ISCHEMIC HEART DISEASE Ischaemic heart disease IHD is
















- Slides: 41

ISCHEMIC HEART DISEASE
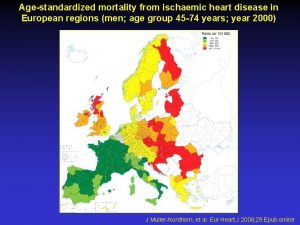
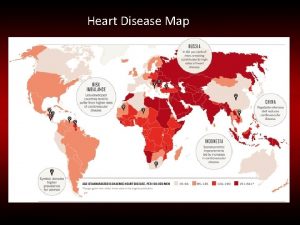
• Ischaemic heart disease (IHD) is defined as acute or chronic form of cardiac disability arising from imbalance between the myocardial supply and demand for oxygenated blood. • Alternate term ‘coronary artery disease (CAD)’. • IHD or CAD is the leading cause of death in most developed countries
ETIOPATHOGENESIS • IHD is invariably caused by disease affecting the coronary arteries. i) coronary atherosclerosis ii) superadded changes in coronary atherosclerosis iii) non-atherosclerotic causes
I. Coronary Atherosclerosis • Coronary atherosclerosis resulting in ‘fixed’ obstruction is the major cause of IHD in more than 90% cases.
1. Distribution. • Highest incidence being in the anterior descending branch of the left coronary, followed in decreasing frequency, by the right coronary artery and still less in circumflex branch of the left coronary. • About one third of cases have single-vessel disease, most often left anterior descending arterial involvement; another one-third have twovessel disease, and the remainder have three major vessel disease.
2. Location. • Significant stenotic lesions that may produce chronic myocardial ischaemia show more than 75% (threefourth) reduction in the cross-sectional area of a coronary artery or its branch. • The area of severest involvement is about 3 to 4 cm from the coronary ostia, more often at or near the bifurcation of the arteries.
3. Fixed atherosclerotic plaques. • The atherosclerotic plaques in the coronaries are more often eccentrically located bulging into the lumen from one side. • There may be concentric thickening of the wall of the artery. • Complications like calcification, coronary thrombosis, ulceration, haemorrhage, rupture and aneurysm formation.
II. Superadded Changes in Coronary Atherosclerosis • The attacks of acute coronary syndromes, are precipitated by certain changes superimposed on a pre-existing fixed coronary atheromatous plaque. 1. Acute changes in chronic atheromatous plaque 2. Coronary artery thrombosis 3. Local platelet aggregation and coronary artery spasm.

III. Non-atherosclerotic Causes • Cause IHD in less than 10% of cases. 1. Vasospasm 2. Stenosis of coronary ostia 3. Arteritis 4. Embolism 5. Thrombotic diseases 6. Trauma 7. Aneurysms 8. Compression
EFFECTS OF MYOCARDIAL ISCHAEMIA • Development of lesions in the coronaries is not always accompanied by cardiac disease. • Depending upon the suddenness of onset, duration, degree, location and extent of the area affected by myocardial ischaemia, the range of changes and clinical features may vary from an asymptomatic state at one extreme to immediate mortality at another.

EFFECTS OF MYOCARDIAL ISCHAEMIA

• The term acute coronary syndromes include a triad of Øacute myocardial infarction Øunstable angina Øsudden cardiac death
ANGINA PECTORIS • Angina pectoris is a clinical syndrome of IHD resulting from transient myocardial ischaemia. • Characterised by paroxysmal pain in the substernal or precordial region of the chest which is aggravated by an increase in the demand of the heart and relieved by a decrease in the work of the heart. • Often, the pain radiates to the left arm, neck, jaw or right arm. • More common in men past 5 th decade of life.
• There are 3 overlapping clinical patterns of angina pectoris with some differences in their pathogenesis: i) Stable or typical angina ii) Prinzmetal’s variant angina iii) Unstable or crescendo angina

ACUTE MYOCARDIAL INFARCTION • Most important and feared consequence of coronary artery disease. • Many patients may die within the first few hours of the onset, while remainder suffer from effects of impaired cardiac function. • A significant factor that may prevent or diminish the myocardial damage is the development of collateral circulation through anastomotic channels over a period of time.

