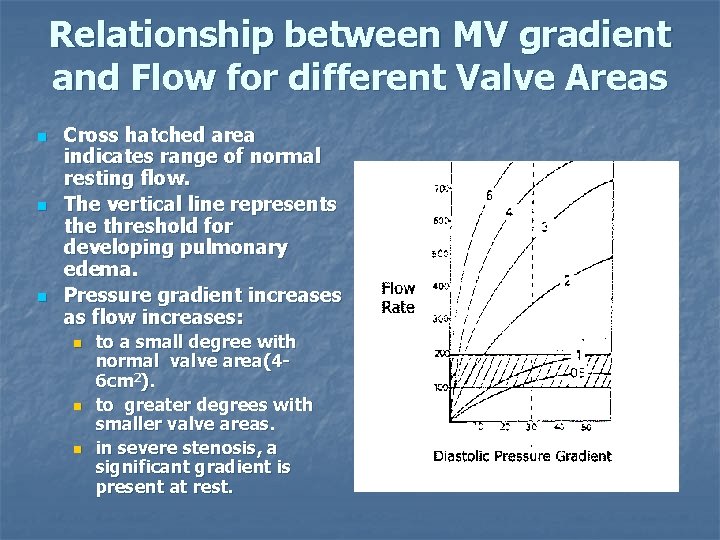
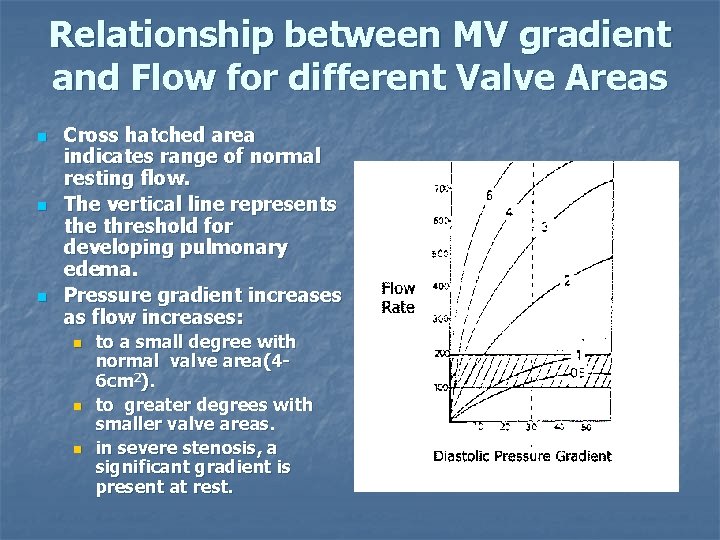
Relationship between MV gradient and Flow for different Valve Areas n n n Cross hatched area indicates range of normal resting flow. The vertical line represents the threshold for developing pulmonary edema. Pressure gradient increases as flow increases: n n n to a small degree with normal valve area(46 cm 2). to greater degrees with smaller valve areas. in severe stenosis, a significant gradient is present at rest.
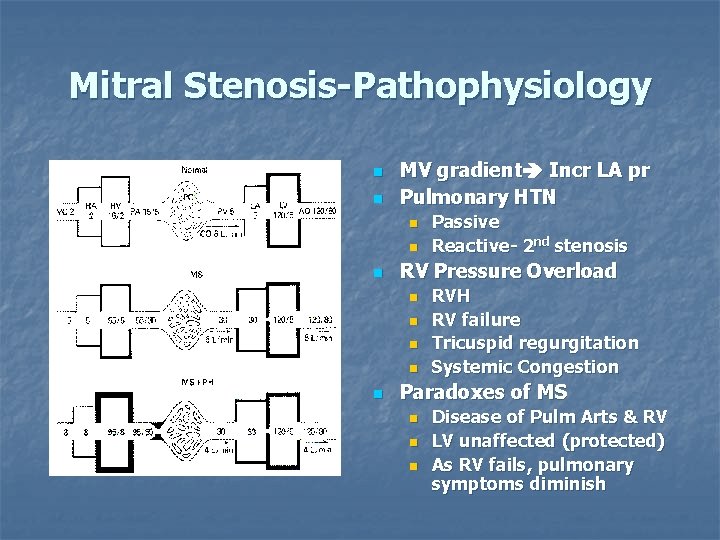
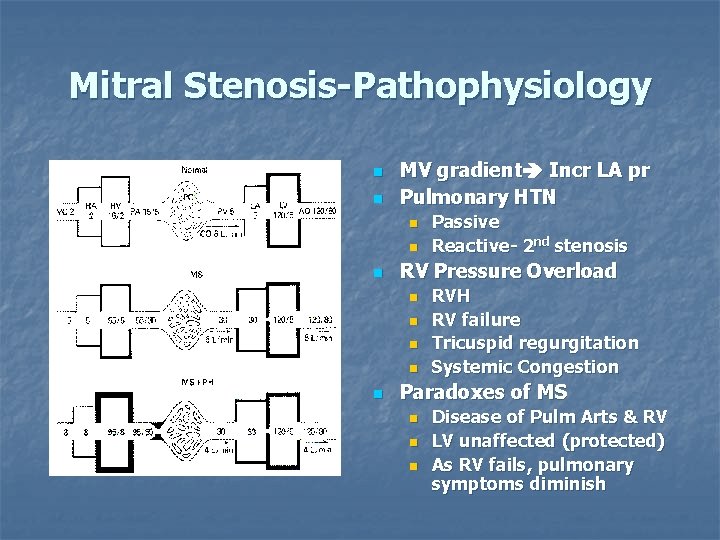
Mitral Stenosis-Pathophysiology n n MV gradient Incr LA pr Pulmonary HTN n n n RV Pressure Overload n n n Passive Reactive- 2 nd stenosis RVH RV failure Tricuspid regurgitation Systemic Congestion Paradoxes of MS n n n Disease of Pulm Arts & RV LV unaffected (protected) As RV fails, pulmonary symptoms diminish
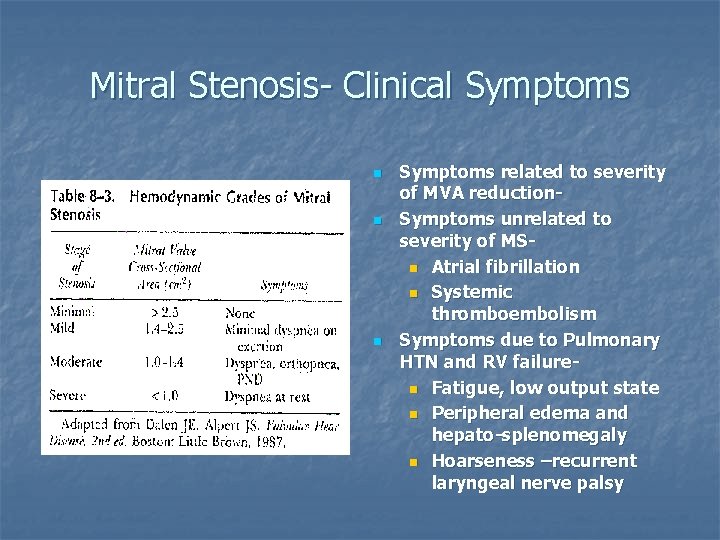
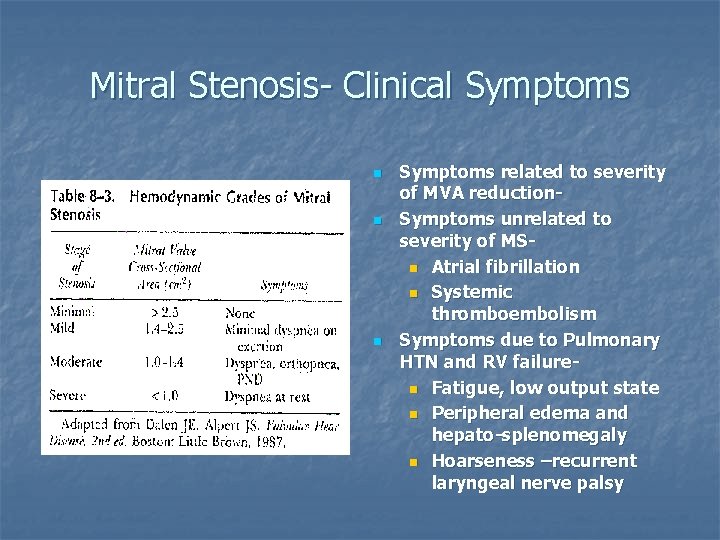
Mitral Stenosis- Clinical Symptoms n n n Symptoms related to severity of MVA reduction. Symptoms unrelated to severity of MSn Atrial fibrillation n Systemic thromboembolism Symptoms due to Pulmonary HTN and RV failuren Fatigue, low output state n Peripheral edema and hepato-splenomegaly n Hoarseness –recurrent laryngeal nerve palsy
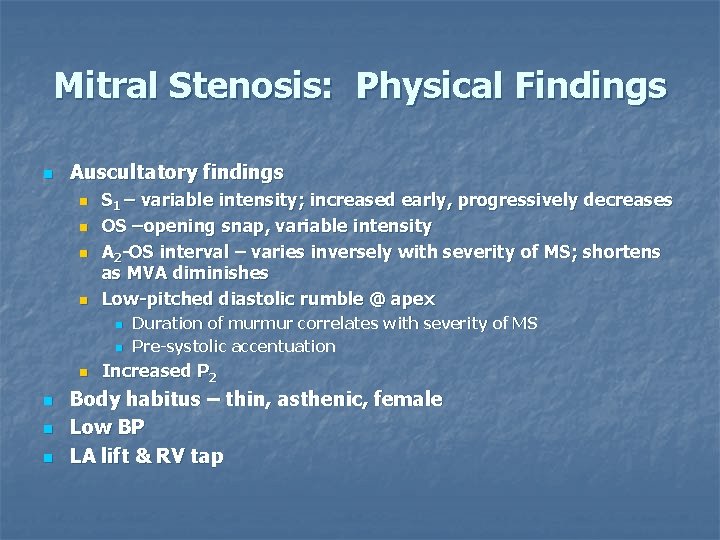
