Cardiovascular Disorders Coronary heart disease Coronary heart disease













- Slides: 49
Cardiovascular Disorders Coronary heart disease
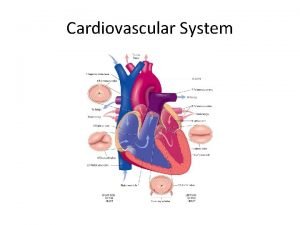
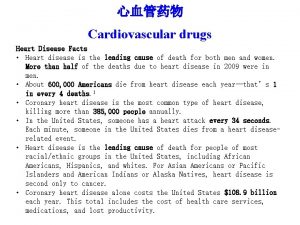
Coronary heart disease • Coronary heart disease (CHD), sometimes described as coronary artery disease (CAD) or ischemic heart disease (IHD), is a condition in which the vascular supply to the heart is impeded by atheroma, thrombosis or spasm of coronary arteries. • This may impair the supply of oxygenated blood to cardiac tissue sufficiently to cause myocardial ischemia which, if severe or prolonged, may cause the death of cardiac muscle cells.
Coronary heart disease • Myocardial ischemia occurs when the oxygen demand exceeds myocardial oxygen supply. The resultant ischemic myocardium releases adenosine, the main mediator of chest pain, by stimulating the A 1 receptors located on the cardiac nerve endings. • Myocardial ischemia may be ‘silent’ if the duration is of insufficient length, the afferent cardiac nerves are damaged (as with diabetics) or there is inhibition of the pain at the spinal or supraspinal level.

Coronary heart disease

Coronary heart disease Factors increasing myocardial oxygen demand often precipitate ischemic episodes and are commonly associated with: - Increased work rate (heart rate) and increased work load (force of contractility). - Ischemia can also arise if oxygen demand is abnormally increased, as may occur in patients with thyrotoxicosis or severe ventricular hypertrophy due to hypertension.

Coronary heart disease - Atheromatous plaques decrease the lumen diameter and, when extensive, reduce the ability of the coronary artery to dilate in response to increased myocardial oxygen demand. - Ischemia may also occur when the oxygen-carrying capacity of blood is impaired, as in iron deficiency anaemia, or when the circulatory volume is depleted.
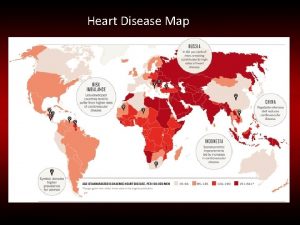
Coronary heart disease Factors that increase the risk of developing CHD Cigarette smoking Raised serum cholesterol Hypertension Diabetes Abdominal obesity Increased personal stress

