Pulmonary Atresia with Intact Ventricular Septum Ali Sepahdari
- Slides: 21
Pulmonary Atresia with Intact Ventricular Septum Ali Sepahdari, MD University of Illinois at Chicago
Background Rare lesion accounting for 1 -1. 5% of all congenital heart disease Complex disease with commonly associated abnormalities of the tricuspid valve, RV, coronary arteries, and left heart. Treatment options vary depending on severity of disease
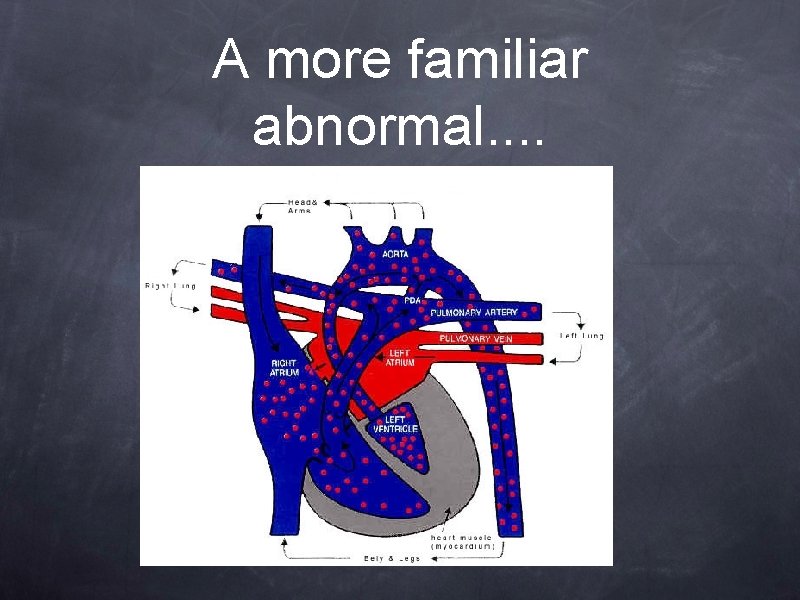
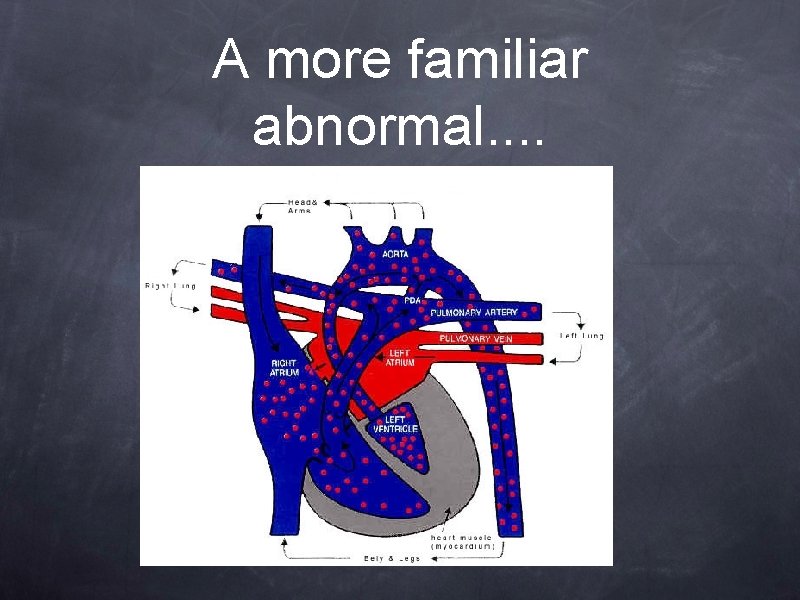
A more familiar abnormal. .
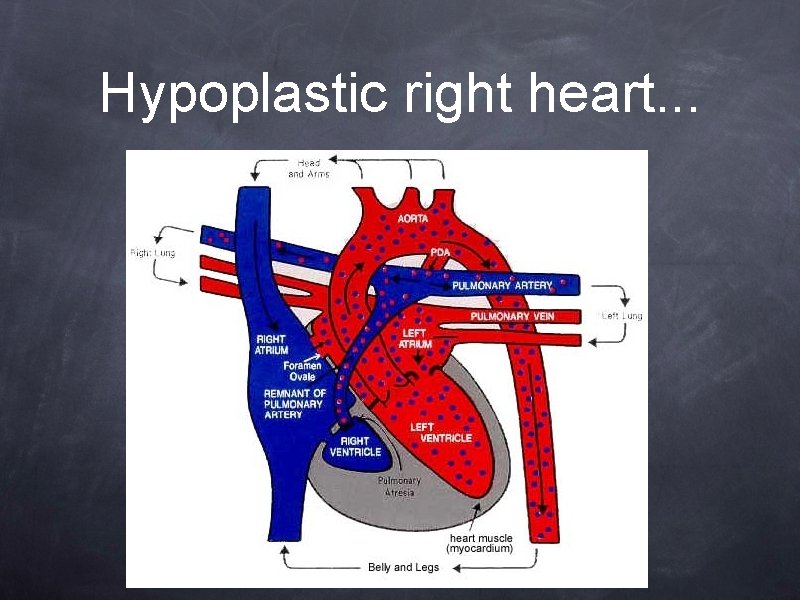
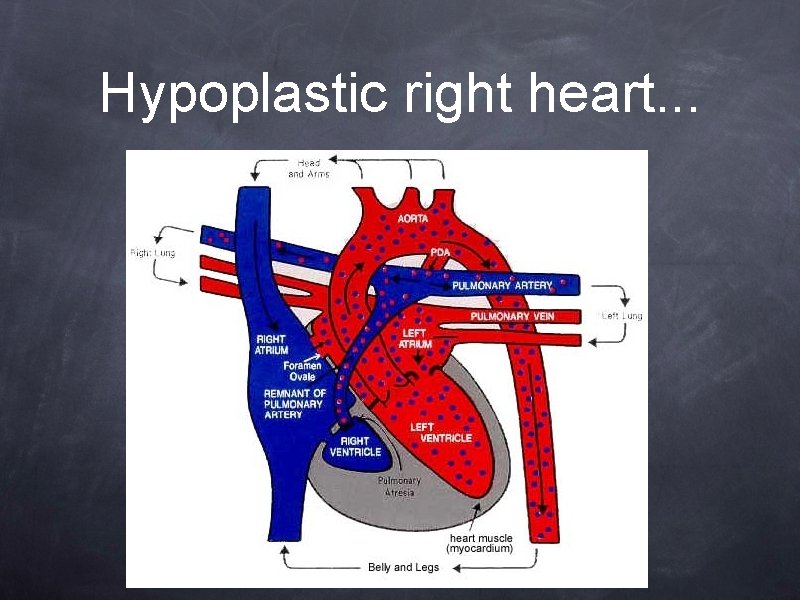
Hypoplastic right heart. . .