Mitral Stenosis: Physical Findings n Auscultatory findings n n S 1 – variable intensity; increased early, progressively decreases OS –opening snap, variable intensity A 2 -OS interval – varies inversely with severity of MS; shortens as MVA diminishes Low-pitched diastolic rumble @ apex n n n Duration of murmur correlates with severity of MS Pre-systolic accentuation Increased P 2 Body habitus – thin, asthenic, female Low BP LA lift & RV tap
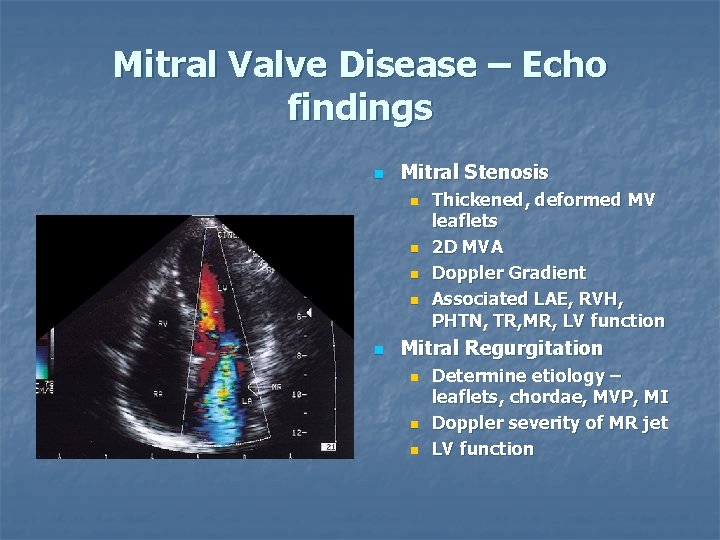
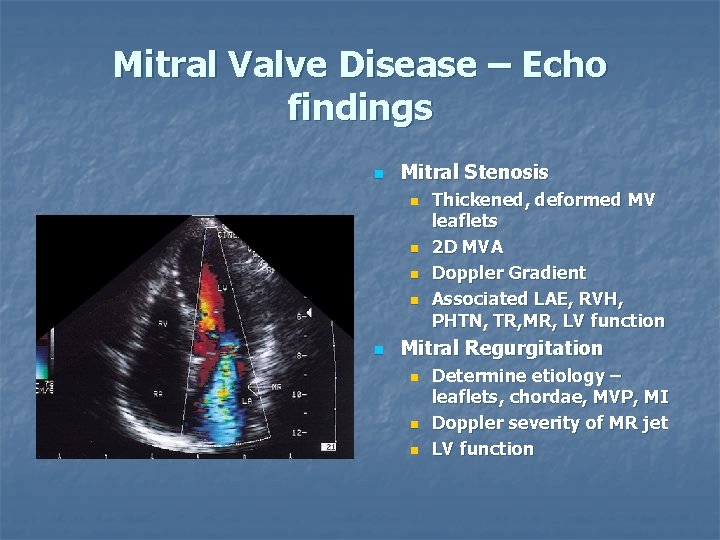
Mitral Valve Disease – Echo findings n Mitral Stenosis n n n Thickened, deformed MV leaflets 2 D MVA Doppler Gradient Associated LAE, RVH, PHTN, TR, MR, LV function Mitral Regurgitation n Determine etiology – leaflets, chordae, MVP, MI Doppler severity of MR jet LV function
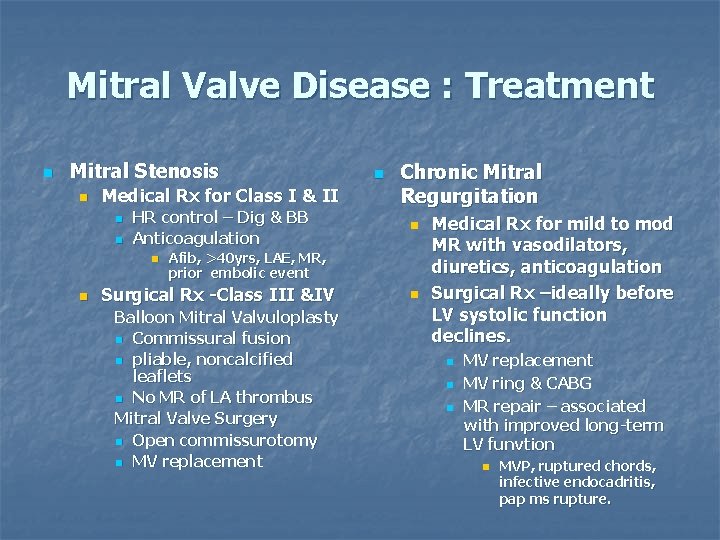
Mitral Valve Disease : Treatment n Mitral Stenosis n Medical Rx for Class I & II n n HR control – Dig & BB Anticoagulation n Chronic Mitral Regurgitation n Afib, >40 yrs, LAE, MR, prior embolic event Surgical Rx -Class III &IV Balloon Mitral Valvuloplasty n Commissural fusion n pliable, noncalcified leaflets n No MR of LA thrombus Mitral Valve Surgery n Open commissurotomy n MV replacement n Medical Rx for mild to mod MR with vasodilators, diuretics, anticoagulation Surgical Rx –ideally before LV systolic function declines. n n n MV replacement MV ring & CABG MR repair – associated with improved long-term LV funvtion n MVP, ruptured chords, infective endocadritis, pap ms rupture.