Coronary heart disease Factors that decrease the risk of CHD Regular consumption of fresh fruit and vegetables Regular exercise Moderate alcohol consumption Modification of factors that increase the risk of CHD
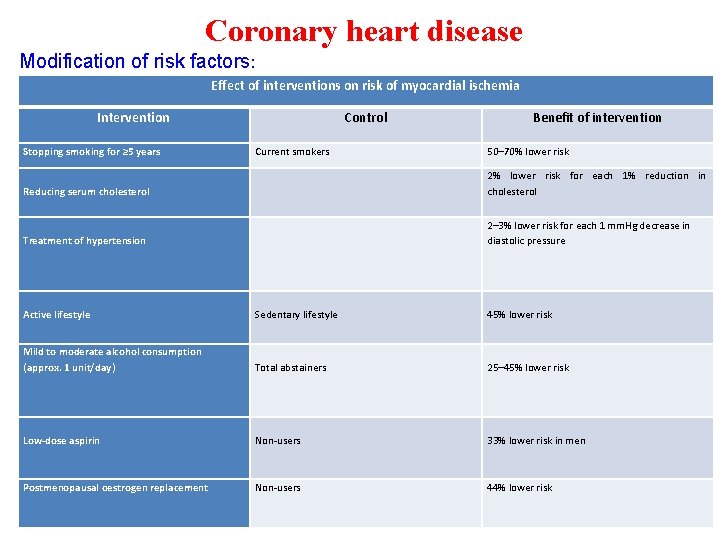
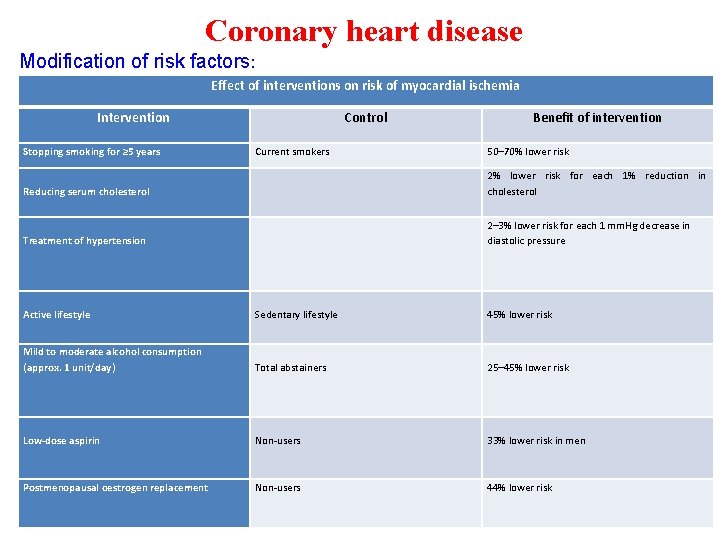
Coronary heart disease Modification of risk factors: Effect of interventions on risk of myocardial ischemia Intervention Stopping smoking for ≥ 5 years Control Current smokers Benefit of intervention 50– 70% lower risk Reducing serum cholesterol 2% lower risk for each 1% reduction in cholesterol Treatment of hypertension 2– 3% lower risk for each 1 mm. Hg decrease in diastolic pressure Active lifestyle Sedentary lifestyle 45% lower risk Mild to moderate alcohol consumption (approx. 1 unit/day) Total abstainers 25– 45% lower risk Low-dose aspirin Non-users 33% lower risk in men Postmenopausal oestrogen replacement Non-users 44% lower risk