INCIDENCE • In developed countries, acute MI accounts for 10 -25% of all deaths. • Age. • Occur at all ages, though the incidence is higher in the elderly. • About 5% of heart attacks occur in young people under the age of 40 years, • Sex. • Males throughout their life are at a significantly higher risk
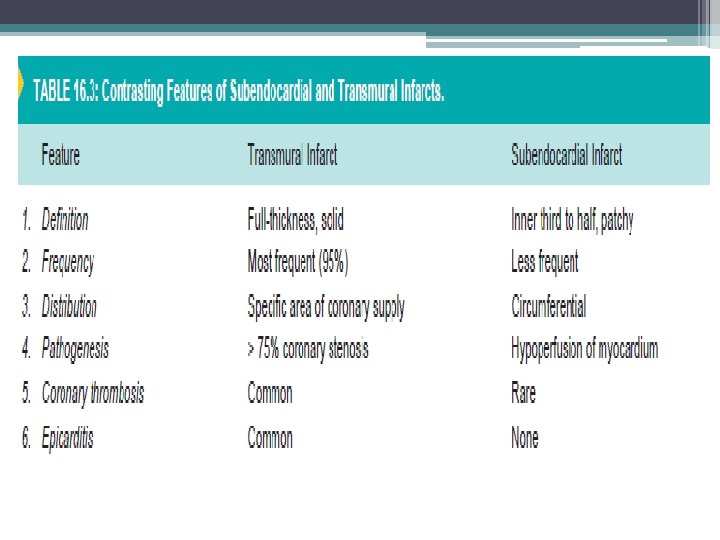
ETIOPATHOGENESIS • Features in the development of acute MI are: 1. Myocardial ischaemia 2. Role of platelets 3. Acute plaque rupture 4. Non-atherosclerotic causes 5. Transmural versus subendocardial infarcts
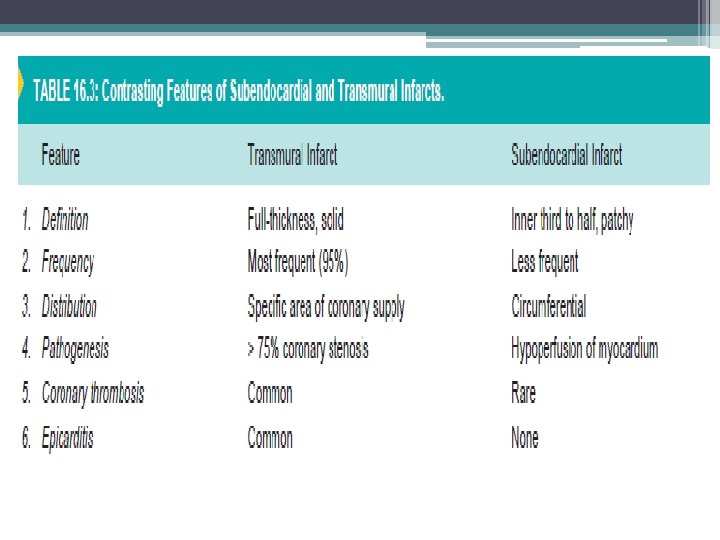