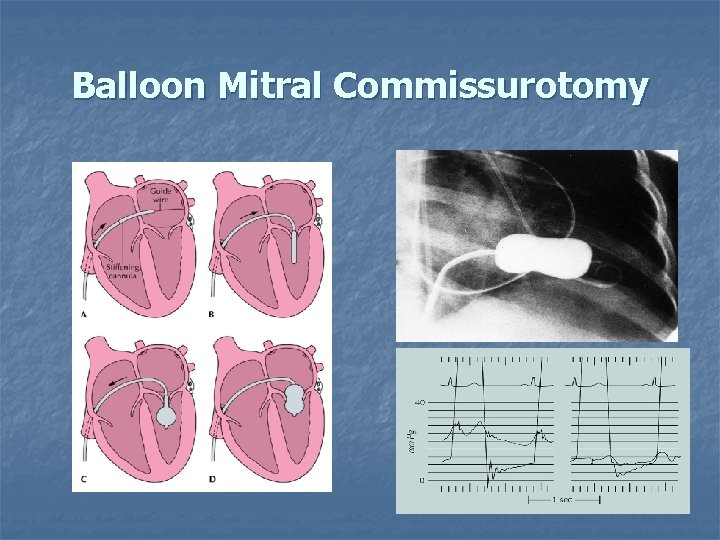
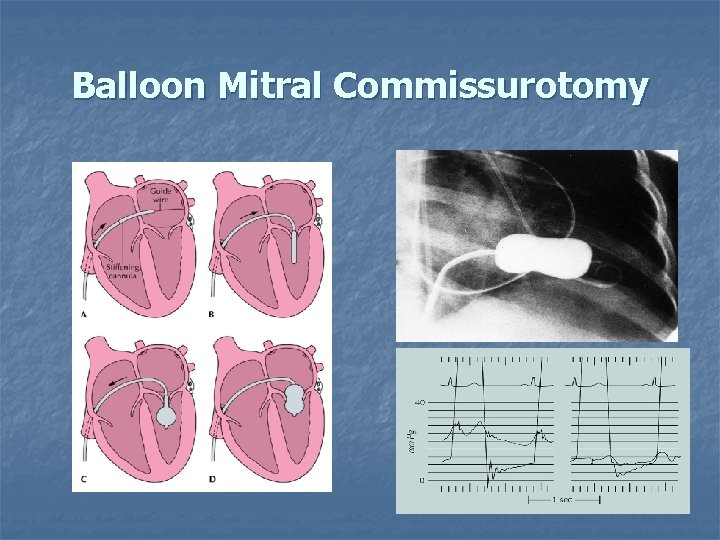
Balloon Mitral Commissurotomy
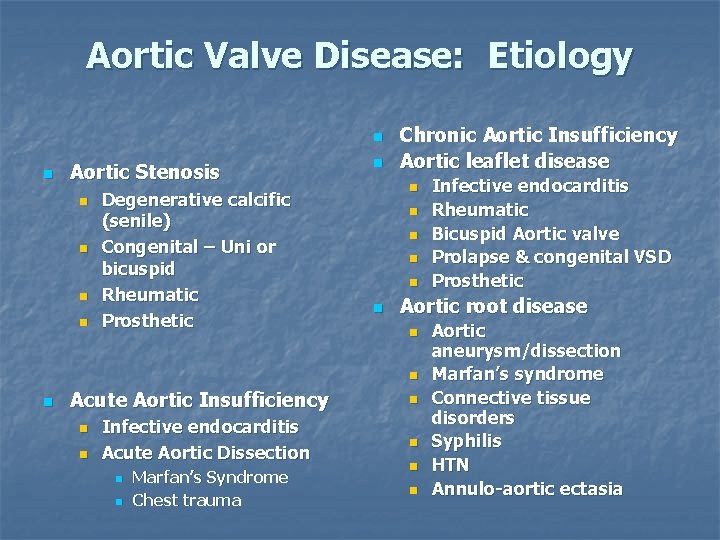
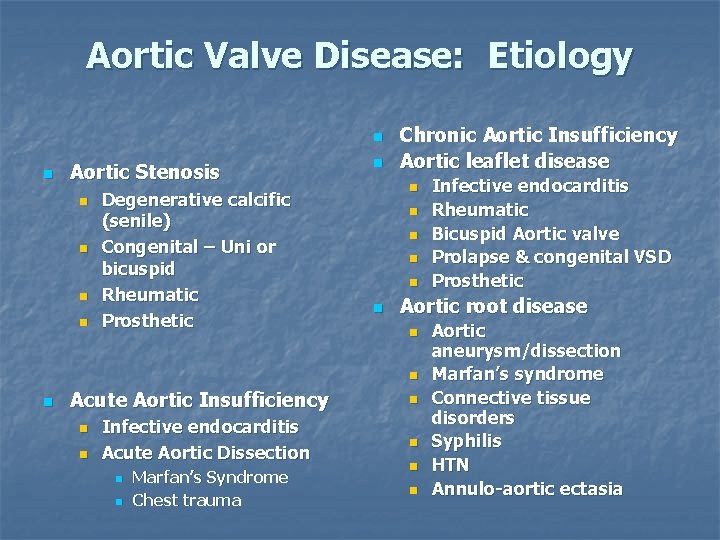
Aortic Valve Disease: Etiology n n Aortic Stenosis n n Degenerative calcific (senile) Congenital – Uni or bicuspid Rheumatic Prosthetic n Chronic Aortic Insufficiency Aortic leaflet disease n n n Aortic root disease n n n Acute Aortic Insufficiency n n Infective endocarditis Acute Aortic Dissection n n Marfan’s Syndrome Chest trauma Infective endocarditis Rheumatic Bicuspid Aortic valve Prolapse & congenital VSD Prosthetic n n Aortic aneurysm/dissection Marfan’s syndrome Connective tissue disorders Syphilis HTN Annulo-aortic ectasia
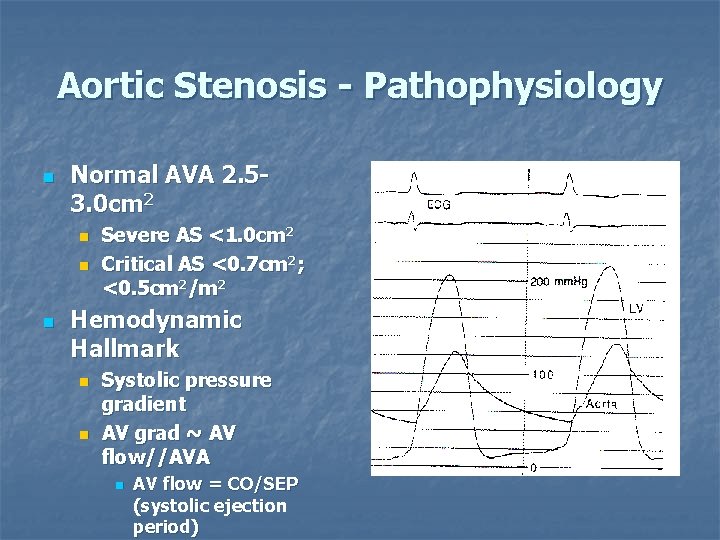