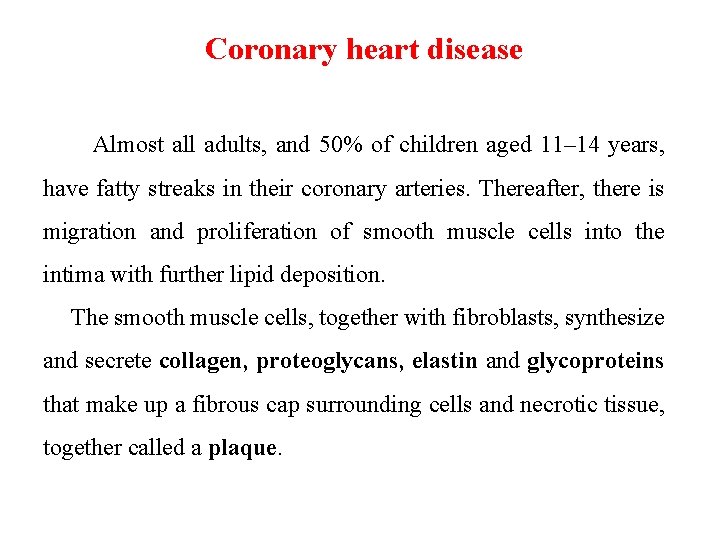
Coronary heart disease Etiology & Pathophysiology The vast majority of CHD occurs in patients with atherosclerosis of the coronary arteries that starts before adulthood. The cause of spontaneous artherosclerosis is unclear, although it is thought that in the presence of hypercholesterolaemia, a non-denuding form of injury occurs to the endothelial lining of coronary arteries and other vessels. This injury is followed by subendothelial migration of monocytes and the accumulation of fatty streaks containing lipid rich- macrophages and T-cells.
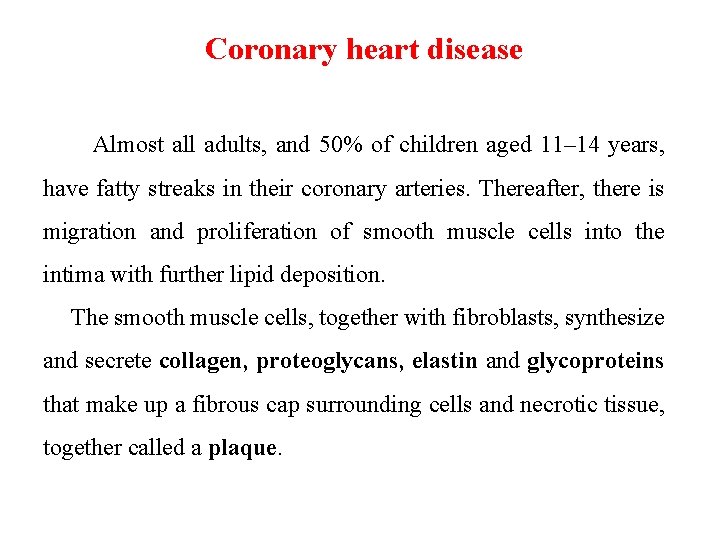
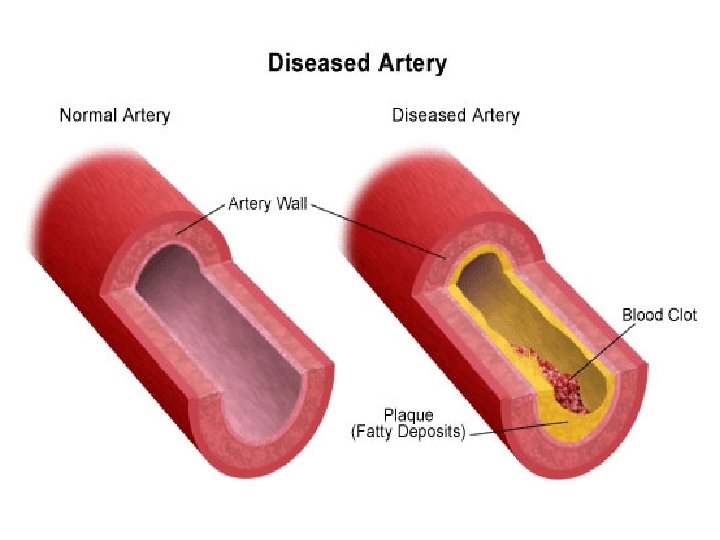
Coronary heart disease Almost all adults, and 50% of children aged 11– 14 years, have fatty streaks in their coronary arteries. Thereafter, there is migration and proliferation of smooth muscle cells into the intima with further lipid deposition. The smooth muscle cells, together with fibroblasts, synthesize and secrete collagen, proteoglycans, elastin and glycoproteins that make up a fibrous cap surrounding cells and necrotic tissue, together called a plaque.
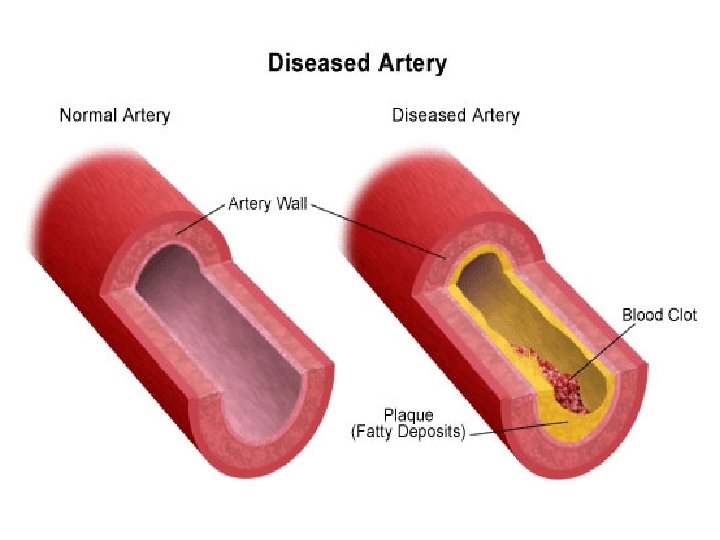
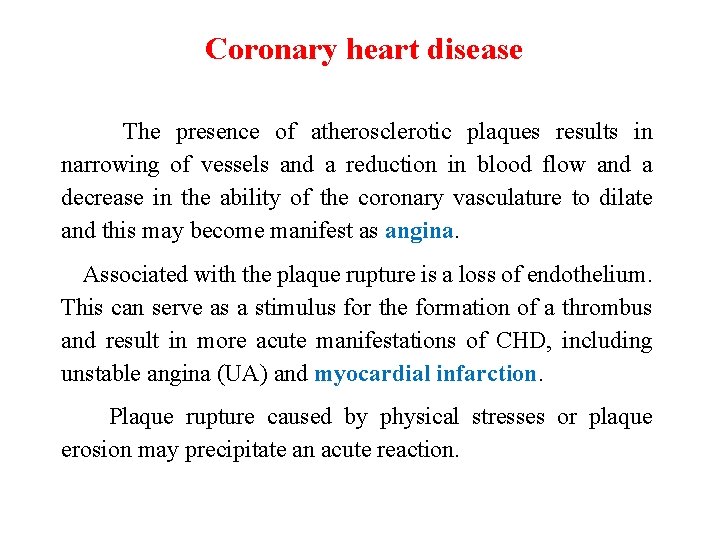
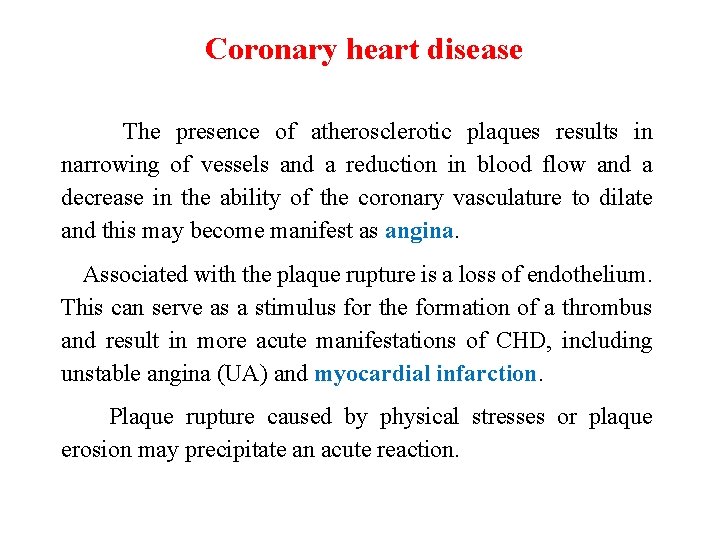
Coronary heart disease The presence of atherosclerotic plaques results in narrowing of vessels and a reduction in blood flow and a decrease in the ability of the coronary vasculature to dilate and this may become manifest as angina. Associated with the plaque rupture is a loss of endothelium. This can serve as a stimulus for the formation of a thrombus and result in more acute manifestations of CHD, including unstable angina (UA) and myocardial infarction. Plaque rupture caused by physical stresses or plaque erosion may precipitate an acute reaction.
Coronary heart disease Other pathological processes are probably involved, including: - Endothelial dysfunction which alters the fibrin–fibrinolysis balance and the vasoconstriction–vasodilation balance. There is interest in the role of statins and angiotensin-converting enzyme (ACE) inhibitors in modifying endothelial function. - Inflammation, many plaques are found to contain inflammatory cells and inflammatory damage is found at the sites of plaque rupture. - Oxidative stress which involves the uncontrolled production of reactive oxygen species (ROS) or a reduction in antioxidant species has been linked in the laboratory to several aspects of cardiovascular pathogenesis including endothelial malfunction, lipid metabolism, atheroma formation and plaque rupture.