LOCATION OF INFARCTS
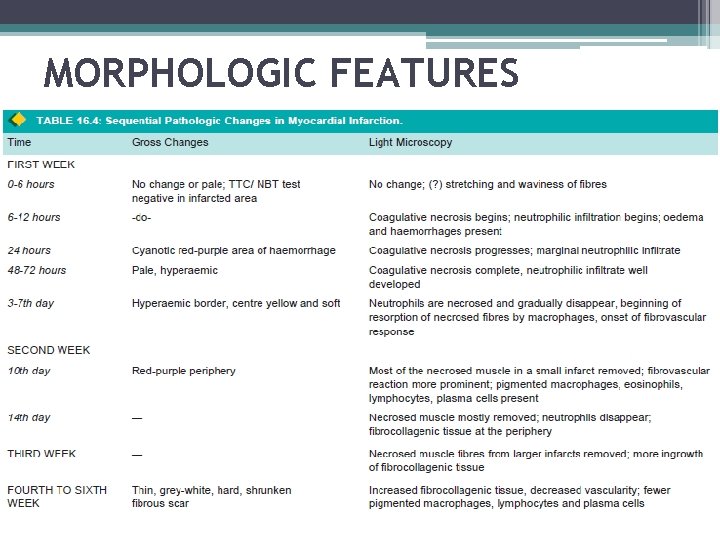
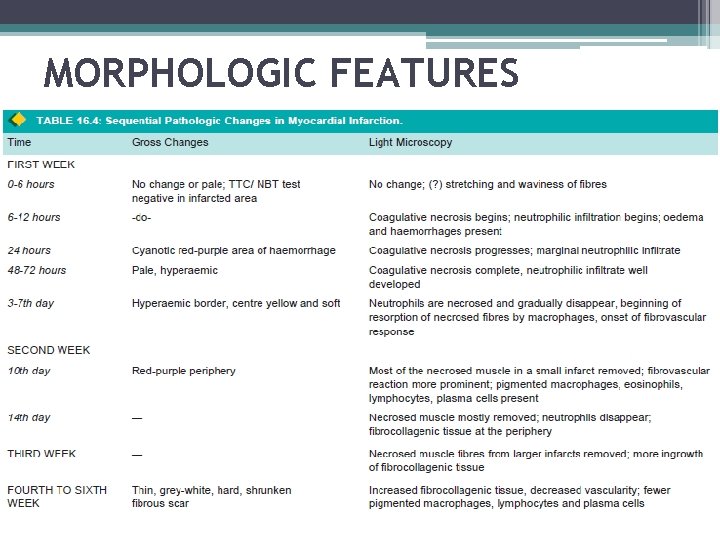
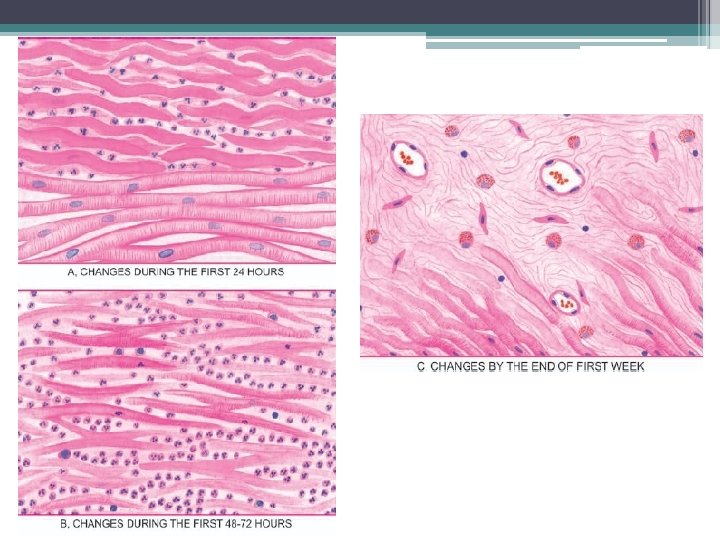
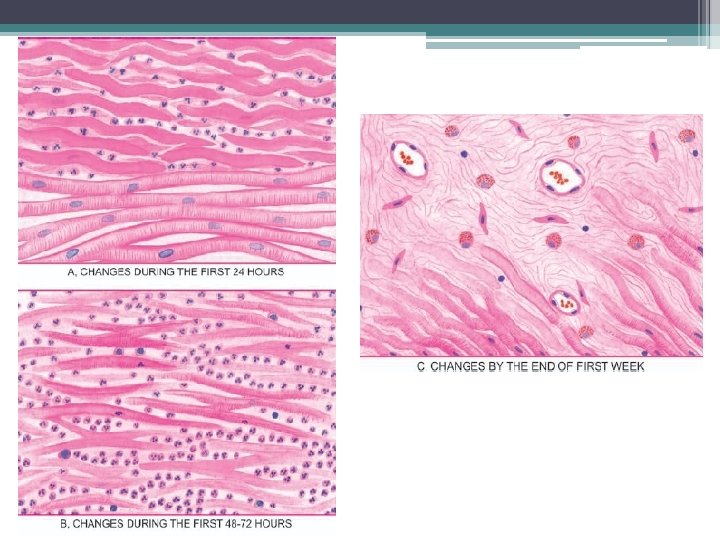
MORPHOLOGIC FEATURES