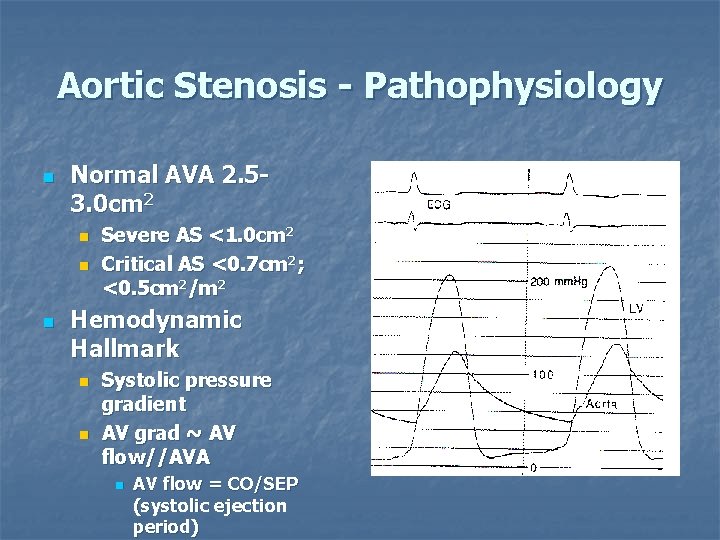
Aortic Stenosis - Pathophysiology n Normal AVA 2. 53. 0 cm 2 n n n Severe AS <1. 0 cm 2 Critical AS <0. 7 cm 2; <0. 5 cm 2/m 2 Hemodynamic Hallmark n n Systolic pressure gradient AV grad ~ AV flow//AVA n AV flow = CO/SEP (systolic ejection period)
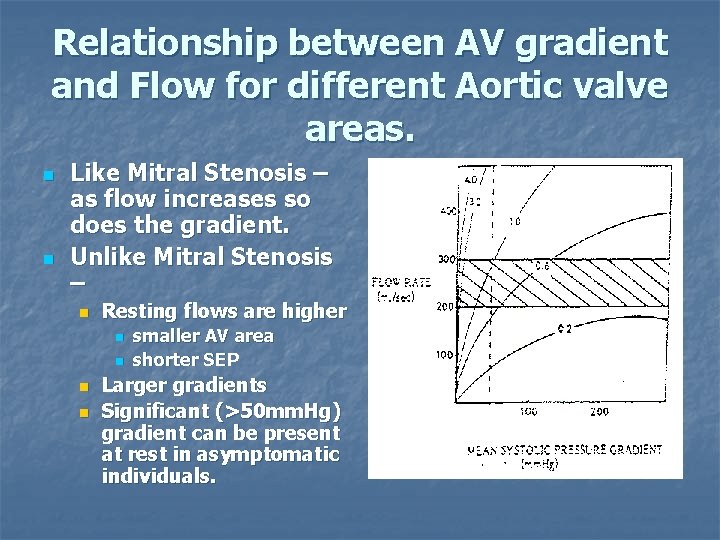
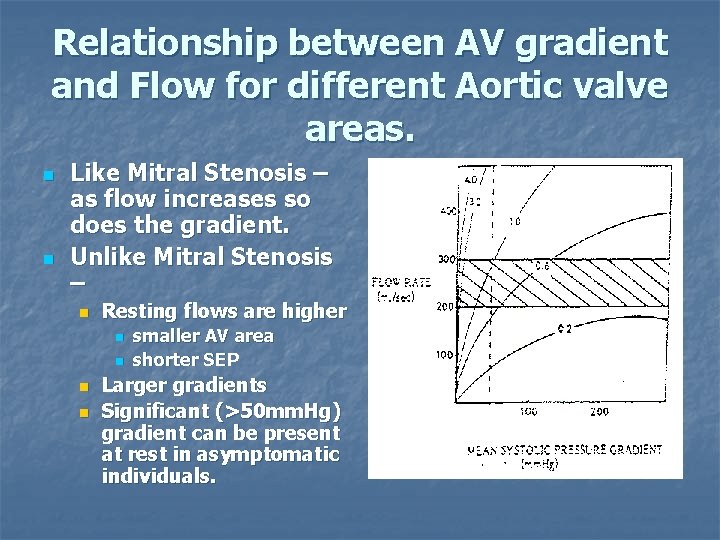
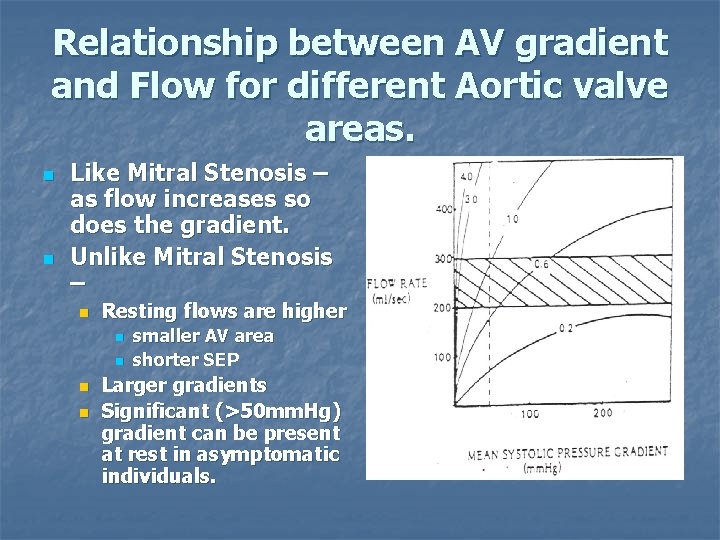
Relationship between AV gradient and Flow for different Aortic valve areas. n n Like Mitral Stenosis – as flow increases so does the gradient. Unlike Mitral Stenosis – n Resting flows are higher n n smaller AV area shorter SEP Larger gradients Significant (>50 mm. Hg) gradient can be present at rest in asymptomatic individuals.