Coronary heart disease Clinical manifestation: The primary clinical manifestation of CHD is chest pain. Chest pain arising from stable coronary atheromatous disease leads to stable angina and normally arises when narrowing of the coronary artery lumen exceeds 50% of the original luminal diameter. Stable angina is characterized by chest pain and breathlessness on exertion; symptoms are relieved promptly by rest.
Coronary heart disease A stable coronary atheromatous plaque may become unstable as a result of either plaque erosion or rupture. This may stimulates the formation of thrombus (by subendothelial lipid and collagen) which causes sudden narrowing of the vessel. The clinical outcomes results under the term of acute coronary syndrome (ACS) which characterized by chest pain of increasing severity either on minimal exertion or, more commonly, at rest (unstable angina). These patients are at high risk of myocardial infarction and death and require hospitalization.
Coronary heart disease Stable angina is a clinical syndrome characterized by discomfort in the chest, jaw, shoulder, back, or arms, typically elicited by exertion or emotional stress and relieved by rest or nitroglycerin. Usually, the discomfort occurs after a predictable level of exertion, classically when climbing hills or stairs, and resolves within a few minutes on resting. Unfortunately, the clinical manifestations of angina are very variable. Many patients mistake the discomfort for indigestion. Some patients, particularly diabetics and the elderly, may not experience pain at all but present with breathlessness or fatigue; this is termed silent ischemia.