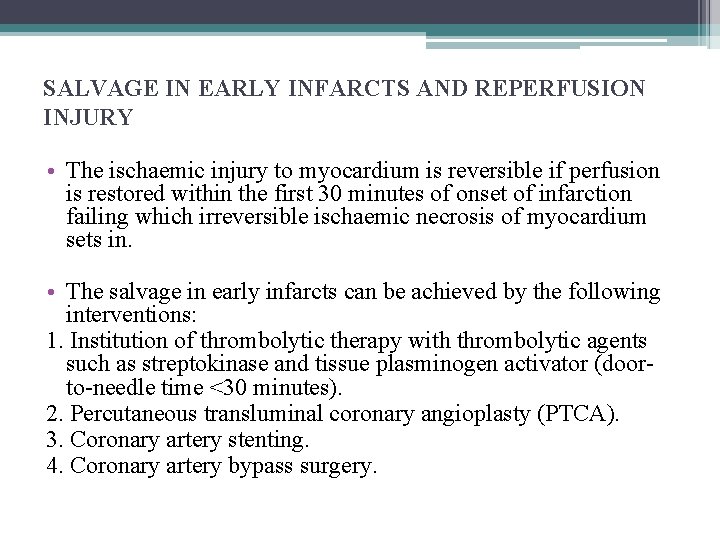
SALVAGE IN EARLY INFARCTS AND REPERFUSION INJURY • The ischaemic injury to myocardium is reversible if perfusion is restored within the first 30 minutes of onset of infarction failing which irreversible ischaemic necrosis of myocardium sets in. • The salvage in early infarcts can be achieved by the following interventions: 1. Institution of thrombolytic therapy with thrombolytic agents such as streptokinase and tissue plasminogen activator (doorto-needle time <30 minutes). 2. Percutaneous transluminal coronary angioplasty (PTCA). 3. Coronary artery stenting. 4. Coronary artery bypass surgery.

• Risk of ischaemic reperfusion injury. • Further myonecrosis during reperfusion occurs due to rapid influx of calcium ions and generation of toxic oxygen free radicals. • Grossly, the myocardial infarct following reperfusion injury appears haemorrhagic rather than pale. • Microscopically, myofibres show contraction band necrosis which are transverse and thick eosinophilic bands.
CHANGES IN EARLY INFARCTS. • By special techniques like electron microscopy, chemical and histochemical studies, changes can be demonstrated in early infarcts before detectable light microscopic alterations appear. 1. Electron microscopic changes. • Evident in less than half an hour on onset of infarction. i) Disappearance of perinuclear glycogen granules within 5 minutes of ischaemia. ii) Swelling of mitochondria in 20 to 30 minutes. iii) Disruption of sarcolemma. iv) Nuclear alterations like peripheral clumping of nuclear chromatin.
2. Chemical and histochemical changes. i) Glycogen depletion in myocardial fibres within 30 to 60 minutes of infarction. ii) Increase in lactic acid in the myocardial fibres. iii) Loss of K+ from the ischaemic fibres. iv) Increase of Na+ in the ischaemic cells. v) Influx of Ca++ into the cells causing irreversible cell injury.
• Based on the above observations and on leakage of enzymes from the ischaemic myocardium, alterations in the concentrations of various enzymes are detected in the blood of these patients.

DIAGNOSIS • The diagnosis of acute MI is made on the observations of 3 types of features Øclinical features ØECG changes Øserum enzyme determinations

1. Clinical features i) Pain ii) Indigestion iii) Apprehension iv) Shock v) Oliguria: Urine flow is usually less than 20 ml per hour. vi) Low grade fever vii) Acute pulmonary oedema