Components of PA. IVS Pulmonic atresia Variable degree of right ventricular hypoplasia Interatrial communication always present Varying degrees of tricuspid valve abnormality Coronary artery abnormalities
Pulmonic atresia Exact cause unknown, but occurs late in development Inflammatory/infectious insult speculated Subtle hemodynamic alterations causing left heart loading is another proposed mechanism Varying degrees of abnormality
RV Hypoplasia Hypertrophied wall Reduced cavity size in 90% of cases 5 -10% of cases have enlarged right heart and Ebstein’s anomaly Unipartite, bipartite, or tripartite RV (controversial)
Tricuspid abnormality Typically expressed as Z score 85% are -2 to -5 SD below mean Average Z = -2. 2 Correlated with RV size Functionally regurgitant (severe in 25%)
Interatrial connection True secundum ASD in 20% Patent PFO in the rest Can be restrictive 5 -10% of the time
Coronary artery abnormalities Persistent right ventricular sinusoids, which may have fistulae to the coronary arteries Presence inversely related to TV diameter, RV cavity size, and degree of TI; correlates directly with RV systolic pressure Coronary circulation can be dependent on these communications, due to coronary artery stenoses (20%)
Pathophysiology Natural history is hypoxia, acidosis, early death (weeks to months) Maintenance of PDA critical initial step LV is overloaded, and pumps mixed blood Can have myocardial ischemia, depending on degree of coronary artery anomaly
Management Cardiac cath to assess coronary arteries If complete myocardial dependence on RV, consensus to avoid decompression Management algorithm is complicated beyond that
Possible repairs “two ventricle repair” – repaired RVOT, conventional physiology “one ventricle repair” (Fontan circulation) -passive systemic venous return to pulmonary arteries, bypassing the heart “one and a half ventricle repair” – RVOT repair + bidirectional Glenn
Management Strategy • After stabilization, initial procedure will be RVOT procedure and/or BT shunt – reassess at 3 -6 mo. • Subsequent procedures may include bidirectional Glenn +/- ASD modification • Fontan at 1 -4 years if single ventricle repair is planned
Radiology’s role All available literature describes combination of echo and angiography in workup of PA. IVS -- CT and MR may have future role TV annular size, coronary arteries are most important TV regurgitant fraction, RV chamber size, morphology, growth Post procedure flow dynamics?
References • Reddy VM and Hanley FL. “Pulmonary Atresia with Intact Ventricular Septum. ” Glenn’s Thoracic and Cardiovascular Surgery. Baue AE (ed). Appleton and Lange, 1996: 1315 -1332. • Mi YP et al. Evolution of the management approach for pulmonary atresia with intact ventricular septum. Heart 2005; 91: 657 -663 • Salvin JW et al. Fetal tricuspid valve size and growth as predictors of outcome in pulmonary atresia with intact ventricular septum. Pediatrics 2006 118(2): e 415 -e 420 • Bichell DP. Evaluation and management of pulmonary atresia with intact ventricular septum. Current Opinion in Cardiology. 1999; 14(1): 60 -66
• Humpl T et al. Percutaneous balloon valvotomy in pulmonary atresia with intact ventricular setpum: impact on patient care. Circulation 2003; 108(7): 826832 • Jahangiri M et al. Improved results with selective management in pulmonary atresia with intact ventricular septum. J of Thoracic and Cardiovascular Surgery. 1999; 118: 1046 -1052 • Rychik J et al. Outcome after operations for pulmonary atresia with intact ventricular septum. J of Thoracic and Cardiovascular Surgery. 1998; 116: 924 -931
 Ali sepahdari
Ali sepahdari Tubes of the heart
Tubes of the heart Intact extensor mechanism
Intact extensor mechanism Polynepritis
Polynepritis Intact reality testing
Intact reality testing Non-intact
Non-intact Intact dentition
Intact dentition Follicle atresia
Follicle atresia Meconium ileus
Meconium ileus Lp atresia ani 2020
Lp atresia ani 2020 Types of ileal atresia
Types of ileal atresia Atresia pulmonar
Atresia pulmonar Hydrohepatosis definition
Hydrohepatosis definition Nrga in echo
Nrga in echo Atresia auris
Atresia auris Intestinal obstruction dynamic and adynamic
Intestinal obstruction dynamic and adynamic Atresia esofagica clasificacion
Atresia esofagica clasificacion Classificação de gross atresia de esôfago
Classificação de gross atresia de esôfago Atresia of salivary gland
Atresia of salivary gland Tubérculo de darwin
Tubérculo de darwin Congenital anomaly
Congenital anomaly Dr piplani
Dr piplani