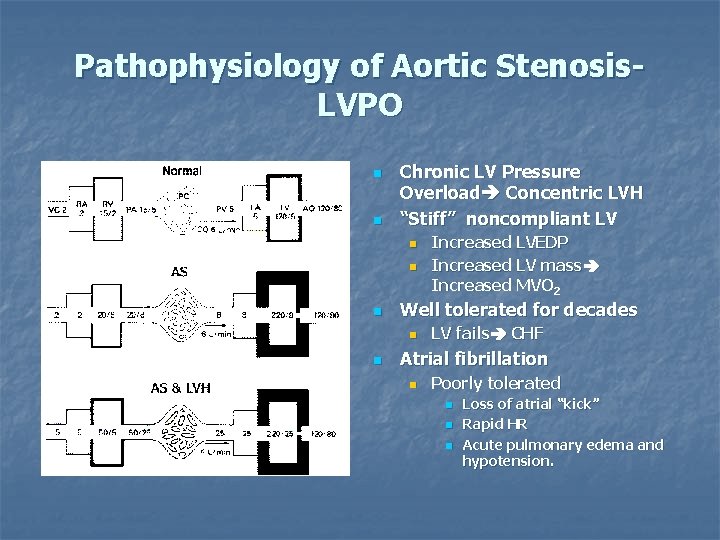
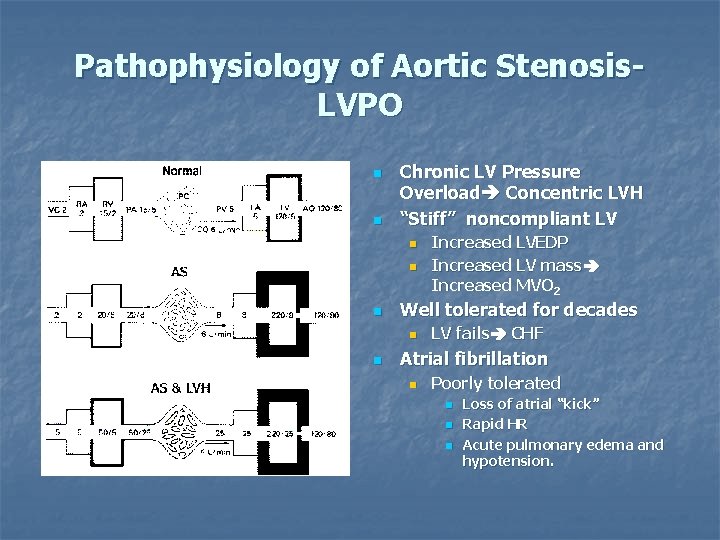
Pathophysiology of Aortic Stenosis. LVPO n n Chronic LV Pressure Overload Concentric LVH “Stiff” noncompliant LV n n n Well tolerated for decades n n Increased LVEDP Increased LV mass Increased MVO 2 LV fails CHF Atrial fibrillation n Poorly tolerated n n n Loss of atrial “kick” Rapid HR Acute pulmonary edema and hypotension.
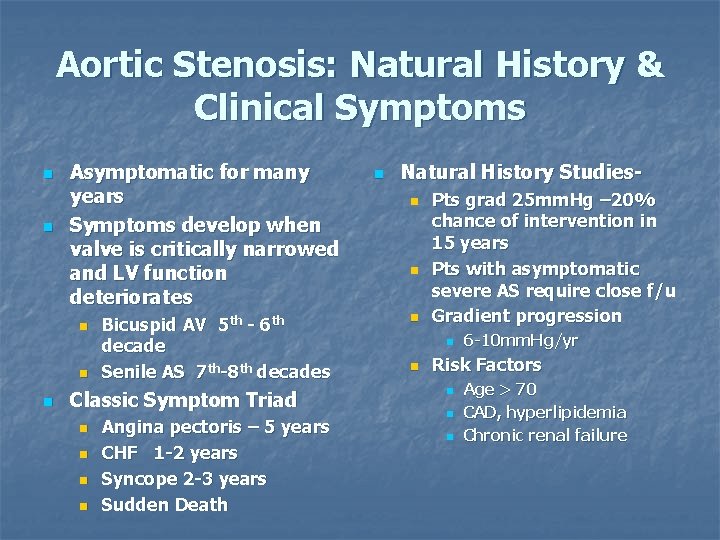
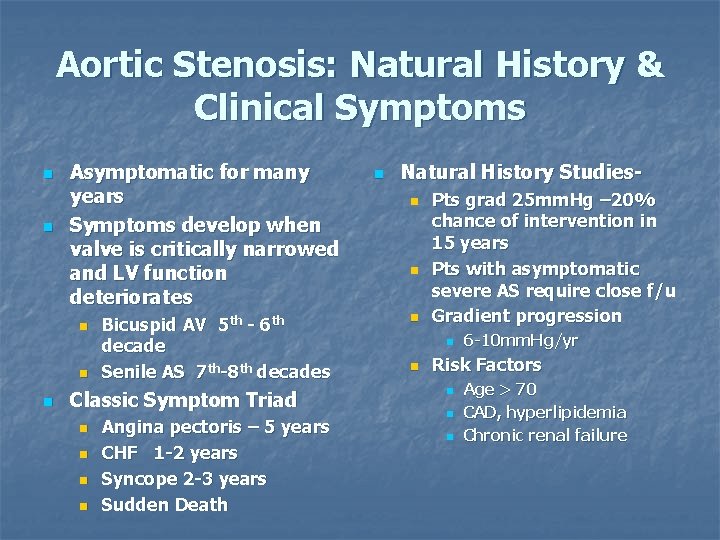
Aortic Stenosis: Natural History & Clinical Symptoms n n Asymptomatic for many years Symptoms develop when valve is critically narrowed and LV function deteriorates n n n Bicuspid AV 5 th - 6 th decade Senile AS 7 th-8 th decades Classic Symptom Triad n n Angina pectoris – 5 years CHF 1 -2 years Syncope 2 -3 years Sudden Death n Natural History Studiesn n n Pts grad 25 mm. Hg – 20% chance of intervention in 15 years Pts with asymptomatic severe AS require close f/u Gradient progression n n 6 -10 mm. Hg/yr Risk Factors n n n Age > 70 CAD, hyperlipidemia Chronic renal failure
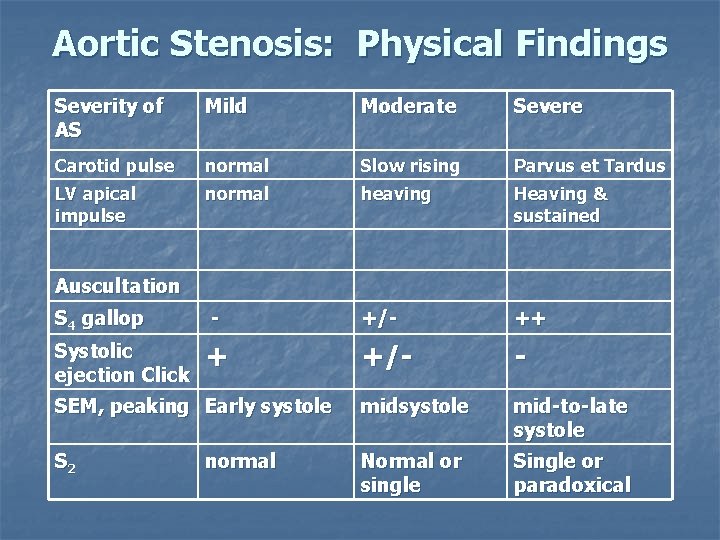
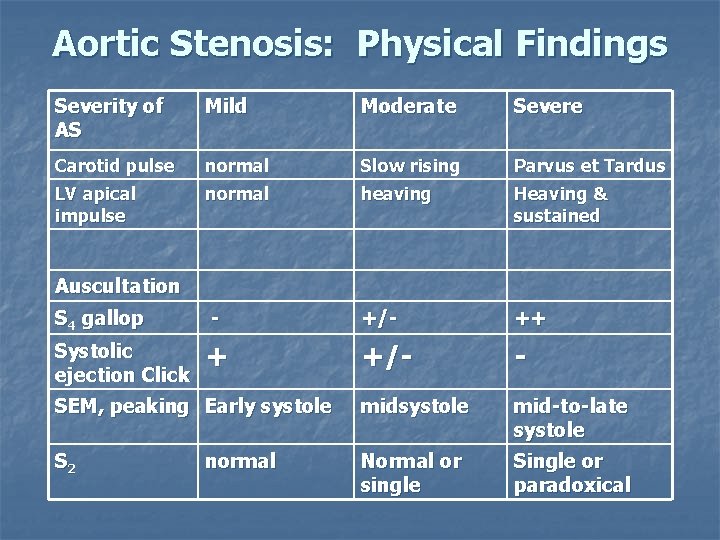
Aortic Stenosis: Physical Findings Severity of AS Mild Moderate Severe Carotid pulse normal Slow rising Parvus et Tardus LV apical impulse normal heaving Heaving & sustained Auscultation S 4 gallop - +/- ++ Systolic ejection Click + +/- - SEM, peaking Early systole mid-to-late systole S 2 Normal or single Single or paradoxical normal