2. ECG changes

3. Serum cardiac markers i) Creatine phosphokinase (CK) and CK-MB ii) Lactic dehydrogenase (LDH) iii) Cardiac-specific troponins (c. Tn) iv) Myoglobin
COMPLICATIONS 1. Arrhythmias 2. Congestive heart failure 3. Cardiogenic shock 4. Mural thrombosis and thromboembolism 5. Rupture 6. Cardiac aneurysm 7. Pericarditis 8. Postmyocardial infarction syndrome
CHRONIC ISCHAEMIC HEART DISEASE • Chronic ischaemic heart disease, ischaemic cardiomyopathy or myocardial fibrosis, are the terms used for focal or diffuse fibrosis in the myocardium characteristically found in elderly patients of progressive IHD. • Such small areas of fibrous scarring are commonly found in the heart of patients who have history of episodes of angina and attacks of MI some years back. • Gradually developing CHF due to decompensation over a period of years. • Occasionally, serious cardiac arrhythmias or infarction may supervene and cause death.
ETIOPATHOGENESIS • In majority of cases, coronary atherosclerosis causes progressive ischaemic myocardial damage and replacement by myocardial fibrosis. • A small percentage of cases may result from other causes such as emboli, coronary arteritis and myocarditis.
MORPHOLOGIC FEATURES Grossly • Heart may be normal in size or hypertrophied. • Left ventricular wall generally shows foci of grey-white fibrosis in brown myocardium. • Healed scars of previous MI may be present. • Valves of the left heart may be distorted, thickened and show calcification. • Coronary arteries invariably show moderate to severe atherosclerosis.

• Microscopically i) There are scattered areas of diffuse myocardial fibrosis, especially around the small blood vessels in the interstitial tissue of the myocardium. ii) Intervening single fibres and groups of myocardial fibres show variation in fibre size and foci of myocytolysis. iii) Areas of brown atrophy of the myocardium may also be present. iv) Coronary arteries show atherosclerotic plaques and may have complicated lesions in the form o superimposed thrombosis.

SUDDEN CARDIAC DEATH • Sudden cardiac death is defined as sudden death within 24 hours of the onset of cardiac symptoms. • Most important cause is coronary atherosclerosis; less commonly it may be due to coronary vasospasm and other non-ischaemic causes. • These include: calcific aortic stenosis, myocarditis of various types, hypertrophic cardiomyopathy, mitral valve prolapse, endocarditis, and hereditary and acquired defects of the conduction system.
• The mechanism of sudden death by myocardial ischaemia is almost always by fatal arrhythmias, chiefly ventricular asystole or fibrillation.
MORPHOLOGIC FEATURES • At autopsy, critical atherosclerotic coronary narrowing (more than 75% compromised lumen) in one or more of the three major coronary arterial trunks with superimposed thrombosis or plaquehaemorrhage. • Healed and new myocardial infarcts are found in many cases.
 Heart disease
Heart disease Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Chronic coronary syndrome
Chronic coronary syndrome Cincinatti stroke scale
Cincinatti stroke scale Ihd
Ihd Pathology
Pathology Ihd
Ihd Mean bp formula
Mean bp formula Acute ischemic stroke algorithm
Acute ischemic stroke algorithm Cns ischemic response
Cns ischemic response Ischemic vs hemorrhagic stroke
Ischemic vs hemorrhagic stroke Optic ischemic neuropathy
Optic ischemic neuropathy Tenecteplase stroke
Tenecteplase stroke Mechanism of ischemic stroke
Mechanism of ischemic stroke Cns ischemic response
Cns ischemic response Ischemic bile duct injury
Ischemic bile duct injury Haemorrhage
Haemorrhage Bharathi viswanathan
Bharathi viswanathan Coronary heart disease
Coronary heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Feline
Feline Farah garmany
Farah garmany Site:slidetodoc.com
Site:slidetodoc.com Causes of valvular heart disease
Causes of valvular heart disease Charyties
Charyties Rheumatic heart disease
Rheumatic heart disease Nyha classification of heart disease
Nyha classification of heart disease Causes of valvular heart disease
Causes of valvular heart disease Heart disease data
Heart disease data Heart disease symptoms
Heart disease symptoms Heart disease
Heart disease 5 terrible ts
5 terrible ts Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Tetralogy of fallot xray
Tetralogy of fallot xray Rheumatic heart disease causes
Rheumatic heart disease causes Heart disease and stroke are the world's biggest killers
Heart disease and stroke are the world's biggest killers Preload and afterload
Preload and afterload Rheumatic heart disease
Rheumatic heart disease Pico question examples heart disease
Pico question examples heart disease Rhuematic fever
Rhuematic fever Right sided heart failure
Right sided heart failure Tet spell
Tet spell