Coronary heart disease Diagnosis: In addition to clinical assessment, further investigations are needed to confirm the diagnosis and assess the need for intervention. - Electrocardiogram (ECG): is normal in more than 50% of patients with angina. However, abnormal ECG may increase the probability of coronary disease; in particular, it may show signs of previous myocardial infarction. - X-ray images: obtained permit confirmation of the diagnosis, aid assessment of prognosis and guide therapy.
Coronary heart disease - Exercise testing: is useful both in confirming the diagnosis and in giving a guide to prognosis. - Coronary angiography: is regarded as the gold standard for the assessment of CHD and involves the passage of a catheter through the arterial circulation and the injection of radioopaque contrast media into the coronary arteries. - Non-invasive techniques: including magnetic resonance imaging (MRI) and multi-slice CT scanning are being developed and tested as alternatives to angiography.


Coronary heart disease Treatment of stable angina: Is based on two principles: • Improve prognosis by preventing myocardial infarction and death. • Relieve or prevent symptoms. Before starting medication therapy; diabetes, hypertension and dyslipidemia in patients with stable angina should be well controlled. Smoking cessation, with or without pharmacological support, and weight loss should be attempted.
Coronary heart disease Symptom relief and prevention In stable angina, much of the drug treatment is directed towards decreasing the workload of the heart and, to a lesser extent, improving coronary blood supply; this provides symptomatic relief and improves prognosis. Therapy to decrease workload is targeted at both decreasing afterload and controlling heart rate. Recent evidence suggests a prognostic benefit when the resting heart rate is controlled below 70 beats/min.
Coronary heart disease Drug treatment is initiated in a stepwise fashion according to symptom relief and side effects. Some patients will require a number of anti-anginal medicines to control their angina symptoms.
Coronary heart disease β-Blockers - They reduce myocardial oxygen demand by blocking βadrenergic receptors, thereby decreasing the heart rate and the force of left ventricular contraction and lowering blood pressure. - The decreased heart rate not only reduces the energy demand on the heart but also permits better perfusion of the subendocardium by the coronary circulation. - β-Blockers may also reduce energy-demanding supraventricular or atrial arrhythmias and counteract the cardiac effects of hyperthyroidism or phaeochromocytoma.
Coronary heart disease - β-Blockers are particularly useful in exertional angina - Patients treated optimally should have a resting heart rate of around 60 beats/min. - β-Blockers should be used with caution in patients with diabetes as the production of insulin is under adrenergic system control and thus their concomitant use may worsen glucose control.
Coronary heart disease - β-Blockers can also mask the symptoms of hypoglycaemia and patients in whom the combination is considered of value should be warned of this. - Their tendency to cause bronchospasm and peripheral vascular spasm means that they are contraindicated in patients with asthma, and used with caution in chronic obstructive airways diseases and peripheral vascular disease as well as in acute heart failure and bradycardia.
Coronary heart disease - Cardioselective agents such as atenolol, bisoprolol and metoprolol are preferred because of their reduced tendency to cause bronchoconstriction, but no β-blocker is completely specific for the heart. - Agents with high lipophilicity, for example, propranolol and metoprolol penetrate CNS and cause nightmares, hallucinations and depression that should not be used in patients with psychiatric disorders.
Coronary heart disease - β-Blockers should not be stopped abruptly for fear of precipitating angina through rebound receptor hypersensitivity. - They are contraindicated in the rare Prinzmetal's angina where coronary spasm is a major factor. - All β-blockers tend to reduce renal blood flow, but this is only important in renal impairment. Drugs eliminated by the kidney (Atenlon, Nadalol & sotalol) may need to be given at lower doses in the renally impaired or in the elderly.
Coronary heart disease Calcium channel blockers (CCBs) - Act on a variety of smooth muscle and cardiac tissues and there a large number of agents which have differing specificities for different body tissues. - Dihydropyridines have no effect on the conducting tissues and are effective arterial dilators, decreasing afterload and improving coronary perfusion but also causing flushing, headaches and reflex tachycardia.