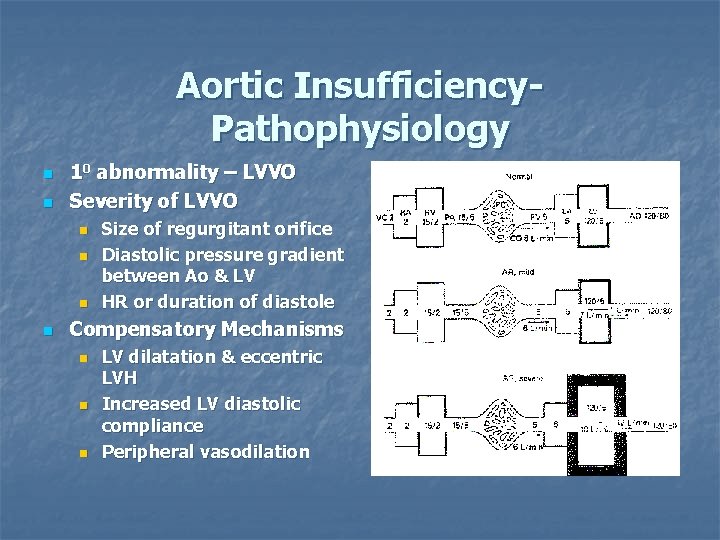
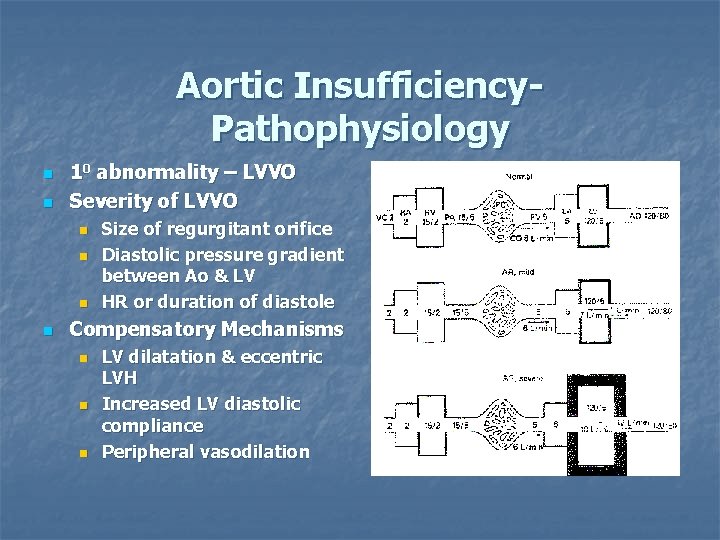
Aortic Insufficiency. Pathophysiology n n 10 abnormality – LVVO Severity of LVVO n n Size of regurgitant orifice Diastolic pressure gradient between Ao & LV HR or duration of diastole Compensatory Mechanisms n n n LV dilatation & eccentric LVH Increased LV diastolic compliance Peripheral vasodilation

LV Volume vs Pressure Overload Feature LVPO (AS) LVVO (MR, AI) LV Volume normal Dilated** Wall thickness Conc. LVH Normal to slightly increased LV compliance “stiff” noncompliant Increased compliance LV diastolic Pr increased Normal to slightly increased LV systolic Pr Increased** Normal to slightly increased LVEF normal increased
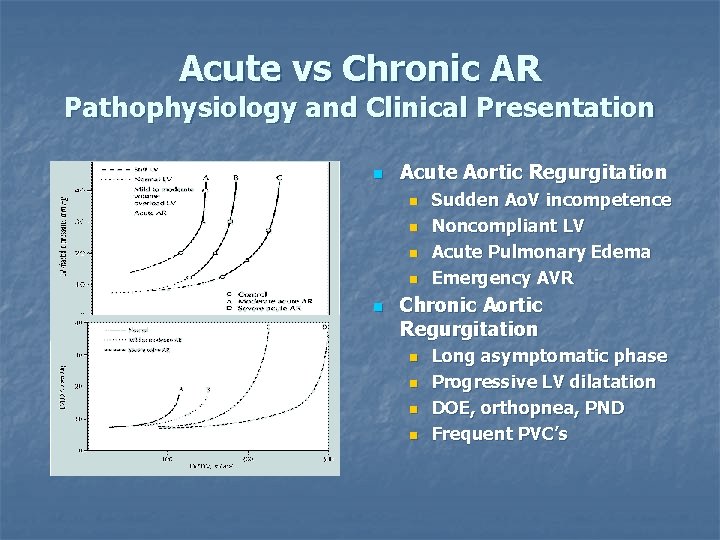
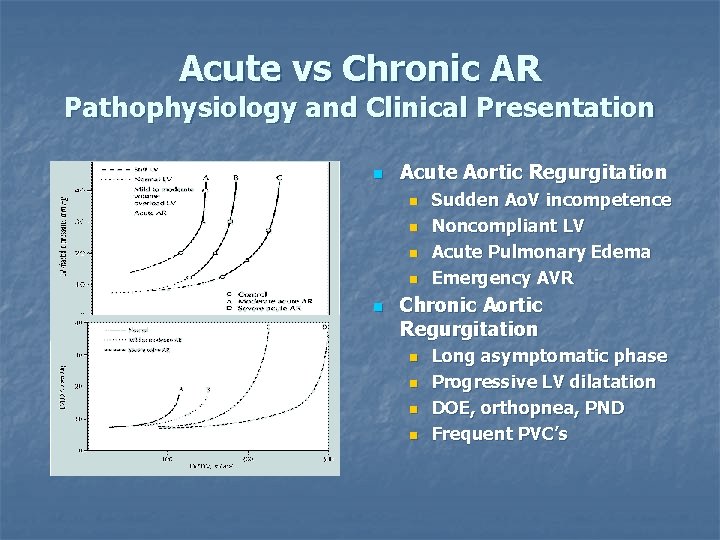
Acute vs Chronic AR Pathophysiology and Clinical Presentation n Acute Aortic Regurgitation n n Sudden Ao. V incompetence Noncompliant LV Acute Pulmonary Edema Emergency AVR Chronic Aortic Regurgitation n n Long asymptomatic phase Progressive LV dilatation DOE, orthopnea, PND Frequent PVC’s
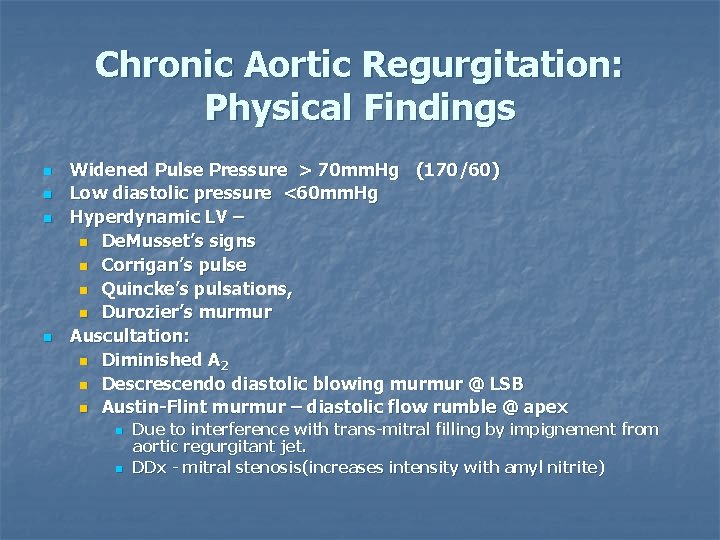
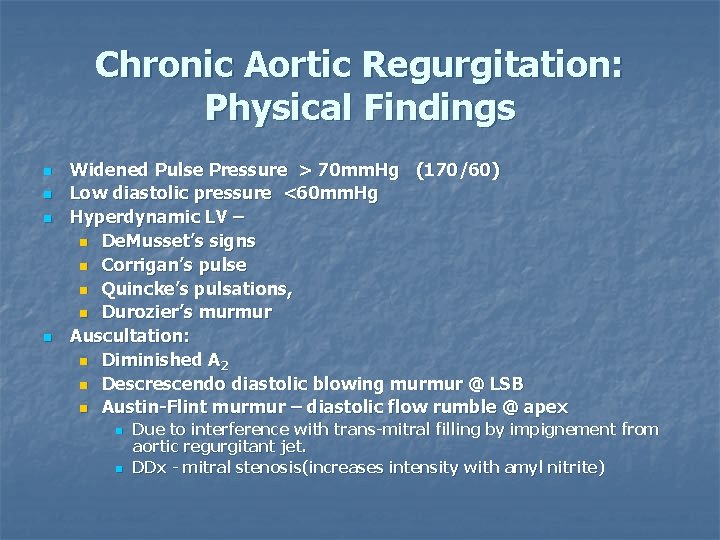