Coronary heart disease - Longer acting dihydropyridines , for example, amlodipine and felodipine or longer acting formulations, for example, nifedipine LA, have demonstrated symptom-relieving potential. - Deltiazem & verapamil, have also been shown to improve symptom control, reduce the frequency of anginal attacks and increase exercise tolerance.
Coronary heart disease - They are suitable for rate control patients in whom β-blockers are contraindicated in regards to respiratory or peripheral vascular disease. - They should be used with caution in patients already receiving β-blockers, as bradycardia and heart block have been reported with this combination. - CCBs have a particular role in the management of Prinzmetal's (variant) angina which is thought to be due to coronary artery spasm.
Coronary heart disease Nitrates Organic nitrates are valuable in angina because: - They dilate veins and thereby decrease preload, dilate arteries to a lesser extent thereby decreasing afterload. - Promote flow in collateral coronary vessels, diverting blood from the epicardium to the endocardium. - They are available in many forms, but all can relax vascular smooth muscle by releasing nitric oxide, which was formerly known as endothelium-derived relaxing factor.
Coronary heart disease Tolerance is one of the main limitations to the use of nitrates: - This develops rapidly, and a ‘nitrate-free’ period of a few hours in each 24 -h period is beneficial in maintaining the effectiveness of treatment. - The nitrate-free period should coincide with the period of lowest risk, and this is usually night time, but not early morning, which is a high-risk period for infarction. - Many patients receiving short-acting nitrates two or three times a day would do well to have their doses between 7 a. m. and 6 p. m. (say, 8 a. m. and 2 p. m. for ISMN).
Coronary heart disease There are many nitrate preparations available, including intravenous infusions, conventional or slow-release tablets and capsules, transdermal patches, sublingual tablets and sprays and adhesive buccal tablets. - Three main nitrates are used: GTN (mainly for sublingual, buccal, transdermal and intravenous routes), ISDN and ISMN. - The sublingual preparations whether sprays or suckable or chewable tablets, are used for the prevention or relief of acute attacks of pain but may induce side effects like: hypotension with dizziness and fainting, and a throbbing headache.
Coronary heart disease - Sustained release tablets do not release the drug over the whole 24 -h period producing a ‘nitrate free period’, whereas patches need to be removed for a few hours each day. - ISDN is metabolized to the mononitrate, whereas the dinitrate is usually given three or four times a day, the mononitrate is given once or twice a day.
Coronary heart disease Nicorandil - Nicorandil is a compound that exhibits the properties of a nitrate but which also activates ATP-dependent potassium channels. Ivabradine - Ivabridine is similar in efficacy to B-BLs and CCBs and may be of particular use in patients in whom β-blockers are contraindicated (symptomatic treatment of chronic stable angina pectoris. - The most frequent adverse drug reactions are dose-dependent transient visual symptoms.
Coronary heart disease Ranolazine - Ranolazine, a selective inhibitor of sodium influx (that current leads to reductions in elevated intracellular calcium levels), attenuates the abnormalities of ventricular repolarization and contractility associated with ischaemia. - It has been shown to increase exercise tolerance, reduce anginal episodes and reduce the use of GTN. - Ranolazine seems to be a safe addition to current traditional drugs for chronic stable angina, especially in aggressive multidrug regimens. - Side effects include dizziness, constipation, & nausea.
Coronary heart disease Maintenance treatment & prevention of thrombus formation One of the major complications arising from atheromatous plaque is thrombus formation. This causes an increase in plaque size and may result in myocardial infarction. Antiplatelet agents, in particular aspirin, are effective in preventing platelet activation and thus thrombus formation.

Coronary heart disease
Coronary heart disease Aspirin acts via irreversible inhibition of platelet COX-1 and thus thromboxane production, which is normally complete action with chronic dosing of 75 mg/day. This antiplatelet action is apparent within an hour of taking a dose of 300 mg. The optimal maintenance dose seems to be 75– 150 mg day, with lower doses having limited cardiac risk protection and higher doses increasing the risk of gastro-intestinal side effects (dyspepsia):
Coronary heart disease - Patients should be advised to take the medicine with or immediately after food. - Enteric-coated preparations are no safer - Patients with ongoing symptoms of dyspepsia may require concomitant acid suppression with a proton pump inhibitor or switching to clopidogrel. - Aspirin may produce allergy, including bronchospasm.