Chronic Aortic Regurgitation: Physical Findings n n Widened Pulse Pressure > 70 mm. Hg (170/60) Low diastolic pressure <60 mm. Hg Hyperdynamic LV – n De. Musset’s signs n Corrigan’s pulse n Quincke’s pulsations, n Durozier’s murmur Auscultation: n Diminished A 2 n Descrescendo diastolic blowing murmur @ LSB n Austin-Flint murmur – diastolic flow rumble @ apex n n Due to interference with trans-mitral filling by impignement from aortic regurgitant jet. DDx - mitral stenosis(increases intensity with amyl nitrite)
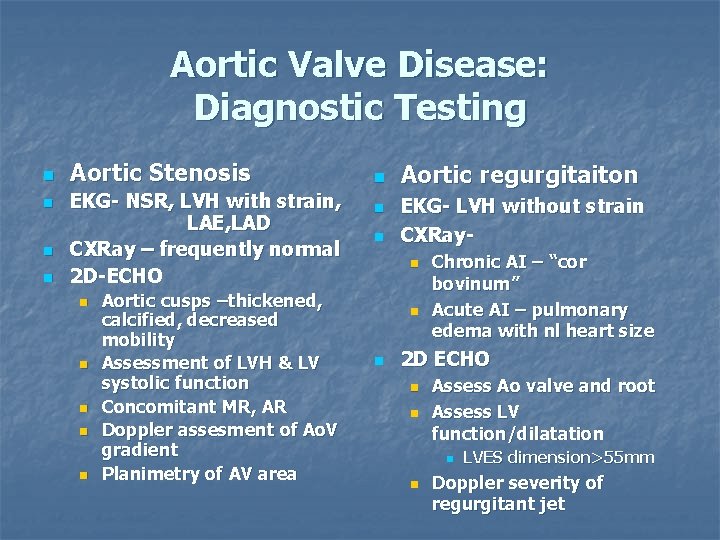
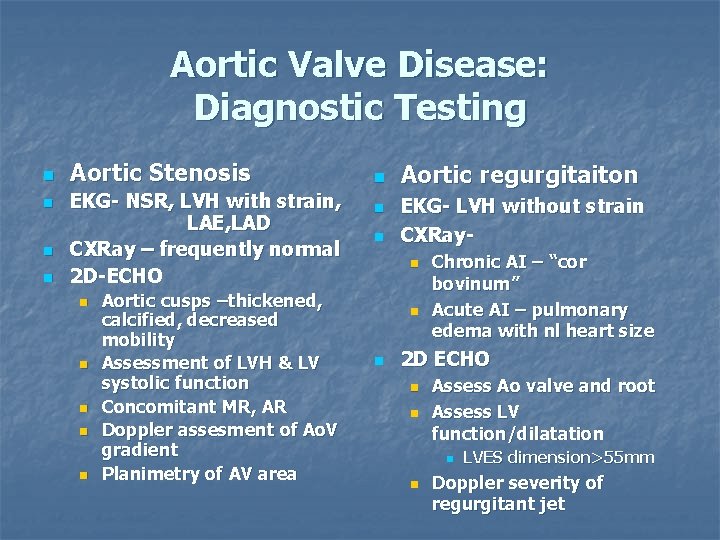
Aortic Valve Disease: Diagnostic Testing n n Aortic Stenosis EKG- NSR, LVH with strain, LAE, LAD CXRay – frequently normal 2 D-ECHO n n n Aortic cusps –thickened, calcified, decreased mobility Assessment of LVH & LV systolic function Concomitant MR, AR Doppler assesment of Ao. V gradient Planimetry of AV area n n n Aortic regurgitaiton EKG- LVH without strain CXRayn n n Chronic AI – “cor bovinum” Acute AI – pulmonary edema with nl heart size 2 D ECHO n n Assess Ao valve and root Assess LV function/dilatation n n LVES dimension>55 mm Doppler severity of regurgitant jet
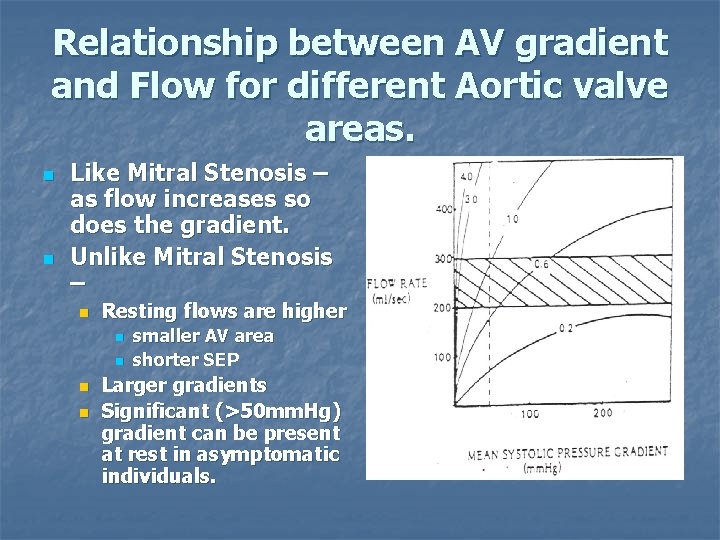
Relationship between AV gradient and Flow for different Aortic valve areas. n n Like Mitral Stenosis – as flow increases so does the gradient. Unlike Mitral Stenosis – n Resting flows are higher n n smaller AV area shorter SEP Larger gradients Significant (>50 mm. Hg) gradient can be present at rest in asymptomatic individuals.