Coronary heart disease Clopidogrel inhibits ADP activation of platelets and is useful as an alternative to aspirin in patients who are allergic or cannot tolerate aspirin. The usual dose is 300 mg once, then 75 mg daily. Although less likely to cause gastric erosion and ulceration, gastro-intestinal bleeding is still a major complication of clopidogrel therapy. There is evidence that the combination of a proton pump inhibitor and aspirin is as effective as using clopidogrel alone in patients with a history of upper gastro-intestinal bleeding.
Coronary heart disease ACE inhibitors are established treatments for hypertension and heart failure, and have proven beneficial post myocardial infarction. - Cause vasodilation by inhibiting the production of angiotensin II. - ACE inhibitors have anti-inflammatory, antithrombotic and antiproliferative properties. Some of these effects are mediated by actions on vascular endothelium and might be expected to be of benefit in all patients with CHD. - ACE inhibitors also reduce the production of ROS.
Coronary heart disease The use of ACE inhibitors in patients without myocardial infarction or left ventricular damage is based on trials: - Identified a delay in the onset of diabetes mellitus in susceptible individuals which may be of long-term benefit to them. - secondary prevention, investigated the effect of ACE inhibitor on patients over 55 years old who had known atherosclerotic disease or diabetes plus one other cardiovascular risk factor.
Coronary heart disease - The use of ACE inhibitor (ramipril) decreased the combined endpoint of stroke, myocardial infarction or cardiovascular death by approximately 22%, and the benefits were independent of blood pressure reduction.
Coronary heart disease Statins should be prescribed alongside lifestyle advice for both primary prevention of CVD and in those with established CVD. All patients with coronary risk factors benefit from reduction of their serum cholesterol level (especially lowdensity lipoprotein-cholesterol LDL-C) in patients with CHD. It is now clear that there is no ‘safe’ level of cholesterol for patients with CHD.
Coronary heart disease In addition to cholesterol-lowering properties, statins also have: - antithrombotic, anti-inflammatory and antiproliferative properties. - They are also important in restoring normal endothelial function and inhibit the production of ROS in the vessel wall. - In most patients with stable angina; these drugs may have beneficial effects independent of cholesterol lowering and this makes them valuable even in patients with ‘normal’cholesterol levels.

 Coronary heart disease
Coronary heart disease Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 The assistant chapter 40
The assistant chapter 40 Coronary artery disease
Coronary artery disease Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Cardiovascular disease risk factor
Cardiovascular disease risk factor The cardiovascular system chapter 11
The cardiovascular system chapter 11 Coronary groove of heart
Coronary groove of heart Circulatory system crash course
Circulatory system crash course Coronary circulation of heart
Coronary circulation of heart Bharathi viswanathan
Bharathi viswanathan Coronary personality
Coronary personality Coronary calcium score guidelines
Coronary calcium score guidelines Acute coronary syndrome
Acute coronary syndrome Dipyrimadole
Dipyrimadole Cantiles line
Cantiles line Right atrioventricular valve
Right atrioventricular valve Mesa coronary calcium score
Mesa coronary calcium score Classification of antianginal drugs
Classification of antianginal drugs Coronary sinusoids
Coronary sinusoids Heart
Heart Qfr coronary
Qfr coronary Coronary ligament
Coronary ligament Sircumflex
Sircumflex Coronary circulation
Coronary circulation Pericardiu
Pericardiu Mesa coronary calcium score
Mesa coronary calcium score Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Cpr routine
Cpr routine Heart veins
Heart veins Coronary blood flow
Coronary blood flow Heart disease
Heart disease Annulus of vieussens
Annulus of vieussens Coronary sulcus
Coronary sulcus Thebasian veins
Thebasian veins Worm like amphibian
Worm like amphibian Anterior aortic sinus
Anterior aortic sinus Pk papyrus stent
Pk papyrus stent Coronary circulation animation
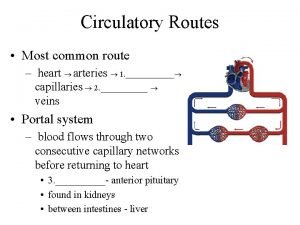
Coronary circulation animation Coronary circulatory routes
Coronary circulatory routes Global registry of acute coronary events
Global registry of acute coronary events Chapter 11 the cardiovascular system figure 11-2
Chapter 11 the cardiovascular system figure 11-2 Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Rutas integrales de atencion en salud
Rutas integrales de atencion en salud Aparato cardiovascular
Aparato cardiovascular Chapter 16 cardiovascular emergencies
Chapter 16 cardiovascular emergencies Ptca
Ptca Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Cardiovascular system
Cardiovascular system Cardiovascular drift
Cardiovascular drift