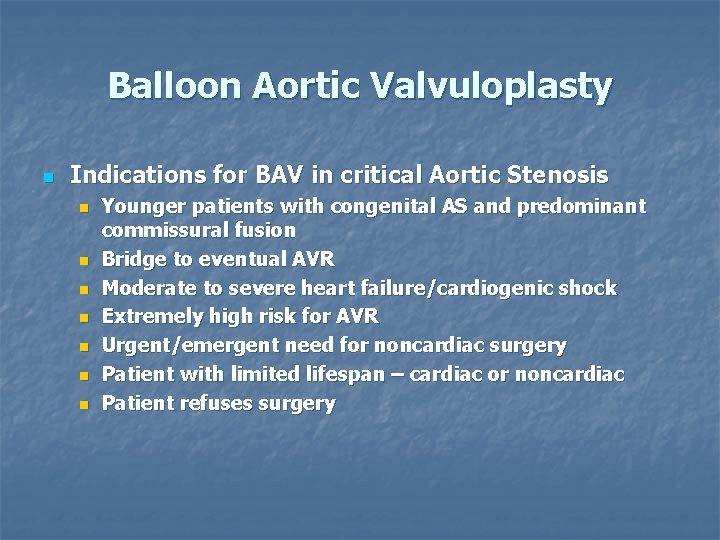
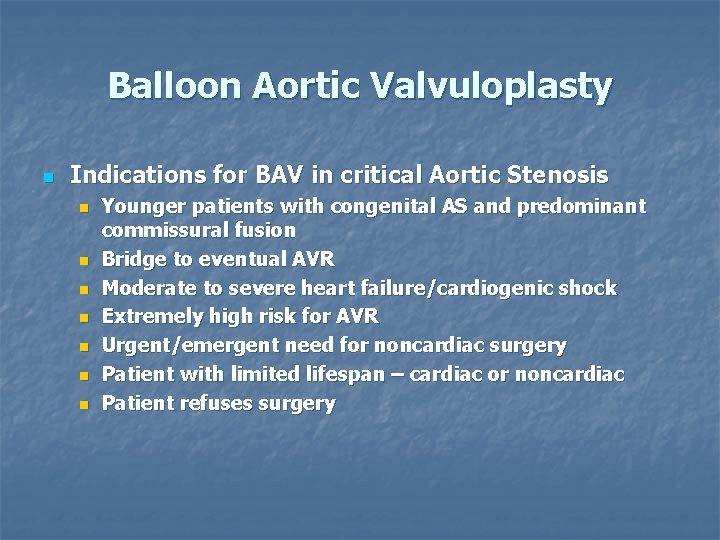
Balloon Aortic Valvuloplasty n Indications for BAV in critical Aortic Stenosis n n n n Younger patients with congenital AS and predominant commissural fusion Bridge to eventual AVR Moderate to severe heart failure/cardiogenic shock Extremely high risk for AVR Urgent/emergent need for noncardiac surgery Patient with limited lifespan – cardiac or noncardiac Patient refuses surgery
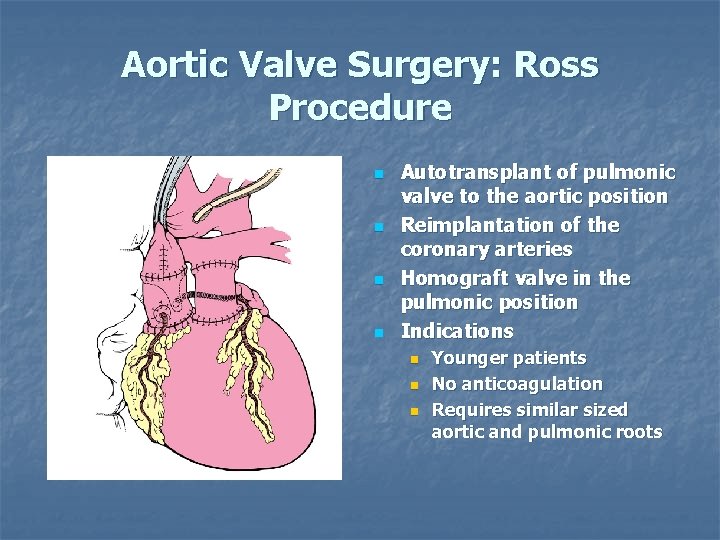
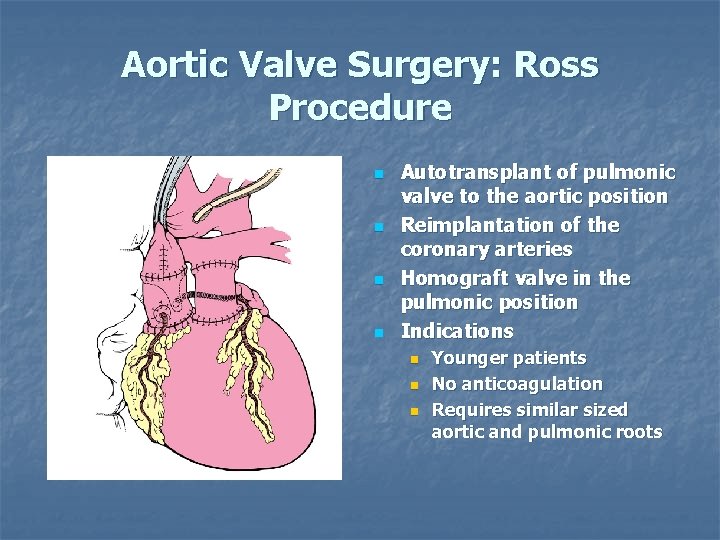
Aortic Valve Surgery: Ross Procedure n n Autotransplant of pulmonic valve to the aortic position Reimplantation of the coronary arteries Homograft valve in the pulmonic position Indications n n n Younger patients No anticoagulation Requires similar sized aortic and pulmonic roots
Valvular Heart Disease The End
 Upper lobe blood diversion
Upper lobe blood diversion Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Dopamine uses
Dopamine uses Causes of valvular heart disease
Causes of valvular heart disease Mitral regurgitation symptoms
Mitral regurgitation symptoms Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Causes of valvular heart disease
Causes of valvular heart disease Site:slidetodoc.com
Site:slidetodoc.com Right sided heart failure
Right sided heart failure Traslape valvular
Traslape valvular Bharathi viswanathan
Bharathi viswanathan Feline
Feline Strepsore
Strepsore /watch?v=0evgft8hgns
/watch?v=0evgft8hgns Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Difference between cyanotic and acyanotic heart disease
Difference between cyanotic and acyanotic heart disease Rhuematic fever
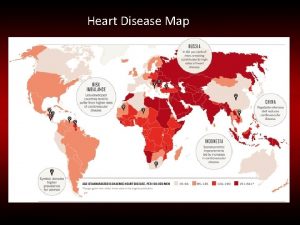
Rhuematic fever Heart disease data
Heart disease data Rheumatic heart disease causes
Rheumatic heart disease causes Nyha class
Nyha class Ahd heart
Ahd heart Asd vs pulmonary stenosis murmur
Asd vs pulmonary stenosis murmur Footbal player wordle
Footbal player wordle Coronary heart disease
Coronary heart disease Samina waqar
Samina waqar Modern treatment of heart disease
Modern treatment of heart disease Heart disease and stroke are the world's biggest killers
Heart disease and stroke are the world's biggest killers Farah garmany
Farah garmany Pediatric knee chest position
Pediatric knee chest position Ischemic heart disease classification
Ischemic heart disease classification Ischemic heart disease
Ischemic heart disease Terrible t's cyanotic heart disease
Terrible t's cyanotic heart disease Chronic rheumatic heart disease
Chronic rheumatic heart disease